User login
B-cell maturation antigen targeted in myeloma trials
NEW YORK – Three novel treatment strategies that target B-cell maturation antigen (BCMA) have shown promise in recent multiple myeloma clinical trials, according to Shaji K. Kumar, MD, of the Mayo Clinic Cancer Center in Rochester, Minn.
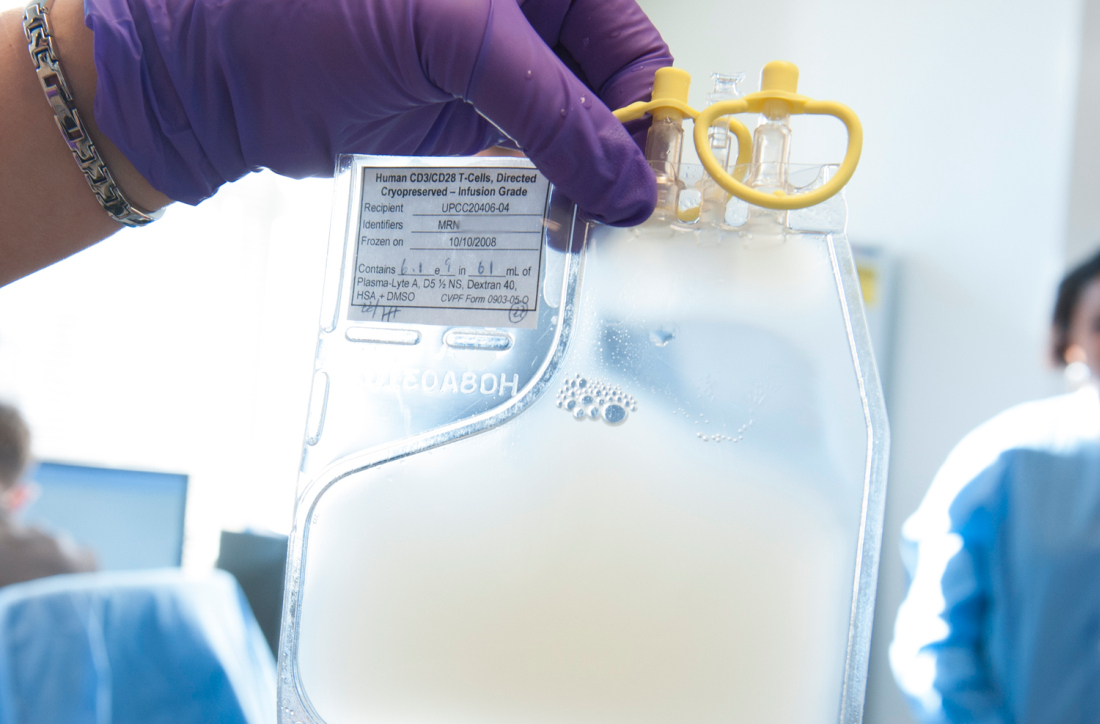
These strategies include B-cell maturation antigen (BCMA)–specific chimeric antigen receptor (CAR) T-cell therapies, bispecific T-cell engagers (BiTEs), and a BCMA antibody–drug conjugate, Dr. Kumar said at the annual congress on Hematologic Malignancies held by the National Comprehensive Cancer Network.
“Clearly, there are a lot of exciting drugs that are currently in clinical trials, but these three platforms appear to be much more advanced than the others, and hopefully we will see that in the clinic in the near future,” Dr. Kumar said.
The antibody-drug conjugate, GSK2857916, is a humanized IgG1 anti-BCMA antibody conjugated to a microtubule-disrupting agent that has produced an overall response rate in 67% in a group of myeloma patients who had previously received multiple standard-of-care agents.
“Some of the responses were quite durable, lasting several months,” he said.
Now, GSK2857916 is being evaluated in a variety of different combinations, including in a phase 2 study of the antibody-drug conjugate in combination with lenalidomide plus dexamethasone, or bortezomib plus dexamethasone, in patients with relapsed or refractory disease.
Some of the most “exciting” data with anti-BCMA CAR T-cell therapy in myeloma involves bb2121, which showed durable clinical responses in heavily pretreated patients, according to data presented at the 2017 annual meeting of the American Society of Hematology.
“The overall response rate is quite significant,” said Dr. Kumar, who related a 94% rate of overall response that was even higher in patients treated with doses of 150 x 106 CAR+ T cells or more. Many of the response were lasting, he said, with five patients in ongoing response for more than 1 year.
“The results are exciting enough that this is actually moving forward with registration trials,” Dr. Kumar said.
Additionally, promising results have been presented on a novel CAR T-cell product, LCAR-B38M, which principally targets BCMA and led to a significant number of patients who achieved stringent complete response that lasted beyond 1 year.
Multiple BCMA-targeting CAR T-cell products that use different vectors and costimulatory molecules are currently undergoing clinical trials, Dr. Kumar said.
In contrast to CAR T-cell products that must be customized to each patient in a process that takes weeks, BiTEs are a ready-made approach to allow T cells to engage with tumor cells.
“In patients with advanced disease, a lot can change in that short time frame, so having an approach that is off the shelf, which is not patient specific, is quite attractive,” Dr. Kumar said.
BCMA-directed BiTE therapies under investigation include AMG 420 and PF-06863135, he added.
Dr. Kumar reported one disclosure related to Dr. Reddy’s Laboratories.
NEW YORK – Three novel treatment strategies that target B-cell maturation antigen (BCMA) have shown promise in recent multiple myeloma clinical trials, according to Shaji K. Kumar, MD, of the Mayo Clinic Cancer Center in Rochester, Minn.
These strategies include B-cell maturation antigen (BCMA)–specific chimeric antigen receptor (CAR) T-cell therapies, bispecific T-cell engagers (BiTEs), and a BCMA antibody–drug conjugate, Dr. Kumar said at the annual congress on Hematologic Malignancies held by the National Comprehensive Cancer Network.
“Clearly, there are a lot of exciting drugs that are currently in clinical trials, but these three platforms appear to be much more advanced than the others, and hopefully we will see that in the clinic in the near future,” Dr. Kumar said.
The antibody-drug conjugate, GSK2857916, is a humanized IgG1 anti-BCMA antibody conjugated to a microtubule-disrupting agent that has produced an overall response rate in 67% in a group of myeloma patients who had previously received multiple standard-of-care agents.
“Some of the responses were quite durable, lasting several months,” he said.
Now, GSK2857916 is being evaluated in a variety of different combinations, including in a phase 2 study of the antibody-drug conjugate in combination with lenalidomide plus dexamethasone, or bortezomib plus dexamethasone, in patients with relapsed or refractory disease.
Some of the most “exciting” data with anti-BCMA CAR T-cell therapy in myeloma involves bb2121, which showed durable clinical responses in heavily pretreated patients, according to data presented at the 2017 annual meeting of the American Society of Hematology.
“The overall response rate is quite significant,” said Dr. Kumar, who related a 94% rate of overall response that was even higher in patients treated with doses of 150 x 106 CAR+ T cells or more. Many of the response were lasting, he said, with five patients in ongoing response for more than 1 year.
“The results are exciting enough that this is actually moving forward with registration trials,” Dr. Kumar said.
Additionally, promising results have been presented on a novel CAR T-cell product, LCAR-B38M, which principally targets BCMA and led to a significant number of patients who achieved stringent complete response that lasted beyond 1 year.
Multiple BCMA-targeting CAR T-cell products that use different vectors and costimulatory molecules are currently undergoing clinical trials, Dr. Kumar said.
In contrast to CAR T-cell products that must be customized to each patient in a process that takes weeks, BiTEs are a ready-made approach to allow T cells to engage with tumor cells.
“In patients with advanced disease, a lot can change in that short time frame, so having an approach that is off the shelf, which is not patient specific, is quite attractive,” Dr. Kumar said.
BCMA-directed BiTE therapies under investigation include AMG 420 and PF-06863135, he added.
Dr. Kumar reported one disclosure related to Dr. Reddy’s Laboratories.
NEW YORK – Three novel treatment strategies that target B-cell maturation antigen (BCMA) have shown promise in recent multiple myeloma clinical trials, according to Shaji K. Kumar, MD, of the Mayo Clinic Cancer Center in Rochester, Minn.
These strategies include B-cell maturation antigen (BCMA)–specific chimeric antigen receptor (CAR) T-cell therapies, bispecific T-cell engagers (BiTEs), and a BCMA antibody–drug conjugate, Dr. Kumar said at the annual congress on Hematologic Malignancies held by the National Comprehensive Cancer Network.
“Clearly, there are a lot of exciting drugs that are currently in clinical trials, but these three platforms appear to be much more advanced than the others, and hopefully we will see that in the clinic in the near future,” Dr. Kumar said.
The antibody-drug conjugate, GSK2857916, is a humanized IgG1 anti-BCMA antibody conjugated to a microtubule-disrupting agent that has produced an overall response rate in 67% in a group of myeloma patients who had previously received multiple standard-of-care agents.
“Some of the responses were quite durable, lasting several months,” he said.
Now, GSK2857916 is being evaluated in a variety of different combinations, including in a phase 2 study of the antibody-drug conjugate in combination with lenalidomide plus dexamethasone, or bortezomib plus dexamethasone, in patients with relapsed or refractory disease.
Some of the most “exciting” data with anti-BCMA CAR T-cell therapy in myeloma involves bb2121, which showed durable clinical responses in heavily pretreated patients, according to data presented at the 2017 annual meeting of the American Society of Hematology.
“The overall response rate is quite significant,” said Dr. Kumar, who related a 94% rate of overall response that was even higher in patients treated with doses of 150 x 106 CAR+ T cells or more. Many of the response were lasting, he said, with five patients in ongoing response for more than 1 year.
“The results are exciting enough that this is actually moving forward with registration trials,” Dr. Kumar said.
Additionally, promising results have been presented on a novel CAR T-cell product, LCAR-B38M, which principally targets BCMA and led to a significant number of patients who achieved stringent complete response that lasted beyond 1 year.
Multiple BCMA-targeting CAR T-cell products that use different vectors and costimulatory molecules are currently undergoing clinical trials, Dr. Kumar said.
In contrast to CAR T-cell products that must be customized to each patient in a process that takes weeks, BiTEs are a ready-made approach to allow T cells to engage with tumor cells.
“In patients with advanced disease, a lot can change in that short time frame, so having an approach that is off the shelf, which is not patient specific, is quite attractive,” Dr. Kumar said.
BCMA-directed BiTE therapies under investigation include AMG 420 and PF-06863135, he added.
Dr. Kumar reported one disclosure related to Dr. Reddy’s Laboratories.
EXPERT ANALYSIS FROM THE NCCN HEMATOLOGIC MALIGNANCIES CONGRESS
IMpower133: Atezolizumab plus standard chemotherapy boosted survival in ES-SCLC
TORONTO – Adding the humanized monoclonal programmed death-ligand 1 (PD-L1) antibody atezolizumab to standard first-line treatment of extensive-stage small cell lung cancer (ES-SCLC) significantly improved overall and progression-free survival in the phase 1/3 IMpower133 trial.
The combination may represent a new standard-of-care regimen for patients with untreated ES-SCLC, which is highly lethal – with 5-year survival of about 1%-3% – and represents about 13% of all lung cancers, Stephen V. Liu, MD, reported at the World Conference on Lung Cancer.
The findings were published simultaneously in the New England Journal of Medicine.
The median overall survival in 201 patients randomized to receive atezolizumab in addition to carboplatin and etoposide was 12.3 months, compared with 10.3 months in 202 patients who received placebo plus carboplatin and etoposide (hazard ratio, 0.7), Dr. Liu of Georgetown University, Washington, and a member of the trial steering committee said at the meeting, sponsored by the International Association for the Study of Lung Cancer.
“That translates to a 30% reduction in the risk of patient death,” he said at a press briefing during the conference. “Patients receiving atezolizumab had a much greater likelihood of being alive at 1 year, with a 1-year survival rate of 51.7% versus 38.2%.”
Median progression-free survival(PFS) also improved with atezolizumab (5.2 months vs. 4.3 months with placebo; HR, 0.77), as did 6-month PFS. At 12 months there was more than a doubling of PFS in the atezolizumab group (5.0% vs. 12.6%), he said.
Participants in the double-blind trial were treatment-naive all-comers with measurable ES-SCLC and good performance status. They received four 21-day cycles of intravenous carboplatin (area under the curve, 5 mg/mL per minute) on day 1 plus intravenous etoposide (100 mg/m2) on days 1-3 with either concurrent 1,200 mg of atezolizumab on day 1 or placebo, followed by maintenance therapy with atezolizumab or placebo until intolerable toxicity or disease progression.
The treatment benefits were seen across many patient subgroups and regardless of tumor mutational burden.
The atezolizumab safety profile was as expected with no new safety signals and did not compromise patients’ ability to complete four treatment cycles, Dr. Liu noted.
The findings are exciting in that they represent the first in decades to show a significant improvement in survival in patients with ES-SCLC, he said. Although most patients have an initial response to standard-of-care chemotherapy, that response isn’t durable. “As much as we expect a response, we also know that it’s transient; we expect a response, we expect relapse. There hasn’t been a change really in the past 20 years, at least, with this regimen that we’ve been using since the 1980s.”
That’s not for lack of trying, he added, noting that more than 40 phase 3 studies have looked at more than 60 different drugs since the 1970s and have “failed to move the needle.”
Immunotherapy, however, has dramatically improved the therapeutic landscape in non–small cell lung cancer, and preclinical data and clinical experience suggest “a possible synergy between checkpoint inhibition and chemotherapy,” which led to this global study, he explained.
“This is the first study in over 20 years to show a significant improvement in survival and progression-free survival in initial treatment of small cell lung cancer. The concurrent administration of atezolizumab with chemotherapy helped people live longer, compared to chemotherapy alone,” Dr. Liu concluded, adding in a press statement that “this is an exciting time in oncology, and we are thrilled to finally see real progress in the SCLC space.”
When questioned about the role of PD-L1 in this population and the possibility of identifying a subgroup in which this treatment may be more cost effective, he noted that tissue samples weren’t required at enrollment in this study, but were collected from some patients, and future analyses will assess those samples to try to determine if there are subsets of patients who derive particular benefit from immunotherapy in this setting.
“But today, in an all-comer population, this combination has improved survival,” he said.
IMpower133 was sponsored by F. Hoffman–La Roche. Dr. Liu is a speaker or advisory board member for Genentech, Pfizer, Takeda, Celgene, Eli Lilly, Taiho Pharmaceutical, Bristol-Myers Squibb, AstraZeneca, and Ignyta, and has received research or grant support from Genentech, Pfizer, Threshold Pharmaceuticals, Clovis Oncology, Corvus Pharmaceuticals, Esanex, Bayer, OncoMed Pharmaceuticals, Ignyta, Merck, Lycera, AstraZeneca, and Molecular Partners.
SOURCE: Liu SV et al. WCLC 2018, Abstract PL02.07.
Invited discussant Natasha B. Leighl, MD, said that, while many questions remain, the IMpower133 findings do present a new standard of care for extensive-stage small cell lung cancer given the hazard ratio of 0.70 for survival, the unmet need in this population, and the 4 decades without progress.
“We have a long way to go to catch up with non–small cell lung cancer, and it starts today,” she said, noting, however, that uptake will vary depending on regulatory and economic thresholds in different areas. “I think that really highlights the urgent need for progress in patient selection, biomarker research, and the need to change our culture to one of tissue collection at trial.
“Finally, small cell lung cancer ... is a preventable disease and we need urgent steps in tobacco control to help us eradicate this killer,” she concluded.
Dr. Leighl is a medical oncologist at Princess Margaret Cancer Centre in Toronto. She has received research, grant, or other support from Novartis, AstraZeneca, Bristol-Myers Squibb, Merck, Pfizer, and the Canadian Agency for Drugs and Technologies in Health.
Invited discussant Natasha B. Leighl, MD, said that, while many questions remain, the IMpower133 findings do present a new standard of care for extensive-stage small cell lung cancer given the hazard ratio of 0.70 for survival, the unmet need in this population, and the 4 decades without progress.
“We have a long way to go to catch up with non–small cell lung cancer, and it starts today,” she said, noting, however, that uptake will vary depending on regulatory and economic thresholds in different areas. “I think that really highlights the urgent need for progress in patient selection, biomarker research, and the need to change our culture to one of tissue collection at trial.
“Finally, small cell lung cancer ... is a preventable disease and we need urgent steps in tobacco control to help us eradicate this killer,” she concluded.
Dr. Leighl is a medical oncologist at Princess Margaret Cancer Centre in Toronto. She has received research, grant, or other support from Novartis, AstraZeneca, Bristol-Myers Squibb, Merck, Pfizer, and the Canadian Agency for Drugs and Technologies in Health.
Invited discussant Natasha B. Leighl, MD, said that, while many questions remain, the IMpower133 findings do present a new standard of care for extensive-stage small cell lung cancer given the hazard ratio of 0.70 for survival, the unmet need in this population, and the 4 decades without progress.
“We have a long way to go to catch up with non–small cell lung cancer, and it starts today,” she said, noting, however, that uptake will vary depending on regulatory and economic thresholds in different areas. “I think that really highlights the urgent need for progress in patient selection, biomarker research, and the need to change our culture to one of tissue collection at trial.
“Finally, small cell lung cancer ... is a preventable disease and we need urgent steps in tobacco control to help us eradicate this killer,” she concluded.
Dr. Leighl is a medical oncologist at Princess Margaret Cancer Centre in Toronto. She has received research, grant, or other support from Novartis, AstraZeneca, Bristol-Myers Squibb, Merck, Pfizer, and the Canadian Agency for Drugs and Technologies in Health.
TORONTO – Adding the humanized monoclonal programmed death-ligand 1 (PD-L1) antibody atezolizumab to standard first-line treatment of extensive-stage small cell lung cancer (ES-SCLC) significantly improved overall and progression-free survival in the phase 1/3 IMpower133 trial.
The combination may represent a new standard-of-care regimen for patients with untreated ES-SCLC, which is highly lethal – with 5-year survival of about 1%-3% – and represents about 13% of all lung cancers, Stephen V. Liu, MD, reported at the World Conference on Lung Cancer.
The findings were published simultaneously in the New England Journal of Medicine.
The median overall survival in 201 patients randomized to receive atezolizumab in addition to carboplatin and etoposide was 12.3 months, compared with 10.3 months in 202 patients who received placebo plus carboplatin and etoposide (hazard ratio, 0.7), Dr. Liu of Georgetown University, Washington, and a member of the trial steering committee said at the meeting, sponsored by the International Association for the Study of Lung Cancer.
“That translates to a 30% reduction in the risk of patient death,” he said at a press briefing during the conference. “Patients receiving atezolizumab had a much greater likelihood of being alive at 1 year, with a 1-year survival rate of 51.7% versus 38.2%.”
Median progression-free survival(PFS) also improved with atezolizumab (5.2 months vs. 4.3 months with placebo; HR, 0.77), as did 6-month PFS. At 12 months there was more than a doubling of PFS in the atezolizumab group (5.0% vs. 12.6%), he said.
Participants in the double-blind trial were treatment-naive all-comers with measurable ES-SCLC and good performance status. They received four 21-day cycles of intravenous carboplatin (area under the curve, 5 mg/mL per minute) on day 1 plus intravenous etoposide (100 mg/m2) on days 1-3 with either concurrent 1,200 mg of atezolizumab on day 1 or placebo, followed by maintenance therapy with atezolizumab or placebo until intolerable toxicity or disease progression.
The treatment benefits were seen across many patient subgroups and regardless of tumor mutational burden.
The atezolizumab safety profile was as expected with no new safety signals and did not compromise patients’ ability to complete four treatment cycles, Dr. Liu noted.
The findings are exciting in that they represent the first in decades to show a significant improvement in survival in patients with ES-SCLC, he said. Although most patients have an initial response to standard-of-care chemotherapy, that response isn’t durable. “As much as we expect a response, we also know that it’s transient; we expect a response, we expect relapse. There hasn’t been a change really in the past 20 years, at least, with this regimen that we’ve been using since the 1980s.”
That’s not for lack of trying, he added, noting that more than 40 phase 3 studies have looked at more than 60 different drugs since the 1970s and have “failed to move the needle.”
Immunotherapy, however, has dramatically improved the therapeutic landscape in non–small cell lung cancer, and preclinical data and clinical experience suggest “a possible synergy between checkpoint inhibition and chemotherapy,” which led to this global study, he explained.
“This is the first study in over 20 years to show a significant improvement in survival and progression-free survival in initial treatment of small cell lung cancer. The concurrent administration of atezolizumab with chemotherapy helped people live longer, compared to chemotherapy alone,” Dr. Liu concluded, adding in a press statement that “this is an exciting time in oncology, and we are thrilled to finally see real progress in the SCLC space.”
When questioned about the role of PD-L1 in this population and the possibility of identifying a subgroup in which this treatment may be more cost effective, he noted that tissue samples weren’t required at enrollment in this study, but were collected from some patients, and future analyses will assess those samples to try to determine if there are subsets of patients who derive particular benefit from immunotherapy in this setting.
“But today, in an all-comer population, this combination has improved survival,” he said.
IMpower133 was sponsored by F. Hoffman–La Roche. Dr. Liu is a speaker or advisory board member for Genentech, Pfizer, Takeda, Celgene, Eli Lilly, Taiho Pharmaceutical, Bristol-Myers Squibb, AstraZeneca, and Ignyta, and has received research or grant support from Genentech, Pfizer, Threshold Pharmaceuticals, Clovis Oncology, Corvus Pharmaceuticals, Esanex, Bayer, OncoMed Pharmaceuticals, Ignyta, Merck, Lycera, AstraZeneca, and Molecular Partners.
SOURCE: Liu SV et al. WCLC 2018, Abstract PL02.07.
TORONTO – Adding the humanized monoclonal programmed death-ligand 1 (PD-L1) antibody atezolizumab to standard first-line treatment of extensive-stage small cell lung cancer (ES-SCLC) significantly improved overall and progression-free survival in the phase 1/3 IMpower133 trial.
The combination may represent a new standard-of-care regimen for patients with untreated ES-SCLC, which is highly lethal – with 5-year survival of about 1%-3% – and represents about 13% of all lung cancers, Stephen V. Liu, MD, reported at the World Conference on Lung Cancer.
The findings were published simultaneously in the New England Journal of Medicine.
The median overall survival in 201 patients randomized to receive atezolizumab in addition to carboplatin and etoposide was 12.3 months, compared with 10.3 months in 202 patients who received placebo plus carboplatin and etoposide (hazard ratio, 0.7), Dr. Liu of Georgetown University, Washington, and a member of the trial steering committee said at the meeting, sponsored by the International Association for the Study of Lung Cancer.
“That translates to a 30% reduction in the risk of patient death,” he said at a press briefing during the conference. “Patients receiving atezolizumab had a much greater likelihood of being alive at 1 year, with a 1-year survival rate of 51.7% versus 38.2%.”
Median progression-free survival(PFS) also improved with atezolizumab (5.2 months vs. 4.3 months with placebo; HR, 0.77), as did 6-month PFS. At 12 months there was more than a doubling of PFS in the atezolizumab group (5.0% vs. 12.6%), he said.
Participants in the double-blind trial were treatment-naive all-comers with measurable ES-SCLC and good performance status. They received four 21-day cycles of intravenous carboplatin (area under the curve, 5 mg/mL per minute) on day 1 plus intravenous etoposide (100 mg/m2) on days 1-3 with either concurrent 1,200 mg of atezolizumab on day 1 or placebo, followed by maintenance therapy with atezolizumab or placebo until intolerable toxicity or disease progression.
The treatment benefits were seen across many patient subgroups and regardless of tumor mutational burden.
The atezolizumab safety profile was as expected with no new safety signals and did not compromise patients’ ability to complete four treatment cycles, Dr. Liu noted.
The findings are exciting in that they represent the first in decades to show a significant improvement in survival in patients with ES-SCLC, he said. Although most patients have an initial response to standard-of-care chemotherapy, that response isn’t durable. “As much as we expect a response, we also know that it’s transient; we expect a response, we expect relapse. There hasn’t been a change really in the past 20 years, at least, with this regimen that we’ve been using since the 1980s.”
That’s not for lack of trying, he added, noting that more than 40 phase 3 studies have looked at more than 60 different drugs since the 1970s and have “failed to move the needle.”
Immunotherapy, however, has dramatically improved the therapeutic landscape in non–small cell lung cancer, and preclinical data and clinical experience suggest “a possible synergy between checkpoint inhibition and chemotherapy,” which led to this global study, he explained.
“This is the first study in over 20 years to show a significant improvement in survival and progression-free survival in initial treatment of small cell lung cancer. The concurrent administration of atezolizumab with chemotherapy helped people live longer, compared to chemotherapy alone,” Dr. Liu concluded, adding in a press statement that “this is an exciting time in oncology, and we are thrilled to finally see real progress in the SCLC space.”
When questioned about the role of PD-L1 in this population and the possibility of identifying a subgroup in which this treatment may be more cost effective, he noted that tissue samples weren’t required at enrollment in this study, but were collected from some patients, and future analyses will assess those samples to try to determine if there are subsets of patients who derive particular benefit from immunotherapy in this setting.
“But today, in an all-comer population, this combination has improved survival,” he said.
IMpower133 was sponsored by F. Hoffman–La Roche. Dr. Liu is a speaker or advisory board member for Genentech, Pfizer, Takeda, Celgene, Eli Lilly, Taiho Pharmaceutical, Bristol-Myers Squibb, AstraZeneca, and Ignyta, and has received research or grant support from Genentech, Pfizer, Threshold Pharmaceuticals, Clovis Oncology, Corvus Pharmaceuticals, Esanex, Bayer, OncoMed Pharmaceuticals, Ignyta, Merck, Lycera, AstraZeneca, and Molecular Partners.
SOURCE: Liu SV et al. WCLC 2018, Abstract PL02.07.
REPORTING FROM WCLC 2018
Key clinical point: Immunotherapy added to standard chemotherapy improves survival outcomes in extensive-stage small cell lung cancer.
Major finding: Median overall survival was 12.3 months with atezolizumab versus 10.3 months with placebo (HR, 0.7).
Study details: A global phase 1/3 study of 403 extensive-stage small cell lung cancer patients.
Disclosures: IMpower 133 was sponsored by F. Hoffman–La Roche. Dr. Liu is a speaker or advisory board member for Genentech, Pfizer, Takeda, Celgene, Eli Lilly, Taiho Pharmaceutical, Bristol-Myers Squibb, AstraZeneca, and Ignyta, and has received research or grant support from Genentech, Pfizer, Threshold Pharmaceuticals, Clovis Oncology, Corvus Pharmaceuticals, Esanex, Bayer, OncoMed Pharmaceuticals, Ignyta, Merck, Lycera, AstraZeneca, and Molecular Partners.
Source: Liu SV et al. WCLC 2018, Abstract PL02.07.
Checkpoint inhibitor linked to antiphospholipid syndrome in melanoma patient
A patient with melanoma experienced antiphospholipid syndrome following multiple infusions of the PD-1 inhibitor pembrolizumab, according to authors of a recent case report.
Presence of Raynaud phenomenon and high levels of antiphospholipid antibodies led to the diagnosis of antiphospholipid syndrome in the patient, who had stage IIIB unresectable melanoma.
This report provides additional evidence that this syndrome is an immune-related adverse event associated with checkpoint inhibitor therapy, said Alexandra Picard, MD, of Hôpital Archet, Nice, France, and coauthors.
“Due to the increased use of anti PD-1 therapies, clinicians should be aware of this new potential immune-mediated toxic effect that manifests as antiphospholipid syndrome,” the researchers wrote. The report is in JAMA Dermatology.
“Great caution” should be exercised when considering use of immune checkpoint inhibitors in patients with a history of antiphospholipid syndrome, the authors added.
The woman in this report was over 60 years of age and had first presented with superficial melanoma on her right calf, followed by recurrent lymph node metastases over the next few years, all of which were surgically treated.
Following a PET-CT scan showing a new metastatic lymph node, the woman started pembrolizumab 2 mg/kg every 3 weeks and had a partial response within 3 months, the investigators reported.
After the tenth infusion, however, the patient developed bilateral secondary Raynaud phenomenon that followed a typical discoloration sequence and resulted in a necrotic lesion at the tip of one finger.
The patient had no personal or family history of Raynaud phenomenon.
While beta2-glycoprotein 1 antibodies were not elevated, laboratory tests did show anticardiolipin antibodies and lupus anticoagulants at elevated levels, the investigators said, noting that repeat testing at 12 weeks confirmed positivity of antiphospholipid antibodies.
The Raynaud phenomenon disappeared and the necrotic lesion healed after pembrolizumab was stopped and prednisolone treatment was started, they added.
No recurrence of either was noted at the last follow-up.
Previous reports have described antiphospholipid syndrome in advanced melanoma patients treated with alfa-2b interferon alone or in combination with anti-interleukin 2, the authors said in their discussion of the case.
In addition, there has been another recent report of antiphospholipid syndrome associated with the CTLA4 inhibitor ipilimumab and the PD-1 inhibitor nivolumab, they said. In that case, testing for antiphospholipid antibodies revealed elevated beta2-glycoprotein 1 antibody levels.
“We hypothesize that [antiphospholipid syndrome] is a kind of autoimmunity induced by anti–PD-1 due to the expansive expression of the immune system against tumor cells,” the researchers wrote.
Although a case of cancer-associated antiphospholipid syndrome could not be ruled out in the present report, the rapid and complete resolution of symptoms after treatment discontinuation suggested that pembrolizumab, a “known immunostimulant,” was the cause, they said.
While antibodies against PD-1 have improved melanoma prognosis, they are associated with a wide range of immune-related adverse effects in the skin, gastrointestinal tract, liver, and endocrine system, Dr. Picard and coauthors noted.
They reported having no conflicts of interest.
SOURCE: Sanchez A, et al. JAMA Derm. 2018 Sep 19. doi: 10.1001/jamadermatol.2018.2770.
A patient with melanoma experienced antiphospholipid syndrome following multiple infusions of the PD-1 inhibitor pembrolizumab, according to authors of a recent case report.
Presence of Raynaud phenomenon and high levels of antiphospholipid antibodies led to the diagnosis of antiphospholipid syndrome in the patient, who had stage IIIB unresectable melanoma.
This report provides additional evidence that this syndrome is an immune-related adverse event associated with checkpoint inhibitor therapy, said Alexandra Picard, MD, of Hôpital Archet, Nice, France, and coauthors.
“Due to the increased use of anti PD-1 therapies, clinicians should be aware of this new potential immune-mediated toxic effect that manifests as antiphospholipid syndrome,” the researchers wrote. The report is in JAMA Dermatology.
“Great caution” should be exercised when considering use of immune checkpoint inhibitors in patients with a history of antiphospholipid syndrome, the authors added.
The woman in this report was over 60 years of age and had first presented with superficial melanoma on her right calf, followed by recurrent lymph node metastases over the next few years, all of which were surgically treated.
Following a PET-CT scan showing a new metastatic lymph node, the woman started pembrolizumab 2 mg/kg every 3 weeks and had a partial response within 3 months, the investigators reported.
After the tenth infusion, however, the patient developed bilateral secondary Raynaud phenomenon that followed a typical discoloration sequence and resulted in a necrotic lesion at the tip of one finger.
The patient had no personal or family history of Raynaud phenomenon.
While beta2-glycoprotein 1 antibodies were not elevated, laboratory tests did show anticardiolipin antibodies and lupus anticoagulants at elevated levels, the investigators said, noting that repeat testing at 12 weeks confirmed positivity of antiphospholipid antibodies.
The Raynaud phenomenon disappeared and the necrotic lesion healed after pembrolizumab was stopped and prednisolone treatment was started, they added.
No recurrence of either was noted at the last follow-up.
Previous reports have described antiphospholipid syndrome in advanced melanoma patients treated with alfa-2b interferon alone or in combination with anti-interleukin 2, the authors said in their discussion of the case.
In addition, there has been another recent report of antiphospholipid syndrome associated with the CTLA4 inhibitor ipilimumab and the PD-1 inhibitor nivolumab, they said. In that case, testing for antiphospholipid antibodies revealed elevated beta2-glycoprotein 1 antibody levels.
“We hypothesize that [antiphospholipid syndrome] is a kind of autoimmunity induced by anti–PD-1 due to the expansive expression of the immune system against tumor cells,” the researchers wrote.
Although a case of cancer-associated antiphospholipid syndrome could not be ruled out in the present report, the rapid and complete resolution of symptoms after treatment discontinuation suggested that pembrolizumab, a “known immunostimulant,” was the cause, they said.
While antibodies against PD-1 have improved melanoma prognosis, they are associated with a wide range of immune-related adverse effects in the skin, gastrointestinal tract, liver, and endocrine system, Dr. Picard and coauthors noted.
They reported having no conflicts of interest.
SOURCE: Sanchez A, et al. JAMA Derm. 2018 Sep 19. doi: 10.1001/jamadermatol.2018.2770.
A patient with melanoma experienced antiphospholipid syndrome following multiple infusions of the PD-1 inhibitor pembrolizumab, according to authors of a recent case report.
Presence of Raynaud phenomenon and high levels of antiphospholipid antibodies led to the diagnosis of antiphospholipid syndrome in the patient, who had stage IIIB unresectable melanoma.
This report provides additional evidence that this syndrome is an immune-related adverse event associated with checkpoint inhibitor therapy, said Alexandra Picard, MD, of Hôpital Archet, Nice, France, and coauthors.
“Due to the increased use of anti PD-1 therapies, clinicians should be aware of this new potential immune-mediated toxic effect that manifests as antiphospholipid syndrome,” the researchers wrote. The report is in JAMA Dermatology.
“Great caution” should be exercised when considering use of immune checkpoint inhibitors in patients with a history of antiphospholipid syndrome, the authors added.
The woman in this report was over 60 years of age and had first presented with superficial melanoma on her right calf, followed by recurrent lymph node metastases over the next few years, all of which were surgically treated.
Following a PET-CT scan showing a new metastatic lymph node, the woman started pembrolizumab 2 mg/kg every 3 weeks and had a partial response within 3 months, the investigators reported.
After the tenth infusion, however, the patient developed bilateral secondary Raynaud phenomenon that followed a typical discoloration sequence and resulted in a necrotic lesion at the tip of one finger.
The patient had no personal or family history of Raynaud phenomenon.
While beta2-glycoprotein 1 antibodies were not elevated, laboratory tests did show anticardiolipin antibodies and lupus anticoagulants at elevated levels, the investigators said, noting that repeat testing at 12 weeks confirmed positivity of antiphospholipid antibodies.
The Raynaud phenomenon disappeared and the necrotic lesion healed after pembrolizumab was stopped and prednisolone treatment was started, they added.
No recurrence of either was noted at the last follow-up.
Previous reports have described antiphospholipid syndrome in advanced melanoma patients treated with alfa-2b interferon alone or in combination with anti-interleukin 2, the authors said in their discussion of the case.
In addition, there has been another recent report of antiphospholipid syndrome associated with the CTLA4 inhibitor ipilimumab and the PD-1 inhibitor nivolumab, they said. In that case, testing for antiphospholipid antibodies revealed elevated beta2-glycoprotein 1 antibody levels.
“We hypothesize that [antiphospholipid syndrome] is a kind of autoimmunity induced by anti–PD-1 due to the expansive expression of the immune system against tumor cells,” the researchers wrote.
Although a case of cancer-associated antiphospholipid syndrome could not be ruled out in the present report, the rapid and complete resolution of symptoms after treatment discontinuation suggested that pembrolizumab, a “known immunostimulant,” was the cause, they said.
While antibodies against PD-1 have improved melanoma prognosis, they are associated with a wide range of immune-related adverse effects in the skin, gastrointestinal tract, liver, and endocrine system, Dr. Picard and coauthors noted.
They reported having no conflicts of interest.
SOURCE: Sanchez A, et al. JAMA Derm. 2018 Sep 19. doi: 10.1001/jamadermatol.2018.2770.
FROM JAMA DERMATOLOGY
Key clinical point: Antiphospholipid syndrome appears to be an immune-related adverse event associated with anti-PD-1 therapy.
Major finding: A melanoma patient receiving pembrolizumab was diagnosed with antiphospholipid syndrome that resolved following discontinuation of that treatment.
Study details: Case report of a woman in her 60s with stage IIIB unresectable melanoma who was treated with pembrolizumab 2 mg/kg every 3 weeks.
Disclosures: The authors reported no conflicts of interest.
Source: Sanchez A et al. JAMA Derm. 2018 Sep 19. doi: 10.1001/jamadermatol.2018.2770.
First reported case of induced resistance to tisagenlecleucel
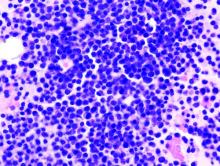
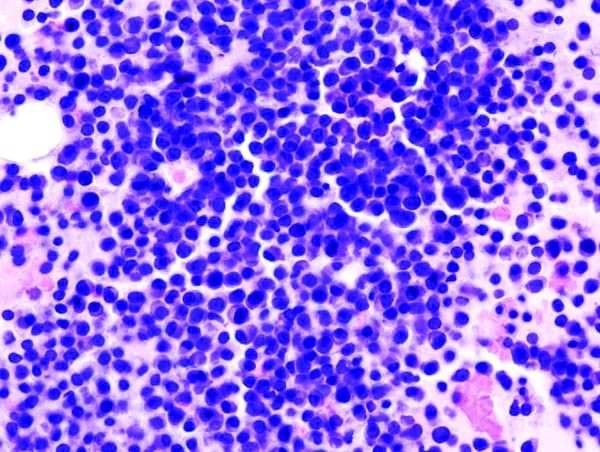
Unintentional transduction of a single leukemic B cell appears to have induced resistance to CTL019 (tisagenlecleucel, Kymriah) therapy, a recent case study suggests.
A total of 9 months after receiving a seemingly successful CD19-targeted chimeric antigen receptor (CAR) T-cell (CTL019; tisagenlecleucel) infusion, a 20-year-old man with B-cell acute lymphoblastic leukemia (B-ALL) had a frank relapse, with more than 90% bone marrow infiltration of CAR-transduced B-cell leukemia cells. Further investigation showed that the CAR gene had unintentionally been added to a solitary leukemic B cell during the CAR T-cell manufacturing process, reported Marco Ruella, MD, of the University of Pennsylvania, Philadelphia.
“The transduction of a single leukemic cell with an anti-CD19 CAR lentivirus during CTL019 manufacturing is sufficient to mediate resistance through masking of the CD19 epitope. This is a rare event, as this is the only case out of 369 patients reported worldwide at the time of publication. ... These findings illustrate the need for improved manufacturing technologies that can purge residual contaminating tumor cells from engineered T cells,” the authors wrote in Nature Medicine.
The findings also confirm the cancer stem cell hypothesis in humans, “given that clonal analysis indicated that the relapse and subsequent death of the patient were attributed to the progeny of a single leukemic blast cell with extensive replicative capacity, both in culture and in vivo,” they wrote.
Initially, “the infused CTL019 cells displayed the typical pattern of in vivo engraftment and expansion by CAR19-specific flow cytometry, followed by decline to an undetectable level in the peripheral blood” of the affected patient, the authors wrote. “The expansion and contraction phases and long-term persistence of CAR T cells were confirmed via qPCR using CAR-specific primers.” The patient was in complete remission at day 28.
However, they added, routine peripheral blood monitoring with quantitative polymerase chain reaction for CAR-specific sequences identified “the emergence of a second expansion phase of CAR cells starting at day 252, which did not correlate with re-expansion of CAR + T cells by flow cytometry.” Frank relapse soon followed.
Analysis confirmed “that the lack of detection of CD19 by flow cytometry was due to CAR19 binding in cis to CD19 on the surface of leukemic blasts, thus masking the epitope from detection by standard flow cytometry,” the authors wrote.
Study funding was provided by Bristol-Myers Squibb, Novartis, the National Institutes of Health, and others. Dr. Ruella and several of his colleagues work under a research collaboration involving the University of Pennsylvania and the Novartis Institutes of Biomedical Research and are inventors of intellectual property licensed by the University of Pennsylvania to Novartis.
SOURCE: Ruella M et al. Nat Med. 2018 Oct 1. doi: 10.1038/s41591-018-0201-9.
Unintentional transduction of a single leukemic B cell appears to have induced resistance to CTL019 (tisagenlecleucel, Kymriah) therapy, a recent case study suggests.
A total of 9 months after receiving a seemingly successful CD19-targeted chimeric antigen receptor (CAR) T-cell (CTL019; tisagenlecleucel) infusion, a 20-year-old man with B-cell acute lymphoblastic leukemia (B-ALL) had a frank relapse, with more than 90% bone marrow infiltration of CAR-transduced B-cell leukemia cells. Further investigation showed that the CAR gene had unintentionally been added to a solitary leukemic B cell during the CAR T-cell manufacturing process, reported Marco Ruella, MD, of the University of Pennsylvania, Philadelphia.
“The transduction of a single leukemic cell with an anti-CD19 CAR lentivirus during CTL019 manufacturing is sufficient to mediate resistance through masking of the CD19 epitope. This is a rare event, as this is the only case out of 369 patients reported worldwide at the time of publication. ... These findings illustrate the need for improved manufacturing technologies that can purge residual contaminating tumor cells from engineered T cells,” the authors wrote in Nature Medicine.
The findings also confirm the cancer stem cell hypothesis in humans, “given that clonal analysis indicated that the relapse and subsequent death of the patient were attributed to the progeny of a single leukemic blast cell with extensive replicative capacity, both in culture and in vivo,” they wrote.
Initially, “the infused CTL019 cells displayed the typical pattern of in vivo engraftment and expansion by CAR19-specific flow cytometry, followed by decline to an undetectable level in the peripheral blood” of the affected patient, the authors wrote. “The expansion and contraction phases and long-term persistence of CAR T cells were confirmed via qPCR using CAR-specific primers.” The patient was in complete remission at day 28.
However, they added, routine peripheral blood monitoring with quantitative polymerase chain reaction for CAR-specific sequences identified “the emergence of a second expansion phase of CAR cells starting at day 252, which did not correlate with re-expansion of CAR + T cells by flow cytometry.” Frank relapse soon followed.
Analysis confirmed “that the lack of detection of CD19 by flow cytometry was due to CAR19 binding in cis to CD19 on the surface of leukemic blasts, thus masking the epitope from detection by standard flow cytometry,” the authors wrote.
Study funding was provided by Bristol-Myers Squibb, Novartis, the National Institutes of Health, and others. Dr. Ruella and several of his colleagues work under a research collaboration involving the University of Pennsylvania and the Novartis Institutes of Biomedical Research and are inventors of intellectual property licensed by the University of Pennsylvania to Novartis.
SOURCE: Ruella M et al. Nat Med. 2018 Oct 1. doi: 10.1038/s41591-018-0201-9.
Unintentional transduction of a single leukemic B cell appears to have induced resistance to CTL019 (tisagenlecleucel, Kymriah) therapy, a recent case study suggests.
A total of 9 months after receiving a seemingly successful CD19-targeted chimeric antigen receptor (CAR) T-cell (CTL019; tisagenlecleucel) infusion, a 20-year-old man with B-cell acute lymphoblastic leukemia (B-ALL) had a frank relapse, with more than 90% bone marrow infiltration of CAR-transduced B-cell leukemia cells. Further investigation showed that the CAR gene had unintentionally been added to a solitary leukemic B cell during the CAR T-cell manufacturing process, reported Marco Ruella, MD, of the University of Pennsylvania, Philadelphia.
“The transduction of a single leukemic cell with an anti-CD19 CAR lentivirus during CTL019 manufacturing is sufficient to mediate resistance through masking of the CD19 epitope. This is a rare event, as this is the only case out of 369 patients reported worldwide at the time of publication. ... These findings illustrate the need for improved manufacturing technologies that can purge residual contaminating tumor cells from engineered T cells,” the authors wrote in Nature Medicine.
The findings also confirm the cancer stem cell hypothesis in humans, “given that clonal analysis indicated that the relapse and subsequent death of the patient were attributed to the progeny of a single leukemic blast cell with extensive replicative capacity, both in culture and in vivo,” they wrote.
Initially, “the infused CTL019 cells displayed the typical pattern of in vivo engraftment and expansion by CAR19-specific flow cytometry, followed by decline to an undetectable level in the peripheral blood” of the affected patient, the authors wrote. “The expansion and contraction phases and long-term persistence of CAR T cells were confirmed via qPCR using CAR-specific primers.” The patient was in complete remission at day 28.
However, they added, routine peripheral blood monitoring with quantitative polymerase chain reaction for CAR-specific sequences identified “the emergence of a second expansion phase of CAR cells starting at day 252, which did not correlate with re-expansion of CAR + T cells by flow cytometry.” Frank relapse soon followed.
Analysis confirmed “that the lack of detection of CD19 by flow cytometry was due to CAR19 binding in cis to CD19 on the surface of leukemic blasts, thus masking the epitope from detection by standard flow cytometry,” the authors wrote.
Study funding was provided by Bristol-Myers Squibb, Novartis, the National Institutes of Health, and others. Dr. Ruella and several of his colleagues work under a research collaboration involving the University of Pennsylvania and the Novartis Institutes of Biomedical Research and are inventors of intellectual property licensed by the University of Pennsylvania to Novartis.
SOURCE: Ruella M et al. Nat Med. 2018 Oct 1. doi: 10.1038/s41591-018-0201-9.
FROM NATURE MEDICINE
Key clinical point: Unintentional transduction of a single leukemic B cell induced resistance to CTL019 (tisagenlecleucel) therapy.
Major finding: A patient with B-cell acute lymphoblastic leukemia (B-ALL) had frank relapse 9 months after a CTL019 infusion, with more than 90% bone marrow infiltration of chimeric antigen receptor–transduced B-cell leukemia cells.
Study details: A case study of a 20-year-old male with B-ALL undergoing CTL019 therapy.
Disclosures: Study funding was provided by Bristol-Myers Squibb, Novartis, the National Institutes of Health, and others. Dr. Ruella and several of his colleagues work under a research collaboration involving the University of Pennsylvania and the Novartis Institutes of Biomedical Research and are inventors of intellectual property licensed by the University of Pennsylvania to Novartis.
Source: Ruella M et al. Nat Med. 2018 Oct 1. doi: 10.1038/s41591-018-0201-9.
Researchers share Nobel Prize for cancer immunotherapy discoveries
Two researchers who made groundbreaking discoveries leading to the development of immune checkpoint therapy have jointly received the 2018 Nobel Prize in Physiology or Medicine.
James P. Allison, PhD, and Tasuku Honjo, MD, PhD, share the prize for their work in showing how strategies for “inhibiting the brakes” on T cells can be used in the treatment of cancer, the Nobel Assembly at Karolinska Institutet, Stockholm, said in a news release.
The discoveries of Dr. Allison and Dr. Honjo represent a landmark in the fight against cancer, according to the Nobel Assembly.
“This new form of immunotherapy unleashes a vigorous, and often durable, immune response directed against essentially any tumor already recognized by the immune system,” members of the Nobel Committee and Assembly said in a simultaneously published manuscript explaining the scientific background behind the discovery.
The “unprecedented” research activity in the immune checkpoint field demonstrates how influential the discoveries of Dr. Allison and Dr. Honjo have been, molecular genetics professor C. I. Edvard Smith, MD, PhD, and coauthors said in the manuscript.
Their findings have “conferred great benefit on mankind” and add a “new pillar” to existing cancer treatments, Dr. Smith and coauthors said in their report.
Dr. Allison was one of several scientists to observe that the cytotoxic T-lymphocyte antigen 4 (CTLA4) protein functions as a brake on T cells, the Nobel Assembly said in the press release. He developed an antibody that could bind to CTLA4 and block its function, and demonstrated its activity in experiments taking place near the end of 1994.
The “spectacular” results showed that, in mice, the antibodies could inhibit the brake and unlock antitumor T-cell activity, according to the release.
Studies of CTLA-4 blockade in humans from several research groups yielded promising results, and in 2010, a major breakthrough came, according to the Nobel Assembly, when it was reported that the CTLA4 blocker ipilimumab improved survival in patients with metastatic melanoma.
Dr. Honjo discovered the programmed cell death protein (PD-1) in 1992, a few years before Dr. Allison’s discovery, and explored its function in experiments carried out over many years at his laboratory at Kyoto University.
Dr. Honjo’s experiments showed that PD-1 functioned as a T-cell brake, but by a different mechanism than CTLA4, paving the way for studying PD-1 as a target of cancer treatment.
That led to a considerable amount of clinical development, including a key 2012 study showing that patients treated with the anti-PD-1 antibody nivolumab led to long-term remissions and possible cures in some patients, the assembly said in their press release.
Scientists have attempted to harness the immune system in the fight against cancer for more than 100 years, according to the assembly. “Until the seminal discoveries by the two laureates, progress into clinical development was modest. Checkpoint therapy has now revolutionized cancer treatment and has fundamentally changed the way we view how cancer can be managed.”
Two researchers who made groundbreaking discoveries leading to the development of immune checkpoint therapy have jointly received the 2018 Nobel Prize in Physiology or Medicine.
James P. Allison, PhD, and Tasuku Honjo, MD, PhD, share the prize for their work in showing how strategies for “inhibiting the brakes” on T cells can be used in the treatment of cancer, the Nobel Assembly at Karolinska Institutet, Stockholm, said in a news release.
The discoveries of Dr. Allison and Dr. Honjo represent a landmark in the fight against cancer, according to the Nobel Assembly.
“This new form of immunotherapy unleashes a vigorous, and often durable, immune response directed against essentially any tumor already recognized by the immune system,” members of the Nobel Committee and Assembly said in a simultaneously published manuscript explaining the scientific background behind the discovery.
The “unprecedented” research activity in the immune checkpoint field demonstrates how influential the discoveries of Dr. Allison and Dr. Honjo have been, molecular genetics professor C. I. Edvard Smith, MD, PhD, and coauthors said in the manuscript.
Their findings have “conferred great benefit on mankind” and add a “new pillar” to existing cancer treatments, Dr. Smith and coauthors said in their report.
Dr. Allison was one of several scientists to observe that the cytotoxic T-lymphocyte antigen 4 (CTLA4) protein functions as a brake on T cells, the Nobel Assembly said in the press release. He developed an antibody that could bind to CTLA4 and block its function, and demonstrated its activity in experiments taking place near the end of 1994.
The “spectacular” results showed that, in mice, the antibodies could inhibit the brake and unlock antitumor T-cell activity, according to the release.
Studies of CTLA-4 blockade in humans from several research groups yielded promising results, and in 2010, a major breakthrough came, according to the Nobel Assembly, when it was reported that the CTLA4 blocker ipilimumab improved survival in patients with metastatic melanoma.
Dr. Honjo discovered the programmed cell death protein (PD-1) in 1992, a few years before Dr. Allison’s discovery, and explored its function in experiments carried out over many years at his laboratory at Kyoto University.
Dr. Honjo’s experiments showed that PD-1 functioned as a T-cell brake, but by a different mechanism than CTLA4, paving the way for studying PD-1 as a target of cancer treatment.
That led to a considerable amount of clinical development, including a key 2012 study showing that patients treated with the anti-PD-1 antibody nivolumab led to long-term remissions and possible cures in some patients, the assembly said in their press release.
Scientists have attempted to harness the immune system in the fight against cancer for more than 100 years, according to the assembly. “Until the seminal discoveries by the two laureates, progress into clinical development was modest. Checkpoint therapy has now revolutionized cancer treatment and has fundamentally changed the way we view how cancer can be managed.”
Two researchers who made groundbreaking discoveries leading to the development of immune checkpoint therapy have jointly received the 2018 Nobel Prize in Physiology or Medicine.
James P. Allison, PhD, and Tasuku Honjo, MD, PhD, share the prize for their work in showing how strategies for “inhibiting the brakes” on T cells can be used in the treatment of cancer, the Nobel Assembly at Karolinska Institutet, Stockholm, said in a news release.
The discoveries of Dr. Allison and Dr. Honjo represent a landmark in the fight against cancer, according to the Nobel Assembly.
“This new form of immunotherapy unleashes a vigorous, and often durable, immune response directed against essentially any tumor already recognized by the immune system,” members of the Nobel Committee and Assembly said in a simultaneously published manuscript explaining the scientific background behind the discovery.
The “unprecedented” research activity in the immune checkpoint field demonstrates how influential the discoveries of Dr. Allison and Dr. Honjo have been, molecular genetics professor C. I. Edvard Smith, MD, PhD, and coauthors said in the manuscript.
Their findings have “conferred great benefit on mankind” and add a “new pillar” to existing cancer treatments, Dr. Smith and coauthors said in their report.
Dr. Allison was one of several scientists to observe that the cytotoxic T-lymphocyte antigen 4 (CTLA4) protein functions as a brake on T cells, the Nobel Assembly said in the press release. He developed an antibody that could bind to CTLA4 and block its function, and demonstrated its activity in experiments taking place near the end of 1994.
The “spectacular” results showed that, in mice, the antibodies could inhibit the brake and unlock antitumor T-cell activity, according to the release.
Studies of CTLA-4 blockade in humans from several research groups yielded promising results, and in 2010, a major breakthrough came, according to the Nobel Assembly, when it was reported that the CTLA4 blocker ipilimumab improved survival in patients with metastatic melanoma.
Dr. Honjo discovered the programmed cell death protein (PD-1) in 1992, a few years before Dr. Allison’s discovery, and explored its function in experiments carried out over many years at his laboratory at Kyoto University.
Dr. Honjo’s experiments showed that PD-1 functioned as a T-cell brake, but by a different mechanism than CTLA4, paving the way for studying PD-1 as a target of cancer treatment.
That led to a considerable amount of clinical development, including a key 2012 study showing that patients treated with the anti-PD-1 antibody nivolumab led to long-term remissions and possible cures in some patients, the assembly said in their press release.
Scientists have attempted to harness the immune system in the fight against cancer for more than 100 years, according to the assembly. “Until the seminal discoveries by the two laureates, progress into clinical development was modest. Checkpoint therapy has now revolutionized cancer treatment and has fundamentally changed the way we view how cancer can be managed.”
Endogenous retroviruses may unlock new immunotherapy targets
Future epigenetic drugs could activate human endogenous retroviruses (HERVs) in cancer cells to enable immunotherapy, investigators suggest.
Activated HERVs may sensitize cancer cells or serve as novel tumor-associated antigenic targets, reported Anders Steenholdt Attermann, PhD, of the department of micro- and nanotechnology at the Technical University of Denmark in Kongens Lyngby, and colleagues.
A remarkable 8% of the human genome is composed of HERVs.
“They are remnants of retroviral germline infections that resulted in chromosomal integration into all the cells of the progeny, but their viral replication is defective in the present-day human genome,” the authors wrote in Annals of Oncology.
The therapeutic potential for these remnants is complex, as is their relationship with the immune system and neoplasia. Studies dating back to 2002 have found unique associations between HERVs and various types of cancer, including renal cell carcinoma, melanoma, gastrointestinal cancer, colorectal cancer, and breast cancer.
“Early data point towards distinct features for the expression profiles of different HERVs,” the authors wrote, “but these characteristics remain to be fully elucidated. There may be substantial differences in their biological effects, potential roles in immune sensitization, and ability to form an antigen reservoir.”
HERVs may be activated by cancer or epigenetic drugs. While certain cancers may activate particular HERVs into targetable antigens, other cancer-activated HERVs actually shield tumors from the immune system. Still other HERVs require epigenetic drugs for activation, such as DNA methyltransferase inhibitors. These drugs could transform HERVs into “intrinsic adjuvants” or novel antigens; either of which may improve the efficacy of existing immunotherapies like checkpoint inhibitors.
To leverage HERVs for immunotherapy, a better understanding of immune tolerance is needed. Some research suggests that since HERVs share similarities with exogenous viruses, tolerance to HERVs must be incomplete to allow for immune responses to exogenous viruses. In contrast, incomplete tolerance would conceivably lead to autoimmune disease.
“Hence, peripheral tolerance and ignorance mechanisms may play prominent roles in the control of HERV-specific T-cell recognition in healthy individuals,” the authors wrote. “Understanding the differences in HERV expression in the thymus and peripheral tissues would be of great importance for the use of HERVs as immunotherapeutic targets.”
When more clearly understood, HERVs may feature in emerging combination therapies.
“The combination of epigenetic drugs and immunotherapy is exciting for future cancer therapy,” the authors wrote, “especially for cancer types with low mutational burden that respond poorly to immunotherapy or cancer types with poor responses to immune checkpoint inhibitor treatment.”
It appears that the authors’ excitement is shared – almost 50 clinical trials are currently studying epigenetic drug/immunotherapy combinations.
Study funding was provided by the Lundbeck Foundation Fellowship, the European Research Council, the stand-up-to-cancer (SU2C) epigenetic dream team, and StG 677268 NextDART.
SOURCE: Attermann et al. Ann Oncol. 2018 Sep 18. doi: 10.1093/annonc/mdy413.
Future epigenetic drugs could activate human endogenous retroviruses (HERVs) in cancer cells to enable immunotherapy, investigators suggest.
Activated HERVs may sensitize cancer cells or serve as novel tumor-associated antigenic targets, reported Anders Steenholdt Attermann, PhD, of the department of micro- and nanotechnology at the Technical University of Denmark in Kongens Lyngby, and colleagues.
A remarkable 8% of the human genome is composed of HERVs.
“They are remnants of retroviral germline infections that resulted in chromosomal integration into all the cells of the progeny, but their viral replication is defective in the present-day human genome,” the authors wrote in Annals of Oncology.
The therapeutic potential for these remnants is complex, as is their relationship with the immune system and neoplasia. Studies dating back to 2002 have found unique associations between HERVs and various types of cancer, including renal cell carcinoma, melanoma, gastrointestinal cancer, colorectal cancer, and breast cancer.
“Early data point towards distinct features for the expression profiles of different HERVs,” the authors wrote, “but these characteristics remain to be fully elucidated. There may be substantial differences in their biological effects, potential roles in immune sensitization, and ability to form an antigen reservoir.”
HERVs may be activated by cancer or epigenetic drugs. While certain cancers may activate particular HERVs into targetable antigens, other cancer-activated HERVs actually shield tumors from the immune system. Still other HERVs require epigenetic drugs for activation, such as DNA methyltransferase inhibitors. These drugs could transform HERVs into “intrinsic adjuvants” or novel antigens; either of which may improve the efficacy of existing immunotherapies like checkpoint inhibitors.
To leverage HERVs for immunotherapy, a better understanding of immune tolerance is needed. Some research suggests that since HERVs share similarities with exogenous viruses, tolerance to HERVs must be incomplete to allow for immune responses to exogenous viruses. In contrast, incomplete tolerance would conceivably lead to autoimmune disease.
“Hence, peripheral tolerance and ignorance mechanisms may play prominent roles in the control of HERV-specific T-cell recognition in healthy individuals,” the authors wrote. “Understanding the differences in HERV expression in the thymus and peripheral tissues would be of great importance for the use of HERVs as immunotherapeutic targets.”
When more clearly understood, HERVs may feature in emerging combination therapies.
“The combination of epigenetic drugs and immunotherapy is exciting for future cancer therapy,” the authors wrote, “especially for cancer types with low mutational burden that respond poorly to immunotherapy or cancer types with poor responses to immune checkpoint inhibitor treatment.”
It appears that the authors’ excitement is shared – almost 50 clinical trials are currently studying epigenetic drug/immunotherapy combinations.
Study funding was provided by the Lundbeck Foundation Fellowship, the European Research Council, the stand-up-to-cancer (SU2C) epigenetic dream team, and StG 677268 NextDART.
SOURCE: Attermann et al. Ann Oncol. 2018 Sep 18. doi: 10.1093/annonc/mdy413.
Future epigenetic drugs could activate human endogenous retroviruses (HERVs) in cancer cells to enable immunotherapy, investigators suggest.
Activated HERVs may sensitize cancer cells or serve as novel tumor-associated antigenic targets, reported Anders Steenholdt Attermann, PhD, of the department of micro- and nanotechnology at the Technical University of Denmark in Kongens Lyngby, and colleagues.
A remarkable 8% of the human genome is composed of HERVs.
“They are remnants of retroviral germline infections that resulted in chromosomal integration into all the cells of the progeny, but their viral replication is defective in the present-day human genome,” the authors wrote in Annals of Oncology.
The therapeutic potential for these remnants is complex, as is their relationship with the immune system and neoplasia. Studies dating back to 2002 have found unique associations between HERVs and various types of cancer, including renal cell carcinoma, melanoma, gastrointestinal cancer, colorectal cancer, and breast cancer.
“Early data point towards distinct features for the expression profiles of different HERVs,” the authors wrote, “but these characteristics remain to be fully elucidated. There may be substantial differences in their biological effects, potential roles in immune sensitization, and ability to form an antigen reservoir.”
HERVs may be activated by cancer or epigenetic drugs. While certain cancers may activate particular HERVs into targetable antigens, other cancer-activated HERVs actually shield tumors from the immune system. Still other HERVs require epigenetic drugs for activation, such as DNA methyltransferase inhibitors. These drugs could transform HERVs into “intrinsic adjuvants” or novel antigens; either of which may improve the efficacy of existing immunotherapies like checkpoint inhibitors.
To leverage HERVs for immunotherapy, a better understanding of immune tolerance is needed. Some research suggests that since HERVs share similarities with exogenous viruses, tolerance to HERVs must be incomplete to allow for immune responses to exogenous viruses. In contrast, incomplete tolerance would conceivably lead to autoimmune disease.
“Hence, peripheral tolerance and ignorance mechanisms may play prominent roles in the control of HERV-specific T-cell recognition in healthy individuals,” the authors wrote. “Understanding the differences in HERV expression in the thymus and peripheral tissues would be of great importance for the use of HERVs as immunotherapeutic targets.”
When more clearly understood, HERVs may feature in emerging combination therapies.
“The combination of epigenetic drugs and immunotherapy is exciting for future cancer therapy,” the authors wrote, “especially for cancer types with low mutational burden that respond poorly to immunotherapy or cancer types with poor responses to immune checkpoint inhibitor treatment.”
It appears that the authors’ excitement is shared – almost 50 clinical trials are currently studying epigenetic drug/immunotherapy combinations.
Study funding was provided by the Lundbeck Foundation Fellowship, the European Research Council, the stand-up-to-cancer (SU2C) epigenetic dream team, and StG 677268 NextDART.
SOURCE: Attermann et al. Ann Oncol. 2018 Sep 18. doi: 10.1093/annonc/mdy413.
FROM ANNALS OF ONCOLOGY
Key clinical point: Future epigenetic drugs may activate human endogenous retroviruses (HERVs) in cancer cells to enable immunotherapeutic targeting.
Major finding: Almost 50 clinical trials are currently investigating combinations of immunotherapies and epigenetic drugs.
Study details: A review article covering HERVs and their relationship with epigenetic drugs and immunotherapy.
Disclosures: Study funding was provided by the Lundbeck Foundation Fellowship, the European Research Council, the stand-up-to-cancer (SU2C) epigenetic dream team, and StG 677268 NextDART. No conflicts of interest were reported.
Source: Attermann et al. Ann Oncol. 2018 Sep 18. doi: 10.1093/annonc/mdy413.
PACIFIC trial: Durvalumab improves both OS and PFS in stage III NSCLC
TORONTO – The programmed death-ligand 1 (PD-L1) inhibitor durvalumab significantly improves overall survival in patients with stage III unresectable non–small-cell lung cancer without progression after chemoradiotherapy, according to updated results from the global phase 3 PACIFIC study.
The findings, presented at the World Conference on Lung Cancer, follow a prior report from the study showing improved progression-free survival (PFS) in durvalumab-treated patients (stratified hazard ratio, 0.52), and together these survival benefits mark the first major advance in this disease setting in decades,” Scott J. Antonia, MD, reported at the conference, sponsored by the International Association for the Study of Lung Cancer (IASLC).
“The fact is this is a new standard of care treatment for the patients with this disease,” he said, adding that “in all likelihood we are improving the cure rate for the patients with this disease.”
The findings were published simultaneously in the New England Journal of Medicine.
Overall survival at a median follow-up of 25.2 months in 473 patients randomized to receive durvalumab was significantly greater than among 236 who received placebo (stratified HR, 0.68; median survival not reached vs. 28.7 months in the groups, respectively), said Dr. Antonia of the H. Lee Moffitt Cancer Center and Research Institute, and professor of oncologic sciences at the University of South Florida, Tampa.
Durvalumab also improved overall survival in all prespecified subgroups, and PFS was similar to that in previous reports (stratified HR 0.51; median of 17.2 vs. 5.6 months with durvalumab and placebo, respectively), he said, noting that “interestingly, patients who were nonsmokers did benefit from durvalumab.”
This is notable because prior research suggests that never-smokers with advanced stage cancer have less of a chance of responding to immunotherapy (although they should still be offered immunotherapy), he explained.
“Also interestingly, it appears as if cisplatin was the better drug to use in the conventional therapy portion of the treatment,” he said.
Durvalumab also provided continued improvement vs. placebo in time to death or distant metastasis (stratified HR, 0.53), time to second progression (stratified HR, 0.58), time to first subsequent therapy or death (stratified HR, 0.58), and time to second subsequent therapy or death (stratified HR, 0.63).
Study subjects were patients with World Health Organization Performance Status scores of 0 or 1 with any PD-L1 tumor status, who received at least two cycles of conventional standard-of-care platinum-based chemoradiotherapy (CRT). They were randomized between May 2014 and April 2016 – at 1-42 days after CRT – to receive intravenous durvalumab at a dose of 10 mg/kg given intravenously every 2 weeks or placebo, and were stratified by age, gender, and smoking history.
Durvalumab was well tolerated; 30.5% and 26.1% of treatment and placebo patients, respectively, had grade 3/4 adverse events, and 15.4% and 9.8%, respectively, discontinued because of adverse events.
“There were no new safety signals with this longer follow-up,” Dr. Antonia said.
After study treatment ended, 41% and 54% in the groups, respectively, received additional anticancer therapy, and 8% and 22.4%, respectively, received additional immunotherapy, he noted.
The results are not only statistically significant, but clinically meaningful, and they offer new hope for patients with a disease that, in those who receive chemoradiotherapy, has a 3-year survival rate of only about 27%, he said.
During a press briefing at the conference, moderator Frances Shepherd, MD, a medical oncologist at Princess Margaret Cancer Centre in Toronto and a past president of the International Association for the Study of Lung Cancer, called the results “very exciting” given that this type of cancer represents about a third of all lung cancers and therefore affects an “enormous number of patients in Canada and globally.”
The PACIFIC trial was sponsored by AstraZeneca. Dr. Antonia reported being a speaker or advisory board member or receiving funding support from AstraZeneca and numerous other companies. Dr. Shepherd reported receiving honoraria and support from AstraZeneca and others. She is a speaker or advisory board member for Eli Lilly, AstraZeneca, and Merck, and she has ownership Interest in Eli Lilly and AstraZeneca.
SOURCE: Antonia S et al., WCLC 2018 Abstract PL02.01.
TORONTO – The programmed death-ligand 1 (PD-L1) inhibitor durvalumab significantly improves overall survival in patients with stage III unresectable non–small-cell lung cancer without progression after chemoradiotherapy, according to updated results from the global phase 3 PACIFIC study.
The findings, presented at the World Conference on Lung Cancer, follow a prior report from the study showing improved progression-free survival (PFS) in durvalumab-treated patients (stratified hazard ratio, 0.52), and together these survival benefits mark the first major advance in this disease setting in decades,” Scott J. Antonia, MD, reported at the conference, sponsored by the International Association for the Study of Lung Cancer (IASLC).
“The fact is this is a new standard of care treatment for the patients with this disease,” he said, adding that “in all likelihood we are improving the cure rate for the patients with this disease.”
The findings were published simultaneously in the New England Journal of Medicine.
Overall survival at a median follow-up of 25.2 months in 473 patients randomized to receive durvalumab was significantly greater than among 236 who received placebo (stratified HR, 0.68; median survival not reached vs. 28.7 months in the groups, respectively), said Dr. Antonia of the H. Lee Moffitt Cancer Center and Research Institute, and professor of oncologic sciences at the University of South Florida, Tampa.
Durvalumab also improved overall survival in all prespecified subgroups, and PFS was similar to that in previous reports (stratified HR 0.51; median of 17.2 vs. 5.6 months with durvalumab and placebo, respectively), he said, noting that “interestingly, patients who were nonsmokers did benefit from durvalumab.”
This is notable because prior research suggests that never-smokers with advanced stage cancer have less of a chance of responding to immunotherapy (although they should still be offered immunotherapy), he explained.
“Also interestingly, it appears as if cisplatin was the better drug to use in the conventional therapy portion of the treatment,” he said.
Durvalumab also provided continued improvement vs. placebo in time to death or distant metastasis (stratified HR, 0.53), time to second progression (stratified HR, 0.58), time to first subsequent therapy or death (stratified HR, 0.58), and time to second subsequent therapy or death (stratified HR, 0.63).
Study subjects were patients with World Health Organization Performance Status scores of 0 or 1 with any PD-L1 tumor status, who received at least two cycles of conventional standard-of-care platinum-based chemoradiotherapy (CRT). They were randomized between May 2014 and April 2016 – at 1-42 days after CRT – to receive intravenous durvalumab at a dose of 10 mg/kg given intravenously every 2 weeks or placebo, and were stratified by age, gender, and smoking history.
Durvalumab was well tolerated; 30.5% and 26.1% of treatment and placebo patients, respectively, had grade 3/4 adverse events, and 15.4% and 9.8%, respectively, discontinued because of adverse events.
“There were no new safety signals with this longer follow-up,” Dr. Antonia said.
After study treatment ended, 41% and 54% in the groups, respectively, received additional anticancer therapy, and 8% and 22.4%, respectively, received additional immunotherapy, he noted.
The results are not only statistically significant, but clinically meaningful, and they offer new hope for patients with a disease that, in those who receive chemoradiotherapy, has a 3-year survival rate of only about 27%, he said.
During a press briefing at the conference, moderator Frances Shepherd, MD, a medical oncologist at Princess Margaret Cancer Centre in Toronto and a past president of the International Association for the Study of Lung Cancer, called the results “very exciting” given that this type of cancer represents about a third of all lung cancers and therefore affects an “enormous number of patients in Canada and globally.”
The PACIFIC trial was sponsored by AstraZeneca. Dr. Antonia reported being a speaker or advisory board member or receiving funding support from AstraZeneca and numerous other companies. Dr. Shepherd reported receiving honoraria and support from AstraZeneca and others. She is a speaker or advisory board member for Eli Lilly, AstraZeneca, and Merck, and she has ownership Interest in Eli Lilly and AstraZeneca.
SOURCE: Antonia S et al., WCLC 2018 Abstract PL02.01.
TORONTO – The programmed death-ligand 1 (PD-L1) inhibitor durvalumab significantly improves overall survival in patients with stage III unresectable non–small-cell lung cancer without progression after chemoradiotherapy, according to updated results from the global phase 3 PACIFIC study.
The findings, presented at the World Conference on Lung Cancer, follow a prior report from the study showing improved progression-free survival (PFS) in durvalumab-treated patients (stratified hazard ratio, 0.52), and together these survival benefits mark the first major advance in this disease setting in decades,” Scott J. Antonia, MD, reported at the conference, sponsored by the International Association for the Study of Lung Cancer (IASLC).
“The fact is this is a new standard of care treatment for the patients with this disease,” he said, adding that “in all likelihood we are improving the cure rate for the patients with this disease.”
The findings were published simultaneously in the New England Journal of Medicine.
Overall survival at a median follow-up of 25.2 months in 473 patients randomized to receive durvalumab was significantly greater than among 236 who received placebo (stratified HR, 0.68; median survival not reached vs. 28.7 months in the groups, respectively), said Dr. Antonia of the H. Lee Moffitt Cancer Center and Research Institute, and professor of oncologic sciences at the University of South Florida, Tampa.
Durvalumab also improved overall survival in all prespecified subgroups, and PFS was similar to that in previous reports (stratified HR 0.51; median of 17.2 vs. 5.6 months with durvalumab and placebo, respectively), he said, noting that “interestingly, patients who were nonsmokers did benefit from durvalumab.”
This is notable because prior research suggests that never-smokers with advanced stage cancer have less of a chance of responding to immunotherapy (although they should still be offered immunotherapy), he explained.
“Also interestingly, it appears as if cisplatin was the better drug to use in the conventional therapy portion of the treatment,” he said.
Durvalumab also provided continued improvement vs. placebo in time to death or distant metastasis (stratified HR, 0.53), time to second progression (stratified HR, 0.58), time to first subsequent therapy or death (stratified HR, 0.58), and time to second subsequent therapy or death (stratified HR, 0.63).
Study subjects were patients with World Health Organization Performance Status scores of 0 or 1 with any PD-L1 tumor status, who received at least two cycles of conventional standard-of-care platinum-based chemoradiotherapy (CRT). They were randomized between May 2014 and April 2016 – at 1-42 days after CRT – to receive intravenous durvalumab at a dose of 10 mg/kg given intravenously every 2 weeks or placebo, and were stratified by age, gender, and smoking history.
Durvalumab was well tolerated; 30.5% and 26.1% of treatment and placebo patients, respectively, had grade 3/4 adverse events, and 15.4% and 9.8%, respectively, discontinued because of adverse events.
“There were no new safety signals with this longer follow-up,” Dr. Antonia said.
After study treatment ended, 41% and 54% in the groups, respectively, received additional anticancer therapy, and 8% and 22.4%, respectively, received additional immunotherapy, he noted.
The results are not only statistically significant, but clinically meaningful, and they offer new hope for patients with a disease that, in those who receive chemoradiotherapy, has a 3-year survival rate of only about 27%, he said.
During a press briefing at the conference, moderator Frances Shepherd, MD, a medical oncologist at Princess Margaret Cancer Centre in Toronto and a past president of the International Association for the Study of Lung Cancer, called the results “very exciting” given that this type of cancer represents about a third of all lung cancers and therefore affects an “enormous number of patients in Canada and globally.”
The PACIFIC trial was sponsored by AstraZeneca. Dr. Antonia reported being a speaker or advisory board member or receiving funding support from AstraZeneca and numerous other companies. Dr. Shepherd reported receiving honoraria and support from AstraZeneca and others. She is a speaker or advisory board member for Eli Lilly, AstraZeneca, and Merck, and she has ownership Interest in Eli Lilly and AstraZeneca.
SOURCE: Antonia S et al., WCLC 2018 Abstract PL02.01.
REPORTING FROM WCLC 2018
Key clinical point: Durvalumab improves survival in stage III unresectable NSCLC patients without progression after CRT.
Major finding: Median overall survival not reached vs. 28.7 months for durvalumab compared with placebo (stratified HR, 0.58).
Study details: The global, randomized, placebo-controlled phase 3 PACIFIC trial of 709 patients.
Disclosures: The PACIFIC trial was sponsored by AstraZeneca. Dr. Antonia reported being a speaker or advisory board member or receiving funding support from AstraZeneca and numerous other companies. Dr. Shepherd reported receiving honoraria and support from AstraZeneca and others. She is a speaker or advisory board member for Eli Lilly, AstraZeneca, and Merck, and she has ownership Interest in Eli Lilly and AstraZeneca.
Source: Antonia S et al. WCLC 2018 Abstract PL02.01.
CAR T-cell studies dominate ongoing cellular therapy trials
NEW YORK – The cell therapy landscape increasingly involves strategies beyond chimeric antigen receptor (CAR) T-cell therapy, but those studies still predominate among investigational trials, according to Frederick L. Locke, MD, of Moffitt Cancer Center in Tampa.
Researchers are looking at CAR T-cell therapy for earlier lines of treatment, especially in patients with aggressive lymphomas, Dr. Locke said at the annual congress on Hematologic Malignancies held by the National Comprehensive Cancer Network.
Of 753 trials examining cell therapies and listed at ClinicalTrials.gov as of March 30, 2018, about half (404) were CAR T-cell therapies. The others included T-cell receptor therapies, tumor infiltrating lymphocyte therapies, dendritic cell vaccines, and natural killer cell–based therapies, according to an article in Nature Reviews.
“The development isn’t just here in the United States,” Dr. Locke said. “It’s really global. We see a lot of activity in Europe, but also in China. We’re seeing medical advances across the world through molecular biology and gene engineering of T cells and other immune cells which can be adoptively transferred into patients.”
That activity includes studies seeking to move CAR T-cell therapy earlier in the treatment paradigm for some diseases, he added. “CAR T-cell therapy in non-Hodgkin lymphoma is really beginning a paradigm shift, at least in my mind.”
Several large, randomized trials that are now comparing CD19 CAR T-cell therapy with second-line standard-of-care therapies for patients with aggressive B-cell lymphomas. Among those trials is ZUMA-7, a phase 3, randomized trial comparing axicabtagene ciloleucel with standard-of-care treatment in patients with relapsed or refractory diffuse large B-cell lymphoma.
While prognosis remains poor for relapsed or progressing aggressive B-cell lymphomas treated with chemotherapy, data to date suggest CAR T-cell therapy produces durable, long-term remissions in about 40% of patients at “a year out and counting,” Dr. Locke said.
He presented a proposed treatment algorithm that included R-CHOP chemotherapy up front and CAR T-cell therapy in later lines of treatment, an approach that Dr. Locke speculated could result in a cure rate of perhaps 80% in large-cell lymphomas.
Encouraging longer-term data is emerging, with some patients with aggressive T-cell lymphomas now without recurrence for 5 years or more following a single infusion of CAR T-cell therapy, he said.
Dr. Locke reported a financial disclosure related to Cellular Biomedicine Group.
NEW YORK – The cell therapy landscape increasingly involves strategies beyond chimeric antigen receptor (CAR) T-cell therapy, but those studies still predominate among investigational trials, according to Frederick L. Locke, MD, of Moffitt Cancer Center in Tampa.
Researchers are looking at CAR T-cell therapy for earlier lines of treatment, especially in patients with aggressive lymphomas, Dr. Locke said at the annual congress on Hematologic Malignancies held by the National Comprehensive Cancer Network.
Of 753 trials examining cell therapies and listed at ClinicalTrials.gov as of March 30, 2018, about half (404) were CAR T-cell therapies. The others included T-cell receptor therapies, tumor infiltrating lymphocyte therapies, dendritic cell vaccines, and natural killer cell–based therapies, according to an article in Nature Reviews.
“The development isn’t just here in the United States,” Dr. Locke said. “It’s really global. We see a lot of activity in Europe, but also in China. We’re seeing medical advances across the world through molecular biology and gene engineering of T cells and other immune cells which can be adoptively transferred into patients.”
That activity includes studies seeking to move CAR T-cell therapy earlier in the treatment paradigm for some diseases, he added. “CAR T-cell therapy in non-Hodgkin lymphoma is really beginning a paradigm shift, at least in my mind.”
Several large, randomized trials that are now comparing CD19 CAR T-cell therapy with second-line standard-of-care therapies for patients with aggressive B-cell lymphomas. Among those trials is ZUMA-7, a phase 3, randomized trial comparing axicabtagene ciloleucel with standard-of-care treatment in patients with relapsed or refractory diffuse large B-cell lymphoma.
While prognosis remains poor for relapsed or progressing aggressive B-cell lymphomas treated with chemotherapy, data to date suggest CAR T-cell therapy produces durable, long-term remissions in about 40% of patients at “a year out and counting,” Dr. Locke said.
He presented a proposed treatment algorithm that included R-CHOP chemotherapy up front and CAR T-cell therapy in later lines of treatment, an approach that Dr. Locke speculated could result in a cure rate of perhaps 80% in large-cell lymphomas.
Encouraging longer-term data is emerging, with some patients with aggressive T-cell lymphomas now without recurrence for 5 years or more following a single infusion of CAR T-cell therapy, he said.
Dr. Locke reported a financial disclosure related to Cellular Biomedicine Group.
NEW YORK – The cell therapy landscape increasingly involves strategies beyond chimeric antigen receptor (CAR) T-cell therapy, but those studies still predominate among investigational trials, according to Frederick L. Locke, MD, of Moffitt Cancer Center in Tampa.
Researchers are looking at CAR T-cell therapy for earlier lines of treatment, especially in patients with aggressive lymphomas, Dr. Locke said at the annual congress on Hematologic Malignancies held by the National Comprehensive Cancer Network.
Of 753 trials examining cell therapies and listed at ClinicalTrials.gov as of March 30, 2018, about half (404) were CAR T-cell therapies. The others included T-cell receptor therapies, tumor infiltrating lymphocyte therapies, dendritic cell vaccines, and natural killer cell–based therapies, according to an article in Nature Reviews.
“The development isn’t just here in the United States,” Dr. Locke said. “It’s really global. We see a lot of activity in Europe, but also in China. We’re seeing medical advances across the world through molecular biology and gene engineering of T cells and other immune cells which can be adoptively transferred into patients.”
That activity includes studies seeking to move CAR T-cell therapy earlier in the treatment paradigm for some diseases, he added. “CAR T-cell therapy in non-Hodgkin lymphoma is really beginning a paradigm shift, at least in my mind.”
Several large, randomized trials that are now comparing CD19 CAR T-cell therapy with second-line standard-of-care therapies for patients with aggressive B-cell lymphomas. Among those trials is ZUMA-7, a phase 3, randomized trial comparing axicabtagene ciloleucel with standard-of-care treatment in patients with relapsed or refractory diffuse large B-cell lymphoma.
While prognosis remains poor for relapsed or progressing aggressive B-cell lymphomas treated with chemotherapy, data to date suggest CAR T-cell therapy produces durable, long-term remissions in about 40% of patients at “a year out and counting,” Dr. Locke said.
He presented a proposed treatment algorithm that included R-CHOP chemotherapy up front and CAR T-cell therapy in later lines of treatment, an approach that Dr. Locke speculated could result in a cure rate of perhaps 80% in large-cell lymphomas.
Encouraging longer-term data is emerging, with some patients with aggressive T-cell lymphomas now without recurrence for 5 years or more following a single infusion of CAR T-cell therapy, he said.
Dr. Locke reported a financial disclosure related to Cellular Biomedicine Group.
EXPERT ANALYSIS FROM THE NCCN HEMATOLOGIC MALIGNANCIES CONGRESS
Dramatic response from pembrolizumab in patient with Lynch syndrome
A woman with two distinct primary tumors achieved complete regression of both after pembrolizumab therapy, investigators report.
This is the first documented instance of a checkpoint inhibitor leading to this kind of simultaneous regression, reported Benjamin Musher, MD, of Baylor College of Medicine, Houston, and his coauthors.
The patient was a 55-year-old woman with a family history of gastric, uterine, and colon cancer. After presenting with weight loss, fatigue, and abdominal pain, colonoscopy showed a 5-cm mucosal lesion. A subsequent PET-CT scan revealed a 12-cm hepatic mass with multiple other liver masses, and bulky lymph nodes nearby. Site biopsies showed two primary cancer types: colonic adenocarcinoma and intrahepatic cholangiocarcinoma.
“Additional staining ... for proteins that repair mismatched DNA showed an absence of MLH1 expression. Sequencing of the patient’s DNA revealed a deleterious mutation in MLH1, which confirmed that Lynch syndrome caused both types of cancer,” the authors wrote in Annals of Internal Medicine.
Lynch syndrome (also called hereditary nonpolyposis colorectal cancer), is an autosomal dominant condition that incurs a high risk of colorectal, pancreatic, bile duct, ovarian, gastric, and uterine cancer. Patients may present with more than one type of cancer simultaneously, as occurred in this case study.
Following diagnosis, the patient started pembrolizumab monotherapy (200 mg IV Q3W). After 16 months the tumors were undetectable by colonoscopy or PET-CT; 2 months later the patient was free of cancer symptoms.
“To our knowledge, our case report is the first to document complete regression of 2 simultaneous types of cancer after treatment with an immune checkpoint inhibitor,” the authors wrote.
But why the dramatic response?
“The types of cancer that develop because of a mismatch repair deficiency contain more mutations than most other kinds of cancer,” the authors explained. These highly mutated cells are recognized by the host immune system, but responses are limited, in part, by programmed cell death proteins. “These events make checkpoint inhibition an attractive and potentially effective treatment for mismatch repair deficient cancer.
“We believe that this case emphasizes the importance of eliciting a thorough family history in patients with cancer and considering the presence of multiple types of primary cancer in a patient with an extensive family history of cancer,” the authors concluded. “It also shows the value of identifying mismatch repair deficiency, [in which] immunotherapy can yield dramatic and durable benefit.”
Dr. Musher reported compensation from LOKON pharmaceuticals.
SOURCE: Musher et al. Ann Intern Med. 2018 Sep 24. doi: 10.7326/L18-0360.
A woman with two distinct primary tumors achieved complete regression of both after pembrolizumab therapy, investigators report.
This is the first documented instance of a checkpoint inhibitor leading to this kind of simultaneous regression, reported Benjamin Musher, MD, of Baylor College of Medicine, Houston, and his coauthors.
The patient was a 55-year-old woman with a family history of gastric, uterine, and colon cancer. After presenting with weight loss, fatigue, and abdominal pain, colonoscopy showed a 5-cm mucosal lesion. A subsequent PET-CT scan revealed a 12-cm hepatic mass with multiple other liver masses, and bulky lymph nodes nearby. Site biopsies showed two primary cancer types: colonic adenocarcinoma and intrahepatic cholangiocarcinoma.
“Additional staining ... for proteins that repair mismatched DNA showed an absence of MLH1 expression. Sequencing of the patient’s DNA revealed a deleterious mutation in MLH1, which confirmed that Lynch syndrome caused both types of cancer,” the authors wrote in Annals of Internal Medicine.
Lynch syndrome (also called hereditary nonpolyposis colorectal cancer), is an autosomal dominant condition that incurs a high risk of colorectal, pancreatic, bile duct, ovarian, gastric, and uterine cancer. Patients may present with more than one type of cancer simultaneously, as occurred in this case study.
Following diagnosis, the patient started pembrolizumab monotherapy (200 mg IV Q3W). After 16 months the tumors were undetectable by colonoscopy or PET-CT; 2 months later the patient was free of cancer symptoms.
“To our knowledge, our case report is the first to document complete regression of 2 simultaneous types of cancer after treatment with an immune checkpoint inhibitor,” the authors wrote.
But why the dramatic response?
“The types of cancer that develop because of a mismatch repair deficiency contain more mutations than most other kinds of cancer,” the authors explained. These highly mutated cells are recognized by the host immune system, but responses are limited, in part, by programmed cell death proteins. “These events make checkpoint inhibition an attractive and potentially effective treatment for mismatch repair deficient cancer.
“We believe that this case emphasizes the importance of eliciting a thorough family history in patients with cancer and considering the presence of multiple types of primary cancer in a patient with an extensive family history of cancer,” the authors concluded. “It also shows the value of identifying mismatch repair deficiency, [in which] immunotherapy can yield dramatic and durable benefit.”
Dr. Musher reported compensation from LOKON pharmaceuticals.
SOURCE: Musher et al. Ann Intern Med. 2018 Sep 24. doi: 10.7326/L18-0360.
A woman with two distinct primary tumors achieved complete regression of both after pembrolizumab therapy, investigators report.
This is the first documented instance of a checkpoint inhibitor leading to this kind of simultaneous regression, reported Benjamin Musher, MD, of Baylor College of Medicine, Houston, and his coauthors.
The patient was a 55-year-old woman with a family history of gastric, uterine, and colon cancer. After presenting with weight loss, fatigue, and abdominal pain, colonoscopy showed a 5-cm mucosal lesion. A subsequent PET-CT scan revealed a 12-cm hepatic mass with multiple other liver masses, and bulky lymph nodes nearby. Site biopsies showed two primary cancer types: colonic adenocarcinoma and intrahepatic cholangiocarcinoma.
“Additional staining ... for proteins that repair mismatched DNA showed an absence of MLH1 expression. Sequencing of the patient’s DNA revealed a deleterious mutation in MLH1, which confirmed that Lynch syndrome caused both types of cancer,” the authors wrote in Annals of Internal Medicine.
Lynch syndrome (also called hereditary nonpolyposis colorectal cancer), is an autosomal dominant condition that incurs a high risk of colorectal, pancreatic, bile duct, ovarian, gastric, and uterine cancer. Patients may present with more than one type of cancer simultaneously, as occurred in this case study.
Following diagnosis, the patient started pembrolizumab monotherapy (200 mg IV Q3W). After 16 months the tumors were undetectable by colonoscopy or PET-CT; 2 months later the patient was free of cancer symptoms.
“To our knowledge, our case report is the first to document complete regression of 2 simultaneous types of cancer after treatment with an immune checkpoint inhibitor,” the authors wrote.
But why the dramatic response?
“The types of cancer that develop because of a mismatch repair deficiency contain more mutations than most other kinds of cancer,” the authors explained. These highly mutated cells are recognized by the host immune system, but responses are limited, in part, by programmed cell death proteins. “These events make checkpoint inhibition an attractive and potentially effective treatment for mismatch repair deficient cancer.
“We believe that this case emphasizes the importance of eliciting a thorough family history in patients with cancer and considering the presence of multiple types of primary cancer in a patient with an extensive family history of cancer,” the authors concluded. “It also shows the value of identifying mismatch repair deficiency, [in which] immunotherapy can yield dramatic and durable benefit.”
Dr. Musher reported compensation from LOKON pharmaceuticals.
SOURCE: Musher et al. Ann Intern Med. 2018 Sep 24. doi: 10.7326/L18-0360.
FROM ANNALS OF INTERNAL MEDICINE
Key clinical point: Pembrolizumab may provide complete tumor regression in patients with mismatch repair deficiency (Lynch syndrome) who have more than one type of cancer.
Major finding: A woman with primary colonic adenocarcinoma and primary intrahepatic cholangiocarcinoma achieved complete regression of both tumor types after pembrolizumab therapy.
Study details: A case study of a 55-year-old woman with Lynch syndrome who had a family history of gastric, uterine, and colon cancer.
Disclosures: Dr. Musher reported receiving compensation from Lokon.
Source: Musher et al. Ann Intern Med. 2018 Sep 24. doi: 10.7326/L18-0360.
PD-1/PD-L1 treatment linked to hyperprogressive disease in lung cancer patients
Hyperprogressive disease is a new pattern of progression that may be more prevalent in patients with non–small-cell lung cancer receiving treatment with PD-1/PD-L1 inhibitors than in those receiving chemotherapy, results of a multicenter retrospective study suggest.
Nearly 14% of patients treated with PD/1/PD-L1 inhibitors had hyperprogressive disease in the study, compared with about 5% of patients treated with chemotherapy, the investigators reported.
This acceleration of tumor growth during therapy was associated with a high metastatic burden before treatment, and with a poor prognosis after treatment, wrote Benjamin Besse, MD, PhD, of the cancer medicine department at Gustave Roussy, Villejuif, France, and his colleagues.
Based on these findings, disease evolution should be carefully monitored to identify “hyperprogressors” among non–small-cell lung cancer (NSCLC) patients receiving PD-1/PD-L1 inhibitors, Dr. Besse and his colleagues said.
“Because of the poor overall survival associated with hyperprogressive disease, an early switch to salvage chemotherapy in these patients should be considered,” they wrote in JAMA Oncology.
This is believed to be the first study to look at incidence of hyperprogressive disease after PD-1/PD-L1 therapy specifically in NSCLC patients, and the first in any tumor type to include a chemotherapy treatment control group, according to Dr. Besse and his coauthors.
In one other recent report, hyperprogressive disease was seen in 9% of advanced cancers, and in a second recent investigation, it was seen in 29% of head and neck cancer patients, they said.
Although those proportions appear different, that could be due to differing interpretations of hyperprogressive disease, as there is no consensus on the optimal definition, they noted.
In this study, which included 406 patients with advanced NSCLC treated with PD-1/PD-L1 inhibitors and 59 treated with chemotherapy, hyperprogressive disease was defined as progressive disease observed at the first computed tomography scan and an absolute increase in tumor growth rate of 50% or more per month.
A total of 56 patients (13.8%) in the PD-1/PD-L1 treatment group met that definition for hyperprogressive disease, the investigators found. By comparison, three patients (5.1%) in the chemotherapy treatment group had hyperprogressive disease.
With a median follow-up of 12.1 months in the PD-1/PD-L1 group, the median overall survival was 13.4 months. Median overall survival for those with progressive disease was 6.2 months, and significantly lower at 3.4 months for those who had experienced hyperprogressive disease (P = .002), Dr. Besse and his coinvestigators found.
Moreover, 42.6% patients with progressive disease had two or more metastatic sites, compared with 62.5% of patients with hyperprogressive disease (P = .006), they reported.
The phenomenon of hyperprogressive disease might explain the initial excess in deaths seen in some phase 3 trials, Dr. Besse said in an interview posted on the JAMA Oncology website.
“In most of the second-line trials that compared single-agent immunotherapy to single-agent chemotherapy, overall survival curves crossed, meaning that there were an extra number of deaths in the immunotherapy arm,” he said in the interview. “That led us to evaluate the speed of progression.”
Based on the study results, Dr. Besse recommends early assessment by CT scan at 6 or 8 weeks after the start of immunotherapy. “If a patient has hyperprogressive disease, you don’t have much time to react,” he said. “You have to switch to a new treatment quite early.”
Dr. Besse reported receiving research funding from AstraZeneca, Boehringer, Bristol-Myers Squibb, Clovis Oncology, GlaxoSmithKline, Eli Lilly, Inivata, Merck Sharp & Dohme, Onxeo, OSE Pharma, Pfizer, Roche/Genentech, and Servier.
SOURCE: Ferrara R et al. JAMA Oncol. 2018 Sep 6. doi: 10.1001/jamaoncol.2018.3676.
Hyperprogressive disease is a new pattern of progression that may be more prevalent in patients with non–small-cell lung cancer receiving treatment with PD-1/PD-L1 inhibitors than in those receiving chemotherapy, results of a multicenter retrospective study suggest.
Nearly 14% of patients treated with PD/1/PD-L1 inhibitors had hyperprogressive disease in the study, compared with about 5% of patients treated with chemotherapy, the investigators reported.
This acceleration of tumor growth during therapy was associated with a high metastatic burden before treatment, and with a poor prognosis after treatment, wrote Benjamin Besse, MD, PhD, of the cancer medicine department at Gustave Roussy, Villejuif, France, and his colleagues.
Based on these findings, disease evolution should be carefully monitored to identify “hyperprogressors” among non–small-cell lung cancer (NSCLC) patients receiving PD-1/PD-L1 inhibitors, Dr. Besse and his colleagues said.
“Because of the poor overall survival associated with hyperprogressive disease, an early switch to salvage chemotherapy in these patients should be considered,” they wrote in JAMA Oncology.
This is believed to be the first study to look at incidence of hyperprogressive disease after PD-1/PD-L1 therapy specifically in NSCLC patients, and the first in any tumor type to include a chemotherapy treatment control group, according to Dr. Besse and his coauthors.
In one other recent report, hyperprogressive disease was seen in 9% of advanced cancers, and in a second recent investigation, it was seen in 29% of head and neck cancer patients, they said.
Although those proportions appear different, that could be due to differing interpretations of hyperprogressive disease, as there is no consensus on the optimal definition, they noted.
In this study, which included 406 patients with advanced NSCLC treated with PD-1/PD-L1 inhibitors and 59 treated with chemotherapy, hyperprogressive disease was defined as progressive disease observed at the first computed tomography scan and an absolute increase in tumor growth rate of 50% or more per month.
A total of 56 patients (13.8%) in the PD-1/PD-L1 treatment group met that definition for hyperprogressive disease, the investigators found. By comparison, three patients (5.1%) in the chemotherapy treatment group had hyperprogressive disease.
With a median follow-up of 12.1 months in the PD-1/PD-L1 group, the median overall survival was 13.4 months. Median overall survival for those with progressive disease was 6.2 months, and significantly lower at 3.4 months for those who had experienced hyperprogressive disease (P = .002), Dr. Besse and his coinvestigators found.
Moreover, 42.6% patients with progressive disease had two or more metastatic sites, compared with 62.5% of patients with hyperprogressive disease (P = .006), they reported.
The phenomenon of hyperprogressive disease might explain the initial excess in deaths seen in some phase 3 trials, Dr. Besse said in an interview posted on the JAMA Oncology website.
“In most of the second-line trials that compared single-agent immunotherapy to single-agent chemotherapy, overall survival curves crossed, meaning that there were an extra number of deaths in the immunotherapy arm,” he said in the interview. “That led us to evaluate the speed of progression.”
Based on the study results, Dr. Besse recommends early assessment by CT scan at 6 or 8 weeks after the start of immunotherapy. “If a patient has hyperprogressive disease, you don’t have much time to react,” he said. “You have to switch to a new treatment quite early.”
Dr. Besse reported receiving research funding from AstraZeneca, Boehringer, Bristol-Myers Squibb, Clovis Oncology, GlaxoSmithKline, Eli Lilly, Inivata, Merck Sharp & Dohme, Onxeo, OSE Pharma, Pfizer, Roche/Genentech, and Servier.
SOURCE: Ferrara R et al. JAMA Oncol. 2018 Sep 6. doi: 10.1001/jamaoncol.2018.3676.
Hyperprogressive disease is a new pattern of progression that may be more prevalent in patients with non–small-cell lung cancer receiving treatment with PD-1/PD-L1 inhibitors than in those receiving chemotherapy, results of a multicenter retrospective study suggest.
Nearly 14% of patients treated with PD/1/PD-L1 inhibitors had hyperprogressive disease in the study, compared with about 5% of patients treated with chemotherapy, the investigators reported.
This acceleration of tumor growth during therapy was associated with a high metastatic burden before treatment, and with a poor prognosis after treatment, wrote Benjamin Besse, MD, PhD, of the cancer medicine department at Gustave Roussy, Villejuif, France, and his colleagues.
Based on these findings, disease evolution should be carefully monitored to identify “hyperprogressors” among non–small-cell lung cancer (NSCLC) patients receiving PD-1/PD-L1 inhibitors, Dr. Besse and his colleagues said.
“Because of the poor overall survival associated with hyperprogressive disease, an early switch to salvage chemotherapy in these patients should be considered,” they wrote in JAMA Oncology.
This is believed to be the first study to look at incidence of hyperprogressive disease after PD-1/PD-L1 therapy specifically in NSCLC patients, and the first in any tumor type to include a chemotherapy treatment control group, according to Dr. Besse and his coauthors.
In one other recent report, hyperprogressive disease was seen in 9% of advanced cancers, and in a second recent investigation, it was seen in 29% of head and neck cancer patients, they said.
Although those proportions appear different, that could be due to differing interpretations of hyperprogressive disease, as there is no consensus on the optimal definition, they noted.
In this study, which included 406 patients with advanced NSCLC treated with PD-1/PD-L1 inhibitors and 59 treated with chemotherapy, hyperprogressive disease was defined as progressive disease observed at the first computed tomography scan and an absolute increase in tumor growth rate of 50% or more per month.
A total of 56 patients (13.8%) in the PD-1/PD-L1 treatment group met that definition for hyperprogressive disease, the investigators found. By comparison, three patients (5.1%) in the chemotherapy treatment group had hyperprogressive disease.
With a median follow-up of 12.1 months in the PD-1/PD-L1 group, the median overall survival was 13.4 months. Median overall survival for those with progressive disease was 6.2 months, and significantly lower at 3.4 months for those who had experienced hyperprogressive disease (P = .002), Dr. Besse and his coinvestigators found.
Moreover, 42.6% patients with progressive disease had two or more metastatic sites, compared with 62.5% of patients with hyperprogressive disease (P = .006), they reported.
The phenomenon of hyperprogressive disease might explain the initial excess in deaths seen in some phase 3 trials, Dr. Besse said in an interview posted on the JAMA Oncology website.
“In most of the second-line trials that compared single-agent immunotherapy to single-agent chemotherapy, overall survival curves crossed, meaning that there were an extra number of deaths in the immunotherapy arm,” he said in the interview. “That led us to evaluate the speed of progression.”
Based on the study results, Dr. Besse recommends early assessment by CT scan at 6 or 8 weeks after the start of immunotherapy. “If a patient has hyperprogressive disease, you don’t have much time to react,” he said. “You have to switch to a new treatment quite early.”
Dr. Besse reported receiving research funding from AstraZeneca, Boehringer, Bristol-Myers Squibb, Clovis Oncology, GlaxoSmithKline, Eli Lilly, Inivata, Merck Sharp & Dohme, Onxeo, OSE Pharma, Pfizer, Roche/Genentech, and Servier.
SOURCE: Ferrara R et al. JAMA Oncol. 2018 Sep 6. doi: 10.1001/jamaoncol.2018.3676.
FROM JAMA ONCOLOGY
Key clinical point: Hyperprogressive disease is a new pattern of progression that appears to be associated with PD-1/PD-L1 treatment of various cancers.
Major finding: Nearly 14% of non–small-cell lung cancer patients had hyperprogression in this study, compared with about 5% of patients receiving chemotherapy.
Study details: A retrospective, multicenter study comprising 406 patients with advanced NSCLC treated with PD-1/PD-L1 inhibitors and 59 treated with chemotherapy.
Disclosures: The authors reported disclosures related to AstraZeneca, Boehringer, Bristol-Myers Squibb, Clovis Oncology, GlaxoSmithKline, Eli Lilly, Inivata, Merck Sharp & Dohme, Onxeo, OSE Pharma, Pfizer, Roche/Genentech, and Servier, among others.
Source: Ferrara R et al. JAMA Oncol. 2018 Sep 6. doi: 10.1001/jamaoncol.2018.3676.