User login
Inexperience is the main cause of unsafe driving among teens
NEW ORLEANS – Teens need to drive for a wide range of reasons, from going to and from school or work to overall mobility, but driving still is the most dangerous thing teenagers do, according to Brian Johnston, MD, MPH, professor of pediatrics at the University of Washington in Seattle.
Motor vehicle traffic accidents continue to be the leading cause of death of adolescents aged 15-19 years, according to 2017 data from the National Center for Health Statistics at the Centers for the Disease Control and Prevention.
“Inexperience drives the statistics we see,” Dr. Johnston said at the annual meeting of the American Academy of Pediatrics. “There is a steep learning curve among drivers of all ages, and crash rates are highest during the first few months after teens begin driving without supervision.”
Although the risk of accidents is higher than average for any new driver, it’s disproportionately higher for younger teens, compared with other ages: 16-year-old novice drivers have a higher accident risk than that of 17-year-olds, whose risk is similar to that of 18- and 19-year-old novices.
How long drivers have been licensed has a far bigger impact on crash risk, Dr. Johnston said (Traffic Inj. Prev. 2009 Jun;10[3]:209-19).
But the risk of an accident also increases with each additional passenger a teen driver has, particularly for younger and male drivers (Traffic Inj Prev. 2013;14[3]:283-92). More passengers likely means more distraction, and distraction, driving too fast for road conditions, and not scanning the roadway are the three most common errors – together accounting for about half of all teen drivers’ crashes.
Risk factors for accidents
Speed is a contributing factor in just over a third (36%) of teens’ fatal crashes. Adolescents drive faster and keep shorter following distances than adults do. But as with adults, wearing seat belts substantially reduces the risk of death in accidents.
Nationally, 90% of drivers use seat belts, with higher rates in states with primary enforcement (92%) than those in states with secondary enforcement (83%).
But barely more than half (54%) of U.S. high school students say they “always” wear a seat belt, and just under half of teens (47%) who died in crashes in 2017 weren’t wearing one. As seen in adults, teens are more likely to buckle up, by 12%, in states with primary seat belt laws.
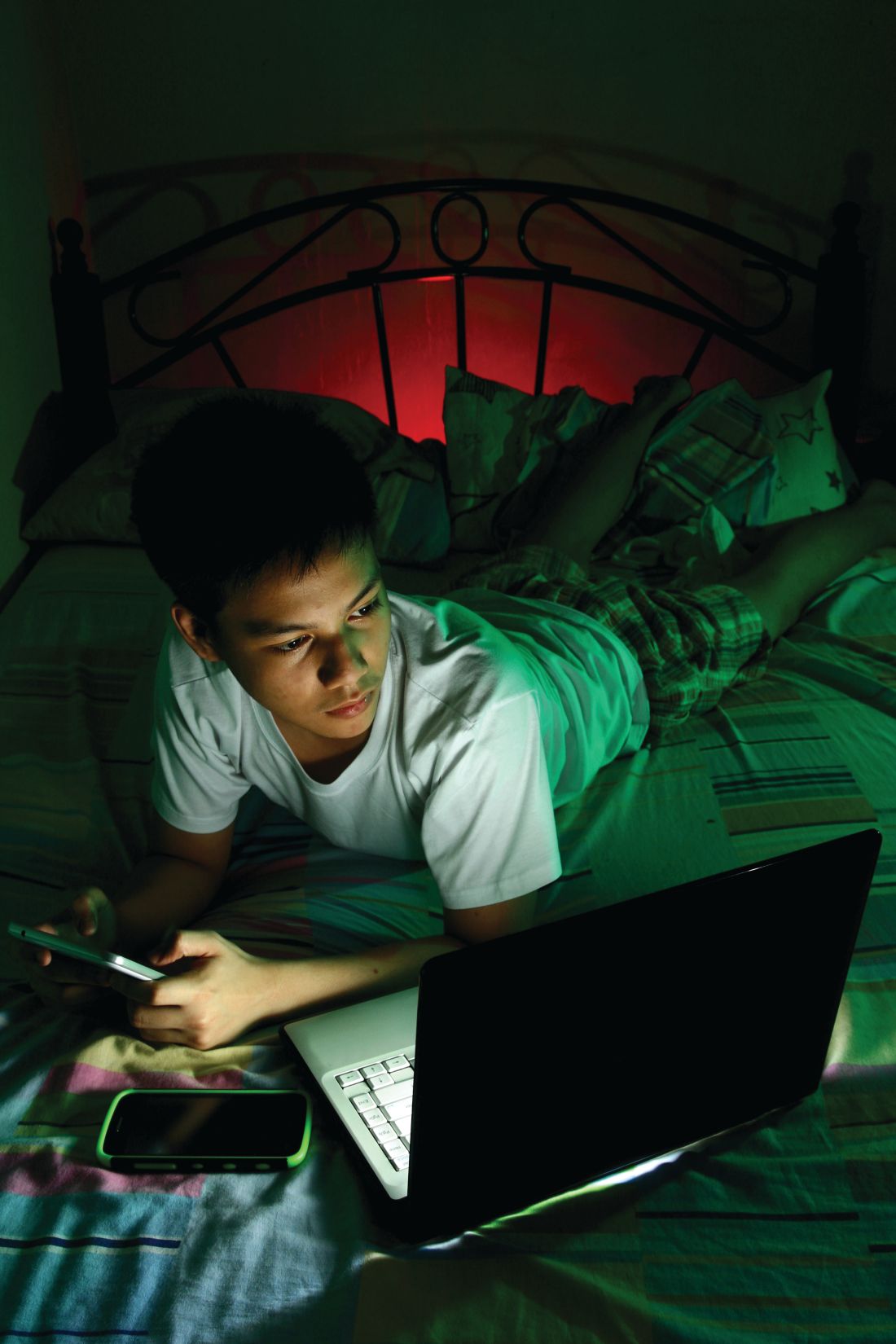
Distraction during driving can be visual, manual, or cognitive – and handheld electronic devices such as smartphones cause all three distraction types. Cell phones nearly double the proportion of teen drivers who die in crashes, from 7% to 13%.
But if teens can keep their eyes on the roadway at all times, even the risks posed by cellphones drop considerably.
“The best evidence shows that secondary tasks only degrade driving performance when they require drivers to look away from the road,” Dr. Johnston said. Looking away for 2 seconds or longer increases crash risk more than fivefold.
Two other risk factors for teen car accidents are drowsiness and nighttime driving. Sleepiness can play a role in crashes at any time of day, and Dr. Johnston noted that some research has associated later high school start times with reduced crash risk.
Teens aged 16-19 years are about four times more likely to have a car accident at night than during the day per each mile driven, the pediatrician noted. Many licensing laws restrict teen driving starting at 11 p.m. or later, but about 50%-60% of their crashes occur between 9 and 11 p.m.
One reason for the increased risk is less experience driving in more difficult conditions, but teens also are more likely to have teen passengers, to be driving excessively fast, or to be under the influence of alcohol at night.
Adolescents’ crash risk is higher than that of adults for any level of blood alcohol content. Self-reported driving after drinking dropped by almost half – from 10% to 5.5% – from 2013 to 2017, but alcohol still is implicated in a substantial number of fatal teen crashes.
As drunk driving has declined, however, driving while under the influence of marijuana has been increasing. According to the National Highway Traffic Safety Administration, case control studies show drivers with tetrahydrocannabinol (THC) in their blood have a 25% increased risk of accidents – but the excess risk associated with THC vanishes when researchers control for age, sex, and concurrent use of alcohol. Not enough research exists to determine what the crash risk would be for adolescent drivers using THC alone.
A less-recognized risk factor for car accidents in teen drivers is ADHD, which increases a teen’s risk of crashing by 36%, particularly in the first month after getting a license, Dr. Johnston said.
ADHD medication appears to mitigate the danger, according to data: Crash risk was 40% lower in adult drivers with ADHD during months they filled their stimulant prescriptions. But one study found only 12% of teens with ADHD filled their prescriptions the month they got their license, and adolescents may not take their medications or still have them in their system on weekends or at night.
Teens recovering from concussion also may have an increased risk. Some evidence suggests driving impairment continues even when other symptoms have resolved, but not enough data exist to determine appropriate criteria for clearing teens to begin driving again.
Interventions to improve teens’ driving safety
Most teens take a basic driver education course before getting their licenses, but no evidence shows that it reduces risk of citations, crashes, or injury. In fact, “skid control training and other kinds of advanced skill training seem to increase crash risk, particularly among young males,” Dr. Johnston said.
What helps teens most is, ironically, more driving.
“If I say inexperience is the single most important risk factor for dying in a crash as a teen, driving experience is the intervention,” he said. More time spent driving – “with supervision in particular, and under diverse conditions,” Dr. Johnston said – increases the repertoire of skills and abilities.
Parents should be encouraged to ride along as their teens drive under diverse road conditions: different roads, different times of the day, and different weather conditions, for example. Parents can narrate their own driving, pointing out hazards and times when they slow down for increased caution, Dr. Johnston said. It might feel “awkward and unnatural,” but “some of the things you as a driver notice all the time are novel to teen drivers.”
Parents can influence road safety for teens in terms of their own behavior and in selecting a safer vehicle. A strong correlation exists between parental texting while driving when children are younger and what they do as teen drivers, for example.
Safer vehicles are bigger, heavier cars with electronic stability control, which reduces risk of death about as much as wearing seat belts. Parents should avoid vehicles with high horsepower and look for cars with the best safety ratings they can afford, Dr. Johnston said.
Several special features in newer cars can help reduce crash risk, such as blind spot detection, automatic breaking, collision avoidance systems, lane departure warning systems, and driver drowsiness detection. Parents may worry that relying on this technology could reduce teens’ learning, but it actually can compensate for skill deficits as they are becoming more skilled drivers.
Parents can look into feedback programs such as smartphone apps or other in-car units that allow parents to see data on teens’ speed, unsafe driving, “near-misses,” and similar driving behaviors. Research has shown that unsafe driving in newly licensed teens dropped by 66% over 4 months of using one of these feedback programs, compared with teens who didn’t use it.
Dr. Johnston also discussed the idea of prelicensure medical exams, similar to physicals that are required before playing sports. These already exist for commercial licenses in most states, but no data exist on whether it’s effective for teens. The goal would be to promote a discussion between parents and their teens about driving: reviewing medications the teen is taking and whether they affect driving; discussing safety of different vehicles; and assessing the teens’ risks, including any cognitive or other medical conditions that could affect driving safety. Even if such a “driving physical” is not currently required, pediatricians can do their own version of one with families.
Dr. Johnston had no disclosures.
NEW ORLEANS – Teens need to drive for a wide range of reasons, from going to and from school or work to overall mobility, but driving still is the most dangerous thing teenagers do, according to Brian Johnston, MD, MPH, professor of pediatrics at the University of Washington in Seattle.
Motor vehicle traffic accidents continue to be the leading cause of death of adolescents aged 15-19 years, according to 2017 data from the National Center for Health Statistics at the Centers for the Disease Control and Prevention.
“Inexperience drives the statistics we see,” Dr. Johnston said at the annual meeting of the American Academy of Pediatrics. “There is a steep learning curve among drivers of all ages, and crash rates are highest during the first few months after teens begin driving without supervision.”
Although the risk of accidents is higher than average for any new driver, it’s disproportionately higher for younger teens, compared with other ages: 16-year-old novice drivers have a higher accident risk than that of 17-year-olds, whose risk is similar to that of 18- and 19-year-old novices.
How long drivers have been licensed has a far bigger impact on crash risk, Dr. Johnston said (Traffic Inj. Prev. 2009 Jun;10[3]:209-19).
But the risk of an accident also increases with each additional passenger a teen driver has, particularly for younger and male drivers (Traffic Inj Prev. 2013;14[3]:283-92). More passengers likely means more distraction, and distraction, driving too fast for road conditions, and not scanning the roadway are the three most common errors – together accounting for about half of all teen drivers’ crashes.
Risk factors for accidents
Speed is a contributing factor in just over a third (36%) of teens’ fatal crashes. Adolescents drive faster and keep shorter following distances than adults do. But as with adults, wearing seat belts substantially reduces the risk of death in accidents.
Nationally, 90% of drivers use seat belts, with higher rates in states with primary enforcement (92%) than those in states with secondary enforcement (83%).
But barely more than half (54%) of U.S. high school students say they “always” wear a seat belt, and just under half of teens (47%) who died in crashes in 2017 weren’t wearing one. As seen in adults, teens are more likely to buckle up, by 12%, in states with primary seat belt laws.
Distraction during driving can be visual, manual, or cognitive – and handheld electronic devices such as smartphones cause all three distraction types. Cell phones nearly double the proportion of teen drivers who die in crashes, from 7% to 13%.
But if teens can keep their eyes on the roadway at all times, even the risks posed by cellphones drop considerably.
“The best evidence shows that secondary tasks only degrade driving performance when they require drivers to look away from the road,” Dr. Johnston said. Looking away for 2 seconds or longer increases crash risk more than fivefold.
Two other risk factors for teen car accidents are drowsiness and nighttime driving. Sleepiness can play a role in crashes at any time of day, and Dr. Johnston noted that some research has associated later high school start times with reduced crash risk.
Teens aged 16-19 years are about four times more likely to have a car accident at night than during the day per each mile driven, the pediatrician noted. Many licensing laws restrict teen driving starting at 11 p.m. or later, but about 50%-60% of their crashes occur between 9 and 11 p.m.
One reason for the increased risk is less experience driving in more difficult conditions, but teens also are more likely to have teen passengers, to be driving excessively fast, or to be under the influence of alcohol at night.
Adolescents’ crash risk is higher than that of adults for any level of blood alcohol content. Self-reported driving after drinking dropped by almost half – from 10% to 5.5% – from 2013 to 2017, but alcohol still is implicated in a substantial number of fatal teen crashes.
As drunk driving has declined, however, driving while under the influence of marijuana has been increasing. According to the National Highway Traffic Safety Administration, case control studies show drivers with tetrahydrocannabinol (THC) in their blood have a 25% increased risk of accidents – but the excess risk associated with THC vanishes when researchers control for age, sex, and concurrent use of alcohol. Not enough research exists to determine what the crash risk would be for adolescent drivers using THC alone.
A less-recognized risk factor for car accidents in teen drivers is ADHD, which increases a teen’s risk of crashing by 36%, particularly in the first month after getting a license, Dr. Johnston said.
ADHD medication appears to mitigate the danger, according to data: Crash risk was 40% lower in adult drivers with ADHD during months they filled their stimulant prescriptions. But one study found only 12% of teens with ADHD filled their prescriptions the month they got their license, and adolescents may not take their medications or still have them in their system on weekends or at night.
Teens recovering from concussion also may have an increased risk. Some evidence suggests driving impairment continues even when other symptoms have resolved, but not enough data exist to determine appropriate criteria for clearing teens to begin driving again.
Interventions to improve teens’ driving safety
Most teens take a basic driver education course before getting their licenses, but no evidence shows that it reduces risk of citations, crashes, or injury. In fact, “skid control training and other kinds of advanced skill training seem to increase crash risk, particularly among young males,” Dr. Johnston said.
What helps teens most is, ironically, more driving.
“If I say inexperience is the single most important risk factor for dying in a crash as a teen, driving experience is the intervention,” he said. More time spent driving – “with supervision in particular, and under diverse conditions,” Dr. Johnston said – increases the repertoire of skills and abilities.
Parents should be encouraged to ride along as their teens drive under diverse road conditions: different roads, different times of the day, and different weather conditions, for example. Parents can narrate their own driving, pointing out hazards and times when they slow down for increased caution, Dr. Johnston said. It might feel “awkward and unnatural,” but “some of the things you as a driver notice all the time are novel to teen drivers.”
Parents can influence road safety for teens in terms of their own behavior and in selecting a safer vehicle. A strong correlation exists between parental texting while driving when children are younger and what they do as teen drivers, for example.
Safer vehicles are bigger, heavier cars with electronic stability control, which reduces risk of death about as much as wearing seat belts. Parents should avoid vehicles with high horsepower and look for cars with the best safety ratings they can afford, Dr. Johnston said.
Several special features in newer cars can help reduce crash risk, such as blind spot detection, automatic breaking, collision avoidance systems, lane departure warning systems, and driver drowsiness detection. Parents may worry that relying on this technology could reduce teens’ learning, but it actually can compensate for skill deficits as they are becoming more skilled drivers.
Parents can look into feedback programs such as smartphone apps or other in-car units that allow parents to see data on teens’ speed, unsafe driving, “near-misses,” and similar driving behaviors. Research has shown that unsafe driving in newly licensed teens dropped by 66% over 4 months of using one of these feedback programs, compared with teens who didn’t use it.
Dr. Johnston also discussed the idea of prelicensure medical exams, similar to physicals that are required before playing sports. These already exist for commercial licenses in most states, but no data exist on whether it’s effective for teens. The goal would be to promote a discussion between parents and their teens about driving: reviewing medications the teen is taking and whether they affect driving; discussing safety of different vehicles; and assessing the teens’ risks, including any cognitive or other medical conditions that could affect driving safety. Even if such a “driving physical” is not currently required, pediatricians can do their own version of one with families.
Dr. Johnston had no disclosures.
NEW ORLEANS – Teens need to drive for a wide range of reasons, from going to and from school or work to overall mobility, but driving still is the most dangerous thing teenagers do, according to Brian Johnston, MD, MPH, professor of pediatrics at the University of Washington in Seattle.
Motor vehicle traffic accidents continue to be the leading cause of death of adolescents aged 15-19 years, according to 2017 data from the National Center for Health Statistics at the Centers for the Disease Control and Prevention.
“Inexperience drives the statistics we see,” Dr. Johnston said at the annual meeting of the American Academy of Pediatrics. “There is a steep learning curve among drivers of all ages, and crash rates are highest during the first few months after teens begin driving without supervision.”
Although the risk of accidents is higher than average for any new driver, it’s disproportionately higher for younger teens, compared with other ages: 16-year-old novice drivers have a higher accident risk than that of 17-year-olds, whose risk is similar to that of 18- and 19-year-old novices.
How long drivers have been licensed has a far bigger impact on crash risk, Dr. Johnston said (Traffic Inj. Prev. 2009 Jun;10[3]:209-19).
But the risk of an accident also increases with each additional passenger a teen driver has, particularly for younger and male drivers (Traffic Inj Prev. 2013;14[3]:283-92). More passengers likely means more distraction, and distraction, driving too fast for road conditions, and not scanning the roadway are the three most common errors – together accounting for about half of all teen drivers’ crashes.
Risk factors for accidents
Speed is a contributing factor in just over a third (36%) of teens’ fatal crashes. Adolescents drive faster and keep shorter following distances than adults do. But as with adults, wearing seat belts substantially reduces the risk of death in accidents.
Nationally, 90% of drivers use seat belts, with higher rates in states with primary enforcement (92%) than those in states with secondary enforcement (83%).
But barely more than half (54%) of U.S. high school students say they “always” wear a seat belt, and just under half of teens (47%) who died in crashes in 2017 weren’t wearing one. As seen in adults, teens are more likely to buckle up, by 12%, in states with primary seat belt laws.
Distraction during driving can be visual, manual, or cognitive – and handheld electronic devices such as smartphones cause all three distraction types. Cell phones nearly double the proportion of teen drivers who die in crashes, from 7% to 13%.
But if teens can keep their eyes on the roadway at all times, even the risks posed by cellphones drop considerably.
“The best evidence shows that secondary tasks only degrade driving performance when they require drivers to look away from the road,” Dr. Johnston said. Looking away for 2 seconds or longer increases crash risk more than fivefold.
Two other risk factors for teen car accidents are drowsiness and nighttime driving. Sleepiness can play a role in crashes at any time of day, and Dr. Johnston noted that some research has associated later high school start times with reduced crash risk.
Teens aged 16-19 years are about four times more likely to have a car accident at night than during the day per each mile driven, the pediatrician noted. Many licensing laws restrict teen driving starting at 11 p.m. or later, but about 50%-60% of their crashes occur between 9 and 11 p.m.
One reason for the increased risk is less experience driving in more difficult conditions, but teens also are more likely to have teen passengers, to be driving excessively fast, or to be under the influence of alcohol at night.
Adolescents’ crash risk is higher than that of adults for any level of blood alcohol content. Self-reported driving after drinking dropped by almost half – from 10% to 5.5% – from 2013 to 2017, but alcohol still is implicated in a substantial number of fatal teen crashes.
As drunk driving has declined, however, driving while under the influence of marijuana has been increasing. According to the National Highway Traffic Safety Administration, case control studies show drivers with tetrahydrocannabinol (THC) in their blood have a 25% increased risk of accidents – but the excess risk associated with THC vanishes when researchers control for age, sex, and concurrent use of alcohol. Not enough research exists to determine what the crash risk would be for adolescent drivers using THC alone.
A less-recognized risk factor for car accidents in teen drivers is ADHD, which increases a teen’s risk of crashing by 36%, particularly in the first month after getting a license, Dr. Johnston said.
ADHD medication appears to mitigate the danger, according to data: Crash risk was 40% lower in adult drivers with ADHD during months they filled their stimulant prescriptions. But one study found only 12% of teens with ADHD filled their prescriptions the month they got their license, and adolescents may not take their medications or still have them in their system on weekends or at night.
Teens recovering from concussion also may have an increased risk. Some evidence suggests driving impairment continues even when other symptoms have resolved, but not enough data exist to determine appropriate criteria for clearing teens to begin driving again.
Interventions to improve teens’ driving safety
Most teens take a basic driver education course before getting their licenses, but no evidence shows that it reduces risk of citations, crashes, or injury. In fact, “skid control training and other kinds of advanced skill training seem to increase crash risk, particularly among young males,” Dr. Johnston said.
What helps teens most is, ironically, more driving.
“If I say inexperience is the single most important risk factor for dying in a crash as a teen, driving experience is the intervention,” he said. More time spent driving – “with supervision in particular, and under diverse conditions,” Dr. Johnston said – increases the repertoire of skills and abilities.
Parents should be encouraged to ride along as their teens drive under diverse road conditions: different roads, different times of the day, and different weather conditions, for example. Parents can narrate their own driving, pointing out hazards and times when they slow down for increased caution, Dr. Johnston said. It might feel “awkward and unnatural,” but “some of the things you as a driver notice all the time are novel to teen drivers.”
Parents can influence road safety for teens in terms of their own behavior and in selecting a safer vehicle. A strong correlation exists between parental texting while driving when children are younger and what they do as teen drivers, for example.
Safer vehicles are bigger, heavier cars with electronic stability control, which reduces risk of death about as much as wearing seat belts. Parents should avoid vehicles with high horsepower and look for cars with the best safety ratings they can afford, Dr. Johnston said.
Several special features in newer cars can help reduce crash risk, such as blind spot detection, automatic breaking, collision avoidance systems, lane departure warning systems, and driver drowsiness detection. Parents may worry that relying on this technology could reduce teens’ learning, but it actually can compensate for skill deficits as they are becoming more skilled drivers.
Parents can look into feedback programs such as smartphone apps or other in-car units that allow parents to see data on teens’ speed, unsafe driving, “near-misses,” and similar driving behaviors. Research has shown that unsafe driving in newly licensed teens dropped by 66% over 4 months of using one of these feedback programs, compared with teens who didn’t use it.
Dr. Johnston also discussed the idea of prelicensure medical exams, similar to physicals that are required before playing sports. These already exist for commercial licenses in most states, but no data exist on whether it’s effective for teens. The goal would be to promote a discussion between parents and their teens about driving: reviewing medications the teen is taking and whether they affect driving; discussing safety of different vehicles; and assessing the teens’ risks, including any cognitive or other medical conditions that could affect driving safety. Even if such a “driving physical” is not currently required, pediatricians can do their own version of one with families.
Dr. Johnston had no disclosures.
Newborns’ maternal protection against measles wanes within 6 months
according to new research.
In fact, most of the 196 infants’ maternal measles antibodies had dropped below the protective threshold by 3 months of age – well before the recommended age of 12-15 months for the first dose of MMR vaccine.
The odds of inadequate protection doubled for each additional month of age, Michelle Science, MD, of the University of Toronto and associates reported in Pediatrics.
“The widening gap between loss of maternal antibodies and measles vaccination described in our study leaves infants vulnerable to measles for much of their infancy and highlights the need for further research to support public health policy,” Dr. Science and colleagues wrote.
The findings are not surprising for a setting in which measles has been eliminated and align with results from past research, Huong Q. McLean, PhD, MPH, of the Marshfield (Wis.) Clinic Research Institute and Walter A. Orenstein, MD, of Emory University in Atlanta wrote in an accompanying editorial (Pediatrics. 2019 Nov 21. doi: 10.1542/peds.2019-2541).
However, this susceptibility prior to receiving the MMR has taken on a new significance more recently, Dr. McLean and Dr. Orenstein suggested.
“In light of increasing measles outbreaks during the past year reaching levels not recorded in the United States since 1992 and increased measles elsewhere, coupled with the risk of severe illness in infants, there is increased concern regarding the protection of infants against measles,” the editorialists wrote.
Dr. Science and colleagues tested serum samples from 196 term infants, all under 12 months old, for antibodies against measles. The sera had been previously collected at a single tertiary care center in Ontario for clinical testing and then stored. Measles has been eliminated in Canada since 1998.
The researchers randomly selected 25 samples for each of eight different age groups: up to 30 days old; 1 month (31-60 days); 2 months (61-89 days); 3 months (90-119 days); 4 months; 5 months; 6-9 months; and 9-11 months.
Just over half the babies (56%) were male, and 35% had an underlying condition, but none had conditions that might affect antibody levels. The conditions were primarily a developmental delay or otherwise affecting the central nervous system, liver, or gastrointestinal function. Mean maternal age was 32 years.
To ensure high test sensitivity, the researchers used the plaque-reduction neutralization test (PRNT) to test for measles-neutralizing antibodies instead of using enzyme-linked immunosorbent assay (ELISA) because “ELISA sensitivity decreases as antibody titers decrease,” Dr. Science and colleagues wrote. They used a neutralization titer of less than 192 mIU/mL as the threshold for protection against measles.
When the researchers calculated the predicted standardized mean antibody titer for infants with a mother aged 32 years, they determined their mean to be 541 mIU/mL at 1 month, 142 mIU/mL at 3 months (below the measles threshold of susceptibility of 192 mIU/mL) , and 64 mIU/mL at 6 months. None of the infants had measles antibodies above the protective threshold at 6 months old, the authors noted.
Children’s odds of susceptibility to measles doubled for each additional month of age, after adjustment for infant sex and maternal age (odds ratio, 2.13). Children’s likelihood of susceptibility to measles modestly increased as maternal age increased in 5-year increments from 25 to 40 years.
Children with an underlying conditions had greater susceptibility to measles (83%), compared with those without a comorbidity (68%, P = .03). No difference in susceptibility existed between males and females or based on gestational age at birth (ranging from 37 to 41 weeks).
The Advisory Committee on Immunization Practices permits measles vaccination “as early as 6 months for infants who plan to travel internationally, infants with ongoing risk for exposure during measles outbreaks and as postexposure prophylaxis,” Dr. McLean and Dr. Orenstein noted in their editorial.
They discussed the rationale for various changes in the recommended schedule for measles immunization, based on changes in epidemiology of the disease and improved understanding of the immune response to vaccination since the vaccine became available in 1963. Then they posed the question of whether the recommendation should be revised again.
“Ideally, the schedule should minimize the risk of measles and its complications and optimize vaccine-induced protection,” Dr. McLean and Dr. Orenstein wrote.
They argued that the evidence cannot currently support changing the first MMR dose to a younger age because measles incidence in the United States remains extremely low outside of the extraordinary outbreaks in 2014 and 2019. Further, infants under 12 months of age make up less than 15% of measles cases during outbreaks, and unvaccinated people make up more than 70% of cases.
Rather, they stated, this new study emphasizes the importance of following the current schedule, with consideration of an earlier schedule only warranted during outbreaks.
“Health care providers must work to maintain high levels of coverage with 2 doses of MMR among vaccine-eligible populations and minimize pockets of susceptibility to prevent transmission to infants and prevent reestablishment of endemic transmission,” they concluded.
The research was funded by the Public Health Ontario Project Initiation Fund. The authors had no relevant financial disclosures. The editorialists had no external funding and no relevant financial disclosures.
SOURCE: Science M et al. Pediatrics. 2019 Nov 21. doi: 10.1542/peds.2019-0630.
according to new research.
In fact, most of the 196 infants’ maternal measles antibodies had dropped below the protective threshold by 3 months of age – well before the recommended age of 12-15 months for the first dose of MMR vaccine.
The odds of inadequate protection doubled for each additional month of age, Michelle Science, MD, of the University of Toronto and associates reported in Pediatrics.
“The widening gap between loss of maternal antibodies and measles vaccination described in our study leaves infants vulnerable to measles for much of their infancy and highlights the need for further research to support public health policy,” Dr. Science and colleagues wrote.
The findings are not surprising for a setting in which measles has been eliminated and align with results from past research, Huong Q. McLean, PhD, MPH, of the Marshfield (Wis.) Clinic Research Institute and Walter A. Orenstein, MD, of Emory University in Atlanta wrote in an accompanying editorial (Pediatrics. 2019 Nov 21. doi: 10.1542/peds.2019-2541).
However, this susceptibility prior to receiving the MMR has taken on a new significance more recently, Dr. McLean and Dr. Orenstein suggested.
“In light of increasing measles outbreaks during the past year reaching levels not recorded in the United States since 1992 and increased measles elsewhere, coupled with the risk of severe illness in infants, there is increased concern regarding the protection of infants against measles,” the editorialists wrote.
Dr. Science and colleagues tested serum samples from 196 term infants, all under 12 months old, for antibodies against measles. The sera had been previously collected at a single tertiary care center in Ontario for clinical testing and then stored. Measles has been eliminated in Canada since 1998.
The researchers randomly selected 25 samples for each of eight different age groups: up to 30 days old; 1 month (31-60 days); 2 months (61-89 days); 3 months (90-119 days); 4 months; 5 months; 6-9 months; and 9-11 months.
Just over half the babies (56%) were male, and 35% had an underlying condition, but none had conditions that might affect antibody levels. The conditions were primarily a developmental delay or otherwise affecting the central nervous system, liver, or gastrointestinal function. Mean maternal age was 32 years.
To ensure high test sensitivity, the researchers used the plaque-reduction neutralization test (PRNT) to test for measles-neutralizing antibodies instead of using enzyme-linked immunosorbent assay (ELISA) because “ELISA sensitivity decreases as antibody titers decrease,” Dr. Science and colleagues wrote. They used a neutralization titer of less than 192 mIU/mL as the threshold for protection against measles.
When the researchers calculated the predicted standardized mean antibody titer for infants with a mother aged 32 years, they determined their mean to be 541 mIU/mL at 1 month, 142 mIU/mL at 3 months (below the measles threshold of susceptibility of 192 mIU/mL) , and 64 mIU/mL at 6 months. None of the infants had measles antibodies above the protective threshold at 6 months old, the authors noted.
Children’s odds of susceptibility to measles doubled for each additional month of age, after adjustment for infant sex and maternal age (odds ratio, 2.13). Children’s likelihood of susceptibility to measles modestly increased as maternal age increased in 5-year increments from 25 to 40 years.
Children with an underlying conditions had greater susceptibility to measles (83%), compared with those without a comorbidity (68%, P = .03). No difference in susceptibility existed between males and females or based on gestational age at birth (ranging from 37 to 41 weeks).
The Advisory Committee on Immunization Practices permits measles vaccination “as early as 6 months for infants who plan to travel internationally, infants with ongoing risk for exposure during measles outbreaks and as postexposure prophylaxis,” Dr. McLean and Dr. Orenstein noted in their editorial.
They discussed the rationale for various changes in the recommended schedule for measles immunization, based on changes in epidemiology of the disease and improved understanding of the immune response to vaccination since the vaccine became available in 1963. Then they posed the question of whether the recommendation should be revised again.
“Ideally, the schedule should minimize the risk of measles and its complications and optimize vaccine-induced protection,” Dr. McLean and Dr. Orenstein wrote.
They argued that the evidence cannot currently support changing the first MMR dose to a younger age because measles incidence in the United States remains extremely low outside of the extraordinary outbreaks in 2014 and 2019. Further, infants under 12 months of age make up less than 15% of measles cases during outbreaks, and unvaccinated people make up more than 70% of cases.
Rather, they stated, this new study emphasizes the importance of following the current schedule, with consideration of an earlier schedule only warranted during outbreaks.
“Health care providers must work to maintain high levels of coverage with 2 doses of MMR among vaccine-eligible populations and minimize pockets of susceptibility to prevent transmission to infants and prevent reestablishment of endemic transmission,” they concluded.
The research was funded by the Public Health Ontario Project Initiation Fund. The authors had no relevant financial disclosures. The editorialists had no external funding and no relevant financial disclosures.
SOURCE: Science M et al. Pediatrics. 2019 Nov 21. doi: 10.1542/peds.2019-0630.
according to new research.
In fact, most of the 196 infants’ maternal measles antibodies had dropped below the protective threshold by 3 months of age – well before the recommended age of 12-15 months for the first dose of MMR vaccine.
The odds of inadequate protection doubled for each additional month of age, Michelle Science, MD, of the University of Toronto and associates reported in Pediatrics.
“The widening gap between loss of maternal antibodies and measles vaccination described in our study leaves infants vulnerable to measles for much of their infancy and highlights the need for further research to support public health policy,” Dr. Science and colleagues wrote.
The findings are not surprising for a setting in which measles has been eliminated and align with results from past research, Huong Q. McLean, PhD, MPH, of the Marshfield (Wis.) Clinic Research Institute and Walter A. Orenstein, MD, of Emory University in Atlanta wrote in an accompanying editorial (Pediatrics. 2019 Nov 21. doi: 10.1542/peds.2019-2541).
However, this susceptibility prior to receiving the MMR has taken on a new significance more recently, Dr. McLean and Dr. Orenstein suggested.
“In light of increasing measles outbreaks during the past year reaching levels not recorded in the United States since 1992 and increased measles elsewhere, coupled with the risk of severe illness in infants, there is increased concern regarding the protection of infants against measles,” the editorialists wrote.
Dr. Science and colleagues tested serum samples from 196 term infants, all under 12 months old, for antibodies against measles. The sera had been previously collected at a single tertiary care center in Ontario for clinical testing and then stored. Measles has been eliminated in Canada since 1998.
The researchers randomly selected 25 samples for each of eight different age groups: up to 30 days old; 1 month (31-60 days); 2 months (61-89 days); 3 months (90-119 days); 4 months; 5 months; 6-9 months; and 9-11 months.
Just over half the babies (56%) were male, and 35% had an underlying condition, but none had conditions that might affect antibody levels. The conditions were primarily a developmental delay or otherwise affecting the central nervous system, liver, or gastrointestinal function. Mean maternal age was 32 years.
To ensure high test sensitivity, the researchers used the plaque-reduction neutralization test (PRNT) to test for measles-neutralizing antibodies instead of using enzyme-linked immunosorbent assay (ELISA) because “ELISA sensitivity decreases as antibody titers decrease,” Dr. Science and colleagues wrote. They used a neutralization titer of less than 192 mIU/mL as the threshold for protection against measles.
When the researchers calculated the predicted standardized mean antibody titer for infants with a mother aged 32 years, they determined their mean to be 541 mIU/mL at 1 month, 142 mIU/mL at 3 months (below the measles threshold of susceptibility of 192 mIU/mL) , and 64 mIU/mL at 6 months. None of the infants had measles antibodies above the protective threshold at 6 months old, the authors noted.
Children’s odds of susceptibility to measles doubled for each additional month of age, after adjustment for infant sex and maternal age (odds ratio, 2.13). Children’s likelihood of susceptibility to measles modestly increased as maternal age increased in 5-year increments from 25 to 40 years.
Children with an underlying conditions had greater susceptibility to measles (83%), compared with those without a comorbidity (68%, P = .03). No difference in susceptibility existed between males and females or based on gestational age at birth (ranging from 37 to 41 weeks).
The Advisory Committee on Immunization Practices permits measles vaccination “as early as 6 months for infants who plan to travel internationally, infants with ongoing risk for exposure during measles outbreaks and as postexposure prophylaxis,” Dr. McLean and Dr. Orenstein noted in their editorial.
They discussed the rationale for various changes in the recommended schedule for measles immunization, based on changes in epidemiology of the disease and improved understanding of the immune response to vaccination since the vaccine became available in 1963. Then they posed the question of whether the recommendation should be revised again.
“Ideally, the schedule should minimize the risk of measles and its complications and optimize vaccine-induced protection,” Dr. McLean and Dr. Orenstein wrote.
They argued that the evidence cannot currently support changing the first MMR dose to a younger age because measles incidence in the United States remains extremely low outside of the extraordinary outbreaks in 2014 and 2019. Further, infants under 12 months of age make up less than 15% of measles cases during outbreaks, and unvaccinated people make up more than 70% of cases.
Rather, they stated, this new study emphasizes the importance of following the current schedule, with consideration of an earlier schedule only warranted during outbreaks.
“Health care providers must work to maintain high levels of coverage with 2 doses of MMR among vaccine-eligible populations and minimize pockets of susceptibility to prevent transmission to infants and prevent reestablishment of endemic transmission,” they concluded.
The research was funded by the Public Health Ontario Project Initiation Fund. The authors had no relevant financial disclosures. The editorialists had no external funding and no relevant financial disclosures.
SOURCE: Science M et al. Pediatrics. 2019 Nov 21. doi: 10.1542/peds.2019-0630.
FROM PEDIATRICS
Key clinical point: Infants’ maternal measles antibodies fell below protective levels by 6 months old.
Major finding: Infants were twice as likely not to have protective immunity against measles for each month of age after birth (odds ratio, 2.13).
Study details: The findings are based on measles antibody testing of 196 serum samples from infants born in a tertiary care center in Ontario.
Disclosures: The research was funded by the Public Health Ontario Project Initiation Fund. The authors had no relevant financial disclosures.
Source: Science M et al. Pediatrics. 2019 Nov 21. doi: 10.1542/peds.2019-0630.
POTS heterogeneity requires individualized treatment
AUSTIN, TEX. – Postural orthostatic tachycardia syndrome (POTS) is not a single disorder, but rather includes multiple overlapping subtypes, according to Steven Vernino, MD, PhD, a professor of neurology at the University of Texas, Dallas.
“It’s pretty well established that there’s a heterogeneous spectrum of disorders that can present this way,” Dr. Vernino told attendees at the annual meeting of the American Association for Neuromuscular and Electrodiagnostic Medicine. “Investigation is somewhat difficult because we have limited tools.”
In his overview of POTS, Dr. Vernino defined it as a chronic condition with an “inappropriate orthostatic increase in heart rate” and symptoms that persist for at least 6 months. The heart rate increase should be at least 30 beats per minute – or 40 bpm in those aged 12-19 years – within 5-10 minutes of quiet standing or an upright tilt, but the patient lacks orthostatic hypotension. Often, however, other symptoms continue even if the tachycardia is not always present.
These symptoms range widely, including fainting, shortness of breath, headaches, fatigue, fibromyalgia, dizziness, brain fog, chest tightens, sensitivity to light or sound, tingling, heat intolerance, and gastrointestinal problems. Pain is particularly common.
Though peak incidence occurs around age 14 years, the average age of patients with POTS is 30 years. Women comprise 86% of those with POTS and 93% of patients are white, though this last figure may result from multiple reporting biases. A quarter of patients are disabled to a degree similar to heart failure or chronic obstructive pulmonary disease, he said.
Prevalence estimates are all over the map, ranging in academic literature from “up to 1% of teens” to “millions of Americans,” Dr. Vernino said. A commonly accepted range puts the estimate at 500,000 to 3 million Americans, the number used by Dysautonomia International.
Key to treatment of POTS is assessing possible underlying causes and individualizing treatment based on likely contributing etiologies, such as hypovolemia, deconditioning, and autoimmunity, Dr. Vernino said.
Classifications and etiologies of POTS
With its various possible etiologies, “it’s our job as physicians to try to understand, if you can, what the underlying the etiology is and try to address that,” Dr. Vernino said. About 11% of patients have a family history of POTS, and some research has suggested genes that may be involved, including the one that encodes the norepinephrine transporter and alpha tryptase.
Patients with neuropathic POTS have a mild or partial peripheral autonomic neuropathy “that causes a problem with the vasomotor function so that when patients stand, they don’t have an adequate increase in vascular tone, blood pools in the feet and they develop relative hypovolemia, and the autonomic nervous system compensates with tachycardia,” he said. The Quantitative Sudomotor Axon Reflex Test may show distal sweating, and a skin biopsy can be done to assess intraepidermal nerve fiber density.
Hyperadrenergic POTS involves “the presence of a dramatic, excessive rise of norepinephrine” and can involve tremor, nausea, sweating, and headache when patients are upright, Dr. Vernino said.
“These are patients who appear, clinically and in laboratory testing, to have inappropriate sympathetic response to standing up,” he said, and they may have orthostatic hypertension along with an increased heart rate.
Other subtypes of POTS can overlap neuropathic and hyperadrenergic types, which can also overlap one another. About 30% of patients appear hypovolemic, with a 13%-17% volume deficit, even with copious intake of water and sodium, he said. Despite this deficit, renin levels are typically normal in these patients, and aldosterone levels may be paradoxically low. Reduced red blood cell mass may be present, too (Circulation. 2005 Apr 5;111[13]:1574-82).
“What causes that and how that’s related to the other features is a bit unclear, and then, either as a primary or as a secondary component of POTS, there can be cardiac deconditioning,” Dr. Vernino said, requiring quantitative ECG. “It’s unclear whether that deconditioning happens as a consequence of disability from POTS or as a primary part of it.”
Questions still exist regarding whether autoimmunity is one of the underpinnings of POTS, Dr. Vernino said. It’s associated with elevated inflammatory biomarker levels and systemic autoimmune disorders such as Sjögren’s syndrome, as well as with antiphospholipid antibodies.
“More recently there’s been evidence on specific autoantibodies that have been found in POTS patients, and we’re still working through what all that means,” he said. “The real question is whether these antibodies are the cause of POTS” versus an effect or an epiphenomenon.
These antibodies include some G protein–coupled receptor antibodies, such as adrenergic receptor autoantibodies, angiotensin II type 1 receptor antibodies, and muscarinic acetylcholine receptor M3 antibodies. Others include thyroid autoantibodies, ganglionic acetylcholine receptor antibodies, and IgG antibodies, as well as several dozen cardiac membrane proteins.
Comorbidities and risk factors
Although 41% of patients with POTS report some health event preceding onset of symptoms, it’s unclear which, if any, of these events may be related to the condition. The most common antecedent event is infection, reported by 41% of patients in the “Big POTS Survey” conducted by Dysautonomia International, Dr. Vernino said. Other antecedent events reported included surgery (12%), pregnancy (9%), an accident (6%), vaccination (6%), puberty (5%), concussion (4%), and emotional trauma (3%). Research has found associations with migraine, concussion, and infection.
Comorbidities are also common, reported by 84% of patients in the same survey. Migraine, vitamin D deficiency, and joint hypermobility (Ehlers-Danlos syndrome type 3) top the list of comorbidities, and various autoimmune conditions, particularly Sjögren’s syndrome, may co-occur with POTS. Other comorbidities include small fiber neuropathy, mast-cell activation syndrome, chronic fatigue, gastrointestinal problems, vasovagal syncope, and sleeping difficulties.
Joint hypermobility appears to be a “pretty strong risk factor for development” of POTS, Dr. Vernino said, and patients may even be involved in activities where that’s helpful, such as gymnastics. “You can make this diagnosis clinically – there isn’t a genetic test for joint hypermobility syndrome – and you usually don’t have the other features of Marfan syndrome,” he told attendees.
Other risk factors include low body mass, mitral valve prolapse, migraine, anxiety, irritable bowel syndrome, prolonged bed rest after an illness, and mast-cell activation syndrome.
Prognosis and treatment
POTS is very common but often still unrecognized, Dr. Vernino said, “because the symptoms are somewhat diverse and broad and vague.” Even providers who recognize POTS can become preoccupied with “the heart rate increase being the whole picture, but there are many other symptoms, and that leads to a significant impact on the quality of life of these patients.”
The course of POTS varies across patients. In about half of patients, symptoms persist but the severity improves, and one in five patients fully resolve. Severity only tends to worsen over time in about 3.5% of patients, and severity remains constant in 8.7% (J Pediatr. 2016 Jun;173:149-53. doi: 10.1016/j.jpeds.2016.02.035).
“It would probably be simpler if POTS was a single entity that had a single etiology that we could target,” Dr. Vernino said. But its heterogeneity means “we have to investigate patients individually and understand their particular situation, individualize their treatment, whether it be nonpharmacological or pharmacological, to their particular potential etiologies.”
Dr. Vernino has received research support from Genentech, Grifols, Athena/Quest, Biohaven Pharmaceutical, Dysautonomia International, and the Rex Griswold Foundation.
AUSTIN, TEX. – Postural orthostatic tachycardia syndrome (POTS) is not a single disorder, but rather includes multiple overlapping subtypes, according to Steven Vernino, MD, PhD, a professor of neurology at the University of Texas, Dallas.
“It’s pretty well established that there’s a heterogeneous spectrum of disorders that can present this way,” Dr. Vernino told attendees at the annual meeting of the American Association for Neuromuscular and Electrodiagnostic Medicine. “Investigation is somewhat difficult because we have limited tools.”
In his overview of POTS, Dr. Vernino defined it as a chronic condition with an “inappropriate orthostatic increase in heart rate” and symptoms that persist for at least 6 months. The heart rate increase should be at least 30 beats per minute – or 40 bpm in those aged 12-19 years – within 5-10 minutes of quiet standing or an upright tilt, but the patient lacks orthostatic hypotension. Often, however, other symptoms continue even if the tachycardia is not always present.
These symptoms range widely, including fainting, shortness of breath, headaches, fatigue, fibromyalgia, dizziness, brain fog, chest tightens, sensitivity to light or sound, tingling, heat intolerance, and gastrointestinal problems. Pain is particularly common.
Though peak incidence occurs around age 14 years, the average age of patients with POTS is 30 years. Women comprise 86% of those with POTS and 93% of patients are white, though this last figure may result from multiple reporting biases. A quarter of patients are disabled to a degree similar to heart failure or chronic obstructive pulmonary disease, he said.
Prevalence estimates are all over the map, ranging in academic literature from “up to 1% of teens” to “millions of Americans,” Dr. Vernino said. A commonly accepted range puts the estimate at 500,000 to 3 million Americans, the number used by Dysautonomia International.
Key to treatment of POTS is assessing possible underlying causes and individualizing treatment based on likely contributing etiologies, such as hypovolemia, deconditioning, and autoimmunity, Dr. Vernino said.
Classifications and etiologies of POTS
With its various possible etiologies, “it’s our job as physicians to try to understand, if you can, what the underlying the etiology is and try to address that,” Dr. Vernino said. About 11% of patients have a family history of POTS, and some research has suggested genes that may be involved, including the one that encodes the norepinephrine transporter and alpha tryptase.
Patients with neuropathic POTS have a mild or partial peripheral autonomic neuropathy “that causes a problem with the vasomotor function so that when patients stand, they don’t have an adequate increase in vascular tone, blood pools in the feet and they develop relative hypovolemia, and the autonomic nervous system compensates with tachycardia,” he said. The Quantitative Sudomotor Axon Reflex Test may show distal sweating, and a skin biopsy can be done to assess intraepidermal nerve fiber density.
Hyperadrenergic POTS involves “the presence of a dramatic, excessive rise of norepinephrine” and can involve tremor, nausea, sweating, and headache when patients are upright, Dr. Vernino said.
“These are patients who appear, clinically and in laboratory testing, to have inappropriate sympathetic response to standing up,” he said, and they may have orthostatic hypertension along with an increased heart rate.
Other subtypes of POTS can overlap neuropathic and hyperadrenergic types, which can also overlap one another. About 30% of patients appear hypovolemic, with a 13%-17% volume deficit, even with copious intake of water and sodium, he said. Despite this deficit, renin levels are typically normal in these patients, and aldosterone levels may be paradoxically low. Reduced red blood cell mass may be present, too (Circulation. 2005 Apr 5;111[13]:1574-82).
“What causes that and how that’s related to the other features is a bit unclear, and then, either as a primary or as a secondary component of POTS, there can be cardiac deconditioning,” Dr. Vernino said, requiring quantitative ECG. “It’s unclear whether that deconditioning happens as a consequence of disability from POTS or as a primary part of it.”
Questions still exist regarding whether autoimmunity is one of the underpinnings of POTS, Dr. Vernino said. It’s associated with elevated inflammatory biomarker levels and systemic autoimmune disorders such as Sjögren’s syndrome, as well as with antiphospholipid antibodies.
“More recently there’s been evidence on specific autoantibodies that have been found in POTS patients, and we’re still working through what all that means,” he said. “The real question is whether these antibodies are the cause of POTS” versus an effect or an epiphenomenon.
These antibodies include some G protein–coupled receptor antibodies, such as adrenergic receptor autoantibodies, angiotensin II type 1 receptor antibodies, and muscarinic acetylcholine receptor M3 antibodies. Others include thyroid autoantibodies, ganglionic acetylcholine receptor antibodies, and IgG antibodies, as well as several dozen cardiac membrane proteins.
Comorbidities and risk factors
Although 41% of patients with POTS report some health event preceding onset of symptoms, it’s unclear which, if any, of these events may be related to the condition. The most common antecedent event is infection, reported by 41% of patients in the “Big POTS Survey” conducted by Dysautonomia International, Dr. Vernino said. Other antecedent events reported included surgery (12%), pregnancy (9%), an accident (6%), vaccination (6%), puberty (5%), concussion (4%), and emotional trauma (3%). Research has found associations with migraine, concussion, and infection.
Comorbidities are also common, reported by 84% of patients in the same survey. Migraine, vitamin D deficiency, and joint hypermobility (Ehlers-Danlos syndrome type 3) top the list of comorbidities, and various autoimmune conditions, particularly Sjögren’s syndrome, may co-occur with POTS. Other comorbidities include small fiber neuropathy, mast-cell activation syndrome, chronic fatigue, gastrointestinal problems, vasovagal syncope, and sleeping difficulties.
Joint hypermobility appears to be a “pretty strong risk factor for development” of POTS, Dr. Vernino said, and patients may even be involved in activities where that’s helpful, such as gymnastics. “You can make this diagnosis clinically – there isn’t a genetic test for joint hypermobility syndrome – and you usually don’t have the other features of Marfan syndrome,” he told attendees.
Other risk factors include low body mass, mitral valve prolapse, migraine, anxiety, irritable bowel syndrome, prolonged bed rest after an illness, and mast-cell activation syndrome.
Prognosis and treatment
POTS is very common but often still unrecognized, Dr. Vernino said, “because the symptoms are somewhat diverse and broad and vague.” Even providers who recognize POTS can become preoccupied with “the heart rate increase being the whole picture, but there are many other symptoms, and that leads to a significant impact on the quality of life of these patients.”
The course of POTS varies across patients. In about half of patients, symptoms persist but the severity improves, and one in five patients fully resolve. Severity only tends to worsen over time in about 3.5% of patients, and severity remains constant in 8.7% (J Pediatr. 2016 Jun;173:149-53. doi: 10.1016/j.jpeds.2016.02.035).
“It would probably be simpler if POTS was a single entity that had a single etiology that we could target,” Dr. Vernino said. But its heterogeneity means “we have to investigate patients individually and understand their particular situation, individualize their treatment, whether it be nonpharmacological or pharmacological, to their particular potential etiologies.”
Dr. Vernino has received research support from Genentech, Grifols, Athena/Quest, Biohaven Pharmaceutical, Dysautonomia International, and the Rex Griswold Foundation.
AUSTIN, TEX. – Postural orthostatic tachycardia syndrome (POTS) is not a single disorder, but rather includes multiple overlapping subtypes, according to Steven Vernino, MD, PhD, a professor of neurology at the University of Texas, Dallas.
“It’s pretty well established that there’s a heterogeneous spectrum of disorders that can present this way,” Dr. Vernino told attendees at the annual meeting of the American Association for Neuromuscular and Electrodiagnostic Medicine. “Investigation is somewhat difficult because we have limited tools.”
In his overview of POTS, Dr. Vernino defined it as a chronic condition with an “inappropriate orthostatic increase in heart rate” and symptoms that persist for at least 6 months. The heart rate increase should be at least 30 beats per minute – or 40 bpm in those aged 12-19 years – within 5-10 minutes of quiet standing or an upright tilt, but the patient lacks orthostatic hypotension. Often, however, other symptoms continue even if the tachycardia is not always present.
These symptoms range widely, including fainting, shortness of breath, headaches, fatigue, fibromyalgia, dizziness, brain fog, chest tightens, sensitivity to light or sound, tingling, heat intolerance, and gastrointestinal problems. Pain is particularly common.
Though peak incidence occurs around age 14 years, the average age of patients with POTS is 30 years. Women comprise 86% of those with POTS and 93% of patients are white, though this last figure may result from multiple reporting biases. A quarter of patients are disabled to a degree similar to heart failure or chronic obstructive pulmonary disease, he said.
Prevalence estimates are all over the map, ranging in academic literature from “up to 1% of teens” to “millions of Americans,” Dr. Vernino said. A commonly accepted range puts the estimate at 500,000 to 3 million Americans, the number used by Dysautonomia International.
Key to treatment of POTS is assessing possible underlying causes and individualizing treatment based on likely contributing etiologies, such as hypovolemia, deconditioning, and autoimmunity, Dr. Vernino said.
Classifications and etiologies of POTS
With its various possible etiologies, “it’s our job as physicians to try to understand, if you can, what the underlying the etiology is and try to address that,” Dr. Vernino said. About 11% of patients have a family history of POTS, and some research has suggested genes that may be involved, including the one that encodes the norepinephrine transporter and alpha tryptase.
Patients with neuropathic POTS have a mild or partial peripheral autonomic neuropathy “that causes a problem with the vasomotor function so that when patients stand, they don’t have an adequate increase in vascular tone, blood pools in the feet and they develop relative hypovolemia, and the autonomic nervous system compensates with tachycardia,” he said. The Quantitative Sudomotor Axon Reflex Test may show distal sweating, and a skin biopsy can be done to assess intraepidermal nerve fiber density.
Hyperadrenergic POTS involves “the presence of a dramatic, excessive rise of norepinephrine” and can involve tremor, nausea, sweating, and headache when patients are upright, Dr. Vernino said.
“These are patients who appear, clinically and in laboratory testing, to have inappropriate sympathetic response to standing up,” he said, and they may have orthostatic hypertension along with an increased heart rate.
Other subtypes of POTS can overlap neuropathic and hyperadrenergic types, which can also overlap one another. About 30% of patients appear hypovolemic, with a 13%-17% volume deficit, even with copious intake of water and sodium, he said. Despite this deficit, renin levels are typically normal in these patients, and aldosterone levels may be paradoxically low. Reduced red blood cell mass may be present, too (Circulation. 2005 Apr 5;111[13]:1574-82).
“What causes that and how that’s related to the other features is a bit unclear, and then, either as a primary or as a secondary component of POTS, there can be cardiac deconditioning,” Dr. Vernino said, requiring quantitative ECG. “It’s unclear whether that deconditioning happens as a consequence of disability from POTS or as a primary part of it.”
Questions still exist regarding whether autoimmunity is one of the underpinnings of POTS, Dr. Vernino said. It’s associated with elevated inflammatory biomarker levels and systemic autoimmune disorders such as Sjögren’s syndrome, as well as with antiphospholipid antibodies.
“More recently there’s been evidence on specific autoantibodies that have been found in POTS patients, and we’re still working through what all that means,” he said. “The real question is whether these antibodies are the cause of POTS” versus an effect or an epiphenomenon.
These antibodies include some G protein–coupled receptor antibodies, such as adrenergic receptor autoantibodies, angiotensin II type 1 receptor antibodies, and muscarinic acetylcholine receptor M3 antibodies. Others include thyroid autoantibodies, ganglionic acetylcholine receptor antibodies, and IgG antibodies, as well as several dozen cardiac membrane proteins.
Comorbidities and risk factors
Although 41% of patients with POTS report some health event preceding onset of symptoms, it’s unclear which, if any, of these events may be related to the condition. The most common antecedent event is infection, reported by 41% of patients in the “Big POTS Survey” conducted by Dysautonomia International, Dr. Vernino said. Other antecedent events reported included surgery (12%), pregnancy (9%), an accident (6%), vaccination (6%), puberty (5%), concussion (4%), and emotional trauma (3%). Research has found associations with migraine, concussion, and infection.
Comorbidities are also common, reported by 84% of patients in the same survey. Migraine, vitamin D deficiency, and joint hypermobility (Ehlers-Danlos syndrome type 3) top the list of comorbidities, and various autoimmune conditions, particularly Sjögren’s syndrome, may co-occur with POTS. Other comorbidities include small fiber neuropathy, mast-cell activation syndrome, chronic fatigue, gastrointestinal problems, vasovagal syncope, and sleeping difficulties.
Joint hypermobility appears to be a “pretty strong risk factor for development” of POTS, Dr. Vernino said, and patients may even be involved in activities where that’s helpful, such as gymnastics. “You can make this diagnosis clinically – there isn’t a genetic test for joint hypermobility syndrome – and you usually don’t have the other features of Marfan syndrome,” he told attendees.
Other risk factors include low body mass, mitral valve prolapse, migraine, anxiety, irritable bowel syndrome, prolonged bed rest after an illness, and mast-cell activation syndrome.
Prognosis and treatment
POTS is very common but often still unrecognized, Dr. Vernino said, “because the symptoms are somewhat diverse and broad and vague.” Even providers who recognize POTS can become preoccupied with “the heart rate increase being the whole picture, but there are many other symptoms, and that leads to a significant impact on the quality of life of these patients.”
The course of POTS varies across patients. In about half of patients, symptoms persist but the severity improves, and one in five patients fully resolve. Severity only tends to worsen over time in about 3.5% of patients, and severity remains constant in 8.7% (J Pediatr. 2016 Jun;173:149-53. doi: 10.1016/j.jpeds.2016.02.035).
“It would probably be simpler if POTS was a single entity that had a single etiology that we could target,” Dr. Vernino said. But its heterogeneity means “we have to investigate patients individually and understand their particular situation, individualize their treatment, whether it be nonpharmacological or pharmacological, to their particular potential etiologies.”
Dr. Vernino has received research support from Genentech, Grifols, Athena/Quest, Biohaven Pharmaceutical, Dysautonomia International, and the Rex Griswold Foundation.
EXPERT ANALYSIS FROM AANEM 2019
Suicide screening crucial in pediatric medical settings
and screening can take as little as 20 seconds, according to Lisa Horowitz, PhD, MPH, a staff scientist and clinical psychologist at the National Institute of Mental Health, Bethesda, Md.
But clinicians need to use validated screening instruments that are both population specific and site specific, and they need practice guidelines to treat patients screening positive.
Currently, many practitioners use depression screens – such as question #9 on suicide ideation and self harm on the Patient Health Questionnaire for Adolescents (PHQ-A) – to identify suicide risk, but preliminary data suggest these screens often are inadequate, Dr. Horowitz said. Just one question, especially one without precise language, does not appear to identify as many at-risk youths as more direct questions about suicidal thoughts and behaviors.
A Pathways to Clinical Care suicide risk screening work group therefore designed a three-tiered clinical pathway for suicide risk screenings in emergency departments, inpatient care, and outpatient primary care. It begins with the Ask Suicide-Screening Questions (ASQ), which takes about 20 seconds and was specifically developed for pediatric patients in the emergency department and validated in both inpatient and outpatient settings.
Dr Horowitz, also the lead principal investigator for development of the ASQ, currently is leading six National Institute of Mental Health studies to validate and implement the screening tool in medical settings. She explained the three-tiered system during a session on youth suicide screening at the Pediatric Academic Societies annual meeting in Baltimore this year.
If a patient screens positive on the ASQ, a trained clinician should conduct a brief suicide safety assessment (BSSA), which takes approximately 10 minutes, Dr Horowitz said. Those who screen positive on the BSSA should receive the Patient Resource List and then be referred for a full mental health and safety evaluation, which takes about 30 minutes. Resources, such as nurse scripts and parent/guardian flyers, are available at the NIMH website, as well as translations of the ASQ in Arabic, Chinese, Dutch, French, Hebrew, Italian, Japanese, Korean, Portuguese, Russian, Somali, Spanish, and Vietnamese.
Acknowledging the importance of suicide screening
During the same session, John V. Campo, MD, an assistant dean for behavioral health and professor of behavioral medicine and psychiatry at West Virginia University in Morgantown, discussed why suicide risk screening is so crucial in general medical settings. As someone who trained as a pediatrician before crossing over to behavioral health, he acknowledged that primary care physicians already have many priorities to cover in short visits, and that the national answer to most public health problems is to deal with it in primary care.
“Anyone who has done primary care pediatrics understands the challenges involved with screening for anything – particularly when you identify someone who is extensively at risk,” he said.
But suicide has a disproportionately high impact on young populations, and “identifying youth at risk for suicide identifies a group of young people who are at risk for a variety of threats to their health and well-being,” he said.
For youth aged 10-19 years in 2016, suicide was the second leading cause of death behind accidents, according to the Centers for Disease Control and Prevention (Natl Vital Stat Rep. 2018 Jun;67[4]:1-16). In fact, accidents, suicide, and homicide account for three-quarters of deaths among youth aged 10-24 years (Natl Vital Stat Rep. 2019 Jun;68[6]:1-77), yet it’s typically the other 25% that most physicians trained for in residency.
“Suicide kills more kids than cancer, heart disease, infections – all kinds, sepsis, meningitis, pneumonia, influenza, HIV, respiratory conditions. Suicide kills more young people every year than all of that [combined],” Dr. Campo said. “And yet, when you walk through a modern emergency department, we see all these specialized programs for those who present with physical trauma or chest pain or all these other things, but zero specialized mental health services. There’s a disconnect.”
There is some good news in the data, he said. Observational data have shown that suicide rates negatively correlate with indicators of better access to health and medical health services, and researchers increasingly are identifying proven strategies that help prevent suicide in young people – once they have been identified.
But that’s the problem, “and we all know it,” Dr. Campo continued. “Most youth who are at risk for suicide aren’t recognized, and those who are recognized most often are untreated or inadequately treated,” he said. Further, “the best predictor of future behavior is past behavior,” but most adolescents die by suicide on their first attempt.
Again, however, Dr. Campo pivoted to the good news. Data also have shown that most youth who die by suicide had at least one health contact in the previous year, which means there are opportunities for screening and intervention.
The most common risk factor for suicide is having a mental health or substance use condition, present in about 90% of completed suicides and affecting approximately one in five youth. Prevalence is even higher in those with physical health conditions and among those with Medicaid or no insurance (J Child Psychol Psychiatry. 2006 Mar-Apr;47[3-4]372-94).
Yet, “the majority of them have not been treated at all for mental disorder, which seems to be the most important remediable risk factor for suicide, and even fewer are in current treatment at the time of the death,” Dr. Campo said. Suicide also is correlated with a number of other high-risk behaviors or circumstances, such as “vulnerabilities to substance abuse, riding in a car with someone who is intoxicated, carrying a weapon to school, fighting, and meeting criteria for depression” (Pediatrics. 2010 May;125[5]:945-52). Screening for suicide risk therefore allows physicians to identify youth vulnerable to a wide range of risks, conditions, or death.
Overcoming barriers to suicide screening in primary care
Given the high prevalence of suicide and its link to so many other risks for youth, screening in primary care can send the message that suicide screening “really is a part of health care,” Dr. Campo said. Incorporating screening into primary care also can help overcome distrust of behavioral health specialists in the general public and stigma associated with behavioral health disorders.
Primary care screening emphasizes the importance and credibility of mental health and challenges attitudinal barriers to care, he said.
At the same time, however, he acknowledged that providers themselves often are uneasy about addressing behavioral health. Therefore, “having the guideline and the expectation [of suicide risk screening] really drives home the point that this needs to be integrated into the rest of primary care,” he said. “It’s also consistent with the idea of the medical home.” With suicide the second leading cause of death among youth, “if there’s anything that we’re going to be thinking about screening for, one would think suicide would be high on the list.”
In fact, observational evidence has shown that educating and training primary care providers to recognize people with depression or a high risk for suicide can reduce suicide attempts and the suicide rate, Dr. Campo said (JAMA Psychiatry. 2017 Jun 1;74[6]:563-70). It also can help with the mismatch between where at-risk patients are and where behavioral health specialists are. About 90% of behavioral health specialists work only in specialty settings, and only 5% typically work in general medical settings, he said. Yet “most people who are in mental distress or in crisis don’t present in specialty behavioral health settings. They present in general medical settings.”
More data are needed to demonstrate more definitively whether and how much suicide risk screening changes outcomes, but we know a few things, Dr. Campo said, summing up his key points: “We know suicide’s a major source of mortality in youth that’s been relatively neglected in pediatric health care. Second, we know that suicide risk is associated with risk for other important causes of death, for mental disorders, and for alcohol and substance use.
“We know that most suicide decedents are unrecognized prior to the time of death, and those who are recognized often are not treated. We know that the majority of suicide deaths occur on the very first attempt. We also know that we increasingly have treatments, mental disorders that can be identified, and remediable risk factors, and [that at-risk youth] typically present at general medical settings. Beyond that, focusing on the general medical setting has both conceptual and practical advantages as a site for really helping us to detect patients at risk and then managing them.”
No funding was used for the presentations. Dr. Horowitz and Dr. Campo had no relevant financial disclosures.
and screening can take as little as 20 seconds, according to Lisa Horowitz, PhD, MPH, a staff scientist and clinical psychologist at the National Institute of Mental Health, Bethesda, Md.
But clinicians need to use validated screening instruments that are both population specific and site specific, and they need practice guidelines to treat patients screening positive.
Currently, many practitioners use depression screens – such as question #9 on suicide ideation and self harm on the Patient Health Questionnaire for Adolescents (PHQ-A) – to identify suicide risk, but preliminary data suggest these screens often are inadequate, Dr. Horowitz said. Just one question, especially one without precise language, does not appear to identify as many at-risk youths as more direct questions about suicidal thoughts and behaviors.
A Pathways to Clinical Care suicide risk screening work group therefore designed a three-tiered clinical pathway for suicide risk screenings in emergency departments, inpatient care, and outpatient primary care. It begins with the Ask Suicide-Screening Questions (ASQ), which takes about 20 seconds and was specifically developed for pediatric patients in the emergency department and validated in both inpatient and outpatient settings.
Dr Horowitz, also the lead principal investigator for development of the ASQ, currently is leading six National Institute of Mental Health studies to validate and implement the screening tool in medical settings. She explained the three-tiered system during a session on youth suicide screening at the Pediatric Academic Societies annual meeting in Baltimore this year.
If a patient screens positive on the ASQ, a trained clinician should conduct a brief suicide safety assessment (BSSA), which takes approximately 10 minutes, Dr Horowitz said. Those who screen positive on the BSSA should receive the Patient Resource List and then be referred for a full mental health and safety evaluation, which takes about 30 minutes. Resources, such as nurse scripts and parent/guardian flyers, are available at the NIMH website, as well as translations of the ASQ in Arabic, Chinese, Dutch, French, Hebrew, Italian, Japanese, Korean, Portuguese, Russian, Somali, Spanish, and Vietnamese.
Acknowledging the importance of suicide screening
During the same session, John V. Campo, MD, an assistant dean for behavioral health and professor of behavioral medicine and psychiatry at West Virginia University in Morgantown, discussed why suicide risk screening is so crucial in general medical settings. As someone who trained as a pediatrician before crossing over to behavioral health, he acknowledged that primary care physicians already have many priorities to cover in short visits, and that the national answer to most public health problems is to deal with it in primary care.
“Anyone who has done primary care pediatrics understands the challenges involved with screening for anything – particularly when you identify someone who is extensively at risk,” he said.
But suicide has a disproportionately high impact on young populations, and “identifying youth at risk for suicide identifies a group of young people who are at risk for a variety of threats to their health and well-being,” he said.
For youth aged 10-19 years in 2016, suicide was the second leading cause of death behind accidents, according to the Centers for Disease Control and Prevention (Natl Vital Stat Rep. 2018 Jun;67[4]:1-16). In fact, accidents, suicide, and homicide account for three-quarters of deaths among youth aged 10-24 years (Natl Vital Stat Rep. 2019 Jun;68[6]:1-77), yet it’s typically the other 25% that most physicians trained for in residency.
“Suicide kills more kids than cancer, heart disease, infections – all kinds, sepsis, meningitis, pneumonia, influenza, HIV, respiratory conditions. Suicide kills more young people every year than all of that [combined],” Dr. Campo said. “And yet, when you walk through a modern emergency department, we see all these specialized programs for those who present with physical trauma or chest pain or all these other things, but zero specialized mental health services. There’s a disconnect.”
There is some good news in the data, he said. Observational data have shown that suicide rates negatively correlate with indicators of better access to health and medical health services, and researchers increasingly are identifying proven strategies that help prevent suicide in young people – once they have been identified.
But that’s the problem, “and we all know it,” Dr. Campo continued. “Most youth who are at risk for suicide aren’t recognized, and those who are recognized most often are untreated or inadequately treated,” he said. Further, “the best predictor of future behavior is past behavior,” but most adolescents die by suicide on their first attempt.
Again, however, Dr. Campo pivoted to the good news. Data also have shown that most youth who die by suicide had at least one health contact in the previous year, which means there are opportunities for screening and intervention.
The most common risk factor for suicide is having a mental health or substance use condition, present in about 90% of completed suicides and affecting approximately one in five youth. Prevalence is even higher in those with physical health conditions and among those with Medicaid or no insurance (J Child Psychol Psychiatry. 2006 Mar-Apr;47[3-4]372-94).
Yet, “the majority of them have not been treated at all for mental disorder, which seems to be the most important remediable risk factor for suicide, and even fewer are in current treatment at the time of the death,” Dr. Campo said. Suicide also is correlated with a number of other high-risk behaviors or circumstances, such as “vulnerabilities to substance abuse, riding in a car with someone who is intoxicated, carrying a weapon to school, fighting, and meeting criteria for depression” (Pediatrics. 2010 May;125[5]:945-52). Screening for suicide risk therefore allows physicians to identify youth vulnerable to a wide range of risks, conditions, or death.
Overcoming barriers to suicide screening in primary care
Given the high prevalence of suicide and its link to so many other risks for youth, screening in primary care can send the message that suicide screening “really is a part of health care,” Dr. Campo said. Incorporating screening into primary care also can help overcome distrust of behavioral health specialists in the general public and stigma associated with behavioral health disorders.
Primary care screening emphasizes the importance and credibility of mental health and challenges attitudinal barriers to care, he said.
At the same time, however, he acknowledged that providers themselves often are uneasy about addressing behavioral health. Therefore, “having the guideline and the expectation [of suicide risk screening] really drives home the point that this needs to be integrated into the rest of primary care,” he said. “It’s also consistent with the idea of the medical home.” With suicide the second leading cause of death among youth, “if there’s anything that we’re going to be thinking about screening for, one would think suicide would be high on the list.”
In fact, observational evidence has shown that educating and training primary care providers to recognize people with depression or a high risk for suicide can reduce suicide attempts and the suicide rate, Dr. Campo said (JAMA Psychiatry. 2017 Jun 1;74[6]:563-70). It also can help with the mismatch between where at-risk patients are and where behavioral health specialists are. About 90% of behavioral health specialists work only in specialty settings, and only 5% typically work in general medical settings, he said. Yet “most people who are in mental distress or in crisis don’t present in specialty behavioral health settings. They present in general medical settings.”
More data are needed to demonstrate more definitively whether and how much suicide risk screening changes outcomes, but we know a few things, Dr. Campo said, summing up his key points: “We know suicide’s a major source of mortality in youth that’s been relatively neglected in pediatric health care. Second, we know that suicide risk is associated with risk for other important causes of death, for mental disorders, and for alcohol and substance use.
“We know that most suicide decedents are unrecognized prior to the time of death, and those who are recognized often are not treated. We know that the majority of suicide deaths occur on the very first attempt. We also know that we increasingly have treatments, mental disorders that can be identified, and remediable risk factors, and [that at-risk youth] typically present at general medical settings. Beyond that, focusing on the general medical setting has both conceptual and practical advantages as a site for really helping us to detect patients at risk and then managing them.”
No funding was used for the presentations. Dr. Horowitz and Dr. Campo had no relevant financial disclosures.
and screening can take as little as 20 seconds, according to Lisa Horowitz, PhD, MPH, a staff scientist and clinical psychologist at the National Institute of Mental Health, Bethesda, Md.
But clinicians need to use validated screening instruments that are both population specific and site specific, and they need practice guidelines to treat patients screening positive.
Currently, many practitioners use depression screens – such as question #9 on suicide ideation and self harm on the Patient Health Questionnaire for Adolescents (PHQ-A) – to identify suicide risk, but preliminary data suggest these screens often are inadequate, Dr. Horowitz said. Just one question, especially one without precise language, does not appear to identify as many at-risk youths as more direct questions about suicidal thoughts and behaviors.
A Pathways to Clinical Care suicide risk screening work group therefore designed a three-tiered clinical pathway for suicide risk screenings in emergency departments, inpatient care, and outpatient primary care. It begins with the Ask Suicide-Screening Questions (ASQ), which takes about 20 seconds and was specifically developed for pediatric patients in the emergency department and validated in both inpatient and outpatient settings.
Dr Horowitz, also the lead principal investigator for development of the ASQ, currently is leading six National Institute of Mental Health studies to validate and implement the screening tool in medical settings. She explained the three-tiered system during a session on youth suicide screening at the Pediatric Academic Societies annual meeting in Baltimore this year.
If a patient screens positive on the ASQ, a trained clinician should conduct a brief suicide safety assessment (BSSA), which takes approximately 10 minutes, Dr Horowitz said. Those who screen positive on the BSSA should receive the Patient Resource List and then be referred for a full mental health and safety evaluation, which takes about 30 minutes. Resources, such as nurse scripts and parent/guardian flyers, are available at the NIMH website, as well as translations of the ASQ in Arabic, Chinese, Dutch, French, Hebrew, Italian, Japanese, Korean, Portuguese, Russian, Somali, Spanish, and Vietnamese.
Acknowledging the importance of suicide screening
During the same session, John V. Campo, MD, an assistant dean for behavioral health and professor of behavioral medicine and psychiatry at West Virginia University in Morgantown, discussed why suicide risk screening is so crucial in general medical settings. As someone who trained as a pediatrician before crossing over to behavioral health, he acknowledged that primary care physicians already have many priorities to cover in short visits, and that the national answer to most public health problems is to deal with it in primary care.
“Anyone who has done primary care pediatrics understands the challenges involved with screening for anything – particularly when you identify someone who is extensively at risk,” he said.
But suicide has a disproportionately high impact on young populations, and “identifying youth at risk for suicide identifies a group of young people who are at risk for a variety of threats to their health and well-being,” he said.
For youth aged 10-19 years in 2016, suicide was the second leading cause of death behind accidents, according to the Centers for Disease Control and Prevention (Natl Vital Stat Rep. 2018 Jun;67[4]:1-16). In fact, accidents, suicide, and homicide account for three-quarters of deaths among youth aged 10-24 years (Natl Vital Stat Rep. 2019 Jun;68[6]:1-77), yet it’s typically the other 25% that most physicians trained for in residency.
“Suicide kills more kids than cancer, heart disease, infections – all kinds, sepsis, meningitis, pneumonia, influenza, HIV, respiratory conditions. Suicide kills more young people every year than all of that [combined],” Dr. Campo said. “And yet, when you walk through a modern emergency department, we see all these specialized programs for those who present with physical trauma or chest pain or all these other things, but zero specialized mental health services. There’s a disconnect.”
There is some good news in the data, he said. Observational data have shown that suicide rates negatively correlate with indicators of better access to health and medical health services, and researchers increasingly are identifying proven strategies that help prevent suicide in young people – once they have been identified.
But that’s the problem, “and we all know it,” Dr. Campo continued. “Most youth who are at risk for suicide aren’t recognized, and those who are recognized most often are untreated or inadequately treated,” he said. Further, “the best predictor of future behavior is past behavior,” but most adolescents die by suicide on their first attempt.
Again, however, Dr. Campo pivoted to the good news. Data also have shown that most youth who die by suicide had at least one health contact in the previous year, which means there are opportunities for screening and intervention.
The most common risk factor for suicide is having a mental health or substance use condition, present in about 90% of completed suicides and affecting approximately one in five youth. Prevalence is even higher in those with physical health conditions and among those with Medicaid or no insurance (J Child Psychol Psychiatry. 2006 Mar-Apr;47[3-4]372-94).
Yet, “the majority of them have not been treated at all for mental disorder, which seems to be the most important remediable risk factor for suicide, and even fewer are in current treatment at the time of the death,” Dr. Campo said. Suicide also is correlated with a number of other high-risk behaviors or circumstances, such as “vulnerabilities to substance abuse, riding in a car with someone who is intoxicated, carrying a weapon to school, fighting, and meeting criteria for depression” (Pediatrics. 2010 May;125[5]:945-52). Screening for suicide risk therefore allows physicians to identify youth vulnerable to a wide range of risks, conditions, or death.
Overcoming barriers to suicide screening in primary care
Given the high prevalence of suicide and its link to so many other risks for youth, screening in primary care can send the message that suicide screening “really is a part of health care,” Dr. Campo said. Incorporating screening into primary care also can help overcome distrust of behavioral health specialists in the general public and stigma associated with behavioral health disorders.
Primary care screening emphasizes the importance and credibility of mental health and challenges attitudinal barriers to care, he said.
At the same time, however, he acknowledged that providers themselves often are uneasy about addressing behavioral health. Therefore, “having the guideline and the expectation [of suicide risk screening] really drives home the point that this needs to be integrated into the rest of primary care,” he said. “It’s also consistent with the idea of the medical home.” With suicide the second leading cause of death among youth, “if there’s anything that we’re going to be thinking about screening for, one would think suicide would be high on the list.”
In fact, observational evidence has shown that educating and training primary care providers to recognize people with depression or a high risk for suicide can reduce suicide attempts and the suicide rate, Dr. Campo said (JAMA Psychiatry. 2017 Jun 1;74[6]:563-70). It also can help with the mismatch between where at-risk patients are and where behavioral health specialists are. About 90% of behavioral health specialists work only in specialty settings, and only 5% typically work in general medical settings, he said. Yet “most people who are in mental distress or in crisis don’t present in specialty behavioral health settings. They present in general medical settings.”
More data are needed to demonstrate more definitively whether and how much suicide risk screening changes outcomes, but we know a few things, Dr. Campo said, summing up his key points: “We know suicide’s a major source of mortality in youth that’s been relatively neglected in pediatric health care. Second, we know that suicide risk is associated with risk for other important causes of death, for mental disorders, and for alcohol and substance use.
“We know that most suicide decedents are unrecognized prior to the time of death, and those who are recognized often are not treated. We know that the majority of suicide deaths occur on the very first attempt. We also know that we increasingly have treatments, mental disorders that can be identified, and remediable risk factors, and [that at-risk youth] typically present at general medical settings. Beyond that, focusing on the general medical setting has both conceptual and practical advantages as a site for really helping us to detect patients at risk and then managing them.”
No funding was used for the presentations. Dr. Horowitz and Dr. Campo had no relevant financial disclosures.
Without action, every child will be affected by climate change
As wildfires increase the likelihood of respiratory illnesses for residents in California and Queensland, Australia, a new report from the Lancet warns that such health risks will become increasingly common without action to address climate change. But, the authors stressed, it’s still possible to prevent some health effects and mitigate others.
Given the magnitude of the issue, lead author Nick Watts, MBBS, MA, framed the issue in terms of what an individual child born today will face in his or her future. If the world continues on its current trajectory, such a child will eventually live in a world at least 4º C above average preindustrial temperatures.
“We roughly know what that looks like from a climate perspective,” said Dr. Watts, executive director of The Lancet Countdown: Tracking Progress on Health and Climate Change, during a telebriefing on the report.
“We have no idea of what that looks like from a public health perspective, but we know it is catastrophic,” he continued. “We know that it has the potential to undermine the last 50 years of gains in public health and overwhelm the health systems that we rely on.”
Health sector a significant, growing contributor
The report described the changes to which climate change has already contributed and addresses both the health threats and the way institutions and states are currently responding to those threats. It also included policy briefs specific to individual countries and an extensive appendix with projections data.
The authors noted that progress in mitigating fossil fuel combustion – the biggest driver of rising temperatures – is “intermittent at best,” with carbon dioxide emissions continuing to rise in 2018. The past decade has included 8 of the 10 hottest years on record. “Many of the indicators contained in this report suggest the world is following this ‘business as usual’ pathway,” the authors wrote.
In fact, the trend of coal-produced energy that had been declining actually increased 1.7% between 2016 and 2018. Perhaps ironically, given the focus of the report, “the healthcare sector is responsible for about 4.6% of global emissions, a value which is steadily rising across most major economies,” Dr. Watts and colleagues reported.
The potential health risks from climate change range from increased chronic illness, such as asthma and cardiovascular disease, to the increased spread of infectious diseases, especially vector-borne diseases, including dengue fever, malaria, and chikungunya. Increases in the frequency and intensity of severe weather events can lead to increased acute and longer-term morbidity and mortality.
Though children will suffer the brunt of negative health impact from climate change, the effects will touch people at every stage of life, from in utero development through old age, the authors emphasized.
“Downward trends in global yield potential for all major crops tracked since 1960 threaten food production and food security, with infants often the worst affected by the potentially permanent effects of undernutrition,” the authors reported. Children are also most susceptible to diarrheal disease and infectious diseases, particularly dengue.
Mitigating actions available
But the report focused as much on solutions and mitigation strategies as it did on the worst-case scenario without action. Speakers during the telebriefing emphasized the responsibility of all people, including physicians and other health care providers, to play a role in countering the public health disaster that could result from inaction on climate.
“Thankfully, here we have the treatment for climate change, solutions to shift away from the carbon pollution and towards clean energy and working to find the best way to protect ourselves and each other from climate change,” Renee N. Salas, MD, MPH, lead author of the 2019 Lancet Countdown U.S. Policy Brief and a Harvard C-CHANGE Fellow, said during the press briefing. “All we need is political will.”
Salas compared the present moment to that period when a physician still has the ability to save a critically ill patient’s life with fast action.
“If I don’t act quickly, the patient may still die even though that treatment would have saved their life earlier,” she said. “We are in that narrow window.”
Physicians have a responsibility to speak to patients and families frankly about not only specific conditions, such as asthma, but also the climate-related causes of those conditions, such as increasing air pollution, said Gina McCarthy, director of the Harvard Center for Climate, Health and the Global Environment and the 13th administrator U.S. Environmental Policy Administration. Physicians are trusted advisers and therefore need to speak up because climate change is “about the health and well-being and the future of children,” she said.
Political polarization is one of the biggest challenges to addressing climate change and stymies efforts to take action, according to Richard Carmona, MD, who served as the 17th U.S. Surgeon General.
“The thing that frustrated me as a surgeon general and continues to frustrate me today is that these very scientifically vetted issues are reduced to political currency that creates divisiveness, and things don’t get done,” he said during the briefing.
“We have to move beyond that and elevate this discussion to one of the survival of our civilization and the health and safety and security of all nations in the world,” continued Dr. Carmona, who is also a professor of public health at the University of Arizona in Tucson.
The report notes that the warming is already “occurring faster than governments are able, or willing, to respond,” likely contributing to the increased outcry across the world from youth about the need to act.
And anyone can take some kind of action, Ms. McCarthy said. Her aim is to make the reality of climate change effects personal so that people understand its impact on them as well as what they can do.
“The report provides a list of actions that policy makers can take today to reduce the threat of climate change” as well as information on “how we can adapt and be more resilient as communities” while facing climate change’s challenges, she said.
Ms. McCarthy encouraged people to pay particular attention to the report’s mitigation and adaptation recommendations, “because I want them to know that climate change isn’t a lost cause,” she said. The actions people can demand of policymakers will not only avoid the worst-case health scenario but can also improve health today, she added.
“We can do better than to dwell on the problem,” Ms. McCarthy said. “We need people now to be hopeful about climate change, to do as others have suggested and demand action and take action in their own lives. We can use that to really drive solutions.”
Annual report assesses numerous indicators
The Lancet Countdown is an annual report supported by the Wellcome Trust that pulls together research from 35 academic institutions and United Nations agencies across the world to provide an update on what the authors described as “41 health indicators across five key domains: climate change impacts, exposures and vulnerability; adaptation, planning, and resilience for health; mitigation action and health cobenefits; economics and finance; [and] public and political engagement.”
Given the complexity of the issue of climate change and the wide range of possible effects and preventive measures, contributing researchers included not just climate scientists but also ecologists, mathematicians, engineers, hydrologists, social and political scientists, physicians and other public health professionals, and experts in energy, food, and transportation.
The research was supported by the Wellcome Trust. Multiple authors also received support from a range of government institutions and public and private foundations and fellowships. No relevant financial relationships were noted.
SOURCE: Watts N et al. Lancet. 2019 Nov 13. doi: 10.1016/S0140-6736(19)32596-6.
This story first appeared in Medscape.com.
As wildfires increase the likelihood of respiratory illnesses for residents in California and Queensland, Australia, a new report from the Lancet warns that such health risks will become increasingly common without action to address climate change. But, the authors stressed, it’s still possible to prevent some health effects and mitigate others.
Given the magnitude of the issue, lead author Nick Watts, MBBS, MA, framed the issue in terms of what an individual child born today will face in his or her future. If the world continues on its current trajectory, such a child will eventually live in a world at least 4º C above average preindustrial temperatures.
“We roughly know what that looks like from a climate perspective,” said Dr. Watts, executive director of The Lancet Countdown: Tracking Progress on Health and Climate Change, during a telebriefing on the report.
“We have no idea of what that looks like from a public health perspective, but we know it is catastrophic,” he continued. “We know that it has the potential to undermine the last 50 years of gains in public health and overwhelm the health systems that we rely on.”
Health sector a significant, growing contributor
The report described the changes to which climate change has already contributed and addresses both the health threats and the way institutions and states are currently responding to those threats. It also included policy briefs specific to individual countries and an extensive appendix with projections data.
The authors noted that progress in mitigating fossil fuel combustion – the biggest driver of rising temperatures – is “intermittent at best,” with carbon dioxide emissions continuing to rise in 2018. The past decade has included 8 of the 10 hottest years on record. “Many of the indicators contained in this report suggest the world is following this ‘business as usual’ pathway,” the authors wrote.
In fact, the trend of coal-produced energy that had been declining actually increased 1.7% between 2016 and 2018. Perhaps ironically, given the focus of the report, “the healthcare sector is responsible for about 4.6% of global emissions, a value which is steadily rising across most major economies,” Dr. Watts and colleagues reported.
The potential health risks from climate change range from increased chronic illness, such as asthma and cardiovascular disease, to the increased spread of infectious diseases, especially vector-borne diseases, including dengue fever, malaria, and chikungunya. Increases in the frequency and intensity of severe weather events can lead to increased acute and longer-term morbidity and mortality.
Though children will suffer the brunt of negative health impact from climate change, the effects will touch people at every stage of life, from in utero development through old age, the authors emphasized.
“Downward trends in global yield potential for all major crops tracked since 1960 threaten food production and food security, with infants often the worst affected by the potentially permanent effects of undernutrition,” the authors reported. Children are also most susceptible to diarrheal disease and infectious diseases, particularly dengue.
Mitigating actions available
But the report focused as much on solutions and mitigation strategies as it did on the worst-case scenario without action. Speakers during the telebriefing emphasized the responsibility of all people, including physicians and other health care providers, to play a role in countering the public health disaster that could result from inaction on climate.
“Thankfully, here we have the treatment for climate change, solutions to shift away from the carbon pollution and towards clean energy and working to find the best way to protect ourselves and each other from climate change,” Renee N. Salas, MD, MPH, lead author of the 2019 Lancet Countdown U.S. Policy Brief and a Harvard C-CHANGE Fellow, said during the press briefing. “All we need is political will.”
Salas compared the present moment to that period when a physician still has the ability to save a critically ill patient’s life with fast action.
“If I don’t act quickly, the patient may still die even though that treatment would have saved their life earlier,” she said. “We are in that narrow window.”
Physicians have a responsibility to speak to patients and families frankly about not only specific conditions, such as asthma, but also the climate-related causes of those conditions, such as increasing air pollution, said Gina McCarthy, director of the Harvard Center for Climate, Health and the Global Environment and the 13th administrator U.S. Environmental Policy Administration. Physicians are trusted advisers and therefore need to speak up because climate change is “about the health and well-being and the future of children,” she said.
Political polarization is one of the biggest challenges to addressing climate change and stymies efforts to take action, according to Richard Carmona, MD, who served as the 17th U.S. Surgeon General.
“The thing that frustrated me as a surgeon general and continues to frustrate me today is that these very scientifically vetted issues are reduced to political currency that creates divisiveness, and things don’t get done,” he said during the briefing.
“We have to move beyond that and elevate this discussion to one of the survival of our civilization and the health and safety and security of all nations in the world,” continued Dr. Carmona, who is also a professor of public health at the University of Arizona in Tucson.
The report notes that the warming is already “occurring faster than governments are able, or willing, to respond,” likely contributing to the increased outcry across the world from youth about the need to act.
And anyone can take some kind of action, Ms. McCarthy said. Her aim is to make the reality of climate change effects personal so that people understand its impact on them as well as what they can do.
“The report provides a list of actions that policy makers can take today to reduce the threat of climate change” as well as information on “how we can adapt and be more resilient as communities” while facing climate change’s challenges, she said.
Ms. McCarthy encouraged people to pay particular attention to the report’s mitigation and adaptation recommendations, “because I want them to know that climate change isn’t a lost cause,” she said. The actions people can demand of policymakers will not only avoid the worst-case health scenario but can also improve health today, she added.
“We can do better than to dwell on the problem,” Ms. McCarthy said. “We need people now to be hopeful about climate change, to do as others have suggested and demand action and take action in their own lives. We can use that to really drive solutions.”
Annual report assesses numerous indicators
The Lancet Countdown is an annual report supported by the Wellcome Trust that pulls together research from 35 academic institutions and United Nations agencies across the world to provide an update on what the authors described as “41 health indicators across five key domains: climate change impacts, exposures and vulnerability; adaptation, planning, and resilience for health; mitigation action and health cobenefits; economics and finance; [and] public and political engagement.”
Given the complexity of the issue of climate change and the wide range of possible effects and preventive measures, contributing researchers included not just climate scientists but also ecologists, mathematicians, engineers, hydrologists, social and political scientists, physicians and other public health professionals, and experts in energy, food, and transportation.
The research was supported by the Wellcome Trust. Multiple authors also received support from a range of government institutions and public and private foundations and fellowships. No relevant financial relationships were noted.
SOURCE: Watts N et al. Lancet. 2019 Nov 13. doi: 10.1016/S0140-6736(19)32596-6.
This story first appeared in Medscape.com.
As wildfires increase the likelihood of respiratory illnesses for residents in California and Queensland, Australia, a new report from the Lancet warns that such health risks will become increasingly common without action to address climate change. But, the authors stressed, it’s still possible to prevent some health effects and mitigate others.
Given the magnitude of the issue, lead author Nick Watts, MBBS, MA, framed the issue in terms of what an individual child born today will face in his or her future. If the world continues on its current trajectory, such a child will eventually live in a world at least 4º C above average preindustrial temperatures.
“We roughly know what that looks like from a climate perspective,” said Dr. Watts, executive director of The Lancet Countdown: Tracking Progress on Health and Climate Change, during a telebriefing on the report.
“We have no idea of what that looks like from a public health perspective, but we know it is catastrophic,” he continued. “We know that it has the potential to undermine the last 50 years of gains in public health and overwhelm the health systems that we rely on.”
Health sector a significant, growing contributor
The report described the changes to which climate change has already contributed and addresses both the health threats and the way institutions and states are currently responding to those threats. It also included policy briefs specific to individual countries and an extensive appendix with projections data.
The authors noted that progress in mitigating fossil fuel combustion – the biggest driver of rising temperatures – is “intermittent at best,” with carbon dioxide emissions continuing to rise in 2018. The past decade has included 8 of the 10 hottest years on record. “Many of the indicators contained in this report suggest the world is following this ‘business as usual’ pathway,” the authors wrote.
In fact, the trend of coal-produced energy that had been declining actually increased 1.7% between 2016 and 2018. Perhaps ironically, given the focus of the report, “the healthcare sector is responsible for about 4.6% of global emissions, a value which is steadily rising across most major economies,” Dr. Watts and colleagues reported.
The potential health risks from climate change range from increased chronic illness, such as asthma and cardiovascular disease, to the increased spread of infectious diseases, especially vector-borne diseases, including dengue fever, malaria, and chikungunya. Increases in the frequency and intensity of severe weather events can lead to increased acute and longer-term morbidity and mortality.
Though children will suffer the brunt of negative health impact from climate change, the effects will touch people at every stage of life, from in utero development through old age, the authors emphasized.
“Downward trends in global yield potential for all major crops tracked since 1960 threaten food production and food security, with infants often the worst affected by the potentially permanent effects of undernutrition,” the authors reported. Children are also most susceptible to diarrheal disease and infectious diseases, particularly dengue.
Mitigating actions available
But the report focused as much on solutions and mitigation strategies as it did on the worst-case scenario without action. Speakers during the telebriefing emphasized the responsibility of all people, including physicians and other health care providers, to play a role in countering the public health disaster that could result from inaction on climate.
“Thankfully, here we have the treatment for climate change, solutions to shift away from the carbon pollution and towards clean energy and working to find the best way to protect ourselves and each other from climate change,” Renee N. Salas, MD, MPH, lead author of the 2019 Lancet Countdown U.S. Policy Brief and a Harvard C-CHANGE Fellow, said during the press briefing. “All we need is political will.”
Salas compared the present moment to that period when a physician still has the ability to save a critically ill patient’s life with fast action.
“If I don’t act quickly, the patient may still die even though that treatment would have saved their life earlier,” she said. “We are in that narrow window.”
Physicians have a responsibility to speak to patients and families frankly about not only specific conditions, such as asthma, but also the climate-related causes of those conditions, such as increasing air pollution, said Gina McCarthy, director of the Harvard Center for Climate, Health and the Global Environment and the 13th administrator U.S. Environmental Policy Administration. Physicians are trusted advisers and therefore need to speak up because climate change is “about the health and well-being and the future of children,” she said.
Political polarization is one of the biggest challenges to addressing climate change and stymies efforts to take action, according to Richard Carmona, MD, who served as the 17th U.S. Surgeon General.
“The thing that frustrated me as a surgeon general and continues to frustrate me today is that these very scientifically vetted issues are reduced to political currency that creates divisiveness, and things don’t get done,” he said during the briefing.
“We have to move beyond that and elevate this discussion to one of the survival of our civilization and the health and safety and security of all nations in the world,” continued Dr. Carmona, who is also a professor of public health at the University of Arizona in Tucson.
The report notes that the warming is already “occurring faster than governments are able, or willing, to respond,” likely contributing to the increased outcry across the world from youth about the need to act.
And anyone can take some kind of action, Ms. McCarthy said. Her aim is to make the reality of climate change effects personal so that people understand its impact on them as well as what they can do.
“The report provides a list of actions that policy makers can take today to reduce the threat of climate change” as well as information on “how we can adapt and be more resilient as communities” while facing climate change’s challenges, she said.
Ms. McCarthy encouraged people to pay particular attention to the report’s mitigation and adaptation recommendations, “because I want them to know that climate change isn’t a lost cause,” she said. The actions people can demand of policymakers will not only avoid the worst-case health scenario but can also improve health today, she added.
“We can do better than to dwell on the problem,” Ms. McCarthy said. “We need people now to be hopeful about climate change, to do as others have suggested and demand action and take action in their own lives. We can use that to really drive solutions.”
Annual report assesses numerous indicators
The Lancet Countdown is an annual report supported by the Wellcome Trust that pulls together research from 35 academic institutions and United Nations agencies across the world to provide an update on what the authors described as “41 health indicators across five key domains: climate change impacts, exposures and vulnerability; adaptation, planning, and resilience for health; mitigation action and health cobenefits; economics and finance; [and] public and political engagement.”
Given the complexity of the issue of climate change and the wide range of possible effects and preventive measures, contributing researchers included not just climate scientists but also ecologists, mathematicians, engineers, hydrologists, social and political scientists, physicians and other public health professionals, and experts in energy, food, and transportation.
The research was supported by the Wellcome Trust. Multiple authors also received support from a range of government institutions and public and private foundations and fellowships. No relevant financial relationships were noted.
SOURCE: Watts N et al. Lancet. 2019 Nov 13. doi: 10.1016/S0140-6736(19)32596-6.
This story first appeared in Medscape.com.
Don’t miss neuromuscular complications of cancer immunotherapy
AUSTIN, TEX. – Neuromuscular complications from immunotherapy for cancer are rare, but they occur often enough that it is helpful to know which ones can result from different immunotherapies and how to distinguish them from non–adverse event conditions, according to Christopher Trevino, MD, a neuro-oncologist at Tulane University in New Orleans.
At the annual meeting of the American Association for Neuromuscular and Electrodiagnostic Medicine, Dr. Trevino reviewed immunotherapy types, particularly immune checkpoint inhibitors, and the most common neuromuscular complications – primarily neuropathy, myasthenia gravis (MG), myositis, and encephalitis or meningitis.
“Timing of onset is a critical component to assist in identifying immune checkpoint inhibitor–associated versus non–immune checkpoint inhibitor–associated neuromuscular disease,” Dr. Trevino told attendees. Prompt recognition can be particularly urgent for MG because crisis and death rates are higher when induced by immunotherapy and require quick treatment. “Understanding the mechanisms of action sets a foundation for treatment approach,” he added.
Any part of the nervous system can be affected by immunotherapy toxicity, he said, and syndromes often overlap, with the peripheral nervous system typically more often affected than the central nervous system. Neurologic immune-related adverse events typically occur within four cycles of therapy – about 12 weeks after therapy initiation – but should always involve a work-up to exclude effects from the cancer itself, other neuromuscular diagnoses unrelated to therapy, and other toxicities from chemotherapy.
Recommended first-line treatment is halting immunotherapy with or without corticosteroids, after which most patients improve, often with “rapid, complete resolution of symptoms,” Dr. Trevino said. Restarting immunotherapy treatment is possible in some patients, though.
CAR T-cell and dendritic cell vaccine therapies
Four main types of immunotherapy exist: viral therapy, vaccine therapy, immune checkpoint inhibitors, and adoptive cell transfer, such as chimeric antigen receptor (CAR) T-cell therapy. Dr. Trevino focused on checkpoint inhibitors and adoptive cell transfer.
CAR T-cell therapy is a multistep treatment process that involves first removing blood from the patient to obtain their T cells. These are used to create and grow CAR T cells in the lab so that they can be infused back into the patient. The cells then bind to cancer cells and destroy them. Examples of approved CAR T-cell therapy include Yescarta (axicabtagene ciloleucel) for some types of non-Hodgkin lymphoma and Kymriah (tisagenlecleucel) for acute lymphoblastic leukemia (ALL).
Dendritic cell vaccines are similar to CAR T-cell therapy in that they also use the patient’s own immune cells to create cancer-killing cells that the patient then receives back. The only currently approved dendritic cell vaccine is Provenge (sipuleucel-T) for advanced prostate cancer.
The main toxicity to watch for from CAR T-cell therapy and dendritic cell vaccines is cytokine release syndrome (CRS). It can begin anywhere from 1-14 days after the infusion and involves T-cell expansion in the body that leads to a cytokine storm. Symptoms are wide ranging, including fatigue, fever, loss of appetite, tachycardia, hypotension, pain, rash, diarrhea, headache, confusion, seizures, muscle and joint pain, tachypnea, hypoxia and hallucinations, among others.
Specific central neurotoxicities that can result from CAR T-cell therapy include encephalopathy, cerebral edema, seizures and status epilepticus, cerebral vasospasm, and aphasia.
Immune checkpoint inhibitor toxicities
Immune checkpoint inhibitors are drugs that interrupt a cancer’s ability to hijack the immune system; they block the proteins that hold back T-cells from attacking the cancer, thereby releasing the immune system to go after the malignant cells.
The two most common types of immune checkpoint inhibitors are those targeting the programmed cell death protein 1 (PD-1) and programmed death-ligand 1 (PD-L1) pathways. The three currently approved PD-1 inhibitors are pembrolizumab (Keytruda), nivolumab (Opdivo), and cemiplimab (Libtayo), which can treat nearly a dozen malignancies affecting different organs. Atezolizumab (Tecentriq), avelumab (Bavencio), and durvalumab (Imfinzi) are the three currently approved PD-L1 inhibitors, indicated for urothelial carcinoma and a handful of other cancers, such as small-cell and non–small cell lung cancer and triple negative breast cancer.
The only other type of approved checkpoint inhibitor is ipilimumab (Yervoy), which targets the CTLA-4 protein. A number of other checkpoint inhibitors are in trials, however, such as ones targeting pathways involving OX40, ICOS, TIM3, and LAG-3 (J Hematol Oncol. 2018. doi: 10.1186/s13045-018-0582-8).
Immune-related adverse events are less common with PD-1 or PD-L1 inhibitors – a rate of 5%-10% – compared with adverse events from CTLA-4 inhibitors, which occur in about 15% of patients. Neurologic complications occur even more rarely – about 1%-4% of all immune checkpoint inhibitor therapies – and primarily include MG, Guillain-Barré syndrome (GBS), chronic inflammatory demyelinating polyneuropathy (CIDP), and inflammatory myositis (Muscle Nerve. 2018;58[1]:10-22).
Treatment with multiple checkpoint inhibitors increases the likelihood of severe adverse events, with rates of up to 30%-50% of patients with dual treatment.
Distinguishing features of neuromuscular immunotherapy-related adverse events
MG is the most common neuromuscular immune-related adverse event from immune checkpoint inhibitors and tends to occur 3-12 weeks after beginning treatment, frequently comorbid with inflammatory myopathy or cardiomyopathy, Dr. Trevino said. About two-thirds of cases are de novo, while the remaining one-third involve preexisting MG; no reports of Lambert-Eaton myasthenic syndrome have been linked to checkpoint inhibitors.
Several characteristics distinguish checkpoint inhibitor–associated MG from standard MG. Standard MG can be ocular with or without bulbar or appendicular weakness, whereas immunotherapy-related MG is rarely only ocular (about 18% of cases). Immunotherapy-related MG involves an MG crisis at diagnosis in up to 50% of cases and has high mortality, both of which are rarer with standard MG.
While standard MG can be seronegative or involve AChR, MuSK, or LRP4 antibodies, about two-thirds of immunotherapy-related MG cases are positive for AChR antibodies. LRP4 antibodies are rare with MG from checkpoint inhibitors, and no MuSK antibodies have been reported in these cases. Creatine kinase (CK) or troponin I (TnI) elevation occurs in about 87% of patients with checkpoint inhibitor-induced MG, but standard MG doesn’t typically involve increased CK levels.
Inflammatory myositis (IM), the second most common neuromuscular adverse event from immunotherapy, tends to occur 2-15 weeks after immune checkpoint inhibitor therapy and can involve polymyositis, necrotizing autoimmune myopathy, dermatomyositis, granulomatous myositis, or other nonspecific myositis and myopathies.
Though proximal weakness occurs with IM both associated with immunotherapy and not, ocular symptoms are unique to cases associated with therapy and occur in about half of them. Myalgia, dyspnea, and dysphagia can all occur with checkpoint inhibitor–associated IM but don’t generally occur with standard IM. Immunotherapy-related IM is usually seronegative for myositis antibodies and doesn’t generally cause abnormalities in electromyography, compared with increased exertional activity and early recruitment of myopathic motor units in electromyography with standard IM.
GBS and CIDP are the third most common cause of neuromuscular complications from checkpoint inhibitors. The main distinguishing feature of these conditions from those not related to immunotherapy is that they occur anywhere from 4 to 68 weeks after therapy begins. Presentation is otherwise similar whether related to checkpoint inhibitors or not.
Aside from GBS and CIDP, other neuropathies that can result from immunotherapy complications include acute cranial neuropathies, axonal or demyelinating neuropathies, motor polyradiculopathy, vasculitic neuropathy, and plexopathy.
Neuromuscular complications other than those described above can also occur from checkpoint inhibitor therapy, such as enteric neuropathy, polyradiculitis, and meningo-radiculo-neuritis, but these are much rarer.
Four organizations have developed consensus guidelines for immune checkpoint inhibitor toxicities: the European Society for Medical Oncology (ESMO, 2017), Society for Immunotherapy of Cancer (SITC, 2017), American Society of Clinical Oncology (ASCO, 2018), and National Comprehensive Cancer Network (NCCN, 2019).
Dr Trevino had no disclosures.
AUSTIN, TEX. – Neuromuscular complications from immunotherapy for cancer are rare, but they occur often enough that it is helpful to know which ones can result from different immunotherapies and how to distinguish them from non–adverse event conditions, according to Christopher Trevino, MD, a neuro-oncologist at Tulane University in New Orleans.
At the annual meeting of the American Association for Neuromuscular and Electrodiagnostic Medicine, Dr. Trevino reviewed immunotherapy types, particularly immune checkpoint inhibitors, and the most common neuromuscular complications – primarily neuropathy, myasthenia gravis (MG), myositis, and encephalitis or meningitis.
“Timing of onset is a critical component to assist in identifying immune checkpoint inhibitor–associated versus non–immune checkpoint inhibitor–associated neuromuscular disease,” Dr. Trevino told attendees. Prompt recognition can be particularly urgent for MG because crisis and death rates are higher when induced by immunotherapy and require quick treatment. “Understanding the mechanisms of action sets a foundation for treatment approach,” he added.
Any part of the nervous system can be affected by immunotherapy toxicity, he said, and syndromes often overlap, with the peripheral nervous system typically more often affected than the central nervous system. Neurologic immune-related adverse events typically occur within four cycles of therapy – about 12 weeks after therapy initiation – but should always involve a work-up to exclude effects from the cancer itself, other neuromuscular diagnoses unrelated to therapy, and other toxicities from chemotherapy.
Recommended first-line treatment is halting immunotherapy with or without corticosteroids, after which most patients improve, often with “rapid, complete resolution of symptoms,” Dr. Trevino said. Restarting immunotherapy treatment is possible in some patients, though.
CAR T-cell and dendritic cell vaccine therapies
Four main types of immunotherapy exist: viral therapy, vaccine therapy, immune checkpoint inhibitors, and adoptive cell transfer, such as chimeric antigen receptor (CAR) T-cell therapy. Dr. Trevino focused on checkpoint inhibitors and adoptive cell transfer.
CAR T-cell therapy is a multistep treatment process that involves first removing blood from the patient to obtain their T cells. These are used to create and grow CAR T cells in the lab so that they can be infused back into the patient. The cells then bind to cancer cells and destroy them. Examples of approved CAR T-cell therapy include Yescarta (axicabtagene ciloleucel) for some types of non-Hodgkin lymphoma and Kymriah (tisagenlecleucel) for acute lymphoblastic leukemia (ALL).
Dendritic cell vaccines are similar to CAR T-cell therapy in that they also use the patient’s own immune cells to create cancer-killing cells that the patient then receives back. The only currently approved dendritic cell vaccine is Provenge (sipuleucel-T) for advanced prostate cancer.
The main toxicity to watch for from CAR T-cell therapy and dendritic cell vaccines is cytokine release syndrome (CRS). It can begin anywhere from 1-14 days after the infusion and involves T-cell expansion in the body that leads to a cytokine storm. Symptoms are wide ranging, including fatigue, fever, loss of appetite, tachycardia, hypotension, pain, rash, diarrhea, headache, confusion, seizures, muscle and joint pain, tachypnea, hypoxia and hallucinations, among others.
Specific central neurotoxicities that can result from CAR T-cell therapy include encephalopathy, cerebral edema, seizures and status epilepticus, cerebral vasospasm, and aphasia.
Immune checkpoint inhibitor toxicities
Immune checkpoint inhibitors are drugs that interrupt a cancer’s ability to hijack the immune system; they block the proteins that hold back T-cells from attacking the cancer, thereby releasing the immune system to go after the malignant cells.
The two most common types of immune checkpoint inhibitors are those targeting the programmed cell death protein 1 (PD-1) and programmed death-ligand 1 (PD-L1) pathways. The three currently approved PD-1 inhibitors are pembrolizumab (Keytruda), nivolumab (Opdivo), and cemiplimab (Libtayo), which can treat nearly a dozen malignancies affecting different organs. Atezolizumab (Tecentriq), avelumab (Bavencio), and durvalumab (Imfinzi) are the three currently approved PD-L1 inhibitors, indicated for urothelial carcinoma and a handful of other cancers, such as small-cell and non–small cell lung cancer and triple negative breast cancer.
The only other type of approved checkpoint inhibitor is ipilimumab (Yervoy), which targets the CTLA-4 protein. A number of other checkpoint inhibitors are in trials, however, such as ones targeting pathways involving OX40, ICOS, TIM3, and LAG-3 (J Hematol Oncol. 2018. doi: 10.1186/s13045-018-0582-8).
Immune-related adverse events are less common with PD-1 or PD-L1 inhibitors – a rate of 5%-10% – compared with adverse events from CTLA-4 inhibitors, which occur in about 15% of patients. Neurologic complications occur even more rarely – about 1%-4% of all immune checkpoint inhibitor therapies – and primarily include MG, Guillain-Barré syndrome (GBS), chronic inflammatory demyelinating polyneuropathy (CIDP), and inflammatory myositis (Muscle Nerve. 2018;58[1]:10-22).
Treatment with multiple checkpoint inhibitors increases the likelihood of severe adverse events, with rates of up to 30%-50% of patients with dual treatment.
Distinguishing features of neuromuscular immunotherapy-related adverse events
MG is the most common neuromuscular immune-related adverse event from immune checkpoint inhibitors and tends to occur 3-12 weeks after beginning treatment, frequently comorbid with inflammatory myopathy or cardiomyopathy, Dr. Trevino said. About two-thirds of cases are de novo, while the remaining one-third involve preexisting MG; no reports of Lambert-Eaton myasthenic syndrome have been linked to checkpoint inhibitors.
Several characteristics distinguish checkpoint inhibitor–associated MG from standard MG. Standard MG can be ocular with or without bulbar or appendicular weakness, whereas immunotherapy-related MG is rarely only ocular (about 18% of cases). Immunotherapy-related MG involves an MG crisis at diagnosis in up to 50% of cases and has high mortality, both of which are rarer with standard MG.
While standard MG can be seronegative or involve AChR, MuSK, or LRP4 antibodies, about two-thirds of immunotherapy-related MG cases are positive for AChR antibodies. LRP4 antibodies are rare with MG from checkpoint inhibitors, and no MuSK antibodies have been reported in these cases. Creatine kinase (CK) or troponin I (TnI) elevation occurs in about 87% of patients with checkpoint inhibitor-induced MG, but standard MG doesn’t typically involve increased CK levels.
Inflammatory myositis (IM), the second most common neuromuscular adverse event from immunotherapy, tends to occur 2-15 weeks after immune checkpoint inhibitor therapy and can involve polymyositis, necrotizing autoimmune myopathy, dermatomyositis, granulomatous myositis, or other nonspecific myositis and myopathies.
Though proximal weakness occurs with IM both associated with immunotherapy and not, ocular symptoms are unique to cases associated with therapy and occur in about half of them. Myalgia, dyspnea, and dysphagia can all occur with checkpoint inhibitor–associated IM but don’t generally occur with standard IM. Immunotherapy-related IM is usually seronegative for myositis antibodies and doesn’t generally cause abnormalities in electromyography, compared with increased exertional activity and early recruitment of myopathic motor units in electromyography with standard IM.
GBS and CIDP are the third most common cause of neuromuscular complications from checkpoint inhibitors. The main distinguishing feature of these conditions from those not related to immunotherapy is that they occur anywhere from 4 to 68 weeks after therapy begins. Presentation is otherwise similar whether related to checkpoint inhibitors or not.
Aside from GBS and CIDP, other neuropathies that can result from immunotherapy complications include acute cranial neuropathies, axonal or demyelinating neuropathies, motor polyradiculopathy, vasculitic neuropathy, and plexopathy.
Neuromuscular complications other than those described above can also occur from checkpoint inhibitor therapy, such as enteric neuropathy, polyradiculitis, and meningo-radiculo-neuritis, but these are much rarer.
Four organizations have developed consensus guidelines for immune checkpoint inhibitor toxicities: the European Society for Medical Oncology (ESMO, 2017), Society for Immunotherapy of Cancer (SITC, 2017), American Society of Clinical Oncology (ASCO, 2018), and National Comprehensive Cancer Network (NCCN, 2019).
Dr Trevino had no disclosures.
AUSTIN, TEX. – Neuromuscular complications from immunotherapy for cancer are rare, but they occur often enough that it is helpful to know which ones can result from different immunotherapies and how to distinguish them from non–adverse event conditions, according to Christopher Trevino, MD, a neuro-oncologist at Tulane University in New Orleans.
At the annual meeting of the American Association for Neuromuscular and Electrodiagnostic Medicine, Dr. Trevino reviewed immunotherapy types, particularly immune checkpoint inhibitors, and the most common neuromuscular complications – primarily neuropathy, myasthenia gravis (MG), myositis, and encephalitis or meningitis.
“Timing of onset is a critical component to assist in identifying immune checkpoint inhibitor–associated versus non–immune checkpoint inhibitor–associated neuromuscular disease,” Dr. Trevino told attendees. Prompt recognition can be particularly urgent for MG because crisis and death rates are higher when induced by immunotherapy and require quick treatment. “Understanding the mechanisms of action sets a foundation for treatment approach,” he added.
Any part of the nervous system can be affected by immunotherapy toxicity, he said, and syndromes often overlap, with the peripheral nervous system typically more often affected than the central nervous system. Neurologic immune-related adverse events typically occur within four cycles of therapy – about 12 weeks after therapy initiation – but should always involve a work-up to exclude effects from the cancer itself, other neuromuscular diagnoses unrelated to therapy, and other toxicities from chemotherapy.
Recommended first-line treatment is halting immunotherapy with or without corticosteroids, after which most patients improve, often with “rapid, complete resolution of symptoms,” Dr. Trevino said. Restarting immunotherapy treatment is possible in some patients, though.
CAR T-cell and dendritic cell vaccine therapies
Four main types of immunotherapy exist: viral therapy, vaccine therapy, immune checkpoint inhibitors, and adoptive cell transfer, such as chimeric antigen receptor (CAR) T-cell therapy. Dr. Trevino focused on checkpoint inhibitors and adoptive cell transfer.
CAR T-cell therapy is a multistep treatment process that involves first removing blood from the patient to obtain their T cells. These are used to create and grow CAR T cells in the lab so that they can be infused back into the patient. The cells then bind to cancer cells and destroy them. Examples of approved CAR T-cell therapy include Yescarta (axicabtagene ciloleucel) for some types of non-Hodgkin lymphoma and Kymriah (tisagenlecleucel) for acute lymphoblastic leukemia (ALL).
Dendritic cell vaccines are similar to CAR T-cell therapy in that they also use the patient’s own immune cells to create cancer-killing cells that the patient then receives back. The only currently approved dendritic cell vaccine is Provenge (sipuleucel-T) for advanced prostate cancer.
The main toxicity to watch for from CAR T-cell therapy and dendritic cell vaccines is cytokine release syndrome (CRS). It can begin anywhere from 1-14 days after the infusion and involves T-cell expansion in the body that leads to a cytokine storm. Symptoms are wide ranging, including fatigue, fever, loss of appetite, tachycardia, hypotension, pain, rash, diarrhea, headache, confusion, seizures, muscle and joint pain, tachypnea, hypoxia and hallucinations, among others.
Specific central neurotoxicities that can result from CAR T-cell therapy include encephalopathy, cerebral edema, seizures and status epilepticus, cerebral vasospasm, and aphasia.
Immune checkpoint inhibitor toxicities
Immune checkpoint inhibitors are drugs that interrupt a cancer’s ability to hijack the immune system; they block the proteins that hold back T-cells from attacking the cancer, thereby releasing the immune system to go after the malignant cells.
The two most common types of immune checkpoint inhibitors are those targeting the programmed cell death protein 1 (PD-1) and programmed death-ligand 1 (PD-L1) pathways. The three currently approved PD-1 inhibitors are pembrolizumab (Keytruda), nivolumab (Opdivo), and cemiplimab (Libtayo), which can treat nearly a dozen malignancies affecting different organs. Atezolizumab (Tecentriq), avelumab (Bavencio), and durvalumab (Imfinzi) are the three currently approved PD-L1 inhibitors, indicated for urothelial carcinoma and a handful of other cancers, such as small-cell and non–small cell lung cancer and triple negative breast cancer.
The only other type of approved checkpoint inhibitor is ipilimumab (Yervoy), which targets the CTLA-4 protein. A number of other checkpoint inhibitors are in trials, however, such as ones targeting pathways involving OX40, ICOS, TIM3, and LAG-3 (J Hematol Oncol. 2018. doi: 10.1186/s13045-018-0582-8).
Immune-related adverse events are less common with PD-1 or PD-L1 inhibitors – a rate of 5%-10% – compared with adverse events from CTLA-4 inhibitors, which occur in about 15% of patients. Neurologic complications occur even more rarely – about 1%-4% of all immune checkpoint inhibitor therapies – and primarily include MG, Guillain-Barré syndrome (GBS), chronic inflammatory demyelinating polyneuropathy (CIDP), and inflammatory myositis (Muscle Nerve. 2018;58[1]:10-22).
Treatment with multiple checkpoint inhibitors increases the likelihood of severe adverse events, with rates of up to 30%-50% of patients with dual treatment.
Distinguishing features of neuromuscular immunotherapy-related adverse events
MG is the most common neuromuscular immune-related adverse event from immune checkpoint inhibitors and tends to occur 3-12 weeks after beginning treatment, frequently comorbid with inflammatory myopathy or cardiomyopathy, Dr. Trevino said. About two-thirds of cases are de novo, while the remaining one-third involve preexisting MG; no reports of Lambert-Eaton myasthenic syndrome have been linked to checkpoint inhibitors.
Several characteristics distinguish checkpoint inhibitor–associated MG from standard MG. Standard MG can be ocular with or without bulbar or appendicular weakness, whereas immunotherapy-related MG is rarely only ocular (about 18% of cases). Immunotherapy-related MG involves an MG crisis at diagnosis in up to 50% of cases and has high mortality, both of which are rarer with standard MG.
While standard MG can be seronegative or involve AChR, MuSK, or LRP4 antibodies, about two-thirds of immunotherapy-related MG cases are positive for AChR antibodies. LRP4 antibodies are rare with MG from checkpoint inhibitors, and no MuSK antibodies have been reported in these cases. Creatine kinase (CK) or troponin I (TnI) elevation occurs in about 87% of patients with checkpoint inhibitor-induced MG, but standard MG doesn’t typically involve increased CK levels.
Inflammatory myositis (IM), the second most common neuromuscular adverse event from immunotherapy, tends to occur 2-15 weeks after immune checkpoint inhibitor therapy and can involve polymyositis, necrotizing autoimmune myopathy, dermatomyositis, granulomatous myositis, or other nonspecific myositis and myopathies.
Though proximal weakness occurs with IM both associated with immunotherapy and not, ocular symptoms are unique to cases associated with therapy and occur in about half of them. Myalgia, dyspnea, and dysphagia can all occur with checkpoint inhibitor–associated IM but don’t generally occur with standard IM. Immunotherapy-related IM is usually seronegative for myositis antibodies and doesn’t generally cause abnormalities in electromyography, compared with increased exertional activity and early recruitment of myopathic motor units in electromyography with standard IM.
GBS and CIDP are the third most common cause of neuromuscular complications from checkpoint inhibitors. The main distinguishing feature of these conditions from those not related to immunotherapy is that they occur anywhere from 4 to 68 weeks after therapy begins. Presentation is otherwise similar whether related to checkpoint inhibitors or not.
Aside from GBS and CIDP, other neuropathies that can result from immunotherapy complications include acute cranial neuropathies, axonal or demyelinating neuropathies, motor polyradiculopathy, vasculitic neuropathy, and plexopathy.
Neuromuscular complications other than those described above can also occur from checkpoint inhibitor therapy, such as enteric neuropathy, polyradiculitis, and meningo-radiculo-neuritis, but these are much rarer.
Four organizations have developed consensus guidelines for immune checkpoint inhibitor toxicities: the European Society for Medical Oncology (ESMO, 2017), Society for Immunotherapy of Cancer (SITC, 2017), American Society of Clinical Oncology (ASCO, 2018), and National Comprehensive Cancer Network (NCCN, 2019).
Dr Trevino had no disclosures.
EXPERT ANALYSIS FROM AANEM 2019
Helping adolescents get enough quality sleep
NEW ORLEANS – Social media and electronics aren’t the only barriers to a good night’s sleep for teens, according to Adiaha I. A. Spinks-Franklin, MD, MPH, a pediatrician at Texas Children’s Hospital in Houston.
Another half-dozen “sleep enemies” interfere with adolescents’ sleep and can contribute to insomnia or other sleep disorders, she told attendees at the annual meeting of the American Academy of Pediatrics.
Knowing what normal sleep physiology looks like in youth and understanding the most common sleep enemies and sleep-behavior problems can help you use effective interventions to help your patients get the sleep they need, she said.
Infants need the most sleep, about 12-16 hours each 24-hour period, including naps, for those aged 4-12 months. As they grow into toddlerhood and preschool age, children gradually need less: Children aged 1-2 years need 11-14 hours and children aged 3-5 years need 10-13 hours, including naps. By the time children are in school, ages 6-12, they should have dropped their naps and need 9-12 hours a night.
In fact, 75% of high school seniors get less than 8 hours of sleep a day and live with a chronic sleep debt, Dr. Spinks-Franklin said.
Although social media use and electronics in the bedroom – TVs, computers, cell phones, and video games – can certainly contribute to inadequate sleep, a heavy academic load and extracurricular activities can be just as problematic, Dr. Spinks-Franklin said. Teens who work after school also may have difficulty getting enough sleep, especially if they also have to balance a heavier academic load or even one or two extracurricular activities.
Socializing with friends also can interfere with sleep, especially when get-togethers run late; drinking caffeinated drinks in the afternoon onward can make it difficult for adolescents to get the sleep they need as well. Less-modifiable contributors to too little sleep are stress and early school start times, Dr. Spinks-Franklin said.
The two most common sleep problems seen in teens are insomnia and delayed sleep phase syndrome. Addressing these is important because the effects of chronic insufficient sleep can have far-reaching consequences. Obesity and related chronic health conditions are associated with inadequate sleep, as are poor academic performance, poor judgment, poor executive functioning, and mental health disorders like depression.
Short-term effects of insufficient sleep also can be problematic and can exacerbate existing sleep problems, such as sleeping in on the weekends to “catch up” on sleep or drinking more caffeine to try to stay awake during the day. Increased caffeine intake can interfere with non-REM deep sleep, Dr. Spinks-Franklin said, and therefore reduce the quality of sleep even if the person gets the total hours they need.
Insomnia in adolescents
Insomnia can refer to difficulty falling asleep, staying asleep, sleeping for long enough, or getting enough sleep in one period of time even when the opportunity is there. Some people may have no trouble falling asleep, but they wake up too early – before they have had gotten the sleep they need – and cannot return to sleep.
To be insomnia, the problem must occur “despite having enough time available for sleep,” Dr. Spinks-Franklin said. “Patient who restrict the amount of time for sleep due to work or social commitments may have trouble sleeping and daytime sleepiness but do not have insomnia.”
Daytime impairment also is part of the American Academy of Sleep Medicine’s definition of insomnia. The rare teen who doesn’t need as much sleep as average and functions without difficulty during the day does not necessarily have insomnia.
But the impairment may not necessarily just be fatigue or sleepiness. In fact, many of the symptoms are the same as those seen with ADHD.
Daytime consequences of insomnia can include the following:
- Depression, feeling sad or “blue,” or emotional hypersensitivity.
- Mood swings, crankiness, or irritability.
- Difficulty concentrating or paying attention, poor memory, mind wandering, or even inability to sit still.
- Job or school problems, such as not being able to finish homework, not finishing tasks they start, or forgetfulness.
- Difficulty in social situations, such as discomfort with others or problems with friends.
- Daytime sleepiness, even when unable to actually take a nap.
- Behavioral problems, such as hyperactivity, impulsivity, or aggression.
- Frequent mistakes, especially at work, at school, or while driving (often “errors of omission,” such as not seeing a street sign or not hearing an instruction).
- Lower levels of motivation or initiative, feeling less energetic.
- Excessive worry about sleep.
Evaluation of insomnia can be framed with “the three-factor model,” which includes predisposing factors, precipitating factors, and perpetuating factors.
Predisposing factors – those that indicate a person already may be at risk for insomnia – include potential genetic influences as well as their typical response to stress. “Do they sleep more or less?” Dr. Spinks-Franklin said. Even teens predisposed to insomnia may not develop it, however, without a precipitating trigger.
These triggers could include stress, anxiety, poor initial sleep hygiene that becomes a pattern, dietary intake or behaviors (such as drinking caffeine or eating too much or too late in the evening), changes to their schedule, or side effects of medications.
Once insomnia begins, various factors can then perpetuate the cycle, including some of those that triggered it, such as anxiety or a school or work schedule. Sometimes it can be difficult to pinpoint the factor prolonging insomnia, such as the unconscious reward of going to work or school late with few or no consequences.
Delayed sleep phase syndrome
Delayed sleep phase syndrome occurs when someone has a delayed onset of melatonin secretion that pushes back the time when they can fall asleep. Melatonin is the neurotransmitter produced by the pineal gland that signals the start of nighttime. Although it has a hereditary component, delayed sleep phase syndrome also can result from a pattern of poor sleep onset and sleeping in on the weekends.
Dr. Spinks-Franklin described the typical cycle: A teen doesn’t go to sleep until after midnight and then wants to sleep in later in the morning. Because they have to wake up early for school, they sleep in on the weekends to try to regain the sleep they lost. Sleeping in pushes their circadian rhythm even later, perpetuating the problem.
Interventions for sleep disorders
The recommended treatment for insomnia is cognitive-behavior therapy for insomnia, for which strong evidence exists. Before seeking cognitive-behavior therapy, however, families can work to improve sleep hygiene and reduce stimuli that contribute to insomnia.
Teens should avoid screens for at least 1 hour before bedtime and avoid caffeine and exercise for at least 4 hours before going to bed. They also need to develop a schedule with a consistent bedtime and wake-up time, including on the weekends. They should avoid sleeping in on the weekends or taking naps during the day, Dr. Spinks-Franklin said.
Delayed sleep phase syndrome is more resistant to treatment and has a high recurrence rate, she said, and it requires commitment from the parent and their child to address it successfully. Teens with this condition also can start with sleep hygiene practices: a consistent wake-up time that they maintain on the weekends and no daytime naps. Phototherapy in the morning can be added to hopefully induce an earlier onset of melatonin release in the evening.
The next step is making changes to the youth’s schedule, particularly evening and/or weekend activities. They can try to gradually advance their biological clock by changing their sleep schedule.
Dr. Spinks-Franklin also briefly addressed the use of over-the-counter melatonin supplements for treating sleep problems. Melatonin can be effective for treating insomnia by improving sleep onset and sleep quality, particularly in children and teens with autism spectrum disorder or ADHD.
Dr. Spinks-Franklin had no disclosures, and her presentation used no outside funding.
NEW ORLEANS – Social media and electronics aren’t the only barriers to a good night’s sleep for teens, according to Adiaha I. A. Spinks-Franklin, MD, MPH, a pediatrician at Texas Children’s Hospital in Houston.
Another half-dozen “sleep enemies” interfere with adolescents’ sleep and can contribute to insomnia or other sleep disorders, she told attendees at the annual meeting of the American Academy of Pediatrics.
Knowing what normal sleep physiology looks like in youth and understanding the most common sleep enemies and sleep-behavior problems can help you use effective interventions to help your patients get the sleep they need, she said.
Infants need the most sleep, about 12-16 hours each 24-hour period, including naps, for those aged 4-12 months. As they grow into toddlerhood and preschool age, children gradually need less: Children aged 1-2 years need 11-14 hours and children aged 3-5 years need 10-13 hours, including naps. By the time children are in school, ages 6-12, they should have dropped their naps and need 9-12 hours a night.
In fact, 75% of high school seniors get less than 8 hours of sleep a day and live with a chronic sleep debt, Dr. Spinks-Franklin said.
Although social media use and electronics in the bedroom – TVs, computers, cell phones, and video games – can certainly contribute to inadequate sleep, a heavy academic load and extracurricular activities can be just as problematic, Dr. Spinks-Franklin said. Teens who work after school also may have difficulty getting enough sleep, especially if they also have to balance a heavier academic load or even one or two extracurricular activities.
Socializing with friends also can interfere with sleep, especially when get-togethers run late; drinking caffeinated drinks in the afternoon onward can make it difficult for adolescents to get the sleep they need as well. Less-modifiable contributors to too little sleep are stress and early school start times, Dr. Spinks-Franklin said.
The two most common sleep problems seen in teens are insomnia and delayed sleep phase syndrome. Addressing these is important because the effects of chronic insufficient sleep can have far-reaching consequences. Obesity and related chronic health conditions are associated with inadequate sleep, as are poor academic performance, poor judgment, poor executive functioning, and mental health disorders like depression.
Short-term effects of insufficient sleep also can be problematic and can exacerbate existing sleep problems, such as sleeping in on the weekends to “catch up” on sleep or drinking more caffeine to try to stay awake during the day. Increased caffeine intake can interfere with non-REM deep sleep, Dr. Spinks-Franklin said, and therefore reduce the quality of sleep even if the person gets the total hours they need.
Insomnia in adolescents
Insomnia can refer to difficulty falling asleep, staying asleep, sleeping for long enough, or getting enough sleep in one period of time even when the opportunity is there. Some people may have no trouble falling asleep, but they wake up too early – before they have had gotten the sleep they need – and cannot return to sleep.
To be insomnia, the problem must occur “despite having enough time available for sleep,” Dr. Spinks-Franklin said. “Patient who restrict the amount of time for sleep due to work or social commitments may have trouble sleeping and daytime sleepiness but do not have insomnia.”
Daytime impairment also is part of the American Academy of Sleep Medicine’s definition of insomnia. The rare teen who doesn’t need as much sleep as average and functions without difficulty during the day does not necessarily have insomnia.
But the impairment may not necessarily just be fatigue or sleepiness. In fact, many of the symptoms are the same as those seen with ADHD.
Daytime consequences of insomnia can include the following:
- Depression, feeling sad or “blue,” or emotional hypersensitivity.
- Mood swings, crankiness, or irritability.
- Difficulty concentrating or paying attention, poor memory, mind wandering, or even inability to sit still.
- Job or school problems, such as not being able to finish homework, not finishing tasks they start, or forgetfulness.
- Difficulty in social situations, such as discomfort with others or problems with friends.
- Daytime sleepiness, even when unable to actually take a nap.
- Behavioral problems, such as hyperactivity, impulsivity, or aggression.
- Frequent mistakes, especially at work, at school, or while driving (often “errors of omission,” such as not seeing a street sign or not hearing an instruction).
- Lower levels of motivation or initiative, feeling less energetic.
- Excessive worry about sleep.
Evaluation of insomnia can be framed with “the three-factor model,” which includes predisposing factors, precipitating factors, and perpetuating factors.
Predisposing factors – those that indicate a person already may be at risk for insomnia – include potential genetic influences as well as their typical response to stress. “Do they sleep more or less?” Dr. Spinks-Franklin said. Even teens predisposed to insomnia may not develop it, however, without a precipitating trigger.
These triggers could include stress, anxiety, poor initial sleep hygiene that becomes a pattern, dietary intake or behaviors (such as drinking caffeine or eating too much or too late in the evening), changes to their schedule, or side effects of medications.
Once insomnia begins, various factors can then perpetuate the cycle, including some of those that triggered it, such as anxiety or a school or work schedule. Sometimes it can be difficult to pinpoint the factor prolonging insomnia, such as the unconscious reward of going to work or school late with few or no consequences.
Delayed sleep phase syndrome
Delayed sleep phase syndrome occurs when someone has a delayed onset of melatonin secretion that pushes back the time when they can fall asleep. Melatonin is the neurotransmitter produced by the pineal gland that signals the start of nighttime. Although it has a hereditary component, delayed sleep phase syndrome also can result from a pattern of poor sleep onset and sleeping in on the weekends.
Dr. Spinks-Franklin described the typical cycle: A teen doesn’t go to sleep until after midnight and then wants to sleep in later in the morning. Because they have to wake up early for school, they sleep in on the weekends to try to regain the sleep they lost. Sleeping in pushes their circadian rhythm even later, perpetuating the problem.
Interventions for sleep disorders
The recommended treatment for insomnia is cognitive-behavior therapy for insomnia, for which strong evidence exists. Before seeking cognitive-behavior therapy, however, families can work to improve sleep hygiene and reduce stimuli that contribute to insomnia.
Teens should avoid screens for at least 1 hour before bedtime and avoid caffeine and exercise for at least 4 hours before going to bed. They also need to develop a schedule with a consistent bedtime and wake-up time, including on the weekends. They should avoid sleeping in on the weekends or taking naps during the day, Dr. Spinks-Franklin said.
Delayed sleep phase syndrome is more resistant to treatment and has a high recurrence rate, she said, and it requires commitment from the parent and their child to address it successfully. Teens with this condition also can start with sleep hygiene practices: a consistent wake-up time that they maintain on the weekends and no daytime naps. Phototherapy in the morning can be added to hopefully induce an earlier onset of melatonin release in the evening.
The next step is making changes to the youth’s schedule, particularly evening and/or weekend activities. They can try to gradually advance their biological clock by changing their sleep schedule.
Dr. Spinks-Franklin also briefly addressed the use of over-the-counter melatonin supplements for treating sleep problems. Melatonin can be effective for treating insomnia by improving sleep onset and sleep quality, particularly in children and teens with autism spectrum disorder or ADHD.
Dr. Spinks-Franklin had no disclosures, and her presentation used no outside funding.
NEW ORLEANS – Social media and electronics aren’t the only barriers to a good night’s sleep for teens, according to Adiaha I. A. Spinks-Franklin, MD, MPH, a pediatrician at Texas Children’s Hospital in Houston.
Another half-dozen “sleep enemies” interfere with adolescents’ sleep and can contribute to insomnia or other sleep disorders, she told attendees at the annual meeting of the American Academy of Pediatrics.
Knowing what normal sleep physiology looks like in youth and understanding the most common sleep enemies and sleep-behavior problems can help you use effective interventions to help your patients get the sleep they need, she said.
Infants need the most sleep, about 12-16 hours each 24-hour period, including naps, for those aged 4-12 months. As they grow into toddlerhood and preschool age, children gradually need less: Children aged 1-2 years need 11-14 hours and children aged 3-5 years need 10-13 hours, including naps. By the time children are in school, ages 6-12, they should have dropped their naps and need 9-12 hours a night.
In fact, 75% of high school seniors get less than 8 hours of sleep a day and live with a chronic sleep debt, Dr. Spinks-Franklin said.
Although social media use and electronics in the bedroom – TVs, computers, cell phones, and video games – can certainly contribute to inadequate sleep, a heavy academic load and extracurricular activities can be just as problematic, Dr. Spinks-Franklin said. Teens who work after school also may have difficulty getting enough sleep, especially if they also have to balance a heavier academic load or even one or two extracurricular activities.
Socializing with friends also can interfere with sleep, especially when get-togethers run late; drinking caffeinated drinks in the afternoon onward can make it difficult for adolescents to get the sleep they need as well. Less-modifiable contributors to too little sleep are stress and early school start times, Dr. Spinks-Franklin said.
The two most common sleep problems seen in teens are insomnia and delayed sleep phase syndrome. Addressing these is important because the effects of chronic insufficient sleep can have far-reaching consequences. Obesity and related chronic health conditions are associated with inadequate sleep, as are poor academic performance, poor judgment, poor executive functioning, and mental health disorders like depression.
Short-term effects of insufficient sleep also can be problematic and can exacerbate existing sleep problems, such as sleeping in on the weekends to “catch up” on sleep or drinking more caffeine to try to stay awake during the day. Increased caffeine intake can interfere with non-REM deep sleep, Dr. Spinks-Franklin said, and therefore reduce the quality of sleep even if the person gets the total hours they need.
Insomnia in adolescents
Insomnia can refer to difficulty falling asleep, staying asleep, sleeping for long enough, or getting enough sleep in one period of time even when the opportunity is there. Some people may have no trouble falling asleep, but they wake up too early – before they have had gotten the sleep they need – and cannot return to sleep.
To be insomnia, the problem must occur “despite having enough time available for sleep,” Dr. Spinks-Franklin said. “Patient who restrict the amount of time for sleep due to work or social commitments may have trouble sleeping and daytime sleepiness but do not have insomnia.”
Daytime impairment also is part of the American Academy of Sleep Medicine’s definition of insomnia. The rare teen who doesn’t need as much sleep as average and functions without difficulty during the day does not necessarily have insomnia.
But the impairment may not necessarily just be fatigue or sleepiness. In fact, many of the symptoms are the same as those seen with ADHD.
Daytime consequences of insomnia can include the following:
- Depression, feeling sad or “blue,” or emotional hypersensitivity.
- Mood swings, crankiness, or irritability.
- Difficulty concentrating or paying attention, poor memory, mind wandering, or even inability to sit still.
- Job or school problems, such as not being able to finish homework, not finishing tasks they start, or forgetfulness.
- Difficulty in social situations, such as discomfort with others or problems with friends.
- Daytime sleepiness, even when unable to actually take a nap.
- Behavioral problems, such as hyperactivity, impulsivity, or aggression.
- Frequent mistakes, especially at work, at school, or while driving (often “errors of omission,” such as not seeing a street sign or not hearing an instruction).
- Lower levels of motivation or initiative, feeling less energetic.
- Excessive worry about sleep.
Evaluation of insomnia can be framed with “the three-factor model,” which includes predisposing factors, precipitating factors, and perpetuating factors.
Predisposing factors – those that indicate a person already may be at risk for insomnia – include potential genetic influences as well as their typical response to stress. “Do they sleep more or less?” Dr. Spinks-Franklin said. Even teens predisposed to insomnia may not develop it, however, without a precipitating trigger.
These triggers could include stress, anxiety, poor initial sleep hygiene that becomes a pattern, dietary intake or behaviors (such as drinking caffeine or eating too much or too late in the evening), changes to their schedule, or side effects of medications.
Once insomnia begins, various factors can then perpetuate the cycle, including some of those that triggered it, such as anxiety or a school or work schedule. Sometimes it can be difficult to pinpoint the factor prolonging insomnia, such as the unconscious reward of going to work or school late with few or no consequences.
Delayed sleep phase syndrome
Delayed sleep phase syndrome occurs when someone has a delayed onset of melatonin secretion that pushes back the time when they can fall asleep. Melatonin is the neurotransmitter produced by the pineal gland that signals the start of nighttime. Although it has a hereditary component, delayed sleep phase syndrome also can result from a pattern of poor sleep onset and sleeping in on the weekends.
Dr. Spinks-Franklin described the typical cycle: A teen doesn’t go to sleep until after midnight and then wants to sleep in later in the morning. Because they have to wake up early for school, they sleep in on the weekends to try to regain the sleep they lost. Sleeping in pushes their circadian rhythm even later, perpetuating the problem.
Interventions for sleep disorders
The recommended treatment for insomnia is cognitive-behavior therapy for insomnia, for which strong evidence exists. Before seeking cognitive-behavior therapy, however, families can work to improve sleep hygiene and reduce stimuli that contribute to insomnia.
Teens should avoid screens for at least 1 hour before bedtime and avoid caffeine and exercise for at least 4 hours before going to bed. They also need to develop a schedule with a consistent bedtime and wake-up time, including on the weekends. They should avoid sleeping in on the weekends or taking naps during the day, Dr. Spinks-Franklin said.
Delayed sleep phase syndrome is more resistant to treatment and has a high recurrence rate, she said, and it requires commitment from the parent and their child to address it successfully. Teens with this condition also can start with sleep hygiene practices: a consistent wake-up time that they maintain on the weekends and no daytime naps. Phototherapy in the morning can be added to hopefully induce an earlier onset of melatonin release in the evening.
The next step is making changes to the youth’s schedule, particularly evening and/or weekend activities. They can try to gradually advance their biological clock by changing their sleep schedule.
Dr. Spinks-Franklin also briefly addressed the use of over-the-counter melatonin supplements for treating sleep problems. Melatonin can be effective for treating insomnia by improving sleep onset and sleep quality, particularly in children and teens with autism spectrum disorder or ADHD.
Dr. Spinks-Franklin had no disclosures, and her presentation used no outside funding.
EXPERT ANALYSIS FROM AAP 19
Ataluren shows real-world benefit for nonsense mutation Duchenne muscular dystrophy
AUSTIN, TEX. – , according to new data.
“Participants in the STRIDE Registry [real-world patients] showed a reduction in functional decline over 48 weeks, compared with patients receiving placebo” in the trial, reported Abdallah Delage of PTC Therapeutics in Zug, Switzerland, and his associates.
Duchenne muscular dystrophy affects an estimated 1 in 3,600-6,000 male births globally, about 10%-15% of whom have nonsense mutation DMD. This mutation causes a truncated, nonfunctional dystrophin protein due to a premature stop codon, the authors explained. Ataluren “promotes ribosomal read-through of the premature stop codon to produce a full-length dystrophin protein,” they explained.
Ataluren is currently approved for ambulatory patients age 2 and older with nonsense mutation DMD in the European Union and several other European countries. Israel, Korea, Chile, and Ukraine have approved it for patients aged 5 and older.
The Strategic Targeting of Registries and International Database of Excellence (STRIDE) Registry contains real-world data from patients using ataluren as part of an ongoing multicenter observational postapproval safety study. The investigators are tracking patients for at least 5 years after enrollment in 14 countries where ataluren is approved or commercially available through early-access programs. Patients take 40 mg/kg daily: 10 mg/kg in the morning, 10 mg/kg midday, and 20 mg/kg in the evening.
The researchers compared outcomes in 216 patients in the STRIDE Registry with participants in a randomized controlled phase 3 study of ataluren involving 228 boys, aged 7-16, who received ataluren (n = 114) or placebo (n = 114) for 48 weeks. Patients were an average 9 years old in STRIDE and in both arms of the randomized controlled trial.
The STRIDE Registry participants, comprising 184 ambulatory and 26 nonambulatory patients at enrollment, had at least 48 weeks between their first and last assessment. All of the patients in the phase 3 study and 88.6% of the STRIDE Registry patients were receiving corticosteroids along with ataluren. The researchers compared the 184 ambulatory STRIDE participants with the participants of the randomized controlled trial for one primary and four secondary endpoints from baseline to 48 weeks.
For the primary endpoint, 6-minute walk distance, average distance was 35 meters shorter than baseline in STRIDE Registry participants (n = 66), 42.2 meters shorter in the patients receiving ataluren in the phase 3 study (n = 109), and 57.6 meters shorter in RCT patients receiving placebo in the phase 3 trial (n = 109).
A secondary endpoint, the time it took patients to walk or run 10 meters, increased 1.6 seconds from baseline to 48 weeks in STRIDE Registry participants (n = 61), 2.3 seconds in participants receiving ataluren in the phase 3 trial (n = 109), and 3.5 seconds in study participants receiving placebo (n = 110).
Another secondary endpoint, the change in time it took for patients to stand from supine position from baseline to 48 weeks, was 2.9 additional seconds for STRIDE participants (n = 55), 3.8 additional seconds in study participants receiving ataluren (n = 101), and 3.9 additional seconds in study participants receiving placebo (n = 96).
Two final secondary endpoints were the changes in time to climb four stairs and to descend four stairs from baseline to 48 weeks. STRIDE participants (n = 47) climbed four stairs 1.2 seconds more slowly at 48 weeks, compared with 2.7 seconds more slowly in the participants who received ataluren in the phase 3 trial (n = 105) and 4.5 seconds more slowly in those who received placebo. Descending four stairs took 0.5 more seconds at 48 weeks in STRIDE participants (n = 40), 2.2 more seconds in participants who received ataluren in the phase 3 trial (n = 106), and 4.0 more seconds in those who received placebo (n = 100).
At least one adverse event occurred in 20.7% of registry participants; seven of these were considered treatment related. Treatment-related side effects included abdominal pain, vomiting, headache, stomach ache, diarrhea, and increased serum lipids.
The study and STRIDE Registry is funded by PTC Therapeutics with TREAT-NMD and the Cooperative International Neuromuscular Research Group. Mr. Delage and five other authors are employees of PTC Therapeutics, and six authors had received speaker or consultancy fees or served on the advisory board of a variety of companies.
SOURCE: Delage A et al. AANEM 2019, Abstract 115.
AUSTIN, TEX. – , according to new data.
“Participants in the STRIDE Registry [real-world patients] showed a reduction in functional decline over 48 weeks, compared with patients receiving placebo” in the trial, reported Abdallah Delage of PTC Therapeutics in Zug, Switzerland, and his associates.
Duchenne muscular dystrophy affects an estimated 1 in 3,600-6,000 male births globally, about 10%-15% of whom have nonsense mutation DMD. This mutation causes a truncated, nonfunctional dystrophin protein due to a premature stop codon, the authors explained. Ataluren “promotes ribosomal read-through of the premature stop codon to produce a full-length dystrophin protein,” they explained.
Ataluren is currently approved for ambulatory patients age 2 and older with nonsense mutation DMD in the European Union and several other European countries. Israel, Korea, Chile, and Ukraine have approved it for patients aged 5 and older.
The Strategic Targeting of Registries and International Database of Excellence (STRIDE) Registry contains real-world data from patients using ataluren as part of an ongoing multicenter observational postapproval safety study. The investigators are tracking patients for at least 5 years after enrollment in 14 countries where ataluren is approved or commercially available through early-access programs. Patients take 40 mg/kg daily: 10 mg/kg in the morning, 10 mg/kg midday, and 20 mg/kg in the evening.
The researchers compared outcomes in 216 patients in the STRIDE Registry with participants in a randomized controlled phase 3 study of ataluren involving 228 boys, aged 7-16, who received ataluren (n = 114) or placebo (n = 114) for 48 weeks. Patients were an average 9 years old in STRIDE and in both arms of the randomized controlled trial.
The STRIDE Registry participants, comprising 184 ambulatory and 26 nonambulatory patients at enrollment, had at least 48 weeks between their first and last assessment. All of the patients in the phase 3 study and 88.6% of the STRIDE Registry patients were receiving corticosteroids along with ataluren. The researchers compared the 184 ambulatory STRIDE participants with the participants of the randomized controlled trial for one primary and four secondary endpoints from baseline to 48 weeks.
For the primary endpoint, 6-minute walk distance, average distance was 35 meters shorter than baseline in STRIDE Registry participants (n = 66), 42.2 meters shorter in the patients receiving ataluren in the phase 3 study (n = 109), and 57.6 meters shorter in RCT patients receiving placebo in the phase 3 trial (n = 109).
A secondary endpoint, the time it took patients to walk or run 10 meters, increased 1.6 seconds from baseline to 48 weeks in STRIDE Registry participants (n = 61), 2.3 seconds in participants receiving ataluren in the phase 3 trial (n = 109), and 3.5 seconds in study participants receiving placebo (n = 110).
Another secondary endpoint, the change in time it took for patients to stand from supine position from baseline to 48 weeks, was 2.9 additional seconds for STRIDE participants (n = 55), 3.8 additional seconds in study participants receiving ataluren (n = 101), and 3.9 additional seconds in study participants receiving placebo (n = 96).
Two final secondary endpoints were the changes in time to climb four stairs and to descend four stairs from baseline to 48 weeks. STRIDE participants (n = 47) climbed four stairs 1.2 seconds more slowly at 48 weeks, compared with 2.7 seconds more slowly in the participants who received ataluren in the phase 3 trial (n = 105) and 4.5 seconds more slowly in those who received placebo. Descending four stairs took 0.5 more seconds at 48 weeks in STRIDE participants (n = 40), 2.2 more seconds in participants who received ataluren in the phase 3 trial (n = 106), and 4.0 more seconds in those who received placebo (n = 100).
At least one adverse event occurred in 20.7% of registry participants; seven of these were considered treatment related. Treatment-related side effects included abdominal pain, vomiting, headache, stomach ache, diarrhea, and increased serum lipids.
The study and STRIDE Registry is funded by PTC Therapeutics with TREAT-NMD and the Cooperative International Neuromuscular Research Group. Mr. Delage and five other authors are employees of PTC Therapeutics, and six authors had received speaker or consultancy fees or served on the advisory board of a variety of companies.
SOURCE: Delage A et al. AANEM 2019, Abstract 115.
AUSTIN, TEX. – , according to new data.
“Participants in the STRIDE Registry [real-world patients] showed a reduction in functional decline over 48 weeks, compared with patients receiving placebo” in the trial, reported Abdallah Delage of PTC Therapeutics in Zug, Switzerland, and his associates.
Duchenne muscular dystrophy affects an estimated 1 in 3,600-6,000 male births globally, about 10%-15% of whom have nonsense mutation DMD. This mutation causes a truncated, nonfunctional dystrophin protein due to a premature stop codon, the authors explained. Ataluren “promotes ribosomal read-through of the premature stop codon to produce a full-length dystrophin protein,” they explained.
Ataluren is currently approved for ambulatory patients age 2 and older with nonsense mutation DMD in the European Union and several other European countries. Israel, Korea, Chile, and Ukraine have approved it for patients aged 5 and older.
The Strategic Targeting of Registries and International Database of Excellence (STRIDE) Registry contains real-world data from patients using ataluren as part of an ongoing multicenter observational postapproval safety study. The investigators are tracking patients for at least 5 years after enrollment in 14 countries where ataluren is approved or commercially available through early-access programs. Patients take 40 mg/kg daily: 10 mg/kg in the morning, 10 mg/kg midday, and 20 mg/kg in the evening.
The researchers compared outcomes in 216 patients in the STRIDE Registry with participants in a randomized controlled phase 3 study of ataluren involving 228 boys, aged 7-16, who received ataluren (n = 114) or placebo (n = 114) for 48 weeks. Patients were an average 9 years old in STRIDE and in both arms of the randomized controlled trial.
The STRIDE Registry participants, comprising 184 ambulatory and 26 nonambulatory patients at enrollment, had at least 48 weeks between their first and last assessment. All of the patients in the phase 3 study and 88.6% of the STRIDE Registry patients were receiving corticosteroids along with ataluren. The researchers compared the 184 ambulatory STRIDE participants with the participants of the randomized controlled trial for one primary and four secondary endpoints from baseline to 48 weeks.
For the primary endpoint, 6-minute walk distance, average distance was 35 meters shorter than baseline in STRIDE Registry participants (n = 66), 42.2 meters shorter in the patients receiving ataluren in the phase 3 study (n = 109), and 57.6 meters shorter in RCT patients receiving placebo in the phase 3 trial (n = 109).
A secondary endpoint, the time it took patients to walk or run 10 meters, increased 1.6 seconds from baseline to 48 weeks in STRIDE Registry participants (n = 61), 2.3 seconds in participants receiving ataluren in the phase 3 trial (n = 109), and 3.5 seconds in study participants receiving placebo (n = 110).
Another secondary endpoint, the change in time it took for patients to stand from supine position from baseline to 48 weeks, was 2.9 additional seconds for STRIDE participants (n = 55), 3.8 additional seconds in study participants receiving ataluren (n = 101), and 3.9 additional seconds in study participants receiving placebo (n = 96).
Two final secondary endpoints were the changes in time to climb four stairs and to descend four stairs from baseline to 48 weeks. STRIDE participants (n = 47) climbed four stairs 1.2 seconds more slowly at 48 weeks, compared with 2.7 seconds more slowly in the participants who received ataluren in the phase 3 trial (n = 105) and 4.5 seconds more slowly in those who received placebo. Descending four stairs took 0.5 more seconds at 48 weeks in STRIDE participants (n = 40), 2.2 more seconds in participants who received ataluren in the phase 3 trial (n = 106), and 4.0 more seconds in those who received placebo (n = 100).
At least one adverse event occurred in 20.7% of registry participants; seven of these were considered treatment related. Treatment-related side effects included abdominal pain, vomiting, headache, stomach ache, diarrhea, and increased serum lipids.
The study and STRIDE Registry is funded by PTC Therapeutics with TREAT-NMD and the Cooperative International Neuromuscular Research Group. Mr. Delage and five other authors are employees of PTC Therapeutics, and six authors had received speaker or consultancy fees or served on the advisory board of a variety of companies.
SOURCE: Delage A et al. AANEM 2019, Abstract 115.
REPORTING FROM AANEM 2019
Thromboembolic events more likely among CIDP patients with CVAD
AUSTIN, TEX. – Patients with chronic inflammatory demyelinating polyneuropathy (CIDP) who receive intravenous immunoglobulin (IVIg) appear to have an increased risk of thromboembolic events if it is administered with a central venous access device (CVAD) when compared against those without a CVAD, according to a recent study.
Although CVADs can reliably deliver IVIg, they also represent an established risk factor for thromboembolic events, Ami Patel, PhD, a senior epidemiologist at CSL Behring, and colleagues noted on their poster at the annual meeting of the American Association for Neuromuscular and Electrodiagnostic Medicine.
The results suggest a need for physicians to be vigilant about patients’ potential risk factors for thromboembolic events, Dr. Patel said in an interview. Further research is planned, however, because the current study did not control for other risk factors or explore other possible confounding, she said.
Dr. Patel and her associates analyzed U.S. claims data (IBM/Truven MarketScan) from 2006 to 2018 and included all patients with a CIDP diagnosis claim and a postdiagnosis code for IVIg. A code for CVAD up to 2 months before CIDP diagnosis without removal before IVIg treatment ended determined those with CVAD exposure, and thromboembolic events included any codes related to arterial, venous, or vascular prostheses.
The researchers then compared patients in a case-control fashion, matching each one with a CVAD to five patients of similar demographics without a CVAD. Characteristics used for matching included medical insurance type, prescription data availability, sex, age, geographic region, and years enrolled in the database.
Among 7,447 patients with at least one IVIg claim, 11.8% (n = 882) had CVAD exposure and 88.2% (n = 6,565) did not. Of those without a CVAD, 3,642 patients were matched to patients with CVAD. A quarter (25.4%) of patients with a CVAD had a thromboembolic event, compared with 11.2% of matched patients without CVADs (P less than .0001).
In the year leading up to IVIg therapy, 16.9% of those with a CVAD and 10.9% of matched patients without one had a previous thromboembolic event (P less than .0001). Patients with a CVAD also had significantly higher rates of hypertension (51.9% vs. 45.0% with placebo; P less than .001) and anticoagulation therapy (7.0% vs. 5.2% with placebo; P less than .05). Differences between the groups were not significant for diabetes (26.9% vs. 24.2%) and hyperlipidemia (19.1% vs. 17.8%).
Occlusion and stenosis of the carotid artery was the most common arterial thromboembolic outcome, occurring in 5.3% of those with a CVAD and in 2.8% of those without a CVAD. The most common venous thromboembolic event was acute venous embolism and thrombosis of lower-extremity deep vessels, which occurred in 7% of those with a CVAD and in 1.8% of those without.
The researchers also compared inpatient admissions and emergency department visits among those with and without a CVAD; both rates were higher in patients with a CVAD. Visits to the emergency department occurred at a rate of 0.14 events per month for those with a CVAD (2.01 distinct months with a claim) and 0.09 events per month for those without a CVAD (0.65 distinct months with a claim). Patients with a CVAD had 1.44 months with an inpatient admissions claim, in comparison with 0.41 months among matched patients without a CVAD. Inpatient admission frequency per month was 0.14 for those with a CVAD and 0.08 for those without.
The research was funded by CSL Behring. Dr. Patel and two of the other five authors are employees of CSL Behring.
SOURCE: Patel A et al. AANEM 2019, Abstract 94.
AUSTIN, TEX. – Patients with chronic inflammatory demyelinating polyneuropathy (CIDP) who receive intravenous immunoglobulin (IVIg) appear to have an increased risk of thromboembolic events if it is administered with a central venous access device (CVAD) when compared against those without a CVAD, according to a recent study.
Although CVADs can reliably deliver IVIg, they also represent an established risk factor for thromboembolic events, Ami Patel, PhD, a senior epidemiologist at CSL Behring, and colleagues noted on their poster at the annual meeting of the American Association for Neuromuscular and Electrodiagnostic Medicine.
The results suggest a need for physicians to be vigilant about patients’ potential risk factors for thromboembolic events, Dr. Patel said in an interview. Further research is planned, however, because the current study did not control for other risk factors or explore other possible confounding, she said.
Dr. Patel and her associates analyzed U.S. claims data (IBM/Truven MarketScan) from 2006 to 2018 and included all patients with a CIDP diagnosis claim and a postdiagnosis code for IVIg. A code for CVAD up to 2 months before CIDP diagnosis without removal before IVIg treatment ended determined those with CVAD exposure, and thromboembolic events included any codes related to arterial, venous, or vascular prostheses.
The researchers then compared patients in a case-control fashion, matching each one with a CVAD to five patients of similar demographics without a CVAD. Characteristics used for matching included medical insurance type, prescription data availability, sex, age, geographic region, and years enrolled in the database.
Among 7,447 patients with at least one IVIg claim, 11.8% (n = 882) had CVAD exposure and 88.2% (n = 6,565) did not. Of those without a CVAD, 3,642 patients were matched to patients with CVAD. A quarter (25.4%) of patients with a CVAD had a thromboembolic event, compared with 11.2% of matched patients without CVADs (P less than .0001).
In the year leading up to IVIg therapy, 16.9% of those with a CVAD and 10.9% of matched patients without one had a previous thromboembolic event (P less than .0001). Patients with a CVAD also had significantly higher rates of hypertension (51.9% vs. 45.0% with placebo; P less than .001) and anticoagulation therapy (7.0% vs. 5.2% with placebo; P less than .05). Differences between the groups were not significant for diabetes (26.9% vs. 24.2%) and hyperlipidemia (19.1% vs. 17.8%).
Occlusion and stenosis of the carotid artery was the most common arterial thromboembolic outcome, occurring in 5.3% of those with a CVAD and in 2.8% of those without a CVAD. The most common venous thromboembolic event was acute venous embolism and thrombosis of lower-extremity deep vessels, which occurred in 7% of those with a CVAD and in 1.8% of those without.
The researchers also compared inpatient admissions and emergency department visits among those with and without a CVAD; both rates were higher in patients with a CVAD. Visits to the emergency department occurred at a rate of 0.14 events per month for those with a CVAD (2.01 distinct months with a claim) and 0.09 events per month for those without a CVAD (0.65 distinct months with a claim). Patients with a CVAD had 1.44 months with an inpatient admissions claim, in comparison with 0.41 months among matched patients without a CVAD. Inpatient admission frequency per month was 0.14 for those with a CVAD and 0.08 for those without.
The research was funded by CSL Behring. Dr. Patel and two of the other five authors are employees of CSL Behring.
SOURCE: Patel A et al. AANEM 2019, Abstract 94.
AUSTIN, TEX. – Patients with chronic inflammatory demyelinating polyneuropathy (CIDP) who receive intravenous immunoglobulin (IVIg) appear to have an increased risk of thromboembolic events if it is administered with a central venous access device (CVAD) when compared against those without a CVAD, according to a recent study.
Although CVADs can reliably deliver IVIg, they also represent an established risk factor for thromboembolic events, Ami Patel, PhD, a senior epidemiologist at CSL Behring, and colleagues noted on their poster at the annual meeting of the American Association for Neuromuscular and Electrodiagnostic Medicine.
The results suggest a need for physicians to be vigilant about patients’ potential risk factors for thromboembolic events, Dr. Patel said in an interview. Further research is planned, however, because the current study did not control for other risk factors or explore other possible confounding, she said.
Dr. Patel and her associates analyzed U.S. claims data (IBM/Truven MarketScan) from 2006 to 2018 and included all patients with a CIDP diagnosis claim and a postdiagnosis code for IVIg. A code for CVAD up to 2 months before CIDP diagnosis without removal before IVIg treatment ended determined those with CVAD exposure, and thromboembolic events included any codes related to arterial, venous, or vascular prostheses.
The researchers then compared patients in a case-control fashion, matching each one with a CVAD to five patients of similar demographics without a CVAD. Characteristics used for matching included medical insurance type, prescription data availability, sex, age, geographic region, and years enrolled in the database.
Among 7,447 patients with at least one IVIg claim, 11.8% (n = 882) had CVAD exposure and 88.2% (n = 6,565) did not. Of those without a CVAD, 3,642 patients were matched to patients with CVAD. A quarter (25.4%) of patients with a CVAD had a thromboembolic event, compared with 11.2% of matched patients without CVADs (P less than .0001).
In the year leading up to IVIg therapy, 16.9% of those with a CVAD and 10.9% of matched patients without one had a previous thromboembolic event (P less than .0001). Patients with a CVAD also had significantly higher rates of hypertension (51.9% vs. 45.0% with placebo; P less than .001) and anticoagulation therapy (7.0% vs. 5.2% with placebo; P less than .05). Differences between the groups were not significant for diabetes (26.9% vs. 24.2%) and hyperlipidemia (19.1% vs. 17.8%).
Occlusion and stenosis of the carotid artery was the most common arterial thromboembolic outcome, occurring in 5.3% of those with a CVAD and in 2.8% of those without a CVAD. The most common venous thromboembolic event was acute venous embolism and thrombosis of lower-extremity deep vessels, which occurred in 7% of those with a CVAD and in 1.8% of those without.
The researchers also compared inpatient admissions and emergency department visits among those with and without a CVAD; both rates were higher in patients with a CVAD. Visits to the emergency department occurred at a rate of 0.14 events per month for those with a CVAD (2.01 distinct months with a claim) and 0.09 events per month for those without a CVAD (0.65 distinct months with a claim). Patients with a CVAD had 1.44 months with an inpatient admissions claim, in comparison with 0.41 months among matched patients without a CVAD. Inpatient admission frequency per month was 0.14 for those with a CVAD and 0.08 for those without.
The research was funded by CSL Behring. Dr. Patel and two of the other five authors are employees of CSL Behring.
SOURCE: Patel A et al. AANEM 2019, Abstract 94.
REPORTING FROM AANEM 2019
CMT1A neuropathy improves with investigational drug PXT3003
AUSTIN, TEX. – , according to new research.
“The study has established for the first time that patients after up to 15 months of treatment had a statistically significant and clinically relevant disability improvement as illustrated by the change from baseline of their ONLS [Overall Neurology Limitations Scale] scale,” concluded Florian Thomas, MD, PhD, of Hackensack (N.J.) University Medical Center, and his associates at Pharnext. “PXT3003 with dose 4 has at least stabilized, even improved, the disease.”
The researchers presented their findings in a poster at the annual meeting of the American Association for Neuromuscular and Electrodiagnostic Medicine.
The PLEO-CMT study was an international, multicenter, randomized, double-blind, placebo-controlled, phase 3 trial that evaluated the efficacy and safety of PXT3003, an oral 3-drug combination, for CMT1A. CMT1A neuropathy, occurring in an estimated 1 in 5,000 people, is characterized by distal muscle atrophy that affects walking and causes stocking-glove sensory loss and lower quality of life.
The trial enrolled 323 patients, aged 16-65, who had mild to moderate CMT1A that had been genetically confirmed. The modified full set analysis (n = 235), which represented the main study analysis for the primary endpoint, included a placebo group of 87 participants while two other groups received one of two doses of the fixed-dose drug combination twice daily: Ninety-three participants received 3 mg baclofen, 0.35 mg naltrexone, and 105 mg sorbitol (dose 1), and 55 participants received twice that dose (dose 2).
The primary endpoint was mean change from baseline to 12 and 15 months on the ONLS. At baseline, 90% of patients had an ONLS score of 2-4, and the researchers determined an average 0.3 points reduction to be a clinically meaningful effect.
Secondary endpoints included the 10-meter walk test, the 9-hole peg test, and a subscore of Charcot-Marie-Tooth neuropathy score version 2 (CMTNSv2).
Only those taking the higher dose (dose 2) showed a clinically significant drop in ONLS, –0.37 points, compared with those taking placebo (P = .0008). The in-group change from baseline to 15 months in ONLS score for patients taking dose 2 showed a trend of improvement that did not reach significance (–0.20; P = .098).
Participants receiving dose 2 of PXT3003 also walked 0.47 seconds faster on the 10-meter walk test, compared with those receiving placebo (P = .016). No significant differences occurred in the other secondary endpoints, although nonsignificant trends of improvement occurred.
Treatment-emergent adverse events were similar across all three groups and led to trial withdrawal at similar rates for dose 1 (5.5%), dose 2 (5.3%), and placebo (5.9%). One serious adverse event, benign thyroid adenoma, led to trial withdrawal, but no serious adverse events occurred related to the treatment.
Pharnext funded the research. Dr. Thomas is a researcher with Pharnext and Acceleron and has received speaking or advisory board fees from Novartis, Acceleron, Sanofi, and Genentech. The other seven authors are employees of Pharnext.
SOURCE: Thomas F et al. AANEM 2019, Abstract 92.
AUSTIN, TEX. – , according to new research.
“The study has established for the first time that patients after up to 15 months of treatment had a statistically significant and clinically relevant disability improvement as illustrated by the change from baseline of their ONLS [Overall Neurology Limitations Scale] scale,” concluded Florian Thomas, MD, PhD, of Hackensack (N.J.) University Medical Center, and his associates at Pharnext. “PXT3003 with dose 4 has at least stabilized, even improved, the disease.”
The researchers presented their findings in a poster at the annual meeting of the American Association for Neuromuscular and Electrodiagnostic Medicine.
The PLEO-CMT study was an international, multicenter, randomized, double-blind, placebo-controlled, phase 3 trial that evaluated the efficacy and safety of PXT3003, an oral 3-drug combination, for CMT1A. CMT1A neuropathy, occurring in an estimated 1 in 5,000 people, is characterized by distal muscle atrophy that affects walking and causes stocking-glove sensory loss and lower quality of life.
The trial enrolled 323 patients, aged 16-65, who had mild to moderate CMT1A that had been genetically confirmed. The modified full set analysis (n = 235), which represented the main study analysis for the primary endpoint, included a placebo group of 87 participants while two other groups received one of two doses of the fixed-dose drug combination twice daily: Ninety-three participants received 3 mg baclofen, 0.35 mg naltrexone, and 105 mg sorbitol (dose 1), and 55 participants received twice that dose (dose 2).
The primary endpoint was mean change from baseline to 12 and 15 months on the ONLS. At baseline, 90% of patients had an ONLS score of 2-4, and the researchers determined an average 0.3 points reduction to be a clinically meaningful effect.
Secondary endpoints included the 10-meter walk test, the 9-hole peg test, and a subscore of Charcot-Marie-Tooth neuropathy score version 2 (CMTNSv2).
Only those taking the higher dose (dose 2) showed a clinically significant drop in ONLS, –0.37 points, compared with those taking placebo (P = .0008). The in-group change from baseline to 15 months in ONLS score for patients taking dose 2 showed a trend of improvement that did not reach significance (–0.20; P = .098).
Participants receiving dose 2 of PXT3003 also walked 0.47 seconds faster on the 10-meter walk test, compared with those receiving placebo (P = .016). No significant differences occurred in the other secondary endpoints, although nonsignificant trends of improvement occurred.
Treatment-emergent adverse events were similar across all three groups and led to trial withdrawal at similar rates for dose 1 (5.5%), dose 2 (5.3%), and placebo (5.9%). One serious adverse event, benign thyroid adenoma, led to trial withdrawal, but no serious adverse events occurred related to the treatment.
Pharnext funded the research. Dr. Thomas is a researcher with Pharnext and Acceleron and has received speaking or advisory board fees from Novartis, Acceleron, Sanofi, and Genentech. The other seven authors are employees of Pharnext.
SOURCE: Thomas F et al. AANEM 2019, Abstract 92.
AUSTIN, TEX. – , according to new research.
“The study has established for the first time that patients after up to 15 months of treatment had a statistically significant and clinically relevant disability improvement as illustrated by the change from baseline of their ONLS [Overall Neurology Limitations Scale] scale,” concluded Florian Thomas, MD, PhD, of Hackensack (N.J.) University Medical Center, and his associates at Pharnext. “PXT3003 with dose 4 has at least stabilized, even improved, the disease.”
The researchers presented their findings in a poster at the annual meeting of the American Association for Neuromuscular and Electrodiagnostic Medicine.
The PLEO-CMT study was an international, multicenter, randomized, double-blind, placebo-controlled, phase 3 trial that evaluated the efficacy and safety of PXT3003, an oral 3-drug combination, for CMT1A. CMT1A neuropathy, occurring in an estimated 1 in 5,000 people, is characterized by distal muscle atrophy that affects walking and causes stocking-glove sensory loss and lower quality of life.
The trial enrolled 323 patients, aged 16-65, who had mild to moderate CMT1A that had been genetically confirmed. The modified full set analysis (n = 235), which represented the main study analysis for the primary endpoint, included a placebo group of 87 participants while two other groups received one of two doses of the fixed-dose drug combination twice daily: Ninety-three participants received 3 mg baclofen, 0.35 mg naltrexone, and 105 mg sorbitol (dose 1), and 55 participants received twice that dose (dose 2).
The primary endpoint was mean change from baseline to 12 and 15 months on the ONLS. At baseline, 90% of patients had an ONLS score of 2-4, and the researchers determined an average 0.3 points reduction to be a clinically meaningful effect.
Secondary endpoints included the 10-meter walk test, the 9-hole peg test, and a subscore of Charcot-Marie-Tooth neuropathy score version 2 (CMTNSv2).
Only those taking the higher dose (dose 2) showed a clinically significant drop in ONLS, –0.37 points, compared with those taking placebo (P = .0008). The in-group change from baseline to 15 months in ONLS score for patients taking dose 2 showed a trend of improvement that did not reach significance (–0.20; P = .098).
Participants receiving dose 2 of PXT3003 also walked 0.47 seconds faster on the 10-meter walk test, compared with those receiving placebo (P = .016). No significant differences occurred in the other secondary endpoints, although nonsignificant trends of improvement occurred.
Treatment-emergent adverse events were similar across all three groups and led to trial withdrawal at similar rates for dose 1 (5.5%), dose 2 (5.3%), and placebo (5.9%). One serious adverse event, benign thyroid adenoma, led to trial withdrawal, but no serious adverse events occurred related to the treatment.
Pharnext funded the research. Dr. Thomas is a researcher with Pharnext and Acceleron and has received speaking or advisory board fees from Novartis, Acceleron, Sanofi, and Genentech. The other seven authors are employees of Pharnext.
SOURCE: Thomas F et al. AANEM 2019, Abstract 92.
REPORTING FROM AANEM 2019