User login
Stage 2 Meaningful Use Rule Delays Implementation
Doctors who want to earn Medicare and Medicaid incentives for the meaningful use of electronic health records will not have to meet so-called stage 2 requirements until 2014, under final federal regulations that were released on Aug. 23.
More than 120,000 eligible health care professionals and more than 3,300 hospitals have qualified to receive such incentive payments under stage 1 of meaningful use, which requires physicians to certify that EHRs can capture and report data, among other issues, according to the Health and Human Services department.
Under stage 2, users must show that they can exchange data with other providers and that they can give patients secure online access to their health information.
Original federal proposals required providers to meet stage 2 requirements next year. The delay was hailed by at least one group of physicians.
"MGMA is pleased that the Centers for Medicare and Medicaid Services responded to our concerns regarding several of the proposed stage 2 meaningful use requirements," said Dr. Susan Turney, president and CEO of MGMA-ACMPE, the merged entity of the Medical Group Management Association (MGMA) and the American College of Medical Practice Executives (ACMPE), in a statement."Extending the start for stage 2 until 2014 was a necessary step to permit medical groups sufficient time to implement new software," she added.
Dr. Turney also said that MGMA-ACMPE members applauded some other changes to the proposal, including "lowering the thresholds for achieving certain measures such as mandatory online access and electronic exchange of summary of care documents."
Other important provisions in the final rule exempt certain physicians from the penalties that will be assessed come 2015 on those providers who do not adopt EHRs.
Physicians or hospitals will be exempt from the 1% reduction in Medicare reimbursement if they can show that the following apply to them:
• They lack Internet access, or face barriers to obtaining health information technology infrastructure.
• They are newly practicing.
• They have to contend with unforeseen circumstances, such as natural disasters.
The rule also makes exceptions for physicians who have limited interaction with patients, who practice at multiple locations, or who have no control over the availability of EHRs at locations that make up more than half of their patient encounters.
"These exclusions will allow physicians to achieve meaningful use with fewer hurdles," said Dr. Turney.
The American Medical Association took a more cautious approach, at least in an initial statement by board chair Steven J. Stack. "In a comment letter submitted by the AMA and 100 state and specialty medical societies in May, recommendations were outlined to eliminate physician roadblocks and encourage greater physician participation," said Dr. Stack. "We will carefully review the final rule and hope to see the changes we advocated for to promote widespread adoption and meaningful use of EHRs by physicians."
The rule also further clarifies certification criteria for EHRs, and modifies the certification program to "cut red tape and make the certification process more efficient," according to an HHS statement. All EHRs that have been certified under the 2011 rules can be used until 2014.
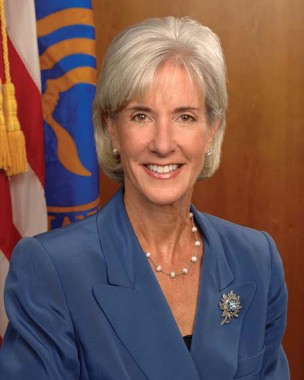
"The changes we’re announcing today will lead to more coordination of patient care, reduced medical errors, elimination of duplicate screenings and tests and greater patient engagement in their own care," said HHS Secretary Kathleen Sebelius in the statement.
Doctors who want to earn Medicare and Medicaid incentives for the meaningful use of electronic health records will not have to meet so-called stage 2 requirements until 2014, under final federal regulations that were released on Aug. 23.
More than 120,000 eligible health care professionals and more than 3,300 hospitals have qualified to receive such incentive payments under stage 1 of meaningful use, which requires physicians to certify that EHRs can capture and report data, among other issues, according to the Health and Human Services department.
Under stage 2, users must show that they can exchange data with other providers and that they can give patients secure online access to their health information.
Original federal proposals required providers to meet stage 2 requirements next year. The delay was hailed by at least one group of physicians.
"MGMA is pleased that the Centers for Medicare and Medicaid Services responded to our concerns regarding several of the proposed stage 2 meaningful use requirements," said Dr. Susan Turney, president and CEO of MGMA-ACMPE, the merged entity of the Medical Group Management Association (MGMA) and the American College of Medical Practice Executives (ACMPE), in a statement."Extending the start for stage 2 until 2014 was a necessary step to permit medical groups sufficient time to implement new software," she added.
Dr. Turney also said that MGMA-ACMPE members applauded some other changes to the proposal, including "lowering the thresholds for achieving certain measures such as mandatory online access and electronic exchange of summary of care documents."
Other important provisions in the final rule exempt certain physicians from the penalties that will be assessed come 2015 on those providers who do not adopt EHRs.
Physicians or hospitals will be exempt from the 1% reduction in Medicare reimbursement if they can show that the following apply to them:
• They lack Internet access, or face barriers to obtaining health information technology infrastructure.
• They are newly practicing.
• They have to contend with unforeseen circumstances, such as natural disasters.
The rule also makes exceptions for physicians who have limited interaction with patients, who practice at multiple locations, or who have no control over the availability of EHRs at locations that make up more than half of their patient encounters.
"These exclusions will allow physicians to achieve meaningful use with fewer hurdles," said Dr. Turney.
The American Medical Association took a more cautious approach, at least in an initial statement by board chair Steven J. Stack. "In a comment letter submitted by the AMA and 100 state and specialty medical societies in May, recommendations were outlined to eliminate physician roadblocks and encourage greater physician participation," said Dr. Stack. "We will carefully review the final rule and hope to see the changes we advocated for to promote widespread adoption and meaningful use of EHRs by physicians."
The rule also further clarifies certification criteria for EHRs, and modifies the certification program to "cut red tape and make the certification process more efficient," according to an HHS statement. All EHRs that have been certified under the 2011 rules can be used until 2014.
"The changes we’re announcing today will lead to more coordination of patient care, reduced medical errors, elimination of duplicate screenings and tests and greater patient engagement in their own care," said HHS Secretary Kathleen Sebelius in the statement.
Doctors who want to earn Medicare and Medicaid incentives for the meaningful use of electronic health records will not have to meet so-called stage 2 requirements until 2014, under final federal regulations that were released on Aug. 23.
More than 120,000 eligible health care professionals and more than 3,300 hospitals have qualified to receive such incentive payments under stage 1 of meaningful use, which requires physicians to certify that EHRs can capture and report data, among other issues, according to the Health and Human Services department.
Under stage 2, users must show that they can exchange data with other providers and that they can give patients secure online access to their health information.
Original federal proposals required providers to meet stage 2 requirements next year. The delay was hailed by at least one group of physicians.
"MGMA is pleased that the Centers for Medicare and Medicaid Services responded to our concerns regarding several of the proposed stage 2 meaningful use requirements," said Dr. Susan Turney, president and CEO of MGMA-ACMPE, the merged entity of the Medical Group Management Association (MGMA) and the American College of Medical Practice Executives (ACMPE), in a statement."Extending the start for stage 2 until 2014 was a necessary step to permit medical groups sufficient time to implement new software," she added.
Dr. Turney also said that MGMA-ACMPE members applauded some other changes to the proposal, including "lowering the thresholds for achieving certain measures such as mandatory online access and electronic exchange of summary of care documents."
Other important provisions in the final rule exempt certain physicians from the penalties that will be assessed come 2015 on those providers who do not adopt EHRs.
Physicians or hospitals will be exempt from the 1% reduction in Medicare reimbursement if they can show that the following apply to them:
• They lack Internet access, or face barriers to obtaining health information technology infrastructure.
• They are newly practicing.
• They have to contend with unforeseen circumstances, such as natural disasters.
The rule also makes exceptions for physicians who have limited interaction with patients, who practice at multiple locations, or who have no control over the availability of EHRs at locations that make up more than half of their patient encounters.
"These exclusions will allow physicians to achieve meaningful use with fewer hurdles," said Dr. Turney.
The American Medical Association took a more cautious approach, at least in an initial statement by board chair Steven J. Stack. "In a comment letter submitted by the AMA and 100 state and specialty medical societies in May, recommendations were outlined to eliminate physician roadblocks and encourage greater physician participation," said Dr. Stack. "We will carefully review the final rule and hope to see the changes we advocated for to promote widespread adoption and meaningful use of EHRs by physicians."
The rule also further clarifies certification criteria for EHRs, and modifies the certification program to "cut red tape and make the certification process more efficient," according to an HHS statement. All EHRs that have been certified under the 2011 rules can be used until 2014.
"The changes we’re announcing today will lead to more coordination of patient care, reduced medical errors, elimination of duplicate screenings and tests and greater patient engagement in their own care," said HHS Secretary Kathleen Sebelius in the statement.
FDA Approves Marqibo for Acute Lymphoblastic Leukemia
The Food and Drug Administration on Aug. 9 approved Marqibo, a liposomal encapsulated version of vincristine, to treat relapsed and refractory Philadelphia chromosome–negative acute lymphoblastic leukemia in adults.
Marqibo was approved for patients who have relapsed twice or more, or whose disease has failed at least two chemotherapy regimens. A nanoparticle formulation of vincristine that allows for dose-intensive treatment, it is manufactured by Talon Therapeutics of South San Francisco, Calif.
Acute lymphoblastic leukemia (ALL) is diagnosed in about 6,000 adults each year; the Philadelphia chromosome negative type is rare. Talon estimated that about 500 patients a year would be eligible for Marqibo therapy. The FDA designated it as an orphan drug.
"Marqibo provides an additional option for Philadelphia chromosome–negative acute lymphoblastic leukemia patients whose disease is unresponsive to available therapies," Dr. Richard Pazdur, director of the Office of Hematology and Oncology Products in the FDA’s Center for Drug Evaluation and Research, said in a statement.
The drug was approved under the agency’s accelerated approval regulations. The FDA said that the data showed that Marqibo had an effect on a surrogate end point – in this case, the response rate – that was likely to predict clinical benefit.
But Marqibo received lukewarm backing from the FDA’s Oncologic Drugs Advisory Committee in late March, in part because the panelists were not impressed with its efficacy.
According to the FDA’s approval statement, of 65 patients enrolled in a phase II study, 10 (15%) had either a complete remission or complete remission with incomplete blood count recovery. The median duration of remission was 28 days. The median time to the first event of relapse, death, or next therapy was 56 days, said the FDA.
The FDA advisers also were concerned about safety, noting that 76% of patients in trials had serious adverse events such as neutropenia, hypotension, respiratory distress, and cardiac arrest. The drug will carry a boxed warning that it should only be administered intravenously because it is deadly if administered in other ways, in particular into the spinal fluid.
The warning states that Marqibo has different dosage recommendations than does vincristine sulfate injection alone. To avoid overdose, drug name and dosing should be verified before administration, said the agency.
Talon said in a statement that the drug should be given at a dose of 2.25 mg/m2 intravenously over 1 hour once every 7 days.
"We are delighted that Marqibo will be available to a patient population with an underserved hematologic malignancy," Dr. Steven R. Deitcher, Talon president and chief executive officer, said in the statement.
The Food and Drug Administration on Aug. 9 approved Marqibo, a liposomal encapsulated version of vincristine, to treat relapsed and refractory Philadelphia chromosome–negative acute lymphoblastic leukemia in adults.
Marqibo was approved for patients who have relapsed twice or more, or whose disease has failed at least two chemotherapy regimens. A nanoparticle formulation of vincristine that allows for dose-intensive treatment, it is manufactured by Talon Therapeutics of South San Francisco, Calif.
Acute lymphoblastic leukemia (ALL) is diagnosed in about 6,000 adults each year; the Philadelphia chromosome negative type is rare. Talon estimated that about 500 patients a year would be eligible for Marqibo therapy. The FDA designated it as an orphan drug.
"Marqibo provides an additional option for Philadelphia chromosome–negative acute lymphoblastic leukemia patients whose disease is unresponsive to available therapies," Dr. Richard Pazdur, director of the Office of Hematology and Oncology Products in the FDA’s Center for Drug Evaluation and Research, said in a statement.
The drug was approved under the agency’s accelerated approval regulations. The FDA said that the data showed that Marqibo had an effect on a surrogate end point – in this case, the response rate – that was likely to predict clinical benefit.
But Marqibo received lukewarm backing from the FDA’s Oncologic Drugs Advisory Committee in late March, in part because the panelists were not impressed with its efficacy.
According to the FDA’s approval statement, of 65 patients enrolled in a phase II study, 10 (15%) had either a complete remission or complete remission with incomplete blood count recovery. The median duration of remission was 28 days. The median time to the first event of relapse, death, or next therapy was 56 days, said the FDA.
The FDA advisers also were concerned about safety, noting that 76% of patients in trials had serious adverse events such as neutropenia, hypotension, respiratory distress, and cardiac arrest. The drug will carry a boxed warning that it should only be administered intravenously because it is deadly if administered in other ways, in particular into the spinal fluid.
The warning states that Marqibo has different dosage recommendations than does vincristine sulfate injection alone. To avoid overdose, drug name and dosing should be verified before administration, said the agency.
Talon said in a statement that the drug should be given at a dose of 2.25 mg/m2 intravenously over 1 hour once every 7 days.
"We are delighted that Marqibo will be available to a patient population with an underserved hematologic malignancy," Dr. Steven R. Deitcher, Talon president and chief executive officer, said in the statement.
The Food and Drug Administration on Aug. 9 approved Marqibo, a liposomal encapsulated version of vincristine, to treat relapsed and refractory Philadelphia chromosome–negative acute lymphoblastic leukemia in adults.
Marqibo was approved for patients who have relapsed twice or more, or whose disease has failed at least two chemotherapy regimens. A nanoparticle formulation of vincristine that allows for dose-intensive treatment, it is manufactured by Talon Therapeutics of South San Francisco, Calif.
Acute lymphoblastic leukemia (ALL) is diagnosed in about 6,000 adults each year; the Philadelphia chromosome negative type is rare. Talon estimated that about 500 patients a year would be eligible for Marqibo therapy. The FDA designated it as an orphan drug.
"Marqibo provides an additional option for Philadelphia chromosome–negative acute lymphoblastic leukemia patients whose disease is unresponsive to available therapies," Dr. Richard Pazdur, director of the Office of Hematology and Oncology Products in the FDA’s Center for Drug Evaluation and Research, said in a statement.
The drug was approved under the agency’s accelerated approval regulations. The FDA said that the data showed that Marqibo had an effect on a surrogate end point – in this case, the response rate – that was likely to predict clinical benefit.
But Marqibo received lukewarm backing from the FDA’s Oncologic Drugs Advisory Committee in late March, in part because the panelists were not impressed with its efficacy.
According to the FDA’s approval statement, of 65 patients enrolled in a phase II study, 10 (15%) had either a complete remission or complete remission with incomplete blood count recovery. The median duration of remission was 28 days. The median time to the first event of relapse, death, or next therapy was 56 days, said the FDA.
The FDA advisers also were concerned about safety, noting that 76% of patients in trials had serious adverse events such as neutropenia, hypotension, respiratory distress, and cardiac arrest. The drug will carry a boxed warning that it should only be administered intravenously because it is deadly if administered in other ways, in particular into the spinal fluid.
The warning states that Marqibo has different dosage recommendations than does vincristine sulfate injection alone. To avoid overdose, drug name and dosing should be verified before administration, said the agency.
Talon said in a statement that the drug should be given at a dose of 2.25 mg/m2 intravenously over 1 hour once every 7 days.
"We are delighted that Marqibo will be available to a patient population with an underserved hematologic malignancy," Dr. Steven R. Deitcher, Talon president and chief executive officer, said in the statement.
Feds Investigating Interventional Cardiac Procedures at HCA
The nation’s largest hospital chain, Hospital Corporation of America, has acknowledged that it may be the subject of a federal inquiry into the appropriateness of interventional cardiology procedures at its hospitals in Florida.
The company said in a second quarter earnings call with investors that the U.S. Attorney’s office in Miami had requested information on the medical necessity of such services at 10 hospitals. The revelation came in advance of a lengthy Aug. 6 exposé in the New York Times about questionable cardiology practices at many of HCA’s hospitals.
HCA chairman and CEO Richard Bracken told investors that the company knew the article was going to appear, but was not sure of the exact content. Mr. Bracken also said that HCA would not answer any further questions, but directed investors to a statement on its website.
In that statement, the company said that it was difficult to determine medical necessity of cardiac catheterizations and percutaneous coronary interventions. "These physician-driven decisions have been and are the subject of much debate within the cardiology community," said the statement. Physicians may disagree among themselves, and experts may also not come to consensus, it said. Regarding the volume of the procedures, the company said that "trends for HCA-affiliated hospitals are similar to the rest of the nation for these procedures," and that the number of those procedures had actually declined at HCA-affiliated facilities.
Appropriateness of stenting and other percutaneous cardiac procedures has continued to attract attention, in part because of a Maryland cardiologist, Dr. Mark Midei, who was found to have inserted hundreds of stents unnecessarily, at a cost of millions to Medicare. Dr. Midei has since been the subject of multiple suits alleging harm.
Maryland is now the first state in the nation to have a law that attempts to regulate cardiac procedures. The legislation – signed into law in May by Gov. Martin O’Malley (D) – requires the state "to appoint a Clinical Advisory Group to establish regulations to write requirements for peer or independent review of the placement of stents in heart patients in order to ensure consistency with guidelines developed by the American College of Cardiology and other cardiovascular organizations," according to the Maryland chapter of the American College of Cardiology.
The nation’s largest hospital chain, Hospital Corporation of America, has acknowledged that it may be the subject of a federal inquiry into the appropriateness of interventional cardiology procedures at its hospitals in Florida.
The company said in a second quarter earnings call with investors that the U.S. Attorney’s office in Miami had requested information on the medical necessity of such services at 10 hospitals. The revelation came in advance of a lengthy Aug. 6 exposé in the New York Times about questionable cardiology practices at many of HCA’s hospitals.
HCA chairman and CEO Richard Bracken told investors that the company knew the article was going to appear, but was not sure of the exact content. Mr. Bracken also said that HCA would not answer any further questions, but directed investors to a statement on its website.
In that statement, the company said that it was difficult to determine medical necessity of cardiac catheterizations and percutaneous coronary interventions. "These physician-driven decisions have been and are the subject of much debate within the cardiology community," said the statement. Physicians may disagree among themselves, and experts may also not come to consensus, it said. Regarding the volume of the procedures, the company said that "trends for HCA-affiliated hospitals are similar to the rest of the nation for these procedures," and that the number of those procedures had actually declined at HCA-affiliated facilities.
Appropriateness of stenting and other percutaneous cardiac procedures has continued to attract attention, in part because of a Maryland cardiologist, Dr. Mark Midei, who was found to have inserted hundreds of stents unnecessarily, at a cost of millions to Medicare. Dr. Midei has since been the subject of multiple suits alleging harm.
Maryland is now the first state in the nation to have a law that attempts to regulate cardiac procedures. The legislation – signed into law in May by Gov. Martin O’Malley (D) – requires the state "to appoint a Clinical Advisory Group to establish regulations to write requirements for peer or independent review of the placement of stents in heart patients in order to ensure consistency with guidelines developed by the American College of Cardiology and other cardiovascular organizations," according to the Maryland chapter of the American College of Cardiology.
The nation’s largest hospital chain, Hospital Corporation of America, has acknowledged that it may be the subject of a federal inquiry into the appropriateness of interventional cardiology procedures at its hospitals in Florida.
The company said in a second quarter earnings call with investors that the U.S. Attorney’s office in Miami had requested information on the medical necessity of such services at 10 hospitals. The revelation came in advance of a lengthy Aug. 6 exposé in the New York Times about questionable cardiology practices at many of HCA’s hospitals.
HCA chairman and CEO Richard Bracken told investors that the company knew the article was going to appear, but was not sure of the exact content. Mr. Bracken also said that HCA would not answer any further questions, but directed investors to a statement on its website.
In that statement, the company said that it was difficult to determine medical necessity of cardiac catheterizations and percutaneous coronary interventions. "These physician-driven decisions have been and are the subject of much debate within the cardiology community," said the statement. Physicians may disagree among themselves, and experts may also not come to consensus, it said. Regarding the volume of the procedures, the company said that "trends for HCA-affiliated hospitals are similar to the rest of the nation for these procedures," and that the number of those procedures had actually declined at HCA-affiliated facilities.
Appropriateness of stenting and other percutaneous cardiac procedures has continued to attract attention, in part because of a Maryland cardiologist, Dr. Mark Midei, who was found to have inserted hundreds of stents unnecessarily, at a cost of millions to Medicare. Dr. Midei has since been the subject of multiple suits alleging harm.
Maryland is now the first state in the nation to have a law that attempts to regulate cardiac procedures. The legislation – signed into law in May by Gov. Martin O’Malley (D) – requires the state "to appoint a Clinical Advisory Group to establish regulations to write requirements for peer or independent review of the placement of stents in heart patients in order to ensure consistency with guidelines developed by the American College of Cardiology and other cardiovascular organizations," according to the Maryland chapter of the American College of Cardiology.
Preventive Services for Women Gain Coverage Under ACA
With new preventive health services under an Affordable Care Act requirement that went into effect on Aug. 1, more women may begin seeking health care and screenings.
For plans that begin Aug. 1 or later, most insurers will be required to cover mammograms, cervical cancer screening, and other preventive services without copayments, coinsurance, or deductibles. The covered services are based on recommendations made by the Institute of Medicine in July 2011.
The Department of Health and Human Services estimates that 47 million women are in health plans that will now have to cover the services.
"This law puts women and their doctors, not insurance companies or the government, in charge of health care decisions," HHS Secretary Kathleen Sebelius said in a statement.
Senator Barbara Mikulski (D-Md.), who sponsored a bill that called for the coverage and that eventually was incorporated into the ACA, said that the benefits will end discriminatory insurance practices, where women are "charged more but get less." She added, in a statement: "My amendment, and this law, was always about people, about access, about preventing deadly diseases, and about keeping the doors of doctors’ offices open to the women of America."
The benefit includes a once-yearly well-woman visit, in which the patient can access any or all of more than 20 preventive services. Among those are counseling and testing for sexually transmitted diseases, counseling about the BRCA genetic mutation, osteoporosis screening for women over age 60, a variety of counseling and testing for pregnant women, and breastfeeding support.
"An annual well-woman visit is a fundamental part of medical care and promotes prevention practices, recognizes risk factors for disease, identifies medical problems, and establishes the often life-long patient-physician relationship. This annual visit provides an excellent opportunity for ob.gyns. to counsel patients about maintaining a healthy lifestyle and minimizing health risks," ACOG President James T. Breeden said in a statement.
The coverage also includes contraception, which is defined as all Food and Drug Administration–approved methods and sterilization procedures.
That benefit was lauded by Dr. Breeden. "Planned pregnancies – for which most women require contraception – allow women to optimize their own health before pregnancy and childbirth, leading to healthier pregnancies and healthier babies," he said, adding that unintended pregnancy could worsen a preexisting health condition, such as diabetes, hypertension, or coronary artery disease.
"Planned pregnancies improve the health of children because adequate birth spacing reduces the risk of low birth weight and preterm birth," he added.
Contraception coverage was criticized, however, by others who said it violated religious freedom. "Through this mandate, the administration is promoting an approach to religious freedom that is more grudging and arbitrary than any yet seen in federal law," Cardinal Daniel DiNardo, chair of the U.S. Bishops’ Committee on Pro-Life Activities, said in a letter to members of the House and Senate, sent shortly after the benefits took effect.
The letter urged Congress to overturn this particular benefit and end free contraception coverage.
Cardinal DiNardo noted that Catholic business owners have filed suit – in Colorado, Pennsylvania, Missouri, and Michigan – to block the contraceptive coverage.
In late July, a federal judge in Colorado temporarily blocked the federal government from enforcing the mandate against Hercules Industries, which filed the suit.
Under the law, employers that do not comply can be penalized. But there is an exemption for nonprofit organizations with religious objections to contraceptive coverage. That exemption will last until 2014, when the ACA goes fully into effect.
At that time, among other provisions that will take effect, insurers will no longer be able to limit coverage of preexisting conditions. Women are the "poster children for why we need this," Sen. Benjamin Cardin (D-Md.) said at a Senate briefing announcing the new preventive services on Aug. 1.
Insurers also will not be allowed to charge women higher premiums based on their gender, he said.
With new preventive health services under an Affordable Care Act requirement that went into effect on Aug. 1, more women may begin seeking health care and screenings.
For plans that begin Aug. 1 or later, most insurers will be required to cover mammograms, cervical cancer screening, and other preventive services without copayments, coinsurance, or deductibles. The covered services are based on recommendations made by the Institute of Medicine in July 2011.
The Department of Health and Human Services estimates that 47 million women are in health plans that will now have to cover the services.
"This law puts women and their doctors, not insurance companies or the government, in charge of health care decisions," HHS Secretary Kathleen Sebelius said in a statement.
Senator Barbara Mikulski (D-Md.), who sponsored a bill that called for the coverage and that eventually was incorporated into the ACA, said that the benefits will end discriminatory insurance practices, where women are "charged more but get less." She added, in a statement: "My amendment, and this law, was always about people, about access, about preventing deadly diseases, and about keeping the doors of doctors’ offices open to the women of America."
The benefit includes a once-yearly well-woman visit, in which the patient can access any or all of more than 20 preventive services. Among those are counseling and testing for sexually transmitted diseases, counseling about the BRCA genetic mutation, osteoporosis screening for women over age 60, a variety of counseling and testing for pregnant women, and breastfeeding support.
"An annual well-woman visit is a fundamental part of medical care and promotes prevention practices, recognizes risk factors for disease, identifies medical problems, and establishes the often life-long patient-physician relationship. This annual visit provides an excellent opportunity for ob.gyns. to counsel patients about maintaining a healthy lifestyle and minimizing health risks," ACOG President James T. Breeden said in a statement.
The coverage also includes contraception, which is defined as all Food and Drug Administration–approved methods and sterilization procedures.
That benefit was lauded by Dr. Breeden. "Planned pregnancies – for which most women require contraception – allow women to optimize their own health before pregnancy and childbirth, leading to healthier pregnancies and healthier babies," he said, adding that unintended pregnancy could worsen a preexisting health condition, such as diabetes, hypertension, or coronary artery disease.
"Planned pregnancies improve the health of children because adequate birth spacing reduces the risk of low birth weight and preterm birth," he added.
Contraception coverage was criticized, however, by others who said it violated religious freedom. "Through this mandate, the administration is promoting an approach to religious freedom that is more grudging and arbitrary than any yet seen in federal law," Cardinal Daniel DiNardo, chair of the U.S. Bishops’ Committee on Pro-Life Activities, said in a letter to members of the House and Senate, sent shortly after the benefits took effect.
The letter urged Congress to overturn this particular benefit and end free contraception coverage.
Cardinal DiNardo noted that Catholic business owners have filed suit – in Colorado, Pennsylvania, Missouri, and Michigan – to block the contraceptive coverage.
In late July, a federal judge in Colorado temporarily blocked the federal government from enforcing the mandate against Hercules Industries, which filed the suit.
Under the law, employers that do not comply can be penalized. But there is an exemption for nonprofit organizations with religious objections to contraceptive coverage. That exemption will last until 2014, when the ACA goes fully into effect.
At that time, among other provisions that will take effect, insurers will no longer be able to limit coverage of preexisting conditions. Women are the "poster children for why we need this," Sen. Benjamin Cardin (D-Md.) said at a Senate briefing announcing the new preventive services on Aug. 1.
Insurers also will not be allowed to charge women higher premiums based on their gender, he said.
With new preventive health services under an Affordable Care Act requirement that went into effect on Aug. 1, more women may begin seeking health care and screenings.
For plans that begin Aug. 1 or later, most insurers will be required to cover mammograms, cervical cancer screening, and other preventive services without copayments, coinsurance, or deductibles. The covered services are based on recommendations made by the Institute of Medicine in July 2011.
The Department of Health and Human Services estimates that 47 million women are in health plans that will now have to cover the services.
"This law puts women and their doctors, not insurance companies or the government, in charge of health care decisions," HHS Secretary Kathleen Sebelius said in a statement.
Senator Barbara Mikulski (D-Md.), who sponsored a bill that called for the coverage and that eventually was incorporated into the ACA, said that the benefits will end discriminatory insurance practices, where women are "charged more but get less." She added, in a statement: "My amendment, and this law, was always about people, about access, about preventing deadly diseases, and about keeping the doors of doctors’ offices open to the women of America."
The benefit includes a once-yearly well-woman visit, in which the patient can access any or all of more than 20 preventive services. Among those are counseling and testing for sexually transmitted diseases, counseling about the BRCA genetic mutation, osteoporosis screening for women over age 60, a variety of counseling and testing for pregnant women, and breastfeeding support.
"An annual well-woman visit is a fundamental part of medical care and promotes prevention practices, recognizes risk factors for disease, identifies medical problems, and establishes the often life-long patient-physician relationship. This annual visit provides an excellent opportunity for ob.gyns. to counsel patients about maintaining a healthy lifestyle and minimizing health risks," ACOG President James T. Breeden said in a statement.
The coverage also includes contraception, which is defined as all Food and Drug Administration–approved methods and sterilization procedures.
That benefit was lauded by Dr. Breeden. "Planned pregnancies – for which most women require contraception – allow women to optimize their own health before pregnancy and childbirth, leading to healthier pregnancies and healthier babies," he said, adding that unintended pregnancy could worsen a preexisting health condition, such as diabetes, hypertension, or coronary artery disease.
"Planned pregnancies improve the health of children because adequate birth spacing reduces the risk of low birth weight and preterm birth," he added.
Contraception coverage was criticized, however, by others who said it violated religious freedom. "Through this mandate, the administration is promoting an approach to religious freedom that is more grudging and arbitrary than any yet seen in federal law," Cardinal Daniel DiNardo, chair of the U.S. Bishops’ Committee on Pro-Life Activities, said in a letter to members of the House and Senate, sent shortly after the benefits took effect.
The letter urged Congress to overturn this particular benefit and end free contraception coverage.
Cardinal DiNardo noted that Catholic business owners have filed suit – in Colorado, Pennsylvania, Missouri, and Michigan – to block the contraceptive coverage.
In late July, a federal judge in Colorado temporarily blocked the federal government from enforcing the mandate against Hercules Industries, which filed the suit.
Under the law, employers that do not comply can be penalized. But there is an exemption for nonprofit organizations with religious objections to contraceptive coverage. That exemption will last until 2014, when the ACA goes fully into effect.
At that time, among other provisions that will take effect, insurers will no longer be able to limit coverage of preexisting conditions. Women are the "poster children for why we need this," Sen. Benjamin Cardin (D-Md.) said at a Senate briefing announcing the new preventive services on Aug. 1.
Insurers also will not be allowed to charge women higher premiums based on their gender, he said.
In Massachusetts, Physicians Bearing Brunt of Reform Effort
Six years into Massachusetts’ ambitious effort to overhaul its health system, there are fewer uninsured residents but costs continue to rise. Physicians say that cost containment will be a major challenge going forward – and likely will hit them hard.
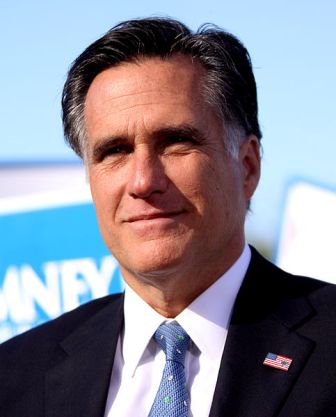
Signed into law in 2006 by then-Gov. Mitt Romney, the health reform program, called "An Act Providing Access to Affordable, Quality, Accountable Health Care," essentially requires all state residents to acquire health insurance. The state Medicaid program was expanded to cover those at higher income levels, and a health insurance exchange was created to offer private insurance to all others. The state completely covers plans for residents with incomes below 150% of the federal poverty level and subsidizes others up to 300% of the poverty level.
Those who do not buy insurance are charged a penalty on their state tax return, based on income.
The success or failure of the plan is being closely watched, as it is widely considered the model for the federal Affordable Care Act.
Now, almost 98% of adults and close to 100% of children in Massachusetts have health insurance, Dr. JudyAnn Bigby, health and human services secretary for the commonwealth, said at a recent presentation in Washington.
With better and more regular access to care, more residents are receiving preventive services.
"Our rates of screening for colon cancer, cervical cancer, [and] prostate cancer have all gone up significantly," Dr. Bigby said, adding that "we also know people are getting better care for diabetes." Emergency department visits for nonurgent conditions also have declined, especially for patients with asthma and chronic obstructive pulmonary disease.
Reform has been mostly well-received by both doctors and patients. A 2011 poll by the Harvard School of Public Health and the Boston Globe found that 63% of residents said they supported the law.
A 2009 poll of physicians found similar views. Of 2,125 respondents, 70% said they thought reform had been a good thing.
However, in spite of all the positives, 50% said that the medical practice environment had worsened since reform. The biggest complaint: the law‘s administrative burden.
Dr. Joseph W. Gravel Jr., president of the Massachusetts Academy of Family Physicians, agreed, adding that his practice employs a huge number of people just to do paperwork. It seems that "paperwork is used almost as a cost reduction strategy, it seems sometimes to a primary care doctor," he said in an interview.
Physicians in the Harvard survey also expressed concerns about rising costs, and were split on the law’s impact on access to primary care: Roughly a quarter said the law was hurting access, whereas the same number said it was helping.
The concept behind the reform law "was brilliant," because it increased insurance coverage and gave patients incentives to get preventive care, said Dr. Richard Dupee, governor of the Massachusetts chapter of the American College of Physicians. But at the same time, he said, the law "discincentivizes doctors from seeing patients because the reimbursement is so poor."
Dr. Louis Kuchnir, president of the Massachusetts Academy of Dermatology, said that although the law has increased the number of people with coverage, they do not have any better access to dermatology care.
"Very few dermatologists can afford to participate," he said in an interview. The reimbursement for Medicaid and the state-subsidized plan "is less than our overhead in many cases."
And with the law’s cost-containment requirements now on the books, things may get worse. Dr. Dupee said that "the handwriting is on the wall: Reimbursement is going to start going down across the board. Otherwise, there is no way to manage the cost of this thing."
Cost Containment Lags
No rigorous cost controls were included in the reform plan when implementation started. The intention was to get everyone covered first and then begin looking at the cost side of the equation.
A 2008 addition to the law began laying the groundwork for cost control by setting up several councils to study how best to rein in spending. The main work is in a 2011 proposal by Gov. Deval Patrick (D), which urged a shift from fee for service to global payment for state employees, Medicaid recipients, and enrollees in the Commonwealth Care program. Those groups account for about 25% of the state’s residents.
The law will also establish a new primary care residency program, supported by the state’s Department of Public Health, to increase the number of such physicians.
In addition, in June, Gov. Patrick signed into law a $32.5 billion budget for fiscal 2013 that mandates some $700 million in savings in health care.
Gov. Patrick estimated in a recent speech that the state spends $67 billion a year on health care and that it would account for 54% of the state’s budget in the fiscal year that ended June 30, with most of it going to the state’s Medicaid program, and to subsidies for Commonwealth Care.
Health costs have been and still are higher in Massachusetts than almost anywhere else in America. The average total medical expenditure in the commercial market was $414 per member per month in 2010, which was a 3% increase over 2009 expenditures, according to the commonwealth’s division of health care finance and policy. Not huge, but a growing burden.
The state’s Division of Health Care Finance and Policy said that premium increases slowed from 2008 to 2010, but still grew 7.5% in the commercial market. But that slowdown likely merely reflects cost shifting, said the agency, adding that employers are providing fewer benefits and charging higher copays. And that is potentially translating to reduced care, Dr. Kuchnir said.
State residents with private insurance "seem to be getting less and paying more, which is of course a negative for good medical care and for access," said Dr. Kuchnir.
Costs are partly being driven by an overreliance on tertiary medical centers, said Dr. Gravel. The majority of inpatient care is given at tertiary – not community – hospitals, he said.
Indeed, the state’s Division of Health Care Finance and Policy determined that inpatient hospital expenses grew 9% in 2010, more than any other spending category.
Transitioning From Fee for Service
Dr. Gravel also blamed the continued dominance of the fee-for-service system for continued rising costs.
Physician expenses grew only 2% in 2010, according to the Division of Health Care Finance and Policy. But expenses varied significantly, depending on location and size of the physician group, according to data collected by the agency.
Gov. Patrick has encouraged the development of ACOs (Accountable Care Organizations) and new payment models to address variation and to create higher quality, more-efficient care. One model that seems to be making a difference is the Alternative Quality Contract, developed by Blue Cross Blue Shield of Massachusetts. In 2009, BCBSMA struck global payment agreements under the AQC with seven organizations; four more joined in 2010, and in March, Boston Medical Center joined. At that time, the Blues said that two-thirds of the physicians in its in-state HMO network, who provided care to 76% of its members, were covered under an AQC. The contract is for 5 years and is similar to a patient-centered medical home, where patients are assigned primary care physicians.
The AQC physicians "now significantly outperform the rest of BCBSMA’s fee-for-service network on a comprehensive set of quality and outcome measures," said a Blues release.
A recent study in Health Affairs seemed to back that assertion (2012 July [doi:10.1377/hlthaff.2012.0327]). The biggest gains so far were in the second year of the contracts; the same was true for savings, which were 1.9% in the first year and 3.3% in the second year, when compared with nonparticipating physicians. The results suggest that global payments work to reduce costs, but that that providers needed time to adjust to the global budgeting, according to the study.
Harvard Pilgrim Health Care, the second-largest insurer with 733,000 enrollees, and Tufts Health Plan have also recently negotiated global payment contracts with their provider networks.
Dr. Dupee, who is chief of the geriatrics service at Tufts Medical Center, Boston, said that the AQC model can work only for physicians who are part of an ACO. "You have to have the data," he said, adding that without an electronic health record, it’s not easy to determine who’s due for a mammogram or whose hemoglobin A1C level is controlled.
The shift to global payment will likely hasten the demise of solo and small private practices, he said.
How Does It Work in Massachusetts?
Most Massachusetts residents now have some kind of health insurance. As of the end of 2010 (the latest figures available), 411,000 residents had gained coverage under the health care reform law, according to the commonwealth’s Division of Health Care Finance and Policy. About 5.4 million of the state’s 6.5 million residents were covered.
Plans are chosen through the health insurance exchange, called the Commonwealth Health Insurance Connector. Those plans include the following:
• Commonwealth Care. Open to anyone with an income of up to 300% of the federal poverty line. The state subsidizes their coverage and pays for coverage for those with incomes up to 150% of the poverty line.
• Commonwealth Choice. Plans – rated bronze, silver, or gold – must meet certain coverage and cost standards.
• Mass Health. This is the state Medicaid plan, which covers children in families up to 300% of the poverty level.
As is the case in the U.S. Affordable Care Act, there are disincentives for residents and employers to go without health coverage. Employers with 11 or more workers must either cover their workers or pay the state a contribution of up to $295 per year per worker.
Adults with incomes greater than 150% of the poverty level must either buy insurance or pay a penalty. In 2011, penalties ranged from $19 to $101 a month.
As more residents gain coverage, the number paying the penalty has decreased: In 2008, 45,000 paid; in 2010, 44,000 were assessed a penalty.
Can the Workforce Keep Up?
Many private practice physicians – especially those in primary care – are also struggling to meet demand.
Dr. Bigby, the state HHS secretary, said that fears about a primary care shortage had not been realized. Within a year of the reform’s being enacted, the state’s community health system had increased physician and nurse practitioner appointments by 50,000 visits, she said. But Dr. Gravel and Dr. Dupee said there was a continued shortage of primary care doctors, and that there were gaps in access. Hospitals have not increased the number of training slots over the last 6 years, they said.
"The hospitals have been slow to transform their training to primary care because the basic incentives have been to produce specialists," said Dr. Gravel, director for the Lawrence (Mass.) Family Medicine Residency program.
Primary care residents generate less clinical revenue, and cost more to train, said Dr. Gravel. The Affordable Care Act made it possible for his program to expand from 8 residents to 10. But state funds for family medicine training were reduced 3 years ago.
When residents finish training, they are not as interested in private practice, said Dr. Dupee. Instead, they go to work for hospitals or community clinics, where they have a guaranteed salary and less administrative hassle.
There are no clinics in many areas of the state, such as between Boston and Worcester, or between Worcester and Springfield, said Dr. Dupee. "Rural areas are underserved and will continue to be until something is done about it," he said.
Both he and Dr. Gravel also said that they believe many primary care physicians in their 50s will be retiring sooner rather than later, driven out by the shift out of fee for service.
Dr. Kuchnir agreed that private practices were threatened, mostly by the lower reimbursement offered by state plans. It’s not a question of having enough physicians to meet the demand for care, but whether the compensation is enough for practices to survive, he said.
He and the other physicians agreed, however, that it was a good thing that most state residents could now get insurance, because they can now also get needed care.
And unlike other states, the doctor is not "left holding the bag when patients can’t get what they need," said Dr. Gravel.
Six years into Massachusetts’ ambitious effort to overhaul its health system, there are fewer uninsured residents but costs continue to rise. Physicians say that cost containment will be a major challenge going forward – and likely will hit them hard.
Signed into law in 2006 by then-Gov. Mitt Romney, the health reform program, called "An Act Providing Access to Affordable, Quality, Accountable Health Care," essentially requires all state residents to acquire health insurance. The state Medicaid program was expanded to cover those at higher income levels, and a health insurance exchange was created to offer private insurance to all others. The state completely covers plans for residents with incomes below 150% of the federal poverty level and subsidizes others up to 300% of the poverty level.
Those who do not buy insurance are charged a penalty on their state tax return, based on income.
The success or failure of the plan is being closely watched, as it is widely considered the model for the federal Affordable Care Act.
Now, almost 98% of adults and close to 100% of children in Massachusetts have health insurance, Dr. JudyAnn Bigby, health and human services secretary for the commonwealth, said at a recent presentation in Washington.
With better and more regular access to care, more residents are receiving preventive services.
"Our rates of screening for colon cancer, cervical cancer, [and] prostate cancer have all gone up significantly," Dr. Bigby said, adding that "we also know people are getting better care for diabetes." Emergency department visits for nonurgent conditions also have declined, especially for patients with asthma and chronic obstructive pulmonary disease.
Reform has been mostly well-received by both doctors and patients. A 2011 poll by the Harvard School of Public Health and the Boston Globe found that 63% of residents said they supported the law.
A 2009 poll of physicians found similar views. Of 2,125 respondents, 70% said they thought reform had been a good thing.
However, in spite of all the positives, 50% said that the medical practice environment had worsened since reform. The biggest complaint: the law‘s administrative burden.
Dr. Joseph W. Gravel Jr., president of the Massachusetts Academy of Family Physicians, agreed, adding that his practice employs a huge number of people just to do paperwork. It seems that "paperwork is used almost as a cost reduction strategy, it seems sometimes to a primary care doctor," he said in an interview.
Physicians in the Harvard survey also expressed concerns about rising costs, and were split on the law’s impact on access to primary care: Roughly a quarter said the law was hurting access, whereas the same number said it was helping.
The concept behind the reform law "was brilliant," because it increased insurance coverage and gave patients incentives to get preventive care, said Dr. Richard Dupee, governor of the Massachusetts chapter of the American College of Physicians. But at the same time, he said, the law "discincentivizes doctors from seeing patients because the reimbursement is so poor."
Dr. Louis Kuchnir, president of the Massachusetts Academy of Dermatology, said that although the law has increased the number of people with coverage, they do not have any better access to dermatology care.
"Very few dermatologists can afford to participate," he said in an interview. The reimbursement for Medicaid and the state-subsidized plan "is less than our overhead in many cases."
And with the law’s cost-containment requirements now on the books, things may get worse. Dr. Dupee said that "the handwriting is on the wall: Reimbursement is going to start going down across the board. Otherwise, there is no way to manage the cost of this thing."
Cost Containment Lags
No rigorous cost controls were included in the reform plan when implementation started. The intention was to get everyone covered first and then begin looking at the cost side of the equation.
A 2008 addition to the law began laying the groundwork for cost control by setting up several councils to study how best to rein in spending. The main work is in a 2011 proposal by Gov. Deval Patrick (D), which urged a shift from fee for service to global payment for state employees, Medicaid recipients, and enrollees in the Commonwealth Care program. Those groups account for about 25% of the state’s residents.
The law will also establish a new primary care residency program, supported by the state’s Department of Public Health, to increase the number of such physicians.
In addition, in June, Gov. Patrick signed into law a $32.5 billion budget for fiscal 2013 that mandates some $700 million in savings in health care.
Gov. Patrick estimated in a recent speech that the state spends $67 billion a year on health care and that it would account for 54% of the state’s budget in the fiscal year that ended June 30, with most of it going to the state’s Medicaid program, and to subsidies for Commonwealth Care.
Health costs have been and still are higher in Massachusetts than almost anywhere else in America. The average total medical expenditure in the commercial market was $414 per member per month in 2010, which was a 3% increase over 2009 expenditures, according to the commonwealth’s division of health care finance and policy. Not huge, but a growing burden.
The state’s Division of Health Care Finance and Policy said that premium increases slowed from 2008 to 2010, but still grew 7.5% in the commercial market. But that slowdown likely merely reflects cost shifting, said the agency, adding that employers are providing fewer benefits and charging higher copays. And that is potentially translating to reduced care, Dr. Kuchnir said.
State residents with private insurance "seem to be getting less and paying more, which is of course a negative for good medical care and for access," said Dr. Kuchnir.
Costs are partly being driven by an overreliance on tertiary medical centers, said Dr. Gravel. The majority of inpatient care is given at tertiary – not community – hospitals, he said.
Indeed, the state’s Division of Health Care Finance and Policy determined that inpatient hospital expenses grew 9% in 2010, more than any other spending category.
Transitioning From Fee for Service
Dr. Gravel also blamed the continued dominance of the fee-for-service system for continued rising costs.
Physician expenses grew only 2% in 2010, according to the Division of Health Care Finance and Policy. But expenses varied significantly, depending on location and size of the physician group, according to data collected by the agency.
Gov. Patrick has encouraged the development of ACOs (Accountable Care Organizations) and new payment models to address variation and to create higher quality, more-efficient care. One model that seems to be making a difference is the Alternative Quality Contract, developed by Blue Cross Blue Shield of Massachusetts. In 2009, BCBSMA struck global payment agreements under the AQC with seven organizations; four more joined in 2010, and in March, Boston Medical Center joined. At that time, the Blues said that two-thirds of the physicians in its in-state HMO network, who provided care to 76% of its members, were covered under an AQC. The contract is for 5 years and is similar to a patient-centered medical home, where patients are assigned primary care physicians.
The AQC physicians "now significantly outperform the rest of BCBSMA’s fee-for-service network on a comprehensive set of quality and outcome measures," said a Blues release.
A recent study in Health Affairs seemed to back that assertion (2012 July [doi:10.1377/hlthaff.2012.0327]). The biggest gains so far were in the second year of the contracts; the same was true for savings, which were 1.9% in the first year and 3.3% in the second year, when compared with nonparticipating physicians. The results suggest that global payments work to reduce costs, but that that providers needed time to adjust to the global budgeting, according to the study.
Harvard Pilgrim Health Care, the second-largest insurer with 733,000 enrollees, and Tufts Health Plan have also recently negotiated global payment contracts with their provider networks.
Dr. Dupee, who is chief of the geriatrics service at Tufts Medical Center, Boston, said that the AQC model can work only for physicians who are part of an ACO. "You have to have the data," he said, adding that without an electronic health record, it’s not easy to determine who’s due for a mammogram or whose hemoglobin A1C level is controlled.
The shift to global payment will likely hasten the demise of solo and small private practices, he said.
How Does It Work in Massachusetts?
Most Massachusetts residents now have some kind of health insurance. As of the end of 2010 (the latest figures available), 411,000 residents had gained coverage under the health care reform law, according to the commonwealth’s Division of Health Care Finance and Policy. About 5.4 million of the state’s 6.5 million residents were covered.
Plans are chosen through the health insurance exchange, called the Commonwealth Health Insurance Connector. Those plans include the following:
• Commonwealth Care. Open to anyone with an income of up to 300% of the federal poverty line. The state subsidizes their coverage and pays for coverage for those with incomes up to 150% of the poverty line.
• Commonwealth Choice. Plans – rated bronze, silver, or gold – must meet certain coverage and cost standards.
• Mass Health. This is the state Medicaid plan, which covers children in families up to 300% of the poverty level.
As is the case in the U.S. Affordable Care Act, there are disincentives for residents and employers to go without health coverage. Employers with 11 or more workers must either cover their workers or pay the state a contribution of up to $295 per year per worker.
Adults with incomes greater than 150% of the poverty level must either buy insurance or pay a penalty. In 2011, penalties ranged from $19 to $101 a month.
As more residents gain coverage, the number paying the penalty has decreased: In 2008, 45,000 paid; in 2010, 44,000 were assessed a penalty.
Can the Workforce Keep Up?
Many private practice physicians – especially those in primary care – are also struggling to meet demand.
Dr. Bigby, the state HHS secretary, said that fears about a primary care shortage had not been realized. Within a year of the reform’s being enacted, the state’s community health system had increased physician and nurse practitioner appointments by 50,000 visits, she said. But Dr. Gravel and Dr. Dupee said there was a continued shortage of primary care doctors, and that there were gaps in access. Hospitals have not increased the number of training slots over the last 6 years, they said.
"The hospitals have been slow to transform their training to primary care because the basic incentives have been to produce specialists," said Dr. Gravel, director for the Lawrence (Mass.) Family Medicine Residency program.
Primary care residents generate less clinical revenue, and cost more to train, said Dr. Gravel. The Affordable Care Act made it possible for his program to expand from 8 residents to 10. But state funds for family medicine training were reduced 3 years ago.
When residents finish training, they are not as interested in private practice, said Dr. Dupee. Instead, they go to work for hospitals or community clinics, where they have a guaranteed salary and less administrative hassle.
There are no clinics in many areas of the state, such as between Boston and Worcester, or between Worcester and Springfield, said Dr. Dupee. "Rural areas are underserved and will continue to be until something is done about it," he said.
Both he and Dr. Gravel also said that they believe many primary care physicians in their 50s will be retiring sooner rather than later, driven out by the shift out of fee for service.
Dr. Kuchnir agreed that private practices were threatened, mostly by the lower reimbursement offered by state plans. It’s not a question of having enough physicians to meet the demand for care, but whether the compensation is enough for practices to survive, he said.
He and the other physicians agreed, however, that it was a good thing that most state residents could now get insurance, because they can now also get needed care.
And unlike other states, the doctor is not "left holding the bag when patients can’t get what they need," said Dr. Gravel.
Six years into Massachusetts’ ambitious effort to overhaul its health system, there are fewer uninsured residents but costs continue to rise. Physicians say that cost containment will be a major challenge going forward – and likely will hit them hard.
Signed into law in 2006 by then-Gov. Mitt Romney, the health reform program, called "An Act Providing Access to Affordable, Quality, Accountable Health Care," essentially requires all state residents to acquire health insurance. The state Medicaid program was expanded to cover those at higher income levels, and a health insurance exchange was created to offer private insurance to all others. The state completely covers plans for residents with incomes below 150% of the federal poverty level and subsidizes others up to 300% of the poverty level.
Those who do not buy insurance are charged a penalty on their state tax return, based on income.
The success or failure of the plan is being closely watched, as it is widely considered the model for the federal Affordable Care Act.
Now, almost 98% of adults and close to 100% of children in Massachusetts have health insurance, Dr. JudyAnn Bigby, health and human services secretary for the commonwealth, said at a recent presentation in Washington.
With better and more regular access to care, more residents are receiving preventive services.
"Our rates of screening for colon cancer, cervical cancer, [and] prostate cancer have all gone up significantly," Dr. Bigby said, adding that "we also know people are getting better care for diabetes." Emergency department visits for nonurgent conditions also have declined, especially for patients with asthma and chronic obstructive pulmonary disease.
Reform has been mostly well-received by both doctors and patients. A 2011 poll by the Harvard School of Public Health and the Boston Globe found that 63% of residents said they supported the law.
A 2009 poll of physicians found similar views. Of 2,125 respondents, 70% said they thought reform had been a good thing.
However, in spite of all the positives, 50% said that the medical practice environment had worsened since reform. The biggest complaint: the law‘s administrative burden.
Dr. Joseph W. Gravel Jr., president of the Massachusetts Academy of Family Physicians, agreed, adding that his practice employs a huge number of people just to do paperwork. It seems that "paperwork is used almost as a cost reduction strategy, it seems sometimes to a primary care doctor," he said in an interview.
Physicians in the Harvard survey also expressed concerns about rising costs, and were split on the law’s impact on access to primary care: Roughly a quarter said the law was hurting access, whereas the same number said it was helping.
The concept behind the reform law "was brilliant," because it increased insurance coverage and gave patients incentives to get preventive care, said Dr. Richard Dupee, governor of the Massachusetts chapter of the American College of Physicians. But at the same time, he said, the law "discincentivizes doctors from seeing patients because the reimbursement is so poor."
Dr. Louis Kuchnir, president of the Massachusetts Academy of Dermatology, said that although the law has increased the number of people with coverage, they do not have any better access to dermatology care.
"Very few dermatologists can afford to participate," he said in an interview. The reimbursement for Medicaid and the state-subsidized plan "is less than our overhead in many cases."
And with the law’s cost-containment requirements now on the books, things may get worse. Dr. Dupee said that "the handwriting is on the wall: Reimbursement is going to start going down across the board. Otherwise, there is no way to manage the cost of this thing."
Cost Containment Lags
No rigorous cost controls were included in the reform plan when implementation started. The intention was to get everyone covered first and then begin looking at the cost side of the equation.
A 2008 addition to the law began laying the groundwork for cost control by setting up several councils to study how best to rein in spending. The main work is in a 2011 proposal by Gov. Deval Patrick (D), which urged a shift from fee for service to global payment for state employees, Medicaid recipients, and enrollees in the Commonwealth Care program. Those groups account for about 25% of the state’s residents.
The law will also establish a new primary care residency program, supported by the state’s Department of Public Health, to increase the number of such physicians.
In addition, in June, Gov. Patrick signed into law a $32.5 billion budget for fiscal 2013 that mandates some $700 million in savings in health care.
Gov. Patrick estimated in a recent speech that the state spends $67 billion a year on health care and that it would account for 54% of the state’s budget in the fiscal year that ended June 30, with most of it going to the state’s Medicaid program, and to subsidies for Commonwealth Care.
Health costs have been and still are higher in Massachusetts than almost anywhere else in America. The average total medical expenditure in the commercial market was $414 per member per month in 2010, which was a 3% increase over 2009 expenditures, according to the commonwealth’s division of health care finance and policy. Not huge, but a growing burden.
The state’s Division of Health Care Finance and Policy said that premium increases slowed from 2008 to 2010, but still grew 7.5% in the commercial market. But that slowdown likely merely reflects cost shifting, said the agency, adding that employers are providing fewer benefits and charging higher copays. And that is potentially translating to reduced care, Dr. Kuchnir said.
State residents with private insurance "seem to be getting less and paying more, which is of course a negative for good medical care and for access," said Dr. Kuchnir.
Costs are partly being driven by an overreliance on tertiary medical centers, said Dr. Gravel. The majority of inpatient care is given at tertiary – not community – hospitals, he said.
Indeed, the state’s Division of Health Care Finance and Policy determined that inpatient hospital expenses grew 9% in 2010, more than any other spending category.
Transitioning From Fee for Service
Dr. Gravel also blamed the continued dominance of the fee-for-service system for continued rising costs.
Physician expenses grew only 2% in 2010, according to the Division of Health Care Finance and Policy. But expenses varied significantly, depending on location and size of the physician group, according to data collected by the agency.
Gov. Patrick has encouraged the development of ACOs (Accountable Care Organizations) and new payment models to address variation and to create higher quality, more-efficient care. One model that seems to be making a difference is the Alternative Quality Contract, developed by Blue Cross Blue Shield of Massachusetts. In 2009, BCBSMA struck global payment agreements under the AQC with seven organizations; four more joined in 2010, and in March, Boston Medical Center joined. At that time, the Blues said that two-thirds of the physicians in its in-state HMO network, who provided care to 76% of its members, were covered under an AQC. The contract is for 5 years and is similar to a patient-centered medical home, where patients are assigned primary care physicians.
The AQC physicians "now significantly outperform the rest of BCBSMA’s fee-for-service network on a comprehensive set of quality and outcome measures," said a Blues release.
A recent study in Health Affairs seemed to back that assertion (2012 July [doi:10.1377/hlthaff.2012.0327]). The biggest gains so far were in the second year of the contracts; the same was true for savings, which were 1.9% in the first year and 3.3% in the second year, when compared with nonparticipating physicians. The results suggest that global payments work to reduce costs, but that that providers needed time to adjust to the global budgeting, according to the study.
Harvard Pilgrim Health Care, the second-largest insurer with 733,000 enrollees, and Tufts Health Plan have also recently negotiated global payment contracts with their provider networks.
Dr. Dupee, who is chief of the geriatrics service at Tufts Medical Center, Boston, said that the AQC model can work only for physicians who are part of an ACO. "You have to have the data," he said, adding that without an electronic health record, it’s not easy to determine who’s due for a mammogram or whose hemoglobin A1C level is controlled.
The shift to global payment will likely hasten the demise of solo and small private practices, he said.
How Does It Work in Massachusetts?
Most Massachusetts residents now have some kind of health insurance. As of the end of 2010 (the latest figures available), 411,000 residents had gained coverage under the health care reform law, according to the commonwealth’s Division of Health Care Finance and Policy. About 5.4 million of the state’s 6.5 million residents were covered.
Plans are chosen through the health insurance exchange, called the Commonwealth Health Insurance Connector. Those plans include the following:
• Commonwealth Care. Open to anyone with an income of up to 300% of the federal poverty line. The state subsidizes their coverage and pays for coverage for those with incomes up to 150% of the poverty line.
• Commonwealth Choice. Plans – rated bronze, silver, or gold – must meet certain coverage and cost standards.
• Mass Health. This is the state Medicaid plan, which covers children in families up to 300% of the poverty level.
As is the case in the U.S. Affordable Care Act, there are disincentives for residents and employers to go without health coverage. Employers with 11 or more workers must either cover their workers or pay the state a contribution of up to $295 per year per worker.
Adults with incomes greater than 150% of the poverty level must either buy insurance or pay a penalty. In 2011, penalties ranged from $19 to $101 a month.
As more residents gain coverage, the number paying the penalty has decreased: In 2008, 45,000 paid; in 2010, 44,000 were assessed a penalty.
Can the Workforce Keep Up?
Many private practice physicians – especially those in primary care – are also struggling to meet demand.
Dr. Bigby, the state HHS secretary, said that fears about a primary care shortage had not been realized. Within a year of the reform’s being enacted, the state’s community health system had increased physician and nurse practitioner appointments by 50,000 visits, she said. But Dr. Gravel and Dr. Dupee said there was a continued shortage of primary care doctors, and that there were gaps in access. Hospitals have not increased the number of training slots over the last 6 years, they said.
"The hospitals have been slow to transform their training to primary care because the basic incentives have been to produce specialists," said Dr. Gravel, director for the Lawrence (Mass.) Family Medicine Residency program.
Primary care residents generate less clinical revenue, and cost more to train, said Dr. Gravel. The Affordable Care Act made it possible for his program to expand from 8 residents to 10. But state funds for family medicine training were reduced 3 years ago.
When residents finish training, they are not as interested in private practice, said Dr. Dupee. Instead, they go to work for hospitals or community clinics, where they have a guaranteed salary and less administrative hassle.
There are no clinics in many areas of the state, such as between Boston and Worcester, or between Worcester and Springfield, said Dr. Dupee. "Rural areas are underserved and will continue to be until something is done about it," he said.
Both he and Dr. Gravel also said that they believe many primary care physicians in their 50s will be retiring sooner rather than later, driven out by the shift out of fee for service.
Dr. Kuchnir agreed that private practices were threatened, mostly by the lower reimbursement offered by state plans. It’s not a question of having enough physicians to meet the demand for care, but whether the compensation is enough for practices to survive, he said.
He and the other physicians agreed, however, that it was a good thing that most state residents could now get insurance, because they can now also get needed care.
And unlike other states, the doctor is not "left holding the bag when patients can’t get what they need," said Dr. Gravel.
SUSP Program Launched to Cut Surgical Site Infections
A new program being spearheaded by surgeons at Johns Hopkins University, Baltimore, and patient safety experts aims to dramatically reduce surgical site infections, which occur in almost a third of colorectal procedures and are a major reason for readmissions.
According to a fact sheet on the Surgical Unit-Based Safety Program (SUSP), each year about 50 million people undergo surgery in the United States. Of those, 1 million develop serious complications and more than 150,000 die within 30 days.
The goals of SUSP are to reduce surgical site infections (SSIs), to document use of checklistlike methods to improve safety, and to document the culture of safety through use of the Hospital Survey of Patient Safety Culture.
SUSP is designed to build on the success of the Comprehensive Unit-Based Safety Program (CUSP), which was developed by the Johns Hopkins Armstrong Institute for Patient Safety and Quality. Results of the CUSP program were recently reported in the Journal of the American College of Surgeons.
The CUSP Study
After CUSP was adopted in 2009 by colorectal surgeons at Johns Hopkins, colorectal surgical site infections were reduced by a third in the first year and saved the hospital $168,000-$280,000, according to the study (J. Am. Coll. Surg. 2012;215:193-200).
Surgical site infections occur in 15%-30% of colorectal procedures and lead to as much as $1 billion in costs for longer admissions, readmissions, and treatment.
"Until now, there’s been little evidence on how to effectively address SSIs among this group of patients," said Dr. Elizabeth Wick of the department of surgery at Johns Hopkins, who was the lead investigator.
Dr. Wick and her associates analyzed outcomes after implementation of CUSP, which was developed by Dr. Peter Pronovost, director of the Armstrong Institute at Hopkins
The Hopkins colorectal CUSP team of 36 people included a representative from surgery, nursing, and anesthesia; a team coach; and a hospital executive who was committed to helping the project, according to the researchers.
After attending a lecture on patient safety, all members of the team completed an anonymous two-question assessment that asked how an SSI might develop in the next patient and what could be done to prevent it.
The team identified 95 areas of concern and picked six interventions to focus on to improve care: standardization of skin preparation and prescription of chlorhexidine showers; restricted use of oral bowel-cleansing solution before a procedure; warming of patients in the preanesthesia area; adoption of enhanced sterile techniques for bowel and skin; and addressing lapses in preoperative prophylactic antibiotics.
The team met monthly, using checklists and monitoring progress to address problems quickly. "The benefits of a bottom-up vs. a top-down approach to patient safety were immediately obvious," said Dr. Wick in a statement.
The study consisted of all consecutive colorectal surgery patients who were included in the American College of Surgeons’ NSQIP (National Surgical Quality Improvement Program) from July 2009 to July 2011. Procedures included open and laparoscopic colectomies and proctectomies, but not abdominal perineal resections. SSI rates that were collected using NSQIP were compared from the first year (2009-2010) to the second year (2010-2011); there were 278 patients in the first cohort and 324 in the second.
During that first year, the 27% (76) of patients had an SSI. By the second year, only 18% (59) of patients had an infection, for a decrease of 33%.
The authors said that CUSP seems to be effective, in part because it bridges the divide between frontline staff and senior leaders. The NSQIP outcome measures also helped the team to effectively monitor SSI rates, said the authors.
CUSP/SUSP in Practice
The CUSP model has been applied successfully to decrease central line–associated bloodstream infections in the intensive care unit, as well as to cut mortality and length of stay in a statewide program, the MHA (Michigan Health and Hospital Association) Keystone Intensive Care Unit project.
The elements of CUSP are not well validated in the operating room, however, and there’s little data on how the program could potentially impact other types of infections or complications – even though the program is in use at 1,200 ICUs in 47 states, said Dr. Sean M. Berenholtz, physician director of inpatient quality and safety at the Armstrong Institute. The aim of the SUSP is to adapt the CUSP practices to the OR, Dr. Berenholtz said in an interview.
Project teams consisting of experts from the Agency for Healthcare Research and Quality (AHRQ), the Armstrong Institute, the American College of Surgeons, the University of Pennsylvania in Philadelphia, and the World Health Organization’s Patient Safety Programme will assist SUSP participants.
The CUSP model combines knowledge from both clinical science and social science. The first step is to educate staff on the science of patient safety – most importantly, communicating the idea that "the vast majority of preventable complications don’t belong to an individual surgeon or an individual nurse," but occur within the organization of the health care system, Dr. Berenholtz said.
The project leaders then ask the staff to complete an anonymous, two-question assessment that gauges their experience of how complications develop and what might be done to prevent them. Next, a unit-based improvement team is assigned an executive partner from the Armstrong Institute who meets with the team at least monthly to help prioritize improvement efforts and lead them through any bureaucratic hurdles they may face at their hospitals. Goals are set and agreed upon.
The team then tries to learn from "defects" within the process, and identifies ways to prevent mistakes, especially among the surgeons, nurses, anesthesiologists, and technicians who work in the OR. Finally, tools such as checklists are used to foster teamwork and improvement. SUSP leaders will ask improvement teams to use "briefings" and "debriefings" to learn from mistakes and move forward.
There’s plenty of motivation for hospitals to want to reduce SSIs. The Centers for Medicare and Medicaid Services, as part of the Surgical Care Improvement Project (SCIP), requires public reporting of surgical quality measures, including SSIs.
For instance, hospitals are supposed to report whether patients are given the right antibiotic at the right time. But the measure doesn’t tell anyone whether the patient’s outcome actually improved, noted Dr. Berenholtz. The SUSP goes beyond those SCIP measures to determine which factors at the local level might lead to SSIs at that particular facility, and to identify what intervention works at that particular location.
"It’s clear that there is no single fix for surgical site infections in colorectal surgery," said Dr. Wick, who has worked on content for the SUSP and has helped to present it to interested facilities.
"There are best practices, but not a clear-cut bundle; so for each hospital, whatever they implement will be a little different," she said, adding that the SUSP allows each facility to tailor interventions and improvements to its particular environment.
The AHRQ is funding the 4-year SUSP initiative. Initially, the focus will be on colorectal surgery, but the program will expand to other surgical specialties with the aim of preventing harm from complications such as pneumonia, pulmonary embolisms, and deep vein thrombosis, said Dr. Berenholtz, who is also with the department of surgery and the department of anesthesia and critical care medicine at Johns Hopkins.
The first cohort of hospitals to participate in the SUSP will be in Tennessee, Colorado, and Florida, with a second cohort slated to begin in September. It is not clear exactly how many hospitals will be involved; SUSP organizers are waiting to receive all final letters of commitment, Dr. Berenholtz said. The aim is to reach as many hospitals as possible; there is no upper limit on participants.
An electronic health record is not required for participation, but hospitals need to be able to collect data on the incidence of SSIs.
The organizers are primarily going through the CMS-funded Hospital Engagement Networks (HENs). These are state, local, and regional networks that began forming in December 2011 and will work to develop learning collaboratives for hospitals, as well as provide patient safety initiatives such as the SUSP.
At the end of the 4 years, it is hoped that the HENs will continue to find ways to reduce complications and improve patient safety, Dr. Berenholtz said.
"We hope it ends up that hundreds – if not thousands – of lives will be saved," he said.
Dr. Berenholtz disclosed that he receives grant funding from the Agency for Healthcare Research and Quality, the National Institutes of Health, and the Robert Wood Johnson Foundation, and that he has received speaking honoraria from various hospitals related to patient safety and quality. Dr. Wick and her coauthors reported no conflicts.
A new program being spearheaded by surgeons at Johns Hopkins University, Baltimore, and patient safety experts aims to dramatically reduce surgical site infections, which occur in almost a third of colorectal procedures and are a major reason for readmissions.
According to a fact sheet on the Surgical Unit-Based Safety Program (SUSP), each year about 50 million people undergo surgery in the United States. Of those, 1 million develop serious complications and more than 150,000 die within 30 days.
The goals of SUSP are to reduce surgical site infections (SSIs), to document use of checklistlike methods to improve safety, and to document the culture of safety through use of the Hospital Survey of Patient Safety Culture.
SUSP is designed to build on the success of the Comprehensive Unit-Based Safety Program (CUSP), which was developed by the Johns Hopkins Armstrong Institute for Patient Safety and Quality. Results of the CUSP program were recently reported in the Journal of the American College of Surgeons.
The CUSP Study
After CUSP was adopted in 2009 by colorectal surgeons at Johns Hopkins, colorectal surgical site infections were reduced by a third in the first year and saved the hospital $168,000-$280,000, according to the study (J. Am. Coll. Surg. 2012;215:193-200).
Surgical site infections occur in 15%-30% of colorectal procedures and lead to as much as $1 billion in costs for longer admissions, readmissions, and treatment.
"Until now, there’s been little evidence on how to effectively address SSIs among this group of patients," said Dr. Elizabeth Wick of the department of surgery at Johns Hopkins, who was the lead investigator.
Dr. Wick and her associates analyzed outcomes after implementation of CUSP, which was developed by Dr. Peter Pronovost, director of the Armstrong Institute at Hopkins
The Hopkins colorectal CUSP team of 36 people included a representative from surgery, nursing, and anesthesia; a team coach; and a hospital executive who was committed to helping the project, according to the researchers.
After attending a lecture on patient safety, all members of the team completed an anonymous two-question assessment that asked how an SSI might develop in the next patient and what could be done to prevent it.
The team identified 95 areas of concern and picked six interventions to focus on to improve care: standardization of skin preparation and prescription of chlorhexidine showers; restricted use of oral bowel-cleansing solution before a procedure; warming of patients in the preanesthesia area; adoption of enhanced sterile techniques for bowel and skin; and addressing lapses in preoperative prophylactic antibiotics.
The team met monthly, using checklists and monitoring progress to address problems quickly. "The benefits of a bottom-up vs. a top-down approach to patient safety were immediately obvious," said Dr. Wick in a statement.
The study consisted of all consecutive colorectal surgery patients who were included in the American College of Surgeons’ NSQIP (National Surgical Quality Improvement Program) from July 2009 to July 2011. Procedures included open and laparoscopic colectomies and proctectomies, but not abdominal perineal resections. SSI rates that were collected using NSQIP were compared from the first year (2009-2010) to the second year (2010-2011); there were 278 patients in the first cohort and 324 in the second.
During that first year, the 27% (76) of patients had an SSI. By the second year, only 18% (59) of patients had an infection, for a decrease of 33%.
The authors said that CUSP seems to be effective, in part because it bridges the divide between frontline staff and senior leaders. The NSQIP outcome measures also helped the team to effectively monitor SSI rates, said the authors.
CUSP/SUSP in Practice
The CUSP model has been applied successfully to decrease central line–associated bloodstream infections in the intensive care unit, as well as to cut mortality and length of stay in a statewide program, the MHA (Michigan Health and Hospital Association) Keystone Intensive Care Unit project.
The elements of CUSP are not well validated in the operating room, however, and there’s little data on how the program could potentially impact other types of infections or complications – even though the program is in use at 1,200 ICUs in 47 states, said Dr. Sean M. Berenholtz, physician director of inpatient quality and safety at the Armstrong Institute. The aim of the SUSP is to adapt the CUSP practices to the OR, Dr. Berenholtz said in an interview.
Project teams consisting of experts from the Agency for Healthcare Research and Quality (AHRQ), the Armstrong Institute, the American College of Surgeons, the University of Pennsylvania in Philadelphia, and the World Health Organization’s Patient Safety Programme will assist SUSP participants.
The CUSP model combines knowledge from both clinical science and social science. The first step is to educate staff on the science of patient safety – most importantly, communicating the idea that "the vast majority of preventable complications don’t belong to an individual surgeon or an individual nurse," but occur within the organization of the health care system, Dr. Berenholtz said.
The project leaders then ask the staff to complete an anonymous, two-question assessment that gauges their experience of how complications develop and what might be done to prevent them. Next, a unit-based improvement team is assigned an executive partner from the Armstrong Institute who meets with the team at least monthly to help prioritize improvement efforts and lead them through any bureaucratic hurdles they may face at their hospitals. Goals are set and agreed upon.
The team then tries to learn from "defects" within the process, and identifies ways to prevent mistakes, especially among the surgeons, nurses, anesthesiologists, and technicians who work in the OR. Finally, tools such as checklists are used to foster teamwork and improvement. SUSP leaders will ask improvement teams to use "briefings" and "debriefings" to learn from mistakes and move forward.
There’s plenty of motivation for hospitals to want to reduce SSIs. The Centers for Medicare and Medicaid Services, as part of the Surgical Care Improvement Project (SCIP), requires public reporting of surgical quality measures, including SSIs.
For instance, hospitals are supposed to report whether patients are given the right antibiotic at the right time. But the measure doesn’t tell anyone whether the patient’s outcome actually improved, noted Dr. Berenholtz. The SUSP goes beyond those SCIP measures to determine which factors at the local level might lead to SSIs at that particular facility, and to identify what intervention works at that particular location.
"It’s clear that there is no single fix for surgical site infections in colorectal surgery," said Dr. Wick, who has worked on content for the SUSP and has helped to present it to interested facilities.
"There are best practices, but not a clear-cut bundle; so for each hospital, whatever they implement will be a little different," she said, adding that the SUSP allows each facility to tailor interventions and improvements to its particular environment.
The AHRQ is funding the 4-year SUSP initiative. Initially, the focus will be on colorectal surgery, but the program will expand to other surgical specialties with the aim of preventing harm from complications such as pneumonia, pulmonary embolisms, and deep vein thrombosis, said Dr. Berenholtz, who is also with the department of surgery and the department of anesthesia and critical care medicine at Johns Hopkins.
The first cohort of hospitals to participate in the SUSP will be in Tennessee, Colorado, and Florida, with a second cohort slated to begin in September. It is not clear exactly how many hospitals will be involved; SUSP organizers are waiting to receive all final letters of commitment, Dr. Berenholtz said. The aim is to reach as many hospitals as possible; there is no upper limit on participants.
An electronic health record is not required for participation, but hospitals need to be able to collect data on the incidence of SSIs.
The organizers are primarily going through the CMS-funded Hospital Engagement Networks (HENs). These are state, local, and regional networks that began forming in December 2011 and will work to develop learning collaboratives for hospitals, as well as provide patient safety initiatives such as the SUSP.
At the end of the 4 years, it is hoped that the HENs will continue to find ways to reduce complications and improve patient safety, Dr. Berenholtz said.
"We hope it ends up that hundreds – if not thousands – of lives will be saved," he said.
Dr. Berenholtz disclosed that he receives grant funding from the Agency for Healthcare Research and Quality, the National Institutes of Health, and the Robert Wood Johnson Foundation, and that he has received speaking honoraria from various hospitals related to patient safety and quality. Dr. Wick and her coauthors reported no conflicts.
A new program being spearheaded by surgeons at Johns Hopkins University, Baltimore, and patient safety experts aims to dramatically reduce surgical site infections, which occur in almost a third of colorectal procedures and are a major reason for readmissions.
According to a fact sheet on the Surgical Unit-Based Safety Program (SUSP), each year about 50 million people undergo surgery in the United States. Of those, 1 million develop serious complications and more than 150,000 die within 30 days.
The goals of SUSP are to reduce surgical site infections (SSIs), to document use of checklistlike methods to improve safety, and to document the culture of safety through use of the Hospital Survey of Patient Safety Culture.
SUSP is designed to build on the success of the Comprehensive Unit-Based Safety Program (CUSP), which was developed by the Johns Hopkins Armstrong Institute for Patient Safety and Quality. Results of the CUSP program were recently reported in the Journal of the American College of Surgeons.
The CUSP Study
After CUSP was adopted in 2009 by colorectal surgeons at Johns Hopkins, colorectal surgical site infections were reduced by a third in the first year and saved the hospital $168,000-$280,000, according to the study (J. Am. Coll. Surg. 2012;215:193-200).
Surgical site infections occur in 15%-30% of colorectal procedures and lead to as much as $1 billion in costs for longer admissions, readmissions, and treatment.
"Until now, there’s been little evidence on how to effectively address SSIs among this group of patients," said Dr. Elizabeth Wick of the department of surgery at Johns Hopkins, who was the lead investigator.
Dr. Wick and her associates analyzed outcomes after implementation of CUSP, which was developed by Dr. Peter Pronovost, director of the Armstrong Institute at Hopkins
The Hopkins colorectal CUSP team of 36 people included a representative from surgery, nursing, and anesthesia; a team coach; and a hospital executive who was committed to helping the project, according to the researchers.
After attending a lecture on patient safety, all members of the team completed an anonymous two-question assessment that asked how an SSI might develop in the next patient and what could be done to prevent it.
The team identified 95 areas of concern and picked six interventions to focus on to improve care: standardization of skin preparation and prescription of chlorhexidine showers; restricted use of oral bowel-cleansing solution before a procedure; warming of patients in the preanesthesia area; adoption of enhanced sterile techniques for bowel and skin; and addressing lapses in preoperative prophylactic antibiotics.
The team met monthly, using checklists and monitoring progress to address problems quickly. "The benefits of a bottom-up vs. a top-down approach to patient safety were immediately obvious," said Dr. Wick in a statement.
The study consisted of all consecutive colorectal surgery patients who were included in the American College of Surgeons’ NSQIP (National Surgical Quality Improvement Program) from July 2009 to July 2011. Procedures included open and laparoscopic colectomies and proctectomies, but not abdominal perineal resections. SSI rates that were collected using NSQIP were compared from the first year (2009-2010) to the second year (2010-2011); there were 278 patients in the first cohort and 324 in the second.
During that first year, the 27% (76) of patients had an SSI. By the second year, only 18% (59) of patients had an infection, for a decrease of 33%.
The authors said that CUSP seems to be effective, in part because it bridges the divide between frontline staff and senior leaders. The NSQIP outcome measures also helped the team to effectively monitor SSI rates, said the authors.
CUSP/SUSP in Practice
The CUSP model has been applied successfully to decrease central line–associated bloodstream infections in the intensive care unit, as well as to cut mortality and length of stay in a statewide program, the MHA (Michigan Health and Hospital Association) Keystone Intensive Care Unit project.
The elements of CUSP are not well validated in the operating room, however, and there’s little data on how the program could potentially impact other types of infections or complications – even though the program is in use at 1,200 ICUs in 47 states, said Dr. Sean M. Berenholtz, physician director of inpatient quality and safety at the Armstrong Institute. The aim of the SUSP is to adapt the CUSP practices to the OR, Dr. Berenholtz said in an interview.
Project teams consisting of experts from the Agency for Healthcare Research and Quality (AHRQ), the Armstrong Institute, the American College of Surgeons, the University of Pennsylvania in Philadelphia, and the World Health Organization’s Patient Safety Programme will assist SUSP participants.
The CUSP model combines knowledge from both clinical science and social science. The first step is to educate staff on the science of patient safety – most importantly, communicating the idea that "the vast majority of preventable complications don’t belong to an individual surgeon or an individual nurse," but occur within the organization of the health care system, Dr. Berenholtz said.
The project leaders then ask the staff to complete an anonymous, two-question assessment that gauges their experience of how complications develop and what might be done to prevent them. Next, a unit-based improvement team is assigned an executive partner from the Armstrong Institute who meets with the team at least monthly to help prioritize improvement efforts and lead them through any bureaucratic hurdles they may face at their hospitals. Goals are set and agreed upon.
The team then tries to learn from "defects" within the process, and identifies ways to prevent mistakes, especially among the surgeons, nurses, anesthesiologists, and technicians who work in the OR. Finally, tools such as checklists are used to foster teamwork and improvement. SUSP leaders will ask improvement teams to use "briefings" and "debriefings" to learn from mistakes and move forward.
There’s plenty of motivation for hospitals to want to reduce SSIs. The Centers for Medicare and Medicaid Services, as part of the Surgical Care Improvement Project (SCIP), requires public reporting of surgical quality measures, including SSIs.
For instance, hospitals are supposed to report whether patients are given the right antibiotic at the right time. But the measure doesn’t tell anyone whether the patient’s outcome actually improved, noted Dr. Berenholtz. The SUSP goes beyond those SCIP measures to determine which factors at the local level might lead to SSIs at that particular facility, and to identify what intervention works at that particular location.
"It’s clear that there is no single fix for surgical site infections in colorectal surgery," said Dr. Wick, who has worked on content for the SUSP and has helped to present it to interested facilities.
"There are best practices, but not a clear-cut bundle; so for each hospital, whatever they implement will be a little different," she said, adding that the SUSP allows each facility to tailor interventions and improvements to its particular environment.
The AHRQ is funding the 4-year SUSP initiative. Initially, the focus will be on colorectal surgery, but the program will expand to other surgical specialties with the aim of preventing harm from complications such as pneumonia, pulmonary embolisms, and deep vein thrombosis, said Dr. Berenholtz, who is also with the department of surgery and the department of anesthesia and critical care medicine at Johns Hopkins.
The first cohort of hospitals to participate in the SUSP will be in Tennessee, Colorado, and Florida, with a second cohort slated to begin in September. It is not clear exactly how many hospitals will be involved; SUSP organizers are waiting to receive all final letters of commitment, Dr. Berenholtz said. The aim is to reach as many hospitals as possible; there is no upper limit on participants.
An electronic health record is not required for participation, but hospitals need to be able to collect data on the incidence of SSIs.
The organizers are primarily going through the CMS-funded Hospital Engagement Networks (HENs). These are state, local, and regional networks that began forming in December 2011 and will work to develop learning collaboratives for hospitals, as well as provide patient safety initiatives such as the SUSP.
At the end of the 4 years, it is hoped that the HENs will continue to find ways to reduce complications and improve patient safety, Dr. Berenholtz said.
"We hope it ends up that hundreds – if not thousands – of lives will be saved," he said.
Dr. Berenholtz disclosed that he receives grant funding from the Agency for Healthcare Research and Quality, the National Institutes of Health, and the Robert Wood Johnson Foundation, and that he has received speaking honoraria from various hospitals related to patient safety and quality. Dr. Wick and her coauthors reported no conflicts.
Physicians Weigh In on ACA Ruling
The Supreme Court's decision to largely uphold the Affordable Care Act in essence preserved the status quo for the health system and took away some uncertainty - but only in the short term. The congressional and presidential elections in November could bring further changes to the law.
For now, though, the nation's physicians are pondering the court's ruling and how it will affect their practices. Concerns remain regarding some aspects of the law, and there is uncertainty on what the justices' Medicaid decision means.
Christian Shalgian, director of the division of advocacy and health policy at the American College of Surgeons, said he was surprised by the ruling, adding that surgeons are more concerned about what the law doesn't do than what it does.
"The biggest issue in my mind [with] the Affordable Care Act is what's not included in the [law]," said Mr. Shalgian. "The Medicare physician payment issue is one that's driving health care costs, and it needs to be fixed."
However, many other physician groups praised the court's opinions, noting that keeping the law in place would increase health care coverage and maintain the ACA's enhanced preventive care benefits.
"We are pleased that this decision means millions of Americans can look forward to the coverage they need to get healthy and stay healthy," said Dr. Jeremy Lazarus, president of the American Medical Association, in a statement. "This decision protects important improvements, such as ending coverage denials due to preexisting conditions and lifetime caps on insurance and allowing the 2.5 million young adults up to age 26 who gained coverage under the law to stay on their parents' health insurance policies."
Dr. David L. Bronson, president of the American College of Physicians, noted in a statement that although the group did not take a position on the constitutional issues, "we believe that the individual insurance mandate, combined with the ACA's subsidies to buy qualified coverage through state marketplaces (exchanges), Medicaid expansion to more low-income persons, and consumer protections against insurance practices that deny or limit coverage, are the most effective ways to expand coverage to nearly all Americans."
The American Academy of Family Physicians said that keeping the law in place will also allow the continuation of efforts to boost the breadth and depth of primary care.
"The Supreme Court decision maintains already-launched initiatives that support wider implementation of the patient-centered medical home and that value primary medical care through payment incentives for primary care physicians," said Dr. Glen Stream, AAFP president, in a statement.
Oncologists noted that they were pleased that many provisions that protect cancer patients would continue to stay intact, such as coverage for preventive screenings like colonoscopies and mammograms, the elimination of lifetime caps and preexisting condition exclusions for insurance plans, and the requirement that private insurers cover the cost of participating in clinical trials.
Cardiologists also applauded the fact that provisions ensuring preventive care and coverage of preexisting conditions would stay in place. American College of Cardiology president William Zoghbi said in a statement that the organization "favors provisions in the law that support preventive care, access to care, elimination of waste, and a payment system that encourages quality." However, the transformation is not complete. "Hard work remains ahead before we arrive at a sustainable payment system that emphasizes value and a strong patient-doctor relationship," said Dr. Zoghbi.
Because the law basically remains the same - for now - the 2.3% excise tax on medical devices will still go into effect on Jan. 1, 2013. AdvaMed, an industry lobbying group, said that it will continue to try to overturn that tax, which could end up driving up the cost of devices such as pacemakers.
The largely positive statements from organized medicine did not hide the fact that many individual physicians are still fearful of the law's effect on their practice.
In a survey of 644 primary care physicians that was conducted the day the Supreme Court ruled, 66% of respondents said that they did not believe the law could achieve health care coverage for all Americans. The poll was conducted by MDLinx, a Web-based information provider for doctors. "The survey showed a surprisingly high level of skepticism among primary care physicians," said Stephen Smith, chief marketing officer for MDLinx, in a statement. The poll also found that only 21% said that increased patient volume would have an "extremely positive" impact on their medical practice. Almost half said it would have an "extremely negative" impact. Respondents expressed concerns about the shortage of primary care doctors.
And most physician organizations indicated their continuing dissatisfaction with some parts of the law, including the Independent Payment Advisory Board, or IPAB, and the lack of any concrete malpractice reform.
The American Association of Clinical Urologists (AACU), the American Urological Association (AUA), and the Large Urology Group Practice Association (LUGPA) issued a joint statement, noting that "we are concerned that there are key aspects to this law that will, ultimately, hurt this nation's ability to provide widespread care for its citizens," including the IPAB. Mr. Shalgian said that the IPAB has been an issue for the ACS since it was first proposed.
At a press briefing called by the Republican Doctors Caucus, Rep. Phil Gingrey (R-Ga.), an ob.gyn., said that he and his fellow caucus members would work to overturn most if not all of the ACA, starting with the IPAB.
Some of Rep. Gingrey's colleagues were adamant that they'd do everything possible to overturn the law. Rep. Tom Price (R-Ga.), an orthopedic surgeon, said that the ACA "violates accessibility, violates affordability, violates quality, violates choices."
Rep. Paul Broun (R-Ga.) called the Act a "destroyer." He said it would "destroy a patient's ability to go to see a doctor and get the quality care they desperately need." Added Dr. Broun, "Obamacare must be repealed. It must be replaced with some policy that will make health care cheaper for everyone, provide coverage for all Americans, and save Medicare from going broke."
With the Supreme Court's efforts in the rear-view mirror, Republicans renewed their vow to repeal all or part of the ACA; however, that's unlikely to happen as long as Democrats maintain control of the Senate and the White House.
If Republicans win a majority in the Senate in November, and if Mitt Romney wins the presidential election, there could be major change.
In the meantime, most physician groups said they would work to fix the parts of the law that were objectionable.
Mr. Shalgian said that the ACS will be exploring options for medical liability reform during the annual Clinical Congress in Chicago.
Dr. Stream of the AAFP said that such reform is essential. "The [ACA] provides a foundation for reforming our health care system, but much work still lies ahead including a permanent replacement for the Sustainable Growth Rate formula and meaningful medical liability reform," he said.
Dr. Bronson of the ACP said that the organization realizes that "even with the Supreme Court's ruling, the political debate over the ACA continues and that its future is a major issue in the 2012 election."
He added, "We hope that a day will come when the debate will no longer be polarized between repeal on one hand, or keeping the law exactly as it is on the other, but on preserving all of the good things that it does while making needed improvements," among which would be "meaningful reforms to the medical liability system."
The Supreme Court's decision to largely uphold the Affordable Care Act in essence preserved the status quo for the health system and took away some uncertainty - but only in the short term. The congressional and presidential elections in November could bring further changes to the law.
For now, though, the nation's physicians are pondering the court's ruling and how it will affect their practices. Concerns remain regarding some aspects of the law, and there is uncertainty on what the justices' Medicaid decision means.
Christian Shalgian, director of the division of advocacy and health policy at the American College of Surgeons, said he was surprised by the ruling, adding that surgeons are more concerned about what the law doesn't do than what it does.
"The biggest issue in my mind [with] the Affordable Care Act is what's not included in the [law]," said Mr. Shalgian. "The Medicare physician payment issue is one that's driving health care costs, and it needs to be fixed."
However, many other physician groups praised the court's opinions, noting that keeping the law in place would increase health care coverage and maintain the ACA's enhanced preventive care benefits.
"We are pleased that this decision means millions of Americans can look forward to the coverage they need to get healthy and stay healthy," said Dr. Jeremy Lazarus, president of the American Medical Association, in a statement. "This decision protects important improvements, such as ending coverage denials due to preexisting conditions and lifetime caps on insurance and allowing the 2.5 million young adults up to age 26 who gained coverage under the law to stay on their parents' health insurance policies."
Dr. David L. Bronson, president of the American College of Physicians, noted in a statement that although the group did not take a position on the constitutional issues, "we believe that the individual insurance mandate, combined with the ACA's subsidies to buy qualified coverage through state marketplaces (exchanges), Medicaid expansion to more low-income persons, and consumer protections against insurance practices that deny or limit coverage, are the most effective ways to expand coverage to nearly all Americans."
The American Academy of Family Physicians said that keeping the law in place will also allow the continuation of efforts to boost the breadth and depth of primary care.
"The Supreme Court decision maintains already-launched initiatives that support wider implementation of the patient-centered medical home and that value primary medical care through payment incentives for primary care physicians," said Dr. Glen Stream, AAFP president, in a statement.
Oncologists noted that they were pleased that many provisions that protect cancer patients would continue to stay intact, such as coverage for preventive screenings like colonoscopies and mammograms, the elimination of lifetime caps and preexisting condition exclusions for insurance plans, and the requirement that private insurers cover the cost of participating in clinical trials.
Cardiologists also applauded the fact that provisions ensuring preventive care and coverage of preexisting conditions would stay in place. American College of Cardiology president William Zoghbi said in a statement that the organization "favors provisions in the law that support preventive care, access to care, elimination of waste, and a payment system that encourages quality." However, the transformation is not complete. "Hard work remains ahead before we arrive at a sustainable payment system that emphasizes value and a strong patient-doctor relationship," said Dr. Zoghbi.
Because the law basically remains the same - for now - the 2.3% excise tax on medical devices will still go into effect on Jan. 1, 2013. AdvaMed, an industry lobbying group, said that it will continue to try to overturn that tax, which could end up driving up the cost of devices such as pacemakers.
The largely positive statements from organized medicine did not hide the fact that many individual physicians are still fearful of the law's effect on their practice.
In a survey of 644 primary care physicians that was conducted the day the Supreme Court ruled, 66% of respondents said that they did not believe the law could achieve health care coverage for all Americans. The poll was conducted by MDLinx, a Web-based information provider for doctors. "The survey showed a surprisingly high level of skepticism among primary care physicians," said Stephen Smith, chief marketing officer for MDLinx, in a statement. The poll also found that only 21% said that increased patient volume would have an "extremely positive" impact on their medical practice. Almost half said it would have an "extremely negative" impact. Respondents expressed concerns about the shortage of primary care doctors.
And most physician organizations indicated their continuing dissatisfaction with some parts of the law, including the Independent Payment Advisory Board, or IPAB, and the lack of any concrete malpractice reform.
The American Association of Clinical Urologists (AACU), the American Urological Association (AUA), and the Large Urology Group Practice Association (LUGPA) issued a joint statement, noting that "we are concerned that there are key aspects to this law that will, ultimately, hurt this nation's ability to provide widespread care for its citizens," including the IPAB. Mr. Shalgian said that the IPAB has been an issue for the ACS since it was first proposed.
At a press briefing called by the Republican Doctors Caucus, Rep. Phil Gingrey (R-Ga.), an ob.gyn., said that he and his fellow caucus members would work to overturn most if not all of the ACA, starting with the IPAB.
Some of Rep. Gingrey's colleagues were adamant that they'd do everything possible to overturn the law. Rep. Tom Price (R-Ga.), an orthopedic surgeon, said that the ACA "violates accessibility, violates affordability, violates quality, violates choices."
Rep. Paul Broun (R-Ga.) called the Act a "destroyer." He said it would "destroy a patient's ability to go to see a doctor and get the quality care they desperately need." Added Dr. Broun, "Obamacare must be repealed. It must be replaced with some policy that will make health care cheaper for everyone, provide coverage for all Americans, and save Medicare from going broke."
With the Supreme Court's efforts in the rear-view mirror, Republicans renewed their vow to repeal all or part of the ACA; however, that's unlikely to happen as long as Democrats maintain control of the Senate and the White House.
If Republicans win a majority in the Senate in November, and if Mitt Romney wins the presidential election, there could be major change.
In the meantime, most physician groups said they would work to fix the parts of the law that were objectionable.
Mr. Shalgian said that the ACS will be exploring options for medical liability reform during the annual Clinical Congress in Chicago.
Dr. Stream of the AAFP said that such reform is essential. "The [ACA] provides a foundation for reforming our health care system, but much work still lies ahead including a permanent replacement for the Sustainable Growth Rate formula and meaningful medical liability reform," he said.
Dr. Bronson of the ACP said that the organization realizes that "even with the Supreme Court's ruling, the political debate over the ACA continues and that its future is a major issue in the 2012 election."
He added, "We hope that a day will come when the debate will no longer be polarized between repeal on one hand, or keeping the law exactly as it is on the other, but on preserving all of the good things that it does while making needed improvements," among which would be "meaningful reforms to the medical liability system."
The Supreme Court's decision to largely uphold the Affordable Care Act in essence preserved the status quo for the health system and took away some uncertainty - but only in the short term. The congressional and presidential elections in November could bring further changes to the law.
For now, though, the nation's physicians are pondering the court's ruling and how it will affect their practices. Concerns remain regarding some aspects of the law, and there is uncertainty on what the justices' Medicaid decision means.
Christian Shalgian, director of the division of advocacy and health policy at the American College of Surgeons, said he was surprised by the ruling, adding that surgeons are more concerned about what the law doesn't do than what it does.
"The biggest issue in my mind [with] the Affordable Care Act is what's not included in the [law]," said Mr. Shalgian. "The Medicare physician payment issue is one that's driving health care costs, and it needs to be fixed."
However, many other physician groups praised the court's opinions, noting that keeping the law in place would increase health care coverage and maintain the ACA's enhanced preventive care benefits.
"We are pleased that this decision means millions of Americans can look forward to the coverage they need to get healthy and stay healthy," said Dr. Jeremy Lazarus, president of the American Medical Association, in a statement. "This decision protects important improvements, such as ending coverage denials due to preexisting conditions and lifetime caps on insurance and allowing the 2.5 million young adults up to age 26 who gained coverage under the law to stay on their parents' health insurance policies."
Dr. David L. Bronson, president of the American College of Physicians, noted in a statement that although the group did not take a position on the constitutional issues, "we believe that the individual insurance mandate, combined with the ACA's subsidies to buy qualified coverage through state marketplaces (exchanges), Medicaid expansion to more low-income persons, and consumer protections against insurance practices that deny or limit coverage, are the most effective ways to expand coverage to nearly all Americans."
The American Academy of Family Physicians said that keeping the law in place will also allow the continuation of efforts to boost the breadth and depth of primary care.
"The Supreme Court decision maintains already-launched initiatives that support wider implementation of the patient-centered medical home and that value primary medical care through payment incentives for primary care physicians," said Dr. Glen Stream, AAFP president, in a statement.
Oncologists noted that they were pleased that many provisions that protect cancer patients would continue to stay intact, such as coverage for preventive screenings like colonoscopies and mammograms, the elimination of lifetime caps and preexisting condition exclusions for insurance plans, and the requirement that private insurers cover the cost of participating in clinical trials.
Cardiologists also applauded the fact that provisions ensuring preventive care and coverage of preexisting conditions would stay in place. American College of Cardiology president William Zoghbi said in a statement that the organization "favors provisions in the law that support preventive care, access to care, elimination of waste, and a payment system that encourages quality." However, the transformation is not complete. "Hard work remains ahead before we arrive at a sustainable payment system that emphasizes value and a strong patient-doctor relationship," said Dr. Zoghbi.
Because the law basically remains the same - for now - the 2.3% excise tax on medical devices will still go into effect on Jan. 1, 2013. AdvaMed, an industry lobbying group, said that it will continue to try to overturn that tax, which could end up driving up the cost of devices such as pacemakers.
The largely positive statements from organized medicine did not hide the fact that many individual physicians are still fearful of the law's effect on their practice.
In a survey of 644 primary care physicians that was conducted the day the Supreme Court ruled, 66% of respondents said that they did not believe the law could achieve health care coverage for all Americans. The poll was conducted by MDLinx, a Web-based information provider for doctors. "The survey showed a surprisingly high level of skepticism among primary care physicians," said Stephen Smith, chief marketing officer for MDLinx, in a statement. The poll also found that only 21% said that increased patient volume would have an "extremely positive" impact on their medical practice. Almost half said it would have an "extremely negative" impact. Respondents expressed concerns about the shortage of primary care doctors.
And most physician organizations indicated their continuing dissatisfaction with some parts of the law, including the Independent Payment Advisory Board, or IPAB, and the lack of any concrete malpractice reform.
The American Association of Clinical Urologists (AACU), the American Urological Association (AUA), and the Large Urology Group Practice Association (LUGPA) issued a joint statement, noting that "we are concerned that there are key aspects to this law that will, ultimately, hurt this nation's ability to provide widespread care for its citizens," including the IPAB. Mr. Shalgian said that the IPAB has been an issue for the ACS since it was first proposed.
At a press briefing called by the Republican Doctors Caucus, Rep. Phil Gingrey (R-Ga.), an ob.gyn., said that he and his fellow caucus members would work to overturn most if not all of the ACA, starting with the IPAB.
Some of Rep. Gingrey's colleagues were adamant that they'd do everything possible to overturn the law. Rep. Tom Price (R-Ga.), an orthopedic surgeon, said that the ACA "violates accessibility, violates affordability, violates quality, violates choices."
Rep. Paul Broun (R-Ga.) called the Act a "destroyer." He said it would "destroy a patient's ability to go to see a doctor and get the quality care they desperately need." Added Dr. Broun, "Obamacare must be repealed. It must be replaced with some policy that will make health care cheaper for everyone, provide coverage for all Americans, and save Medicare from going broke."
With the Supreme Court's efforts in the rear-view mirror, Republicans renewed their vow to repeal all or part of the ACA; however, that's unlikely to happen as long as Democrats maintain control of the Senate and the White House.
If Republicans win a majority in the Senate in November, and if Mitt Romney wins the presidential election, there could be major change.
In the meantime, most physician groups said they would work to fix the parts of the law that were objectionable.
Mr. Shalgian said that the ACS will be exploring options for medical liability reform during the annual Clinical Congress in Chicago.
Dr. Stream of the AAFP said that such reform is essential. "The [ACA] provides a foundation for reforming our health care system, but much work still lies ahead including a permanent replacement for the Sustainable Growth Rate formula and meaningful medical liability reform," he said.
Dr. Bronson of the ACP said that the organization realizes that "even with the Supreme Court's ruling, the political debate over the ACA continues and that its future is a major issue in the 2012 election."
He added, "We hope that a day will come when the debate will no longer be polarized between repeal on one hand, or keeping the law exactly as it is on the other, but on preserving all of the good things that it does while making needed improvements," among which would be "meaningful reforms to the medical liability system."
Radiation Oncologists Say Medicare Cuts Could Shutter Practices
Radiation oncologists say they could be forced to shut their doors or consolidate their practices, if the proposed cuts to radiation therapy in the 2013 Medicare physician fee schedule are allowed to stay in place.
And this is likely to hasten a shift of services out of the community and into the hospital, according to officials at the American Society for Radiation Oncology (ASTRO), which surveyed its membership in the wake of the Centers for Medicare and Medicaid Services’ proposed rule in early July.
"Some patients will likely receive their care in radiation therapy centers at a far greater distance from their home in both hospital-based facilities and larger freestanding centers that survive these cuts," said Dr. Michael L. Steinberg, president of the ASTRO’s board of directors, in an interview.
With the closure of radiation therapy centers, physicians would seek employment in surviving freestanding or hospital-based facilities, he added,
The CMS is proposing a 15% reduction in payment for IMRT (Intensity Modulated Radiation Therapy) and SBRT (Stereotactic Body Radiation Therapy). The agency also proposed a 19% cut for community-based radiation therapy centers.
IMRT and SBRT account for about a third of Medicare spending on radiation therapy, according to a spokeswoman for the ASTRO. Medicare and Medicaid are the predominant payers for radiation therapy, which is delivered to two-thirds of the nation’s 1.5 million cancer patients annually.
The ASTRO survey, which was conducted online, received about 600 responses. (There are about 4,500 radiation oncologists in the United States.) Of the 599 who participated, almost 60% were from community practices or combined community- and hospital-based practices. The results reported were only for that 60%.
Physicians were not asked about the impact of the almost-29% overall cut in physician pay called for by Medicare’s Sustainable Growth Rate (SGR) formula.
If just the close-to-20% cut for radiation therapy centers goes into effect, 35% of practices said they would probably have to close their doors, and 64% said they would consolidate. Both actions would lead to longer wait times for treatment, said ASTRO CEO Laura Thevenot in a briefing with reporters.
The consequences may also mean that physicians will spend less time with patients – that is, with those patients who would still be able to access a radiation oncologist. Some 70% of respondents said they would limit Medicare patients if the cuts go through, and 49% said they would stop accepting Medicare patients altogether.
Radiation oncologists also said they would cut back on purchases of new technology and lay off support staff and other nonphysician employees.
"The likely end result for limited access to radiation therapy – an integral form of care used in nearly 70% of all cancer patients – would be an erosion in the gains in cure rates, quality of life, and other clinical outcomes that have been achieved in our country over the last 20 years," said Dr. Constantine A. Mantz, a radiation oncologist in Ft. Myers, Fla., during the press briefing.
Ms. Thevenot said that the CMS had used faulty information to calculate the true costs of IMRT and SBRT, and that the agency should revisit the codes for both procedures.
Added Dr. Steinberg in a statement, "ASTRO welcomes a comprehensive review of these procedure codes and supports the necessary sophistication of a process, such as provided by the [American Medical Association’s Relative Value Scale Update Committee (RUC)], to value complex medical procedures including IMRT and SBRT." He is also professor and chairman of radiation oncology at the University of California, Los Angeles.
According to Ms. Thevenot, IMRT was reviewed by AMA’s RUC in fall 2010, and SBRT was reviewed in February 2011.
The ASTRO has also enlisted the support of Congress to overturn the cuts. Representatives Joe Pitts (R-Penn.) and Frank Pallone (D-N.J.), along with Rep. Mike Rogers (R-Mich.), have been circulating a letter decrying the cuts that will eventually be sent to officials at the CMS. The organization says that a "similar bipartisan letter is being drafted in the Senate."
Radiation oncologists say they could be forced to shut their doors or consolidate their practices, if the proposed cuts to radiation therapy in the 2013 Medicare physician fee schedule are allowed to stay in place.
And this is likely to hasten a shift of services out of the community and into the hospital, according to officials at the American Society for Radiation Oncology (ASTRO), which surveyed its membership in the wake of the Centers for Medicare and Medicaid Services’ proposed rule in early July.
"Some patients will likely receive their care in radiation therapy centers at a far greater distance from their home in both hospital-based facilities and larger freestanding centers that survive these cuts," said Dr. Michael L. Steinberg, president of the ASTRO’s board of directors, in an interview.
With the closure of radiation therapy centers, physicians would seek employment in surviving freestanding or hospital-based facilities, he added,
The CMS is proposing a 15% reduction in payment for IMRT (Intensity Modulated Radiation Therapy) and SBRT (Stereotactic Body Radiation Therapy). The agency also proposed a 19% cut for community-based radiation therapy centers.
IMRT and SBRT account for about a third of Medicare spending on radiation therapy, according to a spokeswoman for the ASTRO. Medicare and Medicaid are the predominant payers for radiation therapy, which is delivered to two-thirds of the nation’s 1.5 million cancer patients annually.
The ASTRO survey, which was conducted online, received about 600 responses. (There are about 4,500 radiation oncologists in the United States.) Of the 599 who participated, almost 60% were from community practices or combined community- and hospital-based practices. The results reported were only for that 60%.
Physicians were not asked about the impact of the almost-29% overall cut in physician pay called for by Medicare’s Sustainable Growth Rate (SGR) formula.
If just the close-to-20% cut for radiation therapy centers goes into effect, 35% of practices said they would probably have to close their doors, and 64% said they would consolidate. Both actions would lead to longer wait times for treatment, said ASTRO CEO Laura Thevenot in a briefing with reporters.
The consequences may also mean that physicians will spend less time with patients – that is, with those patients who would still be able to access a radiation oncologist. Some 70% of respondents said they would limit Medicare patients if the cuts go through, and 49% said they would stop accepting Medicare patients altogether.
Radiation oncologists also said they would cut back on purchases of new technology and lay off support staff and other nonphysician employees.
"The likely end result for limited access to radiation therapy – an integral form of care used in nearly 70% of all cancer patients – would be an erosion in the gains in cure rates, quality of life, and other clinical outcomes that have been achieved in our country over the last 20 years," said Dr. Constantine A. Mantz, a radiation oncologist in Ft. Myers, Fla., during the press briefing.
Ms. Thevenot said that the CMS had used faulty information to calculate the true costs of IMRT and SBRT, and that the agency should revisit the codes for both procedures.
Added Dr. Steinberg in a statement, "ASTRO welcomes a comprehensive review of these procedure codes and supports the necessary sophistication of a process, such as provided by the [American Medical Association’s Relative Value Scale Update Committee (RUC)], to value complex medical procedures including IMRT and SBRT." He is also professor and chairman of radiation oncology at the University of California, Los Angeles.
According to Ms. Thevenot, IMRT was reviewed by AMA’s RUC in fall 2010, and SBRT was reviewed in February 2011.
The ASTRO has also enlisted the support of Congress to overturn the cuts. Representatives Joe Pitts (R-Penn.) and Frank Pallone (D-N.J.), along with Rep. Mike Rogers (R-Mich.), have been circulating a letter decrying the cuts that will eventually be sent to officials at the CMS. The organization says that a "similar bipartisan letter is being drafted in the Senate."
Radiation oncologists say they could be forced to shut their doors or consolidate their practices, if the proposed cuts to radiation therapy in the 2013 Medicare physician fee schedule are allowed to stay in place.
And this is likely to hasten a shift of services out of the community and into the hospital, according to officials at the American Society for Radiation Oncology (ASTRO), which surveyed its membership in the wake of the Centers for Medicare and Medicaid Services’ proposed rule in early July.
"Some patients will likely receive their care in radiation therapy centers at a far greater distance from their home in both hospital-based facilities and larger freestanding centers that survive these cuts," said Dr. Michael L. Steinberg, president of the ASTRO’s board of directors, in an interview.
With the closure of radiation therapy centers, physicians would seek employment in surviving freestanding or hospital-based facilities, he added,
The CMS is proposing a 15% reduction in payment for IMRT (Intensity Modulated Radiation Therapy) and SBRT (Stereotactic Body Radiation Therapy). The agency also proposed a 19% cut for community-based radiation therapy centers.
IMRT and SBRT account for about a third of Medicare spending on radiation therapy, according to a spokeswoman for the ASTRO. Medicare and Medicaid are the predominant payers for radiation therapy, which is delivered to two-thirds of the nation’s 1.5 million cancer patients annually.
The ASTRO survey, which was conducted online, received about 600 responses. (There are about 4,500 radiation oncologists in the United States.) Of the 599 who participated, almost 60% were from community practices or combined community- and hospital-based practices. The results reported were only for that 60%.
Physicians were not asked about the impact of the almost-29% overall cut in physician pay called for by Medicare’s Sustainable Growth Rate (SGR) formula.
If just the close-to-20% cut for radiation therapy centers goes into effect, 35% of practices said they would probably have to close their doors, and 64% said they would consolidate. Both actions would lead to longer wait times for treatment, said ASTRO CEO Laura Thevenot in a briefing with reporters.
The consequences may also mean that physicians will spend less time with patients – that is, with those patients who would still be able to access a radiation oncologist. Some 70% of respondents said they would limit Medicare patients if the cuts go through, and 49% said they would stop accepting Medicare patients altogether.
Radiation oncologists also said they would cut back on purchases of new technology and lay off support staff and other nonphysician employees.
"The likely end result for limited access to radiation therapy – an integral form of care used in nearly 70% of all cancer patients – would be an erosion in the gains in cure rates, quality of life, and other clinical outcomes that have been achieved in our country over the last 20 years," said Dr. Constantine A. Mantz, a radiation oncologist in Ft. Myers, Fla., during the press briefing.
Ms. Thevenot said that the CMS had used faulty information to calculate the true costs of IMRT and SBRT, and that the agency should revisit the codes for both procedures.
Added Dr. Steinberg in a statement, "ASTRO welcomes a comprehensive review of these procedure codes and supports the necessary sophistication of a process, such as provided by the [American Medical Association’s Relative Value Scale Update Committee (RUC)], to value complex medical procedures including IMRT and SBRT." He is also professor and chairman of radiation oncology at the University of California, Los Angeles.
According to Ms. Thevenot, IMRT was reviewed by AMA’s RUC in fall 2010, and SBRT was reviewed in February 2011.
The ASTRO has also enlisted the support of Congress to overturn the cuts. Representatives Joe Pitts (R-Penn.) and Frank Pallone (D-N.J.), along with Rep. Mike Rogers (R-Mich.), have been circulating a letter decrying the cuts that will eventually be sent to officials at the CMS. The organization says that a "similar bipartisan letter is being drafted in the Senate."
AIDS Clinicians Back Treatment as Prevention
WASHINGTON – A large international society of AIDS clinicians is endorsing the use of treatment as prevention and pre-exposure prophylaxis as a means of containing the epidemic.
With the two approaches gaining currency, primary care physicians and ob.gyns. will likely be called upon to deliver the therapies.
The consensus statement, issued by the International Association of Physicians in AIDS Care (IAPAC), is the end result of a gathering of experts in June.
Treatment as Prevention (TasP) gained credence after publication of the HIV Prevention Trials Network (HPTN) 052 study in the New England Journal of Medicine last August (N. Engl. J. Med. 2011;365:493-505). The trial more or less definitively proved that giving antiretroviral treatment significantly reduces the rate of sexual transmission of HIV.
Pre-Exposure Prophylaxis (PrEP) has been shown to reduce infection with the virus in heterosexuals and homosexuals who might get exposed through risky sexual activity. In July, the Food and Drug Administration approved Truvada (a drug that combines tenofovir disoproxil fumarate with emtricitabine) for use as PrEP among sexually active adults at risk for HIV infection.
"The group felt that the paradigm for using antiretroviral therapy as prevention had been established," said Dr. Kenneth Mayer, chairman of the IAPAC TasP/PrEP Advisory Committee, and medical research director at the Fenway Institute in Boston. "We know that this works. The issue now is implementation," he said in a press briefing at the 19th International AIDS Conference.
The consensus backs the idea of offering treatment to those who want to start. But, said Dr. Mayer, the question is, "How do we scale up training providers so they can do this in a competent way so we can manage people in an optimal way?"
Dr. Julio Montaner, also a member of the IAPAC TasP/PrEP Advisory Committee, said that studies in Africa had shown that therapy could be given by nonspecialists and even by nonphysicians. "It is abundantly clear that we have made treatment of HIV more complicated than it needs to be," said Dr. Montaner, director of the British Columbia Centre for Excellence in HIV/AIDS in Vancouver, B.C.
Now that regimens have become simpler, safer, and better tolerated, "I’m very optimistic that we are going to increasingly see treatment being supervised by people other than the specialists," he said. Dr. Montaner noted that in British Columbia, treatment is predominantly being initiated by family physicians.
Another key issue: For TasP to work, people need to know their HIV status. So the consensus backs higher levels of HIV testing.
Other challenges to implementing TasP include resource limitations; how to evaluate the quality of care; ethical issues; and how to monitor people for increases in risky behavior and suboptimal adherence, said Dr. Mayer.
Monitoring risky behavior will also be a challenge with PrEP, he said. There are also questions about the optimal dose and timing of the dose, he said, adding that much more research needs to be done on PrEP, relative to TasP.
PrEP is not a standalone therapy, he said. "It has to be part of a comprehensive prevention package," that includes behavioral interventions, said Dr. Mayer. And it is not meant to be a lifetime therapy. It should be used at a time of acute risk, he said, adding that PrEP is "a measure to get them through a period where they might otherwise become HIV infected."
The full consensus statement is available at the IAPAC website. It will also be shared with many physician groups, including the American College of Physicians, the American Academy of Family Practitioners, and the American Congress of Obstetricians and Gynecologists, said Dr. Mayer in an interview.
WASHINGTON – A large international society of AIDS clinicians is endorsing the use of treatment as prevention and pre-exposure prophylaxis as a means of containing the epidemic.
With the two approaches gaining currency, primary care physicians and ob.gyns. will likely be called upon to deliver the therapies.
The consensus statement, issued by the International Association of Physicians in AIDS Care (IAPAC), is the end result of a gathering of experts in June.
Treatment as Prevention (TasP) gained credence after publication of the HIV Prevention Trials Network (HPTN) 052 study in the New England Journal of Medicine last August (N. Engl. J. Med. 2011;365:493-505). The trial more or less definitively proved that giving antiretroviral treatment significantly reduces the rate of sexual transmission of HIV.
Pre-Exposure Prophylaxis (PrEP) has been shown to reduce infection with the virus in heterosexuals and homosexuals who might get exposed through risky sexual activity. In July, the Food and Drug Administration approved Truvada (a drug that combines tenofovir disoproxil fumarate with emtricitabine) for use as PrEP among sexually active adults at risk for HIV infection.
"The group felt that the paradigm for using antiretroviral therapy as prevention had been established," said Dr. Kenneth Mayer, chairman of the IAPAC TasP/PrEP Advisory Committee, and medical research director at the Fenway Institute in Boston. "We know that this works. The issue now is implementation," he said in a press briefing at the 19th International AIDS Conference.
The consensus backs the idea of offering treatment to those who want to start. But, said Dr. Mayer, the question is, "How do we scale up training providers so they can do this in a competent way so we can manage people in an optimal way?"
Dr. Julio Montaner, also a member of the IAPAC TasP/PrEP Advisory Committee, said that studies in Africa had shown that therapy could be given by nonspecialists and even by nonphysicians. "It is abundantly clear that we have made treatment of HIV more complicated than it needs to be," said Dr. Montaner, director of the British Columbia Centre for Excellence in HIV/AIDS in Vancouver, B.C.
Now that regimens have become simpler, safer, and better tolerated, "I’m very optimistic that we are going to increasingly see treatment being supervised by people other than the specialists," he said. Dr. Montaner noted that in British Columbia, treatment is predominantly being initiated by family physicians.
Another key issue: For TasP to work, people need to know their HIV status. So the consensus backs higher levels of HIV testing.
Other challenges to implementing TasP include resource limitations; how to evaluate the quality of care; ethical issues; and how to monitor people for increases in risky behavior and suboptimal adherence, said Dr. Mayer.
Monitoring risky behavior will also be a challenge with PrEP, he said. There are also questions about the optimal dose and timing of the dose, he said, adding that much more research needs to be done on PrEP, relative to TasP.
PrEP is not a standalone therapy, he said. "It has to be part of a comprehensive prevention package," that includes behavioral interventions, said Dr. Mayer. And it is not meant to be a lifetime therapy. It should be used at a time of acute risk, he said, adding that PrEP is "a measure to get them through a period where they might otherwise become HIV infected."
The full consensus statement is available at the IAPAC website. It will also be shared with many physician groups, including the American College of Physicians, the American Academy of Family Practitioners, and the American Congress of Obstetricians and Gynecologists, said Dr. Mayer in an interview.
WASHINGTON – A large international society of AIDS clinicians is endorsing the use of treatment as prevention and pre-exposure prophylaxis as a means of containing the epidemic.
With the two approaches gaining currency, primary care physicians and ob.gyns. will likely be called upon to deliver the therapies.
The consensus statement, issued by the International Association of Physicians in AIDS Care (IAPAC), is the end result of a gathering of experts in June.
Treatment as Prevention (TasP) gained credence after publication of the HIV Prevention Trials Network (HPTN) 052 study in the New England Journal of Medicine last August (N. Engl. J. Med. 2011;365:493-505). The trial more or less definitively proved that giving antiretroviral treatment significantly reduces the rate of sexual transmission of HIV.
Pre-Exposure Prophylaxis (PrEP) has been shown to reduce infection with the virus in heterosexuals and homosexuals who might get exposed through risky sexual activity. In July, the Food and Drug Administration approved Truvada (a drug that combines tenofovir disoproxil fumarate with emtricitabine) for use as PrEP among sexually active adults at risk for HIV infection.
"The group felt that the paradigm for using antiretroviral therapy as prevention had been established," said Dr. Kenneth Mayer, chairman of the IAPAC TasP/PrEP Advisory Committee, and medical research director at the Fenway Institute in Boston. "We know that this works. The issue now is implementation," he said in a press briefing at the 19th International AIDS Conference.
The consensus backs the idea of offering treatment to those who want to start. But, said Dr. Mayer, the question is, "How do we scale up training providers so they can do this in a competent way so we can manage people in an optimal way?"
Dr. Julio Montaner, also a member of the IAPAC TasP/PrEP Advisory Committee, said that studies in Africa had shown that therapy could be given by nonspecialists and even by nonphysicians. "It is abundantly clear that we have made treatment of HIV more complicated than it needs to be," said Dr. Montaner, director of the British Columbia Centre for Excellence in HIV/AIDS in Vancouver, B.C.
Now that regimens have become simpler, safer, and better tolerated, "I’m very optimistic that we are going to increasingly see treatment being supervised by people other than the specialists," he said. Dr. Montaner noted that in British Columbia, treatment is predominantly being initiated by family physicians.
Another key issue: For TasP to work, people need to know their HIV status. So the consensus backs higher levels of HIV testing.
Other challenges to implementing TasP include resource limitations; how to evaluate the quality of care; ethical issues; and how to monitor people for increases in risky behavior and suboptimal adherence, said Dr. Mayer.
Monitoring risky behavior will also be a challenge with PrEP, he said. There are also questions about the optimal dose and timing of the dose, he said, adding that much more research needs to be done on PrEP, relative to TasP.
PrEP is not a standalone therapy, he said. "It has to be part of a comprehensive prevention package," that includes behavioral interventions, said Dr. Mayer. And it is not meant to be a lifetime therapy. It should be used at a time of acute risk, he said, adding that PrEP is "a measure to get them through a period where they might otherwise become HIV infected."
The full consensus statement is available at the IAPAC website. It will also be shared with many physician groups, including the American College of Physicians, the American Academy of Family Practitioners, and the American Congress of Obstetricians and Gynecologists, said Dr. Mayer in an interview.
AT THE 19TH INTERNATIONAL AIDS CONFERENCE
Feds: 89 New ACOs Up and Running as of July 1
Another 89 accountable care organizations had opened their doors for business as of July 1, the Health and Human Services department announced July 9.
That brings the total to 154 groups that have agreed to be held accountable for improving the quality of care they provide while simultaneously reducing costs, including 32 participating in the pioneer ACO model announced in December, as well as six physician group practice transition demonstration organizations that began in early 2011.
Some 2.4 million Medicare beneficiaries in 40 states and Washington, D.C., now are cared for by an ACO, the department announced.
At least 400 more organizations have said they will apply to become an ACO when the Centers for Medicare and Medicaid Services (CMS) begins in August accepting applications for 2013, according to Jonathan Blum, principal deputy administrator for CMS and director of its Center for Medicare.
In a briefing with reporters, Mr. Blum did not directly address whether the program could be hurt by expected attempts to defund the Affordable Care Act. Instead, he said, "This is a program that is going to grow substantially over time."
ACOs are meant to be led by physicians, working in conjunction with hospitals and other providers to deliver more efficient and better-quality care. "We really see this being led by the physician community to improve patient care," Mr. Blum said.
Of the 89 new ACOs, "almost half are physician-driven organizations serving fewer than 10,000 beneficiaries, demonstrating that smaller organizations are interested in operating as ACOs," according to a CMS statement.
However, the requirement that an ACO serve at least 5,000 Medicare beneficiaries continues to be a difficult hurdle for physician groups that would otherwise like to participate, said Mr. Blum.
The ACO effort is also known as the Medicare Shared Savings Program. The organizations that agree to participate are given the opportunity to share in whatever savings are generated. CMS estimates that the government’s savings from the program could be up to $940 million over 4 years.
One of the newest ACOs is the Westmed Medical Group, a Westchester County, New York–based physician-owned and managed multispecialty group practice that was founded in 1996, and includes 225 physicians and 1,000 employees.
Dr. Simeon Schwartz, president and CEO, said that each of group’s nine sites generally offers primary care; surgical, specialty, radiology, and lab services; and urgent care.
Westmed expects to generate savings of 5%-10% over the course of the group’s 3-year contract, mostly by shifting care from the inpatient to the outpatient setting through better coordination, he said at the press briefing. He added that providing urgent care – keeping patients out of the emergency department – is another way to save money.
In a statement, HHS Secretary Kathleen Sebelius said that having better care coordination will be one of the keys to generating savings.
"We applaud every one of these doctors, hospitals, health centers, and others for working together to ensure millions of people with Medicare get better, more patient-centered, coordinated care," she said.
Another 89 accountable care organizations had opened their doors for business as of July 1, the Health and Human Services department announced July 9.
That brings the total to 154 groups that have agreed to be held accountable for improving the quality of care they provide while simultaneously reducing costs, including 32 participating in the pioneer ACO model announced in December, as well as six physician group practice transition demonstration organizations that began in early 2011.
Some 2.4 million Medicare beneficiaries in 40 states and Washington, D.C., now are cared for by an ACO, the department announced.
At least 400 more organizations have said they will apply to become an ACO when the Centers for Medicare and Medicaid Services (CMS) begins in August accepting applications for 2013, according to Jonathan Blum, principal deputy administrator for CMS and director of its Center for Medicare.
In a briefing with reporters, Mr. Blum did not directly address whether the program could be hurt by expected attempts to defund the Affordable Care Act. Instead, he said, "This is a program that is going to grow substantially over time."
ACOs are meant to be led by physicians, working in conjunction with hospitals and other providers to deliver more efficient and better-quality care. "We really see this being led by the physician community to improve patient care," Mr. Blum said.
Of the 89 new ACOs, "almost half are physician-driven organizations serving fewer than 10,000 beneficiaries, demonstrating that smaller organizations are interested in operating as ACOs," according to a CMS statement.
However, the requirement that an ACO serve at least 5,000 Medicare beneficiaries continues to be a difficult hurdle for physician groups that would otherwise like to participate, said Mr. Blum.
The ACO effort is also known as the Medicare Shared Savings Program. The organizations that agree to participate are given the opportunity to share in whatever savings are generated. CMS estimates that the government’s savings from the program could be up to $940 million over 4 years.
One of the newest ACOs is the Westmed Medical Group, a Westchester County, New York–based physician-owned and managed multispecialty group practice that was founded in 1996, and includes 225 physicians and 1,000 employees.
Dr. Simeon Schwartz, president and CEO, said that each of group’s nine sites generally offers primary care; surgical, specialty, radiology, and lab services; and urgent care.
Westmed expects to generate savings of 5%-10% over the course of the group’s 3-year contract, mostly by shifting care from the inpatient to the outpatient setting through better coordination, he said at the press briefing. He added that providing urgent care – keeping patients out of the emergency department – is another way to save money.
In a statement, HHS Secretary Kathleen Sebelius said that having better care coordination will be one of the keys to generating savings.
"We applaud every one of these doctors, hospitals, health centers, and others for working together to ensure millions of people with Medicare get better, more patient-centered, coordinated care," she said.
Another 89 accountable care organizations had opened their doors for business as of July 1, the Health and Human Services department announced July 9.
That brings the total to 154 groups that have agreed to be held accountable for improving the quality of care they provide while simultaneously reducing costs, including 32 participating in the pioneer ACO model announced in December, as well as six physician group practice transition demonstration organizations that began in early 2011.
Some 2.4 million Medicare beneficiaries in 40 states and Washington, D.C., now are cared for by an ACO, the department announced.
At least 400 more organizations have said they will apply to become an ACO when the Centers for Medicare and Medicaid Services (CMS) begins in August accepting applications for 2013, according to Jonathan Blum, principal deputy administrator for CMS and director of its Center for Medicare.
In a briefing with reporters, Mr. Blum did not directly address whether the program could be hurt by expected attempts to defund the Affordable Care Act. Instead, he said, "This is a program that is going to grow substantially over time."
ACOs are meant to be led by physicians, working in conjunction with hospitals and other providers to deliver more efficient and better-quality care. "We really see this being led by the physician community to improve patient care," Mr. Blum said.
Of the 89 new ACOs, "almost half are physician-driven organizations serving fewer than 10,000 beneficiaries, demonstrating that smaller organizations are interested in operating as ACOs," according to a CMS statement.
However, the requirement that an ACO serve at least 5,000 Medicare beneficiaries continues to be a difficult hurdle for physician groups that would otherwise like to participate, said Mr. Blum.
The ACO effort is also known as the Medicare Shared Savings Program. The organizations that agree to participate are given the opportunity to share in whatever savings are generated. CMS estimates that the government’s savings from the program could be up to $940 million over 4 years.
One of the newest ACOs is the Westmed Medical Group, a Westchester County, New York–based physician-owned and managed multispecialty group practice that was founded in 1996, and includes 225 physicians and 1,000 employees.
Dr. Simeon Schwartz, president and CEO, said that each of group’s nine sites generally offers primary care; surgical, specialty, radiology, and lab services; and urgent care.
Westmed expects to generate savings of 5%-10% over the course of the group’s 3-year contract, mostly by shifting care from the inpatient to the outpatient setting through better coordination, he said at the press briefing. He added that providing urgent care – keeping patients out of the emergency department – is another way to save money.
In a statement, HHS Secretary Kathleen Sebelius said that having better care coordination will be one of the keys to generating savings.
"We applaud every one of these doctors, hospitals, health centers, and others for working together to ensure millions of people with Medicare get better, more patient-centered, coordinated care," she said.