User login
Sharon Worcester is an award-winning medical journalist for MDedge News. She has been with the company since 1996, first as the Southeast Bureau Chief (1996-2009) when the company was known as International Medical News Group, then as a freelance writer (2010-2015) before returning as a reporter in 2015. She previously worked as a daily newspaper reporter covering health and local government. Sharon currently reports primarily on oncology and hematology. She has a BA from Eckerd College and an MA in Mass Communication/Print Journalism from the University of Florida. Connect with her via LinkedIn and follow her on twitter @SW_MedReporter.
Facial emotion recognition impaired early in schizophrenia, stable across disease course
Deficits in facial emotion recognition are apparent early in the course of schizophrenia but remain stable throughout the course of the disease, findings from a cross-sectional study suggest.
In the study of 43 patients with putative prodromal syndrome, 50 patients with a first episode of schizophrenia with very recent onset, 44 patients with multi-episode schizophrenia, and 86 unaffected healthy control subjects, deficits in the recognition of sadness and disgust were apparent in prodromal individuals, and deficits in recognition of all negative emotions were apparent in both first- and multi-episode patients, Dr. Anna Comparelli of Sapienza University of Rome, and her colleagues reported online in Schizophrenia Research.
Specifically, the patients with putative prodromal syndrome (the ultra-high-risk group) performed significantly worse than did healthy control subjects on recognition of sadness and disgust; the first-episode patients performed worse than did healthy controls on recognition of sadness, disgust, anger, and fear; and the multi-episode patients performed worse than did healthy controls on sadness, disgust, anger, fear, and happiness.
After adjustment for sociodemographic and clinical variables that differed significantly between the groups, and after correction for age, sex, and Positive and Negative Syndrome Scale (PANSS) positive and total scores, the significant differences between the groups were confirmed (Schizophrenia Res. 2012 Dec. 6 [doi: 10.1016/j.schres.2012.11.005]).
Patients in the ultra-high-risk group did worse than did healthy controls in recognizing sadness and disgust (P < .001), and those with first-episode psychosis performed worse than did healthy control subjects for sadness, disgust, anger, and fear (all P < .001). Meanwhile, multi-episode patients did worse than did healthy control subjects on sadness, disgust, anger, fear (P < .001), and happiness (P < .05).
The findings support those from previous studies demonstrating that emotion recognition deficit is specific for negative emotions in both first- and multi-episode schizophrenia patients, and they are among the first to compare deficits in emotion recognition in ultra-high-risk and chronic patients, the investigators said.
"Importantly, we did not see any evidence of progression or improvement over the three phases of illness. In fact, a new finding of our study is that, in this cross-sectional cohort, the deficit in facial emotion recognition is stable over the course of illness, not differing between prodromal, [first-episode schizophrenia], and [multi-episode schizophrenia]," they added.
This fits the pattern of a vulnerability indicator, as opposed to an indicator of severity or chronicity, and suggests emotion processing dysfunction as a possible endophenotype related to genetic risk, they said.
"Further studies on social cognition addressing its trend to impair, improve, or remain stable across the course of illness and whether there is any relationship with the progression of other cognitive domains are needed," they added.
Though limited by the fact that a possible role of antipsychotic drugs in emotion recognition was not ruled out and by the cross-sectional study design, this study nonetheless represents "a step toward better elucidation of the possible role of emotion recognition impairment in schizophrenia following its prodromal manifestations," the investigators said.
"The understanding of the interactions between neurocognition, social cognition, and social functioning in schizophrenia should be a goal for future research in the field of early intervention in psychosis. In fact, complex neurofunctional and psychological mechanisms underlying social cognition and functioning may highlight correct strategies for prevention and intervention."
Dr. Comparelli reported having no disclosures.
Deficits in facial emotion recognition are apparent early in the course of schizophrenia but remain stable throughout the course of the disease, findings from a cross-sectional study suggest.
In the study of 43 patients with putative prodromal syndrome, 50 patients with a first episode of schizophrenia with very recent onset, 44 patients with multi-episode schizophrenia, and 86 unaffected healthy control subjects, deficits in the recognition of sadness and disgust were apparent in prodromal individuals, and deficits in recognition of all negative emotions were apparent in both first- and multi-episode patients, Dr. Anna Comparelli of Sapienza University of Rome, and her colleagues reported online in Schizophrenia Research.
Specifically, the patients with putative prodromal syndrome (the ultra-high-risk group) performed significantly worse than did healthy control subjects on recognition of sadness and disgust; the first-episode patients performed worse than did healthy controls on recognition of sadness, disgust, anger, and fear; and the multi-episode patients performed worse than did healthy controls on sadness, disgust, anger, fear, and happiness.
After adjustment for sociodemographic and clinical variables that differed significantly between the groups, and after correction for age, sex, and Positive and Negative Syndrome Scale (PANSS) positive and total scores, the significant differences between the groups were confirmed (Schizophrenia Res. 2012 Dec. 6 [doi: 10.1016/j.schres.2012.11.005]).
Patients in the ultra-high-risk group did worse than did healthy controls in recognizing sadness and disgust (P < .001), and those with first-episode psychosis performed worse than did healthy control subjects for sadness, disgust, anger, and fear (all P < .001). Meanwhile, multi-episode patients did worse than did healthy control subjects on sadness, disgust, anger, fear (P < .001), and happiness (P < .05).
The findings support those from previous studies demonstrating that emotion recognition deficit is specific for negative emotions in both first- and multi-episode schizophrenia patients, and they are among the first to compare deficits in emotion recognition in ultra-high-risk and chronic patients, the investigators said.
"Importantly, we did not see any evidence of progression or improvement over the three phases of illness. In fact, a new finding of our study is that, in this cross-sectional cohort, the deficit in facial emotion recognition is stable over the course of illness, not differing between prodromal, [first-episode schizophrenia], and [multi-episode schizophrenia]," they added.
This fits the pattern of a vulnerability indicator, as opposed to an indicator of severity or chronicity, and suggests emotion processing dysfunction as a possible endophenotype related to genetic risk, they said.
"Further studies on social cognition addressing its trend to impair, improve, or remain stable across the course of illness and whether there is any relationship with the progression of other cognitive domains are needed," they added.
Though limited by the fact that a possible role of antipsychotic drugs in emotion recognition was not ruled out and by the cross-sectional study design, this study nonetheless represents "a step toward better elucidation of the possible role of emotion recognition impairment in schizophrenia following its prodromal manifestations," the investigators said.
"The understanding of the interactions between neurocognition, social cognition, and social functioning in schizophrenia should be a goal for future research in the field of early intervention in psychosis. In fact, complex neurofunctional and psychological mechanisms underlying social cognition and functioning may highlight correct strategies for prevention and intervention."
Dr. Comparelli reported having no disclosures.
Deficits in facial emotion recognition are apparent early in the course of schizophrenia but remain stable throughout the course of the disease, findings from a cross-sectional study suggest.
In the study of 43 patients with putative prodromal syndrome, 50 patients with a first episode of schizophrenia with very recent onset, 44 patients with multi-episode schizophrenia, and 86 unaffected healthy control subjects, deficits in the recognition of sadness and disgust were apparent in prodromal individuals, and deficits in recognition of all negative emotions were apparent in both first- and multi-episode patients, Dr. Anna Comparelli of Sapienza University of Rome, and her colleagues reported online in Schizophrenia Research.
Specifically, the patients with putative prodromal syndrome (the ultra-high-risk group) performed significantly worse than did healthy control subjects on recognition of sadness and disgust; the first-episode patients performed worse than did healthy controls on recognition of sadness, disgust, anger, and fear; and the multi-episode patients performed worse than did healthy controls on sadness, disgust, anger, fear, and happiness.
After adjustment for sociodemographic and clinical variables that differed significantly between the groups, and after correction for age, sex, and Positive and Negative Syndrome Scale (PANSS) positive and total scores, the significant differences between the groups were confirmed (Schizophrenia Res. 2012 Dec. 6 [doi: 10.1016/j.schres.2012.11.005]).
Patients in the ultra-high-risk group did worse than did healthy controls in recognizing sadness and disgust (P < .001), and those with first-episode psychosis performed worse than did healthy control subjects for sadness, disgust, anger, and fear (all P < .001). Meanwhile, multi-episode patients did worse than did healthy control subjects on sadness, disgust, anger, fear (P < .001), and happiness (P < .05).
The findings support those from previous studies demonstrating that emotion recognition deficit is specific for negative emotions in both first- and multi-episode schizophrenia patients, and they are among the first to compare deficits in emotion recognition in ultra-high-risk and chronic patients, the investigators said.
"Importantly, we did not see any evidence of progression or improvement over the three phases of illness. In fact, a new finding of our study is that, in this cross-sectional cohort, the deficit in facial emotion recognition is stable over the course of illness, not differing between prodromal, [first-episode schizophrenia], and [multi-episode schizophrenia]," they added.
This fits the pattern of a vulnerability indicator, as opposed to an indicator of severity or chronicity, and suggests emotion processing dysfunction as a possible endophenotype related to genetic risk, they said.
"Further studies on social cognition addressing its trend to impair, improve, or remain stable across the course of illness and whether there is any relationship with the progression of other cognitive domains are needed," they added.
Though limited by the fact that a possible role of antipsychotic drugs in emotion recognition was not ruled out and by the cross-sectional study design, this study nonetheless represents "a step toward better elucidation of the possible role of emotion recognition impairment in schizophrenia following its prodromal manifestations," the investigators said.
"The understanding of the interactions between neurocognition, social cognition, and social functioning in schizophrenia should be a goal for future research in the field of early intervention in psychosis. In fact, complex neurofunctional and psychological mechanisms underlying social cognition and functioning may highlight correct strategies for prevention and intervention."
Dr. Comparelli reported having no disclosures.
FROM SCHIZOPHRENIA RESEARCH
Major Finding: Patients in the ultra-high-risk group did worse than did healthy controls in recognizing sadness and disgust (P < .001), and those with first-episode psychosis performed worse than did healthy control subjects for sadness, disgust, anger, and fear (all P < .001). Meanwhile, multi-episode patients did worse than did healthy control subjects on sadness, disgust, anger, fear (P < .001), and happiness (P < .05).
Data Source: A cross-sectional study of 137 patients with psychiatric illness and 86 controls.
Disclosures: Dr. Comparelli reported having no disclosures.
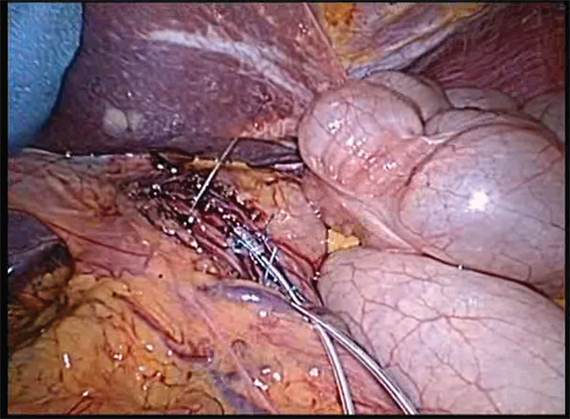
Lower esophageal electrical stimulation therapy targets GERD
Electrical stimulation of the lower esophageal sphincter using an implanted device shows promise for the treatment of gastroesophageal reflux, according to findings from three recent studies.
In one open-label pilot extension study, 77% of 23 patients treated with EndoStim’s Lower Esophageal Sphincter (LES) stimulation system reported normalization of (or at least a 50% reduction in) distal esophageal acid exposure at 12 months’ follow-up, Dr. Edy Soffer reported in October at the annual meeting of the American College of Gastroenterology.
The patients also experienced significant improvement in their median GERD-Health Related Quality of Life (GERD-HRQL) score while implanted with the LES stimulation system (LES-EST), compared with their score while on proton pump inhibitor (PPI) therapy (increase of 9 vs. 2 points) and while off PPI therapy (increase of 23.5 vs. 2), said Dr. Soffer, professor of clinical medicine and director of the GI motility program at the University of Southern California, Los Angeles.
All but one patient reported cessation of regular PPI use, and no implantation- or stimulation-related unanticipated adverse events or "untoward sensation" due to stimulation occurred during follow-up; nor was swallowing function as assessed by manometry affected.
Patients included in the study were GERD patients with a mean age of 53 years who were at least partially responsive to PPI therapy, and who had off-PPI GERD-HRQL scores of at least 20, as well as hiatal hernia.
The findings indicate that LES-EST, which uses low-energy electrical pulses to strengthen a weak or dysfunctional lower esophageal sphincter, is safe and effective for long-term use, he said.
In an interview, Dr. Soffer said that the findings have held up at 18 months of follow-up.
"The results are comparable to those observed at 12 months with regard to control of symptoms, and with near elimination of the use of PPIs," he said, noting that the safety profile remains excellent, with no new adverse event reported beyond those seen at 12 months’ follow-up.
Physiological studies such as esophageal pH will be conducted at 24 months, he said.
In a related study presented in a poster at the meeting, Michael Crowell, Ph.D., looked more closely at the effects of LES-EST on both distal and proximal esophageal acid exposure in a post hoc analysis.
In 19 patients with a median age of 54 years, LES-EST was associated with normalization of total and upright proximal esophageal acid exposure, which improved from 0.4% and 0.6%, respectively, at baseline to 0% at 12 months’ follow-up. Supine esophageal acid exposure was unchanged from 0% at baseline, said Dr. Crowell of the Mayo Clinic, Scottsdale, Ariz.
This was true even among seven patients with abnormal proximal esophageal pH, whose total, upright, and supine proximal esophageal acid exposure values at baseline were 1.7%, 2.9%, and 0.3%, respectively. Distal esophageal pH improved from 10.2% to 3.6% for the entire cohort, and from 9.3% to 3.4% in those seven patients.
Patients in this study had GERD that was at least partially responsive to PPIs, a hiatal hernia of less than 3 cm, and esophagitis of less than Los Angeles Classification grade D. Electrical stimulation was administered for 220 microseconds at 20 Hz and 5-8 mA in 6-12 30-minute sessions starting on day 1 after implantation.
No gastrointestinal side effects occurred in the patients, nor were there any device- or procedure-related adverse events.
LES-EST may be effective in treating proximal GERD, Dr. Crowell concluded.
In an interview, he added that the findings are important, particularly for the one-third of patients who remain symptomatic on PPIs.
"LES dysfunction is the root cause of GERD. Medications such as PPIs block stomach acid production, but do not address the pathophysiology of GERD. Hence, more than a third of patients continue to suffer from symptoms despite maximal medical therapy," he said.
Additionally, there are significant safety concerns with long-term acid suppression, he noted.
LES-EST, on the other hand, addresses the root cause of GERD by improving LES pressure and function, thereby restoring the LES physiology and its barrier function, preventing reflux of gastric acid into the esophagus.
"LES stimulation does not affect normal LES relaxation, allowing for the patient to swallow normally, and has no side effects," he said.
In a third, unrelated study also reported in a poster at the meeting, LES-EST was similarly effective.
Of 11 patients treated with EndoStim’s LES stimulation system as part of an international multicenter study, 10 were able to discontinue PPI therapy at 3-6 months of follow-up, according to Dr. Arjan J. Bredenoord of Academic Medical Center Utrecht, Rotterdam.
Those 10 patients experienced significant improvements in median GERD-HRQL scores from 32 (off PPIs) and 22 (on PPIs) to 9 (on LES-EST) at 3 months, and the scores remained stable at 9 points in 3 patients who were followed for 6 months.
Median esophageal acid exposure improved from 11.8% at baseline to 7.8% at 3 months and 7.3% at 6 months, Dr. Bredenoord said.
The remaining patient suffered a small bowl trocar perforation during implantation of the device and underwent successful repair. An additional 13 adverse events, including 1 serious adverse event, were reported in 4 patients. Nine of these were related to the device or procedure, including seven complaints of pain at the implant site and one case of postoperative nausea.
The treatment was safe, with no GI or cardiac side effects, Dr. Bredenoord concluded, noting that long-term safety and efficacy results in a larger group of patients are currently being analyzed.
In an interview, Dr. Bredenoord noted that the findings are among the first in patients outside South America, where the earliest trials of the EndoStim LES stimulation system were conducted.
"The data confirm the favorable outcome of the patients in Chile, and show that both symptoms and reflux are reduced in European patients as well," he said.
However, the experience remains limited, and additional study comparing the device with other treatments and/or with placebo is needed, as are longer-term outcomes data.
"I think that although these results suggest this is a promising treatment, it would be best to treat patients only in trials" at this point, he said. Because trial participants have been carefully selected, it remains unclear whether this treatment is suitable for the entire GERD population, he added.
Dr. Soffer agreed, and said that if the results are reproduced in additional studies with a larger number of patients, the intervention will provide an alternative therapy for GERD patients who are not satisfied with PPIs or who have concerns about side effects and the chronic use of treatment, and who also have concerns about the established surgical treatment for GERD.
"The importance of this intervention is in providing a bridge between the currently established drug therapy for GERD [PPIs] and the established surgical therapy [fundoplication]. While PPIs are effective in a substantial number of GERD patients, they do not correct the underlying pathophysiology of GERD, resulting in a substantial number of patients who remain symptomatic in spite of therapy," he said.
These patients can be offered fundoplication, which is effective in expert hands, but the surgery has side effects and is performed less and less often, he added.
"Consequently, there is a search for a bridge intervention, endoscopic or surgical, for the treatment of GERD," he said.
LES-EST appears to have the potential to be such a bridge intervention.
"The procedure is simple and nondisruptive, and addresses pathophysiology. The safety profile thus far is excellent, and the effect on esophageal acid exposure, symptoms, and PPI use is sustained over a period of 12-18 moths. Furthermore, the treatment can be optimized to individual needs by adjusting delivery of stimulation to coincide with periods when symptoms and acid reflux are detected," he said.
All three of these studies presented at the meeting were supported by EndoStim BV. Dr. Soffer disclosed that he has stockholder/ownership interest in the company. Dr. Crowell disclosed that he has served as a consultant to the company. Dr. Bredenoord reported receiving grant and/or research support from the company.
Gastroesophageal reflux disease is one of the most common chronic gastrointestinal disorders. The mainstay of medical therapy is to suppress gastric acid secretion with medications such as PPIs. An alternative approach to acid suppression is modulation of the antireflux barrier, composed of the lower esophageal sphincter (LES) and the crural diaphragm. Surgical fundoplication is a well-established method to augment the function of the antireflux barrier. Fundoplication has proven effective in high-quality trials, but it also has well-documented side effects such as dysphagia, bloating, and diarrhea in a subset of patients.
Additional means of enhancing the function of the antireflux barrier include pharmacological inhibition of transient LES relaxations (TLESR) with various agents and several endoscopic antireflux procedures. Unfortunately, the use of TLESR inhibitors and endoscopic procedures for GERD is very limited due to side effects and adverse events, along with insufficient efficacy.
Electrical stimulation of the LES has been previously shown to increase LES resting tone in an animal model (Am. J. Physiol. Gastrointest. Liver Physiol. 2008;295:G389-94). More recently, in a 6-month, open-label trial, electrical stimulation of the LES was found to reduce or eliminate PPI use and to improve symptoms and 24-hour esophageal pH parameters in GERD patients who were at least partially responsive to PPIs (Surg. Endosc. 2012 Oct. 17 [doi: 10.1007/s00464-012-2561-4]).
During the recent American College of Gastroenterology meeting, 1-year data for the open-label trial mentioned above was presented by Dr. Soffer, Dr. Crowell, and their collaborators, showing that improvement in symptoms, PPI use, and distal esophageal acid exposure persisted at 12 months with minimal side effects or adverse events.
Preliminary results of an international multicenter trial of LES electrical stimulation for refractory GERD were also presented at the meeting by Dr. Bredenoord and his colleagues. They found that LES electrical stimulation improved symptoms, PPI use, and esophageal acid exposure in this group of patients, but the preliminary number of patients was small and follow-up was mostly limited to 3 months. Importantly, they did report some adverse events.
These studies provide additional information to suggest that electrical stimulation of the LES may be an effective treatment for GERD. While the available data is compelling, more work will be required to evaluate the durability of the procedure, assess long-term safety and side effects, study the effects of stimulation on esophageal sensation, and define which GERD patients are best suited for this treatment. This will be ideally accomplished by randomized controlled trials that will compare electrical stimulation of the LES to the well-established pharmacological and surgical approaches currently used to treat GERD.
Marcelo F. Vela, M.D., is an associate professor of medicine and director of gastrointestinal motility at Baylor College of Medicine and the Michael E. DeBakey VA Medical Center, both in Houston. He is a member of an advisory panel for Given Imaging.
Gastroesophageal reflux disease is one of the most common chronic gastrointestinal disorders. The mainstay of medical therapy is to suppress gastric acid secretion with medications such as PPIs. An alternative approach to acid suppression is modulation of the antireflux barrier, composed of the lower esophageal sphincter (LES) and the crural diaphragm. Surgical fundoplication is a well-established method to augment the function of the antireflux barrier. Fundoplication has proven effective in high-quality trials, but it also has well-documented side effects such as dysphagia, bloating, and diarrhea in a subset of patients.
Additional means of enhancing the function of the antireflux barrier include pharmacological inhibition of transient LES relaxations (TLESR) with various agents and several endoscopic antireflux procedures. Unfortunately, the use of TLESR inhibitors and endoscopic procedures for GERD is very limited due to side effects and adverse events, along with insufficient efficacy.
Electrical stimulation of the LES has been previously shown to increase LES resting tone in an animal model (Am. J. Physiol. Gastrointest. Liver Physiol. 2008;295:G389-94). More recently, in a 6-month, open-label trial, electrical stimulation of the LES was found to reduce or eliminate PPI use and to improve symptoms and 24-hour esophageal pH parameters in GERD patients who were at least partially responsive to PPIs (Surg. Endosc. 2012 Oct. 17 [doi: 10.1007/s00464-012-2561-4]).
During the recent American College of Gastroenterology meeting, 1-year data for the open-label trial mentioned above was presented by Dr. Soffer, Dr. Crowell, and their collaborators, showing that improvement in symptoms, PPI use, and distal esophageal acid exposure persisted at 12 months with minimal side effects or adverse events.
Preliminary results of an international multicenter trial of LES electrical stimulation for refractory GERD were also presented at the meeting by Dr. Bredenoord and his colleagues. They found that LES electrical stimulation improved symptoms, PPI use, and esophageal acid exposure in this group of patients, but the preliminary number of patients was small and follow-up was mostly limited to 3 months. Importantly, they did report some adverse events.
These studies provide additional information to suggest that electrical stimulation of the LES may be an effective treatment for GERD. While the available data is compelling, more work will be required to evaluate the durability of the procedure, assess long-term safety and side effects, study the effects of stimulation on esophageal sensation, and define which GERD patients are best suited for this treatment. This will be ideally accomplished by randomized controlled trials that will compare electrical stimulation of the LES to the well-established pharmacological and surgical approaches currently used to treat GERD.
Marcelo F. Vela, M.D., is an associate professor of medicine and director of gastrointestinal motility at Baylor College of Medicine and the Michael E. DeBakey VA Medical Center, both in Houston. He is a member of an advisory panel for Given Imaging.
Gastroesophageal reflux disease is one of the most common chronic gastrointestinal disorders. The mainstay of medical therapy is to suppress gastric acid secretion with medications such as PPIs. An alternative approach to acid suppression is modulation of the antireflux barrier, composed of the lower esophageal sphincter (LES) and the crural diaphragm. Surgical fundoplication is a well-established method to augment the function of the antireflux barrier. Fundoplication has proven effective in high-quality trials, but it also has well-documented side effects such as dysphagia, bloating, and diarrhea in a subset of patients.
Additional means of enhancing the function of the antireflux barrier include pharmacological inhibition of transient LES relaxations (TLESR) with various agents and several endoscopic antireflux procedures. Unfortunately, the use of TLESR inhibitors and endoscopic procedures for GERD is very limited due to side effects and adverse events, along with insufficient efficacy.
Electrical stimulation of the LES has been previously shown to increase LES resting tone in an animal model (Am. J. Physiol. Gastrointest. Liver Physiol. 2008;295:G389-94). More recently, in a 6-month, open-label trial, electrical stimulation of the LES was found to reduce or eliminate PPI use and to improve symptoms and 24-hour esophageal pH parameters in GERD patients who were at least partially responsive to PPIs (Surg. Endosc. 2012 Oct. 17 [doi: 10.1007/s00464-012-2561-4]).
During the recent American College of Gastroenterology meeting, 1-year data for the open-label trial mentioned above was presented by Dr. Soffer, Dr. Crowell, and their collaborators, showing that improvement in symptoms, PPI use, and distal esophageal acid exposure persisted at 12 months with minimal side effects or adverse events.
Preliminary results of an international multicenter trial of LES electrical stimulation for refractory GERD were also presented at the meeting by Dr. Bredenoord and his colleagues. They found that LES electrical stimulation improved symptoms, PPI use, and esophageal acid exposure in this group of patients, but the preliminary number of patients was small and follow-up was mostly limited to 3 months. Importantly, they did report some adverse events.
These studies provide additional information to suggest that electrical stimulation of the LES may be an effective treatment for GERD. While the available data is compelling, more work will be required to evaluate the durability of the procedure, assess long-term safety and side effects, study the effects of stimulation on esophageal sensation, and define which GERD patients are best suited for this treatment. This will be ideally accomplished by randomized controlled trials that will compare electrical stimulation of the LES to the well-established pharmacological and surgical approaches currently used to treat GERD.
Marcelo F. Vela, M.D., is an associate professor of medicine and director of gastrointestinal motility at Baylor College of Medicine and the Michael E. DeBakey VA Medical Center, both in Houston. He is a member of an advisory panel for Given Imaging.
Electrical stimulation of the lower esophageal sphincter using an implanted device shows promise for the treatment of gastroesophageal reflux, according to findings from three recent studies.
In one open-label pilot extension study, 77% of 23 patients treated with EndoStim’s Lower Esophageal Sphincter (LES) stimulation system reported normalization of (or at least a 50% reduction in) distal esophageal acid exposure at 12 months’ follow-up, Dr. Edy Soffer reported in October at the annual meeting of the American College of Gastroenterology.
The patients also experienced significant improvement in their median GERD-Health Related Quality of Life (GERD-HRQL) score while implanted with the LES stimulation system (LES-EST), compared with their score while on proton pump inhibitor (PPI) therapy (increase of 9 vs. 2 points) and while off PPI therapy (increase of 23.5 vs. 2), said Dr. Soffer, professor of clinical medicine and director of the GI motility program at the University of Southern California, Los Angeles.
All but one patient reported cessation of regular PPI use, and no implantation- or stimulation-related unanticipated adverse events or "untoward sensation" due to stimulation occurred during follow-up; nor was swallowing function as assessed by manometry affected.
Patients included in the study were GERD patients with a mean age of 53 years who were at least partially responsive to PPI therapy, and who had off-PPI GERD-HRQL scores of at least 20, as well as hiatal hernia.
The findings indicate that LES-EST, which uses low-energy electrical pulses to strengthen a weak or dysfunctional lower esophageal sphincter, is safe and effective for long-term use, he said.
In an interview, Dr. Soffer said that the findings have held up at 18 months of follow-up.
"The results are comparable to those observed at 12 months with regard to control of symptoms, and with near elimination of the use of PPIs," he said, noting that the safety profile remains excellent, with no new adverse event reported beyond those seen at 12 months’ follow-up.
Physiological studies such as esophageal pH will be conducted at 24 months, he said.
In a related study presented in a poster at the meeting, Michael Crowell, Ph.D., looked more closely at the effects of LES-EST on both distal and proximal esophageal acid exposure in a post hoc analysis.
In 19 patients with a median age of 54 years, LES-EST was associated with normalization of total and upright proximal esophageal acid exposure, which improved from 0.4% and 0.6%, respectively, at baseline to 0% at 12 months’ follow-up. Supine esophageal acid exposure was unchanged from 0% at baseline, said Dr. Crowell of the Mayo Clinic, Scottsdale, Ariz.
This was true even among seven patients with abnormal proximal esophageal pH, whose total, upright, and supine proximal esophageal acid exposure values at baseline were 1.7%, 2.9%, and 0.3%, respectively. Distal esophageal pH improved from 10.2% to 3.6% for the entire cohort, and from 9.3% to 3.4% in those seven patients.
Patients in this study had GERD that was at least partially responsive to PPIs, a hiatal hernia of less than 3 cm, and esophagitis of less than Los Angeles Classification grade D. Electrical stimulation was administered for 220 microseconds at 20 Hz and 5-8 mA in 6-12 30-minute sessions starting on day 1 after implantation.
No gastrointestinal side effects occurred in the patients, nor were there any device- or procedure-related adverse events.
LES-EST may be effective in treating proximal GERD, Dr. Crowell concluded.
In an interview, he added that the findings are important, particularly for the one-third of patients who remain symptomatic on PPIs.
"LES dysfunction is the root cause of GERD. Medications such as PPIs block stomach acid production, but do not address the pathophysiology of GERD. Hence, more than a third of patients continue to suffer from symptoms despite maximal medical therapy," he said.
Additionally, there are significant safety concerns with long-term acid suppression, he noted.
LES-EST, on the other hand, addresses the root cause of GERD by improving LES pressure and function, thereby restoring the LES physiology and its barrier function, preventing reflux of gastric acid into the esophagus.
"LES stimulation does not affect normal LES relaxation, allowing for the patient to swallow normally, and has no side effects," he said.
In a third, unrelated study also reported in a poster at the meeting, LES-EST was similarly effective.
Of 11 patients treated with EndoStim’s LES stimulation system as part of an international multicenter study, 10 were able to discontinue PPI therapy at 3-6 months of follow-up, according to Dr. Arjan J. Bredenoord of Academic Medical Center Utrecht, Rotterdam.
Those 10 patients experienced significant improvements in median GERD-HRQL scores from 32 (off PPIs) and 22 (on PPIs) to 9 (on LES-EST) at 3 months, and the scores remained stable at 9 points in 3 patients who were followed for 6 months.
Median esophageal acid exposure improved from 11.8% at baseline to 7.8% at 3 months and 7.3% at 6 months, Dr. Bredenoord said.
The remaining patient suffered a small bowl trocar perforation during implantation of the device and underwent successful repair. An additional 13 adverse events, including 1 serious adverse event, were reported in 4 patients. Nine of these were related to the device or procedure, including seven complaints of pain at the implant site and one case of postoperative nausea.
The treatment was safe, with no GI or cardiac side effects, Dr. Bredenoord concluded, noting that long-term safety and efficacy results in a larger group of patients are currently being analyzed.
In an interview, Dr. Bredenoord noted that the findings are among the first in patients outside South America, where the earliest trials of the EndoStim LES stimulation system were conducted.
"The data confirm the favorable outcome of the patients in Chile, and show that both symptoms and reflux are reduced in European patients as well," he said.
However, the experience remains limited, and additional study comparing the device with other treatments and/or with placebo is needed, as are longer-term outcomes data.
"I think that although these results suggest this is a promising treatment, it would be best to treat patients only in trials" at this point, he said. Because trial participants have been carefully selected, it remains unclear whether this treatment is suitable for the entire GERD population, he added.
Dr. Soffer agreed, and said that if the results are reproduced in additional studies with a larger number of patients, the intervention will provide an alternative therapy for GERD patients who are not satisfied with PPIs or who have concerns about side effects and the chronic use of treatment, and who also have concerns about the established surgical treatment for GERD.
"The importance of this intervention is in providing a bridge between the currently established drug therapy for GERD [PPIs] and the established surgical therapy [fundoplication]. While PPIs are effective in a substantial number of GERD patients, they do not correct the underlying pathophysiology of GERD, resulting in a substantial number of patients who remain symptomatic in spite of therapy," he said.
These patients can be offered fundoplication, which is effective in expert hands, but the surgery has side effects and is performed less and less often, he added.
"Consequently, there is a search for a bridge intervention, endoscopic or surgical, for the treatment of GERD," he said.
LES-EST appears to have the potential to be such a bridge intervention.
"The procedure is simple and nondisruptive, and addresses pathophysiology. The safety profile thus far is excellent, and the effect on esophageal acid exposure, symptoms, and PPI use is sustained over a period of 12-18 moths. Furthermore, the treatment can be optimized to individual needs by adjusting delivery of stimulation to coincide with periods when symptoms and acid reflux are detected," he said.
All three of these studies presented at the meeting were supported by EndoStim BV. Dr. Soffer disclosed that he has stockholder/ownership interest in the company. Dr. Crowell disclosed that he has served as a consultant to the company. Dr. Bredenoord reported receiving grant and/or research support from the company.
Electrical stimulation of the lower esophageal sphincter using an implanted device shows promise for the treatment of gastroesophageal reflux, according to findings from three recent studies.
In one open-label pilot extension study, 77% of 23 patients treated with EndoStim’s Lower Esophageal Sphincter (LES) stimulation system reported normalization of (or at least a 50% reduction in) distal esophageal acid exposure at 12 months’ follow-up, Dr. Edy Soffer reported in October at the annual meeting of the American College of Gastroenterology.
The patients also experienced significant improvement in their median GERD-Health Related Quality of Life (GERD-HRQL) score while implanted with the LES stimulation system (LES-EST), compared with their score while on proton pump inhibitor (PPI) therapy (increase of 9 vs. 2 points) and while off PPI therapy (increase of 23.5 vs. 2), said Dr. Soffer, professor of clinical medicine and director of the GI motility program at the University of Southern California, Los Angeles.
All but one patient reported cessation of regular PPI use, and no implantation- or stimulation-related unanticipated adverse events or "untoward sensation" due to stimulation occurred during follow-up; nor was swallowing function as assessed by manometry affected.
Patients included in the study were GERD patients with a mean age of 53 years who were at least partially responsive to PPI therapy, and who had off-PPI GERD-HRQL scores of at least 20, as well as hiatal hernia.
The findings indicate that LES-EST, which uses low-energy electrical pulses to strengthen a weak or dysfunctional lower esophageal sphincter, is safe and effective for long-term use, he said.
In an interview, Dr. Soffer said that the findings have held up at 18 months of follow-up.
"The results are comparable to those observed at 12 months with regard to control of symptoms, and with near elimination of the use of PPIs," he said, noting that the safety profile remains excellent, with no new adverse event reported beyond those seen at 12 months’ follow-up.
Physiological studies such as esophageal pH will be conducted at 24 months, he said.
In a related study presented in a poster at the meeting, Michael Crowell, Ph.D., looked more closely at the effects of LES-EST on both distal and proximal esophageal acid exposure in a post hoc analysis.
In 19 patients with a median age of 54 years, LES-EST was associated with normalization of total and upright proximal esophageal acid exposure, which improved from 0.4% and 0.6%, respectively, at baseline to 0% at 12 months’ follow-up. Supine esophageal acid exposure was unchanged from 0% at baseline, said Dr. Crowell of the Mayo Clinic, Scottsdale, Ariz.
This was true even among seven patients with abnormal proximal esophageal pH, whose total, upright, and supine proximal esophageal acid exposure values at baseline were 1.7%, 2.9%, and 0.3%, respectively. Distal esophageal pH improved from 10.2% to 3.6% for the entire cohort, and from 9.3% to 3.4% in those seven patients.
Patients in this study had GERD that was at least partially responsive to PPIs, a hiatal hernia of less than 3 cm, and esophagitis of less than Los Angeles Classification grade D. Electrical stimulation was administered for 220 microseconds at 20 Hz and 5-8 mA in 6-12 30-minute sessions starting on day 1 after implantation.
No gastrointestinal side effects occurred in the patients, nor were there any device- or procedure-related adverse events.
LES-EST may be effective in treating proximal GERD, Dr. Crowell concluded.
In an interview, he added that the findings are important, particularly for the one-third of patients who remain symptomatic on PPIs.
"LES dysfunction is the root cause of GERD. Medications such as PPIs block stomach acid production, but do not address the pathophysiology of GERD. Hence, more than a third of patients continue to suffer from symptoms despite maximal medical therapy," he said.
Additionally, there are significant safety concerns with long-term acid suppression, he noted.
LES-EST, on the other hand, addresses the root cause of GERD by improving LES pressure and function, thereby restoring the LES physiology and its barrier function, preventing reflux of gastric acid into the esophagus.
"LES stimulation does not affect normal LES relaxation, allowing for the patient to swallow normally, and has no side effects," he said.
In a third, unrelated study also reported in a poster at the meeting, LES-EST was similarly effective.
Of 11 patients treated with EndoStim’s LES stimulation system as part of an international multicenter study, 10 were able to discontinue PPI therapy at 3-6 months of follow-up, according to Dr. Arjan J. Bredenoord of Academic Medical Center Utrecht, Rotterdam.
Those 10 patients experienced significant improvements in median GERD-HRQL scores from 32 (off PPIs) and 22 (on PPIs) to 9 (on LES-EST) at 3 months, and the scores remained stable at 9 points in 3 patients who were followed for 6 months.
Median esophageal acid exposure improved from 11.8% at baseline to 7.8% at 3 months and 7.3% at 6 months, Dr. Bredenoord said.
The remaining patient suffered a small bowl trocar perforation during implantation of the device and underwent successful repair. An additional 13 adverse events, including 1 serious adverse event, were reported in 4 patients. Nine of these were related to the device or procedure, including seven complaints of pain at the implant site and one case of postoperative nausea.
The treatment was safe, with no GI or cardiac side effects, Dr. Bredenoord concluded, noting that long-term safety and efficacy results in a larger group of patients are currently being analyzed.
In an interview, Dr. Bredenoord noted that the findings are among the first in patients outside South America, where the earliest trials of the EndoStim LES stimulation system were conducted.
"The data confirm the favorable outcome of the patients in Chile, and show that both symptoms and reflux are reduced in European patients as well," he said.
However, the experience remains limited, and additional study comparing the device with other treatments and/or with placebo is needed, as are longer-term outcomes data.
"I think that although these results suggest this is a promising treatment, it would be best to treat patients only in trials" at this point, he said. Because trial participants have been carefully selected, it remains unclear whether this treatment is suitable for the entire GERD population, he added.
Dr. Soffer agreed, and said that if the results are reproduced in additional studies with a larger number of patients, the intervention will provide an alternative therapy for GERD patients who are not satisfied with PPIs or who have concerns about side effects and the chronic use of treatment, and who also have concerns about the established surgical treatment for GERD.
"The importance of this intervention is in providing a bridge between the currently established drug therapy for GERD [PPIs] and the established surgical therapy [fundoplication]. While PPIs are effective in a substantial number of GERD patients, they do not correct the underlying pathophysiology of GERD, resulting in a substantial number of patients who remain symptomatic in spite of therapy," he said.
These patients can be offered fundoplication, which is effective in expert hands, but the surgery has side effects and is performed less and less often, he added.
"Consequently, there is a search for a bridge intervention, endoscopic or surgical, for the treatment of GERD," he said.
LES-EST appears to have the potential to be such a bridge intervention.
"The procedure is simple and nondisruptive, and addresses pathophysiology. The safety profile thus far is excellent, and the effect on esophageal acid exposure, symptoms, and PPI use is sustained over a period of 12-18 moths. Furthermore, the treatment can be optimized to individual needs by adjusting delivery of stimulation to coincide with periods when symptoms and acid reflux are detected," he said.
All three of these studies presented at the meeting were supported by EndoStim BV. Dr. Soffer disclosed that he has stockholder/ownership interest in the company. Dr. Crowell disclosed that he has served as a consultant to the company. Dr. Bredenoord reported receiving grant and/or research support from the company.
FROM THE ANNUAL MEETING OF THE AMERICAN COLLEGE OF GASTROENTEROLOGY
Deficits in empathic abilities appear to be disorder specific
Behavioral empathy performance differs by psychiatric disorder, with the strongest impairment occurring in schizophrenia patients followed by bipolar patients, and with the strongest association between clinical characteristics and empathy performance occurring in patients with depression, according to findings from a case-control study.
The finding that impairments in emotional competencies are disorder specific could enable better characterization of patient groups and allow for more tailored psychotherapeutic interventions, reported Birgit Derntl, Ph.D., of the University of Vienna, and colleagues.
They compared 72 patients – 24 each with schizophrenia, bipolar disorder, and depression – with 24 healthy age-, gender-, and verbal intelligence–matched controls. All participants performed three tasks focused on emotion recognition, emotional perspective taking, and affective responsiveness.
Emotion recognition was significantly better among the controls, compared with those in the schizophrenia and bipolar groups, with a trend toward significance compared with those in the depression group (Schizophrenia Res. 2012;142:58-64 [doi:10.1016/j.schres.2012.09.020]).
"A significant effect of emotion, but no significant emotion-by-group interaction emerged. Post hoc analysis of the significant emotion effect showed highest accuracy for happy conditions followed by neutral, anger, fear, disgust, and sad conditions," they said.
Emotional perspective taking, after researchers controlled for emotion recognition and affective responsiveness performance, also was significantly increased among the controls, compared with the schizophrenia patients. The schizophrenia patients also performed significantly worse than did the bipolar group on this task. No differences were seen between controls and depression patients, controls and bipolar patients, or depression patients and bipolar patients.
As with emotion recognition, a significant main effect of emotion was seen with emotional perspective taking, but no significant emotion-by-group interaction emerged for this measure, and post hoc analysis of the significant emotion effects showed highest accuracy for happy conditions followed by neutral, anger, disgust, fear, and sad conditions.
Similarly, affective responsiveness was highly significantly better among controls than among the other three groups after researchers controlled for emotion recognition and perspective taking performance, and the schizophrenia patients performed significantly worse than did the bipolar and depression patients. The bipolar and depression groups did not differ.
A significant main effect of emotion and a significant group-by-emotion interaction was seen for this measure; a significant group effect was seen for all negative emotions and neutral conditions, but no group effect was seen for happiness.
"Comparing the overall accuracy across all tasks revealed a significant task effect, with lowest accuracy in affective responsiveness and highest in emotional perspective taking," the investigators said, noting that a significant group effect occurred, with controls outperforming the schizophrenia and bipolar groups, and trending toward outperforming the depression group. The schizophrenia group performed worse than did both the bipolar and depression groups, and the bipolar and depression groups did not differ. A similar and significant task-by-group interaction was observed.
No significant differences were seen when comparing actual behavioral performance and self-reported empathy in any of the groups. Notably, however, the bipolar patients had significantly lower self-reported empathy sum scores, compared with the controls and the depression patients.
As for the association between clinical characteristics and empathy performance, symptom severity scores correlated with accuracy in affective responsiveness only in the depression group. Scores in the bipolar group and schizophrenia group were not correlated with accuracy in any of the empathy tasks, the investigators said.
Furthermore, duration of illness in the depression group, but not the other groups, was significantly and negatively associated with affective responsiveness score, indicating worse performance with longer disease duration.
Study participants were adults with a mean age of 41 years who were recruited from academic medical centers. Empathy tasks to assess emotion recognition involved the use of pictures of faces depicting five basic emotions and neutral expressions, which participants were asked to identify. Emotional perspective taking was assessed by asking participants to identify basic emotions and neutral scenes depicted in pictures involving social interaction; the face of one person in each picture was masked, and the participants were asked to infer the corresponding emotional expression of the masked face based on which expression would fit the emotional situation.
Affective responsiveness was assessed by asking participants to describe how short written sentences describing real-life emotional and emotionally neutral situations would make them feel if they were experiencing those situations.
While the study is limited by small sample size and by incomplete data regarding history of psychotic episodes (which have been shown to worsen cognitive performance in bipolar patients), and also by the fact that some participants were chronic patients and most were medicated, it nonetheless highlights that schizophrenia patients are particularly characterized by severe impairment in emotional perspective taking and affective responsiveness, when compared with healthy controls and patients with affective disorders, the investigators said.
"Taken together, this study showed that analysis of specificity of empathic deficits helps to better characterize emotional deficits in patients suffering from severe psychiatric disorder. Moreover, our data provide input for disorder-specific psychotherapeutic treatment," they noted.
The findings underscore a need for training to improve high-level emotional competencies, particularly in schizophrenia patients. This training should go beyond emotion recognition training. Also, therapists should encourage patients with bipolar disorder to correct any negative self-evaluation with respect to empathic competencies, especially "by relying on accurate perspective taking in complex social situations as a particular resource," they concluded.
This study was funded by a grant from the IZKF. Dr. Derntl reported receiving support from the German Research Foundation.
Behavioral empathy performance differs by psychiatric disorder, with the strongest impairment occurring in schizophrenia patients followed by bipolar patients, and with the strongest association between clinical characteristics and empathy performance occurring in patients with depression, according to findings from a case-control study.
The finding that impairments in emotional competencies are disorder specific could enable better characterization of patient groups and allow for more tailored psychotherapeutic interventions, reported Birgit Derntl, Ph.D., of the University of Vienna, and colleagues.
They compared 72 patients – 24 each with schizophrenia, bipolar disorder, and depression – with 24 healthy age-, gender-, and verbal intelligence–matched controls. All participants performed three tasks focused on emotion recognition, emotional perspective taking, and affective responsiveness.
Emotion recognition was significantly better among the controls, compared with those in the schizophrenia and bipolar groups, with a trend toward significance compared with those in the depression group (Schizophrenia Res. 2012;142:58-64 [doi:10.1016/j.schres.2012.09.020]).
"A significant effect of emotion, but no significant emotion-by-group interaction emerged. Post hoc analysis of the significant emotion effect showed highest accuracy for happy conditions followed by neutral, anger, fear, disgust, and sad conditions," they said.
Emotional perspective taking, after researchers controlled for emotion recognition and affective responsiveness performance, also was significantly increased among the controls, compared with the schizophrenia patients. The schizophrenia patients also performed significantly worse than did the bipolar group on this task. No differences were seen between controls and depression patients, controls and bipolar patients, or depression patients and bipolar patients.
As with emotion recognition, a significant main effect of emotion was seen with emotional perspective taking, but no significant emotion-by-group interaction emerged for this measure, and post hoc analysis of the significant emotion effects showed highest accuracy for happy conditions followed by neutral, anger, disgust, fear, and sad conditions.
Similarly, affective responsiveness was highly significantly better among controls than among the other three groups after researchers controlled for emotion recognition and perspective taking performance, and the schizophrenia patients performed significantly worse than did the bipolar and depression patients. The bipolar and depression groups did not differ.
A significant main effect of emotion and a significant group-by-emotion interaction was seen for this measure; a significant group effect was seen for all negative emotions and neutral conditions, but no group effect was seen for happiness.
"Comparing the overall accuracy across all tasks revealed a significant task effect, with lowest accuracy in affective responsiveness and highest in emotional perspective taking," the investigators said, noting that a significant group effect occurred, with controls outperforming the schizophrenia and bipolar groups, and trending toward outperforming the depression group. The schizophrenia group performed worse than did both the bipolar and depression groups, and the bipolar and depression groups did not differ. A similar and significant task-by-group interaction was observed.
No significant differences were seen when comparing actual behavioral performance and self-reported empathy in any of the groups. Notably, however, the bipolar patients had significantly lower self-reported empathy sum scores, compared with the controls and the depression patients.
As for the association between clinical characteristics and empathy performance, symptom severity scores correlated with accuracy in affective responsiveness only in the depression group. Scores in the bipolar group and schizophrenia group were not correlated with accuracy in any of the empathy tasks, the investigators said.
Furthermore, duration of illness in the depression group, but not the other groups, was significantly and negatively associated with affective responsiveness score, indicating worse performance with longer disease duration.
Study participants were adults with a mean age of 41 years who were recruited from academic medical centers. Empathy tasks to assess emotion recognition involved the use of pictures of faces depicting five basic emotions and neutral expressions, which participants were asked to identify. Emotional perspective taking was assessed by asking participants to identify basic emotions and neutral scenes depicted in pictures involving social interaction; the face of one person in each picture was masked, and the participants were asked to infer the corresponding emotional expression of the masked face based on which expression would fit the emotional situation.
Affective responsiveness was assessed by asking participants to describe how short written sentences describing real-life emotional and emotionally neutral situations would make them feel if they were experiencing those situations.
While the study is limited by small sample size and by incomplete data regarding history of psychotic episodes (which have been shown to worsen cognitive performance in bipolar patients), and also by the fact that some participants were chronic patients and most were medicated, it nonetheless highlights that schizophrenia patients are particularly characterized by severe impairment in emotional perspective taking and affective responsiveness, when compared with healthy controls and patients with affective disorders, the investigators said.
"Taken together, this study showed that analysis of specificity of empathic deficits helps to better characterize emotional deficits in patients suffering from severe psychiatric disorder. Moreover, our data provide input for disorder-specific psychotherapeutic treatment," they noted.
The findings underscore a need for training to improve high-level emotional competencies, particularly in schizophrenia patients. This training should go beyond emotion recognition training. Also, therapists should encourage patients with bipolar disorder to correct any negative self-evaluation with respect to empathic competencies, especially "by relying on accurate perspective taking in complex social situations as a particular resource," they concluded.
This study was funded by a grant from the IZKF. Dr. Derntl reported receiving support from the German Research Foundation.
Behavioral empathy performance differs by psychiatric disorder, with the strongest impairment occurring in schizophrenia patients followed by bipolar patients, and with the strongest association between clinical characteristics and empathy performance occurring in patients with depression, according to findings from a case-control study.
The finding that impairments in emotional competencies are disorder specific could enable better characterization of patient groups and allow for more tailored psychotherapeutic interventions, reported Birgit Derntl, Ph.D., of the University of Vienna, and colleagues.
They compared 72 patients – 24 each with schizophrenia, bipolar disorder, and depression – with 24 healthy age-, gender-, and verbal intelligence–matched controls. All participants performed three tasks focused on emotion recognition, emotional perspective taking, and affective responsiveness.
Emotion recognition was significantly better among the controls, compared with those in the schizophrenia and bipolar groups, with a trend toward significance compared with those in the depression group (Schizophrenia Res. 2012;142:58-64 [doi:10.1016/j.schres.2012.09.020]).
"A significant effect of emotion, but no significant emotion-by-group interaction emerged. Post hoc analysis of the significant emotion effect showed highest accuracy for happy conditions followed by neutral, anger, fear, disgust, and sad conditions," they said.
Emotional perspective taking, after researchers controlled for emotion recognition and affective responsiveness performance, also was significantly increased among the controls, compared with the schizophrenia patients. The schizophrenia patients also performed significantly worse than did the bipolar group on this task. No differences were seen between controls and depression patients, controls and bipolar patients, or depression patients and bipolar patients.
As with emotion recognition, a significant main effect of emotion was seen with emotional perspective taking, but no significant emotion-by-group interaction emerged for this measure, and post hoc analysis of the significant emotion effects showed highest accuracy for happy conditions followed by neutral, anger, disgust, fear, and sad conditions.
Similarly, affective responsiveness was highly significantly better among controls than among the other three groups after researchers controlled for emotion recognition and perspective taking performance, and the schizophrenia patients performed significantly worse than did the bipolar and depression patients. The bipolar and depression groups did not differ.
A significant main effect of emotion and a significant group-by-emotion interaction was seen for this measure; a significant group effect was seen for all negative emotions and neutral conditions, but no group effect was seen for happiness.
"Comparing the overall accuracy across all tasks revealed a significant task effect, with lowest accuracy in affective responsiveness and highest in emotional perspective taking," the investigators said, noting that a significant group effect occurred, with controls outperforming the schizophrenia and bipolar groups, and trending toward outperforming the depression group. The schizophrenia group performed worse than did both the bipolar and depression groups, and the bipolar and depression groups did not differ. A similar and significant task-by-group interaction was observed.
No significant differences were seen when comparing actual behavioral performance and self-reported empathy in any of the groups. Notably, however, the bipolar patients had significantly lower self-reported empathy sum scores, compared with the controls and the depression patients.
As for the association between clinical characteristics and empathy performance, symptom severity scores correlated with accuracy in affective responsiveness only in the depression group. Scores in the bipolar group and schizophrenia group were not correlated with accuracy in any of the empathy tasks, the investigators said.
Furthermore, duration of illness in the depression group, but not the other groups, was significantly and negatively associated with affective responsiveness score, indicating worse performance with longer disease duration.
Study participants were adults with a mean age of 41 years who were recruited from academic medical centers. Empathy tasks to assess emotion recognition involved the use of pictures of faces depicting five basic emotions and neutral expressions, which participants were asked to identify. Emotional perspective taking was assessed by asking participants to identify basic emotions and neutral scenes depicted in pictures involving social interaction; the face of one person in each picture was masked, and the participants were asked to infer the corresponding emotional expression of the masked face based on which expression would fit the emotional situation.
Affective responsiveness was assessed by asking participants to describe how short written sentences describing real-life emotional and emotionally neutral situations would make them feel if they were experiencing those situations.
While the study is limited by small sample size and by incomplete data regarding history of psychotic episodes (which have been shown to worsen cognitive performance in bipolar patients), and also by the fact that some participants were chronic patients and most were medicated, it nonetheless highlights that schizophrenia patients are particularly characterized by severe impairment in emotional perspective taking and affective responsiveness, when compared with healthy controls and patients with affective disorders, the investigators said.
"Taken together, this study showed that analysis of specificity of empathic deficits helps to better characterize emotional deficits in patients suffering from severe psychiatric disorder. Moreover, our data provide input for disorder-specific psychotherapeutic treatment," they noted.
The findings underscore a need for training to improve high-level emotional competencies, particularly in schizophrenia patients. This training should go beyond emotion recognition training. Also, therapists should encourage patients with bipolar disorder to correct any negative self-evaluation with respect to empathic competencies, especially "by relying on accurate perspective taking in complex social situations as a particular resource," they concluded.
This study was funded by a grant from the IZKF. Dr. Derntl reported receiving support from the German Research Foundation.
FROM SCHIZOPHRENIA RESEARCH
Major Finding: Schizophrenia patients have the strongest impairment in empathic performance, followed by bipolar patients. The strongest association between clinical characteristics and empathy performance is in patients with depression.
Data Source: A case-control study of 72 patients – 24 each with schizophrenia, bipolar disorder, and depression.
Disclosures: This study was funded by a grant from the IZKF. Dr. Derntl reported receiving support from the German Research Foundation.
Late stop to antirheumatics may risk postsurgical infection
WASHINGTON – The risk of infection following orthopedic surgery is increased in patients with inflammatory rheumatic disease, compared with those with degenerative disease or traumatic injury, according to findings from a review of more than 50,000 surgical procedures.
The risk is greatest in those inflammatory rheumatic disease patients treated with conventional disease-modifying anti-rheumatic drugs (cDMARDs) or tumor necrosis factor (TNF) inhibitors, especially those receiving more than one cDMARD or TNF inhibitor with a long administration interval, and when surgery takes place without discontinuation of treatment, Catrina B. Scherrer reported at the annual meeting of the American College of Rheumatology.
Of 50,359 surgical procedures performed in 37,137 patients from a hospital surgery registry, 422 resulted in surgery-related infections. Of these infections, 49 occurred in 2,472 patients with an inflammatory rheumatic disease (IRD; 2%), and 373 occurred in 47,887 patients with degenerative disease/posttraumatic injury (0.8%). The difference was statistically significant, even after adjustment for other risk factors, including age, gender, diabetes, being overweight, cardiovascular disease, smoking, and type of surgery, said Ms. Scherrer of the Schulthess Clinic, Zürich.
The lowest rates of infection occurred with hand and shoulder surgery; the highest rates occurred with elbow surgery, she noted.
In 1,329 patients in the IRD group for whom complete information about medication was available, 171 (13%) had documented use of TNF inhibitors, and 49 of these (29%) discontinued treatment more than three administration intervals before surgery. Of the remaining 122 TNF inhibitor users, the time lag was three or fewer administration intervals.
An increased infection rate was seen in those who used more than one cDMARD (odds ratio, 2.425) and more than one TNF inhibitor (OR, 2.627) prior to surgery, and the risk of infection was increased tenfold when surgery was performed within one administration interval (OR, 10.047).
Patients who had their last treatment within one administration interval before surgery included 81% of infliximab users, compared with only 33% of adalimumab users and 24% of etanercept users, Ms. Scherrer noted.
Surgery patients in this study were followed over 8 years as part of a single-center surgery registry. The findings, which are limited by the study’s retrospective design and thus require confirmation in prospective studies, are nonetheless important because patients with aggressive disease such as IRDs frequently require orthopedic surgery.
The study findings suggest that IRD patients are, in general, at high risk of postoperative infection, that special attention should be paid to patients using more than one cDMARD or TNF inhibitor with long administration intervals, and that the last intake of TNF inhibitors – particularly infliximab – should be at least more than one administration interval before planned surgery, as the risk of postoperative infection is significantly increased if surgery occurs within this period, she concluded.
Ms. Scherrer reported having no disclosures.
WASHINGTON – The risk of infection following orthopedic surgery is increased in patients with inflammatory rheumatic disease, compared with those with degenerative disease or traumatic injury, according to findings from a review of more than 50,000 surgical procedures.
The risk is greatest in those inflammatory rheumatic disease patients treated with conventional disease-modifying anti-rheumatic drugs (cDMARDs) or tumor necrosis factor (TNF) inhibitors, especially those receiving more than one cDMARD or TNF inhibitor with a long administration interval, and when surgery takes place without discontinuation of treatment, Catrina B. Scherrer reported at the annual meeting of the American College of Rheumatology.
Of 50,359 surgical procedures performed in 37,137 patients from a hospital surgery registry, 422 resulted in surgery-related infections. Of these infections, 49 occurred in 2,472 patients with an inflammatory rheumatic disease (IRD; 2%), and 373 occurred in 47,887 patients with degenerative disease/posttraumatic injury (0.8%). The difference was statistically significant, even after adjustment for other risk factors, including age, gender, diabetes, being overweight, cardiovascular disease, smoking, and type of surgery, said Ms. Scherrer of the Schulthess Clinic, Zürich.
The lowest rates of infection occurred with hand and shoulder surgery; the highest rates occurred with elbow surgery, she noted.
In 1,329 patients in the IRD group for whom complete information about medication was available, 171 (13%) had documented use of TNF inhibitors, and 49 of these (29%) discontinued treatment more than three administration intervals before surgery. Of the remaining 122 TNF inhibitor users, the time lag was three or fewer administration intervals.
An increased infection rate was seen in those who used more than one cDMARD (odds ratio, 2.425) and more than one TNF inhibitor (OR, 2.627) prior to surgery, and the risk of infection was increased tenfold when surgery was performed within one administration interval (OR, 10.047).
Patients who had their last treatment within one administration interval before surgery included 81% of infliximab users, compared with only 33% of adalimumab users and 24% of etanercept users, Ms. Scherrer noted.
Surgery patients in this study were followed over 8 years as part of a single-center surgery registry. The findings, which are limited by the study’s retrospective design and thus require confirmation in prospective studies, are nonetheless important because patients with aggressive disease such as IRDs frequently require orthopedic surgery.
The study findings suggest that IRD patients are, in general, at high risk of postoperative infection, that special attention should be paid to patients using more than one cDMARD or TNF inhibitor with long administration intervals, and that the last intake of TNF inhibitors – particularly infliximab – should be at least more than one administration interval before planned surgery, as the risk of postoperative infection is significantly increased if surgery occurs within this period, she concluded.
Ms. Scherrer reported having no disclosures.
WASHINGTON – The risk of infection following orthopedic surgery is increased in patients with inflammatory rheumatic disease, compared with those with degenerative disease or traumatic injury, according to findings from a review of more than 50,000 surgical procedures.
The risk is greatest in those inflammatory rheumatic disease patients treated with conventional disease-modifying anti-rheumatic drugs (cDMARDs) or tumor necrosis factor (TNF) inhibitors, especially those receiving more than one cDMARD or TNF inhibitor with a long administration interval, and when surgery takes place without discontinuation of treatment, Catrina B. Scherrer reported at the annual meeting of the American College of Rheumatology.
Of 50,359 surgical procedures performed in 37,137 patients from a hospital surgery registry, 422 resulted in surgery-related infections. Of these infections, 49 occurred in 2,472 patients with an inflammatory rheumatic disease (IRD; 2%), and 373 occurred in 47,887 patients with degenerative disease/posttraumatic injury (0.8%). The difference was statistically significant, even after adjustment for other risk factors, including age, gender, diabetes, being overweight, cardiovascular disease, smoking, and type of surgery, said Ms. Scherrer of the Schulthess Clinic, Zürich.
The lowest rates of infection occurred with hand and shoulder surgery; the highest rates occurred with elbow surgery, she noted.
In 1,329 patients in the IRD group for whom complete information about medication was available, 171 (13%) had documented use of TNF inhibitors, and 49 of these (29%) discontinued treatment more than three administration intervals before surgery. Of the remaining 122 TNF inhibitor users, the time lag was three or fewer administration intervals.
An increased infection rate was seen in those who used more than one cDMARD (odds ratio, 2.425) and more than one TNF inhibitor (OR, 2.627) prior to surgery, and the risk of infection was increased tenfold when surgery was performed within one administration interval (OR, 10.047).
Patients who had their last treatment within one administration interval before surgery included 81% of infliximab users, compared with only 33% of adalimumab users and 24% of etanercept users, Ms. Scherrer noted.
Surgery patients in this study were followed over 8 years as part of a single-center surgery registry. The findings, which are limited by the study’s retrospective design and thus require confirmation in prospective studies, are nonetheless important because patients with aggressive disease such as IRDs frequently require orthopedic surgery.
The study findings suggest that IRD patients are, in general, at high risk of postoperative infection, that special attention should be paid to patients using more than one cDMARD or TNF inhibitor with long administration intervals, and that the last intake of TNF inhibitors – particularly infliximab – should be at least more than one administration interval before planned surgery, as the risk of postoperative infection is significantly increased if surgery occurs within this period, she concluded.
Ms. Scherrer reported having no disclosures.
AT THE ANNUAL MEETING OF THE AMERICAN COLLEGE OF RHEUMATOLOGY
Major Finding: An increased infection rate was seen in patients who used more than one cDMARD (odds ratio, 2.425) and more than one TNF inhibitor (OR, 2.627) prior to surgery, and the risk of infection was increased 10-fold when surgery was performed within one treatment administration interval (OR, 10.047).
Data Source: A retrospective study of surgery cases.
Disclosures: Ms. Scherrer reported having no disclosures.
Chronic constipation may increase colorectal cancer risk
Chronic constipation may predispose affected patients to developing colorectal cancer and benign neoplasms, according to an analysis of data from a large retrospective U.S. claims database.
The risk of developing colorectal cancer was 1.78 times higher among 28,854 adults with chronic constipation than among 86,562 controls without chronic constipation, and the risk of developing benign neoplasms was 2.7 times higher in those with chronic constipation, Dr. Nicholas Talley reported in a poster at the annual meeting of the American College of Gastroenterology.
The risk of colorectal cancer and benign neoplasms among those with chronic constipation remained "consistently high" after researchers controlled for potential confounding factors, including age, gender, family history of malignancies, and other nongastrointestinal morbidities, said Dr. Talley of the University of Newcastle, Callaghan, New South Wales, Australia.
Patients included adults aged older than 18 years who received at least two diagnoses of chronic constipation 60-365 days apart between January 1999 and September 2011. Those with irritable bowel syndrome or diarrhea were excluded, as were those who did not remain enrolled in their health plans for at least 12 months from the date of their first eligible diagnosis of constipation.
The investigators matched control subjects, who had never been diagnosed with constipation and never had a prescription filled for a laxative during the observation period, with case patients in a 1:3 ratio based on year of birth, sex, and region of residence.
Patients and controls had a mean age of 61.9 years, and one-third were men. The mean observation period was nearly 4 years.
The prevalence of colorectal cancer in this study was 2.7% in the patients and 1.7% in the controls; the prevalence of benign neoplasms was 24.8% in the patients and 11.9% in the controls, Dr. Talley said.
Although the findings do not prove a causal link between chronic constipation and colorectal cancer or benign neoplasms, they do suggest a strong association, he said in a press statement.
"The postulated causal link is that longer transit times increase the duration of contact between the colonic mucosa and concentrated carcinogens such as bile acids in the lumen," he said.
This association deserves further investigation to more thoroughly explore and to better understand possible causal elements, he added.
This is particularly important because prospective cohort studies have failed to identify a similar association to that seen in this retrospective review, suggesting that those findings are affected by recall bias, he said.
While further study is needed, practitioners should be aware of the potential relationship between chronic constipation and development of colorectal cancer and benign neoplasms, and should monitor and treat patients accordingly, he concluded.
Dr. Talley received research support from Takeda Pharmaceuticals International, which supported the study. Coauthors were employed by Takeda or by Analysis Group Inc., which has received consulting fees from Takeda.
Chronic constipation may predispose affected patients to developing colorectal cancer and benign neoplasms, according to an analysis of data from a large retrospective U.S. claims database.
The risk of developing colorectal cancer was 1.78 times higher among 28,854 adults with chronic constipation than among 86,562 controls without chronic constipation, and the risk of developing benign neoplasms was 2.7 times higher in those with chronic constipation, Dr. Nicholas Talley reported in a poster at the annual meeting of the American College of Gastroenterology.
The risk of colorectal cancer and benign neoplasms among those with chronic constipation remained "consistently high" after researchers controlled for potential confounding factors, including age, gender, family history of malignancies, and other nongastrointestinal morbidities, said Dr. Talley of the University of Newcastle, Callaghan, New South Wales, Australia.
Patients included adults aged older than 18 years who received at least two diagnoses of chronic constipation 60-365 days apart between January 1999 and September 2011. Those with irritable bowel syndrome or diarrhea were excluded, as were those who did not remain enrolled in their health plans for at least 12 months from the date of their first eligible diagnosis of constipation.
The investigators matched control subjects, who had never been diagnosed with constipation and never had a prescription filled for a laxative during the observation period, with case patients in a 1:3 ratio based on year of birth, sex, and region of residence.
Patients and controls had a mean age of 61.9 years, and one-third were men. The mean observation period was nearly 4 years.
The prevalence of colorectal cancer in this study was 2.7% in the patients and 1.7% in the controls; the prevalence of benign neoplasms was 24.8% in the patients and 11.9% in the controls, Dr. Talley said.
Although the findings do not prove a causal link between chronic constipation and colorectal cancer or benign neoplasms, they do suggest a strong association, he said in a press statement.
"The postulated causal link is that longer transit times increase the duration of contact between the colonic mucosa and concentrated carcinogens such as bile acids in the lumen," he said.
This association deserves further investigation to more thoroughly explore and to better understand possible causal elements, he added.
This is particularly important because prospective cohort studies have failed to identify a similar association to that seen in this retrospective review, suggesting that those findings are affected by recall bias, he said.
While further study is needed, practitioners should be aware of the potential relationship between chronic constipation and development of colorectal cancer and benign neoplasms, and should monitor and treat patients accordingly, he concluded.
Dr. Talley received research support from Takeda Pharmaceuticals International, which supported the study. Coauthors were employed by Takeda or by Analysis Group Inc., which has received consulting fees from Takeda.
Chronic constipation may predispose affected patients to developing colorectal cancer and benign neoplasms, according to an analysis of data from a large retrospective U.S. claims database.
The risk of developing colorectal cancer was 1.78 times higher among 28,854 adults with chronic constipation than among 86,562 controls without chronic constipation, and the risk of developing benign neoplasms was 2.7 times higher in those with chronic constipation, Dr. Nicholas Talley reported in a poster at the annual meeting of the American College of Gastroenterology.
The risk of colorectal cancer and benign neoplasms among those with chronic constipation remained "consistently high" after researchers controlled for potential confounding factors, including age, gender, family history of malignancies, and other nongastrointestinal morbidities, said Dr. Talley of the University of Newcastle, Callaghan, New South Wales, Australia.
Patients included adults aged older than 18 years who received at least two diagnoses of chronic constipation 60-365 days apart between January 1999 and September 2011. Those with irritable bowel syndrome or diarrhea were excluded, as were those who did not remain enrolled in their health plans for at least 12 months from the date of their first eligible diagnosis of constipation.
The investigators matched control subjects, who had never been diagnosed with constipation and never had a prescription filled for a laxative during the observation period, with case patients in a 1:3 ratio based on year of birth, sex, and region of residence.
Patients and controls had a mean age of 61.9 years, and one-third were men. The mean observation period was nearly 4 years.
The prevalence of colorectal cancer in this study was 2.7% in the patients and 1.7% in the controls; the prevalence of benign neoplasms was 24.8% in the patients and 11.9% in the controls, Dr. Talley said.
Although the findings do not prove a causal link between chronic constipation and colorectal cancer or benign neoplasms, they do suggest a strong association, he said in a press statement.
"The postulated causal link is that longer transit times increase the duration of contact between the colonic mucosa and concentrated carcinogens such as bile acids in the lumen," he said.
This association deserves further investigation to more thoroughly explore and to better understand possible causal elements, he added.
This is particularly important because prospective cohort studies have failed to identify a similar association to that seen in this retrospective review, suggesting that those findings are affected by recall bias, he said.
While further study is needed, practitioners should be aware of the potential relationship between chronic constipation and development of colorectal cancer and benign neoplasms, and should monitor and treat patients accordingly, he concluded.
Dr. Talley received research support from Takeda Pharmaceuticals International, which supported the study. Coauthors were employed by Takeda or by Analysis Group Inc., which has received consulting fees from Takeda.
FROM THE ANNUAL MEETING OF THE AMERICAN COLLEGE OF GASTROENTEROLOGY
Major Finding: The risk of developing colorectal cancer was 1.78 times higher in 28,854 adults with chronic constipation than in 86,562 controls without chronic constipation, and the risk of developing benign neoplasms was 2.7 times higher in those with chronic constipation.
Data Source: A large retrospective U.S. claims database.
Disclosures: Dr. Talley received research support from Takeda Pharmaceuticals International, which supported the study. Coauthors were employed by Takeda or by Analysis Group Inc., which has received consulting fees from Takeda.
No short-term benefit of hydroxychloroquine found for primary Sjögren’s
WASHINGTON – Hydroxychloroquine had no short-term efficacy for primary Sjögren’s syndrome in a randomized, double-blind, placebo-controlled trial involving 120 patients.
The favorable overall response rate after 6 months was low and nearly identical at 19.6% and 19.2%, respectively, in 56 patients treated with 400 mg/day of hydroxychloroquine and 64 patients who received placebo, Dr. Jacques-Eric Gottenberg reported at the annual meeting of the American College of Rheumatology.
Favorable overall response was defined as at least a 30% improvement between weeks 0 and 24 in the values on two of three visual analog scales for dryness, pain, and fatigue. Additionally, no significant differences were seen between the groups with respect to evolution of systemic disease activity, dryness, or quality of life, and no significant differences were observed between patients with anti-SSA/SSB autoantibodies; high IgG levels; or systemic, skin, or articular involvement at enrollment, said Dr. Gottenberg of Strasbourg (France) University Hospital.
Among those in the active treatment group, however, a trend toward decreased serum IgG was noted – from 15.5 g/L at enrollment to 13.4 g/L at week 24, compared with 14.2 g/L to 13.0 g/L in the placebo arm. Also, a significant decrease of IgM – from 1.3 g/L to 1.1 g/L vs. no change from 1.4 g/L in the placebo arm – was seen.
Patients included in the study were mostly women (91.7%) with a mean age of 56 years and a median disease duration of 5 years. About 55% had anti-SSA positivity, and nearly a third (30%) had systemic disease involvement at enrollment. The patients’ median EULAR Sjögren’s Syndrome Disease Activity Index (ESSDAI) and EULAR Sjögren’s Syndrome Patient Reported Index (ESSPRI) scores were 2 and 6.3, respectively.
All patients fulfilled the European-American consensus group criteria for primary Sjögren’s syndrome, and all but one patient in the treatment arm had detectable blood levels of hydroxychloroquine at 6 months, indicating a high level of compliance with the study protocol, Dr. Gottenberg said.
The evolution of systemic disease was measured using the ESSDAI and ESSPRI scores; dryness was measured using Schirmer’s test and unstimulated salivary flow; and quality of life was measured using the short form health survey (SF-36), the Hospital Anxiety and Depression Scale, the Profile of Fatigue and Discomfort scale, and the Sicca Symptoms Inventory.
The findings are important given the frequency at which hydroxychloroquine is prescribed in patients with primary Sjögren’s syndrome. For example, at the time of enrollment in the Assessment of Systemic Signs and Evolution of Primary Sjögren’s Syndrome (ASSESS) prospective cohort, 56% of 395 patients had been or were being treated with hydroxychloroquine, Dr. Gottenberg said, noting that the drug is most often prescribed for arthralgias, synovitis, or purpura but is also prescribed for dryness and fatigue.
Despite the extensive use of hydroxychloroquine in these patients, few studies of its efficacy have been conducted. Except for one small, crossover trial involving only 19 patients, no controlled trials have compared hydroxychloroquine and placebo, he said.
The crossover trial was negative, except for demonstrating beneficial effects on erythrocyte sedimentation rate and IgG and IgM levels.
The current study raises questions about the value of short-term hydroxychloroquine treatment in patients with primary Sjögren’s syndrome, but it does not address the possibility of benefit with long-term treatment. Additionally, analyses are ongoing to determine if treatment has any therapeutic effect in patients with an interferon signature, he said.
Dr. Gottenberg and his colleagues had no disclosures to report.
WASHINGTON – Hydroxychloroquine had no short-term efficacy for primary Sjögren’s syndrome in a randomized, double-blind, placebo-controlled trial involving 120 patients.
The favorable overall response rate after 6 months was low and nearly identical at 19.6% and 19.2%, respectively, in 56 patients treated with 400 mg/day of hydroxychloroquine and 64 patients who received placebo, Dr. Jacques-Eric Gottenberg reported at the annual meeting of the American College of Rheumatology.
Favorable overall response was defined as at least a 30% improvement between weeks 0 and 24 in the values on two of three visual analog scales for dryness, pain, and fatigue. Additionally, no significant differences were seen between the groups with respect to evolution of systemic disease activity, dryness, or quality of life, and no significant differences were observed between patients with anti-SSA/SSB autoantibodies; high IgG levels; or systemic, skin, or articular involvement at enrollment, said Dr. Gottenberg of Strasbourg (France) University Hospital.
Among those in the active treatment group, however, a trend toward decreased serum IgG was noted – from 15.5 g/L at enrollment to 13.4 g/L at week 24, compared with 14.2 g/L to 13.0 g/L in the placebo arm. Also, a significant decrease of IgM – from 1.3 g/L to 1.1 g/L vs. no change from 1.4 g/L in the placebo arm – was seen.
Patients included in the study were mostly women (91.7%) with a mean age of 56 years and a median disease duration of 5 years. About 55% had anti-SSA positivity, and nearly a third (30%) had systemic disease involvement at enrollment. The patients’ median EULAR Sjögren’s Syndrome Disease Activity Index (ESSDAI) and EULAR Sjögren’s Syndrome Patient Reported Index (ESSPRI) scores were 2 and 6.3, respectively.
All patients fulfilled the European-American consensus group criteria for primary Sjögren’s syndrome, and all but one patient in the treatment arm had detectable blood levels of hydroxychloroquine at 6 months, indicating a high level of compliance with the study protocol, Dr. Gottenberg said.
The evolution of systemic disease was measured using the ESSDAI and ESSPRI scores; dryness was measured using Schirmer’s test and unstimulated salivary flow; and quality of life was measured using the short form health survey (SF-36), the Hospital Anxiety and Depression Scale, the Profile of Fatigue and Discomfort scale, and the Sicca Symptoms Inventory.
The findings are important given the frequency at which hydroxychloroquine is prescribed in patients with primary Sjögren’s syndrome. For example, at the time of enrollment in the Assessment of Systemic Signs and Evolution of Primary Sjögren’s Syndrome (ASSESS) prospective cohort, 56% of 395 patients had been or were being treated with hydroxychloroquine, Dr. Gottenberg said, noting that the drug is most often prescribed for arthralgias, synovitis, or purpura but is also prescribed for dryness and fatigue.
Despite the extensive use of hydroxychloroquine in these patients, few studies of its efficacy have been conducted. Except for one small, crossover trial involving only 19 patients, no controlled trials have compared hydroxychloroquine and placebo, he said.
The crossover trial was negative, except for demonstrating beneficial effects on erythrocyte sedimentation rate and IgG and IgM levels.
The current study raises questions about the value of short-term hydroxychloroquine treatment in patients with primary Sjögren’s syndrome, but it does not address the possibility of benefit with long-term treatment. Additionally, analyses are ongoing to determine if treatment has any therapeutic effect in patients with an interferon signature, he said.
Dr. Gottenberg and his colleagues had no disclosures to report.
WASHINGTON – Hydroxychloroquine had no short-term efficacy for primary Sjögren’s syndrome in a randomized, double-blind, placebo-controlled trial involving 120 patients.
The favorable overall response rate after 6 months was low and nearly identical at 19.6% and 19.2%, respectively, in 56 patients treated with 400 mg/day of hydroxychloroquine and 64 patients who received placebo, Dr. Jacques-Eric Gottenberg reported at the annual meeting of the American College of Rheumatology.
Favorable overall response was defined as at least a 30% improvement between weeks 0 and 24 in the values on two of three visual analog scales for dryness, pain, and fatigue. Additionally, no significant differences were seen between the groups with respect to evolution of systemic disease activity, dryness, or quality of life, and no significant differences were observed between patients with anti-SSA/SSB autoantibodies; high IgG levels; or systemic, skin, or articular involvement at enrollment, said Dr. Gottenberg of Strasbourg (France) University Hospital.
Among those in the active treatment group, however, a trend toward decreased serum IgG was noted – from 15.5 g/L at enrollment to 13.4 g/L at week 24, compared with 14.2 g/L to 13.0 g/L in the placebo arm. Also, a significant decrease of IgM – from 1.3 g/L to 1.1 g/L vs. no change from 1.4 g/L in the placebo arm – was seen.
Patients included in the study were mostly women (91.7%) with a mean age of 56 years and a median disease duration of 5 years. About 55% had anti-SSA positivity, and nearly a third (30%) had systemic disease involvement at enrollment. The patients’ median EULAR Sjögren’s Syndrome Disease Activity Index (ESSDAI) and EULAR Sjögren’s Syndrome Patient Reported Index (ESSPRI) scores were 2 and 6.3, respectively.
All patients fulfilled the European-American consensus group criteria for primary Sjögren’s syndrome, and all but one patient in the treatment arm had detectable blood levels of hydroxychloroquine at 6 months, indicating a high level of compliance with the study protocol, Dr. Gottenberg said.
The evolution of systemic disease was measured using the ESSDAI and ESSPRI scores; dryness was measured using Schirmer’s test and unstimulated salivary flow; and quality of life was measured using the short form health survey (SF-36), the Hospital Anxiety and Depression Scale, the Profile of Fatigue and Discomfort scale, and the Sicca Symptoms Inventory.
The findings are important given the frequency at which hydroxychloroquine is prescribed in patients with primary Sjögren’s syndrome. For example, at the time of enrollment in the Assessment of Systemic Signs and Evolution of Primary Sjögren’s Syndrome (ASSESS) prospective cohort, 56% of 395 patients had been or were being treated with hydroxychloroquine, Dr. Gottenberg said, noting that the drug is most often prescribed for arthralgias, synovitis, or purpura but is also prescribed for dryness and fatigue.
Despite the extensive use of hydroxychloroquine in these patients, few studies of its efficacy have been conducted. Except for one small, crossover trial involving only 19 patients, no controlled trials have compared hydroxychloroquine and placebo, he said.
The crossover trial was negative, except for demonstrating beneficial effects on erythrocyte sedimentation rate and IgG and IgM levels.
The current study raises questions about the value of short-term hydroxychloroquine treatment in patients with primary Sjögren’s syndrome, but it does not address the possibility of benefit with long-term treatment. Additionally, analyses are ongoing to determine if treatment has any therapeutic effect in patients with an interferon signature, he said.
Dr. Gottenberg and his colleagues had no disclosures to report.
AT THE ANNUAL MEETING OF THE AMERICAN COLLEGE OF RHEUMATOLOGY
Major Finding: The favorable overall response rate after 6 months was 19.6% for treatment with hydroxychloroquine and 19.2% with placebo.
Data Source: Randomized, double-blind, controlled trial of 400 mg/day hydroxychloroquine vs. placebo in 120 patients.
Disclosures: Dr. Gottenberg and his colleagues had no disclosures to report.
New and emerging therapies for malignant pleural disease
ATLANTA – New treatment approaches are emerging in the treatment of malignant pleural disease.
Until recently, talc pleurodesis, the standard of care, and repeated thoracentesis were the only options for treating symptomatic patients with malignant pleural disease established by cytology or biopsy, Dr. Najib Rahman said at the annual meeting of the American College of Chest Physicians.
"We need more novel, less toxic, and more effective agents," Dr. Rahman said, noting that these are exciting and important areas of research, especially given how common malignant pleural disease is – and how the incidence is increasing because of the aging of the population.
One newer option is the use of an indwelling catheter, said Dr. Rahman of the University of Oxford (England). "We can completely bypass the whole idea of pleurodesis and go for an indwelling catheter." As for the continued use of talc pleurodesis, the focus should be on identifying the best agents and improving upon current practices.
"All of us feel talc isn’t as good as it could be," he said, noting that the procedure is painful and is associated with various toxicities.
Nonetheless, talc pleurodesis is considered the most effective agent for the treatment of patients with malignant pleural effusion, and data suggest that the success rate is about 75%.
In a meta-analysis of 46 randomized controlled trials comprising more than 2,000 patients, talc was shown to be superior to bleomycin and tetracycline (risk ratios of 0.63 and 0.50, respectively).
However, some questions remain about how to best use talc pleurodesis. For example, it is unclear whether poudrage or slurry is the best approach for instillation, he said. Further, talc is associated with significant toxicity; 8 (4%) of 196 patients in one study experienced acute respiratory distress syndrome and 5 of those patients died, and 41 of 4,030 patients (1%) in another study experienced acute respiratory failure.
Although studies have suggested better safety with graded talc (French talc), compared with non-graded talc (U.S. talc), limitations of those studies raise questions about the findings. Also lacking with respect to talc is information on the best analgesic strategy, appropriate tube size, and predictors of outcomes, he said.
Newer options under consideration for pleurodesis include the bacterial proteins OK-432, staphylococcal super antigen, and Lipoteichoic Acid (LTAT).
Bacterial proteins are promising for pleurodesis because they are proinflammatory and potentially less toxic than other agents.
OK-432, or Picabinil, is a bacterial protein commonly used in Japan (where talc is not available), but not yet available in the western hemisphere, Dr. Rahman said.
In a single randomized controlled trial, the radiological complete response rate in 23 treated patients was 73%, compared with 41% for those treated with mitomycin C. OK-432 was associated with a longer effusion-free survival (7 months vs. 1.5 months) but was also associated with greater toxicity.
"So, clearly there are some interesting ideas there, but certainly no definitive data," he said.
Staphylococcal super antigen has been shown to induce cytotoxic T-cell differentiation in animal models of melanoma, and is associated with anti-tumor cytokine production, as well as with evidence of tumor regression and metastasis treatment. The complete response rate was 79% in one small study in 14 consecutive patients with non–small cell lung cancer. Patients were treated with repeated intrapleural instillation of staphylococcal super antigen at 100-400 pg once or twice per week until effusion resolved.
Furthermore, median survival was 2.0 months for 13 patients with malignant pleural effusion treated with talc pleurodesis, compared with 7.9 months for 14 patients treated with staphylococcal super antigen. While this is not comparative data, the survival with staphylococcal super antigen was better than one might expect in this patient population.
"Potentially there are some interesting signals here that might suggest this stuff may do more than just seal the pleural space, and may help to regress the cancer," Dr. Rahman said.
LTAT also shows promise. It has various immune effects, including activating toll-like receptor pathways. In a dose escalation study, he and his colleagues found that at 1-month follow-up, the overall success rate was 75%, while the success rate among those receiving greater than 750 mcg of LTAT was 86%, suggesting that this treatment is "doing something to pleural fluid production," he said.
No significant toxicity occurred at doses below 3,000 mcg. This early evidence of efficacy requires confirmation in additional studies, he said.
Another innovative area with respect to the treatment of malignant pleural disease involves the direct biological control of pleural fluid production with profibrotic cytokines such as TGF-beta.
"So rather than sealing the cavity, this is turning off the tap at the source," Dr. Rahman said.
Although this approach has not yet been studied in humans, it has significant potential advantages including low toxicity and robust pleurodesis. Also, it is not affected by steroids. "I think maybe in the next 5 or 10 years this will be an interesting area of research," he said.
Direct biological manipulation with anti-angiogenic agents such as zolendronic acid also is an important area of research, as is gene therapy and immune therapy for cancer control.
Currently, about 300,000 cases occur in the United Kingdom and the United States each year, and an estimated 100,000 additional cases each year are expected by 2055. The average hospital will see about 250 new cases per year, he said.
Dr. Rahman has received drugs and matched placebos for clinical trials, technical equipment for trials, and/or funding for trials or research from Roche, Genentech, Boehringer, Lunamed, Syder-Med, Rocket Medical UK, GE Medical, NIHR, HTA Trials, MRC, UKCRN, CRUK, BLF, and UNKRCI. He has also served as a consultant to Rocket Medical.
ATLANTA – New treatment approaches are emerging in the treatment of malignant pleural disease.
Until recently, talc pleurodesis, the standard of care, and repeated thoracentesis were the only options for treating symptomatic patients with malignant pleural disease established by cytology or biopsy, Dr. Najib Rahman said at the annual meeting of the American College of Chest Physicians.
"We need more novel, less toxic, and more effective agents," Dr. Rahman said, noting that these are exciting and important areas of research, especially given how common malignant pleural disease is – and how the incidence is increasing because of the aging of the population.
One newer option is the use of an indwelling catheter, said Dr. Rahman of the University of Oxford (England). "We can completely bypass the whole idea of pleurodesis and go for an indwelling catheter." As for the continued use of talc pleurodesis, the focus should be on identifying the best agents and improving upon current practices.
"All of us feel talc isn’t as good as it could be," he said, noting that the procedure is painful and is associated with various toxicities.
Nonetheless, talc pleurodesis is considered the most effective agent for the treatment of patients with malignant pleural effusion, and data suggest that the success rate is about 75%.
In a meta-analysis of 46 randomized controlled trials comprising more than 2,000 patients, talc was shown to be superior to bleomycin and tetracycline (risk ratios of 0.63 and 0.50, respectively).
However, some questions remain about how to best use talc pleurodesis. For example, it is unclear whether poudrage or slurry is the best approach for instillation, he said. Further, talc is associated with significant toxicity; 8 (4%) of 196 patients in one study experienced acute respiratory distress syndrome and 5 of those patients died, and 41 of 4,030 patients (1%) in another study experienced acute respiratory failure.
Although studies have suggested better safety with graded talc (French talc), compared with non-graded talc (U.S. talc), limitations of those studies raise questions about the findings. Also lacking with respect to talc is information on the best analgesic strategy, appropriate tube size, and predictors of outcomes, he said.
Newer options under consideration for pleurodesis include the bacterial proteins OK-432, staphylococcal super antigen, and Lipoteichoic Acid (LTAT).
Bacterial proteins are promising for pleurodesis because they are proinflammatory and potentially less toxic than other agents.
OK-432, or Picabinil, is a bacterial protein commonly used in Japan (where talc is not available), but not yet available in the western hemisphere, Dr. Rahman said.
In a single randomized controlled trial, the radiological complete response rate in 23 treated patients was 73%, compared with 41% for those treated with mitomycin C. OK-432 was associated with a longer effusion-free survival (7 months vs. 1.5 months) but was also associated with greater toxicity.
"So, clearly there are some interesting ideas there, but certainly no definitive data," he said.
Staphylococcal super antigen has been shown to induce cytotoxic T-cell differentiation in animal models of melanoma, and is associated with anti-tumor cytokine production, as well as with evidence of tumor regression and metastasis treatment. The complete response rate was 79% in one small study in 14 consecutive patients with non–small cell lung cancer. Patients were treated with repeated intrapleural instillation of staphylococcal super antigen at 100-400 pg once or twice per week until effusion resolved.
Furthermore, median survival was 2.0 months for 13 patients with malignant pleural effusion treated with talc pleurodesis, compared with 7.9 months for 14 patients treated with staphylococcal super antigen. While this is not comparative data, the survival with staphylococcal super antigen was better than one might expect in this patient population.
"Potentially there are some interesting signals here that might suggest this stuff may do more than just seal the pleural space, and may help to regress the cancer," Dr. Rahman said.
LTAT also shows promise. It has various immune effects, including activating toll-like receptor pathways. In a dose escalation study, he and his colleagues found that at 1-month follow-up, the overall success rate was 75%, while the success rate among those receiving greater than 750 mcg of LTAT was 86%, suggesting that this treatment is "doing something to pleural fluid production," he said.
No significant toxicity occurred at doses below 3,000 mcg. This early evidence of efficacy requires confirmation in additional studies, he said.
Another innovative area with respect to the treatment of malignant pleural disease involves the direct biological control of pleural fluid production with profibrotic cytokines such as TGF-beta.
"So rather than sealing the cavity, this is turning off the tap at the source," Dr. Rahman said.
Although this approach has not yet been studied in humans, it has significant potential advantages including low toxicity and robust pleurodesis. Also, it is not affected by steroids. "I think maybe in the next 5 or 10 years this will be an interesting area of research," he said.
Direct biological manipulation with anti-angiogenic agents such as zolendronic acid also is an important area of research, as is gene therapy and immune therapy for cancer control.
Currently, about 300,000 cases occur in the United Kingdom and the United States each year, and an estimated 100,000 additional cases each year are expected by 2055. The average hospital will see about 250 new cases per year, he said.
Dr. Rahman has received drugs and matched placebos for clinical trials, technical equipment for trials, and/or funding for trials or research from Roche, Genentech, Boehringer, Lunamed, Syder-Med, Rocket Medical UK, GE Medical, NIHR, HTA Trials, MRC, UKCRN, CRUK, BLF, and UNKRCI. He has also served as a consultant to Rocket Medical.
ATLANTA – New treatment approaches are emerging in the treatment of malignant pleural disease.
Until recently, talc pleurodesis, the standard of care, and repeated thoracentesis were the only options for treating symptomatic patients with malignant pleural disease established by cytology or biopsy, Dr. Najib Rahman said at the annual meeting of the American College of Chest Physicians.
"We need more novel, less toxic, and more effective agents," Dr. Rahman said, noting that these are exciting and important areas of research, especially given how common malignant pleural disease is – and how the incidence is increasing because of the aging of the population.
One newer option is the use of an indwelling catheter, said Dr. Rahman of the University of Oxford (England). "We can completely bypass the whole idea of pleurodesis and go for an indwelling catheter." As for the continued use of talc pleurodesis, the focus should be on identifying the best agents and improving upon current practices.
"All of us feel talc isn’t as good as it could be," he said, noting that the procedure is painful and is associated with various toxicities.
Nonetheless, talc pleurodesis is considered the most effective agent for the treatment of patients with malignant pleural effusion, and data suggest that the success rate is about 75%.
In a meta-analysis of 46 randomized controlled trials comprising more than 2,000 patients, talc was shown to be superior to bleomycin and tetracycline (risk ratios of 0.63 and 0.50, respectively).
However, some questions remain about how to best use talc pleurodesis. For example, it is unclear whether poudrage or slurry is the best approach for instillation, he said. Further, talc is associated with significant toxicity; 8 (4%) of 196 patients in one study experienced acute respiratory distress syndrome and 5 of those patients died, and 41 of 4,030 patients (1%) in another study experienced acute respiratory failure.
Although studies have suggested better safety with graded talc (French talc), compared with non-graded talc (U.S. talc), limitations of those studies raise questions about the findings. Also lacking with respect to talc is information on the best analgesic strategy, appropriate tube size, and predictors of outcomes, he said.
Newer options under consideration for pleurodesis include the bacterial proteins OK-432, staphylococcal super antigen, and Lipoteichoic Acid (LTAT).
Bacterial proteins are promising for pleurodesis because they are proinflammatory and potentially less toxic than other agents.
OK-432, or Picabinil, is a bacterial protein commonly used in Japan (where talc is not available), but not yet available in the western hemisphere, Dr. Rahman said.
In a single randomized controlled trial, the radiological complete response rate in 23 treated patients was 73%, compared with 41% for those treated with mitomycin C. OK-432 was associated with a longer effusion-free survival (7 months vs. 1.5 months) but was also associated with greater toxicity.
"So, clearly there are some interesting ideas there, but certainly no definitive data," he said.
Staphylococcal super antigen has been shown to induce cytotoxic T-cell differentiation in animal models of melanoma, and is associated with anti-tumor cytokine production, as well as with evidence of tumor regression and metastasis treatment. The complete response rate was 79% in one small study in 14 consecutive patients with non–small cell lung cancer. Patients were treated with repeated intrapleural instillation of staphylococcal super antigen at 100-400 pg once or twice per week until effusion resolved.
Furthermore, median survival was 2.0 months for 13 patients with malignant pleural effusion treated with talc pleurodesis, compared with 7.9 months for 14 patients treated with staphylococcal super antigen. While this is not comparative data, the survival with staphylococcal super antigen was better than one might expect in this patient population.
"Potentially there are some interesting signals here that might suggest this stuff may do more than just seal the pleural space, and may help to regress the cancer," Dr. Rahman said.
LTAT also shows promise. It has various immune effects, including activating toll-like receptor pathways. In a dose escalation study, he and his colleagues found that at 1-month follow-up, the overall success rate was 75%, while the success rate among those receiving greater than 750 mcg of LTAT was 86%, suggesting that this treatment is "doing something to pleural fluid production," he said.
No significant toxicity occurred at doses below 3,000 mcg. This early evidence of efficacy requires confirmation in additional studies, he said.
Another innovative area with respect to the treatment of malignant pleural disease involves the direct biological control of pleural fluid production with profibrotic cytokines such as TGF-beta.
"So rather than sealing the cavity, this is turning off the tap at the source," Dr. Rahman said.
Although this approach has not yet been studied in humans, it has significant potential advantages including low toxicity and robust pleurodesis. Also, it is not affected by steroids. "I think maybe in the next 5 or 10 years this will be an interesting area of research," he said.
Direct biological manipulation with anti-angiogenic agents such as zolendronic acid also is an important area of research, as is gene therapy and immune therapy for cancer control.
Currently, about 300,000 cases occur in the United Kingdom and the United States each year, and an estimated 100,000 additional cases each year are expected by 2055. The average hospital will see about 250 new cases per year, he said.
Dr. Rahman has received drugs and matched placebos for clinical trials, technical equipment for trials, and/or funding for trials or research from Roche, Genentech, Boehringer, Lunamed, Syder-Med, Rocket Medical UK, GE Medical, NIHR, HTA Trials, MRC, UKCRN, CRUK, BLF, and UNKRCI. He has also served as a consultant to Rocket Medical.
EXPERT ANALYSIS FROM THE ANNUAL MEETING OF THE AMERICAN COLLEGE OF CHEST PHYSICIANS
Project provides simplified approach to sepsis for rural hospitals
ATLANTA – A Kansas-based program that aims to improve sepsis-related outcomes in rural hospital settings is proving successful and could serve as a model for rural hospitals nationwide.
The program, known as "The Kansas Sepsis Project," was initiated by the Midwest Critical Care Collaborative, and focuses on a simplified approach to sepsis resuscitation for the purpose of reducing sepsis mortality, Dr. Steven Q. Simpson reported at the annual meeting of the American College of Chest Physicians.
Sepsis affects more than 10,000 Kansans each year, and the sepsis-related mortality rate is 30%-50% in most Kansas hospitals, which exceeds the mortality rate associated with acute myocardial infarction, said Dr. Simpson of the University of Kansas Medical Center, Kansas City.
One goal of the sepsis project is to reduce that rate by 10% by the end of 2015.
According to the Midwest Critical Care Collaborative website, a 20% reduction is possible if specific plans for recognition and treatment as outlined by the project are put in place.
The project, which is open to any interested facility including those not based in Kansas, involves baseline surveys, live and online training, ongoing data collection and analysis, formation of performance improvement planning based on those analyses, and – hopefully – changed behavior and reduced sepsis mortality, said Dr. Simpson.
The website states that participants learn to:
• Recognize cardinal features of severe sepsis.
• Initiate rapid, organized care for severe sepsis.
• Evaluate in-house data for recognizing and caring for severe sepsis patients.
• Initiate a performance improvement program, and improve outcomes for patients with severe sepsis.
Participants also have access to useful Web-based tools, such as a severe sepsis screener and a severe sepsis tracker for small hospitals, both of which help to ensure that proper protocols are followed, and that data are tracked.
A severe sepsis protocol for emergency management in small, referring hospitals states that whenever possible, nine steps should be completed within 2 hours for patients with infection, systemic inflammatory response syndrome, and dysfunction of one or more organs. The steps are, if possible:
• Draw blood for serum lactate measurement.
• Draw two sets of blood cultures – before antibiotics are initiated, if possible; however, do not delay antibiotics for the sake of completing this step.
• Start two peripheral intravenous lines (use 18 gauge or larger).
• Initiate broad-spectrum antibiotics as soon as possible.
• Give 2 L of normal saline solution or lactated Ringer’s solution, wide open.
• Draw blood for a complete blood count with a differential, basic chemistry panel if this has not already been done.
• Administer supplemental oxygen to maintain oxygen saturation measured by pulse oximeter above 90%.
• Initiate norepinephrine or dopamine if shock is present. This maintains a mean arterial pressure of 65 mm Hg or greater. Continue intravenous crystalloid at 250 mL/hr.
• Transfer the patient if serum lactate is 4 mmol/L or greater, if systolic blood pressure remains below 90 mm Hg, or if mean arterial pressure is less than 60 mm Hg after 2 L of crystalloid. Place a central venous catheter only if this can be accomplished without delaying transfer.
Following this protocol and using the tools available through the project is leading to dramatic improvements in outcomes. At one hospital, for example, a review of 67 charts from 2009 and 2010 revealed that of 28 cases that met criteria for sepsis, none was identified as such.
Since the hospital entered the project, an additional 61 patients screened positive. Of those, 59 had the severe sepsis tracker completed, 56 had blood cultures drawn prior to administration of broad-spectrum antibiotics, and 57 received broad-spectrum antibiotics within 1 hour of presentation.
Additionally, 22 of the 59 patients for whom the severe sepsis tracker was completed had hypotension, and 18 of those received a 20-mL/kg fluid bolus within 2 hours of diagnosis.
Overall, 54 of the 59 patients who had the severe sepsis tracker completed survived their hospitalization. Only 2 of 35 patients with severe sepsis (5.7%) required transfer to a larger facility because of deterioration in their condition, compared with 7 of 28 patients (25%) in the group from the 2009-2010 preproject chart review.
Numerous states across the United States, especially in the Midwest and Northwest, have rural populations of less than 86 per square mile, similar to Kansas, with 1.330 small facilities serving rural populations located many miles from the nearest referral hospital, and could benefit from this approach to sepsis resuscitation, Dr. Simpson said.
The need for attention to the problem of sepsis is apparent not only based on the high mortality rates, but also in the outcomes of focus group research showing that only 42% of responding physicians from rural settings consider themselves to be "very knowledgeable" about sepsis diagnosis, treatments, and complications; while the same percentage consider themselves "not too knowledgeable," 4% say they are not at all knowledgeable, and 12% say they aren’t sure how knowledgeable they are, he said.
Similarly, only 2% of respondents said they are extremely knowledgeable about the differences among uncomplicated sepsis, severe sepsis, and septic shock; 27% said they are very knowledgeable; 61% said they are not too knowledgeable; 4% said they are not at all knowledgeable; and 6% said they are unsure how knowledgeable they are.
Few respondents were familiar with the Early Goal-Directed Therapy protocol or the Surviving Sepsis Campaign, and most admitted that the likelihood of missed sepsis diagnoses is high at their institution.
Most (about 85%) agreed that additional training would be extremely beneficial.
Although several challenges and hurdles exist with respect to improving sepsis outcomes in rural settings, including staffing issues, the lack of recognition of the extent of the problem, and the fact that sepsis is not yet a Joint Commission core measure, the results thus far of the Kansas Sepsis Project suggest positive change is within reach, Dr. Simpson said.
For more information about the project, click here.
The Kansas Sepsis Project is supported by the One Breath Foundation in the form of the Third Eli Lilly Distinguished Scholar in Critical Care Medicine Award. Dr. Simpson reported having no relevant financial disclosures.
ATLANTA – A Kansas-based program that aims to improve sepsis-related outcomes in rural hospital settings is proving successful and could serve as a model for rural hospitals nationwide.
The program, known as "The Kansas Sepsis Project," was initiated by the Midwest Critical Care Collaborative, and focuses on a simplified approach to sepsis resuscitation for the purpose of reducing sepsis mortality, Dr. Steven Q. Simpson reported at the annual meeting of the American College of Chest Physicians.
Sepsis affects more than 10,000 Kansans each year, and the sepsis-related mortality rate is 30%-50% in most Kansas hospitals, which exceeds the mortality rate associated with acute myocardial infarction, said Dr. Simpson of the University of Kansas Medical Center, Kansas City.
One goal of the sepsis project is to reduce that rate by 10% by the end of 2015.
According to the Midwest Critical Care Collaborative website, a 20% reduction is possible if specific plans for recognition and treatment as outlined by the project are put in place.
The project, which is open to any interested facility including those not based in Kansas, involves baseline surveys, live and online training, ongoing data collection and analysis, formation of performance improvement planning based on those analyses, and – hopefully – changed behavior and reduced sepsis mortality, said Dr. Simpson.
The website states that participants learn to:
• Recognize cardinal features of severe sepsis.
• Initiate rapid, organized care for severe sepsis.
• Evaluate in-house data for recognizing and caring for severe sepsis patients.
• Initiate a performance improvement program, and improve outcomes for patients with severe sepsis.
Participants also have access to useful Web-based tools, such as a severe sepsis screener and a severe sepsis tracker for small hospitals, both of which help to ensure that proper protocols are followed, and that data are tracked.
A severe sepsis protocol for emergency management in small, referring hospitals states that whenever possible, nine steps should be completed within 2 hours for patients with infection, systemic inflammatory response syndrome, and dysfunction of one or more organs. The steps are, if possible:
• Draw blood for serum lactate measurement.
• Draw two sets of blood cultures – before antibiotics are initiated, if possible; however, do not delay antibiotics for the sake of completing this step.
• Start two peripheral intravenous lines (use 18 gauge or larger).
• Initiate broad-spectrum antibiotics as soon as possible.
• Give 2 L of normal saline solution or lactated Ringer’s solution, wide open.
• Draw blood for a complete blood count with a differential, basic chemistry panel if this has not already been done.
• Administer supplemental oxygen to maintain oxygen saturation measured by pulse oximeter above 90%.
• Initiate norepinephrine or dopamine if shock is present. This maintains a mean arterial pressure of 65 mm Hg or greater. Continue intravenous crystalloid at 250 mL/hr.
• Transfer the patient if serum lactate is 4 mmol/L or greater, if systolic blood pressure remains below 90 mm Hg, or if mean arterial pressure is less than 60 mm Hg after 2 L of crystalloid. Place a central venous catheter only if this can be accomplished without delaying transfer.
Following this protocol and using the tools available through the project is leading to dramatic improvements in outcomes. At one hospital, for example, a review of 67 charts from 2009 and 2010 revealed that of 28 cases that met criteria for sepsis, none was identified as such.
Since the hospital entered the project, an additional 61 patients screened positive. Of those, 59 had the severe sepsis tracker completed, 56 had blood cultures drawn prior to administration of broad-spectrum antibiotics, and 57 received broad-spectrum antibiotics within 1 hour of presentation.
Additionally, 22 of the 59 patients for whom the severe sepsis tracker was completed had hypotension, and 18 of those received a 20-mL/kg fluid bolus within 2 hours of diagnosis.
Overall, 54 of the 59 patients who had the severe sepsis tracker completed survived their hospitalization. Only 2 of 35 patients with severe sepsis (5.7%) required transfer to a larger facility because of deterioration in their condition, compared with 7 of 28 patients (25%) in the group from the 2009-2010 preproject chart review.
Numerous states across the United States, especially in the Midwest and Northwest, have rural populations of less than 86 per square mile, similar to Kansas, with 1.330 small facilities serving rural populations located many miles from the nearest referral hospital, and could benefit from this approach to sepsis resuscitation, Dr. Simpson said.
The need for attention to the problem of sepsis is apparent not only based on the high mortality rates, but also in the outcomes of focus group research showing that only 42% of responding physicians from rural settings consider themselves to be "very knowledgeable" about sepsis diagnosis, treatments, and complications; while the same percentage consider themselves "not too knowledgeable," 4% say they are not at all knowledgeable, and 12% say they aren’t sure how knowledgeable they are, he said.
Similarly, only 2% of respondents said they are extremely knowledgeable about the differences among uncomplicated sepsis, severe sepsis, and septic shock; 27% said they are very knowledgeable; 61% said they are not too knowledgeable; 4% said they are not at all knowledgeable; and 6% said they are unsure how knowledgeable they are.
Few respondents were familiar with the Early Goal-Directed Therapy protocol or the Surviving Sepsis Campaign, and most admitted that the likelihood of missed sepsis diagnoses is high at their institution.
Most (about 85%) agreed that additional training would be extremely beneficial.
Although several challenges and hurdles exist with respect to improving sepsis outcomes in rural settings, including staffing issues, the lack of recognition of the extent of the problem, and the fact that sepsis is not yet a Joint Commission core measure, the results thus far of the Kansas Sepsis Project suggest positive change is within reach, Dr. Simpson said.
For more information about the project, click here.
The Kansas Sepsis Project is supported by the One Breath Foundation in the form of the Third Eli Lilly Distinguished Scholar in Critical Care Medicine Award. Dr. Simpson reported having no relevant financial disclosures.
ATLANTA – A Kansas-based program that aims to improve sepsis-related outcomes in rural hospital settings is proving successful and could serve as a model for rural hospitals nationwide.
The program, known as "The Kansas Sepsis Project," was initiated by the Midwest Critical Care Collaborative, and focuses on a simplified approach to sepsis resuscitation for the purpose of reducing sepsis mortality, Dr. Steven Q. Simpson reported at the annual meeting of the American College of Chest Physicians.
Sepsis affects more than 10,000 Kansans each year, and the sepsis-related mortality rate is 30%-50% in most Kansas hospitals, which exceeds the mortality rate associated with acute myocardial infarction, said Dr. Simpson of the University of Kansas Medical Center, Kansas City.
One goal of the sepsis project is to reduce that rate by 10% by the end of 2015.
According to the Midwest Critical Care Collaborative website, a 20% reduction is possible if specific plans for recognition and treatment as outlined by the project are put in place.
The project, which is open to any interested facility including those not based in Kansas, involves baseline surveys, live and online training, ongoing data collection and analysis, formation of performance improvement planning based on those analyses, and – hopefully – changed behavior and reduced sepsis mortality, said Dr. Simpson.
The website states that participants learn to:
• Recognize cardinal features of severe sepsis.
• Initiate rapid, organized care for severe sepsis.
• Evaluate in-house data for recognizing and caring for severe sepsis patients.
• Initiate a performance improvement program, and improve outcomes for patients with severe sepsis.
Participants also have access to useful Web-based tools, such as a severe sepsis screener and a severe sepsis tracker for small hospitals, both of which help to ensure that proper protocols are followed, and that data are tracked.
A severe sepsis protocol for emergency management in small, referring hospitals states that whenever possible, nine steps should be completed within 2 hours for patients with infection, systemic inflammatory response syndrome, and dysfunction of one or more organs. The steps are, if possible:
• Draw blood for serum lactate measurement.
• Draw two sets of blood cultures – before antibiotics are initiated, if possible; however, do not delay antibiotics for the sake of completing this step.
• Start two peripheral intravenous lines (use 18 gauge or larger).
• Initiate broad-spectrum antibiotics as soon as possible.
• Give 2 L of normal saline solution or lactated Ringer’s solution, wide open.
• Draw blood for a complete blood count with a differential, basic chemistry panel if this has not already been done.
• Administer supplemental oxygen to maintain oxygen saturation measured by pulse oximeter above 90%.
• Initiate norepinephrine or dopamine if shock is present. This maintains a mean arterial pressure of 65 mm Hg or greater. Continue intravenous crystalloid at 250 mL/hr.
• Transfer the patient if serum lactate is 4 mmol/L or greater, if systolic blood pressure remains below 90 mm Hg, or if mean arterial pressure is less than 60 mm Hg after 2 L of crystalloid. Place a central venous catheter only if this can be accomplished without delaying transfer.
Following this protocol and using the tools available through the project is leading to dramatic improvements in outcomes. At one hospital, for example, a review of 67 charts from 2009 and 2010 revealed that of 28 cases that met criteria for sepsis, none was identified as such.
Since the hospital entered the project, an additional 61 patients screened positive. Of those, 59 had the severe sepsis tracker completed, 56 had blood cultures drawn prior to administration of broad-spectrum antibiotics, and 57 received broad-spectrum antibiotics within 1 hour of presentation.
Additionally, 22 of the 59 patients for whom the severe sepsis tracker was completed had hypotension, and 18 of those received a 20-mL/kg fluid bolus within 2 hours of diagnosis.
Overall, 54 of the 59 patients who had the severe sepsis tracker completed survived their hospitalization. Only 2 of 35 patients with severe sepsis (5.7%) required transfer to a larger facility because of deterioration in their condition, compared with 7 of 28 patients (25%) in the group from the 2009-2010 preproject chart review.
Numerous states across the United States, especially in the Midwest and Northwest, have rural populations of less than 86 per square mile, similar to Kansas, with 1.330 small facilities serving rural populations located many miles from the nearest referral hospital, and could benefit from this approach to sepsis resuscitation, Dr. Simpson said.
The need for attention to the problem of sepsis is apparent not only based on the high mortality rates, but also in the outcomes of focus group research showing that only 42% of responding physicians from rural settings consider themselves to be "very knowledgeable" about sepsis diagnosis, treatments, and complications; while the same percentage consider themselves "not too knowledgeable," 4% say they are not at all knowledgeable, and 12% say they aren’t sure how knowledgeable they are, he said.
Similarly, only 2% of respondents said they are extremely knowledgeable about the differences among uncomplicated sepsis, severe sepsis, and septic shock; 27% said they are very knowledgeable; 61% said they are not too knowledgeable; 4% said they are not at all knowledgeable; and 6% said they are unsure how knowledgeable they are.
Few respondents were familiar with the Early Goal-Directed Therapy protocol or the Surviving Sepsis Campaign, and most admitted that the likelihood of missed sepsis diagnoses is high at their institution.
Most (about 85%) agreed that additional training would be extremely beneficial.
Although several challenges and hurdles exist with respect to improving sepsis outcomes in rural settings, including staffing issues, the lack of recognition of the extent of the problem, and the fact that sepsis is not yet a Joint Commission core measure, the results thus far of the Kansas Sepsis Project suggest positive change is within reach, Dr. Simpson said.
For more information about the project, click here.
The Kansas Sepsis Project is supported by the One Breath Foundation in the form of the Third Eli Lilly Distinguished Scholar in Critical Care Medicine Award. Dr. Simpson reported having no relevant financial disclosures.
AT THE ANNUAL MEETING OF THE AMERICAN COLLEGE OF CHEST PHYSICIANS
Recess Is In: Daily Play Cuts Childhood Obesity
SAN ANTONIO – Vigorous aerobic exercise performed for 20 or 40 minutes, 5 days per week, improved fitness and was associated with dose-dependent benefits on insulin resistance and general and visceral adiposity in a randomized controlled trial involving 222 children who were overweight or obese and sedentary.
The intensity of the exercise appeared to be the most important factor for improving aerobic fitness, but volume of exercise was important for reducing adiposity and diabetes risk, Catherine L. Davis, Ph.D., reported at the annual meeting of the Obesity Society.
Fitness, as measured using the adjusted mean difference in peak VO2, was similar for 73 children randomized to 40 minutes of daily exercise (the high-dose exercise group) and 71 children randomized to 20 minutes of daily exercise (the low-dose group). Fitness was significantly greater for exercise groups compared with 78 controls. The adjusted mean difference in peak VO2 was 2.4 mL/kg per minute from baseline to 13-weeks’ follow-up for both groups vs. the control group, said Dr. Davis of the Medical College of Georgia, Augusta.
Changes in body fat were measured using dual x-ray absorptiometry, and changes in visceral fat were measured using magnetic resonance imaging. The adjusted mean differences were -1.4% for the high-dose exercise group and -0.8% for the low-dose exercise group compared with controls. For visceral fat, the differences were -3.9% and -2.8%, respectively.
Reductions in the insulin area under the curve were measured using an oral glucose tolerance test. The adjusted mean difference was -3.56 x 103 microU/mL for the high-dose exercise group and -2.96 x 103 microU/mL for the low-dose exercise group compared with controls. There were no differences in outcomes based on sex or race.
The presentation of the findings coincided with their publication (JAMA 2012;308:1103-12).
Children in the study were aged 7-11 years (mean of 9.4 years) with an average body mass index of 26. Most (85%) were obese and 28% had prediabetes. The students were recruited from 15 public schools between 2003 and 2006, and were randomized to the high-dose or low-dose exercise groups or to a control group, Dr. Davis said. Six cohorts of 30-40 students participated during the study period.
Both the high- and low-dose groups exercised during an after-school program 5 days each week; exercise was vigorous, but game based, with an emphasis on intensity, fun, and safety rather than competition or skill enhancement. Average daily heart rate was calculated, and students earned bonus points for achieving a rate above 150 beats per minute. These points were used to "purchase" various prizes.
The control group did not participate in an after-school program but met monthly for a "lifestyle class," mainly for the purpose of maintaining contact for follow-up.
One-third of elementary school students in the United States are either overweight or obese, Dr. Davis said. The risk of diabetes in this population has increased as a result – often developing by puberty, with potentially dire consequences for long-term health. Prior to this study, dose-response data with respect to physical activity among children had been lacking.
"Even just 20 minutes of vigorous physical activity on a daily basis makes a big difference after just a few months," she said.
Recent data suggesting a benefit of such activity on cognition and math achievement also could convince schools to make efforts to offer daily exercise for children, she added.
This study was supported by grants from the National Institutes of Health and the Salvador de Madariaga Program of the Spanish Ministry of Education and Science. Dr. Davis and her colleagues reported having no conflicts of interest.
SAN ANTONIO – Vigorous aerobic exercise performed for 20 or 40 minutes, 5 days per week, improved fitness and was associated with dose-dependent benefits on insulin resistance and general and visceral adiposity in a randomized controlled trial involving 222 children who were overweight or obese and sedentary.
The intensity of the exercise appeared to be the most important factor for improving aerobic fitness, but volume of exercise was important for reducing adiposity and diabetes risk, Catherine L. Davis, Ph.D., reported at the annual meeting of the Obesity Society.
Fitness, as measured using the adjusted mean difference in peak VO2, was similar for 73 children randomized to 40 minutes of daily exercise (the high-dose exercise group) and 71 children randomized to 20 minutes of daily exercise (the low-dose group). Fitness was significantly greater for exercise groups compared with 78 controls. The adjusted mean difference in peak VO2 was 2.4 mL/kg per minute from baseline to 13-weeks’ follow-up for both groups vs. the control group, said Dr. Davis of the Medical College of Georgia, Augusta.
Changes in body fat were measured using dual x-ray absorptiometry, and changes in visceral fat were measured using magnetic resonance imaging. The adjusted mean differences were -1.4% for the high-dose exercise group and -0.8% for the low-dose exercise group compared with controls. For visceral fat, the differences were -3.9% and -2.8%, respectively.
Reductions in the insulin area under the curve were measured using an oral glucose tolerance test. The adjusted mean difference was -3.56 x 103 microU/mL for the high-dose exercise group and -2.96 x 103 microU/mL for the low-dose exercise group compared with controls. There were no differences in outcomes based on sex or race.
The presentation of the findings coincided with their publication (JAMA 2012;308:1103-12).
Children in the study were aged 7-11 years (mean of 9.4 years) with an average body mass index of 26. Most (85%) were obese and 28% had prediabetes. The students were recruited from 15 public schools between 2003 and 2006, and were randomized to the high-dose or low-dose exercise groups or to a control group, Dr. Davis said. Six cohorts of 30-40 students participated during the study period.
Both the high- and low-dose groups exercised during an after-school program 5 days each week; exercise was vigorous, but game based, with an emphasis on intensity, fun, and safety rather than competition or skill enhancement. Average daily heart rate was calculated, and students earned bonus points for achieving a rate above 150 beats per minute. These points were used to "purchase" various prizes.
The control group did not participate in an after-school program but met monthly for a "lifestyle class," mainly for the purpose of maintaining contact for follow-up.
One-third of elementary school students in the United States are either overweight or obese, Dr. Davis said. The risk of diabetes in this population has increased as a result – often developing by puberty, with potentially dire consequences for long-term health. Prior to this study, dose-response data with respect to physical activity among children had been lacking.
"Even just 20 minutes of vigorous physical activity on a daily basis makes a big difference after just a few months," she said.
Recent data suggesting a benefit of such activity on cognition and math achievement also could convince schools to make efforts to offer daily exercise for children, she added.
This study was supported by grants from the National Institutes of Health and the Salvador de Madariaga Program of the Spanish Ministry of Education and Science. Dr. Davis and her colleagues reported having no conflicts of interest.
SAN ANTONIO – Vigorous aerobic exercise performed for 20 or 40 minutes, 5 days per week, improved fitness and was associated with dose-dependent benefits on insulin resistance and general and visceral adiposity in a randomized controlled trial involving 222 children who were overweight or obese and sedentary.
The intensity of the exercise appeared to be the most important factor for improving aerobic fitness, but volume of exercise was important for reducing adiposity and diabetes risk, Catherine L. Davis, Ph.D., reported at the annual meeting of the Obesity Society.
Fitness, as measured using the adjusted mean difference in peak VO2, was similar for 73 children randomized to 40 minutes of daily exercise (the high-dose exercise group) and 71 children randomized to 20 minutes of daily exercise (the low-dose group). Fitness was significantly greater for exercise groups compared with 78 controls. The adjusted mean difference in peak VO2 was 2.4 mL/kg per minute from baseline to 13-weeks’ follow-up for both groups vs. the control group, said Dr. Davis of the Medical College of Georgia, Augusta.
Changes in body fat were measured using dual x-ray absorptiometry, and changes in visceral fat were measured using magnetic resonance imaging. The adjusted mean differences were -1.4% for the high-dose exercise group and -0.8% for the low-dose exercise group compared with controls. For visceral fat, the differences were -3.9% and -2.8%, respectively.
Reductions in the insulin area under the curve were measured using an oral glucose tolerance test. The adjusted mean difference was -3.56 x 103 microU/mL for the high-dose exercise group and -2.96 x 103 microU/mL for the low-dose exercise group compared with controls. There were no differences in outcomes based on sex or race.
The presentation of the findings coincided with their publication (JAMA 2012;308:1103-12).
Children in the study were aged 7-11 years (mean of 9.4 years) with an average body mass index of 26. Most (85%) were obese and 28% had prediabetes. The students were recruited from 15 public schools between 2003 and 2006, and were randomized to the high-dose or low-dose exercise groups or to a control group, Dr. Davis said. Six cohorts of 30-40 students participated during the study period.
Both the high- and low-dose groups exercised during an after-school program 5 days each week; exercise was vigorous, but game based, with an emphasis on intensity, fun, and safety rather than competition or skill enhancement. Average daily heart rate was calculated, and students earned bonus points for achieving a rate above 150 beats per minute. These points were used to "purchase" various prizes.
The control group did not participate in an after-school program but met monthly for a "lifestyle class," mainly for the purpose of maintaining contact for follow-up.
One-third of elementary school students in the United States are either overweight or obese, Dr. Davis said. The risk of diabetes in this population has increased as a result – often developing by puberty, with potentially dire consequences for long-term health. Prior to this study, dose-response data with respect to physical activity among children had been lacking.
"Even just 20 minutes of vigorous physical activity on a daily basis makes a big difference after just a few months," she said.
Recent data suggesting a benefit of such activity on cognition and math achievement also could convince schools to make efforts to offer daily exercise for children, she added.
This study was supported by grants from the National Institutes of Health and the Salvador de Madariaga Program of the Spanish Ministry of Education and Science. Dr. Davis and her colleagues reported having no conflicts of interest.
AT THE ANNUAL MEETING OF THE OBESITY SOCIETY
Major Finding: Changes in body fat were -1.4% for children randomized to 40 minutes per day of exercise and -0.8% for children randomized to 20 minutes per day of exercise, compared with controls.
Data Source: This was a randomized controlled trial involving 222 children who were overweight or obese and sedentary.
Disclosures: This study was supported by grants from the National Institutes of Health and the Salvador de Madariaga Program of the Spanish Ministry of Education and Science. Dr. Davis and her colleagues reported having no conflicts of interest.
Ischemic Stroke Rates Same for Anti-TNFs vs. nbDMARDs in RA
WASHINGTON – Exposure to anti-tumor necrosis factor therapy does not appear to be associated with a greater short-term risk of ischemic stroke in patients with rheumatoid arthritis when compared with exposure to nonbiologic disease-modifying antirheumatic drug therapy, according to findings from the British Society for Rheumatology Biologics Register-Rheumatoid Arthritis.
Of 130 verified incident ischemic cerebrovascular accidents that occurred among participants in that large prospective cohort study of RA patients, 109 occurred in 11,642 patients treated with anti–tumor necrosis factor drugs (anti-TNFs) for an incidence rate of 178/100,000 person-years, and 21 occurred in 3,271 patients in a comparator group of biologic-naive patients who had been treated with only nonbiologic disease-modifying antirheumatic drugs (nbDMARDs) for an incident rate of 175/100,000 person-years, Dr. Audrey S. Low reported at the annual meeting of the American College of Rheumatology.
The incident rates did not differ significantly, and no association was seen between ever exposure to anti-TNF drugs and ischemic stroke risk after adjustment for confounders using a propensity score based on age, sex, ethnicity, body mass index, disease activity score, disease duration, Health Assessment Questionnaire score, prior nbDMARD use, steroid use at baseline, year of entry to the study, smoking, baseline drugs, and history of cancer, hypertension, ischemic heart disease, diabetes, depression, and chronic lung disease (hazard ratio, 0.88), said Dr. Low of the University of Manchester (England).
Patients in the British Society for Rheumatology Biologics Register–Rheumatoid Arthritis (BSRBR-RA) were recruited during 2001-2008 and were followed semiannually for 3 years, then annually thereafter. All serious adverse events, such as stroke, and all drug therapy were reported. Events reported through Oct. 21, 2010, were included in this analysis.
The investigators also linked study subjects to the national death register and collected information from medical records; a concerted effort was made to classify stroke types.
The anti-TNF and nbDMARD groups differed with respect to several factors: The anti-TNF cohort was younger, included more women, and had higher disease activity, longer disease duration, and higher levels of disability. That cohort also used more DMARDs, more steroids, and more nonsteroidal cyclo-oxygenase-2 (COX-2) inhibitors. However, the rates of hypertension and diabetes were similar in the anti-TNF and nbDMARD cohorts.
This study is among the largest to show that anti-TNF therapy does not increase stroke risk in RA patients, when compared with nbDMARDS, Dr. Low said.
"We know that patients with RA are at risk of increased cardiovascular morbidity and mortality, and that includes stroke," she said, noting that several other observational studies and meta-analyses have demonstrated an overall increase in that risk.
However, outcomes have varied in studies comparing anti-TNF–treated RA patients and controls, with some showing as much as a 60% increase in ischemic stroke risk and others demonstrating a 30% reduction in risk.
In this large cohort of European patients with RA, no association was seen between the short-term risk of ischemic stroke and the use of anti-TNF therapy, she said, adding that additional follow-up is needed to assess risk over time.
Dr. Low reported having no relevant financial disclosures.
WASHINGTON – Exposure to anti-tumor necrosis factor therapy does not appear to be associated with a greater short-term risk of ischemic stroke in patients with rheumatoid arthritis when compared with exposure to nonbiologic disease-modifying antirheumatic drug therapy, according to findings from the British Society for Rheumatology Biologics Register-Rheumatoid Arthritis.
Of 130 verified incident ischemic cerebrovascular accidents that occurred among participants in that large prospective cohort study of RA patients, 109 occurred in 11,642 patients treated with anti–tumor necrosis factor drugs (anti-TNFs) for an incidence rate of 178/100,000 person-years, and 21 occurred in 3,271 patients in a comparator group of biologic-naive patients who had been treated with only nonbiologic disease-modifying antirheumatic drugs (nbDMARDs) for an incident rate of 175/100,000 person-years, Dr. Audrey S. Low reported at the annual meeting of the American College of Rheumatology.
The incident rates did not differ significantly, and no association was seen between ever exposure to anti-TNF drugs and ischemic stroke risk after adjustment for confounders using a propensity score based on age, sex, ethnicity, body mass index, disease activity score, disease duration, Health Assessment Questionnaire score, prior nbDMARD use, steroid use at baseline, year of entry to the study, smoking, baseline drugs, and history of cancer, hypertension, ischemic heart disease, diabetes, depression, and chronic lung disease (hazard ratio, 0.88), said Dr. Low of the University of Manchester (England).
Patients in the British Society for Rheumatology Biologics Register–Rheumatoid Arthritis (BSRBR-RA) were recruited during 2001-2008 and were followed semiannually for 3 years, then annually thereafter. All serious adverse events, such as stroke, and all drug therapy were reported. Events reported through Oct. 21, 2010, were included in this analysis.
The investigators also linked study subjects to the national death register and collected information from medical records; a concerted effort was made to classify stroke types.
The anti-TNF and nbDMARD groups differed with respect to several factors: The anti-TNF cohort was younger, included more women, and had higher disease activity, longer disease duration, and higher levels of disability. That cohort also used more DMARDs, more steroids, and more nonsteroidal cyclo-oxygenase-2 (COX-2) inhibitors. However, the rates of hypertension and diabetes were similar in the anti-TNF and nbDMARD cohorts.
This study is among the largest to show that anti-TNF therapy does not increase stroke risk in RA patients, when compared with nbDMARDS, Dr. Low said.
"We know that patients with RA are at risk of increased cardiovascular morbidity and mortality, and that includes stroke," she said, noting that several other observational studies and meta-analyses have demonstrated an overall increase in that risk.
However, outcomes have varied in studies comparing anti-TNF–treated RA patients and controls, with some showing as much as a 60% increase in ischemic stroke risk and others demonstrating a 30% reduction in risk.
In this large cohort of European patients with RA, no association was seen between the short-term risk of ischemic stroke and the use of anti-TNF therapy, she said, adding that additional follow-up is needed to assess risk over time.
Dr. Low reported having no relevant financial disclosures.
WASHINGTON – Exposure to anti-tumor necrosis factor therapy does not appear to be associated with a greater short-term risk of ischemic stroke in patients with rheumatoid arthritis when compared with exposure to nonbiologic disease-modifying antirheumatic drug therapy, according to findings from the British Society for Rheumatology Biologics Register-Rheumatoid Arthritis.
Of 130 verified incident ischemic cerebrovascular accidents that occurred among participants in that large prospective cohort study of RA patients, 109 occurred in 11,642 patients treated with anti–tumor necrosis factor drugs (anti-TNFs) for an incidence rate of 178/100,000 person-years, and 21 occurred in 3,271 patients in a comparator group of biologic-naive patients who had been treated with only nonbiologic disease-modifying antirheumatic drugs (nbDMARDs) for an incident rate of 175/100,000 person-years, Dr. Audrey S. Low reported at the annual meeting of the American College of Rheumatology.
The incident rates did not differ significantly, and no association was seen between ever exposure to anti-TNF drugs and ischemic stroke risk after adjustment for confounders using a propensity score based on age, sex, ethnicity, body mass index, disease activity score, disease duration, Health Assessment Questionnaire score, prior nbDMARD use, steroid use at baseline, year of entry to the study, smoking, baseline drugs, and history of cancer, hypertension, ischemic heart disease, diabetes, depression, and chronic lung disease (hazard ratio, 0.88), said Dr. Low of the University of Manchester (England).
Patients in the British Society for Rheumatology Biologics Register–Rheumatoid Arthritis (BSRBR-RA) were recruited during 2001-2008 and were followed semiannually for 3 years, then annually thereafter. All serious adverse events, such as stroke, and all drug therapy were reported. Events reported through Oct. 21, 2010, were included in this analysis.
The investigators also linked study subjects to the national death register and collected information from medical records; a concerted effort was made to classify stroke types.
The anti-TNF and nbDMARD groups differed with respect to several factors: The anti-TNF cohort was younger, included more women, and had higher disease activity, longer disease duration, and higher levels of disability. That cohort also used more DMARDs, more steroids, and more nonsteroidal cyclo-oxygenase-2 (COX-2) inhibitors. However, the rates of hypertension and diabetes were similar in the anti-TNF and nbDMARD cohorts.
This study is among the largest to show that anti-TNF therapy does not increase stroke risk in RA patients, when compared with nbDMARDS, Dr. Low said.
"We know that patients with RA are at risk of increased cardiovascular morbidity and mortality, and that includes stroke," she said, noting that several other observational studies and meta-analyses have demonstrated an overall increase in that risk.
However, outcomes have varied in studies comparing anti-TNF–treated RA patients and controls, with some showing as much as a 60% increase in ischemic stroke risk and others demonstrating a 30% reduction in risk.
In this large cohort of European patients with RA, no association was seen between the short-term risk of ischemic stroke and the use of anti-TNF therapy, she said, adding that additional follow-up is needed to assess risk over time.
Dr. Low reported having no relevant financial disclosures.
AT THE ANNUAL MEETING OF THE AMERICAN COLLEGE OF RHEUMATOLOGY
Major Finding: Of 130 verified incident ischemic cerebrovascular accidents, 109 occurred in 11,642 patients treated with anti–tumor necrosis factor drugs for an incident rate of 178/100,000 person-years, and 21 occurred in 3,271 patients who had been treated with only nonbiologic disease-modifying antirheumatic drugs for an incident rate of 175/100,000 person-years. The incident rates did not differ significantly after adjustment for possible confounders (hazard ratio, 0.88).
Data Source: Data are from the British Society for Rheumatology Biologics Register–Rheumatoid Arthritis.
Disclosures: Dr. Low reported having no relevant financial disclosures.