User login
Primary care inaccurately estimates cancer risk
Primary care physicians’ assessments of the risks and benefits of cancer screening didn’t match with reality, based on the results of a survey of beliefs and behaviors around cancer risk.
"We were really surprised at the high percentage of physicians who were inaccurately estimating risk," said Dr. Laura-Mae Baldwin, professor of family medicine at the University of Washington, Seattle, who presented on behalf of her colleagues a slice of data from the survey of 3,200 physicians. "This has the potential for average-risk patients to receive unnecessary testing, and for high-risk patients to miss opportunities for prevention or early detection."
The cross-sectional national survey used the 2008 American Medical Association master file to randomly sample family physicians, general internists, and obstetrician-gynecologists. The physicians were all under age 65 and practiced in either a hospital or an office. They were contacted by mail, and given encouragement in the form of a $20 bill. In a second mailing, nonresponders received a written note from Dr. Baldwin. Overall, there was a 62% response rate: 591 family physicians, 414 general internists, and 569 ob.gyns. took part.
Survey participants were given a 12-page booklet with a particular patient vignette and a photo of the patient. The example included a medical and family history, along with age, race, sex, insurance status, and some other characteristics.
The researchers focused on ovarian cancer in particular because the Centers for Disease Control and Prevention, which funded the study, had a special interest in that cancer.
For instance, one vignette presented a 51-year-old white woman who came in because she wanted to be sure she was up to date on various tests. She had no medical problems, but had not seen a physician in 3 years. Her father had hypertension and her mother died of ovarian cancer at age 65. The other family history was negative, and there was an unremarkable physical exam.
The researchers had 258 variations for the different vignettes, varying age, race, insurance status, whether the patient asked for ovarian cancer screening, and family history. Physicians were asked to give their best estimate for this patient, and for other example patients, of risk for breast, ovarian, and colon cancer. They were asked to state whether the patient had a risk that was the same as that of the general population, somewhat higher, or much higher.
For a woman who was at the same risk as the general population for ovarian cancer, 72% of physicians were in agreement. However, 26% estimated the women were at somewhat higher risk and 1%, at much higher risk. For women at somewhat higher risk for ovarian cancer, however, 7% of physicians correctly assessed risk. Risk was assessed as somewhat higher or much higher by 90%, Dr. Baldwin reported at the annual meeting of the North American Primary Care Research Group.
For a woman at high risk for ovarian cancer, 35% of physicians correctly estimated that risk. Most physicians estimated risk as somewhat higher, but 11% thought her risk was the same as that for the general population.
The assessments of risk for colon cancer were similarly inaccurate. For the vignette of the woman at the same risk as the general population, 62% of physicians were on target, and 39% overestimated the risk.
There were no significant differences among the specialties, but ob.gyns. tended to be more accurate in their screening decisions, said Dr. Baldwin. An analysis showed that providers’ personal history with cancer influenced their recommended screening behaviors, said Dr. Baldwin. She did not present specific data on that issue.
The study did have some limitations in that physicians were given somewhat limited information about the patient’s risk. Dr. Baldwin said it’s important to study physician behaviors further, especially since so many in the survey underestimated risk in a woman who clearly was at high risk for ovarian cancer.
Primary care physicians’ assessments of the risks and benefits of cancer screening didn’t match with reality, based on the results of a survey of beliefs and behaviors around cancer risk.
"We were really surprised at the high percentage of physicians who were inaccurately estimating risk," said Dr. Laura-Mae Baldwin, professor of family medicine at the University of Washington, Seattle, who presented on behalf of her colleagues a slice of data from the survey of 3,200 physicians. "This has the potential for average-risk patients to receive unnecessary testing, and for high-risk patients to miss opportunities for prevention or early detection."
The cross-sectional national survey used the 2008 American Medical Association master file to randomly sample family physicians, general internists, and obstetrician-gynecologists. The physicians were all under age 65 and practiced in either a hospital or an office. They were contacted by mail, and given encouragement in the form of a $20 bill. In a second mailing, nonresponders received a written note from Dr. Baldwin. Overall, there was a 62% response rate: 591 family physicians, 414 general internists, and 569 ob.gyns. took part.
Survey participants were given a 12-page booklet with a particular patient vignette and a photo of the patient. The example included a medical and family history, along with age, race, sex, insurance status, and some other characteristics.
The researchers focused on ovarian cancer in particular because the Centers for Disease Control and Prevention, which funded the study, had a special interest in that cancer.
For instance, one vignette presented a 51-year-old white woman who came in because she wanted to be sure she was up to date on various tests. She had no medical problems, but had not seen a physician in 3 years. Her father had hypertension and her mother died of ovarian cancer at age 65. The other family history was negative, and there was an unremarkable physical exam.
The researchers had 258 variations for the different vignettes, varying age, race, insurance status, whether the patient asked for ovarian cancer screening, and family history. Physicians were asked to give their best estimate for this patient, and for other example patients, of risk for breast, ovarian, and colon cancer. They were asked to state whether the patient had a risk that was the same as that of the general population, somewhat higher, or much higher.
For a woman who was at the same risk as the general population for ovarian cancer, 72% of physicians were in agreement. However, 26% estimated the women were at somewhat higher risk and 1%, at much higher risk. For women at somewhat higher risk for ovarian cancer, however, 7% of physicians correctly assessed risk. Risk was assessed as somewhat higher or much higher by 90%, Dr. Baldwin reported at the annual meeting of the North American Primary Care Research Group.
For a woman at high risk for ovarian cancer, 35% of physicians correctly estimated that risk. Most physicians estimated risk as somewhat higher, but 11% thought her risk was the same as that for the general population.
The assessments of risk for colon cancer were similarly inaccurate. For the vignette of the woman at the same risk as the general population, 62% of physicians were on target, and 39% overestimated the risk.
There were no significant differences among the specialties, but ob.gyns. tended to be more accurate in their screening decisions, said Dr. Baldwin. An analysis showed that providers’ personal history with cancer influenced their recommended screening behaviors, said Dr. Baldwin. She did not present specific data on that issue.
The study did have some limitations in that physicians were given somewhat limited information about the patient’s risk. Dr. Baldwin said it’s important to study physician behaviors further, especially since so many in the survey underestimated risk in a woman who clearly was at high risk for ovarian cancer.
Primary care physicians’ assessments of the risks and benefits of cancer screening didn’t match with reality, based on the results of a survey of beliefs and behaviors around cancer risk.
"We were really surprised at the high percentage of physicians who were inaccurately estimating risk," said Dr. Laura-Mae Baldwin, professor of family medicine at the University of Washington, Seattle, who presented on behalf of her colleagues a slice of data from the survey of 3,200 physicians. "This has the potential for average-risk patients to receive unnecessary testing, and for high-risk patients to miss opportunities for prevention or early detection."
The cross-sectional national survey used the 2008 American Medical Association master file to randomly sample family physicians, general internists, and obstetrician-gynecologists. The physicians were all under age 65 and practiced in either a hospital or an office. They were contacted by mail, and given encouragement in the form of a $20 bill. In a second mailing, nonresponders received a written note from Dr. Baldwin. Overall, there was a 62% response rate: 591 family physicians, 414 general internists, and 569 ob.gyns. took part.
Survey participants were given a 12-page booklet with a particular patient vignette and a photo of the patient. The example included a medical and family history, along with age, race, sex, insurance status, and some other characteristics.
The researchers focused on ovarian cancer in particular because the Centers for Disease Control and Prevention, which funded the study, had a special interest in that cancer.
For instance, one vignette presented a 51-year-old white woman who came in because she wanted to be sure she was up to date on various tests. She had no medical problems, but had not seen a physician in 3 years. Her father had hypertension and her mother died of ovarian cancer at age 65. The other family history was negative, and there was an unremarkable physical exam.
The researchers had 258 variations for the different vignettes, varying age, race, insurance status, whether the patient asked for ovarian cancer screening, and family history. Physicians were asked to give their best estimate for this patient, and for other example patients, of risk for breast, ovarian, and colon cancer. They were asked to state whether the patient had a risk that was the same as that of the general population, somewhat higher, or much higher.
For a woman who was at the same risk as the general population for ovarian cancer, 72% of physicians were in agreement. However, 26% estimated the women were at somewhat higher risk and 1%, at much higher risk. For women at somewhat higher risk for ovarian cancer, however, 7% of physicians correctly assessed risk. Risk was assessed as somewhat higher or much higher by 90%, Dr. Baldwin reported at the annual meeting of the North American Primary Care Research Group.
For a woman at high risk for ovarian cancer, 35% of physicians correctly estimated that risk. Most physicians estimated risk as somewhat higher, but 11% thought her risk was the same as that for the general population.
The assessments of risk for colon cancer were similarly inaccurate. For the vignette of the woman at the same risk as the general population, 62% of physicians were on target, and 39% overestimated the risk.
There were no significant differences among the specialties, but ob.gyns. tended to be more accurate in their screening decisions, said Dr. Baldwin. An analysis showed that providers’ personal history with cancer influenced their recommended screening behaviors, said Dr. Baldwin. She did not present specific data on that issue.
The study did have some limitations in that physicians were given somewhat limited information about the patient’s risk. Dr. Baldwin said it’s important to study physician behaviors further, especially since so many in the survey underestimated risk in a woman who clearly was at high risk for ovarian cancer.
AT THE ANNUAL MEETING OF THE NORTH AMERICAN PRIMARY CARE RESEARCH GROUP
Major Finding: For a woman at high risk for ovarian cancer, 35% of surveyed physicians correctly estimated that risk, and 11% thought her risk was the same as that for the general population.
Data Source: Data from a national, cross-sectional survey of 3,200 physicians.
Disclosures: The study was funded by the Centers for Disease Control and Prevention.
Newly labeled sunscreens surface on shelves
Sunscreens that have proven their protective ability and feature updated, more-consumer-friendly labeling are hitting store shelves, but they currently share space with older products that may not have passed muster with the Food and Drug Administration.
This mix of old and new packaging coincides with an FDA announcement that, later this year, it will review sunscreen ingredient safety and the potential approval of additional UVA-blocking agents.
In January, the agency issued its semiannual agenda for the coming year. That list included two sunscreen-related items.
The FDA said it would issue an "advance notice of proposed rulemaking" in July on how it will address sunscreen ingredient safety, which is the first step in a three-step process that culminates in a final rule.
The agency also said it would take a similar early step in the regulatory process for new ingredients manufacturers would like to add to their products.
At least six additional UVA filters are awaiting FDA approval, said Dr. Steven Q. Wang, director of dermatologic surgery and dermatology at the Memorial Sloan-Kettering Cancer Center, Basking Ridge, N.J. Currently, only two UVA-blocking agents – avobenzone and zinc oxide – are approved in the United States, but many others are available in Europe and elsewhere around the world.
Dr. Wang said he is looking forward to progress on UVA blockers; he noted that although both UVA and UVB contribute to skin cancer development, UVA penetrates deeper into the skin, contributes to more DNA damage, and plays a larger role in skin aging. A study of sunscreens from 1997 to 2009 by Dr. Wang showed that increasing numbers of products contained either avobenzone or zinc oxide, matching their claims of UVA protection.
In the late 1990s, 81% of the products surveyed claimed to protect against UVA, but only 5% actually contained a UVA blocker. By 2009, 80% of the products still made the claim, and 70% contained UVA-blocking agents. The study was published in the January issue of the journal Photochemical & Photobiological Sciences (Photochem. Photobiol. Sci. 2013;12:197-202).
Based on these findings, many of the products on the market in the past decade already met the FDA’s new criteria – announced in June 2011 – to claim protection against skin cancer, Dr. Wang said. And, clinicians and consumers should be reassured that products that meet the FDA labeling rules are effective and safe, he added.
Because they have already met the FDA’s effectiveness criteria, most products have not needed to be reformulated, said Farah Ahmed, chair of the sunscreen task force at the Personal Care Products Council.
But manufacturers have relabeled products to conform to the FDA’s rules, she said. The Council estimates that at least 4,500 products marketed in the United States claim an SPF, which subjects them to the FDA sunscreen rules. The product list includes not only sunscreens but lip balms, daily moisturizers, makeup, and any other product that contains a sunscreen component.
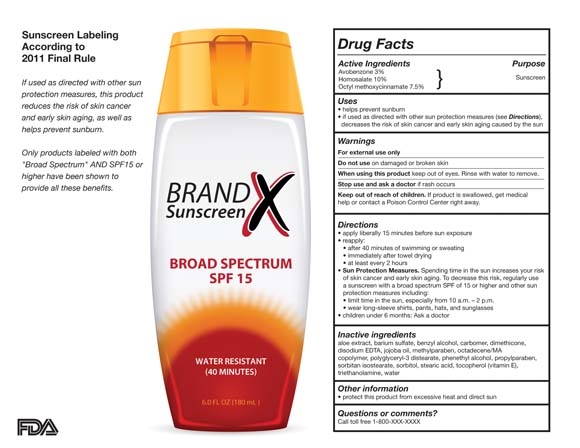
Products that have proved through testing that they protect against UVA and UVB radiation can claim that they are "broad spectrum" and will be labeled as SPF 15 or higher. The label also will be able to claim that the product can protect against sunburn, and, if used as directed with other sun protection measures, can reduce the risk of skin cancer and early skin aging.
Any product not labeled as "broad spectrum" or that has an SPF value between 2 and 14 will carry a warning: "Skin Cancer/Skin Aging Alert: Spending time in the sun increases your risk of skin cancer and early skin aging. This product has been shown only to help prevent sunburn, not skin cancer or early skin aging."
Under the revised labeling, no product can claim to be waterproof or sweatproof. If a product claims to be water resistant, the product’s label must state how long a user "can expect to get the declared SPF level of protection while swimming or sweating, based on standard testing," according to the FDA.
For more information, visit the agency’s website.
There may still be products on store shelves that have the old labeling, said Ms. Ahmed. That’s because the FDA has allowed a phase-in. Retailers also can choose to sell remaining stocks of the old products or remove them. "I think we’ll continue to see a mix of both products on the shelves," said Ms. Ahmed.
The situation creates the potential for confusion among consumers, although the FDA rules were meant to create a uniform label to help increase sun protection knowledge and the use of sun protection products.
Dr. Wang says he is telling patients to look for products that are labeled "broad spectrum" on the front, which is the best indicator that they are newly labeled and in compliance with FDA rules.
The FDA has been criticized for years for not finalizing the "monograph" – the accepted criteria or recipe – for sunscreen products. Although a final monograph is nowhere in sight, Dr. Wang said that he thought the agency had "done a reasonable job" in setting the cutoff point for products that could claim UVA protection against cancer at the accepted wavelength of 370 nm.
The FDA also plans to examine whether products labeled with an SPF greater than 50 provide any better protection than an SPF 50 sunscreen. The agency proposed in June 2011 that sunscreens with an SPF greater than 50 be labeled "SPF 50-plus," but nothing further has been issued. For now, consumers will continue to see sunscreens labeled as SPF 70, 80, or even 100.
There has been some difference of opinion on whether higher-SPF products are more beneficial. Dr. Wang said he recommends an SPF 30 product for daily use, but suggests higher SPFs for recreational activities that put users in the sun for longer periods.
The FDA also asked for more data on sunscreen-containing wipes, powders, body washes, and shampoos.
Finally, there may be some controversy down the road when the agency takes a closer look at the safety of ingredients in sun protection products. The Washington-based Environmental Working Group has criticized the safety of some of those ingredients – in particular oxybenzone and retinyl palmitate – and did so again last year in its annual review of sunscreens.
The American Academy of Dermatology refuted the group, saying that there is no evidence that these ingredients are dangerous. The AAD backs the use of a water-resistant, broad-spectrum sunscreen that protects against UVA and UVB radiation, with an SPF 30 or higher, in conjunction with limiting sun exposure and wearing sun-protective clothing.
Dr. Wang agrees that oxybenzone and retinyl palmitate appear to be safe, but he says that some manufacturers have been removing the vitamin A derivative because of the bad publicity. Oxybenzone also may be removed as newer UVA blockers are approved, he said. "But right now, we don’t have any other alternatives," he noted.
For help selecting and using sunscreens effectively, click here.
Dr. Wang disclosed that he is a consultant for L’Oreal, and that he has collaborated with researchers at Procter & Gamble, but has not received any compensation from that company.
On Twitter @aliciaault
Sunscreens that have proven their protective ability and feature updated, more-consumer-friendly labeling are hitting store shelves, but they currently share space with older products that may not have passed muster with the Food and Drug Administration.
This mix of old and new packaging coincides with an FDA announcement that, later this year, it will review sunscreen ingredient safety and the potential approval of additional UVA-blocking agents.
In January, the agency issued its semiannual agenda for the coming year. That list included two sunscreen-related items.
The FDA said it would issue an "advance notice of proposed rulemaking" in July on how it will address sunscreen ingredient safety, which is the first step in a three-step process that culminates in a final rule.
The agency also said it would take a similar early step in the regulatory process for new ingredients manufacturers would like to add to their products.
At least six additional UVA filters are awaiting FDA approval, said Dr. Steven Q. Wang, director of dermatologic surgery and dermatology at the Memorial Sloan-Kettering Cancer Center, Basking Ridge, N.J. Currently, only two UVA-blocking agents – avobenzone and zinc oxide – are approved in the United States, but many others are available in Europe and elsewhere around the world.
Dr. Wang said he is looking forward to progress on UVA blockers; he noted that although both UVA and UVB contribute to skin cancer development, UVA penetrates deeper into the skin, contributes to more DNA damage, and plays a larger role in skin aging. A study of sunscreens from 1997 to 2009 by Dr. Wang showed that increasing numbers of products contained either avobenzone or zinc oxide, matching their claims of UVA protection.
In the late 1990s, 81% of the products surveyed claimed to protect against UVA, but only 5% actually contained a UVA blocker. By 2009, 80% of the products still made the claim, and 70% contained UVA-blocking agents. The study was published in the January issue of the journal Photochemical & Photobiological Sciences (Photochem. Photobiol. Sci. 2013;12:197-202).
Based on these findings, many of the products on the market in the past decade already met the FDA’s new criteria – announced in June 2011 – to claim protection against skin cancer, Dr. Wang said. And, clinicians and consumers should be reassured that products that meet the FDA labeling rules are effective and safe, he added.
Because they have already met the FDA’s effectiveness criteria, most products have not needed to be reformulated, said Farah Ahmed, chair of the sunscreen task force at the Personal Care Products Council.
But manufacturers have relabeled products to conform to the FDA’s rules, she said. The Council estimates that at least 4,500 products marketed in the United States claim an SPF, which subjects them to the FDA sunscreen rules. The product list includes not only sunscreens but lip balms, daily moisturizers, makeup, and any other product that contains a sunscreen component.
Products that have proved through testing that they protect against UVA and UVB radiation can claim that they are "broad spectrum" and will be labeled as SPF 15 or higher. The label also will be able to claim that the product can protect against sunburn, and, if used as directed with other sun protection measures, can reduce the risk of skin cancer and early skin aging.
Any product not labeled as "broad spectrum" or that has an SPF value between 2 and 14 will carry a warning: "Skin Cancer/Skin Aging Alert: Spending time in the sun increases your risk of skin cancer and early skin aging. This product has been shown only to help prevent sunburn, not skin cancer or early skin aging."
Under the revised labeling, no product can claim to be waterproof or sweatproof. If a product claims to be water resistant, the product’s label must state how long a user "can expect to get the declared SPF level of protection while swimming or sweating, based on standard testing," according to the FDA.
For more information, visit the agency’s website.
There may still be products on store shelves that have the old labeling, said Ms. Ahmed. That’s because the FDA has allowed a phase-in. Retailers also can choose to sell remaining stocks of the old products or remove them. "I think we’ll continue to see a mix of both products on the shelves," said Ms. Ahmed.
The situation creates the potential for confusion among consumers, although the FDA rules were meant to create a uniform label to help increase sun protection knowledge and the use of sun protection products.
Dr. Wang says he is telling patients to look for products that are labeled "broad spectrum" on the front, which is the best indicator that they are newly labeled and in compliance with FDA rules.
The FDA has been criticized for years for not finalizing the "monograph" – the accepted criteria or recipe – for sunscreen products. Although a final monograph is nowhere in sight, Dr. Wang said that he thought the agency had "done a reasonable job" in setting the cutoff point for products that could claim UVA protection against cancer at the accepted wavelength of 370 nm.
The FDA also plans to examine whether products labeled with an SPF greater than 50 provide any better protection than an SPF 50 sunscreen. The agency proposed in June 2011 that sunscreens with an SPF greater than 50 be labeled "SPF 50-plus," but nothing further has been issued. For now, consumers will continue to see sunscreens labeled as SPF 70, 80, or even 100.
There has been some difference of opinion on whether higher-SPF products are more beneficial. Dr. Wang said he recommends an SPF 30 product for daily use, but suggests higher SPFs for recreational activities that put users in the sun for longer periods.
The FDA also asked for more data on sunscreen-containing wipes, powders, body washes, and shampoos.
Finally, there may be some controversy down the road when the agency takes a closer look at the safety of ingredients in sun protection products. The Washington-based Environmental Working Group has criticized the safety of some of those ingredients – in particular oxybenzone and retinyl palmitate – and did so again last year in its annual review of sunscreens.
The American Academy of Dermatology refuted the group, saying that there is no evidence that these ingredients are dangerous. The AAD backs the use of a water-resistant, broad-spectrum sunscreen that protects against UVA and UVB radiation, with an SPF 30 or higher, in conjunction with limiting sun exposure and wearing sun-protective clothing.
Dr. Wang agrees that oxybenzone and retinyl palmitate appear to be safe, but he says that some manufacturers have been removing the vitamin A derivative because of the bad publicity. Oxybenzone also may be removed as newer UVA blockers are approved, he said. "But right now, we don’t have any other alternatives," he noted.
For help selecting and using sunscreens effectively, click here.
Dr. Wang disclosed that he is a consultant for L’Oreal, and that he has collaborated with researchers at Procter & Gamble, but has not received any compensation from that company.
On Twitter @aliciaault
Sunscreens that have proven their protective ability and feature updated, more-consumer-friendly labeling are hitting store shelves, but they currently share space with older products that may not have passed muster with the Food and Drug Administration.
This mix of old and new packaging coincides with an FDA announcement that, later this year, it will review sunscreen ingredient safety and the potential approval of additional UVA-blocking agents.
In January, the agency issued its semiannual agenda for the coming year. That list included two sunscreen-related items.
The FDA said it would issue an "advance notice of proposed rulemaking" in July on how it will address sunscreen ingredient safety, which is the first step in a three-step process that culminates in a final rule.
The agency also said it would take a similar early step in the regulatory process for new ingredients manufacturers would like to add to their products.
At least six additional UVA filters are awaiting FDA approval, said Dr. Steven Q. Wang, director of dermatologic surgery and dermatology at the Memorial Sloan-Kettering Cancer Center, Basking Ridge, N.J. Currently, only two UVA-blocking agents – avobenzone and zinc oxide – are approved in the United States, but many others are available in Europe and elsewhere around the world.
Dr. Wang said he is looking forward to progress on UVA blockers; he noted that although both UVA and UVB contribute to skin cancer development, UVA penetrates deeper into the skin, contributes to more DNA damage, and plays a larger role in skin aging. A study of sunscreens from 1997 to 2009 by Dr. Wang showed that increasing numbers of products contained either avobenzone or zinc oxide, matching their claims of UVA protection.
In the late 1990s, 81% of the products surveyed claimed to protect against UVA, but only 5% actually contained a UVA blocker. By 2009, 80% of the products still made the claim, and 70% contained UVA-blocking agents. The study was published in the January issue of the journal Photochemical & Photobiological Sciences (Photochem. Photobiol. Sci. 2013;12:197-202).
Based on these findings, many of the products on the market in the past decade already met the FDA’s new criteria – announced in June 2011 – to claim protection against skin cancer, Dr. Wang said. And, clinicians and consumers should be reassured that products that meet the FDA labeling rules are effective and safe, he added.
Because they have already met the FDA’s effectiveness criteria, most products have not needed to be reformulated, said Farah Ahmed, chair of the sunscreen task force at the Personal Care Products Council.
But manufacturers have relabeled products to conform to the FDA’s rules, she said. The Council estimates that at least 4,500 products marketed in the United States claim an SPF, which subjects them to the FDA sunscreen rules. The product list includes not only sunscreens but lip balms, daily moisturizers, makeup, and any other product that contains a sunscreen component.
Products that have proved through testing that they protect against UVA and UVB radiation can claim that they are "broad spectrum" and will be labeled as SPF 15 or higher. The label also will be able to claim that the product can protect against sunburn, and, if used as directed with other sun protection measures, can reduce the risk of skin cancer and early skin aging.
Any product not labeled as "broad spectrum" or that has an SPF value between 2 and 14 will carry a warning: "Skin Cancer/Skin Aging Alert: Spending time in the sun increases your risk of skin cancer and early skin aging. This product has been shown only to help prevent sunburn, not skin cancer or early skin aging."
Under the revised labeling, no product can claim to be waterproof or sweatproof. If a product claims to be water resistant, the product’s label must state how long a user "can expect to get the declared SPF level of protection while swimming or sweating, based on standard testing," according to the FDA.
For more information, visit the agency’s website.
There may still be products on store shelves that have the old labeling, said Ms. Ahmed. That’s because the FDA has allowed a phase-in. Retailers also can choose to sell remaining stocks of the old products or remove them. "I think we’ll continue to see a mix of both products on the shelves," said Ms. Ahmed.
The situation creates the potential for confusion among consumers, although the FDA rules were meant to create a uniform label to help increase sun protection knowledge and the use of sun protection products.
Dr. Wang says he is telling patients to look for products that are labeled "broad spectrum" on the front, which is the best indicator that they are newly labeled and in compliance with FDA rules.
The FDA has been criticized for years for not finalizing the "monograph" – the accepted criteria or recipe – for sunscreen products. Although a final monograph is nowhere in sight, Dr. Wang said that he thought the agency had "done a reasonable job" in setting the cutoff point for products that could claim UVA protection against cancer at the accepted wavelength of 370 nm.
The FDA also plans to examine whether products labeled with an SPF greater than 50 provide any better protection than an SPF 50 sunscreen. The agency proposed in June 2011 that sunscreens with an SPF greater than 50 be labeled "SPF 50-plus," but nothing further has been issued. For now, consumers will continue to see sunscreens labeled as SPF 70, 80, or even 100.
There has been some difference of opinion on whether higher-SPF products are more beneficial. Dr. Wang said he recommends an SPF 30 product for daily use, but suggests higher SPFs for recreational activities that put users in the sun for longer periods.
The FDA also asked for more data on sunscreen-containing wipes, powders, body washes, and shampoos.
Finally, there may be some controversy down the road when the agency takes a closer look at the safety of ingredients in sun protection products. The Washington-based Environmental Working Group has criticized the safety of some of those ingredients – in particular oxybenzone and retinyl palmitate – and did so again last year in its annual review of sunscreens.
The American Academy of Dermatology refuted the group, saying that there is no evidence that these ingredients are dangerous. The AAD backs the use of a water-resistant, broad-spectrum sunscreen that protects against UVA and UVB radiation, with an SPF 30 or higher, in conjunction with limiting sun exposure and wearing sun-protective clothing.
Dr. Wang agrees that oxybenzone and retinyl palmitate appear to be safe, but he says that some manufacturers have been removing the vitamin A derivative because of the bad publicity. Oxybenzone also may be removed as newer UVA blockers are approved, he said. "But right now, we don’t have any other alternatives," he noted.
For help selecting and using sunscreens effectively, click here.
Dr. Wang disclosed that he is a consultant for L’Oreal, and that he has collaborated with researchers at Procter & Gamble, but has not received any compensation from that company.
On Twitter @aliciaault
Physician spending a top driver of health costs in 2011
WASHINGTON – Spending on physician and clinical services was the second biggest driver of the increase in health costs in 2011, according to the Centers for Medicare and Medicaid Services.
The nation spent $2.7 trillion on health care in 2011, or about $8,600 per person, according to an annual tally by CMS economists published Jan. 7 in the journal Health Affairs (2013;32:87-99).
The Affordable Care Act (ACA) had only a minimal impact on health spending in 2011, mainly because most of the provisions do not go into effect until 2014, according to the CMS officials.
Slightly more than 70% of the nation’s health bill is paid for by some form of insurance – 33% by private insurance, 21% by Medicare, and 15% by Medicaid, with the remainder paid by other programs.
Health spending has stayed relatively stable over the last 3 years, rising 3.9% in each of the years 2009, 2010, and 2011, which are historically low numbers. Health care also has consumed a similar share of the nation’s gross domestic product (18%) each year for the past few years.
Despite the stability, spending grew in certain areas, indicating that the nation could be poised for a rebound in spending growth. In particular, spending on prescription drugs and physician and clinical services grew faster than in previous years. But it’s not all bad news, according to Rick Foster, chief actuary for the CMS.
"There’s a growing amount of evidence that health care providers are getting it – getting that the future can’t be the same as the past – that the future will have to involve greater efforts for efficiency," Mr. Foster said at a briefing called by the CMS to discuss the analysis. He added that eventually, these efficiencies could offset other factors contributing to the growth in health spending.
Physician and clinical services are considered a single spending category by the CMS. Clinical services include outpatient care centers, freestanding ambulatory surgical centers, and medical and diagnostic labs.
In 2011, private and public payers spent $541 billion on physician and clinical services, accounting for 21% of the total $2.7 trillion health bill. Private health insurers covered 46% of the bill and Medicare paid 23%. Overall, there was a 4.3% increase in the growth of physician and clinical spending in 2011, which is still lower than the growth from 2002 to 2008. Physician spending, which accounts for 80% of the category, grew 3.6%, up from 2.8% the previous year.
The increase in growth was primarily driven by the complexity of services, said Micah Hartman, a statistician in the CMS Office of the Actuary, and the lead author of the report.
Physician and clinical spending also helped to drive an increase in Medicare spending, also due to increased complexity of care. But costs also went up as beneficiaries took advantage of free preventive services offered under the ACA, Mr. Hartman said.
Physician and clinical spending grew 7.6% in 2011, after 2 years of unusually slow growth. Overall, Medicare spent $554 billion in 2011. Seventy-five percent of that was spent on fee-for-service care; the remainder was spent for the Medicare Advantage program.
Medicaid spending shifted considerably in 2011.
Back in 2009, Medicaid saw a recession-related jump in enrollment. Federal legislation at the time increased the federal share of spending, cushioning the states from costs associated with the swell in enrollment. But by mid-2011, that increased federal match expired. As a result, the federal government’s Medicaid tab dropped by 7%, while the state share increased by 22%. Overall, states spent $29 billion more in 2011, even as they curbed benefits, restricted eligibility, and cut back on reimbursement rates, said Anne B. Martin, an economist in the CMS Office of the Actuary.
Another area where the health reform law may have had an impact was Medicare prescription drug spending. In 2011, Medicare beneficiaries spent less out of pocket because those who hit a spending level called the donut hole received a 50% discount on all additional brand name drugs.
That new benefit helped drive the growth of prescription drug spending to about 3%, compared to 0.4% in 2010.
Patients also shouldered a heavy load for those prescriptions and for other medical services. Out-of-pocket spending grew 3% in 2011, to $307 billion, accounting for 11% of total health spending. The increase was slightly more than in 2009-to-2010, but less than in the previous decade.
Patients spent more out-of-pocket in part because they are being asked to pay more by employer-sponsored plans and because increasingly, they are electing coverage through high-deductible health plans, also known as consumer-directed plans. Enrollment has grown by 20% a year the last few years; currently about 17% of insured Americans are in such plans, Mr. Hartman said.
In theory, the high-deductible plans make patients more cost-conscious. But their impact is not clear, Mr. Foster said. "The evidence is mixed to date as to how well these plans are working," he said, adding that costs are lower, but it’s unclear if that’s because the incentives are working or because healthier people are using the plans.
WASHINGTON – Spending on physician and clinical services was the second biggest driver of the increase in health costs in 2011, according to the Centers for Medicare and Medicaid Services.
The nation spent $2.7 trillion on health care in 2011, or about $8,600 per person, according to an annual tally by CMS economists published Jan. 7 in the journal Health Affairs (2013;32:87-99).
The Affordable Care Act (ACA) had only a minimal impact on health spending in 2011, mainly because most of the provisions do not go into effect until 2014, according to the CMS officials.
Slightly more than 70% of the nation’s health bill is paid for by some form of insurance – 33% by private insurance, 21% by Medicare, and 15% by Medicaid, with the remainder paid by other programs.
Health spending has stayed relatively stable over the last 3 years, rising 3.9% in each of the years 2009, 2010, and 2011, which are historically low numbers. Health care also has consumed a similar share of the nation’s gross domestic product (18%) each year for the past few years.
Despite the stability, spending grew in certain areas, indicating that the nation could be poised for a rebound in spending growth. In particular, spending on prescription drugs and physician and clinical services grew faster than in previous years. But it’s not all bad news, according to Rick Foster, chief actuary for the CMS.
"There’s a growing amount of evidence that health care providers are getting it – getting that the future can’t be the same as the past – that the future will have to involve greater efforts for efficiency," Mr. Foster said at a briefing called by the CMS to discuss the analysis. He added that eventually, these efficiencies could offset other factors contributing to the growth in health spending.
Physician and clinical services are considered a single spending category by the CMS. Clinical services include outpatient care centers, freestanding ambulatory surgical centers, and medical and diagnostic labs.
In 2011, private and public payers spent $541 billion on physician and clinical services, accounting for 21% of the total $2.7 trillion health bill. Private health insurers covered 46% of the bill and Medicare paid 23%. Overall, there was a 4.3% increase in the growth of physician and clinical spending in 2011, which is still lower than the growth from 2002 to 2008. Physician spending, which accounts for 80% of the category, grew 3.6%, up from 2.8% the previous year.
The increase in growth was primarily driven by the complexity of services, said Micah Hartman, a statistician in the CMS Office of the Actuary, and the lead author of the report.
Physician and clinical spending also helped to drive an increase in Medicare spending, also due to increased complexity of care. But costs also went up as beneficiaries took advantage of free preventive services offered under the ACA, Mr. Hartman said.
Physician and clinical spending grew 7.6% in 2011, after 2 years of unusually slow growth. Overall, Medicare spent $554 billion in 2011. Seventy-five percent of that was spent on fee-for-service care; the remainder was spent for the Medicare Advantage program.
Medicaid spending shifted considerably in 2011.
Back in 2009, Medicaid saw a recession-related jump in enrollment. Federal legislation at the time increased the federal share of spending, cushioning the states from costs associated with the swell in enrollment. But by mid-2011, that increased federal match expired. As a result, the federal government’s Medicaid tab dropped by 7%, while the state share increased by 22%. Overall, states spent $29 billion more in 2011, even as they curbed benefits, restricted eligibility, and cut back on reimbursement rates, said Anne B. Martin, an economist in the CMS Office of the Actuary.
Another area where the health reform law may have had an impact was Medicare prescription drug spending. In 2011, Medicare beneficiaries spent less out of pocket because those who hit a spending level called the donut hole received a 50% discount on all additional brand name drugs.
That new benefit helped drive the growth of prescription drug spending to about 3%, compared to 0.4% in 2010.
Patients also shouldered a heavy load for those prescriptions and for other medical services. Out-of-pocket spending grew 3% in 2011, to $307 billion, accounting for 11% of total health spending. The increase was slightly more than in 2009-to-2010, but less than in the previous decade.
Patients spent more out-of-pocket in part because they are being asked to pay more by employer-sponsored plans and because increasingly, they are electing coverage through high-deductible health plans, also known as consumer-directed plans. Enrollment has grown by 20% a year the last few years; currently about 17% of insured Americans are in such plans, Mr. Hartman said.
In theory, the high-deductible plans make patients more cost-conscious. But their impact is not clear, Mr. Foster said. "The evidence is mixed to date as to how well these plans are working," he said, adding that costs are lower, but it’s unclear if that’s because the incentives are working or because healthier people are using the plans.
WASHINGTON – Spending on physician and clinical services was the second biggest driver of the increase in health costs in 2011, according to the Centers for Medicare and Medicaid Services.
The nation spent $2.7 trillion on health care in 2011, or about $8,600 per person, according to an annual tally by CMS economists published Jan. 7 in the journal Health Affairs (2013;32:87-99).
The Affordable Care Act (ACA) had only a minimal impact on health spending in 2011, mainly because most of the provisions do not go into effect until 2014, according to the CMS officials.
Slightly more than 70% of the nation’s health bill is paid for by some form of insurance – 33% by private insurance, 21% by Medicare, and 15% by Medicaid, with the remainder paid by other programs.
Health spending has stayed relatively stable over the last 3 years, rising 3.9% in each of the years 2009, 2010, and 2011, which are historically low numbers. Health care also has consumed a similar share of the nation’s gross domestic product (18%) each year for the past few years.
Despite the stability, spending grew in certain areas, indicating that the nation could be poised for a rebound in spending growth. In particular, spending on prescription drugs and physician and clinical services grew faster than in previous years. But it’s not all bad news, according to Rick Foster, chief actuary for the CMS.
"There’s a growing amount of evidence that health care providers are getting it – getting that the future can’t be the same as the past – that the future will have to involve greater efforts for efficiency," Mr. Foster said at a briefing called by the CMS to discuss the analysis. He added that eventually, these efficiencies could offset other factors contributing to the growth in health spending.
Physician and clinical services are considered a single spending category by the CMS. Clinical services include outpatient care centers, freestanding ambulatory surgical centers, and medical and diagnostic labs.
In 2011, private and public payers spent $541 billion on physician and clinical services, accounting for 21% of the total $2.7 trillion health bill. Private health insurers covered 46% of the bill and Medicare paid 23%. Overall, there was a 4.3% increase in the growth of physician and clinical spending in 2011, which is still lower than the growth from 2002 to 2008. Physician spending, which accounts for 80% of the category, grew 3.6%, up from 2.8% the previous year.
The increase in growth was primarily driven by the complexity of services, said Micah Hartman, a statistician in the CMS Office of the Actuary, and the lead author of the report.
Physician and clinical spending also helped to drive an increase in Medicare spending, also due to increased complexity of care. But costs also went up as beneficiaries took advantage of free preventive services offered under the ACA, Mr. Hartman said.
Physician and clinical spending grew 7.6% in 2011, after 2 years of unusually slow growth. Overall, Medicare spent $554 billion in 2011. Seventy-five percent of that was spent on fee-for-service care; the remainder was spent for the Medicare Advantage program.
Medicaid spending shifted considerably in 2011.
Back in 2009, Medicaid saw a recession-related jump in enrollment. Federal legislation at the time increased the federal share of spending, cushioning the states from costs associated with the swell in enrollment. But by mid-2011, that increased federal match expired. As a result, the federal government’s Medicaid tab dropped by 7%, while the state share increased by 22%. Overall, states spent $29 billion more in 2011, even as they curbed benefits, restricted eligibility, and cut back on reimbursement rates, said Anne B. Martin, an economist in the CMS Office of the Actuary.
Another area where the health reform law may have had an impact was Medicare prescription drug spending. In 2011, Medicare beneficiaries spent less out of pocket because those who hit a spending level called the donut hole received a 50% discount on all additional brand name drugs.
That new benefit helped drive the growth of prescription drug spending to about 3%, compared to 0.4% in 2010.
Patients also shouldered a heavy load for those prescriptions and for other medical services. Out-of-pocket spending grew 3% in 2011, to $307 billion, accounting for 11% of total health spending. The increase was slightly more than in 2009-to-2010, but less than in the previous decade.
Patients spent more out-of-pocket in part because they are being asked to pay more by employer-sponsored plans and because increasingly, they are electing coverage through high-deductible health plans, also known as consumer-directed plans. Enrollment has grown by 20% a year the last few years; currently about 17% of insured Americans are in such plans, Mr. Hartman said.
In theory, the high-deductible plans make patients more cost-conscious. But their impact is not clear, Mr. Foster said. "The evidence is mixed to date as to how well these plans are working," he said, adding that costs are lower, but it’s unclear if that’s because the incentives are working or because healthier people are using the plans.
AT A BRIEFING CALLED BY THE CENTERS FOR MEDICARE AND MEDICAID SERVICES
Higher costs for internists, better preventive care?
NEW ORLEANS – The cost of care may be more expensive at an internist’s office, but it appears that internists may do a better job than family physicians in offering preventive care services such as flu shots and cancer screenings.
That’s according to an observational study of some 30,000 adults who had an internist, family physician, or specialist as their usual source of care.
Dr. Joshua J. Fenton of the department of family and community medicine at the University of California, Davis, and his colleagues analyzed data from the Medical Expenditures Panel Survey from 2000 to 2008 and selected adults who responded that they had one of those physicians as a usual source of care in the previous year. Surgeons and ob.gyns were excluded because the authors wanted to study prostate cancer screening, in addition to other outcomes.
Previous research has consistently shown that internists and specialists have higher costs than family physicians, but there have been few data showing whether those higher costs are justified through the delivery of better care – specifically, better preventive care. The authors hypothesized that preventive care delivery would be similar across the three physician groups, Dr. Fenton said at the annual meeting of the North American Primary Care Research Group.
Of the 29,503 adults who were selected, 73% had a family physician as their usual source of care, 23% had an internist, and 4% a specialist. Those who received their care from an internist or specialist were slightly older, had a greater illness burden, had a higher income, and were more likely to live in urban areas, he said.
On an unadjusted basis, the annual care expenditures were $4,682 for those seeing an FP, $6,356 for an internist, and $9,147 for specialist. After adjusting for a variety of factors, including use of care in the previous year, the cost for internists was 10% more and for specialists was 33% more than the cost for family physicians.
People seeing an internist had significantly increased odds of receiving a flu shot in the study year, when compared with a family physician. The odds of getting a shot with a specialist were similar to those with a family physician.
For mammograms – 11,806 women had one during the study year – those with an internist were slightly more likely to get the screen. About 82% of those seeing an internist had a mammogram, compared with 79% of those seeing a family physician and 78% of those seeing a specialist. Pap smear screening rates were similar across the three physician groups, with about 82% getting the test.
Some 15,000 patients had an up-to-date colorectal screen – defined as a fecal occult test within the prior year or lower endoscopy within the previous 5 years. Rates were highest for internists, at 53%, compared with 48% of those seeing a family physician and 44% of those using a specialist.
Patients seeing an internist also had significantly increased odds of having a prostate-specific antigen test.
The study was limited by its cross-sectional and observational design, said Dr. Fenton, who also noted that it’s possible that some preventive care may have been delivered by providers other than the usual source of care.
The finding that internists delivered more preventive services, however, "raises some questions about cost-effectiveness and value," he said.
Dr. Fenton reported no conflicts.
NEW ORLEANS – The cost of care may be more expensive at an internist’s office, but it appears that internists may do a better job than family physicians in offering preventive care services such as flu shots and cancer screenings.
That’s according to an observational study of some 30,000 adults who had an internist, family physician, or specialist as their usual source of care.
Dr. Joshua J. Fenton of the department of family and community medicine at the University of California, Davis, and his colleagues analyzed data from the Medical Expenditures Panel Survey from 2000 to 2008 and selected adults who responded that they had one of those physicians as a usual source of care in the previous year. Surgeons and ob.gyns were excluded because the authors wanted to study prostate cancer screening, in addition to other outcomes.
Previous research has consistently shown that internists and specialists have higher costs than family physicians, but there have been few data showing whether those higher costs are justified through the delivery of better care – specifically, better preventive care. The authors hypothesized that preventive care delivery would be similar across the three physician groups, Dr. Fenton said at the annual meeting of the North American Primary Care Research Group.
Of the 29,503 adults who were selected, 73% had a family physician as their usual source of care, 23% had an internist, and 4% a specialist. Those who received their care from an internist or specialist were slightly older, had a greater illness burden, had a higher income, and were more likely to live in urban areas, he said.
On an unadjusted basis, the annual care expenditures were $4,682 for those seeing an FP, $6,356 for an internist, and $9,147 for specialist. After adjusting for a variety of factors, including use of care in the previous year, the cost for internists was 10% more and for specialists was 33% more than the cost for family physicians.
People seeing an internist had significantly increased odds of receiving a flu shot in the study year, when compared with a family physician. The odds of getting a shot with a specialist were similar to those with a family physician.
For mammograms – 11,806 women had one during the study year – those with an internist were slightly more likely to get the screen. About 82% of those seeing an internist had a mammogram, compared with 79% of those seeing a family physician and 78% of those seeing a specialist. Pap smear screening rates were similar across the three physician groups, with about 82% getting the test.
Some 15,000 patients had an up-to-date colorectal screen – defined as a fecal occult test within the prior year or lower endoscopy within the previous 5 years. Rates were highest for internists, at 53%, compared with 48% of those seeing a family physician and 44% of those using a specialist.
Patients seeing an internist also had significantly increased odds of having a prostate-specific antigen test.
The study was limited by its cross-sectional and observational design, said Dr. Fenton, who also noted that it’s possible that some preventive care may have been delivered by providers other than the usual source of care.
The finding that internists delivered more preventive services, however, "raises some questions about cost-effectiveness and value," he said.
Dr. Fenton reported no conflicts.
NEW ORLEANS – The cost of care may be more expensive at an internist’s office, but it appears that internists may do a better job than family physicians in offering preventive care services such as flu shots and cancer screenings.
That’s according to an observational study of some 30,000 adults who had an internist, family physician, or specialist as their usual source of care.
Dr. Joshua J. Fenton of the department of family and community medicine at the University of California, Davis, and his colleagues analyzed data from the Medical Expenditures Panel Survey from 2000 to 2008 and selected adults who responded that they had one of those physicians as a usual source of care in the previous year. Surgeons and ob.gyns were excluded because the authors wanted to study prostate cancer screening, in addition to other outcomes.
Previous research has consistently shown that internists and specialists have higher costs than family physicians, but there have been few data showing whether those higher costs are justified through the delivery of better care – specifically, better preventive care. The authors hypothesized that preventive care delivery would be similar across the three physician groups, Dr. Fenton said at the annual meeting of the North American Primary Care Research Group.
Of the 29,503 adults who were selected, 73% had a family physician as their usual source of care, 23% had an internist, and 4% a specialist. Those who received their care from an internist or specialist were slightly older, had a greater illness burden, had a higher income, and were more likely to live in urban areas, he said.
On an unadjusted basis, the annual care expenditures were $4,682 for those seeing an FP, $6,356 for an internist, and $9,147 for specialist. After adjusting for a variety of factors, including use of care in the previous year, the cost for internists was 10% more and for specialists was 33% more than the cost for family physicians.
People seeing an internist had significantly increased odds of receiving a flu shot in the study year, when compared with a family physician. The odds of getting a shot with a specialist were similar to those with a family physician.
For mammograms – 11,806 women had one during the study year – those with an internist were slightly more likely to get the screen. About 82% of those seeing an internist had a mammogram, compared with 79% of those seeing a family physician and 78% of those seeing a specialist. Pap smear screening rates were similar across the three physician groups, with about 82% getting the test.
Some 15,000 patients had an up-to-date colorectal screen – defined as a fecal occult test within the prior year or lower endoscopy within the previous 5 years. Rates were highest for internists, at 53%, compared with 48% of those seeing a family physician and 44% of those using a specialist.
Patients seeing an internist also had significantly increased odds of having a prostate-specific antigen test.
The study was limited by its cross-sectional and observational design, said Dr. Fenton, who also noted that it’s possible that some preventive care may have been delivered by providers other than the usual source of care.
The finding that internists delivered more preventive services, however, "raises some questions about cost-effectiveness and value," he said.
Dr. Fenton reported no conflicts.
AT THE ANNUAL MEETING OF THE NORTH AMERICAN PRIMARY CARE RESEARCH GROUP
Major Finding: Internists delivered more preventive care than family physicians, but costs overall were 10% greater.
Data Source: A cross-sectional study of adults responding to the Medical Expenditures Panel Survey from 2000 to 2008 who had a family physician, internist, or specialist as a usual source of care.
Disclosures: Dr. Fenton reported no conflicts.
FDA approves teduglutide for short bowel syndrome
The Food and Drug Administration on Dec. 21 approved teduglutide, to be marketed under the trade name Gattex, to treat adults with short bowel syndrome (SBS) who need parenteral nutrition.
Teduglutide, a recombinant analogue of human glucagon-like peptide-2 (GLP-2), was unanimously recommended for approval by an FDA advisory panel in October. It is a once-daily subcutaneous injection that helps improve intestinal absorption of fluids and nutrients, reducing the frequency and volume of parenteral nutrition.
"Considering Gattex has been shown to significantly reduce or in some cases even eliminate the requirement for parenteral support, it may become a cornerstone therapy in the management of short bowel syndrome." Dr. Ken Fujioka of the Nutrition and Metabolic Research Center, Scripps Clinic, Del Mar, Calif., said in a statement issued by Gattex’s maker, NPA Pharmaceuticals.
It is the third drug to be approved by the FDA for SBS patients who are dependent on parenteral nutrition. Somatropin (Zorbtive) was approved in 2003 and glutamine (Nutrestore) in 2004.
"Today’s approval expands the available treatment options for patients with this life-threatening condition," Dr. Victoria Kusiak, deputy director of the Office of Drug Evaluation III in the FDA Center for Drug Evaluation and Research, said in a statement. "Because Gattex may cause other serious health conditions, it is critical that patients and health care professionals understand the drug’s potential and known safety risks."
Teduglutide therapy increases the risk of developing cancer and polyps in the intestine, obstructions in the intestine, gallbladder disease, biliary tract disease, and pancreatic disease. The drug will have a Risk Evaluation and Mitigation Strategy, consisting of a communication plan and training for prescribers, according to the FDA.
Pivotal data on the drug were published in September in Gastroenterology (Gastroenterology 2012 Sept. 13 [doi:10.1053/j.gastro.2012.09.007]).
The Food and Drug Administration on Dec. 21 approved teduglutide, to be marketed under the trade name Gattex, to treat adults with short bowel syndrome (SBS) who need parenteral nutrition.
Teduglutide, a recombinant analogue of human glucagon-like peptide-2 (GLP-2), was unanimously recommended for approval by an FDA advisory panel in October. It is a once-daily subcutaneous injection that helps improve intestinal absorption of fluids and nutrients, reducing the frequency and volume of parenteral nutrition.
"Considering Gattex has been shown to significantly reduce or in some cases even eliminate the requirement for parenteral support, it may become a cornerstone therapy in the management of short bowel syndrome." Dr. Ken Fujioka of the Nutrition and Metabolic Research Center, Scripps Clinic, Del Mar, Calif., said in a statement issued by Gattex’s maker, NPA Pharmaceuticals.
It is the third drug to be approved by the FDA for SBS patients who are dependent on parenteral nutrition. Somatropin (Zorbtive) was approved in 2003 and glutamine (Nutrestore) in 2004.
"Today’s approval expands the available treatment options for patients with this life-threatening condition," Dr. Victoria Kusiak, deputy director of the Office of Drug Evaluation III in the FDA Center for Drug Evaluation and Research, said in a statement. "Because Gattex may cause other serious health conditions, it is critical that patients and health care professionals understand the drug’s potential and known safety risks."
Teduglutide therapy increases the risk of developing cancer and polyps in the intestine, obstructions in the intestine, gallbladder disease, biliary tract disease, and pancreatic disease. The drug will have a Risk Evaluation and Mitigation Strategy, consisting of a communication plan and training for prescribers, according to the FDA.
Pivotal data on the drug were published in September in Gastroenterology (Gastroenterology 2012 Sept. 13 [doi:10.1053/j.gastro.2012.09.007]).
The Food and Drug Administration on Dec. 21 approved teduglutide, to be marketed under the trade name Gattex, to treat adults with short bowel syndrome (SBS) who need parenteral nutrition.
Teduglutide, a recombinant analogue of human glucagon-like peptide-2 (GLP-2), was unanimously recommended for approval by an FDA advisory panel in October. It is a once-daily subcutaneous injection that helps improve intestinal absorption of fluids and nutrients, reducing the frequency and volume of parenteral nutrition.
"Considering Gattex has been shown to significantly reduce or in some cases even eliminate the requirement for parenteral support, it may become a cornerstone therapy in the management of short bowel syndrome." Dr. Ken Fujioka of the Nutrition and Metabolic Research Center, Scripps Clinic, Del Mar, Calif., said in a statement issued by Gattex’s maker, NPA Pharmaceuticals.
It is the third drug to be approved by the FDA for SBS patients who are dependent on parenteral nutrition. Somatropin (Zorbtive) was approved in 2003 and glutamine (Nutrestore) in 2004.
"Today’s approval expands the available treatment options for patients with this life-threatening condition," Dr. Victoria Kusiak, deputy director of the Office of Drug Evaluation III in the FDA Center for Drug Evaluation and Research, said in a statement. "Because Gattex may cause other serious health conditions, it is critical that patients and health care professionals understand the drug’s potential and known safety risks."
Teduglutide therapy increases the risk of developing cancer and polyps in the intestine, obstructions in the intestine, gallbladder disease, biliary tract disease, and pancreatic disease. The drug will have a Risk Evaluation and Mitigation Strategy, consisting of a communication plan and training for prescribers, according to the FDA.
Pivotal data on the drug were published in September in Gastroenterology (Gastroenterology 2012 Sept. 13 [doi:10.1053/j.gastro.2012.09.007]).
Marijuana most popular drug of abuse among teens
WASHINGTON – Marijuana remains popular with U.S. teenagers, with steady and even rising rates of use, according to a key federal survey.
This year’s data from the annual Monitoring the Future survey found that marijuana was the No. 1 drug used by students in the 8th, 10th, and 12th grades. About 35% of high school seniors said they smoked pot in the past year, consistent with 2011 usage. Daily use among seniors also stayed flat, at around 7%.
Of concern is the declining number of seniors who view marijuana use as risky. Only 20% of seniors said occasional use was harmful, the lowest rate recorded since 1983. Higher numbers of 8th and 10th graders consider pot smoking to be risky, but those figures declined as well.
Dr. Nora D. Volkow, director of the National Institute on Drug Abuse, said that teen perception of harm might be decreasing in part because of the ongoing debate over legalized medical marijuana and recent state efforts that decriminalized recreational use.
Previous NIDA studies have shown that teens believe that anything used for medicinal purposes – such as prescription painkillers – are inherently less dangerous. Also, many teens will not use drugs because they are illegal. Without laws prohibiting use, "that deterrent is not present," Dr. Volkow said at a press conference called by NIDA.
But marijuana is not harmless, Dr. Volkow noted. A study published earlier this year found that heavy marijuana use in the teen years contributed to lower IQs and impaired mental abilities (Proc. Natl. Acad. Sci. USA 2012;109:E2657-64 [doi:10.1073/pnas.1206820109]).
"We are increasingly concerned that regular or daily use of marijuana is robbing many young people of their potential to achieve and excel in school or other aspects of life," she said.
Synthetic marijuana, also known as spice or K-2, was the second most popular drug among high school seniors, with 11% reporting they had used it in the past year. A little more than 4% of 8th graders said they’d used the substance.
Dr. Volkow cautioned that synthetic cannabinoids were just as dangerous as is the plant form, and possibly more so, given that the active drug could be concentrated. Many ingredients that can be found in synthetic marijuana have been banned by the Drug Enforcement Administration.
Prescription drug abuse continues to be of concern. Among seniors, Adderall was the third most used drug. About 8% said they had used the prescription stimulant in the previous year, often for a nonmedical use. Vicodin was close behind, with 7.5% of seniors having used it within the past year. The majority of 12th graders (68%) said they were given the prescription medications by friends or relatives; 38% said they had bought the drug from friends or relatives, about a third said they had gotten it by prescription, and 22% said they took it from friends or relatives.
So called "bath salts" were included in the Monitoring the Future survey this year for the first time. "Bath salts" is the street name for a group of designer amphetamine-like stimulants that are sold over the counter. Only 1.3% of seniors reported using the products, a relatively low rate that may reflect heavy publicity about their dangers, Gil Kerlikowske, director of the White House Office of National Drug Control Policy, said at the briefing.
The survey also showed that both tobacco and alcohol use have declined significantly over the years. Alcohol use is at its lowest since the survey began in 1975. About 70% of high school seniors said they’d ever used alcohol, down from a peak of 90%.
For tobacco, there were significant declines in lifetime use among 8th graders: 16% in 2012 compared with a peak of 50% in 1996. For 10th graders, 28% said they had ever smoked tobacco, down from a peak of 61% in 1996. Rates of use of smokeless tobacco and other tobacco products continued to stay steady.
"So as we look at these numbers and we look again in trying to determine what they tell us, I think they identify the areas where we need to pay attention and don’t become complacent," Dr. Volkow said.
More than 45,000 students from 395 public and private schools took part in the Monitoring the Future survey this year. Since 1975, the survey has measured the drug, alcohol, and cigarette use and related attitudes of U.S. high school seniors; 8th and 10th graders were added to the survey in 1991. The survey is funded by NIDA and conducted by University of Michigan investigators led by Lloyd Johnston, Ph.D.
WASHINGTON – Marijuana remains popular with U.S. teenagers, with steady and even rising rates of use, according to a key federal survey.
This year’s data from the annual Monitoring the Future survey found that marijuana was the No. 1 drug used by students in the 8th, 10th, and 12th grades. About 35% of high school seniors said they smoked pot in the past year, consistent with 2011 usage. Daily use among seniors also stayed flat, at around 7%.
Of concern is the declining number of seniors who view marijuana use as risky. Only 20% of seniors said occasional use was harmful, the lowest rate recorded since 1983. Higher numbers of 8th and 10th graders consider pot smoking to be risky, but those figures declined as well.
Dr. Nora D. Volkow, director of the National Institute on Drug Abuse, said that teen perception of harm might be decreasing in part because of the ongoing debate over legalized medical marijuana and recent state efforts that decriminalized recreational use.
Previous NIDA studies have shown that teens believe that anything used for medicinal purposes – such as prescription painkillers – are inherently less dangerous. Also, many teens will not use drugs because they are illegal. Without laws prohibiting use, "that deterrent is not present," Dr. Volkow said at a press conference called by NIDA.
But marijuana is not harmless, Dr. Volkow noted. A study published earlier this year found that heavy marijuana use in the teen years contributed to lower IQs and impaired mental abilities (Proc. Natl. Acad. Sci. USA 2012;109:E2657-64 [doi:10.1073/pnas.1206820109]).
"We are increasingly concerned that regular or daily use of marijuana is robbing many young people of their potential to achieve and excel in school or other aspects of life," she said.
Synthetic marijuana, also known as spice or K-2, was the second most popular drug among high school seniors, with 11% reporting they had used it in the past year. A little more than 4% of 8th graders said they’d used the substance.
Dr. Volkow cautioned that synthetic cannabinoids were just as dangerous as is the plant form, and possibly more so, given that the active drug could be concentrated. Many ingredients that can be found in synthetic marijuana have been banned by the Drug Enforcement Administration.
Prescription drug abuse continues to be of concern. Among seniors, Adderall was the third most used drug. About 8% said they had used the prescription stimulant in the previous year, often for a nonmedical use. Vicodin was close behind, with 7.5% of seniors having used it within the past year. The majority of 12th graders (68%) said they were given the prescription medications by friends or relatives; 38% said they had bought the drug from friends or relatives, about a third said they had gotten it by prescription, and 22% said they took it from friends or relatives.
So called "bath salts" were included in the Monitoring the Future survey this year for the first time. "Bath salts" is the street name for a group of designer amphetamine-like stimulants that are sold over the counter. Only 1.3% of seniors reported using the products, a relatively low rate that may reflect heavy publicity about their dangers, Gil Kerlikowske, director of the White House Office of National Drug Control Policy, said at the briefing.
The survey also showed that both tobacco and alcohol use have declined significantly over the years. Alcohol use is at its lowest since the survey began in 1975. About 70% of high school seniors said they’d ever used alcohol, down from a peak of 90%.
For tobacco, there were significant declines in lifetime use among 8th graders: 16% in 2012 compared with a peak of 50% in 1996. For 10th graders, 28% said they had ever smoked tobacco, down from a peak of 61% in 1996. Rates of use of smokeless tobacco and other tobacco products continued to stay steady.
"So as we look at these numbers and we look again in trying to determine what they tell us, I think they identify the areas where we need to pay attention and don’t become complacent," Dr. Volkow said.
More than 45,000 students from 395 public and private schools took part in the Monitoring the Future survey this year. Since 1975, the survey has measured the drug, alcohol, and cigarette use and related attitudes of U.S. high school seniors; 8th and 10th graders were added to the survey in 1991. The survey is funded by NIDA and conducted by University of Michigan investigators led by Lloyd Johnston, Ph.D.
WASHINGTON – Marijuana remains popular with U.S. teenagers, with steady and even rising rates of use, according to a key federal survey.
This year’s data from the annual Monitoring the Future survey found that marijuana was the No. 1 drug used by students in the 8th, 10th, and 12th grades. About 35% of high school seniors said they smoked pot in the past year, consistent with 2011 usage. Daily use among seniors also stayed flat, at around 7%.
Of concern is the declining number of seniors who view marijuana use as risky. Only 20% of seniors said occasional use was harmful, the lowest rate recorded since 1983. Higher numbers of 8th and 10th graders consider pot smoking to be risky, but those figures declined as well.
Dr. Nora D. Volkow, director of the National Institute on Drug Abuse, said that teen perception of harm might be decreasing in part because of the ongoing debate over legalized medical marijuana and recent state efforts that decriminalized recreational use.
Previous NIDA studies have shown that teens believe that anything used for medicinal purposes – such as prescription painkillers – are inherently less dangerous. Also, many teens will not use drugs because they are illegal. Without laws prohibiting use, "that deterrent is not present," Dr. Volkow said at a press conference called by NIDA.
But marijuana is not harmless, Dr. Volkow noted. A study published earlier this year found that heavy marijuana use in the teen years contributed to lower IQs and impaired mental abilities (Proc. Natl. Acad. Sci. USA 2012;109:E2657-64 [doi:10.1073/pnas.1206820109]).
"We are increasingly concerned that regular or daily use of marijuana is robbing many young people of their potential to achieve and excel in school or other aspects of life," she said.
Synthetic marijuana, also known as spice or K-2, was the second most popular drug among high school seniors, with 11% reporting they had used it in the past year. A little more than 4% of 8th graders said they’d used the substance.
Dr. Volkow cautioned that synthetic cannabinoids were just as dangerous as is the plant form, and possibly more so, given that the active drug could be concentrated. Many ingredients that can be found in synthetic marijuana have been banned by the Drug Enforcement Administration.
Prescription drug abuse continues to be of concern. Among seniors, Adderall was the third most used drug. About 8% said they had used the prescription stimulant in the previous year, often for a nonmedical use. Vicodin was close behind, with 7.5% of seniors having used it within the past year. The majority of 12th graders (68%) said they were given the prescription medications by friends or relatives; 38% said they had bought the drug from friends or relatives, about a third said they had gotten it by prescription, and 22% said they took it from friends or relatives.
So called "bath salts" were included in the Monitoring the Future survey this year for the first time. "Bath salts" is the street name for a group of designer amphetamine-like stimulants that are sold over the counter. Only 1.3% of seniors reported using the products, a relatively low rate that may reflect heavy publicity about their dangers, Gil Kerlikowske, director of the White House Office of National Drug Control Policy, said at the briefing.
The survey also showed that both tobacco and alcohol use have declined significantly over the years. Alcohol use is at its lowest since the survey began in 1975. About 70% of high school seniors said they’d ever used alcohol, down from a peak of 90%.
For tobacco, there were significant declines in lifetime use among 8th graders: 16% in 2012 compared with a peak of 50% in 1996. For 10th graders, 28% said they had ever smoked tobacco, down from a peak of 61% in 1996. Rates of use of smokeless tobacco and other tobacco products continued to stay steady.
"So as we look at these numbers and we look again in trying to determine what they tell us, I think they identify the areas where we need to pay attention and don’t become complacent," Dr. Volkow said.
More than 45,000 students from 395 public and private schools took part in the Monitoring the Future survey this year. Since 1975, the survey has measured the drug, alcohol, and cigarette use and related attitudes of U.S. high school seniors; 8th and 10th graders were added to the survey in 1991. The survey is funded by NIDA and conducted by University of Michigan investigators led by Lloyd Johnston, Ph.D.
AT A PRESS CONFERENCE CALLED BY THE NATIONAL INSTITUTE ON DRUG ABUSE
Major Finding: One in five high school seniors believe marijuana use is harmful.
Data Source: Monitoring the Future, a survey of 45,449 U.S. teens in the 8th, 10th, and 12th grades.
Disclosures: The study is funded by the National Institute on Drug Abuse.
How long should a cough last?
NEW ORLEANS – Patients tend to underestimate how long a cough should last, leading to unnecessary and inappropriate use of antibiotics, according to a review of the evidence and a survey of patient beliefs.
Cough is the third most frequent reason for physician office visits, and yet doctors and patients don’t seem to have an understanding of the natural history of cough and the expected duration, said Dr. Mark Ebell of the department of epidemiology at the University of Georgia College of Public Health in Athens.
The National Ambulatory Medical Survey in 2007 showed that there were 27 million outpatient visits for cough that year. That constitutes 2%-3% of all family practice visits, said Dr. Ebell. Half of patients received an antibiotic for their cough, and half the time, it was a broad spectrum antibiotic.
"There are some real issues with how we manage cough," said Dr. Ebell. Cough can indicate a condition that needs medical attention and a prescription therapy, but often, it is treated without evidence for antibiotics because the patient or doctor is uncomfortable with its duration.
Before patients ask their doctor how long a cough should last, they are likely to ask Google, he said. In conducting his own Google search, he found estimates ranging from 7 days to 14 days.
To get a sense of what patients think, Dr. Ebell and his colleagues surveyed Georgia residents by adding questions to the Georgia Poll, which is conducted twice a year by the Survey Research Center at the University of Georgia. Potential participants – aged 18 years or older – are randomly selected and contacted by phone. Almost 500 participated; 63% were women. It was an older population because the survey is conducted through landlines.
Participants were asked about their beliefs concerning antibiotics and the effectiveness of these drugs when the main symptom was a cough. They were asked how long they think it would take for the cough to get better if they were not taking any medicine, in six different scenarios: dry cough, coughing up yellow mucus or green mucus, or any of those kinds of cough with a slight fever, or no fever.
Patients with self-reported chronic lung disease or asthma were excluded from the survey.
Some respondents thought they would be better in as few as 2 days. Some thought the cough would last several months, but almost everyone thought it would take less than 2 weeks. There was not much difference between the scenarios, except when the scenario involved green phlegm.
The participants who had previously used antibiotics thought the cough would last longer, as did women, whites, and those with less education.
To determine how long a cough actually does last, Dr. Ebell conducted a literature search. After combing through several 100,000 potential studies, excluding those in sinusitis or people with a clear bacterial diagnosis, and focusing on those in community-dwelling, otherwise healthy adults with undifferentiated acute cough or bronchitis, he and his colleagues were left with 18 studies. In the end, only 5 of those 18 provided useful data.
The mean duration was 17-18 days. "So now we know how long a cough lasts," said Dr. Ebell.
Although the cough usually improves significantly in 2 weeks, most patients think it should be over in a week. "And that’s a big driver, or may be a big driver, of antibiotic use," he said. It may also lead to patients seeking repeat visits after 4 days, or asking for a "better" antibiotic after 8 or 9 days, which results in more prescriptions for broad spectrum antibiotics.
And the next time around, they are likely to say that the only drug that works for them is a broad spectrum antibiotic.
Dr. Ebell and his colleagues said they are exploring the clinical issue further, researching what physicians believe about cough, how messages in the media influence behavior, and whether there might be a discrepancy between the reality of an acute illness – its natural history – and perception.
Most importantly, he said he hopes to determine whether his findings can be used "to educate patients, to educate physicians, and hopefully create more realistic expectations about the duration of a cough [and] the duration of an acute illness, and thereby, hopefully reduce the demand for antibiotics."
Dr. Ebell reported having no relevant financial conflicts.
NEW ORLEANS – Patients tend to underestimate how long a cough should last, leading to unnecessary and inappropriate use of antibiotics, according to a review of the evidence and a survey of patient beliefs.
Cough is the third most frequent reason for physician office visits, and yet doctors and patients don’t seem to have an understanding of the natural history of cough and the expected duration, said Dr. Mark Ebell of the department of epidemiology at the University of Georgia College of Public Health in Athens.
The National Ambulatory Medical Survey in 2007 showed that there were 27 million outpatient visits for cough that year. That constitutes 2%-3% of all family practice visits, said Dr. Ebell. Half of patients received an antibiotic for their cough, and half the time, it was a broad spectrum antibiotic.
"There are some real issues with how we manage cough," said Dr. Ebell. Cough can indicate a condition that needs medical attention and a prescription therapy, but often, it is treated without evidence for antibiotics because the patient or doctor is uncomfortable with its duration.
Before patients ask their doctor how long a cough should last, they are likely to ask Google, he said. In conducting his own Google search, he found estimates ranging from 7 days to 14 days.
To get a sense of what patients think, Dr. Ebell and his colleagues surveyed Georgia residents by adding questions to the Georgia Poll, which is conducted twice a year by the Survey Research Center at the University of Georgia. Potential participants – aged 18 years or older – are randomly selected and contacted by phone. Almost 500 participated; 63% were women. It was an older population because the survey is conducted through landlines.
Participants were asked about their beliefs concerning antibiotics and the effectiveness of these drugs when the main symptom was a cough. They were asked how long they think it would take for the cough to get better if they were not taking any medicine, in six different scenarios: dry cough, coughing up yellow mucus or green mucus, or any of those kinds of cough with a slight fever, or no fever.
Patients with self-reported chronic lung disease or asthma were excluded from the survey.
Some respondents thought they would be better in as few as 2 days. Some thought the cough would last several months, but almost everyone thought it would take less than 2 weeks. There was not much difference between the scenarios, except when the scenario involved green phlegm.
The participants who had previously used antibiotics thought the cough would last longer, as did women, whites, and those with less education.
To determine how long a cough actually does last, Dr. Ebell conducted a literature search. After combing through several 100,000 potential studies, excluding those in sinusitis or people with a clear bacterial diagnosis, and focusing on those in community-dwelling, otherwise healthy adults with undifferentiated acute cough or bronchitis, he and his colleagues were left with 18 studies. In the end, only 5 of those 18 provided useful data.
The mean duration was 17-18 days. "So now we know how long a cough lasts," said Dr. Ebell.
Although the cough usually improves significantly in 2 weeks, most patients think it should be over in a week. "And that’s a big driver, or may be a big driver, of antibiotic use," he said. It may also lead to patients seeking repeat visits after 4 days, or asking for a "better" antibiotic after 8 or 9 days, which results in more prescriptions for broad spectrum antibiotics.
And the next time around, they are likely to say that the only drug that works for them is a broad spectrum antibiotic.
Dr. Ebell and his colleagues said they are exploring the clinical issue further, researching what physicians believe about cough, how messages in the media influence behavior, and whether there might be a discrepancy between the reality of an acute illness – its natural history – and perception.
Most importantly, he said he hopes to determine whether his findings can be used "to educate patients, to educate physicians, and hopefully create more realistic expectations about the duration of a cough [and] the duration of an acute illness, and thereby, hopefully reduce the demand for antibiotics."
Dr. Ebell reported having no relevant financial conflicts.
NEW ORLEANS – Patients tend to underestimate how long a cough should last, leading to unnecessary and inappropriate use of antibiotics, according to a review of the evidence and a survey of patient beliefs.
Cough is the third most frequent reason for physician office visits, and yet doctors and patients don’t seem to have an understanding of the natural history of cough and the expected duration, said Dr. Mark Ebell of the department of epidemiology at the University of Georgia College of Public Health in Athens.
The National Ambulatory Medical Survey in 2007 showed that there were 27 million outpatient visits for cough that year. That constitutes 2%-3% of all family practice visits, said Dr. Ebell. Half of patients received an antibiotic for their cough, and half the time, it was a broad spectrum antibiotic.
"There are some real issues with how we manage cough," said Dr. Ebell. Cough can indicate a condition that needs medical attention and a prescription therapy, but often, it is treated without evidence for antibiotics because the patient or doctor is uncomfortable with its duration.
Before patients ask their doctor how long a cough should last, they are likely to ask Google, he said. In conducting his own Google search, he found estimates ranging from 7 days to 14 days.
To get a sense of what patients think, Dr. Ebell and his colleagues surveyed Georgia residents by adding questions to the Georgia Poll, which is conducted twice a year by the Survey Research Center at the University of Georgia. Potential participants – aged 18 years or older – are randomly selected and contacted by phone. Almost 500 participated; 63% were women. It was an older population because the survey is conducted through landlines.
Participants were asked about their beliefs concerning antibiotics and the effectiveness of these drugs when the main symptom was a cough. They were asked how long they think it would take for the cough to get better if they were not taking any medicine, in six different scenarios: dry cough, coughing up yellow mucus or green mucus, or any of those kinds of cough with a slight fever, or no fever.
Patients with self-reported chronic lung disease or asthma were excluded from the survey.
Some respondents thought they would be better in as few as 2 days. Some thought the cough would last several months, but almost everyone thought it would take less than 2 weeks. There was not much difference between the scenarios, except when the scenario involved green phlegm.
The participants who had previously used antibiotics thought the cough would last longer, as did women, whites, and those with less education.
To determine how long a cough actually does last, Dr. Ebell conducted a literature search. After combing through several 100,000 potential studies, excluding those in sinusitis or people with a clear bacterial diagnosis, and focusing on those in community-dwelling, otherwise healthy adults with undifferentiated acute cough or bronchitis, he and his colleagues were left with 18 studies. In the end, only 5 of those 18 provided useful data.
The mean duration was 17-18 days. "So now we know how long a cough lasts," said Dr. Ebell.
Although the cough usually improves significantly in 2 weeks, most patients think it should be over in a week. "And that’s a big driver, or may be a big driver, of antibiotic use," he said. It may also lead to patients seeking repeat visits after 4 days, or asking for a "better" antibiotic after 8 or 9 days, which results in more prescriptions for broad spectrum antibiotics.
And the next time around, they are likely to say that the only drug that works for them is a broad spectrum antibiotic.
Dr. Ebell and his colleagues said they are exploring the clinical issue further, researching what physicians believe about cough, how messages in the media influence behavior, and whether there might be a discrepancy between the reality of an acute illness – its natural history – and perception.
Most importantly, he said he hopes to determine whether his findings can be used "to educate patients, to educate physicians, and hopefully create more realistic expectations about the duration of a cough [and] the duration of an acute illness, and thereby, hopefully reduce the demand for antibiotics."
Dr. Ebell reported having no relevant financial conflicts.
AT THE ANNUAL MEETING OF THE NORTH AMERICAN PRIMARY CARE RESEARCH GROUP
Major Finding: Acute cough due to nonbacterial causes lasts 17-18 days, but patients believe that a cough should resolve in a week or two.
Data Source: A survey of 500 patients.
Disclosures: Dr. Ebell reported having no relevant financial conflicts.
Get Ready for E&M Coding, Experts Advise
Psychiatrists are girding themselves for major changes in how they bill for their services starting Jan. 1, due to changes in the Current Procedural Terminology codes that were finalized in the 2013 Medicare Physician Fee Schedule.
The bottom line: Some psychiatrists, especially those who primarily do outpatient work, may have a steep learning curve with little additional payoff initially, according to Dr. Ronald Burd, chairman of the American Psychiatric Association committee on codes, RBRVS (Resource-Based Relative Value Scale), and reimbursement.
All psychiatrists will see increased pressure to start using evaluation and management (E&M) codes, which requires knowing the system and more documentation from the physician.
"If you’re used to using the E&M codes for inpatient work, it should translate pretty easily for outpatient work," said Dr. Jeremy S. Musher, who serves on the APA committee on codes, RBRVS, and reimbursement, and is the APA adviser to the American Medical Association (AMA) Relative Value Update Committee (RUC).
"But for psychiatrists who have not used E&M codes, there will be some learning involved in how to use, how to document, and how to bill," he said in an interview.
Reimbursement should eventually rise, but for the first year, the codes have been assigned interim values that aren’t much higher than current pay. Values may rise in 2014, after the professional societies have had a chance to survey psychiatrists on the new codes and the RUC looks at revaluing those codes, said Dr. Musher, medical director for psychiatric emergency services at the Western Psychiatric Institute and Clinic at the University of Pittsburgh Medical Center and president and CEO of the consulting company the Musher Group.
The goal of the coding changes is for all psychiatrists to have "the opportunity to be appropriately reimbursed for the intensity of the work they do," Dr. Burd, who is also inpatient medical director for Sanford Health Services in Fargo, N.D., said in an interview.
The coding revision has been in process for several years, according to Dr. Musher. All codes are reviewed and revised periodically. When some of the psychiatric codes came up for review, the APA and other mental health societies suggested that the codes be revised to pay psychiatrists more appropriately.
Since the last major revision of the codes in 1998, psychiatrists have been locked into an outpatient medication management code (90862) that pays a flat rate, he explained. But patients have become more complex, presenting with an increasing number of comorbidities. Patients are also more complicated from a psychiatric standpoint because many have been shifted from the inpatient to the outpatient environment, he said. "The payment structure we are operating under does not account for that," Dr. Musher said.
The new codes more accurately reflect what psychiatrists do, he said. Under the new system, the 90862 pharmacologic management code has been deleted. There is a 90863 code now, which was created for psychologists in states where they have prescriptive privileges. But these codes should not be used by psychiatrists or midlevel providers, according to Dr. Burd.
Previously, the key intake code was 90801 and could be used when intake was done by a social worker, or a geriatric psychiatrist or a nurse practitioner. The argument was made that the level of work is different among those providers, Dr. Burd said. In recognition of that, in 2013 two intake codes will be available: 90792 for medical services, and 90791 for nonmedical services.
The psychiatric diagnostic evaluation code can be used in any setting, inpatient or outpatient. And it can be used more than once; if an evaluation spans several appointments, the code can be used for reassessments, Dr. Burd said.
In 2013, more psychiatric services will now be covered by E&M codes. Currently, E&M codes are used for psychotherapy, as these services are time based. For example, a psychiatrist can bill for 20-30 minutes of face-to-face contact, which would be mostly psychotherapy, and there would be a small amount of E&M involved, Dr. Burd said.
In the coming year, the situation is reversed. The psychiatrist will specify the level of E&M work done during the patient appointment and then add on codes for psychotherapy work, he said. Using a specific E&M will allow for greater accuracy for physician work during that time. Those codes require documenting the patient’s history, the exam, and the physician’s decision making for the E&M portion of the visit, with the psychotherapy component based on the time spent delivering psychotherapy.
It’s a bit ironic that in an era of bundling of services, there is unbundling for psychiatry – physicians will submit two codes for services that previously had a single value, Dr. Burd pointed out.
New codes also are available for crisis psychotherapy. The base code of 90839 will be used for the initial contact; the add-on code of 90840 will be available for every additional 30-minute increment.
Finally, the Current Procedural Terminology (CPT) eliminated a parallel set of codes that existed for interactive services such as play therapy or e-mailing patients, Dr. Burd said. Instead, "the modifier 90785 can be added to pretty much any code."
If a psychiatrist previously billed a 90802 as an intake with interaction, "I’d now bill at 90792 or 91 plus the interactive code of 90875," he said.
For psychiatrists trying to get up to speed, the APA conducts webinar "train the trainer" sessions so that psychiatrists can help bring local colleagues up to speed, Dr. Musher said. He also will present the new codes at the AMA’s annual CPT symposium for coders from physician practices. Subspecialty groups such as the American Association for Geriatric Psychiatry also will hold webinars.
The APA is set to provide documentation templates to members via its website. And the organization is working with payers to ensure they have a uniform interpretation of the new codes and that their systems will be set up to understand the new codes, Dr. Burd said.
He urged psychiatrists to educate themselves, starting by getting a copy of the CPT for 2013 and reading it, especially the section on E&M codes, he said.
Long term, there’s an upside for psychiatrists, Dr. Burd said. Many have been locked into low-value contracts, he noted. By using higher-level codes, "they’ll be able to bill for higher-level service."
Psychiatrists are girding themselves for major changes in how they bill for their services starting Jan. 1, due to changes in the Current Procedural Terminology codes that were finalized in the 2013 Medicare Physician Fee Schedule.
The bottom line: Some psychiatrists, especially those who primarily do outpatient work, may have a steep learning curve with little additional payoff initially, according to Dr. Ronald Burd, chairman of the American Psychiatric Association committee on codes, RBRVS (Resource-Based Relative Value Scale), and reimbursement.
All psychiatrists will see increased pressure to start using evaluation and management (E&M) codes, which requires knowing the system and more documentation from the physician.
"If you’re used to using the E&M codes for inpatient work, it should translate pretty easily for outpatient work," said Dr. Jeremy S. Musher, who serves on the APA committee on codes, RBRVS, and reimbursement, and is the APA adviser to the American Medical Association (AMA) Relative Value Update Committee (RUC).
"But for psychiatrists who have not used E&M codes, there will be some learning involved in how to use, how to document, and how to bill," he said in an interview.
Reimbursement should eventually rise, but for the first year, the codes have been assigned interim values that aren’t much higher than current pay. Values may rise in 2014, after the professional societies have had a chance to survey psychiatrists on the new codes and the RUC looks at revaluing those codes, said Dr. Musher, medical director for psychiatric emergency services at the Western Psychiatric Institute and Clinic at the University of Pittsburgh Medical Center and president and CEO of the consulting company the Musher Group.
The goal of the coding changes is for all psychiatrists to have "the opportunity to be appropriately reimbursed for the intensity of the work they do," Dr. Burd, who is also inpatient medical director for Sanford Health Services in Fargo, N.D., said in an interview.
The coding revision has been in process for several years, according to Dr. Musher. All codes are reviewed and revised periodically. When some of the psychiatric codes came up for review, the APA and other mental health societies suggested that the codes be revised to pay psychiatrists more appropriately.
Since the last major revision of the codes in 1998, psychiatrists have been locked into an outpatient medication management code (90862) that pays a flat rate, he explained. But patients have become more complex, presenting with an increasing number of comorbidities. Patients are also more complicated from a psychiatric standpoint because many have been shifted from the inpatient to the outpatient environment, he said. "The payment structure we are operating under does not account for that," Dr. Musher said.
The new codes more accurately reflect what psychiatrists do, he said. Under the new system, the 90862 pharmacologic management code has been deleted. There is a 90863 code now, which was created for psychologists in states where they have prescriptive privileges. But these codes should not be used by psychiatrists or midlevel providers, according to Dr. Burd.
Previously, the key intake code was 90801 and could be used when intake was done by a social worker, or a geriatric psychiatrist or a nurse practitioner. The argument was made that the level of work is different among those providers, Dr. Burd said. In recognition of that, in 2013 two intake codes will be available: 90792 for medical services, and 90791 for nonmedical services.
The psychiatric diagnostic evaluation code can be used in any setting, inpatient or outpatient. And it can be used more than once; if an evaluation spans several appointments, the code can be used for reassessments, Dr. Burd said.
In 2013, more psychiatric services will now be covered by E&M codes. Currently, E&M codes are used for psychotherapy, as these services are time based. For example, a psychiatrist can bill for 20-30 minutes of face-to-face contact, which would be mostly psychotherapy, and there would be a small amount of E&M involved, Dr. Burd said.
In the coming year, the situation is reversed. The psychiatrist will specify the level of E&M work done during the patient appointment and then add on codes for psychotherapy work, he said. Using a specific E&M will allow for greater accuracy for physician work during that time. Those codes require documenting the patient’s history, the exam, and the physician’s decision making for the E&M portion of the visit, with the psychotherapy component based on the time spent delivering psychotherapy.
It’s a bit ironic that in an era of bundling of services, there is unbundling for psychiatry – physicians will submit two codes for services that previously had a single value, Dr. Burd pointed out.
New codes also are available for crisis psychotherapy. The base code of 90839 will be used for the initial contact; the add-on code of 90840 will be available for every additional 30-minute increment.
Finally, the Current Procedural Terminology (CPT) eliminated a parallel set of codes that existed for interactive services such as play therapy or e-mailing patients, Dr. Burd said. Instead, "the modifier 90785 can be added to pretty much any code."
If a psychiatrist previously billed a 90802 as an intake with interaction, "I’d now bill at 90792 or 91 plus the interactive code of 90875," he said.
For psychiatrists trying to get up to speed, the APA conducts webinar "train the trainer" sessions so that psychiatrists can help bring local colleagues up to speed, Dr. Musher said. He also will present the new codes at the AMA’s annual CPT symposium for coders from physician practices. Subspecialty groups such as the American Association for Geriatric Psychiatry also will hold webinars.
The APA is set to provide documentation templates to members via its website. And the organization is working with payers to ensure they have a uniform interpretation of the new codes and that their systems will be set up to understand the new codes, Dr. Burd said.
He urged psychiatrists to educate themselves, starting by getting a copy of the CPT for 2013 and reading it, especially the section on E&M codes, he said.
Long term, there’s an upside for psychiatrists, Dr. Burd said. Many have been locked into low-value contracts, he noted. By using higher-level codes, "they’ll be able to bill for higher-level service."
Psychiatrists are girding themselves for major changes in how they bill for their services starting Jan. 1, due to changes in the Current Procedural Terminology codes that were finalized in the 2013 Medicare Physician Fee Schedule.
The bottom line: Some psychiatrists, especially those who primarily do outpatient work, may have a steep learning curve with little additional payoff initially, according to Dr. Ronald Burd, chairman of the American Psychiatric Association committee on codes, RBRVS (Resource-Based Relative Value Scale), and reimbursement.
All psychiatrists will see increased pressure to start using evaluation and management (E&M) codes, which requires knowing the system and more documentation from the physician.
"If you’re used to using the E&M codes for inpatient work, it should translate pretty easily for outpatient work," said Dr. Jeremy S. Musher, who serves on the APA committee on codes, RBRVS, and reimbursement, and is the APA adviser to the American Medical Association (AMA) Relative Value Update Committee (RUC).
"But for psychiatrists who have not used E&M codes, there will be some learning involved in how to use, how to document, and how to bill," he said in an interview.
Reimbursement should eventually rise, but for the first year, the codes have been assigned interim values that aren’t much higher than current pay. Values may rise in 2014, after the professional societies have had a chance to survey psychiatrists on the new codes and the RUC looks at revaluing those codes, said Dr. Musher, medical director for psychiatric emergency services at the Western Psychiatric Institute and Clinic at the University of Pittsburgh Medical Center and president and CEO of the consulting company the Musher Group.
The goal of the coding changes is for all psychiatrists to have "the opportunity to be appropriately reimbursed for the intensity of the work they do," Dr. Burd, who is also inpatient medical director for Sanford Health Services in Fargo, N.D., said in an interview.
The coding revision has been in process for several years, according to Dr. Musher. All codes are reviewed and revised periodically. When some of the psychiatric codes came up for review, the APA and other mental health societies suggested that the codes be revised to pay psychiatrists more appropriately.
Since the last major revision of the codes in 1998, psychiatrists have been locked into an outpatient medication management code (90862) that pays a flat rate, he explained. But patients have become more complex, presenting with an increasing number of comorbidities. Patients are also more complicated from a psychiatric standpoint because many have been shifted from the inpatient to the outpatient environment, he said. "The payment structure we are operating under does not account for that," Dr. Musher said.
The new codes more accurately reflect what psychiatrists do, he said. Under the new system, the 90862 pharmacologic management code has been deleted. There is a 90863 code now, which was created for psychologists in states where they have prescriptive privileges. But these codes should not be used by psychiatrists or midlevel providers, according to Dr. Burd.
Previously, the key intake code was 90801 and could be used when intake was done by a social worker, or a geriatric psychiatrist or a nurse practitioner. The argument was made that the level of work is different among those providers, Dr. Burd said. In recognition of that, in 2013 two intake codes will be available: 90792 for medical services, and 90791 for nonmedical services.
The psychiatric diagnostic evaluation code can be used in any setting, inpatient or outpatient. And it can be used more than once; if an evaluation spans several appointments, the code can be used for reassessments, Dr. Burd said.
In 2013, more psychiatric services will now be covered by E&M codes. Currently, E&M codes are used for psychotherapy, as these services are time based. For example, a psychiatrist can bill for 20-30 minutes of face-to-face contact, which would be mostly psychotherapy, and there would be a small amount of E&M involved, Dr. Burd said.
In the coming year, the situation is reversed. The psychiatrist will specify the level of E&M work done during the patient appointment and then add on codes for psychotherapy work, he said. Using a specific E&M will allow for greater accuracy for physician work during that time. Those codes require documenting the patient’s history, the exam, and the physician’s decision making for the E&M portion of the visit, with the psychotherapy component based on the time spent delivering psychotherapy.
It’s a bit ironic that in an era of bundling of services, there is unbundling for psychiatry – physicians will submit two codes for services that previously had a single value, Dr. Burd pointed out.
New codes also are available for crisis psychotherapy. The base code of 90839 will be used for the initial contact; the add-on code of 90840 will be available for every additional 30-minute increment.
Finally, the Current Procedural Terminology (CPT) eliminated a parallel set of codes that existed for interactive services such as play therapy or e-mailing patients, Dr. Burd said. Instead, "the modifier 90785 can be added to pretty much any code."
If a psychiatrist previously billed a 90802 as an intake with interaction, "I’d now bill at 90792 or 91 plus the interactive code of 90875," he said.
For psychiatrists trying to get up to speed, the APA conducts webinar "train the trainer" sessions so that psychiatrists can help bring local colleagues up to speed, Dr. Musher said. He also will present the new codes at the AMA’s annual CPT symposium for coders from physician practices. Subspecialty groups such as the American Association for Geriatric Psychiatry also will hold webinars.
The APA is set to provide documentation templates to members via its website. And the organization is working with payers to ensure they have a uniform interpretation of the new codes and that their systems will be set up to understand the new codes, Dr. Burd said.
He urged psychiatrists to educate themselves, starting by getting a copy of the CPT for 2013 and reading it, especially the section on E&M codes, he said.
Long term, there’s an upside for psychiatrists, Dr. Burd said. Many have been locked into low-value contracts, he noted. By using higher-level codes, "they’ll be able to bill for higher-level service."
New Analysis Confirms ACA-Related PCP Shortage
NEW ORLEANS – Supply of primary care physicians is unlikely to meet demand when the Affordable Care Act is fully implemented in 2014 and shortages will be more acute in some regions that others.
Overall, the expansion of health insurance to a wider population is likely to mean that the United States will need an additional 8,000 primary care physicians over what is currently projected, or a 3% increase in the current workforce, by 2025, Stephen M. Petterson, Ph.D., reported at the annual meeting of the North American Primary Care Research Group.
While that may not seem to be a huge increase, the nation will need 43,000 additional primary care doctors just to keep pace with population growth and the aging of that population.
Taking into account population growth, the aging of the population, and the impact of the ACA, the number of office visits in the United States will increase from 462 million in 2008 to 565 million in 2025 (Ann. Fam. Med. 2012;10:503-9). Dr. Petterson and his colleagues noted that their analysis is the first look at the ACA’s impact specifically on the primary care workforce and primary care services.
To get at that data, the authors used the Medical Expenditure Panel Survey (MEPS) to calculate the use of office-based primary care in 2008, U.S. Census Bureau projections for population estimates, and the American Medical Association Masterfile to calculate the number of primary care physicians and determine the number of visits per physician.
They determined that 46% of all physician office visits are to primary care physicians. MEPS data show that in 2008, there were 977 million office visits to physicians, 462 million of which were to primary care physicians. Women made more office visits than did men, older adults more than younger ones, and the insured more than the uninsured.
Previous studies have shown that when people gain insurance coverage, they tend to use more services, said Dr. Petterson, research director at the Robert Graham Center, a primary care think tank in Washington, D.C.
Based on their analysis, by 2025, an estimated 260,687 practicing primary care physicians will be needed – an increase of 51,880 from today. Most of the additional workforce can be built gradually, to accommodate aging and population growth, they said. But there will be a more urgent need in 2014 and 2015 when the ACA is fully implemented and there will be an additional 20 million primary care visits.
The ACA proposes to build the primary care workforce through expanding the number of primary care residents and increasing training for physician assistants and nurse practitioners. But that will only produce an estimated 500 additional physicians, said the authors, noting that "even if these positions were maintained for 10 years, only 5,000 additional primary care physicians would be trained."
The need for more primary care doctors varies geographically, Dr. Petterson said at the meeting.
Some states, those with a low number of uninsured, small populations, or a relatively high concentration of physicians, won’t need to bump up their numbers by much. Those states include Vermont, North Dakota, Wyoming, Delaware, the District of Columbia, South Dakota, Hawaii, Rhode Island, New Hampshire, and Montana.
The 10 states that will require the largest increase in the workforce are New Jersey, Pennsylvania, Ohio, North Carolina, Georgia, Illinois, New York, Florida, Texas, and California. These states have a high number of uninsured patients and a relatively low ratio of primary care physicians to the overall population, Dr. Petterson said. On the low end, New Jersey will need to increase its workforce by about 3%, or 200 or so new physicians. Texas and California are looking at a 7% and a 5% increase respectively, he said.
"The sudden influx of newly insured patients will exacerbate this situation," he said.
The authors had no relevant conflicts of interest; the study was funded in part by the Agency for Healthcare Research and Quality.
NEW ORLEANS – Supply of primary care physicians is unlikely to meet demand when the Affordable Care Act is fully implemented in 2014 and shortages will be more acute in some regions that others.
Overall, the expansion of health insurance to a wider population is likely to mean that the United States will need an additional 8,000 primary care physicians over what is currently projected, or a 3% increase in the current workforce, by 2025, Stephen M. Petterson, Ph.D., reported at the annual meeting of the North American Primary Care Research Group.
While that may not seem to be a huge increase, the nation will need 43,000 additional primary care doctors just to keep pace with population growth and the aging of that population.
Taking into account population growth, the aging of the population, and the impact of the ACA, the number of office visits in the United States will increase from 462 million in 2008 to 565 million in 2025 (Ann. Fam. Med. 2012;10:503-9). Dr. Petterson and his colleagues noted that their analysis is the first look at the ACA’s impact specifically on the primary care workforce and primary care services.
To get at that data, the authors used the Medical Expenditure Panel Survey (MEPS) to calculate the use of office-based primary care in 2008, U.S. Census Bureau projections for population estimates, and the American Medical Association Masterfile to calculate the number of primary care physicians and determine the number of visits per physician.
They determined that 46% of all physician office visits are to primary care physicians. MEPS data show that in 2008, there were 977 million office visits to physicians, 462 million of which were to primary care physicians. Women made more office visits than did men, older adults more than younger ones, and the insured more than the uninsured.
Previous studies have shown that when people gain insurance coverage, they tend to use more services, said Dr. Petterson, research director at the Robert Graham Center, a primary care think tank in Washington, D.C.
Based on their analysis, by 2025, an estimated 260,687 practicing primary care physicians will be needed – an increase of 51,880 from today. Most of the additional workforce can be built gradually, to accommodate aging and population growth, they said. But there will be a more urgent need in 2014 and 2015 when the ACA is fully implemented and there will be an additional 20 million primary care visits.
The ACA proposes to build the primary care workforce through expanding the number of primary care residents and increasing training for physician assistants and nurse practitioners. But that will only produce an estimated 500 additional physicians, said the authors, noting that "even if these positions were maintained for 10 years, only 5,000 additional primary care physicians would be trained."
The need for more primary care doctors varies geographically, Dr. Petterson said at the meeting.
Some states, those with a low number of uninsured, small populations, or a relatively high concentration of physicians, won’t need to bump up their numbers by much. Those states include Vermont, North Dakota, Wyoming, Delaware, the District of Columbia, South Dakota, Hawaii, Rhode Island, New Hampshire, and Montana.
The 10 states that will require the largest increase in the workforce are New Jersey, Pennsylvania, Ohio, North Carolina, Georgia, Illinois, New York, Florida, Texas, and California. These states have a high number of uninsured patients and a relatively low ratio of primary care physicians to the overall population, Dr. Petterson said. On the low end, New Jersey will need to increase its workforce by about 3%, or 200 or so new physicians. Texas and California are looking at a 7% and a 5% increase respectively, he said.
"The sudden influx of newly insured patients will exacerbate this situation," he said.
The authors had no relevant conflicts of interest; the study was funded in part by the Agency for Healthcare Research and Quality.
NEW ORLEANS – Supply of primary care physicians is unlikely to meet demand when the Affordable Care Act is fully implemented in 2014 and shortages will be more acute in some regions that others.
Overall, the expansion of health insurance to a wider population is likely to mean that the United States will need an additional 8,000 primary care physicians over what is currently projected, or a 3% increase in the current workforce, by 2025, Stephen M. Petterson, Ph.D., reported at the annual meeting of the North American Primary Care Research Group.
While that may not seem to be a huge increase, the nation will need 43,000 additional primary care doctors just to keep pace with population growth and the aging of that population.
Taking into account population growth, the aging of the population, and the impact of the ACA, the number of office visits in the United States will increase from 462 million in 2008 to 565 million in 2025 (Ann. Fam. Med. 2012;10:503-9). Dr. Petterson and his colleagues noted that their analysis is the first look at the ACA’s impact specifically on the primary care workforce and primary care services.
To get at that data, the authors used the Medical Expenditure Panel Survey (MEPS) to calculate the use of office-based primary care in 2008, U.S. Census Bureau projections for population estimates, and the American Medical Association Masterfile to calculate the number of primary care physicians and determine the number of visits per physician.
They determined that 46% of all physician office visits are to primary care physicians. MEPS data show that in 2008, there were 977 million office visits to physicians, 462 million of which were to primary care physicians. Women made more office visits than did men, older adults more than younger ones, and the insured more than the uninsured.
Previous studies have shown that when people gain insurance coverage, they tend to use more services, said Dr. Petterson, research director at the Robert Graham Center, a primary care think tank in Washington, D.C.
Based on their analysis, by 2025, an estimated 260,687 practicing primary care physicians will be needed – an increase of 51,880 from today. Most of the additional workforce can be built gradually, to accommodate aging and population growth, they said. But there will be a more urgent need in 2014 and 2015 when the ACA is fully implemented and there will be an additional 20 million primary care visits.
The ACA proposes to build the primary care workforce through expanding the number of primary care residents and increasing training for physician assistants and nurse practitioners. But that will only produce an estimated 500 additional physicians, said the authors, noting that "even if these positions were maintained for 10 years, only 5,000 additional primary care physicians would be trained."
The need for more primary care doctors varies geographically, Dr. Petterson said at the meeting.
Some states, those with a low number of uninsured, small populations, or a relatively high concentration of physicians, won’t need to bump up their numbers by much. Those states include Vermont, North Dakota, Wyoming, Delaware, the District of Columbia, South Dakota, Hawaii, Rhode Island, New Hampshire, and Montana.
The 10 states that will require the largest increase in the workforce are New Jersey, Pennsylvania, Ohio, North Carolina, Georgia, Illinois, New York, Florida, Texas, and California. These states have a high number of uninsured patients and a relatively low ratio of primary care physicians to the overall population, Dr. Petterson said. On the low end, New Jersey will need to increase its workforce by about 3%, or 200 or so new physicians. Texas and California are looking at a 7% and a 5% increase respectively, he said.
"The sudden influx of newly insured patients will exacerbate this situation," he said.
The authors had no relevant conflicts of interest; the study was funded in part by the Agency for Healthcare Research and Quality.
AT THE ANNUAL MEETING OF THE NORTH AMERICAN PRIMARY CARE RESEARCH GROUP
Major Finding: Due to the Affordable Care Act, the nation will need at least 8,000 more primary care physicians.
Data Source: The authors analyzed population data, physician numbers, and physician usage data to project the number of primary care physicians needed by 2025.
Disclosures: The authors reported no conflicts. The study was funded in part by the Agency for Healthcare Research and Quality.
Cardiology Sees Wins, Losses in Medicare Fee Schedule
The Medicare physician fee schedule for 2013 is a mixed bag for cardiologists, with impending cuts based on the Sustainable Growth Rate formula as well as a cut to pay for imaging and certain procedures, and the possibility of a slight uptick for care coordination.
"This year’s final rule cuts payments for important cardiovascular services at a time when many cardiology practices are already vulnerable," said Dr. William Zoghbi, president of the American College of Cardiology, in a statement.
Under current law, the SGR formula will kick in Jan. 1 and lop one-fourth off doctors’ pay under Medicare, unless Congress steps in to halt the cut.
In issuing the fee schedule final regulation on Nov. 1, the Obama administration noted that Congress has reversed the mandated cut every year since 2003.
The administration "is committed to fixing the SGR update methodology and ensuring these payment cuts do not take effect," according to a statement. "Predictable, fiscally responsible physician payments are essential for Medicare to sustain quality and lower health care costs over the long term."
The American College of Cardiology also called for pay predictability. "The ongoing uncertainties about Medicare payments that are a direct result of the SGR formula make it nearly impossible to plan and invest in the future," Dr. Zoghbi said.
Even with an SGR fix, cardiologists will see an average 2% reduction in pay because of an expansion of the multiple procedure payment reduction policy. Under that policy, the Centers for Medicare and Medicaid Services reduces payment for a second and subsequent advanced imaging service that is done in the same session or on the same day by the same provider. That policy now applies to the technical component of certain cardiovascular and ophthalmologic diagnostic tests and for imaging services. Essentially, it cuts pay for those services by 25%.
Among the services that will be affected: complete electrocardiogram (CPT code 93000), cardiovascular stress test (93015), and ambulatory blood pressure monitoring (93784).
The move was expected, but the ACC is "definitely disappointed," according to Brian Whitman, associate director of regulatory affairs at the College. The continuing reductions will help to push many cardiologists into hospital-based employment, he predicted.
The fee schedule final rule also outlined a new set of codes that pays physicians to coordinate care within 30 days of discharge from a hospital or nursing home. The rule creates two new CPT codes (99495 and 99496) that can be used for patient care that is not face to face, such as phone consults, chart reviews, and e-mail communications.
While primary care physicians are expected to report these codes most often, cardiologists will also be involved occasionally in these care transitions, Mr. Whitman said.
Cardiologists who run heart failure clinics or who are heart failure specialists, or who may be involved in post–myocardial infarction care are likely to use the transition codes, he added.
Starting next year, a physician using the codes can also conduct the discharge, but he or she must also have had an existing relationship with the patient, defined as having had at least one face-to-face visit within the previous 3 years.
Also included in the final rule: changes to the value-based modifier program. The modifier is designed to pay physicians based on the quality of care they deliver. In the proposed rule issued in July, physicians in groups of 25 or larger would have been subject to the new pay plan in 2015. The final rule increases the size of the group to 100 initially. According to the CMS, the change was made so the agency – and physicians – could gain experience with the methodology and approach before the program is expanded to smaller physician groups.
The value-based modifier will be expanded to all physicians in 2017.
The final rule also outlines how the CMS will expand the Physician Compare website, which was launched in 2010 and currently includes basic information about approved Medicare providers, and whether they are considered successful prescribers under the Medicare Electronic Prescribing Incentive Program. The Affordable Care Act requires the CMS to start making physician performance data available in 2013.
The agency says that next year it will post the names of physicians who successfully report on the Physician Quality Reporting System’s Cardiovascular Prevention measures, as part of the Health and Human Services department’s Million Hearts campaign.
In another final rule issued Nov. 1, the CMS announced that, as expected, it will pay certain providers the Medicare pay rate for certain primary care services provided under Medicaid in 2013 and 2014.
As called for under the Affordable Care Act, the CMS will pay Medicare rates for evaluation and management codes between 99201 and 99499 when they are used by physicians who are board certified by the American Board of Medical Specialties, the American Osteopathic Association, and the American Board of Physician Specialties.
The codes cover not just primary care, but also hospital observation and consultation for inpatient services provided by nonadmitting physicians, emergency department services, and critical care services.
The CMS estimated that increasing the Medicaid pay will cost $5.6 billion in 2013 and $5.7 billion in 2014.
Since the rule is written to cover subspecialists, cardiologists – especially pediatric cardiologists – are likely to benefit from this pay parity rule, Mr. Whitman said.
The rules will be published in the Federal Register on Nov. 16 and comments will close on Dec. 31. Both rules take effect Jan. 1, 2013.
The Medicare physician fee schedule for 2013 is a mixed bag for cardiologists, with impending cuts based on the Sustainable Growth Rate formula as well as a cut to pay for imaging and certain procedures, and the possibility of a slight uptick for care coordination.
"This year’s final rule cuts payments for important cardiovascular services at a time when many cardiology practices are already vulnerable," said Dr. William Zoghbi, president of the American College of Cardiology, in a statement.
Under current law, the SGR formula will kick in Jan. 1 and lop one-fourth off doctors’ pay under Medicare, unless Congress steps in to halt the cut.
In issuing the fee schedule final regulation on Nov. 1, the Obama administration noted that Congress has reversed the mandated cut every year since 2003.
The administration "is committed to fixing the SGR update methodology and ensuring these payment cuts do not take effect," according to a statement. "Predictable, fiscally responsible physician payments are essential for Medicare to sustain quality and lower health care costs over the long term."
The American College of Cardiology also called for pay predictability. "The ongoing uncertainties about Medicare payments that are a direct result of the SGR formula make it nearly impossible to plan and invest in the future," Dr. Zoghbi said.
Even with an SGR fix, cardiologists will see an average 2% reduction in pay because of an expansion of the multiple procedure payment reduction policy. Under that policy, the Centers for Medicare and Medicaid Services reduces payment for a second and subsequent advanced imaging service that is done in the same session or on the same day by the same provider. That policy now applies to the technical component of certain cardiovascular and ophthalmologic diagnostic tests and for imaging services. Essentially, it cuts pay for those services by 25%.
Among the services that will be affected: complete electrocardiogram (CPT code 93000), cardiovascular stress test (93015), and ambulatory blood pressure monitoring (93784).
The move was expected, but the ACC is "definitely disappointed," according to Brian Whitman, associate director of regulatory affairs at the College. The continuing reductions will help to push many cardiologists into hospital-based employment, he predicted.
The fee schedule final rule also outlined a new set of codes that pays physicians to coordinate care within 30 days of discharge from a hospital or nursing home. The rule creates two new CPT codes (99495 and 99496) that can be used for patient care that is not face to face, such as phone consults, chart reviews, and e-mail communications.
While primary care physicians are expected to report these codes most often, cardiologists will also be involved occasionally in these care transitions, Mr. Whitman said.
Cardiologists who run heart failure clinics or who are heart failure specialists, or who may be involved in post–myocardial infarction care are likely to use the transition codes, he added.
Starting next year, a physician using the codes can also conduct the discharge, but he or she must also have had an existing relationship with the patient, defined as having had at least one face-to-face visit within the previous 3 years.
Also included in the final rule: changes to the value-based modifier program. The modifier is designed to pay physicians based on the quality of care they deliver. In the proposed rule issued in July, physicians in groups of 25 or larger would have been subject to the new pay plan in 2015. The final rule increases the size of the group to 100 initially. According to the CMS, the change was made so the agency – and physicians – could gain experience with the methodology and approach before the program is expanded to smaller physician groups.
The value-based modifier will be expanded to all physicians in 2017.
The final rule also outlines how the CMS will expand the Physician Compare website, which was launched in 2010 and currently includes basic information about approved Medicare providers, and whether they are considered successful prescribers under the Medicare Electronic Prescribing Incentive Program. The Affordable Care Act requires the CMS to start making physician performance data available in 2013.
The agency says that next year it will post the names of physicians who successfully report on the Physician Quality Reporting System’s Cardiovascular Prevention measures, as part of the Health and Human Services department’s Million Hearts campaign.
In another final rule issued Nov. 1, the CMS announced that, as expected, it will pay certain providers the Medicare pay rate for certain primary care services provided under Medicaid in 2013 and 2014.
As called for under the Affordable Care Act, the CMS will pay Medicare rates for evaluation and management codes between 99201 and 99499 when they are used by physicians who are board certified by the American Board of Medical Specialties, the American Osteopathic Association, and the American Board of Physician Specialties.
The codes cover not just primary care, but also hospital observation and consultation for inpatient services provided by nonadmitting physicians, emergency department services, and critical care services.
The CMS estimated that increasing the Medicaid pay will cost $5.6 billion in 2013 and $5.7 billion in 2014.
Since the rule is written to cover subspecialists, cardiologists – especially pediatric cardiologists – are likely to benefit from this pay parity rule, Mr. Whitman said.
The rules will be published in the Federal Register on Nov. 16 and comments will close on Dec. 31. Both rules take effect Jan. 1, 2013.
The Medicare physician fee schedule for 2013 is a mixed bag for cardiologists, with impending cuts based on the Sustainable Growth Rate formula as well as a cut to pay for imaging and certain procedures, and the possibility of a slight uptick for care coordination.
"This year’s final rule cuts payments for important cardiovascular services at a time when many cardiology practices are already vulnerable," said Dr. William Zoghbi, president of the American College of Cardiology, in a statement.
Under current law, the SGR formula will kick in Jan. 1 and lop one-fourth off doctors’ pay under Medicare, unless Congress steps in to halt the cut.
In issuing the fee schedule final regulation on Nov. 1, the Obama administration noted that Congress has reversed the mandated cut every year since 2003.
The administration "is committed to fixing the SGR update methodology and ensuring these payment cuts do not take effect," according to a statement. "Predictable, fiscally responsible physician payments are essential for Medicare to sustain quality and lower health care costs over the long term."
The American College of Cardiology also called for pay predictability. "The ongoing uncertainties about Medicare payments that are a direct result of the SGR formula make it nearly impossible to plan and invest in the future," Dr. Zoghbi said.
Even with an SGR fix, cardiologists will see an average 2% reduction in pay because of an expansion of the multiple procedure payment reduction policy. Under that policy, the Centers for Medicare and Medicaid Services reduces payment for a second and subsequent advanced imaging service that is done in the same session or on the same day by the same provider. That policy now applies to the technical component of certain cardiovascular and ophthalmologic diagnostic tests and for imaging services. Essentially, it cuts pay for those services by 25%.
Among the services that will be affected: complete electrocardiogram (CPT code 93000), cardiovascular stress test (93015), and ambulatory blood pressure monitoring (93784).
The move was expected, but the ACC is "definitely disappointed," according to Brian Whitman, associate director of regulatory affairs at the College. The continuing reductions will help to push many cardiologists into hospital-based employment, he predicted.
The fee schedule final rule also outlined a new set of codes that pays physicians to coordinate care within 30 days of discharge from a hospital or nursing home. The rule creates two new CPT codes (99495 and 99496) that can be used for patient care that is not face to face, such as phone consults, chart reviews, and e-mail communications.
While primary care physicians are expected to report these codes most often, cardiologists will also be involved occasionally in these care transitions, Mr. Whitman said.
Cardiologists who run heart failure clinics or who are heart failure specialists, or who may be involved in post–myocardial infarction care are likely to use the transition codes, he added.
Starting next year, a physician using the codes can also conduct the discharge, but he or she must also have had an existing relationship with the patient, defined as having had at least one face-to-face visit within the previous 3 years.
Also included in the final rule: changes to the value-based modifier program. The modifier is designed to pay physicians based on the quality of care they deliver. In the proposed rule issued in July, physicians in groups of 25 or larger would have been subject to the new pay plan in 2015. The final rule increases the size of the group to 100 initially. According to the CMS, the change was made so the agency – and physicians – could gain experience with the methodology and approach before the program is expanded to smaller physician groups.
The value-based modifier will be expanded to all physicians in 2017.
The final rule also outlines how the CMS will expand the Physician Compare website, which was launched in 2010 and currently includes basic information about approved Medicare providers, and whether they are considered successful prescribers under the Medicare Electronic Prescribing Incentive Program. The Affordable Care Act requires the CMS to start making physician performance data available in 2013.
The agency says that next year it will post the names of physicians who successfully report on the Physician Quality Reporting System’s Cardiovascular Prevention measures, as part of the Health and Human Services department’s Million Hearts campaign.
In another final rule issued Nov. 1, the CMS announced that, as expected, it will pay certain providers the Medicare pay rate for certain primary care services provided under Medicaid in 2013 and 2014.
As called for under the Affordable Care Act, the CMS will pay Medicare rates for evaluation and management codes between 99201 and 99499 when they are used by physicians who are board certified by the American Board of Medical Specialties, the American Osteopathic Association, and the American Board of Physician Specialties.
The codes cover not just primary care, but also hospital observation and consultation for inpatient services provided by nonadmitting physicians, emergency department services, and critical care services.
The CMS estimated that increasing the Medicaid pay will cost $5.6 billion in 2013 and $5.7 billion in 2014.
Since the rule is written to cover subspecialists, cardiologists – especially pediatric cardiologists – are likely to benefit from this pay parity rule, Mr. Whitman said.
The rules will be published in the Federal Register on Nov. 16 and comments will close on Dec. 31. Both rules take effect Jan. 1, 2013.