User login
AMA delegates decry ICD-10, EHRs
CHICAGO – Coding and computers were among key concerns for physician leaders at the American Medical Association’s annual House of Delegates meeting.
Resolutions from several delegations aimed to delay or scuttle the transition to the newest incarnation of the International Classification of Diseases, ICD-10.
Delegates from the American College of Rheumatology (ACR) introduced a resolution urging the association to keep up its campaign to stop ICD-10 implementation, specifically via federal legislation.
Without a statement supporting delay, there is a "perception out there that the AMA has essentially caved on the issue of ICD-10," said ACR delegate Dr. Gary Bryant . "Now that’s not my perception, but I believe it’s the perception, to some degree, among American physicians."
The House adopted instead a resolution calling for the AMA to support federal legislation to delay ICD-10 implementation for 2 years. During that time, payers would not be allowed to deny payment based on the specificity of the diagnosis, but they would be required to provide feedback in the case of an incorrect diagnosis. The resolution was brought by the Colorado delegation.
Dr. Reid Blackwelder, president-elect of the American Academy of Family Physicians, spoke in favor of the resolution.
"It’s not likely that we’re moving from ICD-9, we are." Instead, the resolution "allows our members to have a period of time to get used to the sticker shock," he said.
Another issue is that "ICD-10 initially came into use in 1994 and was never designed to be computer-savvy. ICD-11 is due in 2015, and will be designed to be easily coded by computer software," said Dr. Peter Kaufman, the AGA’s delegate to AMA. "If we go to ICD-10 in 2014, or even 2016, when will we be able to go to the newer, more appropriate 11th Revision?"
The AMA has estimated that the cost of implementing ICD-10 could range from $83,290 to more than $2.7 million per practice, depending on practice size.
Delegates cited major problems with electronic health record interoperability, and some also sought to slow the adoption of electronic health records.
Karthik Sarmah medical student alternate delegate in the California delegation, cited interoperability as a major concern.
"The lack of interoperability is the primary driver of why so many people in this room hate their EHR system," he said, adding that interoperability standards exist, but that there are no incentives for venders to create ways to allow physicians to share their patient data with each other.
Dr. Melissa Garretson, a delegate from the American Academy of Pediatrics, agreed.
"I can’t tell you the number of times I have to repeat labs," and CT scans because data can’t be accessed from other physicians, Dr. Garretson said. She called the lack of interoperability an unfunded mandate on physicians because the vendors aren’t making it possible. "If we force them to do this through legislation, it will finally happen."
Kaufman testified \"there are strong interoperability standards already out there. They may only cover limited amounts of data but they work between programs well. The problem is that while they were required when EHRs were certified by CCHIT, with the advent of Meaningful Use, that requirement to use the same specific standard was no longer mandatory.\" Kaufman went on to state that the standards committees were woefully short of practicing physicians, and called for doctors to join the process to the standards could be completed and be workable for clinicians.
Other delegates were skeptical.
"I have been waiting now for about 12 years for this interoperability to occur and I think I’ll either be retired or dead before it finally does," said Dr. Arthur E. Palamara, a vascular surgeon with the Florida delegation.
The House approved a resolution "seeking legislation or regulation to require all EHR vendors to utilize standard and interoperable software technology to enable cost efficient use of electronic health records across all health care delivery systems including institutional and community based settings of care delivery."
On Twitter @aliciaault
CHICAGO – Coding and computers were among key concerns for physician leaders at the American Medical Association’s annual House of Delegates meeting.
Resolutions from several delegations aimed to delay or scuttle the transition to the newest incarnation of the International Classification of Diseases, ICD-10.
Delegates from the American College of Rheumatology (ACR) introduced a resolution urging the association to keep up its campaign to stop ICD-10 implementation, specifically via federal legislation.
Without a statement supporting delay, there is a "perception out there that the AMA has essentially caved on the issue of ICD-10," said ACR delegate Dr. Gary Bryant . "Now that’s not my perception, but I believe it’s the perception, to some degree, among American physicians."
The House adopted instead a resolution calling for the AMA to support federal legislation to delay ICD-10 implementation for 2 years. During that time, payers would not be allowed to deny payment based on the specificity of the diagnosis, but they would be required to provide feedback in the case of an incorrect diagnosis. The resolution was brought by the Colorado delegation.
Dr. Reid Blackwelder, president-elect of the American Academy of Family Physicians, spoke in favor of the resolution.
"It’s not likely that we’re moving from ICD-9, we are." Instead, the resolution "allows our members to have a period of time to get used to the sticker shock," he said.
Another issue is that "ICD-10 initially came into use in 1994 and was never designed to be computer-savvy. ICD-11 is due in 2015, and will be designed to be easily coded by computer software," said Dr. Peter Kaufman, the AGA’s delegate to AMA. "If we go to ICD-10 in 2014, or even 2016, when will we be able to go to the newer, more appropriate 11th Revision?"
The AMA has estimated that the cost of implementing ICD-10 could range from $83,290 to more than $2.7 million per practice, depending on practice size.
Delegates cited major problems with electronic health record interoperability, and some also sought to slow the adoption of electronic health records.
Karthik Sarmah medical student alternate delegate in the California delegation, cited interoperability as a major concern.
"The lack of interoperability is the primary driver of why so many people in this room hate their EHR system," he said, adding that interoperability standards exist, but that there are no incentives for venders to create ways to allow physicians to share their patient data with each other.
Dr. Melissa Garretson, a delegate from the American Academy of Pediatrics, agreed.
"I can’t tell you the number of times I have to repeat labs," and CT scans because data can’t be accessed from other physicians, Dr. Garretson said. She called the lack of interoperability an unfunded mandate on physicians because the vendors aren’t making it possible. "If we force them to do this through legislation, it will finally happen."
Kaufman testified \"there are strong interoperability standards already out there. They may only cover limited amounts of data but they work between programs well. The problem is that while they were required when EHRs were certified by CCHIT, with the advent of Meaningful Use, that requirement to use the same specific standard was no longer mandatory.\" Kaufman went on to state that the standards committees were woefully short of practicing physicians, and called for doctors to join the process to the standards could be completed and be workable for clinicians.
Other delegates were skeptical.
"I have been waiting now for about 12 years for this interoperability to occur and I think I’ll either be retired or dead before it finally does," said Dr. Arthur E. Palamara, a vascular surgeon with the Florida delegation.
The House approved a resolution "seeking legislation or regulation to require all EHR vendors to utilize standard and interoperable software technology to enable cost efficient use of electronic health records across all health care delivery systems including institutional and community based settings of care delivery."
On Twitter @aliciaault
CHICAGO – Coding and computers were among key concerns for physician leaders at the American Medical Association’s annual House of Delegates meeting.
Resolutions from several delegations aimed to delay or scuttle the transition to the newest incarnation of the International Classification of Diseases, ICD-10.
Delegates from the American College of Rheumatology (ACR) introduced a resolution urging the association to keep up its campaign to stop ICD-10 implementation, specifically via federal legislation.
Without a statement supporting delay, there is a "perception out there that the AMA has essentially caved on the issue of ICD-10," said ACR delegate Dr. Gary Bryant . "Now that’s not my perception, but I believe it’s the perception, to some degree, among American physicians."
The House adopted instead a resolution calling for the AMA to support federal legislation to delay ICD-10 implementation for 2 years. During that time, payers would not be allowed to deny payment based on the specificity of the diagnosis, but they would be required to provide feedback in the case of an incorrect diagnosis. The resolution was brought by the Colorado delegation.
Dr. Reid Blackwelder, president-elect of the American Academy of Family Physicians, spoke in favor of the resolution.
"It’s not likely that we’re moving from ICD-9, we are." Instead, the resolution "allows our members to have a period of time to get used to the sticker shock," he said.
Another issue is that "ICD-10 initially came into use in 1994 and was never designed to be computer-savvy. ICD-11 is due in 2015, and will be designed to be easily coded by computer software," said Dr. Peter Kaufman, the AGA’s delegate to AMA. "If we go to ICD-10 in 2014, or even 2016, when will we be able to go to the newer, more appropriate 11th Revision?"
The AMA has estimated that the cost of implementing ICD-10 could range from $83,290 to more than $2.7 million per practice, depending on practice size.
Delegates cited major problems with electronic health record interoperability, and some also sought to slow the adoption of electronic health records.
Karthik Sarmah medical student alternate delegate in the California delegation, cited interoperability as a major concern.
"The lack of interoperability is the primary driver of why so many people in this room hate their EHR system," he said, adding that interoperability standards exist, but that there are no incentives for venders to create ways to allow physicians to share their patient data with each other.
Dr. Melissa Garretson, a delegate from the American Academy of Pediatrics, agreed.
"I can’t tell you the number of times I have to repeat labs," and CT scans because data can’t be accessed from other physicians, Dr. Garretson said. She called the lack of interoperability an unfunded mandate on physicians because the vendors aren’t making it possible. "If we force them to do this through legislation, it will finally happen."
Kaufman testified \"there are strong interoperability standards already out there. They may only cover limited amounts of data but they work between programs well. The problem is that while they were required when EHRs were certified by CCHIT, with the advent of Meaningful Use, that requirement to use the same specific standard was no longer mandatory.\" Kaufman went on to state that the standards committees were woefully short of practicing physicians, and called for doctors to join the process to the standards could be completed and be workable for clinicians.
Other delegates were skeptical.
"I have been waiting now for about 12 years for this interoperability to occur and I think I’ll either be retired or dead before it finally does," said Dr. Arthur E. Palamara, a vascular surgeon with the Florida delegation.
The House approved a resolution "seeking legislation or regulation to require all EHR vendors to utilize standard and interoperable software technology to enable cost efficient use of electronic health records across all health care delivery systems including institutional and community based settings of care delivery."
On Twitter @aliciaault
AT THE AMA HOUSE OF DELEGATES
Kennedy seeks to unite mental health advocates with new foundation
Former congressman Patrick Kennedy has started a new organization that aims to bring mental health advocates together.
Mr. Kennedy, who represented Rhode Island in the House of Representatives from 1995 to 2011, was a coauthor of the 2008 Mental Health Parity and Addiction Equity Act (MHPAEA). The act requires that companies with more that 50 employees provide group health insurance that includes mental health/substance abuse benefits equivalent to medical/surgical benefits at no additional charge. Mr. Kennedy also has spoken at length about his personal struggles with bipolar disorder and addiction.
In debuting the Kennedy Forum – and an inaugural conference in Boston in October – Mr. Kennedy said in a statement, "We need a national conversation on mental health that will allow us to finally remove the stigma surrounding mental illness and to once-and-for-all achieve parity by treating the brain the same way we treat the rest of the body. I look forward to bringing together the brightest minds and boldest voices in the mental health, substance use, and intellectual disability community for this annual event."
Mr. Kennedy also noted that the final rules implementing the 2008 law are due this fall. Interim final rules were released in January 2010 and have been applied to health coverage that began July 1 of that year. A few months later, several behavioral health companies – Magellan Health Services, Beacon Health Strategies, and ValueOptions – filed suit to delay implementation of the final rule, seeking further clarity on how the 2008 law would mesh with the Affordable Care Act.
Last March, the Obama administration gave a little bit more insight into how those laws might interact when it spelled out the ACA’s essential health benefits. The final rule for that aspect of the act emphasized that health insurers must cover mental health and substance abuse services starting in 2014. The essential health benefit rule also broadened the parity requirement for mental health coverage, first established under the MHPAEA.
On Twitter @aliciaault
Former congressman Patrick Kennedy has started a new organization that aims to bring mental health advocates together.
Mr. Kennedy, who represented Rhode Island in the House of Representatives from 1995 to 2011, was a coauthor of the 2008 Mental Health Parity and Addiction Equity Act (MHPAEA). The act requires that companies with more that 50 employees provide group health insurance that includes mental health/substance abuse benefits equivalent to medical/surgical benefits at no additional charge. Mr. Kennedy also has spoken at length about his personal struggles with bipolar disorder and addiction.
In debuting the Kennedy Forum – and an inaugural conference in Boston in October – Mr. Kennedy said in a statement, "We need a national conversation on mental health that will allow us to finally remove the stigma surrounding mental illness and to once-and-for-all achieve parity by treating the brain the same way we treat the rest of the body. I look forward to bringing together the brightest minds and boldest voices in the mental health, substance use, and intellectual disability community for this annual event."
Mr. Kennedy also noted that the final rules implementing the 2008 law are due this fall. Interim final rules were released in January 2010 and have been applied to health coverage that began July 1 of that year. A few months later, several behavioral health companies – Magellan Health Services, Beacon Health Strategies, and ValueOptions – filed suit to delay implementation of the final rule, seeking further clarity on how the 2008 law would mesh with the Affordable Care Act.
Last March, the Obama administration gave a little bit more insight into how those laws might interact when it spelled out the ACA’s essential health benefits. The final rule for that aspect of the act emphasized that health insurers must cover mental health and substance abuse services starting in 2014. The essential health benefit rule also broadened the parity requirement for mental health coverage, first established under the MHPAEA.
On Twitter @aliciaault
Former congressman Patrick Kennedy has started a new organization that aims to bring mental health advocates together.
Mr. Kennedy, who represented Rhode Island in the House of Representatives from 1995 to 2011, was a coauthor of the 2008 Mental Health Parity and Addiction Equity Act (MHPAEA). The act requires that companies with more that 50 employees provide group health insurance that includes mental health/substance abuse benefits equivalent to medical/surgical benefits at no additional charge. Mr. Kennedy also has spoken at length about his personal struggles with bipolar disorder and addiction.
In debuting the Kennedy Forum – and an inaugural conference in Boston in October – Mr. Kennedy said in a statement, "We need a national conversation on mental health that will allow us to finally remove the stigma surrounding mental illness and to once-and-for-all achieve parity by treating the brain the same way we treat the rest of the body. I look forward to bringing together the brightest minds and boldest voices in the mental health, substance use, and intellectual disability community for this annual event."
Mr. Kennedy also noted that the final rules implementing the 2008 law are due this fall. Interim final rules were released in January 2010 and have been applied to health coverage that began July 1 of that year. A few months later, several behavioral health companies – Magellan Health Services, Beacon Health Strategies, and ValueOptions – filed suit to delay implementation of the final rule, seeking further clarity on how the 2008 law would mesh with the Affordable Care Act.
Last March, the Obama administration gave a little bit more insight into how those laws might interact when it spelled out the ACA’s essential health benefits. The final rule for that aspect of the act emphasized that health insurers must cover mental health and substance abuse services starting in 2014. The essential health benefit rule also broadened the parity requirement for mental health coverage, first established under the MHPAEA.
On Twitter @aliciaault
Doctors: Major responsibility for cost control is not ours
When it comes to reducing health costs, physicians believe burden of responsibility lies primarily with plaintiffs attorneys, followed by insurers, hospitals, drug and device makers, patients, and, lastly, themselves.
Those conclusions are based on 2,438 responses from some 3,900 physicians randomly surveyed in 2012. Dr. Jon C. Tilburt of the Mayo Clinic, Rochester, Minn., and his colleagues reported their findings July 23 in JAMA.
When asked whether individual physicians should have a major responsibility in reducing health costs, 36% of respondents said yes. Sixty percent said that trial lawyers bore the major burden, with health insurers coming in a close second.
More than half said that drug and device companies, hospitals and health systems, and patients also should have major responsibility for cost containment. A total of 44% said the government had that responsibility (JAMA 2013;310:380-8 [doi:10.1001/jama.2013.8278]).
Physicians also were asked about their enthusiasm for various cost-control strategies and to examine their own role in cost containment by assessing their knowledge of prices of procedures and tests and their desire to personally curb costs in their practice. The authors asked about and analyzed potential barriers to physicians becoming more cost conscious, as well.
Doctors were very enthusiastic about improving the quality and efficiency of care, primarily through promoting continuity of care and going after fraud and abuse. Expanding access to preventive care was also warmly received. Physicians were also enthusiastic about limiting access to expensive treatments that had shown little benefit, using cost-effectiveness data to choose a therapy, and promoting head-to-head trials of competing therapies.
Just over half of respondents said that cutting pay for the highest-paid specialists should be embraced.
Eliminating fee for service altogether was rejected by 70% of respondents. Ninety percent said that they weren’t enthusiastic about letting the Medicare Sustainable Growth Rate cuts take effect. Two-thirds said that bundled pay and penalties for readmissions – both cost-control keystones advanced by the Obama administration – were not attractive.
Not surprisingly, increasing use of electronic health records also got a strong negative response, with 29% saying they were "not enthusiastic."
When it came to their own practice, 76% said they were aware of the costs of treatments or tests they recommended, and 84% said that cost is important whether a patient pays out of pocket or not.
When it comes to individual physicians’ responsibility for reducing health costs, the responses were very mixed.
The survey participants largely agreed that "trying to contain costs is the responsibility of every physician" (85%) and that physicians should take a more prominent role in eliminating unnecessary tests (89%). But by almost the same percentages, physicians also said that they should be devoted to their individual patients, even if a test or therapy was expensive, and that they should not deny services to their patients because someone else might need it more.
"This apparent inconsistency may reflect inherent tensions in professional roles to serve patients individually and society as a whole," Dr. Tilburt and colleagues wrote.
Finally, physicians overwhelmingly said that fear of malpractice had substantially decreased their enjoyment of practicing medicine. The authors rated that fear as a barrier to cost-conscious practice. They also found that 43% of physicians admitted they ordered more tests when they did not know the patient as well. Half said that being more cost conscious was the right thing to do, but large numbers said that it might not make a difference or could make things worse. A total of 40% said it would not limit unreasonable patient demands, and 28% said it could erode patients’ trust.
Dr. Tilburt and his colleagues pointed out that the findings should be viewed with caution in part because it could not fully reflect the opinions of all American physicians. Further, opinions could be in flux, given how much has changed since even a year ago.
They suggested that policy makers move slowly when it comes to changing payment models, and instead target areas where doctors seem to be enthusiastic, including improving quality of care and using comparative effectiveness data.
The study was funded by the Greenwall Foundation and the Mayo Clinic. The authors reported having no financial conflicts.
On Twitter @aliciaault
If there was ever an "all-hands-on-deck" moment in the history of health care, that moment is now. The findings of this study suggest that physician do not yet have the mentality this historical moment demands. Indeed, this survey suggests that in the face of this new and uncertain moment in the reform of the health care system, physicians are lapsing into the well-known, cautious, instinctual approaches humans adopt whenever confronted by uncertainty: Blame others and persevere with "business as usual."
Physicians have moved beyond denying that health care costs are a problem. Yet, they are not quite willing to accept physicians’ primary responsibility and take action. The study findings suggest that physicians are ambivalent; they reject transformative solutions, such as eliminating fee-for-service or bundled payments, which address the seriousness of the cost problem.
This study by Tilburt et al. indicates that the medical profession is not there yet – that many physicians would prefer to sit on the sidelines while other actors in the health care system do the real work of reform.
This could marginalize and demote physicians.
Dr. Ezekiel J. Emanuel is an ethicist at the University of Pennsylvania, Philadelphia. He reported no related conflicts. These remarks were taken from an editorial accompanying Dr. Tilburt’s study.(JAMA 2013;310:374-5)
If there was ever an "all-hands-on-deck" moment in the history of health care, that moment is now. The findings of this study suggest that physician do not yet have the mentality this historical moment demands. Indeed, this survey suggests that in the face of this new and uncertain moment in the reform of the health care system, physicians are lapsing into the well-known, cautious, instinctual approaches humans adopt whenever confronted by uncertainty: Blame others and persevere with "business as usual."
Physicians have moved beyond denying that health care costs are a problem. Yet, they are not quite willing to accept physicians’ primary responsibility and take action. The study findings suggest that physicians are ambivalent; they reject transformative solutions, such as eliminating fee-for-service or bundled payments, which address the seriousness of the cost problem.
This study by Tilburt et al. indicates that the medical profession is not there yet – that many physicians would prefer to sit on the sidelines while other actors in the health care system do the real work of reform.
This could marginalize and demote physicians.
Dr. Ezekiel J. Emanuel is an ethicist at the University of Pennsylvania, Philadelphia. He reported no related conflicts. These remarks were taken from an editorial accompanying Dr. Tilburt’s study.(JAMA 2013;310:374-5)
If there was ever an "all-hands-on-deck" moment in the history of health care, that moment is now. The findings of this study suggest that physician do not yet have the mentality this historical moment demands. Indeed, this survey suggests that in the face of this new and uncertain moment in the reform of the health care system, physicians are lapsing into the well-known, cautious, instinctual approaches humans adopt whenever confronted by uncertainty: Blame others and persevere with "business as usual."
Physicians have moved beyond denying that health care costs are a problem. Yet, they are not quite willing to accept physicians’ primary responsibility and take action. The study findings suggest that physicians are ambivalent; they reject transformative solutions, such as eliminating fee-for-service or bundled payments, which address the seriousness of the cost problem.
This study by Tilburt et al. indicates that the medical profession is not there yet – that many physicians would prefer to sit on the sidelines while other actors in the health care system do the real work of reform.
This could marginalize and demote physicians.
Dr. Ezekiel J. Emanuel is an ethicist at the University of Pennsylvania, Philadelphia. He reported no related conflicts. These remarks were taken from an editorial accompanying Dr. Tilburt’s study.(JAMA 2013;310:374-5)
When it comes to reducing health costs, physicians believe burden of responsibility lies primarily with plaintiffs attorneys, followed by insurers, hospitals, drug and device makers, patients, and, lastly, themselves.
Those conclusions are based on 2,438 responses from some 3,900 physicians randomly surveyed in 2012. Dr. Jon C. Tilburt of the Mayo Clinic, Rochester, Minn., and his colleagues reported their findings July 23 in JAMA.
When asked whether individual physicians should have a major responsibility in reducing health costs, 36% of respondents said yes. Sixty percent said that trial lawyers bore the major burden, with health insurers coming in a close second.
More than half said that drug and device companies, hospitals and health systems, and patients also should have major responsibility for cost containment. A total of 44% said the government had that responsibility (JAMA 2013;310:380-8 [doi:10.1001/jama.2013.8278]).
Physicians also were asked about their enthusiasm for various cost-control strategies and to examine their own role in cost containment by assessing their knowledge of prices of procedures and tests and their desire to personally curb costs in their practice. The authors asked about and analyzed potential barriers to physicians becoming more cost conscious, as well.
Doctors were very enthusiastic about improving the quality and efficiency of care, primarily through promoting continuity of care and going after fraud and abuse. Expanding access to preventive care was also warmly received. Physicians were also enthusiastic about limiting access to expensive treatments that had shown little benefit, using cost-effectiveness data to choose a therapy, and promoting head-to-head trials of competing therapies.
Just over half of respondents said that cutting pay for the highest-paid specialists should be embraced.
Eliminating fee for service altogether was rejected by 70% of respondents. Ninety percent said that they weren’t enthusiastic about letting the Medicare Sustainable Growth Rate cuts take effect. Two-thirds said that bundled pay and penalties for readmissions – both cost-control keystones advanced by the Obama administration – were not attractive.
Not surprisingly, increasing use of electronic health records also got a strong negative response, with 29% saying they were "not enthusiastic."
When it came to their own practice, 76% said they were aware of the costs of treatments or tests they recommended, and 84% said that cost is important whether a patient pays out of pocket or not.
When it comes to individual physicians’ responsibility for reducing health costs, the responses were very mixed.
The survey participants largely agreed that "trying to contain costs is the responsibility of every physician" (85%) and that physicians should take a more prominent role in eliminating unnecessary tests (89%). But by almost the same percentages, physicians also said that they should be devoted to their individual patients, even if a test or therapy was expensive, and that they should not deny services to their patients because someone else might need it more.
"This apparent inconsistency may reflect inherent tensions in professional roles to serve patients individually and society as a whole," Dr. Tilburt and colleagues wrote.
Finally, physicians overwhelmingly said that fear of malpractice had substantially decreased their enjoyment of practicing medicine. The authors rated that fear as a barrier to cost-conscious practice. They also found that 43% of physicians admitted they ordered more tests when they did not know the patient as well. Half said that being more cost conscious was the right thing to do, but large numbers said that it might not make a difference or could make things worse. A total of 40% said it would not limit unreasonable patient demands, and 28% said it could erode patients’ trust.
Dr. Tilburt and his colleagues pointed out that the findings should be viewed with caution in part because it could not fully reflect the opinions of all American physicians. Further, opinions could be in flux, given how much has changed since even a year ago.
They suggested that policy makers move slowly when it comes to changing payment models, and instead target areas where doctors seem to be enthusiastic, including improving quality of care and using comparative effectiveness data.
The study was funded by the Greenwall Foundation and the Mayo Clinic. The authors reported having no financial conflicts.
On Twitter @aliciaault
When it comes to reducing health costs, physicians believe burden of responsibility lies primarily with plaintiffs attorneys, followed by insurers, hospitals, drug and device makers, patients, and, lastly, themselves.
Those conclusions are based on 2,438 responses from some 3,900 physicians randomly surveyed in 2012. Dr. Jon C. Tilburt of the Mayo Clinic, Rochester, Minn., and his colleagues reported their findings July 23 in JAMA.
When asked whether individual physicians should have a major responsibility in reducing health costs, 36% of respondents said yes. Sixty percent said that trial lawyers bore the major burden, with health insurers coming in a close second.
More than half said that drug and device companies, hospitals and health systems, and patients also should have major responsibility for cost containment. A total of 44% said the government had that responsibility (JAMA 2013;310:380-8 [doi:10.1001/jama.2013.8278]).
Physicians also were asked about their enthusiasm for various cost-control strategies and to examine their own role in cost containment by assessing their knowledge of prices of procedures and tests and their desire to personally curb costs in their practice. The authors asked about and analyzed potential barriers to physicians becoming more cost conscious, as well.
Doctors were very enthusiastic about improving the quality and efficiency of care, primarily through promoting continuity of care and going after fraud and abuse. Expanding access to preventive care was also warmly received. Physicians were also enthusiastic about limiting access to expensive treatments that had shown little benefit, using cost-effectiveness data to choose a therapy, and promoting head-to-head trials of competing therapies.
Just over half of respondents said that cutting pay for the highest-paid specialists should be embraced.
Eliminating fee for service altogether was rejected by 70% of respondents. Ninety percent said that they weren’t enthusiastic about letting the Medicare Sustainable Growth Rate cuts take effect. Two-thirds said that bundled pay and penalties for readmissions – both cost-control keystones advanced by the Obama administration – were not attractive.
Not surprisingly, increasing use of electronic health records also got a strong negative response, with 29% saying they were "not enthusiastic."
When it came to their own practice, 76% said they were aware of the costs of treatments or tests they recommended, and 84% said that cost is important whether a patient pays out of pocket or not.
When it comes to individual physicians’ responsibility for reducing health costs, the responses were very mixed.
The survey participants largely agreed that "trying to contain costs is the responsibility of every physician" (85%) and that physicians should take a more prominent role in eliminating unnecessary tests (89%). But by almost the same percentages, physicians also said that they should be devoted to their individual patients, even if a test or therapy was expensive, and that they should not deny services to their patients because someone else might need it more.
"This apparent inconsistency may reflect inherent tensions in professional roles to serve patients individually and society as a whole," Dr. Tilburt and colleagues wrote.
Finally, physicians overwhelmingly said that fear of malpractice had substantially decreased their enjoyment of practicing medicine. The authors rated that fear as a barrier to cost-conscious practice. They also found that 43% of physicians admitted they ordered more tests when they did not know the patient as well. Half said that being more cost conscious was the right thing to do, but large numbers said that it might not make a difference or could make things worse. A total of 40% said it would not limit unreasonable patient demands, and 28% said it could erode patients’ trust.
Dr. Tilburt and his colleagues pointed out that the findings should be viewed with caution in part because it could not fully reflect the opinions of all American physicians. Further, opinions could be in flux, given how much has changed since even a year ago.
They suggested that policy makers move slowly when it comes to changing payment models, and instead target areas where doctors seem to be enthusiastic, including improving quality of care and using comparative effectiveness data.
The study was funded by the Greenwall Foundation and the Mayo Clinic. The authors reported having no financial conflicts.
On Twitter @aliciaault
FROM JAMA
Major finding: Sixty percent of responding physicians believe that trial attorneys bear major responsibility for reducing health costs.
Data source: A random survey of 3,900 physicians.
Disclosures: The study was funded by the Greenwall Foundation and the Mayo Clinic. The authors reported having no financial conflicts.
Sunshine apps track industry payments
Two new smartphone apps aim to help log drug, device, and diagnostic manufacturer payments to doctors and health care providers, as called for by the Affordable Care Act.
To promote transparency in relationships between providers and industry, the ACA requires that manufacturers track and report payments for consulting, honoraria, and more.
Originally known as the Sunshine Act, the effort is now called the Open Payments Program by the Centers for Medicare and Medicaid Services (CMS).
While physicians are not required to inventory anything of value they receive from manufacturers, CMS and many medical professional societies advise that they do so.
The app for physicians – Open Payments for Physicians – is designed to help doctors keep tabs on all their transactions in real time. Users can manually enter all the information regarding a particular transaction, for example, the receipt of a grant payment or a gift that’s worth more than $10.
The app is free and can be downloaded from the iTunes App Store or from Google Play.
CMS also created an app for industry representatives to use (Open Payments for Industry).
Industry users and physician users can exchange information with their apps. By using a built-in QR (quick response) code reader, the manufacturer can transfer a record of a transaction to the physician for review, according to the agency.
In a blog post, CMS Program Integrity Director Dr. Peter Budetti said the agency’s "foray into mobile technology is about providing user-friendly tools for doctors, manufacturers, and others in the health care industry to use in working with us to implement the law in a smart way."
The idea is that physicians can use the records contained in the app to compare what’s reported by manufacturers to CMS. There is a 45-day lag between when the data are reported to CMS and posted publicly. Physicians have that window to challenge the reports before they are posted on the Open Payments website. Corrections can be made later, but the erroneous data will likely stay public for awhile.
The first year of the program will be a little bit more forgiving. Data collected beginning Aug. 1 won’t be publicly reported until September 2014.
The apps can’t be used to directly transfer data to CMS, said the agency, which added that although it developed the apps, it will not "validate the accuracy of data stored in the apps, nor will it be responsible for protecting data stored in the apps."
aault@frontlinemedcom.com On Twitter @aliciaault
Two new smartphone apps aim to help log drug, device, and diagnostic manufacturer payments to doctors and health care providers, as called for by the Affordable Care Act.
To promote transparency in relationships between providers and industry, the ACA requires that manufacturers track and report payments for consulting, honoraria, and more.
Originally known as the Sunshine Act, the effort is now called the Open Payments Program by the Centers for Medicare and Medicaid Services (CMS).
While physicians are not required to inventory anything of value they receive from manufacturers, CMS and many medical professional societies advise that they do so.
The app for physicians – Open Payments for Physicians – is designed to help doctors keep tabs on all their transactions in real time. Users can manually enter all the information regarding a particular transaction, for example, the receipt of a grant payment or a gift that’s worth more than $10.
The app is free and can be downloaded from the iTunes App Store or from Google Play.
CMS also created an app for industry representatives to use (Open Payments for Industry).
Industry users and physician users can exchange information with their apps. By using a built-in QR (quick response) code reader, the manufacturer can transfer a record of a transaction to the physician for review, according to the agency.
In a blog post, CMS Program Integrity Director Dr. Peter Budetti said the agency’s "foray into mobile technology is about providing user-friendly tools for doctors, manufacturers, and others in the health care industry to use in working with us to implement the law in a smart way."
The idea is that physicians can use the records contained in the app to compare what’s reported by manufacturers to CMS. There is a 45-day lag between when the data are reported to CMS and posted publicly. Physicians have that window to challenge the reports before they are posted on the Open Payments website. Corrections can be made later, but the erroneous data will likely stay public for awhile.
The first year of the program will be a little bit more forgiving. Data collected beginning Aug. 1 won’t be publicly reported until September 2014.
The apps can’t be used to directly transfer data to CMS, said the agency, which added that although it developed the apps, it will not "validate the accuracy of data stored in the apps, nor will it be responsible for protecting data stored in the apps."
aault@frontlinemedcom.com On Twitter @aliciaault
Two new smartphone apps aim to help log drug, device, and diagnostic manufacturer payments to doctors and health care providers, as called for by the Affordable Care Act.
To promote transparency in relationships between providers and industry, the ACA requires that manufacturers track and report payments for consulting, honoraria, and more.
Originally known as the Sunshine Act, the effort is now called the Open Payments Program by the Centers for Medicare and Medicaid Services (CMS).
While physicians are not required to inventory anything of value they receive from manufacturers, CMS and many medical professional societies advise that they do so.
The app for physicians – Open Payments for Physicians – is designed to help doctors keep tabs on all their transactions in real time. Users can manually enter all the information regarding a particular transaction, for example, the receipt of a grant payment or a gift that’s worth more than $10.
The app is free and can be downloaded from the iTunes App Store or from Google Play.
CMS also created an app for industry representatives to use (Open Payments for Industry).
Industry users and physician users can exchange information with their apps. By using a built-in QR (quick response) code reader, the manufacturer can transfer a record of a transaction to the physician for review, according to the agency.
In a blog post, CMS Program Integrity Director Dr. Peter Budetti said the agency’s "foray into mobile technology is about providing user-friendly tools for doctors, manufacturers, and others in the health care industry to use in working with us to implement the law in a smart way."
The idea is that physicians can use the records contained in the app to compare what’s reported by manufacturers to CMS. There is a 45-day lag between when the data are reported to CMS and posted publicly. Physicians have that window to challenge the reports before they are posted on the Open Payments website. Corrections can be made later, but the erroneous data will likely stay public for awhile.
The first year of the program will be a little bit more forgiving. Data collected beginning Aug. 1 won’t be publicly reported until September 2014.
The apps can’t be used to directly transfer data to CMS, said the agency, which added that although it developed the apps, it will not "validate the accuracy of data stored in the apps, nor will it be responsible for protecting data stored in the apps."
aault@frontlinemedcom.com On Twitter @aliciaault
GAO: In-house pathology is a conflict
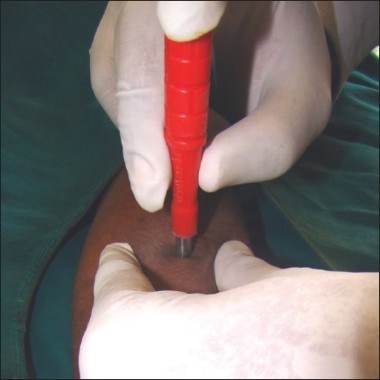
Physicians may be profiting by referring pathology services on biopsies to in-house labs or to pathology labs where they have an ownership stake, according to a report from the Government Accountability Office released July 16.
The agency found that three specialties – dermatology, gastroenterology, and urology – accounted for 90% of the self-referrals in 2010. Dermatologists alone accounted for half of those self-referrals.
The practice is costing Medicare millions and resulting in excess treatments, according to the report. The agency estimated that overall in 2010, self-referring providers likely referred 918,000 more pathology services than did physicians referring to labs in which they did not have a stake. The extra tests cost Medicare about $69 million out of a total $1.28 billion tab paid to physicians, pathologists, and labs in that year.
Overall, from 2004 to 2010, "the number of self-referred anatomic pathology services more than doubled, growing from 1.06 million services to about 2.26 million services, while non–self-referred services grew about 38%, from about 5.64 million services to about 7.77 million services," according to the report.
Self-referring providers include those who have an ownership stake in a clinical lab, but more commonly, those who prepare and/or evaluate specimens in their practices.
Referrals were highest for physicians in the year after they began to self-refer, suggesting that referrals were driven by financial incentives, not by any change in clinical practice or by any demographic change, according to the GAO.
Calling these physicians "switchers," the GAO found a 24% increase in referrals for pathology services among dermatologists who self-referred in 2010, compared to only a 0.3% increase for those who sent biopsy specimens elsewhere.
The GAO conducted its investigation at the request of Rep. Henry A. Waxman (D-Calif.), Rep. Sander Levin (D-Mich.), Sen. Max Baucus (D-Mont.), and Sen. Chuck Grassley (R-Iowa).
"The analysis suggests that financial incentives for self-referring providers is likely a major factor driving the increase in referrals for these services," Rep. Waxman said in a joint statement from the legislators.
"As Congress looks to rein in unnecessary spending, my colleagues and I should explore this area in greater depth," he said.
Sen. Grassley added, "Federal policy should drive doctors to make decisions based on quality of care, not financial relationships. The taxpayers shouldn’t have to pay for services that aren’t medically necessary."
The GAO suggested that the Centers for Medicare and Medicaid Services should require providers to state on claims whether a service was self-referred, and that the agency should limit payment so that physicians aren’t rewarded for higher numbers of specimens per biopsy.
In comments to the GAO on the report, the American Academy of Dermatology Association said that it agreed that the CMS should develop a way to ensure the appropriateness of biopsy procedures. But the AADA expressed concern about limitations on financial incentives, saying that dermatologists should be encouraged to perform biopsies. The AADA also said that dermatologists should be allowed to prepare and review their own specimens "because they receive considerable training as part of their education."
On Twitter @aliciaault
Physicians may be profiting by referring pathology services on biopsies to in-house labs or to pathology labs where they have an ownership stake, according to a report from the Government Accountability Office released July 16.
The agency found that three specialties – dermatology, gastroenterology, and urology – accounted for 90% of the self-referrals in 2010. Dermatologists alone accounted for half of those self-referrals.
The practice is costing Medicare millions and resulting in excess treatments, according to the report. The agency estimated that overall in 2010, self-referring providers likely referred 918,000 more pathology services than did physicians referring to labs in which they did not have a stake. The extra tests cost Medicare about $69 million out of a total $1.28 billion tab paid to physicians, pathologists, and labs in that year.
Overall, from 2004 to 2010, "the number of self-referred anatomic pathology services more than doubled, growing from 1.06 million services to about 2.26 million services, while non–self-referred services grew about 38%, from about 5.64 million services to about 7.77 million services," according to the report.
Self-referring providers include those who have an ownership stake in a clinical lab, but more commonly, those who prepare and/or evaluate specimens in their practices.
Referrals were highest for physicians in the year after they began to self-refer, suggesting that referrals were driven by financial incentives, not by any change in clinical practice or by any demographic change, according to the GAO.
Calling these physicians "switchers," the GAO found a 24% increase in referrals for pathology services among dermatologists who self-referred in 2010, compared to only a 0.3% increase for those who sent biopsy specimens elsewhere.
The GAO conducted its investigation at the request of Rep. Henry A. Waxman (D-Calif.), Rep. Sander Levin (D-Mich.), Sen. Max Baucus (D-Mont.), and Sen. Chuck Grassley (R-Iowa).
"The analysis suggests that financial incentives for self-referring providers is likely a major factor driving the increase in referrals for these services," Rep. Waxman said in a joint statement from the legislators.
"As Congress looks to rein in unnecessary spending, my colleagues and I should explore this area in greater depth," he said.
Sen. Grassley added, "Federal policy should drive doctors to make decisions based on quality of care, not financial relationships. The taxpayers shouldn’t have to pay for services that aren’t medically necessary."
The GAO suggested that the Centers for Medicare and Medicaid Services should require providers to state on claims whether a service was self-referred, and that the agency should limit payment so that physicians aren’t rewarded for higher numbers of specimens per biopsy.
In comments to the GAO on the report, the American Academy of Dermatology Association said that it agreed that the CMS should develop a way to ensure the appropriateness of biopsy procedures. But the AADA expressed concern about limitations on financial incentives, saying that dermatologists should be encouraged to perform biopsies. The AADA also said that dermatologists should be allowed to prepare and review their own specimens "because they receive considerable training as part of their education."
On Twitter @aliciaault
Physicians may be profiting by referring pathology services on biopsies to in-house labs or to pathology labs where they have an ownership stake, according to a report from the Government Accountability Office released July 16.
The agency found that three specialties – dermatology, gastroenterology, and urology – accounted for 90% of the self-referrals in 2010. Dermatologists alone accounted for half of those self-referrals.
The practice is costing Medicare millions and resulting in excess treatments, according to the report. The agency estimated that overall in 2010, self-referring providers likely referred 918,000 more pathology services than did physicians referring to labs in which they did not have a stake. The extra tests cost Medicare about $69 million out of a total $1.28 billion tab paid to physicians, pathologists, and labs in that year.
Overall, from 2004 to 2010, "the number of self-referred anatomic pathology services more than doubled, growing from 1.06 million services to about 2.26 million services, while non–self-referred services grew about 38%, from about 5.64 million services to about 7.77 million services," according to the report.
Self-referring providers include those who have an ownership stake in a clinical lab, but more commonly, those who prepare and/or evaluate specimens in their practices.
Referrals were highest for physicians in the year after they began to self-refer, suggesting that referrals were driven by financial incentives, not by any change in clinical practice or by any demographic change, according to the GAO.
Calling these physicians "switchers," the GAO found a 24% increase in referrals for pathology services among dermatologists who self-referred in 2010, compared to only a 0.3% increase for those who sent biopsy specimens elsewhere.
The GAO conducted its investigation at the request of Rep. Henry A. Waxman (D-Calif.), Rep. Sander Levin (D-Mich.), Sen. Max Baucus (D-Mont.), and Sen. Chuck Grassley (R-Iowa).
"The analysis suggests that financial incentives for self-referring providers is likely a major factor driving the increase in referrals for these services," Rep. Waxman said in a joint statement from the legislators.
"As Congress looks to rein in unnecessary spending, my colleagues and I should explore this area in greater depth," he said.
Sen. Grassley added, "Federal policy should drive doctors to make decisions based on quality of care, not financial relationships. The taxpayers shouldn’t have to pay for services that aren’t medically necessary."
The GAO suggested that the Centers for Medicare and Medicaid Services should require providers to state on claims whether a service was self-referred, and that the agency should limit payment so that physicians aren’t rewarded for higher numbers of specimens per biopsy.
In comments to the GAO on the report, the American Academy of Dermatology Association said that it agreed that the CMS should develop a way to ensure the appropriateness of biopsy procedures. But the AADA expressed concern about limitations on financial incentives, saying that dermatologists should be encouraged to perform biopsies. The AADA also said that dermatologists should be allowed to prepare and review their own specimens "because they receive considerable training as part of their education."
On Twitter @aliciaault
Disability, not death, colors Americans' health
WASHINGTON – Americans are increasingly living with disabling conditions rather than dying from fatal diseases, while their nation lags behind its economic peers in addressing risk factors that contribute to poor health and premature death.
That’s according to several studies highlighted at the briefing.
"We’ve identified substantial areas where the U.S. can make progress and hopefully narrow the gap between what we’ve observed in the U.S. and the [peer] countries," Dr. Christopher Murray, director of the Institute for Health Metrics and Evaluation at the University of Washington, Seattle, and the lead author of the studies, said at an Institute of Medicine briefing July 10. "There’s also a role, we believe, for enhanced primary care – management of blood pressure, cholesterol, and encouragement of physical activity of patients."
The main study, published on July 10 in JAMA, is "an extraordinary publication," said Dr. Howard Bauchner, the journal’s editor in chief. "This is the first comprehensive box score of American health that’s ever been published."
The JAMA study, along with two companions, adds to the growing body of evidence that diet and physical activity – as well as smoking – are among the most important determinants of health, outside of socioeconomic factors.
Both Dr. Murray and Dr. Bauchner said that it was critical for physicians to discuss these lifestyle issues with patients, but also to monitor risk factors like hypertension, cholesterol, and blood sugar, especially in women, who are, in some areas of the country, facing rising death rates from heart disease in particular.
The United States has succeeded in reducing deaths from ischemic heart disease, HIV/AIDS, sudden infant death syndrome, and certain cancers, according to researchers from the U.S. Burden of Disease Collaborators, a group of academic, private, and government researchers from around the world.
But chronic disability from lung cancer, musculoskeletal pain, neurologic conditions, diabetes, and mental health/substance-use disorders – in particular, opioid abuse – is growing rapidly (JAMA 2013 July 10 [doi: 10.1001/jama.2013.13805]).
Substance abuse is not only disabling, but also contributes to premature death, the investigators found. More years of life lost were lost due to drug use disorders in 2010 than from prostate cancer and ovarian cancer combined, rising 448% between 1990 and 2010. Drug use went from 44th on the list of leading causes of years of life lost to 15th.
Alzheimer’s disease, liver cancer, Parkinson’s disease, and kidney cancer are also gaining among the causes of premature death.
"The United States spends more than the rest of the world on health care and leads the world in the quality and quantity of its health research, but that doesn’t add up to better health outcomes," Dr. Murray said in a statement. "The country has done a good job of preventing premature deaths from stroke, but when it comes to lung cancer, preterm birth complications, and a range of other causes, the country isn’t keeping pace with high-income countries in Europe, Asia, and elsewhere."
The study looked at death and disability from 291 diseases, conditions, and injuries, and also examined 67 risk factors for death and disability. The authors used the same methodology as that employed in the Global Burden of Disease Study 2010 (Lancet 2012:380;2055-2058).
In the U.S. study, the top 10 causes of years of life lost in 2010 were ischemic heart disease (16%), lung cancer (7%), stroke (4%), chronic obstructive pulmonary disease (4%), road injury (4%), self-harm (3%), diabetes (3%), cirrhosis (3%), Alzheimer’s disease (3%), and colorectal cancer (2%).
From 1990 to 2010, the average life expectancy for Americans increased from 75.2 to 78.2 years. But the "healthy life expectancy" – the number of years someone can expect to live in good health – went from 65.8 years to 68.1 years during the same period. The gap between average life expectancy and healthy life expectancy rose from 9.4 years in 1990 to 10.1 years in 2010.
When compared with 34 nations in Europe, Asia, and North America, the United States fell in rankings on almost every health measure from 1990 to 2010. For life expectancy at birth, the U.S. dropped from 20th to 27th.
Poor diet and not enough physical activity, along with smoking and uncontrolled blood pressure and cholesterol, were behind the drops, according to the investigators. The United States ranked 27th in disease burden risk from dietary factors and was also ranked 27th for body mass index. For healthy blood sugar, the United States was ranked 29th.
The United States is near the bottom when it comes to death rates. America ranks 27th among the 34 comparator countries. Only the Czech Republic, Poland, Estonia, Mexico, Turkey, Slovakia, and Hungary had higher death rates.
Meanwhile, two other studies examined life expectancy and physical activity on a county-by-county basis in America. Both were conducted by researchers at the Institute for Health Metrics and Evaluation, and both were published online in the open-access, peer-reviewed journal Population Health Metrics, which is edited by Dr. Murray.
In the first study, "Prevalence of Physical Activity and Obesity in US Counties, 2001-2011: A Road Map for Action," physical activity did not increase overall in the United States during the study period (2001-2009), but the percentage of the population considered obese did. The authors found that just because an area had higher physical activity levels did not mean that there would be a corresponding drop in obesity. They wrote that from 2001 to 2009, "for every 1 percentage point increase in physical activity, obesity prevalence was 0.11 percentage points lower" (Popul. Health Metr. 2013;11:7 [doi: 10.1186/1478-7954-11-7]).
Some counties – in Florida, Georgia, and Kentucky – saw large gains in physical activity. Among women, for instance, the largest increase in sufficient physical activity (defined as 150 minutes of moderate activity or 75 minutes of vigorous activity weekly) was seen in Morgan County, Ky., where the rate rose from 26% to 44% during 2001-2009.
Generally, physical activity was worse for men and women who lived along the Texas-Mexico border, the Mississippi Valley, parts of the Deep South, and West Virginia, according to the study.
Douglas County, Colo., had the highest rate of activity in the United States (90%) for men in 2011, while Marin County, Calif., had highest rate for women (90%). Wolfe County, Ky., had the lowest rate for men (55%), and McDowell County, W.Va., had the lowest rate for women (51%).
Obesity rates tended to track with activity rates, with higher rates in the South and lower rates in urban areas like San Francisco, New York, and Washington, D.C.
The authors also published a county-by-county analysis of life expectancy, "Left Behind: Widening Disparities for Males and Females in US County Life Expectancy, 1985-2010." They reported that among the top-achieving counties, female life expectancy in 2010 was 85 years (or about 5 years more than the national average) and male life expectancy was 81.7 years (also about 5 years greater than the national average). But, they said, in many counties there has been no increase, or in some cases, declines in life expectancy, especially for women. There was a dramatic increase in inequality in life expectancy at birth among U.S. counties between 1985 and 2010, they concluded (Popul. Health Metr. 2013;11:8 [doi: 10.1186/1478-7954-11-8]).
Dr. Murray’s work is supported in part by the National Institutes of Health and in part by the Bill and Melinda Gates Foundation.
aault@frontlinemedcom.com On Twitter @aliciaault
Despite a level of health expenditures that would have seemed unthinkable a generation ago, the health of the U.S. population has improved only gradually and has fallen behind the pace of progress in many other wealthy nations.
The authors’ determination to generate consistent data across a range of national settings and to focus on specific diseases as causes of death is a source of strength and of limitations to the study. The strength is the capacity to compare in a consistent way. The limitation is reliance on data types that are universally available and on analyses that relate to specific disease conditions rather than to overall mortality. The most glaring omission in the assessment of risk factors, as the authors acknowledge, is the role of social factors such as income and inequality as a risk of premature death and disability. This omission should not be allowed to mislead policy makers, because differences in socioeconomic status and other social circumstances are strongly related to differences in mortality, as has been emphasized in a recent, comprehensive assessment by the National Research Council and the Institute of Medicine on U.S. health in comparison with other countries.
Setting the United States on a healthier course will surely require leadership at all levels of government and across the public and private sectors and actively engaging the health professions and the public. Analyses such as the U.S. Burden of Disease can help identify priorities for research and action and monitor the state of progress over time.
Dr. Harvey V. Fineberg is the president of the Institute of Medicine in Washington, D.C. These remarks were taken from his editorial accompanying the JAMA study. He reported no conflicts of interest.
Despite a level of health expenditures that would have seemed unthinkable a generation ago, the health of the U.S. population has improved only gradually and has fallen behind the pace of progress in many other wealthy nations.
The authors’ determination to generate consistent data across a range of national settings and to focus on specific diseases as causes of death is a source of strength and of limitations to the study. The strength is the capacity to compare in a consistent way. The limitation is reliance on data types that are universally available and on analyses that relate to specific disease conditions rather than to overall mortality. The most glaring omission in the assessment of risk factors, as the authors acknowledge, is the role of social factors such as income and inequality as a risk of premature death and disability. This omission should not be allowed to mislead policy makers, because differences in socioeconomic status and other social circumstances are strongly related to differences in mortality, as has been emphasized in a recent, comprehensive assessment by the National Research Council and the Institute of Medicine on U.S. health in comparison with other countries.
Setting the United States on a healthier course will surely require leadership at all levels of government and across the public and private sectors and actively engaging the health professions and the public. Analyses such as the U.S. Burden of Disease can help identify priorities for research and action and monitor the state of progress over time.
Dr. Harvey V. Fineberg is the president of the Institute of Medicine in Washington, D.C. These remarks were taken from his editorial accompanying the JAMA study. He reported no conflicts of interest.
Despite a level of health expenditures that would have seemed unthinkable a generation ago, the health of the U.S. population has improved only gradually and has fallen behind the pace of progress in many other wealthy nations.
The authors’ determination to generate consistent data across a range of national settings and to focus on specific diseases as causes of death is a source of strength and of limitations to the study. The strength is the capacity to compare in a consistent way. The limitation is reliance on data types that are universally available and on analyses that relate to specific disease conditions rather than to overall mortality. The most glaring omission in the assessment of risk factors, as the authors acknowledge, is the role of social factors such as income and inequality as a risk of premature death and disability. This omission should not be allowed to mislead policy makers, because differences in socioeconomic status and other social circumstances are strongly related to differences in mortality, as has been emphasized in a recent, comprehensive assessment by the National Research Council and the Institute of Medicine on U.S. health in comparison with other countries.
Setting the United States on a healthier course will surely require leadership at all levels of government and across the public and private sectors and actively engaging the health professions and the public. Analyses such as the U.S. Burden of Disease can help identify priorities for research and action and monitor the state of progress over time.
Dr. Harvey V. Fineberg is the president of the Institute of Medicine in Washington, D.C. These remarks were taken from his editorial accompanying the JAMA study. He reported no conflicts of interest.
WASHINGTON – Americans are increasingly living with disabling conditions rather than dying from fatal diseases, while their nation lags behind its economic peers in addressing risk factors that contribute to poor health and premature death.
That’s according to several studies highlighted at the briefing.
"We’ve identified substantial areas where the U.S. can make progress and hopefully narrow the gap between what we’ve observed in the U.S. and the [peer] countries," Dr. Christopher Murray, director of the Institute for Health Metrics and Evaluation at the University of Washington, Seattle, and the lead author of the studies, said at an Institute of Medicine briefing July 10. "There’s also a role, we believe, for enhanced primary care – management of blood pressure, cholesterol, and encouragement of physical activity of patients."
The main study, published on July 10 in JAMA, is "an extraordinary publication," said Dr. Howard Bauchner, the journal’s editor in chief. "This is the first comprehensive box score of American health that’s ever been published."
The JAMA study, along with two companions, adds to the growing body of evidence that diet and physical activity – as well as smoking – are among the most important determinants of health, outside of socioeconomic factors.
Both Dr. Murray and Dr. Bauchner said that it was critical for physicians to discuss these lifestyle issues with patients, but also to monitor risk factors like hypertension, cholesterol, and blood sugar, especially in women, who are, in some areas of the country, facing rising death rates from heart disease in particular.
The United States has succeeded in reducing deaths from ischemic heart disease, HIV/AIDS, sudden infant death syndrome, and certain cancers, according to researchers from the U.S. Burden of Disease Collaborators, a group of academic, private, and government researchers from around the world.
But chronic disability from lung cancer, musculoskeletal pain, neurologic conditions, diabetes, and mental health/substance-use disorders – in particular, opioid abuse – is growing rapidly (JAMA 2013 July 10 [doi: 10.1001/jama.2013.13805]).
Substance abuse is not only disabling, but also contributes to premature death, the investigators found. More years of life lost were lost due to drug use disorders in 2010 than from prostate cancer and ovarian cancer combined, rising 448% between 1990 and 2010. Drug use went from 44th on the list of leading causes of years of life lost to 15th.
Alzheimer’s disease, liver cancer, Parkinson’s disease, and kidney cancer are also gaining among the causes of premature death.
"The United States spends more than the rest of the world on health care and leads the world in the quality and quantity of its health research, but that doesn’t add up to better health outcomes," Dr. Murray said in a statement. "The country has done a good job of preventing premature deaths from stroke, but when it comes to lung cancer, preterm birth complications, and a range of other causes, the country isn’t keeping pace with high-income countries in Europe, Asia, and elsewhere."
The study looked at death and disability from 291 diseases, conditions, and injuries, and also examined 67 risk factors for death and disability. The authors used the same methodology as that employed in the Global Burden of Disease Study 2010 (Lancet 2012:380;2055-2058).
In the U.S. study, the top 10 causes of years of life lost in 2010 were ischemic heart disease (16%), lung cancer (7%), stroke (4%), chronic obstructive pulmonary disease (4%), road injury (4%), self-harm (3%), diabetes (3%), cirrhosis (3%), Alzheimer’s disease (3%), and colorectal cancer (2%).
From 1990 to 2010, the average life expectancy for Americans increased from 75.2 to 78.2 years. But the "healthy life expectancy" – the number of years someone can expect to live in good health – went from 65.8 years to 68.1 years during the same period. The gap between average life expectancy and healthy life expectancy rose from 9.4 years in 1990 to 10.1 years in 2010.
When compared with 34 nations in Europe, Asia, and North America, the United States fell in rankings on almost every health measure from 1990 to 2010. For life expectancy at birth, the U.S. dropped from 20th to 27th.
Poor diet and not enough physical activity, along with smoking and uncontrolled blood pressure and cholesterol, were behind the drops, according to the investigators. The United States ranked 27th in disease burden risk from dietary factors and was also ranked 27th for body mass index. For healthy blood sugar, the United States was ranked 29th.
The United States is near the bottom when it comes to death rates. America ranks 27th among the 34 comparator countries. Only the Czech Republic, Poland, Estonia, Mexico, Turkey, Slovakia, and Hungary had higher death rates.
Meanwhile, two other studies examined life expectancy and physical activity on a county-by-county basis in America. Both were conducted by researchers at the Institute for Health Metrics and Evaluation, and both were published online in the open-access, peer-reviewed journal Population Health Metrics, which is edited by Dr. Murray.
In the first study, "Prevalence of Physical Activity and Obesity in US Counties, 2001-2011: A Road Map for Action," physical activity did not increase overall in the United States during the study period (2001-2009), but the percentage of the population considered obese did. The authors found that just because an area had higher physical activity levels did not mean that there would be a corresponding drop in obesity. They wrote that from 2001 to 2009, "for every 1 percentage point increase in physical activity, obesity prevalence was 0.11 percentage points lower" (Popul. Health Metr. 2013;11:7 [doi: 10.1186/1478-7954-11-7]).
Some counties – in Florida, Georgia, and Kentucky – saw large gains in physical activity. Among women, for instance, the largest increase in sufficient physical activity (defined as 150 minutes of moderate activity or 75 minutes of vigorous activity weekly) was seen in Morgan County, Ky., where the rate rose from 26% to 44% during 2001-2009.
Generally, physical activity was worse for men and women who lived along the Texas-Mexico border, the Mississippi Valley, parts of the Deep South, and West Virginia, according to the study.
Douglas County, Colo., had the highest rate of activity in the United States (90%) for men in 2011, while Marin County, Calif., had highest rate for women (90%). Wolfe County, Ky., had the lowest rate for men (55%), and McDowell County, W.Va., had the lowest rate for women (51%).
Obesity rates tended to track with activity rates, with higher rates in the South and lower rates in urban areas like San Francisco, New York, and Washington, D.C.
The authors also published a county-by-county analysis of life expectancy, "Left Behind: Widening Disparities for Males and Females in US County Life Expectancy, 1985-2010." They reported that among the top-achieving counties, female life expectancy in 2010 was 85 years (or about 5 years more than the national average) and male life expectancy was 81.7 years (also about 5 years greater than the national average). But, they said, in many counties there has been no increase, or in some cases, declines in life expectancy, especially for women. There was a dramatic increase in inequality in life expectancy at birth among U.S. counties between 1985 and 2010, they concluded (Popul. Health Metr. 2013;11:8 [doi: 10.1186/1478-7954-11-8]).
Dr. Murray’s work is supported in part by the National Institutes of Health and in part by the Bill and Melinda Gates Foundation.
aault@frontlinemedcom.com On Twitter @aliciaault
WASHINGTON – Americans are increasingly living with disabling conditions rather than dying from fatal diseases, while their nation lags behind its economic peers in addressing risk factors that contribute to poor health and premature death.
That’s according to several studies highlighted at the briefing.
"We’ve identified substantial areas where the U.S. can make progress and hopefully narrow the gap between what we’ve observed in the U.S. and the [peer] countries," Dr. Christopher Murray, director of the Institute for Health Metrics and Evaluation at the University of Washington, Seattle, and the lead author of the studies, said at an Institute of Medicine briefing July 10. "There’s also a role, we believe, for enhanced primary care – management of blood pressure, cholesterol, and encouragement of physical activity of patients."
The main study, published on July 10 in JAMA, is "an extraordinary publication," said Dr. Howard Bauchner, the journal’s editor in chief. "This is the first comprehensive box score of American health that’s ever been published."
The JAMA study, along with two companions, adds to the growing body of evidence that diet and physical activity – as well as smoking – are among the most important determinants of health, outside of socioeconomic factors.
Both Dr. Murray and Dr. Bauchner said that it was critical for physicians to discuss these lifestyle issues with patients, but also to monitor risk factors like hypertension, cholesterol, and blood sugar, especially in women, who are, in some areas of the country, facing rising death rates from heart disease in particular.
The United States has succeeded in reducing deaths from ischemic heart disease, HIV/AIDS, sudden infant death syndrome, and certain cancers, according to researchers from the U.S. Burden of Disease Collaborators, a group of academic, private, and government researchers from around the world.
But chronic disability from lung cancer, musculoskeletal pain, neurologic conditions, diabetes, and mental health/substance-use disorders – in particular, opioid abuse – is growing rapidly (JAMA 2013 July 10 [doi: 10.1001/jama.2013.13805]).
Substance abuse is not only disabling, but also contributes to premature death, the investigators found. More years of life lost were lost due to drug use disorders in 2010 than from prostate cancer and ovarian cancer combined, rising 448% between 1990 and 2010. Drug use went from 44th on the list of leading causes of years of life lost to 15th.
Alzheimer’s disease, liver cancer, Parkinson’s disease, and kidney cancer are also gaining among the causes of premature death.
"The United States spends more than the rest of the world on health care and leads the world in the quality and quantity of its health research, but that doesn’t add up to better health outcomes," Dr. Murray said in a statement. "The country has done a good job of preventing premature deaths from stroke, but when it comes to lung cancer, preterm birth complications, and a range of other causes, the country isn’t keeping pace with high-income countries in Europe, Asia, and elsewhere."
The study looked at death and disability from 291 diseases, conditions, and injuries, and also examined 67 risk factors for death and disability. The authors used the same methodology as that employed in the Global Burden of Disease Study 2010 (Lancet 2012:380;2055-2058).
In the U.S. study, the top 10 causes of years of life lost in 2010 were ischemic heart disease (16%), lung cancer (7%), stroke (4%), chronic obstructive pulmonary disease (4%), road injury (4%), self-harm (3%), diabetes (3%), cirrhosis (3%), Alzheimer’s disease (3%), and colorectal cancer (2%).
From 1990 to 2010, the average life expectancy for Americans increased from 75.2 to 78.2 years. But the "healthy life expectancy" – the number of years someone can expect to live in good health – went from 65.8 years to 68.1 years during the same period. The gap between average life expectancy and healthy life expectancy rose from 9.4 years in 1990 to 10.1 years in 2010.
When compared with 34 nations in Europe, Asia, and North America, the United States fell in rankings on almost every health measure from 1990 to 2010. For life expectancy at birth, the U.S. dropped from 20th to 27th.
Poor diet and not enough physical activity, along with smoking and uncontrolled blood pressure and cholesterol, were behind the drops, according to the investigators. The United States ranked 27th in disease burden risk from dietary factors and was also ranked 27th for body mass index. For healthy blood sugar, the United States was ranked 29th.
The United States is near the bottom when it comes to death rates. America ranks 27th among the 34 comparator countries. Only the Czech Republic, Poland, Estonia, Mexico, Turkey, Slovakia, and Hungary had higher death rates.
Meanwhile, two other studies examined life expectancy and physical activity on a county-by-county basis in America. Both were conducted by researchers at the Institute for Health Metrics and Evaluation, and both were published online in the open-access, peer-reviewed journal Population Health Metrics, which is edited by Dr. Murray.
In the first study, "Prevalence of Physical Activity and Obesity in US Counties, 2001-2011: A Road Map for Action," physical activity did not increase overall in the United States during the study period (2001-2009), but the percentage of the population considered obese did. The authors found that just because an area had higher physical activity levels did not mean that there would be a corresponding drop in obesity. They wrote that from 2001 to 2009, "for every 1 percentage point increase in physical activity, obesity prevalence was 0.11 percentage points lower" (Popul. Health Metr. 2013;11:7 [doi: 10.1186/1478-7954-11-7]).
Some counties – in Florida, Georgia, and Kentucky – saw large gains in physical activity. Among women, for instance, the largest increase in sufficient physical activity (defined as 150 minutes of moderate activity or 75 minutes of vigorous activity weekly) was seen in Morgan County, Ky., where the rate rose from 26% to 44% during 2001-2009.
Generally, physical activity was worse for men and women who lived along the Texas-Mexico border, the Mississippi Valley, parts of the Deep South, and West Virginia, according to the study.
Douglas County, Colo., had the highest rate of activity in the United States (90%) for men in 2011, while Marin County, Calif., had highest rate for women (90%). Wolfe County, Ky., had the lowest rate for men (55%), and McDowell County, W.Va., had the lowest rate for women (51%).
Obesity rates tended to track with activity rates, with higher rates in the South and lower rates in urban areas like San Francisco, New York, and Washington, D.C.
The authors also published a county-by-county analysis of life expectancy, "Left Behind: Widening Disparities for Males and Females in US County Life Expectancy, 1985-2010." They reported that among the top-achieving counties, female life expectancy in 2010 was 85 years (or about 5 years more than the national average) and male life expectancy was 81.7 years (also about 5 years greater than the national average). But, they said, in many counties there has been no increase, or in some cases, declines in life expectancy, especially for women. There was a dramatic increase in inequality in life expectancy at birth among U.S. counties between 1985 and 2010, they concluded (Popul. Health Metr. 2013;11:8 [doi: 10.1186/1478-7954-11-8]).
Dr. Murray’s work is supported in part by the National Institutes of Health and in part by the Bill and Melinda Gates Foundation.
aault@frontlinemedcom.com On Twitter @aliciaault
AT A PRESS BRIEFING HELD BY JAMA AND THE INSTITUTE OF MEDICINE
CPCI participants were off to a slow start
BALTIMORE – Even primary care practices that were well along the continuum of delivering more sophisticated care were lagging when it comes to better-coordinating care, according to findings from a baseline study of the 497 practices participating in the Centers for Medicare and Medicaid Services Comprehensive Primary Care Initiative (CPCI).
The CMS selected 502 practices – that were already making ample use of electronic health records and, in many cases, acting as patient-centered medical homes – to participate in the initiative. Several practices dropped out. The remaining 497 began receiving financial incentives to cut the cost of care and improve quality in the fall of 2012. The practices received a $20/member per month of care management fee for 2 years from CMS and other payers, covering Medicare patients. The fee drops to $15/member per month for the second 2 years of the program. After that, physician practices have the opportunity to share savings with the CMS and the other payers.
To be eligible for the CPCI, practices had to serve at least 120 Medicare patients and be heavy users of electronic health records (EHRs).
Rachel Shapiro, a researcher with Mathematica Policy Research, presented results from a survey of all 497 of the practices. They were queried at baseline, before they began receiving any financial incentives or other assistance from the CMS. The agency hired Mathematica and Group Health Research Institute to conduct on-going surveys to gauge how well the practices are doing in meeting the CPCI objectives over the next 5 years.
Those objectives include:
• Intensive care management for patients with multiple medical conditions, including creating care plans for each individual patient.
• Ensuring access to care 24 hours a day, 7 days a week.
• Delivering preventive care on an appropriate and timely basis.
• Engaging patients and caregivers in their care.
• Coordinating care “across the medical neighborhood.”
The first survey was e-mailed to the practices from October to December 2012; all 497 responded, said Ms. Shapiro. Most of the practices had between one and four clinicians, including physicians, nurse practitioners, and physician assistants. Only 12% are multispecialty practices, but 46% are owned by a larger entity. Of the participating practices, 41% had been certified as a patient-centered medical home and 79% had reached stage 1 of meaningful use under the CMS’ criteria for EHRs.
They assessed their performance before CPCI began, on six measures: access and continuity; planned chronic and preventive care; patient and caregiver engagement; care coordination across the medical neighborhood; continuous quality improvement; and, risk-stratified care management. The practices assigned themselves scores of 1 to 12, with a higher score indicating better implementation of the goals. Practices averaged a score of 8 for the measures of access and care planning. At bottom, the practices scored a 4, on average, for risk-stratified care management.
There was definitely room for improvement across the board, said Ms. Shapiro. She noted that innovative ways to engage and communicate with patients – such as e-mail, texting, group visits, and phone visits – were not available at 54% of the practices. Of the reporting practices, 24% made limited use of such methods.
Integration of practice guidelines into care was reported by 60% practices, but only 16% routinely use care plans. The same percentage does not have access to registry or full panel data from the practice to help identify issues across a number of patients rather than just reacting to an individual patient, Ms. Shapiro said. Only a third of practices said they had a care manager.
Patient and caregiver engagement is also lacking. Only 16% of practices routinely collect patient and caregiver feedback.
All the practices make referrals to specialists, but often, they are not transmitting full information to that clinician.
Of the reporting practices, 77% do not conduct quality improvement activities, citing a lack of resources and staff.
Ms. Shapiro and her colleagues looked at whether being a medical home or a meaningful user made any difference in terms of scoring. They also looked at the effect of practice size. Designated medical homes reported better functioning, but practice size did not make a difference. Meaningful users of EHRs had better scores, but only in continuous quality improvement and risk stratification.
The study shows that even practices that were somewhat sophisticated before the start of the initiative still have a ways to go in terms of delivering better-coordinated care, said Ms. Shapiro. She noted that these practices will likely progress, though, as they will be given technical assistance tailored to their unique needs and also quarterly reports to track performance and improvements in patient care.
BALTIMORE – Even primary care practices that were well along the continuum of delivering more sophisticated care were lagging when it comes to better-coordinating care, according to findings from a baseline study of the 497 practices participating in the Centers for Medicare and Medicaid Services Comprehensive Primary Care Initiative (CPCI).
The CMS selected 502 practices – that were already making ample use of electronic health records and, in many cases, acting as patient-centered medical homes – to participate in the initiative. Several practices dropped out. The remaining 497 began receiving financial incentives to cut the cost of care and improve quality in the fall of 2012. The practices received a $20/member per month of care management fee for 2 years from CMS and other payers, covering Medicare patients. The fee drops to $15/member per month for the second 2 years of the program. After that, physician practices have the opportunity to share savings with the CMS and the other payers.
To be eligible for the CPCI, practices had to serve at least 120 Medicare patients and be heavy users of electronic health records (EHRs).
Rachel Shapiro, a researcher with Mathematica Policy Research, presented results from a survey of all 497 of the practices. They were queried at baseline, before they began receiving any financial incentives or other assistance from the CMS. The agency hired Mathematica and Group Health Research Institute to conduct on-going surveys to gauge how well the practices are doing in meeting the CPCI objectives over the next 5 years.
Those objectives include:
• Intensive care management for patients with multiple medical conditions, including creating care plans for each individual patient.
• Ensuring access to care 24 hours a day, 7 days a week.
• Delivering preventive care on an appropriate and timely basis.
• Engaging patients and caregivers in their care.
• Coordinating care “across the medical neighborhood.”
The first survey was e-mailed to the practices from October to December 2012; all 497 responded, said Ms. Shapiro. Most of the practices had between one and four clinicians, including physicians, nurse practitioners, and physician assistants. Only 12% are multispecialty practices, but 46% are owned by a larger entity. Of the participating practices, 41% had been certified as a patient-centered medical home and 79% had reached stage 1 of meaningful use under the CMS’ criteria for EHRs.
They assessed their performance before CPCI began, on six measures: access and continuity; planned chronic and preventive care; patient and caregiver engagement; care coordination across the medical neighborhood; continuous quality improvement; and, risk-stratified care management. The practices assigned themselves scores of 1 to 12, with a higher score indicating better implementation of the goals. Practices averaged a score of 8 for the measures of access and care planning. At bottom, the practices scored a 4, on average, for risk-stratified care management.
There was definitely room for improvement across the board, said Ms. Shapiro. She noted that innovative ways to engage and communicate with patients – such as e-mail, texting, group visits, and phone visits – were not available at 54% of the practices. Of the reporting practices, 24% made limited use of such methods.
Integration of practice guidelines into care was reported by 60% practices, but only 16% routinely use care plans. The same percentage does not have access to registry or full panel data from the practice to help identify issues across a number of patients rather than just reacting to an individual patient, Ms. Shapiro said. Only a third of practices said they had a care manager.
Patient and caregiver engagement is also lacking. Only 16% of practices routinely collect patient and caregiver feedback.
All the practices make referrals to specialists, but often, they are not transmitting full information to that clinician.
Of the reporting practices, 77% do not conduct quality improvement activities, citing a lack of resources and staff.
Ms. Shapiro and her colleagues looked at whether being a medical home or a meaningful user made any difference in terms of scoring. They also looked at the effect of practice size. Designated medical homes reported better functioning, but practice size did not make a difference. Meaningful users of EHRs had better scores, but only in continuous quality improvement and risk stratification.
The study shows that even practices that were somewhat sophisticated before the start of the initiative still have a ways to go in terms of delivering better-coordinated care, said Ms. Shapiro. She noted that these practices will likely progress, though, as they will be given technical assistance tailored to their unique needs and also quarterly reports to track performance and improvements in patient care.
BALTIMORE – Even primary care practices that were well along the continuum of delivering more sophisticated care were lagging when it comes to better-coordinating care, according to findings from a baseline study of the 497 practices participating in the Centers for Medicare and Medicaid Services Comprehensive Primary Care Initiative (CPCI).
The CMS selected 502 practices – that were already making ample use of electronic health records and, in many cases, acting as patient-centered medical homes – to participate in the initiative. Several practices dropped out. The remaining 497 began receiving financial incentives to cut the cost of care and improve quality in the fall of 2012. The practices received a $20/member per month of care management fee for 2 years from CMS and other payers, covering Medicare patients. The fee drops to $15/member per month for the second 2 years of the program. After that, physician practices have the opportunity to share savings with the CMS and the other payers.
To be eligible for the CPCI, practices had to serve at least 120 Medicare patients and be heavy users of electronic health records (EHRs).
Rachel Shapiro, a researcher with Mathematica Policy Research, presented results from a survey of all 497 of the practices. They were queried at baseline, before they began receiving any financial incentives or other assistance from the CMS. The agency hired Mathematica and Group Health Research Institute to conduct on-going surveys to gauge how well the practices are doing in meeting the CPCI objectives over the next 5 years.
Those objectives include:
• Intensive care management for patients with multiple medical conditions, including creating care plans for each individual patient.
• Ensuring access to care 24 hours a day, 7 days a week.
• Delivering preventive care on an appropriate and timely basis.
• Engaging patients and caregivers in their care.
• Coordinating care “across the medical neighborhood.”
The first survey was e-mailed to the practices from October to December 2012; all 497 responded, said Ms. Shapiro. Most of the practices had between one and four clinicians, including physicians, nurse practitioners, and physician assistants. Only 12% are multispecialty practices, but 46% are owned by a larger entity. Of the participating practices, 41% had been certified as a patient-centered medical home and 79% had reached stage 1 of meaningful use under the CMS’ criteria for EHRs.
They assessed their performance before CPCI began, on six measures: access and continuity; planned chronic and preventive care; patient and caregiver engagement; care coordination across the medical neighborhood; continuous quality improvement; and, risk-stratified care management. The practices assigned themselves scores of 1 to 12, with a higher score indicating better implementation of the goals. Practices averaged a score of 8 for the measures of access and care planning. At bottom, the practices scored a 4, on average, for risk-stratified care management.
There was definitely room for improvement across the board, said Ms. Shapiro. She noted that innovative ways to engage and communicate with patients – such as e-mail, texting, group visits, and phone visits – were not available at 54% of the practices. Of the reporting practices, 24% made limited use of such methods.
Integration of practice guidelines into care was reported by 60% practices, but only 16% routinely use care plans. The same percentage does not have access to registry or full panel data from the practice to help identify issues across a number of patients rather than just reacting to an individual patient, Ms. Shapiro said. Only a third of practices said they had a care manager.
Patient and caregiver engagement is also lacking. Only 16% of practices routinely collect patient and caregiver feedback.
All the practices make referrals to specialists, but often, they are not transmitting full information to that clinician.
Of the reporting practices, 77% do not conduct quality improvement activities, citing a lack of resources and staff.
Ms. Shapiro and her colleagues looked at whether being a medical home or a meaningful user made any difference in terms of scoring. They also looked at the effect of practice size. Designated medical homes reported better functioning, but practice size did not make a difference. Meaningful users of EHRs had better scores, but only in continuous quality improvement and risk stratification.
The study shows that even practices that were somewhat sophisticated before the start of the initiative still have a ways to go in terms of delivering better-coordinated care, said Ms. Shapiro. She noted that these practices will likely progress, though, as they will be given technical assistance tailored to their unique needs and also quarterly reports to track performance and improvements in patient care.
AT ACADEMYHEALTH 2013
QI modules help fuel diabetes care gains
BALTIMORE – Family physicians were able to improve clinical care for diabetics when they used self-directed quality improvement modules.
That’s the lesson from a study of some 8,000 family physicians who participated in the American Board of Family Medicine’s (ABFM) maintenance of certification (MOC) process. Part of that process includes a performance improvement module – called the Performance in Practice Module – and physicians can choose disease states for that module.
Dr. Lars Peterson, research director at the ABFM, presented the analysis of the initial experiences with the diabetes module at AcademyHealth’s annual research meeting here.
For the quality improvement part of the MOC process, physicians first complete a tutorial on quality improvement theory and methods. They then select 10 charts to abstract—generally, the first 10 patients with the particular condition--and choose up to seven quality measures for improvement. The quality measures come from the National Quality Forum, said Dr. Peterson.
Physicians submit their performance data to the ABFM; in return, physicians get a benchmarking report that compares their performance with other physicians, both before the intervention and after.
The 7,924 physicians analyzed for the study had been in practice an average 13 years and were 48 years old on average. They took an average of 6 months to complete the practice module. Three-quarters of the practices were in urban areas; 11% were large rural practices, and 8% were small rural practices.
Almost half the participants chose the diabetic foot exam and retina exam as the measure for improvement. Not surprisingly, these were the areas with the lowest performance metrics at baseline. Fewer than 15% chose blood pressure and hemoglobin A1c. The remainder chose other measures.
At baseline, only 68% of physicians conducted a foot exam. After going through the improvement process, 86% of physicians were looking at their patients’ feet. Only 56% of patients had a retina exam initially; after the module, 71% had gotten the exam.
There was also significant improvement in HbA1c control, with 60% in control before the intervention and 62% after. The number of patients who had normalized their blood pressure rose from 54% to 57%. There were also gains in smoking cessation – from 87% to 93%.
The only measure in which there was not significant improvement was in getting low-density lipoprotein (LDL) levels down to less than 100 mg/dL. Initially, 63% of patients achieved this measure; after the intervention, that had risen to just 64%.
To ensure that physicians weren’t just picking their best patients, the ABFM also surveyed patients, said Dr. Peterson. When asked about their care, at baseline, 76% said the doctor had checked their feet. After the intervention, that had risen to 90%. Patients getting eye exams rose from 70% to 80%. When asked if they had an HbA1c test, initially 92% said yes. After the process, 96% of patients said they’d had their blood sugar tested. Only 77% of patients knew their blood pressure goal at baseline. Post intervention, 86% were knowledgeable.
Dr. Peterson said the ABFM hoped to leverage the quality improvement aspect of the MOC process to help lower costs and improve patient care. In the future, the goal is to move the QI modules beyond a handful of patients to a physician’s full panel, complete with continuous feedback, he said.
On Twitter @aliciaault
BALTIMORE – Family physicians were able to improve clinical care for diabetics when they used self-directed quality improvement modules.
That’s the lesson from a study of some 8,000 family physicians who participated in the American Board of Family Medicine’s (ABFM) maintenance of certification (MOC) process. Part of that process includes a performance improvement module – called the Performance in Practice Module – and physicians can choose disease states for that module.
Dr. Lars Peterson, research director at the ABFM, presented the analysis of the initial experiences with the diabetes module at AcademyHealth’s annual research meeting here.
For the quality improvement part of the MOC process, physicians first complete a tutorial on quality improvement theory and methods. They then select 10 charts to abstract—generally, the first 10 patients with the particular condition--and choose up to seven quality measures for improvement. The quality measures come from the National Quality Forum, said Dr. Peterson.
Physicians submit their performance data to the ABFM; in return, physicians get a benchmarking report that compares their performance with other physicians, both before the intervention and after.
The 7,924 physicians analyzed for the study had been in practice an average 13 years and were 48 years old on average. They took an average of 6 months to complete the practice module. Three-quarters of the practices were in urban areas; 11% were large rural practices, and 8% were small rural practices.
Almost half the participants chose the diabetic foot exam and retina exam as the measure for improvement. Not surprisingly, these were the areas with the lowest performance metrics at baseline. Fewer than 15% chose blood pressure and hemoglobin A1c. The remainder chose other measures.
At baseline, only 68% of physicians conducted a foot exam. After going through the improvement process, 86% of physicians were looking at their patients’ feet. Only 56% of patients had a retina exam initially; after the module, 71% had gotten the exam.
There was also significant improvement in HbA1c control, with 60% in control before the intervention and 62% after. The number of patients who had normalized their blood pressure rose from 54% to 57%. There were also gains in smoking cessation – from 87% to 93%.
The only measure in which there was not significant improvement was in getting low-density lipoprotein (LDL) levels down to less than 100 mg/dL. Initially, 63% of patients achieved this measure; after the intervention, that had risen to just 64%.
To ensure that physicians weren’t just picking their best patients, the ABFM also surveyed patients, said Dr. Peterson. When asked about their care, at baseline, 76% said the doctor had checked their feet. After the intervention, that had risen to 90%. Patients getting eye exams rose from 70% to 80%. When asked if they had an HbA1c test, initially 92% said yes. After the process, 96% of patients said they’d had their blood sugar tested. Only 77% of patients knew their blood pressure goal at baseline. Post intervention, 86% were knowledgeable.
Dr. Peterson said the ABFM hoped to leverage the quality improvement aspect of the MOC process to help lower costs and improve patient care. In the future, the goal is to move the QI modules beyond a handful of patients to a physician’s full panel, complete with continuous feedback, he said.
On Twitter @aliciaault
BALTIMORE – Family physicians were able to improve clinical care for diabetics when they used self-directed quality improvement modules.
That’s the lesson from a study of some 8,000 family physicians who participated in the American Board of Family Medicine’s (ABFM) maintenance of certification (MOC) process. Part of that process includes a performance improvement module – called the Performance in Practice Module – and physicians can choose disease states for that module.
Dr. Lars Peterson, research director at the ABFM, presented the analysis of the initial experiences with the diabetes module at AcademyHealth’s annual research meeting here.
For the quality improvement part of the MOC process, physicians first complete a tutorial on quality improvement theory and methods. They then select 10 charts to abstract—generally, the first 10 patients with the particular condition--and choose up to seven quality measures for improvement. The quality measures come from the National Quality Forum, said Dr. Peterson.
Physicians submit their performance data to the ABFM; in return, physicians get a benchmarking report that compares their performance with other physicians, both before the intervention and after.
The 7,924 physicians analyzed for the study had been in practice an average 13 years and were 48 years old on average. They took an average of 6 months to complete the practice module. Three-quarters of the practices were in urban areas; 11% were large rural practices, and 8% were small rural practices.
Almost half the participants chose the diabetic foot exam and retina exam as the measure for improvement. Not surprisingly, these were the areas with the lowest performance metrics at baseline. Fewer than 15% chose blood pressure and hemoglobin A1c. The remainder chose other measures.
At baseline, only 68% of physicians conducted a foot exam. After going through the improvement process, 86% of physicians were looking at their patients’ feet. Only 56% of patients had a retina exam initially; after the module, 71% had gotten the exam.
There was also significant improvement in HbA1c control, with 60% in control before the intervention and 62% after. The number of patients who had normalized their blood pressure rose from 54% to 57%. There were also gains in smoking cessation – from 87% to 93%.
The only measure in which there was not significant improvement was in getting low-density lipoprotein (LDL) levels down to less than 100 mg/dL. Initially, 63% of patients achieved this measure; after the intervention, that had risen to just 64%.
To ensure that physicians weren’t just picking their best patients, the ABFM also surveyed patients, said Dr. Peterson. When asked about their care, at baseline, 76% said the doctor had checked their feet. After the intervention, that had risen to 90%. Patients getting eye exams rose from 70% to 80%. When asked if they had an HbA1c test, initially 92% said yes. After the process, 96% of patients said they’d had their blood sugar tested. Only 77% of patients knew their blood pressure goal at baseline. Post intervention, 86% were knowledgeable.
Dr. Peterson said the ABFM hoped to leverage the quality improvement aspect of the MOC process to help lower costs and improve patient care. In the future, the goal is to move the QI modules beyond a handful of patients to a physician’s full panel, complete with continuous feedback, he said.
On Twitter @aliciaault
AT ACADEMYHEALTH 2013
Major finding: After completing a self-improvement module, the number of physicians conducting a foot exam rose from 68% to 86%, and those conducting retina exams rose from 56% to 71%.
Data source: An observational study of the actions and quality outcomes of the first 7,924 physicians who completed the American Board of Family Medicine’s self-reported quality improvement module for diabetes.
Disclosures: Dr. Peterson and his colleagues reported having no financial disclosures.
Congressional committee takes on Part B drug cost cuts
WASHINGTON – Democrats and Republicans at a recent House hearing agreed on one thing: that budget cuts to Medicare Part B are hurting both doctors and patients.
At issue are automatic, across-the-board cuts under sequestration to both Medicare Part B payments for drugs administered in physicians’ offices and cuts to the fees physicians are paid to administer those drugs.
Rep. Joe Pitts (R-Pa.), chairman of the House Energy and Commerce Committee’s Subcommittee on Health, said that these sequestration cuts were not only putting the squeeze on physician practices, but also potentially harming patients.
"Reimbursement rates have caused the shift of some patient populations such as those with primary immune deficiency diseases and other rare diseases, from treatment in the physician office to treatment in the hospital outpatient department – arguably the worst setting for someone with a compromised immune system," he said at the subcommittee hearing held June 28.
When sequestration went into effect April 1, Medicare physician pay was cut 2%. Part B payments for drugs also were cut by 2%.
But the impact has been much greater, testified Dr. Barry Brooks, an oncologist based in Dallas. The two cuts together have amounted to a 28% reduction in payment for certain services, he said at the hearing. "It has put us underwater."
Rep. Renee Ellmers (R-N.C.), a member of the Health subcommittee, noted that she had introduced a bill to exempt Part B drugs from sequestration – the Cancer Patient Protection Act of 2013 (H.R. 1416), which at press time had 91 cosponsors in the House.
"I feel very strongly we need to pass this piece of legislation," Rep. Ellmers said. She added that while sequestration was necessary, it had resulted in unintended consequences, such as harming Medicare patients with cancer.
But Rep. Henry Waxman (D-Calif.), who also serves on the Health subcommittee, said that that had not been an unforeseen possibility. He said that sequestration should not have gone into effect, as "it was supposed to be so ridiculous that we would avoid it."
Meanwhile, he said he did see a need to potentially pay less for Part B drugs.
Last October, the Government Accountability Office analyzed the 55 highest-cost drugs paid for by Medicare Part B, and found that they represented 85% ($16.9 billion) of the almost $20 billion Part B spent on drugs in 2010, according to testimony from James Cosgrove, director of health care at the GAO.
The 10 most costly drugs accounted for about 45% of all Part B drug spending that year. The top 5 were epoetin-alfa (Epogen, for dialysis-related anemia), rituximab (Rituxan, for lymphomas and rheumatoid arthritis), ranibizumab (Lucentis, for age-related macular degeneration), bevacizumab (Avastin, for colorectal cancer, breast cancer, kidney cancer, and glioblastoma), and infliximab (Remicade, for rheumatoid arthritis, psoriatic arthritis, and Crohn’s disease).
"We should make sure Medicare is getting a good deal," Rep. Waxman said, suggesting that negotiations with drug makers or seeking rebates might be one way to cut costs.
Dr. Brooks also complained that hospitals eligible to buy drugs through the federal 340B discount program can get chemotherapy drugs at lower cost – and are reimbursed at a higher rate – that can community oncologists. Meanwhile, patients may have to travel farther to receive care at a hospital, and pay higher out-of-pocket costs, he said.
Another area of concern for oncologists, rheumatologists, and others who administer Part B drugs: the prompt pay discount. Medicare includes those discounts from manufacturers when it calculates how much it reimburses physicians, which essentially leads to a reduction in their pay. That policy has meant that oncologists haven’t been able to cover costs for years, Dr. Brooks said.
Rep. Ed Whitfield (R-Ky.) and Rep. Gene Green (D-Tex.) have introduced legislation to exclude those discounts. The bill, H.R. 800, has 56 cosponsors in the House, and a companion was introduced in the Senate by Pat Roberts (R-Kan.).
Community oncology practices are feeling the pressure. According to a recent survey by the Community Oncology Alliance, in the past 15 months, there has been a 20% increase in clinic closings and a 20% increase in practices that have become affiliated with or been bought by a hospital.
On Twitter @aliciaault
WASHINGTON – Democrats and Republicans at a recent House hearing agreed on one thing: that budget cuts to Medicare Part B are hurting both doctors and patients.
At issue are automatic, across-the-board cuts under sequestration to both Medicare Part B payments for drugs administered in physicians’ offices and cuts to the fees physicians are paid to administer those drugs.
Rep. Joe Pitts (R-Pa.), chairman of the House Energy and Commerce Committee’s Subcommittee on Health, said that these sequestration cuts were not only putting the squeeze on physician practices, but also potentially harming patients.
"Reimbursement rates have caused the shift of some patient populations such as those with primary immune deficiency diseases and other rare diseases, from treatment in the physician office to treatment in the hospital outpatient department – arguably the worst setting for someone with a compromised immune system," he said at the subcommittee hearing held June 28.
When sequestration went into effect April 1, Medicare physician pay was cut 2%. Part B payments for drugs also were cut by 2%.
But the impact has been much greater, testified Dr. Barry Brooks, an oncologist based in Dallas. The two cuts together have amounted to a 28% reduction in payment for certain services, he said at the hearing. "It has put us underwater."
Rep. Renee Ellmers (R-N.C.), a member of the Health subcommittee, noted that she had introduced a bill to exempt Part B drugs from sequestration – the Cancer Patient Protection Act of 2013 (H.R. 1416), which at press time had 91 cosponsors in the House.
"I feel very strongly we need to pass this piece of legislation," Rep. Ellmers said. She added that while sequestration was necessary, it had resulted in unintended consequences, such as harming Medicare patients with cancer.
But Rep. Henry Waxman (D-Calif.), who also serves on the Health subcommittee, said that that had not been an unforeseen possibility. He said that sequestration should not have gone into effect, as "it was supposed to be so ridiculous that we would avoid it."
Meanwhile, he said he did see a need to potentially pay less for Part B drugs.
Last October, the Government Accountability Office analyzed the 55 highest-cost drugs paid for by Medicare Part B, and found that they represented 85% ($16.9 billion) of the almost $20 billion Part B spent on drugs in 2010, according to testimony from James Cosgrove, director of health care at the GAO.
The 10 most costly drugs accounted for about 45% of all Part B drug spending that year. The top 5 were epoetin-alfa (Epogen, for dialysis-related anemia), rituximab (Rituxan, for lymphomas and rheumatoid arthritis), ranibizumab (Lucentis, for age-related macular degeneration), bevacizumab (Avastin, for colorectal cancer, breast cancer, kidney cancer, and glioblastoma), and infliximab (Remicade, for rheumatoid arthritis, psoriatic arthritis, and Crohn’s disease).
"We should make sure Medicare is getting a good deal," Rep. Waxman said, suggesting that negotiations with drug makers or seeking rebates might be one way to cut costs.
Dr. Brooks also complained that hospitals eligible to buy drugs through the federal 340B discount program can get chemotherapy drugs at lower cost – and are reimbursed at a higher rate – that can community oncologists. Meanwhile, patients may have to travel farther to receive care at a hospital, and pay higher out-of-pocket costs, he said.
Another area of concern for oncologists, rheumatologists, and others who administer Part B drugs: the prompt pay discount. Medicare includes those discounts from manufacturers when it calculates how much it reimburses physicians, which essentially leads to a reduction in their pay. That policy has meant that oncologists haven’t been able to cover costs for years, Dr. Brooks said.
Rep. Ed Whitfield (R-Ky.) and Rep. Gene Green (D-Tex.) have introduced legislation to exclude those discounts. The bill, H.R. 800, has 56 cosponsors in the House, and a companion was introduced in the Senate by Pat Roberts (R-Kan.).
Community oncology practices are feeling the pressure. According to a recent survey by the Community Oncology Alliance, in the past 15 months, there has been a 20% increase in clinic closings and a 20% increase in practices that have become affiliated with or been bought by a hospital.
On Twitter @aliciaault
WASHINGTON – Democrats and Republicans at a recent House hearing agreed on one thing: that budget cuts to Medicare Part B are hurting both doctors and patients.
At issue are automatic, across-the-board cuts under sequestration to both Medicare Part B payments for drugs administered in physicians’ offices and cuts to the fees physicians are paid to administer those drugs.
Rep. Joe Pitts (R-Pa.), chairman of the House Energy and Commerce Committee’s Subcommittee on Health, said that these sequestration cuts were not only putting the squeeze on physician practices, but also potentially harming patients.
"Reimbursement rates have caused the shift of some patient populations such as those with primary immune deficiency diseases and other rare diseases, from treatment in the physician office to treatment in the hospital outpatient department – arguably the worst setting for someone with a compromised immune system," he said at the subcommittee hearing held June 28.
When sequestration went into effect April 1, Medicare physician pay was cut 2%. Part B payments for drugs also were cut by 2%.
But the impact has been much greater, testified Dr. Barry Brooks, an oncologist based in Dallas. The two cuts together have amounted to a 28% reduction in payment for certain services, he said at the hearing. "It has put us underwater."
Rep. Renee Ellmers (R-N.C.), a member of the Health subcommittee, noted that she had introduced a bill to exempt Part B drugs from sequestration – the Cancer Patient Protection Act of 2013 (H.R. 1416), which at press time had 91 cosponsors in the House.
"I feel very strongly we need to pass this piece of legislation," Rep. Ellmers said. She added that while sequestration was necessary, it had resulted in unintended consequences, such as harming Medicare patients with cancer.
But Rep. Henry Waxman (D-Calif.), who also serves on the Health subcommittee, said that that had not been an unforeseen possibility. He said that sequestration should not have gone into effect, as "it was supposed to be so ridiculous that we would avoid it."
Meanwhile, he said he did see a need to potentially pay less for Part B drugs.
Last October, the Government Accountability Office analyzed the 55 highest-cost drugs paid for by Medicare Part B, and found that they represented 85% ($16.9 billion) of the almost $20 billion Part B spent on drugs in 2010, according to testimony from James Cosgrove, director of health care at the GAO.
The 10 most costly drugs accounted for about 45% of all Part B drug spending that year. The top 5 were epoetin-alfa (Epogen, for dialysis-related anemia), rituximab (Rituxan, for lymphomas and rheumatoid arthritis), ranibizumab (Lucentis, for age-related macular degeneration), bevacizumab (Avastin, for colorectal cancer, breast cancer, kidney cancer, and glioblastoma), and infliximab (Remicade, for rheumatoid arthritis, psoriatic arthritis, and Crohn’s disease).
"We should make sure Medicare is getting a good deal," Rep. Waxman said, suggesting that negotiations with drug makers or seeking rebates might be one way to cut costs.
Dr. Brooks also complained that hospitals eligible to buy drugs through the federal 340B discount program can get chemotherapy drugs at lower cost – and are reimbursed at a higher rate – that can community oncologists. Meanwhile, patients may have to travel farther to receive care at a hospital, and pay higher out-of-pocket costs, he said.
Another area of concern for oncologists, rheumatologists, and others who administer Part B drugs: the prompt pay discount. Medicare includes those discounts from manufacturers when it calculates how much it reimburses physicians, which essentially leads to a reduction in their pay. That policy has meant that oncologists haven’t been able to cover costs for years, Dr. Brooks said.
Rep. Ed Whitfield (R-Ky.) and Rep. Gene Green (D-Tex.) have introduced legislation to exclude those discounts. The bill, H.R. 800, has 56 cosponsors in the House, and a companion was introduced in the Senate by Pat Roberts (R-Kan.).
Community oncology practices are feeling the pressure. According to a recent survey by the Community Oncology Alliance, in the past 15 months, there has been a 20% increase in clinic closings and a 20% increase in practices that have become affiliated with or been bought by a hospital.
On Twitter @aliciaault
AT A HOUSE OF REPRESENTATIVES HEARING
AMA delegates decry ICD-10, EHRs
CHICAGO – Coding and computers were among key concerns for physician leaders at the American Medical Association’s annual House of Delegates meeting.
Resolutions from several delegations aimed to delay or scuttle the transition to the newest incarnation of the International Classification of Diseases, ICD-10.
Delegates from the American College of Rheumatology (ACR) introduced a resolution urging the association to keep up its campaign to stop ICD-10 implementation, specifically via federal legislation.
Without a statement supporting delay, there is a "perception out there that the AMA has essentially caved on the issue of ICD-10," said Dr. Gary Bryant, an ACR delegate. "Now that’s not my perception, but I believe it’s the perception, to some degree, among American physicians."
The House adopted instead a resolution calling for the AMA to support federal legislation to delay ICD-10 implementation for 2 years. During that time, payers would not be allowed to deny payment based on the specificity of the diagnosis, but they would be required to provide feedback in the case of an incorrect diagnosis. The resolution was brought by the Colorado delegation.
Dr. Reid Blackwelder, president-elect of the American Academy of Family Physicians, spoke in favor of the resolution.
"It’s not likely that we’re moving from ICD-9, we are." Instead, the resolution "allows our members to have a period of time to get used to the sticker shock," he said.
The AMA has estimated that the cost of implementing ICD-10 could range from $83,290 to more than $2.7 million per practice, depending on practice size.
Delegates also sought to slow the adoption of electronic health records, citing major problems with interoperability.
Karthik Sarmah, medical student alternate delegate in the California delegation, cited interoperability as a major concern.
"The lack of interoperability is the primary driver of why so many people in this room hate their EHR system," he said, adding that interoperability standards exist, but that there are no incentives for venders to create ways to allow physicians to share their patient data with each other.
Dr. Melissa Garretson, a delegate from the American Academy of Pediatrics, agreed.
"I can’t tell you the number of times I have to repeat labs," and CT scans because data can’t be accessed from other physicians, Dr. Garretson said. She called the lack of interoperability an unfunded mandate on physicians because the vendors aren’t making it possible. "If we force them to do this through legislation, it will finally happen."
Other delegates were skeptical.
"I have been waiting now for about 12 years for this interoperability to occur and I think I’ll either be retired or dead before it finally does," said Dr. Arthur E. Palamara, a vascular surgeon with the Florida delegation.
The House approved a resolution "seeking legislation or regulation to require all EHR vendors to use standard and interoperable software technology to enable cost-efficient use of electronic health records across all health care delivery systems, including institutional and community-based settings of care delivery."
On Twitter @aliciaault
CHICAGO – Coding and computers were among key concerns for physician leaders at the American Medical Association’s annual House of Delegates meeting.
Resolutions from several delegations aimed to delay or scuttle the transition to the newest incarnation of the International Classification of Diseases, ICD-10.
Delegates from the American College of Rheumatology (ACR) introduced a resolution urging the association to keep up its campaign to stop ICD-10 implementation, specifically via federal legislation.
Without a statement supporting delay, there is a "perception out there that the AMA has essentially caved on the issue of ICD-10," said Dr. Gary Bryant, an ACR delegate. "Now that’s not my perception, but I believe it’s the perception, to some degree, among American physicians."
The House adopted instead a resolution calling for the AMA to support federal legislation to delay ICD-10 implementation for 2 years. During that time, payers would not be allowed to deny payment based on the specificity of the diagnosis, but they would be required to provide feedback in the case of an incorrect diagnosis. The resolution was brought by the Colorado delegation.
Dr. Reid Blackwelder, president-elect of the American Academy of Family Physicians, spoke in favor of the resolution.
"It’s not likely that we’re moving from ICD-9, we are." Instead, the resolution "allows our members to have a period of time to get used to the sticker shock," he said.
The AMA has estimated that the cost of implementing ICD-10 could range from $83,290 to more than $2.7 million per practice, depending on practice size.
Delegates also sought to slow the adoption of electronic health records, citing major problems with interoperability.
Karthik Sarmah, medical student alternate delegate in the California delegation, cited interoperability as a major concern.
"The lack of interoperability is the primary driver of why so many people in this room hate their EHR system," he said, adding that interoperability standards exist, but that there are no incentives for venders to create ways to allow physicians to share their patient data with each other.
Dr. Melissa Garretson, a delegate from the American Academy of Pediatrics, agreed.
"I can’t tell you the number of times I have to repeat labs," and CT scans because data can’t be accessed from other physicians, Dr. Garretson said. She called the lack of interoperability an unfunded mandate on physicians because the vendors aren’t making it possible. "If we force them to do this through legislation, it will finally happen."
Other delegates were skeptical.
"I have been waiting now for about 12 years for this interoperability to occur and I think I’ll either be retired or dead before it finally does," said Dr. Arthur E. Palamara, a vascular surgeon with the Florida delegation.
The House approved a resolution "seeking legislation or regulation to require all EHR vendors to use standard and interoperable software technology to enable cost-efficient use of electronic health records across all health care delivery systems, including institutional and community-based settings of care delivery."
On Twitter @aliciaault
CHICAGO – Coding and computers were among key concerns for physician leaders at the American Medical Association’s annual House of Delegates meeting.
Resolutions from several delegations aimed to delay or scuttle the transition to the newest incarnation of the International Classification of Diseases, ICD-10.
Delegates from the American College of Rheumatology (ACR) introduced a resolution urging the association to keep up its campaign to stop ICD-10 implementation, specifically via federal legislation.
Without a statement supporting delay, there is a "perception out there that the AMA has essentially caved on the issue of ICD-10," said Dr. Gary Bryant, an ACR delegate. "Now that’s not my perception, but I believe it’s the perception, to some degree, among American physicians."
The House adopted instead a resolution calling for the AMA to support federal legislation to delay ICD-10 implementation for 2 years. During that time, payers would not be allowed to deny payment based on the specificity of the diagnosis, but they would be required to provide feedback in the case of an incorrect diagnosis. The resolution was brought by the Colorado delegation.
Dr. Reid Blackwelder, president-elect of the American Academy of Family Physicians, spoke in favor of the resolution.
"It’s not likely that we’re moving from ICD-9, we are." Instead, the resolution "allows our members to have a period of time to get used to the sticker shock," he said.
The AMA has estimated that the cost of implementing ICD-10 could range from $83,290 to more than $2.7 million per practice, depending on practice size.
Delegates also sought to slow the adoption of electronic health records, citing major problems with interoperability.
Karthik Sarmah, medical student alternate delegate in the California delegation, cited interoperability as a major concern.
"The lack of interoperability is the primary driver of why so many people in this room hate their EHR system," he said, adding that interoperability standards exist, but that there are no incentives for venders to create ways to allow physicians to share their patient data with each other.
Dr. Melissa Garretson, a delegate from the American Academy of Pediatrics, agreed.
"I can’t tell you the number of times I have to repeat labs," and CT scans because data can’t be accessed from other physicians, Dr. Garretson said. She called the lack of interoperability an unfunded mandate on physicians because the vendors aren’t making it possible. "If we force them to do this through legislation, it will finally happen."
Other delegates were skeptical.
"I have been waiting now for about 12 years for this interoperability to occur and I think I’ll either be retired or dead before it finally does," said Dr. Arthur E. Palamara, a vascular surgeon with the Florida delegation.
The House approved a resolution "seeking legislation or regulation to require all EHR vendors to use standard and interoperable software technology to enable cost-efficient use of electronic health records across all health care delivery systems, including institutional and community-based settings of care delivery."
On Twitter @aliciaault
AT THE AMA HOUSE OF DELEGATES