User login
Hospitals appear to be making progress in keeping down the number of elective deliveries performed before 39 weeks’ gestation, according to data from the Leapfrog Group's annual hospital survey.
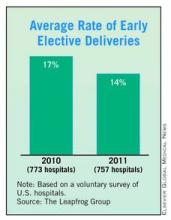
The survey of 757 hospitals found that 39% of reporting hospitals had early elective delivery rates of 5% or less in 2011, compared with 30% the previous year. And the average rate for early elective deliveries among these hospitals dropped from 17% to 14% between 2010 and 2011.
But there is still wide variation, with rates ranging from a low of less than 5% to more than 40%, according to the Leapfrog data.
"Of the hospitals that reported an elective delivery rate in 2010 and 2011, 65% improved their performance. This is extremely promising news. We are making a difference in the lives of women and newborns," Leapfrog CEO Leah Binder said in a written statement. "But there is still work to be done. We are seeing far too many newborns delivered early and without a medical reason, and there are still a number of hospitals who refuse to make this information public."
The Leapfrog Group, a coalition of public and private purchasers of employee health benefits that works on health care quality improvement, began collecting data on early elective deliveries in 2009 and first publicly reported hospital data in 2010. The group has identified the trend toward early deliveries as both a safety and economic issue. For instance, women who are induced in weeks 37 and 38 have a higher risk of needing a cesarean section than women who go into labor on their own.
Studies have also linked early elective deliveries to postpartum complications such as hematoma, wound dehiscence, anemia, endometriosis, urinary tract infections, and sepsis, according to the Leapfrog Group. On the economic side, early deliveries tend to be more costly. One estimate published in 2010 finds that nearly $1 billion in U.S. health care costs could be saved each year by reducing the early delivery rate by 1.7%. Those savings would be achieved mainly by reducing the number of days newborns spend in neonatal intensive care units (Am. J. Obstet. Gynecol. 2010;203:e1-6).
As part of the Leapfrog survey, hospitals were asked to report on the percentage of nonmedically indicated deliveries by induction or cesarean section between 37 and 39 completed weeks of gestation. These are deliveries in which the mothers had not already gone into active labor or experienced a spontaneous rupture of membranes.
Hospitals appear to be making progress in keeping down the number of elective deliveries performed before 39 weeks’ gestation, according to data from the Leapfrog Group's annual hospital survey.
The survey of 757 hospitals found that 39% of reporting hospitals had early elective delivery rates of 5% or less in 2011, compared with 30% the previous year. And the average rate for early elective deliveries among these hospitals dropped from 17% to 14% between 2010 and 2011.
But there is still wide variation, with rates ranging from a low of less than 5% to more than 40%, according to the Leapfrog data.
"Of the hospitals that reported an elective delivery rate in 2010 and 2011, 65% improved their performance. This is extremely promising news. We are making a difference in the lives of women and newborns," Leapfrog CEO Leah Binder said in a written statement. "But there is still work to be done. We are seeing far too many newborns delivered early and without a medical reason, and there are still a number of hospitals who refuse to make this information public."
The Leapfrog Group, a coalition of public and private purchasers of employee health benefits that works on health care quality improvement, began collecting data on early elective deliveries in 2009 and first publicly reported hospital data in 2010. The group has identified the trend toward early deliveries as both a safety and economic issue. For instance, women who are induced in weeks 37 and 38 have a higher risk of needing a cesarean section than women who go into labor on their own.
Studies have also linked early elective deliveries to postpartum complications such as hematoma, wound dehiscence, anemia, endometriosis, urinary tract infections, and sepsis, according to the Leapfrog Group. On the economic side, early deliveries tend to be more costly. One estimate published in 2010 finds that nearly $1 billion in U.S. health care costs could be saved each year by reducing the early delivery rate by 1.7%. Those savings would be achieved mainly by reducing the number of days newborns spend in neonatal intensive care units (Am. J. Obstet. Gynecol. 2010;203:e1-6).
As part of the Leapfrog survey, hospitals were asked to report on the percentage of nonmedically indicated deliveries by induction or cesarean section between 37 and 39 completed weeks of gestation. These are deliveries in which the mothers had not already gone into active labor or experienced a spontaneous rupture of membranes.
Hospitals appear to be making progress in keeping down the number of elective deliveries performed before 39 weeks’ gestation, according to data from the Leapfrog Group's annual hospital survey.
The survey of 757 hospitals found that 39% of reporting hospitals had early elective delivery rates of 5% or less in 2011, compared with 30% the previous year. And the average rate for early elective deliveries among these hospitals dropped from 17% to 14% between 2010 and 2011.
But there is still wide variation, with rates ranging from a low of less than 5% to more than 40%, according to the Leapfrog data.
"Of the hospitals that reported an elective delivery rate in 2010 and 2011, 65% improved their performance. This is extremely promising news. We are making a difference in the lives of women and newborns," Leapfrog CEO Leah Binder said in a written statement. "But there is still work to be done. We are seeing far too many newborns delivered early and without a medical reason, and there are still a number of hospitals who refuse to make this information public."
The Leapfrog Group, a coalition of public and private purchasers of employee health benefits that works on health care quality improvement, began collecting data on early elective deliveries in 2009 and first publicly reported hospital data in 2010. The group has identified the trend toward early deliveries as both a safety and economic issue. For instance, women who are induced in weeks 37 and 38 have a higher risk of needing a cesarean section than women who go into labor on their own.
Studies have also linked early elective deliveries to postpartum complications such as hematoma, wound dehiscence, anemia, endometriosis, urinary tract infections, and sepsis, according to the Leapfrog Group. On the economic side, early deliveries tend to be more costly. One estimate published in 2010 finds that nearly $1 billion in U.S. health care costs could be saved each year by reducing the early delivery rate by 1.7%. Those savings would be achieved mainly by reducing the number of days newborns spend in neonatal intensive care units (Am. J. Obstet. Gynecol. 2010;203:e1-6).
As part of the Leapfrog survey, hospitals were asked to report on the percentage of nonmedically indicated deliveries by induction or cesarean section between 37 and 39 completed weeks of gestation. These are deliveries in which the mothers had not already gone into active labor or experienced a spontaneous rupture of membranes.
FROM THE LEAPFROG GROUP