User login
Hospitalist Staffing Affects 30-Day All-Cause Readmission Rates
Background: The Centers for Medicare & Medicaid Services (CMS) tracks 30-day all-cause readmission rates as a quality measure. Prior studies have looked at various hospital factors associated with lower readmission rates but have not looked at hospitalist staffing levels, level of physician integration with the hospital, and the adoption of a medical home model.
Study design: Retrospective cohort study.
Setting: Private hospitals.
Synopsis: Using the American Hospital Association Annual Survey of Hospitals, CMS Hospital Compare, and Area Health Resources File of private hospitals with no missing data, the study reviewed data from 1,756 hospitals and found the median 30-day all-cause readmission rate to be 16%, with the middle 50% of hospitals’ readmission rate between 15.2% and 16.5%. All hospitals used hospitalists to provide care. Fifty-one percent of hospitals reported fully integrated, or employed, physicians. Twenty-nine percent reported establishment of a medical home.
The study found that higher hospitalist staffing levels were associated with significantly lower readmission rates. Fully integrated hospitals had a lower readmission rate than not fully integrated (15.86% versus 15.93%). Also, physician-owned hospitals had a lower readmission rate than non-physician-owned hospitals, and hospitals that had adopted a medical home model had significantly lower readmission rates. Readmission rates were significantly higher for major teaching hospitals (16.9% versus 15.76% minor teaching versus 15.83% nonteaching).
Bottom line: High hospitalist staffing levels, full integration of the hospitalists, and physician-owned hospitals were associated with lower 30-day all-cause readmission rates for private hospitals.
Citation: Al-Amin M. Hospital characteristics and 30-day all-cause readmission rates [published online ahead of print May 17, 2016]. J Hosp Med. doi:10.1002/jhm.2606
Background: The Centers for Medicare & Medicaid Services (CMS) tracks 30-day all-cause readmission rates as a quality measure. Prior studies have looked at various hospital factors associated with lower readmission rates but have not looked at hospitalist staffing levels, level of physician integration with the hospital, and the adoption of a medical home model.
Study design: Retrospective cohort study.
Setting: Private hospitals.
Synopsis: Using the American Hospital Association Annual Survey of Hospitals, CMS Hospital Compare, and Area Health Resources File of private hospitals with no missing data, the study reviewed data from 1,756 hospitals and found the median 30-day all-cause readmission rate to be 16%, with the middle 50% of hospitals’ readmission rate between 15.2% and 16.5%. All hospitals used hospitalists to provide care. Fifty-one percent of hospitals reported fully integrated, or employed, physicians. Twenty-nine percent reported establishment of a medical home.
The study found that higher hospitalist staffing levels were associated with significantly lower readmission rates. Fully integrated hospitals had a lower readmission rate than not fully integrated (15.86% versus 15.93%). Also, physician-owned hospitals had a lower readmission rate than non-physician-owned hospitals, and hospitals that had adopted a medical home model had significantly lower readmission rates. Readmission rates were significantly higher for major teaching hospitals (16.9% versus 15.76% minor teaching versus 15.83% nonteaching).
Bottom line: High hospitalist staffing levels, full integration of the hospitalists, and physician-owned hospitals were associated with lower 30-day all-cause readmission rates for private hospitals.
Citation: Al-Amin M. Hospital characteristics and 30-day all-cause readmission rates [published online ahead of print May 17, 2016]. J Hosp Med. doi:10.1002/jhm.2606
Background: The Centers for Medicare & Medicaid Services (CMS) tracks 30-day all-cause readmission rates as a quality measure. Prior studies have looked at various hospital factors associated with lower readmission rates but have not looked at hospitalist staffing levels, level of physician integration with the hospital, and the adoption of a medical home model.
Study design: Retrospective cohort study.
Setting: Private hospitals.
Synopsis: Using the American Hospital Association Annual Survey of Hospitals, CMS Hospital Compare, and Area Health Resources File of private hospitals with no missing data, the study reviewed data from 1,756 hospitals and found the median 30-day all-cause readmission rate to be 16%, with the middle 50% of hospitals’ readmission rate between 15.2% and 16.5%. All hospitals used hospitalists to provide care. Fifty-one percent of hospitals reported fully integrated, or employed, physicians. Twenty-nine percent reported establishment of a medical home.
The study found that higher hospitalist staffing levels were associated with significantly lower readmission rates. Fully integrated hospitals had a lower readmission rate than not fully integrated (15.86% versus 15.93%). Also, physician-owned hospitals had a lower readmission rate than non-physician-owned hospitals, and hospitals that had adopted a medical home model had significantly lower readmission rates. Readmission rates were significantly higher for major teaching hospitals (16.9% versus 15.76% minor teaching versus 15.83% nonteaching).
Bottom line: High hospitalist staffing levels, full integration of the hospitalists, and physician-owned hospitals were associated with lower 30-day all-cause readmission rates for private hospitals.
Citation: Al-Amin M. Hospital characteristics and 30-day all-cause readmission rates [published online ahead of print May 17, 2016]. J Hosp Med. doi:10.1002/jhm.2606
Oral Antibiotics for Infective Endocarditis May Be Safe in Low-Risk Patients
Background: Treating infective endocarditis with four to six weeks of intravenous antibiotics carries a high cost. There are data to support oral antibiotics for right-sided endocarditis due to methicillin-sensitive Staphylococcus aureus (with ciprofloxacin and rifampicin), but experience in using oral antibiotics for infective endocarditis is limited.
Study design: Cohort study.
Setting: Large academic hospital in France.
Synopsis: The researchers included 426 patients with definitive or probable endocarditis by Duke criteria. After an initial period of treatment with intravenous (IV) antibiotics, 50% of the identified group was transitioned to oral antibiotics (amoxicillin alone in 50% and combinations of fluoroquinolones, rifampicin, amoxicillin, and clindamycin in the others).
The risk of death was not increased in the group treated with oral antibiotics when adjusted for the four biggest predictors of death (age >65, type 1 diabetes mellitus, disinsertion of prosthetic valve, and endocarditis due to S. aureus). Nine patients treated with IV antibiotics experienced relapsed endocarditis compared to two patients treated with oral antibiotics.
Patients selected for treatment with oral antibiotics were less likely to have severe disease, significant comorbidities, or infection with S. aureus. The length of treatment with IV antibiotics before switching to oral antibiotics varied widely.
Bottom line: It’s possible low-risk patients with infective endocarditis may be treated with oral antibiotics, but more data are needed.
Citation: Mzabi A, Kernéis S, Richaud C, Podglajen I, Fernandez-Gerlinger MP, Mainardi, JL. Switch to oral antibiotics in the treatment of infective endocarditis is not associated with increased risk of mortality in non-severely ill patients [published online ahead of print April 16, 2016]. Clin Microbiol Infect. doi:10.1016/j.cmi.2016.04.003.
Background: Treating infective endocarditis with four to six weeks of intravenous antibiotics carries a high cost. There are data to support oral antibiotics for right-sided endocarditis due to methicillin-sensitive Staphylococcus aureus (with ciprofloxacin and rifampicin), but experience in using oral antibiotics for infective endocarditis is limited.
Study design: Cohort study.
Setting: Large academic hospital in France.
Synopsis: The researchers included 426 patients with definitive or probable endocarditis by Duke criteria. After an initial period of treatment with intravenous (IV) antibiotics, 50% of the identified group was transitioned to oral antibiotics (amoxicillin alone in 50% and combinations of fluoroquinolones, rifampicin, amoxicillin, and clindamycin in the others).
The risk of death was not increased in the group treated with oral antibiotics when adjusted for the four biggest predictors of death (age >65, type 1 diabetes mellitus, disinsertion of prosthetic valve, and endocarditis due to S. aureus). Nine patients treated with IV antibiotics experienced relapsed endocarditis compared to two patients treated with oral antibiotics.
Patients selected for treatment with oral antibiotics were less likely to have severe disease, significant comorbidities, or infection with S. aureus. The length of treatment with IV antibiotics before switching to oral antibiotics varied widely.
Bottom line: It’s possible low-risk patients with infective endocarditis may be treated with oral antibiotics, but more data are needed.
Citation: Mzabi A, Kernéis S, Richaud C, Podglajen I, Fernandez-Gerlinger MP, Mainardi, JL. Switch to oral antibiotics in the treatment of infective endocarditis is not associated with increased risk of mortality in non-severely ill patients [published online ahead of print April 16, 2016]. Clin Microbiol Infect. doi:10.1016/j.cmi.2016.04.003.
Background: Treating infective endocarditis with four to six weeks of intravenous antibiotics carries a high cost. There are data to support oral antibiotics for right-sided endocarditis due to methicillin-sensitive Staphylococcus aureus (with ciprofloxacin and rifampicin), but experience in using oral antibiotics for infective endocarditis is limited.
Study design: Cohort study.
Setting: Large academic hospital in France.
Synopsis: The researchers included 426 patients with definitive or probable endocarditis by Duke criteria. After an initial period of treatment with intravenous (IV) antibiotics, 50% of the identified group was transitioned to oral antibiotics (amoxicillin alone in 50% and combinations of fluoroquinolones, rifampicin, amoxicillin, and clindamycin in the others).
The risk of death was not increased in the group treated with oral antibiotics when adjusted for the four biggest predictors of death (age >65, type 1 diabetes mellitus, disinsertion of prosthetic valve, and endocarditis due to S. aureus). Nine patients treated with IV antibiotics experienced relapsed endocarditis compared to two patients treated with oral antibiotics.
Patients selected for treatment with oral antibiotics were less likely to have severe disease, significant comorbidities, or infection with S. aureus. The length of treatment with IV antibiotics before switching to oral antibiotics varied widely.
Bottom line: It’s possible low-risk patients with infective endocarditis may be treated with oral antibiotics, but more data are needed.
Citation: Mzabi A, Kernéis S, Richaud C, Podglajen I, Fernandez-Gerlinger MP, Mainardi, JL. Switch to oral antibiotics in the treatment of infective endocarditis is not associated with increased risk of mortality in non-severely ill patients [published online ahead of print April 16, 2016]. Clin Microbiol Infect. doi:10.1016/j.cmi.2016.04.003.
Providing Effective Palliative Care in the Era of Value
Although effective palliative care has always been a must-have for patients and caregivers facing serious illness, it hasn’t always been readily available. With the emergence of value-based healthcare models—and their potent incentives to reduce avoidable readmissions—there is renewed hope that such care will be accessible to those who need it.
Palliative and end-of-life care have long been promoted as core skills for hospitalists. The topic has regularly been included at SHM annual meetings and other prominent hospital medicine conferences, in the American Board of Internal Medicine blueprint for recognition of focused practice in hospital medicine, and in a number of influential references for hospitalists. Still, as I look at hospitalist programs around the country, there is a clear need to improve hospitalists’ delivery of palliative and end-of-life care.
Care of patients with chronic illness in their last two years of life accounts for a third of all Medicare spending.1 As hospitalists, we encounter many of these patients as they are hospitalized—and often re-hospitalized. Palliative care, which can improve quality of life and decrease costs for patients while leading to increased satisfaction and better outcomes for caregivers, can help alleviate unneeded and unwanted aggressive interventions like hospitalization.2,3
In its 2014 report, Dying in America, the Institute of Medicine (IOM) identified several areas for improvement, including better advance care planning and payment systems supporting high quality end-of-life care.4 As I write this column in mid 2016, there are two notable achievements since the IOM report: two E&M codes for advance care planning and a substantial and growing number of hospitalist patients in alternative payment models like bundled payments or ACOs.5 I believe we are entering a time when the availability of good palliative care will be accelerated due to broader forces in healthcare that for the first time align incentives between patients’ wishes and how care is paid for.
Palliative Care Skills for Hospitalists
The following are key actions for physicians in addressing palliative care for the hospitalized patient. At the risk of oversimplifying the discipline, I offer a few key actions for hospitalists to keep in mind.
Identify patients who would benefit from palliative care. The surprise question—“Would I be surprised if this patient died in the next year?”—has the ability to predict which patients would benefit from palliative care. In one observation from a group of patients with cancer, a “no” answer identified 60% of patients who died within a year.6 The surprise question has previously been shown to be predictive in other cancer and non-cancer populations.7,8
Weisman and Meier suggest using the following in a checklist at the time of hospital admission as “primary criteria to screen for unmet palliative care needs”:9
- The surprise question
- Frequent admissions
- Admission prompted by difficult-to-control physical or psychological symptoms
- Complex care requirements
- Decline in function, feeding intolerance, or unintended decline in weight
Hold a “goals of care” meeting. A notable step forward for supporting conversations between physicians and patients occurred on Jan. 1, when the Centers for Medicare & Medicaid Services (CMS) announced the Advance Care Planning E&M codes. These are CPT codes 99497 and 99498. They can be used on the same day as other E&M codes and cover discussions regarding advance care planning issues including discussing advance directives, appointing a healthcare proxy or durable power of attorney, discussing a living will, or addressing orders for life-sustaining treatment like the role of hydration or future hospitalizations. (For more information on how to use them, visit the CMS website and search for the FAQ.)
What should hospitalists concentrate on when having “goals of care” conversations with patients and caregivers? Ariadne Labs, a Harvard-affiliated health innovation group, offers the following as elements of a serious illness conversation:10
- Patients’ understanding of their illness
- Patients’ preferences for information and for family involvement
- Personal life goals, fears, and anxieties
- Trade-offs they are willing to accept
For hospitalists, an important area to pay particular attention to is the role of future hospitalizations in patients’ wishes for care, as some patients, if offered appropriate symptom control, would prefer to remain at home.
Two other crucial elements of inpatient palliative care—offer psychosocial support and symptom relief and hand off patient to effective post-hospital palliative care—are outside the scope of this article. However, they should be kept in mind and, of course, applied.
Understand the role of the palliative care consultation. Busy hospitalists might reasonably think, “I simply don’t have time to address palliative care in patients who aren’t likely to die during this hospitalization or soon after.” The palliative care consult service, if available, should be accessed when patients are identified as palliative care candidates but the primary hospitalist does not have the time or resources—including specialized knowledge in some cases—to deliver adequate palliative care. Palliative care specialists can also help bridge the gap between inpatient and outpatient palliative care resources.
In sum, the move to value-based payment models and the new advance care planning E&M codes provide a renewed focus—with more aligned incentives—and the opportunity to provide good palliative care to all who need it.
For hospitalists, identifying those who would benefit from palliative care and working with the healthcare team to ensure the care is delivered are at the heart of our professional mission. TH
References
- End-of-life care. The Darmouth Atlas of Health Care website. Accessed June 23, 2016.
- Gade G, Venohr I, Conner D, et al. Impact of an inpatient palliative care team: a randomized control trial. J Palliat Med. 2008;11(2):180-190.
- Morrison RS, Penrod JD, Cassel JB, et al. Cost savings associated with US hospital palliative care consultation programs. Arch Int Med. 2008;168(16):1783-1790.
- Institute of Medicine. Dying in America: Improving Quality and Honoring Individual Preferences near the End of Life. 2014.
- BPCI Model 2: Retrospective acute & post acute care episode. Centers for Medicare & Medicaid Services website. Accessed June 24, 2016.
- Vick JB, Pertsch N, Hutchings M, et al. The utility of the surprise question in identifying patients most at risk of death. J Clin Oncol. 2015;33(suppl):8.
- Moss AH, Ganjoo J, Sharma S, et al. Utility of the “surprise” question to identify dialysis patients with high mortality. Clin J Am Soc Nephrol. 2008;3:1379-1384.
- Moss AH, Lunney JR, Culp S, et al. Prognostic significance of the “surprise” question in cancer patients. J Palliat Med. 2010;13(7):837-840.
- Weissman D, Meier C. Identifying patients in need of a palliative care assessment in the hospital setting: a consensus report from the Center to Advance Palliative Care. J Palliat Med. 2011;14(1):17-23.
- Serious illness care resources. Ariadne Labs website. Accessed June 24, 2016.
Although effective palliative care has always been a must-have for patients and caregivers facing serious illness, it hasn’t always been readily available. With the emergence of value-based healthcare models—and their potent incentives to reduce avoidable readmissions—there is renewed hope that such care will be accessible to those who need it.
Palliative and end-of-life care have long been promoted as core skills for hospitalists. The topic has regularly been included at SHM annual meetings and other prominent hospital medicine conferences, in the American Board of Internal Medicine blueprint for recognition of focused practice in hospital medicine, and in a number of influential references for hospitalists. Still, as I look at hospitalist programs around the country, there is a clear need to improve hospitalists’ delivery of palliative and end-of-life care.
Care of patients with chronic illness in their last two years of life accounts for a third of all Medicare spending.1 As hospitalists, we encounter many of these patients as they are hospitalized—and often re-hospitalized. Palliative care, which can improve quality of life and decrease costs for patients while leading to increased satisfaction and better outcomes for caregivers, can help alleviate unneeded and unwanted aggressive interventions like hospitalization.2,3
In its 2014 report, Dying in America, the Institute of Medicine (IOM) identified several areas for improvement, including better advance care planning and payment systems supporting high quality end-of-life care.4 As I write this column in mid 2016, there are two notable achievements since the IOM report: two E&M codes for advance care planning and a substantial and growing number of hospitalist patients in alternative payment models like bundled payments or ACOs.5 I believe we are entering a time when the availability of good palliative care will be accelerated due to broader forces in healthcare that for the first time align incentives between patients’ wishes and how care is paid for.
Palliative Care Skills for Hospitalists
The following are key actions for physicians in addressing palliative care for the hospitalized patient. At the risk of oversimplifying the discipline, I offer a few key actions for hospitalists to keep in mind.
Identify patients who would benefit from palliative care. The surprise question—“Would I be surprised if this patient died in the next year?”—has the ability to predict which patients would benefit from palliative care. In one observation from a group of patients with cancer, a “no” answer identified 60% of patients who died within a year.6 The surprise question has previously been shown to be predictive in other cancer and non-cancer populations.7,8
Weisman and Meier suggest using the following in a checklist at the time of hospital admission as “primary criteria to screen for unmet palliative care needs”:9
- The surprise question
- Frequent admissions
- Admission prompted by difficult-to-control physical or psychological symptoms
- Complex care requirements
- Decline in function, feeding intolerance, or unintended decline in weight
Hold a “goals of care” meeting. A notable step forward for supporting conversations between physicians and patients occurred on Jan. 1, when the Centers for Medicare & Medicaid Services (CMS) announced the Advance Care Planning E&M codes. These are CPT codes 99497 and 99498. They can be used on the same day as other E&M codes and cover discussions regarding advance care planning issues including discussing advance directives, appointing a healthcare proxy or durable power of attorney, discussing a living will, or addressing orders for life-sustaining treatment like the role of hydration or future hospitalizations. (For more information on how to use them, visit the CMS website and search for the FAQ.)
What should hospitalists concentrate on when having “goals of care” conversations with patients and caregivers? Ariadne Labs, a Harvard-affiliated health innovation group, offers the following as elements of a serious illness conversation:10
- Patients’ understanding of their illness
- Patients’ preferences for information and for family involvement
- Personal life goals, fears, and anxieties
- Trade-offs they are willing to accept
For hospitalists, an important area to pay particular attention to is the role of future hospitalizations in patients’ wishes for care, as some patients, if offered appropriate symptom control, would prefer to remain at home.
Two other crucial elements of inpatient palliative care—offer psychosocial support and symptom relief and hand off patient to effective post-hospital palliative care—are outside the scope of this article. However, they should be kept in mind and, of course, applied.
Understand the role of the palliative care consultation. Busy hospitalists might reasonably think, “I simply don’t have time to address palliative care in patients who aren’t likely to die during this hospitalization or soon after.” The palliative care consult service, if available, should be accessed when patients are identified as palliative care candidates but the primary hospitalist does not have the time or resources—including specialized knowledge in some cases—to deliver adequate palliative care. Palliative care specialists can also help bridge the gap between inpatient and outpatient palliative care resources.
In sum, the move to value-based payment models and the new advance care planning E&M codes provide a renewed focus—with more aligned incentives—and the opportunity to provide good palliative care to all who need it.
For hospitalists, identifying those who would benefit from palliative care and working with the healthcare team to ensure the care is delivered are at the heart of our professional mission. TH
References
- End-of-life care. The Darmouth Atlas of Health Care website. Accessed June 23, 2016.
- Gade G, Venohr I, Conner D, et al. Impact of an inpatient palliative care team: a randomized control trial. J Palliat Med. 2008;11(2):180-190.
- Morrison RS, Penrod JD, Cassel JB, et al. Cost savings associated with US hospital palliative care consultation programs. Arch Int Med. 2008;168(16):1783-1790.
- Institute of Medicine. Dying in America: Improving Quality and Honoring Individual Preferences near the End of Life. 2014.
- BPCI Model 2: Retrospective acute & post acute care episode. Centers for Medicare & Medicaid Services website. Accessed June 24, 2016.
- Vick JB, Pertsch N, Hutchings M, et al. The utility of the surprise question in identifying patients most at risk of death. J Clin Oncol. 2015;33(suppl):8.
- Moss AH, Ganjoo J, Sharma S, et al. Utility of the “surprise” question to identify dialysis patients with high mortality. Clin J Am Soc Nephrol. 2008;3:1379-1384.
- Moss AH, Lunney JR, Culp S, et al. Prognostic significance of the “surprise” question in cancer patients. J Palliat Med. 2010;13(7):837-840.
- Weissman D, Meier C. Identifying patients in need of a palliative care assessment in the hospital setting: a consensus report from the Center to Advance Palliative Care. J Palliat Med. 2011;14(1):17-23.
- Serious illness care resources. Ariadne Labs website. Accessed June 24, 2016.
Although effective palliative care has always been a must-have for patients and caregivers facing serious illness, it hasn’t always been readily available. With the emergence of value-based healthcare models—and their potent incentives to reduce avoidable readmissions—there is renewed hope that such care will be accessible to those who need it.
Palliative and end-of-life care have long been promoted as core skills for hospitalists. The topic has regularly been included at SHM annual meetings and other prominent hospital medicine conferences, in the American Board of Internal Medicine blueprint for recognition of focused practice in hospital medicine, and in a number of influential references for hospitalists. Still, as I look at hospitalist programs around the country, there is a clear need to improve hospitalists’ delivery of palliative and end-of-life care.
Care of patients with chronic illness in their last two years of life accounts for a third of all Medicare spending.1 As hospitalists, we encounter many of these patients as they are hospitalized—and often re-hospitalized. Palliative care, which can improve quality of life and decrease costs for patients while leading to increased satisfaction and better outcomes for caregivers, can help alleviate unneeded and unwanted aggressive interventions like hospitalization.2,3
In its 2014 report, Dying in America, the Institute of Medicine (IOM) identified several areas for improvement, including better advance care planning and payment systems supporting high quality end-of-life care.4 As I write this column in mid 2016, there are two notable achievements since the IOM report: two E&M codes for advance care planning and a substantial and growing number of hospitalist patients in alternative payment models like bundled payments or ACOs.5 I believe we are entering a time when the availability of good palliative care will be accelerated due to broader forces in healthcare that for the first time align incentives between patients’ wishes and how care is paid for.
Palliative Care Skills for Hospitalists
The following are key actions for physicians in addressing palliative care for the hospitalized patient. At the risk of oversimplifying the discipline, I offer a few key actions for hospitalists to keep in mind.
Identify patients who would benefit from palliative care. The surprise question—“Would I be surprised if this patient died in the next year?”—has the ability to predict which patients would benefit from palliative care. In one observation from a group of patients with cancer, a “no” answer identified 60% of patients who died within a year.6 The surprise question has previously been shown to be predictive in other cancer and non-cancer populations.7,8
Weisman and Meier suggest using the following in a checklist at the time of hospital admission as “primary criteria to screen for unmet palliative care needs”:9
- The surprise question
- Frequent admissions
- Admission prompted by difficult-to-control physical or psychological symptoms
- Complex care requirements
- Decline in function, feeding intolerance, or unintended decline in weight
Hold a “goals of care” meeting. A notable step forward for supporting conversations between physicians and patients occurred on Jan. 1, when the Centers for Medicare & Medicaid Services (CMS) announced the Advance Care Planning E&M codes. These are CPT codes 99497 and 99498. They can be used on the same day as other E&M codes and cover discussions regarding advance care planning issues including discussing advance directives, appointing a healthcare proxy or durable power of attorney, discussing a living will, or addressing orders for life-sustaining treatment like the role of hydration or future hospitalizations. (For more information on how to use them, visit the CMS website and search for the FAQ.)
What should hospitalists concentrate on when having “goals of care” conversations with patients and caregivers? Ariadne Labs, a Harvard-affiliated health innovation group, offers the following as elements of a serious illness conversation:10
- Patients’ understanding of their illness
- Patients’ preferences for information and for family involvement
- Personal life goals, fears, and anxieties
- Trade-offs they are willing to accept
For hospitalists, an important area to pay particular attention to is the role of future hospitalizations in patients’ wishes for care, as some patients, if offered appropriate symptom control, would prefer to remain at home.
Two other crucial elements of inpatient palliative care—offer psychosocial support and symptom relief and hand off patient to effective post-hospital palliative care—are outside the scope of this article. However, they should be kept in mind and, of course, applied.
Understand the role of the palliative care consultation. Busy hospitalists might reasonably think, “I simply don’t have time to address palliative care in patients who aren’t likely to die during this hospitalization or soon after.” The palliative care consult service, if available, should be accessed when patients are identified as palliative care candidates but the primary hospitalist does not have the time or resources—including specialized knowledge in some cases—to deliver adequate palliative care. Palliative care specialists can also help bridge the gap between inpatient and outpatient palliative care resources.
In sum, the move to value-based payment models and the new advance care planning E&M codes provide a renewed focus—with more aligned incentives—and the opportunity to provide good palliative care to all who need it.
For hospitalists, identifying those who would benefit from palliative care and working with the healthcare team to ensure the care is delivered are at the heart of our professional mission. TH
References
- End-of-life care. The Darmouth Atlas of Health Care website. Accessed June 23, 2016.
- Gade G, Venohr I, Conner D, et al. Impact of an inpatient palliative care team: a randomized control trial. J Palliat Med. 2008;11(2):180-190.
- Morrison RS, Penrod JD, Cassel JB, et al. Cost savings associated with US hospital palliative care consultation programs. Arch Int Med. 2008;168(16):1783-1790.
- Institute of Medicine. Dying in America: Improving Quality and Honoring Individual Preferences near the End of Life. 2014.
- BPCI Model 2: Retrospective acute & post acute care episode. Centers for Medicare & Medicaid Services website. Accessed June 24, 2016.
- Vick JB, Pertsch N, Hutchings M, et al. The utility of the surprise question in identifying patients most at risk of death. J Clin Oncol. 2015;33(suppl):8.
- Moss AH, Ganjoo J, Sharma S, et al. Utility of the “surprise” question to identify dialysis patients with high mortality. Clin J Am Soc Nephrol. 2008;3:1379-1384.
- Moss AH, Lunney JR, Culp S, et al. Prognostic significance of the “surprise” question in cancer patients. J Palliat Med. 2010;13(7):837-840.
- Weissman D, Meier C. Identifying patients in need of a palliative care assessment in the hospital setting: a consensus report from the Center to Advance Palliative Care. J Palliat Med. 2011;14(1):17-23.
- Serious illness care resources. Ariadne Labs website. Accessed June 24, 2016.
Communication Crossroads: Managing Patient Interactions, Online Personas on Social Media
The pitfalls that can complicate the intersection of social media and patient privacy often come as no surprise when they arise, but digital communications, and social media sites in particular, also have made many positive contributions to the medical profession.
“Social media allows physicians to communicate with each other, to publicize items of interest, to solicit input from colleagues—even people that we don’t know—on a variety of topics,” says Brian Clay, MD, SFHM, interim chief medical informatics officer and associate program director of the internal medicine residency-training program at the University of California at San Diego.
But there is a dark side of social media, too, and some physicians have made significant missteps in social media use. Ryan Greysen, MD, MHS, FHM, assistant professor in the division of hospital medicine at the University of California at San Francisco, has authored multiple studies on physician violations of online professionalism. In a report published in the March 2012 issue of JAMA, Dr. Greysen and co-authors note that 92% of the executive directors at state medical and osteopathic boards surveyed reported encountering at least one violation of online professionalism.3 Another report in the January 2013 issue of the Annals of Internal Medicine co-authored by Dr. Greysen notes that 71% of state medical boards have investigated physicians for violations of professionalism online.4 The consequences of these errors in judgment can be dire: Should your employer come across it or a colleague report it, you could lose your position and even lose your license.
Professional Guidelines
To avoid these significant and potentially career-ending blunders, the American College of Physicians (ACP)—in conjunction with the Federation of State Medical Boards (FSMB)—published recommendations offering ethical guidance in preserving the patient-physician relationship in context of social media.5 Similarly, the American Medical Association (AMA) published an opinion on professionalism in the use of social media.6 Their guidelines can be summarized in five succinct points.
- Maintain standards of professional ethics in online communications, including respect for patient privacy.
Katherine Chretien, MD, associate professor of medicine at George Washington University in Washington, D.C., a clinical associate professor in medicine at the Uniformed Services University of the Health Sciences in Bethesda, Md., and chief of the hospitalist section at the Veterans Affairs Medical Center also in Washington, D.C., warns physicians to use the utmost caution to maintain patient anonymity when publishing case stories online. When publishing clinical vignettes, physician blogs, and other forms of online media, all details that can identify a patient must be completely removed, including all forms of the date (references to “yesterday” or “last week,” for example, can identify the date). Check anything you intend to publish against the HIPPA list of 18 identifiers.7 (See “HIPPA Identifiers” below)
“The safest way to proceed when publishing patient narratives online is to get consent,” Dr. Chretien says. “If consent is not possible, as in cases of incidents that occurred several years ago, change the personal details, such as location, and clearly disclose that you have. Or make the example very general.” For example, instead of discussing how frustrated you became with a patient with asthma who you saw at a particular hospital in a certain year (a clear violation of patient privacy), paint the illustration in broad strokes. Dr. Chretien suggests you might phrase your observations in this way: “One of the frustrations I find when treating asthma patients is …”
It would also be wise to seek advice from colleagues before posting patient information, she notes.
- Do not blur the boundaries between your professional and social spheres.
In a 2011 study, Gabriel Bosslet, MD, assistant professor of clinical medicine and associate director of the fellowship in pulmonary and critical care medicine at Indiana University–Purdue University at Indianapolis, noted that 34% of participating physicians reported receiving a Facebook friend request from a patient or patient’s family member. As Dr. Chretien points out, this is less of a problem for hospitalists than private-practice physicians because the relationship with patients is transitory. The AMA, as well as the ACP and FSMB, note that physicians should not “friend” patients, accept friend requests, or contact patients through social media. Physicians are advised to keep their public and professional online personas separate, even to the point of creating distinct online identities for their personal and professional lives.
- Maintain professionalism in your online persona, and continually monitor your online image to ensure it reflects positively on yourself and the medical profession.
Some physicians fall into the trap of placing questionable postings on their personal pages, including posting content that can be inappropriate for public consumption or venting about patients and employers. Stories or incidents that medical professionals find intriguing or exciting may be disturbing to those outside their community, and medical humor can be offensive.
“[Physicians] assume [their social media page] is their personal space, so they can post whatever they want,” adds Dr. Chretien. “Part of their error is that they believe they are addressing a small group of close friends, but they forget that postings go out to the larger, peripheral audience of all Facebook friends and can often be accessed by the general public.” An ill-considered anecdote can damage not only your own reputation but also the overall perception of the profession. Physicians are always viewed in their professional role, even in social interactions.
- Use email and other forms of electronic communication only in cases of an established physician-patient relationship and only with informed patient consent. Documentation of these communications should be kept in the patient’s medical record.
Any request a physician receives for medical advice through a social media site or email must be handled with caution. The ACP and FSMB state that email and text communications with established patients can be beneficial but should occur only after both parties discuss privacy risks, the appropriate types of information that will be exchanged electronically, and how long patients should expect to wait for a physician response. Patient preference should guide the use of electronic communication with physicians, especially text messaging, says Dr. Greysen.
- Be aware that any postings on the Internet, because of its significant and unprecedented reach, can have future career ramifications. Consequently, physicians are advised to frequently monitor their online presence to control their image.
Dr. Greysen points out that presenting a positive image of physicians in the media is not a new challenge. “Physicians have been publishing books about their experiences for decades. But posting online without oversight, or in the moment without reflection, can be devastating to a physician’s career because the reach of the Internet is exponentially vaster than that of any printed material,” Dr. Greysen says.
Deliver Better Healthcare through Social Media
Perhaps one of the most dramatic ways in which social media is positively impacting healthcare is the FOAM movement, or free open access medical education. Jeanne Farnan, MD, associate professor of medicine at the University of Chicago Department of Medicine and lead author of the ACP and FSMB social media position paper, points to the dynamic collection of resources and tools for ongoing medical education as well as the community that participates in openly sharing knowledge as examples. FOAM resources are predominantly social media based and include blogs, podcasts, tweets, online videos, graphics, web-based applications, text documents, and photographs, many of which are available by following the Twitter feed @FOAMed (see “FOAM Links” below). This FOAM community is dedicated to the belief that high-quality medical education resources and interactions should be free and accessible to all who care for patients and especially to those who educate future physicians.8
Social media also affords physicians the opportunity to be a force in public health policies. “There is an active group of physician and medical student social media users in the blogosphere and on Twitter who use their social media presence for activism, and this presence is intimately tied to how they see themselves as a medical professional,” Dr. Farnan says. “They blog and tweet about medical education issues and other public topics such as access to care and care disparity.”
Michelle Vangel, director of insight services with Cision, a Chicago-based public relations company specializing in social media communications, praises the power of social media for raising awareness of public health issues.
“In terms of public health, social media is valuable to better understand how health-related news resonates with the public,” Vangel says. “Two salient examples of major health crises reactions tracked on social media were the Ebola outbreak in Africa and the measles outbreak at Disneyland in California. At times, there was near hysteria over Ebola and vaccine debates, with misinformation spreading quickly. However, many hospitals and physicians tried to get ahead of the hysteria by providing concise, accurate information on different social media platforms, with Facebook often a popular channel to post information.”
Social media sites can also help by making emotional support available at disease-specific sites. These communities address the patient experience of the disease that goes beyond purely medical disease information. Vangel points to several online communities that “host pivotal conversations for patients,” she says. “There are Facebook community pages dedicated to a host of conditions, including diabetes, hypertension, and cystic fibrosis, where patients discuss the challenges of medication compliance, side effects, and even dissatisfaction with healthcare professionals. BabyCenter.com provides message boards about a wide array of topics for people trying to conceive, pregnant women with health conditions, and parents of babies with health issues. CancerForums.net and the health and wellness boards at DelphiForums.com provide support to specific disease populations.”
Vangel encourages physicians to monitor online patient-support sites to better understand the difficulties patients experience while under treatment. These sites can also help physicians recognize and address the gaps in patient understanding about various diseases and explore programs geared toward the populations suffering from a wide range of conditions. TH
Maybelle Cowan-Lincoln is a freelance writer in New Jersey.
References
- Photos of drinking, grinning aid mission doctors cause uproar. CNN website. Accessed December 2, 2015.
- Terhune C. Hospital violated patient confidentiality, state says. Los Angeles Times website. Accessed December 3, 2015.
- Greysen SR, Chretien KC, Kind T, Young A, Gross CP. Physician violations of online professionalism and disciplinary actions: a national survey of state medical boards. JAMA. 2012;(307):1141-1142.
- Greysen SR, Johnson D, Kind T, et al. Online professional investigations by state medical boards: first, do no harm. Ann Intern Med. 2013;(158):124-130.
- New recommendations offer physicians ethical guidance for preserving trust in patient-physician relationships and the profession when using social media. American College of Physicians website. Accessed July 3, 2015.
- Opinion 9.124—professionalism in the use of social media. American Medical Association website. Accessed July 3, 2015.
- HIPPA PHI: list of 18 identifiers and definition of PHI. The Committee for Protection of Human Subjects website. Accessed July 10, 2015.
- FOAM. Life in the Fastlane website. Accessed September 6, 2015.
The pitfalls that can complicate the intersection of social media and patient privacy often come as no surprise when they arise, but digital communications, and social media sites in particular, also have made many positive contributions to the medical profession.
“Social media allows physicians to communicate with each other, to publicize items of interest, to solicit input from colleagues—even people that we don’t know—on a variety of topics,” says Brian Clay, MD, SFHM, interim chief medical informatics officer and associate program director of the internal medicine residency-training program at the University of California at San Diego.
But there is a dark side of social media, too, and some physicians have made significant missteps in social media use. Ryan Greysen, MD, MHS, FHM, assistant professor in the division of hospital medicine at the University of California at San Francisco, has authored multiple studies on physician violations of online professionalism. In a report published in the March 2012 issue of JAMA, Dr. Greysen and co-authors note that 92% of the executive directors at state medical and osteopathic boards surveyed reported encountering at least one violation of online professionalism.3 Another report in the January 2013 issue of the Annals of Internal Medicine co-authored by Dr. Greysen notes that 71% of state medical boards have investigated physicians for violations of professionalism online.4 The consequences of these errors in judgment can be dire: Should your employer come across it or a colleague report it, you could lose your position and even lose your license.
Professional Guidelines
To avoid these significant and potentially career-ending blunders, the American College of Physicians (ACP)—in conjunction with the Federation of State Medical Boards (FSMB)—published recommendations offering ethical guidance in preserving the patient-physician relationship in context of social media.5 Similarly, the American Medical Association (AMA) published an opinion on professionalism in the use of social media.6 Their guidelines can be summarized in five succinct points.
- Maintain standards of professional ethics in online communications, including respect for patient privacy.
Katherine Chretien, MD, associate professor of medicine at George Washington University in Washington, D.C., a clinical associate professor in medicine at the Uniformed Services University of the Health Sciences in Bethesda, Md., and chief of the hospitalist section at the Veterans Affairs Medical Center also in Washington, D.C., warns physicians to use the utmost caution to maintain patient anonymity when publishing case stories online. When publishing clinical vignettes, physician blogs, and other forms of online media, all details that can identify a patient must be completely removed, including all forms of the date (references to “yesterday” or “last week,” for example, can identify the date). Check anything you intend to publish against the HIPPA list of 18 identifiers.7 (See “HIPPA Identifiers” below)
“The safest way to proceed when publishing patient narratives online is to get consent,” Dr. Chretien says. “If consent is not possible, as in cases of incidents that occurred several years ago, change the personal details, such as location, and clearly disclose that you have. Or make the example very general.” For example, instead of discussing how frustrated you became with a patient with asthma who you saw at a particular hospital in a certain year (a clear violation of patient privacy), paint the illustration in broad strokes. Dr. Chretien suggests you might phrase your observations in this way: “One of the frustrations I find when treating asthma patients is …”
It would also be wise to seek advice from colleagues before posting patient information, she notes.
- Do not blur the boundaries between your professional and social spheres.
In a 2011 study, Gabriel Bosslet, MD, assistant professor of clinical medicine and associate director of the fellowship in pulmonary and critical care medicine at Indiana University–Purdue University at Indianapolis, noted that 34% of participating physicians reported receiving a Facebook friend request from a patient or patient’s family member. As Dr. Chretien points out, this is less of a problem for hospitalists than private-practice physicians because the relationship with patients is transitory. The AMA, as well as the ACP and FSMB, note that physicians should not “friend” patients, accept friend requests, or contact patients through social media. Physicians are advised to keep their public and professional online personas separate, even to the point of creating distinct online identities for their personal and professional lives.
- Maintain professionalism in your online persona, and continually monitor your online image to ensure it reflects positively on yourself and the medical profession.
Some physicians fall into the trap of placing questionable postings on their personal pages, including posting content that can be inappropriate for public consumption or venting about patients and employers. Stories or incidents that medical professionals find intriguing or exciting may be disturbing to those outside their community, and medical humor can be offensive.
“[Physicians] assume [their social media page] is their personal space, so they can post whatever they want,” adds Dr. Chretien. “Part of their error is that they believe they are addressing a small group of close friends, but they forget that postings go out to the larger, peripheral audience of all Facebook friends and can often be accessed by the general public.” An ill-considered anecdote can damage not only your own reputation but also the overall perception of the profession. Physicians are always viewed in their professional role, even in social interactions.
- Use email and other forms of electronic communication only in cases of an established physician-patient relationship and only with informed patient consent. Documentation of these communications should be kept in the patient’s medical record.
Any request a physician receives for medical advice through a social media site or email must be handled with caution. The ACP and FSMB state that email and text communications with established patients can be beneficial but should occur only after both parties discuss privacy risks, the appropriate types of information that will be exchanged electronically, and how long patients should expect to wait for a physician response. Patient preference should guide the use of electronic communication with physicians, especially text messaging, says Dr. Greysen.
- Be aware that any postings on the Internet, because of its significant and unprecedented reach, can have future career ramifications. Consequently, physicians are advised to frequently monitor their online presence to control their image.
Dr. Greysen points out that presenting a positive image of physicians in the media is not a new challenge. “Physicians have been publishing books about their experiences for decades. But posting online without oversight, or in the moment without reflection, can be devastating to a physician’s career because the reach of the Internet is exponentially vaster than that of any printed material,” Dr. Greysen says.
Deliver Better Healthcare through Social Media
Perhaps one of the most dramatic ways in which social media is positively impacting healthcare is the FOAM movement, or free open access medical education. Jeanne Farnan, MD, associate professor of medicine at the University of Chicago Department of Medicine and lead author of the ACP and FSMB social media position paper, points to the dynamic collection of resources and tools for ongoing medical education as well as the community that participates in openly sharing knowledge as examples. FOAM resources are predominantly social media based and include blogs, podcasts, tweets, online videos, graphics, web-based applications, text documents, and photographs, many of which are available by following the Twitter feed @FOAMed (see “FOAM Links” below). This FOAM community is dedicated to the belief that high-quality medical education resources and interactions should be free and accessible to all who care for patients and especially to those who educate future physicians.8
Social media also affords physicians the opportunity to be a force in public health policies. “There is an active group of physician and medical student social media users in the blogosphere and on Twitter who use their social media presence for activism, and this presence is intimately tied to how they see themselves as a medical professional,” Dr. Farnan says. “They blog and tweet about medical education issues and other public topics such as access to care and care disparity.”
Michelle Vangel, director of insight services with Cision, a Chicago-based public relations company specializing in social media communications, praises the power of social media for raising awareness of public health issues.
“In terms of public health, social media is valuable to better understand how health-related news resonates with the public,” Vangel says. “Two salient examples of major health crises reactions tracked on social media were the Ebola outbreak in Africa and the measles outbreak at Disneyland in California. At times, there was near hysteria over Ebola and vaccine debates, with misinformation spreading quickly. However, many hospitals and physicians tried to get ahead of the hysteria by providing concise, accurate information on different social media platforms, with Facebook often a popular channel to post information.”
Social media sites can also help by making emotional support available at disease-specific sites. These communities address the patient experience of the disease that goes beyond purely medical disease information. Vangel points to several online communities that “host pivotal conversations for patients,” she says. “There are Facebook community pages dedicated to a host of conditions, including diabetes, hypertension, and cystic fibrosis, where patients discuss the challenges of medication compliance, side effects, and even dissatisfaction with healthcare professionals. BabyCenter.com provides message boards about a wide array of topics for people trying to conceive, pregnant women with health conditions, and parents of babies with health issues. CancerForums.net and the health and wellness boards at DelphiForums.com provide support to specific disease populations.”
Vangel encourages physicians to monitor online patient-support sites to better understand the difficulties patients experience while under treatment. These sites can also help physicians recognize and address the gaps in patient understanding about various diseases and explore programs geared toward the populations suffering from a wide range of conditions. TH
Maybelle Cowan-Lincoln is a freelance writer in New Jersey.
References
- Photos of drinking, grinning aid mission doctors cause uproar. CNN website. Accessed December 2, 2015.
- Terhune C. Hospital violated patient confidentiality, state says. Los Angeles Times website. Accessed December 3, 2015.
- Greysen SR, Chretien KC, Kind T, Young A, Gross CP. Physician violations of online professionalism and disciplinary actions: a national survey of state medical boards. JAMA. 2012;(307):1141-1142.
- Greysen SR, Johnson D, Kind T, et al. Online professional investigations by state medical boards: first, do no harm. Ann Intern Med. 2013;(158):124-130.
- New recommendations offer physicians ethical guidance for preserving trust in patient-physician relationships and the profession when using social media. American College of Physicians website. Accessed July 3, 2015.
- Opinion 9.124—professionalism in the use of social media. American Medical Association website. Accessed July 3, 2015.
- HIPPA PHI: list of 18 identifiers and definition of PHI. The Committee for Protection of Human Subjects website. Accessed July 10, 2015.
- FOAM. Life in the Fastlane website. Accessed September 6, 2015.
The pitfalls that can complicate the intersection of social media and patient privacy often come as no surprise when they arise, but digital communications, and social media sites in particular, also have made many positive contributions to the medical profession.
“Social media allows physicians to communicate with each other, to publicize items of interest, to solicit input from colleagues—even people that we don’t know—on a variety of topics,” says Brian Clay, MD, SFHM, interim chief medical informatics officer and associate program director of the internal medicine residency-training program at the University of California at San Diego.
But there is a dark side of social media, too, and some physicians have made significant missteps in social media use. Ryan Greysen, MD, MHS, FHM, assistant professor in the division of hospital medicine at the University of California at San Francisco, has authored multiple studies on physician violations of online professionalism. In a report published in the March 2012 issue of JAMA, Dr. Greysen and co-authors note that 92% of the executive directors at state medical and osteopathic boards surveyed reported encountering at least one violation of online professionalism.3 Another report in the January 2013 issue of the Annals of Internal Medicine co-authored by Dr. Greysen notes that 71% of state medical boards have investigated physicians for violations of professionalism online.4 The consequences of these errors in judgment can be dire: Should your employer come across it or a colleague report it, you could lose your position and even lose your license.
Professional Guidelines
To avoid these significant and potentially career-ending blunders, the American College of Physicians (ACP)—in conjunction with the Federation of State Medical Boards (FSMB)—published recommendations offering ethical guidance in preserving the patient-physician relationship in context of social media.5 Similarly, the American Medical Association (AMA) published an opinion on professionalism in the use of social media.6 Their guidelines can be summarized in five succinct points.
- Maintain standards of professional ethics in online communications, including respect for patient privacy.
Katherine Chretien, MD, associate professor of medicine at George Washington University in Washington, D.C., a clinical associate professor in medicine at the Uniformed Services University of the Health Sciences in Bethesda, Md., and chief of the hospitalist section at the Veterans Affairs Medical Center also in Washington, D.C., warns physicians to use the utmost caution to maintain patient anonymity when publishing case stories online. When publishing clinical vignettes, physician blogs, and other forms of online media, all details that can identify a patient must be completely removed, including all forms of the date (references to “yesterday” or “last week,” for example, can identify the date). Check anything you intend to publish against the HIPPA list of 18 identifiers.7 (See “HIPPA Identifiers” below)
“The safest way to proceed when publishing patient narratives online is to get consent,” Dr. Chretien says. “If consent is not possible, as in cases of incidents that occurred several years ago, change the personal details, such as location, and clearly disclose that you have. Or make the example very general.” For example, instead of discussing how frustrated you became with a patient with asthma who you saw at a particular hospital in a certain year (a clear violation of patient privacy), paint the illustration in broad strokes. Dr. Chretien suggests you might phrase your observations in this way: “One of the frustrations I find when treating asthma patients is …”
It would also be wise to seek advice from colleagues before posting patient information, she notes.
- Do not blur the boundaries between your professional and social spheres.
In a 2011 study, Gabriel Bosslet, MD, assistant professor of clinical medicine and associate director of the fellowship in pulmonary and critical care medicine at Indiana University–Purdue University at Indianapolis, noted that 34% of participating physicians reported receiving a Facebook friend request from a patient or patient’s family member. As Dr. Chretien points out, this is less of a problem for hospitalists than private-practice physicians because the relationship with patients is transitory. The AMA, as well as the ACP and FSMB, note that physicians should not “friend” patients, accept friend requests, or contact patients through social media. Physicians are advised to keep their public and professional online personas separate, even to the point of creating distinct online identities for their personal and professional lives.
- Maintain professionalism in your online persona, and continually monitor your online image to ensure it reflects positively on yourself and the medical profession.
Some physicians fall into the trap of placing questionable postings on their personal pages, including posting content that can be inappropriate for public consumption or venting about patients and employers. Stories or incidents that medical professionals find intriguing or exciting may be disturbing to those outside their community, and medical humor can be offensive.
“[Physicians] assume [their social media page] is their personal space, so they can post whatever they want,” adds Dr. Chretien. “Part of their error is that they believe they are addressing a small group of close friends, but they forget that postings go out to the larger, peripheral audience of all Facebook friends and can often be accessed by the general public.” An ill-considered anecdote can damage not only your own reputation but also the overall perception of the profession. Physicians are always viewed in their professional role, even in social interactions.
- Use email and other forms of electronic communication only in cases of an established physician-patient relationship and only with informed patient consent. Documentation of these communications should be kept in the patient’s medical record.
Any request a physician receives for medical advice through a social media site or email must be handled with caution. The ACP and FSMB state that email and text communications with established patients can be beneficial but should occur only after both parties discuss privacy risks, the appropriate types of information that will be exchanged electronically, and how long patients should expect to wait for a physician response. Patient preference should guide the use of electronic communication with physicians, especially text messaging, says Dr. Greysen.
- Be aware that any postings on the Internet, because of its significant and unprecedented reach, can have future career ramifications. Consequently, physicians are advised to frequently monitor their online presence to control their image.
Dr. Greysen points out that presenting a positive image of physicians in the media is not a new challenge. “Physicians have been publishing books about their experiences for decades. But posting online without oversight, or in the moment without reflection, can be devastating to a physician’s career because the reach of the Internet is exponentially vaster than that of any printed material,” Dr. Greysen says.
Deliver Better Healthcare through Social Media
Perhaps one of the most dramatic ways in which social media is positively impacting healthcare is the FOAM movement, or free open access medical education. Jeanne Farnan, MD, associate professor of medicine at the University of Chicago Department of Medicine and lead author of the ACP and FSMB social media position paper, points to the dynamic collection of resources and tools for ongoing medical education as well as the community that participates in openly sharing knowledge as examples. FOAM resources are predominantly social media based and include blogs, podcasts, tweets, online videos, graphics, web-based applications, text documents, and photographs, many of which are available by following the Twitter feed @FOAMed (see “FOAM Links” below). This FOAM community is dedicated to the belief that high-quality medical education resources and interactions should be free and accessible to all who care for patients and especially to those who educate future physicians.8
Social media also affords physicians the opportunity to be a force in public health policies. “There is an active group of physician and medical student social media users in the blogosphere and on Twitter who use their social media presence for activism, and this presence is intimately tied to how they see themselves as a medical professional,” Dr. Farnan says. “They blog and tweet about medical education issues and other public topics such as access to care and care disparity.”
Michelle Vangel, director of insight services with Cision, a Chicago-based public relations company specializing in social media communications, praises the power of social media for raising awareness of public health issues.
“In terms of public health, social media is valuable to better understand how health-related news resonates with the public,” Vangel says. “Two salient examples of major health crises reactions tracked on social media were the Ebola outbreak in Africa and the measles outbreak at Disneyland in California. At times, there was near hysteria over Ebola and vaccine debates, with misinformation spreading quickly. However, many hospitals and physicians tried to get ahead of the hysteria by providing concise, accurate information on different social media platforms, with Facebook often a popular channel to post information.”
Social media sites can also help by making emotional support available at disease-specific sites. These communities address the patient experience of the disease that goes beyond purely medical disease information. Vangel points to several online communities that “host pivotal conversations for patients,” she says. “There are Facebook community pages dedicated to a host of conditions, including diabetes, hypertension, and cystic fibrosis, where patients discuss the challenges of medication compliance, side effects, and even dissatisfaction with healthcare professionals. BabyCenter.com provides message boards about a wide array of topics for people trying to conceive, pregnant women with health conditions, and parents of babies with health issues. CancerForums.net and the health and wellness boards at DelphiForums.com provide support to specific disease populations.”
Vangel encourages physicians to monitor online patient-support sites to better understand the difficulties patients experience while under treatment. These sites can also help physicians recognize and address the gaps in patient understanding about various diseases and explore programs geared toward the populations suffering from a wide range of conditions. TH
Maybelle Cowan-Lincoln is a freelance writer in New Jersey.
References
- Photos of drinking, grinning aid mission doctors cause uproar. CNN website. Accessed December 2, 2015.
- Terhune C. Hospital violated patient confidentiality, state says. Los Angeles Times website. Accessed December 3, 2015.
- Greysen SR, Chretien KC, Kind T, Young A, Gross CP. Physician violations of online professionalism and disciplinary actions: a national survey of state medical boards. JAMA. 2012;(307):1141-1142.
- Greysen SR, Johnson D, Kind T, et al. Online professional investigations by state medical boards: first, do no harm. Ann Intern Med. 2013;(158):124-130.
- New recommendations offer physicians ethical guidance for preserving trust in patient-physician relationships and the profession when using social media. American College of Physicians website. Accessed July 3, 2015.
- Opinion 9.124—professionalism in the use of social media. American Medical Association website. Accessed July 3, 2015.
- HIPPA PHI: list of 18 identifiers and definition of PHI. The Committee for Protection of Human Subjects website. Accessed July 10, 2015.
- FOAM. Life in the Fastlane website. Accessed September 6, 2015.
How Should a Hospitalized Patient with Newly Diagnosed Cirrhosis Be Evaluated and Managed?
The Case
A 50-year-old man with no known medical history presents with two months of increasing abdominal distension. Exam is notable for scleral icterus, telangiectasias on the upper chest, abdominal distention with a positive fluid wave, and bilateral pitting lower-extremity edema. An abdominal ultrasound shows large ascites and a nodular liver consistent with cirrhosis. How should this patient with newly diagnosed cirrhosis be evaluated and managed?
Background
Cirrhosis is a leading cause of death among people ages 25–64 and associated with a mortality rate of 11.5 per 100,000 people.1 In 2010, 101,000 people were discharged from the hospital with chronic liver disease and cirrhosis as the first-listed diagnosis.2 Given the myriad etiologies and the asymptomatic nature of many of these conditions, hospitalists frequently encounter patients presenting with advanced disease.
Evaluation
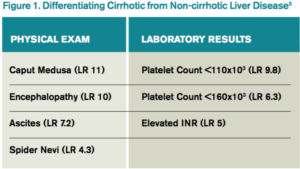
The gold standard for diagnosis is liver biopsy, although this is now usually reserved for atypical cases or where the etiology of cirrhosis is unclear. Alcohol and viral hepatitis (B and C) are the most common causes of chronic liver disease, with nonalcoholic steatohepatitis (NASH) increasing in prevalence. Other less common etiologies and characteristic test findings are listed in Figure 2.
Recently, the Centers for Disease Control and Prevention (CDC) recommended that adults born between 1945 and 1965 receive one-time testing for hepatitis C virus (HCV) infection, regardless of other risk factors, given the higher prevalence in this birth cohort and the introduction of newer oral treatments that achieve sustained virologic response.3
Management
The three classic complications of cirrhosis that will typically prompt inpatient admission are volume overload/ascites, gastrointestinal variceal bleeding, and hepatic encephalopathy.
Volume overload/ascites. Ascites is the most common major complication of cirrhosis, with roughly 50% of patients with asymptomatic cirrhosis developing ascites within 10 years.4 Ascites development portends a poor prognosis, with a mortality of 15% within one year and 44% within five years of diagnosis.4 Patients presenting with new-onset ascites should have a diagnostic paracentesis performed to determine the etiology and evaluate for infection.
Ascitic fluid should be sent for an albumin level and a cell count with differential. A serum-ascites albumin gradient (SAAG) of greater than or equal to 1.1 g/dL is consistent with portal hypertension and cirrhosis, while values less than 1.1 g/dL suggest a non-cirrhotic cause, such as infection or malignancy. Due to the high prevalence of spontaneous bacterial peritonitis (SBP) in hospitalized patients, fluid should also be immediately inoculated in aerobic and anaerobic culture bottles at the bedside, as this has been shown to improve the yield compared to inoculation of culture bottles in the laboratory. Other testing (such as cytology for the evaluation of malignancy) should only be performed if there is significant concern for a particular disease since the vast majority of cases are secondary to uncomplicated cirrhosis.4
In patients with a large amount of ascites and related symptoms (eg, abdominal pain, shortness of breath), therapeutic paracentesis should be performed. Although there is controversy over the need for routine albumin administration, guidelines currently recommend the infusion of 6–8 g of albumin per liter of ascites removed for paracentesis volumes of greater than 4–5 liters.4
No data support the routine administration of fresh frozen plasma (FFP) or platelets prior to paracentesis. Although significant complications of paracentesis (including bowel perforation and hemorrhage) may occur, these are exceedingly rare. Ultrasonography can be used to decrease risks and identify suitable pockets of fluid to tap, even when fluid is not obvious on physical exam alone.5
For patients with significant edema or ascites that is due to portal hypertension (SAAG >1.1 g/dL), the first-line therapy is sodium restriction to less than 2,000 mg/day. Consulting a nutritionist may be beneficial for patient education.
For patients with significant natriuresis (>78 mmol daily urine sodium excretion), dietary restriction alone can manage fluid retention. Most patients (85%–90%), however, require diuretics to increase sodium output. Single-agent spironolactone is more efficacious than single-agent furosemide, but diuresis is improved when both agents are used.4 A dosing regimen of once-daily 40 mg furosemide and 100 mg spironolactone is the recommended starting regimen to promote diuresis while maintaining normokalemia. Due to the long half-life of spironolactone, the dose can be increased every three to five days if needed for diuresis.4
Gastroesophageal variceal bleeding. Approximately 50% of patients with cirrhosis have gastroesophageal varices as a consequence of portal hypertension, with prevalence increasing in those with more severe disease.6 As many patients with cirrhosis have advanced disease at the time of diagnosis, it is recommended that patients be referred for endoscopic screening when diagnosed.6 Nonselective beta-blockers decrease the risk of bleeding in patients with known varices but should not be initiated empirically in all patients with cirrhosis given significant side effects, including worsening of ascites.
There is increasing evidence that there is a “window” period for beta-blocker use in cirrhosis with the window opening after the diagnosis of varices and the window closing at advanced stages of disease (marked by an episode of spontaneous bacterial peritonitis, refractory ascites, or hepatorenal syndrome, for example).7
Hepatic encephalopathy. Hepatic encephalopathy (HE) is another complication of portal hypertension and is seen in 10%–14% of patients at the time of cirrhosis diagnosis.8 Overt HE is estimated to occur in 30%–40% of patients with cirrhosis at some point during their disease course, and more subtle forms (minimal or covert HE) are seen in up to 80%.8 HE can cause numerous neurologic and psychiatric issues including personality changes, poor memory, sleep-wake disturbances, and alterations in consciousness.
In patients with an episode of encephalopathy, precipitating factors should be evaluated. Typical precipitants include infections, bleeding, electrolyte disorders, and constipation. Ammonia levels are frequently drawn as part of the evaluation of hepatic encephalopathy, but elevated levels do not significantly change diagnostic probabilities or add prognostic information.8 A low ammonia level, on the other hand, may be useful in lowering the probability of hepatic encephalopathy in a patient with altered mental status of unknown etiology.8
Routine primary prophylaxis of HE in all patients with cirrhosis is not currently recommended. Treatment is only recommended in patients with overt HE, with secondary prophylaxis administered following an episode due to the high risk for recurrence.
Other Issues
VTE prophylaxis. Although patients with cirrhosis are often presumed to be “auto-anticoagulated” due to an elevated international normalized ratio (INR), they experience thrombotic complications during hospitalization at the same rate or higher than patients with other chronic illnesses.9 Unfortunately, studies examining venous thromboembolism (VTE) prophylaxis in hospitalized patients have generally excluded cirrhotics. Therefore, risks/benefits of prophylaxis need to be considered on an individual basis, taking into account the presence of varices (if known), platelet count, and other VTE risk factors.
Drugs to avoid. As detailed above, nonselective beta-blockers should be avoided when outside the “window” period of benefit. Patients with cirrhosis should be counseled to avoid nonsteroidal anti-inflammatory drugs (NSAIDs) due to an increased risk of bleeding and renal dysfunction. ACE inhibitors (ACE-Is) and angiotensin-receptor blockers (ARBs) can also precipitate renal dysfunction and should generally be avoided unless strongly indicated for another diagnosis.
There is conflicting evidence with regard to whether the use of proton-pump inhibitors (PPIs) in cirrhotics increases the risk of SBP.10,11 Nevertheless, it is prudent to reevaluate the need for PPIs in patients with cirrhosis to determine where a true indication exists.
Post-hospitalization care. Patients with a new diagnosis of cirrhosis require screening for esophageal varices and hepatocellular carcinoma (HCC), with frequency of subsequent testing based on initial results. They should also be immunized against hepatitis A (HAV) and hepatitis B (HBV), if not already immune. Specific treatments are available for many causes of cirrhosis, including new antiviral agents against hepatitis C (HCV), and liver transplantation is an option for select patients. Given the complexity of subsequent diagnostic and treatment options, patients with new cirrhosis should be referred to a gastroenterologist or hepatologist, if possible.
Back to the Case
The patient is hospitalized, and a large-volume paracentesis is performed. Four liters are removed without the administration of albumin. Ascitic fluid analysis reveals a SAAG of greater than 1.1 g/dL and a polymorphonuclear cell count of 50 cell/mm3, suggesting ascites due to portal hypertension and ruling out infection. Nutrition is consulted and educates the patient on a restricted-sodium diet. Furosemide is started at 40 mg daily; spironolactone is started at 100 mg daily. Initial workup and serologies demonstrate active HCV infection (HCV RNA positive), with immunity to HBV due to vaccination. HAV vaccination is administered given lack of seropositivity. The patient is screened for alcohol and found not to drink alcohol. By the time of discharge, the patient is experiencing daily 0.5 kg weight loss due to diuretics and has stable renal function. The patient is referred to outpatient gastroenterology for gastroesophageal variceal screening and consideration of HCV treatment and/or liver transplantation.
Bottom Line
Workup and management of cirrhosis should focus on revealing the underlying etiology, managing complications, and discharging patients with a comprehensive follow-up plan. TH
Dr. Sehgal and Dr. Hanson are hospitalists in the division of hospital medicine at the University of Texas Health Science Center at San Antonio and the South Texas Veterans Health Care System.
References
- Heron M. Deaths: leading causes for 2012. Natl Vital Stat Rep. 2015;64(10):1-93.
- Chronic liver disease and cirrhosis. Centers for Disease Control and Prevention website. Accessed March 17, 2016.
- Smith BD, Morgan RL, Beckett GA, Falck-Ytter Y, Holtzman D, Ward JW. Hepatitis C virus testing of persons born during 1945-1965: recommendations from the Centers for Disease Control and Prevention. Ann Intern Med. 2012;157(11):817-822. doi:10.7326/0003-4819-157-9-201211060-00529.
- Runyon BA, AASLD. Introduction to the revised American Association for the Study of Liver Diseases Practice Guideline management of adult patients with ascites due to cirrhosis 2012. Hepatology. 2013;57(4):1651-1653. doi:10.1002/hep.26359.
- Udell JA, Wang CS, Tinmouth J, et al. Does this patient with liver disease have cirrhosis? JAMA. 2012;307(8):832-842. doi:10.1001/jama.2012.186.
- Garcia-Tsao G, Sanyal AJ, Grace ND, Carey W, Practice Guidelines Committee of the American Association for the Study of Liver Diseases, Practice Parameters Committee of the American College of Gastroenterology. Prevention and management of gastroesophageal varices and variceal hemorrhage in cirrhosis. Hepatology. 2007;46(3):922-938. doi:10.1002/hep.21907.
- Mandorfer M, Bota S, Schwabl P, et al. Nonselective β blockers increase risk for hepatorenal syndrome and death in patients with cirrhosis and spontaneous bacterial peritonitis. Gastroenterology. 2014;146(7):1680-90.e1. doi:10.1053/j.gastro.2014.03.005.
- Vilstrup H, Amodio P, Bajaj J, et al. Hepatic encephalopathy in chronic liver disease: 2014 Practice Guideline by the American Association for the Study of Liver Diseases and the European Association for the Study of the Liver. Hepatology. 2014;60(2):715-735. doi:10.1002/hep.27210.
- Khoury T, Ayman AR, Cohen J, Daher S, Shmuel C, Mizrahi M. The complex role of anticoagulation in cirrhosis: an updated review of where we are and where we are going. Digestion. 2016;93(2):149-159. doi:10.1159/000442877.
- Terg R, Casciato P, Garbe C, et al. Proton pump inhibitor therapy does not increase the incidence of spontaneous bacterial peritonitis in cirrhosis: a multicenter prospective study. J Hepatol. 2015;62(5):1056-1060. doi:10.1016/j.jhep.2014.11.036.
- Deshpande A, Pasupuleti V, Thota P, et al. Acid-suppressive therapy is associated with spontaneous bacterial peritonitis in cirrhotic patients: a meta-analysis. J Gastroenterol Hepatol. 2013;28(2):235-242. doi:10.1111/jgh.12065.
Key Points
- Cirrhosis has many etiologies, and new diagnoses require further investigation as to the underlying etiology.
- Initial management should focus on evaluation and treatment of complications, including ascites, esophageal varices, and hepatic encephalopathy.
- A diagnostic paracentesis, salt restriction, and a nutrition consult are the initial therapies for ascites although most patients will also require diuretics to increase sodium excretion.
- Once stabilized, the cirrhotic patient will require specialty care for possible liver biopsy (if etiology remains unclear), treatment (eg, HCV antivirals), and/or referral for liver transplantation.
The Case
A 50-year-old man with no known medical history presents with two months of increasing abdominal distension. Exam is notable for scleral icterus, telangiectasias on the upper chest, abdominal distention with a positive fluid wave, and bilateral pitting lower-extremity edema. An abdominal ultrasound shows large ascites and a nodular liver consistent with cirrhosis. How should this patient with newly diagnosed cirrhosis be evaluated and managed?
Background
Cirrhosis is a leading cause of death among people ages 25–64 and associated with a mortality rate of 11.5 per 100,000 people.1 In 2010, 101,000 people were discharged from the hospital with chronic liver disease and cirrhosis as the first-listed diagnosis.2 Given the myriad etiologies and the asymptomatic nature of many of these conditions, hospitalists frequently encounter patients presenting with advanced disease.
Evaluation
The gold standard for diagnosis is liver biopsy, although this is now usually reserved for atypical cases or where the etiology of cirrhosis is unclear. Alcohol and viral hepatitis (B and C) are the most common causes of chronic liver disease, with nonalcoholic steatohepatitis (NASH) increasing in prevalence. Other less common etiologies and characteristic test findings are listed in Figure 2.
Recently, the Centers for Disease Control and Prevention (CDC) recommended that adults born between 1945 and 1965 receive one-time testing for hepatitis C virus (HCV) infection, regardless of other risk factors, given the higher prevalence in this birth cohort and the introduction of newer oral treatments that achieve sustained virologic response.3
Management
The three classic complications of cirrhosis that will typically prompt inpatient admission are volume overload/ascites, gastrointestinal variceal bleeding, and hepatic encephalopathy.
Volume overload/ascites. Ascites is the most common major complication of cirrhosis, with roughly 50% of patients with asymptomatic cirrhosis developing ascites within 10 years.4 Ascites development portends a poor prognosis, with a mortality of 15% within one year and 44% within five years of diagnosis.4 Patients presenting with new-onset ascites should have a diagnostic paracentesis performed to determine the etiology and evaluate for infection.
Ascitic fluid should be sent for an albumin level and a cell count with differential. A serum-ascites albumin gradient (SAAG) of greater than or equal to 1.1 g/dL is consistent with portal hypertension and cirrhosis, while values less than 1.1 g/dL suggest a non-cirrhotic cause, such as infection or malignancy. Due to the high prevalence of spontaneous bacterial peritonitis (SBP) in hospitalized patients, fluid should also be immediately inoculated in aerobic and anaerobic culture bottles at the bedside, as this has been shown to improve the yield compared to inoculation of culture bottles in the laboratory. Other testing (such as cytology for the evaluation of malignancy) should only be performed if there is significant concern for a particular disease since the vast majority of cases are secondary to uncomplicated cirrhosis.4
In patients with a large amount of ascites and related symptoms (eg, abdominal pain, shortness of breath), therapeutic paracentesis should be performed. Although there is controversy over the need for routine albumin administration, guidelines currently recommend the infusion of 6–8 g of albumin per liter of ascites removed for paracentesis volumes of greater than 4–5 liters.4
No data support the routine administration of fresh frozen plasma (FFP) or platelets prior to paracentesis. Although significant complications of paracentesis (including bowel perforation and hemorrhage) may occur, these are exceedingly rare. Ultrasonography can be used to decrease risks and identify suitable pockets of fluid to tap, even when fluid is not obvious on physical exam alone.5
For patients with significant edema or ascites that is due to portal hypertension (SAAG >1.1 g/dL), the first-line therapy is sodium restriction to less than 2,000 mg/day. Consulting a nutritionist may be beneficial for patient education.
For patients with significant natriuresis (>78 mmol daily urine sodium excretion), dietary restriction alone can manage fluid retention. Most patients (85%–90%), however, require diuretics to increase sodium output. Single-agent spironolactone is more efficacious than single-agent furosemide, but diuresis is improved when both agents are used.4 A dosing regimen of once-daily 40 mg furosemide and 100 mg spironolactone is the recommended starting regimen to promote diuresis while maintaining normokalemia. Due to the long half-life of spironolactone, the dose can be increased every three to five days if needed for diuresis.4
Gastroesophageal variceal bleeding. Approximately 50% of patients with cirrhosis have gastroesophageal varices as a consequence of portal hypertension, with prevalence increasing in those with more severe disease.6 As many patients with cirrhosis have advanced disease at the time of diagnosis, it is recommended that patients be referred for endoscopic screening when diagnosed.6 Nonselective beta-blockers decrease the risk of bleeding in patients with known varices but should not be initiated empirically in all patients with cirrhosis given significant side effects, including worsening of ascites.
There is increasing evidence that there is a “window” period for beta-blocker use in cirrhosis with the window opening after the diagnosis of varices and the window closing at advanced stages of disease (marked by an episode of spontaneous bacterial peritonitis, refractory ascites, or hepatorenal syndrome, for example).7
Hepatic encephalopathy. Hepatic encephalopathy (HE) is another complication of portal hypertension and is seen in 10%–14% of patients at the time of cirrhosis diagnosis.8 Overt HE is estimated to occur in 30%–40% of patients with cirrhosis at some point during their disease course, and more subtle forms (minimal or covert HE) are seen in up to 80%.8 HE can cause numerous neurologic and psychiatric issues including personality changes, poor memory, sleep-wake disturbances, and alterations in consciousness.
In patients with an episode of encephalopathy, precipitating factors should be evaluated. Typical precipitants include infections, bleeding, electrolyte disorders, and constipation. Ammonia levels are frequently drawn as part of the evaluation of hepatic encephalopathy, but elevated levels do not significantly change diagnostic probabilities or add prognostic information.8 A low ammonia level, on the other hand, may be useful in lowering the probability of hepatic encephalopathy in a patient with altered mental status of unknown etiology.8
Routine primary prophylaxis of HE in all patients with cirrhosis is not currently recommended. Treatment is only recommended in patients with overt HE, with secondary prophylaxis administered following an episode due to the high risk for recurrence.
Other Issues
VTE prophylaxis. Although patients with cirrhosis are often presumed to be “auto-anticoagulated” due to an elevated international normalized ratio (INR), they experience thrombotic complications during hospitalization at the same rate or higher than patients with other chronic illnesses.9 Unfortunately, studies examining venous thromboembolism (VTE) prophylaxis in hospitalized patients have generally excluded cirrhotics. Therefore, risks/benefits of prophylaxis need to be considered on an individual basis, taking into account the presence of varices (if known), platelet count, and other VTE risk factors.
Drugs to avoid. As detailed above, nonselective beta-blockers should be avoided when outside the “window” period of benefit. Patients with cirrhosis should be counseled to avoid nonsteroidal anti-inflammatory drugs (NSAIDs) due to an increased risk of bleeding and renal dysfunction. ACE inhibitors (ACE-Is) and angiotensin-receptor blockers (ARBs) can also precipitate renal dysfunction and should generally be avoided unless strongly indicated for another diagnosis.
There is conflicting evidence with regard to whether the use of proton-pump inhibitors (PPIs) in cirrhotics increases the risk of SBP.10,11 Nevertheless, it is prudent to reevaluate the need for PPIs in patients with cirrhosis to determine where a true indication exists.
Post-hospitalization care. Patients with a new diagnosis of cirrhosis require screening for esophageal varices and hepatocellular carcinoma (HCC), with frequency of subsequent testing based on initial results. They should also be immunized against hepatitis A (HAV) and hepatitis B (HBV), if not already immune. Specific treatments are available for many causes of cirrhosis, including new antiviral agents against hepatitis C (HCV), and liver transplantation is an option for select patients. Given the complexity of subsequent diagnostic and treatment options, patients with new cirrhosis should be referred to a gastroenterologist or hepatologist, if possible.
Back to the Case
The patient is hospitalized, and a large-volume paracentesis is performed. Four liters are removed without the administration of albumin. Ascitic fluid analysis reveals a SAAG of greater than 1.1 g/dL and a polymorphonuclear cell count of 50 cell/mm3, suggesting ascites due to portal hypertension and ruling out infection. Nutrition is consulted and educates the patient on a restricted-sodium diet. Furosemide is started at 40 mg daily; spironolactone is started at 100 mg daily. Initial workup and serologies demonstrate active HCV infection (HCV RNA positive), with immunity to HBV due to vaccination. HAV vaccination is administered given lack of seropositivity. The patient is screened for alcohol and found not to drink alcohol. By the time of discharge, the patient is experiencing daily 0.5 kg weight loss due to diuretics and has stable renal function. The patient is referred to outpatient gastroenterology for gastroesophageal variceal screening and consideration of HCV treatment and/or liver transplantation.
Bottom Line
Workup and management of cirrhosis should focus on revealing the underlying etiology, managing complications, and discharging patients with a comprehensive follow-up plan. TH
Dr. Sehgal and Dr. Hanson are hospitalists in the division of hospital medicine at the University of Texas Health Science Center at San Antonio and the South Texas Veterans Health Care System.
References
- Heron M. Deaths: leading causes for 2012. Natl Vital Stat Rep. 2015;64(10):1-93.
- Chronic liver disease and cirrhosis. Centers for Disease Control and Prevention website. Accessed March 17, 2016.
- Smith BD, Morgan RL, Beckett GA, Falck-Ytter Y, Holtzman D, Ward JW. Hepatitis C virus testing of persons born during 1945-1965: recommendations from the Centers for Disease Control and Prevention. Ann Intern Med. 2012;157(11):817-822. doi:10.7326/0003-4819-157-9-201211060-00529.
- Runyon BA, AASLD. Introduction to the revised American Association for the Study of Liver Diseases Practice Guideline management of adult patients with ascites due to cirrhosis 2012. Hepatology. 2013;57(4):1651-1653. doi:10.1002/hep.26359.
- Udell JA, Wang CS, Tinmouth J, et al. Does this patient with liver disease have cirrhosis? JAMA. 2012;307(8):832-842. doi:10.1001/jama.2012.186.
- Garcia-Tsao G, Sanyal AJ, Grace ND, Carey W, Practice Guidelines Committee of the American Association for the Study of Liver Diseases, Practice Parameters Committee of the American College of Gastroenterology. Prevention and management of gastroesophageal varices and variceal hemorrhage in cirrhosis. Hepatology. 2007;46(3):922-938. doi:10.1002/hep.21907.
- Mandorfer M, Bota S, Schwabl P, et al. Nonselective β blockers increase risk for hepatorenal syndrome and death in patients with cirrhosis and spontaneous bacterial peritonitis. Gastroenterology. 2014;146(7):1680-90.e1. doi:10.1053/j.gastro.2014.03.005.
- Vilstrup H, Amodio P, Bajaj J, et al. Hepatic encephalopathy in chronic liver disease: 2014 Practice Guideline by the American Association for the Study of Liver Diseases and the European Association for the Study of the Liver. Hepatology. 2014;60(2):715-735. doi:10.1002/hep.27210.
- Khoury T, Ayman AR, Cohen J, Daher S, Shmuel C, Mizrahi M. The complex role of anticoagulation in cirrhosis: an updated review of where we are and where we are going. Digestion. 2016;93(2):149-159. doi:10.1159/000442877.
- Terg R, Casciato P, Garbe C, et al. Proton pump inhibitor therapy does not increase the incidence of spontaneous bacterial peritonitis in cirrhosis: a multicenter prospective study. J Hepatol. 2015;62(5):1056-1060. doi:10.1016/j.jhep.2014.11.036.
- Deshpande A, Pasupuleti V, Thota P, et al. Acid-suppressive therapy is associated with spontaneous bacterial peritonitis in cirrhotic patients: a meta-analysis. J Gastroenterol Hepatol. 2013;28(2):235-242. doi:10.1111/jgh.12065.
Key Points
- Cirrhosis has many etiologies, and new diagnoses require further investigation as to the underlying etiology.
- Initial management should focus on evaluation and treatment of complications, including ascites, esophageal varices, and hepatic encephalopathy.
- A diagnostic paracentesis, salt restriction, and a nutrition consult are the initial therapies for ascites although most patients will also require diuretics to increase sodium excretion.
- Once stabilized, the cirrhotic patient will require specialty care for possible liver biopsy (if etiology remains unclear), treatment (eg, HCV antivirals), and/or referral for liver transplantation.
The Case
A 50-year-old man with no known medical history presents with two months of increasing abdominal distension. Exam is notable for scleral icterus, telangiectasias on the upper chest, abdominal distention with a positive fluid wave, and bilateral pitting lower-extremity edema. An abdominal ultrasound shows large ascites and a nodular liver consistent with cirrhosis. How should this patient with newly diagnosed cirrhosis be evaluated and managed?
Background
Cirrhosis is a leading cause of death among people ages 25–64 and associated with a mortality rate of 11.5 per 100,000 people.1 In 2010, 101,000 people were discharged from the hospital with chronic liver disease and cirrhosis as the first-listed diagnosis.2 Given the myriad etiologies and the asymptomatic nature of many of these conditions, hospitalists frequently encounter patients presenting with advanced disease.
Evaluation
The gold standard for diagnosis is liver biopsy, although this is now usually reserved for atypical cases or where the etiology of cirrhosis is unclear. Alcohol and viral hepatitis (B and C) are the most common causes of chronic liver disease, with nonalcoholic steatohepatitis (NASH) increasing in prevalence. Other less common etiologies and characteristic test findings are listed in Figure 2.
Recently, the Centers for Disease Control and Prevention (CDC) recommended that adults born between 1945 and 1965 receive one-time testing for hepatitis C virus (HCV) infection, regardless of other risk factors, given the higher prevalence in this birth cohort and the introduction of newer oral treatments that achieve sustained virologic response.3
Management
The three classic complications of cirrhosis that will typically prompt inpatient admission are volume overload/ascites, gastrointestinal variceal bleeding, and hepatic encephalopathy.
Volume overload/ascites. Ascites is the most common major complication of cirrhosis, with roughly 50% of patients with asymptomatic cirrhosis developing ascites within 10 years.4 Ascites development portends a poor prognosis, with a mortality of 15% within one year and 44% within five years of diagnosis.4 Patients presenting with new-onset ascites should have a diagnostic paracentesis performed to determine the etiology and evaluate for infection.
Ascitic fluid should be sent for an albumin level and a cell count with differential. A serum-ascites albumin gradient (SAAG) of greater than or equal to 1.1 g/dL is consistent with portal hypertension and cirrhosis, while values less than 1.1 g/dL suggest a non-cirrhotic cause, such as infection or malignancy. Due to the high prevalence of spontaneous bacterial peritonitis (SBP) in hospitalized patients, fluid should also be immediately inoculated in aerobic and anaerobic culture bottles at the bedside, as this has been shown to improve the yield compared to inoculation of culture bottles in the laboratory. Other testing (such as cytology for the evaluation of malignancy) should only be performed if there is significant concern for a particular disease since the vast majority of cases are secondary to uncomplicated cirrhosis.4
In patients with a large amount of ascites and related symptoms (eg, abdominal pain, shortness of breath), therapeutic paracentesis should be performed. Although there is controversy over the need for routine albumin administration, guidelines currently recommend the infusion of 6–8 g of albumin per liter of ascites removed for paracentesis volumes of greater than 4–5 liters.4
No data support the routine administration of fresh frozen plasma (FFP) or platelets prior to paracentesis. Although significant complications of paracentesis (including bowel perforation and hemorrhage) may occur, these are exceedingly rare. Ultrasonography can be used to decrease risks and identify suitable pockets of fluid to tap, even when fluid is not obvious on physical exam alone.5
For patients with significant edema or ascites that is due to portal hypertension (SAAG >1.1 g/dL), the first-line therapy is sodium restriction to less than 2,000 mg/day. Consulting a nutritionist may be beneficial for patient education.
For patients with significant natriuresis (>78 mmol daily urine sodium excretion), dietary restriction alone can manage fluid retention. Most patients (85%–90%), however, require diuretics to increase sodium output. Single-agent spironolactone is more efficacious than single-agent furosemide, but diuresis is improved when both agents are used.4 A dosing regimen of once-daily 40 mg furosemide and 100 mg spironolactone is the recommended starting regimen to promote diuresis while maintaining normokalemia. Due to the long half-life of spironolactone, the dose can be increased every three to five days if needed for diuresis.4
Gastroesophageal variceal bleeding. Approximately 50% of patients with cirrhosis have gastroesophageal varices as a consequence of portal hypertension, with prevalence increasing in those with more severe disease.6 As many patients with cirrhosis have advanced disease at the time of diagnosis, it is recommended that patients be referred for endoscopic screening when diagnosed.6 Nonselective beta-blockers decrease the risk of bleeding in patients with known varices but should not be initiated empirically in all patients with cirrhosis given significant side effects, including worsening of ascites.
There is increasing evidence that there is a “window” period for beta-blocker use in cirrhosis with the window opening after the diagnosis of varices and the window closing at advanced stages of disease (marked by an episode of spontaneous bacterial peritonitis, refractory ascites, or hepatorenal syndrome, for example).7
Hepatic encephalopathy. Hepatic encephalopathy (HE) is another complication of portal hypertension and is seen in 10%–14% of patients at the time of cirrhosis diagnosis.8 Overt HE is estimated to occur in 30%–40% of patients with cirrhosis at some point during their disease course, and more subtle forms (minimal or covert HE) are seen in up to 80%.8 HE can cause numerous neurologic and psychiatric issues including personality changes, poor memory, sleep-wake disturbances, and alterations in consciousness.
In patients with an episode of encephalopathy, precipitating factors should be evaluated. Typical precipitants include infections, bleeding, electrolyte disorders, and constipation. Ammonia levels are frequently drawn as part of the evaluation of hepatic encephalopathy, but elevated levels do not significantly change diagnostic probabilities or add prognostic information.8 A low ammonia level, on the other hand, may be useful in lowering the probability of hepatic encephalopathy in a patient with altered mental status of unknown etiology.8
Routine primary prophylaxis of HE in all patients with cirrhosis is not currently recommended. Treatment is only recommended in patients with overt HE, with secondary prophylaxis administered following an episode due to the high risk for recurrence.
Other Issues
VTE prophylaxis. Although patients with cirrhosis are often presumed to be “auto-anticoagulated” due to an elevated international normalized ratio (INR), they experience thrombotic complications during hospitalization at the same rate or higher than patients with other chronic illnesses.9 Unfortunately, studies examining venous thromboembolism (VTE) prophylaxis in hospitalized patients have generally excluded cirrhotics. Therefore, risks/benefits of prophylaxis need to be considered on an individual basis, taking into account the presence of varices (if known), platelet count, and other VTE risk factors.
Drugs to avoid. As detailed above, nonselective beta-blockers should be avoided when outside the “window” period of benefit. Patients with cirrhosis should be counseled to avoid nonsteroidal anti-inflammatory drugs (NSAIDs) due to an increased risk of bleeding and renal dysfunction. ACE inhibitors (ACE-Is) and angiotensin-receptor blockers (ARBs) can also precipitate renal dysfunction and should generally be avoided unless strongly indicated for another diagnosis.
There is conflicting evidence with regard to whether the use of proton-pump inhibitors (PPIs) in cirrhotics increases the risk of SBP.10,11 Nevertheless, it is prudent to reevaluate the need for PPIs in patients with cirrhosis to determine where a true indication exists.
Post-hospitalization care. Patients with a new diagnosis of cirrhosis require screening for esophageal varices and hepatocellular carcinoma (HCC), with frequency of subsequent testing based on initial results. They should also be immunized against hepatitis A (HAV) and hepatitis B (HBV), if not already immune. Specific treatments are available for many causes of cirrhosis, including new antiviral agents against hepatitis C (HCV), and liver transplantation is an option for select patients. Given the complexity of subsequent diagnostic and treatment options, patients with new cirrhosis should be referred to a gastroenterologist or hepatologist, if possible.
Back to the Case
The patient is hospitalized, and a large-volume paracentesis is performed. Four liters are removed without the administration of albumin. Ascitic fluid analysis reveals a SAAG of greater than 1.1 g/dL and a polymorphonuclear cell count of 50 cell/mm3, suggesting ascites due to portal hypertension and ruling out infection. Nutrition is consulted and educates the patient on a restricted-sodium diet. Furosemide is started at 40 mg daily; spironolactone is started at 100 mg daily. Initial workup and serologies demonstrate active HCV infection (HCV RNA positive), with immunity to HBV due to vaccination. HAV vaccination is administered given lack of seropositivity. The patient is screened for alcohol and found not to drink alcohol. By the time of discharge, the patient is experiencing daily 0.5 kg weight loss due to diuretics and has stable renal function. The patient is referred to outpatient gastroenterology for gastroesophageal variceal screening and consideration of HCV treatment and/or liver transplantation.
Bottom Line
Workup and management of cirrhosis should focus on revealing the underlying etiology, managing complications, and discharging patients with a comprehensive follow-up plan. TH
Dr. Sehgal and Dr. Hanson are hospitalists in the division of hospital medicine at the University of Texas Health Science Center at San Antonio and the South Texas Veterans Health Care System.
References
- Heron M. Deaths: leading causes for 2012. Natl Vital Stat Rep. 2015;64(10):1-93.
- Chronic liver disease and cirrhosis. Centers for Disease Control and Prevention website. Accessed March 17, 2016.
- Smith BD, Morgan RL, Beckett GA, Falck-Ytter Y, Holtzman D, Ward JW. Hepatitis C virus testing of persons born during 1945-1965: recommendations from the Centers for Disease Control and Prevention. Ann Intern Med. 2012;157(11):817-822. doi:10.7326/0003-4819-157-9-201211060-00529.
- Runyon BA, AASLD. Introduction to the revised American Association for the Study of Liver Diseases Practice Guideline management of adult patients with ascites due to cirrhosis 2012. Hepatology. 2013;57(4):1651-1653. doi:10.1002/hep.26359.
- Udell JA, Wang CS, Tinmouth J, et al. Does this patient with liver disease have cirrhosis? JAMA. 2012;307(8):832-842. doi:10.1001/jama.2012.186.
- Garcia-Tsao G, Sanyal AJ, Grace ND, Carey W, Practice Guidelines Committee of the American Association for the Study of Liver Diseases, Practice Parameters Committee of the American College of Gastroenterology. Prevention and management of gastroesophageal varices and variceal hemorrhage in cirrhosis. Hepatology. 2007;46(3):922-938. doi:10.1002/hep.21907.
- Mandorfer M, Bota S, Schwabl P, et al. Nonselective β blockers increase risk for hepatorenal syndrome and death in patients with cirrhosis and spontaneous bacterial peritonitis. Gastroenterology. 2014;146(7):1680-90.e1. doi:10.1053/j.gastro.2014.03.005.
- Vilstrup H, Amodio P, Bajaj J, et al. Hepatic encephalopathy in chronic liver disease: 2014 Practice Guideline by the American Association for the Study of Liver Diseases and the European Association for the Study of the Liver. Hepatology. 2014;60(2):715-735. doi:10.1002/hep.27210.
- Khoury T, Ayman AR, Cohen J, Daher S, Shmuel C, Mizrahi M. The complex role of anticoagulation in cirrhosis: an updated review of where we are and where we are going. Digestion. 2016;93(2):149-159. doi:10.1159/000442877.
- Terg R, Casciato P, Garbe C, et al. Proton pump inhibitor therapy does not increase the incidence of spontaneous bacterial peritonitis in cirrhosis: a multicenter prospective study. J Hepatol. 2015;62(5):1056-1060. doi:10.1016/j.jhep.2014.11.036.
- Deshpande A, Pasupuleti V, Thota P, et al. Acid-suppressive therapy is associated with spontaneous bacterial peritonitis in cirrhotic patients: a meta-analysis. J Gastroenterol Hepatol. 2013;28(2):235-242. doi:10.1111/jgh.12065.
Key Points
- Cirrhosis has many etiologies, and new diagnoses require further investigation as to the underlying etiology.
- Initial management should focus on evaluation and treatment of complications, including ascites, esophageal varices, and hepatic encephalopathy.
- A diagnostic paracentesis, salt restriction, and a nutrition consult are the initial therapies for ascites although most patients will also require diuretics to increase sodium excretion.
- Once stabilized, the cirrhotic patient will require specialty care for possible liver biopsy (if etiology remains unclear), treatment (eg, HCV antivirals), and/or referral for liver transplantation.
AAP Proposes Update to Evaluating, Managing Febrile Infants Guideline
Presenter: Kenneth Roberts, MD
One of PHM16’s most highly attended sessions was about anticipated updated from the American Academy of Pediatrics (AAP) to its guidelines for febrile infants ages 7¬–90 days. The proposed update stresses the need to separate individual components of serious bacterial infections (UTI, bacteremia, and meningitis) as the incidence and clinical course can vary greatly in this population.
The proposed inclusion criteria for infants for this algorithm require an infant to be full-term (37–43 weeks’ gestation), aged 7–90 days, well-appearing, and presenting with a temperature of 38°C. Proposed exclusion criteria include perinatal/prenatal/neonatal maternal fever, infection, or antimicrobial treatment; the presence of any evident infection; being technology-dependent; and the presence of congenital anomalies.
The proposed guideline update will aim to stratify management by ages 7–28 days, 29–60 days, and 61–90 days to provide the most appropriate and directed treatment. It will also include a role for inflammatory markers and allow for a “kinder, gentler” approach, including withholding certain treatments and procedures if infants are at low risk of infection. An active need for observation may be appropriate for certain infants as well.
Key Takeaway
It is likely that the AAP will update its algorithm for the management of well-appearing febrile infants ages 7–28 days, 29–60 days and 60–90 days. It will help standardize care in this population but should not be used as a substitute for clinical judgment. The new guidelines are expected to be published in early 2017.
Chandani DeZure, MD, FAAP, is a pediatric hospitalist at Children’s National Health System and instructor of pediatrics at George Washington University School of Medicine & Health Sciences in Washington, D.C.
Presenter: Kenneth Roberts, MD
One of PHM16’s most highly attended sessions was about anticipated updated from the American Academy of Pediatrics (AAP) to its guidelines for febrile infants ages 7¬–90 days. The proposed update stresses the need to separate individual components of serious bacterial infections (UTI, bacteremia, and meningitis) as the incidence and clinical course can vary greatly in this population.
The proposed inclusion criteria for infants for this algorithm require an infant to be full-term (37–43 weeks’ gestation), aged 7–90 days, well-appearing, and presenting with a temperature of 38°C. Proposed exclusion criteria include perinatal/prenatal/neonatal maternal fever, infection, or antimicrobial treatment; the presence of any evident infection; being technology-dependent; and the presence of congenital anomalies.
The proposed guideline update will aim to stratify management by ages 7–28 days, 29–60 days, and 61–90 days to provide the most appropriate and directed treatment. It will also include a role for inflammatory markers and allow for a “kinder, gentler” approach, including withholding certain treatments and procedures if infants are at low risk of infection. An active need for observation may be appropriate for certain infants as well.
Key Takeaway
It is likely that the AAP will update its algorithm for the management of well-appearing febrile infants ages 7–28 days, 29–60 days and 60–90 days. It will help standardize care in this population but should not be used as a substitute for clinical judgment. The new guidelines are expected to be published in early 2017.
Chandani DeZure, MD, FAAP, is a pediatric hospitalist at Children’s National Health System and instructor of pediatrics at George Washington University School of Medicine & Health Sciences in Washington, D.C.
Presenter: Kenneth Roberts, MD
One of PHM16’s most highly attended sessions was about anticipated updated from the American Academy of Pediatrics (AAP) to its guidelines for febrile infants ages 7¬–90 days. The proposed update stresses the need to separate individual components of serious bacterial infections (UTI, bacteremia, and meningitis) as the incidence and clinical course can vary greatly in this population.
The proposed inclusion criteria for infants for this algorithm require an infant to be full-term (37–43 weeks’ gestation), aged 7–90 days, well-appearing, and presenting with a temperature of 38°C. Proposed exclusion criteria include perinatal/prenatal/neonatal maternal fever, infection, or antimicrobial treatment; the presence of any evident infection; being technology-dependent; and the presence of congenital anomalies.
The proposed guideline update will aim to stratify management by ages 7–28 days, 29–60 days, and 61–90 days to provide the most appropriate and directed treatment. It will also include a role for inflammatory markers and allow for a “kinder, gentler” approach, including withholding certain treatments and procedures if infants are at low risk of infection. An active need for observation may be appropriate for certain infants as well.
Key Takeaway
It is likely that the AAP will update its algorithm for the management of well-appearing febrile infants ages 7–28 days, 29–60 days and 60–90 days. It will help standardize care in this population but should not be used as a substitute for clinical judgment. The new guidelines are expected to be published in early 2017.
Chandani DeZure, MD, FAAP, is a pediatric hospitalist at Children’s National Health System and instructor of pediatrics at George Washington University School of Medicine & Health Sciences in Washington, D.C.
PHM16: Visual Clues Can Help Establish a Diagnosis
PHM16’s Visual Diagnosis: Signs and Why They Matter session led by Dr. Kenneth Roberts and guest presenters was a review of case presentations in which visual clues were vital to establishing a diagnosis. Though much of the content was presented with pictures, the emphasis was placed on the importance of correct diagnosis to avoid both misdiagnoses/over-diagnoses and the potential harm that may result from inappropriate treatment. This may also translate into poor utilization of resources and significant financial burden that can result from the unnecessary hospitalization of a patient.
Many of the presented cases (such as the Gianotti-Crosti toddler over-diagnosed as eczema herpeticum, a child with pseudochromhidrosis misdiagnosed as a cyanotic disease, the case of phytophotodermatitis mistaken as child abuse, and a teen treated for 2 years for JIA before diagnosis of hypertrophic osteoarthropathy was made) highlighted examples in which there was extensive workup, hospitalization, subspecialty evaluation, and even incorrect treatment of patients.
In other instances, such as Henoch-Schonlein purpura, Waardenburg syndrome, or McCune-Albright syndrome, the correct diagnosis is necessary to help guide management and future treatment, including subspecialty evaluation.
Many diseases with visual presentations also have a benign course and require no treatment, and acknowledging this is important in providing reassurance to a family that may be very anxious over the physical appearance of their child.
This session underscores the need for experience and exposure to various signs, not only with rare medical conditions, but also in common illnesses such as Kawasaki and scarlet fever that may present similarly.
Key Takeaway:
Providers should have a high index of suspicion and use visual clues to make the correct diagnosis in order to guide treatment, avoid harm in children, and ensure appropriate utilization of resources.
Chandani DeZure, MD, FAAP, is a pediatric Hospitalist at Children’s National Health System, Instruction of Pediatrics at George Washington University’s School of Medicine and Health Sciences in Washington, D.C.
PHM16’s Visual Diagnosis: Signs and Why They Matter session led by Dr. Kenneth Roberts and guest presenters was a review of case presentations in which visual clues were vital to establishing a diagnosis. Though much of the content was presented with pictures, the emphasis was placed on the importance of correct diagnosis to avoid both misdiagnoses/over-diagnoses and the potential harm that may result from inappropriate treatment. This may also translate into poor utilization of resources and significant financial burden that can result from the unnecessary hospitalization of a patient.
Many of the presented cases (such as the Gianotti-Crosti toddler over-diagnosed as eczema herpeticum, a child with pseudochromhidrosis misdiagnosed as a cyanotic disease, the case of phytophotodermatitis mistaken as child abuse, and a teen treated for 2 years for JIA before diagnosis of hypertrophic osteoarthropathy was made) highlighted examples in which there was extensive workup, hospitalization, subspecialty evaluation, and even incorrect treatment of patients.
In other instances, such as Henoch-Schonlein purpura, Waardenburg syndrome, or McCune-Albright syndrome, the correct diagnosis is necessary to help guide management and future treatment, including subspecialty evaluation.
Many diseases with visual presentations also have a benign course and require no treatment, and acknowledging this is important in providing reassurance to a family that may be very anxious over the physical appearance of their child.
This session underscores the need for experience and exposure to various signs, not only with rare medical conditions, but also in common illnesses such as Kawasaki and scarlet fever that may present similarly.
Key Takeaway:
Providers should have a high index of suspicion and use visual clues to make the correct diagnosis in order to guide treatment, avoid harm in children, and ensure appropriate utilization of resources.
Chandani DeZure, MD, FAAP, is a pediatric Hospitalist at Children’s National Health System, Instruction of Pediatrics at George Washington University’s School of Medicine and Health Sciences in Washington, D.C.
PHM16’s Visual Diagnosis: Signs and Why They Matter session led by Dr. Kenneth Roberts and guest presenters was a review of case presentations in which visual clues were vital to establishing a diagnosis. Though much of the content was presented with pictures, the emphasis was placed on the importance of correct diagnosis to avoid both misdiagnoses/over-diagnoses and the potential harm that may result from inappropriate treatment. This may also translate into poor utilization of resources and significant financial burden that can result from the unnecessary hospitalization of a patient.
Many of the presented cases (such as the Gianotti-Crosti toddler over-diagnosed as eczema herpeticum, a child with pseudochromhidrosis misdiagnosed as a cyanotic disease, the case of phytophotodermatitis mistaken as child abuse, and a teen treated for 2 years for JIA before diagnosis of hypertrophic osteoarthropathy was made) highlighted examples in which there was extensive workup, hospitalization, subspecialty evaluation, and even incorrect treatment of patients.
In other instances, such as Henoch-Schonlein purpura, Waardenburg syndrome, or McCune-Albright syndrome, the correct diagnosis is necessary to help guide management and future treatment, including subspecialty evaluation.
Many diseases with visual presentations also have a benign course and require no treatment, and acknowledging this is important in providing reassurance to a family that may be very anxious over the physical appearance of their child.
This session underscores the need for experience and exposure to various signs, not only with rare medical conditions, but also in common illnesses such as Kawasaki and scarlet fever that may present similarly.
Key Takeaway:
Providers should have a high index of suspicion and use visual clues to make the correct diagnosis in order to guide treatment, avoid harm in children, and ensure appropriate utilization of resources.
Chandani DeZure, MD, FAAP, is a pediatric Hospitalist at Children’s National Health System, Instruction of Pediatrics at George Washington University’s School of Medicine and Health Sciences in Washington, D.C.
PHM16: The New AAP Clinical Practice Guideline on Evaluating, Managing Febrile Infants
One of PHM16’s most highly-attended sessions was an update on the anticipated AAP guidelines for febrile infants between ages 7-90 days given by Dr. Kenneth Roberts. The goal is to give evidence-based guidelines, not rules, from the most recent literature available. It also stresses the need to separate individual components of serious bacterial infections (UTI, bacteremia, and meningitis) as the incidence and clinical course can vary greatly in this population.
The inclusion criteria for infants for this upcoming algorithm require an infant to be full-term (37-43 weeks gestation), aged 7-90 days, well-appearing, and presenting with a temperature of 38 degrees Celsius.
Exclusion criteria include perinatal/prenatal/neonatal: maternal fever, infection, or antimicrobial treatment, the presence of any evident infection, being technology-dependent, and the presence of congenital anomalies.
The updated guideline will aim to stratify management by age 7-28 days, 29-60 days, and 61 to 90 days to provide the most appropriate and directed treatment.
It will also include a role for inflammatory markers, and allow for a “kinder, gentler” approach to the management of febrile infants aged 7-90 days including withholding certain treatments and procedures if infants are at low risk of infection. An active, not passive, need for observation may be appropriate for certain infants as well. These guidelines should be tailored for individual patients to provide the best care possible while minimizing risk in this population.
Key Takeaway:
An updated AAP Practice guideline algorithm for the management of well-appearing febrile infants 7-28 days, 29-60 days, and 60-90 days will be coming in the near future that will help standardize care in this population, but should not be used as a substitute for clinical judgment.
Chandani DeZure, MD, FAAP, is a pediatric hospitalist at Children’s National Health System, Instruction of Pediatrics at George Washington University’s School of Medicine and Health Sciences in Washington, D.C.
One of PHM16’s most highly-attended sessions was an update on the anticipated AAP guidelines for febrile infants between ages 7-90 days given by Dr. Kenneth Roberts. The goal is to give evidence-based guidelines, not rules, from the most recent literature available. It also stresses the need to separate individual components of serious bacterial infections (UTI, bacteremia, and meningitis) as the incidence and clinical course can vary greatly in this population.
The inclusion criteria for infants for this upcoming algorithm require an infant to be full-term (37-43 weeks gestation), aged 7-90 days, well-appearing, and presenting with a temperature of 38 degrees Celsius.
Exclusion criteria include perinatal/prenatal/neonatal: maternal fever, infection, or antimicrobial treatment, the presence of any evident infection, being technology-dependent, and the presence of congenital anomalies.
The updated guideline will aim to stratify management by age 7-28 days, 29-60 days, and 61 to 90 days to provide the most appropriate and directed treatment.
It will also include a role for inflammatory markers, and allow for a “kinder, gentler” approach to the management of febrile infants aged 7-90 days including withholding certain treatments and procedures if infants are at low risk of infection. An active, not passive, need for observation may be appropriate for certain infants as well. These guidelines should be tailored for individual patients to provide the best care possible while minimizing risk in this population.
Key Takeaway:
An updated AAP Practice guideline algorithm for the management of well-appearing febrile infants 7-28 days, 29-60 days, and 60-90 days will be coming in the near future that will help standardize care in this population, but should not be used as a substitute for clinical judgment.
Chandani DeZure, MD, FAAP, is a pediatric hospitalist at Children’s National Health System, Instruction of Pediatrics at George Washington University’s School of Medicine and Health Sciences in Washington, D.C.
One of PHM16’s most highly-attended sessions was an update on the anticipated AAP guidelines for febrile infants between ages 7-90 days given by Dr. Kenneth Roberts. The goal is to give evidence-based guidelines, not rules, from the most recent literature available. It also stresses the need to separate individual components of serious bacterial infections (UTI, bacteremia, and meningitis) as the incidence and clinical course can vary greatly in this population.
The inclusion criteria for infants for this upcoming algorithm require an infant to be full-term (37-43 weeks gestation), aged 7-90 days, well-appearing, and presenting with a temperature of 38 degrees Celsius.
Exclusion criteria include perinatal/prenatal/neonatal: maternal fever, infection, or antimicrobial treatment, the presence of any evident infection, being technology-dependent, and the presence of congenital anomalies.
The updated guideline will aim to stratify management by age 7-28 days, 29-60 days, and 61 to 90 days to provide the most appropriate and directed treatment.
It will also include a role for inflammatory markers, and allow for a “kinder, gentler” approach to the management of febrile infants aged 7-90 days including withholding certain treatments and procedures if infants are at low risk of infection. An active, not passive, need for observation may be appropriate for certain infants as well. These guidelines should be tailored for individual patients to provide the best care possible while minimizing risk in this population.
Key Takeaway:
An updated AAP Practice guideline algorithm for the management of well-appearing febrile infants 7-28 days, 29-60 days, and 60-90 days will be coming in the near future that will help standardize care in this population, but should not be used as a substitute for clinical judgment.
Chandani DeZure, MD, FAAP, is a pediatric hospitalist at Children’s National Health System, Instruction of Pediatrics at George Washington University’s School of Medicine and Health Sciences in Washington, D.C.
Genetic Makeup Influences Risk of Diabetes: Study
CHICAGO - A study examining the genes of more than 120,000 people from Europe, Asia, Africa and the Americas has offered the clearest picture yet of the genes that drive type 2 diabetes.
The study, published July 11 in the journal Nature, puts to rest a decades-long debate over the genetics that influence the risk of diabetes, which affects one in 10 people over the course of their lifetime.
And it has identified more than a dozen specific genes directly involved in the development of type 2 diabetes that might serve as potential drug targets.
"There was a whole furious debate that arose about this," said Dr. Francis Collins, director of the National Institutes of Health, one of more than 300 scientists collaborating on the work.
Prior studies turned up more than 80 spots in the genome associated with the development of adult-onset diabetes, but most of these genetic errors were common, meaning they occurred frequently in the population, and they explained only a small fraction of disease risk.
These discoveries were based on genome-wide association studies or GWAS, which used gene chips that scan thousands of genes at a time. Researchers used these to scan DNA from large populations of individuals with a specific disease and compare them with DNA from similar groups of healthy people.
Critics, including geneticist Dr. David Goldstein at Columbia University, argued that such studies were a waste of resources because they only found common variants that explained just a small fraction of the risk for disease.
He said the really important drivers of common diseases such as diabetes and schizophrenia were more likely to be found in extremely rare genes, those occurring in individuals or in families, not those shared by large populations of people.
Goldstein "argued very persuasively that it was all about rare variants and we were all going down the wrong road looking at the common ones," Collins said in a telephone interview.
The new study took a deeper look, using next-generation sequencing to search the entire genetic code of 2,657 people with and without diabetes to assess the contribution of both rare and common genes driving diabetes.
They also sequenced all of the protein-making genes in 12,940 people, and used statistical methods to estimate risk in another 111,548 people with less complete DNA data.
They found that, indeed, most of the genetic risk for type 2 diabetes is caused by common mistakes in the genetic code, with each mistake contributing only a small portion of an individual's risk for developing the disease.
"What this study says quite definitively for diabetes is the vast majority of hereditary risk variants are in fact these common ones, and the rare ones, while they pop up here and there, are a much smaller contribution," Collins said.
The study also turned up more than a dozen examples where variants alter the way proteins are made, suggesting that these gene variants have some direct impact on the development of type 2 diabetes.
"These represent promising avenues for efforts to design new ways to treat or prevent the disease," said Mark McCarthy, a senior author of the study from Oxford University.
All of the data will be made publicly available online through the Accelerating Medicines Partnership, a public-private partnership between the NIH, the U.S. Food and Drug Administration, 10 drug companies and several nonprofits.
Goldstein said the work was "a careful, solid investigation" that does not change his view much overall, adding that it was time to "quit arguing."
"What I care about now is finding the exact variants that infer risk, and understanding how they do so," he said.
SOURCE: http://go.nature.com/29DlL5i
Nature 2016.
CHICAGO - A study examining the genes of more than 120,000 people from Europe, Asia, Africa and the Americas has offered the clearest picture yet of the genes that drive type 2 diabetes.
The study, published July 11 in the journal Nature, puts to rest a decades-long debate over the genetics that influence the risk of diabetes, which affects one in 10 people over the course of their lifetime.
And it has identified more than a dozen specific genes directly involved in the development of type 2 diabetes that might serve as potential drug targets.
"There was a whole furious debate that arose about this," said Dr. Francis Collins, director of the National Institutes of Health, one of more than 300 scientists collaborating on the work.
Prior studies turned up more than 80 spots in the genome associated with the development of adult-onset diabetes, but most of these genetic errors were common, meaning they occurred frequently in the population, and they explained only a small fraction of disease risk.
These discoveries were based on genome-wide association studies or GWAS, which used gene chips that scan thousands of genes at a time. Researchers used these to scan DNA from large populations of individuals with a specific disease and compare them with DNA from similar groups of healthy people.
Critics, including geneticist Dr. David Goldstein at Columbia University, argued that such studies were a waste of resources because they only found common variants that explained just a small fraction of the risk for disease.
He said the really important drivers of common diseases such as diabetes and schizophrenia were more likely to be found in extremely rare genes, those occurring in individuals or in families, not those shared by large populations of people.
Goldstein "argued very persuasively that it was all about rare variants and we were all going down the wrong road looking at the common ones," Collins said in a telephone interview.
The new study took a deeper look, using next-generation sequencing to search the entire genetic code of 2,657 people with and without diabetes to assess the contribution of both rare and common genes driving diabetes.
They also sequenced all of the protein-making genes in 12,940 people, and used statistical methods to estimate risk in another 111,548 people with less complete DNA data.
They found that, indeed, most of the genetic risk for type 2 diabetes is caused by common mistakes in the genetic code, with each mistake contributing only a small portion of an individual's risk for developing the disease.
"What this study says quite definitively for diabetes is the vast majority of hereditary risk variants are in fact these common ones, and the rare ones, while they pop up here and there, are a much smaller contribution," Collins said.
The study also turned up more than a dozen examples where variants alter the way proteins are made, suggesting that these gene variants have some direct impact on the development of type 2 diabetes.
"These represent promising avenues for efforts to design new ways to treat or prevent the disease," said Mark McCarthy, a senior author of the study from Oxford University.
All of the data will be made publicly available online through the Accelerating Medicines Partnership, a public-private partnership between the NIH, the U.S. Food and Drug Administration, 10 drug companies and several nonprofits.
Goldstein said the work was "a careful, solid investigation" that does not change his view much overall, adding that it was time to "quit arguing."
"What I care about now is finding the exact variants that infer risk, and understanding how they do so," he said.
SOURCE: http://go.nature.com/29DlL5i
Nature 2016.
CHICAGO - A study examining the genes of more than 120,000 people from Europe, Asia, Africa and the Americas has offered the clearest picture yet of the genes that drive type 2 diabetes.
The study, published July 11 in the journal Nature, puts to rest a decades-long debate over the genetics that influence the risk of diabetes, which affects one in 10 people over the course of their lifetime.
And it has identified more than a dozen specific genes directly involved in the development of type 2 diabetes that might serve as potential drug targets.
"There was a whole furious debate that arose about this," said Dr. Francis Collins, director of the National Institutes of Health, one of more than 300 scientists collaborating on the work.
Prior studies turned up more than 80 spots in the genome associated with the development of adult-onset diabetes, but most of these genetic errors were common, meaning they occurred frequently in the population, and they explained only a small fraction of disease risk.
These discoveries were based on genome-wide association studies or GWAS, which used gene chips that scan thousands of genes at a time. Researchers used these to scan DNA from large populations of individuals with a specific disease and compare them with DNA from similar groups of healthy people.
Critics, including geneticist Dr. David Goldstein at Columbia University, argued that such studies were a waste of resources because they only found common variants that explained just a small fraction of the risk for disease.
He said the really important drivers of common diseases such as diabetes and schizophrenia were more likely to be found in extremely rare genes, those occurring in individuals or in families, not those shared by large populations of people.
Goldstein "argued very persuasively that it was all about rare variants and we were all going down the wrong road looking at the common ones," Collins said in a telephone interview.
The new study took a deeper look, using next-generation sequencing to search the entire genetic code of 2,657 people with and without diabetes to assess the contribution of both rare and common genes driving diabetes.
They also sequenced all of the protein-making genes in 12,940 people, and used statistical methods to estimate risk in another 111,548 people with less complete DNA data.
They found that, indeed, most of the genetic risk for type 2 diabetes is caused by common mistakes in the genetic code, with each mistake contributing only a small portion of an individual's risk for developing the disease.
"What this study says quite definitively for diabetes is the vast majority of hereditary risk variants are in fact these common ones, and the rare ones, while they pop up here and there, are a much smaller contribution," Collins said.
The study also turned up more than a dozen examples where variants alter the way proteins are made, suggesting that these gene variants have some direct impact on the development of type 2 diabetes.
"These represent promising avenues for efforts to design new ways to treat or prevent the disease," said Mark McCarthy, a senior author of the study from Oxford University.
All of the data will be made publicly available online through the Accelerating Medicines Partnership, a public-private partnership between the NIH, the U.S. Food and Drug Administration, 10 drug companies and several nonprofits.
Goldstein said the work was "a careful, solid investigation" that does not change his view much overall, adding that it was time to "quit arguing."
"What I care about now is finding the exact variants that infer risk, and understanding how they do so," he said.
SOURCE: http://go.nature.com/29DlL5i
Nature 2016.
Atrial Fibrillation Linked with Greater Alcohol Access
NEW YORK - Greater access to alcohol is linked with more atrial fibrillation but less myocardial infarction and congestive heart failure, researchers report.
Dr. Gregory M. Marcus, from the Division of Cardiology at the University of California, San Francisco, and colleagues conducted an observational cohort study of differences in health outcomes based on alcohol sales laws by county in Texas.
All patients were residents of Texas, 21 years old or older, and were admitted to hospitals in Texas between 2005 and 2010. More than 1 million patients were included in the analysis.
Of the counties, 47 were wet (no restrictions on the sale of alcohol) and 29 were dry (prohibition of alcohol sales). Seven of them changed from dry to wet during the study period.
The main cardiovascular outcomes were atrial fibrillation, acute myocardial infarction, and congestive heart failure.
After multivariable adjustment, wet county residents had a greater prevalence (odds ratio 1.05, p=0.007) and incidence (HR 1.07, p=0.014) of atrial fibrillation.
Prevalence of myocardial infarction was lower (OR 0.83, p<0.001), as was its incidence (HR 0.91, p=0.019). Prevalence of congestive heart failure was also lower (OR 0.87, p<0.001).
In the seven dry counties that changed their status to wet, the post-conversion interval (from dry to wet county status) was associated with greater odds of hospitalization for atrial fibrillation (OR 1.07, p=0.001) and congestive heart failure (OR 1.07, p<0.001).
The researchers found no difference in acute myocardial infarction (OR 0.99, p=0.746).
"Cardiovascular disease is the most common cause of death worldwide, and alcohol is the most widely consumed drug in the United States," said Dr. Rory Brett Weiner, a cardiologist at Massachusetts General Hospital in Boston.
He said that studying the impact of alcohol intake on incident cardiovascular disease is important for its public health implications.
"Differences in laws affecting access to alcohol are associated with changes in health outcomes, both harmful and protective," said Dr. Marcus, "but the study's findings shouldn't be used to change any specific legislation."
Dr. Weiner agreed. "The study design minimizes confounders commonly seen in prior research that relied on self-report," he said, "but it still doesn't provide conclusive evidence with regard to the use of alcohol and incident cardiovascular disease."
Dr. Weiner said that the study did not contain information on the level of individual alcohol exposure, and therefore, the impact of the 'dose' of alcohol on cardiovascular outcomes could not be ascertained.
"Based on the question at hand -- the impact of alcohol -- it's unlikely that a randomized controlled study will ever be performed," he said, "so analyses like the current one are important."
According to Dr. Marcus, "We still don't understand the mechanisms underlying the relationship between alcohol and cardiovascular disease, and have a long way to go to achieve the sort of personalized medicine needed to figure out how to counsel an individual patient on their particular "prescribed" amount, if any, of alcohol."
The National Institute on Alcohol Abuse and Alcoholism supported this research. Dr. Marcus reported research support from Medtronic and Pfizer and equity interest in InCarda.
SOURCE: http://bit.ly/1tlx1cx
BMJ 2016
NEW YORK - Greater access to alcohol is linked with more atrial fibrillation but less myocardial infarction and congestive heart failure, researchers report.
Dr. Gregory M. Marcus, from the Division of Cardiology at the University of California, San Francisco, and colleagues conducted an observational cohort study of differences in health outcomes based on alcohol sales laws by county in Texas.
All patients were residents of Texas, 21 years old or older, and were admitted to hospitals in Texas between 2005 and 2010. More than 1 million patients were included in the analysis.
Of the counties, 47 were wet (no restrictions on the sale of alcohol) and 29 were dry (prohibition of alcohol sales). Seven of them changed from dry to wet during the study period.
The main cardiovascular outcomes were atrial fibrillation, acute myocardial infarction, and congestive heart failure.
After multivariable adjustment, wet county residents had a greater prevalence (odds ratio 1.05, p=0.007) and incidence (HR 1.07, p=0.014) of atrial fibrillation.
Prevalence of myocardial infarction was lower (OR 0.83, p<0.001), as was its incidence (HR 0.91, p=0.019). Prevalence of congestive heart failure was also lower (OR 0.87, p<0.001).
In the seven dry counties that changed their status to wet, the post-conversion interval (from dry to wet county status) was associated with greater odds of hospitalization for atrial fibrillation (OR 1.07, p=0.001) and congestive heart failure (OR 1.07, p<0.001).
The researchers found no difference in acute myocardial infarction (OR 0.99, p=0.746).
"Cardiovascular disease is the most common cause of death worldwide, and alcohol is the most widely consumed drug in the United States," said Dr. Rory Brett Weiner, a cardiologist at Massachusetts General Hospital in Boston.
He said that studying the impact of alcohol intake on incident cardiovascular disease is important for its public health implications.
"Differences in laws affecting access to alcohol are associated with changes in health outcomes, both harmful and protective," said Dr. Marcus, "but the study's findings shouldn't be used to change any specific legislation."
Dr. Weiner agreed. "The study design minimizes confounders commonly seen in prior research that relied on self-report," he said, "but it still doesn't provide conclusive evidence with regard to the use of alcohol and incident cardiovascular disease."
Dr. Weiner said that the study did not contain information on the level of individual alcohol exposure, and therefore, the impact of the 'dose' of alcohol on cardiovascular outcomes could not be ascertained.
"Based on the question at hand -- the impact of alcohol -- it's unlikely that a randomized controlled study will ever be performed," he said, "so analyses like the current one are important."
According to Dr. Marcus, "We still don't understand the mechanisms underlying the relationship between alcohol and cardiovascular disease, and have a long way to go to achieve the sort of personalized medicine needed to figure out how to counsel an individual patient on their particular "prescribed" amount, if any, of alcohol."
The National Institute on Alcohol Abuse and Alcoholism supported this research. Dr. Marcus reported research support from Medtronic and Pfizer and equity interest in InCarda.
SOURCE: http://bit.ly/1tlx1cx
BMJ 2016
NEW YORK - Greater access to alcohol is linked with more atrial fibrillation but less myocardial infarction and congestive heart failure, researchers report.
Dr. Gregory M. Marcus, from the Division of Cardiology at the University of California, San Francisco, and colleagues conducted an observational cohort study of differences in health outcomes based on alcohol sales laws by county in Texas.
All patients were residents of Texas, 21 years old or older, and were admitted to hospitals in Texas between 2005 and 2010. More than 1 million patients were included in the analysis.
Of the counties, 47 were wet (no restrictions on the sale of alcohol) and 29 were dry (prohibition of alcohol sales). Seven of them changed from dry to wet during the study period.
The main cardiovascular outcomes were atrial fibrillation, acute myocardial infarction, and congestive heart failure.
After multivariable adjustment, wet county residents had a greater prevalence (odds ratio 1.05, p=0.007) and incidence (HR 1.07, p=0.014) of atrial fibrillation.
Prevalence of myocardial infarction was lower (OR 0.83, p<0.001), as was its incidence (HR 0.91, p=0.019). Prevalence of congestive heart failure was also lower (OR 0.87, p<0.001).
In the seven dry counties that changed their status to wet, the post-conversion interval (from dry to wet county status) was associated with greater odds of hospitalization for atrial fibrillation (OR 1.07, p=0.001) and congestive heart failure (OR 1.07, p<0.001).
The researchers found no difference in acute myocardial infarction (OR 0.99, p=0.746).
"Cardiovascular disease is the most common cause of death worldwide, and alcohol is the most widely consumed drug in the United States," said Dr. Rory Brett Weiner, a cardiologist at Massachusetts General Hospital in Boston.
He said that studying the impact of alcohol intake on incident cardiovascular disease is important for its public health implications.
"Differences in laws affecting access to alcohol are associated with changes in health outcomes, both harmful and protective," said Dr. Marcus, "but the study's findings shouldn't be used to change any specific legislation."
Dr. Weiner agreed. "The study design minimizes confounders commonly seen in prior research that relied on self-report," he said, "but it still doesn't provide conclusive evidence with regard to the use of alcohol and incident cardiovascular disease."
Dr. Weiner said that the study did not contain information on the level of individual alcohol exposure, and therefore, the impact of the 'dose' of alcohol on cardiovascular outcomes could not be ascertained.
"Based on the question at hand -- the impact of alcohol -- it's unlikely that a randomized controlled study will ever be performed," he said, "so analyses like the current one are important."
According to Dr. Marcus, "We still don't understand the mechanisms underlying the relationship between alcohol and cardiovascular disease, and have a long way to go to achieve the sort of personalized medicine needed to figure out how to counsel an individual patient on their particular "prescribed" amount, if any, of alcohol."
The National Institute on Alcohol Abuse and Alcoholism supported this research. Dr. Marcus reported research support from Medtronic and Pfizer and equity interest in InCarda.
SOURCE: http://bit.ly/1tlx1cx
BMJ 2016