User login
Sharon Worcester is an award-winning medical journalist for MDedge News. She has been with the company since 1996, first as the Southeast Bureau Chief (1996-2009) when the company was known as International Medical News Group, then as a freelance writer (2010-2015) before returning as a reporter in 2015. She previously worked as a daily newspaper reporter covering health and local government. Sharon currently reports primarily on oncology and hematology. She has a BA from Eckerd College and an MA in Mass Communication/Print Journalism from the University of Florida. Connect with her via LinkedIn and follow her on twitter @SW_MedReporter.
FDA committee recommends approval of tofacitinib for PsA
Convinced largely by encouraging efficacy data, the Food and Drug Administration’s Arthritis Advisory Committee voted overwhelmingly in favor of approval of tofacitinib for the treatment of adult patients with active psoriatic arthritis.
If approved by the FDA, which usually adheres to advisory committee recommendations, the oral inhibitor of Janus-associated kinases (JAK) would be the first JAK inhibitor approved for the treatment of psoriatic arthritis (PsA). Pfizer submitted supplemental new drug applications (sNDAs) for both tofacitinib tablets (Xeljanz) and tofacitinib extended-release tablets (Xeljanz XR) at a dose of 5 mg twice daily and 11 mg once daily, respectively and, despite some reservations with respect to adverse events and lack of evidence regarding inhibition of radiographic progression, the committee voted 10-1 in favor of approval at an Aug. 3 meeting.
“I voted yes and, although there are safety concerns, I feel like it’s nothing different than what we see with other biologics, and I want to make sure that patients have options,” said Jennifer Horonjeff, PhD, a research fellow and patient advocate with the Center for Immune Disease with Onset in Childhood at Columbia University Medical Center, New York, and a consumer representative on the committee.
Dr. Horonjeff added that she hopes there is continued conversation between the sponsor and the FDA on “what we can do to make patients aware of these risks.”
Similarly, committee member Daniel H. Solomon, MD, a professor of medicine at Harvard Medical School and chief of the section of clinical sciences in the divisions of rheumatology and pharmacoepidemiology at Brigham and Women’s Hospital, both in Boston, said he sees a “great opportunity for risk mitigation that the sponsor and the [FDA] can take together.”
“We have a clear risk, we have a clear strategy for mitigating the risk, and there are going to be a lot more people exposed to this drug with a known risk, so let’s do something about it,” Dr. Solomon said about a plan put forward by Pfizer, and discussed at some length, to mitigate risks through measures such as vaccination against herpes zoster and additional study.
Temporary voting member Steven Meisel, PharmD, system director of patient safety at Fairview Health Services in Minneapolis added: “These are nasty drugs, but I think those who use them understand that, and this is no different than any of the other nasty drugs in these categories.”
Diane Aronson, a patient representative and temporary voting member on the committee, cast the only vote against approval, citing concerns about the lack of inhibition of radiographic progression of the disease and about the infection risks in a vulnerable population.
Tofacitinib was initially approved in 2012 at a dose of 5 mg, twice daily, for the treatment of adults with moderately to severely active rheumatoid arthritis who had an inadequate response or intolerance to methotrexate. The extended-release formulation was approved in 2016 at a dose of 11 mg daily.
With respect to the current sNDAs, Pfizer presented data from two placebo-controlled phase 3 trials in patients with psoriatic arthritis. The FDA deemed these trials to be adequate and well-controlled, providing “corroborating evidence of the efficacy of tofacitinib for reducing signs and symptoms of PsA, based on the proportion of patients experiencing the American College of Rheumatology (ACR) 20% response criteria,” according to a report presented to the committee. The report also noted that both phase 3 trials provided evidence of improvement in physical function, but did not provide sufficient evidence that tofacitinib inhibits radiographic progression in PsA.
The report also stated that the safety profile of tofacitinib in PsA was consistent with that established in RA; risks include serious infections, opportunistic infections, malignancy, gastrointestinal perforation, and laboratory abnormalities, including elevations in low-density lipoprotein and triglycerides.
“No new safety signals were identified in PsA,” the report states.
Of note, the sNDAs do not include an indication for generalized psoriasis; an application for that indication was withdrawn in 2016, and Dr. Meisel cautioned against any “unintentional leakage of the use of this drug for generalized psoriasis.”
He and others also cautioned against any implied endorsement in labeling that the drug inhibits radiographic progression of PsA.
Two individuals who participated in the open public hearing portion of the meeting each urged the committee to recommend approval of the sNDAs, with one, Stephen Marmaras, manager of state and national advocacy for the Global Healthy Living Foundation, noting that the joint pain and stiffness associated with PsA are a primary concern of patients.
“Our members with psoriatic arthritis overwhelmingly prioritize joint pain and stiffness as the most bothersome symptoms they experience,” Mr. Marmaras said. “With that in mind, we were encouraged to read that tofacitinib has particularly notable efficacy in treating the joint symptoms of the disease in clinical trials.”
All voting advisory committee members were screened and cleared with respect to potential conflicts of interest.
Convinced largely by encouraging efficacy data, the Food and Drug Administration’s Arthritis Advisory Committee voted overwhelmingly in favor of approval of tofacitinib for the treatment of adult patients with active psoriatic arthritis.
If approved by the FDA, which usually adheres to advisory committee recommendations, the oral inhibitor of Janus-associated kinases (JAK) would be the first JAK inhibitor approved for the treatment of psoriatic arthritis (PsA). Pfizer submitted supplemental new drug applications (sNDAs) for both tofacitinib tablets (Xeljanz) and tofacitinib extended-release tablets (Xeljanz XR) at a dose of 5 mg twice daily and 11 mg once daily, respectively and, despite some reservations with respect to adverse events and lack of evidence regarding inhibition of radiographic progression, the committee voted 10-1 in favor of approval at an Aug. 3 meeting.
“I voted yes and, although there are safety concerns, I feel like it’s nothing different than what we see with other biologics, and I want to make sure that patients have options,” said Jennifer Horonjeff, PhD, a research fellow and patient advocate with the Center for Immune Disease with Onset in Childhood at Columbia University Medical Center, New York, and a consumer representative on the committee.
Dr. Horonjeff added that she hopes there is continued conversation between the sponsor and the FDA on “what we can do to make patients aware of these risks.”
Similarly, committee member Daniel H. Solomon, MD, a professor of medicine at Harvard Medical School and chief of the section of clinical sciences in the divisions of rheumatology and pharmacoepidemiology at Brigham and Women’s Hospital, both in Boston, said he sees a “great opportunity for risk mitigation that the sponsor and the [FDA] can take together.”
“We have a clear risk, we have a clear strategy for mitigating the risk, and there are going to be a lot more people exposed to this drug with a known risk, so let’s do something about it,” Dr. Solomon said about a plan put forward by Pfizer, and discussed at some length, to mitigate risks through measures such as vaccination against herpes zoster and additional study.
Temporary voting member Steven Meisel, PharmD, system director of patient safety at Fairview Health Services in Minneapolis added: “These are nasty drugs, but I think those who use them understand that, and this is no different than any of the other nasty drugs in these categories.”
Diane Aronson, a patient representative and temporary voting member on the committee, cast the only vote against approval, citing concerns about the lack of inhibition of radiographic progression of the disease and about the infection risks in a vulnerable population.
Tofacitinib was initially approved in 2012 at a dose of 5 mg, twice daily, for the treatment of adults with moderately to severely active rheumatoid arthritis who had an inadequate response or intolerance to methotrexate. The extended-release formulation was approved in 2016 at a dose of 11 mg daily.
With respect to the current sNDAs, Pfizer presented data from two placebo-controlled phase 3 trials in patients with psoriatic arthritis. The FDA deemed these trials to be adequate and well-controlled, providing “corroborating evidence of the efficacy of tofacitinib for reducing signs and symptoms of PsA, based on the proportion of patients experiencing the American College of Rheumatology (ACR) 20% response criteria,” according to a report presented to the committee. The report also noted that both phase 3 trials provided evidence of improvement in physical function, but did not provide sufficient evidence that tofacitinib inhibits radiographic progression in PsA.
The report also stated that the safety profile of tofacitinib in PsA was consistent with that established in RA; risks include serious infections, opportunistic infections, malignancy, gastrointestinal perforation, and laboratory abnormalities, including elevations in low-density lipoprotein and triglycerides.
“No new safety signals were identified in PsA,” the report states.
Of note, the sNDAs do not include an indication for generalized psoriasis; an application for that indication was withdrawn in 2016, and Dr. Meisel cautioned against any “unintentional leakage of the use of this drug for generalized psoriasis.”
He and others also cautioned against any implied endorsement in labeling that the drug inhibits radiographic progression of PsA.
Two individuals who participated in the open public hearing portion of the meeting each urged the committee to recommend approval of the sNDAs, with one, Stephen Marmaras, manager of state and national advocacy for the Global Healthy Living Foundation, noting that the joint pain and stiffness associated with PsA are a primary concern of patients.
“Our members with psoriatic arthritis overwhelmingly prioritize joint pain and stiffness as the most bothersome symptoms they experience,” Mr. Marmaras said. “With that in mind, we were encouraged to read that tofacitinib has particularly notable efficacy in treating the joint symptoms of the disease in clinical trials.”
All voting advisory committee members were screened and cleared with respect to potential conflicts of interest.
Convinced largely by encouraging efficacy data, the Food and Drug Administration’s Arthritis Advisory Committee voted overwhelmingly in favor of approval of tofacitinib for the treatment of adult patients with active psoriatic arthritis.
If approved by the FDA, which usually adheres to advisory committee recommendations, the oral inhibitor of Janus-associated kinases (JAK) would be the first JAK inhibitor approved for the treatment of psoriatic arthritis (PsA). Pfizer submitted supplemental new drug applications (sNDAs) for both tofacitinib tablets (Xeljanz) and tofacitinib extended-release tablets (Xeljanz XR) at a dose of 5 mg twice daily and 11 mg once daily, respectively and, despite some reservations with respect to adverse events and lack of evidence regarding inhibition of radiographic progression, the committee voted 10-1 in favor of approval at an Aug. 3 meeting.
“I voted yes and, although there are safety concerns, I feel like it’s nothing different than what we see with other biologics, and I want to make sure that patients have options,” said Jennifer Horonjeff, PhD, a research fellow and patient advocate with the Center for Immune Disease with Onset in Childhood at Columbia University Medical Center, New York, and a consumer representative on the committee.
Dr. Horonjeff added that she hopes there is continued conversation between the sponsor and the FDA on “what we can do to make patients aware of these risks.”
Similarly, committee member Daniel H. Solomon, MD, a professor of medicine at Harvard Medical School and chief of the section of clinical sciences in the divisions of rheumatology and pharmacoepidemiology at Brigham and Women’s Hospital, both in Boston, said he sees a “great opportunity for risk mitigation that the sponsor and the [FDA] can take together.”
“We have a clear risk, we have a clear strategy for mitigating the risk, and there are going to be a lot more people exposed to this drug with a known risk, so let’s do something about it,” Dr. Solomon said about a plan put forward by Pfizer, and discussed at some length, to mitigate risks through measures such as vaccination against herpes zoster and additional study.
Temporary voting member Steven Meisel, PharmD, system director of patient safety at Fairview Health Services in Minneapolis added: “These are nasty drugs, but I think those who use them understand that, and this is no different than any of the other nasty drugs in these categories.”
Diane Aronson, a patient representative and temporary voting member on the committee, cast the only vote against approval, citing concerns about the lack of inhibition of radiographic progression of the disease and about the infection risks in a vulnerable population.
Tofacitinib was initially approved in 2012 at a dose of 5 mg, twice daily, for the treatment of adults with moderately to severely active rheumatoid arthritis who had an inadequate response or intolerance to methotrexate. The extended-release formulation was approved in 2016 at a dose of 11 mg daily.
With respect to the current sNDAs, Pfizer presented data from two placebo-controlled phase 3 trials in patients with psoriatic arthritis. The FDA deemed these trials to be adequate and well-controlled, providing “corroborating evidence of the efficacy of tofacitinib for reducing signs and symptoms of PsA, based on the proportion of patients experiencing the American College of Rheumatology (ACR) 20% response criteria,” according to a report presented to the committee. The report also noted that both phase 3 trials provided evidence of improvement in physical function, but did not provide sufficient evidence that tofacitinib inhibits radiographic progression in PsA.
The report also stated that the safety profile of tofacitinib in PsA was consistent with that established in RA; risks include serious infections, opportunistic infections, malignancy, gastrointestinal perforation, and laboratory abnormalities, including elevations in low-density lipoprotein and triglycerides.
“No new safety signals were identified in PsA,” the report states.
Of note, the sNDAs do not include an indication for generalized psoriasis; an application for that indication was withdrawn in 2016, and Dr. Meisel cautioned against any “unintentional leakage of the use of this drug for generalized psoriasis.”
He and others also cautioned against any implied endorsement in labeling that the drug inhibits radiographic progression of PsA.
Two individuals who participated in the open public hearing portion of the meeting each urged the committee to recommend approval of the sNDAs, with one, Stephen Marmaras, manager of state and national advocacy for the Global Healthy Living Foundation, noting that the joint pain and stiffness associated with PsA are a primary concern of patients.
“Our members with psoriatic arthritis overwhelmingly prioritize joint pain and stiffness as the most bothersome symptoms they experience,” Mr. Marmaras said. “With that in mind, we were encouraged to read that tofacitinib has particularly notable efficacy in treating the joint symptoms of the disease in clinical trials.”
All voting advisory committee members were screened and cleared with respect to potential conflicts of interest.
FDA committee rejects sirukumab approval on safety concerns
Citing safety concerns, the Food and Drug Administration’s Arthritis Advisory Committee voted overwhelmingly against recommending FDA approval of the interleukin-6 inhibitor sirukumab for refractory rheumatoid arthritis.
Janssen Biotech submitted a biologics license application (BLA) for the monoclonal antibody, seeking an indication for adults with moderately to severely active rheumatoid arthritis (RA) who had an inadequate response or intolerance to one or more prior disease-modifying antirheumatic drugs, but despite agreeing unanimously that the data presented by the applicant provided substantial evidence of efficacy for this indication, the committee voted 12-1 against approval at an Aug. 2 meeting.
“I’m not sure whether the safety signal is of concern or not. I don’t think there’s enough data here to know that. It’s concerning, and it may be just noise, but it may also be real and I’m not willing to ... be supportive of the notion that it’s safe enough to take its place along with other biologicals,” said temporary voting member David T. Felson, MD, professor of medicine and public health at Boston University.
Similarly, temporary voting member Erica Brittain, PhD, said the mortality concerns swayed her vote.
“It was a very close call for me. I do think there’s a real argument to be made about bias in the analysis that shows some possibility of a difference. On the other hand, I just couldn’t get past the uncertainty, and when we’re talking about mortality it’s hard to dismiss that,” said Dr. Brittain, a mathematical statistician and deputy chief of the Biostatistics Research Branch at the National Institute of Allergy and Infectious Diseases.
Michael H. Weisman, MD, also a temporary voting member and chair of rheumatology at Cedars-Sinai Medical Center in Los Angeles, said that if the indication had been narrowed – perhaps to those who showed a biologic response – he would have voted “yes.”
Temporary voting member James Katz, MD, was the only committee member to vote in favor of approval.
“I actually voted yes because this drug doesn’t scare me any more than all the other drugs I use. I’m very scared by all the biological agents, and this is no different,” said Dr. Katz, director of the Rheumatology Fellowship and Training Branch at the National Institute of Arthritis and Musculoskeletal Diseases.
Sirukumab differs from two other approved monoclonal antibodies that target the IL-6 pathway for the treatment of patients with RA – tocilizumab (Actemra) and sarilumab (Kevzara) – in that it targets IL-6, while the others target the IL-6 receptor. This slight difference could make a difference for some highly refractory patients who had failed to respond to prior treatments, according to applicant presentations at the meeting.
The efficacy and safety of the agent were assessed in a phase 2 dose-ranging study, as well in three pivotal phase 3 studies. Two of the phase 3 studies compared 100 mg twice weekly and 50 mg four times weekly doses of subcutaneous sirukumab to placebo – which were shown to have similar efficacy for reducing the signs and symptoms of RA – and a third compared those two doses against adalimumab (Humira) and showed that it was not superior to adalimumab for efficacy.
One phase 3 placebo-controlled study involving 878 refractory patients was published in February in The Lancet and showed that sirukumab was associated with rapid and sustained improvements in RA signs and symptoms, physical function, and health status, as well as improvement in physical and mental well-being.
However, a safety signal – a trend of increased overall mortality with sirukumab vs. placebo – emerged from the studies. The mortality was mainly associated with major adverse cardiovascular events, infection, and malignancy.
Three speakers, including RA patients or patient representatives, participated in the open public hearing portion of the committee meeting, and all spoke in favor of approval of sirukumab, but ultimately the committee agreed that the limited benefits of the agent – given that it does not involve an entirely new mechanism of action – did not outweigh the unknowns regarding safety.
Committee chairperson Daniel H. Solomon, MD, professor of medicine at Harvard Medical School and chief of the section of clinical sciences at Brigham and Women’s Hospital, both in Boston, said longer-term outcomes data with a clear comparator are needed.
The FDA will now consider the committee’s recommendations in making its final determination regarding the BLA.
All voting advisory committee members were screened and cleared with respect to potential conflicts of interest.
Citing safety concerns, the Food and Drug Administration’s Arthritis Advisory Committee voted overwhelmingly against recommending FDA approval of the interleukin-6 inhibitor sirukumab for refractory rheumatoid arthritis.
Janssen Biotech submitted a biologics license application (BLA) for the monoclonal antibody, seeking an indication for adults with moderately to severely active rheumatoid arthritis (RA) who had an inadequate response or intolerance to one or more prior disease-modifying antirheumatic drugs, but despite agreeing unanimously that the data presented by the applicant provided substantial evidence of efficacy for this indication, the committee voted 12-1 against approval at an Aug. 2 meeting.
“I’m not sure whether the safety signal is of concern or not. I don’t think there’s enough data here to know that. It’s concerning, and it may be just noise, but it may also be real and I’m not willing to ... be supportive of the notion that it’s safe enough to take its place along with other biologicals,” said temporary voting member David T. Felson, MD, professor of medicine and public health at Boston University.
Similarly, temporary voting member Erica Brittain, PhD, said the mortality concerns swayed her vote.
“It was a very close call for me. I do think there’s a real argument to be made about bias in the analysis that shows some possibility of a difference. On the other hand, I just couldn’t get past the uncertainty, and when we’re talking about mortality it’s hard to dismiss that,” said Dr. Brittain, a mathematical statistician and deputy chief of the Biostatistics Research Branch at the National Institute of Allergy and Infectious Diseases.
Michael H. Weisman, MD, also a temporary voting member and chair of rheumatology at Cedars-Sinai Medical Center in Los Angeles, said that if the indication had been narrowed – perhaps to those who showed a biologic response – he would have voted “yes.”
Temporary voting member James Katz, MD, was the only committee member to vote in favor of approval.
“I actually voted yes because this drug doesn’t scare me any more than all the other drugs I use. I’m very scared by all the biological agents, and this is no different,” said Dr. Katz, director of the Rheumatology Fellowship and Training Branch at the National Institute of Arthritis and Musculoskeletal Diseases.
Sirukumab differs from two other approved monoclonal antibodies that target the IL-6 pathway for the treatment of patients with RA – tocilizumab (Actemra) and sarilumab (Kevzara) – in that it targets IL-6, while the others target the IL-6 receptor. This slight difference could make a difference for some highly refractory patients who had failed to respond to prior treatments, according to applicant presentations at the meeting.
The efficacy and safety of the agent were assessed in a phase 2 dose-ranging study, as well in three pivotal phase 3 studies. Two of the phase 3 studies compared 100 mg twice weekly and 50 mg four times weekly doses of subcutaneous sirukumab to placebo – which were shown to have similar efficacy for reducing the signs and symptoms of RA – and a third compared those two doses against adalimumab (Humira) and showed that it was not superior to adalimumab for efficacy.
One phase 3 placebo-controlled study involving 878 refractory patients was published in February in The Lancet and showed that sirukumab was associated with rapid and sustained improvements in RA signs and symptoms, physical function, and health status, as well as improvement in physical and mental well-being.
However, a safety signal – a trend of increased overall mortality with sirukumab vs. placebo – emerged from the studies. The mortality was mainly associated with major adverse cardiovascular events, infection, and malignancy.
Three speakers, including RA patients or patient representatives, participated in the open public hearing portion of the committee meeting, and all spoke in favor of approval of sirukumab, but ultimately the committee agreed that the limited benefits of the agent – given that it does not involve an entirely new mechanism of action – did not outweigh the unknowns regarding safety.
Committee chairperson Daniel H. Solomon, MD, professor of medicine at Harvard Medical School and chief of the section of clinical sciences at Brigham and Women’s Hospital, both in Boston, said longer-term outcomes data with a clear comparator are needed.
The FDA will now consider the committee’s recommendations in making its final determination regarding the BLA.
All voting advisory committee members were screened and cleared with respect to potential conflicts of interest.
Citing safety concerns, the Food and Drug Administration’s Arthritis Advisory Committee voted overwhelmingly against recommending FDA approval of the interleukin-6 inhibitor sirukumab for refractory rheumatoid arthritis.
Janssen Biotech submitted a biologics license application (BLA) for the monoclonal antibody, seeking an indication for adults with moderately to severely active rheumatoid arthritis (RA) who had an inadequate response or intolerance to one or more prior disease-modifying antirheumatic drugs, but despite agreeing unanimously that the data presented by the applicant provided substantial evidence of efficacy for this indication, the committee voted 12-1 against approval at an Aug. 2 meeting.
“I’m not sure whether the safety signal is of concern or not. I don’t think there’s enough data here to know that. It’s concerning, and it may be just noise, but it may also be real and I’m not willing to ... be supportive of the notion that it’s safe enough to take its place along with other biologicals,” said temporary voting member David T. Felson, MD, professor of medicine and public health at Boston University.
Similarly, temporary voting member Erica Brittain, PhD, said the mortality concerns swayed her vote.
“It was a very close call for me. I do think there’s a real argument to be made about bias in the analysis that shows some possibility of a difference. On the other hand, I just couldn’t get past the uncertainty, and when we’re talking about mortality it’s hard to dismiss that,” said Dr. Brittain, a mathematical statistician and deputy chief of the Biostatistics Research Branch at the National Institute of Allergy and Infectious Diseases.
Michael H. Weisman, MD, also a temporary voting member and chair of rheumatology at Cedars-Sinai Medical Center in Los Angeles, said that if the indication had been narrowed – perhaps to those who showed a biologic response – he would have voted “yes.”
Temporary voting member James Katz, MD, was the only committee member to vote in favor of approval.
“I actually voted yes because this drug doesn’t scare me any more than all the other drugs I use. I’m very scared by all the biological agents, and this is no different,” said Dr. Katz, director of the Rheumatology Fellowship and Training Branch at the National Institute of Arthritis and Musculoskeletal Diseases.
Sirukumab differs from two other approved monoclonal antibodies that target the IL-6 pathway for the treatment of patients with RA – tocilizumab (Actemra) and sarilumab (Kevzara) – in that it targets IL-6, while the others target the IL-6 receptor. This slight difference could make a difference for some highly refractory patients who had failed to respond to prior treatments, according to applicant presentations at the meeting.
The efficacy and safety of the agent were assessed in a phase 2 dose-ranging study, as well in three pivotal phase 3 studies. Two of the phase 3 studies compared 100 mg twice weekly and 50 mg four times weekly doses of subcutaneous sirukumab to placebo – which were shown to have similar efficacy for reducing the signs and symptoms of RA – and a third compared those two doses against adalimumab (Humira) and showed that it was not superior to adalimumab for efficacy.
One phase 3 placebo-controlled study involving 878 refractory patients was published in February in The Lancet and showed that sirukumab was associated with rapid and sustained improvements in RA signs and symptoms, physical function, and health status, as well as improvement in physical and mental well-being.
However, a safety signal – a trend of increased overall mortality with sirukumab vs. placebo – emerged from the studies. The mortality was mainly associated with major adverse cardiovascular events, infection, and malignancy.
Three speakers, including RA patients or patient representatives, participated in the open public hearing portion of the committee meeting, and all spoke in favor of approval of sirukumab, but ultimately the committee agreed that the limited benefits of the agent – given that it does not involve an entirely new mechanism of action – did not outweigh the unknowns regarding safety.
Committee chairperson Daniel H. Solomon, MD, professor of medicine at Harvard Medical School and chief of the section of clinical sciences at Brigham and Women’s Hospital, both in Boston, said longer-term outcomes data with a clear comparator are needed.
The FDA will now consider the committee’s recommendations in making its final determination regarding the BLA.
All voting advisory committee members were screened and cleared with respect to potential conflicts of interest.
Stopping statins after stroke may up recurrent stroke risk
Discontinuing statin therapy 3-6 months after a stroke may increase the risk of recurrent stroke within a year, according to findings from a large retrospective Taiwanese cohort study.
And being older or male in the Stroke Belt increases the likelihood that statins won’t be prescribed at all at the time of hospital discharge after a stroke, a separate cohort study from the United States suggests.
Both studies were reported online in the Journal of the American Heart Association.
Of 45,151 ischemic stroke patients from the Taiwan National Health Insurance Research Database who were on a moderate- or high-intensity statin within 90 days of discharge after an ischemic stroke between 2001 and 2012, 3,175 (7%) were on a reduced dosage by the 90- to 180-day period, and 8,353 (18.5%) were not on any statin by that period. After adjustment for numerous factors including age, sex, several comorbid conditions, and stroke severity index, discontinuation of statins was associated with an increased hazard of recurrent ischemic or hemorrhagic stroke (6.2% vs. 4.4%; adjusted hazard ratio [HR], 1.42), Meng Lee, MD, of Chang Gung Memorial Hospital, Chiayi Branch, Puzy, Taiwan and colleagues reported.
Discontinuation of statins was also linked to higher risks of ischemic stroke (5.6% vs. 3.9%, adjusted HR, 1.45), all-cause mortality (1.4% vs. 1%; adjusted HR, 1.37), all major events (7.8% vs. 5.6%, adjusted HR 1.38), and any hospitalization (31.7% vs. 27.1%; adjusted HR, 1.19), but had neutral effects on intracerebral hemorrhage and myocardial infarction.
“Reduced dosage statin therapy was not associated with increased risks of ischemic stroke, intracerebral hemorrhage, all-cause mortality, myocardial infarction, or all major events,” they said.
The findings support and extend those of some prior studies, and the study “affirms the deleterious effect of stopping statins after the initial period following a stroke,” they noted, adding: “Our study has both clinical and policy implications ... After a stroke due to large or small vessel atherosclerosis, patients are at high risk of recurrent stroke and should be treated aggressively in the absence of clear contraindications. Physicians also need to increase awareness among stroke patients about the potential risk of discontinuing their medications and to encourage greater adherence.”
Statin therapy should not be discontinued in the absence of a “highly compelling reason for doing so,” they added, concluding that prospective studies are needed to clarify the mechanisms underlying the association between statin discontinuation and higher recurrent stroke risk.
In a press statement, Dr. Lee said that based on these “real world” findings, statins should be a lifelong therapy for ischemic stroke patients who need a statin to lower cholesterol.
“Discontinuation of statin treatment in patients with ischemic stroke should be strongly discouraged in any stage, acute or chronic, of stroke,” Dr. Lee said. “Shifting to low-intensity statin therapy could be an alternative for stroke patients not able to tolerate moderate or high-intensity statin therapy in the years following a stroke.”
As for the findings regarding starting statin therapy at the time of discharge, an analysis of discharge prescriptions for U.S. ischemic stroke patients from the REGARDS (Reasons for Geographic and Racial Differences in Stroke) study showed that 48.7% of 323 patients who were not statin users at the time of admission and who had no history of atrial fibrillation were prescribed a statin at discharge.
Overall, after adjustment for age, race, sex, numerous comorbid conditions, impaired cognition, current smoking status, stroke buckle or Stroke Belt residence, and other factors, patients aged 65 years and older were less likely to receive a statin prescription at discharge (risk ratio, 0.75), and those with dyslipidemia were more likely to be prescribed a stain at discharge (risk ratio, 1.67), Karen C. Albright, PhD, DO, of the Birmingham (Ala.) VA Medical Center, and her colleagues found.
Further, there were no significant overall differences in statin prescribing by race (black:white risk ratio, 1.13), or by sex (male:female risk ratio, 0.97).
When subjects were analyzed based on Stroke Belt residence (defined as residence in Alabama, Arkansas, Georgia, Indiana, Kentucky, Louisiana, Mississippi, North Carolina, South Carolina, Tennessee, and Virginia), adults aged 65 and older in the Stroke Belt were 47% less likely to be discharged on a statin, compared with younger patients (risk ratio, 0.53). This association was not observed in non–Stroke Belt residents (risk ratio, 1.14), the investigators found (J Am Heart Assoc. 2017 Aug 2. doi: 10.1161/JAHA.117.005523).
Also, among non–Stroke Belt residents, blacks were more likely to be discharged on a statin (risk ratio, 1.42), but this association was not seen in the Stroke Belt (risk ratio, 0.93).
Male Stroke Belt residents were 31% less likely than were female Stroke Belt residents to be discharged on a statin (risk ratio, 0.69), while men who were non–Stroke Belt residents were more likely than were female non–Stroke Belt residents to be discharged on a statin (risk ratio 1.38).
“Although statin prescribing increased over time in the current study, statins were prescribed at discharge to only 49% of patients with ischemic stroke. This represents a treatment gap given current American College of Cardiology/American Heart Association recommendations,” the investigators wrote.
This gap was particularly seen in men and those over aged 65 years – but not among blacks – in the Stroke Belt.
This leaves the reasons for higher rates of recurrent stroke in blacks unresolved, they noted.
“A next step in our efforts to understand the reasons for the higher rate of recurrent stroke in blacks is to evaluate statin adherence in ischemic stroke survivors,” they said.
The Taiwanese cohort study was funded by the Ministry of Science and Technology, Taiwan and Chang Gung Memorial Hospital, Taiwan. Dr. Lee and colleagues reported having no disclosures. The REGARDS study was funded by the National Institutes of Health and the Department of Health and Human Services. Dr. Albright reported having no disclosures, as did all other authors except Paul Muntner, PhD, who receives research support from Amgen Inc.
Discontinuing statin therapy 3-6 months after a stroke may increase the risk of recurrent stroke within a year, according to findings from a large retrospective Taiwanese cohort study.
And being older or male in the Stroke Belt increases the likelihood that statins won’t be prescribed at all at the time of hospital discharge after a stroke, a separate cohort study from the United States suggests.
Both studies were reported online in the Journal of the American Heart Association.
Of 45,151 ischemic stroke patients from the Taiwan National Health Insurance Research Database who were on a moderate- or high-intensity statin within 90 days of discharge after an ischemic stroke between 2001 and 2012, 3,175 (7%) were on a reduced dosage by the 90- to 180-day period, and 8,353 (18.5%) were not on any statin by that period. After adjustment for numerous factors including age, sex, several comorbid conditions, and stroke severity index, discontinuation of statins was associated with an increased hazard of recurrent ischemic or hemorrhagic stroke (6.2% vs. 4.4%; adjusted hazard ratio [HR], 1.42), Meng Lee, MD, of Chang Gung Memorial Hospital, Chiayi Branch, Puzy, Taiwan and colleagues reported.
Discontinuation of statins was also linked to higher risks of ischemic stroke (5.6% vs. 3.9%, adjusted HR, 1.45), all-cause mortality (1.4% vs. 1%; adjusted HR, 1.37), all major events (7.8% vs. 5.6%, adjusted HR 1.38), and any hospitalization (31.7% vs. 27.1%; adjusted HR, 1.19), but had neutral effects on intracerebral hemorrhage and myocardial infarction.
“Reduced dosage statin therapy was not associated with increased risks of ischemic stroke, intracerebral hemorrhage, all-cause mortality, myocardial infarction, or all major events,” they said.
The findings support and extend those of some prior studies, and the study “affirms the deleterious effect of stopping statins after the initial period following a stroke,” they noted, adding: “Our study has both clinical and policy implications ... After a stroke due to large or small vessel atherosclerosis, patients are at high risk of recurrent stroke and should be treated aggressively in the absence of clear contraindications. Physicians also need to increase awareness among stroke patients about the potential risk of discontinuing their medications and to encourage greater adherence.”
Statin therapy should not be discontinued in the absence of a “highly compelling reason for doing so,” they added, concluding that prospective studies are needed to clarify the mechanisms underlying the association between statin discontinuation and higher recurrent stroke risk.
In a press statement, Dr. Lee said that based on these “real world” findings, statins should be a lifelong therapy for ischemic stroke patients who need a statin to lower cholesterol.
“Discontinuation of statin treatment in patients with ischemic stroke should be strongly discouraged in any stage, acute or chronic, of stroke,” Dr. Lee said. “Shifting to low-intensity statin therapy could be an alternative for stroke patients not able to tolerate moderate or high-intensity statin therapy in the years following a stroke.”
As for the findings regarding starting statin therapy at the time of discharge, an analysis of discharge prescriptions for U.S. ischemic stroke patients from the REGARDS (Reasons for Geographic and Racial Differences in Stroke) study showed that 48.7% of 323 patients who were not statin users at the time of admission and who had no history of atrial fibrillation were prescribed a statin at discharge.
Overall, after adjustment for age, race, sex, numerous comorbid conditions, impaired cognition, current smoking status, stroke buckle or Stroke Belt residence, and other factors, patients aged 65 years and older were less likely to receive a statin prescription at discharge (risk ratio, 0.75), and those with dyslipidemia were more likely to be prescribed a stain at discharge (risk ratio, 1.67), Karen C. Albright, PhD, DO, of the Birmingham (Ala.) VA Medical Center, and her colleagues found.
Further, there were no significant overall differences in statin prescribing by race (black:white risk ratio, 1.13), or by sex (male:female risk ratio, 0.97).
When subjects were analyzed based on Stroke Belt residence (defined as residence in Alabama, Arkansas, Georgia, Indiana, Kentucky, Louisiana, Mississippi, North Carolina, South Carolina, Tennessee, and Virginia), adults aged 65 and older in the Stroke Belt were 47% less likely to be discharged on a statin, compared with younger patients (risk ratio, 0.53). This association was not observed in non–Stroke Belt residents (risk ratio, 1.14), the investigators found (J Am Heart Assoc. 2017 Aug 2. doi: 10.1161/JAHA.117.005523).
Also, among non–Stroke Belt residents, blacks were more likely to be discharged on a statin (risk ratio, 1.42), but this association was not seen in the Stroke Belt (risk ratio, 0.93).
Male Stroke Belt residents were 31% less likely than were female Stroke Belt residents to be discharged on a statin (risk ratio, 0.69), while men who were non–Stroke Belt residents were more likely than were female non–Stroke Belt residents to be discharged on a statin (risk ratio 1.38).
“Although statin prescribing increased over time in the current study, statins were prescribed at discharge to only 49% of patients with ischemic stroke. This represents a treatment gap given current American College of Cardiology/American Heart Association recommendations,” the investigators wrote.
This gap was particularly seen in men and those over aged 65 years – but not among blacks – in the Stroke Belt.
This leaves the reasons for higher rates of recurrent stroke in blacks unresolved, they noted.
“A next step in our efforts to understand the reasons for the higher rate of recurrent stroke in blacks is to evaluate statin adherence in ischemic stroke survivors,” they said.
The Taiwanese cohort study was funded by the Ministry of Science and Technology, Taiwan and Chang Gung Memorial Hospital, Taiwan. Dr. Lee and colleagues reported having no disclosures. The REGARDS study was funded by the National Institutes of Health and the Department of Health and Human Services. Dr. Albright reported having no disclosures, as did all other authors except Paul Muntner, PhD, who receives research support from Amgen Inc.
Discontinuing statin therapy 3-6 months after a stroke may increase the risk of recurrent stroke within a year, according to findings from a large retrospective Taiwanese cohort study.
And being older or male in the Stroke Belt increases the likelihood that statins won’t be prescribed at all at the time of hospital discharge after a stroke, a separate cohort study from the United States suggests.
Both studies were reported online in the Journal of the American Heart Association.
Of 45,151 ischemic stroke patients from the Taiwan National Health Insurance Research Database who were on a moderate- or high-intensity statin within 90 days of discharge after an ischemic stroke between 2001 and 2012, 3,175 (7%) were on a reduced dosage by the 90- to 180-day period, and 8,353 (18.5%) were not on any statin by that period. After adjustment for numerous factors including age, sex, several comorbid conditions, and stroke severity index, discontinuation of statins was associated with an increased hazard of recurrent ischemic or hemorrhagic stroke (6.2% vs. 4.4%; adjusted hazard ratio [HR], 1.42), Meng Lee, MD, of Chang Gung Memorial Hospital, Chiayi Branch, Puzy, Taiwan and colleagues reported.
Discontinuation of statins was also linked to higher risks of ischemic stroke (5.6% vs. 3.9%, adjusted HR, 1.45), all-cause mortality (1.4% vs. 1%; adjusted HR, 1.37), all major events (7.8% vs. 5.6%, adjusted HR 1.38), and any hospitalization (31.7% vs. 27.1%; adjusted HR, 1.19), but had neutral effects on intracerebral hemorrhage and myocardial infarction.
“Reduced dosage statin therapy was not associated with increased risks of ischemic stroke, intracerebral hemorrhage, all-cause mortality, myocardial infarction, or all major events,” they said.
The findings support and extend those of some prior studies, and the study “affirms the deleterious effect of stopping statins after the initial period following a stroke,” they noted, adding: “Our study has both clinical and policy implications ... After a stroke due to large or small vessel atherosclerosis, patients are at high risk of recurrent stroke and should be treated aggressively in the absence of clear contraindications. Physicians also need to increase awareness among stroke patients about the potential risk of discontinuing their medications and to encourage greater adherence.”
Statin therapy should not be discontinued in the absence of a “highly compelling reason for doing so,” they added, concluding that prospective studies are needed to clarify the mechanisms underlying the association between statin discontinuation and higher recurrent stroke risk.
In a press statement, Dr. Lee said that based on these “real world” findings, statins should be a lifelong therapy for ischemic stroke patients who need a statin to lower cholesterol.
“Discontinuation of statin treatment in patients with ischemic stroke should be strongly discouraged in any stage, acute or chronic, of stroke,” Dr. Lee said. “Shifting to low-intensity statin therapy could be an alternative for stroke patients not able to tolerate moderate or high-intensity statin therapy in the years following a stroke.”
As for the findings regarding starting statin therapy at the time of discharge, an analysis of discharge prescriptions for U.S. ischemic stroke patients from the REGARDS (Reasons for Geographic and Racial Differences in Stroke) study showed that 48.7% of 323 patients who were not statin users at the time of admission and who had no history of atrial fibrillation were prescribed a statin at discharge.
Overall, after adjustment for age, race, sex, numerous comorbid conditions, impaired cognition, current smoking status, stroke buckle or Stroke Belt residence, and other factors, patients aged 65 years and older were less likely to receive a statin prescription at discharge (risk ratio, 0.75), and those with dyslipidemia were more likely to be prescribed a stain at discharge (risk ratio, 1.67), Karen C. Albright, PhD, DO, of the Birmingham (Ala.) VA Medical Center, and her colleagues found.
Further, there were no significant overall differences in statin prescribing by race (black:white risk ratio, 1.13), or by sex (male:female risk ratio, 0.97).
When subjects were analyzed based on Stroke Belt residence (defined as residence in Alabama, Arkansas, Georgia, Indiana, Kentucky, Louisiana, Mississippi, North Carolina, South Carolina, Tennessee, and Virginia), adults aged 65 and older in the Stroke Belt were 47% less likely to be discharged on a statin, compared with younger patients (risk ratio, 0.53). This association was not observed in non–Stroke Belt residents (risk ratio, 1.14), the investigators found (J Am Heart Assoc. 2017 Aug 2. doi: 10.1161/JAHA.117.005523).
Also, among non–Stroke Belt residents, blacks were more likely to be discharged on a statin (risk ratio, 1.42), but this association was not seen in the Stroke Belt (risk ratio, 0.93).
Male Stroke Belt residents were 31% less likely than were female Stroke Belt residents to be discharged on a statin (risk ratio, 0.69), while men who were non–Stroke Belt residents were more likely than were female non–Stroke Belt residents to be discharged on a statin (risk ratio 1.38).
“Although statin prescribing increased over time in the current study, statins were prescribed at discharge to only 49% of patients with ischemic stroke. This represents a treatment gap given current American College of Cardiology/American Heart Association recommendations,” the investigators wrote.
This gap was particularly seen in men and those over aged 65 years – but not among blacks – in the Stroke Belt.
This leaves the reasons for higher rates of recurrent stroke in blacks unresolved, they noted.
“A next step in our efforts to understand the reasons for the higher rate of recurrent stroke in blacks is to evaluate statin adherence in ischemic stroke survivors,” they said.
The Taiwanese cohort study was funded by the Ministry of Science and Technology, Taiwan and Chang Gung Memorial Hospital, Taiwan. Dr. Lee and colleagues reported having no disclosures. The REGARDS study was funded by the National Institutes of Health and the Department of Health and Human Services. Dr. Albright reported having no disclosures, as did all other authors except Paul Muntner, PhD, who receives research support from Amgen Inc.
FROM JOURNAL OF THE AMERICAN HEART ASSOCIATION
Key clinical point:
Major finding: Discontinuation of statins 90-180 days after ischemic stroke was associated with an increased hazard of recurrent ischemic or hemorrhagic stroke (6.2% vs. 4.4%; adjusted hazard ratio [HR], 1.42).
Data source: Cohort studies in Taiwan and the United States involving 45,151 and 323 patients, respectively.
Disclosures: The Taiwanese cohort study was funded by the Ministry of Science and Technology, Taiwan and Chang Gung Memorial Hospital, Taiwan. Dr. Lee and colleagues reported having no disclosures. The REGARDS study was funded by the National Institutes of Health and the Department of Health and Human Services. Dr. Albright reported having no disclosures, as did all other authors except Paul Muntner, PhD, who receives research support from Amgen Inc.
Novel device aims to make cervical cancer screening more accessible
A novel vaginal inserter currently in development at Duke University for use with a miniature colposcope proved feasible for comfortable, speculum-free cervical image capture in a recent study.
Along with allowing for more comfortable – and possibly self-facilitated – cervical cancer screening, the device could have important implications for providing care and improving screening rates in underserved, low-resource communities in the United States and around the world, according to Mercy N. Asiedu, a graduate student research assistant in the Duke University department of biomedical engineering.
Ms. Asiedu is part of a team that has been working to develop effective, low-cost methods for diagnosing cervical and breast cancer, particularly in low-resource regions.
A device such as the integrated inserter and colposcope could potentially be purchased over the counter at a local pharmacy and used for “self checkups,” or used in clinics to facilitate a more comfortable, patient-friendly approach to exams here in the United States, she said in an interview.
“But in other countries, one of the bigger benefits [relates to] cultural factors that deter women from going in for gynecological exams,” Ms. Asiedu said.
Overcoming screening barriers
Invasive cervical cancer ranks as the second most common female cancer in low and middle-income countries and the seventh most common in high-income countries, she and her colleagues wrote in a study published in PLoS ONE (12[5]:e0177782. doi: 10.1371/journal.pone.0177782).
The discrepancies between high- and low-resource areas largely result from the fact that visualization of the cervix via colposcopy using a standard approach requires a highly-trained professional and expensive equipment that is not easily accessible in underserved regions.
But even in the United states, the use of a standard speculum to expand the vaginal canal has been identified as a factor in the resistance of some women to undergo screening. Embarrassment and fear of pain have also been reported as potential barriers to screening.
The ability to self-insert can also help reduce pain associated with the exam, as it allows the user to adjust positioning when there is discomfort, she said.
A speculum alternative
The inserter is a tampon-sized tubular device designed as an alternative to a standard speculum, and is used with the Pocket Colposcope, a miniature pen-sized colposcope also developed by Duke University researchers and validated by physicians worldwide as providing image quality comparable to high-end, state-of-the-art digital colposcopes.
The current rendition of the inserter device has a funnel-like, curved tip measuring approximately 2.6 cm in diameter, a channel for insertion of a 2-megapixel mini-USB camera with LED illumination for the cervical image capture (as opposed to the 5-megapixel camera typically used with the Pocket Colposcope in the setting of standard speculum use), and can connect to a number of devices such as smartphones and laptop computers for image display.
“The curved tip enables easy manipulation of the cervix, especially in cases where the patient has a tilted uterus,” Ms Asiedu and her colleagues wrote in PLoS. “Our design also enables manipulation of the cervix for cervical imaging of women with tilted uteri, a condition that affects about 20% of women and is difficult and painful when using the standard speculum for manipulation.”
Using a custom-made vaginal phantom, the researchers tested various designs and demonstrated that it was able to withstand a range of supine vaginal pressures. In addition, 12 of 15 healthy volunteers achieved adequate cervical image capture after self-insertion of the device, and 14 of the 15 women expressed an overall preference for the inserter over the speculum (based on past experience). All of the volunteers said the inserter was slightly more, or much more, comfortable than a standard speculum, and noted that comfort was a particular benefit.
Prior to self-insertion, the volunteers typically received about 5 minutes of instruction using a pelvic mannequin. Images were captured and displayed on a mobile device once the cervix was in view.
From a patient perspective, the volunteer study “was almost universally positive,” John W. Schmitt, MD, professor of obstetrics and gynecology, as well as global health, at Duke, said in an interview. He conducted the clinical portion of the research.
From the clinician perspective, there is a bit of a learning curve, he added.
“I’ve approached it with what I’d call healthy skepticism,” he said, noting that traditional specula have been around for ages, and are easy to use. “I’ve used them for a long time and I know how, so there’s a learning curve to get it right [with the new device], but as I’ve done more and more, it’s becoming really obvious that this can be used, and ... it’s got real potential to make for a more comfortable internal exam.”
That is particularly true if the size and design can be maintained while also allowing channels to be added to allow solutions, such as acetic acid or Lugol’s solution, to be applied to the cervix to help with visualization – all while keeping the camera in place and allowing the insertion of swabs for obtaining samples from the cervix, he said.
Future directions
Efforts are underway to further improve the design for better visualization, ease of use, and comfort. The next phase of study will involve comparing visualization between the device and a standard speculum for routine exams and more advanced cancer screening exams. Ms. Asiedu said the researchers are also seeking to modify the inserter to accommodate the original Pocket Colposcope with a 5-megapixel camera for better image quality.
Should the inserter and colposcope be validated in further studies, the potential benefits are numerous, she said, explaining that the device’s potential for expanding access to screening are driven by its portability and low cost; the 2-megapixel camera currently used with the device costs about $54, compared with $20,000 for a standard-of-care digital colposcope. The estimated cost of the inserter under mass production would be less than $1.
It may be possible to produce the inserter in varying sizes to match cervix size. There are other potential uses for the device, including at-home viewing of the cervical os to gauge cervical dilation during labor and to detect false labor, she and her colleagues noted.
One limitation, which is also a problem with current methods of visual inspection of the cervix, is lack of ability to see the squamocolumnar junction.
“It is therefore not a replacement for gold standard pathology, where cells from the squamocolumnar junction are removed for pathology. However, our device can aid in guiding biopsies and has merit for places that lack gold standard biopsy,” they wrote, noting that future studies will compare cervix samples collected via the inserter versus a standard speculum to explore the possibility of self-sampling.
Efforts also are underway to develop an algorithm for making a diagnosis based on such samples, Ms. Asiedu said.
Given that 11 of the 15 volunteers in the study said that self-screening with the device was more difficult than having a physician perform the exam, another longitudinal study will look at whether ease of use improves over time, she said.
“There’s a lot of work to be done to get it where it could be routinely used,” Dr. Schmitt said. “Even for someone like me who does have this healthy skepticism, this might really be a profound change in the way we do pelvic exams.”
A word of caution
But Michael R. Caudle, MD, an ob.gyn. with Cherokee Health Systems in Knoxville, Tenn., urged caution, at least among rural U.S. health centers, with any approach that involves only visualizing the cervix. His concern is that this type of device could give women “false reassurances.”
“The promulgation of Pap smears and HPV testing would be the direction rural sites should go,” he said. “Colposcopy requires biopsies to rule out serious disease.”
He noted that the American Society for Colposcopy and Cervical Pathology (ASCCP) provides training for mid-level providers to do these evaluations.
“I think this is better than looking only. We see tragedies from women not getting adequate follow-up for abnormal paps, so making this even more removed from proper oversight is a concern. There have been attempts in the past to send photos of the cervix for evaluation and one problem again was the lack of biopsies.
“Rural health departments do a good job at triaging abnormal paps, and expansion of this, in my opinion, is a better idea,” he said.
The Duke University study was supported by the National Institutes of Health. Ms. Asiedu reported having no disclosures, but two of her coauthors founded companies and developed technologies related to this work where the investigators or Duke may benefit financially if the system is sold commercially. Ms. Asiedu and her coauthors have filed a provisional patent application for the concept of the system.
A novel vaginal inserter currently in development at Duke University for use with a miniature colposcope proved feasible for comfortable, speculum-free cervical image capture in a recent study.
Along with allowing for more comfortable – and possibly self-facilitated – cervical cancer screening, the device could have important implications for providing care and improving screening rates in underserved, low-resource communities in the United States and around the world, according to Mercy N. Asiedu, a graduate student research assistant in the Duke University department of biomedical engineering.
Ms. Asiedu is part of a team that has been working to develop effective, low-cost methods for diagnosing cervical and breast cancer, particularly in low-resource regions.
A device such as the integrated inserter and colposcope could potentially be purchased over the counter at a local pharmacy and used for “self checkups,” or used in clinics to facilitate a more comfortable, patient-friendly approach to exams here in the United States, she said in an interview.
“But in other countries, one of the bigger benefits [relates to] cultural factors that deter women from going in for gynecological exams,” Ms. Asiedu said.
Overcoming screening barriers
Invasive cervical cancer ranks as the second most common female cancer in low and middle-income countries and the seventh most common in high-income countries, she and her colleagues wrote in a study published in PLoS ONE (12[5]:e0177782. doi: 10.1371/journal.pone.0177782).
The discrepancies between high- and low-resource areas largely result from the fact that visualization of the cervix via colposcopy using a standard approach requires a highly-trained professional and expensive equipment that is not easily accessible in underserved regions.
But even in the United states, the use of a standard speculum to expand the vaginal canal has been identified as a factor in the resistance of some women to undergo screening. Embarrassment and fear of pain have also been reported as potential barriers to screening.
The ability to self-insert can also help reduce pain associated with the exam, as it allows the user to adjust positioning when there is discomfort, she said.
A speculum alternative
The inserter is a tampon-sized tubular device designed as an alternative to a standard speculum, and is used with the Pocket Colposcope, a miniature pen-sized colposcope also developed by Duke University researchers and validated by physicians worldwide as providing image quality comparable to high-end, state-of-the-art digital colposcopes.
The current rendition of the inserter device has a funnel-like, curved tip measuring approximately 2.6 cm in diameter, a channel for insertion of a 2-megapixel mini-USB camera with LED illumination for the cervical image capture (as opposed to the 5-megapixel camera typically used with the Pocket Colposcope in the setting of standard speculum use), and can connect to a number of devices such as smartphones and laptop computers for image display.
“The curved tip enables easy manipulation of the cervix, especially in cases where the patient has a tilted uterus,” Ms Asiedu and her colleagues wrote in PLoS. “Our design also enables manipulation of the cervix for cervical imaging of women with tilted uteri, a condition that affects about 20% of women and is difficult and painful when using the standard speculum for manipulation.”
Using a custom-made vaginal phantom, the researchers tested various designs and demonstrated that it was able to withstand a range of supine vaginal pressures. In addition, 12 of 15 healthy volunteers achieved adequate cervical image capture after self-insertion of the device, and 14 of the 15 women expressed an overall preference for the inserter over the speculum (based on past experience). All of the volunteers said the inserter was slightly more, or much more, comfortable than a standard speculum, and noted that comfort was a particular benefit.
Prior to self-insertion, the volunteers typically received about 5 minutes of instruction using a pelvic mannequin. Images were captured and displayed on a mobile device once the cervix was in view.
From a patient perspective, the volunteer study “was almost universally positive,” John W. Schmitt, MD, professor of obstetrics and gynecology, as well as global health, at Duke, said in an interview. He conducted the clinical portion of the research.
From the clinician perspective, there is a bit of a learning curve, he added.
“I’ve approached it with what I’d call healthy skepticism,” he said, noting that traditional specula have been around for ages, and are easy to use. “I’ve used them for a long time and I know how, so there’s a learning curve to get it right [with the new device], but as I’ve done more and more, it’s becoming really obvious that this can be used, and ... it’s got real potential to make for a more comfortable internal exam.”
That is particularly true if the size and design can be maintained while also allowing channels to be added to allow solutions, such as acetic acid or Lugol’s solution, to be applied to the cervix to help with visualization – all while keeping the camera in place and allowing the insertion of swabs for obtaining samples from the cervix, he said.
Future directions
Efforts are underway to further improve the design for better visualization, ease of use, and comfort. The next phase of study will involve comparing visualization between the device and a standard speculum for routine exams and more advanced cancer screening exams. Ms. Asiedu said the researchers are also seeking to modify the inserter to accommodate the original Pocket Colposcope with a 5-megapixel camera for better image quality.
Should the inserter and colposcope be validated in further studies, the potential benefits are numerous, she said, explaining that the device’s potential for expanding access to screening are driven by its portability and low cost; the 2-megapixel camera currently used with the device costs about $54, compared with $20,000 for a standard-of-care digital colposcope. The estimated cost of the inserter under mass production would be less than $1.
It may be possible to produce the inserter in varying sizes to match cervix size. There are other potential uses for the device, including at-home viewing of the cervical os to gauge cervical dilation during labor and to detect false labor, she and her colleagues noted.
One limitation, which is also a problem with current methods of visual inspection of the cervix, is lack of ability to see the squamocolumnar junction.
“It is therefore not a replacement for gold standard pathology, where cells from the squamocolumnar junction are removed for pathology. However, our device can aid in guiding biopsies and has merit for places that lack gold standard biopsy,” they wrote, noting that future studies will compare cervix samples collected via the inserter versus a standard speculum to explore the possibility of self-sampling.
Efforts also are underway to develop an algorithm for making a diagnosis based on such samples, Ms. Asiedu said.
Given that 11 of the 15 volunteers in the study said that self-screening with the device was more difficult than having a physician perform the exam, another longitudinal study will look at whether ease of use improves over time, she said.
“There’s a lot of work to be done to get it where it could be routinely used,” Dr. Schmitt said. “Even for someone like me who does have this healthy skepticism, this might really be a profound change in the way we do pelvic exams.”
A word of caution
But Michael R. Caudle, MD, an ob.gyn. with Cherokee Health Systems in Knoxville, Tenn., urged caution, at least among rural U.S. health centers, with any approach that involves only visualizing the cervix. His concern is that this type of device could give women “false reassurances.”
“The promulgation of Pap smears and HPV testing would be the direction rural sites should go,” he said. “Colposcopy requires biopsies to rule out serious disease.”
He noted that the American Society for Colposcopy and Cervical Pathology (ASCCP) provides training for mid-level providers to do these evaluations.
“I think this is better than looking only. We see tragedies from women not getting adequate follow-up for abnormal paps, so making this even more removed from proper oversight is a concern. There have been attempts in the past to send photos of the cervix for evaluation and one problem again was the lack of biopsies.
“Rural health departments do a good job at triaging abnormal paps, and expansion of this, in my opinion, is a better idea,” he said.
The Duke University study was supported by the National Institutes of Health. Ms. Asiedu reported having no disclosures, but two of her coauthors founded companies and developed technologies related to this work where the investigators or Duke may benefit financially if the system is sold commercially. Ms. Asiedu and her coauthors have filed a provisional patent application for the concept of the system.
A novel vaginal inserter currently in development at Duke University for use with a miniature colposcope proved feasible for comfortable, speculum-free cervical image capture in a recent study.
Along with allowing for more comfortable – and possibly self-facilitated – cervical cancer screening, the device could have important implications for providing care and improving screening rates in underserved, low-resource communities in the United States and around the world, according to Mercy N. Asiedu, a graduate student research assistant in the Duke University department of biomedical engineering.
Ms. Asiedu is part of a team that has been working to develop effective, low-cost methods for diagnosing cervical and breast cancer, particularly in low-resource regions.
A device such as the integrated inserter and colposcope could potentially be purchased over the counter at a local pharmacy and used for “self checkups,” or used in clinics to facilitate a more comfortable, patient-friendly approach to exams here in the United States, she said in an interview.
“But in other countries, one of the bigger benefits [relates to] cultural factors that deter women from going in for gynecological exams,” Ms. Asiedu said.
Overcoming screening barriers
Invasive cervical cancer ranks as the second most common female cancer in low and middle-income countries and the seventh most common in high-income countries, she and her colleagues wrote in a study published in PLoS ONE (12[5]:e0177782. doi: 10.1371/journal.pone.0177782).
The discrepancies between high- and low-resource areas largely result from the fact that visualization of the cervix via colposcopy using a standard approach requires a highly-trained professional and expensive equipment that is not easily accessible in underserved regions.
But even in the United states, the use of a standard speculum to expand the vaginal canal has been identified as a factor in the resistance of some women to undergo screening. Embarrassment and fear of pain have also been reported as potential barriers to screening.
The ability to self-insert can also help reduce pain associated with the exam, as it allows the user to adjust positioning when there is discomfort, she said.
A speculum alternative
The inserter is a tampon-sized tubular device designed as an alternative to a standard speculum, and is used with the Pocket Colposcope, a miniature pen-sized colposcope also developed by Duke University researchers and validated by physicians worldwide as providing image quality comparable to high-end, state-of-the-art digital colposcopes.
The current rendition of the inserter device has a funnel-like, curved tip measuring approximately 2.6 cm in diameter, a channel for insertion of a 2-megapixel mini-USB camera with LED illumination for the cervical image capture (as opposed to the 5-megapixel camera typically used with the Pocket Colposcope in the setting of standard speculum use), and can connect to a number of devices such as smartphones and laptop computers for image display.
“The curved tip enables easy manipulation of the cervix, especially in cases where the patient has a tilted uterus,” Ms Asiedu and her colleagues wrote in PLoS. “Our design also enables manipulation of the cervix for cervical imaging of women with tilted uteri, a condition that affects about 20% of women and is difficult and painful when using the standard speculum for manipulation.”
Using a custom-made vaginal phantom, the researchers tested various designs and demonstrated that it was able to withstand a range of supine vaginal pressures. In addition, 12 of 15 healthy volunteers achieved adequate cervical image capture after self-insertion of the device, and 14 of the 15 women expressed an overall preference for the inserter over the speculum (based on past experience). All of the volunteers said the inserter was slightly more, or much more, comfortable than a standard speculum, and noted that comfort was a particular benefit.
Prior to self-insertion, the volunteers typically received about 5 minutes of instruction using a pelvic mannequin. Images were captured and displayed on a mobile device once the cervix was in view.
From a patient perspective, the volunteer study “was almost universally positive,” John W. Schmitt, MD, professor of obstetrics and gynecology, as well as global health, at Duke, said in an interview. He conducted the clinical portion of the research.
From the clinician perspective, there is a bit of a learning curve, he added.
“I’ve approached it with what I’d call healthy skepticism,” he said, noting that traditional specula have been around for ages, and are easy to use. “I’ve used them for a long time and I know how, so there’s a learning curve to get it right [with the new device], but as I’ve done more and more, it’s becoming really obvious that this can be used, and ... it’s got real potential to make for a more comfortable internal exam.”
That is particularly true if the size and design can be maintained while also allowing channels to be added to allow solutions, such as acetic acid or Lugol’s solution, to be applied to the cervix to help with visualization – all while keeping the camera in place and allowing the insertion of swabs for obtaining samples from the cervix, he said.
Future directions
Efforts are underway to further improve the design for better visualization, ease of use, and comfort. The next phase of study will involve comparing visualization between the device and a standard speculum for routine exams and more advanced cancer screening exams. Ms. Asiedu said the researchers are also seeking to modify the inserter to accommodate the original Pocket Colposcope with a 5-megapixel camera for better image quality.
Should the inserter and colposcope be validated in further studies, the potential benefits are numerous, she said, explaining that the device’s potential for expanding access to screening are driven by its portability and low cost; the 2-megapixel camera currently used with the device costs about $54, compared with $20,000 for a standard-of-care digital colposcope. The estimated cost of the inserter under mass production would be less than $1.
It may be possible to produce the inserter in varying sizes to match cervix size. There are other potential uses for the device, including at-home viewing of the cervical os to gauge cervical dilation during labor and to detect false labor, she and her colleagues noted.
One limitation, which is also a problem with current methods of visual inspection of the cervix, is lack of ability to see the squamocolumnar junction.
“It is therefore not a replacement for gold standard pathology, where cells from the squamocolumnar junction are removed for pathology. However, our device can aid in guiding biopsies and has merit for places that lack gold standard biopsy,” they wrote, noting that future studies will compare cervix samples collected via the inserter versus a standard speculum to explore the possibility of self-sampling.
Efforts also are underway to develop an algorithm for making a diagnosis based on such samples, Ms. Asiedu said.
Given that 11 of the 15 volunteers in the study said that self-screening with the device was more difficult than having a physician perform the exam, another longitudinal study will look at whether ease of use improves over time, she said.
“There’s a lot of work to be done to get it where it could be routinely used,” Dr. Schmitt said. “Even for someone like me who does have this healthy skepticism, this might really be a profound change in the way we do pelvic exams.”
A word of caution
But Michael R. Caudle, MD, an ob.gyn. with Cherokee Health Systems in Knoxville, Tenn., urged caution, at least among rural U.S. health centers, with any approach that involves only visualizing the cervix. His concern is that this type of device could give women “false reassurances.”
“The promulgation of Pap smears and HPV testing would be the direction rural sites should go,” he said. “Colposcopy requires biopsies to rule out serious disease.”
He noted that the American Society for Colposcopy and Cervical Pathology (ASCCP) provides training for mid-level providers to do these evaluations.
“I think this is better than looking only. We see tragedies from women not getting adequate follow-up for abnormal paps, so making this even more removed from proper oversight is a concern. There have been attempts in the past to send photos of the cervix for evaluation and one problem again was the lack of biopsies.
“Rural health departments do a good job at triaging abnormal paps, and expansion of this, in my opinion, is a better idea,” he said.
The Duke University study was supported by the National Institutes of Health. Ms. Asiedu reported having no disclosures, but two of her coauthors founded companies and developed technologies related to this work where the investigators or Duke may benefit financially if the system is sold commercially. Ms. Asiedu and her coauthors have filed a provisional patent application for the concept of the system.
Glioblastoma: Prognosis is poor, but new therapies are emerging
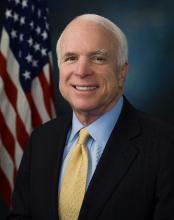
The questioning of former FBI director James B. Comey by Sen. John McCain (R-Ariz.) during a June 8 Senate Intelligence Committee hearing raised more than a few eyebrows; Sen. McCain seemed confused and disoriented, at one point referring to Mr. Comey as “President Comey,” but a possible medical explanation emerged soon after.
On July 14, Sen. McCain, 80, underwent surgery to remove a 5-cm blood clot that had been discovered above his left eye during a physical, and on July 19, the Mayo Clinic in Phoenix, where he had undergone the procedure, announced at his request that, “subsequent tissue pathology revealed that a primary brain tumor known as a glioblastoma was associated with the blood clot.”
Glioblastoma features
While Sen. McCain’s symptoms can’t necessarily be attributed to the glioblastoma, it is not unusual for glioblastoma patients to present with some sort of neurologic deficit, such as speech issues, unilateral weakness, or confusion, according to Eudocia Quant Lee, MD, a neuro-oncologist at Dana-Farber Cancer Institute, Boston.
Neuro-oncologist Manmeet Singh Ahluwalia, MD, of the Cleveland Clinic said seizures, persistent headaches, double or blurred vision, and changes in ability to think and learn can also be presenting symptoms.
Glioblastoma is the most common malignant primary brain tumor diagnosed in adults, with an estimated 12,000-13,000 new cases occurring each year in the United States. It is more common among older adults but can occur in younger patients. It arises in the brain and generally stays within the central nervous system, Dr. Lee explained, noting that it is much less common than lung cancer, breast cancer, and melanoma.
This is particularly true for older patients.
Prognosis and age
“We know, in general – as with most cancers – that the older you’re diagnosed with your cancer, the poorer your prognosis is,” she said, adding that other health issues and the ability to tolerate treatment can affect outcomes.
Outcomes also can be affected by type of surgery, functional status, extent of treatment, and molecular subtypes of the glioblastoma, Dr. Ahluwalia said.
Survival generally ranges about 14-18 months, although about 10% of patients live 5 years or longer.
The study, presented in a poster by Michael Weller, MD, of University Hospital and University of Zürich and his colleagues, also showed that, compared with the 398 older patients who survived less than 2 years (median, 6.2 months), those who survived longer had “more intensive up-front treatment and a trend toward higher initial Karnofsky performance scores as distinguishing clinical factors.”
In addition, molecular analyses showed more frequent O6-methylguanine-DNA methyltransferase (MGMT) promoter methylation in those with longer survival, while isocitrate dehydrogenase (IDH) mutations were restricted to single patients.
“Collectively, our findings confirm that LTS is rare in elderly patients with glioblastoma and that clinical and tumor-associated molecular factors linked to LTS resemble those in standard-age patients, except for less common IDH mutation,” the investigators wrote.
Another abstract published online in conjunction with the ASCO annual meeting looked at outcomes, based on age and MGMT analysis, and similarly found that aggressive treatment with chemoradiation is associated with better outcomes in both younger and older patients.
In that study by Suryanarayan Mohapatra, MD, of Cleveland Clinic–Fairview Hospital, and his colleagues – including Dr. Ahluwalia – 567 of 1,165 patients were aged 65 years or older. The benefits of chemoradiation therapy, which was associated with a significantly lower risk of death vs. radiation therapy alone in the study, were more pronounced among the older patients (hazard ratio, 0.45 vs. 0.61 for those under age 65 years), but the difference did not reach statistical significance.
Dr. Mohapatra and his colleagues also showed that more aggressive therapy resulted in better overall and progression-free survival regardless of MGMT methylation status, but that there was no difference between the age groups on this measure. Overall and progression-free survival also were significantly better with gross-total resection and subtotal resection vs. biopsy only, and with diagnosis during 2009 and later vs. during 2007-2008. However, a difference between the two age groups was seen with respect to overall survival only among those diagnosed during 2009 or later, with a more prominent impact among the younger group, the investigators reported.
“Older individuals often get less aggressive treatment. However, based on the research, active and functional older patients should get aggressive treatment,” Dr. Ahluwalia said. “We advocate tailor-made treatment that takes into account patient condition, location of tumor, functional status, etc., in addition to patient age.”
Standard treatment approaches
The first step in the treatment of glioblastomas is maximal safe therapy, Dr. Lee said.
“You want to achieve as much of a resection as possible without leaving the patient with some sort of permanent neurologic deficit that could severely compromise the quality of their life,” she explained.
Sen. McCain’s tumor was “completely resected by imaging criteria,” according to the Mayo Clinic statement, which also noted that treatment options might include a combination of chemotherapy and radiation.
Indeed, the standard of care for glioblastomas after surgery is combined chemotherapy and radiation – typically given as approximately 6 weeks of radiation combined with oral temozolomide chemotherapy – followed by 6 monthly cycles of temozolomide, she explained.
Radiation is sometimes given for only 3 weeks, but this option is mainly reserved for elderly patients, she said, adding that trials in patients aged 65-70 years have shown that this shorter course of radiation can be equally effective but potentially less toxic.
Emerging treatment approaches
Another treatment that has shown promise involves the use of tumor-treating fields (TTFields) – a locoregionally delivered antimitotic treatment that disrupts cell division and organelle assembly.
A 2015 phase 3 trial showed that adding TTFields to maintenance temozolomide significantly prolonged progression-free and overall survival, Dr. Ahluwalia said.
Other studies, including two presented during poster sessions at the ASCO annual meeting, have shown a progression-free survival benefit with the addition of bevacizumab to the treatment regimen. One open-label phase 2 study showed that hypofractionated radiotherapy in combination with IV bevacizumab every 2 weeks vs. radiotherapy alone in newly diagnosed patients over age 65 years improved progression-free survival (median, 7.6 vs. 4.8 months), but not overall survival (median, 12.1 vs. 12.2 months).
Another phase 2 study presented by Phioanh (Leia) Nghiemphu, MD, of the University of California, Los Angeles, showed that in newly diagnosed patients aged 70 years and older, upfront treatment with bevacizumab and temozolomide was associated with promising survival benefits (overall survival, 12.3 months; progression-free survival, 5.1 months) and tolerable side effects. The best survival in multivariate analysis was in patients who received radiotherapy at progression; it was unclear whether the addition of bevacizumab led to a survival advantage, but it may have allowed delay of radiotherapy treatment, she noted.
“Although we have no cure for glioblastoma, treatments can control tumor growth for a period of time, and there are additional promising therapies emerging every day to treat this deadly cancer, she said in an interview. “There has been increasing interest in developing better therapies for the older patients with glioblastoma with less toxicity and still-robust survival, such as the addition of bevacizumab or a short course of radiotherapy with temozolomide chemotherapy.”
Dr. Ahluwalia encourages clinical trial participation for patients diagnosed with glioblastoma and noted that he is particularly excited about immunotherapy and targeted therapy trials.
Dr. Lee has served as consultant to Eli Lilly. Dr. Ahluwalia disclosed a financial relationship with multiple companies, including Novocure, which markets a TTFields device. Dr. Weller disclosed a financial relationships with multiple companies, including Novocure; Merck Sharp & Dohme, which markets temozolomide; and Roche, which markets bevacizumab. Dr. Nghiemphu has received research funding from Genentech/Roche and Novartis. Dr. Mohapatra reporting having no disclosures.
The questioning of former FBI director James B. Comey by Sen. John McCain (R-Ariz.) during a June 8 Senate Intelligence Committee hearing raised more than a few eyebrows; Sen. McCain seemed confused and disoriented, at one point referring to Mr. Comey as “President Comey,” but a possible medical explanation emerged soon after.
On July 14, Sen. McCain, 80, underwent surgery to remove a 5-cm blood clot that had been discovered above his left eye during a physical, and on July 19, the Mayo Clinic in Phoenix, where he had undergone the procedure, announced at his request that, “subsequent tissue pathology revealed that a primary brain tumor known as a glioblastoma was associated with the blood clot.”
Glioblastoma features
While Sen. McCain’s symptoms can’t necessarily be attributed to the glioblastoma, it is not unusual for glioblastoma patients to present with some sort of neurologic deficit, such as speech issues, unilateral weakness, or confusion, according to Eudocia Quant Lee, MD, a neuro-oncologist at Dana-Farber Cancer Institute, Boston.
Neuro-oncologist Manmeet Singh Ahluwalia, MD, of the Cleveland Clinic said seizures, persistent headaches, double or blurred vision, and changes in ability to think and learn can also be presenting symptoms.
Glioblastoma is the most common malignant primary brain tumor diagnosed in adults, with an estimated 12,000-13,000 new cases occurring each year in the United States. It is more common among older adults but can occur in younger patients. It arises in the brain and generally stays within the central nervous system, Dr. Lee explained, noting that it is much less common than lung cancer, breast cancer, and melanoma.
This is particularly true for older patients.
Prognosis and age
“We know, in general – as with most cancers – that the older you’re diagnosed with your cancer, the poorer your prognosis is,” she said, adding that other health issues and the ability to tolerate treatment can affect outcomes.
Outcomes also can be affected by type of surgery, functional status, extent of treatment, and molecular subtypes of the glioblastoma, Dr. Ahluwalia said.
Survival generally ranges about 14-18 months, although about 10% of patients live 5 years or longer.
The study, presented in a poster by Michael Weller, MD, of University Hospital and University of Zürich and his colleagues, also showed that, compared with the 398 older patients who survived less than 2 years (median, 6.2 months), those who survived longer had “more intensive up-front treatment and a trend toward higher initial Karnofsky performance scores as distinguishing clinical factors.”
In addition, molecular analyses showed more frequent O6-methylguanine-DNA methyltransferase (MGMT) promoter methylation in those with longer survival, while isocitrate dehydrogenase (IDH) mutations were restricted to single patients.
“Collectively, our findings confirm that LTS is rare in elderly patients with glioblastoma and that clinical and tumor-associated molecular factors linked to LTS resemble those in standard-age patients, except for less common IDH mutation,” the investigators wrote.
Another abstract published online in conjunction with the ASCO annual meeting looked at outcomes, based on age and MGMT analysis, and similarly found that aggressive treatment with chemoradiation is associated with better outcomes in both younger and older patients.
In that study by Suryanarayan Mohapatra, MD, of Cleveland Clinic–Fairview Hospital, and his colleagues – including Dr. Ahluwalia – 567 of 1,165 patients were aged 65 years or older. The benefits of chemoradiation therapy, which was associated with a significantly lower risk of death vs. radiation therapy alone in the study, were more pronounced among the older patients (hazard ratio, 0.45 vs. 0.61 for those under age 65 years), but the difference did not reach statistical significance.
Dr. Mohapatra and his colleagues also showed that more aggressive therapy resulted in better overall and progression-free survival regardless of MGMT methylation status, but that there was no difference between the age groups on this measure. Overall and progression-free survival also were significantly better with gross-total resection and subtotal resection vs. biopsy only, and with diagnosis during 2009 and later vs. during 2007-2008. However, a difference between the two age groups was seen with respect to overall survival only among those diagnosed during 2009 or later, with a more prominent impact among the younger group, the investigators reported.
“Older individuals often get less aggressive treatment. However, based on the research, active and functional older patients should get aggressive treatment,” Dr. Ahluwalia said. “We advocate tailor-made treatment that takes into account patient condition, location of tumor, functional status, etc., in addition to patient age.”
Standard treatment approaches
The first step in the treatment of glioblastomas is maximal safe therapy, Dr. Lee said.
“You want to achieve as much of a resection as possible without leaving the patient with some sort of permanent neurologic deficit that could severely compromise the quality of their life,” she explained.
Sen. McCain’s tumor was “completely resected by imaging criteria,” according to the Mayo Clinic statement, which also noted that treatment options might include a combination of chemotherapy and radiation.
Indeed, the standard of care for glioblastomas after surgery is combined chemotherapy and radiation – typically given as approximately 6 weeks of radiation combined with oral temozolomide chemotherapy – followed by 6 monthly cycles of temozolomide, she explained.
Radiation is sometimes given for only 3 weeks, but this option is mainly reserved for elderly patients, she said, adding that trials in patients aged 65-70 years have shown that this shorter course of radiation can be equally effective but potentially less toxic.
Emerging treatment approaches
Another treatment that has shown promise involves the use of tumor-treating fields (TTFields) – a locoregionally delivered antimitotic treatment that disrupts cell division and organelle assembly.
A 2015 phase 3 trial showed that adding TTFields to maintenance temozolomide significantly prolonged progression-free and overall survival, Dr. Ahluwalia said.
Other studies, including two presented during poster sessions at the ASCO annual meeting, have shown a progression-free survival benefit with the addition of bevacizumab to the treatment regimen. One open-label phase 2 study showed that hypofractionated radiotherapy in combination with IV bevacizumab every 2 weeks vs. radiotherapy alone in newly diagnosed patients over age 65 years improved progression-free survival (median, 7.6 vs. 4.8 months), but not overall survival (median, 12.1 vs. 12.2 months).
Another phase 2 study presented by Phioanh (Leia) Nghiemphu, MD, of the University of California, Los Angeles, showed that in newly diagnosed patients aged 70 years and older, upfront treatment with bevacizumab and temozolomide was associated with promising survival benefits (overall survival, 12.3 months; progression-free survival, 5.1 months) and tolerable side effects. The best survival in multivariate analysis was in patients who received radiotherapy at progression; it was unclear whether the addition of bevacizumab led to a survival advantage, but it may have allowed delay of radiotherapy treatment, she noted.
“Although we have no cure for glioblastoma, treatments can control tumor growth for a period of time, and there are additional promising therapies emerging every day to treat this deadly cancer, she said in an interview. “There has been increasing interest in developing better therapies for the older patients with glioblastoma with less toxicity and still-robust survival, such as the addition of bevacizumab or a short course of radiotherapy with temozolomide chemotherapy.”
Dr. Ahluwalia encourages clinical trial participation for patients diagnosed with glioblastoma and noted that he is particularly excited about immunotherapy and targeted therapy trials.
Dr. Lee has served as consultant to Eli Lilly. Dr. Ahluwalia disclosed a financial relationship with multiple companies, including Novocure, which markets a TTFields device. Dr. Weller disclosed a financial relationships with multiple companies, including Novocure; Merck Sharp & Dohme, which markets temozolomide; and Roche, which markets bevacizumab. Dr. Nghiemphu has received research funding from Genentech/Roche and Novartis. Dr. Mohapatra reporting having no disclosures.
The questioning of former FBI director James B. Comey by Sen. John McCain (R-Ariz.) during a June 8 Senate Intelligence Committee hearing raised more than a few eyebrows; Sen. McCain seemed confused and disoriented, at one point referring to Mr. Comey as “President Comey,” but a possible medical explanation emerged soon after.
On July 14, Sen. McCain, 80, underwent surgery to remove a 5-cm blood clot that had been discovered above his left eye during a physical, and on July 19, the Mayo Clinic in Phoenix, where he had undergone the procedure, announced at his request that, “subsequent tissue pathology revealed that a primary brain tumor known as a glioblastoma was associated with the blood clot.”
Glioblastoma features
While Sen. McCain’s symptoms can’t necessarily be attributed to the glioblastoma, it is not unusual for glioblastoma patients to present with some sort of neurologic deficit, such as speech issues, unilateral weakness, or confusion, according to Eudocia Quant Lee, MD, a neuro-oncologist at Dana-Farber Cancer Institute, Boston.
Neuro-oncologist Manmeet Singh Ahluwalia, MD, of the Cleveland Clinic said seizures, persistent headaches, double or blurred vision, and changes in ability to think and learn can also be presenting symptoms.
Glioblastoma is the most common malignant primary brain tumor diagnosed in adults, with an estimated 12,000-13,000 new cases occurring each year in the United States. It is more common among older adults but can occur in younger patients. It arises in the brain and generally stays within the central nervous system, Dr. Lee explained, noting that it is much less common than lung cancer, breast cancer, and melanoma.
This is particularly true for older patients.
Prognosis and age
“We know, in general – as with most cancers – that the older you’re diagnosed with your cancer, the poorer your prognosis is,” she said, adding that other health issues and the ability to tolerate treatment can affect outcomes.
Outcomes also can be affected by type of surgery, functional status, extent of treatment, and molecular subtypes of the glioblastoma, Dr. Ahluwalia said.
Survival generally ranges about 14-18 months, although about 10% of patients live 5 years or longer.
The study, presented in a poster by Michael Weller, MD, of University Hospital and University of Zürich and his colleagues, also showed that, compared with the 398 older patients who survived less than 2 years (median, 6.2 months), those who survived longer had “more intensive up-front treatment and a trend toward higher initial Karnofsky performance scores as distinguishing clinical factors.”
In addition, molecular analyses showed more frequent O6-methylguanine-DNA methyltransferase (MGMT) promoter methylation in those with longer survival, while isocitrate dehydrogenase (IDH) mutations were restricted to single patients.
“Collectively, our findings confirm that LTS is rare in elderly patients with glioblastoma and that clinical and tumor-associated molecular factors linked to LTS resemble those in standard-age patients, except for less common IDH mutation,” the investigators wrote.
Another abstract published online in conjunction with the ASCO annual meeting looked at outcomes, based on age and MGMT analysis, and similarly found that aggressive treatment with chemoradiation is associated with better outcomes in both younger and older patients.
In that study by Suryanarayan Mohapatra, MD, of Cleveland Clinic–Fairview Hospital, and his colleagues – including Dr. Ahluwalia – 567 of 1,165 patients were aged 65 years or older. The benefits of chemoradiation therapy, which was associated with a significantly lower risk of death vs. radiation therapy alone in the study, were more pronounced among the older patients (hazard ratio, 0.45 vs. 0.61 for those under age 65 years), but the difference did not reach statistical significance.
Dr. Mohapatra and his colleagues also showed that more aggressive therapy resulted in better overall and progression-free survival regardless of MGMT methylation status, but that there was no difference between the age groups on this measure. Overall and progression-free survival also were significantly better with gross-total resection and subtotal resection vs. biopsy only, and with diagnosis during 2009 and later vs. during 2007-2008. However, a difference between the two age groups was seen with respect to overall survival only among those diagnosed during 2009 or later, with a more prominent impact among the younger group, the investigators reported.
“Older individuals often get less aggressive treatment. However, based on the research, active and functional older patients should get aggressive treatment,” Dr. Ahluwalia said. “We advocate tailor-made treatment that takes into account patient condition, location of tumor, functional status, etc., in addition to patient age.”
Standard treatment approaches
The first step in the treatment of glioblastomas is maximal safe therapy, Dr. Lee said.
“You want to achieve as much of a resection as possible without leaving the patient with some sort of permanent neurologic deficit that could severely compromise the quality of their life,” she explained.
Sen. McCain’s tumor was “completely resected by imaging criteria,” according to the Mayo Clinic statement, which also noted that treatment options might include a combination of chemotherapy and radiation.
Indeed, the standard of care for glioblastomas after surgery is combined chemotherapy and radiation – typically given as approximately 6 weeks of radiation combined with oral temozolomide chemotherapy – followed by 6 monthly cycles of temozolomide, she explained.
Radiation is sometimes given for only 3 weeks, but this option is mainly reserved for elderly patients, she said, adding that trials in patients aged 65-70 years have shown that this shorter course of radiation can be equally effective but potentially less toxic.
Emerging treatment approaches
Another treatment that has shown promise involves the use of tumor-treating fields (TTFields) – a locoregionally delivered antimitotic treatment that disrupts cell division and organelle assembly.
A 2015 phase 3 trial showed that adding TTFields to maintenance temozolomide significantly prolonged progression-free and overall survival, Dr. Ahluwalia said.
Other studies, including two presented during poster sessions at the ASCO annual meeting, have shown a progression-free survival benefit with the addition of bevacizumab to the treatment regimen. One open-label phase 2 study showed that hypofractionated radiotherapy in combination with IV bevacizumab every 2 weeks vs. radiotherapy alone in newly diagnosed patients over age 65 years improved progression-free survival (median, 7.6 vs. 4.8 months), but not overall survival (median, 12.1 vs. 12.2 months).
Another phase 2 study presented by Phioanh (Leia) Nghiemphu, MD, of the University of California, Los Angeles, showed that in newly diagnosed patients aged 70 years and older, upfront treatment with bevacizumab and temozolomide was associated with promising survival benefits (overall survival, 12.3 months; progression-free survival, 5.1 months) and tolerable side effects. The best survival in multivariate analysis was in patients who received radiotherapy at progression; it was unclear whether the addition of bevacizumab led to a survival advantage, but it may have allowed delay of radiotherapy treatment, she noted.
“Although we have no cure for glioblastoma, treatments can control tumor growth for a period of time, and there are additional promising therapies emerging every day to treat this deadly cancer, she said in an interview. “There has been increasing interest in developing better therapies for the older patients with glioblastoma with less toxicity and still-robust survival, such as the addition of bevacizumab or a short course of radiotherapy with temozolomide chemotherapy.”
Dr. Ahluwalia encourages clinical trial participation for patients diagnosed with glioblastoma and noted that he is particularly excited about immunotherapy and targeted therapy trials.
Dr. Lee has served as consultant to Eli Lilly. Dr. Ahluwalia disclosed a financial relationship with multiple companies, including Novocure, which markets a TTFields device. Dr. Weller disclosed a financial relationships with multiple companies, including Novocure; Merck Sharp & Dohme, which markets temozolomide; and Roche, which markets bevacizumab. Dr. Nghiemphu has received research funding from Genentech/Roche and Novartis. Dr. Mohapatra reporting having no disclosures.
VA cohort study: Individualize SSI prophylaxis based on patient factors
The combined use of vancomycin and a beta-lactam antibiotic for prophylaxis against surgical site infections is associated with both benefits and harms, according to findings from a national propensity-score–adjusted retrospective cohort study.
For example, the combination treatment reduced surgical site infections (SSIs) 30 days after cardiac surgical procedures but increased the risk of postoperative acute kidney injury (AKI) in some patients, Westyn Branch-Elliman, MD, of the VA Boston Healthcare System and her colleagues reported online July 10 in PLOS Medicine.
Among cardiac surgery patients, the incidence of surgical site infections was significantly lower for the 6,953 patients treated with both drugs vs. the 12,834 treated with a single agent (0.95% vs. 1.48%), the investigators found (PLOS Med. 2017 Jul 10. doi: 10.1371/journal.pmed.1002340).
SSI benefit with combination therapy
“After controlling for age, diabetes, ASA [American Society of Anesthesiologists] score, mupirocin administration, current smoking status, and preoperative MRSA [methicillin-resistant Staphylococcus aureus] colonization status, receipt of combination antimicrobial prophylaxis was associated with reduced SSI risk following cardiac surgical procedures (adjusted risk ratio, 0.61),” they wrote, noting that, when combination therapy was compared with either of the agents alone, the associations were similar and that no association between SSI reduction and the combination regimen was seen for the other types of surgical procedures assessed.
Secondary analyses showed that, among the cardiac patients, differences in the rates of SSIs were seen based on MRSA status in patients undergoing cardiac surgery. Among MRSA-colonized patients, SSIs occurred in 8 of 346 patients (2.3%) who received combination prophylaxis vs. 4 of 100 patients (4%) who received vancomycin alone (aRR, 0.53), and, among MRSA-negative and MRSA-unknown cardiac surgery patients, SSIs occurred in 58 of 6,607 patients (0.88%) receiving combination prophylaxis and 146 of 10,215 patients (1.4%) receiving a beta-lactam alone (aRR, 0.60).
“Among MRSA-colonized patients undergoing cardiac surgery, the associated absolute risk reduction for SSI was approximately triple that of the absolute risk reduction in MRSA-negative or -unknown patients, with a [number needed to treat] to prevent 1 SSI of 53 for the MRSA-colonized group, compared with 176 for the MRSA-negative or -unknown groups,” they wrote.
The incidence of Clostridium difficile infection was similar in both exposure groups (0.72% and 0.81% with combination and single agent prophylaxis, respectively).
Higher AKI risk with combination therapy
“In contrast, combination versus single prophylaxis was associated with higher relative risk of AKI in the 7-day postoperative period after adjusting for prophylaxis regimen duration, age, diabetes, ASA score, and smoking,” they said.
The rate of AKI was 23.75% among patients receiving combination prophylaxis, compared with 20.79% and 13.93% among those receiving vancomycin alone and a beta-lactam alone, respectively.
Significant associations between absolute risk of AKI and receipt of combination regimens were seen across all types of procedures, the investigators said.
“Overall, the NNH [number needed to harm] to cause one episode of AKI in cardiac surgery patients receiving combination therapy was 22, and, for stage 3 AKI, 167. The NNH associated with one additional episode of any postoperative AKI after receipt of combination therapy was 76 following orthopedic procedures and 25 following vascular surgical procedures,” they said.
The optimal approach for preventing SSIs is unclear. Although the multidisciplinary Clinical Practice Guidelines for Antimicrobial Prophylaxis in Surgery recommend single agent prophylaxis most often, with a beta-lactam antibiotic, for most surgical procedures, the use of vancomycin alone is a consideration in MRSA-colonized patients and in centers with a high MRSA incidence, and combination prophylaxis with a beta-lactam plus vancomycin is increasing. However, the relative risks and benefit of this strategy have not been carefully studied, the investigators said.
Thus, the investigators used a propensity-adjusted, log-binomial regression model stratified by type of surgical procedure among the cases identified in the Veterans Affairs cohort to assess the association between SSIs and receipt of combination prophylaxis versus single agent prophylaxis.
Though limited by the observational study design and by factors such as a predominantly male and slightly older and more rural population, the findings suggest that “clinicians may need to individualize prophylaxis strategy based on patient-specific factors that influence the risk-versus-benefit equation,” they said, concluding that “future studies are needed to evaluate the utility of MRSA screening protocols for optimizing and individualizing surgical prophylaxis regimen.”
This study was funded by Veterans Affairs Health Services Research and Development. Dr. Branch-Elliman reported having no disclosures. One other author, Eli Perencevich, MD, received an investigator initiated Grant from Merck Pharmaceuticals in 2013.
The combined use of vancomycin and a beta-lactam antibiotic for prophylaxis against surgical site infections is associated with both benefits and harms, according to findings from a national propensity-score–adjusted retrospective cohort study.
For example, the combination treatment reduced surgical site infections (SSIs) 30 days after cardiac surgical procedures but increased the risk of postoperative acute kidney injury (AKI) in some patients, Westyn Branch-Elliman, MD, of the VA Boston Healthcare System and her colleagues reported online July 10 in PLOS Medicine.
Among cardiac surgery patients, the incidence of surgical site infections was significantly lower for the 6,953 patients treated with both drugs vs. the 12,834 treated with a single agent (0.95% vs. 1.48%), the investigators found (PLOS Med. 2017 Jul 10. doi: 10.1371/journal.pmed.1002340).
SSI benefit with combination therapy
“After controlling for age, diabetes, ASA [American Society of Anesthesiologists] score, mupirocin administration, current smoking status, and preoperative MRSA [methicillin-resistant Staphylococcus aureus] colonization status, receipt of combination antimicrobial prophylaxis was associated with reduced SSI risk following cardiac surgical procedures (adjusted risk ratio, 0.61),” they wrote, noting that, when combination therapy was compared with either of the agents alone, the associations were similar and that no association between SSI reduction and the combination regimen was seen for the other types of surgical procedures assessed.
Secondary analyses showed that, among the cardiac patients, differences in the rates of SSIs were seen based on MRSA status in patients undergoing cardiac surgery. Among MRSA-colonized patients, SSIs occurred in 8 of 346 patients (2.3%) who received combination prophylaxis vs. 4 of 100 patients (4%) who received vancomycin alone (aRR, 0.53), and, among MRSA-negative and MRSA-unknown cardiac surgery patients, SSIs occurred in 58 of 6,607 patients (0.88%) receiving combination prophylaxis and 146 of 10,215 patients (1.4%) receiving a beta-lactam alone (aRR, 0.60).
“Among MRSA-colonized patients undergoing cardiac surgery, the associated absolute risk reduction for SSI was approximately triple that of the absolute risk reduction in MRSA-negative or -unknown patients, with a [number needed to treat] to prevent 1 SSI of 53 for the MRSA-colonized group, compared with 176 for the MRSA-negative or -unknown groups,” they wrote.
The incidence of Clostridium difficile infection was similar in both exposure groups (0.72% and 0.81% with combination and single agent prophylaxis, respectively).
Higher AKI risk with combination therapy
“In contrast, combination versus single prophylaxis was associated with higher relative risk of AKI in the 7-day postoperative period after adjusting for prophylaxis regimen duration, age, diabetes, ASA score, and smoking,” they said.
The rate of AKI was 23.75% among patients receiving combination prophylaxis, compared with 20.79% and 13.93% among those receiving vancomycin alone and a beta-lactam alone, respectively.
Significant associations between absolute risk of AKI and receipt of combination regimens were seen across all types of procedures, the investigators said.
“Overall, the NNH [number needed to harm] to cause one episode of AKI in cardiac surgery patients receiving combination therapy was 22, and, for stage 3 AKI, 167. The NNH associated with one additional episode of any postoperative AKI after receipt of combination therapy was 76 following orthopedic procedures and 25 following vascular surgical procedures,” they said.
The optimal approach for preventing SSIs is unclear. Although the multidisciplinary Clinical Practice Guidelines for Antimicrobial Prophylaxis in Surgery recommend single agent prophylaxis most often, with a beta-lactam antibiotic, for most surgical procedures, the use of vancomycin alone is a consideration in MRSA-colonized patients and in centers with a high MRSA incidence, and combination prophylaxis with a beta-lactam plus vancomycin is increasing. However, the relative risks and benefit of this strategy have not been carefully studied, the investigators said.
Thus, the investigators used a propensity-adjusted, log-binomial regression model stratified by type of surgical procedure among the cases identified in the Veterans Affairs cohort to assess the association between SSIs and receipt of combination prophylaxis versus single agent prophylaxis.
Though limited by the observational study design and by factors such as a predominantly male and slightly older and more rural population, the findings suggest that “clinicians may need to individualize prophylaxis strategy based on patient-specific factors that influence the risk-versus-benefit equation,” they said, concluding that “future studies are needed to evaluate the utility of MRSA screening protocols for optimizing and individualizing surgical prophylaxis regimen.”
This study was funded by Veterans Affairs Health Services Research and Development. Dr. Branch-Elliman reported having no disclosures. One other author, Eli Perencevich, MD, received an investigator initiated Grant from Merck Pharmaceuticals in 2013.
The combined use of vancomycin and a beta-lactam antibiotic for prophylaxis against surgical site infections is associated with both benefits and harms, according to findings from a national propensity-score–adjusted retrospective cohort study.
For example, the combination treatment reduced surgical site infections (SSIs) 30 days after cardiac surgical procedures but increased the risk of postoperative acute kidney injury (AKI) in some patients, Westyn Branch-Elliman, MD, of the VA Boston Healthcare System and her colleagues reported online July 10 in PLOS Medicine.
Among cardiac surgery patients, the incidence of surgical site infections was significantly lower for the 6,953 patients treated with both drugs vs. the 12,834 treated with a single agent (0.95% vs. 1.48%), the investigators found (PLOS Med. 2017 Jul 10. doi: 10.1371/journal.pmed.1002340).
SSI benefit with combination therapy
“After controlling for age, diabetes, ASA [American Society of Anesthesiologists] score, mupirocin administration, current smoking status, and preoperative MRSA [methicillin-resistant Staphylococcus aureus] colonization status, receipt of combination antimicrobial prophylaxis was associated with reduced SSI risk following cardiac surgical procedures (adjusted risk ratio, 0.61),” they wrote, noting that, when combination therapy was compared with either of the agents alone, the associations were similar and that no association between SSI reduction and the combination regimen was seen for the other types of surgical procedures assessed.
Secondary analyses showed that, among the cardiac patients, differences in the rates of SSIs were seen based on MRSA status in patients undergoing cardiac surgery. Among MRSA-colonized patients, SSIs occurred in 8 of 346 patients (2.3%) who received combination prophylaxis vs. 4 of 100 patients (4%) who received vancomycin alone (aRR, 0.53), and, among MRSA-negative and MRSA-unknown cardiac surgery patients, SSIs occurred in 58 of 6,607 patients (0.88%) receiving combination prophylaxis and 146 of 10,215 patients (1.4%) receiving a beta-lactam alone (aRR, 0.60).
“Among MRSA-colonized patients undergoing cardiac surgery, the associated absolute risk reduction for SSI was approximately triple that of the absolute risk reduction in MRSA-negative or -unknown patients, with a [number needed to treat] to prevent 1 SSI of 53 for the MRSA-colonized group, compared with 176 for the MRSA-negative or -unknown groups,” they wrote.
The incidence of Clostridium difficile infection was similar in both exposure groups (0.72% and 0.81% with combination and single agent prophylaxis, respectively).
Higher AKI risk with combination therapy
“In contrast, combination versus single prophylaxis was associated with higher relative risk of AKI in the 7-day postoperative period after adjusting for prophylaxis regimen duration, age, diabetes, ASA score, and smoking,” they said.
The rate of AKI was 23.75% among patients receiving combination prophylaxis, compared with 20.79% and 13.93% among those receiving vancomycin alone and a beta-lactam alone, respectively.
Significant associations between absolute risk of AKI and receipt of combination regimens were seen across all types of procedures, the investigators said.
“Overall, the NNH [number needed to harm] to cause one episode of AKI in cardiac surgery patients receiving combination therapy was 22, and, for stage 3 AKI, 167. The NNH associated with one additional episode of any postoperative AKI after receipt of combination therapy was 76 following orthopedic procedures and 25 following vascular surgical procedures,” they said.
The optimal approach for preventing SSIs is unclear. Although the multidisciplinary Clinical Practice Guidelines for Antimicrobial Prophylaxis in Surgery recommend single agent prophylaxis most often, with a beta-lactam antibiotic, for most surgical procedures, the use of vancomycin alone is a consideration in MRSA-colonized patients and in centers with a high MRSA incidence, and combination prophylaxis with a beta-lactam plus vancomycin is increasing. However, the relative risks and benefit of this strategy have not been carefully studied, the investigators said.
Thus, the investigators used a propensity-adjusted, log-binomial regression model stratified by type of surgical procedure among the cases identified in the Veterans Affairs cohort to assess the association between SSIs and receipt of combination prophylaxis versus single agent prophylaxis.
Though limited by the observational study design and by factors such as a predominantly male and slightly older and more rural population, the findings suggest that “clinicians may need to individualize prophylaxis strategy based on patient-specific factors that influence the risk-versus-benefit equation,” they said, concluding that “future studies are needed to evaluate the utility of MRSA screening protocols for optimizing and individualizing surgical prophylaxis regimen.”
This study was funded by Veterans Affairs Health Services Research and Development. Dr. Branch-Elliman reported having no disclosures. One other author, Eli Perencevich, MD, received an investigator initiated Grant from Merck Pharmaceuticals in 2013.
FROM PLOS MEDICINE
Key clinical point:
Major finding: The SSI incidence was 0.95% vs. 1.48% with combination vs. single agent–therapy in cardiac surgery patients. Acute kidney injuries occurred in 23.75% of all surgery patients receiving combination prophylaxis, compared with 20.79% and 13.93% with vancomycin or a beta-lactam, respectively.
Data source: A retrospective cohort study of more than 70,000 surgical procedures.
Disclosures: This study was funded by Veterans Affairs Health Services Research and Development. Dr. Branch-Elliman reported having no disclosures. One other author, Eli Perencevich, MD, received an investigator initiated grant from Merck Pharmaceuticals in 2013.
M13-982 trial in del(17p) CLL: High, durable response rates to venetoclax
New York – Venetoclax monotherapy is associated with high and durable objective response rates in patients with del(17p) chronic lymphocytic leukemia (CLL), according to efficacy findings from the open-label M13-982 trial.
Additionally, a safety expansion of the pivotal phase 2 study showed that treatment was well tolerated, and assessment of minimal residual disease (MRD) status in the peripheral blood and bone marrow of study participants correlated with the 24-month progression-free survival estimate of 100% for patients with complete remission/complete remission with incomplete blood count recovery (CR/CRi), Stephan Stilgenbauer, MD, of the University of Ulm, Germany, and his colleagues reported in a poster at the annual meeting of the International Workshop on Chronic Lymphocytic Leukemia.
That response was maintained at 1 year in 85% of participants.
The current findings, which represent data through April 2017 for those 107 patients from the main cohort, as well as for 51 patients in the safety expansion study, show an overall response rate of 77%, with 20% CR/CRi.
The median time to first response was 1 month, and time to CR/CRi was 9.8 months, they said.
Estimates at 24 months for duration of response, progression-free survival, and overall survival were 66%, 54%, and 73%, respectively.
Additionally, objective responses were seen in four of five previously untreated patients who were enrolled in the safety expansion, and two of them had complete remissions. One patient with best response of stable disease decided to discontinue treatment but remained in follow-up with stable disease.
“All patients were alive at the time of analysis and remain progression free,” the investigators wrote.
In 18 patients who received prior B-cell receptor pathway inhibitor (BCRi) therapy, the objective response rate was 61% and the complete remission rate was 11%, with 12-month, progression-free and overall survival estimates of 50% and 54%, respectively.
Treatment-emergent adverse events of any grade occurred in 98% of patients, and led to dosing interruption in 40% and dosing adjustment in 17%. The most common adverse event was neutropenia; grade 3/4 neutropenia occurred in 40% of patients.
Neutropenia lead to a dose reduction in 8% of patients and to treatment interruption in 6% of patients; no discontinuations were reported.
Infections occurred in 81% of 158 patients, and grade 3/4 infections occurred in 23%; these infections were consistent with the underlying disease, the investigators said.
Laboratory tumor lysis syndrome (TLS) occurred in 5% of patients, but there were no episodes of clinical TLS, they said, noting that five TLS patients required dose interruptions. TLS occurred in four patients with medium risk at screening and in four with high risk. All episodes of TLS occurred during initial dosing or ramp-up, and all resolved. Affected patients were able to resume venetoclax with dose escalation to 400 mg/day.
The rate of minimal residual disease negativity was 30% in the intention-to-treat population as demonstrated by flow cytometry and confirmed by next generation sequencing (NGS) in 21 of 29 patients with an evaluable matched time point specimen. Bone marrow MRD negativity was observed in 20 patients by flow cytometry, and in 9 patients by NGS.
When looking at flow cytometry and NGS data combined, the MRD negativity rate in peripheral blood was 25% overall and 40% in evaluable patients, and the MRD negativity rate in bone marrow was 11% overall and 24% in evaluable patients.
Of those who achieved CR/CRi, 69% were MRD negative in peripheral blood by flow cytometry, with a 24-month, progression-free survival estimate of 100%, and 13 of those had confirmed MRD-negative blood by NGS, 2 had MRD-positive blood by NGS at a matched flow cytometry assessment, and 7 were not evaluated by NGS. For the remaining CR/CRi patients, who were MRD-positive by flow cytometry, the 24-month progression-free survival estimate was 86%.
Study participants in the main cohort were adults with a median age of 67 years who had relapsed/refractory CLL with an indication for treatment by iwCLL criteria, del(17p), good performance status, adequate bone marrow function, and creatinine clearance of at least 50 mg/min. They received a single test dose of 20 mg on day 1, with gradual ramp up to 400 mg over 4-5 weeks based on laboratory assessments. All were hospitalized for the first 20 mg and 50 mg venetoclax doses during ramp up.
Those in the safety expansion were treated with once-daily oral venetoclax starting at a dose of 20 mg/day for 1 week and ramped up to 400 mg by week 5. To mitigate TLS risk, uric acid–lowering agents and hydration were started at least 72 hours prior to administering the first dose. Those with high TLS risk – and some with medium risk – were hospitalized for the first 20-mg and 50-mg doses. Those with low TLS risk – and most with medium risk – received initial venetoclax dosing in an outpatient setting.
“Continued follow-up of patients in this trial will provide additional data on the durability of response with venetoclax in patients with del(17p) CLL,” the investigators wrote.
This study was supported by AbbVie and Genentech. Dr. Stilgenbauer received research funding, honoraria, and travel support from AbbVie, Amgen, Boehringer Ingelheim, Celgene, Genentech, Genzyme, Gilead, GSK, Janssen, Mundipharma, Novartis, Pharmacyclics, Hoffmann La-Roche, and Sanofi.
New York – Venetoclax monotherapy is associated with high and durable objective response rates in patients with del(17p) chronic lymphocytic leukemia (CLL), according to efficacy findings from the open-label M13-982 trial.
Additionally, a safety expansion of the pivotal phase 2 study showed that treatment was well tolerated, and assessment of minimal residual disease (MRD) status in the peripheral blood and bone marrow of study participants correlated with the 24-month progression-free survival estimate of 100% for patients with complete remission/complete remission with incomplete blood count recovery (CR/CRi), Stephan Stilgenbauer, MD, of the University of Ulm, Germany, and his colleagues reported in a poster at the annual meeting of the International Workshop on Chronic Lymphocytic Leukemia.
That response was maintained at 1 year in 85% of participants.
The current findings, which represent data through April 2017 for those 107 patients from the main cohort, as well as for 51 patients in the safety expansion study, show an overall response rate of 77%, with 20% CR/CRi.
The median time to first response was 1 month, and time to CR/CRi was 9.8 months, they said.
Estimates at 24 months for duration of response, progression-free survival, and overall survival were 66%, 54%, and 73%, respectively.
Additionally, objective responses were seen in four of five previously untreated patients who were enrolled in the safety expansion, and two of them had complete remissions. One patient with best response of stable disease decided to discontinue treatment but remained in follow-up with stable disease.
“All patients were alive at the time of analysis and remain progression free,” the investigators wrote.
In 18 patients who received prior B-cell receptor pathway inhibitor (BCRi) therapy, the objective response rate was 61% and the complete remission rate was 11%, with 12-month, progression-free and overall survival estimates of 50% and 54%, respectively.
Treatment-emergent adverse events of any grade occurred in 98% of patients, and led to dosing interruption in 40% and dosing adjustment in 17%. The most common adverse event was neutropenia; grade 3/4 neutropenia occurred in 40% of patients.
Neutropenia lead to a dose reduction in 8% of patients and to treatment interruption in 6% of patients; no discontinuations were reported.
Infections occurred in 81% of 158 patients, and grade 3/4 infections occurred in 23%; these infections were consistent with the underlying disease, the investigators said.
Laboratory tumor lysis syndrome (TLS) occurred in 5% of patients, but there were no episodes of clinical TLS, they said, noting that five TLS patients required dose interruptions. TLS occurred in four patients with medium risk at screening and in four with high risk. All episodes of TLS occurred during initial dosing or ramp-up, and all resolved. Affected patients were able to resume venetoclax with dose escalation to 400 mg/day.
The rate of minimal residual disease negativity was 30% in the intention-to-treat population as demonstrated by flow cytometry and confirmed by next generation sequencing (NGS) in 21 of 29 patients with an evaluable matched time point specimen. Bone marrow MRD negativity was observed in 20 patients by flow cytometry, and in 9 patients by NGS.
When looking at flow cytometry and NGS data combined, the MRD negativity rate in peripheral blood was 25% overall and 40% in evaluable patients, and the MRD negativity rate in bone marrow was 11% overall and 24% in evaluable patients.
Of those who achieved CR/CRi, 69% were MRD negative in peripheral blood by flow cytometry, with a 24-month, progression-free survival estimate of 100%, and 13 of those had confirmed MRD-negative blood by NGS, 2 had MRD-positive blood by NGS at a matched flow cytometry assessment, and 7 were not evaluated by NGS. For the remaining CR/CRi patients, who were MRD-positive by flow cytometry, the 24-month progression-free survival estimate was 86%.
Study participants in the main cohort were adults with a median age of 67 years who had relapsed/refractory CLL with an indication for treatment by iwCLL criteria, del(17p), good performance status, adequate bone marrow function, and creatinine clearance of at least 50 mg/min. They received a single test dose of 20 mg on day 1, with gradual ramp up to 400 mg over 4-5 weeks based on laboratory assessments. All were hospitalized for the first 20 mg and 50 mg venetoclax doses during ramp up.
Those in the safety expansion were treated with once-daily oral venetoclax starting at a dose of 20 mg/day for 1 week and ramped up to 400 mg by week 5. To mitigate TLS risk, uric acid–lowering agents and hydration were started at least 72 hours prior to administering the first dose. Those with high TLS risk – and some with medium risk – were hospitalized for the first 20-mg and 50-mg doses. Those with low TLS risk – and most with medium risk – received initial venetoclax dosing in an outpatient setting.
“Continued follow-up of patients in this trial will provide additional data on the durability of response with venetoclax in patients with del(17p) CLL,” the investigators wrote.
This study was supported by AbbVie and Genentech. Dr. Stilgenbauer received research funding, honoraria, and travel support from AbbVie, Amgen, Boehringer Ingelheim, Celgene, Genentech, Genzyme, Gilead, GSK, Janssen, Mundipharma, Novartis, Pharmacyclics, Hoffmann La-Roche, and Sanofi.
New York – Venetoclax monotherapy is associated with high and durable objective response rates in patients with del(17p) chronic lymphocytic leukemia (CLL), according to efficacy findings from the open-label M13-982 trial.
Additionally, a safety expansion of the pivotal phase 2 study showed that treatment was well tolerated, and assessment of minimal residual disease (MRD) status in the peripheral blood and bone marrow of study participants correlated with the 24-month progression-free survival estimate of 100% for patients with complete remission/complete remission with incomplete blood count recovery (CR/CRi), Stephan Stilgenbauer, MD, of the University of Ulm, Germany, and his colleagues reported in a poster at the annual meeting of the International Workshop on Chronic Lymphocytic Leukemia.
That response was maintained at 1 year in 85% of participants.
The current findings, which represent data through April 2017 for those 107 patients from the main cohort, as well as for 51 patients in the safety expansion study, show an overall response rate of 77%, with 20% CR/CRi.
The median time to first response was 1 month, and time to CR/CRi was 9.8 months, they said.
Estimates at 24 months for duration of response, progression-free survival, and overall survival were 66%, 54%, and 73%, respectively.
Additionally, objective responses were seen in four of five previously untreated patients who were enrolled in the safety expansion, and two of them had complete remissions. One patient with best response of stable disease decided to discontinue treatment but remained in follow-up with stable disease.
“All patients were alive at the time of analysis and remain progression free,” the investigators wrote.
In 18 patients who received prior B-cell receptor pathway inhibitor (BCRi) therapy, the objective response rate was 61% and the complete remission rate was 11%, with 12-month, progression-free and overall survival estimates of 50% and 54%, respectively.
Treatment-emergent adverse events of any grade occurred in 98% of patients, and led to dosing interruption in 40% and dosing adjustment in 17%. The most common adverse event was neutropenia; grade 3/4 neutropenia occurred in 40% of patients.
Neutropenia lead to a dose reduction in 8% of patients and to treatment interruption in 6% of patients; no discontinuations were reported.
Infections occurred in 81% of 158 patients, and grade 3/4 infections occurred in 23%; these infections were consistent with the underlying disease, the investigators said.
Laboratory tumor lysis syndrome (TLS) occurred in 5% of patients, but there were no episodes of clinical TLS, they said, noting that five TLS patients required dose interruptions. TLS occurred in four patients with medium risk at screening and in four with high risk. All episodes of TLS occurred during initial dosing or ramp-up, and all resolved. Affected patients were able to resume venetoclax with dose escalation to 400 mg/day.
The rate of minimal residual disease negativity was 30% in the intention-to-treat population as demonstrated by flow cytometry and confirmed by next generation sequencing (NGS) in 21 of 29 patients with an evaluable matched time point specimen. Bone marrow MRD negativity was observed in 20 patients by flow cytometry, and in 9 patients by NGS.
When looking at flow cytometry and NGS data combined, the MRD negativity rate in peripheral blood was 25% overall and 40% in evaluable patients, and the MRD negativity rate in bone marrow was 11% overall and 24% in evaluable patients.
Of those who achieved CR/CRi, 69% were MRD negative in peripheral blood by flow cytometry, with a 24-month, progression-free survival estimate of 100%, and 13 of those had confirmed MRD-negative blood by NGS, 2 had MRD-positive blood by NGS at a matched flow cytometry assessment, and 7 were not evaluated by NGS. For the remaining CR/CRi patients, who were MRD-positive by flow cytometry, the 24-month progression-free survival estimate was 86%.
Study participants in the main cohort were adults with a median age of 67 years who had relapsed/refractory CLL with an indication for treatment by iwCLL criteria, del(17p), good performance status, adequate bone marrow function, and creatinine clearance of at least 50 mg/min. They received a single test dose of 20 mg on day 1, with gradual ramp up to 400 mg over 4-5 weeks based on laboratory assessments. All were hospitalized for the first 20 mg and 50 mg venetoclax doses during ramp up.
Those in the safety expansion were treated with once-daily oral venetoclax starting at a dose of 20 mg/day for 1 week and ramped up to 400 mg by week 5. To mitigate TLS risk, uric acid–lowering agents and hydration were started at least 72 hours prior to administering the first dose. Those with high TLS risk – and some with medium risk – were hospitalized for the first 20-mg and 50-mg doses. Those with low TLS risk – and most with medium risk – received initial venetoclax dosing in an outpatient setting.
“Continued follow-up of patients in this trial will provide additional data on the durability of response with venetoclax in patients with del(17p) CLL,” the investigators wrote.
This study was supported by AbbVie and Genentech. Dr. Stilgenbauer received research funding, honoraria, and travel support from AbbVie, Amgen, Boehringer Ingelheim, Celgene, Genentech, Genzyme, Gilead, GSK, Janssen, Mundipharma, Novartis, Pharmacyclics, Hoffmann La-Roche, and Sanofi.
AT THE iwCLL MEETING
Key clinical point:
Major finding: At April 2017 data analysis, the overall response rate was 77% with 20% CR/CRi.
Data source: The phase 2 open-label M13-982 Trial and safety expansion cohort of 158 total patients.
Disclosures: This study was supported by AbbVie and Genentech. Dr. Stilgenbauer received research funding, honoraria, and travel support from AbbVie, Amgen, Boehringer Ingelheim, Celgene, Genentech, Genzyme, Gilead, GSK, Janssen, Mundipharma, Novartis, Pharmacyclics, Hoffmann La-Roche, and Sanofi.
TKI dose de-escalation feasible in CML with stable MMR
Tyrosine kinase inhibitor de-escalation is generally safe and may lead to symptom improvement in patients with chronic myeloid leukemia who respond well to the therapy, according to an interim analysis of the nonrandomized phase 2 DESTINY trial.
The findings imply that some patients are unnecessarily overtreated, as responses were sometimes maintained with lower tyrosine kinase inhibitor (TKI) doses, according to Richard E. Clark, MD, of the University of Liverpool, England, and his colleagues (Lancet Haematol. 2017 May 26;4:e310-16).
Of 174 patients with chronic myeloid leukemia (CML) in first chronic phase who had received TKIs for at least 3 years and who were either in stable molecular response 4 logs below the standard arbitrary baseline (MR4, 125 patients) or stable major molecular response (MMR) but not MR4 (49 patients) for at least 12 months at the time of enrollment, 12 (7%) had molecular recurrence during 12 months of half-dose TKI therapy, and all patients who experienced molecular recurrence regained MMR within 4 months of being back on full-dose TKIs, the researchers noted.
The median time to recovery was 77 days.
The recurrence rate was significantly lower in the MR4 cohort than in the MMR cohort (2% vs. 19%; hazard ratio, 0.12), and time to relapse was significantly longer in the MR4 cohort (median, 8.7 vs. 4.4 months), the investigators said.
Recurrence was not associated with age, sex, weight, performance status, BCR-ABL1 transcript type, or duration of TKI therapy, which was a median of 6.9 years overall, they noted.
During the first 3 months of de-escalation, adverse events associated with treatment, including lethargy, diarrhea, rash, and nausea, all improved.
Adverse events during de-escalation occurred in 16 patients, and included one fatality due to worsening of peripheral arterial occlusive disease, but all were deemed unrelated to the TKI or underlying chronic CML, the investigators noted.
Study subjects were adults with positive BCR-ABL1 transcripts, with either e13a2, e14a2, or e19a2 fusion transcript. They were enrolled between December 2013 and April 2015 from 20 hospitals in the United Kingdom; 148 were receiving imatinib, 16 were receiving nilotinib, and 10 were receiving dasatinib. They received half of their standard dose of imatinib (200 mg daily), dasatinib (50 mg daily), or nilotinib (200 mg twice daily) for 12 months. Recurrence during de-escalation was defined as BCR-ABL1:ABL1 ratio greater than 0.1% on two consecutive measurements.
“Although several studies of TKI cessation have been reported, little is known about the feasibility of treatment de-escalation in patients with stable molecular responses,” the investigators wrote, adding that the current study shows that de-escalation is “clearly safe for patients in stable MR4 or deeper remission” and could be a “reasonable option.”
This “practice-changing view” is reinforced by the finding of general improvement of adverse events in both cohorts, they said.
Also of note, de-escalation in this study was associated with savings of almost half the expected TKI costs, they added.
The findings imply that many patients with stable responses might be able to maintain responses on lower TKI doses, they concluded, adding that studies of more ambitious de-escalation are warranted.
Newcastle University and Bloodwise funded the study. Dr. Clark received other grants from Bloodwise during the study, as well as grants and personal fees from Novartis, Bristol-Myers Squibb, and Pfizer, and personal fees from Ariad/Incyte.
The interim DESTINY trial findings indicate the feasibility of a dose reduction approach to minimize adverse events associated with TKI treatment and to improve quality of life, Elisabetta Abruzzese, MD, wrote in an editorial.
De-escalation also appears to provide important cost savings, she noted (Lancet Haematol. 2017 Jul;4:e304-5).
“For patients who are unable to stop therapy, adjustment of the treatment doses without jeopardizing the clinical outcome has important clinical implications. Combination of reduced dosage TKIs with newer (ABL001) or older approaches (immunomodulation) might represent a future answer to that,” she said.
Dr. Abruzzese is with Tor Vergata University, Rome. She reported receiving personal fees from Ariad/Incyte, and serving on the advisory board or as a consultant for Novartis, Pfizer, Ariad/Incyte, and Bristol-Myers Squibb.
The interim DESTINY trial findings indicate the feasibility of a dose reduction approach to minimize adverse events associated with TKI treatment and to improve quality of life, Elisabetta Abruzzese, MD, wrote in an editorial.
De-escalation also appears to provide important cost savings, she noted (Lancet Haematol. 2017 Jul;4:e304-5).
“For patients who are unable to stop therapy, adjustment of the treatment doses without jeopardizing the clinical outcome has important clinical implications. Combination of reduced dosage TKIs with newer (ABL001) or older approaches (immunomodulation) might represent a future answer to that,” she said.
Dr. Abruzzese is with Tor Vergata University, Rome. She reported receiving personal fees from Ariad/Incyte, and serving on the advisory board or as a consultant for Novartis, Pfizer, Ariad/Incyte, and Bristol-Myers Squibb.
The interim DESTINY trial findings indicate the feasibility of a dose reduction approach to minimize adverse events associated with TKI treatment and to improve quality of life, Elisabetta Abruzzese, MD, wrote in an editorial.
De-escalation also appears to provide important cost savings, she noted (Lancet Haematol. 2017 Jul;4:e304-5).
“For patients who are unable to stop therapy, adjustment of the treatment doses without jeopardizing the clinical outcome has important clinical implications. Combination of reduced dosage TKIs with newer (ABL001) or older approaches (immunomodulation) might represent a future answer to that,” she said.
Dr. Abruzzese is with Tor Vergata University, Rome. She reported receiving personal fees from Ariad/Incyte, and serving on the advisory board or as a consultant for Novartis, Pfizer, Ariad/Incyte, and Bristol-Myers Squibb.
Tyrosine kinase inhibitor de-escalation is generally safe and may lead to symptom improvement in patients with chronic myeloid leukemia who respond well to the therapy, according to an interim analysis of the nonrandomized phase 2 DESTINY trial.
The findings imply that some patients are unnecessarily overtreated, as responses were sometimes maintained with lower tyrosine kinase inhibitor (TKI) doses, according to Richard E. Clark, MD, of the University of Liverpool, England, and his colleagues (Lancet Haematol. 2017 May 26;4:e310-16).
Of 174 patients with chronic myeloid leukemia (CML) in first chronic phase who had received TKIs for at least 3 years and who were either in stable molecular response 4 logs below the standard arbitrary baseline (MR4, 125 patients) or stable major molecular response (MMR) but not MR4 (49 patients) for at least 12 months at the time of enrollment, 12 (7%) had molecular recurrence during 12 months of half-dose TKI therapy, and all patients who experienced molecular recurrence regained MMR within 4 months of being back on full-dose TKIs, the researchers noted.
The median time to recovery was 77 days.
The recurrence rate was significantly lower in the MR4 cohort than in the MMR cohort (2% vs. 19%; hazard ratio, 0.12), and time to relapse was significantly longer in the MR4 cohort (median, 8.7 vs. 4.4 months), the investigators said.
Recurrence was not associated with age, sex, weight, performance status, BCR-ABL1 transcript type, or duration of TKI therapy, which was a median of 6.9 years overall, they noted.
During the first 3 months of de-escalation, adverse events associated with treatment, including lethargy, diarrhea, rash, and nausea, all improved.
Adverse events during de-escalation occurred in 16 patients, and included one fatality due to worsening of peripheral arterial occlusive disease, but all were deemed unrelated to the TKI or underlying chronic CML, the investigators noted.
Study subjects were adults with positive BCR-ABL1 transcripts, with either e13a2, e14a2, or e19a2 fusion transcript. They were enrolled between December 2013 and April 2015 from 20 hospitals in the United Kingdom; 148 were receiving imatinib, 16 were receiving nilotinib, and 10 were receiving dasatinib. They received half of their standard dose of imatinib (200 mg daily), dasatinib (50 mg daily), or nilotinib (200 mg twice daily) for 12 months. Recurrence during de-escalation was defined as BCR-ABL1:ABL1 ratio greater than 0.1% on two consecutive measurements.
“Although several studies of TKI cessation have been reported, little is known about the feasibility of treatment de-escalation in patients with stable molecular responses,” the investigators wrote, adding that the current study shows that de-escalation is “clearly safe for patients in stable MR4 or deeper remission” and could be a “reasonable option.”
This “practice-changing view” is reinforced by the finding of general improvement of adverse events in both cohorts, they said.
Also of note, de-escalation in this study was associated with savings of almost half the expected TKI costs, they added.
The findings imply that many patients with stable responses might be able to maintain responses on lower TKI doses, they concluded, adding that studies of more ambitious de-escalation are warranted.
Newcastle University and Bloodwise funded the study. Dr. Clark received other grants from Bloodwise during the study, as well as grants and personal fees from Novartis, Bristol-Myers Squibb, and Pfizer, and personal fees from Ariad/Incyte.
Tyrosine kinase inhibitor de-escalation is generally safe and may lead to symptom improvement in patients with chronic myeloid leukemia who respond well to the therapy, according to an interim analysis of the nonrandomized phase 2 DESTINY trial.
The findings imply that some patients are unnecessarily overtreated, as responses were sometimes maintained with lower tyrosine kinase inhibitor (TKI) doses, according to Richard E. Clark, MD, of the University of Liverpool, England, and his colleagues (Lancet Haematol. 2017 May 26;4:e310-16).
Of 174 patients with chronic myeloid leukemia (CML) in first chronic phase who had received TKIs for at least 3 years and who were either in stable molecular response 4 logs below the standard arbitrary baseline (MR4, 125 patients) or stable major molecular response (MMR) but not MR4 (49 patients) for at least 12 months at the time of enrollment, 12 (7%) had molecular recurrence during 12 months of half-dose TKI therapy, and all patients who experienced molecular recurrence regained MMR within 4 months of being back on full-dose TKIs, the researchers noted.
The median time to recovery was 77 days.
The recurrence rate was significantly lower in the MR4 cohort than in the MMR cohort (2% vs. 19%; hazard ratio, 0.12), and time to relapse was significantly longer in the MR4 cohort (median, 8.7 vs. 4.4 months), the investigators said.
Recurrence was not associated with age, sex, weight, performance status, BCR-ABL1 transcript type, or duration of TKI therapy, which was a median of 6.9 years overall, they noted.
During the first 3 months of de-escalation, adverse events associated with treatment, including lethargy, diarrhea, rash, and nausea, all improved.
Adverse events during de-escalation occurred in 16 patients, and included one fatality due to worsening of peripheral arterial occlusive disease, but all were deemed unrelated to the TKI or underlying chronic CML, the investigators noted.
Study subjects were adults with positive BCR-ABL1 transcripts, with either e13a2, e14a2, or e19a2 fusion transcript. They were enrolled between December 2013 and April 2015 from 20 hospitals in the United Kingdom; 148 were receiving imatinib, 16 were receiving nilotinib, and 10 were receiving dasatinib. They received half of their standard dose of imatinib (200 mg daily), dasatinib (50 mg daily), or nilotinib (200 mg twice daily) for 12 months. Recurrence during de-escalation was defined as BCR-ABL1:ABL1 ratio greater than 0.1% on two consecutive measurements.
“Although several studies of TKI cessation have been reported, little is known about the feasibility of treatment de-escalation in patients with stable molecular responses,” the investigators wrote, adding that the current study shows that de-escalation is “clearly safe for patients in stable MR4 or deeper remission” and could be a “reasonable option.”
This “practice-changing view” is reinforced by the finding of general improvement of adverse events in both cohorts, they said.
Also of note, de-escalation in this study was associated with savings of almost half the expected TKI costs, they added.
The findings imply that many patients with stable responses might be able to maintain responses on lower TKI doses, they concluded, adding that studies of more ambitious de-escalation are warranted.
Newcastle University and Bloodwise funded the study. Dr. Clark received other grants from Bloodwise during the study, as well as grants and personal fees from Novartis, Bristol-Myers Squibb, and Pfizer, and personal fees from Ariad/Incyte.
FROM LANCET HAEMATOLOGY
Key clinical point:
Major finding: Only 12 of 174 CML patients had molecular recurrence during 12 months of half-dose TKI therapy, and all regained MMR within 4 months of being back on full-dose TKIs.
Data source: The nonrandomized phase 2 DESTINY study of 174 adults with CML.
Disclosures: Newcastle University and Bloodwise funded the study. Dr. Clark received other grants from Bloodwise during the study, as well as grants and personal fees from Novartis, Bristol-Myers Squibb, and Pfizer, and personal fees from Ariad/Incyte.
Study: No increased mortality with ACA-prompted readmission declines
Concerns that efforts to reduce 30-day hospital readmission rates under the Affordable Care Act’s Hospital Readmission Reduction Program might lead to unintended increases in mortality rates appear to be unfounded, according to a review of more than 6.7 million hospitalizations for heart failure, acute myocardial infarction, or pneumonia between 2008 and 2014.
In fact, reductions in 30-day readmission rates among Medicare fee-for-service beneficiaries are weakly but significantly correlated with reductions in hospital 30-day mortality rates after discharge, according to Kumar Dharmarajan, MD, of Yale New Haven (Conn.) Health, and colleagues (JAMA 2017 Jul 18;318[3]:270-8. doi: 10.1001/jama.2017.8444).
From 2008 to 2014, the RARRs declined in aggregate across hospitals (–0.053% for heart failure, –0.044% for acute MI, and –0.033% for pneumonia).
“In contrast, monthly aggregate trends across hospitals in 30-day risk-adjusted mortality rates after discharge varied by admitting condition” the investigators said.
For heart failure, acute MI, and pneumonia, there was an increase of 0.008%, a decrease of 0.003%, and an increase of 0.001%, respectively, they said. However, paired monthly trends in 30-day RARRs and 30-day RAMRs after discharge “identified concomitant reduction in readmission and mortality rates within hospitals.”
Correlation coefficients of the paired monthly trends for heart failure, acute MI, and pneumonia in 2008-2014 were 0.066, 0.067, and 0.108, respectively.
“Paired trends in hospital 30-day risk-adjusted readmission rates and both 90-day risk-adjusted mortality rates after discharge and 90-day risk-adjusted mortality rates after the admission date also identified concomitant reductions in readmission and mortality rates within hospitals,” the authors wrote.
The findings “do not support increasing postdischarge mortality related to reducing hospital readmissions,” they concluded.
The authors work under contract with the Centers for Medicare & Medicaid Services to develop and maintain performance measures. Dr. Dharmarajan reported serving as a consultant and scientific advisory board member for Clover Health at the time this research was performed. He is supported by grants from the National Institute on Aging and the American Federation for Aging Research, and the Yale Claude D. Pepper Older Americans Independence Center.
The findings by Dharmarajan and colleagues are “certainly good news,” Karen E. Joynt Maddox, MD, wrote in an editorial.
The study provides support for strategies that hospitals are using to reduce readmissions, and also underscores the importance of evaluating unintended consequences of policy changes such as the Affordable Care Act’s Hospital Readmissions Reduction Program (HRRP), she said (JAMA. 2017 Jul 18;318[3]:243-4).
The study did not address the possibility that attention to reducing readmissions has taken priority over reducing mortality, which could have the unintended consequence of slowing improvements in mortality, she noted, suggesting that for this and other reasons it may be “time to reexamine and reengineer the HRRP to avoid unintended consequences and to ensure that its incentives are fully aligned with the ultimate goal of improving the health outcomes of patients.
“Only with full knowledge of the advantages and disadvantages of a particular policy decision can policy makers and advocates work to craft statutes and rules that maximize benefits while minimizing harms,” she wrote.
Dr. Joynt Maddox is with Brigham and Women’s Hospital, Boston. She is supported by a grant from the National Heart, Lung, and Blood Institute.
The findings by Dharmarajan and colleagues are “certainly good news,” Karen E. Joynt Maddox, MD, wrote in an editorial.
The study provides support for strategies that hospitals are using to reduce readmissions, and also underscores the importance of evaluating unintended consequences of policy changes such as the Affordable Care Act’s Hospital Readmissions Reduction Program (HRRP), she said (JAMA. 2017 Jul 18;318[3]:243-4).
The study did not address the possibility that attention to reducing readmissions has taken priority over reducing mortality, which could have the unintended consequence of slowing improvements in mortality, she noted, suggesting that for this and other reasons it may be “time to reexamine and reengineer the HRRP to avoid unintended consequences and to ensure that its incentives are fully aligned with the ultimate goal of improving the health outcomes of patients.
“Only with full knowledge of the advantages and disadvantages of a particular policy decision can policy makers and advocates work to craft statutes and rules that maximize benefits while minimizing harms,” she wrote.
Dr. Joynt Maddox is with Brigham and Women’s Hospital, Boston. She is supported by a grant from the National Heart, Lung, and Blood Institute.
The findings by Dharmarajan and colleagues are “certainly good news,” Karen E. Joynt Maddox, MD, wrote in an editorial.
The study provides support for strategies that hospitals are using to reduce readmissions, and also underscores the importance of evaluating unintended consequences of policy changes such as the Affordable Care Act’s Hospital Readmissions Reduction Program (HRRP), she said (JAMA. 2017 Jul 18;318[3]:243-4).
The study did not address the possibility that attention to reducing readmissions has taken priority over reducing mortality, which could have the unintended consequence of slowing improvements in mortality, she noted, suggesting that for this and other reasons it may be “time to reexamine and reengineer the HRRP to avoid unintended consequences and to ensure that its incentives are fully aligned with the ultimate goal of improving the health outcomes of patients.
“Only with full knowledge of the advantages and disadvantages of a particular policy decision can policy makers and advocates work to craft statutes and rules that maximize benefits while minimizing harms,” she wrote.
Dr. Joynt Maddox is with Brigham and Women’s Hospital, Boston. She is supported by a grant from the National Heart, Lung, and Blood Institute.
Concerns that efforts to reduce 30-day hospital readmission rates under the Affordable Care Act’s Hospital Readmission Reduction Program might lead to unintended increases in mortality rates appear to be unfounded, according to a review of more than 6.7 million hospitalizations for heart failure, acute myocardial infarction, or pneumonia between 2008 and 2014.
In fact, reductions in 30-day readmission rates among Medicare fee-for-service beneficiaries are weakly but significantly correlated with reductions in hospital 30-day mortality rates after discharge, according to Kumar Dharmarajan, MD, of Yale New Haven (Conn.) Health, and colleagues (JAMA 2017 Jul 18;318[3]:270-8. doi: 10.1001/jama.2017.8444).
From 2008 to 2014, the RARRs declined in aggregate across hospitals (–0.053% for heart failure, –0.044% for acute MI, and –0.033% for pneumonia).
“In contrast, monthly aggregate trends across hospitals in 30-day risk-adjusted mortality rates after discharge varied by admitting condition” the investigators said.
For heart failure, acute MI, and pneumonia, there was an increase of 0.008%, a decrease of 0.003%, and an increase of 0.001%, respectively, they said. However, paired monthly trends in 30-day RARRs and 30-day RAMRs after discharge “identified concomitant reduction in readmission and mortality rates within hospitals.”
Correlation coefficients of the paired monthly trends for heart failure, acute MI, and pneumonia in 2008-2014 were 0.066, 0.067, and 0.108, respectively.
“Paired trends in hospital 30-day risk-adjusted readmission rates and both 90-day risk-adjusted mortality rates after discharge and 90-day risk-adjusted mortality rates after the admission date also identified concomitant reductions in readmission and mortality rates within hospitals,” the authors wrote.
The findings “do not support increasing postdischarge mortality related to reducing hospital readmissions,” they concluded.
The authors work under contract with the Centers for Medicare & Medicaid Services to develop and maintain performance measures. Dr. Dharmarajan reported serving as a consultant and scientific advisory board member for Clover Health at the time this research was performed. He is supported by grants from the National Institute on Aging and the American Federation for Aging Research, and the Yale Claude D. Pepper Older Americans Independence Center.
Concerns that efforts to reduce 30-day hospital readmission rates under the Affordable Care Act’s Hospital Readmission Reduction Program might lead to unintended increases in mortality rates appear to be unfounded, according to a review of more than 6.7 million hospitalizations for heart failure, acute myocardial infarction, or pneumonia between 2008 and 2014.
In fact, reductions in 30-day readmission rates among Medicare fee-for-service beneficiaries are weakly but significantly correlated with reductions in hospital 30-day mortality rates after discharge, according to Kumar Dharmarajan, MD, of Yale New Haven (Conn.) Health, and colleagues (JAMA 2017 Jul 18;318[3]:270-8. doi: 10.1001/jama.2017.8444).
From 2008 to 2014, the RARRs declined in aggregate across hospitals (–0.053% for heart failure, –0.044% for acute MI, and –0.033% for pneumonia).
“In contrast, monthly aggregate trends across hospitals in 30-day risk-adjusted mortality rates after discharge varied by admitting condition” the investigators said.
For heart failure, acute MI, and pneumonia, there was an increase of 0.008%, a decrease of 0.003%, and an increase of 0.001%, respectively, they said. However, paired monthly trends in 30-day RARRs and 30-day RAMRs after discharge “identified concomitant reduction in readmission and mortality rates within hospitals.”
Correlation coefficients of the paired monthly trends for heart failure, acute MI, and pneumonia in 2008-2014 were 0.066, 0.067, and 0.108, respectively.
“Paired trends in hospital 30-day risk-adjusted readmission rates and both 90-day risk-adjusted mortality rates after discharge and 90-day risk-adjusted mortality rates after the admission date also identified concomitant reductions in readmission and mortality rates within hospitals,” the authors wrote.
The findings “do not support increasing postdischarge mortality related to reducing hospital readmissions,” they concluded.
The authors work under contract with the Centers for Medicare & Medicaid Services to develop and maintain performance measures. Dr. Dharmarajan reported serving as a consultant and scientific advisory board member for Clover Health at the time this research was performed. He is supported by grants from the National Institute on Aging and the American Federation for Aging Research, and the Yale Claude D. Pepper Older Americans Independence Center.
FROM JAMA
Key clinical point:
Major finding: Correlation coefficients of the paired monthly trends for heart failure, acute myocardial infarction, and pneumonia in 2008-2014 were 0.066, 0.067, and 0.108, respectively.
Data source: A retrospective review of more than 6.7 million hospitalized Medicare fee-for-service beneficiaries.
Disclosures: The authors work under contract with the Centers for Medicare & Medicaid Services to develop and maintain performance measures. Dr. Dharmarajan reported serving as a consultant and scientific advisory board member for Clover Health at the time this research was performed. He is supported by grants from the National Institute on Aging and the American Federation for Aging Research, and the Yale Claude D. Pepper Older Americans Independence Center.
Report: Opioid epidemic fight must increase substantially and immediately
A concerted, multiagency, multipronged counterattack is needed to break the opioid epidemic’s grip on the nation, according to a new report from the National Academies of Sciences, Engineering, and Medicine.
The report, commissioned by the Food and Drug Administration to strengthen its own 2016 Opioids Action Plan, presents a national strategy for addressing this “urgent public health priority.”
“The ongoing opioid crisis lies at the intersection of two substantial public health challenges – reducing the burden of suffering from pain and containing the rising toll of the harms that can result from the use of opioid medications,” according to a summary of the report, “Pain Management and the Opioid Epidemic: Balancing Societal and Individual Benefits and Risks of Prescription Opioid Use.”
The National Academies’ Committee on Pain Management and Regulatory Strategies to Address Prescription Opioid Abuse spent more than a year studying the matter and developing the report. Among its recommendations is a call for investment in research to better understand pain and opioid use disorder.
“We have a specific lack of knowledge about how pain and opiate use disorder [OUD] interact – that is, why patients in pain might be more or less at risk for the development of opiate use disorder when exposed to either illicit or prescription medication,” committee member David Clark, MD, professor of anesthesia, perioperative pain medicine, and pain at Stanford (Calif.) University, said during a webinar on the report.
“This leads up to one of our first recommendations, which is to invest in research to better understand pain and opiate use disorder,” Dr. Clark said. “We want to emphasize that we need to improve our understanding of the neurobiology of pain,” which will, hopefully, provide a better foundation for the development of nonopioid treatments.
The committee also recommended that the FDA:
- Incorporate public health considerations into opioid-related regulatory decisions.
- Require additional studies along with the collection and analysis of data needed to thoroughly assess broad public health considerations.
- Ensure that public health considerations are adequately incorporated into clinical development.
- Increase transparency of regulatory decisions for opioids in light of the proposed systems approach.
“The committee believes a commitment to transparency is critical to maintain balance between preserving access to opioids when needed and mitigating opioid-related harms and to maintain public trust,” the report’s authors said. “The committee also believes aggressive use of the FDA’s currently available authorities, such as Risk Evaluation and Mitigation Strategies (REMS), safety labeling changes, and risk communications is critical to supporting the safe and effective use of opioids.”
The committee also recommended strengthening the postapproval oversight of opioids.
A full review of currently marketed and approved opioids was also recommended, as was the application of public health consideration to opioid scheduling decisions.
“The particular characteristics of opioids, we believe, require a certain amount of what we term ‘opioid exceptionalism’ from the regulator in terms of trying to consider the larger societal effects of approval and use of opioid medication,” committee member Aaron S. Kesselheim, MD, JD, of Harvard Medical School, Boston, said during the webinar. “We believe that this public health approach is both reasonable for the FDA, given the fact that it is primarily a public health agency, and can be implemented at all different levels of the development process.”
Strategies recommended by the committee for the FDA, state agencies, health professionals, and relevant private organizations, such as through public-private partnerships, include:
- Restricting the supply of opioids, with careful attention to risks and benefits of interventions aimed at reducing the supply in the community. Recommendation: Improve access to drug take-back programs.
- Improving prescribing practices. Recommendations: Establish comprehensive pain education materials and curricula for health care providers; facilitate reimbursement for comprehensive pain management; and improve the use of prescription drug monitoring program data for surveillance and intervention.
- Reducing demand. Recommendations: Evaluate the impact on patient and public education about opioids on promoting safe and effective pain management; expand treatment for opioid use disorder; improve education regarding treatment of OUD for health care providers; and remove barriers to coverage of approved medication for OUD treatment.
- Reducing harm. Recommendations: Leverage prescribers and pharmacists to help address opioid use disorder; and improve access to naloxone and safe injection equipment.
According to the report, containing the opioid epidemic and ameliorating its harmful effects on society through the development of these strategies will require “years of sustained and coordinated effort.”
Indeed, things will get worse before they get better, the committee predicted.
“Trends indicate that premature deaths associated with the use of opioids are likely to climb and that opioid overdose and other opioid-related harm will dramatically reduce quality of life for many people for years to come,” the report’s authors noted. “Access to evidence-based treatment for OUD and efforts to prevent overdose deaths and other harms should therefore be increased substantially and immediately as a public health priority.”
A concerted, multiagency, multipronged counterattack is needed to break the opioid epidemic’s grip on the nation, according to a new report from the National Academies of Sciences, Engineering, and Medicine.
The report, commissioned by the Food and Drug Administration to strengthen its own 2016 Opioids Action Plan, presents a national strategy for addressing this “urgent public health priority.”
“The ongoing opioid crisis lies at the intersection of two substantial public health challenges – reducing the burden of suffering from pain and containing the rising toll of the harms that can result from the use of opioid medications,” according to a summary of the report, “Pain Management and the Opioid Epidemic: Balancing Societal and Individual Benefits and Risks of Prescription Opioid Use.”
The National Academies’ Committee on Pain Management and Regulatory Strategies to Address Prescription Opioid Abuse spent more than a year studying the matter and developing the report. Among its recommendations is a call for investment in research to better understand pain and opioid use disorder.
“We have a specific lack of knowledge about how pain and opiate use disorder [OUD] interact – that is, why patients in pain might be more or less at risk for the development of opiate use disorder when exposed to either illicit or prescription medication,” committee member David Clark, MD, professor of anesthesia, perioperative pain medicine, and pain at Stanford (Calif.) University, said during a webinar on the report.
“This leads up to one of our first recommendations, which is to invest in research to better understand pain and opiate use disorder,” Dr. Clark said. “We want to emphasize that we need to improve our understanding of the neurobiology of pain,” which will, hopefully, provide a better foundation for the development of nonopioid treatments.
The committee also recommended that the FDA:
- Incorporate public health considerations into opioid-related regulatory decisions.
- Require additional studies along with the collection and analysis of data needed to thoroughly assess broad public health considerations.
- Ensure that public health considerations are adequately incorporated into clinical development.
- Increase transparency of regulatory decisions for opioids in light of the proposed systems approach.
“The committee believes a commitment to transparency is critical to maintain balance between preserving access to opioids when needed and mitigating opioid-related harms and to maintain public trust,” the report’s authors said. “The committee also believes aggressive use of the FDA’s currently available authorities, such as Risk Evaluation and Mitigation Strategies (REMS), safety labeling changes, and risk communications is critical to supporting the safe and effective use of opioids.”
The committee also recommended strengthening the postapproval oversight of opioids.
A full review of currently marketed and approved opioids was also recommended, as was the application of public health consideration to opioid scheduling decisions.
“The particular characteristics of opioids, we believe, require a certain amount of what we term ‘opioid exceptionalism’ from the regulator in terms of trying to consider the larger societal effects of approval and use of opioid medication,” committee member Aaron S. Kesselheim, MD, JD, of Harvard Medical School, Boston, said during the webinar. “We believe that this public health approach is both reasonable for the FDA, given the fact that it is primarily a public health agency, and can be implemented at all different levels of the development process.”
Strategies recommended by the committee for the FDA, state agencies, health professionals, and relevant private organizations, such as through public-private partnerships, include:
- Restricting the supply of opioids, with careful attention to risks and benefits of interventions aimed at reducing the supply in the community. Recommendation: Improve access to drug take-back programs.
- Improving prescribing practices. Recommendations: Establish comprehensive pain education materials and curricula for health care providers; facilitate reimbursement for comprehensive pain management; and improve the use of prescription drug monitoring program data for surveillance and intervention.
- Reducing demand. Recommendations: Evaluate the impact on patient and public education about opioids on promoting safe and effective pain management; expand treatment for opioid use disorder; improve education regarding treatment of OUD for health care providers; and remove barriers to coverage of approved medication for OUD treatment.
- Reducing harm. Recommendations: Leverage prescribers and pharmacists to help address opioid use disorder; and improve access to naloxone and safe injection equipment.
According to the report, containing the opioid epidemic and ameliorating its harmful effects on society through the development of these strategies will require “years of sustained and coordinated effort.”
Indeed, things will get worse before they get better, the committee predicted.
“Trends indicate that premature deaths associated with the use of opioids are likely to climb and that opioid overdose and other opioid-related harm will dramatically reduce quality of life for many people for years to come,” the report’s authors noted. “Access to evidence-based treatment for OUD and efforts to prevent overdose deaths and other harms should therefore be increased substantially and immediately as a public health priority.”
A concerted, multiagency, multipronged counterattack is needed to break the opioid epidemic’s grip on the nation, according to a new report from the National Academies of Sciences, Engineering, and Medicine.
The report, commissioned by the Food and Drug Administration to strengthen its own 2016 Opioids Action Plan, presents a national strategy for addressing this “urgent public health priority.”
“The ongoing opioid crisis lies at the intersection of two substantial public health challenges – reducing the burden of suffering from pain and containing the rising toll of the harms that can result from the use of opioid medications,” according to a summary of the report, “Pain Management and the Opioid Epidemic: Balancing Societal and Individual Benefits and Risks of Prescription Opioid Use.”
The National Academies’ Committee on Pain Management and Regulatory Strategies to Address Prescription Opioid Abuse spent more than a year studying the matter and developing the report. Among its recommendations is a call for investment in research to better understand pain and opioid use disorder.
“We have a specific lack of knowledge about how pain and opiate use disorder [OUD] interact – that is, why patients in pain might be more or less at risk for the development of opiate use disorder when exposed to either illicit or prescription medication,” committee member David Clark, MD, professor of anesthesia, perioperative pain medicine, and pain at Stanford (Calif.) University, said during a webinar on the report.
“This leads up to one of our first recommendations, which is to invest in research to better understand pain and opiate use disorder,” Dr. Clark said. “We want to emphasize that we need to improve our understanding of the neurobiology of pain,” which will, hopefully, provide a better foundation for the development of nonopioid treatments.
The committee also recommended that the FDA:
- Incorporate public health considerations into opioid-related regulatory decisions.
- Require additional studies along with the collection and analysis of data needed to thoroughly assess broad public health considerations.
- Ensure that public health considerations are adequately incorporated into clinical development.
- Increase transparency of regulatory decisions for opioids in light of the proposed systems approach.
“The committee believes a commitment to transparency is critical to maintain balance between preserving access to opioids when needed and mitigating opioid-related harms and to maintain public trust,” the report’s authors said. “The committee also believes aggressive use of the FDA’s currently available authorities, such as Risk Evaluation and Mitigation Strategies (REMS), safety labeling changes, and risk communications is critical to supporting the safe and effective use of opioids.”
The committee also recommended strengthening the postapproval oversight of opioids.
A full review of currently marketed and approved opioids was also recommended, as was the application of public health consideration to opioid scheduling decisions.
“The particular characteristics of opioids, we believe, require a certain amount of what we term ‘opioid exceptionalism’ from the regulator in terms of trying to consider the larger societal effects of approval and use of opioid medication,” committee member Aaron S. Kesselheim, MD, JD, of Harvard Medical School, Boston, said during the webinar. “We believe that this public health approach is both reasonable for the FDA, given the fact that it is primarily a public health agency, and can be implemented at all different levels of the development process.”
Strategies recommended by the committee for the FDA, state agencies, health professionals, and relevant private organizations, such as through public-private partnerships, include:
- Restricting the supply of opioids, with careful attention to risks and benefits of interventions aimed at reducing the supply in the community. Recommendation: Improve access to drug take-back programs.
- Improving prescribing practices. Recommendations: Establish comprehensive pain education materials and curricula for health care providers; facilitate reimbursement for comprehensive pain management; and improve the use of prescription drug monitoring program data for surveillance and intervention.
- Reducing demand. Recommendations: Evaluate the impact on patient and public education about opioids on promoting safe and effective pain management; expand treatment for opioid use disorder; improve education regarding treatment of OUD for health care providers; and remove barriers to coverage of approved medication for OUD treatment.
- Reducing harm. Recommendations: Leverage prescribers and pharmacists to help address opioid use disorder; and improve access to naloxone and safe injection equipment.
According to the report, containing the opioid epidemic and ameliorating its harmful effects on society through the development of these strategies will require “years of sustained and coordinated effort.”
Indeed, things will get worse before they get better, the committee predicted.
“Trends indicate that premature deaths associated with the use of opioids are likely to climb and that opioid overdose and other opioid-related harm will dramatically reduce quality of life for many people for years to come,” the report’s authors noted. “Access to evidence-based treatment for OUD and efforts to prevent overdose deaths and other harms should therefore be increased substantially and immediately as a public health priority.”