User login
Australia’s rotavirus outbreak wasn’t caused by vaccine effectiveness decline
In 2017, the Australian state of New South Wales experienced an outbreak of rotavirus gastroenteritis in children despite a high level of rotavirus immunization. In a new study, researchers reported evidence that suggests a decline in vaccine effectiveness (VE) isn’t the cause, although they found that VE declines over time as children age.
“More analysis is required to investigate how novel or unusual strains ... interact with rotavirus vaccines and whether antigenic changes affect VE and challenge vaccination programs,” the study authors wrote in Pediatrics.
Researchers led by Julia E. Maguire, BSc, MSci(Epi), of Australia’s National Center for Immunization Research and the Australian National University, Canberra, launched the analysis in the wake of a 2017 outbreak of 2,319 rotavirus cases in New South Wales, a 210% increase over the rate in 2016. (The state, the largest in Australia, has about 7.5 million residents.)
The study authors tracked VE from 2010 to 2017 by analyzing 9,517 rotavirus cases in the state (50% male; median age, 5 years). Half weren’t eligible for rotavirus immunization because of their age; of the rest, 31% weren’t vaccinated.
Ms. Maguire and associates found that “In our study, two doses of RV1 [the Rotarix vaccine] was 73.7% effective in protecting children aged 6 months to 9 years against laboratory-confirmed rotavirus over our 8-year study period. Somewhat surprisingly in the 2017 outbreak year, a high two-dose VE of 88.4% in those aged 6-11 months was also observed.”
They added that “the median age of rotavirus cases has increased in Australia over the last 8 years from 3.9 years in 2010 to 7.1 years in 2017. Adults and older children born before the availability of vaccination in Australia are unimmunized and may have been less likely to have repeated subclinical infections because of reductions in virus circulation overall, resulting in less immune boosting.”
Going forward, the study authors wrote that “investigation of population-level VE in relation to rotavirus genotype data should continue in a range of settings to improve our understanding of rotavirus vaccines and the impact they have on disease across the age spectrum over time.”
In an accompanying commentary, Benjamin Lee, MD, and E. Ross Colgate, PhD, of the University of Vermont, Burlington, wrote that Australia’s adoption of rotavirus immunization in 2017 “with state-level implementation of either Rotarix or RotaTeq ... enabled a fascinating natural experiment of VE and strain selection.”
Pressure from vaccines “potentially enables the emergence of novel strains,” they wrote. “Despite this, large-scale strain replacement has not been demonstrated in rotaviruses, in contrast to the development of pneumococcal serotype replacement that was seen after pneumococcal conjugate vaccine introduction. Similarly, there has been no evidence of widespread vaccine escape due to antigenic drift or shift, as occurs with another important segmented RNA virus, influenza A.”
As Dr. Lee and Dr. Colgate noted, 100 million children worldwide remain unvaccinated against rotavirus, and more than 128,000 die because of rotavirus-associated gastroenteritis each year. “Improving vaccine access and coverage and solving the riddle of [oral rotavirus vaccine] underperformance in low-income countries are urgent priorities, which may ultimately require next-generation oral and/or parenteral vaccines, a number of which are under development and in clinical trials. In addition, because the emergence of novel strains of disease-causing pathogens is always a possibility, vigilance in rotavirus surveillance, including genotype assessment, should remain a priority for public health programs.”
The study was funded by Australia’s National Center for Immunization Research and Surveillance, which receives government funding. The Australian Rotavirus Surveillance Program is supported by government funding and the vaccine companies Commonwealth Serum Laboratories and GlaxoSmithKline. Ms. Maguire is supported by an Australian Government Research Training Program Scholarship. One author is director of the Australian Rotavirus Surveillance Program, which received funding as above. The other study authors and the commentary authors reported no relevant financial disclosures.
SOURCES: Maguire JE et al. Pediatrics. 2019 Sep 17. doi: 10.1542/peds.2019-1024; Lee B, Colgate ER. Pediatrics. 2019 Sep 17. doi: 10.1542/peds.2019-2426.
In 2017, the Australian state of New South Wales experienced an outbreak of rotavirus gastroenteritis in children despite a high level of rotavirus immunization. In a new study, researchers reported evidence that suggests a decline in vaccine effectiveness (VE) isn’t the cause, although they found that VE declines over time as children age.
“More analysis is required to investigate how novel or unusual strains ... interact with rotavirus vaccines and whether antigenic changes affect VE and challenge vaccination programs,” the study authors wrote in Pediatrics.
Researchers led by Julia E. Maguire, BSc, MSci(Epi), of Australia’s National Center for Immunization Research and the Australian National University, Canberra, launched the analysis in the wake of a 2017 outbreak of 2,319 rotavirus cases in New South Wales, a 210% increase over the rate in 2016. (The state, the largest in Australia, has about 7.5 million residents.)
The study authors tracked VE from 2010 to 2017 by analyzing 9,517 rotavirus cases in the state (50% male; median age, 5 years). Half weren’t eligible for rotavirus immunization because of their age; of the rest, 31% weren’t vaccinated.
Ms. Maguire and associates found that “In our study, two doses of RV1 [the Rotarix vaccine] was 73.7% effective in protecting children aged 6 months to 9 years against laboratory-confirmed rotavirus over our 8-year study period. Somewhat surprisingly in the 2017 outbreak year, a high two-dose VE of 88.4% in those aged 6-11 months was also observed.”
They added that “the median age of rotavirus cases has increased in Australia over the last 8 years from 3.9 years in 2010 to 7.1 years in 2017. Adults and older children born before the availability of vaccination in Australia are unimmunized and may have been less likely to have repeated subclinical infections because of reductions in virus circulation overall, resulting in less immune boosting.”
Going forward, the study authors wrote that “investigation of population-level VE in relation to rotavirus genotype data should continue in a range of settings to improve our understanding of rotavirus vaccines and the impact they have on disease across the age spectrum over time.”
In an accompanying commentary, Benjamin Lee, MD, and E. Ross Colgate, PhD, of the University of Vermont, Burlington, wrote that Australia’s adoption of rotavirus immunization in 2017 “with state-level implementation of either Rotarix or RotaTeq ... enabled a fascinating natural experiment of VE and strain selection.”
Pressure from vaccines “potentially enables the emergence of novel strains,” they wrote. “Despite this, large-scale strain replacement has not been demonstrated in rotaviruses, in contrast to the development of pneumococcal serotype replacement that was seen after pneumococcal conjugate vaccine introduction. Similarly, there has been no evidence of widespread vaccine escape due to antigenic drift or shift, as occurs with another important segmented RNA virus, influenza A.”
As Dr. Lee and Dr. Colgate noted, 100 million children worldwide remain unvaccinated against rotavirus, and more than 128,000 die because of rotavirus-associated gastroenteritis each year. “Improving vaccine access and coverage and solving the riddle of [oral rotavirus vaccine] underperformance in low-income countries are urgent priorities, which may ultimately require next-generation oral and/or parenteral vaccines, a number of which are under development and in clinical trials. In addition, because the emergence of novel strains of disease-causing pathogens is always a possibility, vigilance in rotavirus surveillance, including genotype assessment, should remain a priority for public health programs.”
The study was funded by Australia’s National Center for Immunization Research and Surveillance, which receives government funding. The Australian Rotavirus Surveillance Program is supported by government funding and the vaccine companies Commonwealth Serum Laboratories and GlaxoSmithKline. Ms. Maguire is supported by an Australian Government Research Training Program Scholarship. One author is director of the Australian Rotavirus Surveillance Program, which received funding as above. The other study authors and the commentary authors reported no relevant financial disclosures.
SOURCES: Maguire JE et al. Pediatrics. 2019 Sep 17. doi: 10.1542/peds.2019-1024; Lee B, Colgate ER. Pediatrics. 2019 Sep 17. doi: 10.1542/peds.2019-2426.
In 2017, the Australian state of New South Wales experienced an outbreak of rotavirus gastroenteritis in children despite a high level of rotavirus immunization. In a new study, researchers reported evidence that suggests a decline in vaccine effectiveness (VE) isn’t the cause, although they found that VE declines over time as children age.
“More analysis is required to investigate how novel or unusual strains ... interact with rotavirus vaccines and whether antigenic changes affect VE and challenge vaccination programs,” the study authors wrote in Pediatrics.
Researchers led by Julia E. Maguire, BSc, MSci(Epi), of Australia’s National Center for Immunization Research and the Australian National University, Canberra, launched the analysis in the wake of a 2017 outbreak of 2,319 rotavirus cases in New South Wales, a 210% increase over the rate in 2016. (The state, the largest in Australia, has about 7.5 million residents.)
The study authors tracked VE from 2010 to 2017 by analyzing 9,517 rotavirus cases in the state (50% male; median age, 5 years). Half weren’t eligible for rotavirus immunization because of their age; of the rest, 31% weren’t vaccinated.
Ms. Maguire and associates found that “In our study, two doses of RV1 [the Rotarix vaccine] was 73.7% effective in protecting children aged 6 months to 9 years against laboratory-confirmed rotavirus over our 8-year study period. Somewhat surprisingly in the 2017 outbreak year, a high two-dose VE of 88.4% in those aged 6-11 months was also observed.”
They added that “the median age of rotavirus cases has increased in Australia over the last 8 years from 3.9 years in 2010 to 7.1 years in 2017. Adults and older children born before the availability of vaccination in Australia are unimmunized and may have been less likely to have repeated subclinical infections because of reductions in virus circulation overall, resulting in less immune boosting.”
Going forward, the study authors wrote that “investigation of population-level VE in relation to rotavirus genotype data should continue in a range of settings to improve our understanding of rotavirus vaccines and the impact they have on disease across the age spectrum over time.”
In an accompanying commentary, Benjamin Lee, MD, and E. Ross Colgate, PhD, of the University of Vermont, Burlington, wrote that Australia’s adoption of rotavirus immunization in 2017 “with state-level implementation of either Rotarix or RotaTeq ... enabled a fascinating natural experiment of VE and strain selection.”
Pressure from vaccines “potentially enables the emergence of novel strains,” they wrote. “Despite this, large-scale strain replacement has not been demonstrated in rotaviruses, in contrast to the development of pneumococcal serotype replacement that was seen after pneumococcal conjugate vaccine introduction. Similarly, there has been no evidence of widespread vaccine escape due to antigenic drift or shift, as occurs with another important segmented RNA virus, influenza A.”
As Dr. Lee and Dr. Colgate noted, 100 million children worldwide remain unvaccinated against rotavirus, and more than 128,000 die because of rotavirus-associated gastroenteritis each year. “Improving vaccine access and coverage and solving the riddle of [oral rotavirus vaccine] underperformance in low-income countries are urgent priorities, which may ultimately require next-generation oral and/or parenteral vaccines, a number of which are under development and in clinical trials. In addition, because the emergence of novel strains of disease-causing pathogens is always a possibility, vigilance in rotavirus surveillance, including genotype assessment, should remain a priority for public health programs.”
The study was funded by Australia’s National Center for Immunization Research and Surveillance, which receives government funding. The Australian Rotavirus Surveillance Program is supported by government funding and the vaccine companies Commonwealth Serum Laboratories and GlaxoSmithKline. Ms. Maguire is supported by an Australian Government Research Training Program Scholarship. One author is director of the Australian Rotavirus Surveillance Program, which received funding as above. The other study authors and the commentary authors reported no relevant financial disclosures.
SOURCES: Maguire JE et al. Pediatrics. 2019 Sep 17. doi: 10.1542/peds.2019-1024; Lee B, Colgate ER. Pediatrics. 2019 Sep 17. doi: 10.1542/peds.2019-2426.
FROM PEDIATRICS
Bariatric surgery has mostly positive impact in knee arthroplasty
a large study has found.
The study, led by Yicun Wang, PhD, of Nanjing (China) University was published in the Journal of Arthroplasty. “Generally speaking, bariatric surgery decreases some postoperative complications, decreases length of stay, and lowers mortality,” the study investigators wrote, [but] anemia and blood transfusion seem to be more common in patients with prior bariatric surgery.
They analyzed the effect of bariatric surgery on subsequent arthroplasty in morbidly obese patients in the United States using Nationwide Inpatient Sample 2006-2014 data on total hip arthroplasty (THA) and total knee arthroplasty (TKA). The researchers defined morbid obese patients as those with a body mass index higher than 40 kg/m2.
Among patients who underwent TKA, the researchers compared a group of 9,803 morbidly obese patients with the same number of patients who had undergone bariatric surgery. The two groups were matched by age, sex, income, primary insurance payer, and race.
There were large differences between the bariatric surgery group vs. morbidly obese group: Pulmonary embolism was much more common in the morbid obesity group (odds ratio, 0.22; 95% confidence interval, 0.05-1.03; P = .0346) while blood transfusion was more common in the bariatric surgery group (OR, 1.76; 95% CI, 1.52-2.03; P less than .0001).
For TKA, the researchers used the same approach to analyze 2,540 matched pairs of patients. In the bariatric surgery vs. morbidly obese comparison, pulmonary embolism was more common in the morbidly obese group (OR, 0.34; 95% CI, 0.20-0.57; P less than .0001), as were respiratory complications (OR, 0.45; 95% CI, 0.26-0.78; P = .0032) and death (OR, 0.07; 95% CI, 0.01-0.50; P = .0005). But the bariatric surgery group had higher levels of blood transfusion (OR, 1.87; 95% CI, 1.71-2.04; P less than .0001) and anemia (OR, 1.16; 95% CI, 1.09-1.24; P less than .0001).
Going forward, the researchers write, “future studies on these patients should attempt to evaluate the impact of bariatric surgery on the long-term outcomes of arthroplasty.”
The study was supported by various funders including the National Natural Science Foundation of China, the Natural Science Foundation of Guangdong Province, the Project of Administration of Traditional Chinese Medicine of Guangdong Province and others. No author disclosures are reported.
SOURCE: Wang Y et al. J Arthroplasty. 2019;S0883-5403(19)30667-9.
a large study has found.
The study, led by Yicun Wang, PhD, of Nanjing (China) University was published in the Journal of Arthroplasty. “Generally speaking, bariatric surgery decreases some postoperative complications, decreases length of stay, and lowers mortality,” the study investigators wrote, [but] anemia and blood transfusion seem to be more common in patients with prior bariatric surgery.
They analyzed the effect of bariatric surgery on subsequent arthroplasty in morbidly obese patients in the United States using Nationwide Inpatient Sample 2006-2014 data on total hip arthroplasty (THA) and total knee arthroplasty (TKA). The researchers defined morbid obese patients as those with a body mass index higher than 40 kg/m2.
Among patients who underwent TKA, the researchers compared a group of 9,803 morbidly obese patients with the same number of patients who had undergone bariatric surgery. The two groups were matched by age, sex, income, primary insurance payer, and race.
There were large differences between the bariatric surgery group vs. morbidly obese group: Pulmonary embolism was much more common in the morbid obesity group (odds ratio, 0.22; 95% confidence interval, 0.05-1.03; P = .0346) while blood transfusion was more common in the bariatric surgery group (OR, 1.76; 95% CI, 1.52-2.03; P less than .0001).
For TKA, the researchers used the same approach to analyze 2,540 matched pairs of patients. In the bariatric surgery vs. morbidly obese comparison, pulmonary embolism was more common in the morbidly obese group (OR, 0.34; 95% CI, 0.20-0.57; P less than .0001), as were respiratory complications (OR, 0.45; 95% CI, 0.26-0.78; P = .0032) and death (OR, 0.07; 95% CI, 0.01-0.50; P = .0005). But the bariatric surgery group had higher levels of blood transfusion (OR, 1.87; 95% CI, 1.71-2.04; P less than .0001) and anemia (OR, 1.16; 95% CI, 1.09-1.24; P less than .0001).
Going forward, the researchers write, “future studies on these patients should attempt to evaluate the impact of bariatric surgery on the long-term outcomes of arthroplasty.”
The study was supported by various funders including the National Natural Science Foundation of China, the Natural Science Foundation of Guangdong Province, the Project of Administration of Traditional Chinese Medicine of Guangdong Province and others. No author disclosures are reported.
SOURCE: Wang Y et al. J Arthroplasty. 2019;S0883-5403(19)30667-9.
a large study has found.
The study, led by Yicun Wang, PhD, of Nanjing (China) University was published in the Journal of Arthroplasty. “Generally speaking, bariatric surgery decreases some postoperative complications, decreases length of stay, and lowers mortality,” the study investigators wrote, [but] anemia and blood transfusion seem to be more common in patients with prior bariatric surgery.
They analyzed the effect of bariatric surgery on subsequent arthroplasty in morbidly obese patients in the United States using Nationwide Inpatient Sample 2006-2014 data on total hip arthroplasty (THA) and total knee arthroplasty (TKA). The researchers defined morbid obese patients as those with a body mass index higher than 40 kg/m2.
Among patients who underwent TKA, the researchers compared a group of 9,803 morbidly obese patients with the same number of patients who had undergone bariatric surgery. The two groups were matched by age, sex, income, primary insurance payer, and race.
There were large differences between the bariatric surgery group vs. morbidly obese group: Pulmonary embolism was much more common in the morbid obesity group (odds ratio, 0.22; 95% confidence interval, 0.05-1.03; P = .0346) while blood transfusion was more common in the bariatric surgery group (OR, 1.76; 95% CI, 1.52-2.03; P less than .0001).
For TKA, the researchers used the same approach to analyze 2,540 matched pairs of patients. In the bariatric surgery vs. morbidly obese comparison, pulmonary embolism was more common in the morbidly obese group (OR, 0.34; 95% CI, 0.20-0.57; P less than .0001), as were respiratory complications (OR, 0.45; 95% CI, 0.26-0.78; P = .0032) and death (OR, 0.07; 95% CI, 0.01-0.50; P = .0005). But the bariatric surgery group had higher levels of blood transfusion (OR, 1.87; 95% CI, 1.71-2.04; P less than .0001) and anemia (OR, 1.16; 95% CI, 1.09-1.24; P less than .0001).
Going forward, the researchers write, “future studies on these patients should attempt to evaluate the impact of bariatric surgery on the long-term outcomes of arthroplasty.”
The study was supported by various funders including the National Natural Science Foundation of China, the Natural Science Foundation of Guangdong Province, the Project of Administration of Traditional Chinese Medicine of Guangdong Province and others. No author disclosures are reported.
SOURCE: Wang Y et al. J Arthroplasty. 2019;S0883-5403(19)30667-9.
FROM THE JOURNAL OF ARTHROPLASTY
Drug doses for heart failure could possibly be halved for women
Men and women react differently to common drugs used to treat heart failure with reduced ejection fraction (HFrEF), according to findings from a new European study, and women may be able to safely cut their doses in half and get the same level of relief as that provided by larger doses.
“This study ... brings into question what the true optimal medical therapy is for women versus men,” the study authors, led by Bernadet T. Santema, MD, of the University Medical Center Groningen (the Netherlands), wrote in an article published in the Lancet.
Dr. Santema and colleagues noted that current guidelines for the use of ACE inhibitors or angiotensin-receptor blockers (ARBs) and beta-blockers for men and women with heart failure do not differentiate between the genders, despite findings showing that, “with the same dose, the maximum plasma concentrations of ACE inhibitors, ARBs, and beta-blockers were up to 2.5 times higher in women than in men.”
In addition, the researchers wrote, women are much more likely than men to suffer side effects from medications, and the effects tend to be more severe.
HFrEF accounts for an estimated 50% of the 5.7 million patients with heart failure in the United States (Nat Rev Dis Primers. 2017 Aug 24. doi: 10.1038/nrdp.2017.58; Card Fail Rev. 2017;3[1]:7-11.)
For the new study, researchers launched an ad hoc analysis of the findings of a prospective study of HFrEF patients in 11 European countries (1,308 men and 402 women) who took drugs in the three classes. Patients were receiving suboptimal medication doses at the start of the study, and physicians were encouraged to increase their medication. The median follow-up for the primary endpoint was 21 months.
“In men, the lowest hazards of death or hospitalization for heart failure occurred at 100% of the recommended dose of ACE inhibitors or ARBs and beta-blockers, but women showed about 30% lower risk at only 50% of the recommended doses, with no further decrease in risk at higher dose levels,” the researchers wrote. “These sex differences were still present after adjusting for clinical covariates, including age and body surface area.”
The researchers analyzed an Asian registry (3,539 men, 961 women) as a comparison and found the identical numbers.
“Our study provides evidence supporting the hypothesis that women with HFrEF might have the best outcomes with lower doses of ACE inhibitors or ARBs and beta-blockers than do men, and lower doses than recommended in international guidelines for heart failure,” they wrote. However, they added that it was not likely that sex-specific studies analyzing doses would be performed.
In an accompanying editorial, Heather P. Whitley, PharmD, and Warren D. Smith, PharmD, noted that clinical research has often failed to take gender differences into account. They wrote that the study – the first of its kind – was well executed and raises important questions, but the analysis did not take into account the prevalence of adverse effects or the serum concentrations of the various medications. Although those limitations weaken the findings, the study still offers evidence that gender-based, drug-dose guidelines deserve consideration, wrote Dr. Whitley, of Auburn (Ala.) University, and Dr. Smith, of Baptist Health System, Montgomery, Ala (Lancet. 2019 Aug 22. doi: 10.1016/S0140-6736[19]31812-4).
The study was funded by the European Commission. Several study authors reported various disclosures. Dr. Whitley and Dr. Smith reported no conflicts of interest.
SOURCE: Santema BT et al. Lancet. 2019 Aug 22. doi: 10.1016/S0140-6736(19)31792-1.
Men and women react differently to common drugs used to treat heart failure with reduced ejection fraction (HFrEF), according to findings from a new European study, and women may be able to safely cut their doses in half and get the same level of relief as that provided by larger doses.
“This study ... brings into question what the true optimal medical therapy is for women versus men,” the study authors, led by Bernadet T. Santema, MD, of the University Medical Center Groningen (the Netherlands), wrote in an article published in the Lancet.
Dr. Santema and colleagues noted that current guidelines for the use of ACE inhibitors or angiotensin-receptor blockers (ARBs) and beta-blockers for men and women with heart failure do not differentiate between the genders, despite findings showing that, “with the same dose, the maximum plasma concentrations of ACE inhibitors, ARBs, and beta-blockers were up to 2.5 times higher in women than in men.”
In addition, the researchers wrote, women are much more likely than men to suffer side effects from medications, and the effects tend to be more severe.
HFrEF accounts for an estimated 50% of the 5.7 million patients with heart failure in the United States (Nat Rev Dis Primers. 2017 Aug 24. doi: 10.1038/nrdp.2017.58; Card Fail Rev. 2017;3[1]:7-11.)
For the new study, researchers launched an ad hoc analysis of the findings of a prospective study of HFrEF patients in 11 European countries (1,308 men and 402 women) who took drugs in the three classes. Patients were receiving suboptimal medication doses at the start of the study, and physicians were encouraged to increase their medication. The median follow-up for the primary endpoint was 21 months.
“In men, the lowest hazards of death or hospitalization for heart failure occurred at 100% of the recommended dose of ACE inhibitors or ARBs and beta-blockers, but women showed about 30% lower risk at only 50% of the recommended doses, with no further decrease in risk at higher dose levels,” the researchers wrote. “These sex differences were still present after adjusting for clinical covariates, including age and body surface area.”
The researchers analyzed an Asian registry (3,539 men, 961 women) as a comparison and found the identical numbers.
“Our study provides evidence supporting the hypothesis that women with HFrEF might have the best outcomes with lower doses of ACE inhibitors or ARBs and beta-blockers than do men, and lower doses than recommended in international guidelines for heart failure,” they wrote. However, they added that it was not likely that sex-specific studies analyzing doses would be performed.
In an accompanying editorial, Heather P. Whitley, PharmD, and Warren D. Smith, PharmD, noted that clinical research has often failed to take gender differences into account. They wrote that the study – the first of its kind – was well executed and raises important questions, but the analysis did not take into account the prevalence of adverse effects or the serum concentrations of the various medications. Although those limitations weaken the findings, the study still offers evidence that gender-based, drug-dose guidelines deserve consideration, wrote Dr. Whitley, of Auburn (Ala.) University, and Dr. Smith, of Baptist Health System, Montgomery, Ala (Lancet. 2019 Aug 22. doi: 10.1016/S0140-6736[19]31812-4).
The study was funded by the European Commission. Several study authors reported various disclosures. Dr. Whitley and Dr. Smith reported no conflicts of interest.
SOURCE: Santema BT et al. Lancet. 2019 Aug 22. doi: 10.1016/S0140-6736(19)31792-1.
Men and women react differently to common drugs used to treat heart failure with reduced ejection fraction (HFrEF), according to findings from a new European study, and women may be able to safely cut their doses in half and get the same level of relief as that provided by larger doses.
“This study ... brings into question what the true optimal medical therapy is for women versus men,” the study authors, led by Bernadet T. Santema, MD, of the University Medical Center Groningen (the Netherlands), wrote in an article published in the Lancet.
Dr. Santema and colleagues noted that current guidelines for the use of ACE inhibitors or angiotensin-receptor blockers (ARBs) and beta-blockers for men and women with heart failure do not differentiate between the genders, despite findings showing that, “with the same dose, the maximum plasma concentrations of ACE inhibitors, ARBs, and beta-blockers were up to 2.5 times higher in women than in men.”
In addition, the researchers wrote, women are much more likely than men to suffer side effects from medications, and the effects tend to be more severe.
HFrEF accounts for an estimated 50% of the 5.7 million patients with heart failure in the United States (Nat Rev Dis Primers. 2017 Aug 24. doi: 10.1038/nrdp.2017.58; Card Fail Rev. 2017;3[1]:7-11.)
For the new study, researchers launched an ad hoc analysis of the findings of a prospective study of HFrEF patients in 11 European countries (1,308 men and 402 women) who took drugs in the three classes. Patients were receiving suboptimal medication doses at the start of the study, and physicians were encouraged to increase their medication. The median follow-up for the primary endpoint was 21 months.
“In men, the lowest hazards of death or hospitalization for heart failure occurred at 100% of the recommended dose of ACE inhibitors or ARBs and beta-blockers, but women showed about 30% lower risk at only 50% of the recommended doses, with no further decrease in risk at higher dose levels,” the researchers wrote. “These sex differences were still present after adjusting for clinical covariates, including age and body surface area.”
The researchers analyzed an Asian registry (3,539 men, 961 women) as a comparison and found the identical numbers.
“Our study provides evidence supporting the hypothesis that women with HFrEF might have the best outcomes with lower doses of ACE inhibitors or ARBs and beta-blockers than do men, and lower doses than recommended in international guidelines for heart failure,” they wrote. However, they added that it was not likely that sex-specific studies analyzing doses would be performed.
In an accompanying editorial, Heather P. Whitley, PharmD, and Warren D. Smith, PharmD, noted that clinical research has often failed to take gender differences into account. They wrote that the study – the first of its kind – was well executed and raises important questions, but the analysis did not take into account the prevalence of adverse effects or the serum concentrations of the various medications. Although those limitations weaken the findings, the study still offers evidence that gender-based, drug-dose guidelines deserve consideration, wrote Dr. Whitley, of Auburn (Ala.) University, and Dr. Smith, of Baptist Health System, Montgomery, Ala (Lancet. 2019 Aug 22. doi: 10.1016/S0140-6736[19]31812-4).
The study was funded by the European Commission. Several study authors reported various disclosures. Dr. Whitley and Dr. Smith reported no conflicts of interest.
SOURCE: Santema BT et al. Lancet. 2019 Aug 22. doi: 10.1016/S0140-6736(19)31792-1.
FROM THE LANCET
Be alert to deep SSI risk after knee surgery
Deep surgical-site infections (SSIs) and septic arthritis are not uncommon after the surgeries for periarticular knee fractures, a meta-analysis of existing research found.
A smaller analysis of 1,567 patients found that 2.4% had septic arthritis. “Surgeons managing periarticular knee fractures should be vigilant when wounds are not pristine,” the investigators recommended.
The report, which appeared in JAMA Network Open, was led by premed student Grayson R. Norris of High Point (N.C.) University.
The researchers noted that there are widely variable statistics regarding SSI after surgery for periarticular knee fractures. A better understanding of the risk would help orthopedic surgeons, given the mortality risk and extra costs associated with postoperative deep SSIs.
For the analysis, the researchers reviewed 117 studies with 11,432 patients who had fractures in the tibial plateau (61% of studies), distal femur (14%), proximal tibia (11%), patella (9%), and multiple sites (6%). More than two-thirds of the studies were retrospective.
Overall, 5.7% of patients suffered deep SSIs, with the highest percentage in the proximal tibia group (6.4%).
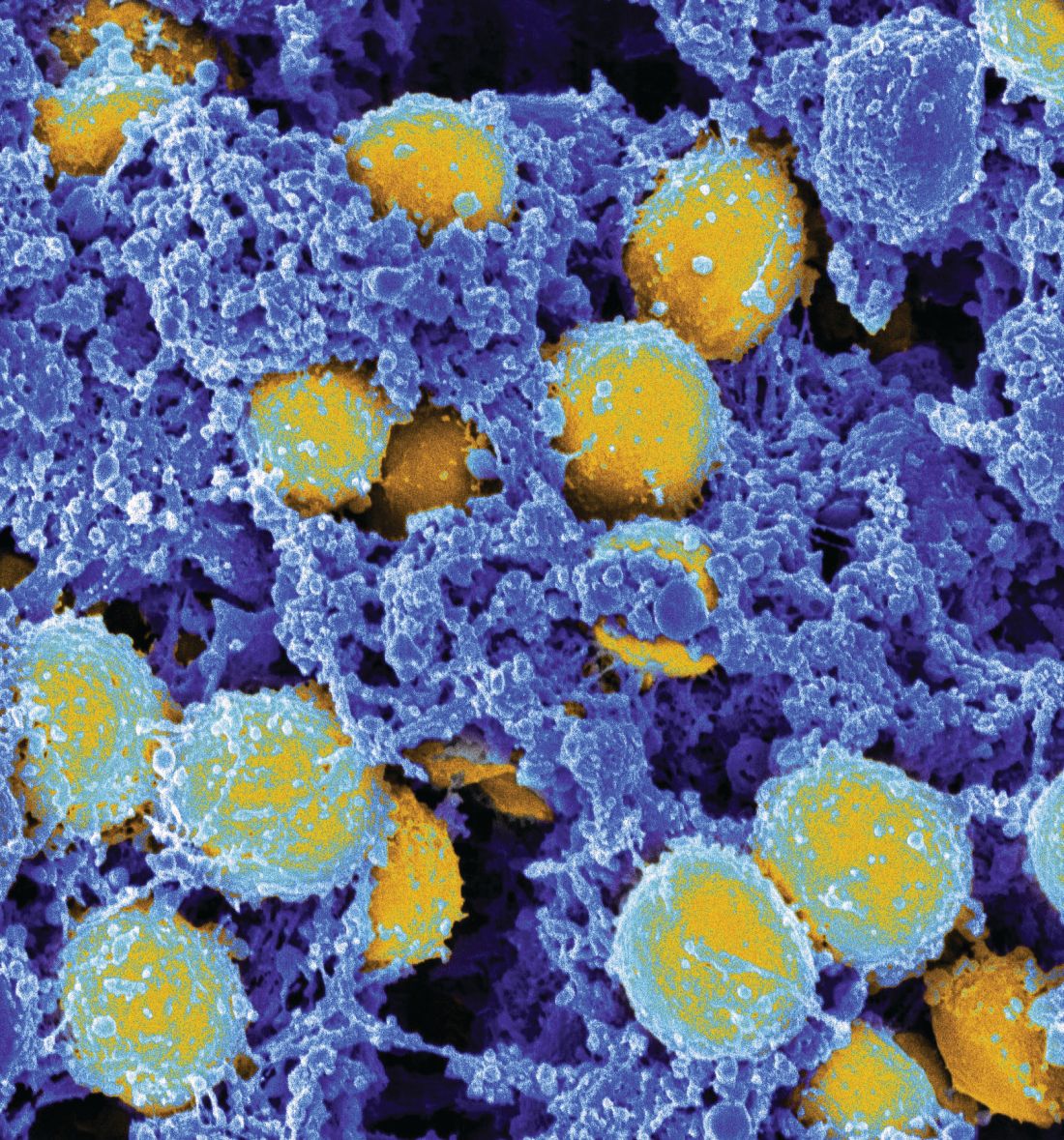
A total of 20 studies examined septic arthritis and found that 2.4% of patients in those studies suffered from the condition. Of 182 cases of deep SSIs with bacterial culture results, methicillin-resistant Staphylococcus aureus (MRSA) and methicillin-susceptible S. aureus were the most common bacteria.
“Considering that MRSA was the most common pathogen in our study and that this pathogen is increasing in prevalence, health care practitioners should revisit the use of specific and appropriate prophylactic antibiotics,” the researchers wrote. “Risk factors, such as open fractures, diabetes, smoking, and, most importantly, compartment syndrome, should alert the treating surgeon to an increased risk. Further work is needed to mitigate the association of these conditions with SSI risk in periarticular knee fractures.”
The researchers added that many of the studies in their analysis were of poor quality. “Authors in orthopedic traumatology should strive to conduct higher-quality research, such as randomized clinical trials and case-control or cohort studies,” they noted.
One author reported receiving grants from Zimmer Biomet and DePuy Synthes outside the submitted work. No other disclosures were reported. No study funding was reported.
SOURCE: Norris GR et al. JAMA Netw Open. 2019;2(8):e199951.
Deep surgical-site infections (SSIs) and septic arthritis are not uncommon after the surgeries for periarticular knee fractures, a meta-analysis of existing research found.
A smaller analysis of 1,567 patients found that 2.4% had septic arthritis. “Surgeons managing periarticular knee fractures should be vigilant when wounds are not pristine,” the investigators recommended.
The report, which appeared in JAMA Network Open, was led by premed student Grayson R. Norris of High Point (N.C.) University.
The researchers noted that there are widely variable statistics regarding SSI after surgery for periarticular knee fractures. A better understanding of the risk would help orthopedic surgeons, given the mortality risk and extra costs associated with postoperative deep SSIs.
For the analysis, the researchers reviewed 117 studies with 11,432 patients who had fractures in the tibial plateau (61% of studies), distal femur (14%), proximal tibia (11%), patella (9%), and multiple sites (6%). More than two-thirds of the studies were retrospective.
Overall, 5.7% of patients suffered deep SSIs, with the highest percentage in the proximal tibia group (6.4%).
A total of 20 studies examined septic arthritis and found that 2.4% of patients in those studies suffered from the condition. Of 182 cases of deep SSIs with bacterial culture results, methicillin-resistant Staphylococcus aureus (MRSA) and methicillin-susceptible S. aureus were the most common bacteria.
“Considering that MRSA was the most common pathogen in our study and that this pathogen is increasing in prevalence, health care practitioners should revisit the use of specific and appropriate prophylactic antibiotics,” the researchers wrote. “Risk factors, such as open fractures, diabetes, smoking, and, most importantly, compartment syndrome, should alert the treating surgeon to an increased risk. Further work is needed to mitigate the association of these conditions with SSI risk in periarticular knee fractures.”
The researchers added that many of the studies in their analysis were of poor quality. “Authors in orthopedic traumatology should strive to conduct higher-quality research, such as randomized clinical trials and case-control or cohort studies,” they noted.
One author reported receiving grants from Zimmer Biomet and DePuy Synthes outside the submitted work. No other disclosures were reported. No study funding was reported.
SOURCE: Norris GR et al. JAMA Netw Open. 2019;2(8):e199951.
Deep surgical-site infections (SSIs) and septic arthritis are not uncommon after the surgeries for periarticular knee fractures, a meta-analysis of existing research found.
A smaller analysis of 1,567 patients found that 2.4% had septic arthritis. “Surgeons managing periarticular knee fractures should be vigilant when wounds are not pristine,” the investigators recommended.
The report, which appeared in JAMA Network Open, was led by premed student Grayson R. Norris of High Point (N.C.) University.
The researchers noted that there are widely variable statistics regarding SSI after surgery for periarticular knee fractures. A better understanding of the risk would help orthopedic surgeons, given the mortality risk and extra costs associated with postoperative deep SSIs.
For the analysis, the researchers reviewed 117 studies with 11,432 patients who had fractures in the tibial plateau (61% of studies), distal femur (14%), proximal tibia (11%), patella (9%), and multiple sites (6%). More than two-thirds of the studies were retrospective.
Overall, 5.7% of patients suffered deep SSIs, with the highest percentage in the proximal tibia group (6.4%).
A total of 20 studies examined septic arthritis and found that 2.4% of patients in those studies suffered from the condition. Of 182 cases of deep SSIs with bacterial culture results, methicillin-resistant Staphylococcus aureus (MRSA) and methicillin-susceptible S. aureus were the most common bacteria.
“Considering that MRSA was the most common pathogen in our study and that this pathogen is increasing in prevalence, health care practitioners should revisit the use of specific and appropriate prophylactic antibiotics,” the researchers wrote. “Risk factors, such as open fractures, diabetes, smoking, and, most importantly, compartment syndrome, should alert the treating surgeon to an increased risk. Further work is needed to mitigate the association of these conditions with SSI risk in periarticular knee fractures.”
The researchers added that many of the studies in their analysis were of poor quality. “Authors in orthopedic traumatology should strive to conduct higher-quality research, such as randomized clinical trials and case-control or cohort studies,” they noted.
One author reported receiving grants from Zimmer Biomet and DePuy Synthes outside the submitted work. No other disclosures were reported. No study funding was reported.
SOURCE: Norris GR et al. JAMA Netw Open. 2019;2(8):e199951.
FROM JAMA NETWORK OPEN
New study confirms rise in U.S. suicide rates, particularly in rural areas
County-by-county analysis cites links to higher density of gun shops, other factors
Suicide rates in the United States climbed from 1999 to 2016, a new cross-sectional study found, and the increases were highest in rural areas.
“These findings are consistent with previous studies demonstrating higher and more rapidly increasing suicide rates in rural areas and are of considerable interest in light of the work by [Anne] Case and [Angus] Deaton,” wrote Danielle L. Steelesmith, PhD, and associates. “While increasing rates of suicide are well documented, little is known about contextual factors associated with county-level suicide rates.” The findings appear in JAMA Network Open.
To examine those contextual factors, Dr. Steelesmith, of the department of psychiatry and behavioral health at the Ohio State University, Columbus, and associates analyzed county-by-county suicide statistics from 1999 to 2016 for adults aged 25-64 years, noting that they “focused on this age range because most studies on mortality trends have focused on this age range.”
The researchers developed 3-year suicide averages for counties for rate “stabilization” purposes. They placed the counties into four categories (large metropolitan, small metropolitan, micropolitan, and rural), and used various data sources to gather various types of statistics about the communities.
Most of those who died by suicide were men (77%), and most (51%) were aged 45-64 years. The median suicide rate per county rose from 15 per 100,000 (1999-2001) to 21 per 100,000 (2014-2016), reported Dr. Steelesmith and associates.
Rural counties only made up 2% of the suicides, compared with 81% in large and small metropolitan counties, but suicide rates were “increasing most rapidly in rural areas, although all county types saw increases during the period studied,” Dr. Steelesmith and associates wrote.
They added that “counties with the highest excess risk of suicide tended to be in Western states (e.g., Colorado, New Mexico, Utah, and Wyoming), Appalachia (e.g., Kentucky, Virginia, and West Virginia), and the Ozarks (e.g., Arkansas and Missouri).”
In addition to the connections between increasing suicide rates, living in a rural area, and a higher density of gun shops, the researchers cited other contextual factors. Among those factors were higher median age and higher percentages of non-Hispanic whites, numbers of residents without health insurance, and veterans. They also found links between higher suicide rates and worse numbers on indexes designed to measure social capital; social fragmentation; and deprivation, a measure encompassing lower education, employment levels, and income.
“Long-term and persistent poverty appears to be more entrenched and economic opportunities more constrained in rural areas,” Dr. Steelesmith and associates wrote. “Greater social isolation, challenges related to transportation and interpersonal communication, and associated difficulties accessing health and mental health services likely contribute to the disproportionate association of deprivation with suicide in rural counties.”
Dr. Steelesmith and associates cited several limitations. One key limitation is that, because the study looked only at adults aged 25-64 years, the results might not be generalizable to youth or elderly adults.
No study funding was reported. One study author reported serving on the scientific advisory board of Clarigent Health and receiving grant support from the National Institute of Mental Health outside of the submitted work. No other disclosures were reported.
SOURCE: Steelesmith DL et al. JAMA Netw Open. 2019 Sep 6. doi: 10.1001/jamanetworkopen.2019.10936.
County-by-county analysis cites links to higher density of gun shops, other factors
County-by-county analysis cites links to higher density of gun shops, other factors
Suicide rates in the United States climbed from 1999 to 2016, a new cross-sectional study found, and the increases were highest in rural areas.
“These findings are consistent with previous studies demonstrating higher and more rapidly increasing suicide rates in rural areas and are of considerable interest in light of the work by [Anne] Case and [Angus] Deaton,” wrote Danielle L. Steelesmith, PhD, and associates. “While increasing rates of suicide are well documented, little is known about contextual factors associated with county-level suicide rates.” The findings appear in JAMA Network Open.
To examine those contextual factors, Dr. Steelesmith, of the department of psychiatry and behavioral health at the Ohio State University, Columbus, and associates analyzed county-by-county suicide statistics from 1999 to 2016 for adults aged 25-64 years, noting that they “focused on this age range because most studies on mortality trends have focused on this age range.”
The researchers developed 3-year suicide averages for counties for rate “stabilization” purposes. They placed the counties into four categories (large metropolitan, small metropolitan, micropolitan, and rural), and used various data sources to gather various types of statistics about the communities.
Most of those who died by suicide were men (77%), and most (51%) were aged 45-64 years. The median suicide rate per county rose from 15 per 100,000 (1999-2001) to 21 per 100,000 (2014-2016), reported Dr. Steelesmith and associates.
Rural counties only made up 2% of the suicides, compared with 81% in large and small metropolitan counties, but suicide rates were “increasing most rapidly in rural areas, although all county types saw increases during the period studied,” Dr. Steelesmith and associates wrote.
They added that “counties with the highest excess risk of suicide tended to be in Western states (e.g., Colorado, New Mexico, Utah, and Wyoming), Appalachia (e.g., Kentucky, Virginia, and West Virginia), and the Ozarks (e.g., Arkansas and Missouri).”
In addition to the connections between increasing suicide rates, living in a rural area, and a higher density of gun shops, the researchers cited other contextual factors. Among those factors were higher median age and higher percentages of non-Hispanic whites, numbers of residents without health insurance, and veterans. They also found links between higher suicide rates and worse numbers on indexes designed to measure social capital; social fragmentation; and deprivation, a measure encompassing lower education, employment levels, and income.
“Long-term and persistent poverty appears to be more entrenched and economic opportunities more constrained in rural areas,” Dr. Steelesmith and associates wrote. “Greater social isolation, challenges related to transportation and interpersonal communication, and associated difficulties accessing health and mental health services likely contribute to the disproportionate association of deprivation with suicide in rural counties.”
Dr. Steelesmith and associates cited several limitations. One key limitation is that, because the study looked only at adults aged 25-64 years, the results might not be generalizable to youth or elderly adults.
No study funding was reported. One study author reported serving on the scientific advisory board of Clarigent Health and receiving grant support from the National Institute of Mental Health outside of the submitted work. No other disclosures were reported.
SOURCE: Steelesmith DL et al. JAMA Netw Open. 2019 Sep 6. doi: 10.1001/jamanetworkopen.2019.10936.
Suicide rates in the United States climbed from 1999 to 2016, a new cross-sectional study found, and the increases were highest in rural areas.
“These findings are consistent with previous studies demonstrating higher and more rapidly increasing suicide rates in rural areas and are of considerable interest in light of the work by [Anne] Case and [Angus] Deaton,” wrote Danielle L. Steelesmith, PhD, and associates. “While increasing rates of suicide are well documented, little is known about contextual factors associated with county-level suicide rates.” The findings appear in JAMA Network Open.
To examine those contextual factors, Dr. Steelesmith, of the department of psychiatry and behavioral health at the Ohio State University, Columbus, and associates analyzed county-by-county suicide statistics from 1999 to 2016 for adults aged 25-64 years, noting that they “focused on this age range because most studies on mortality trends have focused on this age range.”
The researchers developed 3-year suicide averages for counties for rate “stabilization” purposes. They placed the counties into four categories (large metropolitan, small metropolitan, micropolitan, and rural), and used various data sources to gather various types of statistics about the communities.
Most of those who died by suicide were men (77%), and most (51%) were aged 45-64 years. The median suicide rate per county rose from 15 per 100,000 (1999-2001) to 21 per 100,000 (2014-2016), reported Dr. Steelesmith and associates.
Rural counties only made up 2% of the suicides, compared with 81% in large and small metropolitan counties, but suicide rates were “increasing most rapidly in rural areas, although all county types saw increases during the period studied,” Dr. Steelesmith and associates wrote.
They added that “counties with the highest excess risk of suicide tended to be in Western states (e.g., Colorado, New Mexico, Utah, and Wyoming), Appalachia (e.g., Kentucky, Virginia, and West Virginia), and the Ozarks (e.g., Arkansas and Missouri).”
In addition to the connections between increasing suicide rates, living in a rural area, and a higher density of gun shops, the researchers cited other contextual factors. Among those factors were higher median age and higher percentages of non-Hispanic whites, numbers of residents without health insurance, and veterans. They also found links between higher suicide rates and worse numbers on indexes designed to measure social capital; social fragmentation; and deprivation, a measure encompassing lower education, employment levels, and income.
“Long-term and persistent poverty appears to be more entrenched and economic opportunities more constrained in rural areas,” Dr. Steelesmith and associates wrote. “Greater social isolation, challenges related to transportation and interpersonal communication, and associated difficulties accessing health and mental health services likely contribute to the disproportionate association of deprivation with suicide in rural counties.”
Dr. Steelesmith and associates cited several limitations. One key limitation is that, because the study looked only at adults aged 25-64 years, the results might not be generalizable to youth or elderly adults.
No study funding was reported. One study author reported serving on the scientific advisory board of Clarigent Health and receiving grant support from the National Institute of Mental Health outside of the submitted work. No other disclosures were reported.
SOURCE: Steelesmith DL et al. JAMA Netw Open. 2019 Sep 6. doi: 10.1001/jamanetworkopen.2019.10936.
FROM JAMA NETWORK OPEN
Diabetic neuropathy: Often silent, often dangerous
SAN DIEGO – Neuropathy can blur the seriousness of injuries, especially in patients with diabetes, and that can lead to severe consequences such as falls, foot ulcers, gangrene, and amputations, said Lucia M. Novak, MSN, ANP-BC, BC-ADM, CDTC, in a presentation on assessing and treating neuropathies at the Metabolic & Endocrine Disease Summit, sponsored by Global Academy for Medical Education.
As many as half of the cases of diabetic neuropathy may have no symptoms, and more than two-thirds of cases of diabetic neuropathy, even some with obvious symptoms, are ignored or missed by clinicians, said Ms. Novak, director of the Riverside Diabetes Center and adjunct assistant professor at the Uniformed Services University of the Health Sciences, both in Bethesda, Md.
At the same time, she said, diabetic neuropathy is very common. It affects an estimated 10%-15% of newly diagnosed patients with type 2 diabetes, 50% of patients with type 2 disease after 10 years, and as many as 30% of patients with prediabetes.
The condition is less common in type 1 diabetes, affecting an estimated 20% of patients after 20 years, she said.
“All we can do in our patients with type 2 diabetes and diabetic neuropathy, is to slow down the progression, although improving glycemic control can prevent it in type 1,” she said, citing findings suggesting that
A 2012 report analyzed research into the effect of glycemic control on neuropathy in diabetes and found a pair of studies that reported a 60%-70% reduction of risk in patients with type 1 diabetes who received regular insulin dosing. However, the evidence for type 2 diabetes was not as definitive, and analysis of findings from eight randomized, controlled trials in patients with type 2 diabetes supported a relatively small reduction in the development of neuropathy in patients with type 2 diabetes who were receiving enhanced glycemic control (Lancet Neurol. 2012;11[6]:521-34).
Ms. Novak focused mainly on peripheral neuropathy, which is believed to account for 50%-75% of all neuropathy in patients with diabetes. She emphasized the importance of screening because it is crucial for preventing foot ulcers, which affect more than a third of patients with diabetes over their lifetimes.
She recommended following the American Diabetes Association’s 2017 position statement on diabetic neuropathy (Diabetes Care. 2017;40[1]:136-54), beginning with performing a visual examination of the feet at every visit.
Comprehensive screening
In patients with type 1 diabetes, there should be an annual comprehensive screening beginning within 5 years of diagnosis. Patients with type 2 disease should be screened at diagnosis and then annually, as outlined in the ADA statement.
The comprehensive exam involves using tools, such as tuning forks and monofilaments, to test sensation. Different tools are required to test both small and large fibers in the foot, Ms. Novak said, and doing both kinds of testing greatly increases the likelihood of detecting neuropathy.
Check for pulse, bone deformities, dry skin
In addition, “you’ll be feeling for their pulses, looking for bony deformities, and looking at anything is going on between the toes [to make sure] the skin is intact,” she said.
Patients with diabetic neuropathy often have dry skin, she said, so make sure they’re moisturizing. “Look at the condition of their shoes,” she added, “which will tell you how they walk.”
Ill-fitting shoes are a common cause of foot ulcers, said Ms. Novak, who noted that some patients refuse to wear unattractive diabetic shoes and prefer to wear more fashionable – and dangerous – tight-fitting shoes.
Treatment options
Glycemic control makes a difference, especially for patients with type 1, as does control of risk factors, such as obesity. But diabetic neuropathy cannot be reversed.
Pain can be managed with a range of medications. “We can’t cure the neuropathy, we can at least help patients with the symptoms so that they can have a good night’s sleep,” she said.
Ms. Novak also suggested passing on the following snippets of advice to patients:
- Do not walk barefoot.
- Check your feet every day.
- Moisturize your skin, and always dry thoroughly between your toes.
- Seek medical attention if your nails cut into your skin or you develop a callus or areas of redness/warmth.
Global Academy and this news organization are owned by the same parent company. Ms. Novak reported relationships with Nova Nordisk, Sanofi, Janssen, and AstraZeneca.
SAN DIEGO – Neuropathy can blur the seriousness of injuries, especially in patients with diabetes, and that can lead to severe consequences such as falls, foot ulcers, gangrene, and amputations, said Lucia M. Novak, MSN, ANP-BC, BC-ADM, CDTC, in a presentation on assessing and treating neuropathies at the Metabolic & Endocrine Disease Summit, sponsored by Global Academy for Medical Education.
As many as half of the cases of diabetic neuropathy may have no symptoms, and more than two-thirds of cases of diabetic neuropathy, even some with obvious symptoms, are ignored or missed by clinicians, said Ms. Novak, director of the Riverside Diabetes Center and adjunct assistant professor at the Uniformed Services University of the Health Sciences, both in Bethesda, Md.
At the same time, she said, diabetic neuropathy is very common. It affects an estimated 10%-15% of newly diagnosed patients with type 2 diabetes, 50% of patients with type 2 disease after 10 years, and as many as 30% of patients with prediabetes.
The condition is less common in type 1 diabetes, affecting an estimated 20% of patients after 20 years, she said.
“All we can do in our patients with type 2 diabetes and diabetic neuropathy, is to slow down the progression, although improving glycemic control can prevent it in type 1,” she said, citing findings suggesting that
A 2012 report analyzed research into the effect of glycemic control on neuropathy in diabetes and found a pair of studies that reported a 60%-70% reduction of risk in patients with type 1 diabetes who received regular insulin dosing. However, the evidence for type 2 diabetes was not as definitive, and analysis of findings from eight randomized, controlled trials in patients with type 2 diabetes supported a relatively small reduction in the development of neuropathy in patients with type 2 diabetes who were receiving enhanced glycemic control (Lancet Neurol. 2012;11[6]:521-34).
Ms. Novak focused mainly on peripheral neuropathy, which is believed to account for 50%-75% of all neuropathy in patients with diabetes. She emphasized the importance of screening because it is crucial for preventing foot ulcers, which affect more than a third of patients with diabetes over their lifetimes.
She recommended following the American Diabetes Association’s 2017 position statement on diabetic neuropathy (Diabetes Care. 2017;40[1]:136-54), beginning with performing a visual examination of the feet at every visit.
Comprehensive screening
In patients with type 1 diabetes, there should be an annual comprehensive screening beginning within 5 years of diagnosis. Patients with type 2 disease should be screened at diagnosis and then annually, as outlined in the ADA statement.
The comprehensive exam involves using tools, such as tuning forks and monofilaments, to test sensation. Different tools are required to test both small and large fibers in the foot, Ms. Novak said, and doing both kinds of testing greatly increases the likelihood of detecting neuropathy.
Check for pulse, bone deformities, dry skin
In addition, “you’ll be feeling for their pulses, looking for bony deformities, and looking at anything is going on between the toes [to make sure] the skin is intact,” she said.
Patients with diabetic neuropathy often have dry skin, she said, so make sure they’re moisturizing. “Look at the condition of their shoes,” she added, “which will tell you how they walk.”
Ill-fitting shoes are a common cause of foot ulcers, said Ms. Novak, who noted that some patients refuse to wear unattractive diabetic shoes and prefer to wear more fashionable – and dangerous – tight-fitting shoes.
Treatment options
Glycemic control makes a difference, especially for patients with type 1, as does control of risk factors, such as obesity. But diabetic neuropathy cannot be reversed.
Pain can be managed with a range of medications. “We can’t cure the neuropathy, we can at least help patients with the symptoms so that they can have a good night’s sleep,” she said.
Ms. Novak also suggested passing on the following snippets of advice to patients:
- Do not walk barefoot.
- Check your feet every day.
- Moisturize your skin, and always dry thoroughly between your toes.
- Seek medical attention if your nails cut into your skin or you develop a callus or areas of redness/warmth.
Global Academy and this news organization are owned by the same parent company. Ms. Novak reported relationships with Nova Nordisk, Sanofi, Janssen, and AstraZeneca.
SAN DIEGO – Neuropathy can blur the seriousness of injuries, especially in patients with diabetes, and that can lead to severe consequences such as falls, foot ulcers, gangrene, and amputations, said Lucia M. Novak, MSN, ANP-BC, BC-ADM, CDTC, in a presentation on assessing and treating neuropathies at the Metabolic & Endocrine Disease Summit, sponsored by Global Academy for Medical Education.
As many as half of the cases of diabetic neuropathy may have no symptoms, and more than two-thirds of cases of diabetic neuropathy, even some with obvious symptoms, are ignored or missed by clinicians, said Ms. Novak, director of the Riverside Diabetes Center and adjunct assistant professor at the Uniformed Services University of the Health Sciences, both in Bethesda, Md.
At the same time, she said, diabetic neuropathy is very common. It affects an estimated 10%-15% of newly diagnosed patients with type 2 diabetes, 50% of patients with type 2 disease after 10 years, and as many as 30% of patients with prediabetes.
The condition is less common in type 1 diabetes, affecting an estimated 20% of patients after 20 years, she said.
“All we can do in our patients with type 2 diabetes and diabetic neuropathy, is to slow down the progression, although improving glycemic control can prevent it in type 1,” she said, citing findings suggesting that
A 2012 report analyzed research into the effect of glycemic control on neuropathy in diabetes and found a pair of studies that reported a 60%-70% reduction of risk in patients with type 1 diabetes who received regular insulin dosing. However, the evidence for type 2 diabetes was not as definitive, and analysis of findings from eight randomized, controlled trials in patients with type 2 diabetes supported a relatively small reduction in the development of neuropathy in patients with type 2 diabetes who were receiving enhanced glycemic control (Lancet Neurol. 2012;11[6]:521-34).
Ms. Novak focused mainly on peripheral neuropathy, which is believed to account for 50%-75% of all neuropathy in patients with diabetes. She emphasized the importance of screening because it is crucial for preventing foot ulcers, which affect more than a third of patients with diabetes over their lifetimes.
She recommended following the American Diabetes Association’s 2017 position statement on diabetic neuropathy (Diabetes Care. 2017;40[1]:136-54), beginning with performing a visual examination of the feet at every visit.
Comprehensive screening
In patients with type 1 diabetes, there should be an annual comprehensive screening beginning within 5 years of diagnosis. Patients with type 2 disease should be screened at diagnosis and then annually, as outlined in the ADA statement.
The comprehensive exam involves using tools, such as tuning forks and monofilaments, to test sensation. Different tools are required to test both small and large fibers in the foot, Ms. Novak said, and doing both kinds of testing greatly increases the likelihood of detecting neuropathy.
Check for pulse, bone deformities, dry skin
In addition, “you’ll be feeling for their pulses, looking for bony deformities, and looking at anything is going on between the toes [to make sure] the skin is intact,” she said.
Patients with diabetic neuropathy often have dry skin, she said, so make sure they’re moisturizing. “Look at the condition of their shoes,” she added, “which will tell you how they walk.”
Ill-fitting shoes are a common cause of foot ulcers, said Ms. Novak, who noted that some patients refuse to wear unattractive diabetic shoes and prefer to wear more fashionable – and dangerous – tight-fitting shoes.
Treatment options
Glycemic control makes a difference, especially for patients with type 1, as does control of risk factors, such as obesity. But diabetic neuropathy cannot be reversed.
Pain can be managed with a range of medications. “We can’t cure the neuropathy, we can at least help patients with the symptoms so that they can have a good night’s sleep,” she said.
Ms. Novak also suggested passing on the following snippets of advice to patients:
- Do not walk barefoot.
- Check your feet every day.
- Moisturize your skin, and always dry thoroughly between your toes.
- Seek medical attention if your nails cut into your skin or you develop a callus or areas of redness/warmth.
Global Academy and this news organization are owned by the same parent company. Ms. Novak reported relationships with Nova Nordisk, Sanofi, Janssen, and AstraZeneca.
EXPERT ANALYSIS FROM MEDS 2019
Diagnosing and managing diabetes and depression
SAN DIEGO – Nearly 350 years ago, British physician Thomas Willis wrote that diabetes seemed often to occur in patients who were experiencing “significant life stress, sadness, or long sorrow.” That, according to Ellen D. Mandel, DMH, MPA, MS, PA-C, RDN, CDE, a clinical professor at Pace University in New York City, was an important insight into the link between mind and body in patients with diabetes.
“As clinicians, we should be worried about mental illness in our patients with diabetes,” Dr. Mandel, a physician assistant educator, said during a presentation at the Metabolic & Endocrine Disease Summit by Global Academy for Medical Education.
In particular, she said, – and vice versa.
Dr. Mandel pointed to findings suggesting that 11% of patients with diabetes show signs of clinical depression, which is higher than in the general population, with many more believed to have subclinical depression (Diabetes Care. 2015;38[4]:551-60).
Anxiety can be a key factor in trying to understand how diabetes might contribute to depression. “Diabetes is a very stressful condition ... [and patients] may be fatigued and exhausted.” On top of that, they have to make nutrition changes, or at least pay attention to their diet and overall care, all of which can have a cumulatively negative impact on patient well-being.
Conversely, depression can contribute to diabetes. “They kind of go hand in hand,” she said, pointing to depression’s ability to disrupt appetite, diminish energy, and boost levels of cortisol.
Among the findings that provide evidence of a link between diabetes and depression are those from a study in which investigators estimated that for every 1-point increase in depression symptoms, the risk of diabetes will go up by as much as 5% (Clin Diabetes Endocrinol. 2018 Jan 4. doi: 10.1186/s40842-017-0052-1). Moreover, a 2013 review linked the combination of diabetes and depression to an adjusted 1.5-fold increase in risk of all-cause death (PLoS One. 2013 Mar 5. doi: 10.1371/journal.pone.0057058).
Dr. Mandel offered these tips about diagnosing depression in patients with diabetes and helping them feel comfortable:
- Put yourself in the patient’s shoes. “One of the biggest barriers to referring patients to diabetic education is that they don’t want to have to admit to a group that they have diabetes. They keep it to themselves, to their own detriment. In addition, there’s a lot of worry about insurance.” Patients with diabetes often have self-esteem issues and financial or insurance challenges, all of which need to be factored in when working with them, Dr. Mandel said.
- Ask questions and use screening tools. Two simple questions are helpful in starting a conversation and gathering useful information: Over the past 2 weeks, have you often been bothered by [having] little interest or pleasure in doing things? What about being bothered by feeling down, depressed, or hopeless? If the patient answers “yes” to either of these questions, it will be a positive screen, and two “no” answers will be a negative screen. With the “yes” responses, one should follow-up with a screening tool – typically, the one approved by your institution. Dr. Mandel also highlighted the Patient Health Questionnaire depression scale (PHQ-9), which is available online, or the brief, two-item Diabetes Distress Scale (DDS2) questionnaire.
- Keep your own language in mind. “The way you communicate with your patients can elevate their feeling about themselves or destroy how they feel about themselves,” Dr. Mandel said. “We’re trying to stop calling people with diabetes ‘diabetics.’ People don’t want to be labeled like that. Don’t blame yourself if you use this language, but work to make the changes,” Dr. Mandel suggested.
- Watch out for other forms of bias. Beware of unconsciously stereotyping your patients. “It affects how people relate to you, how they adhere to your suggestions, and how much they’ll trust [and confide in] you, which can have clinical implications,” Dr. Mandel said.
Global Academy and this news organization are owned by the same parent company. Dr. Mandel has no disclosures.
SAN DIEGO – Nearly 350 years ago, British physician Thomas Willis wrote that diabetes seemed often to occur in patients who were experiencing “significant life stress, sadness, or long sorrow.” That, according to Ellen D. Mandel, DMH, MPA, MS, PA-C, RDN, CDE, a clinical professor at Pace University in New York City, was an important insight into the link between mind and body in patients with diabetes.
“As clinicians, we should be worried about mental illness in our patients with diabetes,” Dr. Mandel, a physician assistant educator, said during a presentation at the Metabolic & Endocrine Disease Summit by Global Academy for Medical Education.
In particular, she said, – and vice versa.
Dr. Mandel pointed to findings suggesting that 11% of patients with diabetes show signs of clinical depression, which is higher than in the general population, with many more believed to have subclinical depression (Diabetes Care. 2015;38[4]:551-60).
Anxiety can be a key factor in trying to understand how diabetes might contribute to depression. “Diabetes is a very stressful condition ... [and patients] may be fatigued and exhausted.” On top of that, they have to make nutrition changes, or at least pay attention to their diet and overall care, all of which can have a cumulatively negative impact on patient well-being.
Conversely, depression can contribute to diabetes. “They kind of go hand in hand,” she said, pointing to depression’s ability to disrupt appetite, diminish energy, and boost levels of cortisol.
Among the findings that provide evidence of a link between diabetes and depression are those from a study in which investigators estimated that for every 1-point increase in depression symptoms, the risk of diabetes will go up by as much as 5% (Clin Diabetes Endocrinol. 2018 Jan 4. doi: 10.1186/s40842-017-0052-1). Moreover, a 2013 review linked the combination of diabetes and depression to an adjusted 1.5-fold increase in risk of all-cause death (PLoS One. 2013 Mar 5. doi: 10.1371/journal.pone.0057058).
Dr. Mandel offered these tips about diagnosing depression in patients with diabetes and helping them feel comfortable:
- Put yourself in the patient’s shoes. “One of the biggest barriers to referring patients to diabetic education is that they don’t want to have to admit to a group that they have diabetes. They keep it to themselves, to their own detriment. In addition, there’s a lot of worry about insurance.” Patients with diabetes often have self-esteem issues and financial or insurance challenges, all of which need to be factored in when working with them, Dr. Mandel said.
- Ask questions and use screening tools. Two simple questions are helpful in starting a conversation and gathering useful information: Over the past 2 weeks, have you often been bothered by [having] little interest or pleasure in doing things? What about being bothered by feeling down, depressed, or hopeless? If the patient answers “yes” to either of these questions, it will be a positive screen, and two “no” answers will be a negative screen. With the “yes” responses, one should follow-up with a screening tool – typically, the one approved by your institution. Dr. Mandel also highlighted the Patient Health Questionnaire depression scale (PHQ-9), which is available online, or the brief, two-item Diabetes Distress Scale (DDS2) questionnaire.
- Keep your own language in mind. “The way you communicate with your patients can elevate their feeling about themselves or destroy how they feel about themselves,” Dr. Mandel said. “We’re trying to stop calling people with diabetes ‘diabetics.’ People don’t want to be labeled like that. Don’t blame yourself if you use this language, but work to make the changes,” Dr. Mandel suggested.
- Watch out for other forms of bias. Beware of unconsciously stereotyping your patients. “It affects how people relate to you, how they adhere to your suggestions, and how much they’ll trust [and confide in] you, which can have clinical implications,” Dr. Mandel said.
Global Academy and this news organization are owned by the same parent company. Dr. Mandel has no disclosures.
SAN DIEGO – Nearly 350 years ago, British physician Thomas Willis wrote that diabetes seemed often to occur in patients who were experiencing “significant life stress, sadness, or long sorrow.” That, according to Ellen D. Mandel, DMH, MPA, MS, PA-C, RDN, CDE, a clinical professor at Pace University in New York City, was an important insight into the link between mind and body in patients with diabetes.
“As clinicians, we should be worried about mental illness in our patients with diabetes,” Dr. Mandel, a physician assistant educator, said during a presentation at the Metabolic & Endocrine Disease Summit by Global Academy for Medical Education.
In particular, she said, – and vice versa.
Dr. Mandel pointed to findings suggesting that 11% of patients with diabetes show signs of clinical depression, which is higher than in the general population, with many more believed to have subclinical depression (Diabetes Care. 2015;38[4]:551-60).
Anxiety can be a key factor in trying to understand how diabetes might contribute to depression. “Diabetes is a very stressful condition ... [and patients] may be fatigued and exhausted.” On top of that, they have to make nutrition changes, or at least pay attention to their diet and overall care, all of which can have a cumulatively negative impact on patient well-being.
Conversely, depression can contribute to diabetes. “They kind of go hand in hand,” she said, pointing to depression’s ability to disrupt appetite, diminish energy, and boost levels of cortisol.
Among the findings that provide evidence of a link between diabetes and depression are those from a study in which investigators estimated that for every 1-point increase in depression symptoms, the risk of diabetes will go up by as much as 5% (Clin Diabetes Endocrinol. 2018 Jan 4. doi: 10.1186/s40842-017-0052-1). Moreover, a 2013 review linked the combination of diabetes and depression to an adjusted 1.5-fold increase in risk of all-cause death (PLoS One. 2013 Mar 5. doi: 10.1371/journal.pone.0057058).
Dr. Mandel offered these tips about diagnosing depression in patients with diabetes and helping them feel comfortable:
- Put yourself in the patient’s shoes. “One of the biggest barriers to referring patients to diabetic education is that they don’t want to have to admit to a group that they have diabetes. They keep it to themselves, to their own detriment. In addition, there’s a lot of worry about insurance.” Patients with diabetes often have self-esteem issues and financial or insurance challenges, all of which need to be factored in when working with them, Dr. Mandel said.
- Ask questions and use screening tools. Two simple questions are helpful in starting a conversation and gathering useful information: Over the past 2 weeks, have you often been bothered by [having] little interest or pleasure in doing things? What about being bothered by feeling down, depressed, or hopeless? If the patient answers “yes” to either of these questions, it will be a positive screen, and two “no” answers will be a negative screen. With the “yes” responses, one should follow-up with a screening tool – typically, the one approved by your institution. Dr. Mandel also highlighted the Patient Health Questionnaire depression scale (PHQ-9), which is available online, or the brief, two-item Diabetes Distress Scale (DDS2) questionnaire.
- Keep your own language in mind. “The way you communicate with your patients can elevate their feeling about themselves or destroy how they feel about themselves,” Dr. Mandel said. “We’re trying to stop calling people with diabetes ‘diabetics.’ People don’t want to be labeled like that. Don’t blame yourself if you use this language, but work to make the changes,” Dr. Mandel suggested.
- Watch out for other forms of bias. Beware of unconsciously stereotyping your patients. “It affects how people relate to you, how they adhere to your suggestions, and how much they’ll trust [and confide in] you, which can have clinical implications,” Dr. Mandel said.
Global Academy and this news organization are owned by the same parent company. Dr. Mandel has no disclosures.
EXPERT ANALYSIS FROM MEDS 2019
PCOS incidence is on the rise, but it remains underdiagnosed and undermanaged
SAN DIEGO – The incidence of polycystic ovary syndrome (PCOS) is on the rise, and a nurse practitioner urged her colleagues to give it full attention because of the danger it poses to patients.
“Underdiagnosed and undermanaged, it’s complex and a more serious condition than ever before because of the complications that can occur,” said R. Mimi Secor, DNP, FNP-BC, FAANP, FAAN, who spoke at the Metabolic & Endocrine Disease Summit by Global Academy for Medical Education.
PCOS is the most common reproductive endocrine disorder in the United States, affecting more than 5 million women, or an estimated 6%-10% of the population. Obesity is a risk factor, although lean women account for 10% of cases for reasons that are not understood, according to Dr. Secor, a senior lecturer at Advanced Practice Education Associates in Onset, Mass. In addition, the condition is linked to many sequelae, including multiple sclerosis, diabetes, cardiovascular disease, infertility, mental health problems, and cancer, she said.
Dr. Secor offered these pearls about PCOS:
- Understand the predictive value of oligomenorrhea (infrequent menstrual periods) as a sign of PCOS. “If you’re working in a low-income clinic, you can do well to make a diagnosis without a lot of expensive tests,” she said.
- Urge women with PCOS to get pregnant early if they want to have children. “Infertility is a big problem [among these women],” she said. “They shouldn’t wait until they’re 35 to have babies. They should have them in their 20s.”
- Use insulin control as a tool. “Insulin stimulates ovarian production of testosterone. If we can manage patients around insulin, that can be very helpful.” Losing just 5% of body weight can make a difference in insulin control, Dr. Secor said. “Go for a small change, and help [the patient] maintain that.”
- Monitor patients carefully for cancer. Women who don’t ovulate regularly on a monthly basis face a higher risk of uterine cancer, compared with women who ovulate monthly, she said, and tumors can develop with few symptoms. “If [there is] one drop of bleeding more than a year after menopause,” you need to get a mandatory workup to make sure the patient doesn’t have uterine cancer. Biopsy remains the “gold standard” as a diagnostic tool, she reminded attendees.
- Watch for mental health conditions, especially anxiety, in patients with PCOS. “They seem to be wired for anxiety, and they need a lot of emotional support,” Dr. Secor said.
- Hormonal contraceptives can be safe and effective as a treatment for PCOS in women who don’t wish to become pregnant, she said. But be aware that combination contraceptive drugs can affect women emotionally.
Global Academy and this news organization are owned by the same parent company. Dr. Secor disclosed speaker relationships with Duchesnay and Osphena.
SAN DIEGO – The incidence of polycystic ovary syndrome (PCOS) is on the rise, and a nurse practitioner urged her colleagues to give it full attention because of the danger it poses to patients.
“Underdiagnosed and undermanaged, it’s complex and a more serious condition than ever before because of the complications that can occur,” said R. Mimi Secor, DNP, FNP-BC, FAANP, FAAN, who spoke at the Metabolic & Endocrine Disease Summit by Global Academy for Medical Education.
PCOS is the most common reproductive endocrine disorder in the United States, affecting more than 5 million women, or an estimated 6%-10% of the population. Obesity is a risk factor, although lean women account for 10% of cases for reasons that are not understood, according to Dr. Secor, a senior lecturer at Advanced Practice Education Associates in Onset, Mass. In addition, the condition is linked to many sequelae, including multiple sclerosis, diabetes, cardiovascular disease, infertility, mental health problems, and cancer, she said.
Dr. Secor offered these pearls about PCOS:
- Understand the predictive value of oligomenorrhea (infrequent menstrual periods) as a sign of PCOS. “If you’re working in a low-income clinic, you can do well to make a diagnosis without a lot of expensive tests,” she said.
- Urge women with PCOS to get pregnant early if they want to have children. “Infertility is a big problem [among these women],” she said. “They shouldn’t wait until they’re 35 to have babies. They should have them in their 20s.”
- Use insulin control as a tool. “Insulin stimulates ovarian production of testosterone. If we can manage patients around insulin, that can be very helpful.” Losing just 5% of body weight can make a difference in insulin control, Dr. Secor said. “Go for a small change, and help [the patient] maintain that.”
- Monitor patients carefully for cancer. Women who don’t ovulate regularly on a monthly basis face a higher risk of uterine cancer, compared with women who ovulate monthly, she said, and tumors can develop with few symptoms. “If [there is] one drop of bleeding more than a year after menopause,” you need to get a mandatory workup to make sure the patient doesn’t have uterine cancer. Biopsy remains the “gold standard” as a diagnostic tool, she reminded attendees.
- Watch for mental health conditions, especially anxiety, in patients with PCOS. “They seem to be wired for anxiety, and they need a lot of emotional support,” Dr. Secor said.
- Hormonal contraceptives can be safe and effective as a treatment for PCOS in women who don’t wish to become pregnant, she said. But be aware that combination contraceptive drugs can affect women emotionally.
Global Academy and this news organization are owned by the same parent company. Dr. Secor disclosed speaker relationships with Duchesnay and Osphena.
SAN DIEGO – The incidence of polycystic ovary syndrome (PCOS) is on the rise, and a nurse practitioner urged her colleagues to give it full attention because of the danger it poses to patients.
“Underdiagnosed and undermanaged, it’s complex and a more serious condition than ever before because of the complications that can occur,” said R. Mimi Secor, DNP, FNP-BC, FAANP, FAAN, who spoke at the Metabolic & Endocrine Disease Summit by Global Academy for Medical Education.
PCOS is the most common reproductive endocrine disorder in the United States, affecting more than 5 million women, or an estimated 6%-10% of the population. Obesity is a risk factor, although lean women account for 10% of cases for reasons that are not understood, according to Dr. Secor, a senior lecturer at Advanced Practice Education Associates in Onset, Mass. In addition, the condition is linked to many sequelae, including multiple sclerosis, diabetes, cardiovascular disease, infertility, mental health problems, and cancer, she said.
Dr. Secor offered these pearls about PCOS:
- Understand the predictive value of oligomenorrhea (infrequent menstrual periods) as a sign of PCOS. “If you’re working in a low-income clinic, you can do well to make a diagnosis without a lot of expensive tests,” she said.
- Urge women with PCOS to get pregnant early if they want to have children. “Infertility is a big problem [among these women],” she said. “They shouldn’t wait until they’re 35 to have babies. They should have them in their 20s.”
- Use insulin control as a tool. “Insulin stimulates ovarian production of testosterone. If we can manage patients around insulin, that can be very helpful.” Losing just 5% of body weight can make a difference in insulin control, Dr. Secor said. “Go for a small change, and help [the patient] maintain that.”
- Monitor patients carefully for cancer. Women who don’t ovulate regularly on a monthly basis face a higher risk of uterine cancer, compared with women who ovulate monthly, she said, and tumors can develop with few symptoms. “If [there is] one drop of bleeding more than a year after menopause,” you need to get a mandatory workup to make sure the patient doesn’t have uterine cancer. Biopsy remains the “gold standard” as a diagnostic tool, she reminded attendees.
- Watch for mental health conditions, especially anxiety, in patients with PCOS. “They seem to be wired for anxiety, and they need a lot of emotional support,” Dr. Secor said.
- Hormonal contraceptives can be safe and effective as a treatment for PCOS in women who don’t wish to become pregnant, she said. But be aware that combination contraceptive drugs can affect women emotionally.
Global Academy and this news organization are owned by the same parent company. Dr. Secor disclosed speaker relationships with Duchesnay and Osphena.
REPORTING FROM MEDS 2019
Perils of ‘type’-casting: When adult-onset diabetes isn’t what you think it is
SAN DIEGO – We all know about type 1 and type 2 diabetes. But when an adult patient comes in with symptoms suggestive of diabetes, it is never a good idea to assume it’s either one or the other. In fact, said physician assistant Ji Hyun “CJ” Chun, PA-C, MPAS, BC-ADM, there are plenty of other possibilities from cancer, to monogenetic diabetes, to a condition informally known as type 1.5.
“In most cases, it will be type 1 or type 2, but don’t default everything,” Mr. Chun said at the Metabolic & Endocrine Disease Summit by Global Academy for Medical Education.
He offered the following advice on the diagnosis of adult-onset diabetes:
- Don’t forget the 5% ... and the other 5%. In adults, an estimated 90% of cases of diabetes are type 2, but 5% are type 1 and another 5% are secondary to other conditions, said Mr. Chun, who is based at OptumCare Medical Group, Laguna Niguel, Calif., and has served as president of the American Society of Endocrine PAs. In the past, age seemed to be an important tool for diagnosis, because younger patients typically had type 1 diabetes and older patients typically had type 2, he said. But age alone is no longer useful for diagnosis. Cases of type 2 diabetes are much more common in children these days because of the prevalence of obesity in that population, and an estimated 60% of cases of type 1 disease are diagnosed after the age of 20. In fact, patients may develop type 1 into their 30s, 40s, or 50s, he said, depending on the severity of their autoimmunity.
- Keep ‘type 1.5’ in mind. Latent autoimmune diabetes in adults (LADA), also known as type 1.5, is a slowly developing subtype of type 1 diabetes, Mr. Chun said. There is reason to suspect LADA in lean patients, those younger than 50, and those with personal or family histories of autoimmunity, Mr. Chun said.
- Consider monogenetic diabetes. Many conditions can cause secondary diabetes, among them, monogenetic diabetes, which is caused by a single genetic mutation, whereas type 1 and type 2 diabetes are caused by multiple mutations. Monogenetic diabetes causes an estimated 1%-2% of diabetes cases, said Mr. Chun. Research findings have suggested that it is most likely to be misdiagnosed in younger adults, and that patients may go many years without receiving a correct diagnosis. Maturity-onset diabetes of the young (MODY) is a kind of monogenetic diabetes and typically occurs before the age of 25. There are many subtypes, of which one – MODY 2 – requires no treatment at all. In those patients, said Mr. Chun, “you do nothing. You leave them alone.” It is important to keep in mind that the genetic testing for MODY is expensive, Mr Chun cautioned. Some labs charge between $5,000 and $7,000 for panels, so “look for labs that perform cheaper tests,” he advised, adding that he has found a lab that charges just $250.
- Watch out for cancer. There is a long list of other possible causes of secondary diabetes, including Cushing’s syndrome, hyperthyroidism, hemochromatosis (iron overload), and pancreatic cancer. Mr. Chun said he has lost three patients to pancreatic cancer, while two other patients did well. “Keep in mind that these cases aren’t that common, but they’re there.” He suggested that pancreatic cancer should be considered in patients with rapid onset or worsening of diabetes without known cause, abnormal weight loss, abnormal liver/biliary studies, and jaundice.
Global Academy and this news organization are owned by the same parent company. Mr. Chun disclosed that he is on the AstraZeneca speakers bureau and the Sanofi advisory board.
SAN DIEGO – We all know about type 1 and type 2 diabetes. But when an adult patient comes in with symptoms suggestive of diabetes, it is never a good idea to assume it’s either one or the other. In fact, said physician assistant Ji Hyun “CJ” Chun, PA-C, MPAS, BC-ADM, there are plenty of other possibilities from cancer, to monogenetic diabetes, to a condition informally known as type 1.5.
“In most cases, it will be type 1 or type 2, but don’t default everything,” Mr. Chun said at the Metabolic & Endocrine Disease Summit by Global Academy for Medical Education.
He offered the following advice on the diagnosis of adult-onset diabetes:
- Don’t forget the 5% ... and the other 5%. In adults, an estimated 90% of cases of diabetes are type 2, but 5% are type 1 and another 5% are secondary to other conditions, said Mr. Chun, who is based at OptumCare Medical Group, Laguna Niguel, Calif., and has served as president of the American Society of Endocrine PAs. In the past, age seemed to be an important tool for diagnosis, because younger patients typically had type 1 diabetes and older patients typically had type 2, he said. But age alone is no longer useful for diagnosis. Cases of type 2 diabetes are much more common in children these days because of the prevalence of obesity in that population, and an estimated 60% of cases of type 1 disease are diagnosed after the age of 20. In fact, patients may develop type 1 into their 30s, 40s, or 50s, he said, depending on the severity of their autoimmunity.
- Keep ‘type 1.5’ in mind. Latent autoimmune diabetes in adults (LADA), also known as type 1.5, is a slowly developing subtype of type 1 diabetes, Mr. Chun said. There is reason to suspect LADA in lean patients, those younger than 50, and those with personal or family histories of autoimmunity, Mr. Chun said.
- Consider monogenetic diabetes. Many conditions can cause secondary diabetes, among them, monogenetic diabetes, which is caused by a single genetic mutation, whereas type 1 and type 2 diabetes are caused by multiple mutations. Monogenetic diabetes causes an estimated 1%-2% of diabetes cases, said Mr. Chun. Research findings have suggested that it is most likely to be misdiagnosed in younger adults, and that patients may go many years without receiving a correct diagnosis. Maturity-onset diabetes of the young (MODY) is a kind of monogenetic diabetes and typically occurs before the age of 25. There are many subtypes, of which one – MODY 2 – requires no treatment at all. In those patients, said Mr. Chun, “you do nothing. You leave them alone.” It is important to keep in mind that the genetic testing for MODY is expensive, Mr Chun cautioned. Some labs charge between $5,000 and $7,000 for panels, so “look for labs that perform cheaper tests,” he advised, adding that he has found a lab that charges just $250.
- Watch out for cancer. There is a long list of other possible causes of secondary diabetes, including Cushing’s syndrome, hyperthyroidism, hemochromatosis (iron overload), and pancreatic cancer. Mr. Chun said he has lost three patients to pancreatic cancer, while two other patients did well. “Keep in mind that these cases aren’t that common, but they’re there.” He suggested that pancreatic cancer should be considered in patients with rapid onset or worsening of diabetes without known cause, abnormal weight loss, abnormal liver/biliary studies, and jaundice.
Global Academy and this news organization are owned by the same parent company. Mr. Chun disclosed that he is on the AstraZeneca speakers bureau and the Sanofi advisory board.
SAN DIEGO – We all know about type 1 and type 2 diabetes. But when an adult patient comes in with symptoms suggestive of diabetes, it is never a good idea to assume it’s either one or the other. In fact, said physician assistant Ji Hyun “CJ” Chun, PA-C, MPAS, BC-ADM, there are plenty of other possibilities from cancer, to monogenetic diabetes, to a condition informally known as type 1.5.
“In most cases, it will be type 1 or type 2, but don’t default everything,” Mr. Chun said at the Metabolic & Endocrine Disease Summit by Global Academy for Medical Education.
He offered the following advice on the diagnosis of adult-onset diabetes:
- Don’t forget the 5% ... and the other 5%. In adults, an estimated 90% of cases of diabetes are type 2, but 5% are type 1 and another 5% are secondary to other conditions, said Mr. Chun, who is based at OptumCare Medical Group, Laguna Niguel, Calif., and has served as president of the American Society of Endocrine PAs. In the past, age seemed to be an important tool for diagnosis, because younger patients typically had type 1 diabetes and older patients typically had type 2, he said. But age alone is no longer useful for diagnosis. Cases of type 2 diabetes are much more common in children these days because of the prevalence of obesity in that population, and an estimated 60% of cases of type 1 disease are diagnosed after the age of 20. In fact, patients may develop type 1 into their 30s, 40s, or 50s, he said, depending on the severity of their autoimmunity.
- Keep ‘type 1.5’ in mind. Latent autoimmune diabetes in adults (LADA), also known as type 1.5, is a slowly developing subtype of type 1 diabetes, Mr. Chun said. There is reason to suspect LADA in lean patients, those younger than 50, and those with personal or family histories of autoimmunity, Mr. Chun said.
- Consider monogenetic diabetes. Many conditions can cause secondary diabetes, among them, monogenetic diabetes, which is caused by a single genetic mutation, whereas type 1 and type 2 diabetes are caused by multiple mutations. Monogenetic diabetes causes an estimated 1%-2% of diabetes cases, said Mr. Chun. Research findings have suggested that it is most likely to be misdiagnosed in younger adults, and that patients may go many years without receiving a correct diagnosis. Maturity-onset diabetes of the young (MODY) is a kind of monogenetic diabetes and typically occurs before the age of 25. There are many subtypes, of which one – MODY 2 – requires no treatment at all. In those patients, said Mr. Chun, “you do nothing. You leave them alone.” It is important to keep in mind that the genetic testing for MODY is expensive, Mr Chun cautioned. Some labs charge between $5,000 and $7,000 for panels, so “look for labs that perform cheaper tests,” he advised, adding that he has found a lab that charges just $250.
- Watch out for cancer. There is a long list of other possible causes of secondary diabetes, including Cushing’s syndrome, hyperthyroidism, hemochromatosis (iron overload), and pancreatic cancer. Mr. Chun said he has lost three patients to pancreatic cancer, while two other patients did well. “Keep in mind that these cases aren’t that common, but they’re there.” He suggested that pancreatic cancer should be considered in patients with rapid onset or worsening of diabetes without known cause, abnormal weight loss, abnormal liver/biliary studies, and jaundice.
Global Academy and this news organization are owned by the same parent company. Mr. Chun disclosed that he is on the AstraZeneca speakers bureau and the Sanofi advisory board.
REPORTING FROM MEDS 2019
Go easy on the testosterone when treating hypogonadism
SAN DIEGO – A physician assistant urged colleagues to cast a skeptical eye on male patients who try to jump on board the testosterone therapy train.
“I see many patients getting onto testosterone without having had an adequate evaluation. And I see many patients who might not need testosterone replacement,” Ji Hyun “CJ” Chun, PA-C, MPAS, BC-ADM, said at the Metabolic & Endocrine Disease Summit by Global Academy for Medical Education.
Mr. Chun, who is based at OptumCare Medical Group, Laguna Niguel, Calif., and has served as president of the American Society of Endocrine PAs, offered this advice on evaluating male patients for testosterone therapy:
- Pinpoint the type of hypogonadism. After hypogonadism has been confirmed with lab tests, additional testing should be done to distinguish primary from secondary hypogonadism. Primary hypogonadism refers to the failure of the testes to properly produce testosterone and sperm and is indicated by elevated levels of LH and FSH. Secondary hypogonadism is caused by failures of the hypothalamus, the pituitary, or both, to stimulate the testes to produce testosterone and sperm. It is indicated by low or low-normal levels of LH and FSH.
- Determine the cause of hypogonadism. Cases of hypogonadism are either organic or functional. Diagnostic guidelines provided by the Endocrine Society are helpful in determining the proper category, Mr. Chun said (J Clin Endocrinol Metab. 2018;103[5]:1715-44). Functional hypogonadism is caused by some medications; opioids; abuse of steroids, alcohol, or marijuana; and obesity, which also greatly increases the risk of secondary hypogonadism. These factors – and functional hypogonadism itself – can conceivably be stopped and/or reversed. This form of hypogonadism tends to be mild, compared with organic or “classic” hypogonadism, which is permanent and caused by factors such as advanced age, some types of chemotherapy, and testicle removal. “Organic male hypogonadism mimics female menopause,” Mr. Chun said, in areas such as rate of hormonal decline, which is typically rapid, and hormone deficiency, which is profound. When it comes to treatment, “the benefits far outweigh the risks in organic hypogonadism. But if [a patient has] late-onset [functional] hypogonadism, it gets more complicated.”
- Late-onset hypogonadism treatment. What should be done for patients who have late-onset, organic hypogonadism? According to Mr. Chun, the data regarding testosterone therapy in this population are mixed. The Food and Drug Administration has approved testosterone therapy only for men with organic hypogonadism, he said, noting that “none of the FDA-approved testosterone products are approved for use in men with low testosterone levels who lack an associated medical condition.” However, the Endocrine Society guidelines are less restrictive. In its 2018 guidelines, the society frowned on testosterone therapy for men younger than 65 years with age-related hypogonadism. As for older men, it said that for those “who have symptoms or conditions suggestive of testosterone deficiency (such as low libido or unexplained anemia) and consistently and unequivocally low morning testosterone concentrations, we suggest that clinicians offer testosterone therapy on an individualized basis after explicit discussion of the potential risks and benefits.”
- Don’t push for high testosterone levels. When treating patients, “you want to restore the testosterone to an adequate level,” Mr. Chun said. “What’s an adequate level? We don’t know.” He urged colleagues to not overdo it and to consider aiming for a testosterone level ranging between 350 ng/dL and 700 ng/dL. “I get [the levels] to the lowest level at which the patient is symptomatically fine.”
Global Academy and this news organization are owned by the same parent company. Mr. Chun disclosed that he is on the AstraZeneca speakers bureau and the Sanofi advisory board.
SAN DIEGO – A physician assistant urged colleagues to cast a skeptical eye on male patients who try to jump on board the testosterone therapy train.
“I see many patients getting onto testosterone without having had an adequate evaluation. And I see many patients who might not need testosterone replacement,” Ji Hyun “CJ” Chun, PA-C, MPAS, BC-ADM, said at the Metabolic & Endocrine Disease Summit by Global Academy for Medical Education.
Mr. Chun, who is based at OptumCare Medical Group, Laguna Niguel, Calif., and has served as president of the American Society of Endocrine PAs, offered this advice on evaluating male patients for testosterone therapy:
- Pinpoint the type of hypogonadism. After hypogonadism has been confirmed with lab tests, additional testing should be done to distinguish primary from secondary hypogonadism. Primary hypogonadism refers to the failure of the testes to properly produce testosterone and sperm and is indicated by elevated levels of LH and FSH. Secondary hypogonadism is caused by failures of the hypothalamus, the pituitary, or both, to stimulate the testes to produce testosterone and sperm. It is indicated by low or low-normal levels of LH and FSH.
- Determine the cause of hypogonadism. Cases of hypogonadism are either organic or functional. Diagnostic guidelines provided by the Endocrine Society are helpful in determining the proper category, Mr. Chun said (J Clin Endocrinol Metab. 2018;103[5]:1715-44). Functional hypogonadism is caused by some medications; opioids; abuse of steroids, alcohol, or marijuana; and obesity, which also greatly increases the risk of secondary hypogonadism. These factors – and functional hypogonadism itself – can conceivably be stopped and/or reversed. This form of hypogonadism tends to be mild, compared with organic or “classic” hypogonadism, which is permanent and caused by factors such as advanced age, some types of chemotherapy, and testicle removal. “Organic male hypogonadism mimics female menopause,” Mr. Chun said, in areas such as rate of hormonal decline, which is typically rapid, and hormone deficiency, which is profound. When it comes to treatment, “the benefits far outweigh the risks in organic hypogonadism. But if [a patient has] late-onset [functional] hypogonadism, it gets more complicated.”
- Late-onset hypogonadism treatment. What should be done for patients who have late-onset, organic hypogonadism? According to Mr. Chun, the data regarding testosterone therapy in this population are mixed. The Food and Drug Administration has approved testosterone therapy only for men with organic hypogonadism, he said, noting that “none of the FDA-approved testosterone products are approved for use in men with low testosterone levels who lack an associated medical condition.” However, the Endocrine Society guidelines are less restrictive. In its 2018 guidelines, the society frowned on testosterone therapy for men younger than 65 years with age-related hypogonadism. As for older men, it said that for those “who have symptoms or conditions suggestive of testosterone deficiency (such as low libido or unexplained anemia) and consistently and unequivocally low morning testosterone concentrations, we suggest that clinicians offer testosterone therapy on an individualized basis after explicit discussion of the potential risks and benefits.”
- Don’t push for high testosterone levels. When treating patients, “you want to restore the testosterone to an adequate level,” Mr. Chun said. “What’s an adequate level? We don’t know.” He urged colleagues to not overdo it and to consider aiming for a testosterone level ranging between 350 ng/dL and 700 ng/dL. “I get [the levels] to the lowest level at which the patient is symptomatically fine.”
Global Academy and this news organization are owned by the same parent company. Mr. Chun disclosed that he is on the AstraZeneca speakers bureau and the Sanofi advisory board.
SAN DIEGO – A physician assistant urged colleagues to cast a skeptical eye on male patients who try to jump on board the testosterone therapy train.
“I see many patients getting onto testosterone without having had an adequate evaluation. And I see many patients who might not need testosterone replacement,” Ji Hyun “CJ” Chun, PA-C, MPAS, BC-ADM, said at the Metabolic & Endocrine Disease Summit by Global Academy for Medical Education.
Mr. Chun, who is based at OptumCare Medical Group, Laguna Niguel, Calif., and has served as president of the American Society of Endocrine PAs, offered this advice on evaluating male patients for testosterone therapy:
- Pinpoint the type of hypogonadism. After hypogonadism has been confirmed with lab tests, additional testing should be done to distinguish primary from secondary hypogonadism. Primary hypogonadism refers to the failure of the testes to properly produce testosterone and sperm and is indicated by elevated levels of LH and FSH. Secondary hypogonadism is caused by failures of the hypothalamus, the pituitary, or both, to stimulate the testes to produce testosterone and sperm. It is indicated by low or low-normal levels of LH and FSH.
- Determine the cause of hypogonadism. Cases of hypogonadism are either organic or functional. Diagnostic guidelines provided by the Endocrine Society are helpful in determining the proper category, Mr. Chun said (J Clin Endocrinol Metab. 2018;103[5]:1715-44). Functional hypogonadism is caused by some medications; opioids; abuse of steroids, alcohol, or marijuana; and obesity, which also greatly increases the risk of secondary hypogonadism. These factors – and functional hypogonadism itself – can conceivably be stopped and/or reversed. This form of hypogonadism tends to be mild, compared with organic or “classic” hypogonadism, which is permanent and caused by factors such as advanced age, some types of chemotherapy, and testicle removal. “Organic male hypogonadism mimics female menopause,” Mr. Chun said, in areas such as rate of hormonal decline, which is typically rapid, and hormone deficiency, which is profound. When it comes to treatment, “the benefits far outweigh the risks in organic hypogonadism. But if [a patient has] late-onset [functional] hypogonadism, it gets more complicated.”
- Late-onset hypogonadism treatment. What should be done for patients who have late-onset, organic hypogonadism? According to Mr. Chun, the data regarding testosterone therapy in this population are mixed. The Food and Drug Administration has approved testosterone therapy only for men with organic hypogonadism, he said, noting that “none of the FDA-approved testosterone products are approved for use in men with low testosterone levels who lack an associated medical condition.” However, the Endocrine Society guidelines are less restrictive. In its 2018 guidelines, the society frowned on testosterone therapy for men younger than 65 years with age-related hypogonadism. As for older men, it said that for those “who have symptoms or conditions suggestive of testosterone deficiency (such as low libido or unexplained anemia) and consistently and unequivocally low morning testosterone concentrations, we suggest that clinicians offer testosterone therapy on an individualized basis after explicit discussion of the potential risks and benefits.”
- Don’t push for high testosterone levels. When treating patients, “you want to restore the testosterone to an adequate level,” Mr. Chun said. “What’s an adequate level? We don’t know.” He urged colleagues to not overdo it and to consider aiming for a testosterone level ranging between 350 ng/dL and 700 ng/dL. “I get [the levels] to the lowest level at which the patient is symptomatically fine.”
Global Academy and this news organization are owned by the same parent company. Mr. Chun disclosed that he is on the AstraZeneca speakers bureau and the Sanofi advisory board.
REPORTING FROM MEDS 2019