User login
Dermatologists: Beware the ‘insulin ball’
LAS VEGAS – The patient, a 61-year-old man, came to see a dermatologist here about subcutaneous masses on his left arm, abdomen, and on both thighs.
It didn’t take long for Curt Samlaska, MD, of the University of Nevada, Reno, to link the masses to the patient’s daily regimen of seven insulin injections.
But diagnosing the condition required more than asking a few questions. At first, the man appeared to suffer from lipohypertrophy – a lump caused by an accumulation of fat at the site of insulin injections. But, Dr. Samlaska told colleagues, the patient had a different condition that’s barely been discussed in the dermatologic literature – insulin-derived amyloidosis, also known as “insulin ball.”
“It’s probably much more prevalent than we currently appreciate,” said Dr. Samlaska, who spoke in a presentation at the Skin Disease Education Foundation’s annual Las Vegas Dermatology Seminar. “Many cases are not [fully] evaluated and thought to be lipohypertrophy.”
Dr. Samlaska’s patient had suffered from diabetes since age 23 and tightly controls his blood sugar through seven daily injections. He injects short-acting insulin into his arms and abdomen, and long-acting insulin into his thighs.
The masses began appearing about 10 years ago, he told Dr. Samlaska, and he’s suffered more pain while injecting them over time. But the masses are easier to grasp during injections, and the patient’s body did not offer many other sites for injections.
, almost all in endocrinology journals. Ninety percent have a single lump, most commonly in the abdomen, and most have poor glycemic control, he said. (His patient is an outlier.)
Research suggests that insulin balls absorb about 34% of the insulin that’s injected, meaning that patients must inject more than usual to get the same effect. Be careful to advise patients about this, Dr. Samlaska said, because they might try alternative injection sites and get a sudden unexpected flood of insulin – potentially causing hypoglycemia.
He added that another drug – the HIV fusion inhibitor enfuvirtide – also has been linked to amyloidosis.
Pathology can offer insight into whether a mass is an insulin ball or a case of lipohypertrophy, he said. “They’re difficult to distinguish on clinical grounds,” he said, although lipohypertrophy masses are firmer, and they shrink when patients stop injecting insulin. Insulin balls do not.
The treatment for insulin balls is surgical excision, he said. “It’s very easy to do. With the extrusion technique, it comes out like a cheese, like a cyst.”
He said his patient was scheduled to soon undergo excision treatment.
Dr. Samlaska reported no relevant disclosures. SDEF and this news organization are owned by the same parent company.
LAS VEGAS – The patient, a 61-year-old man, came to see a dermatologist here about subcutaneous masses on his left arm, abdomen, and on both thighs.
It didn’t take long for Curt Samlaska, MD, of the University of Nevada, Reno, to link the masses to the patient’s daily regimen of seven insulin injections.
But diagnosing the condition required more than asking a few questions. At first, the man appeared to suffer from lipohypertrophy – a lump caused by an accumulation of fat at the site of insulin injections. But, Dr. Samlaska told colleagues, the patient had a different condition that’s barely been discussed in the dermatologic literature – insulin-derived amyloidosis, also known as “insulin ball.”
“It’s probably much more prevalent than we currently appreciate,” said Dr. Samlaska, who spoke in a presentation at the Skin Disease Education Foundation’s annual Las Vegas Dermatology Seminar. “Many cases are not [fully] evaluated and thought to be lipohypertrophy.”
Dr. Samlaska’s patient had suffered from diabetes since age 23 and tightly controls his blood sugar through seven daily injections. He injects short-acting insulin into his arms and abdomen, and long-acting insulin into his thighs.
The masses began appearing about 10 years ago, he told Dr. Samlaska, and he’s suffered more pain while injecting them over time. But the masses are easier to grasp during injections, and the patient’s body did not offer many other sites for injections.
, almost all in endocrinology journals. Ninety percent have a single lump, most commonly in the abdomen, and most have poor glycemic control, he said. (His patient is an outlier.)
Research suggests that insulin balls absorb about 34% of the insulin that’s injected, meaning that patients must inject more than usual to get the same effect. Be careful to advise patients about this, Dr. Samlaska said, because they might try alternative injection sites and get a sudden unexpected flood of insulin – potentially causing hypoglycemia.
He added that another drug – the HIV fusion inhibitor enfuvirtide – also has been linked to amyloidosis.
Pathology can offer insight into whether a mass is an insulin ball or a case of lipohypertrophy, he said. “They’re difficult to distinguish on clinical grounds,” he said, although lipohypertrophy masses are firmer, and they shrink when patients stop injecting insulin. Insulin balls do not.
The treatment for insulin balls is surgical excision, he said. “It’s very easy to do. With the extrusion technique, it comes out like a cheese, like a cyst.”
He said his patient was scheduled to soon undergo excision treatment.
Dr. Samlaska reported no relevant disclosures. SDEF and this news organization are owned by the same parent company.
LAS VEGAS – The patient, a 61-year-old man, came to see a dermatologist here about subcutaneous masses on his left arm, abdomen, and on both thighs.
It didn’t take long for Curt Samlaska, MD, of the University of Nevada, Reno, to link the masses to the patient’s daily regimen of seven insulin injections.
But diagnosing the condition required more than asking a few questions. At first, the man appeared to suffer from lipohypertrophy – a lump caused by an accumulation of fat at the site of insulin injections. But, Dr. Samlaska told colleagues, the patient had a different condition that’s barely been discussed in the dermatologic literature – insulin-derived amyloidosis, also known as “insulin ball.”
“It’s probably much more prevalent than we currently appreciate,” said Dr. Samlaska, who spoke in a presentation at the Skin Disease Education Foundation’s annual Las Vegas Dermatology Seminar. “Many cases are not [fully] evaluated and thought to be lipohypertrophy.”
Dr. Samlaska’s patient had suffered from diabetes since age 23 and tightly controls his blood sugar through seven daily injections. He injects short-acting insulin into his arms and abdomen, and long-acting insulin into his thighs.
The masses began appearing about 10 years ago, he told Dr. Samlaska, and he’s suffered more pain while injecting them over time. But the masses are easier to grasp during injections, and the patient’s body did not offer many other sites for injections.
, almost all in endocrinology journals. Ninety percent have a single lump, most commonly in the abdomen, and most have poor glycemic control, he said. (His patient is an outlier.)
Research suggests that insulin balls absorb about 34% of the insulin that’s injected, meaning that patients must inject more than usual to get the same effect. Be careful to advise patients about this, Dr. Samlaska said, because they might try alternative injection sites and get a sudden unexpected flood of insulin – potentially causing hypoglycemia.
He added that another drug – the HIV fusion inhibitor enfuvirtide – also has been linked to amyloidosis.
Pathology can offer insight into whether a mass is an insulin ball or a case of lipohypertrophy, he said. “They’re difficult to distinguish on clinical grounds,” he said, although lipohypertrophy masses are firmer, and they shrink when patients stop injecting insulin. Insulin balls do not.
The treatment for insulin balls is surgical excision, he said. “It’s very easy to do. With the extrusion technique, it comes out like a cheese, like a cyst.”
He said his patient was scheduled to soon undergo excision treatment.
Dr. Samlaska reported no relevant disclosures. SDEF and this news organization are owned by the same parent company.
REPORTING FROM SDEF LAS VEGAS DERMATOLOGY SEMINAR
Sweaty patient? Treatments require patient education
LAS VEGAS – at Skin Disease Education Foundation’s annual Las Vegas Dermatology Seminar.
During an examination for another condition, he said, patients may be “sweating and dripping.” However, “you look over that diagnosis because that’s not what they’re there for,” said Dr. Desai, a dermatologist at the University of Texas Southwestern Medical Center in Dallas.
He described one of his patients, who only revealed that she suffered from “horrible, devastating” hyperhidrosis after he’d treated her for years for melasma. The sweating especially affected her because it prevented her from wearing the skin-exposing clothing of her Indian culture.
Delays in treatment are common in hyperhidrosis, which is believed to affect 5% of the world’s population. According to Dr. Desai, research suggests that 85% of patients with hyperhidrosis wait more than 3 years to bring it up with doctors, and half wait more than a decade.
There are many treatments for hyperhidrosis. Some are fairly simple: over-the-counter or prescription antiperspirants, said Dr. Desai, who likes the over-the-counter brand Certain Dri), iontophoresis (application of electric current), topical anticholinergics (including glycopyrronium tosylate cloth wipes, recently approved by the FDA for topical treatment of primary axillary hyperhidrosis for ages 9 years and older), and systemic management. Others are minimally invasive: Botox injections and the miraDry medical device (which relies on thermolysis). And surgical strategies may be an option for severe cases.
On its website, the International Hyperhidrosis Society provides a chart of options for hyperhidrosis in various parts of the body. Treatments tend to focus on the underarms, however, and “we’ve got huge unmet needs for patient options,” Dr. Desai said.
- During his presentation, he provided the following pearls regarding hyperhidrosis treatments:
- Distinguish between antiperspirants, which block sweating, and deodorants, which cover up body odor. “Sometimes I get caught up in the middle of a busy office visit and use these terms interchangeably. They’re really different, but patients and the public tend to equate those together,” he commented.
- Make sure patients understand how to properly use antiperspirants and explain that antiperspirants must be applied to dry skin. “Antiperspirant is forming a clog in the drain” to prevent the release of sweat, he said. “If you apply it to wet skin, you will block that chemical reaction in the duct.”
- Massage in the antiperspirant, he advises, and don’t occlude the skin. Apply twice daily, including before bedtime. “They can use antiperspirant on the hands and the bottom of the feet,”Dr. Desai said. “You want to ensure that they’re using the spray on the surface and in the web space. They can also use antiperspirants on the face, but avoid contact with the eyes.”
- Be careful if you prescribe glycopyrronium cloths off label. These wipes are helpful and they can be used outside the FDA-approved use in the underarms, said Dr. Desai, who said he has palmar hyperhidrosis and has successfully used them on his palms, but he hasn’t found them to be helpful on the soles of his feet.
Dr. Desai recommends 5-minute applications on the palms because the treatment can irritate the face and eyes.
Linda F. Stein Gold, MD, of Henry Ford Health System in Detroit, told the audience about the case of a teacher who touched his eyes after applying the treatment. He went to school, felt ill, and ended up in an emergency department because he had an enlarged pupil. “You just have to tell people this can happen,” she said.
Dr. Desai reported no relevant disclosures.
SDEF and this news organization are owned by the same parent company.
LAS VEGAS – at Skin Disease Education Foundation’s annual Las Vegas Dermatology Seminar.
During an examination for another condition, he said, patients may be “sweating and dripping.” However, “you look over that diagnosis because that’s not what they’re there for,” said Dr. Desai, a dermatologist at the University of Texas Southwestern Medical Center in Dallas.
He described one of his patients, who only revealed that she suffered from “horrible, devastating” hyperhidrosis after he’d treated her for years for melasma. The sweating especially affected her because it prevented her from wearing the skin-exposing clothing of her Indian culture.
Delays in treatment are common in hyperhidrosis, which is believed to affect 5% of the world’s population. According to Dr. Desai, research suggests that 85% of patients with hyperhidrosis wait more than 3 years to bring it up with doctors, and half wait more than a decade.
There are many treatments for hyperhidrosis. Some are fairly simple: over-the-counter or prescription antiperspirants, said Dr. Desai, who likes the over-the-counter brand Certain Dri), iontophoresis (application of electric current), topical anticholinergics (including glycopyrronium tosylate cloth wipes, recently approved by the FDA for topical treatment of primary axillary hyperhidrosis for ages 9 years and older), and systemic management. Others are minimally invasive: Botox injections and the miraDry medical device (which relies on thermolysis). And surgical strategies may be an option for severe cases.
On its website, the International Hyperhidrosis Society provides a chart of options for hyperhidrosis in various parts of the body. Treatments tend to focus on the underarms, however, and “we’ve got huge unmet needs for patient options,” Dr. Desai said.
- During his presentation, he provided the following pearls regarding hyperhidrosis treatments:
- Distinguish between antiperspirants, which block sweating, and deodorants, which cover up body odor. “Sometimes I get caught up in the middle of a busy office visit and use these terms interchangeably. They’re really different, but patients and the public tend to equate those together,” he commented.
- Make sure patients understand how to properly use antiperspirants and explain that antiperspirants must be applied to dry skin. “Antiperspirant is forming a clog in the drain” to prevent the release of sweat, he said. “If you apply it to wet skin, you will block that chemical reaction in the duct.”
- Massage in the antiperspirant, he advises, and don’t occlude the skin. Apply twice daily, including before bedtime. “They can use antiperspirant on the hands and the bottom of the feet,”Dr. Desai said. “You want to ensure that they’re using the spray on the surface and in the web space. They can also use antiperspirants on the face, but avoid contact with the eyes.”
- Be careful if you prescribe glycopyrronium cloths off label. These wipes are helpful and they can be used outside the FDA-approved use in the underarms, said Dr. Desai, who said he has palmar hyperhidrosis and has successfully used them on his palms, but he hasn’t found them to be helpful on the soles of his feet.
Dr. Desai recommends 5-minute applications on the palms because the treatment can irritate the face and eyes.
Linda F. Stein Gold, MD, of Henry Ford Health System in Detroit, told the audience about the case of a teacher who touched his eyes after applying the treatment. He went to school, felt ill, and ended up in an emergency department because he had an enlarged pupil. “You just have to tell people this can happen,” she said.
Dr. Desai reported no relevant disclosures.
SDEF and this news organization are owned by the same parent company.
LAS VEGAS – at Skin Disease Education Foundation’s annual Las Vegas Dermatology Seminar.
During an examination for another condition, he said, patients may be “sweating and dripping.” However, “you look over that diagnosis because that’s not what they’re there for,” said Dr. Desai, a dermatologist at the University of Texas Southwestern Medical Center in Dallas.
He described one of his patients, who only revealed that she suffered from “horrible, devastating” hyperhidrosis after he’d treated her for years for melasma. The sweating especially affected her because it prevented her from wearing the skin-exposing clothing of her Indian culture.
Delays in treatment are common in hyperhidrosis, which is believed to affect 5% of the world’s population. According to Dr. Desai, research suggests that 85% of patients with hyperhidrosis wait more than 3 years to bring it up with doctors, and half wait more than a decade.
There are many treatments for hyperhidrosis. Some are fairly simple: over-the-counter or prescription antiperspirants, said Dr. Desai, who likes the over-the-counter brand Certain Dri), iontophoresis (application of electric current), topical anticholinergics (including glycopyrronium tosylate cloth wipes, recently approved by the FDA for topical treatment of primary axillary hyperhidrosis for ages 9 years and older), and systemic management. Others are minimally invasive: Botox injections and the miraDry medical device (which relies on thermolysis). And surgical strategies may be an option for severe cases.
On its website, the International Hyperhidrosis Society provides a chart of options for hyperhidrosis in various parts of the body. Treatments tend to focus on the underarms, however, and “we’ve got huge unmet needs for patient options,” Dr. Desai said.
- During his presentation, he provided the following pearls regarding hyperhidrosis treatments:
- Distinguish between antiperspirants, which block sweating, and deodorants, which cover up body odor. “Sometimes I get caught up in the middle of a busy office visit and use these terms interchangeably. They’re really different, but patients and the public tend to equate those together,” he commented.
- Make sure patients understand how to properly use antiperspirants and explain that antiperspirants must be applied to dry skin. “Antiperspirant is forming a clog in the drain” to prevent the release of sweat, he said. “If you apply it to wet skin, you will block that chemical reaction in the duct.”
- Massage in the antiperspirant, he advises, and don’t occlude the skin. Apply twice daily, including before bedtime. “They can use antiperspirant on the hands and the bottom of the feet,”Dr. Desai said. “You want to ensure that they’re using the spray on the surface and in the web space. They can also use antiperspirants on the face, but avoid contact with the eyes.”
- Be careful if you prescribe glycopyrronium cloths off label. These wipes are helpful and they can be used outside the FDA-approved use in the underarms, said Dr. Desai, who said he has palmar hyperhidrosis and has successfully used them on his palms, but he hasn’t found them to be helpful on the soles of his feet.
Dr. Desai recommends 5-minute applications on the palms because the treatment can irritate the face and eyes.
Linda F. Stein Gold, MD, of Henry Ford Health System in Detroit, told the audience about the case of a teacher who touched his eyes after applying the treatment. He went to school, felt ill, and ended up in an emergency department because he had an enlarged pupil. “You just have to tell people this can happen,” she said.
Dr. Desai reported no relevant disclosures.
SDEF and this news organization are owned by the same parent company.
REPORTING FROM SDEF LAS VEGAS DERMATOLOGY SEMINAR
Hot tips on uncovering the causes of sweating
LAS VEGAS – It is important to think outside the box and consider whether secondary causes of hyperhidrosis are at play when a patient complains of sweating too much, a dermatologist told his colleagues.
“Look at where the patient fits into the sweating paradigm,” advised Seemal R. Desai, MD, of University of Texas Southwestern Medical Center in Dallas, and consider factors such as where and how often patients are oversweating.
In cases of secondary hyperhidrosis – those that are caused by another condition – said Dr. Desai, who spoke in a presentation at Skin Disease Education Foundation’s annual Las Vegas Dermatology Seminar.
According to Dr. Desai, the answers to several questions can help pinpoint a diagnosis of primary hyperhidrosis (also known as focal or primary focal hyperhidrosis) or secondary hyperhidrosis:
- Where does the sweating occur?
Sweating occurs over large parts of the body in patients with secondary hyperhidrosis, Dr. Desai said, although it is typically limited to certain areas, such as the armpits, palms, or soles in the primary form.
- When did the sweating begin?
When sweating begins in adulthood, he said, there’s a good chance that it has a secondary cause. Sweating that began in childhood is more likely to be the primary form.
- How does sweating occur at night?
Dr. Desai advised: “Ask about sleep patterns. Do you sweat during your sleep or wake up feeling like you’re sweating?” Sweating throughout a sleep cycle – not “night sweats” that are brief in nature – indicate a probable secondary cause, he said.
According to Dr. Desai, the causes of secondary hyperhidrosis are numerous, including hypoglycemia, neural tumors, and cardiovascular conditions. “Typically, if I’m trying to figure out why a patient is having generalized sweating, the No. 1 cause is medications.”
Dr. Desai reported no relevant disclosures. SDEF and this news organization are owned by the same parent company.
LAS VEGAS – It is important to think outside the box and consider whether secondary causes of hyperhidrosis are at play when a patient complains of sweating too much, a dermatologist told his colleagues.
“Look at where the patient fits into the sweating paradigm,” advised Seemal R. Desai, MD, of University of Texas Southwestern Medical Center in Dallas, and consider factors such as where and how often patients are oversweating.
In cases of secondary hyperhidrosis – those that are caused by another condition – said Dr. Desai, who spoke in a presentation at Skin Disease Education Foundation’s annual Las Vegas Dermatology Seminar.
According to Dr. Desai, the answers to several questions can help pinpoint a diagnosis of primary hyperhidrosis (also known as focal or primary focal hyperhidrosis) or secondary hyperhidrosis:
- Where does the sweating occur?
Sweating occurs over large parts of the body in patients with secondary hyperhidrosis, Dr. Desai said, although it is typically limited to certain areas, such as the armpits, palms, or soles in the primary form.
- When did the sweating begin?
When sweating begins in adulthood, he said, there’s a good chance that it has a secondary cause. Sweating that began in childhood is more likely to be the primary form.
- How does sweating occur at night?
Dr. Desai advised: “Ask about sleep patterns. Do you sweat during your sleep or wake up feeling like you’re sweating?” Sweating throughout a sleep cycle – not “night sweats” that are brief in nature – indicate a probable secondary cause, he said.
According to Dr. Desai, the causes of secondary hyperhidrosis are numerous, including hypoglycemia, neural tumors, and cardiovascular conditions. “Typically, if I’m trying to figure out why a patient is having generalized sweating, the No. 1 cause is medications.”
Dr. Desai reported no relevant disclosures. SDEF and this news organization are owned by the same parent company.
LAS VEGAS – It is important to think outside the box and consider whether secondary causes of hyperhidrosis are at play when a patient complains of sweating too much, a dermatologist told his colleagues.
“Look at where the patient fits into the sweating paradigm,” advised Seemal R. Desai, MD, of University of Texas Southwestern Medical Center in Dallas, and consider factors such as where and how often patients are oversweating.
In cases of secondary hyperhidrosis – those that are caused by another condition – said Dr. Desai, who spoke in a presentation at Skin Disease Education Foundation’s annual Las Vegas Dermatology Seminar.
According to Dr. Desai, the answers to several questions can help pinpoint a diagnosis of primary hyperhidrosis (also known as focal or primary focal hyperhidrosis) or secondary hyperhidrosis:
- Where does the sweating occur?
Sweating occurs over large parts of the body in patients with secondary hyperhidrosis, Dr. Desai said, although it is typically limited to certain areas, such as the armpits, palms, or soles in the primary form.
- When did the sweating begin?
When sweating begins in adulthood, he said, there’s a good chance that it has a secondary cause. Sweating that began in childhood is more likely to be the primary form.
- How does sweating occur at night?
Dr. Desai advised: “Ask about sleep patterns. Do you sweat during your sleep or wake up feeling like you’re sweating?” Sweating throughout a sleep cycle – not “night sweats” that are brief in nature – indicate a probable secondary cause, he said.
According to Dr. Desai, the causes of secondary hyperhidrosis are numerous, including hypoglycemia, neural tumors, and cardiovascular conditions. “Typically, if I’m trying to figure out why a patient is having generalized sweating, the No. 1 cause is medications.”
Dr. Desai reported no relevant disclosures. SDEF and this news organization are owned by the same parent company.
REPORTING FROM SDEF LAS VEGAS DERMATOLOGY SEMINAR
Serum test sheds light on Merkel cell carcinoma
LAS VEGAS – Merkel cell carcinoma, an extremely rare form of skin cancer, is often caused by a subclinical virus that routinely inhabits the skin. Now, a serum test of virus antibody levels is offering insight into the state of the disease, according to one dermatologist.
“If you have these antibodies, you have a better prognosis. You can follow those antibodies to test for recurrence or progression,” Isaac Brownell, MD, PhD, of the Dermatology Branch of the National Institutes of Health said at Skin Disease Education Foundation’s annual Las Vegas Dermatology Seminar.
The cancer appears in the skin’s Merkel cells, which contribute to our sense of touch by helping us to discriminate textures. “When you put your hand in your pocket, and you can tell the difference between the front and back of a quarter,” he said, “you’re using the Merkel cells in your fingertips.”
Only about 2,500 cases of Merkel cell carcinoma appear in the United States each year, Dr. Brownell said. It appears more often in elderly white patients, is more common in men than women, and is more likely among immunosuppressed patients, whose risk is increased 15- to 20-fold. Cases are more common in sunnier regions – at least in men – and lesions frequently appear on the head, face, and neck.
Five-year survival is estimated at 51% if the cancer is localized, according to a 2016 study of 9,387 cases that Dr. Brownell highlighted. But survival declines dramatically if it has spread to lymph nodes or distant sites (Ann Surg Oncol. 2016 Oct;23[11]:3564-71).
In recent years, researchers have linked 80% of Merkel cell carcinoma cases to the Merkel cell polyomavirus, he said. The virus normally inhabits our skin with no ill effects, he said. “We all have this virus on our skin. It’s everywhere, and even children have antibodies,” he said. But mutations can lead to Merkel cell carcinoma.
Does it matter if cases are polyomavirus positive or polyomavirus negative? Not really, Dr. Brownell said, since the presence of the virus doesn’t appear to affect overall prognosis. However, he said, serum antibody testing can be helpful in polyomavirus-positive patients because it offers insight into prognosis and tumor burden. For example, “if the baseline titer falls and then starts to go up, they’re likely to have a recurrence, and you’ll want to look out for that,” he said.
Dr. Brownell offered another bit of advice: Be prepared to respond to patients who worry that they have a contagious virus and could be a danger to others. The proper answer, he said, is this: “You don’t have to worry about infecting people. Your tumor is not making the virus, you’re not infectious, and we have the virus on us already.”
For more information about the antibody test, visit merkelcell.org/sero.
Dr. Brownell reported having no relevant disclosures. SDEF and this news organization are owned by the same parent company.
LAS VEGAS – Merkel cell carcinoma, an extremely rare form of skin cancer, is often caused by a subclinical virus that routinely inhabits the skin. Now, a serum test of virus antibody levels is offering insight into the state of the disease, according to one dermatologist.
“If you have these antibodies, you have a better prognosis. You can follow those antibodies to test for recurrence or progression,” Isaac Brownell, MD, PhD, of the Dermatology Branch of the National Institutes of Health said at Skin Disease Education Foundation’s annual Las Vegas Dermatology Seminar.
The cancer appears in the skin’s Merkel cells, which contribute to our sense of touch by helping us to discriminate textures. “When you put your hand in your pocket, and you can tell the difference between the front and back of a quarter,” he said, “you’re using the Merkel cells in your fingertips.”
Only about 2,500 cases of Merkel cell carcinoma appear in the United States each year, Dr. Brownell said. It appears more often in elderly white patients, is more common in men than women, and is more likely among immunosuppressed patients, whose risk is increased 15- to 20-fold. Cases are more common in sunnier regions – at least in men – and lesions frequently appear on the head, face, and neck.
Five-year survival is estimated at 51% if the cancer is localized, according to a 2016 study of 9,387 cases that Dr. Brownell highlighted. But survival declines dramatically if it has spread to lymph nodes or distant sites (Ann Surg Oncol. 2016 Oct;23[11]:3564-71).
In recent years, researchers have linked 80% of Merkel cell carcinoma cases to the Merkel cell polyomavirus, he said. The virus normally inhabits our skin with no ill effects, he said. “We all have this virus on our skin. It’s everywhere, and even children have antibodies,” he said. But mutations can lead to Merkel cell carcinoma.
Does it matter if cases are polyomavirus positive or polyomavirus negative? Not really, Dr. Brownell said, since the presence of the virus doesn’t appear to affect overall prognosis. However, he said, serum antibody testing can be helpful in polyomavirus-positive patients because it offers insight into prognosis and tumor burden. For example, “if the baseline titer falls and then starts to go up, they’re likely to have a recurrence, and you’ll want to look out for that,” he said.
Dr. Brownell offered another bit of advice: Be prepared to respond to patients who worry that they have a contagious virus and could be a danger to others. The proper answer, he said, is this: “You don’t have to worry about infecting people. Your tumor is not making the virus, you’re not infectious, and we have the virus on us already.”
For more information about the antibody test, visit merkelcell.org/sero.
Dr. Brownell reported having no relevant disclosures. SDEF and this news organization are owned by the same parent company.
LAS VEGAS – Merkel cell carcinoma, an extremely rare form of skin cancer, is often caused by a subclinical virus that routinely inhabits the skin. Now, a serum test of virus antibody levels is offering insight into the state of the disease, according to one dermatologist.
“If you have these antibodies, you have a better prognosis. You can follow those antibodies to test for recurrence or progression,” Isaac Brownell, MD, PhD, of the Dermatology Branch of the National Institutes of Health said at Skin Disease Education Foundation’s annual Las Vegas Dermatology Seminar.
The cancer appears in the skin’s Merkel cells, which contribute to our sense of touch by helping us to discriminate textures. “When you put your hand in your pocket, and you can tell the difference between the front and back of a quarter,” he said, “you’re using the Merkel cells in your fingertips.”
Only about 2,500 cases of Merkel cell carcinoma appear in the United States each year, Dr. Brownell said. It appears more often in elderly white patients, is more common in men than women, and is more likely among immunosuppressed patients, whose risk is increased 15- to 20-fold. Cases are more common in sunnier regions – at least in men – and lesions frequently appear on the head, face, and neck.
Five-year survival is estimated at 51% if the cancer is localized, according to a 2016 study of 9,387 cases that Dr. Brownell highlighted. But survival declines dramatically if it has spread to lymph nodes or distant sites (Ann Surg Oncol. 2016 Oct;23[11]:3564-71).
In recent years, researchers have linked 80% of Merkel cell carcinoma cases to the Merkel cell polyomavirus, he said. The virus normally inhabits our skin with no ill effects, he said. “We all have this virus on our skin. It’s everywhere, and even children have antibodies,” he said. But mutations can lead to Merkel cell carcinoma.
Does it matter if cases are polyomavirus positive or polyomavirus negative? Not really, Dr. Brownell said, since the presence of the virus doesn’t appear to affect overall prognosis. However, he said, serum antibody testing can be helpful in polyomavirus-positive patients because it offers insight into prognosis and tumor burden. For example, “if the baseline titer falls and then starts to go up, they’re likely to have a recurrence, and you’ll want to look out for that,” he said.
Dr. Brownell offered another bit of advice: Be prepared to respond to patients who worry that they have a contagious virus and could be a danger to others. The proper answer, he said, is this: “You don’t have to worry about infecting people. Your tumor is not making the virus, you’re not infectious, and we have the virus on us already.”
For more information about the antibody test, visit merkelcell.org/sero.
Dr. Brownell reported having no relevant disclosures. SDEF and this news organization are owned by the same parent company.
REPORTING FROM SDEF LAS VEGAS DERMATOLOGY SEMINAR
Don’t leave dermatomyositis to the rheumatologists
LAS VEGAS – When she brings up dermatomyositis in the context of dermatology, Alisa Femia, MD, often hears from trainees and medical students who assume that this is a condition for rheumatologists to diagnose and treat. That’s not true: Dermatologists need to watch for this potentially fatal connective tissue disorder because they may see it first, she said at Skin Disease Education Foundation’s annual Las Vegas Dermatology Seminar.
“A fifth are clinically amyopathic,” and they may not initially see a rheumatologist, said Dr. Femia, director of inpatient dermatology at the department of dermatology, New York University. “They have normal muscle enzymes and no muscle weakness. It really puts them in our care as dermatologists.”
The challenge is that patient presentations can be subtle, but the stakes may be high, she added. “If we catch them early and treat some of these patients aggressively, we can save their lives.”
During the presentation, :
- Don’t rely on tests like biopsies to absolutely tell you what’s going on. “Clinical examination is the most important test to establish the diagnosis,” she said. “If you’re suspecting dermatomyositis ... get the patient in a gown [for a full-body exam] and look for all the signs that might not be as prominent as they are in our textbooks.”
- Look for the “butterfly” rash on the midface that is unique because it spares the nasolabial folds. “It looks like someone took an eraser and wiped out those areas,” Dr. Femia said. “This is important to help us nail down the diagnosis.”
- Other telltale signs, she said, include erythema on the extensor surfaces of digits, severe itching in the scalp, and a rash on the eyelids.
- Be aware of pulmonary involvement, including interstitial lung disease. In some cases, patients and their physicians wrongly believe that patients with dermatomyositis have asthma or pneumonia. “Pulmonologists are not necessarily aware of lung disease associated with dermatomyositis,” she said.
It’s wise to refer patients with dermatomyositis for malignancy and lung disease screening even if they don’t show signs of muscular involvement. “There’s no significant difference in rates of malignancy or lung disease in classic versus amyopathic dermatomyositis.”
Keep the MDA5 form of dermatomyositis in mind, Dr. Femia said. Anti–melanoma differentiation–associated gene 5 dermatomyositis is linked to rapidly progressive interstitial lung disease, alopecia, arthritis and oral lacerations. “Initially, it can have features of lupus, and the patient can be on immunosuppressive therapy, which mitigates diagnostic findings.”
Dr. Femia disclosed serving as principal investigator for a clinical trial in cutaneous dermatomyositis therapy.
SDEF and this news organization are owned by the same parent company.
LAS VEGAS – When she brings up dermatomyositis in the context of dermatology, Alisa Femia, MD, often hears from trainees and medical students who assume that this is a condition for rheumatologists to diagnose and treat. That’s not true: Dermatologists need to watch for this potentially fatal connective tissue disorder because they may see it first, she said at Skin Disease Education Foundation’s annual Las Vegas Dermatology Seminar.
“A fifth are clinically amyopathic,” and they may not initially see a rheumatologist, said Dr. Femia, director of inpatient dermatology at the department of dermatology, New York University. “They have normal muscle enzymes and no muscle weakness. It really puts them in our care as dermatologists.”
The challenge is that patient presentations can be subtle, but the stakes may be high, she added. “If we catch them early and treat some of these patients aggressively, we can save their lives.”
During the presentation, :
- Don’t rely on tests like biopsies to absolutely tell you what’s going on. “Clinical examination is the most important test to establish the diagnosis,” she said. “If you’re suspecting dermatomyositis ... get the patient in a gown [for a full-body exam] and look for all the signs that might not be as prominent as they are in our textbooks.”
- Look for the “butterfly” rash on the midface that is unique because it spares the nasolabial folds. “It looks like someone took an eraser and wiped out those areas,” Dr. Femia said. “This is important to help us nail down the diagnosis.”
- Other telltale signs, she said, include erythema on the extensor surfaces of digits, severe itching in the scalp, and a rash on the eyelids.
- Be aware of pulmonary involvement, including interstitial lung disease. In some cases, patients and their physicians wrongly believe that patients with dermatomyositis have asthma or pneumonia. “Pulmonologists are not necessarily aware of lung disease associated with dermatomyositis,” she said.
It’s wise to refer patients with dermatomyositis for malignancy and lung disease screening even if they don’t show signs of muscular involvement. “There’s no significant difference in rates of malignancy or lung disease in classic versus amyopathic dermatomyositis.”
Keep the MDA5 form of dermatomyositis in mind, Dr. Femia said. Anti–melanoma differentiation–associated gene 5 dermatomyositis is linked to rapidly progressive interstitial lung disease, alopecia, arthritis and oral lacerations. “Initially, it can have features of lupus, and the patient can be on immunosuppressive therapy, which mitigates diagnostic findings.”
Dr. Femia disclosed serving as principal investigator for a clinical trial in cutaneous dermatomyositis therapy.
SDEF and this news organization are owned by the same parent company.
LAS VEGAS – When she brings up dermatomyositis in the context of dermatology, Alisa Femia, MD, often hears from trainees and medical students who assume that this is a condition for rheumatologists to diagnose and treat. That’s not true: Dermatologists need to watch for this potentially fatal connective tissue disorder because they may see it first, she said at Skin Disease Education Foundation’s annual Las Vegas Dermatology Seminar.
“A fifth are clinically amyopathic,” and they may not initially see a rheumatologist, said Dr. Femia, director of inpatient dermatology at the department of dermatology, New York University. “They have normal muscle enzymes and no muscle weakness. It really puts them in our care as dermatologists.”
The challenge is that patient presentations can be subtle, but the stakes may be high, she added. “If we catch them early and treat some of these patients aggressively, we can save their lives.”
During the presentation, :
- Don’t rely on tests like biopsies to absolutely tell you what’s going on. “Clinical examination is the most important test to establish the diagnosis,” she said. “If you’re suspecting dermatomyositis ... get the patient in a gown [for a full-body exam] and look for all the signs that might not be as prominent as they are in our textbooks.”
- Look for the “butterfly” rash on the midface that is unique because it spares the nasolabial folds. “It looks like someone took an eraser and wiped out those areas,” Dr. Femia said. “This is important to help us nail down the diagnosis.”
- Other telltale signs, she said, include erythema on the extensor surfaces of digits, severe itching in the scalp, and a rash on the eyelids.
- Be aware of pulmonary involvement, including interstitial lung disease. In some cases, patients and their physicians wrongly believe that patients with dermatomyositis have asthma or pneumonia. “Pulmonologists are not necessarily aware of lung disease associated with dermatomyositis,” she said.
It’s wise to refer patients with dermatomyositis for malignancy and lung disease screening even if they don’t show signs of muscular involvement. “There’s no significant difference in rates of malignancy or lung disease in classic versus amyopathic dermatomyositis.”
Keep the MDA5 form of dermatomyositis in mind, Dr. Femia said. Anti–melanoma differentiation–associated gene 5 dermatomyositis is linked to rapidly progressive interstitial lung disease, alopecia, arthritis and oral lacerations. “Initially, it can have features of lupus, and the patient can be on immunosuppressive therapy, which mitigates diagnostic findings.”
Dr. Femia disclosed serving as principal investigator for a clinical trial in cutaneous dermatomyositis therapy.
SDEF and this news organization are owned by the same parent company.
REPORTING FROM SDEF LAS VEGAS DERMATOLOGY SEMINAR
Cutaneous squamous cell cancer staging still requires refinement
LAS VEGAS – Cases of . But even as cSCC draws more attention, two popular staging systems still need refinement, a hematologist-oncologist told dermatologist colleagues.
Both staging systems can be helpful, however, Guilherme Rabinowits, MD, said at Skin Disease Education Foundation’s annual Las Vegas Dermatology Seminar. “The best thing to do is combine both,” he noted, referring to the staging system developed by the Brigham and Women’s Hospital (BWH) and staging systems released in the 7th and 8th editions of the American Joint Committee on Cancer Staging Manual (AJCC 7 and AJCC 8; the latter focuses on head and neck only).
Cutaneous SCC has become a “huge health care burden,” said Dr. Rabinowits of the Miami Cancer Institute/Baptist Health South Florida and Florida International University, Miami. He referred to Medicare data suggesting that cSCC has become as common as basal cell carcinoma (JAMA Dermatol. 2015 Oct;151[10]:1081-6).
While most patients with cSCC have a positive prognosis, he added, the 5-year survival rate among those with the most aggressive disease is only 25%.
As he pointed out, staging systems provide insight into prognosis and treatment, guide appropriate monitoring, and give a common language to clinicians around the world. “When I talk about stage 3, we all understand who we’re talking about,” he said.
Dr. Rabinowits said he formerly worked at BWH so he is especially comfortable with its staging system. It can be appropriate to use both the BWH and AJCC systems at once, he said, noting, however, that studies suggest that the BWH system is superior.
An analysis released in 2014, for example, found that most poor outcomes occurred in patients whose tumors had been rated at lower stages – suggesting less risk – in the AJCC 7 system (J Clin Oncol 2014 Feb 1;32[4]:327-4).
In contrast, the 5% of tumors that were rated at the highest stages in the BWH system – with the highest level of perceived risk – accounted for 70% of nodal metastases and 83% of disease-specific deaths. This group may deserve extra attention in terms of staging and adjuvant treatment in order to improve outcomes, he said.
A study published this year, which compared the BWH and AJCC 8 staging systems, found that they had the same negative predictive value (0.99), while the BWH system showed higher positive predictive value (0.30 vs. 0.17). “Use of BWH tumor classification may minimize the number of patients recommended for radiologic evaluation, close surveillance, and possible adjuvant therapy while still identifying most patients at risk for recurrence, metastasis, and death,” the authors wrote (JAMA Dermatol. 2019 Jul 1;155[7]: 819-25).
As for treatment of localized disease in high-risk patients, Dr. Rabinowits advised turning to a multidisciplinary team for guidance because there are limited prospective randomized data.
Dr. Rabinowits discloses scientific advisory board/consultant relationships (Merck, Regeneron, Sanofi, EMD Serono, Pfizer, and Castle) and shares in Regeneron and Syros Pharmaceuticals. He spoke during a forum on cutaneous malignancies at the meeting.
SDEF and this news organization are owned by the same parent company.
LAS VEGAS – Cases of . But even as cSCC draws more attention, two popular staging systems still need refinement, a hematologist-oncologist told dermatologist colleagues.
Both staging systems can be helpful, however, Guilherme Rabinowits, MD, said at Skin Disease Education Foundation’s annual Las Vegas Dermatology Seminar. “The best thing to do is combine both,” he noted, referring to the staging system developed by the Brigham and Women’s Hospital (BWH) and staging systems released in the 7th and 8th editions of the American Joint Committee on Cancer Staging Manual (AJCC 7 and AJCC 8; the latter focuses on head and neck only).
Cutaneous SCC has become a “huge health care burden,” said Dr. Rabinowits of the Miami Cancer Institute/Baptist Health South Florida and Florida International University, Miami. He referred to Medicare data suggesting that cSCC has become as common as basal cell carcinoma (JAMA Dermatol. 2015 Oct;151[10]:1081-6).
While most patients with cSCC have a positive prognosis, he added, the 5-year survival rate among those with the most aggressive disease is only 25%.
As he pointed out, staging systems provide insight into prognosis and treatment, guide appropriate monitoring, and give a common language to clinicians around the world. “When I talk about stage 3, we all understand who we’re talking about,” he said.
Dr. Rabinowits said he formerly worked at BWH so he is especially comfortable with its staging system. It can be appropriate to use both the BWH and AJCC systems at once, he said, noting, however, that studies suggest that the BWH system is superior.
An analysis released in 2014, for example, found that most poor outcomes occurred in patients whose tumors had been rated at lower stages – suggesting less risk – in the AJCC 7 system (J Clin Oncol 2014 Feb 1;32[4]:327-4).
In contrast, the 5% of tumors that were rated at the highest stages in the BWH system – with the highest level of perceived risk – accounted for 70% of nodal metastases and 83% of disease-specific deaths. This group may deserve extra attention in terms of staging and adjuvant treatment in order to improve outcomes, he said.
A study published this year, which compared the BWH and AJCC 8 staging systems, found that they had the same negative predictive value (0.99), while the BWH system showed higher positive predictive value (0.30 vs. 0.17). “Use of BWH tumor classification may minimize the number of patients recommended for radiologic evaluation, close surveillance, and possible adjuvant therapy while still identifying most patients at risk for recurrence, metastasis, and death,” the authors wrote (JAMA Dermatol. 2019 Jul 1;155[7]: 819-25).
As for treatment of localized disease in high-risk patients, Dr. Rabinowits advised turning to a multidisciplinary team for guidance because there are limited prospective randomized data.
Dr. Rabinowits discloses scientific advisory board/consultant relationships (Merck, Regeneron, Sanofi, EMD Serono, Pfizer, and Castle) and shares in Regeneron and Syros Pharmaceuticals. He spoke during a forum on cutaneous malignancies at the meeting.
SDEF and this news organization are owned by the same parent company.
LAS VEGAS – Cases of . But even as cSCC draws more attention, two popular staging systems still need refinement, a hematologist-oncologist told dermatologist colleagues.
Both staging systems can be helpful, however, Guilherme Rabinowits, MD, said at Skin Disease Education Foundation’s annual Las Vegas Dermatology Seminar. “The best thing to do is combine both,” he noted, referring to the staging system developed by the Brigham and Women’s Hospital (BWH) and staging systems released in the 7th and 8th editions of the American Joint Committee on Cancer Staging Manual (AJCC 7 and AJCC 8; the latter focuses on head and neck only).
Cutaneous SCC has become a “huge health care burden,” said Dr. Rabinowits of the Miami Cancer Institute/Baptist Health South Florida and Florida International University, Miami. He referred to Medicare data suggesting that cSCC has become as common as basal cell carcinoma (JAMA Dermatol. 2015 Oct;151[10]:1081-6).
While most patients with cSCC have a positive prognosis, he added, the 5-year survival rate among those with the most aggressive disease is only 25%.
As he pointed out, staging systems provide insight into prognosis and treatment, guide appropriate monitoring, and give a common language to clinicians around the world. “When I talk about stage 3, we all understand who we’re talking about,” he said.
Dr. Rabinowits said he formerly worked at BWH so he is especially comfortable with its staging system. It can be appropriate to use both the BWH and AJCC systems at once, he said, noting, however, that studies suggest that the BWH system is superior.
An analysis released in 2014, for example, found that most poor outcomes occurred in patients whose tumors had been rated at lower stages – suggesting less risk – in the AJCC 7 system (J Clin Oncol 2014 Feb 1;32[4]:327-4).
In contrast, the 5% of tumors that were rated at the highest stages in the BWH system – with the highest level of perceived risk – accounted for 70% of nodal metastases and 83% of disease-specific deaths. This group may deserve extra attention in terms of staging and adjuvant treatment in order to improve outcomes, he said.
A study published this year, which compared the BWH and AJCC 8 staging systems, found that they had the same negative predictive value (0.99), while the BWH system showed higher positive predictive value (0.30 vs. 0.17). “Use of BWH tumor classification may minimize the number of patients recommended for radiologic evaluation, close surveillance, and possible adjuvant therapy while still identifying most patients at risk for recurrence, metastasis, and death,” the authors wrote (JAMA Dermatol. 2019 Jul 1;155[7]: 819-25).
As for treatment of localized disease in high-risk patients, Dr. Rabinowits advised turning to a multidisciplinary team for guidance because there are limited prospective randomized data.
Dr. Rabinowits discloses scientific advisory board/consultant relationships (Merck, Regeneron, Sanofi, EMD Serono, Pfizer, and Castle) and shares in Regeneron and Syros Pharmaceuticals. He spoke during a forum on cutaneous malignancies at the meeting.
SDEF and this news organization are owned by the same parent company.
EXPERT ANALYSIS FROM SDEF LAS VEGAS DERMATOLOGY SEMINAR
In Oregon, ‘war on melanoma’ takes flight
LAS VEGAS – with the goal of dramatically reducing melanoma deaths in the state of 4.2 million people.
Research shows that “early detection works in melanoma. And awareness seems to be important for the public in detecting melanoma early,” said Sancy Leachman, MD, PhD, professor and chair of the department of dermatology at Oregon Health & Science University, Portland, said at the Skin Disease Education Foundation’s annual Las Vegas Dermatology Seminar.
Dr. Leachman, who is also the John D. Gray chair in melanoma research at OHSU, directs the “War on Melanoma” project, which was inspired by a project in the German state of Schleswig-Holstein that aimed to screen all residents aged over 21 years for melanoma. The project featured an education campaign and population-wide skin cancer screening, and mandated that certain patients – those at high risk and those who needed biopsies – would be referred to dermatologists (Br J Cancer. 2012 Feb 28;106[5]:970-4).
According to Dr. Leachman, the German project was initially a success, and was linked to a 50% decrease in melanoma mortality.
“In Oregon, we thought ‘that sounds very good, so we’re going to try that.’ ” But when it went national, the German project failed, she said, providing lessons for dermatologists in Oregon. “We’re going to try to improve upon the first [German] experiment by making ours controlled with a defined baseline. If it works, the plan is to extend it to select states nationwide.”
The War on Melanoma project was launched earlier this year. According to the university, the program is featuring or will feature the following elements:
- A media campaign called “Start Seeing Melanoma” that’s devoted to educating the public about the early detection of melanoma.
- The release of an iPhone app called MoleMapper that allows users to monitor moles over time.
- Education of medical professionals and partnerships with state-licensed skin care professionals such as massage therapists, cosmetologists, and tattoo artists.
In an interview at the meeting, Dr. Leachman said the project is expected to cost $1 million to $1.5 million over the first 18 months. At that time, she said, researchers will survey residents of Oregon and two control states – Washington and Utah– to see if their knowledge of melanoma has improved, compared with baseline survey results.
In 5 years, researchers plan to begin analyzing melanoma mortality in Oregon and the other states. “We hope to see a decline,” and to link it to increased awareness of melanoma, she said.
Dr. Leachman reported no relevant disclosures. She spoke during a forum on cutaneous malignancies at the meeting.
SDEF and this news organization are owned by the same parent company.
LAS VEGAS – with the goal of dramatically reducing melanoma deaths in the state of 4.2 million people.
Research shows that “early detection works in melanoma. And awareness seems to be important for the public in detecting melanoma early,” said Sancy Leachman, MD, PhD, professor and chair of the department of dermatology at Oregon Health & Science University, Portland, said at the Skin Disease Education Foundation’s annual Las Vegas Dermatology Seminar.
Dr. Leachman, who is also the John D. Gray chair in melanoma research at OHSU, directs the “War on Melanoma” project, which was inspired by a project in the German state of Schleswig-Holstein that aimed to screen all residents aged over 21 years for melanoma. The project featured an education campaign and population-wide skin cancer screening, and mandated that certain patients – those at high risk and those who needed biopsies – would be referred to dermatologists (Br J Cancer. 2012 Feb 28;106[5]:970-4).
According to Dr. Leachman, the German project was initially a success, and was linked to a 50% decrease in melanoma mortality.
“In Oregon, we thought ‘that sounds very good, so we’re going to try that.’ ” But when it went national, the German project failed, she said, providing lessons for dermatologists in Oregon. “We’re going to try to improve upon the first [German] experiment by making ours controlled with a defined baseline. If it works, the plan is to extend it to select states nationwide.”
The War on Melanoma project was launched earlier this year. According to the university, the program is featuring or will feature the following elements:
- A media campaign called “Start Seeing Melanoma” that’s devoted to educating the public about the early detection of melanoma.
- The release of an iPhone app called MoleMapper that allows users to monitor moles over time.
- Education of medical professionals and partnerships with state-licensed skin care professionals such as massage therapists, cosmetologists, and tattoo artists.
In an interview at the meeting, Dr. Leachman said the project is expected to cost $1 million to $1.5 million over the first 18 months. At that time, she said, researchers will survey residents of Oregon and two control states – Washington and Utah– to see if their knowledge of melanoma has improved, compared with baseline survey results.
In 5 years, researchers plan to begin analyzing melanoma mortality in Oregon and the other states. “We hope to see a decline,” and to link it to increased awareness of melanoma, she said.
Dr. Leachman reported no relevant disclosures. She spoke during a forum on cutaneous malignancies at the meeting.
SDEF and this news organization are owned by the same parent company.
LAS VEGAS – with the goal of dramatically reducing melanoma deaths in the state of 4.2 million people.
Research shows that “early detection works in melanoma. And awareness seems to be important for the public in detecting melanoma early,” said Sancy Leachman, MD, PhD, professor and chair of the department of dermatology at Oregon Health & Science University, Portland, said at the Skin Disease Education Foundation’s annual Las Vegas Dermatology Seminar.
Dr. Leachman, who is also the John D. Gray chair in melanoma research at OHSU, directs the “War on Melanoma” project, which was inspired by a project in the German state of Schleswig-Holstein that aimed to screen all residents aged over 21 years for melanoma. The project featured an education campaign and population-wide skin cancer screening, and mandated that certain patients – those at high risk and those who needed biopsies – would be referred to dermatologists (Br J Cancer. 2012 Feb 28;106[5]:970-4).
According to Dr. Leachman, the German project was initially a success, and was linked to a 50% decrease in melanoma mortality.
“In Oregon, we thought ‘that sounds very good, so we’re going to try that.’ ” But when it went national, the German project failed, she said, providing lessons for dermatologists in Oregon. “We’re going to try to improve upon the first [German] experiment by making ours controlled with a defined baseline. If it works, the plan is to extend it to select states nationwide.”
The War on Melanoma project was launched earlier this year. According to the university, the program is featuring or will feature the following elements:
- A media campaign called “Start Seeing Melanoma” that’s devoted to educating the public about the early detection of melanoma.
- The release of an iPhone app called MoleMapper that allows users to monitor moles over time.
- Education of medical professionals and partnerships with state-licensed skin care professionals such as massage therapists, cosmetologists, and tattoo artists.
In an interview at the meeting, Dr. Leachman said the project is expected to cost $1 million to $1.5 million over the first 18 months. At that time, she said, researchers will survey residents of Oregon and two control states – Washington and Utah– to see if their knowledge of melanoma has improved, compared with baseline survey results.
In 5 years, researchers plan to begin analyzing melanoma mortality in Oregon and the other states. “We hope to see a decline,” and to link it to increased awareness of melanoma, she said.
Dr. Leachman reported no relevant disclosures. She spoke during a forum on cutaneous malignancies at the meeting.
SDEF and this news organization are owned by the same parent company.
EXPERT ANALYSIS FROM SDEF LAS VEGAS DERMATOLOGY SEMINAR
New models predict post-op pain in TKA
two-thirds of the time. Major risk factors include pre-operative pain, sensory testing results, anxiety and anticipated pain.
“The results of this study provide some basis for the identification of patients at risk of PPP after TKA and highlight several modifiable factors that may be targeted by clinicians in an attempt to reduce the risk of developing PPP,” write the authors of the study, which appeared in the British Journal of Anaesthesia.
The authors, led by David Rice, PhD, of Auckland University of Technology, note that moderate to severe levels of PPP affect an estimated 10%-34% of patients at least 3 months after TKA surgery. “PPP adversely affects quality of life, is the most important predictor of patient dissatisfaction after TKA, and is a common reason for undergoing revision surgery.”
The researchers, who launched the study to gain insight into the risk factors that can predict PPP, recruited 300 New Zealand volunteers (average age = 69, 48% female, 92% white, average body mass index [BMI] = 31 kg/m2) to be surveyed before and after TKA surgery. They monitored pain and tracked a long list of possible risk factors including psychological traits (such as anxiety, pain catastrophizing and depression), physical traits (such as gender, BMI), and surgical traits (such as total surgery time).
At 6 months, 21% of 291 patients reported moderate to severe pain, and the percentage fell to 16% in 288 patients at 12 months.
The researchers developed two models that successfully predicted moderate-to-severe PPP.
The 6-month model relied on higher levels of preoperative pain intensity, temporal summation (a statistic that’s based on quantitative sensory testing), trait anxiety (a measure of individual anxiety level), and expected pain. It correctly predicted moderate to severe PPP 66% of the time (area under the curve [AUC] = 0.70, sensitivity = 0.72, specificity = 0.64).
The 12-month model relied on higher levels of all the risk factors except for temporal summation and correctly predicted moderate-to-severe PPP 66% of the time (AUC = 0.66, sensitivity = 0.61, specificity = 0.67).
The researchers noted that other research has linked trait anxiety and expected pain to PPP. In regard to anxiety, “cognitive behavioral interventions in the perioperative period aimed at reducing the threat value of surgery and of postoperative pain, improving patients’ coping strategies, and enhancing self-efficacy might help to reduce the risk of PPP after TKA,” the researchers write. “Furthermore, there is some evidence that anxiolytic medications can diminish perioperative anxiety and reduce APOP [acute postoperative pain] although its effects on PPP are unclear.”
Moving forward, the authors write, “strategies to minimize intraoperative nerve injury, reduce preoperative pain intensity, and address preoperative psychological factors such as expected pain and anxiety may lead to improved outcomes after TKA and should be explored.”
The Australia New Zealand College of Anesthetists and Auckland University of Technology funded the study. The study authors report no relevant disclosures.
SOURCE: Rice D et al. Br J Anaesth 2018;804-12. doi: https://doi.org/10.1016/j.bja.2018.05.070.
two-thirds of the time. Major risk factors include pre-operative pain, sensory testing results, anxiety and anticipated pain.
“The results of this study provide some basis for the identification of patients at risk of PPP after TKA and highlight several modifiable factors that may be targeted by clinicians in an attempt to reduce the risk of developing PPP,” write the authors of the study, which appeared in the British Journal of Anaesthesia.
The authors, led by David Rice, PhD, of Auckland University of Technology, note that moderate to severe levels of PPP affect an estimated 10%-34% of patients at least 3 months after TKA surgery. “PPP adversely affects quality of life, is the most important predictor of patient dissatisfaction after TKA, and is a common reason for undergoing revision surgery.”
The researchers, who launched the study to gain insight into the risk factors that can predict PPP, recruited 300 New Zealand volunteers (average age = 69, 48% female, 92% white, average body mass index [BMI] = 31 kg/m2) to be surveyed before and after TKA surgery. They monitored pain and tracked a long list of possible risk factors including psychological traits (such as anxiety, pain catastrophizing and depression), physical traits (such as gender, BMI), and surgical traits (such as total surgery time).
At 6 months, 21% of 291 patients reported moderate to severe pain, and the percentage fell to 16% in 288 patients at 12 months.
The researchers developed two models that successfully predicted moderate-to-severe PPP.
The 6-month model relied on higher levels of preoperative pain intensity, temporal summation (a statistic that’s based on quantitative sensory testing), trait anxiety (a measure of individual anxiety level), and expected pain. It correctly predicted moderate to severe PPP 66% of the time (area under the curve [AUC] = 0.70, sensitivity = 0.72, specificity = 0.64).
The 12-month model relied on higher levels of all the risk factors except for temporal summation and correctly predicted moderate-to-severe PPP 66% of the time (AUC = 0.66, sensitivity = 0.61, specificity = 0.67).
The researchers noted that other research has linked trait anxiety and expected pain to PPP. In regard to anxiety, “cognitive behavioral interventions in the perioperative period aimed at reducing the threat value of surgery and of postoperative pain, improving patients’ coping strategies, and enhancing self-efficacy might help to reduce the risk of PPP after TKA,” the researchers write. “Furthermore, there is some evidence that anxiolytic medications can diminish perioperative anxiety and reduce APOP [acute postoperative pain] although its effects on PPP are unclear.”
Moving forward, the authors write, “strategies to minimize intraoperative nerve injury, reduce preoperative pain intensity, and address preoperative psychological factors such as expected pain and anxiety may lead to improved outcomes after TKA and should be explored.”
The Australia New Zealand College of Anesthetists and Auckland University of Technology funded the study. The study authors report no relevant disclosures.
SOURCE: Rice D et al. Br J Anaesth 2018;804-12. doi: https://doi.org/10.1016/j.bja.2018.05.070.
two-thirds of the time. Major risk factors include pre-operative pain, sensory testing results, anxiety and anticipated pain.
“The results of this study provide some basis for the identification of patients at risk of PPP after TKA and highlight several modifiable factors that may be targeted by clinicians in an attempt to reduce the risk of developing PPP,” write the authors of the study, which appeared in the British Journal of Anaesthesia.
The authors, led by David Rice, PhD, of Auckland University of Technology, note that moderate to severe levels of PPP affect an estimated 10%-34% of patients at least 3 months after TKA surgery. “PPP adversely affects quality of life, is the most important predictor of patient dissatisfaction after TKA, and is a common reason for undergoing revision surgery.”
The researchers, who launched the study to gain insight into the risk factors that can predict PPP, recruited 300 New Zealand volunteers (average age = 69, 48% female, 92% white, average body mass index [BMI] = 31 kg/m2) to be surveyed before and after TKA surgery. They monitored pain and tracked a long list of possible risk factors including psychological traits (such as anxiety, pain catastrophizing and depression), physical traits (such as gender, BMI), and surgical traits (such as total surgery time).
At 6 months, 21% of 291 patients reported moderate to severe pain, and the percentage fell to 16% in 288 patients at 12 months.
The researchers developed two models that successfully predicted moderate-to-severe PPP.
The 6-month model relied on higher levels of preoperative pain intensity, temporal summation (a statistic that’s based on quantitative sensory testing), trait anxiety (a measure of individual anxiety level), and expected pain. It correctly predicted moderate to severe PPP 66% of the time (area under the curve [AUC] = 0.70, sensitivity = 0.72, specificity = 0.64).
The 12-month model relied on higher levels of all the risk factors except for temporal summation and correctly predicted moderate-to-severe PPP 66% of the time (AUC = 0.66, sensitivity = 0.61, specificity = 0.67).
The researchers noted that other research has linked trait anxiety and expected pain to PPP. In regard to anxiety, “cognitive behavioral interventions in the perioperative period aimed at reducing the threat value of surgery and of postoperative pain, improving patients’ coping strategies, and enhancing self-efficacy might help to reduce the risk of PPP after TKA,” the researchers write. “Furthermore, there is some evidence that anxiolytic medications can diminish perioperative anxiety and reduce APOP [acute postoperative pain] although its effects on PPP are unclear.”
Moving forward, the authors write, “strategies to minimize intraoperative nerve injury, reduce preoperative pain intensity, and address preoperative psychological factors such as expected pain and anxiety may lead to improved outcomes after TKA and should be explored.”
The Australia New Zealand College of Anesthetists and Auckland University of Technology funded the study. The study authors report no relevant disclosures.
SOURCE: Rice D et al. Br J Anaesth 2018;804-12. doi: https://doi.org/10.1016/j.bja.2018.05.070.
FROM BRITISH JOURNAL OF ANESTHESIA
What’s the proper place of benzodiazepines in psychiatry?
Tread carefully, but do not eliminate them as an option, two experts advise.
SAN DIEGO – Not long before his presentation at Psych Congress 2019, psychiatrist Rakesh Jain, MD, MPH, chatted with a fellow attendee, a nurse practitioner from Tyler, Tex. As Dr. Jain recalled later, his fellow Texan told him that “it’s not unusual to see patients on three benzodiazepines.”
The nurse practitioner “talks to them about how they need to do things differently, and they forget,” Dr. Jain said. “He’s very worried about them.”
Dr. Jain is familiar with the feeling. Like many mental health professionals, he worries about the role of benzodiazepines, which seem to be both widely used and misused. Figuring out their proper place in psychiatry “may require us to raise our game,” said Dr. Jain, of Texas Tech University in Midland.
What to do? Dr. Jain and a colleague offered the same answer – tread carefully, but do not eliminate them as an option – in two separate sessions at the annual Psych Congress.
As Dr. Jain noted, benzodiazepines are popular, and for good reason. “There are many patients, perhaps hundreds of thousands, who are using benzodiazepines chronically, and they’re doing it right. There’s not a CVS in America where benzodiazepines aren’t well stocked. They’re very inexpensive, and the most costly benzodiazepine is still cheaper than Motrin.”
On the other hand, he said, the medications are linked to addiction and physical dependence. “Thirty percent of those who die of opioid overdoses may not have died if they didn’t have benzodiazepines [in their systems].”
In another presentation, psychiatrist Murray B. Stein, MD, MPH, of the University of California at San Diego and VA San Diego Healthcare System, offered these tips about prescribing benzodiazepines for patients with anxiety.
Be very cautious about prescribing as needed
“It’s rarely indicated to prescribe benzodiazepine [as needed] when you’re treating people with anxiety,” he said. “The main reason is patients don’t know when they need it. They take their pills either when they’re so anxious that they’ve already been freaking out for a long time, or they take it when they’re first starting to feel at least a bit anxious. That leads to taking it to prevent being anxious.”
Allow an as-needed approach in certain situations
However, he said, advise patients to try the medication beforehand so they understand its effects. “I’ve had one occasion where I thought we had a dose worked out well. Somebody had to do a work presentation, and he took the medicine and got up in front of the group. He wasn’t anxious at all. But he couldn’t remember a single thing.”
Don’t use them as patients start SSRIs
Patients can get anxious as they start SSRIs, especially for panic disorders, Dr. Stein said. So it might seem reasonable, as some psychiatrists believe, to add benzodiazepines on a short-term basis.
But Dr. Stein said he is not a fan of this approach. As he noted, benzodiazepines are hard to stop. He prefers to help patients understand possible side effects of SSRIs instead, and he emphasized the importance of being available to help patients get through them.
Dr. Jain and Dr. Stein each reported multiple relationships with industry.
Tread carefully, but do not eliminate them as an option, two experts advise.
Tread carefully, but do not eliminate them as an option, two experts advise.
SAN DIEGO – Not long before his presentation at Psych Congress 2019, psychiatrist Rakesh Jain, MD, MPH, chatted with a fellow attendee, a nurse practitioner from Tyler, Tex. As Dr. Jain recalled later, his fellow Texan told him that “it’s not unusual to see patients on three benzodiazepines.”
The nurse practitioner “talks to them about how they need to do things differently, and they forget,” Dr. Jain said. “He’s very worried about them.”
Dr. Jain is familiar with the feeling. Like many mental health professionals, he worries about the role of benzodiazepines, which seem to be both widely used and misused. Figuring out their proper place in psychiatry “may require us to raise our game,” said Dr. Jain, of Texas Tech University in Midland.
What to do? Dr. Jain and a colleague offered the same answer – tread carefully, but do not eliminate them as an option – in two separate sessions at the annual Psych Congress.
As Dr. Jain noted, benzodiazepines are popular, and for good reason. “There are many patients, perhaps hundreds of thousands, who are using benzodiazepines chronically, and they’re doing it right. There’s not a CVS in America where benzodiazepines aren’t well stocked. They’re very inexpensive, and the most costly benzodiazepine is still cheaper than Motrin.”
On the other hand, he said, the medications are linked to addiction and physical dependence. “Thirty percent of those who die of opioid overdoses may not have died if they didn’t have benzodiazepines [in their systems].”
In another presentation, psychiatrist Murray B. Stein, MD, MPH, of the University of California at San Diego and VA San Diego Healthcare System, offered these tips about prescribing benzodiazepines for patients with anxiety.
Be very cautious about prescribing as needed
“It’s rarely indicated to prescribe benzodiazepine [as needed] when you’re treating people with anxiety,” he said. “The main reason is patients don’t know when they need it. They take their pills either when they’re so anxious that they’ve already been freaking out for a long time, or they take it when they’re first starting to feel at least a bit anxious. That leads to taking it to prevent being anxious.”
Allow an as-needed approach in certain situations
However, he said, advise patients to try the medication beforehand so they understand its effects. “I’ve had one occasion where I thought we had a dose worked out well. Somebody had to do a work presentation, and he took the medicine and got up in front of the group. He wasn’t anxious at all. But he couldn’t remember a single thing.”
Don’t use them as patients start SSRIs
Patients can get anxious as they start SSRIs, especially for panic disorders, Dr. Stein said. So it might seem reasonable, as some psychiatrists believe, to add benzodiazepines on a short-term basis.
But Dr. Stein said he is not a fan of this approach. As he noted, benzodiazepines are hard to stop. He prefers to help patients understand possible side effects of SSRIs instead, and he emphasized the importance of being available to help patients get through them.
Dr. Jain and Dr. Stein each reported multiple relationships with industry.
SAN DIEGO – Not long before his presentation at Psych Congress 2019, psychiatrist Rakesh Jain, MD, MPH, chatted with a fellow attendee, a nurse practitioner from Tyler, Tex. As Dr. Jain recalled later, his fellow Texan told him that “it’s not unusual to see patients on three benzodiazepines.”
The nurse practitioner “talks to them about how they need to do things differently, and they forget,” Dr. Jain said. “He’s very worried about them.”
Dr. Jain is familiar with the feeling. Like many mental health professionals, he worries about the role of benzodiazepines, which seem to be both widely used and misused. Figuring out their proper place in psychiatry “may require us to raise our game,” said Dr. Jain, of Texas Tech University in Midland.
What to do? Dr. Jain and a colleague offered the same answer – tread carefully, but do not eliminate them as an option – in two separate sessions at the annual Psych Congress.
As Dr. Jain noted, benzodiazepines are popular, and for good reason. “There are many patients, perhaps hundreds of thousands, who are using benzodiazepines chronically, and they’re doing it right. There’s not a CVS in America where benzodiazepines aren’t well stocked. They’re very inexpensive, and the most costly benzodiazepine is still cheaper than Motrin.”
On the other hand, he said, the medications are linked to addiction and physical dependence. “Thirty percent of those who die of opioid overdoses may not have died if they didn’t have benzodiazepines [in their systems].”
In another presentation, psychiatrist Murray B. Stein, MD, MPH, of the University of California at San Diego and VA San Diego Healthcare System, offered these tips about prescribing benzodiazepines for patients with anxiety.
Be very cautious about prescribing as needed
“It’s rarely indicated to prescribe benzodiazepine [as needed] when you’re treating people with anxiety,” he said. “The main reason is patients don’t know when they need it. They take their pills either when they’re so anxious that they’ve already been freaking out for a long time, or they take it when they’re first starting to feel at least a bit anxious. That leads to taking it to prevent being anxious.”
Allow an as-needed approach in certain situations
However, he said, advise patients to try the medication beforehand so they understand its effects. “I’ve had one occasion where I thought we had a dose worked out well. Somebody had to do a work presentation, and he took the medicine and got up in front of the group. He wasn’t anxious at all. But he couldn’t remember a single thing.”
Don’t use them as patients start SSRIs
Patients can get anxious as they start SSRIs, especially for panic disorders, Dr. Stein said. So it might seem reasonable, as some psychiatrists believe, to add benzodiazepines on a short-term basis.
But Dr. Stein said he is not a fan of this approach. As he noted, benzodiazepines are hard to stop. He prefers to help patients understand possible side effects of SSRIs instead, and he emphasized the importance of being available to help patients get through them.
Dr. Jain and Dr. Stein each reported multiple relationships with industry.
REPORTING FROM PSYCH CONGRESS 2019
Acoustic pulse boosts laser tattoo removal
In tattoo removal, the impact of laser treatments in single office visits is limited because of the laser’s effects on the skin. Now, a new study suggests that a
“As a result,” the authors of the study wrote, “a lower total number of office visits will likely be required for complete tattoo removal leading to improved convenience and efficiency as well as increased satisfaction for both patients and clinicians.” The study, led by cosmetic surgeon Michael S. Kaminer, MD, of SkinCare Physicians in Chestnut Hill, Mass., appeared in Lasers in Surgery and Medicine.
In the study, he and his coauthors pointed out that tattoos are most frequently removed with short-pulse high-fluence lasers, such as a 1064-nm Nd:YAG Q‐switched (QS) laser. However, “the QS laser has a limited ability to affect the tattoo ink pigment particles in each treatment session due to shielding of the pigment particles caused by both the agglomeration of the pigment particles and laser‐induced epidermal and dermal vacuoles known as ‘whitening.’ ” Therefore, “use of the QS laser often requires 10 or more single‐pass office sessions to achieve acceptable fading results.”
The study evaluated whether the use of a rapid acoustic pulse (RAP) device could reduce the whitening effect by clearing vacuoles and make it possible to increase the number of potential laser passes. In the single-center, prospective trial, they treated 32 black-ink tattoos in 21 patients, dividing the tattoos into zones and treating them differently: One zone received at least three consecutive laser passes alternating with a minute of treatment with the RAP device, one received single-pass laser treatment, and one received no treatment.
Reviewers assessed the tattoos for fading at 12 weeks. Average percent fading was higher in the laser/RAP group, compared with the laser-only group (44% and 25%, respectively, P less than .01). The percentages of tattoos with more than 50% fading (38% vs. 9%, P less than .01) and more than 75% fading (22% vs. 3%, P less than .05) were also higher in the laser/RAP group, compared with the laser-only group.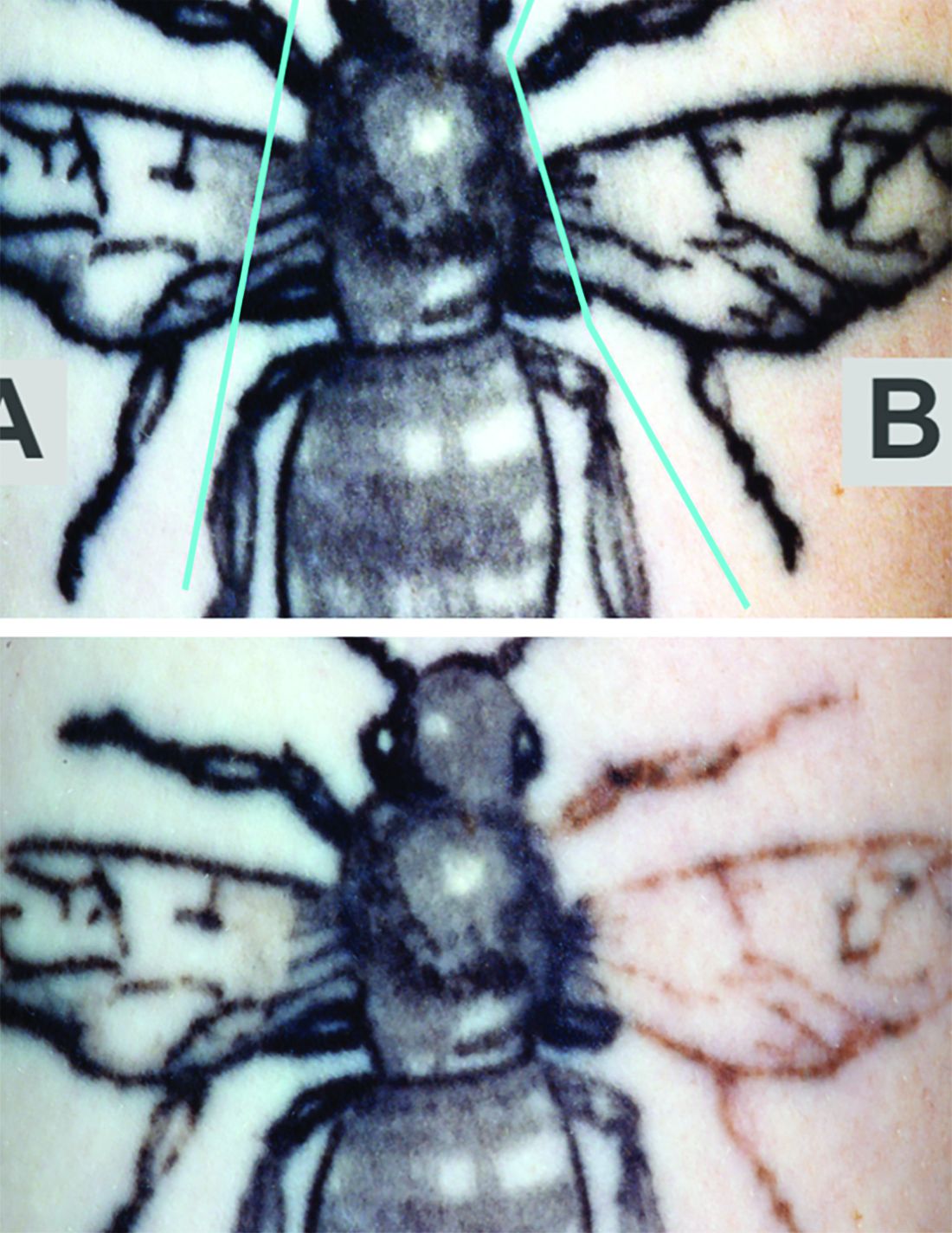
“Further clinical studies will be performed to investigate the broader applicability of the RAP device as an accessory device to reduce the number of laser tattoo removal sessions for other tattoo ink colors in a broader range of skin types,” the researchers commented, noting that the study included patients with Fitzpatrick skin types I-III.
The study was funded by Soliton, which provided the equipment. One of the six authors is an employee of the company The other authors reported no relevant disclosures.
SOURCE: Kaminer MS et al. Lasers Surg Med. 2019 Sep 19. doi: 10.1002/lsm.23163.
In tattoo removal, the impact of laser treatments in single office visits is limited because of the laser’s effects on the skin. Now, a new study suggests that a
“As a result,” the authors of the study wrote, “a lower total number of office visits will likely be required for complete tattoo removal leading to improved convenience and efficiency as well as increased satisfaction for both patients and clinicians.” The study, led by cosmetic surgeon Michael S. Kaminer, MD, of SkinCare Physicians in Chestnut Hill, Mass., appeared in Lasers in Surgery and Medicine.
In the study, he and his coauthors pointed out that tattoos are most frequently removed with short-pulse high-fluence lasers, such as a 1064-nm Nd:YAG Q‐switched (QS) laser. However, “the QS laser has a limited ability to affect the tattoo ink pigment particles in each treatment session due to shielding of the pigment particles caused by both the agglomeration of the pigment particles and laser‐induced epidermal and dermal vacuoles known as ‘whitening.’ ” Therefore, “use of the QS laser often requires 10 or more single‐pass office sessions to achieve acceptable fading results.”
The study evaluated whether the use of a rapid acoustic pulse (RAP) device could reduce the whitening effect by clearing vacuoles and make it possible to increase the number of potential laser passes. In the single-center, prospective trial, they treated 32 black-ink tattoos in 21 patients, dividing the tattoos into zones and treating them differently: One zone received at least three consecutive laser passes alternating with a minute of treatment with the RAP device, one received single-pass laser treatment, and one received no treatment.
Reviewers assessed the tattoos for fading at 12 weeks. Average percent fading was higher in the laser/RAP group, compared with the laser-only group (44% and 25%, respectively, P less than .01). The percentages of tattoos with more than 50% fading (38% vs. 9%, P less than .01) and more than 75% fading (22% vs. 3%, P less than .05) were also higher in the laser/RAP group, compared with the laser-only group.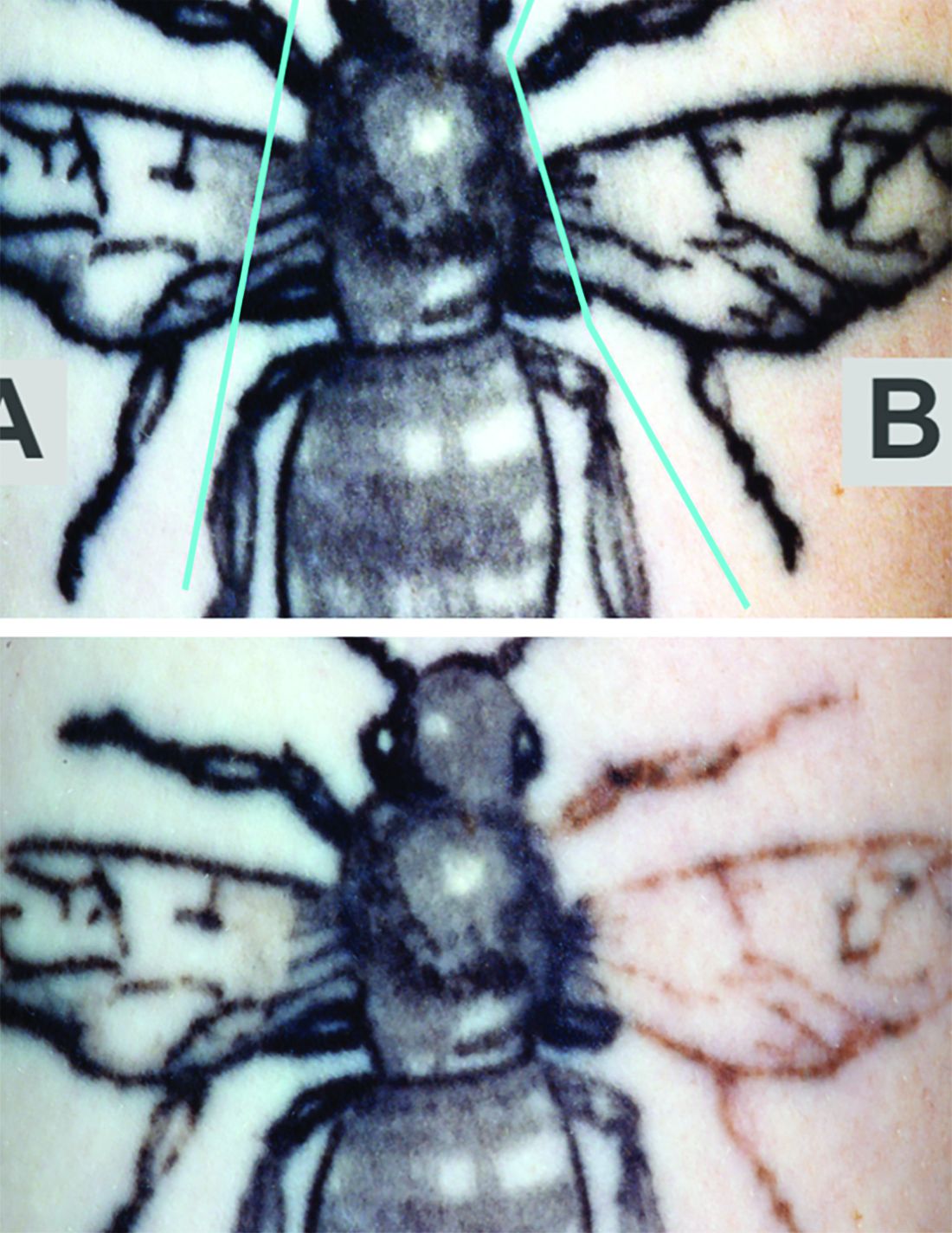
“Further clinical studies will be performed to investigate the broader applicability of the RAP device as an accessory device to reduce the number of laser tattoo removal sessions for other tattoo ink colors in a broader range of skin types,” the researchers commented, noting that the study included patients with Fitzpatrick skin types I-III.
The study was funded by Soliton, which provided the equipment. One of the six authors is an employee of the company The other authors reported no relevant disclosures.
SOURCE: Kaminer MS et al. Lasers Surg Med. 2019 Sep 19. doi: 10.1002/lsm.23163.
In tattoo removal, the impact of laser treatments in single office visits is limited because of the laser’s effects on the skin. Now, a new study suggests that a
“As a result,” the authors of the study wrote, “a lower total number of office visits will likely be required for complete tattoo removal leading to improved convenience and efficiency as well as increased satisfaction for both patients and clinicians.” The study, led by cosmetic surgeon Michael S. Kaminer, MD, of SkinCare Physicians in Chestnut Hill, Mass., appeared in Lasers in Surgery and Medicine.
In the study, he and his coauthors pointed out that tattoos are most frequently removed with short-pulse high-fluence lasers, such as a 1064-nm Nd:YAG Q‐switched (QS) laser. However, “the QS laser has a limited ability to affect the tattoo ink pigment particles in each treatment session due to shielding of the pigment particles caused by both the agglomeration of the pigment particles and laser‐induced epidermal and dermal vacuoles known as ‘whitening.’ ” Therefore, “use of the QS laser often requires 10 or more single‐pass office sessions to achieve acceptable fading results.”
The study evaluated whether the use of a rapid acoustic pulse (RAP) device could reduce the whitening effect by clearing vacuoles and make it possible to increase the number of potential laser passes. In the single-center, prospective trial, they treated 32 black-ink tattoos in 21 patients, dividing the tattoos into zones and treating them differently: One zone received at least three consecutive laser passes alternating with a minute of treatment with the RAP device, one received single-pass laser treatment, and one received no treatment.
Reviewers assessed the tattoos for fading at 12 weeks. Average percent fading was higher in the laser/RAP group, compared with the laser-only group (44% and 25%, respectively, P less than .01). The percentages of tattoos with more than 50% fading (38% vs. 9%, P less than .01) and more than 75% fading (22% vs. 3%, P less than .05) were also higher in the laser/RAP group, compared with the laser-only group.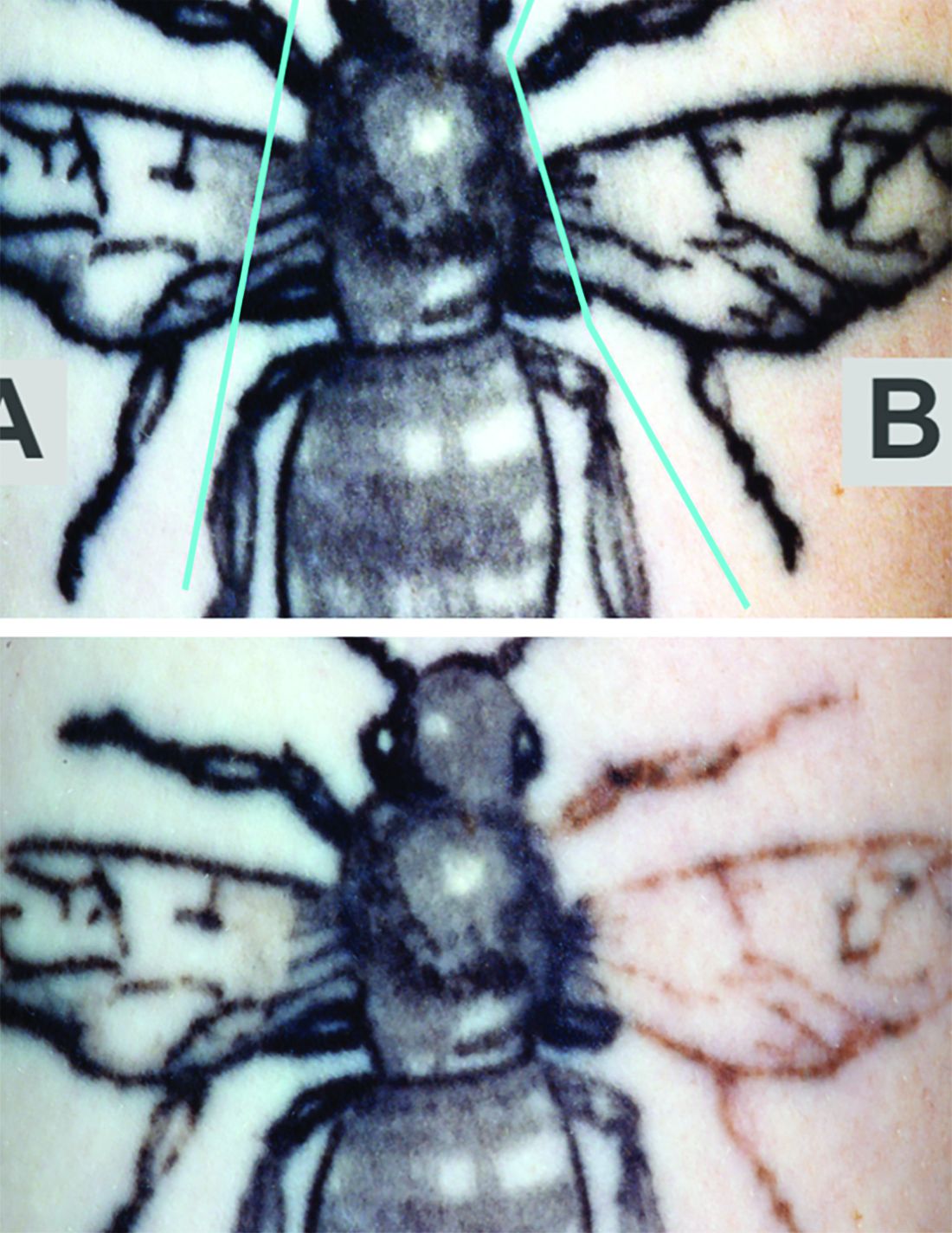
“Further clinical studies will be performed to investigate the broader applicability of the RAP device as an accessory device to reduce the number of laser tattoo removal sessions for other tattoo ink colors in a broader range of skin types,” the researchers commented, noting that the study included patients with Fitzpatrick skin types I-III.
The study was funded by Soliton, which provided the equipment. One of the six authors is an employee of the company The other authors reported no relevant disclosures.
SOURCE: Kaminer MS et al. Lasers Surg Med. 2019 Sep 19. doi: 10.1002/lsm.23163.
FROM LASERS IN SURGERY AND MEDICINE



