User login
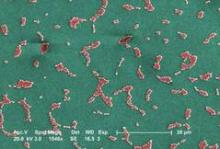
DALLAS – In a surprising twist, multidrug resistance and antibiotic appropriateness were not correlated with mortality in a retrospective analysis of critically ill patients infected with Acinetobacter bacillus.
Acinetobacter infections among critically ill patients are increasing and have been associated with mortality rates of 26%-68%. The mortality rates are thought to be driven by high rates of multidrug resistance and subsequent delays in appropriate antimicrobial therapy, Claire Murphy, Pharm.D., explained at the annual meeting of the Surgical Infection Society.
She presented data on 156 surgical and medical ICU patients with at least one positive Acinetobacter culture and associated clinical symptoms who were admitted to an ICU between January 2006 and December 2009. In-hospital mortality was 35%.
Patients who died had significantly higher APACHE II (Acute Physiology and Chronic Health Evaluation II) II scores than did survivors (22.3 vs. 19.5; P = .02), and were more likely to be surgical patients (50% vs. 33.3%; P = .04) and to be in an immunosuppressed state (33.3% vs. 16.7%; P = .02).
Survivors were significantly younger (53 years vs. 59 years; P = .006), and – inexplicably – more likely to have prior colonization or infection with methicillin-resistant Staphylococcus aureus (4% vs. 2%; P = .04), said Dr. Murphy of the department of surgery at the Ohio State University, Columbus.
Respiratory infections were the most common source of Acinetobacter for all patients. Survivors were more likely to have respiratory sources of infection (82.5% vs. 67%; P = .02), whereas nonsurvivors had a higher incidence of Acinetobacter bacteremia, including both secondary and catheter-related bacteremias (43% vs. 8%; P less than .001).
Multidrug resistance rates were similar among survivors and nonsurvivors at 64% and 70.4%, respectively, although there was a slight trend toward increased resistance among nonsurvivors for cefepime (Maxipime), impinem (Primaxin IV/Primaxin IM), and tigecycline (Tygacil), she said.
Rates of appropriate empirical antibiotic coverage were not significantly different, at 18.5% among nonsurvivors and 28.4% among survivors, although survivors were more likely to receive a broad-spectrum carbapenem as empirical therapy (33% vs. 17%; P = .02).
ICU stay, hospital length of stay, and duration of mechanical ventilation were also similar.
In a multivariate analysis that was adjusted for potential confounders, the independent predictors of mortality were bacteremia (odds ratio, 14.1; P less than .001), immunosuppression (OR, 2.76; P = .04), and higher severity of illness by APACHE II score (OR, 1.1; P = .002).
The use of the carbapenem antibiotic imipenem as directed therapy was protective (OR, 0.29; P = .012).
"A carbapenem should be considered for [empirical] therapy in ICU patients at risk for Acinetobacter infection," Dr. Murphy said.
Invited discussant Dr. Nicholas Namias, chief of trauma and professor of surgery at the University of Miami Health System, observed that the 35% mortality rate was disturbingly high, but not unexpected. He asked whether the use of carbapenems was forced, in a sense, by the susceptibility pattern of the isolate, and whether patients might have done better if they had been given an antibiotic like colistin.
Dr. Murphy agreed that the choice of carbapenem was directed by susceptibility patterns, and remarked that clinicians tend to lean toward a carbapenem because they’re more comfortable administering and dosing a carbapenem (particularly in complex cases, such as obese patients or those on renal replacement therapy) than colistin.
Dr. Namias also asked how empirical therapy is selected, and how the results might look if only carbapenem-resistant patients were included in the analysis. Dr. Murphy replied that the hospital does not have a fixed rotation, but reviews its ICU-specific antibiograms on an annual basis to determine its standard empirical therapy.
The investigators plan to study outcomes in carbapenem-resistant patients, said Dr. Murphy, but she pointed out that more than half of the patients in the current study were carbapenem resistant. She suggested that a carbapenem may still be beneficial in this setting because there are in vitro data showing synergy between carbapenems and other antibiotics, including colistin, tigecycline, and amikacin. Extended infusions of impinem were not used during the study period, although the hospital recently began using 4-hour infusions of doripenem (Doribax).
The authors reported no relevant conflicts of interest.
DALLAS – In a surprising twist, multidrug resistance and antibiotic appropriateness were not correlated with mortality in a retrospective analysis of critically ill patients infected with Acinetobacter bacillus.
Acinetobacter infections among critically ill patients are increasing and have been associated with mortality rates of 26%-68%. The mortality rates are thought to be driven by high rates of multidrug resistance and subsequent delays in appropriate antimicrobial therapy, Claire Murphy, Pharm.D., explained at the annual meeting of the Surgical Infection Society.
She presented data on 156 surgical and medical ICU patients with at least one positive Acinetobacter culture and associated clinical symptoms who were admitted to an ICU between January 2006 and December 2009. In-hospital mortality was 35%.
Patients who died had significantly higher APACHE II (Acute Physiology and Chronic Health Evaluation II) II scores than did survivors (22.3 vs. 19.5; P = .02), and were more likely to be surgical patients (50% vs. 33.3%; P = .04) and to be in an immunosuppressed state (33.3% vs. 16.7%; P = .02).
Survivors were significantly younger (53 years vs. 59 years; P = .006), and – inexplicably – more likely to have prior colonization or infection with methicillin-resistant Staphylococcus aureus (4% vs. 2%; P = .04), said Dr. Murphy of the department of surgery at the Ohio State University, Columbus.
Respiratory infections were the most common source of Acinetobacter for all patients. Survivors were more likely to have respiratory sources of infection (82.5% vs. 67%; P = .02), whereas nonsurvivors had a higher incidence of Acinetobacter bacteremia, including both secondary and catheter-related bacteremias (43% vs. 8%; P less than .001).
Multidrug resistance rates were similar among survivors and nonsurvivors at 64% and 70.4%, respectively, although there was a slight trend toward increased resistance among nonsurvivors for cefepime (Maxipime), impinem (Primaxin IV/Primaxin IM), and tigecycline (Tygacil), she said.
Rates of appropriate empirical antibiotic coverage were not significantly different, at 18.5% among nonsurvivors and 28.4% among survivors, although survivors were more likely to receive a broad-spectrum carbapenem as empirical therapy (33% vs. 17%; P = .02).
ICU stay, hospital length of stay, and duration of mechanical ventilation were also similar.
In a multivariate analysis that was adjusted for potential confounders, the independent predictors of mortality were bacteremia (odds ratio, 14.1; P less than .001), immunosuppression (OR, 2.76; P = .04), and higher severity of illness by APACHE II score (OR, 1.1; P = .002).
The use of the carbapenem antibiotic imipenem as directed therapy was protective (OR, 0.29; P = .012).
"A carbapenem should be considered for [empirical] therapy in ICU patients at risk for Acinetobacter infection," Dr. Murphy said.
Invited discussant Dr. Nicholas Namias, chief of trauma and professor of surgery at the University of Miami Health System, observed that the 35% mortality rate was disturbingly high, but not unexpected. He asked whether the use of carbapenems was forced, in a sense, by the susceptibility pattern of the isolate, and whether patients might have done better if they had been given an antibiotic like colistin.
Dr. Murphy agreed that the choice of carbapenem was directed by susceptibility patterns, and remarked that clinicians tend to lean toward a carbapenem because they’re more comfortable administering and dosing a carbapenem (particularly in complex cases, such as obese patients or those on renal replacement therapy) than colistin.
Dr. Namias also asked how empirical therapy is selected, and how the results might look if only carbapenem-resistant patients were included in the analysis. Dr. Murphy replied that the hospital does not have a fixed rotation, but reviews its ICU-specific antibiograms on an annual basis to determine its standard empirical therapy.
The investigators plan to study outcomes in carbapenem-resistant patients, said Dr. Murphy, but she pointed out that more than half of the patients in the current study were carbapenem resistant. She suggested that a carbapenem may still be beneficial in this setting because there are in vitro data showing synergy between carbapenems and other antibiotics, including colistin, tigecycline, and amikacin. Extended infusions of impinem were not used during the study period, although the hospital recently began using 4-hour infusions of doripenem (Doribax).
The authors reported no relevant conflicts of interest.
DALLAS – In a surprising twist, multidrug resistance and antibiotic appropriateness were not correlated with mortality in a retrospective analysis of critically ill patients infected with Acinetobacter bacillus.
Acinetobacter infections among critically ill patients are increasing and have been associated with mortality rates of 26%-68%. The mortality rates are thought to be driven by high rates of multidrug resistance and subsequent delays in appropriate antimicrobial therapy, Claire Murphy, Pharm.D., explained at the annual meeting of the Surgical Infection Society.
She presented data on 156 surgical and medical ICU patients with at least one positive Acinetobacter culture and associated clinical symptoms who were admitted to an ICU between January 2006 and December 2009. In-hospital mortality was 35%.
Patients who died had significantly higher APACHE II (Acute Physiology and Chronic Health Evaluation II) II scores than did survivors (22.3 vs. 19.5; P = .02), and were more likely to be surgical patients (50% vs. 33.3%; P = .04) and to be in an immunosuppressed state (33.3% vs. 16.7%; P = .02).
Survivors were significantly younger (53 years vs. 59 years; P = .006), and – inexplicably – more likely to have prior colonization or infection with methicillin-resistant Staphylococcus aureus (4% vs. 2%; P = .04), said Dr. Murphy of the department of surgery at the Ohio State University, Columbus.
Respiratory infections were the most common source of Acinetobacter for all patients. Survivors were more likely to have respiratory sources of infection (82.5% vs. 67%; P = .02), whereas nonsurvivors had a higher incidence of Acinetobacter bacteremia, including both secondary and catheter-related bacteremias (43% vs. 8%; P less than .001).
Multidrug resistance rates were similar among survivors and nonsurvivors at 64% and 70.4%, respectively, although there was a slight trend toward increased resistance among nonsurvivors for cefepime (Maxipime), impinem (Primaxin IV/Primaxin IM), and tigecycline (Tygacil), she said.
Rates of appropriate empirical antibiotic coverage were not significantly different, at 18.5% among nonsurvivors and 28.4% among survivors, although survivors were more likely to receive a broad-spectrum carbapenem as empirical therapy (33% vs. 17%; P = .02).
ICU stay, hospital length of stay, and duration of mechanical ventilation were also similar.
In a multivariate analysis that was adjusted for potential confounders, the independent predictors of mortality were bacteremia (odds ratio, 14.1; P less than .001), immunosuppression (OR, 2.76; P = .04), and higher severity of illness by APACHE II score (OR, 1.1; P = .002).
The use of the carbapenem antibiotic imipenem as directed therapy was protective (OR, 0.29; P = .012).
"A carbapenem should be considered for [empirical] therapy in ICU patients at risk for Acinetobacter infection," Dr. Murphy said.
Invited discussant Dr. Nicholas Namias, chief of trauma and professor of surgery at the University of Miami Health System, observed that the 35% mortality rate was disturbingly high, but not unexpected. He asked whether the use of carbapenems was forced, in a sense, by the susceptibility pattern of the isolate, and whether patients might have done better if they had been given an antibiotic like colistin.
Dr. Murphy agreed that the choice of carbapenem was directed by susceptibility patterns, and remarked that clinicians tend to lean toward a carbapenem because they’re more comfortable administering and dosing a carbapenem (particularly in complex cases, such as obese patients or those on renal replacement therapy) than colistin.
Dr. Namias also asked how empirical therapy is selected, and how the results might look if only carbapenem-resistant patients were included in the analysis. Dr. Murphy replied that the hospital does not have a fixed rotation, but reviews its ICU-specific antibiograms on an annual basis to determine its standard empirical therapy.
The investigators plan to study outcomes in carbapenem-resistant patients, said Dr. Murphy, but she pointed out that more than half of the patients in the current study were carbapenem resistant. She suggested that a carbapenem may still be beneficial in this setting because there are in vitro data showing synergy between carbapenems and other antibiotics, including colistin, tigecycline, and amikacin. Extended infusions of impinem were not used during the study period, although the hospital recently began using 4-hour infusions of doripenem (Doribax).
The authors reported no relevant conflicts of interest.
FROM THE ANNUAL MEETING OF THE SURGICAL INFECTION SOCIETY