User login
About 10 million U.S. adults live with serious mental illness (SMI).1 Among military veterans, the number of mental health (MH) diagnoses is increasing with the return of troops from deployment in Iraq and Afghanistan.2-4 This increase has considerable implications for service use at the VA. An estimated 35% of army and marine veterans sought MH services within 1 year of returning from Iraq and Afghanistan.5 Furthermore, there is an association of MH disorders, physical illnesses, and mortality rates among veterans.2,6 Rising MH needs will increase the need for services; not unexpectedly, the VA is one of the largest providers of integrated health care in the U.S.7
Many patients with SMI have additional health issues, secondary to medication adverse effects, medical comorbidities, and other factors.8-12 Furthermore, their rates of preventable risk factors (eg, smoking, alcohol abuse, and poor exercise and diet13,14) are higher. Comorbid medical illnesses can sideline the treatment of mental illness and lead to negative health outcomes.15,16 These medical conditions coupled with SMI may increase overall rates of health care utilization in terms of outpatient visits, procedures, and inpatient hospitalizations. However, the literature on factors associated with health care utilization in veterans with SMI is scant and generally inconclusive.
Findings on utilization of non-MH medical services for veterans with comorbid MH diagnoses are mixed. Operation Enduring Freedom (OEF) and Operation Iraqi Freedom (OIF) veterans with MH diagnoses have been found to use significantly more non-MH medical services than do OEF and OIF veterans without these diagnoses.17 However, other studies have found that veterans with SMI seem to be less likely to use medical services.18,19 For example, in a study of the rate of medical visits for veterans with psychiatric diagnoses, veterans with SMI were found to have fewer outpatient medical visits than do other veterans without SMI.20 Given the high rates of medical comorbidities in veterans with SMI, this finding of reduced rates of medical care is both informative and concerning. However, more information on utilization rates for other types of health care system services is needed.
In addition to MH diagnoses, multiple factors influence the use of health care services. Lower income predicts overall use of mental and medical services for female but not male veterans.21 A large proportion of VA patients are male, and that disparity may affect female veterans’ perceptions and use of VA health care, underscoring the importance of examining the effects of sex in health care utilization.22 Unmarried status, unemployment, and combat experience are other factors associated with higher health care utilization.23,24 Sociodemographic factors, including income and possession of private health insurance, are associated with veterans’ use of VA health care services.25 It is important to understand the effects of these factors on service utilization by veterans with SMI in order to provide them with optimal, targeted health care.
The authors conducted this study to examine factors affecting MH service utilization and health outcomes in veterans with SMI at the VA Palo Alto Health Care System (VAPAHCS). A retrospective data analysis of medical records was performed. More specifically, this study aimed to identify veteran-specific variables (eg, demographics, psychiatric diagnosis, comorbid medical conditions, combat status) associated with health care utilization and outcomes in veterans with SMI. Dependent variables of interest included service utilization, such as rate and length of inpatient hospitalization and frequency of outpatient encounters. Examining predictors of inpatient medical and psychiatric hospitalization (demographic, clinical, or treatment-related factors) can provide insight into which veterans can benefit from targeted, intensive interventions. A better understanding of the factors affecting comprehensive health care service use for veterans with SMI can clarify targeted interventions and follow-up care for an expanding population.
Methods
Study approval was obtained from the institutional review board at Stanford University and the VAPAHCS research and development committee. Medical record data for veterans treated at the VAPAHCS were collected for a 10-year period (fiscal years 2003-2012). The Computerized Patient Record System (CPRS) data were accessed by VA decision support system staff and analyzed with SPSS Version 21.0 (Armonk, NY). Veterans were identified by ICD-9 codes 295.00 through 298.9, as documented in CPRS.
For this study, schizophrenic, psychotic, bipolar, depressive, and mood disorders were classified as SMI. VA clinic codes were used to categorize visits by service: medical (general medical clinic, surgery, pharmacy, laboratory tests), MH (outpatient visits, intakes and assessments), ancillary services (chaplain, social work, administration), residential MH treatment (substance use disorder, domiciliary care), home-based primary care, and home-based MH care. Psychiatric diagnoses were grouped into schizophrenic disorders, unspecified psychotic disorders, bipolar disorders, major depressive disorders (MDD), and mood disorders not otherwise specified (NOS). The demographic variables obtained through medical records included age, service connection, combat flag (deployment to combat zone), service period, and marital status at start of fiscal year 2003.
Over the 10-year period, 15,414 unique patients were classified as having SMI. Veterans who died during this period were removed from the dataset because of concerns about incomplete data (with specific dates of death unavailable, it was difficult to determine whether missed VA visits during a particular year indicated low utilization or death). In addition, inpatient medical and psychiatric visits were excluded from the analysis in an effort to identify how outpatient utilization uniquely affects the frequency of inpatient hospitalization. Last, because the authors wanted to exclude from the analysis all patients who may have had a single consultation at the VA during the 10-year period, they required at least 2 visits per patient. The final dataset consisted of 11,135 patients.
Age differences reported in the literature included a lesser likelihood of MH diagnosis for older returning OEF/OIF veterans,26 and older age as a factor related to veterans’ increased health care use.27 Therefore, age was included as a covariate in the analyses.
Results
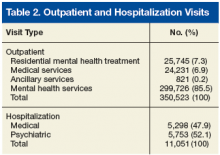
The 11,135 patients included in the study, made a total of 350,523 outpatient visits over the period (Table 1). The mean number of outpatient visits was 6.6 (SD, 11.7; median, 3.5; mode, 2.0; range, 1.0-219.9). Over the 10-year period, 14.0% of patients averaged 1 visit per year, 23.4% averaged 2 visits, 15.6% averaged 3 visits, 10.7% averaged 4 visits, 7.4% averaged 5 visits, and 28.9% averaged 6 or more visits. Table 2 lists the frequencies and percentages of outpatient visits and hospitalizations.
Group Difference T-Test Analysis
Of the 553 OEF/OIF veterans in the study, 225 (40.7%) had combat flags, and 328 (59.3%) did not. Independent- groups t test showed significant group differences in mean number of visits (t[2,964.48] = 9.94, P < .01). Veterans with combat flags averaged significantly fewer visits per year (mean, 4.79; SD, 5.89) than did veterans without flags (mean, 6.89; SD, 12.50), even with age as a covariate (F[1, 10,675] = 34.63, P < .01).
Independent-groups t test showed significant group differences in mean number of nonpsychiatric hospitalizations (t[2,328.68] = 5.00, P < .01). Veterans with combat flags averaged significantly fewer nonpsychiatric hospitalizations per year (mean, 0.34; SD, .99) than did veterans without flags (mean, 0.51; SD, 1.71), even with age as a covariate (F[1, 10,675] = 9.81, P < .01).
Independent-groups t test showed significant group differences in mean number of psychiatric hospitalizations (t[2,706.75] = 7.69, P < .01). Veterans with combat flags averaged significantly fewer psychiatric hospitalizations per year (mean, 0.31; SD, 0.91) than did veterans without flags (mean, 0.55; SD, 1.80), even with age as a covariate (F[1, 10,675] = 23.51, P < .01).
Group Differences by SMI Diagnosis
Mean number of visits. Analysis of covariance (ANCOVA) was used to determine differences among the SMI groups (schizophrenic, psychotic, bipolar, depressive, and mood disorders) in mean number of outpatient visits per year with age as a covariate. With age accounted for, there were significant differences among the SMI groups (F[4, 11,129] = 285.02, P < .01). Therefore, pairwise comparisons were used to examine differences among individual disorders. Veterans with schizophrenic disorders averaged more visits per year (mean, 16.2; SD, 27.12) than did veterans with bipolar disorders (mean, 6.4; SD, 7.8, P < .01) and veterans with MDD (mean, 4.8; SD, 5.5, P < .01). Veterans with schizophrenia also averaged more visits per year than did veterans with mood disorders NOS (mean, 5.2; SD, 5.9, P < .01) and veterans with unspecified psychotic disorders (mean, 5.9; SD, 9.6, P < .01).
Nonpsychiatric hospitalizations. An ANCOVA analysis was used to determine group differences in nonpsychiatric hospitalizations per year with SMI diagnosis as the independent variable and age as a covariate. With age accounted for, there were significant differences among the SMI groups (F[4, 11,129] = 143.02, P < .01). Furthermore, pairwise comparisons were used to examine differences among individual disorders. Veterans with schizophrenic disorders averaged more nonpsychiatric hospitalizations (mean, 1.4; SD, 3.4) than did veterans with bipolar disorders (mean, 0.7; SD, 1.8, P < .01) and veterans with MDD (mean, 0.3; SD, 0.9, P < .01). Veterans with schizophrenia averaged more nonpsychiatric hospitalizations per year than did veterans with mood disorders NOS (mean, 0.3; SD, 0.8, P < .01) and veterans with unspecified psychotic disorders (mean, 0.5; SD, 1.2, P < .01).
Psychiatric hospitalizations. An ANCOVA analysis was used to determine group differences in psychiatric hospitalizations per year with SMI diagnosis as the independent variable and age as a covariate. With age accounted for, there were significant differences among the SMI groups (F[4, 11,129] = 204.64, P < .01). Furthermore, pairwise comparisons were used to examine differences among individual disorders. Veterans with schizophrenic disorders averaged more psychiatric hospitalizations per year (mean, 1.6; SD, 3.4) than did veterans with bipolar disorders (mean, 0.7; SD, 1.9, P < .01) and veterans with MDD (mean, 0.3; SD, 1.0, P < .01). Veterans with schizophrenia averaged more psychiatric hospitalizations per year than did veterans with mood disorders NOS (mean, 0.2; SD, 0.8, P < .01) and veterans with unspecified psychotic disorders (mean, 0.9; SD, 1.8, P < .01).
Group Differences by Marital Status
Mean number of visits. An ANCOVA analysis was used to determine differences among the marital status groups (married, divorced, never married) in mean number of outpatient visits per year with age as a covariate. With age accounted for, there were significant differences among the marital status groups (F[3, 11,130] = 104.37, P < .01). Married veterans averaged fewer visits per year (mean, 4.6; SD, 5.2) than did divorced veterans (mean, 6.2; SD, 9.9, P < .01) and never-married veterans (mean, 9.8; SD, 18.8, P < .01).
Nonpsychiatric hospitalizations. An ANCOVA analysis was used to determine group differences in nonpsychiatric hospitalizations per year with marital status as the independent variable and age as a covariate. With age accounted for, there were significant differences among the marital status groups (F[3, 11,130] = 43.97, P < .01). Married veterans averaged fewer nonpsychiatric hospitalizations per year (mean, 0.27; SD, 1.52) than did divorced veterans (mean, 0.47; SD, 1.30, P < .01) and never-married veterans (mean, 0.75; SD, 2.08, P <.01) Last, married veterans averaged fewer nonpsychiatric hospitalizations than did veterans with other/unknown marital status (mean, 0.5; SD, 1.5, P < .01).
Psychiatric hospitalizations. An ANCOVA analysis was used to determine group differences in mean number of psychiatric hospitalizations per year with marital status as the independent variable and age as a covariate. With age accounted for, there were significant differences among the marital status groups (F[3, 11,130] = 68.94, P < .01). Married veterans averaged fewer psychiatric hospitalizations per year (mean, 0.23; SD, 0.86) than did divorced veterans (mean, 0.55; SD, 1.58, P < .01) and nevermarried veterans (mean, 0.86; SD, 2.53, P < .01).
Predictors of Hospitalization
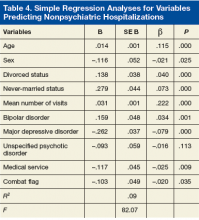
Regression analyses revealed that age, sex, divorced status, never-married status, mean number of visits, bipolar disorders, MDD, mood disorders NOS, unspecified psychotic disorders, residential MH treatment, ancillary services, and combat flag were all significant predictors of total number of both psychiatric hospitalizations (adjusted R2 = .15, F[128.56] = .00) and nonpsychiatric hospitalizations (adjusted R2 = .09, F[82.07] = .00) (Tables 3 & 4).
Discussion
This study examined medical and psychiatric service utilization in veterans with SMI diagnoses. For this population, 85.5% of the total number of VA visits were for MH services, and 52.1% of hospitalizations were for psychiatric care. Medical visits accounted for only 6.9% of outpatient services provided. Although the high utilization of psychiatric services by this SMI population may not be striking in itself, the considerably lower utilization of medical services is notable given the high rates of medical comorbidities associated with SMI. This result confirms findings from other studies.8-10,20 Possibly, VA health care guidelines may account for the lower medical service utilization. For example, the outpatient MH service has a metabolic syndrome clinic with psychiatrist prescribing guidelines for treating veterans who meet the criteria for metabolic syndrome.
The total number of outpatient visits varied widely. The largest percentage of veterans (29%) averaged 6 or more visits per year, followed by 2, 3, 1, and 4 visits. These findings suggest many patients are frequently utilizing services. The implications for inpatient hospitalization are notable, as the study’s data also suggest veterans with more total outpatient visits are at increased risk for hospitalization. The higher number of visits may be attributable to the SMI population’s increased health care needs and may suggest a need to target heavy users of outpatient services with more intensive programs to minimize costly hospitalizations. Mean number of outpatient visits was associated with a slightly higher risk for psychiatric hospitalization, possibly because of increased accessibility to care. Outpatient visits increased the risk for overall hospitalization, and psychiatric hospitalization specifically.
The type of SMI diagnosis predicted total number of outpatient visits, demonstrating that veterans with schizophrenic disorders averaged significantly more outpatient visits per year than did veterans with other SMI diagnoses. Interestingly, results showed that veterans with combat flags averaged significantly fewer outpatient visits than did veterans without flags. This finding is notable, as combat exposure is associated with higher rates of MH diagnoses and relatedly higher service utilization. However, combat veterans with SMI but not posttraumatic stress disorder (PTSD), averaged fewer outpatient visits than did veterans without combat exposure, which was not consistent with earlier findings.28 More research specifically on the effects of combat on veterans with PTSD may help in reconciling these findings. Married veterans averaged significantly fewer outpatient visits per year than did divorced or nevermarried veterans. It may be that social support among married couples is protective in veterans with SMI, or that veterans with SMI are unable to maintain marriages.
Hospitalization Predictors
Several significant predictors of psychiatric hospitalization were noted. Increasing age was negatively related to psychiatric hospitalization. It is possible that older patients with SMI receive other types of care, including board and care homes, or MH intensive case management, in which psychiatric outpatient care is readily provided—reducing the need for psychiatric hospitalization. In addition, married veterans were significantly less likely than were divorced and never-married veterans to have been hospitalized. It is possible that being married is protective for MH and physical health or that being unhealthy is a risk factor for divorce.
The type of SMI diagnosis also significantly predicted hospitalization. Having received specific types of services, including residential MH treatment and ancillary services, was a significant predictor of the total number of psychiatric hospitalizations. Last, having a combat flag negatively predicted psychiatric hospitalization—incongruent with earlier findings.24 These results suggest a profile of a veteran who likely could benefit either from a targeted intervention or from having ready access to a social worker.
Improved understanding of service utilization is vital to providing care to returning veterans. Mental disorders are very common among recent OEF, OIF, and Operation New Dawn veterans.29 As the rate of MH diagnoses climbs, the cost of providing health care grows exponentially. The cost of providing care to veterans with SMI can be addressed by identifying veteran-specific factors to provide intensive outreach and prevent costly hospitalization.
Limitations
The results of this study should be interpreted in light of several limitations. It is plausible that at least some veterans received health care services outside the VA, but non-VA data were not included in this study. Subsequent studies should include a group of veterans with SMI and a control group of veterans without SMI so that patterns of hospitalization and utilization rates can be compared. Also, the present study did not include data on missed appointments, an important variable in service utilization.
Missed appointments may suggest lack of follow-through with regular outpatient services, placing patients at risk for emergency services that require hospitalization. Veterans who had a single consultation were excluded in an effort to examine service utilization patterns of established patients. In future studies, including these patients could be informative in identifying specific patterns in this subpopulation. Fifth, PTSD was excluded from this study in order to identify utilization differences for veterans without PTSD.
Conclusion
Results of this study indicate that special attention should be given to veterans’ demographic and clinical factors, including age, sex, combat flags, marital status, and SMI diagnosis. Through identification of and outreach regarding these veteran-specific factors, it may be possible to use targeted interventions to reduce the need for inpatient hospitalization of veterans with chronic mental illness. Historically, the emphasis on access and outpatient care within the VA health care system drastically reduced the number of inpatient MH days.30 This outcome underscores the importance of outpatient services and suggests that targeted outpatient care can further reduce the need for inpatient MH care. Veterans with these outlined risk factors may benefit from implementation of early preventive measures.
Click here to read the digital edition.
1. Substance Abuse and Mental Health Services Administration. Results From the 2012 National Survey on Drug Use and Health: Mental Health Findings. NSDUH Series H-47, HHS publication SMA 13-4805. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2013.
2. Hoge CW, Terhakopian A, Castro CA, Messer SC, Engel CC. Association of posttraumatic stress disorder with somatic symptoms, health care visits, and absenteeism among Iraq war veterans. Am J Psychiatry. 2007;164(1):150-153.
3. Seal KH, Bertenthal D, Miner CR, Sen S, Marmar C. Bringing the war back home: mental health disorders among 103,788 US veterans returning from Iraq and Afghanistan seen at Department of Veterans Affairs facilities. Arch Intern Med. 2007;167(5):476-482.
4. Lee SE, Fonseca VP, Wolters CL, et al. Health care utilization behavior of veterans who deployed to Afghanistan and Iraq. Mil Med. 2015;180(4):374-379.
5. Hoge CW, Auchterlonie JL, Milliken CS. Mental health problems, use of mental health services, and attrition from military service after returning from deployment to Iraq or Afghanistan. JAMA. 2006;295(9):1023-1032.
6. Kramarow EA, Pastor PN. The health of male veterans and nonveterans aged 25-64: United States, 2007-2010. NCHS Data Brief. 2012;(101):1-8.
7. Elbogen EB, Wagner HR, Johnson SC, et al. Are Iraq and Afghanistan veterans using mental health services? New data from a national random-sample survey. Psychiatr Serv. 2013;64(2):134-141.
8. Bermudes RA, Keck PE Jr, Welge JA. The prevalence of the metabolic syndrome in psychiatric inpatients with primary psychotic and mood disorders. Psychosomatics. 2006;47(6):491-497.
9. Newcomer JW. Metabolic syndrome and mental illness. Am J Manag Care. 2007;13(7 suppl):S170-S177.
10. Toalson P, Ahmed S, Hardy T, Kabinoff G. The metabolic syndrome in patients with severe mental illnesses. Prim Care Companion J Clin Psychiatry. 2004;6(4):152-158.
11. Khatana SA, Kane J, Taveira TH, Bauer MS, Wu WC. Monitoring and prevalence rates of metabolic syndrome in military veterans with serious mental illness. PLoS One. 2011;6(4):e19298.
12. De Hert M, Correll CU, Bobes J, et al. Physical illness in patients with severe mental disorders. I. Prevalence, impact of medications and disparities in health care. World Psychiatry. 2011;10(1):52-77.
13. Lambert TJ, Velakoulis D, Pantelis C. Medical comorbidity in schizophrenia. Med J Aust. 2003;178(suppl):S67-S70.
14. Osborn DP, Nazareth I, King MB. Physical activity, dietary habits, and coronary heart disease risk factor knowledge amongst people with severe mental illness: a cross sectional comparative study in primary care. Soc Psychiatry Psychiatr Epidemiol. 2007;42(10):787-793.
15. Newcomer JW. Medical risk in patients with bipolar disorder and schizophrenia. J Clin Psychiatry. 2007;67(suppl 9):25-30, discussion 36-42.
16. Chwastiak LA, Rosenheck RA, Kazis LE. Association of psychiatric illness and obesity, physical inactivity, and smoking among a national sample of veterans. Psychosomatics. 2011;52(3):230-236.
17. Cohen BE, Gima K, Bertenthal D, Kim S, Marmar CR, Seal KH. Mental health diagnoses and utilization of VA non-mental health medical services among returning Iraq and Afghanistan veterans. J Gen Intern Med. 2010;25(1):18-24.
18. Chwastiak LA, Rosenheck RA, Kazis LE. Utilization of primary care of veterans with psychiatric illness in the national Department of Veterans Affairs Health Care System. J Gen Intern Med. 2008;23(11):1835-1840.
19. VA Office of Research and Development, Health Services Research and Development Service, Quality Enhancement Research Initiative. Mental health. QUERI fact sheet. http://www.hsrd.research.va.gov/publications/internal/mh_factsheet.pdf. Published December 2008. Accessed January 13, 2017.
20. Cradock-O’Leary J, Young AS, Yano EM, Wang M, Lee ML. Use of general medical services by VA patients with psychiatric disorders. Psychiatr Serv. 2002;53(7):874-878.
21. Di Leone BA, Vogt D, Gradus JL, Street AE, Giasson HL, Resick PA. Predictors of mental health care use among male and female veterans deployed in support of the wars in Afghanistan and Iraq. Psychol Serv. 2013;10(2):145-151.
22. Vogt DS, Barry AA, King LA. Toward gender-aware health care: evaluation of an intervention to enhance care for female patients in the VA setting. J Health Psychol. 2008;13(5):624-638.
23. Marshall RP, Jorm AF, Grayson DA, O’Toole BI. Posttraumatic stress disorder and other predictors of health care consumption by Vietnam veterans. Psychiatr Serv. 1998;49(12):1609-1611.
24. Rosenheck R, Massari L. Wartime military service and utilization of VA health care services. Mil Med. 1993;158(4):223-228.
25. Elhai JD, Grubaugh AL, Richardson JD, Egede LE, Creamer M. Outpatient medical and mental healthcare utilization models among military veterans: results from the 2001 National Survey of Veterans. J Psychiatr Res. 2008;42(10):858-867.
26. Seal KH, Bertenthal D, Miner CR, Sen S, Marmar C. Bringing the war back home: mental health disorders among 103,788 US veterans returning from Iraq and Afghanistan seen at Department of Veterans Affairs facilities. Arch Intern Med. 2007;167(5):476-482.
27. Fasoli DR, Glickman ME, Eisen SV. Predisposing characteristics, enabling resources and need as predictors of utilization and clinical outcomes for veterans receiving mental health services. Med Care. 2010;48(4):288-295.
28. Maguen S, Schumm JA, Norris RL, et al. Predictors of mental and physical health service utilization among Vietnam veterans. Psychol Serv. 2007;4(3):168-180.
29. Office of Public Health, Veterans Health Administration. Analysis of VA Health Care Utilization Among Operation Enduring Freedom (OEF), Operation Iraqi Freedom (OIF), and Operation New Dawn (OND) Veterans—Revised. http://www.publichealth.va.gov/docs/epidemiology/healthcare-utilization-report-fy2012-qtr3.pdf. Revised December 2012. Accessed February 6, 2017.
30. Wagner TH, Sinnott P, Siroka AM. Mental health and substance use disorder spending in the Department of Veterans Affairs, fiscal years 2000-2007. Psychiatr Serv. 2011;62(4):389-395.
About 10 million U.S. adults live with serious mental illness (SMI).1 Among military veterans, the number of mental health (MH) diagnoses is increasing with the return of troops from deployment in Iraq and Afghanistan.2-4 This increase has considerable implications for service use at the VA. An estimated 35% of army and marine veterans sought MH services within 1 year of returning from Iraq and Afghanistan.5 Furthermore, there is an association of MH disorders, physical illnesses, and mortality rates among veterans.2,6 Rising MH needs will increase the need for services; not unexpectedly, the VA is one of the largest providers of integrated health care in the U.S.7
Many patients with SMI have additional health issues, secondary to medication adverse effects, medical comorbidities, and other factors.8-12 Furthermore, their rates of preventable risk factors (eg, smoking, alcohol abuse, and poor exercise and diet13,14) are higher. Comorbid medical illnesses can sideline the treatment of mental illness and lead to negative health outcomes.15,16 These medical conditions coupled with SMI may increase overall rates of health care utilization in terms of outpatient visits, procedures, and inpatient hospitalizations. However, the literature on factors associated with health care utilization in veterans with SMI is scant and generally inconclusive.
Findings on utilization of non-MH medical services for veterans with comorbid MH diagnoses are mixed. Operation Enduring Freedom (OEF) and Operation Iraqi Freedom (OIF) veterans with MH diagnoses have been found to use significantly more non-MH medical services than do OEF and OIF veterans without these diagnoses.17 However, other studies have found that veterans with SMI seem to be less likely to use medical services.18,19 For example, in a study of the rate of medical visits for veterans with psychiatric diagnoses, veterans with SMI were found to have fewer outpatient medical visits than do other veterans without SMI.20 Given the high rates of medical comorbidities in veterans with SMI, this finding of reduced rates of medical care is both informative and concerning. However, more information on utilization rates for other types of health care system services is needed.
In addition to MH diagnoses, multiple factors influence the use of health care services. Lower income predicts overall use of mental and medical services for female but not male veterans.21 A large proportion of VA patients are male, and that disparity may affect female veterans’ perceptions and use of VA health care, underscoring the importance of examining the effects of sex in health care utilization.22 Unmarried status, unemployment, and combat experience are other factors associated with higher health care utilization.23,24 Sociodemographic factors, including income and possession of private health insurance, are associated with veterans’ use of VA health care services.25 It is important to understand the effects of these factors on service utilization by veterans with SMI in order to provide them with optimal, targeted health care.
The authors conducted this study to examine factors affecting MH service utilization and health outcomes in veterans with SMI at the VA Palo Alto Health Care System (VAPAHCS). A retrospective data analysis of medical records was performed. More specifically, this study aimed to identify veteran-specific variables (eg, demographics, psychiatric diagnosis, comorbid medical conditions, combat status) associated with health care utilization and outcomes in veterans with SMI. Dependent variables of interest included service utilization, such as rate and length of inpatient hospitalization and frequency of outpatient encounters. Examining predictors of inpatient medical and psychiatric hospitalization (demographic, clinical, or treatment-related factors) can provide insight into which veterans can benefit from targeted, intensive interventions. A better understanding of the factors affecting comprehensive health care service use for veterans with SMI can clarify targeted interventions and follow-up care for an expanding population.
Methods
Study approval was obtained from the institutional review board at Stanford University and the VAPAHCS research and development committee. Medical record data for veterans treated at the VAPAHCS were collected for a 10-year period (fiscal years 2003-2012). The Computerized Patient Record System (CPRS) data were accessed by VA decision support system staff and analyzed with SPSS Version 21.0 (Armonk, NY). Veterans were identified by ICD-9 codes 295.00 through 298.9, as documented in CPRS.
For this study, schizophrenic, psychotic, bipolar, depressive, and mood disorders were classified as SMI. VA clinic codes were used to categorize visits by service: medical (general medical clinic, surgery, pharmacy, laboratory tests), MH (outpatient visits, intakes and assessments), ancillary services (chaplain, social work, administration), residential MH treatment (substance use disorder, domiciliary care), home-based primary care, and home-based MH care. Psychiatric diagnoses were grouped into schizophrenic disorders, unspecified psychotic disorders, bipolar disorders, major depressive disorders (MDD), and mood disorders not otherwise specified (NOS). The demographic variables obtained through medical records included age, service connection, combat flag (deployment to combat zone), service period, and marital status at start of fiscal year 2003.
Over the 10-year period, 15,414 unique patients were classified as having SMI. Veterans who died during this period were removed from the dataset because of concerns about incomplete data (with specific dates of death unavailable, it was difficult to determine whether missed VA visits during a particular year indicated low utilization or death). In addition, inpatient medical and psychiatric visits were excluded from the analysis in an effort to identify how outpatient utilization uniquely affects the frequency of inpatient hospitalization. Last, because the authors wanted to exclude from the analysis all patients who may have had a single consultation at the VA during the 10-year period, they required at least 2 visits per patient. The final dataset consisted of 11,135 patients.
Age differences reported in the literature included a lesser likelihood of MH diagnosis for older returning OEF/OIF veterans,26 and older age as a factor related to veterans’ increased health care use.27 Therefore, age was included as a covariate in the analyses.
Results
The 11,135 patients included in the study, made a total of 350,523 outpatient visits over the period (Table 1). The mean number of outpatient visits was 6.6 (SD, 11.7; median, 3.5; mode, 2.0; range, 1.0-219.9). Over the 10-year period, 14.0% of patients averaged 1 visit per year, 23.4% averaged 2 visits, 15.6% averaged 3 visits, 10.7% averaged 4 visits, 7.4% averaged 5 visits, and 28.9% averaged 6 or more visits. Table 2 lists the frequencies and percentages of outpatient visits and hospitalizations.
Group Difference T-Test Analysis
Of the 553 OEF/OIF veterans in the study, 225 (40.7%) had combat flags, and 328 (59.3%) did not. Independent- groups t test showed significant group differences in mean number of visits (t[2,964.48] = 9.94, P < .01). Veterans with combat flags averaged significantly fewer visits per year (mean, 4.79; SD, 5.89) than did veterans without flags (mean, 6.89; SD, 12.50), even with age as a covariate (F[1, 10,675] = 34.63, P < .01).
Independent-groups t test showed significant group differences in mean number of nonpsychiatric hospitalizations (t[2,328.68] = 5.00, P < .01). Veterans with combat flags averaged significantly fewer nonpsychiatric hospitalizations per year (mean, 0.34; SD, .99) than did veterans without flags (mean, 0.51; SD, 1.71), even with age as a covariate (F[1, 10,675] = 9.81, P < .01).
Independent-groups t test showed significant group differences in mean number of psychiatric hospitalizations (t[2,706.75] = 7.69, P < .01). Veterans with combat flags averaged significantly fewer psychiatric hospitalizations per year (mean, 0.31; SD, 0.91) than did veterans without flags (mean, 0.55; SD, 1.80), even with age as a covariate (F[1, 10,675] = 23.51, P < .01).
Group Differences by SMI Diagnosis
Mean number of visits. Analysis of covariance (ANCOVA) was used to determine differences among the SMI groups (schizophrenic, psychotic, bipolar, depressive, and mood disorders) in mean number of outpatient visits per year with age as a covariate. With age accounted for, there were significant differences among the SMI groups (F[4, 11,129] = 285.02, P < .01). Therefore, pairwise comparisons were used to examine differences among individual disorders. Veterans with schizophrenic disorders averaged more visits per year (mean, 16.2; SD, 27.12) than did veterans with bipolar disorders (mean, 6.4; SD, 7.8, P < .01) and veterans with MDD (mean, 4.8; SD, 5.5, P < .01). Veterans with schizophrenia also averaged more visits per year than did veterans with mood disorders NOS (mean, 5.2; SD, 5.9, P < .01) and veterans with unspecified psychotic disorders (mean, 5.9; SD, 9.6, P < .01).
Nonpsychiatric hospitalizations. An ANCOVA analysis was used to determine group differences in nonpsychiatric hospitalizations per year with SMI diagnosis as the independent variable and age as a covariate. With age accounted for, there were significant differences among the SMI groups (F[4, 11,129] = 143.02, P < .01). Furthermore, pairwise comparisons were used to examine differences among individual disorders. Veterans with schizophrenic disorders averaged more nonpsychiatric hospitalizations (mean, 1.4; SD, 3.4) than did veterans with bipolar disorders (mean, 0.7; SD, 1.8, P < .01) and veterans with MDD (mean, 0.3; SD, 0.9, P < .01). Veterans with schizophrenia averaged more nonpsychiatric hospitalizations per year than did veterans with mood disorders NOS (mean, 0.3; SD, 0.8, P < .01) and veterans with unspecified psychotic disorders (mean, 0.5; SD, 1.2, P < .01).
Psychiatric hospitalizations. An ANCOVA analysis was used to determine group differences in psychiatric hospitalizations per year with SMI diagnosis as the independent variable and age as a covariate. With age accounted for, there were significant differences among the SMI groups (F[4, 11,129] = 204.64, P < .01). Furthermore, pairwise comparisons were used to examine differences among individual disorders. Veterans with schizophrenic disorders averaged more psychiatric hospitalizations per year (mean, 1.6; SD, 3.4) than did veterans with bipolar disorders (mean, 0.7; SD, 1.9, P < .01) and veterans with MDD (mean, 0.3; SD, 1.0, P < .01). Veterans with schizophrenia averaged more psychiatric hospitalizations per year than did veterans with mood disorders NOS (mean, 0.2; SD, 0.8, P < .01) and veterans with unspecified psychotic disorders (mean, 0.9; SD, 1.8, P < .01).
Group Differences by Marital Status
Mean number of visits. An ANCOVA analysis was used to determine differences among the marital status groups (married, divorced, never married) in mean number of outpatient visits per year with age as a covariate. With age accounted for, there were significant differences among the marital status groups (F[3, 11,130] = 104.37, P < .01). Married veterans averaged fewer visits per year (mean, 4.6; SD, 5.2) than did divorced veterans (mean, 6.2; SD, 9.9, P < .01) and never-married veterans (mean, 9.8; SD, 18.8, P < .01).
Nonpsychiatric hospitalizations. An ANCOVA analysis was used to determine group differences in nonpsychiatric hospitalizations per year with marital status as the independent variable and age as a covariate. With age accounted for, there were significant differences among the marital status groups (F[3, 11,130] = 43.97, P < .01). Married veterans averaged fewer nonpsychiatric hospitalizations per year (mean, 0.27; SD, 1.52) than did divorced veterans (mean, 0.47; SD, 1.30, P < .01) and never-married veterans (mean, 0.75; SD, 2.08, P <.01) Last, married veterans averaged fewer nonpsychiatric hospitalizations than did veterans with other/unknown marital status (mean, 0.5; SD, 1.5, P < .01).
Psychiatric hospitalizations. An ANCOVA analysis was used to determine group differences in mean number of psychiatric hospitalizations per year with marital status as the independent variable and age as a covariate. With age accounted for, there were significant differences among the marital status groups (F[3, 11,130] = 68.94, P < .01). Married veterans averaged fewer psychiatric hospitalizations per year (mean, 0.23; SD, 0.86) than did divorced veterans (mean, 0.55; SD, 1.58, P < .01) and nevermarried veterans (mean, 0.86; SD, 2.53, P < .01).
Predictors of Hospitalization
Regression analyses revealed that age, sex, divorced status, never-married status, mean number of visits, bipolar disorders, MDD, mood disorders NOS, unspecified psychotic disorders, residential MH treatment, ancillary services, and combat flag were all significant predictors of total number of both psychiatric hospitalizations (adjusted R2 = .15, F[128.56] = .00) and nonpsychiatric hospitalizations (adjusted R2 = .09, F[82.07] = .00) (Tables 3 & 4).
Discussion
This study examined medical and psychiatric service utilization in veterans with SMI diagnoses. For this population, 85.5% of the total number of VA visits were for MH services, and 52.1% of hospitalizations were for psychiatric care. Medical visits accounted for only 6.9% of outpatient services provided. Although the high utilization of psychiatric services by this SMI population may not be striking in itself, the considerably lower utilization of medical services is notable given the high rates of medical comorbidities associated with SMI. This result confirms findings from other studies.8-10,20 Possibly, VA health care guidelines may account for the lower medical service utilization. For example, the outpatient MH service has a metabolic syndrome clinic with psychiatrist prescribing guidelines for treating veterans who meet the criteria for metabolic syndrome.
The total number of outpatient visits varied widely. The largest percentage of veterans (29%) averaged 6 or more visits per year, followed by 2, 3, 1, and 4 visits. These findings suggest many patients are frequently utilizing services. The implications for inpatient hospitalization are notable, as the study’s data also suggest veterans with more total outpatient visits are at increased risk for hospitalization. The higher number of visits may be attributable to the SMI population’s increased health care needs and may suggest a need to target heavy users of outpatient services with more intensive programs to minimize costly hospitalizations. Mean number of outpatient visits was associated with a slightly higher risk for psychiatric hospitalization, possibly because of increased accessibility to care. Outpatient visits increased the risk for overall hospitalization, and psychiatric hospitalization specifically.
The type of SMI diagnosis predicted total number of outpatient visits, demonstrating that veterans with schizophrenic disorders averaged significantly more outpatient visits per year than did veterans with other SMI diagnoses. Interestingly, results showed that veterans with combat flags averaged significantly fewer outpatient visits than did veterans without flags. This finding is notable, as combat exposure is associated with higher rates of MH diagnoses and relatedly higher service utilization. However, combat veterans with SMI but not posttraumatic stress disorder (PTSD), averaged fewer outpatient visits than did veterans without combat exposure, which was not consistent with earlier findings.28 More research specifically on the effects of combat on veterans with PTSD may help in reconciling these findings. Married veterans averaged significantly fewer outpatient visits per year than did divorced or nevermarried veterans. It may be that social support among married couples is protective in veterans with SMI, or that veterans with SMI are unable to maintain marriages.
Hospitalization Predictors
Several significant predictors of psychiatric hospitalization were noted. Increasing age was negatively related to psychiatric hospitalization. It is possible that older patients with SMI receive other types of care, including board and care homes, or MH intensive case management, in which psychiatric outpatient care is readily provided—reducing the need for psychiatric hospitalization. In addition, married veterans were significantly less likely than were divorced and never-married veterans to have been hospitalized. It is possible that being married is protective for MH and physical health or that being unhealthy is a risk factor for divorce.
The type of SMI diagnosis also significantly predicted hospitalization. Having received specific types of services, including residential MH treatment and ancillary services, was a significant predictor of the total number of psychiatric hospitalizations. Last, having a combat flag negatively predicted psychiatric hospitalization—incongruent with earlier findings.24 These results suggest a profile of a veteran who likely could benefit either from a targeted intervention or from having ready access to a social worker.
Improved understanding of service utilization is vital to providing care to returning veterans. Mental disorders are very common among recent OEF, OIF, and Operation New Dawn veterans.29 As the rate of MH diagnoses climbs, the cost of providing health care grows exponentially. The cost of providing care to veterans with SMI can be addressed by identifying veteran-specific factors to provide intensive outreach and prevent costly hospitalization.
Limitations
The results of this study should be interpreted in light of several limitations. It is plausible that at least some veterans received health care services outside the VA, but non-VA data were not included in this study. Subsequent studies should include a group of veterans with SMI and a control group of veterans without SMI so that patterns of hospitalization and utilization rates can be compared. Also, the present study did not include data on missed appointments, an important variable in service utilization.
Missed appointments may suggest lack of follow-through with regular outpatient services, placing patients at risk for emergency services that require hospitalization. Veterans who had a single consultation were excluded in an effort to examine service utilization patterns of established patients. In future studies, including these patients could be informative in identifying specific patterns in this subpopulation. Fifth, PTSD was excluded from this study in order to identify utilization differences for veterans without PTSD.
Conclusion
Results of this study indicate that special attention should be given to veterans’ demographic and clinical factors, including age, sex, combat flags, marital status, and SMI diagnosis. Through identification of and outreach regarding these veteran-specific factors, it may be possible to use targeted interventions to reduce the need for inpatient hospitalization of veterans with chronic mental illness. Historically, the emphasis on access and outpatient care within the VA health care system drastically reduced the number of inpatient MH days.30 This outcome underscores the importance of outpatient services and suggests that targeted outpatient care can further reduce the need for inpatient MH care. Veterans with these outlined risk factors may benefit from implementation of early preventive measures.
Click here to read the digital edition.
About 10 million U.S. adults live with serious mental illness (SMI).1 Among military veterans, the number of mental health (MH) diagnoses is increasing with the return of troops from deployment in Iraq and Afghanistan.2-4 This increase has considerable implications for service use at the VA. An estimated 35% of army and marine veterans sought MH services within 1 year of returning from Iraq and Afghanistan.5 Furthermore, there is an association of MH disorders, physical illnesses, and mortality rates among veterans.2,6 Rising MH needs will increase the need for services; not unexpectedly, the VA is one of the largest providers of integrated health care in the U.S.7
Many patients with SMI have additional health issues, secondary to medication adverse effects, medical comorbidities, and other factors.8-12 Furthermore, their rates of preventable risk factors (eg, smoking, alcohol abuse, and poor exercise and diet13,14) are higher. Comorbid medical illnesses can sideline the treatment of mental illness and lead to negative health outcomes.15,16 These medical conditions coupled with SMI may increase overall rates of health care utilization in terms of outpatient visits, procedures, and inpatient hospitalizations. However, the literature on factors associated with health care utilization in veterans with SMI is scant and generally inconclusive.
Findings on utilization of non-MH medical services for veterans with comorbid MH diagnoses are mixed. Operation Enduring Freedom (OEF) and Operation Iraqi Freedom (OIF) veterans with MH diagnoses have been found to use significantly more non-MH medical services than do OEF and OIF veterans without these diagnoses.17 However, other studies have found that veterans with SMI seem to be less likely to use medical services.18,19 For example, in a study of the rate of medical visits for veterans with psychiatric diagnoses, veterans with SMI were found to have fewer outpatient medical visits than do other veterans without SMI.20 Given the high rates of medical comorbidities in veterans with SMI, this finding of reduced rates of medical care is both informative and concerning. However, more information on utilization rates for other types of health care system services is needed.
In addition to MH diagnoses, multiple factors influence the use of health care services. Lower income predicts overall use of mental and medical services for female but not male veterans.21 A large proportion of VA patients are male, and that disparity may affect female veterans’ perceptions and use of VA health care, underscoring the importance of examining the effects of sex in health care utilization.22 Unmarried status, unemployment, and combat experience are other factors associated with higher health care utilization.23,24 Sociodemographic factors, including income and possession of private health insurance, are associated with veterans’ use of VA health care services.25 It is important to understand the effects of these factors on service utilization by veterans with SMI in order to provide them with optimal, targeted health care.
The authors conducted this study to examine factors affecting MH service utilization and health outcomes in veterans with SMI at the VA Palo Alto Health Care System (VAPAHCS). A retrospective data analysis of medical records was performed. More specifically, this study aimed to identify veteran-specific variables (eg, demographics, psychiatric diagnosis, comorbid medical conditions, combat status) associated with health care utilization and outcomes in veterans with SMI. Dependent variables of interest included service utilization, such as rate and length of inpatient hospitalization and frequency of outpatient encounters. Examining predictors of inpatient medical and psychiatric hospitalization (demographic, clinical, or treatment-related factors) can provide insight into which veterans can benefit from targeted, intensive interventions. A better understanding of the factors affecting comprehensive health care service use for veterans with SMI can clarify targeted interventions and follow-up care for an expanding population.
Methods
Study approval was obtained from the institutional review board at Stanford University and the VAPAHCS research and development committee. Medical record data for veterans treated at the VAPAHCS were collected for a 10-year period (fiscal years 2003-2012). The Computerized Patient Record System (CPRS) data were accessed by VA decision support system staff and analyzed with SPSS Version 21.0 (Armonk, NY). Veterans were identified by ICD-9 codes 295.00 through 298.9, as documented in CPRS.
For this study, schizophrenic, psychotic, bipolar, depressive, and mood disorders were classified as SMI. VA clinic codes were used to categorize visits by service: medical (general medical clinic, surgery, pharmacy, laboratory tests), MH (outpatient visits, intakes and assessments), ancillary services (chaplain, social work, administration), residential MH treatment (substance use disorder, domiciliary care), home-based primary care, and home-based MH care. Psychiatric diagnoses were grouped into schizophrenic disorders, unspecified psychotic disorders, bipolar disorders, major depressive disorders (MDD), and mood disorders not otherwise specified (NOS). The demographic variables obtained through medical records included age, service connection, combat flag (deployment to combat zone), service period, and marital status at start of fiscal year 2003.
Over the 10-year period, 15,414 unique patients were classified as having SMI. Veterans who died during this period were removed from the dataset because of concerns about incomplete data (with specific dates of death unavailable, it was difficult to determine whether missed VA visits during a particular year indicated low utilization or death). In addition, inpatient medical and psychiatric visits were excluded from the analysis in an effort to identify how outpatient utilization uniquely affects the frequency of inpatient hospitalization. Last, because the authors wanted to exclude from the analysis all patients who may have had a single consultation at the VA during the 10-year period, they required at least 2 visits per patient. The final dataset consisted of 11,135 patients.
Age differences reported in the literature included a lesser likelihood of MH diagnosis for older returning OEF/OIF veterans,26 and older age as a factor related to veterans’ increased health care use.27 Therefore, age was included as a covariate in the analyses.
Results
The 11,135 patients included in the study, made a total of 350,523 outpatient visits over the period (Table 1). The mean number of outpatient visits was 6.6 (SD, 11.7; median, 3.5; mode, 2.0; range, 1.0-219.9). Over the 10-year period, 14.0% of patients averaged 1 visit per year, 23.4% averaged 2 visits, 15.6% averaged 3 visits, 10.7% averaged 4 visits, 7.4% averaged 5 visits, and 28.9% averaged 6 or more visits. Table 2 lists the frequencies and percentages of outpatient visits and hospitalizations.
Group Difference T-Test Analysis
Of the 553 OEF/OIF veterans in the study, 225 (40.7%) had combat flags, and 328 (59.3%) did not. Independent- groups t test showed significant group differences in mean number of visits (t[2,964.48] = 9.94, P < .01). Veterans with combat flags averaged significantly fewer visits per year (mean, 4.79; SD, 5.89) than did veterans without flags (mean, 6.89; SD, 12.50), even with age as a covariate (F[1, 10,675] = 34.63, P < .01).
Independent-groups t test showed significant group differences in mean number of nonpsychiatric hospitalizations (t[2,328.68] = 5.00, P < .01). Veterans with combat flags averaged significantly fewer nonpsychiatric hospitalizations per year (mean, 0.34; SD, .99) than did veterans without flags (mean, 0.51; SD, 1.71), even with age as a covariate (F[1, 10,675] = 9.81, P < .01).
Independent-groups t test showed significant group differences in mean number of psychiatric hospitalizations (t[2,706.75] = 7.69, P < .01). Veterans with combat flags averaged significantly fewer psychiatric hospitalizations per year (mean, 0.31; SD, 0.91) than did veterans without flags (mean, 0.55; SD, 1.80), even with age as a covariate (F[1, 10,675] = 23.51, P < .01).
Group Differences by SMI Diagnosis
Mean number of visits. Analysis of covariance (ANCOVA) was used to determine differences among the SMI groups (schizophrenic, psychotic, bipolar, depressive, and mood disorders) in mean number of outpatient visits per year with age as a covariate. With age accounted for, there were significant differences among the SMI groups (F[4, 11,129] = 285.02, P < .01). Therefore, pairwise comparisons were used to examine differences among individual disorders. Veterans with schizophrenic disorders averaged more visits per year (mean, 16.2; SD, 27.12) than did veterans with bipolar disorders (mean, 6.4; SD, 7.8, P < .01) and veterans with MDD (mean, 4.8; SD, 5.5, P < .01). Veterans with schizophrenia also averaged more visits per year than did veterans with mood disorders NOS (mean, 5.2; SD, 5.9, P < .01) and veterans with unspecified psychotic disorders (mean, 5.9; SD, 9.6, P < .01).
Nonpsychiatric hospitalizations. An ANCOVA analysis was used to determine group differences in nonpsychiatric hospitalizations per year with SMI diagnosis as the independent variable and age as a covariate. With age accounted for, there were significant differences among the SMI groups (F[4, 11,129] = 143.02, P < .01). Furthermore, pairwise comparisons were used to examine differences among individual disorders. Veterans with schizophrenic disorders averaged more nonpsychiatric hospitalizations (mean, 1.4; SD, 3.4) than did veterans with bipolar disorders (mean, 0.7; SD, 1.8, P < .01) and veterans with MDD (mean, 0.3; SD, 0.9, P < .01). Veterans with schizophrenia averaged more nonpsychiatric hospitalizations per year than did veterans with mood disorders NOS (mean, 0.3; SD, 0.8, P < .01) and veterans with unspecified psychotic disorders (mean, 0.5; SD, 1.2, P < .01).
Psychiatric hospitalizations. An ANCOVA analysis was used to determine group differences in psychiatric hospitalizations per year with SMI diagnosis as the independent variable and age as a covariate. With age accounted for, there were significant differences among the SMI groups (F[4, 11,129] = 204.64, P < .01). Furthermore, pairwise comparisons were used to examine differences among individual disorders. Veterans with schizophrenic disorders averaged more psychiatric hospitalizations per year (mean, 1.6; SD, 3.4) than did veterans with bipolar disorders (mean, 0.7; SD, 1.9, P < .01) and veterans with MDD (mean, 0.3; SD, 1.0, P < .01). Veterans with schizophrenia averaged more psychiatric hospitalizations per year than did veterans with mood disorders NOS (mean, 0.2; SD, 0.8, P < .01) and veterans with unspecified psychotic disorders (mean, 0.9; SD, 1.8, P < .01).
Group Differences by Marital Status
Mean number of visits. An ANCOVA analysis was used to determine differences among the marital status groups (married, divorced, never married) in mean number of outpatient visits per year with age as a covariate. With age accounted for, there were significant differences among the marital status groups (F[3, 11,130] = 104.37, P < .01). Married veterans averaged fewer visits per year (mean, 4.6; SD, 5.2) than did divorced veterans (mean, 6.2; SD, 9.9, P < .01) and never-married veterans (mean, 9.8; SD, 18.8, P < .01).
Nonpsychiatric hospitalizations. An ANCOVA analysis was used to determine group differences in nonpsychiatric hospitalizations per year with marital status as the independent variable and age as a covariate. With age accounted for, there were significant differences among the marital status groups (F[3, 11,130] = 43.97, P < .01). Married veterans averaged fewer nonpsychiatric hospitalizations per year (mean, 0.27; SD, 1.52) than did divorced veterans (mean, 0.47; SD, 1.30, P < .01) and never-married veterans (mean, 0.75; SD, 2.08, P <.01) Last, married veterans averaged fewer nonpsychiatric hospitalizations than did veterans with other/unknown marital status (mean, 0.5; SD, 1.5, P < .01).
Psychiatric hospitalizations. An ANCOVA analysis was used to determine group differences in mean number of psychiatric hospitalizations per year with marital status as the independent variable and age as a covariate. With age accounted for, there were significant differences among the marital status groups (F[3, 11,130] = 68.94, P < .01). Married veterans averaged fewer psychiatric hospitalizations per year (mean, 0.23; SD, 0.86) than did divorced veterans (mean, 0.55; SD, 1.58, P < .01) and nevermarried veterans (mean, 0.86; SD, 2.53, P < .01).
Predictors of Hospitalization
Regression analyses revealed that age, sex, divorced status, never-married status, mean number of visits, bipolar disorders, MDD, mood disorders NOS, unspecified psychotic disorders, residential MH treatment, ancillary services, and combat flag were all significant predictors of total number of both psychiatric hospitalizations (adjusted R2 = .15, F[128.56] = .00) and nonpsychiatric hospitalizations (adjusted R2 = .09, F[82.07] = .00) (Tables 3 & 4).
Discussion
This study examined medical and psychiatric service utilization in veterans with SMI diagnoses. For this population, 85.5% of the total number of VA visits were for MH services, and 52.1% of hospitalizations were for psychiatric care. Medical visits accounted for only 6.9% of outpatient services provided. Although the high utilization of psychiatric services by this SMI population may not be striking in itself, the considerably lower utilization of medical services is notable given the high rates of medical comorbidities associated with SMI. This result confirms findings from other studies.8-10,20 Possibly, VA health care guidelines may account for the lower medical service utilization. For example, the outpatient MH service has a metabolic syndrome clinic with psychiatrist prescribing guidelines for treating veterans who meet the criteria for metabolic syndrome.
The total number of outpatient visits varied widely. The largest percentage of veterans (29%) averaged 6 or more visits per year, followed by 2, 3, 1, and 4 visits. These findings suggest many patients are frequently utilizing services. The implications for inpatient hospitalization are notable, as the study’s data also suggest veterans with more total outpatient visits are at increased risk for hospitalization. The higher number of visits may be attributable to the SMI population’s increased health care needs and may suggest a need to target heavy users of outpatient services with more intensive programs to minimize costly hospitalizations. Mean number of outpatient visits was associated with a slightly higher risk for psychiatric hospitalization, possibly because of increased accessibility to care. Outpatient visits increased the risk for overall hospitalization, and psychiatric hospitalization specifically.
The type of SMI diagnosis predicted total number of outpatient visits, demonstrating that veterans with schizophrenic disorders averaged significantly more outpatient visits per year than did veterans with other SMI diagnoses. Interestingly, results showed that veterans with combat flags averaged significantly fewer outpatient visits than did veterans without flags. This finding is notable, as combat exposure is associated with higher rates of MH diagnoses and relatedly higher service utilization. However, combat veterans with SMI but not posttraumatic stress disorder (PTSD), averaged fewer outpatient visits than did veterans without combat exposure, which was not consistent with earlier findings.28 More research specifically on the effects of combat on veterans with PTSD may help in reconciling these findings. Married veterans averaged significantly fewer outpatient visits per year than did divorced or nevermarried veterans. It may be that social support among married couples is protective in veterans with SMI, or that veterans with SMI are unable to maintain marriages.
Hospitalization Predictors
Several significant predictors of psychiatric hospitalization were noted. Increasing age was negatively related to psychiatric hospitalization. It is possible that older patients with SMI receive other types of care, including board and care homes, or MH intensive case management, in which psychiatric outpatient care is readily provided—reducing the need for psychiatric hospitalization. In addition, married veterans were significantly less likely than were divorced and never-married veterans to have been hospitalized. It is possible that being married is protective for MH and physical health or that being unhealthy is a risk factor for divorce.
The type of SMI diagnosis also significantly predicted hospitalization. Having received specific types of services, including residential MH treatment and ancillary services, was a significant predictor of the total number of psychiatric hospitalizations. Last, having a combat flag negatively predicted psychiatric hospitalization—incongruent with earlier findings.24 These results suggest a profile of a veteran who likely could benefit either from a targeted intervention or from having ready access to a social worker.
Improved understanding of service utilization is vital to providing care to returning veterans. Mental disorders are very common among recent OEF, OIF, and Operation New Dawn veterans.29 As the rate of MH diagnoses climbs, the cost of providing health care grows exponentially. The cost of providing care to veterans with SMI can be addressed by identifying veteran-specific factors to provide intensive outreach and prevent costly hospitalization.
Limitations
The results of this study should be interpreted in light of several limitations. It is plausible that at least some veterans received health care services outside the VA, but non-VA data were not included in this study. Subsequent studies should include a group of veterans with SMI and a control group of veterans without SMI so that patterns of hospitalization and utilization rates can be compared. Also, the present study did not include data on missed appointments, an important variable in service utilization.
Missed appointments may suggest lack of follow-through with regular outpatient services, placing patients at risk for emergency services that require hospitalization. Veterans who had a single consultation were excluded in an effort to examine service utilization patterns of established patients. In future studies, including these patients could be informative in identifying specific patterns in this subpopulation. Fifth, PTSD was excluded from this study in order to identify utilization differences for veterans without PTSD.
Conclusion
Results of this study indicate that special attention should be given to veterans’ demographic and clinical factors, including age, sex, combat flags, marital status, and SMI diagnosis. Through identification of and outreach regarding these veteran-specific factors, it may be possible to use targeted interventions to reduce the need for inpatient hospitalization of veterans with chronic mental illness. Historically, the emphasis on access and outpatient care within the VA health care system drastically reduced the number of inpatient MH days.30 This outcome underscores the importance of outpatient services and suggests that targeted outpatient care can further reduce the need for inpatient MH care. Veterans with these outlined risk factors may benefit from implementation of early preventive measures.
Click here to read the digital edition.
1. Substance Abuse and Mental Health Services Administration. Results From the 2012 National Survey on Drug Use and Health: Mental Health Findings. NSDUH Series H-47, HHS publication SMA 13-4805. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2013.
2. Hoge CW, Terhakopian A, Castro CA, Messer SC, Engel CC. Association of posttraumatic stress disorder with somatic symptoms, health care visits, and absenteeism among Iraq war veterans. Am J Psychiatry. 2007;164(1):150-153.
3. Seal KH, Bertenthal D, Miner CR, Sen S, Marmar C. Bringing the war back home: mental health disorders among 103,788 US veterans returning from Iraq and Afghanistan seen at Department of Veterans Affairs facilities. Arch Intern Med. 2007;167(5):476-482.
4. Lee SE, Fonseca VP, Wolters CL, et al. Health care utilization behavior of veterans who deployed to Afghanistan and Iraq. Mil Med. 2015;180(4):374-379.
5. Hoge CW, Auchterlonie JL, Milliken CS. Mental health problems, use of mental health services, and attrition from military service after returning from deployment to Iraq or Afghanistan. JAMA. 2006;295(9):1023-1032.
6. Kramarow EA, Pastor PN. The health of male veterans and nonveterans aged 25-64: United States, 2007-2010. NCHS Data Brief. 2012;(101):1-8.
7. Elbogen EB, Wagner HR, Johnson SC, et al. Are Iraq and Afghanistan veterans using mental health services? New data from a national random-sample survey. Psychiatr Serv. 2013;64(2):134-141.
8. Bermudes RA, Keck PE Jr, Welge JA. The prevalence of the metabolic syndrome in psychiatric inpatients with primary psychotic and mood disorders. Psychosomatics. 2006;47(6):491-497.
9. Newcomer JW. Metabolic syndrome and mental illness. Am J Manag Care. 2007;13(7 suppl):S170-S177.
10. Toalson P, Ahmed S, Hardy T, Kabinoff G. The metabolic syndrome in patients with severe mental illnesses. Prim Care Companion J Clin Psychiatry. 2004;6(4):152-158.
11. Khatana SA, Kane J, Taveira TH, Bauer MS, Wu WC. Monitoring and prevalence rates of metabolic syndrome in military veterans with serious mental illness. PLoS One. 2011;6(4):e19298.
12. De Hert M, Correll CU, Bobes J, et al. Physical illness in patients with severe mental disorders. I. Prevalence, impact of medications and disparities in health care. World Psychiatry. 2011;10(1):52-77.
13. Lambert TJ, Velakoulis D, Pantelis C. Medical comorbidity in schizophrenia. Med J Aust. 2003;178(suppl):S67-S70.
14. Osborn DP, Nazareth I, King MB. Physical activity, dietary habits, and coronary heart disease risk factor knowledge amongst people with severe mental illness: a cross sectional comparative study in primary care. Soc Psychiatry Psychiatr Epidemiol. 2007;42(10):787-793.
15. Newcomer JW. Medical risk in patients with bipolar disorder and schizophrenia. J Clin Psychiatry. 2007;67(suppl 9):25-30, discussion 36-42.
16. Chwastiak LA, Rosenheck RA, Kazis LE. Association of psychiatric illness and obesity, physical inactivity, and smoking among a national sample of veterans. Psychosomatics. 2011;52(3):230-236.
17. Cohen BE, Gima K, Bertenthal D, Kim S, Marmar CR, Seal KH. Mental health diagnoses and utilization of VA non-mental health medical services among returning Iraq and Afghanistan veterans. J Gen Intern Med. 2010;25(1):18-24.
18. Chwastiak LA, Rosenheck RA, Kazis LE. Utilization of primary care of veterans with psychiatric illness in the national Department of Veterans Affairs Health Care System. J Gen Intern Med. 2008;23(11):1835-1840.
19. VA Office of Research and Development, Health Services Research and Development Service, Quality Enhancement Research Initiative. Mental health. QUERI fact sheet. http://www.hsrd.research.va.gov/publications/internal/mh_factsheet.pdf. Published December 2008. Accessed January 13, 2017.
20. Cradock-O’Leary J, Young AS, Yano EM, Wang M, Lee ML. Use of general medical services by VA patients with psychiatric disorders. Psychiatr Serv. 2002;53(7):874-878.
21. Di Leone BA, Vogt D, Gradus JL, Street AE, Giasson HL, Resick PA. Predictors of mental health care use among male and female veterans deployed in support of the wars in Afghanistan and Iraq. Psychol Serv. 2013;10(2):145-151.
22. Vogt DS, Barry AA, King LA. Toward gender-aware health care: evaluation of an intervention to enhance care for female patients in the VA setting. J Health Psychol. 2008;13(5):624-638.
23. Marshall RP, Jorm AF, Grayson DA, O’Toole BI. Posttraumatic stress disorder and other predictors of health care consumption by Vietnam veterans. Psychiatr Serv. 1998;49(12):1609-1611.
24. Rosenheck R, Massari L. Wartime military service and utilization of VA health care services. Mil Med. 1993;158(4):223-228.
25. Elhai JD, Grubaugh AL, Richardson JD, Egede LE, Creamer M. Outpatient medical and mental healthcare utilization models among military veterans: results from the 2001 National Survey of Veterans. J Psychiatr Res. 2008;42(10):858-867.
26. Seal KH, Bertenthal D, Miner CR, Sen S, Marmar C. Bringing the war back home: mental health disorders among 103,788 US veterans returning from Iraq and Afghanistan seen at Department of Veterans Affairs facilities. Arch Intern Med. 2007;167(5):476-482.
27. Fasoli DR, Glickman ME, Eisen SV. Predisposing characteristics, enabling resources and need as predictors of utilization and clinical outcomes for veterans receiving mental health services. Med Care. 2010;48(4):288-295.
28. Maguen S, Schumm JA, Norris RL, et al. Predictors of mental and physical health service utilization among Vietnam veterans. Psychol Serv. 2007;4(3):168-180.
29. Office of Public Health, Veterans Health Administration. Analysis of VA Health Care Utilization Among Operation Enduring Freedom (OEF), Operation Iraqi Freedom (OIF), and Operation New Dawn (OND) Veterans—Revised. http://www.publichealth.va.gov/docs/epidemiology/healthcare-utilization-report-fy2012-qtr3.pdf. Revised December 2012. Accessed February 6, 2017.
30. Wagner TH, Sinnott P, Siroka AM. Mental health and substance use disorder spending in the Department of Veterans Affairs, fiscal years 2000-2007. Psychiatr Serv. 2011;62(4):389-395.
1. Substance Abuse and Mental Health Services Administration. Results From the 2012 National Survey on Drug Use and Health: Mental Health Findings. NSDUH Series H-47, HHS publication SMA 13-4805. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2013.
2. Hoge CW, Terhakopian A, Castro CA, Messer SC, Engel CC. Association of posttraumatic stress disorder with somatic symptoms, health care visits, and absenteeism among Iraq war veterans. Am J Psychiatry. 2007;164(1):150-153.
3. Seal KH, Bertenthal D, Miner CR, Sen S, Marmar C. Bringing the war back home: mental health disorders among 103,788 US veterans returning from Iraq and Afghanistan seen at Department of Veterans Affairs facilities. Arch Intern Med. 2007;167(5):476-482.
4. Lee SE, Fonseca VP, Wolters CL, et al. Health care utilization behavior of veterans who deployed to Afghanistan and Iraq. Mil Med. 2015;180(4):374-379.
5. Hoge CW, Auchterlonie JL, Milliken CS. Mental health problems, use of mental health services, and attrition from military service after returning from deployment to Iraq or Afghanistan. JAMA. 2006;295(9):1023-1032.
6. Kramarow EA, Pastor PN. The health of male veterans and nonveterans aged 25-64: United States, 2007-2010. NCHS Data Brief. 2012;(101):1-8.
7. Elbogen EB, Wagner HR, Johnson SC, et al. Are Iraq and Afghanistan veterans using mental health services? New data from a national random-sample survey. Psychiatr Serv. 2013;64(2):134-141.
8. Bermudes RA, Keck PE Jr, Welge JA. The prevalence of the metabolic syndrome in psychiatric inpatients with primary psychotic and mood disorders. Psychosomatics. 2006;47(6):491-497.
9. Newcomer JW. Metabolic syndrome and mental illness. Am J Manag Care. 2007;13(7 suppl):S170-S177.
10. Toalson P, Ahmed S, Hardy T, Kabinoff G. The metabolic syndrome in patients with severe mental illnesses. Prim Care Companion J Clin Psychiatry. 2004;6(4):152-158.
11. Khatana SA, Kane J, Taveira TH, Bauer MS, Wu WC. Monitoring and prevalence rates of metabolic syndrome in military veterans with serious mental illness. PLoS One. 2011;6(4):e19298.
12. De Hert M, Correll CU, Bobes J, et al. Physical illness in patients with severe mental disorders. I. Prevalence, impact of medications and disparities in health care. World Psychiatry. 2011;10(1):52-77.
13. Lambert TJ, Velakoulis D, Pantelis C. Medical comorbidity in schizophrenia. Med J Aust. 2003;178(suppl):S67-S70.
14. Osborn DP, Nazareth I, King MB. Physical activity, dietary habits, and coronary heart disease risk factor knowledge amongst people with severe mental illness: a cross sectional comparative study in primary care. Soc Psychiatry Psychiatr Epidemiol. 2007;42(10):787-793.
15. Newcomer JW. Medical risk in patients with bipolar disorder and schizophrenia. J Clin Psychiatry. 2007;67(suppl 9):25-30, discussion 36-42.
16. Chwastiak LA, Rosenheck RA, Kazis LE. Association of psychiatric illness and obesity, physical inactivity, and smoking among a national sample of veterans. Psychosomatics. 2011;52(3):230-236.
17. Cohen BE, Gima K, Bertenthal D, Kim S, Marmar CR, Seal KH. Mental health diagnoses and utilization of VA non-mental health medical services among returning Iraq and Afghanistan veterans. J Gen Intern Med. 2010;25(1):18-24.
18. Chwastiak LA, Rosenheck RA, Kazis LE. Utilization of primary care of veterans with psychiatric illness in the national Department of Veterans Affairs Health Care System. J Gen Intern Med. 2008;23(11):1835-1840.
19. VA Office of Research and Development, Health Services Research and Development Service, Quality Enhancement Research Initiative. Mental health. QUERI fact sheet. http://www.hsrd.research.va.gov/publications/internal/mh_factsheet.pdf. Published December 2008. Accessed January 13, 2017.
20. Cradock-O’Leary J, Young AS, Yano EM, Wang M, Lee ML. Use of general medical services by VA patients with psychiatric disorders. Psychiatr Serv. 2002;53(7):874-878.
21. Di Leone BA, Vogt D, Gradus JL, Street AE, Giasson HL, Resick PA. Predictors of mental health care use among male and female veterans deployed in support of the wars in Afghanistan and Iraq. Psychol Serv. 2013;10(2):145-151.
22. Vogt DS, Barry AA, King LA. Toward gender-aware health care: evaluation of an intervention to enhance care for female patients in the VA setting. J Health Psychol. 2008;13(5):624-638.
23. Marshall RP, Jorm AF, Grayson DA, O’Toole BI. Posttraumatic stress disorder and other predictors of health care consumption by Vietnam veterans. Psychiatr Serv. 1998;49(12):1609-1611.
24. Rosenheck R, Massari L. Wartime military service and utilization of VA health care services. Mil Med. 1993;158(4):223-228.
25. Elhai JD, Grubaugh AL, Richardson JD, Egede LE, Creamer M. Outpatient medical and mental healthcare utilization models among military veterans: results from the 2001 National Survey of Veterans. J Psychiatr Res. 2008;42(10):858-867.
26. Seal KH, Bertenthal D, Miner CR, Sen S, Marmar C. Bringing the war back home: mental health disorders among 103,788 US veterans returning from Iraq and Afghanistan seen at Department of Veterans Affairs facilities. Arch Intern Med. 2007;167(5):476-482.
27. Fasoli DR, Glickman ME, Eisen SV. Predisposing characteristics, enabling resources and need as predictors of utilization and clinical outcomes for veterans receiving mental health services. Med Care. 2010;48(4):288-295.
28. Maguen S, Schumm JA, Norris RL, et al. Predictors of mental and physical health service utilization among Vietnam veterans. Psychol Serv. 2007;4(3):168-180.
29. Office of Public Health, Veterans Health Administration. Analysis of VA Health Care Utilization Among Operation Enduring Freedom (OEF), Operation Iraqi Freedom (OIF), and Operation New Dawn (OND) Veterans—Revised. http://www.publichealth.va.gov/docs/epidemiology/healthcare-utilization-report-fy2012-qtr3.pdf. Revised December 2012. Accessed February 6, 2017.
30. Wagner TH, Sinnott P, Siroka AM. Mental health and substance use disorder spending in the Department of Veterans Affairs, fiscal years 2000-2007. Psychiatr Serv. 2011;62(4):389-395.