User login
Sharon Worcester is an award-winning medical journalist for MDedge News. She has been with the company since 1996, first as the Southeast Bureau Chief (1996-2009) when the company was known as International Medical News Group, then as a freelance writer (2010-2015) before returning as a reporter in 2015. She previously worked as a daily newspaper reporter covering health and local government. Sharon currently reports primarily on oncology and hematology. She has a BA from Eckerd College and an MA in Mass Communication/Print Journalism from the University of Florida. Connect with her via LinkedIn and follow her on twitter @SW_MedReporter.
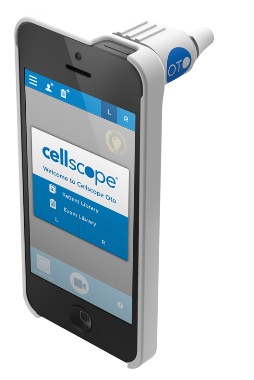
Smartphone technology could enable remote otitis media diagnosis
ORLANDO – A novel smartphone otoscope attachment provides clear, transmittable images of the ear drum or tympanic membrane, and could revolutionize the approach to diagnosing and managing ear infections, according to Dr. Kathryn Rappaport.
In a prospective study involving 63 children who presented to an emergency department between May and December 2012 with upper respiratory tract symptoms, the technology was as effective as a conventional otoscope, and was widely accepted by parents, Dr. Rappaport of Baylor College of Medicine, Houston, reported at the annual meeting of the American Academy of Pediatrics.
After receiving clinical care, each child in the study underwent bilateral otic videoscopy using both the smartphone otoscope (CellScope Oto) and a camera-fitted conventional otoscope. The procedures were performed in random order, said Dr. Rappaport, who was at Emory University in Atlanta when the study was conducted.
Of the children, who had a mean age of 2.9 years, 49 received a clinical diagnosis of acute otitis media by an ED practitioner. Based on independent scoring by four physicians who evaluated 31 CellScope Oto videos and 31 conventional otoscope videos from 26 subjects, there was no difference between the two technologies in either the diagnostic quality of the images or diagnosis confidence ratings.
Diagnosis and treatment decision making were similar with each device. Overall, the physician raters were in fair agreement regarding the clinical ED diagnosis of acute otitis media, while two of the raters had moderate to substantial agreement with the ED diagnosis and two had poor agreement with the ED diagnosis from images obtained via conventional otoscope, Dr. Rappaport said, noting that there was a significant correlation between antimicrobial use and image quality.
This indicated that higher-quality images were more likely to be associated with a definitive diagnosis, she said.
As for parent reactions to the use of the device, most (95%) responded favorably, stating that the CellScope Oto images improved their understanding of their child’s management. Also, 90% said they thought the technology would be easy to use, and they would feel comfortable using it remotely to transmit images to a provider.
The CellScope Oto has the potential to improve diagnosis and management, and to reduce costs associated with acute otitis media in children, Dr. Rappaport said.
The video images can provide a baseline, as well as ongoing documentation of a child’s condition. The video documentation could allow a child to be followed over a period of time – without the need for regular office visits – to help monitor for progression or resolution of middle ear effusion and to guide diagnosis and treatment decision making, she explained.
"Acute otitis media is the most common reason for antimicrobial prescriptions in children. In the future, we would like to study whether the ability to monitor for resolution of a patient’s middle ear effusion using digital imaging with the smartphone otoscope will lead to decreased antimicrobial prescriptions for acute otitis media in children," she said in an interview.
Dr. Rappaport reported having no relevant financial disclosures.
ORLANDO – A novel smartphone otoscope attachment provides clear, transmittable images of the ear drum or tympanic membrane, and could revolutionize the approach to diagnosing and managing ear infections, according to Dr. Kathryn Rappaport.
In a prospective study involving 63 children who presented to an emergency department between May and December 2012 with upper respiratory tract symptoms, the technology was as effective as a conventional otoscope, and was widely accepted by parents, Dr. Rappaport of Baylor College of Medicine, Houston, reported at the annual meeting of the American Academy of Pediatrics.
After receiving clinical care, each child in the study underwent bilateral otic videoscopy using both the smartphone otoscope (CellScope Oto) and a camera-fitted conventional otoscope. The procedures were performed in random order, said Dr. Rappaport, who was at Emory University in Atlanta when the study was conducted.
Of the children, who had a mean age of 2.9 years, 49 received a clinical diagnosis of acute otitis media by an ED practitioner. Based on independent scoring by four physicians who evaluated 31 CellScope Oto videos and 31 conventional otoscope videos from 26 subjects, there was no difference between the two technologies in either the diagnostic quality of the images or diagnosis confidence ratings.
Diagnosis and treatment decision making were similar with each device. Overall, the physician raters were in fair agreement regarding the clinical ED diagnosis of acute otitis media, while two of the raters had moderate to substantial agreement with the ED diagnosis and two had poor agreement with the ED diagnosis from images obtained via conventional otoscope, Dr. Rappaport said, noting that there was a significant correlation between antimicrobial use and image quality.
This indicated that higher-quality images were more likely to be associated with a definitive diagnosis, she said.
As for parent reactions to the use of the device, most (95%) responded favorably, stating that the CellScope Oto images improved their understanding of their child’s management. Also, 90% said they thought the technology would be easy to use, and they would feel comfortable using it remotely to transmit images to a provider.
The CellScope Oto has the potential to improve diagnosis and management, and to reduce costs associated with acute otitis media in children, Dr. Rappaport said.
The video images can provide a baseline, as well as ongoing documentation of a child’s condition. The video documentation could allow a child to be followed over a period of time – without the need for regular office visits – to help monitor for progression or resolution of middle ear effusion and to guide diagnosis and treatment decision making, she explained.
"Acute otitis media is the most common reason for antimicrobial prescriptions in children. In the future, we would like to study whether the ability to monitor for resolution of a patient’s middle ear effusion using digital imaging with the smartphone otoscope will lead to decreased antimicrobial prescriptions for acute otitis media in children," she said in an interview.
Dr. Rappaport reported having no relevant financial disclosures.
ORLANDO – A novel smartphone otoscope attachment provides clear, transmittable images of the ear drum or tympanic membrane, and could revolutionize the approach to diagnosing and managing ear infections, according to Dr. Kathryn Rappaport.
In a prospective study involving 63 children who presented to an emergency department between May and December 2012 with upper respiratory tract symptoms, the technology was as effective as a conventional otoscope, and was widely accepted by parents, Dr. Rappaport of Baylor College of Medicine, Houston, reported at the annual meeting of the American Academy of Pediatrics.
After receiving clinical care, each child in the study underwent bilateral otic videoscopy using both the smartphone otoscope (CellScope Oto) and a camera-fitted conventional otoscope. The procedures were performed in random order, said Dr. Rappaport, who was at Emory University in Atlanta when the study was conducted.
Of the children, who had a mean age of 2.9 years, 49 received a clinical diagnosis of acute otitis media by an ED practitioner. Based on independent scoring by four physicians who evaluated 31 CellScope Oto videos and 31 conventional otoscope videos from 26 subjects, there was no difference between the two technologies in either the diagnostic quality of the images or diagnosis confidence ratings.
Diagnosis and treatment decision making were similar with each device. Overall, the physician raters were in fair agreement regarding the clinical ED diagnosis of acute otitis media, while two of the raters had moderate to substantial agreement with the ED diagnosis and two had poor agreement with the ED diagnosis from images obtained via conventional otoscope, Dr. Rappaport said, noting that there was a significant correlation between antimicrobial use and image quality.
This indicated that higher-quality images were more likely to be associated with a definitive diagnosis, she said.
As for parent reactions to the use of the device, most (95%) responded favorably, stating that the CellScope Oto images improved their understanding of their child’s management. Also, 90% said they thought the technology would be easy to use, and they would feel comfortable using it remotely to transmit images to a provider.
The CellScope Oto has the potential to improve diagnosis and management, and to reduce costs associated with acute otitis media in children, Dr. Rappaport said.
The video images can provide a baseline, as well as ongoing documentation of a child’s condition. The video documentation could allow a child to be followed over a period of time – without the need for regular office visits – to help monitor for progression or resolution of middle ear effusion and to guide diagnosis and treatment decision making, she explained.
"Acute otitis media is the most common reason for antimicrobial prescriptions in children. In the future, we would like to study whether the ability to monitor for resolution of a patient’s middle ear effusion using digital imaging with the smartphone otoscope will lead to decreased antimicrobial prescriptions for acute otitis media in children," she said in an interview.
Dr. Rappaport reported having no relevant financial disclosures.
AT THE AAP NATIONAL CONFERENCE
Major finding: No difference was seen between the smartphone otoscope and a conventional otoscope in either the diagnostic quality of the images or diagnosis confidence ratings.
Data source: A prospective single-site study of 63 children.
Disclosures: Dr. Rappaport reported having no relevant financial disclosures.
Mediterranean diet may lower CKD risk
ATLANTA – Following a Mediterranean-style diet may reduce the risk of chronic kidney disease, findings from the prospective Northern Manhattan Study suggest.
Among 900 subjects from the large community-based, multiethnic cohort who had requisite data available, 14% developed new chronic kidney disease (CKD) during a mean follow-up of 6.9 years. After adjustment for several potential confounders, including demographics, medication use, laboratory values, and medical history, following a Mediterranean-style diet was associated with a 50% reduction in the risk of incident stage 3 CKD, the primary outcome measure of the study (odds ratio, 0.50), Dr. Minesh Khatri of Columbia University, New York, reported at Kidney Week 2013.
Furthermore, each 1-unit increase in a previously developed 9-point score that measured the degree to which a subject followed a Mediterranean-style diet (the MeDi score) was associated with a 17% reduction in CKD risk (OR, 0.83), Dr. Khatri said.
A MeDi score of 5 or higher also was associated with a 42% reduction in the risk of rapid kidney function decline (OR, 0.58), and each 1-point increase in the score was associated with a 12% reduction in risk (OR, 0.88).
Continuous absolute change in estimated glomerular filtration rate (eGFR) was not significantly affected by the MeDi score, but a higher score was associated with a trend toward improvement.
Study participants were adults who were stroke free and had a mean age of 64 years at baseline. They underwent measurement of serum creatinine at baseline and at follow-up, as well as brain magnetic resonance imaging at follow-up. They also completed a dietary questionnaire at baseline, from which the MeDi score was derived.
Most (65%) were Hispanic, and 59% were women. Mean eGFR was 83.1 mL/min, with a mean annualized decline of 1.1 mL/min.
Incident CKD in this study was defined as a follow-up Modification of Diet in Renal Disease eGFR of less than 60 mL/min among subjects with eGFR greater than 60 mL/min at baseline.
"CKD is highly prevalent. The lifetime risk of stage 3 CKD in the United States may be as high as 59% ... [and] the consequences of CKD are of equal magnitude. CKD increases the risk of morbidity and mortality, especially from cardiovascular disease," Dr. Khatri said. Data show that the worse the kidney function, the greater the cardiovascular disease risk and the greater the likelihood of cardiovascular events, he noted.
The financial toll is also extensive, he said during a press briefing at the conference, which was sponsored by the American Society of Nephrology.
"On top of this, the therapeutic armamentarium for CKD is actually relatively limited. We’ve made tremendous strides in treating traditional risk factors such as diabetes, hypertension, and protein in the urine, but most patients with CKD still have progressive kidney function decline over time. This therefore means we need novel approaches to prevent and ameliorate progression of CKD," he said.
Diet may be one such approach. Some diets have been studied in the context of improving CKD, but most studies have focused on protein restriction – an approach that may be harmful in some patients, such as the frail elderly. Few studies have looked at diet in the context of preventing CKD.
The Mediterranean diet – which generally includes high intake of fruits, vegetables, legumes, cereals, fish, and heart-healthy monounsaturated fats; lower intake of dairy, meats, and saturated fats; as well as moderate alcohol intake, has received a great deal of attention with respect to potential cardiovascular benefits. Studies have shown it has important benefits, including improvements in blood pressure, endothelial function, cholesterol, inflammation, and overall cardiovascular risk, Dr. Khatri said.
In fact, results from the randomized controlled PREDIMED study, published in April, demonstrated a 30% reduction in cardiovascular risk among those following a Mediterranean diet, compared with those following a standard low-fat diet (N. Engl. J. Med. 2013;368:1279-90), he noted.
The current study shows that a Mediterranean-style diet may have similarly beneficial effects for reducing CKD risk, which makes sense given the shared risk factors between CKD and cardiovascular disease, he said.
Larger observational trials and randomized controlled trials are needed to confirm these findings and to elucidate the mechanisms by which a Mediterranean-style diet may protect against kidney disease, he said.
This study was funded by the National Institutes of Health. Dr. Khatri reported having no disclosures.
ATLANTA – Following a Mediterranean-style diet may reduce the risk of chronic kidney disease, findings from the prospective Northern Manhattan Study suggest.
Among 900 subjects from the large community-based, multiethnic cohort who had requisite data available, 14% developed new chronic kidney disease (CKD) during a mean follow-up of 6.9 years. After adjustment for several potential confounders, including demographics, medication use, laboratory values, and medical history, following a Mediterranean-style diet was associated with a 50% reduction in the risk of incident stage 3 CKD, the primary outcome measure of the study (odds ratio, 0.50), Dr. Minesh Khatri of Columbia University, New York, reported at Kidney Week 2013.
Furthermore, each 1-unit increase in a previously developed 9-point score that measured the degree to which a subject followed a Mediterranean-style diet (the MeDi score) was associated with a 17% reduction in CKD risk (OR, 0.83), Dr. Khatri said.
A MeDi score of 5 or higher also was associated with a 42% reduction in the risk of rapid kidney function decline (OR, 0.58), and each 1-point increase in the score was associated with a 12% reduction in risk (OR, 0.88).
Continuous absolute change in estimated glomerular filtration rate (eGFR) was not significantly affected by the MeDi score, but a higher score was associated with a trend toward improvement.
Study participants were adults who were stroke free and had a mean age of 64 years at baseline. They underwent measurement of serum creatinine at baseline and at follow-up, as well as brain magnetic resonance imaging at follow-up. They also completed a dietary questionnaire at baseline, from which the MeDi score was derived.
Most (65%) were Hispanic, and 59% were women. Mean eGFR was 83.1 mL/min, with a mean annualized decline of 1.1 mL/min.
Incident CKD in this study was defined as a follow-up Modification of Diet in Renal Disease eGFR of less than 60 mL/min among subjects with eGFR greater than 60 mL/min at baseline.
"CKD is highly prevalent. The lifetime risk of stage 3 CKD in the United States may be as high as 59% ... [and] the consequences of CKD are of equal magnitude. CKD increases the risk of morbidity and mortality, especially from cardiovascular disease," Dr. Khatri said. Data show that the worse the kidney function, the greater the cardiovascular disease risk and the greater the likelihood of cardiovascular events, he noted.
The financial toll is also extensive, he said during a press briefing at the conference, which was sponsored by the American Society of Nephrology.
"On top of this, the therapeutic armamentarium for CKD is actually relatively limited. We’ve made tremendous strides in treating traditional risk factors such as diabetes, hypertension, and protein in the urine, but most patients with CKD still have progressive kidney function decline over time. This therefore means we need novel approaches to prevent and ameliorate progression of CKD," he said.
Diet may be one such approach. Some diets have been studied in the context of improving CKD, but most studies have focused on protein restriction – an approach that may be harmful in some patients, such as the frail elderly. Few studies have looked at diet in the context of preventing CKD.
The Mediterranean diet – which generally includes high intake of fruits, vegetables, legumes, cereals, fish, and heart-healthy monounsaturated fats; lower intake of dairy, meats, and saturated fats; as well as moderate alcohol intake, has received a great deal of attention with respect to potential cardiovascular benefits. Studies have shown it has important benefits, including improvements in blood pressure, endothelial function, cholesterol, inflammation, and overall cardiovascular risk, Dr. Khatri said.
In fact, results from the randomized controlled PREDIMED study, published in April, demonstrated a 30% reduction in cardiovascular risk among those following a Mediterranean diet, compared with those following a standard low-fat diet (N. Engl. J. Med. 2013;368:1279-90), he noted.
The current study shows that a Mediterranean-style diet may have similarly beneficial effects for reducing CKD risk, which makes sense given the shared risk factors between CKD and cardiovascular disease, he said.
Larger observational trials and randomized controlled trials are needed to confirm these findings and to elucidate the mechanisms by which a Mediterranean-style diet may protect against kidney disease, he said.
This study was funded by the National Institutes of Health. Dr. Khatri reported having no disclosures.
ATLANTA – Following a Mediterranean-style diet may reduce the risk of chronic kidney disease, findings from the prospective Northern Manhattan Study suggest.
Among 900 subjects from the large community-based, multiethnic cohort who had requisite data available, 14% developed new chronic kidney disease (CKD) during a mean follow-up of 6.9 years. After adjustment for several potential confounders, including demographics, medication use, laboratory values, and medical history, following a Mediterranean-style diet was associated with a 50% reduction in the risk of incident stage 3 CKD, the primary outcome measure of the study (odds ratio, 0.50), Dr. Minesh Khatri of Columbia University, New York, reported at Kidney Week 2013.
Furthermore, each 1-unit increase in a previously developed 9-point score that measured the degree to which a subject followed a Mediterranean-style diet (the MeDi score) was associated with a 17% reduction in CKD risk (OR, 0.83), Dr. Khatri said.
A MeDi score of 5 or higher also was associated with a 42% reduction in the risk of rapid kidney function decline (OR, 0.58), and each 1-point increase in the score was associated with a 12% reduction in risk (OR, 0.88).
Continuous absolute change in estimated glomerular filtration rate (eGFR) was not significantly affected by the MeDi score, but a higher score was associated with a trend toward improvement.
Study participants were adults who were stroke free and had a mean age of 64 years at baseline. They underwent measurement of serum creatinine at baseline and at follow-up, as well as brain magnetic resonance imaging at follow-up. They also completed a dietary questionnaire at baseline, from which the MeDi score was derived.
Most (65%) were Hispanic, and 59% were women. Mean eGFR was 83.1 mL/min, with a mean annualized decline of 1.1 mL/min.
Incident CKD in this study was defined as a follow-up Modification of Diet in Renal Disease eGFR of less than 60 mL/min among subjects with eGFR greater than 60 mL/min at baseline.
"CKD is highly prevalent. The lifetime risk of stage 3 CKD in the United States may be as high as 59% ... [and] the consequences of CKD are of equal magnitude. CKD increases the risk of morbidity and mortality, especially from cardiovascular disease," Dr. Khatri said. Data show that the worse the kidney function, the greater the cardiovascular disease risk and the greater the likelihood of cardiovascular events, he noted.
The financial toll is also extensive, he said during a press briefing at the conference, which was sponsored by the American Society of Nephrology.
"On top of this, the therapeutic armamentarium for CKD is actually relatively limited. We’ve made tremendous strides in treating traditional risk factors such as diabetes, hypertension, and protein in the urine, but most patients with CKD still have progressive kidney function decline over time. This therefore means we need novel approaches to prevent and ameliorate progression of CKD," he said.
Diet may be one such approach. Some diets have been studied in the context of improving CKD, but most studies have focused on protein restriction – an approach that may be harmful in some patients, such as the frail elderly. Few studies have looked at diet in the context of preventing CKD.
The Mediterranean diet – which generally includes high intake of fruits, vegetables, legumes, cereals, fish, and heart-healthy monounsaturated fats; lower intake of dairy, meats, and saturated fats; as well as moderate alcohol intake, has received a great deal of attention with respect to potential cardiovascular benefits. Studies have shown it has important benefits, including improvements in blood pressure, endothelial function, cholesterol, inflammation, and overall cardiovascular risk, Dr. Khatri said.
In fact, results from the randomized controlled PREDIMED study, published in April, demonstrated a 30% reduction in cardiovascular risk among those following a Mediterranean diet, compared with those following a standard low-fat diet (N. Engl. J. Med. 2013;368:1279-90), he noted.
The current study shows that a Mediterranean-style diet may have similarly beneficial effects for reducing CKD risk, which makes sense given the shared risk factors between CKD and cardiovascular disease, he said.
Larger observational trials and randomized controlled trials are needed to confirm these findings and to elucidate the mechanisms by which a Mediterranean-style diet may protect against kidney disease, he said.
This study was funded by the National Institutes of Health. Dr. Khatri reported having no disclosures.
AT KIDNEY WEEK 2013
Major finding: A Mediterranean-style diet was associated with a 50% reduction in incident CKD.
Data source: A prospective cohort study involving 900 subjects.
Disclosures: This study was funded by the National Institutes of Health. Dr. Khatri reported having no disclosures.
Women’s health groups propose new term for ‘vulvovaginal atrophy’
To varying degrees, vulvovaginal atrophy affects an estimated 20%-40% of menopausal women, but the name of the condition fails to appropriately characterize the range of associated signs and symptoms that women may experience.
Representatives from the North American Menopause Society (NAMS) and the International Society for the Study of Women’s Sexual Health, Inc. (ISSWSH) propose a new term: genitourinary syndrome of menopause, or GSM.
Earlier this year, the two organizations convened a 2-day consensus conference to consider what an appropriate term would encompass. The goal of that conference, according to Dr. Margery Gass of the Cleveland Clinic Center for Specialized Women’s Health and the executive director of NAMS, was to identify a term that was descriptive, comprehensive, and suitable for professionals, consumers, and the media.
Participants reviewed the symptoms and signs of genitourinary aging and the available relevant data, and decided on a number of components that should be covered by the new nomenclature, including the affected anatomy, descriptive factors, problems caused by the condition, and context with respect to life phase, she said in an interview.
Dr. Gass and Dr. David J. Portman, director of the Columbus Center for Women’s Health Research and an adjunct instructor at Ohio State University, Columbus, cochaired the consensus conference. They presented the conclusions from the conference at the annual meeting of the North American Menopause Society in October.
"Several concerns have forced the issue of a name change for this condition," Dr. Gass said, noting that persistent societal resistance to openly discussing women’s sexuality and sexual health is not the least among them.
The word "vagina," for example, still can’t be uttered in many media outlets, she explained. Additionally, the term "atrophy" has unpleasant connotations that aren’t necessarily reflective of the experience of women affected by the condition, she noted.
"In fact, atrophy in and of itself is a natural part of aging – something many women experience – and is not necessarily a problem; some women with atrophy experience no symptoms, while others experience significant symptoms.
"We feel that the name we’re putting forward (genitourinary syndrome of menopause) very accurately describes the parts of the body that are involved – namely the genital system and the lower urinary tract," she said.
The use of the word "syndrome" further allows for a diagnosis based on the range of symptoms women may experience, and doesn’t limit the condition to specific symptoms.
"This is not a disease or a deficiency, so we think ‘genitourinary syndrome of menopause’ is a neutral term that would be acceptable, Dr. Gass said.
A change in the nomenclature could potentially open the door to more productive, health-promoting dialogue. During his presentation at the NAMS meeting, Dr. Portman explained how a term that is more acceptable to patients and the media could have the power to start the conversation, change attitudes, and promote understanding and acceptance of more open communication. He used male sexual dysfunction as an example.
In 1992, a National Institutes of Health consensus development panel determined that the term "erectile dysfunction" was preferable to the term "impotence." Indeed, along with the subsequent approval of Viagra and other drugs related to male sexual health, the term "erectile dysfunction" is now widely used in advertising, promoted by politicians and celebrities, and openly discussed in the community, he said.
In contrast, open discussion about women’s sexuality and sexual health remains constrained. In fact, in a survey of more than 1,000 women – including 330 women aged 60-65 years – 75% "completely agreed" that society constrains the sexual expression of "women my age more so than men my age." Nearly as many completely agreed that society is more accepting of discussion around men’s physical sexual problems than women’s physical sexual problems. More than half completely agreed that "society would prefer to believe that women my age do not have sex."
The use of more "socially acceptable" terminology (the word "penis," like "vagina," is still not used openly, Dr. Gass noted) helped make male sexual health a mainstream topic; it is hoped that transitioning from "vulvovaginal atrophy" to "genitourinary syndrome of menopause," would have a similar effect with respect to women’s sexual health, Dr. Portman said.
GSM would be defined as "a collection of symptoms and signs associated with decreased estrogen levels that can involve the labia majora/minora, vestibule/introitus, clitoris, vagina, urethra, and bladder," conference attendees agreed.
It is a syndrome for which treatment is indicated if symptoms are bothersome; treatment should be individualized based on the severity of symptoms and the woman’s preference after discussion of treatment options and risks and benefits.
In addition to working toward agreement on appropriate nomenclature, the consensus conference participants are developing an assessment tool, currently in draft form, to aid clinicians in evaluating women for the syndrome.
"We feel we’ve identified a number of signs and findings that would help clinicians – particularly those who don’t treat a lot of patients with this condition. The tool – which involves a grid-based design outlining mild, moderate, and severe symptom categories – may prove valuable for providers who want to chart severity or just scan the grid to assist in making a diagnosis," Dr. Gass said. The tool also could prove useful in the research setting, he added.
ISSWSH and NAMS will be publishing the proceedings of the workshop in upcoming issues of their respective journals – the Journal of Sexual Medicine and the journal Menopause.
The groups also plan to put forward the proposed new name at a December meeting of the American College of Obstetricians and Gynecologists. At that meeting, ACOG will review all terminology related to obstetrics and gynecology and update terminology as appropriate.
"We hope to address the ACOG urogynecology and menopause working group to see if the new name is acceptable to that group as well. Personally I think it’s important to have an accurate term that is as neutral as possible," Dr. Gass said.
Dr. Gass reported having no disclosures. Dr. Portman has been a speaker, consultant, or advisory board member for, and/or received grant or research support from Bayer, Noven Pharmaceuticals, Palatin Technologies, and other companies.
To varying degrees, vulvovaginal atrophy affects an estimated 20%-40% of menopausal women, but the name of the condition fails to appropriately characterize the range of associated signs and symptoms that women may experience.
Representatives from the North American Menopause Society (NAMS) and the International Society for the Study of Women’s Sexual Health, Inc. (ISSWSH) propose a new term: genitourinary syndrome of menopause, or GSM.
Earlier this year, the two organizations convened a 2-day consensus conference to consider what an appropriate term would encompass. The goal of that conference, according to Dr. Margery Gass of the Cleveland Clinic Center for Specialized Women’s Health and the executive director of NAMS, was to identify a term that was descriptive, comprehensive, and suitable for professionals, consumers, and the media.
Participants reviewed the symptoms and signs of genitourinary aging and the available relevant data, and decided on a number of components that should be covered by the new nomenclature, including the affected anatomy, descriptive factors, problems caused by the condition, and context with respect to life phase, she said in an interview.
Dr. Gass and Dr. David J. Portman, director of the Columbus Center for Women’s Health Research and an adjunct instructor at Ohio State University, Columbus, cochaired the consensus conference. They presented the conclusions from the conference at the annual meeting of the North American Menopause Society in October.
"Several concerns have forced the issue of a name change for this condition," Dr. Gass said, noting that persistent societal resistance to openly discussing women’s sexuality and sexual health is not the least among them.
The word "vagina," for example, still can’t be uttered in many media outlets, she explained. Additionally, the term "atrophy" has unpleasant connotations that aren’t necessarily reflective of the experience of women affected by the condition, she noted.
"In fact, atrophy in and of itself is a natural part of aging – something many women experience – and is not necessarily a problem; some women with atrophy experience no symptoms, while others experience significant symptoms.
"We feel that the name we’re putting forward (genitourinary syndrome of menopause) very accurately describes the parts of the body that are involved – namely the genital system and the lower urinary tract," she said.
The use of the word "syndrome" further allows for a diagnosis based on the range of symptoms women may experience, and doesn’t limit the condition to specific symptoms.
"This is not a disease or a deficiency, so we think ‘genitourinary syndrome of menopause’ is a neutral term that would be acceptable, Dr. Gass said.
A change in the nomenclature could potentially open the door to more productive, health-promoting dialogue. During his presentation at the NAMS meeting, Dr. Portman explained how a term that is more acceptable to patients and the media could have the power to start the conversation, change attitudes, and promote understanding and acceptance of more open communication. He used male sexual dysfunction as an example.
In 1992, a National Institutes of Health consensus development panel determined that the term "erectile dysfunction" was preferable to the term "impotence." Indeed, along with the subsequent approval of Viagra and other drugs related to male sexual health, the term "erectile dysfunction" is now widely used in advertising, promoted by politicians and celebrities, and openly discussed in the community, he said.
In contrast, open discussion about women’s sexuality and sexual health remains constrained. In fact, in a survey of more than 1,000 women – including 330 women aged 60-65 years – 75% "completely agreed" that society constrains the sexual expression of "women my age more so than men my age." Nearly as many completely agreed that society is more accepting of discussion around men’s physical sexual problems than women’s physical sexual problems. More than half completely agreed that "society would prefer to believe that women my age do not have sex."
The use of more "socially acceptable" terminology (the word "penis," like "vagina," is still not used openly, Dr. Gass noted) helped make male sexual health a mainstream topic; it is hoped that transitioning from "vulvovaginal atrophy" to "genitourinary syndrome of menopause," would have a similar effect with respect to women’s sexual health, Dr. Portman said.
GSM would be defined as "a collection of symptoms and signs associated with decreased estrogen levels that can involve the labia majora/minora, vestibule/introitus, clitoris, vagina, urethra, and bladder," conference attendees agreed.
It is a syndrome for which treatment is indicated if symptoms are bothersome; treatment should be individualized based on the severity of symptoms and the woman’s preference after discussion of treatment options and risks and benefits.
In addition to working toward agreement on appropriate nomenclature, the consensus conference participants are developing an assessment tool, currently in draft form, to aid clinicians in evaluating women for the syndrome.
"We feel we’ve identified a number of signs and findings that would help clinicians – particularly those who don’t treat a lot of patients with this condition. The tool – which involves a grid-based design outlining mild, moderate, and severe symptom categories – may prove valuable for providers who want to chart severity or just scan the grid to assist in making a diagnosis," Dr. Gass said. The tool also could prove useful in the research setting, he added.
ISSWSH and NAMS will be publishing the proceedings of the workshop in upcoming issues of their respective journals – the Journal of Sexual Medicine and the journal Menopause.
The groups also plan to put forward the proposed new name at a December meeting of the American College of Obstetricians and Gynecologists. At that meeting, ACOG will review all terminology related to obstetrics and gynecology and update terminology as appropriate.
"We hope to address the ACOG urogynecology and menopause working group to see if the new name is acceptable to that group as well. Personally I think it’s important to have an accurate term that is as neutral as possible," Dr. Gass said.
Dr. Gass reported having no disclosures. Dr. Portman has been a speaker, consultant, or advisory board member for, and/or received grant or research support from Bayer, Noven Pharmaceuticals, Palatin Technologies, and other companies.
To varying degrees, vulvovaginal atrophy affects an estimated 20%-40% of menopausal women, but the name of the condition fails to appropriately characterize the range of associated signs and symptoms that women may experience.
Representatives from the North American Menopause Society (NAMS) and the International Society for the Study of Women’s Sexual Health, Inc. (ISSWSH) propose a new term: genitourinary syndrome of menopause, or GSM.
Earlier this year, the two organizations convened a 2-day consensus conference to consider what an appropriate term would encompass. The goal of that conference, according to Dr. Margery Gass of the Cleveland Clinic Center for Specialized Women’s Health and the executive director of NAMS, was to identify a term that was descriptive, comprehensive, and suitable for professionals, consumers, and the media.
Participants reviewed the symptoms and signs of genitourinary aging and the available relevant data, and decided on a number of components that should be covered by the new nomenclature, including the affected anatomy, descriptive factors, problems caused by the condition, and context with respect to life phase, she said in an interview.
Dr. Gass and Dr. David J. Portman, director of the Columbus Center for Women’s Health Research and an adjunct instructor at Ohio State University, Columbus, cochaired the consensus conference. They presented the conclusions from the conference at the annual meeting of the North American Menopause Society in October.
"Several concerns have forced the issue of a name change for this condition," Dr. Gass said, noting that persistent societal resistance to openly discussing women’s sexuality and sexual health is not the least among them.
The word "vagina," for example, still can’t be uttered in many media outlets, she explained. Additionally, the term "atrophy" has unpleasant connotations that aren’t necessarily reflective of the experience of women affected by the condition, she noted.
"In fact, atrophy in and of itself is a natural part of aging – something many women experience – and is not necessarily a problem; some women with atrophy experience no symptoms, while others experience significant symptoms.
"We feel that the name we’re putting forward (genitourinary syndrome of menopause) very accurately describes the parts of the body that are involved – namely the genital system and the lower urinary tract," she said.
The use of the word "syndrome" further allows for a diagnosis based on the range of symptoms women may experience, and doesn’t limit the condition to specific symptoms.
"This is not a disease or a deficiency, so we think ‘genitourinary syndrome of menopause’ is a neutral term that would be acceptable, Dr. Gass said.
A change in the nomenclature could potentially open the door to more productive, health-promoting dialogue. During his presentation at the NAMS meeting, Dr. Portman explained how a term that is more acceptable to patients and the media could have the power to start the conversation, change attitudes, and promote understanding and acceptance of more open communication. He used male sexual dysfunction as an example.
In 1992, a National Institutes of Health consensus development panel determined that the term "erectile dysfunction" was preferable to the term "impotence." Indeed, along with the subsequent approval of Viagra and other drugs related to male sexual health, the term "erectile dysfunction" is now widely used in advertising, promoted by politicians and celebrities, and openly discussed in the community, he said.
In contrast, open discussion about women’s sexuality and sexual health remains constrained. In fact, in a survey of more than 1,000 women – including 330 women aged 60-65 years – 75% "completely agreed" that society constrains the sexual expression of "women my age more so than men my age." Nearly as many completely agreed that society is more accepting of discussion around men’s physical sexual problems than women’s physical sexual problems. More than half completely agreed that "society would prefer to believe that women my age do not have sex."
The use of more "socially acceptable" terminology (the word "penis," like "vagina," is still not used openly, Dr. Gass noted) helped make male sexual health a mainstream topic; it is hoped that transitioning from "vulvovaginal atrophy" to "genitourinary syndrome of menopause," would have a similar effect with respect to women’s sexual health, Dr. Portman said.
GSM would be defined as "a collection of symptoms and signs associated with decreased estrogen levels that can involve the labia majora/minora, vestibule/introitus, clitoris, vagina, urethra, and bladder," conference attendees agreed.
It is a syndrome for which treatment is indicated if symptoms are bothersome; treatment should be individualized based on the severity of symptoms and the woman’s preference after discussion of treatment options and risks and benefits.
In addition to working toward agreement on appropriate nomenclature, the consensus conference participants are developing an assessment tool, currently in draft form, to aid clinicians in evaluating women for the syndrome.
"We feel we’ve identified a number of signs and findings that would help clinicians – particularly those who don’t treat a lot of patients with this condition. The tool – which involves a grid-based design outlining mild, moderate, and severe symptom categories – may prove valuable for providers who want to chart severity or just scan the grid to assist in making a diagnosis," Dr. Gass said. The tool also could prove useful in the research setting, he added.
ISSWSH and NAMS will be publishing the proceedings of the workshop in upcoming issues of their respective journals – the Journal of Sexual Medicine and the journal Menopause.
The groups also plan to put forward the proposed new name at a December meeting of the American College of Obstetricians and Gynecologists. At that meeting, ACOG will review all terminology related to obstetrics and gynecology and update terminology as appropriate.
"We hope to address the ACOG urogynecology and menopause working group to see if the new name is acceptable to that group as well. Personally I think it’s important to have an accurate term that is as neutral as possible," Dr. Gass said.
Dr. Gass reported having no disclosures. Dr. Portman has been a speaker, consultant, or advisory board member for, and/or received grant or research support from Bayer, Noven Pharmaceuticals, Palatin Technologies, and other companies.
EXPERT ANALYSIS FROM THE NAMS MEETING
Microarray is ‘go-to’ test for multiple congenital anomalies
ORLANDO – Chromosomal microarray testing is ideal for narrowing down the diagnosis in most patients presenting with multiple congenital anomalies, according to Dr. Laurie Demmer.
"Microarray is the clinical geneticist’s favorite test right now. We order it every day – anytime we see somebody with multiple congenital anomalies, unless it’s obviously Down syndrome or another obvious syndrome," Dr. Demmer said during a "Genetic Testing Boot Camp" session at the annual meeting of the American Academy of Pediatrics.
For children presenting with a suspected syndrome, problems with growth, or a development or autism spectrum disorder, microarray is "really our go-to test right now," said Dr. Demmer, a pediatric clinical geneticist at Levine Children’s Hospital, Charlotte, N.C.
Also, if chromosomal testing demonstrates a certain karyotype, such as a translocation, then microarray testing is the best approach for determining if it is a balanced translocation. If a marker chromosome is detected, microarray will identify it.
Like karyotyping, which is often used when a chromosomal anomaly is suspected, microarray testing provides a look at the whole genome, but it is about 100 times more sensitive than a karyotype. It is high resolution like fluorescent in situ hybridization (FISH), which is a chromosomal testing method often used when a quicker answer is needed to help guide management.
Thus, microarray testing is "kind of the best of both worlds," Dr. Demmer said, adding that with microarray analysis, it is possible to look for small deletions and duplications on all the chromosomes within the whole genome.
At first, microarray testing was targeted; rather than looking at the whole genome, testing was performed to look for known syndromes such as 22q deletions and Williams syndrome and Smith-Magenis syndrome, for example. Expanding the view to the whole genome has allowed for diagnosis of new syndromes that were never known before.
"Every week I get one or two arrays back that are abnormal with a new deletion or duplication that I’d never seen or heard of before," she said, noting that a downside of this is that there’s no clear answer to what should be done with all of these "copy number variants." Currently they are being characterized in databases as a reference.
The latest generation of microarray testing (single nucleotide polymorphism, or SNP array) provides qualitative information not available with oligoarray testing.
"It allows us to tell the difference between chromosomes. ... It gives us the ability to tell if there is identity in the chromosomes," she said, explaining that this may mean identifying uniparental disomy (and likely Prader-Willi syndrome), consanguinity (and degree of relationship), and other circumstances associated with autosomal recessive disease.
A downside of microarray testing is that it only looks for deletions and duplications, and therefore does not detect balanced rearrangements. Thus a balanced translocation will not be detected on microarray testing, and an opportunity for genetic counseling could be missed.
Also, sometimes a copy number variant or deletion or duplication is found, and it is unclear how these should be interpreted.
A general rule of thumb, however, is that the bigger it is, the more likely it is to be significant, Dr. Demmer said, noting that in some of these cases, the parents are tested, and if a parent has the same copy number variant but is normal, the finding is usually a benign change.
Sometimes, however, a parent who has the copy number variant may be "on the spectrum somewhere, but not actually diagnosed, and they may have one of the changes associated with autism."
These cases require special care in interpretation, Dr. Demmer said. "If you’re going to send out for microarrays in your office and it comes back normal, that’s great, but if it comes back anything else, you may want to get a geneticist to help you," she said.
Similarly, unanticipated results – incidental findings – also occur, and these can be tricky to deal with. Examples include cases of unknown consanguinity and incest, she said.
Sometimes the incidental findings lead to improved outcomes. Dr. Demmer described one case involving an intellectually disabled 10-year-old girl who was incidentally found on microarray testing to be at genetic risk for familial adenomatous polyposis (FAP). A gastrointestinal examination showed that she already had thousands of polyps.
"So she has FAP, which we diagnosed by doing the microarray, and probably saved her life, because now we will treat her, and we’re going to prevent the colon cancer," she said.
Dr. Demmer reported having no disclosures.
ORLANDO – Chromosomal microarray testing is ideal for narrowing down the diagnosis in most patients presenting with multiple congenital anomalies, according to Dr. Laurie Demmer.
"Microarray is the clinical geneticist’s favorite test right now. We order it every day – anytime we see somebody with multiple congenital anomalies, unless it’s obviously Down syndrome or another obvious syndrome," Dr. Demmer said during a "Genetic Testing Boot Camp" session at the annual meeting of the American Academy of Pediatrics.
For children presenting with a suspected syndrome, problems with growth, or a development or autism spectrum disorder, microarray is "really our go-to test right now," said Dr. Demmer, a pediatric clinical geneticist at Levine Children’s Hospital, Charlotte, N.C.
Also, if chromosomal testing demonstrates a certain karyotype, such as a translocation, then microarray testing is the best approach for determining if it is a balanced translocation. If a marker chromosome is detected, microarray will identify it.
Like karyotyping, which is often used when a chromosomal anomaly is suspected, microarray testing provides a look at the whole genome, but it is about 100 times more sensitive than a karyotype. It is high resolution like fluorescent in situ hybridization (FISH), which is a chromosomal testing method often used when a quicker answer is needed to help guide management.
Thus, microarray testing is "kind of the best of both worlds," Dr. Demmer said, adding that with microarray analysis, it is possible to look for small deletions and duplications on all the chromosomes within the whole genome.
At first, microarray testing was targeted; rather than looking at the whole genome, testing was performed to look for known syndromes such as 22q deletions and Williams syndrome and Smith-Magenis syndrome, for example. Expanding the view to the whole genome has allowed for diagnosis of new syndromes that were never known before.
"Every week I get one or two arrays back that are abnormal with a new deletion or duplication that I’d never seen or heard of before," she said, noting that a downside of this is that there’s no clear answer to what should be done with all of these "copy number variants." Currently they are being characterized in databases as a reference.
The latest generation of microarray testing (single nucleotide polymorphism, or SNP array) provides qualitative information not available with oligoarray testing.
"It allows us to tell the difference between chromosomes. ... It gives us the ability to tell if there is identity in the chromosomes," she said, explaining that this may mean identifying uniparental disomy (and likely Prader-Willi syndrome), consanguinity (and degree of relationship), and other circumstances associated with autosomal recessive disease.
A downside of microarray testing is that it only looks for deletions and duplications, and therefore does not detect balanced rearrangements. Thus a balanced translocation will not be detected on microarray testing, and an opportunity for genetic counseling could be missed.
Also, sometimes a copy number variant or deletion or duplication is found, and it is unclear how these should be interpreted.
A general rule of thumb, however, is that the bigger it is, the more likely it is to be significant, Dr. Demmer said, noting that in some of these cases, the parents are tested, and if a parent has the same copy number variant but is normal, the finding is usually a benign change.
Sometimes, however, a parent who has the copy number variant may be "on the spectrum somewhere, but not actually diagnosed, and they may have one of the changes associated with autism."
These cases require special care in interpretation, Dr. Demmer said. "If you’re going to send out for microarrays in your office and it comes back normal, that’s great, but if it comes back anything else, you may want to get a geneticist to help you," she said.
Similarly, unanticipated results – incidental findings – also occur, and these can be tricky to deal with. Examples include cases of unknown consanguinity and incest, she said.
Sometimes the incidental findings lead to improved outcomes. Dr. Demmer described one case involving an intellectually disabled 10-year-old girl who was incidentally found on microarray testing to be at genetic risk for familial adenomatous polyposis (FAP). A gastrointestinal examination showed that she already had thousands of polyps.
"So she has FAP, which we diagnosed by doing the microarray, and probably saved her life, because now we will treat her, and we’re going to prevent the colon cancer," she said.
Dr. Demmer reported having no disclosures.
ORLANDO – Chromosomal microarray testing is ideal for narrowing down the diagnosis in most patients presenting with multiple congenital anomalies, according to Dr. Laurie Demmer.
"Microarray is the clinical geneticist’s favorite test right now. We order it every day – anytime we see somebody with multiple congenital anomalies, unless it’s obviously Down syndrome or another obvious syndrome," Dr. Demmer said during a "Genetic Testing Boot Camp" session at the annual meeting of the American Academy of Pediatrics.
For children presenting with a suspected syndrome, problems with growth, or a development or autism spectrum disorder, microarray is "really our go-to test right now," said Dr. Demmer, a pediatric clinical geneticist at Levine Children’s Hospital, Charlotte, N.C.
Also, if chromosomal testing demonstrates a certain karyotype, such as a translocation, then microarray testing is the best approach for determining if it is a balanced translocation. If a marker chromosome is detected, microarray will identify it.
Like karyotyping, which is often used when a chromosomal anomaly is suspected, microarray testing provides a look at the whole genome, but it is about 100 times more sensitive than a karyotype. It is high resolution like fluorescent in situ hybridization (FISH), which is a chromosomal testing method often used when a quicker answer is needed to help guide management.
Thus, microarray testing is "kind of the best of both worlds," Dr. Demmer said, adding that with microarray analysis, it is possible to look for small deletions and duplications on all the chromosomes within the whole genome.
At first, microarray testing was targeted; rather than looking at the whole genome, testing was performed to look for known syndromes such as 22q deletions and Williams syndrome and Smith-Magenis syndrome, for example. Expanding the view to the whole genome has allowed for diagnosis of new syndromes that were never known before.
"Every week I get one or two arrays back that are abnormal with a new deletion or duplication that I’d never seen or heard of before," she said, noting that a downside of this is that there’s no clear answer to what should be done with all of these "copy number variants." Currently they are being characterized in databases as a reference.
The latest generation of microarray testing (single nucleotide polymorphism, or SNP array) provides qualitative information not available with oligoarray testing.
"It allows us to tell the difference between chromosomes. ... It gives us the ability to tell if there is identity in the chromosomes," she said, explaining that this may mean identifying uniparental disomy (and likely Prader-Willi syndrome), consanguinity (and degree of relationship), and other circumstances associated with autosomal recessive disease.
A downside of microarray testing is that it only looks for deletions and duplications, and therefore does not detect balanced rearrangements. Thus a balanced translocation will not be detected on microarray testing, and an opportunity for genetic counseling could be missed.
Also, sometimes a copy number variant or deletion or duplication is found, and it is unclear how these should be interpreted.
A general rule of thumb, however, is that the bigger it is, the more likely it is to be significant, Dr. Demmer said, noting that in some of these cases, the parents are tested, and if a parent has the same copy number variant but is normal, the finding is usually a benign change.
Sometimes, however, a parent who has the copy number variant may be "on the spectrum somewhere, but not actually diagnosed, and they may have one of the changes associated with autism."
These cases require special care in interpretation, Dr. Demmer said. "If you’re going to send out for microarrays in your office and it comes back normal, that’s great, but if it comes back anything else, you may want to get a geneticist to help you," she said.
Similarly, unanticipated results – incidental findings – also occur, and these can be tricky to deal with. Examples include cases of unknown consanguinity and incest, she said.
Sometimes the incidental findings lead to improved outcomes. Dr. Demmer described one case involving an intellectually disabled 10-year-old girl who was incidentally found on microarray testing to be at genetic risk for familial adenomatous polyposis (FAP). A gastrointestinal examination showed that she already had thousands of polyps.
"So she has FAP, which we diagnosed by doing the microarray, and probably saved her life, because now we will treat her, and we’re going to prevent the colon cancer," she said.
Dr. Demmer reported having no disclosures.
EXPERT ANALYSIS FROM THE AAP NATIONAL CONFERENCE
Pediatric firearm injuries vary by age
ORLANDO – The majority of children and adolescents who presented with firearm-related injuries to an urban level 1 trauma center over a 6-year period were black males over age 14 years according to a retrospective review of patient records.
Furthermore, children aged 14 years and younger were more likely than were older children to be shot at home, Dr. Andrea C. Suen reported at the annual meeting of the American Academy of Pediatrics.
The findings, which also characterized other age-related injury patterns, injury sites, and methods of transportation to the hospital, provide important information that could help in the development of effective crime- and injury-prevention strategies, she said.
Of 456 patients aged 18 years and younger who presented to the trauma center between January 2005 and 2010, 78 were aged 14 years or younger and 378 were aged 15-18 years. Overall, 86% were male, and 80% were black, but these figures differed by age group; 72% and 89% of those 14 years and younger and those 15-18 years, respectively, were male, and 64% and 83% of those 14 years and younger and those 15-18 years, respectively, were black, said Dr. Suen, a third-year pediatric emergency medicine fellow at the University of Florida Health Science Center, Jacksonville.
Those aged 14 years and younger were almost four times more likely to be shot at home (odds ratio, 3.76), and were much more likely to arrive by ambulance than by private car or to walk in than those aged 15-18 years.
The most common injury sites among children under age 14 years were the extremities (51% of cases), the trunk (41%), the head (16%), and the neck (9%). Those aged 5-9 years had a greater than sixfold increase in the likelihood of multiple injury sites, compared with those aged 10-14 years (OR, 6.26), she said.
In both age groups, 7.1% of patients died as a result of their injury.
In nearly 70% of cases, the shooter was someone unknown to the patient, and in 64% of cases, the type of firearm was unknown.
The findings of this study illustrate important age-based differences in firearm injuries, and highlight a need for improved reporting in firearm-related incidents, according to primary author and investigator, Dr. Phyllis Hendry of the department of emergency medicine at the university, who noted that hospital and emergency medical services reports in this study often lacked important details – such as patient’s relationship to the shooter and type of gun used – necessary for development of effective prevention strategies.
In an interview, Dr. Hendry further noted that the findings underscore the need for pediatricians to address gun safety and precautions in the home, as firearm-related injuries in children and adolescents are an important cause of preventable injury and mortality.
Also, emergency physicians should consider making a referral to child protective services on pediatric firearm injuries to assess the safety of the home, she said. "In our study, only 13% of patients 0-14 years of age had child-protection referrals documented."
Dr. Suen and Dr. Hendry reported having no disclosures.
ORLANDO – The majority of children and adolescents who presented with firearm-related injuries to an urban level 1 trauma center over a 6-year period were black males over age 14 years according to a retrospective review of patient records.
Furthermore, children aged 14 years and younger were more likely than were older children to be shot at home, Dr. Andrea C. Suen reported at the annual meeting of the American Academy of Pediatrics.
The findings, which also characterized other age-related injury patterns, injury sites, and methods of transportation to the hospital, provide important information that could help in the development of effective crime- and injury-prevention strategies, she said.
Of 456 patients aged 18 years and younger who presented to the trauma center between January 2005 and 2010, 78 were aged 14 years or younger and 378 were aged 15-18 years. Overall, 86% were male, and 80% were black, but these figures differed by age group; 72% and 89% of those 14 years and younger and those 15-18 years, respectively, were male, and 64% and 83% of those 14 years and younger and those 15-18 years, respectively, were black, said Dr. Suen, a third-year pediatric emergency medicine fellow at the University of Florida Health Science Center, Jacksonville.
Those aged 14 years and younger were almost four times more likely to be shot at home (odds ratio, 3.76), and were much more likely to arrive by ambulance than by private car or to walk in than those aged 15-18 years.
The most common injury sites among children under age 14 years were the extremities (51% of cases), the trunk (41%), the head (16%), and the neck (9%). Those aged 5-9 years had a greater than sixfold increase in the likelihood of multiple injury sites, compared with those aged 10-14 years (OR, 6.26), she said.
In both age groups, 7.1% of patients died as a result of their injury.
In nearly 70% of cases, the shooter was someone unknown to the patient, and in 64% of cases, the type of firearm was unknown.
The findings of this study illustrate important age-based differences in firearm injuries, and highlight a need for improved reporting in firearm-related incidents, according to primary author and investigator, Dr. Phyllis Hendry of the department of emergency medicine at the university, who noted that hospital and emergency medical services reports in this study often lacked important details – such as patient’s relationship to the shooter and type of gun used – necessary for development of effective prevention strategies.
In an interview, Dr. Hendry further noted that the findings underscore the need for pediatricians to address gun safety and precautions in the home, as firearm-related injuries in children and adolescents are an important cause of preventable injury and mortality.
Also, emergency physicians should consider making a referral to child protective services on pediatric firearm injuries to assess the safety of the home, she said. "In our study, only 13% of patients 0-14 years of age had child-protection referrals documented."
Dr. Suen and Dr. Hendry reported having no disclosures.
ORLANDO – The majority of children and adolescents who presented with firearm-related injuries to an urban level 1 trauma center over a 6-year period were black males over age 14 years according to a retrospective review of patient records.
Furthermore, children aged 14 years and younger were more likely than were older children to be shot at home, Dr. Andrea C. Suen reported at the annual meeting of the American Academy of Pediatrics.
The findings, which also characterized other age-related injury patterns, injury sites, and methods of transportation to the hospital, provide important information that could help in the development of effective crime- and injury-prevention strategies, she said.
Of 456 patients aged 18 years and younger who presented to the trauma center between January 2005 and 2010, 78 were aged 14 years or younger and 378 were aged 15-18 years. Overall, 86% were male, and 80% were black, but these figures differed by age group; 72% and 89% of those 14 years and younger and those 15-18 years, respectively, were male, and 64% and 83% of those 14 years and younger and those 15-18 years, respectively, were black, said Dr. Suen, a third-year pediatric emergency medicine fellow at the University of Florida Health Science Center, Jacksonville.
Those aged 14 years and younger were almost four times more likely to be shot at home (odds ratio, 3.76), and were much more likely to arrive by ambulance than by private car or to walk in than those aged 15-18 years.
The most common injury sites among children under age 14 years were the extremities (51% of cases), the trunk (41%), the head (16%), and the neck (9%). Those aged 5-9 years had a greater than sixfold increase in the likelihood of multiple injury sites, compared with those aged 10-14 years (OR, 6.26), she said.
In both age groups, 7.1% of patients died as a result of their injury.
In nearly 70% of cases, the shooter was someone unknown to the patient, and in 64% of cases, the type of firearm was unknown.
The findings of this study illustrate important age-based differences in firearm injuries, and highlight a need for improved reporting in firearm-related incidents, according to primary author and investigator, Dr. Phyllis Hendry of the department of emergency medicine at the university, who noted that hospital and emergency medical services reports in this study often lacked important details – such as patient’s relationship to the shooter and type of gun used – necessary for development of effective prevention strategies.
In an interview, Dr. Hendry further noted that the findings underscore the need for pediatricians to address gun safety and precautions in the home, as firearm-related injuries in children and adolescents are an important cause of preventable injury and mortality.
Also, emergency physicians should consider making a referral to child protective services on pediatric firearm injuries to assess the safety of the home, she said. "In our study, only 13% of patients 0-14 years of age had child-protection referrals documented."
Dr. Suen and Dr. Hendry reported having no disclosures.
AT THE AAP NATIONAL CONFERENCE
Major finding: Children aged 14 years and under who experience firearm-related injury are more likely than are older children to be shot at home.
Data source: A retrospective review involving 456 patients.
Disclosures: Dr. Suen and Dr. Hendry reported having no disclosures.
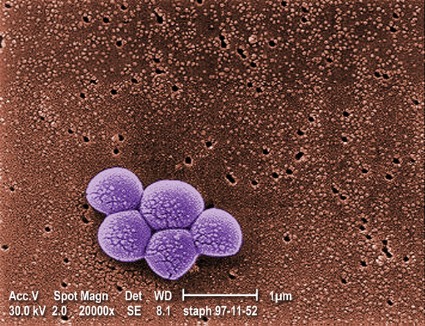
Age-based differences seen in effects of PCV13
SAN FRANCISCO – The incidence of invasive pneumococcal disease among children is declining in the wake of the 2010 introduction of the 13-valent pneumococcal conjugate vaccine, surveillance data suggest.
In New York City during 2011-2012, for example, the incidence of invasive pneumococcal disease (IPD) declined among children under age 5 across all age categories and race/ethnicity groups, Andrea Farnham of the New York City Department of Health and Mental Hygiene reported in a poster at an annual scientific meeting on infectious diseases.
The decline was driven by a reduction in 13-valent pneumococcal conjugate vaccine (PCV13)-type IPD and was temporally associated with the introduction and increased uptake of PCV13 vaccine, she said.
IPD incidence decreased by 70% (from 21.0 to 6.4 cases/100,000) between 2007-2009 and 2011-2012, and PCV13-type IPD incidence decreased 82% (from 15.3 to 2.7 cases/100,000) in that same time period.
The greatest decrease (80%) occurred in children under age 12 months. Decreases were 68% and 62.1% in those aged 12-35 months and 36-59 months, respectively, Ms. Farnham noted.
Another study presented at the meeting showed that 89% of PCV13 serotype disease in Ontario during the second year after the implementation of PCV13 vaccine (2012-2013) occurred in unvaccinated children. Half of the cases (14 of 28) were in children who were not eligible for vaccination, and of the remaining 14, 1 child was unvaccinated, 3 had missed doses, 7 had appropriately received PCV7 vaccine but missed the PCV13 catch-up dose, and 2 received PCV13 vaccine at ages 2 and 4 months but developed IPD at ages 10 and 11 months, respectively, Karen Green, an epidemiologist at Mount Sinai Hospital, Toronto, also reported in a poster.
One apparently healthy 5-year-old developed empyema from serotype 5 disease after receiving age-appropriate vaccination, she noted at the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
The findings suggest that PCV13 vaccination is having a substantial effect on rates of IPD – an effect that could be improved upon with increased vaccine coverage.
A third study suggested that children over age 2 years, in particular, may not be vaccinated appropriately.
In that study, John M. McLaughlin, Ph.D., of Pfizer Specialty Care Medicines Development Group, Collegeville, Penn, showed that although children up to age 1 year had significant reductions in all 13 serotypes covered by the PCV13 vaccine, those aged 2-17 years did not experience a reduction in serotype 19A disease.
Overall, among children aged 0-17 years, the proportion of IPD caused by serotype 19A decreased from 37% in 2008-2009 to 28% in 2010-2011, and the proportion caused by the other 12 serotypes in the PCV13 vaccine decreased from 66% to 48% during the same period.
However, while there was a 44% relative reduction in the proportion of IPD caused by serotypes in the PCV13 vaccine among those aged 0-1 years, there was only a 17% relative reduction in those aged 2-17 years.
"The difference in these two age groups was driven largely by the difference in reduction of the proportion of IPD caused by serotype 19A," he said, explaining that there was a 36% relative reduction in the proportion of IPD caused by serotype 19A among those aged 0-1 years, but no decrease in those aged 2-17 years.
No difference was seen between the 0- to 1-year age group and the 2- to 17-year age group for the remaining serotypes (32% for both groups).
This could be a result of a lack of early indirect effect of vaccination or of the virulence of 19A, or it could be caused by more comorbid disease in the older age group. Comorbidities increased significantly with increasing age, Dr. McLaughlin said, noting that 27% of those aged less than 1 year had comorbid conditions, compared with 32% of those aged 1-2 years, 45% of those aged 3-5 years, and 60% of those aged 6-17 years.
Low PCV13 vaccination rates in older children may also be a factor; in this study, only two children aged 11 years and over had received PCV13 vaccination.
IPD cases in Dr. McLaughlin’s study were identified from eight geographically dispersed children’s hospitals in the U.S. Pediatric Multicenter Pneumococcal Surveillance Study Group. The findings support the Jan. 25, 2013, decision by the Food and Drug Administration to expand the age indication for PCV13 vaccination in children and teens to those aged 6-17 years for prevention of vaccine-type IPD, he concluded (AAP News 2013 March 6 [doi: 10.1542/aapnews.20130306-2]).
Ms. Farnham stressed the importance of vaccination.
"Given the potential of PCV13 to reduce IPD incidence and racial/ethnic disparities, efforts should be focused on increasing coverage of PCV13 and ensuring patients receive all the recommended doses of PCV13," she concluded.
Ms. Green reported working as a grant investigator for, and receiving educational and/or research support from, Pfizer and GlaxoSmithKline. Dr. McLaughlin reported that he is an employee and shareholder of Pfizer. Ms. Farnham reported having no disclosures.
SAN FRANCISCO – The incidence of invasive pneumococcal disease among children is declining in the wake of the 2010 introduction of the 13-valent pneumococcal conjugate vaccine, surveillance data suggest.
In New York City during 2011-2012, for example, the incidence of invasive pneumococcal disease (IPD) declined among children under age 5 across all age categories and race/ethnicity groups, Andrea Farnham of the New York City Department of Health and Mental Hygiene reported in a poster at an annual scientific meeting on infectious diseases.
The decline was driven by a reduction in 13-valent pneumococcal conjugate vaccine (PCV13)-type IPD and was temporally associated with the introduction and increased uptake of PCV13 vaccine, she said.
IPD incidence decreased by 70% (from 21.0 to 6.4 cases/100,000) between 2007-2009 and 2011-2012, and PCV13-type IPD incidence decreased 82% (from 15.3 to 2.7 cases/100,000) in that same time period.
The greatest decrease (80%) occurred in children under age 12 months. Decreases were 68% and 62.1% in those aged 12-35 months and 36-59 months, respectively, Ms. Farnham noted.
Another study presented at the meeting showed that 89% of PCV13 serotype disease in Ontario during the second year after the implementation of PCV13 vaccine (2012-2013) occurred in unvaccinated children. Half of the cases (14 of 28) were in children who were not eligible for vaccination, and of the remaining 14, 1 child was unvaccinated, 3 had missed doses, 7 had appropriately received PCV7 vaccine but missed the PCV13 catch-up dose, and 2 received PCV13 vaccine at ages 2 and 4 months but developed IPD at ages 10 and 11 months, respectively, Karen Green, an epidemiologist at Mount Sinai Hospital, Toronto, also reported in a poster.
One apparently healthy 5-year-old developed empyema from serotype 5 disease after receiving age-appropriate vaccination, she noted at the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
The findings suggest that PCV13 vaccination is having a substantial effect on rates of IPD – an effect that could be improved upon with increased vaccine coverage.
A third study suggested that children over age 2 years, in particular, may not be vaccinated appropriately.
In that study, John M. McLaughlin, Ph.D., of Pfizer Specialty Care Medicines Development Group, Collegeville, Penn, showed that although children up to age 1 year had significant reductions in all 13 serotypes covered by the PCV13 vaccine, those aged 2-17 years did not experience a reduction in serotype 19A disease.
Overall, among children aged 0-17 years, the proportion of IPD caused by serotype 19A decreased from 37% in 2008-2009 to 28% in 2010-2011, and the proportion caused by the other 12 serotypes in the PCV13 vaccine decreased from 66% to 48% during the same period.
However, while there was a 44% relative reduction in the proportion of IPD caused by serotypes in the PCV13 vaccine among those aged 0-1 years, there was only a 17% relative reduction in those aged 2-17 years.
"The difference in these two age groups was driven largely by the difference in reduction of the proportion of IPD caused by serotype 19A," he said, explaining that there was a 36% relative reduction in the proportion of IPD caused by serotype 19A among those aged 0-1 years, but no decrease in those aged 2-17 years.
No difference was seen between the 0- to 1-year age group and the 2- to 17-year age group for the remaining serotypes (32% for both groups).
This could be a result of a lack of early indirect effect of vaccination or of the virulence of 19A, or it could be caused by more comorbid disease in the older age group. Comorbidities increased significantly with increasing age, Dr. McLaughlin said, noting that 27% of those aged less than 1 year had comorbid conditions, compared with 32% of those aged 1-2 years, 45% of those aged 3-5 years, and 60% of those aged 6-17 years.
Low PCV13 vaccination rates in older children may also be a factor; in this study, only two children aged 11 years and over had received PCV13 vaccination.
IPD cases in Dr. McLaughlin’s study were identified from eight geographically dispersed children’s hospitals in the U.S. Pediatric Multicenter Pneumococcal Surveillance Study Group. The findings support the Jan. 25, 2013, decision by the Food and Drug Administration to expand the age indication for PCV13 vaccination in children and teens to those aged 6-17 years for prevention of vaccine-type IPD, he concluded (AAP News 2013 March 6 [doi: 10.1542/aapnews.20130306-2]).
Ms. Farnham stressed the importance of vaccination.
"Given the potential of PCV13 to reduce IPD incidence and racial/ethnic disparities, efforts should be focused on increasing coverage of PCV13 and ensuring patients receive all the recommended doses of PCV13," she concluded.
Ms. Green reported working as a grant investigator for, and receiving educational and/or research support from, Pfizer and GlaxoSmithKline. Dr. McLaughlin reported that he is an employee and shareholder of Pfizer. Ms. Farnham reported having no disclosures.
SAN FRANCISCO – The incidence of invasive pneumococcal disease among children is declining in the wake of the 2010 introduction of the 13-valent pneumococcal conjugate vaccine, surveillance data suggest.
In New York City during 2011-2012, for example, the incidence of invasive pneumococcal disease (IPD) declined among children under age 5 across all age categories and race/ethnicity groups, Andrea Farnham of the New York City Department of Health and Mental Hygiene reported in a poster at an annual scientific meeting on infectious diseases.
The decline was driven by a reduction in 13-valent pneumococcal conjugate vaccine (PCV13)-type IPD and was temporally associated with the introduction and increased uptake of PCV13 vaccine, she said.
IPD incidence decreased by 70% (from 21.0 to 6.4 cases/100,000) between 2007-2009 and 2011-2012, and PCV13-type IPD incidence decreased 82% (from 15.3 to 2.7 cases/100,000) in that same time period.
The greatest decrease (80%) occurred in children under age 12 months. Decreases were 68% and 62.1% in those aged 12-35 months and 36-59 months, respectively, Ms. Farnham noted.
Another study presented at the meeting showed that 89% of PCV13 serotype disease in Ontario during the second year after the implementation of PCV13 vaccine (2012-2013) occurred in unvaccinated children. Half of the cases (14 of 28) were in children who were not eligible for vaccination, and of the remaining 14, 1 child was unvaccinated, 3 had missed doses, 7 had appropriately received PCV7 vaccine but missed the PCV13 catch-up dose, and 2 received PCV13 vaccine at ages 2 and 4 months but developed IPD at ages 10 and 11 months, respectively, Karen Green, an epidemiologist at Mount Sinai Hospital, Toronto, also reported in a poster.
One apparently healthy 5-year-old developed empyema from serotype 5 disease after receiving age-appropriate vaccination, she noted at the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
The findings suggest that PCV13 vaccination is having a substantial effect on rates of IPD – an effect that could be improved upon with increased vaccine coverage.
A third study suggested that children over age 2 years, in particular, may not be vaccinated appropriately.
In that study, John M. McLaughlin, Ph.D., of Pfizer Specialty Care Medicines Development Group, Collegeville, Penn, showed that although children up to age 1 year had significant reductions in all 13 serotypes covered by the PCV13 vaccine, those aged 2-17 years did not experience a reduction in serotype 19A disease.
Overall, among children aged 0-17 years, the proportion of IPD caused by serotype 19A decreased from 37% in 2008-2009 to 28% in 2010-2011, and the proportion caused by the other 12 serotypes in the PCV13 vaccine decreased from 66% to 48% during the same period.
However, while there was a 44% relative reduction in the proportion of IPD caused by serotypes in the PCV13 vaccine among those aged 0-1 years, there was only a 17% relative reduction in those aged 2-17 years.
"The difference in these two age groups was driven largely by the difference in reduction of the proportion of IPD caused by serotype 19A," he said, explaining that there was a 36% relative reduction in the proportion of IPD caused by serotype 19A among those aged 0-1 years, but no decrease in those aged 2-17 years.
No difference was seen between the 0- to 1-year age group and the 2- to 17-year age group for the remaining serotypes (32% for both groups).
This could be a result of a lack of early indirect effect of vaccination or of the virulence of 19A, or it could be caused by more comorbid disease in the older age group. Comorbidities increased significantly with increasing age, Dr. McLaughlin said, noting that 27% of those aged less than 1 year had comorbid conditions, compared with 32% of those aged 1-2 years, 45% of those aged 3-5 years, and 60% of those aged 6-17 years.
Low PCV13 vaccination rates in older children may also be a factor; in this study, only two children aged 11 years and over had received PCV13 vaccination.
IPD cases in Dr. McLaughlin’s study were identified from eight geographically dispersed children’s hospitals in the U.S. Pediatric Multicenter Pneumococcal Surveillance Study Group. The findings support the Jan. 25, 2013, decision by the Food and Drug Administration to expand the age indication for PCV13 vaccination in children and teens to those aged 6-17 years for prevention of vaccine-type IPD, he concluded (AAP News 2013 March 6 [doi: 10.1542/aapnews.20130306-2]).
Ms. Farnham stressed the importance of vaccination.
"Given the potential of PCV13 to reduce IPD incidence and racial/ethnic disparities, efforts should be focused on increasing coverage of PCV13 and ensuring patients receive all the recommended doses of PCV13," she concluded.
Ms. Green reported working as a grant investigator for, and receiving educational and/or research support from, Pfizer and GlaxoSmithKline. Dr. McLaughlin reported that he is an employee and shareholder of Pfizer. Ms. Farnham reported having no disclosures.
AT IDWEEK 2013
Major finding: IPD cases declined following introduction of PCV13.
Data source: Medical chart review and surveillance.
Disclosures: Ms. Green reported working as a grant investigator for, and receiving educational and/or research support from, Pfizer and GlaxoSmithKline. Dr. McLaughlin reported that he is an employee and shareholder of Pfizer. Ms. Farnham reported having no disclosures.
Bicycle helmet use remains low, varies by ethnicity and socioeconomic status
ORLANDO – Only 11.3% of more than 1,200 children involved in bicycle-related accidents were wearing a helmet at the time of the accident, a study showed.
Children over age 12, and those of minority background and lower socioeconomic status, had the lowest rates of helmet use; thus the findings have implications for targeted education and prevention strategies, Dr. Veronica Sullins reported at the annual meeting of the American Academy of Pediatrics.
Of the 1,248 children from Los Angeles County who were included in the retrospective study of all injuries related to pediatric bicycle accidents between 2006 and 2011, most (85%) were boys. More than a third (35.2%) of white children wore helmets, but the rates were much lower for Asian (7.0%), black (6.0%), and Hispanic children (4.2%), said Dr. Sullins of the Harbor-UCLA Medical Center in Torrance, Calif.
This is despite laws mandating helmet use in Los Angeles County, Dr. Sullins noted.
The differences in helmet use also appeared to vary based on socioeconomic status; helmets were worn by 15.2% of those with private insurance, compared with 7.6% of those with public insurance, Dr. Sullins noted.
Children in the study had a median age of 13 years. Those over age 12 were less likely to wear helmets than were those aged 12 years or younger (odds ratio, 0.7).
Emergency surgery was required in 5.9% of the children, and only 34.1% returned to their preinjury status. Nine patients (0.7%) died as a result of their injuries; eight of those were not wearing a helmet.
The findings suggest that targeting low-income middle and high schools and minority communities with bicycle safety education and accident prevention strategies may help improve helmet use in children, Dr. Sullins said.
"We really need to focus our efforts and resources on education programs targeting the highest-risk groups. In Los Angeles County, these groups are middle and high school–aged children, minorities, and those of lower socioeconomic status," Dr. Sullins said in an interview.
According to the Centers for Disease Control and Prevention, an estimated 33 million children ride bicycles – for a total of 10 billion hours - each year, and nearly 400 children die as a result of bicycle crashes.
More than 150,000 emergency department visits each year are due to bicycle-related head injuries.
Helmet use has been shown to reduce bicycle-related head injuries by 80%; yet, as the results of this study and others show, the rate of helmet use remains low. The CDC reports that only 15% of adults and 19% of children wear helmets most or all of the time when riding a bicycle.
"We encourage other investigators to perform similar studies to identify [the highest-risk] groups specific to their regions or cities in order to more efficiently direct local injury prevention programs," Dr. Sullins said in the interview.
She reported having no relevant financial disclosures.
ORLANDO – Only 11.3% of more than 1,200 children involved in bicycle-related accidents were wearing a helmet at the time of the accident, a study showed.
Children over age 12, and those of minority background and lower socioeconomic status, had the lowest rates of helmet use; thus the findings have implications for targeted education and prevention strategies, Dr. Veronica Sullins reported at the annual meeting of the American Academy of Pediatrics.
Of the 1,248 children from Los Angeles County who were included in the retrospective study of all injuries related to pediatric bicycle accidents between 2006 and 2011, most (85%) were boys. More than a third (35.2%) of white children wore helmets, but the rates were much lower for Asian (7.0%), black (6.0%), and Hispanic children (4.2%), said Dr. Sullins of the Harbor-UCLA Medical Center in Torrance, Calif.
This is despite laws mandating helmet use in Los Angeles County, Dr. Sullins noted.
The differences in helmet use also appeared to vary based on socioeconomic status; helmets were worn by 15.2% of those with private insurance, compared with 7.6% of those with public insurance, Dr. Sullins noted.
Children in the study had a median age of 13 years. Those over age 12 were less likely to wear helmets than were those aged 12 years or younger (odds ratio, 0.7).
Emergency surgery was required in 5.9% of the children, and only 34.1% returned to their preinjury status. Nine patients (0.7%) died as a result of their injuries; eight of those were not wearing a helmet.
The findings suggest that targeting low-income middle and high schools and minority communities with bicycle safety education and accident prevention strategies may help improve helmet use in children, Dr. Sullins said.
"We really need to focus our efforts and resources on education programs targeting the highest-risk groups. In Los Angeles County, these groups are middle and high school–aged children, minorities, and those of lower socioeconomic status," Dr. Sullins said in an interview.
According to the Centers for Disease Control and Prevention, an estimated 33 million children ride bicycles – for a total of 10 billion hours - each year, and nearly 400 children die as a result of bicycle crashes.
More than 150,000 emergency department visits each year are due to bicycle-related head injuries.
Helmet use has been shown to reduce bicycle-related head injuries by 80%; yet, as the results of this study and others show, the rate of helmet use remains low. The CDC reports that only 15% of adults and 19% of children wear helmets most or all of the time when riding a bicycle.
"We encourage other investigators to perform similar studies to identify [the highest-risk] groups specific to their regions or cities in order to more efficiently direct local injury prevention programs," Dr. Sullins said in the interview.
She reported having no relevant financial disclosures.
ORLANDO – Only 11.3% of more than 1,200 children involved in bicycle-related accidents were wearing a helmet at the time of the accident, a study showed.
Children over age 12, and those of minority background and lower socioeconomic status, had the lowest rates of helmet use; thus the findings have implications for targeted education and prevention strategies, Dr. Veronica Sullins reported at the annual meeting of the American Academy of Pediatrics.
Of the 1,248 children from Los Angeles County who were included in the retrospective study of all injuries related to pediatric bicycle accidents between 2006 and 2011, most (85%) were boys. More than a third (35.2%) of white children wore helmets, but the rates were much lower for Asian (7.0%), black (6.0%), and Hispanic children (4.2%), said Dr. Sullins of the Harbor-UCLA Medical Center in Torrance, Calif.
This is despite laws mandating helmet use in Los Angeles County, Dr. Sullins noted.
The differences in helmet use also appeared to vary based on socioeconomic status; helmets were worn by 15.2% of those with private insurance, compared with 7.6% of those with public insurance, Dr. Sullins noted.
Children in the study had a median age of 13 years. Those over age 12 were less likely to wear helmets than were those aged 12 years or younger (odds ratio, 0.7).
Emergency surgery was required in 5.9% of the children, and only 34.1% returned to their preinjury status. Nine patients (0.7%) died as a result of their injuries; eight of those were not wearing a helmet.
The findings suggest that targeting low-income middle and high schools and minority communities with bicycle safety education and accident prevention strategies may help improve helmet use in children, Dr. Sullins said.
"We really need to focus our efforts and resources on education programs targeting the highest-risk groups. In Los Angeles County, these groups are middle and high school–aged children, minorities, and those of lower socioeconomic status," Dr. Sullins said in an interview.
According to the Centers for Disease Control and Prevention, an estimated 33 million children ride bicycles – for a total of 10 billion hours - each year, and nearly 400 children die as a result of bicycle crashes.
More than 150,000 emergency department visits each year are due to bicycle-related head injuries.
Helmet use has been shown to reduce bicycle-related head injuries by 80%; yet, as the results of this study and others show, the rate of helmet use remains low. The CDC reports that only 15% of adults and 19% of children wear helmets most or all of the time when riding a bicycle.
"We encourage other investigators to perform similar studies to identify [the highest-risk] groups specific to their regions or cities in order to more efficiently direct local injury prevention programs," Dr. Sullins said in the interview.
She reported having no relevant financial disclosures.
AT THE AAP NATIONAL CONFERENCE
Major finding: Only 11.3% of children injured in bicycle accidents were wearing a helmet (35.2%, 7.0%, 6.0%, and 4.2% of white, Asian, black, and Hispanic children, respectively).
Data source: A retrospective study of 1,248 cases of injury related to bicycle accidents during 2006-2011.
Disclosure: Dr. Sullins reported having no relevant financial disclosures.
Biologic Therapy Doesn’t Preclude Vaccinating Psoriasis Patients
LAS VEGAS – Dermatologists, like all physicians, play an important role not just in the treatment of disease, but also in the prevention of disease, and that means vaccinating patients when indicated, according to Dr. Stephen K. Tyring.
The varicella vaccines, including the chicken pox and shingles vaccines, and the human papillomavirus (HPV), hepatitis, and influenza virus vaccines are among those to consider offering to patients when appropriate, Dr. Tyring said at the Skin Disease Education Foundation’s annual Las Vegas dermatology seminar.
Concerns arise, however, when it comes to vaccinating psoriasis patients who are – or will be – treated with biologics.
Ideally, vaccination should be offered before treatment is initiated, he said, but for some patients – such as those who are under the age for which their insurance company will cover a vaccine (age 50 or 60 for the shingles vaccine, depending on the insurance company, for example) – this may not be possible. In those already taking a biologic drug, the question is how to vaccinate safely and without interfering with treatment efficacy, he said.
"What we usually do – and there’s no absolute golden rule – is ask the patient to stop the drug for one to two half-lives of the drug," said Dr. Tyring of the University of Texas, Houston. We suggest stopping one half-life for killed, subunit, or recombinant virus vaccines and stopping for two half-lives for live attenuated virus vaccines.
With the tumor necrosis factor (TNF) inhibitor etanercept (Enbrel), for example, that means skipping one to two weekly injections.
"That’s a little bit more than a half-life, but if a patient is using Enbrel once or twice a week, the next week, instead of injecting the Enbrel, they can just come in and get the shingles vaccine [Zostavax]," he said.
Adalimumab (Humira), another anti-TNF drug, has a longer half-life, so that has to be taken into account. Things get a little more complicated when it comes to patients treated with ustekinumab (Stelera), which has a particularly long half-life, he noted.
"It’s not quite as easy, because it’s not clear how long to wait after Stelera to give a vaccine. Most efficacy is seen in the first month, and when patients come back at 3 months, they often are starting to get a little psoriasis back. Therefore, 2 months following an injection of Stelera is about the right time to get the vaccine; that way you get the minimum immunosuppression and the maximum chance to respond," he said.
Similarly, with other vaccines like the Gardasil HPV vaccine and the hepatitis A and B vaccines that require a series of shots, the biologic should be stopped for a half-life. This will mean skipping biologic dosing multiple times, but in most cases this won’t be problematic, because it typically takes about 3 months for a patient who is clear to experience significant psoriasis recurrence.
"There’s really no danger in skipping," he said.
While some may advocate waiting two half-lives after vaccination, most experts agree that is unnecessary for killed, recombinant, or subunit (for example, injectable influenza) virus vaccines but is advisable for live attenuated virus vaccines like the intranasal influenza virus vaccine or the herpes zoster vaccine Zostavax, he said.
Dr. Tyring also noted during his presentation that in his experience, concerns about increased infection risk in patients taking TNF inhibitors have been unfounded. In fact, treatment appears to provide an unexpected benefit for those who do become infected with herpes zoster: a reduced risk of postherpetic neuralgia, even among older individuals who are generally at particularly high risk.
After noticing this benefit in his own patients, Dr. Tyring asked his colleagues and found that they, too, had noticed a similar pattern. In 2011, he and his colleagues published a retrospective study of 206 patients on TNF inhibitors who developed herpes zoster, and with only two exceptions involving patients on both a TNF inhibitor and methotrexate, patients universally experienced milder symptoms if they developed shingles while on a TNF inhibitor, he said, noting that this is much lower than rates reported in the literature in the general population (J. Med. Virol. 2011;83:2051-5).
SDEF and this news organization are owned by Frontline Medical Communications.
LAS VEGAS – Dermatologists, like all physicians, play an important role not just in the treatment of disease, but also in the prevention of disease, and that means vaccinating patients when indicated, according to Dr. Stephen K. Tyring.
The varicella vaccines, including the chicken pox and shingles vaccines, and the human papillomavirus (HPV), hepatitis, and influenza virus vaccines are among those to consider offering to patients when appropriate, Dr. Tyring said at the Skin Disease Education Foundation’s annual Las Vegas dermatology seminar.
Concerns arise, however, when it comes to vaccinating psoriasis patients who are – or will be – treated with biologics.
Ideally, vaccination should be offered before treatment is initiated, he said, but for some patients – such as those who are under the age for which their insurance company will cover a vaccine (age 50 or 60 for the shingles vaccine, depending on the insurance company, for example) – this may not be possible. In those already taking a biologic drug, the question is how to vaccinate safely and without interfering with treatment efficacy, he said.
"What we usually do – and there’s no absolute golden rule – is ask the patient to stop the drug for one to two half-lives of the drug," said Dr. Tyring of the University of Texas, Houston. We suggest stopping one half-life for killed, subunit, or recombinant virus vaccines and stopping for two half-lives for live attenuated virus vaccines.
With the tumor necrosis factor (TNF) inhibitor etanercept (Enbrel), for example, that means skipping one to two weekly injections.
"That’s a little bit more than a half-life, but if a patient is using Enbrel once or twice a week, the next week, instead of injecting the Enbrel, they can just come in and get the shingles vaccine [Zostavax]," he said.
Adalimumab (Humira), another anti-TNF drug, has a longer half-life, so that has to be taken into account. Things get a little more complicated when it comes to patients treated with ustekinumab (Stelera), which has a particularly long half-life, he noted.
"It’s not quite as easy, because it’s not clear how long to wait after Stelera to give a vaccine. Most efficacy is seen in the first month, and when patients come back at 3 months, they often are starting to get a little psoriasis back. Therefore, 2 months following an injection of Stelera is about the right time to get the vaccine; that way you get the minimum immunosuppression and the maximum chance to respond," he said.
Similarly, with other vaccines like the Gardasil HPV vaccine and the hepatitis A and B vaccines that require a series of shots, the biologic should be stopped for a half-life. This will mean skipping biologic dosing multiple times, but in most cases this won’t be problematic, because it typically takes about 3 months for a patient who is clear to experience significant psoriasis recurrence.
"There’s really no danger in skipping," he said.
While some may advocate waiting two half-lives after vaccination, most experts agree that is unnecessary for killed, recombinant, or subunit (for example, injectable influenza) virus vaccines but is advisable for live attenuated virus vaccines like the intranasal influenza virus vaccine or the herpes zoster vaccine Zostavax, he said.
Dr. Tyring also noted during his presentation that in his experience, concerns about increased infection risk in patients taking TNF inhibitors have been unfounded. In fact, treatment appears to provide an unexpected benefit for those who do become infected with herpes zoster: a reduced risk of postherpetic neuralgia, even among older individuals who are generally at particularly high risk.
After noticing this benefit in his own patients, Dr. Tyring asked his colleagues and found that they, too, had noticed a similar pattern. In 2011, he and his colleagues published a retrospective study of 206 patients on TNF inhibitors who developed herpes zoster, and with only two exceptions involving patients on both a TNF inhibitor and methotrexate, patients universally experienced milder symptoms if they developed shingles while on a TNF inhibitor, he said, noting that this is much lower than rates reported in the literature in the general population (J. Med. Virol. 2011;83:2051-5).
SDEF and this news organization are owned by Frontline Medical Communications.
LAS VEGAS – Dermatologists, like all physicians, play an important role not just in the treatment of disease, but also in the prevention of disease, and that means vaccinating patients when indicated, according to Dr. Stephen K. Tyring.
The varicella vaccines, including the chicken pox and shingles vaccines, and the human papillomavirus (HPV), hepatitis, and influenza virus vaccines are among those to consider offering to patients when appropriate, Dr. Tyring said at the Skin Disease Education Foundation’s annual Las Vegas dermatology seminar.
Concerns arise, however, when it comes to vaccinating psoriasis patients who are – or will be – treated with biologics.
Ideally, vaccination should be offered before treatment is initiated, he said, but for some patients – such as those who are under the age for which their insurance company will cover a vaccine (age 50 or 60 for the shingles vaccine, depending on the insurance company, for example) – this may not be possible. In those already taking a biologic drug, the question is how to vaccinate safely and without interfering with treatment efficacy, he said.
"What we usually do – and there’s no absolute golden rule – is ask the patient to stop the drug for one to two half-lives of the drug," said Dr. Tyring of the University of Texas, Houston. We suggest stopping one half-life for killed, subunit, or recombinant virus vaccines and stopping for two half-lives for live attenuated virus vaccines.
With the tumor necrosis factor (TNF) inhibitor etanercept (Enbrel), for example, that means skipping one to two weekly injections.
"That’s a little bit more than a half-life, but if a patient is using Enbrel once or twice a week, the next week, instead of injecting the Enbrel, they can just come in and get the shingles vaccine [Zostavax]," he said.
Adalimumab (Humira), another anti-TNF drug, has a longer half-life, so that has to be taken into account. Things get a little more complicated when it comes to patients treated with ustekinumab (Stelera), which has a particularly long half-life, he noted.
"It’s not quite as easy, because it’s not clear how long to wait after Stelera to give a vaccine. Most efficacy is seen in the first month, and when patients come back at 3 months, they often are starting to get a little psoriasis back. Therefore, 2 months following an injection of Stelera is about the right time to get the vaccine; that way you get the minimum immunosuppression and the maximum chance to respond," he said.
Similarly, with other vaccines like the Gardasil HPV vaccine and the hepatitis A and B vaccines that require a series of shots, the biologic should be stopped for a half-life. This will mean skipping biologic dosing multiple times, but in most cases this won’t be problematic, because it typically takes about 3 months for a patient who is clear to experience significant psoriasis recurrence.
"There’s really no danger in skipping," he said.
While some may advocate waiting two half-lives after vaccination, most experts agree that is unnecessary for killed, recombinant, or subunit (for example, injectable influenza) virus vaccines but is advisable for live attenuated virus vaccines like the intranasal influenza virus vaccine or the herpes zoster vaccine Zostavax, he said.
Dr. Tyring also noted during his presentation that in his experience, concerns about increased infection risk in patients taking TNF inhibitors have been unfounded. In fact, treatment appears to provide an unexpected benefit for those who do become infected with herpes zoster: a reduced risk of postherpetic neuralgia, even among older individuals who are generally at particularly high risk.
After noticing this benefit in his own patients, Dr. Tyring asked his colleagues and found that they, too, had noticed a similar pattern. In 2011, he and his colleagues published a retrospective study of 206 patients on TNF inhibitors who developed herpes zoster, and with only two exceptions involving patients on both a TNF inhibitor and methotrexate, patients universally experienced milder symptoms if they developed shingles while on a TNF inhibitor, he said, noting that this is much lower than rates reported in the literature in the general population (J. Med. Virol. 2011;83:2051-5).
SDEF and this news organization are owned by Frontline Medical Communications.
EXPERT ANALYSIS FROM SDEF LAS VEGAS DERMATOLOGY SEMINAR
Biologic therapy doesn’t preclude vaccinating psoriasis patients
LAS VEGAS – Dermatologists, like all physicians, play an important role not just in the treatment of disease, but also in the prevention of disease, and that means vaccinating patients when indicated, according to Dr. Stephen K. Tyring.
The varicella vaccines, including the chicken pox and shingles vaccines, and the human papillomavirus (HPV), hepatitis, and influenza virus vaccines are among those to consider offering to patients when appropriate, Dr. Tyring said at the Skin Disease Education Foundation’s annual Las Vegas dermatology seminar.
Concerns arise, however, when it comes to vaccinating psoriasis patients who are – or will be – treated with biologics.
Ideally, vaccination should be offered before treatment is initiated, he said, but for some patients – such as those who are under the age for which their insurance company will cover a vaccine (age 50 or 60 for the shingles vaccine, depending on the insurance company, for example) – this may not be possible. In those already taking a biologic drug, the question is how to vaccinate safely and without interfering with treatment efficacy, he said.
"What we usually do – and there’s no absolute golden rule – is ask the patient to stop the drug for one to two half-lives of the drug," said Dr. Tyring of the University of Texas, Houston. We suggest stopping one half-life for killed, subunit, or recombinant virus vaccines and stopping for two half-lives for live attenuated virus vaccines.
With the tumor necrosis factor (TNF) inhibitor etanercept (Enbrel), for example, that means skipping one to two weekly injections.
"That’s a little bit more than a half-life, but if a patient is using Enbrel once or twice a week, the next week, instead of injecting the Enbrel, they can just come in and get the shingles vaccine [Zostavax]," he said.
Adalimumab (Humira), another anti-TNF drug, has a longer half-life, so that has to be taken into account. Things get a little more complicated when it comes to patients treated with ustekinumab (Stelera), which has a particularly long half-life, he noted.
"It’s not quite as easy, because it’s not clear how long to wait after Stelera to give a vaccine. Most efficacy is seen in the first month, and when patients come back at 3 months, they often are starting to get a little psoriasis back. Therefore, 2 months following an injection of Stelera is about the right time to get the vaccine; that way you get the minimum immunosuppression and the maximum chance to respond," he said.
Similarly, with other vaccines like the Gardasil HPV vaccine and the hepatitis A and B vaccines that require a series of shots, the biologic should be stopped for a half-life. This will mean skipping biologic dosing multiple times, but in most cases this won’t be problematic, because it typically takes about 3 months for a patient who is clear to experience significant psoriasis recurrence.
"There’s really no danger in skipping," he said.
While some may advocate waiting two half-lives after vaccination, most experts agree that is unnecessary for killed, recombinant, or subunit (for example, injectable influenza) virus vaccines but is advisable for live attenuated virus vaccines like the intranasal influenza virus vaccine or the herpes zoster vaccine Zostavax, he said.
Dr. Tyring also noted during his presentation that in his experience, concerns about increased infection risk in patients taking TNF inhibitors have been unfounded. In fact, treatment appears to provide an unexpected benefit for those who do become infected with herpes zoster: a reduced risk of postherpetic neuralgia, even among older individuals who are generally at particularly high risk.
After noticing this benefit in his own patients, Dr. Tyring asked his colleagues and found that they, too, had noticed a similar pattern. In 2011, he and his colleagues published a retrospective study of 206 patients on TNF inhibitors who developed herpes zoster, and with only two exceptions involving patients on both a TNF inhibitor and methotrexate, patients universally experienced milder symptoms if they developed shingles while on a TNF inhibitor, he said, noting that this is much lower than rates reported in the literature in the general population (J. Med. Virol. 2011;83:2051-5).
SDEF and this news organization are owned by Frontline Medical Communications.
LAS VEGAS – Dermatologists, like all physicians, play an important role not just in the treatment of disease, but also in the prevention of disease, and that means vaccinating patients when indicated, according to Dr. Stephen K. Tyring.
The varicella vaccines, including the chicken pox and shingles vaccines, and the human papillomavirus (HPV), hepatitis, and influenza virus vaccines are among those to consider offering to patients when appropriate, Dr. Tyring said at the Skin Disease Education Foundation’s annual Las Vegas dermatology seminar.
Concerns arise, however, when it comes to vaccinating psoriasis patients who are – or will be – treated with biologics.
Ideally, vaccination should be offered before treatment is initiated, he said, but for some patients – such as those who are under the age for which their insurance company will cover a vaccine (age 50 or 60 for the shingles vaccine, depending on the insurance company, for example) – this may not be possible. In those already taking a biologic drug, the question is how to vaccinate safely and without interfering with treatment efficacy, he said.
"What we usually do – and there’s no absolute golden rule – is ask the patient to stop the drug for one to two half-lives of the drug," said Dr. Tyring of the University of Texas, Houston. We suggest stopping one half-life for killed, subunit, or recombinant virus vaccines and stopping for two half-lives for live attenuated virus vaccines.
With the tumor necrosis factor (TNF) inhibitor etanercept (Enbrel), for example, that means skipping one to two weekly injections.
"That’s a little bit more than a half-life, but if a patient is using Enbrel once or twice a week, the next week, instead of injecting the Enbrel, they can just come in and get the shingles vaccine [Zostavax]," he said.
Adalimumab (Humira), another anti-TNF drug, has a longer half-life, so that has to be taken into account. Things get a little more complicated when it comes to patients treated with ustekinumab (Stelera), which has a particularly long half-life, he noted.
"It’s not quite as easy, because it’s not clear how long to wait after Stelera to give a vaccine. Most efficacy is seen in the first month, and when patients come back at 3 months, they often are starting to get a little psoriasis back. Therefore, 2 months following an injection of Stelera is about the right time to get the vaccine; that way you get the minimum immunosuppression and the maximum chance to respond," he said.
Similarly, with other vaccines like the Gardasil HPV vaccine and the hepatitis A and B vaccines that require a series of shots, the biologic should be stopped for a half-life. This will mean skipping biologic dosing multiple times, but in most cases this won’t be problematic, because it typically takes about 3 months for a patient who is clear to experience significant psoriasis recurrence.
"There’s really no danger in skipping," he said.
While some may advocate waiting two half-lives after vaccination, most experts agree that is unnecessary for killed, recombinant, or subunit (for example, injectable influenza) virus vaccines but is advisable for live attenuated virus vaccines like the intranasal influenza virus vaccine or the herpes zoster vaccine Zostavax, he said.
Dr. Tyring also noted during his presentation that in his experience, concerns about increased infection risk in patients taking TNF inhibitors have been unfounded. In fact, treatment appears to provide an unexpected benefit for those who do become infected with herpes zoster: a reduced risk of postherpetic neuralgia, even among older individuals who are generally at particularly high risk.
After noticing this benefit in his own patients, Dr. Tyring asked his colleagues and found that they, too, had noticed a similar pattern. In 2011, he and his colleagues published a retrospective study of 206 patients on TNF inhibitors who developed herpes zoster, and with only two exceptions involving patients on both a TNF inhibitor and methotrexate, patients universally experienced milder symptoms if they developed shingles while on a TNF inhibitor, he said, noting that this is much lower than rates reported in the literature in the general population (J. Med. Virol. 2011;83:2051-5).
SDEF and this news organization are owned by Frontline Medical Communications.
LAS VEGAS – Dermatologists, like all physicians, play an important role not just in the treatment of disease, but also in the prevention of disease, and that means vaccinating patients when indicated, according to Dr. Stephen K. Tyring.
The varicella vaccines, including the chicken pox and shingles vaccines, and the human papillomavirus (HPV), hepatitis, and influenza virus vaccines are among those to consider offering to patients when appropriate, Dr. Tyring said at the Skin Disease Education Foundation’s annual Las Vegas dermatology seminar.
Concerns arise, however, when it comes to vaccinating psoriasis patients who are – or will be – treated with biologics.
Ideally, vaccination should be offered before treatment is initiated, he said, but for some patients – such as those who are under the age for which their insurance company will cover a vaccine (age 50 or 60 for the shingles vaccine, depending on the insurance company, for example) – this may not be possible. In those already taking a biologic drug, the question is how to vaccinate safely and without interfering with treatment efficacy, he said.
"What we usually do – and there’s no absolute golden rule – is ask the patient to stop the drug for one to two half-lives of the drug," said Dr. Tyring of the University of Texas, Houston. We suggest stopping one half-life for killed, subunit, or recombinant virus vaccines and stopping for two half-lives for live attenuated virus vaccines.
With the tumor necrosis factor (TNF) inhibitor etanercept (Enbrel), for example, that means skipping one to two weekly injections.
"That’s a little bit more than a half-life, but if a patient is using Enbrel once or twice a week, the next week, instead of injecting the Enbrel, they can just come in and get the shingles vaccine [Zostavax]," he said.
Adalimumab (Humira), another anti-TNF drug, has a longer half-life, so that has to be taken into account. Things get a little more complicated when it comes to patients treated with ustekinumab (Stelera), which has a particularly long half-life, he noted.
"It’s not quite as easy, because it’s not clear how long to wait after Stelera to give a vaccine. Most efficacy is seen in the first month, and when patients come back at 3 months, they often are starting to get a little psoriasis back. Therefore, 2 months following an injection of Stelera is about the right time to get the vaccine; that way you get the minimum immunosuppression and the maximum chance to respond," he said.
Similarly, with other vaccines like the Gardasil HPV vaccine and the hepatitis A and B vaccines that require a series of shots, the biologic should be stopped for a half-life. This will mean skipping biologic dosing multiple times, but in most cases this won’t be problematic, because it typically takes about 3 months for a patient who is clear to experience significant psoriasis recurrence.
"There’s really no danger in skipping," he said.
While some may advocate waiting two half-lives after vaccination, most experts agree that is unnecessary for killed, recombinant, or subunit (for example, injectable influenza) virus vaccines but is advisable for live attenuated virus vaccines like the intranasal influenza virus vaccine or the herpes zoster vaccine Zostavax, he said.
Dr. Tyring also noted during his presentation that in his experience, concerns about increased infection risk in patients taking TNF inhibitors have been unfounded. In fact, treatment appears to provide an unexpected benefit for those who do become infected with herpes zoster: a reduced risk of postherpetic neuralgia, even among older individuals who are generally at particularly high risk.
After noticing this benefit in his own patients, Dr. Tyring asked his colleagues and found that they, too, had noticed a similar pattern. In 2011, he and his colleagues published a retrospective study of 206 patients on TNF inhibitors who developed herpes zoster, and with only two exceptions involving patients on both a TNF inhibitor and methotrexate, patients universally experienced milder symptoms if they developed shingles while on a TNF inhibitor, he said, noting that this is much lower than rates reported in the literature in the general population (J. Med. Virol. 2011;83:2051-5).
SDEF and this news organization are owned by Frontline Medical Communications.
EXPERT ANALYSIS FROM SDEF LAS VEGAS DERMATOLOGY SEMINAR
Increasing proportion of musculoskeletal infections involve MRSA
ORLANDO – The proportion of pediatric musculoskeletal infections involving methicillin-resistant Staphylococcus aureus vs. methicillin-sensitive S. aureus has increased dramatically over the past decade, according to a retrospective review of cases.
Between 2001 and 2010, 148 patients at the Children’s Hospital of Philadelphia presented with acute musculoskeletal S. aureus infection, and overall, 37 of those involved methicillin-resistant S. aureus (MRSA), Eric Sarkissian reported at the annual meeting of the American Academy of Pediatrics conference.
The proportion of musculoskeletal cases involving MRSA increased from 12% in 2001-2002 to about 35% in 2010, said Mr. Sarkissian, a 4th-year medical student at Drexel University, Philadelphia.
"Furthermore, we found that MRSA infections were associated with a significantly more complicated hospital stay," Mr. Sarkissian said.
MRSA and methicillin-sensitive S. aureus (MSSA) patients were undergoing magnetic resonance imaging at similar rates, but the average duration of hospitalization was longer for the MRSA patients (13 vs. 8 days), and more MRSA patients required multiple surgical procedures (38% vs. 15%), he said.
In addition, mean presenting C-reactive protein levels were higher in the MRSA vs. MSSA patients (14.7 mg/L vs. 9.8 mg/L), as were infection-related complications, including deep vein thrombosis, septic emboli, septic shock, recurrent infection, and/or avascular necrosis (22% vs. 6%).
MRSA patients also were more often admitted to the ICU for further treatment.
Patients included in this series – the largest known case series of children and adolescents presenting with culture-positive S. aureus osteomyelitis and/or septic arthritis – were consecutive patients with positive cultures of blood, bone, or joint aspirate. Those with postoperative and chronic infections were excluded in an effort to minimize bias caused by nosocomial infections, Mr. Sarkissian noted.
The findings support the ongoing concern that MRSA is evolving and becoming more virulent and invasive over time, compared with MSSA infections. In addition, the findings underscore the need for prompt recognition and aggressive treatment of MRSA musculoskeletal infections, as early recognition is paramount for avoiding sequelae and improving patient outcomes.
"A high index of suspicion is still necessary in the setting of musculoskeletal infections in pediatric patients. Multidisciplinary care provides the most successful opportunity for having improved patient outcomes, and this requires employing broad spectrum antibiotic coverage, using aggressive surgical management, and having an awareness of potential complications," Mr. Sarkissian said.
While clinical prediction models have been developed to help in detecting MRSA infections, outcomes using the models have varied geographically, suggesting that there are unknown regional differences among MRSA cases. It remains to be seen whether available models will be useful for identifying MRSA at presentation, he said.
Mr. Sarkissian reported having no disclosures.
ORLANDO – The proportion of pediatric musculoskeletal infections involving methicillin-resistant Staphylococcus aureus vs. methicillin-sensitive S. aureus has increased dramatically over the past decade, according to a retrospective review of cases.
Between 2001 and 2010, 148 patients at the Children’s Hospital of Philadelphia presented with acute musculoskeletal S. aureus infection, and overall, 37 of those involved methicillin-resistant S. aureus (MRSA), Eric Sarkissian reported at the annual meeting of the American Academy of Pediatrics conference.
The proportion of musculoskeletal cases involving MRSA increased from 12% in 2001-2002 to about 35% in 2010, said Mr. Sarkissian, a 4th-year medical student at Drexel University, Philadelphia.
"Furthermore, we found that MRSA infections were associated with a significantly more complicated hospital stay," Mr. Sarkissian said.
MRSA and methicillin-sensitive S. aureus (MSSA) patients were undergoing magnetic resonance imaging at similar rates, but the average duration of hospitalization was longer for the MRSA patients (13 vs. 8 days), and more MRSA patients required multiple surgical procedures (38% vs. 15%), he said.
In addition, mean presenting C-reactive protein levels were higher in the MRSA vs. MSSA patients (14.7 mg/L vs. 9.8 mg/L), as were infection-related complications, including deep vein thrombosis, septic emboli, septic shock, recurrent infection, and/or avascular necrosis (22% vs. 6%).
MRSA patients also were more often admitted to the ICU for further treatment.
Patients included in this series – the largest known case series of children and adolescents presenting with culture-positive S. aureus osteomyelitis and/or septic arthritis – were consecutive patients with positive cultures of blood, bone, or joint aspirate. Those with postoperative and chronic infections were excluded in an effort to minimize bias caused by nosocomial infections, Mr. Sarkissian noted.
The findings support the ongoing concern that MRSA is evolving and becoming more virulent and invasive over time, compared with MSSA infections. In addition, the findings underscore the need for prompt recognition and aggressive treatment of MRSA musculoskeletal infections, as early recognition is paramount for avoiding sequelae and improving patient outcomes.
"A high index of suspicion is still necessary in the setting of musculoskeletal infections in pediatric patients. Multidisciplinary care provides the most successful opportunity for having improved patient outcomes, and this requires employing broad spectrum antibiotic coverage, using aggressive surgical management, and having an awareness of potential complications," Mr. Sarkissian said.
While clinical prediction models have been developed to help in detecting MRSA infections, outcomes using the models have varied geographically, suggesting that there are unknown regional differences among MRSA cases. It remains to be seen whether available models will be useful for identifying MRSA at presentation, he said.
Mr. Sarkissian reported having no disclosures.
ORLANDO – The proportion of pediatric musculoskeletal infections involving methicillin-resistant Staphylococcus aureus vs. methicillin-sensitive S. aureus has increased dramatically over the past decade, according to a retrospective review of cases.
Between 2001 and 2010, 148 patients at the Children’s Hospital of Philadelphia presented with acute musculoskeletal S. aureus infection, and overall, 37 of those involved methicillin-resistant S. aureus (MRSA), Eric Sarkissian reported at the annual meeting of the American Academy of Pediatrics conference.
The proportion of musculoskeletal cases involving MRSA increased from 12% in 2001-2002 to about 35% in 2010, said Mr. Sarkissian, a 4th-year medical student at Drexel University, Philadelphia.
"Furthermore, we found that MRSA infections were associated with a significantly more complicated hospital stay," Mr. Sarkissian said.
MRSA and methicillin-sensitive S. aureus (MSSA) patients were undergoing magnetic resonance imaging at similar rates, but the average duration of hospitalization was longer for the MRSA patients (13 vs. 8 days), and more MRSA patients required multiple surgical procedures (38% vs. 15%), he said.
In addition, mean presenting C-reactive protein levels were higher in the MRSA vs. MSSA patients (14.7 mg/L vs. 9.8 mg/L), as were infection-related complications, including deep vein thrombosis, septic emboli, septic shock, recurrent infection, and/or avascular necrosis (22% vs. 6%).
MRSA patients also were more often admitted to the ICU for further treatment.
Patients included in this series – the largest known case series of children and adolescents presenting with culture-positive S. aureus osteomyelitis and/or septic arthritis – were consecutive patients with positive cultures of blood, bone, or joint aspirate. Those with postoperative and chronic infections were excluded in an effort to minimize bias caused by nosocomial infections, Mr. Sarkissian noted.
The findings support the ongoing concern that MRSA is evolving and becoming more virulent and invasive over time, compared with MSSA infections. In addition, the findings underscore the need for prompt recognition and aggressive treatment of MRSA musculoskeletal infections, as early recognition is paramount for avoiding sequelae and improving patient outcomes.
"A high index of suspicion is still necessary in the setting of musculoskeletal infections in pediatric patients. Multidisciplinary care provides the most successful opportunity for having improved patient outcomes, and this requires employing broad spectrum antibiotic coverage, using aggressive surgical management, and having an awareness of potential complications," Mr. Sarkissian said.
While clinical prediction models have been developed to help in detecting MRSA infections, outcomes using the models have varied geographically, suggesting that there are unknown regional differences among MRSA cases. It remains to be seen whether available models will be useful for identifying MRSA at presentation, he said.
Mr. Sarkissian reported having no disclosures.
AT THE AAP NATIONAL CONFERENCE
Major finding: The proportion of musculoskeletal infection cases involving MRSA vs. MSSA increased from 12% to 35% between 2001 and 2010.
Data source: A retrospective study of 148 consecutive cases.
Disclosures: Mr. Sarkissian reported having no disclosures.