User login
Top 5 Tips for Becoming an Effective Gastroenterology Consultant
Gastroenterology (GI) subspecialty training is carefully designed to develop expertise in digestive diseases and gastrointestinal endoscopy, while facilitating the transition from generalist to subspecialty consultant. The concept of effective consultation extends far beyond clinical expertise and has been explored repeatedly, beginning with Goldman’s “Ten Commandments” in 1983.1,2 How should these best practices be specifically applied to GI? More importantly, what kind of experience would you want if you were the referring provider or the patient themselves?
Below are
1. Be Kind
Survey studies of medical/surgical residents and attending hospitalists have demonstrated that willingness to accept consultation requests was the single factor consistently rated as most important in determining the quality of the consultation interaction.3,4 Unfortunately, nearly 65% of respondents reported encountering pushback when requesting subspecialty consultation. It is critical to recognize that when you receive a GI consult request, the requester has already decided that it is needed. Whether that request comports with our individual notion of “necessary” or “important,” this is a colleague’s request for help. There are myriad reasons why a request may be made, but they are unified in this principle.
Effective teamwork in healthcare settings enhances clinical performance and patient safety. Positive relationships with colleagues and healthcare team members also mitigate the emotional basis for physician burnout.5 Be kind and courteous to those who seek your assistance. Move beyond the notion of the “bad” or “soft” consult and seek instead to understand how you can help.
A requesting physician may phrase the consult question vaguely or may know that the patient is having a GI-related issue, but simply lack the specific knowledge to know what is needed. In these instances, it is our role to listen and help guide them to the correct thought process to ensure the best care of the patient. These important interactions establish our reputation, create our referral bases, and directly affect our sense of personal satisfaction.
2. Be Timely
GI presents an appealing breadth of pathology, but this also corresponds to a wide variety of indications for consultation and, therefore, urgency of need. In a busy clinical practice, not all requests can be urgently prioritized. However, it is the consultant’s responsibility to identify patients that require urgent evaluation and intervention to avert a potential adverse outcome.
We are well-trained in the medical triage of consultations. There are explicit guidelines for assessing urgency for GI bleeding, foreign body ingestion, choledocholithiasis, and many other indications. However, there are often special contextual circumstances that will elevate the urgency of a seemingly non-urgent consult request. Does the patient have an upcoming surgery or treatment that will depend on your input? Are they facing an imminent loss of insurance coverage? Is their non-severe GI disease leading to more severe impact on non-GI organ systems? The referring provider knows the patient better than you – seek to understand the context of the consult request.
Timeliness also applies to our communication. Communicate recommendations directly to the consulting service as soon as the patient is seen. When a colleague reaches out with a concern about a patient, make sure to take that request seriously. If you are unable to address the concern immediately, at least provide acknowledgment and an estimated timeline for response. As the maxim states, the effectiveness of a consultant is just as dependent on availability as it is on ability.
3. Be Specific
The same survey studies indicate that the second most critical aspect of successful subspecialty consultation is delivering clear recommendations. Accordingly, I always urge my trainees to challenge me when we leave a consult interaction if they feel that our plan is vague or imprecise.
Specificity in consult recommendations is an essential way to demonstrate your expertise and provide value. Clear and definitive recommendations enhance others’ perception of your skill, reduce the need for additional clarifying communication, and lead to more efficient, higher quality care. Avoid vague language, such as asking the requester to “consider” a test or intervention. When recommending medication, specify the dose, frequency, duration, and expected timeline of effect. Rather than recommending “cross-sectional imaging,” specify what modality and protocol. Instead of recommending “adequate resuscitation,” specify your target endpoints. If you engage in multidisciplinary discussion, ensure you strive for a specific group consensus plan and communicate this to all members of the team.
Specificity also applies to the quality of your documentation. Ensure that your clinical notes outline your rationale for your recommended plan, specific contingencies based on results of recommended testing, and a plan for follow-up care. When referring for open-access endoscopy, specifically outline what to look for and which specimens or endoscopic interventions are needed. Be precise in your procedure documentation – avoid vague terms such as small/medium/large and instead quantify in terms of millimeter/centimeter measurement. If you do not adopt specific classification schemes (e.g. Prague classification, Paris classification, Eosinophilic Esophagitis Endoscopic Reference Score, etc.), ensure you provide enough descriptive language to convey an adequate understanding of the findings.
4. Be Helpful
A consultant’s primary directive is to be of service to the consulting provider and the patient. As an educational leader, I am often asked what attributes separate a high-performing trainee from an average one. My feeling is that the most critical attribute is a sense of ownership over patient care.
As a consultant, when others feel we are exhibiting engagement and ownership in a patient’s care, they perceive that we are working together as an effective healthcare team. Interestingly, survey studies of inpatient care show that primary services do not necessarily value assistance with orders or care coordination – they consider these as core aspects of their daily work. What they did value was ongoing daily progress notes/communication, regardless of patient acuity or consulting specialty. This is a potent signal that our continued engagement (both inpatient and outpatient) is perceived as helpful.
Helpfulness is further aided by ensuring mutual understanding. While survey data indicate that sharing specific literature citations may not always be perceived positively, explaining the consultant’s rationale for their recommendations is highly valued. Take the time to tactfully explain your assessment of the patient and why you arrived at your specific recommendations. If your recommendations differ from what the requester expected (e.g. a procedure was expected but is not offered), ensure you explain why and answer questions they may have. This fosters mutual respect and proactively averts conflict or discontent from misunderstanding.
Multidisciplinary collaboration is another important avenue for aiding our patients and colleagues. Studies across a wide range of disease processes (including GI bleeding, IBD, etc.) and medical settings have demonstrated that multidisciplinary collaboration unequivocally improves patient outcomes.6 The success of these collaborations relies on our willingness to fully engage in these conversations, despite the fact that they may often be logistically challenging.
We all know how difficult it can be to locate and organize multiple medical specialists with complex varying clinical schedules and busy personal lives. Choosing to do so demonstrates a dedication to providing the highest level of care and elevates both patient and physician satisfaction. Having chosen to cultivate several ongoing multidisciplinary conferences/collaborations, I can attest to the notion that the outcome is well worth the effort.
5. Be Honest
While we always strive to provide the answers for our patients and colleagues, we must also acknowledge our limitations. Be honest with yourself when you encounter a scenario that pushes beyond the boundaries of your knowledge and comfort. Be willing to admit when you yourself need to consult others or seek an outside referral to provide the care a patient needs. Aspiring physicians often espouse that a devotion to lifelong learning is a key driver of their desire to pursue a career in medicine. These scenarios provide a key opportunity to expand our knowledge while doing what is right for our patients.
Be equally honest about your comfort with “curbside” consultations. Studies show that subspecialists receive on average of 3-4 such requests per week.7 The perception of these interactions is starkly discrepant between the requester and recipient. While over 80% of surveyed primary nonsurgical services felt that curbside consultations were helpful in patient care, a similar proportion of subspecialists expressed concern that insufficient clinical information was provided, even leading to a fear of litigation. While straightforward, informal conversations on narrow, well-defined questions can be helpful and efficient, the consultant should always feel comfortable seeking an opportunity for formal consultation when the details are unclear or the case/question is complex.
Closing Thoughts
Being an effective GI consultant isn’t just about what you know—it’s about how you apply it, how you communicate it, and how you make others feel in the process.
The attributes outlined above are not ancillary traits—they are essential components of high-quality consultation. When consistently applied, they enhance collaboration, improve patient outcomes, and reinforce trust within the healthcare system. By committing to them, you establish your reputation of excellence and play a role in elevating the field of gastroenterology more broadly.
Dr. Kahn is based in the Division of Gastroenterology and Hepatology at Mayo Clinic, Scottsdale, Arizona. He reports no conflicts of interest in regard to this article.
References
1. Goldman L, et al. Ten commandments for effective consultations. Arch Intern Med. 1983 Sep.
2. Salerno SM, et al. Principles of effective consultation: an update for the 21st-century consultant. Arch Intern Med. 2007 Feb. doi: 10.1001/archinte.167.3.271.
3. Adams TN, et al. Hospitalist Perspective of Interactions with Medicine Subspecialty Consult Services. J Hosp Med. 2018 May. doi: 10.12788/jhm.2882.
4. Matsuo T, et al. Essential consultants’ skills and attitudes (Willing CONSULT): a cross-sectional survey. BMC Med Educ. 2021 Jul. doi: 10.1186/s12909-021-02810-9.
5. Welp A, Manser T. Integrating teamwork, clinician occupational well-being and patient safety - development of a conceptual framework based on a systematic review. BMC Health Serv Res. 2016 Jul. doi: 10.1186/s12913-016-1535-y.
6. Webster CS, et al. Interprofessional Learning in Multidisciplinary Healthcare Teams Is Associated With Reduced Patient Mortality: A Quantitative Systematic Review and Meta-analysis. J Patient Saf. 2024 Jan. doi: 10.1097/PTS.0000000000001170.
7. Lin M, et al. Curbside Consultations: The Good, the Bad, and the Ugly. Clin Gastroenterol Hepatol. 2016 Jan. doi: 10.1016/j.cgh.2015.09.026.
Gastroenterology (GI) subspecialty training is carefully designed to develop expertise in digestive diseases and gastrointestinal endoscopy, while facilitating the transition from generalist to subspecialty consultant. The concept of effective consultation extends far beyond clinical expertise and has been explored repeatedly, beginning with Goldman’s “Ten Commandments” in 1983.1,2 How should these best practices be specifically applied to GI? More importantly, what kind of experience would you want if you were the referring provider or the patient themselves?
Below are
1. Be Kind
Survey studies of medical/surgical residents and attending hospitalists have demonstrated that willingness to accept consultation requests was the single factor consistently rated as most important in determining the quality of the consultation interaction.3,4 Unfortunately, nearly 65% of respondents reported encountering pushback when requesting subspecialty consultation. It is critical to recognize that when you receive a GI consult request, the requester has already decided that it is needed. Whether that request comports with our individual notion of “necessary” or “important,” this is a colleague’s request for help. There are myriad reasons why a request may be made, but they are unified in this principle.
Effective teamwork in healthcare settings enhances clinical performance and patient safety. Positive relationships with colleagues and healthcare team members also mitigate the emotional basis for physician burnout.5 Be kind and courteous to those who seek your assistance. Move beyond the notion of the “bad” or “soft” consult and seek instead to understand how you can help.
A requesting physician may phrase the consult question vaguely or may know that the patient is having a GI-related issue, but simply lack the specific knowledge to know what is needed. In these instances, it is our role to listen and help guide them to the correct thought process to ensure the best care of the patient. These important interactions establish our reputation, create our referral bases, and directly affect our sense of personal satisfaction.
2. Be Timely
GI presents an appealing breadth of pathology, but this also corresponds to a wide variety of indications for consultation and, therefore, urgency of need. In a busy clinical practice, not all requests can be urgently prioritized. However, it is the consultant’s responsibility to identify patients that require urgent evaluation and intervention to avert a potential adverse outcome.
We are well-trained in the medical triage of consultations. There are explicit guidelines for assessing urgency for GI bleeding, foreign body ingestion, choledocholithiasis, and many other indications. However, there are often special contextual circumstances that will elevate the urgency of a seemingly non-urgent consult request. Does the patient have an upcoming surgery or treatment that will depend on your input? Are they facing an imminent loss of insurance coverage? Is their non-severe GI disease leading to more severe impact on non-GI organ systems? The referring provider knows the patient better than you – seek to understand the context of the consult request.
Timeliness also applies to our communication. Communicate recommendations directly to the consulting service as soon as the patient is seen. When a colleague reaches out with a concern about a patient, make sure to take that request seriously. If you are unable to address the concern immediately, at least provide acknowledgment and an estimated timeline for response. As the maxim states, the effectiveness of a consultant is just as dependent on availability as it is on ability.
3. Be Specific
The same survey studies indicate that the second most critical aspect of successful subspecialty consultation is delivering clear recommendations. Accordingly, I always urge my trainees to challenge me when we leave a consult interaction if they feel that our plan is vague or imprecise.
Specificity in consult recommendations is an essential way to demonstrate your expertise and provide value. Clear and definitive recommendations enhance others’ perception of your skill, reduce the need for additional clarifying communication, and lead to more efficient, higher quality care. Avoid vague language, such as asking the requester to “consider” a test or intervention. When recommending medication, specify the dose, frequency, duration, and expected timeline of effect. Rather than recommending “cross-sectional imaging,” specify what modality and protocol. Instead of recommending “adequate resuscitation,” specify your target endpoints. If you engage in multidisciplinary discussion, ensure you strive for a specific group consensus plan and communicate this to all members of the team.
Specificity also applies to the quality of your documentation. Ensure that your clinical notes outline your rationale for your recommended plan, specific contingencies based on results of recommended testing, and a plan for follow-up care. When referring for open-access endoscopy, specifically outline what to look for and which specimens or endoscopic interventions are needed. Be precise in your procedure documentation – avoid vague terms such as small/medium/large and instead quantify in terms of millimeter/centimeter measurement. If you do not adopt specific classification schemes (e.g. Prague classification, Paris classification, Eosinophilic Esophagitis Endoscopic Reference Score, etc.), ensure you provide enough descriptive language to convey an adequate understanding of the findings.
4. Be Helpful
A consultant’s primary directive is to be of service to the consulting provider and the patient. As an educational leader, I am often asked what attributes separate a high-performing trainee from an average one. My feeling is that the most critical attribute is a sense of ownership over patient care.
As a consultant, when others feel we are exhibiting engagement and ownership in a patient’s care, they perceive that we are working together as an effective healthcare team. Interestingly, survey studies of inpatient care show that primary services do not necessarily value assistance with orders or care coordination – they consider these as core aspects of their daily work. What they did value was ongoing daily progress notes/communication, regardless of patient acuity or consulting specialty. This is a potent signal that our continued engagement (both inpatient and outpatient) is perceived as helpful.
Helpfulness is further aided by ensuring mutual understanding. While survey data indicate that sharing specific literature citations may not always be perceived positively, explaining the consultant’s rationale for their recommendations is highly valued. Take the time to tactfully explain your assessment of the patient and why you arrived at your specific recommendations. If your recommendations differ from what the requester expected (e.g. a procedure was expected but is not offered), ensure you explain why and answer questions they may have. This fosters mutual respect and proactively averts conflict or discontent from misunderstanding.
Multidisciplinary collaboration is another important avenue for aiding our patients and colleagues. Studies across a wide range of disease processes (including GI bleeding, IBD, etc.) and medical settings have demonstrated that multidisciplinary collaboration unequivocally improves patient outcomes.6 The success of these collaborations relies on our willingness to fully engage in these conversations, despite the fact that they may often be logistically challenging.
We all know how difficult it can be to locate and organize multiple medical specialists with complex varying clinical schedules and busy personal lives. Choosing to do so demonstrates a dedication to providing the highest level of care and elevates both patient and physician satisfaction. Having chosen to cultivate several ongoing multidisciplinary conferences/collaborations, I can attest to the notion that the outcome is well worth the effort.
5. Be Honest
While we always strive to provide the answers for our patients and colleagues, we must also acknowledge our limitations. Be honest with yourself when you encounter a scenario that pushes beyond the boundaries of your knowledge and comfort. Be willing to admit when you yourself need to consult others or seek an outside referral to provide the care a patient needs. Aspiring physicians often espouse that a devotion to lifelong learning is a key driver of their desire to pursue a career in medicine. These scenarios provide a key opportunity to expand our knowledge while doing what is right for our patients.
Be equally honest about your comfort with “curbside” consultations. Studies show that subspecialists receive on average of 3-4 such requests per week.7 The perception of these interactions is starkly discrepant between the requester and recipient. While over 80% of surveyed primary nonsurgical services felt that curbside consultations were helpful in patient care, a similar proportion of subspecialists expressed concern that insufficient clinical information was provided, even leading to a fear of litigation. While straightforward, informal conversations on narrow, well-defined questions can be helpful and efficient, the consultant should always feel comfortable seeking an opportunity for formal consultation when the details are unclear or the case/question is complex.
Closing Thoughts
Being an effective GI consultant isn’t just about what you know—it’s about how you apply it, how you communicate it, and how you make others feel in the process.
The attributes outlined above are not ancillary traits—they are essential components of high-quality consultation. When consistently applied, they enhance collaboration, improve patient outcomes, and reinforce trust within the healthcare system. By committing to them, you establish your reputation of excellence and play a role in elevating the field of gastroenterology more broadly.
Dr. Kahn is based in the Division of Gastroenterology and Hepatology at Mayo Clinic, Scottsdale, Arizona. He reports no conflicts of interest in regard to this article.
References
1. Goldman L, et al. Ten commandments for effective consultations. Arch Intern Med. 1983 Sep.
2. Salerno SM, et al. Principles of effective consultation: an update for the 21st-century consultant. Arch Intern Med. 2007 Feb. doi: 10.1001/archinte.167.3.271.
3. Adams TN, et al. Hospitalist Perspective of Interactions with Medicine Subspecialty Consult Services. J Hosp Med. 2018 May. doi: 10.12788/jhm.2882.
4. Matsuo T, et al. Essential consultants’ skills and attitudes (Willing CONSULT): a cross-sectional survey. BMC Med Educ. 2021 Jul. doi: 10.1186/s12909-021-02810-9.
5. Welp A, Manser T. Integrating teamwork, clinician occupational well-being and patient safety - development of a conceptual framework based on a systematic review. BMC Health Serv Res. 2016 Jul. doi: 10.1186/s12913-016-1535-y.
6. Webster CS, et al. Interprofessional Learning in Multidisciplinary Healthcare Teams Is Associated With Reduced Patient Mortality: A Quantitative Systematic Review and Meta-analysis. J Patient Saf. 2024 Jan. doi: 10.1097/PTS.0000000000001170.
7. Lin M, et al. Curbside Consultations: The Good, the Bad, and the Ugly. Clin Gastroenterol Hepatol. 2016 Jan. doi: 10.1016/j.cgh.2015.09.026.
Gastroenterology (GI) subspecialty training is carefully designed to develop expertise in digestive diseases and gastrointestinal endoscopy, while facilitating the transition from generalist to subspecialty consultant. The concept of effective consultation extends far beyond clinical expertise and has been explored repeatedly, beginning with Goldman’s “Ten Commandments” in 1983.1,2 How should these best practices be specifically applied to GI? More importantly, what kind of experience would you want if you were the referring provider or the patient themselves?
Below are
1. Be Kind
Survey studies of medical/surgical residents and attending hospitalists have demonstrated that willingness to accept consultation requests was the single factor consistently rated as most important in determining the quality of the consultation interaction.3,4 Unfortunately, nearly 65% of respondents reported encountering pushback when requesting subspecialty consultation. It is critical to recognize that when you receive a GI consult request, the requester has already decided that it is needed. Whether that request comports with our individual notion of “necessary” or “important,” this is a colleague’s request for help. There are myriad reasons why a request may be made, but they are unified in this principle.
Effective teamwork in healthcare settings enhances clinical performance and patient safety. Positive relationships with colleagues and healthcare team members also mitigate the emotional basis for physician burnout.5 Be kind and courteous to those who seek your assistance. Move beyond the notion of the “bad” or “soft” consult and seek instead to understand how you can help.
A requesting physician may phrase the consult question vaguely or may know that the patient is having a GI-related issue, but simply lack the specific knowledge to know what is needed. In these instances, it is our role to listen and help guide them to the correct thought process to ensure the best care of the patient. These important interactions establish our reputation, create our referral bases, and directly affect our sense of personal satisfaction.
2. Be Timely
GI presents an appealing breadth of pathology, but this also corresponds to a wide variety of indications for consultation and, therefore, urgency of need. In a busy clinical practice, not all requests can be urgently prioritized. However, it is the consultant’s responsibility to identify patients that require urgent evaluation and intervention to avert a potential adverse outcome.
We are well-trained in the medical triage of consultations. There are explicit guidelines for assessing urgency for GI bleeding, foreign body ingestion, choledocholithiasis, and many other indications. However, there are often special contextual circumstances that will elevate the urgency of a seemingly non-urgent consult request. Does the patient have an upcoming surgery or treatment that will depend on your input? Are they facing an imminent loss of insurance coverage? Is their non-severe GI disease leading to more severe impact on non-GI organ systems? The referring provider knows the patient better than you – seek to understand the context of the consult request.
Timeliness also applies to our communication. Communicate recommendations directly to the consulting service as soon as the patient is seen. When a colleague reaches out with a concern about a patient, make sure to take that request seriously. If you are unable to address the concern immediately, at least provide acknowledgment and an estimated timeline for response. As the maxim states, the effectiveness of a consultant is just as dependent on availability as it is on ability.
3. Be Specific
The same survey studies indicate that the second most critical aspect of successful subspecialty consultation is delivering clear recommendations. Accordingly, I always urge my trainees to challenge me when we leave a consult interaction if they feel that our plan is vague or imprecise.
Specificity in consult recommendations is an essential way to demonstrate your expertise and provide value. Clear and definitive recommendations enhance others’ perception of your skill, reduce the need for additional clarifying communication, and lead to more efficient, higher quality care. Avoid vague language, such as asking the requester to “consider” a test or intervention. When recommending medication, specify the dose, frequency, duration, and expected timeline of effect. Rather than recommending “cross-sectional imaging,” specify what modality and protocol. Instead of recommending “adequate resuscitation,” specify your target endpoints. If you engage in multidisciplinary discussion, ensure you strive for a specific group consensus plan and communicate this to all members of the team.
Specificity also applies to the quality of your documentation. Ensure that your clinical notes outline your rationale for your recommended plan, specific contingencies based on results of recommended testing, and a plan for follow-up care. When referring for open-access endoscopy, specifically outline what to look for and which specimens or endoscopic interventions are needed. Be precise in your procedure documentation – avoid vague terms such as small/medium/large and instead quantify in terms of millimeter/centimeter measurement. If you do not adopt specific classification schemes (e.g. Prague classification, Paris classification, Eosinophilic Esophagitis Endoscopic Reference Score, etc.), ensure you provide enough descriptive language to convey an adequate understanding of the findings.
4. Be Helpful
A consultant’s primary directive is to be of service to the consulting provider and the patient. As an educational leader, I am often asked what attributes separate a high-performing trainee from an average one. My feeling is that the most critical attribute is a sense of ownership over patient care.
As a consultant, when others feel we are exhibiting engagement and ownership in a patient’s care, they perceive that we are working together as an effective healthcare team. Interestingly, survey studies of inpatient care show that primary services do not necessarily value assistance with orders or care coordination – they consider these as core aspects of their daily work. What they did value was ongoing daily progress notes/communication, regardless of patient acuity or consulting specialty. This is a potent signal that our continued engagement (both inpatient and outpatient) is perceived as helpful.
Helpfulness is further aided by ensuring mutual understanding. While survey data indicate that sharing specific literature citations may not always be perceived positively, explaining the consultant’s rationale for their recommendations is highly valued. Take the time to tactfully explain your assessment of the patient and why you arrived at your specific recommendations. If your recommendations differ from what the requester expected (e.g. a procedure was expected but is not offered), ensure you explain why and answer questions they may have. This fosters mutual respect and proactively averts conflict or discontent from misunderstanding.
Multidisciplinary collaboration is another important avenue for aiding our patients and colleagues. Studies across a wide range of disease processes (including GI bleeding, IBD, etc.) and medical settings have demonstrated that multidisciplinary collaboration unequivocally improves patient outcomes.6 The success of these collaborations relies on our willingness to fully engage in these conversations, despite the fact that they may often be logistically challenging.
We all know how difficult it can be to locate and organize multiple medical specialists with complex varying clinical schedules and busy personal lives. Choosing to do so demonstrates a dedication to providing the highest level of care and elevates both patient and physician satisfaction. Having chosen to cultivate several ongoing multidisciplinary conferences/collaborations, I can attest to the notion that the outcome is well worth the effort.
5. Be Honest
While we always strive to provide the answers for our patients and colleagues, we must also acknowledge our limitations. Be honest with yourself when you encounter a scenario that pushes beyond the boundaries of your knowledge and comfort. Be willing to admit when you yourself need to consult others or seek an outside referral to provide the care a patient needs. Aspiring physicians often espouse that a devotion to lifelong learning is a key driver of their desire to pursue a career in medicine. These scenarios provide a key opportunity to expand our knowledge while doing what is right for our patients.
Be equally honest about your comfort with “curbside” consultations. Studies show that subspecialists receive on average of 3-4 such requests per week.7 The perception of these interactions is starkly discrepant between the requester and recipient. While over 80% of surveyed primary nonsurgical services felt that curbside consultations were helpful in patient care, a similar proportion of subspecialists expressed concern that insufficient clinical information was provided, even leading to a fear of litigation. While straightforward, informal conversations on narrow, well-defined questions can be helpful and efficient, the consultant should always feel comfortable seeking an opportunity for formal consultation when the details are unclear or the case/question is complex.
Closing Thoughts
Being an effective GI consultant isn’t just about what you know—it’s about how you apply it, how you communicate it, and how you make others feel in the process.
The attributes outlined above are not ancillary traits—they are essential components of high-quality consultation. When consistently applied, they enhance collaboration, improve patient outcomes, and reinforce trust within the healthcare system. By committing to them, you establish your reputation of excellence and play a role in elevating the field of gastroenterology more broadly.
Dr. Kahn is based in the Division of Gastroenterology and Hepatology at Mayo Clinic, Scottsdale, Arizona. He reports no conflicts of interest in regard to this article.
References
1. Goldman L, et al. Ten commandments for effective consultations. Arch Intern Med. 1983 Sep.
2. Salerno SM, et al. Principles of effective consultation: an update for the 21st-century consultant. Arch Intern Med. 2007 Feb. doi: 10.1001/archinte.167.3.271.
3. Adams TN, et al. Hospitalist Perspective of Interactions with Medicine Subspecialty Consult Services. J Hosp Med. 2018 May. doi: 10.12788/jhm.2882.
4. Matsuo T, et al. Essential consultants’ skills and attitudes (Willing CONSULT): a cross-sectional survey. BMC Med Educ. 2021 Jul. doi: 10.1186/s12909-021-02810-9.
5. Welp A, Manser T. Integrating teamwork, clinician occupational well-being and patient safety - development of a conceptual framework based on a systematic review. BMC Health Serv Res. 2016 Jul. doi: 10.1186/s12913-016-1535-y.
6. Webster CS, et al. Interprofessional Learning in Multidisciplinary Healthcare Teams Is Associated With Reduced Patient Mortality: A Quantitative Systematic Review and Meta-analysis. J Patient Saf. 2024 Jan. doi: 10.1097/PTS.0000000000001170.
7. Lin M, et al. Curbside Consultations: The Good, the Bad, and the Ugly. Clin Gastroenterol Hepatol. 2016 Jan. doi: 10.1016/j.cgh.2015.09.026.
@GiJournal: An online platform to discuss the latest gastroenterology and hepatology publications
The last decade has seen an increased focus on the use of social media for medical education. Twitter, with over 330 million active users, is the most popular social media platform for medical education. We describe here our recent initiative to establish a weekly online gastroenterology-focused journal club on Twitter.
How was the idea conceived?
Sultan Mahmood, MD (@SultanMahmoodMD)
I joined #GITwitter at the end of 2019 and started following some of the leading experts in the field of gastroenterology and hepatology. It was a pleasant surprise to see how easy it was to engage with them and get expert opinions from across the world in real time. #MondayNightIBD, led by Aline Charabaty, MD, had become a phenomenon in the GI community and changed the perception of medical education in the digital world. There were online journal clubs for different medical subspecialties, including #NephroJC, #HOJournalClub, and #DermJC, but none for gastroenterology. Realizing this opportunity, and with guidance from Dr. Charabaty, we started @GiJournal in December of 2019 with weekly discussions.
@GiJournal started off as an informal discussion in which we would post a summary of the article and invite an expert in the field to comment. However, the interest in the journal club quickly took off as we gained more followers and a worldwide audience joined our journal club discussions on a weekly basis. As the COVID-19 pandemic took hold and endoscopy suites around the word closed, interest in online medical education grew. @GIJournal provided a platform for trainees and practicing physicians alike to stay up to date with the latest publications from the comfort of their homes. Needless to say, the journal club has evolved since its inception in that we now work with a team of experts and trainees who run the journal club on a rotating basis.
How does @GiJournal work?
Ijlal Akbar Ali, MD (@IjlalAkbar)
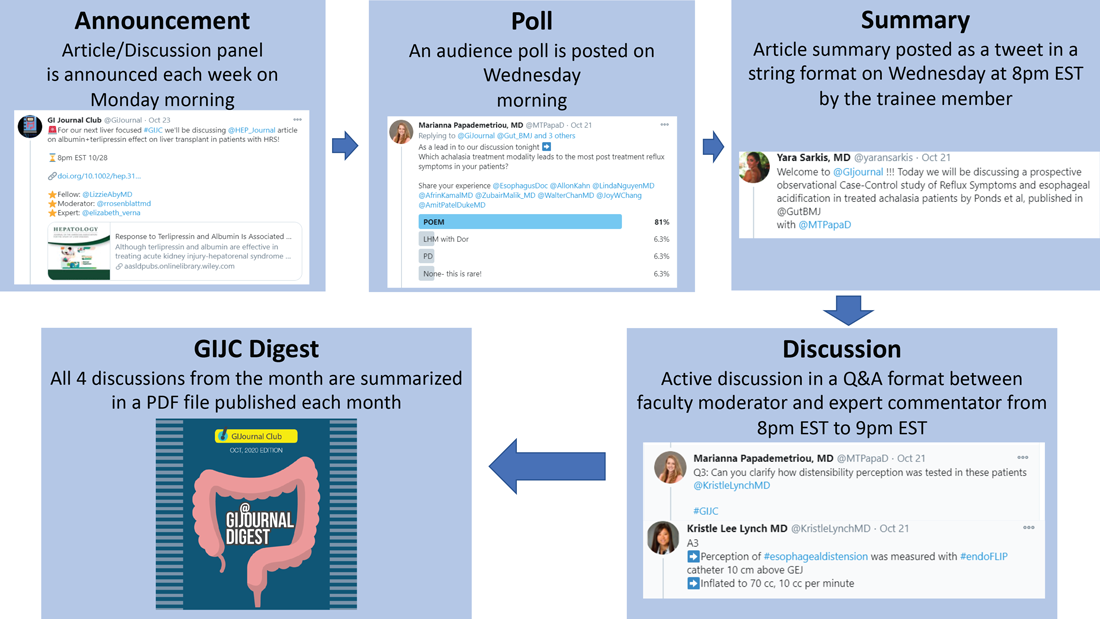
We have a large editorial board with volunteer faculty and trainees, all divided into four special interest groups (general GI/inflammatory bowel disease, interventional endoscopy/bariatric endoscopy, hepatology, and esophageal/motility disorders). Each week, a faculty member and a trainee pick a recently published article from a high-impact GI-focused journal. We also try to invite an expert of international repute (often the authors of the article themselves!) to engage as well. The faculty moderator and invited expert then work with the trainee to plan the session content. We post the topic and article on Monday. At 8 p.m. EST on Wednesday, the trainee posts a series of six to eight tweets summarizing the article. The faculty then asks the invited expert (and audience at large) a series of predetermined questions. Anyone can respond, share their opinion, and direct their own questions toward the moderator and expert who continually check their notifications and respond in real time. This brews into an hour-long discussion which covers not only the methodologic aspects of the article, but clinical practice in general. Discussions often trickle into the next day as people from different time zones participate. Everyone uses #GIJC at the end of their tweets which assists those following the article and facilitates indexing for future review. For those who miss or want to review sessions, we conveniently summarize all articles and corresponding discussions in a monthly publication, @GiJournal Digest, that is posted on Twitter for anyone to download, read and enjoy (Figure 1).
How is this different from any other journal club?
Atoosa Rabiee, MD (@AtoosaRabiee)
@GiJournal is unique in that it provides trainees and practicing gastroenterologists access to interactive discussions with both authors and world-renowned experts in the field. Online journal clubs operate with a flattened hierarchy; as such, they inherently break down access barriers to both the researchers who performed the study and key opinion leaders who commonly participate. There is no boundary as far as institutions or even countries. As a result, our platform has uncovered an unexpected degree of interest in live online discussion, and we have enjoyed collaborating and learning from experts from all over the world. @GiJournal also differs from conventional journal clubs by allowing trainees the opportunity to collaborate and engage with mentors from other institutions. As such, trainees develop relationships with experts in the field outside their home institutions, experts with whom they may not have had contact otherwise.
Although worldwide participation is a key strength of the online @GiJournal platform, it may be challenging for some members to attend the live discussion based on time difference. We account for this in two ways. First, participants are encouraged to continue with comments and questions afterward at their convenience, which allows experts and moderators to continue the conversation, often for several days. Second, to promote inclusivity, we have created a unique, customized publication to summarize and present the key points of conversation for each session. This asynchronous access is a quality not found in more traditional journal club formats. Finally, studies have shown that articles shared on social media tend to have increased citations and higher Altmetric scores.
What are the opportunities for trainees and recent graduates?
Sunil Amin, MD, MPH (@SunilAminMD)
Our surveys have shown that 30%-45% of the @GiJournal discussion participants are trainees. Both gastroenterology fellows and internal medicine residents from around the world are an integral part of each specialty panel for the weekly @GIjournal discussions. Trainees are paired up with a specific faculty mentor and together they choose an article for discussion, create a summary, informal twitter poll, and questions for the discussion. This direct access provides an opportunity for trainees to interact, ask questions, and learn from faculty in an informal atmosphere.
We have heard from multiple trainees who have developed long-term relationships with the experts and faculty mentors they worked with and are now also working on research projects. Additionally, trainees can bring the expertise they have now acquired back to their home institutions to pick articles, add specific teaching points, and enrich their local journal club discussions. Finally, trainees who present on the @GiJournal platform are given unique visibility to the many faculty members and opinion leaders participating in each discussion. This may facilitate future networking opportunities and enhance their CVs for future fellowship or employment applications.
Plans for the future?
Allon Kahn, MD (@AllonKahn)
Despite significant evolution and growth in @GiJournal over the past year, we are still actively working to expand our platform. Modes of online medical education, specifically Twitter-based GI journal club discussions, remain in their infancy. We see this @GiJournal as an opportunity for innovation as we plan for the year ahead. Our top priority for the upcoming year includes obtaining CME approval, which we are currently developing with Integrity CE (an Accreditation Council for Continuing Medical Education–accredited provider of CME for health care professionals). This will give an opportunity for the participants to be awarded CME credit when they participate in our weekly discussions. Other options being explored include starting a podcast and translation of @GiJournal Digest in different languages to reach a wider international audience. Furthermore, with the continued expansion of GI leaders and experts joining and engaging in Twitter, our options for unique and multidisciplinary discussion topics will continue to grow.
How can you join the @GiJournal discussions?
@SultanMahmoodMD
Joining the journal club discussion is easy. Just follow the @GiJournal handle on Twitter and turn on the notifications icon. Although we encourage everyone to “actively” participate in the discussion by asking questions or sharing your personal experience, joining the discussion as an “observer” is also a great way to learn. The discussion starts at 8 p.m. EST every Wednesday. Follow the #GIJC and the @GiJournal handle as questions are posted by the faculty moderator and answered by the experts. Even if you miss the discussion, the @GiJournal Digest is a great way to recap the discussions in an easy-to-read PDF format. The @GiJournal Digest is a monthly publication that archives the four @GiJournal club discussions in the previous month. Follow the link below to access the recent publications: http://ow.ly/uu2550C3RXX
Conclusion
In summary, we believe Twitter-based journal clubs offer an engaging way of virtual learning from the comfort of one’s home and a convenient way to directly interact with the experts. The success of @GiJournal highlights the importance of social media for medical education in the field of gastroenterology and hepatology and we look forward to developing this endeavor further.
Dr. Mahmood is clinical assistant professor of medicine, co–program director of the GI fellowship program, UB division of gastroenterology, hepatology & nutrition, State University of New York at Buffalo; Dr. Rabiee is assistant professor of medicine, director of hepatology, division of gastroenterology and hepatology, Washington DC VA Medical Center, Washington; Dr. Amin is assistant professor of medicine, director of endoscopy, The Lennar Foundation Medical Center, division of digestive health and liver disease, department of medicine, University of Miami; Dr. Kahn is assistant professor of medicine, division of gastroenterology & hepatology, Mayo Clinic, Scottsdale, Ariz.; and Dr. Akbar Ali is a gastroenterology fellow in the division of digestive diseases and nutrition, University of Oklahoma Health Sciences Center, Oklahoma City.
The last decade has seen an increased focus on the use of social media for medical education. Twitter, with over 330 million active users, is the most popular social media platform for medical education. We describe here our recent initiative to establish a weekly online gastroenterology-focused journal club on Twitter.
How was the idea conceived?
Sultan Mahmood, MD (@SultanMahmoodMD)
I joined #GITwitter at the end of 2019 and started following some of the leading experts in the field of gastroenterology and hepatology. It was a pleasant surprise to see how easy it was to engage with them and get expert opinions from across the world in real time. #MondayNightIBD, led by Aline Charabaty, MD, had become a phenomenon in the GI community and changed the perception of medical education in the digital world. There were online journal clubs for different medical subspecialties, including #NephroJC, #HOJournalClub, and #DermJC, but none for gastroenterology. Realizing this opportunity, and with guidance from Dr. Charabaty, we started @GiJournal in December of 2019 with weekly discussions.
@GiJournal started off as an informal discussion in which we would post a summary of the article and invite an expert in the field to comment. However, the interest in the journal club quickly took off as we gained more followers and a worldwide audience joined our journal club discussions on a weekly basis. As the COVID-19 pandemic took hold and endoscopy suites around the word closed, interest in online medical education grew. @GIJournal provided a platform for trainees and practicing physicians alike to stay up to date with the latest publications from the comfort of their homes. Needless to say, the journal club has evolved since its inception in that we now work with a team of experts and trainees who run the journal club on a rotating basis.
How does @GiJournal work?
Ijlal Akbar Ali, MD (@IjlalAkbar)
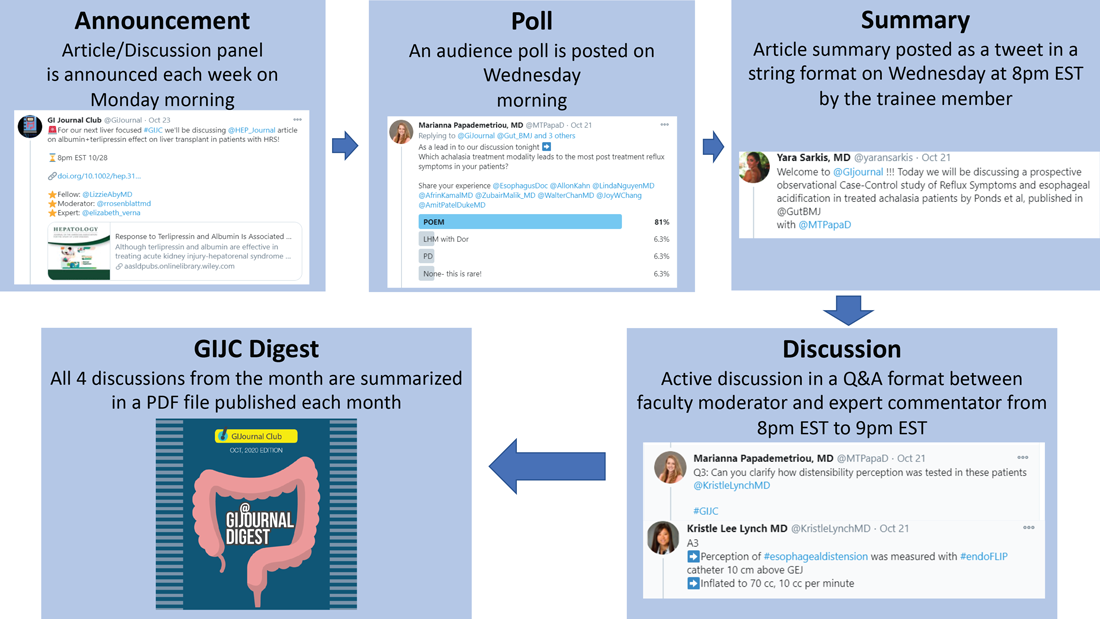
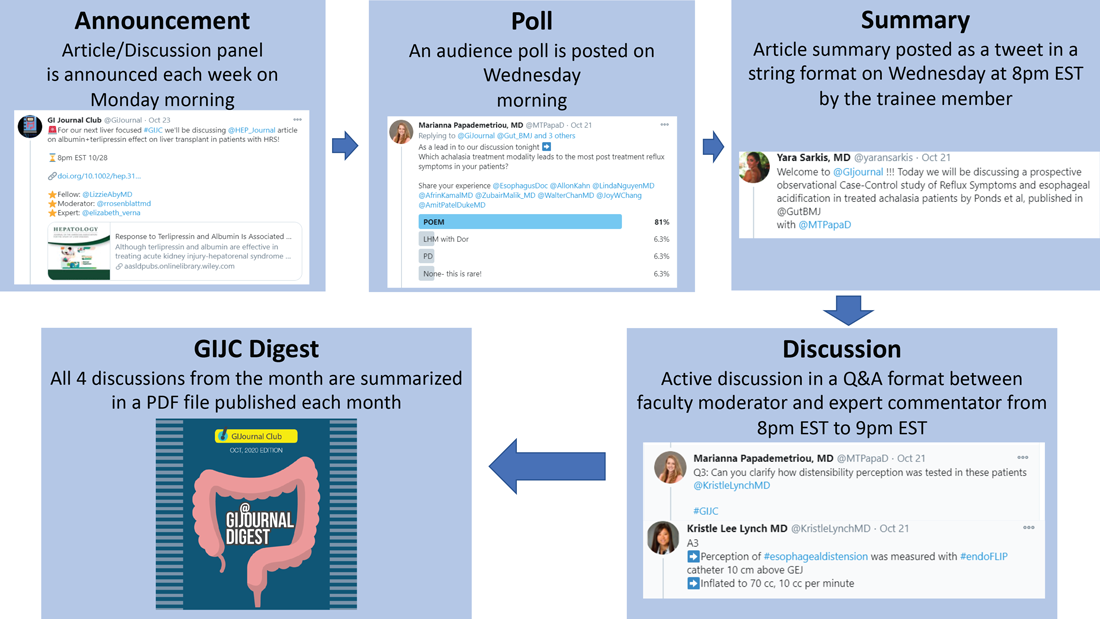
We have a large editorial board with volunteer faculty and trainees, all divided into four special interest groups (general GI/inflammatory bowel disease, interventional endoscopy/bariatric endoscopy, hepatology, and esophageal/motility disorders). Each week, a faculty member and a trainee pick a recently published article from a high-impact GI-focused journal. We also try to invite an expert of international repute (often the authors of the article themselves!) to engage as well. The faculty moderator and invited expert then work with the trainee to plan the session content. We post the topic and article on Monday. At 8 p.m. EST on Wednesday, the trainee posts a series of six to eight tweets summarizing the article. The faculty then asks the invited expert (and audience at large) a series of predetermined questions. Anyone can respond, share their opinion, and direct their own questions toward the moderator and expert who continually check their notifications and respond in real time. This brews into an hour-long discussion which covers not only the methodologic aspects of the article, but clinical practice in general. Discussions often trickle into the next day as people from different time zones participate. Everyone uses #GIJC at the end of their tweets which assists those following the article and facilitates indexing for future review. For those who miss or want to review sessions, we conveniently summarize all articles and corresponding discussions in a monthly publication, @GiJournal Digest, that is posted on Twitter for anyone to download, read and enjoy (Figure 1).
How is this different from any other journal club?
Atoosa Rabiee, MD (@AtoosaRabiee)
@GiJournal is unique in that it provides trainees and practicing gastroenterologists access to interactive discussions with both authors and world-renowned experts in the field. Online journal clubs operate with a flattened hierarchy; as such, they inherently break down access barriers to both the researchers who performed the study and key opinion leaders who commonly participate. There is no boundary as far as institutions or even countries. As a result, our platform has uncovered an unexpected degree of interest in live online discussion, and we have enjoyed collaborating and learning from experts from all over the world. @GiJournal also differs from conventional journal clubs by allowing trainees the opportunity to collaborate and engage with mentors from other institutions. As such, trainees develop relationships with experts in the field outside their home institutions, experts with whom they may not have had contact otherwise.
Although worldwide participation is a key strength of the online @GiJournal platform, it may be challenging for some members to attend the live discussion based on time difference. We account for this in two ways. First, participants are encouraged to continue with comments and questions afterward at their convenience, which allows experts and moderators to continue the conversation, often for several days. Second, to promote inclusivity, we have created a unique, customized publication to summarize and present the key points of conversation for each session. This asynchronous access is a quality not found in more traditional journal club formats. Finally, studies have shown that articles shared on social media tend to have increased citations and higher Altmetric scores.
What are the opportunities for trainees and recent graduates?
Sunil Amin, MD, MPH (@SunilAminMD)
Our surveys have shown that 30%-45% of the @GiJournal discussion participants are trainees. Both gastroenterology fellows and internal medicine residents from around the world are an integral part of each specialty panel for the weekly @GIjournal discussions. Trainees are paired up with a specific faculty mentor and together they choose an article for discussion, create a summary, informal twitter poll, and questions for the discussion. This direct access provides an opportunity for trainees to interact, ask questions, and learn from faculty in an informal atmosphere.
We have heard from multiple trainees who have developed long-term relationships with the experts and faculty mentors they worked with and are now also working on research projects. Additionally, trainees can bring the expertise they have now acquired back to their home institutions to pick articles, add specific teaching points, and enrich their local journal club discussions. Finally, trainees who present on the @GiJournal platform are given unique visibility to the many faculty members and opinion leaders participating in each discussion. This may facilitate future networking opportunities and enhance their CVs for future fellowship or employment applications.
Plans for the future?
Allon Kahn, MD (@AllonKahn)
Despite significant evolution and growth in @GiJournal over the past year, we are still actively working to expand our platform. Modes of online medical education, specifically Twitter-based GI journal club discussions, remain in their infancy. We see this @GiJournal as an opportunity for innovation as we plan for the year ahead. Our top priority for the upcoming year includes obtaining CME approval, which we are currently developing with Integrity CE (an Accreditation Council for Continuing Medical Education–accredited provider of CME for health care professionals). This will give an opportunity for the participants to be awarded CME credit when they participate in our weekly discussions. Other options being explored include starting a podcast and translation of @GiJournal Digest in different languages to reach a wider international audience. Furthermore, with the continued expansion of GI leaders and experts joining and engaging in Twitter, our options for unique and multidisciplinary discussion topics will continue to grow.
How can you join the @GiJournal discussions?
@SultanMahmoodMD
Joining the journal club discussion is easy. Just follow the @GiJournal handle on Twitter and turn on the notifications icon. Although we encourage everyone to “actively” participate in the discussion by asking questions or sharing your personal experience, joining the discussion as an “observer” is also a great way to learn. The discussion starts at 8 p.m. EST every Wednesday. Follow the #GIJC and the @GiJournal handle as questions are posted by the faculty moderator and answered by the experts. Even if you miss the discussion, the @GiJournal Digest is a great way to recap the discussions in an easy-to-read PDF format. The @GiJournal Digest is a monthly publication that archives the four @GiJournal club discussions in the previous month. Follow the link below to access the recent publications: http://ow.ly/uu2550C3RXX
Conclusion
In summary, we believe Twitter-based journal clubs offer an engaging way of virtual learning from the comfort of one’s home and a convenient way to directly interact with the experts. The success of @GiJournal highlights the importance of social media for medical education in the field of gastroenterology and hepatology and we look forward to developing this endeavor further.
Dr. Mahmood is clinical assistant professor of medicine, co–program director of the GI fellowship program, UB division of gastroenterology, hepatology & nutrition, State University of New York at Buffalo; Dr. Rabiee is assistant professor of medicine, director of hepatology, division of gastroenterology and hepatology, Washington DC VA Medical Center, Washington; Dr. Amin is assistant professor of medicine, director of endoscopy, The Lennar Foundation Medical Center, division of digestive health and liver disease, department of medicine, University of Miami; Dr. Kahn is assistant professor of medicine, division of gastroenterology & hepatology, Mayo Clinic, Scottsdale, Ariz.; and Dr. Akbar Ali is a gastroenterology fellow in the division of digestive diseases and nutrition, University of Oklahoma Health Sciences Center, Oklahoma City.
The last decade has seen an increased focus on the use of social media for medical education. Twitter, with over 330 million active users, is the most popular social media platform for medical education. We describe here our recent initiative to establish a weekly online gastroenterology-focused journal club on Twitter.
How was the idea conceived?
Sultan Mahmood, MD (@SultanMahmoodMD)
I joined #GITwitter at the end of 2019 and started following some of the leading experts in the field of gastroenterology and hepatology. It was a pleasant surprise to see how easy it was to engage with them and get expert opinions from across the world in real time. #MondayNightIBD, led by Aline Charabaty, MD, had become a phenomenon in the GI community and changed the perception of medical education in the digital world. There were online journal clubs for different medical subspecialties, including #NephroJC, #HOJournalClub, and #DermJC, but none for gastroenterology. Realizing this opportunity, and with guidance from Dr. Charabaty, we started @GiJournal in December of 2019 with weekly discussions.
@GiJournal started off as an informal discussion in which we would post a summary of the article and invite an expert in the field to comment. However, the interest in the journal club quickly took off as we gained more followers and a worldwide audience joined our journal club discussions on a weekly basis. As the COVID-19 pandemic took hold and endoscopy suites around the word closed, interest in online medical education grew. @GIJournal provided a platform for trainees and practicing physicians alike to stay up to date with the latest publications from the comfort of their homes. Needless to say, the journal club has evolved since its inception in that we now work with a team of experts and trainees who run the journal club on a rotating basis.
How does @GiJournal work?
Ijlal Akbar Ali, MD (@IjlalAkbar)
We have a large editorial board with volunteer faculty and trainees, all divided into four special interest groups (general GI/inflammatory bowel disease, interventional endoscopy/bariatric endoscopy, hepatology, and esophageal/motility disorders). Each week, a faculty member and a trainee pick a recently published article from a high-impact GI-focused journal. We also try to invite an expert of international repute (often the authors of the article themselves!) to engage as well. The faculty moderator and invited expert then work with the trainee to plan the session content. We post the topic and article on Monday. At 8 p.m. EST on Wednesday, the trainee posts a series of six to eight tweets summarizing the article. The faculty then asks the invited expert (and audience at large) a series of predetermined questions. Anyone can respond, share their opinion, and direct their own questions toward the moderator and expert who continually check their notifications and respond in real time. This brews into an hour-long discussion which covers not only the methodologic aspects of the article, but clinical practice in general. Discussions often trickle into the next day as people from different time zones participate. Everyone uses #GIJC at the end of their tweets which assists those following the article and facilitates indexing for future review. For those who miss or want to review sessions, we conveniently summarize all articles and corresponding discussions in a monthly publication, @GiJournal Digest, that is posted on Twitter for anyone to download, read and enjoy (Figure 1).
How is this different from any other journal club?
Atoosa Rabiee, MD (@AtoosaRabiee)
@GiJournal is unique in that it provides trainees and practicing gastroenterologists access to interactive discussions with both authors and world-renowned experts in the field. Online journal clubs operate with a flattened hierarchy; as such, they inherently break down access barriers to both the researchers who performed the study and key opinion leaders who commonly participate. There is no boundary as far as institutions or even countries. As a result, our platform has uncovered an unexpected degree of interest in live online discussion, and we have enjoyed collaborating and learning from experts from all over the world. @GiJournal also differs from conventional journal clubs by allowing trainees the opportunity to collaborate and engage with mentors from other institutions. As such, trainees develop relationships with experts in the field outside their home institutions, experts with whom they may not have had contact otherwise.
Although worldwide participation is a key strength of the online @GiJournal platform, it may be challenging for some members to attend the live discussion based on time difference. We account for this in two ways. First, participants are encouraged to continue with comments and questions afterward at their convenience, which allows experts and moderators to continue the conversation, often for several days. Second, to promote inclusivity, we have created a unique, customized publication to summarize and present the key points of conversation for each session. This asynchronous access is a quality not found in more traditional journal club formats. Finally, studies have shown that articles shared on social media tend to have increased citations and higher Altmetric scores.
What are the opportunities for trainees and recent graduates?
Sunil Amin, MD, MPH (@SunilAminMD)
Our surveys have shown that 30%-45% of the @GiJournal discussion participants are trainees. Both gastroenterology fellows and internal medicine residents from around the world are an integral part of each specialty panel for the weekly @GIjournal discussions. Trainees are paired up with a specific faculty mentor and together they choose an article for discussion, create a summary, informal twitter poll, and questions for the discussion. This direct access provides an opportunity for trainees to interact, ask questions, and learn from faculty in an informal atmosphere.
We have heard from multiple trainees who have developed long-term relationships with the experts and faculty mentors they worked with and are now also working on research projects. Additionally, trainees can bring the expertise they have now acquired back to their home institutions to pick articles, add specific teaching points, and enrich their local journal club discussions. Finally, trainees who present on the @GiJournal platform are given unique visibility to the many faculty members and opinion leaders participating in each discussion. This may facilitate future networking opportunities and enhance their CVs for future fellowship or employment applications.
Plans for the future?
Allon Kahn, MD (@AllonKahn)
Despite significant evolution and growth in @GiJournal over the past year, we are still actively working to expand our platform. Modes of online medical education, specifically Twitter-based GI journal club discussions, remain in their infancy. We see this @GiJournal as an opportunity for innovation as we plan for the year ahead. Our top priority for the upcoming year includes obtaining CME approval, which we are currently developing with Integrity CE (an Accreditation Council for Continuing Medical Education–accredited provider of CME for health care professionals). This will give an opportunity for the participants to be awarded CME credit when they participate in our weekly discussions. Other options being explored include starting a podcast and translation of @GiJournal Digest in different languages to reach a wider international audience. Furthermore, with the continued expansion of GI leaders and experts joining and engaging in Twitter, our options for unique and multidisciplinary discussion topics will continue to grow.
How can you join the @GiJournal discussions?
@SultanMahmoodMD
Joining the journal club discussion is easy. Just follow the @GiJournal handle on Twitter and turn on the notifications icon. Although we encourage everyone to “actively” participate in the discussion by asking questions or sharing your personal experience, joining the discussion as an “observer” is also a great way to learn. The discussion starts at 8 p.m. EST every Wednesday. Follow the #GIJC and the @GiJournal handle as questions are posted by the faculty moderator and answered by the experts. Even if you miss the discussion, the @GiJournal Digest is a great way to recap the discussions in an easy-to-read PDF format. The @GiJournal Digest is a monthly publication that archives the four @GiJournal club discussions in the previous month. Follow the link below to access the recent publications: http://ow.ly/uu2550C3RXX
Conclusion
In summary, we believe Twitter-based journal clubs offer an engaging way of virtual learning from the comfort of one’s home and a convenient way to directly interact with the experts. The success of @GiJournal highlights the importance of social media for medical education in the field of gastroenterology and hepatology and we look forward to developing this endeavor further.
Dr. Mahmood is clinical assistant professor of medicine, co–program director of the GI fellowship program, UB division of gastroenterology, hepatology & nutrition, State University of New York at Buffalo; Dr. Rabiee is assistant professor of medicine, director of hepatology, division of gastroenterology and hepatology, Washington DC VA Medical Center, Washington; Dr. Amin is assistant professor of medicine, director of endoscopy, The Lennar Foundation Medical Center, division of digestive health and liver disease, department of medicine, University of Miami; Dr. Kahn is assistant professor of medicine, division of gastroenterology & hepatology, Mayo Clinic, Scottsdale, Ariz.; and Dr. Akbar Ali is a gastroenterology fellow in the division of digestive diseases and nutrition, University of Oklahoma Health Sciences Center, Oklahoma City.