User login
Identifying type 1 diabetes drivers at risk of mishaps
A risk assessment score could help identify individuals with type 1 diabetes who are at higher risk of driving mishaps and who may benefit from interventions to reduce their risk, a new study suggests.
Writing in the June edition of Diabetes Care, Daniel J. Cox, MD, of the University of Virginia, Charlottesville, and his coauthors reported on their efforts to develop and validate a “Risk Assessment of Diabetic Drivers” (RADD) scoring system.
In the first part of the two-part study, 1,371 drivers with type 1 diabetes filled out a series of questionnaires about diabetes and driving, then recorded their driving mishaps over the subsequent year (Diabetes Care. 2017;40:742-50).
This revealed that annual driving distance, peripheral neuropathy, number of past hypoglycemia-related driving mishaps, and the degree to which the individual is bothered by hypoglycemia in general were all significantly associated with a risk of future driving incidents.
Based on this, the authors developed a scoring system using these factors and identified the optimum cut-off point for maximum sensitivity and specificity.
“The area under the curve, a global measure of model performance, was estimated to be 0.73, indicating that the model performed better than chance at classifying participants into the two risk categories,” the authors wrote.
When applied to the original participants, the model classified 37.5% of them as being high-risk. This group had an average of 3.03 driving mishaps over the 12-month follow-up, compared with 0.87 mishaps in the participants who fell into the lowest 37.5% of risk (P = .002).
In the second part of the study, 1,737 drivers with type 1 diabetes completed a version of the scoring questionnaire online, and 118 low-risk and 372 high-risk individuals were recruited.
The high-risk individuals were randomized either to a 2-month online intervention that aimed at helping people with type 1 diabetes anticipate, prevent, detect, and treat hypoglycemia while driving, as well as a program of motivational interviewing, the online intervention alone, or routine care, with 12 months of follow-up. The low-risk individuals all received routine care only.
As with the first part of the study, researchers saw a significantly lower number of driving mishaps in the low-risk participants, compared with the high-risk participants (1.65 mishaps per driver per year vs. 4.26 mishaps per driver per year; P less than .001).
After adjusting for other factors such as age, sex, method of insulin delivery, and hypoglycemia awareness, the rate of mishaps was still 2.83 times higher in the high-risk group, compared with the low-risk group (P less than .001).
The authors noted that their RADD scoring system did have a false-negative rate of 24%, classifying people as low-risk even though they reported more than one driving mishap in the following 12 months.
“This illustrates that any driver has a risk of being involved in a collision or receiving a citation, and any driver with type 1 diabetes has the additional risk of experiencing disruptive extreme [blood glucose (BG)] that can result in a mishap while driving,” they wrote. “While, ideally, all drivers with type 1 diabetes should measure their BG before driving, they should at least be counseled that, whenever they take more insulin, eat fewer carbohydrates, or engage in more physical activity than usual, they should measure their BG before driving.”
With respect to the impact of the intervention and motivational interviewing, researchers found no significant differences in the rate of mishaps between the groups who received intervention plus interview and those who received the intervention alone, and, as a result, combined these two groups into one.
The high-risk group who underwent the online intervention had fewer driving mishaps than did the high-risk group who received routine care. However, they still had 1.58 times more incidents than did the low-risk individuals who received routine care.
The intervention decreased the risk of mishaps associated with hypoglycemia in high-risk individuals, compared with that in those who recieved routine care, but these individuals still had a higher incidence of hypoglycemia-associated mishaps, compared with the low-risk individuals.
“It is also important to note that [the online intervention] only affected hypoglycemia-related driving mishaps, not hyperglycemia- or nondiabetes-related mishaps,” the authors wrote.
The study was funded by the National Institutes of Health and supported in-kind by LifeScan, Abbott Laboratories, MyGlu.com, dLife.com, and Dex4.com.
A risk assessment score could help identify individuals with type 1 diabetes who are at higher risk of driving mishaps and who may benefit from interventions to reduce their risk, a new study suggests.
Writing in the June edition of Diabetes Care, Daniel J. Cox, MD, of the University of Virginia, Charlottesville, and his coauthors reported on their efforts to develop and validate a “Risk Assessment of Diabetic Drivers” (RADD) scoring system.
In the first part of the two-part study, 1,371 drivers with type 1 diabetes filled out a series of questionnaires about diabetes and driving, then recorded their driving mishaps over the subsequent year (Diabetes Care. 2017;40:742-50).
This revealed that annual driving distance, peripheral neuropathy, number of past hypoglycemia-related driving mishaps, and the degree to which the individual is bothered by hypoglycemia in general were all significantly associated with a risk of future driving incidents.
Based on this, the authors developed a scoring system using these factors and identified the optimum cut-off point for maximum sensitivity and specificity.
“The area under the curve, a global measure of model performance, was estimated to be 0.73, indicating that the model performed better than chance at classifying participants into the two risk categories,” the authors wrote.
When applied to the original participants, the model classified 37.5% of them as being high-risk. This group had an average of 3.03 driving mishaps over the 12-month follow-up, compared with 0.87 mishaps in the participants who fell into the lowest 37.5% of risk (P = .002).
In the second part of the study, 1,737 drivers with type 1 diabetes completed a version of the scoring questionnaire online, and 118 low-risk and 372 high-risk individuals were recruited.
The high-risk individuals were randomized either to a 2-month online intervention that aimed at helping people with type 1 diabetes anticipate, prevent, detect, and treat hypoglycemia while driving, as well as a program of motivational interviewing, the online intervention alone, or routine care, with 12 months of follow-up. The low-risk individuals all received routine care only.
As with the first part of the study, researchers saw a significantly lower number of driving mishaps in the low-risk participants, compared with the high-risk participants (1.65 mishaps per driver per year vs. 4.26 mishaps per driver per year; P less than .001).
After adjusting for other factors such as age, sex, method of insulin delivery, and hypoglycemia awareness, the rate of mishaps was still 2.83 times higher in the high-risk group, compared with the low-risk group (P less than .001).
The authors noted that their RADD scoring system did have a false-negative rate of 24%, classifying people as low-risk even though they reported more than one driving mishap in the following 12 months.
“This illustrates that any driver has a risk of being involved in a collision or receiving a citation, and any driver with type 1 diabetes has the additional risk of experiencing disruptive extreme [blood glucose (BG)] that can result in a mishap while driving,” they wrote. “While, ideally, all drivers with type 1 diabetes should measure their BG before driving, they should at least be counseled that, whenever they take more insulin, eat fewer carbohydrates, or engage in more physical activity than usual, they should measure their BG before driving.”
With respect to the impact of the intervention and motivational interviewing, researchers found no significant differences in the rate of mishaps between the groups who received intervention plus interview and those who received the intervention alone, and, as a result, combined these two groups into one.
The high-risk group who underwent the online intervention had fewer driving mishaps than did the high-risk group who received routine care. However, they still had 1.58 times more incidents than did the low-risk individuals who received routine care.
The intervention decreased the risk of mishaps associated with hypoglycemia in high-risk individuals, compared with that in those who recieved routine care, but these individuals still had a higher incidence of hypoglycemia-associated mishaps, compared with the low-risk individuals.
“It is also important to note that [the online intervention] only affected hypoglycemia-related driving mishaps, not hyperglycemia- or nondiabetes-related mishaps,” the authors wrote.
The study was funded by the National Institutes of Health and supported in-kind by LifeScan, Abbott Laboratories, MyGlu.com, dLife.com, and Dex4.com.
A risk assessment score could help identify individuals with type 1 diabetes who are at higher risk of driving mishaps and who may benefit from interventions to reduce their risk, a new study suggests.
Writing in the June edition of Diabetes Care, Daniel J. Cox, MD, of the University of Virginia, Charlottesville, and his coauthors reported on their efforts to develop and validate a “Risk Assessment of Diabetic Drivers” (RADD) scoring system.
In the first part of the two-part study, 1,371 drivers with type 1 diabetes filled out a series of questionnaires about diabetes and driving, then recorded their driving mishaps over the subsequent year (Diabetes Care. 2017;40:742-50).
This revealed that annual driving distance, peripheral neuropathy, number of past hypoglycemia-related driving mishaps, and the degree to which the individual is bothered by hypoglycemia in general were all significantly associated with a risk of future driving incidents.
Based on this, the authors developed a scoring system using these factors and identified the optimum cut-off point for maximum sensitivity and specificity.
“The area under the curve, a global measure of model performance, was estimated to be 0.73, indicating that the model performed better than chance at classifying participants into the two risk categories,” the authors wrote.
When applied to the original participants, the model classified 37.5% of them as being high-risk. This group had an average of 3.03 driving mishaps over the 12-month follow-up, compared with 0.87 mishaps in the participants who fell into the lowest 37.5% of risk (P = .002).
In the second part of the study, 1,737 drivers with type 1 diabetes completed a version of the scoring questionnaire online, and 118 low-risk and 372 high-risk individuals were recruited.
The high-risk individuals were randomized either to a 2-month online intervention that aimed at helping people with type 1 diabetes anticipate, prevent, detect, and treat hypoglycemia while driving, as well as a program of motivational interviewing, the online intervention alone, or routine care, with 12 months of follow-up. The low-risk individuals all received routine care only.
As with the first part of the study, researchers saw a significantly lower number of driving mishaps in the low-risk participants, compared with the high-risk participants (1.65 mishaps per driver per year vs. 4.26 mishaps per driver per year; P less than .001).
After adjusting for other factors such as age, sex, method of insulin delivery, and hypoglycemia awareness, the rate of mishaps was still 2.83 times higher in the high-risk group, compared with the low-risk group (P less than .001).
The authors noted that their RADD scoring system did have a false-negative rate of 24%, classifying people as low-risk even though they reported more than one driving mishap in the following 12 months.
“This illustrates that any driver has a risk of being involved in a collision or receiving a citation, and any driver with type 1 diabetes has the additional risk of experiencing disruptive extreme [blood glucose (BG)] that can result in a mishap while driving,” they wrote. “While, ideally, all drivers with type 1 diabetes should measure their BG before driving, they should at least be counseled that, whenever they take more insulin, eat fewer carbohydrates, or engage in more physical activity than usual, they should measure their BG before driving.”
With respect to the impact of the intervention and motivational interviewing, researchers found no significant differences in the rate of mishaps between the groups who received intervention plus interview and those who received the intervention alone, and, as a result, combined these two groups into one.
The high-risk group who underwent the online intervention had fewer driving mishaps than did the high-risk group who received routine care. However, they still had 1.58 times more incidents than did the low-risk individuals who received routine care.
The intervention decreased the risk of mishaps associated with hypoglycemia in high-risk individuals, compared with that in those who recieved routine care, but these individuals still had a higher incidence of hypoglycemia-associated mishaps, compared with the low-risk individuals.
“It is also important to note that [the online intervention] only affected hypoglycemia-related driving mishaps, not hyperglycemia- or nondiabetes-related mishaps,” the authors wrote.
The study was funded by the National Institutes of Health and supported in-kind by LifeScan, Abbott Laboratories, MyGlu.com, dLife.com, and Dex4.com.
FROM DIABETES CARE
Key clinical point: A scoring questionnaire could help identify drivers with type 1 diabetes at greater risk of driving mishaps and those who could benefit from an intervention to reduce their risk.
Major finding: Individuals with type 1 diabetes who were classified as high-risk according to a scoring system had a more than threefold greater incidence of driving mishaps than those classified as low-risk.
Data source: A two-part study in 1,371 and 1,737 drivers with type 1 diabetes.
Disclosures: The study was funded by the National Institutes of Health and supported in-kind by LifeScan, Abbott Laboratories, MyGlu.com, dLife.com, and Dex4.com.
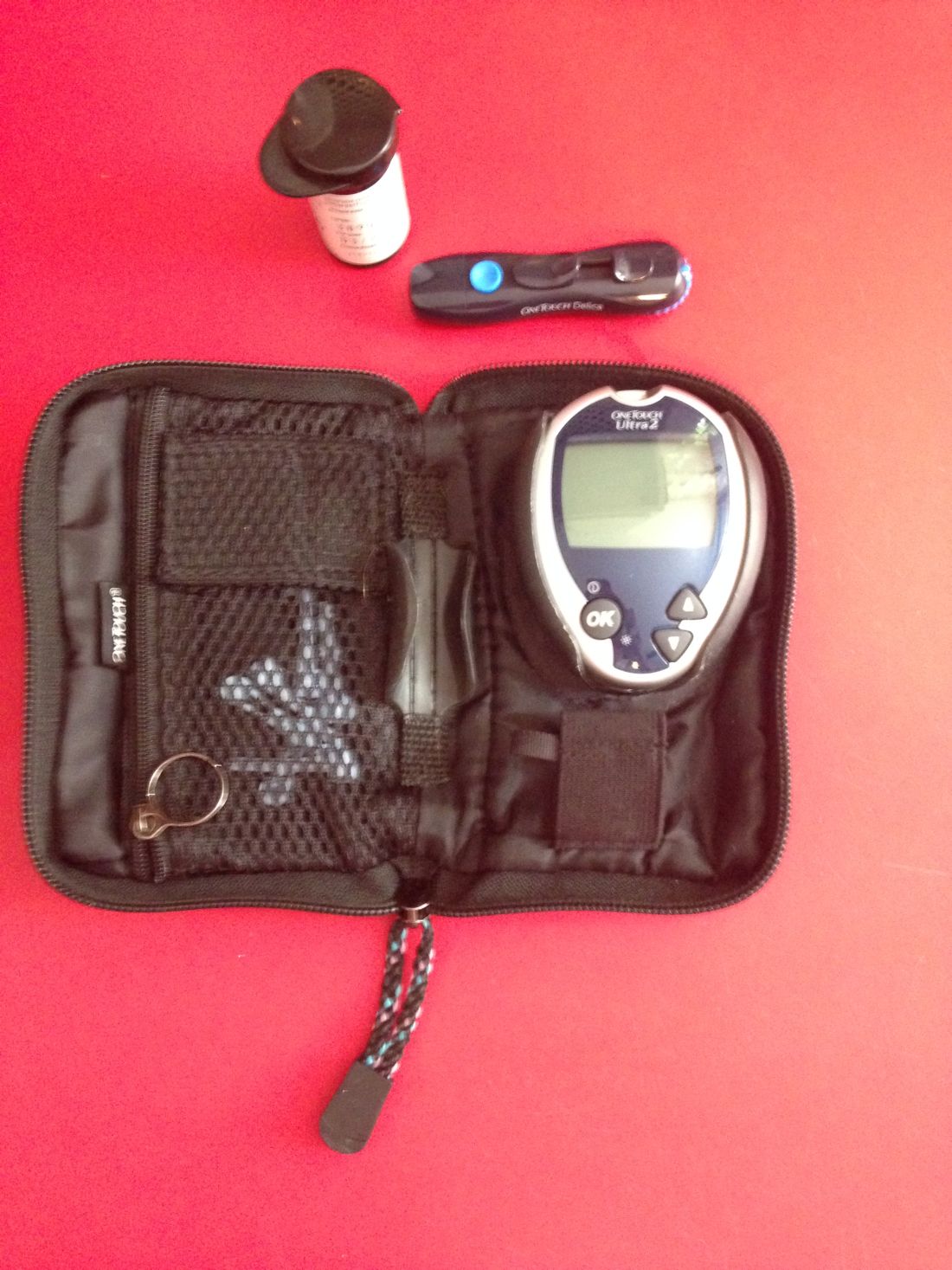
Routine blood glucose monitoring does not improve control or QOL
Self-monitoring of blood glucose in patients with non–insulin-treated type 2 diabetes mellitus (T2DM) does not appear to make any difference to blood glucose control or quality of life, a new study has found.
The researchers report the results of the Monitor Trial in which 418 patients with non–insulin-treated T2DM were randomized either to once-daily self-monitoring of blood glucose with automatic tailored messages, once-daily monitoring with no messages, and no monitoring. Their report appears in the June 10 online edition of JAMA Internal Medicine, timed to appear simultaneously with the data’s presentation at the annual meeting of the American Diabetes Association
2017.1233).
Researchers also saw no significant differences in rates of insulin initiation, the incidence of hypoglycemia, or health care utilization.
“This null result occurred despite training participants and primary care clinicians on the use and interpretation of the meter results,” wrote Laura A. Young, MD, of the University of North Carolina at Chapel Hill.
While the findings reflect data from earlier studies suggesting limited usefulness of self-monitoring of blood glucose in these patients, the authors commented that self-monitoring has persisted as a cornerstone of clinical management of non–insulin-treated T2DM.
“As the first large pragmatic U.S. trial of SMBG [self-monitoring of blood glucose], our findings provide evidence to guide patients and clinicians making important clinical decisions about routine blood glucose monitoring,” they wrote. “Based on these findings, patients and clinicians should engage in dialogue regarding SMBG with the current evidence suggesting that SMBG should not be routine for most patients with non– insulin-treated T2DM.”
The main difference seen between the three groups was in the Summary of Diabetes Self-Care Activities, which the authors said reflected the intervention itself.
Patients taking a GLP-1 agonist at baseline were significantly more likely to increase their dose of the drug if they were in one of the self-monitoring groups, compared with the no-monitoring group, but the authors noted that the numbers were small.
Researchers also saw that African Americans in the self-monitoring with messaging group had significantly lower health-related quality of life scores, compared with the no-monitoring group, although this difference was not seen with the self-monitoring without messaging.
The participants in the trial, which was conducted at 15 primary care practices in central North Carolina, were all older than 30 years and had HbA1c levels between 6.5% and 9.5% in the 6 months before screening.
Compliance rates were similar between the two self-monitoring groups and declined at a similar rate.
The authors cautioned that their study was not powered to examine the effectiveness of self-monitoring versus no monitoring in certain clinical situations, such as the initiation of a new medication or a change in medication dose.
“Proponents of routine SMBG have cited evidence that this testing approach is useful for patients with newly diagnosed diabetes or patients with poorer glycemic control,” they said.” Although disease duration, experience using SMBG, baseline glycemic control, antihyperglycemic treatment, age, race, health literacy, and number of comorbidities made no discernible difference in glycemic control at 52 weeks, absence of evidence is not evidence of absence.”
They also commented on the potential influence of more tailored interventions such as the messaging, saying that while earlier smaller studies had suggested this could be of benefit, this was not shown in their study.
The study was supported by a Patient-Centered Outcomes Research Institute Award and the National Center for Advancing Translational Sciences, National Institutes of Health. Two authors declared grants and nonfinancial support from a range of pharmaceutical companies, and the University of North Carolina licensed its interest in copyright works to Telcare for a glucose messaging and treatment algorithm for the purposes of commercialization.
In most care settings, the statement “you have diabetes” still triggers prescription of a glucometer and instruction on how to perform self-monitoring of blood glucose. Every 3 months thereafter, patients’ glucose logs are reviewed and routine self-monitoring of blood glucose is encouraged, regardless of patients’ risk of hypoglycemia or severe hyperglycemia, because common sense tells us that patients who proactively manage and monitor their diabetes should achieve better outcomes.
The surprising finding of this study make us question the current seemingly common sense–based strategy to encourage routine self-monitoring of blood glucose, and support the Choosing Wisely recommendations of the Society of General Internal Medicine and Endocrine Society that discourage frequent blood glucose monitoring among patients with type 2 diabetes. Routine self-monitoring of blood glucose merits a “less is more” designation because there were no clear benefits accrued, which leaves only possible harms.
Elaine C. Khoong, MD, is from the department of medicine, University of California, San Francisco, and Joseph S. Ross, MD, is from the section of general internal medicine, Yale University School of Medicine and associate editor of JAMA Internal Medicine. These comments are adapted from an accompanying editorial (JAMA Intern Med. 2017. Jun 10. doi: 10.1001/jamainternmed.2017.1233 ). Dr. Ross receives research funding through Yale University from Medtronic and the Food and Drug Administration, from Johnson & Johnson, the Centers for Medicare and Medicaid Services, the Blue Cross Blue Shield Association, and from the Laura and John Arnold Foundation. No other disclosures were declared.
In most care settings, the statement “you have diabetes” still triggers prescription of a glucometer and instruction on how to perform self-monitoring of blood glucose. Every 3 months thereafter, patients’ glucose logs are reviewed and routine self-monitoring of blood glucose is encouraged, regardless of patients’ risk of hypoglycemia or severe hyperglycemia, because common sense tells us that patients who proactively manage and monitor their diabetes should achieve better outcomes.
The surprising finding of this study make us question the current seemingly common sense–based strategy to encourage routine self-monitoring of blood glucose, and support the Choosing Wisely recommendations of the Society of General Internal Medicine and Endocrine Society that discourage frequent blood glucose monitoring among patients with type 2 diabetes. Routine self-monitoring of blood glucose merits a “less is more” designation because there were no clear benefits accrued, which leaves only possible harms.
Elaine C. Khoong, MD, is from the department of medicine, University of California, San Francisco, and Joseph S. Ross, MD, is from the section of general internal medicine, Yale University School of Medicine and associate editor of JAMA Internal Medicine. These comments are adapted from an accompanying editorial (JAMA Intern Med. 2017. Jun 10. doi: 10.1001/jamainternmed.2017.1233 ). Dr. Ross receives research funding through Yale University from Medtronic and the Food and Drug Administration, from Johnson & Johnson, the Centers for Medicare and Medicaid Services, the Blue Cross Blue Shield Association, and from the Laura and John Arnold Foundation. No other disclosures were declared.
In most care settings, the statement “you have diabetes” still triggers prescription of a glucometer and instruction on how to perform self-monitoring of blood glucose. Every 3 months thereafter, patients’ glucose logs are reviewed and routine self-monitoring of blood glucose is encouraged, regardless of patients’ risk of hypoglycemia or severe hyperglycemia, because common sense tells us that patients who proactively manage and monitor their diabetes should achieve better outcomes.
The surprising finding of this study make us question the current seemingly common sense–based strategy to encourage routine self-monitoring of blood glucose, and support the Choosing Wisely recommendations of the Society of General Internal Medicine and Endocrine Society that discourage frequent blood glucose monitoring among patients with type 2 diabetes. Routine self-monitoring of blood glucose merits a “less is more” designation because there were no clear benefits accrued, which leaves only possible harms.
Elaine C. Khoong, MD, is from the department of medicine, University of California, San Francisco, and Joseph S. Ross, MD, is from the section of general internal medicine, Yale University School of Medicine and associate editor of JAMA Internal Medicine. These comments are adapted from an accompanying editorial (JAMA Intern Med. 2017. Jun 10. doi: 10.1001/jamainternmed.2017.1233 ). Dr. Ross receives research funding through Yale University from Medtronic and the Food and Drug Administration, from Johnson & Johnson, the Centers for Medicare and Medicaid Services, the Blue Cross Blue Shield Association, and from the Laura and John Arnold Foundation. No other disclosures were declared.
Self-monitoring of blood glucose in patients with non–insulin-treated type 2 diabetes mellitus (T2DM) does not appear to make any difference to blood glucose control or quality of life, a new study has found.
The researchers report the results of the Monitor Trial in which 418 patients with non–insulin-treated T2DM were randomized either to once-daily self-monitoring of blood glucose with automatic tailored messages, once-daily monitoring with no messages, and no monitoring. Their report appears in the June 10 online edition of JAMA Internal Medicine, timed to appear simultaneously with the data’s presentation at the annual meeting of the American Diabetes Association
2017.1233).
Researchers also saw no significant differences in rates of insulin initiation, the incidence of hypoglycemia, or health care utilization.
“This null result occurred despite training participants and primary care clinicians on the use and interpretation of the meter results,” wrote Laura A. Young, MD, of the University of North Carolina at Chapel Hill.
While the findings reflect data from earlier studies suggesting limited usefulness of self-monitoring of blood glucose in these patients, the authors commented that self-monitoring has persisted as a cornerstone of clinical management of non–insulin-treated T2DM.
“As the first large pragmatic U.S. trial of SMBG [self-monitoring of blood glucose], our findings provide evidence to guide patients and clinicians making important clinical decisions about routine blood glucose monitoring,” they wrote. “Based on these findings, patients and clinicians should engage in dialogue regarding SMBG with the current evidence suggesting that SMBG should not be routine for most patients with non– insulin-treated T2DM.”
The main difference seen between the three groups was in the Summary of Diabetes Self-Care Activities, which the authors said reflected the intervention itself.
Patients taking a GLP-1 agonist at baseline were significantly more likely to increase their dose of the drug if they were in one of the self-monitoring groups, compared with the no-monitoring group, but the authors noted that the numbers were small.
Researchers also saw that African Americans in the self-monitoring with messaging group had significantly lower health-related quality of life scores, compared with the no-monitoring group, although this difference was not seen with the self-monitoring without messaging.
The participants in the trial, which was conducted at 15 primary care practices in central North Carolina, were all older than 30 years and had HbA1c levels between 6.5% and 9.5% in the 6 months before screening.
Compliance rates were similar between the two self-monitoring groups and declined at a similar rate.
The authors cautioned that their study was not powered to examine the effectiveness of self-monitoring versus no monitoring in certain clinical situations, such as the initiation of a new medication or a change in medication dose.
“Proponents of routine SMBG have cited evidence that this testing approach is useful for patients with newly diagnosed diabetes or patients with poorer glycemic control,” they said.” Although disease duration, experience using SMBG, baseline glycemic control, antihyperglycemic treatment, age, race, health literacy, and number of comorbidities made no discernible difference in glycemic control at 52 weeks, absence of evidence is not evidence of absence.”
They also commented on the potential influence of more tailored interventions such as the messaging, saying that while earlier smaller studies had suggested this could be of benefit, this was not shown in their study.
The study was supported by a Patient-Centered Outcomes Research Institute Award and the National Center for Advancing Translational Sciences, National Institutes of Health. Two authors declared grants and nonfinancial support from a range of pharmaceutical companies, and the University of North Carolina licensed its interest in copyright works to Telcare for a glucose messaging and treatment algorithm for the purposes of commercialization.
Self-monitoring of blood glucose in patients with non–insulin-treated type 2 diabetes mellitus (T2DM) does not appear to make any difference to blood glucose control or quality of life, a new study has found.
The researchers report the results of the Monitor Trial in which 418 patients with non–insulin-treated T2DM were randomized either to once-daily self-monitoring of blood glucose with automatic tailored messages, once-daily monitoring with no messages, and no monitoring. Their report appears in the June 10 online edition of JAMA Internal Medicine, timed to appear simultaneously with the data’s presentation at the annual meeting of the American Diabetes Association
2017.1233).
Researchers also saw no significant differences in rates of insulin initiation, the incidence of hypoglycemia, or health care utilization.
“This null result occurred despite training participants and primary care clinicians on the use and interpretation of the meter results,” wrote Laura A. Young, MD, of the University of North Carolina at Chapel Hill.
While the findings reflect data from earlier studies suggesting limited usefulness of self-monitoring of blood glucose in these patients, the authors commented that self-monitoring has persisted as a cornerstone of clinical management of non–insulin-treated T2DM.
“As the first large pragmatic U.S. trial of SMBG [self-monitoring of blood glucose], our findings provide evidence to guide patients and clinicians making important clinical decisions about routine blood glucose monitoring,” they wrote. “Based on these findings, patients and clinicians should engage in dialogue regarding SMBG with the current evidence suggesting that SMBG should not be routine for most patients with non– insulin-treated T2DM.”
The main difference seen between the three groups was in the Summary of Diabetes Self-Care Activities, which the authors said reflected the intervention itself.
Patients taking a GLP-1 agonist at baseline were significantly more likely to increase their dose of the drug if they were in one of the self-monitoring groups, compared with the no-monitoring group, but the authors noted that the numbers were small.
Researchers also saw that African Americans in the self-monitoring with messaging group had significantly lower health-related quality of life scores, compared with the no-monitoring group, although this difference was not seen with the self-monitoring without messaging.
The participants in the trial, which was conducted at 15 primary care practices in central North Carolina, were all older than 30 years and had HbA1c levels between 6.5% and 9.5% in the 6 months before screening.
Compliance rates were similar between the two self-monitoring groups and declined at a similar rate.
The authors cautioned that their study was not powered to examine the effectiveness of self-monitoring versus no monitoring in certain clinical situations, such as the initiation of a new medication or a change in medication dose.
“Proponents of routine SMBG have cited evidence that this testing approach is useful for patients with newly diagnosed diabetes or patients with poorer glycemic control,” they said.” Although disease duration, experience using SMBG, baseline glycemic control, antihyperglycemic treatment, age, race, health literacy, and number of comorbidities made no discernible difference in glycemic control at 52 weeks, absence of evidence is not evidence of absence.”
They also commented on the potential influence of more tailored interventions such as the messaging, saying that while earlier smaller studies had suggested this could be of benefit, this was not shown in their study.
The study was supported by a Patient-Centered Outcomes Research Institute Award and the National Center for Advancing Translational Sciences, National Institutes of Health. Two authors declared grants and nonfinancial support from a range of pharmaceutical companies, and the University of North Carolina licensed its interest in copyright works to Telcare for a glucose messaging and treatment algorithm for the purposes of commercialization.
FROM JAMA INTERNAL MEDICINE
Key clinical point:
Major finding: Patients with non–insulin-treated T2DM who do not use routine self-monitoring of blood glucose show the same blood glucose control and health-related quality of life as those who do self-monitor.
Data source: A 1-year open-label randomized trial in 418 patients with T2DM.
Disclosures: The study was supported by a Patient-Centered Outcomes Research Institute Award and the National Center for Advancing Translational Sciences, National Institutes of Health. Two authors declared grants and nonfinancial support from a range of pharmaceutical companies, and the University of North Carolina licensed its interest in copyright works to Telcare for a glucose messaging and treatment algorithm for the purposes of commercialization.
Limitations with molecular techniques in detecting onychomycosis
Real-time PCR techniques for identifying the pathogens responsible for onychomycosis can offer some advantages over conventional diagnostic approaches but also have their limitations, say the authors of a study published in Mycoses.
Anissa Z. Hafirassou of Frères-Mentouri, Constantine University, Algeria, and colleagues analyzed nail samples from 70 patients with clinical signs of onychomycosis and 15 healthy controls using four different real-time PCR assays – a panfungal, a pandermatophyte, an assay for Candida and one for Aspergillus – and conventional methods.
Most samples were of Trichophyton species and were found in patients with proven onychomycosis. In contrast, the sequencing results from the healthy samples were all negative.
The pandermatophyte analysis found dermatophyte DNA in 60% of cases – most of were proven cases of onychomycosis – representing a sensitivity of 90% compared to positive culture. This analysis showed 90% sensitivity compared to cultures, but there was no correlation between culture results and pandermatophyte RT-PCR in nine cases.
This technique also detected Trichophyton cases in 15 patients who had negative culture results, but found amplification products in three of the control subjects, two of which were Penicillium chrysogenum. However two culture-positive samples showed up as negative with both the panfungal and pandermatophyte methods.
“Due to the low sensitivity of the panfungal assay and the lack of correlation between cultures and PCR results, the possibility of the presence of environmental and colonizing species together with pathological species in nail samples, was studied,” the authors wrote.
Twenty-five fingernail samples that were negative on the panfungal analysis were also tested for Candida and Aspergillus. Candida species were detected in 76% of these samples, and Aspergillus in 60%, while 64% contained mixed populations. Ten samples contained more than one species of Candida and one had two species of Aspergillus.
“Conventional diagnostic methods have several limitations such as time-cost, low sensitivity and the need of skilled personnel,” the authors wrote, noting that the molecular methods also had limitations to their usefulness.
The panfungal method showed low sensitivity, which may have been due to the mix of fungal populations that was found even in healthy controls, the researchers added.
“The pandermatophyte assay was sensitive and specific but only detected dermatophyte species and did not allow differentiation among them,” they wrote.
The role of nondermatophyte species isolated from onychomycosis should be considered carefully, as these are also found in healthy nails, the researchers noted.
The study and one author were supported by the Spanish Fondo de Investigaciones Sanitarias of the Instituto de Salud Carlos III. No conflicts of interest were declared.
Real-time PCR techniques for identifying the pathogens responsible for onychomycosis can offer some advantages over conventional diagnostic approaches but also have their limitations, say the authors of a study published in Mycoses.
Anissa Z. Hafirassou of Frères-Mentouri, Constantine University, Algeria, and colleagues analyzed nail samples from 70 patients with clinical signs of onychomycosis and 15 healthy controls using four different real-time PCR assays – a panfungal, a pandermatophyte, an assay for Candida and one for Aspergillus – and conventional methods.
Most samples were of Trichophyton species and were found in patients with proven onychomycosis. In contrast, the sequencing results from the healthy samples were all negative.
The pandermatophyte analysis found dermatophyte DNA in 60% of cases – most of were proven cases of onychomycosis – representing a sensitivity of 90% compared to positive culture. This analysis showed 90% sensitivity compared to cultures, but there was no correlation between culture results and pandermatophyte RT-PCR in nine cases.
This technique also detected Trichophyton cases in 15 patients who had negative culture results, but found amplification products in three of the control subjects, two of which were Penicillium chrysogenum. However two culture-positive samples showed up as negative with both the panfungal and pandermatophyte methods.
“Due to the low sensitivity of the panfungal assay and the lack of correlation between cultures and PCR results, the possibility of the presence of environmental and colonizing species together with pathological species in nail samples, was studied,” the authors wrote.
Twenty-five fingernail samples that were negative on the panfungal analysis were also tested for Candida and Aspergillus. Candida species were detected in 76% of these samples, and Aspergillus in 60%, while 64% contained mixed populations. Ten samples contained more than one species of Candida and one had two species of Aspergillus.
“Conventional diagnostic methods have several limitations such as time-cost, low sensitivity and the need of skilled personnel,” the authors wrote, noting that the molecular methods also had limitations to their usefulness.
The panfungal method showed low sensitivity, which may have been due to the mix of fungal populations that was found even in healthy controls, the researchers added.
“The pandermatophyte assay was sensitive and specific but only detected dermatophyte species and did not allow differentiation among them,” they wrote.
The role of nondermatophyte species isolated from onychomycosis should be considered carefully, as these are also found in healthy nails, the researchers noted.
The study and one author were supported by the Spanish Fondo de Investigaciones Sanitarias of the Instituto de Salud Carlos III. No conflicts of interest were declared.
Real-time PCR techniques for identifying the pathogens responsible for onychomycosis can offer some advantages over conventional diagnostic approaches but also have their limitations, say the authors of a study published in Mycoses.
Anissa Z. Hafirassou of Frères-Mentouri, Constantine University, Algeria, and colleagues analyzed nail samples from 70 patients with clinical signs of onychomycosis and 15 healthy controls using four different real-time PCR assays – a panfungal, a pandermatophyte, an assay for Candida and one for Aspergillus – and conventional methods.
Most samples were of Trichophyton species and were found in patients with proven onychomycosis. In contrast, the sequencing results from the healthy samples were all negative.
The pandermatophyte analysis found dermatophyte DNA in 60% of cases – most of were proven cases of onychomycosis – representing a sensitivity of 90% compared to positive culture. This analysis showed 90% sensitivity compared to cultures, but there was no correlation between culture results and pandermatophyte RT-PCR in nine cases.
This technique also detected Trichophyton cases in 15 patients who had negative culture results, but found amplification products in three of the control subjects, two of which were Penicillium chrysogenum. However two culture-positive samples showed up as negative with both the panfungal and pandermatophyte methods.
“Due to the low sensitivity of the panfungal assay and the lack of correlation between cultures and PCR results, the possibility of the presence of environmental and colonizing species together with pathological species in nail samples, was studied,” the authors wrote.
Twenty-five fingernail samples that were negative on the panfungal analysis were also tested for Candida and Aspergillus. Candida species were detected in 76% of these samples, and Aspergillus in 60%, while 64% contained mixed populations. Ten samples contained more than one species of Candida and one had two species of Aspergillus.
“Conventional diagnostic methods have several limitations such as time-cost, low sensitivity and the need of skilled personnel,” the authors wrote, noting that the molecular methods also had limitations to their usefulness.
The panfungal method showed low sensitivity, which may have been due to the mix of fungal populations that was found even in healthy controls, the researchers added.
“The pandermatophyte assay was sensitive and specific but only detected dermatophyte species and did not allow differentiation among them,” they wrote.
The role of nondermatophyte species isolated from onychomycosis should be considered carefully, as these are also found in healthy nails, the researchers noted.
The study and one author were supported by the Spanish Fondo de Investigaciones Sanitarias of the Instituto de Salud Carlos III. No conflicts of interest were declared.
FROM MYCOSES
Key clinical point: Real-time PCR techniques for identifying the pathogens in onychomycosis have some advantages over culture but also have their limitations.
Major finding: Panfungal real-time PCR had a sensitivity of 47% and pandermatophyte RT-PCR had a sensitivity of 90% compared to positive culture.
Data source: Analysis of toenail samples from 70 patients with onychomycosis and 15 healthy controls.
Disclosures: The study and one author were supported by the Spanish Fondo de Investigaciones Sanitarias of the Instituto de Salud Carlos III. No conflicts of interest were declared.
Desmoplastic trichoepithelioma may co-occur with BCC
SYDNEY, AUSTRALIA – Watchful waiting may not be the safest approach for managing patients with desmoplastic trichoepithelioma, according to a speaker at the annual meeting of the Australasian College of Dermatologists, who described five cases of the benign tumor combined with basal cell carcinoma.
Desmoplastic trichoepithelioma (DTE), a rare benign tumor that typically presents as a small, slow-growing, asymptomatic, skin-colored lesion on the face, with a depressed nonulcerated center and often raised edges, is managed with watchful waiting or local excision. While its key histopathologic features are narrow cords or strands of basaloid cells, numerous small keratin-filled cysts, and a surrounding desmoplastic core, DTE can be confused with morpheaform basal cell carcinoma (BCC), Tristan Blake, MD, dermatology registrar at Royal Brisbane and Womens’ Hospital, Brisbane, Australia, said at the meeting.
“At this stage, there’s no way to confidently say, looking at the slides, if those cases were desmoplastic trichoepithelioma arising in basal cell carcinoma or vice versa, or if they were a single tumor with divergent differentiation, or an occlusion of two separate tumors,” he said.
Dr. Blake added that this was the first time, to his knowledge, that such a combination had been reported, and that the finding had the potential to change the way DTE is managed.
“How can you now confidently elect to leave or watch the desmoplastic trichoepithelioma patients you have, knowing that not an insignificant portion might also harbor BCC or develop BCC in the future?” he said. This dilemma is made more acute by the fact that DTEs are typically found in younger patients and on the face, he added.
Two dermatopathologists involved in the retrospective review of cases reported that histochemistry was not particularly useful in differentiating DTE from other tumors, he noted.
Patients in the study were also interviewed about their tumors and reported no symptoms; when asked how long the lesions had been there prior to diagnosis, those who could recall said the lesions had likely been present for decades.
In an interview, Dr. Blake said that the discovery of coexisting DTE and BCC was a surprise, and cast doubt on the practice of watchful waiting.
No conflicts of interest were declared.
SYDNEY, AUSTRALIA – Watchful waiting may not be the safest approach for managing patients with desmoplastic trichoepithelioma, according to a speaker at the annual meeting of the Australasian College of Dermatologists, who described five cases of the benign tumor combined with basal cell carcinoma.
Desmoplastic trichoepithelioma (DTE), a rare benign tumor that typically presents as a small, slow-growing, asymptomatic, skin-colored lesion on the face, with a depressed nonulcerated center and often raised edges, is managed with watchful waiting or local excision. While its key histopathologic features are narrow cords or strands of basaloid cells, numerous small keratin-filled cysts, and a surrounding desmoplastic core, DTE can be confused with morpheaform basal cell carcinoma (BCC), Tristan Blake, MD, dermatology registrar at Royal Brisbane and Womens’ Hospital, Brisbane, Australia, said at the meeting.
“At this stage, there’s no way to confidently say, looking at the slides, if those cases were desmoplastic trichoepithelioma arising in basal cell carcinoma or vice versa, or if they were a single tumor with divergent differentiation, or an occlusion of two separate tumors,” he said.
Dr. Blake added that this was the first time, to his knowledge, that such a combination had been reported, and that the finding had the potential to change the way DTE is managed.
“How can you now confidently elect to leave or watch the desmoplastic trichoepithelioma patients you have, knowing that not an insignificant portion might also harbor BCC or develop BCC in the future?” he said. This dilemma is made more acute by the fact that DTEs are typically found in younger patients and on the face, he added.
Two dermatopathologists involved in the retrospective review of cases reported that histochemistry was not particularly useful in differentiating DTE from other tumors, he noted.
Patients in the study were also interviewed about their tumors and reported no symptoms; when asked how long the lesions had been there prior to diagnosis, those who could recall said the lesions had likely been present for decades.
In an interview, Dr. Blake said that the discovery of coexisting DTE and BCC was a surprise, and cast doubt on the practice of watchful waiting.
No conflicts of interest were declared.
SYDNEY, AUSTRALIA – Watchful waiting may not be the safest approach for managing patients with desmoplastic trichoepithelioma, according to a speaker at the annual meeting of the Australasian College of Dermatologists, who described five cases of the benign tumor combined with basal cell carcinoma.
Desmoplastic trichoepithelioma (DTE), a rare benign tumor that typically presents as a small, slow-growing, asymptomatic, skin-colored lesion on the face, with a depressed nonulcerated center and often raised edges, is managed with watchful waiting or local excision. While its key histopathologic features are narrow cords or strands of basaloid cells, numerous small keratin-filled cysts, and a surrounding desmoplastic core, DTE can be confused with morpheaform basal cell carcinoma (BCC), Tristan Blake, MD, dermatology registrar at Royal Brisbane and Womens’ Hospital, Brisbane, Australia, said at the meeting.
“At this stage, there’s no way to confidently say, looking at the slides, if those cases were desmoplastic trichoepithelioma arising in basal cell carcinoma or vice versa, or if they were a single tumor with divergent differentiation, or an occlusion of two separate tumors,” he said.
Dr. Blake added that this was the first time, to his knowledge, that such a combination had been reported, and that the finding had the potential to change the way DTE is managed.
“How can you now confidently elect to leave or watch the desmoplastic trichoepithelioma patients you have, knowing that not an insignificant portion might also harbor BCC or develop BCC in the future?” he said. This dilemma is made more acute by the fact that DTEs are typically found in younger patients and on the face, he added.
Two dermatopathologists involved in the retrospective review of cases reported that histochemistry was not particularly useful in differentiating DTE from other tumors, he noted.
Patients in the study were also interviewed about their tumors and reported no symptoms; when asked how long the lesions had been there prior to diagnosis, those who could recall said the lesions had likely been present for decades.
In an interview, Dr. Blake said that the discovery of coexisting DTE and BCC was a surprise, and cast doubt on the practice of watchful waiting.
No conflicts of interest were declared.
AT ACDASM 2017
Key clinical point: Watchful waiting may no longer be the obvious choice for desmoplastic trichoepithelioma, with evidence that the benign tumor may co-occur with basal cell carcinoma.
Major finding: Researchers reported five cases in which both DTE and BCC were identified in the same pathology specimen.
Data source: A retrospective review of 27 patients with DTE, which included reexamination of specimens.
Disclosures: No conflicts of interest were declared.
Mupirocin plus chlorhexidine halved Mohs surgical-site infections
SYDNEY – All patients undergoing Mohs surgery should be treated with intranasal mupirocin and a chlorhexidine body wash for 5 days before surgery, without any requirement for a nasal swab positive for Staphylococcus aureus, according to Dr. Harvey Smith.
He presented data from a randomized, controlled trial investigating the prevention of surgical-site infection in 1,002 patients undergoing Mohs surgery who had a negative nasal swab result for S. aureus. Patients were randomized to intranasal mupirocin ointment twice daily and chlorhexidine body wash daily for the 5 days before surgery, or no intervention, said Dr. Smith, a dermatologist in group practice in Perth, Australia.
The results add to earlier studies by the same group. The first study – Staph 1 – showed that swab-positive nasal carriage of S. aureus was a greater risk factor for surgical-site infections in Mohs surgery than the Wright criteria, and that decolonization with intranasal mupirocin and chlorhexidine body wash for a few days before surgery reduced the risk of infection in these patients from 12% to 4%.
The second previous study – Staph 2 – showed that using mupirocin and chlorhexidine before surgery was actually superior to the recommended treatment of stat oral cephalexin in reducing the risk of surgical-site infection.
“So, our third paper has been wondering what to do about the silent majority: These are the two-thirds of patients on whom we operate who have a negative swab for S. aureus,” Dr. Harvey said.
A negative nasal swab was not significant, he said, because skin microbiome studies had already demonstrated that humans carry S. aureus in several places, particularly the feet and buttocks.
“What we’re basically saying is we don’t think you need to swab people, because they’ve got it somewhere,” Dr. Harvey said in an interview. “We don’t think risk stratification is useful anymore, because we’ve shown it’s a benefit to everybody.”
The strategy of treating all patients with mupirocin and chlorhexidine, regardless of nasal carriage, rather than using the broad-spectrum cephalexin, fits with the World Health Organization’s global action plan on antimicrobial resistance, Dr. Harvey explained.
While there had been cases of mupirocin resistance in the past, Dr. Harvey said these had been seen in places where the drug had previously been available over the counter, such as New Zealand. However, there was no evidence of resistance developing for such a short course of use as employed in this setting, he said.
An audience member asked about whether there were any side effects from the mupirocin or chlorhexidine. Dr. Harvey said the main potential adverse event from the treatment was the risk of chlorhexidine toxicity to the cornea. However, he said that patients were told not to get the wash near their eyes.
Apart from one or two patients with eczema who could not tolerate the full 5 days of the chlorhexidine, Dr. Harvey said they had now treated more than 4,000 patients with no other side effects observed.
The study was supported by the Australasian College of Dermatologists. No conflicts of interest were declared.
SYDNEY – All patients undergoing Mohs surgery should be treated with intranasal mupirocin and a chlorhexidine body wash for 5 days before surgery, without any requirement for a nasal swab positive for Staphylococcus aureus, according to Dr. Harvey Smith.
He presented data from a randomized, controlled trial investigating the prevention of surgical-site infection in 1,002 patients undergoing Mohs surgery who had a negative nasal swab result for S. aureus. Patients were randomized to intranasal mupirocin ointment twice daily and chlorhexidine body wash daily for the 5 days before surgery, or no intervention, said Dr. Smith, a dermatologist in group practice in Perth, Australia.
The results add to earlier studies by the same group. The first study – Staph 1 – showed that swab-positive nasal carriage of S. aureus was a greater risk factor for surgical-site infections in Mohs surgery than the Wright criteria, and that decolonization with intranasal mupirocin and chlorhexidine body wash for a few days before surgery reduced the risk of infection in these patients from 12% to 4%.
The second previous study – Staph 2 – showed that using mupirocin and chlorhexidine before surgery was actually superior to the recommended treatment of stat oral cephalexin in reducing the risk of surgical-site infection.
“So, our third paper has been wondering what to do about the silent majority: These are the two-thirds of patients on whom we operate who have a negative swab for S. aureus,” Dr. Harvey said.
A negative nasal swab was not significant, he said, because skin microbiome studies had already demonstrated that humans carry S. aureus in several places, particularly the feet and buttocks.
“What we’re basically saying is we don’t think you need to swab people, because they’ve got it somewhere,” Dr. Harvey said in an interview. “We don’t think risk stratification is useful anymore, because we’ve shown it’s a benefit to everybody.”
The strategy of treating all patients with mupirocin and chlorhexidine, regardless of nasal carriage, rather than using the broad-spectrum cephalexin, fits with the World Health Organization’s global action plan on antimicrobial resistance, Dr. Harvey explained.
While there had been cases of mupirocin resistance in the past, Dr. Harvey said these had been seen in places where the drug had previously been available over the counter, such as New Zealand. However, there was no evidence of resistance developing for such a short course of use as employed in this setting, he said.
An audience member asked about whether there were any side effects from the mupirocin or chlorhexidine. Dr. Harvey said the main potential adverse event from the treatment was the risk of chlorhexidine toxicity to the cornea. However, he said that patients were told not to get the wash near their eyes.
Apart from one or two patients with eczema who could not tolerate the full 5 days of the chlorhexidine, Dr. Harvey said they had now treated more than 4,000 patients with no other side effects observed.
The study was supported by the Australasian College of Dermatologists. No conflicts of interest were declared.
SYDNEY – All patients undergoing Mohs surgery should be treated with intranasal mupirocin and a chlorhexidine body wash for 5 days before surgery, without any requirement for a nasal swab positive for Staphylococcus aureus, according to Dr. Harvey Smith.
He presented data from a randomized, controlled trial investigating the prevention of surgical-site infection in 1,002 patients undergoing Mohs surgery who had a negative nasal swab result for S. aureus. Patients were randomized to intranasal mupirocin ointment twice daily and chlorhexidine body wash daily for the 5 days before surgery, or no intervention, said Dr. Smith, a dermatologist in group practice in Perth, Australia.
The results add to earlier studies by the same group. The first study – Staph 1 – showed that swab-positive nasal carriage of S. aureus was a greater risk factor for surgical-site infections in Mohs surgery than the Wright criteria, and that decolonization with intranasal mupirocin and chlorhexidine body wash for a few days before surgery reduced the risk of infection in these patients from 12% to 4%.
The second previous study – Staph 2 – showed that using mupirocin and chlorhexidine before surgery was actually superior to the recommended treatment of stat oral cephalexin in reducing the risk of surgical-site infection.
“So, our third paper has been wondering what to do about the silent majority: These are the two-thirds of patients on whom we operate who have a negative swab for S. aureus,” Dr. Harvey said.
A negative nasal swab was not significant, he said, because skin microbiome studies had already demonstrated that humans carry S. aureus in several places, particularly the feet and buttocks.
“What we’re basically saying is we don’t think you need to swab people, because they’ve got it somewhere,” Dr. Harvey said in an interview. “We don’t think risk stratification is useful anymore, because we’ve shown it’s a benefit to everybody.”
The strategy of treating all patients with mupirocin and chlorhexidine, regardless of nasal carriage, rather than using the broad-spectrum cephalexin, fits with the World Health Organization’s global action plan on antimicrobial resistance, Dr. Harvey explained.
While there had been cases of mupirocin resistance in the past, Dr. Harvey said these had been seen in places where the drug had previously been available over the counter, such as New Zealand. However, there was no evidence of resistance developing for such a short course of use as employed in this setting, he said.
An audience member asked about whether there were any side effects from the mupirocin or chlorhexidine. Dr. Harvey said the main potential adverse event from the treatment was the risk of chlorhexidine toxicity to the cornea. However, he said that patients were told not to get the wash near their eyes.
Apart from one or two patients with eczema who could not tolerate the full 5 days of the chlorhexidine, Dr. Harvey said they had now treated more than 4,000 patients with no other side effects observed.
The study was supported by the Australasian College of Dermatologists. No conflicts of interest were declared.
Key clinical point: Treat all patients undergoing Mohs surgery with intranasal mupirocin and a chlorhexidine body wash for 5 days before surgery, without the need for a nasal swab for Staphylococcus aureus.
Major finding: Treating patients undergoing Mohs surgery with intranasal mupirocin and a chlorhexidine body wash for 5 days before surgery halved the risk of surgical-site infections, even if the patients did not have a positive nasal swab for S. aureus.
Data source: A randomized, controlled trial in 1,002 patients with a negative nasal swab for S. aureus undergoing Mohs surgery.
Disclosures: The study was partly supported by the Australasian College of Dermatologists. No conflicts of interest were declared.
HCV incidence in young women doubled 2006-2014
The incidence of hepatitis C virus infection in reproductive-age women has doubled between 2006 and 2014 while the number of acute cases increased more than threefold, according to data published in the Annals of Internal Medicine.
Researchers analyzed data from the National Notifiable Diseases Surveillance System (NNDSS) from 2006 to 2014 and the Quest Diagnostics Health Trends national database from 2011 to 2014, finding 425,322 women with confirmed HCV infection, 40.4% of whom were aged 15-44 years.
Around half of all acute infections were in non-Hispanic white women, and of the 2,069 women with available risk information, 63% acknowledged injection drug use (Ann Intern Med. 2017 May 8. doi: 10.7326/M16-2350).
The analysis also found 1,859 cases of hepatitis C infection in children aged 2-13 years. According to the Quest data, the proportion of children with current hepatitis C infection was 3.2-fold higher in children aged 2-3 years than in those aged 12-13 years.
Commenting on this age difference, Kathleen N. Ly, MPH, from the Centers for Disease Control and Prevention, and her coauthors noted that it may have been the result of decreased testing over time in children already known to have chronic hepatitis C infection, or could be caused by spontaneous remission of infection, which is more common in infants and children than in adults.
The rate of infection among pregnant women tested for hepatitis C virus between 2011 and 2014 was 0.73%, which the authors calculated would mean that overall, 29,000 women with hepatitis C virus infection gave birth during that period across the United States. Based on data from a recent systematic review and meta-analysis, which found a likely mother-to-child transmission rate of 5.8/100 live births, they estimated that 1,700 infants were born with hepatitis C infection during that period.
“In contrast, only about 200 childhood cases per year are reported to the NNDSS, which may suggest a need for wider screening for HCV in pregnant women and their infants, as is recommended for HIV and hepatitis B virus,” the authors wrote. “However, recommendations for screening in pregnant women and clearer testing guidelines for infants born to HCV-infected mothers do not exist at this time.”
The study was supported by the CDC. One author was an employee of Quest Diagnostics, but no other conflicts of interest were declared.
AGA Resource
The AGA HCV Clinical Service Line provides tools to help you become more efficient, understand quality standards and improve the process of care for patients. Learn more at http://www.gastro.org/patient-care/conditions-diseases/hepatitis-c.
Recognizing hepatitis C infection in pregnant women and neonates is possible, and clinical trials of antiviral therapy may show safety and efficacy in pregnant women and in children. Rather than silence, HCV infection calls out for public health action directed at all aspects of the epidemic, including consideration of screening pregnant women. At the very least, screening of pregnant women for HCV infection risk factors, as well as risk-based testing, requires more emphasis. Another issue in need of attention is the lack of authoritative, consensus-based recommendations for the identification, testing, and case management of newborns of infected mothers.
Much work lies ahead to eradicate HCV, starting with resources for public health surveillance to monitor incidence and prevalence and to fully characterize the infection in the population. Strategies to effectively prevent or cure infection in reproductive-age women and their sexual and needle-sharing partners are critical.
Alfred DeMaria Jr., MD, is from the Massachusetts Department of Public Health. These comments are taken from an accompanying editorial (Ann Intern Med. 2017 May 8. doi: 10.7326/M17-0927). No conflicts of interest were declared.
Recognizing hepatitis C infection in pregnant women and neonates is possible, and clinical trials of antiviral therapy may show safety and efficacy in pregnant women and in children. Rather than silence, HCV infection calls out for public health action directed at all aspects of the epidemic, including consideration of screening pregnant women. At the very least, screening of pregnant women for HCV infection risk factors, as well as risk-based testing, requires more emphasis. Another issue in need of attention is the lack of authoritative, consensus-based recommendations for the identification, testing, and case management of newborns of infected mothers.
Much work lies ahead to eradicate HCV, starting with resources for public health surveillance to monitor incidence and prevalence and to fully characterize the infection in the population. Strategies to effectively prevent or cure infection in reproductive-age women and their sexual and needle-sharing partners are critical.
Alfred DeMaria Jr., MD, is from the Massachusetts Department of Public Health. These comments are taken from an accompanying editorial (Ann Intern Med. 2017 May 8. doi: 10.7326/M17-0927). No conflicts of interest were declared.
Recognizing hepatitis C infection in pregnant women and neonates is possible, and clinical trials of antiviral therapy may show safety and efficacy in pregnant women and in children. Rather than silence, HCV infection calls out for public health action directed at all aspects of the epidemic, including consideration of screening pregnant women. At the very least, screening of pregnant women for HCV infection risk factors, as well as risk-based testing, requires more emphasis. Another issue in need of attention is the lack of authoritative, consensus-based recommendations for the identification, testing, and case management of newborns of infected mothers.
Much work lies ahead to eradicate HCV, starting with resources for public health surveillance to monitor incidence and prevalence and to fully characterize the infection in the population. Strategies to effectively prevent or cure infection in reproductive-age women and their sexual and needle-sharing partners are critical.
Alfred DeMaria Jr., MD, is from the Massachusetts Department of Public Health. These comments are taken from an accompanying editorial (Ann Intern Med. 2017 May 8. doi: 10.7326/M17-0927). No conflicts of interest were declared.
The incidence of hepatitis C virus infection in reproductive-age women has doubled between 2006 and 2014 while the number of acute cases increased more than threefold, according to data published in the Annals of Internal Medicine.
Researchers analyzed data from the National Notifiable Diseases Surveillance System (NNDSS) from 2006 to 2014 and the Quest Diagnostics Health Trends national database from 2011 to 2014, finding 425,322 women with confirmed HCV infection, 40.4% of whom were aged 15-44 years.
Around half of all acute infections were in non-Hispanic white women, and of the 2,069 women with available risk information, 63% acknowledged injection drug use (Ann Intern Med. 2017 May 8. doi: 10.7326/M16-2350).
The analysis also found 1,859 cases of hepatitis C infection in children aged 2-13 years. According to the Quest data, the proportion of children with current hepatitis C infection was 3.2-fold higher in children aged 2-3 years than in those aged 12-13 years.
Commenting on this age difference, Kathleen N. Ly, MPH, from the Centers for Disease Control and Prevention, and her coauthors noted that it may have been the result of decreased testing over time in children already known to have chronic hepatitis C infection, or could be caused by spontaneous remission of infection, which is more common in infants and children than in adults.
The rate of infection among pregnant women tested for hepatitis C virus between 2011 and 2014 was 0.73%, which the authors calculated would mean that overall, 29,000 women with hepatitis C virus infection gave birth during that period across the United States. Based on data from a recent systematic review and meta-analysis, which found a likely mother-to-child transmission rate of 5.8/100 live births, they estimated that 1,700 infants were born with hepatitis C infection during that period.
“In contrast, only about 200 childhood cases per year are reported to the NNDSS, which may suggest a need for wider screening for HCV in pregnant women and their infants, as is recommended for HIV and hepatitis B virus,” the authors wrote. “However, recommendations for screening in pregnant women and clearer testing guidelines for infants born to HCV-infected mothers do not exist at this time.”
The study was supported by the CDC. One author was an employee of Quest Diagnostics, but no other conflicts of interest were declared.
AGA Resource
The AGA HCV Clinical Service Line provides tools to help you become more efficient, understand quality standards and improve the process of care for patients. Learn more at http://www.gastro.org/patient-care/conditions-diseases/hepatitis-c.
The incidence of hepatitis C virus infection in reproductive-age women has doubled between 2006 and 2014 while the number of acute cases increased more than threefold, according to data published in the Annals of Internal Medicine.
Researchers analyzed data from the National Notifiable Diseases Surveillance System (NNDSS) from 2006 to 2014 and the Quest Diagnostics Health Trends national database from 2011 to 2014, finding 425,322 women with confirmed HCV infection, 40.4% of whom were aged 15-44 years.
Around half of all acute infections were in non-Hispanic white women, and of the 2,069 women with available risk information, 63% acknowledged injection drug use (Ann Intern Med. 2017 May 8. doi: 10.7326/M16-2350).
The analysis also found 1,859 cases of hepatitis C infection in children aged 2-13 years. According to the Quest data, the proportion of children with current hepatitis C infection was 3.2-fold higher in children aged 2-3 years than in those aged 12-13 years.
Commenting on this age difference, Kathleen N. Ly, MPH, from the Centers for Disease Control and Prevention, and her coauthors noted that it may have been the result of decreased testing over time in children already known to have chronic hepatitis C infection, or could be caused by spontaneous remission of infection, which is more common in infants and children than in adults.
The rate of infection among pregnant women tested for hepatitis C virus between 2011 and 2014 was 0.73%, which the authors calculated would mean that overall, 29,000 women with hepatitis C virus infection gave birth during that period across the United States. Based on data from a recent systematic review and meta-analysis, which found a likely mother-to-child transmission rate of 5.8/100 live births, they estimated that 1,700 infants were born with hepatitis C infection during that period.
“In contrast, only about 200 childhood cases per year are reported to the NNDSS, which may suggest a need for wider screening for HCV in pregnant women and their infants, as is recommended for HIV and hepatitis B virus,” the authors wrote. “However, recommendations for screening in pregnant women and clearer testing guidelines for infants born to HCV-infected mothers do not exist at this time.”
The study was supported by the CDC. One author was an employee of Quest Diagnostics, but no other conflicts of interest were declared.
AGA Resource
The AGA HCV Clinical Service Line provides tools to help you become more efficient, understand quality standards and improve the process of care for patients. Learn more at http://www.gastro.org/patient-care/conditions-diseases/hepatitis-c.
FROM ANNALS OF INTERNAL MEDICINE
Bariatric patients can conquer obesity, but few achieve BMI < 25
Around one-quarter of obese individuals who undergo Roux-en-Y gastric bypass had sustained, long-term remission of obesity, but far fewer achieved body mass index of under 25 kg/m2 or maintained it over 5 years, new research suggests.
Researchers reported on the outcomes of a retrospective cohort study of 219 patients who underwent Roux-en-Y gastric bypass surgery at a single center between 2008 and 2010 and were followed for up to 7 years after the procedure.
Only 16.9% of female patients achieved a BMI of under 25 kg/m2 – during the study period, and only 2.7% reached this BMI by year 2 and sustained it at least to year 5 of follow-up.
Two males in the study achieved BMI of under 25 during follow-up. One was recorded as having maintained this weight at year 1 and the other at year 4, but no further measurements were available for either.
“Given the low number of patients achieving BMI of less than 25 kg/m2, we also wanted to focus on another important clinical goal of obesity remission (BMI less than 30),” wrote Corey J. Lager, MD, of the University of Michigan, Brehm Center for Diabetes, Ann Arbor, and his coauthors. “Taking into account that the mean BMI prior to surgery in our cohort was 47.1 kg/m2, this target is associated with significant estimated health benefits and likely brings a mortality benefit for patients undergoing gastric bypass.”
The authors said that a conservative estimate of the probability of achieving and sustaining BMI 25 or less after Roux-en-Y gastric bypass was just 2.3%. However, they offered a more liberal estimate – based on the number of patients who were at BMI 25 or under at the last available data point – of 6.8%.
Achieving weight loss to a BMI less than 30 was significantly influenced by age. The group who achieved this weight were on average 3 years younger at baseline than those who did not.
Similarly, initial BMI played a role in outcomes. The women who achieved a BMI below 30 had an initial mean BMI of 43.5, compared with 50.4 in the women who did not achieve this weight (P less than .0001). In males, the mean baseline BMI in those who got their weight below 30 was 44.6, compared with 48.1 in those who did not (P = .18).
Roux-en-Y gastric bypass was also associated with significant and sustained decreases in both systolic and diastolic blood pressure that was similar for both sexes. The maximum mean decrease of 14 ± 7 mm Hg was achieved at 1 year after surgery, and, at 5 years, the mean decrease was 11 ± 3 mm Hg.
The authors commented that, despite “excellent” weight loss being achieved by a majority of patients, the findings show the challenge of weight loss and maintenance in patients with a very high BMI. However, they also pointed to the encouragingly low rates of significant weight regain and the fact that fewer than 1% of patients returned to a weight greater than their preoperative weight. Higher preoperative BMI was correlated with greater weight loss but also negatively correlated with achieving BMI under 30.
The authors concluded with two takeaway messages. First, realistic goals should be set for patients undergoing gastric bypass surgery, with an emphasis on remission of obesity and with a reduced expectation of achievement of BMI under 25 over the long run. In addition, because the higher the initial BMI, the less likely that weight loss will not be maintained, “we should also carefully examine the option of pursuing surgery at lower BMI cutoffs, at which point patients have a greater likelihood of obesity remission.”
The study was supported by the University of Michigan Health System, the National Institutes of Health, and the Nutrition Obesity Research Centers. One author declared grant support and advisory positions with pharmaceutical companies and intellectual property unrelated to the study. Another author is an investigator on a sponsored clinical study. No other conflicts of interest were declared.
Around one-quarter of obese individuals who undergo Roux-en-Y gastric bypass had sustained, long-term remission of obesity, but far fewer achieved body mass index of under 25 kg/m2 or maintained it over 5 years, new research suggests.
Researchers reported on the outcomes of a retrospective cohort study of 219 patients who underwent Roux-en-Y gastric bypass surgery at a single center between 2008 and 2010 and were followed for up to 7 years after the procedure.
Only 16.9% of female patients achieved a BMI of under 25 kg/m2 – during the study period, and only 2.7% reached this BMI by year 2 and sustained it at least to year 5 of follow-up.
Two males in the study achieved BMI of under 25 during follow-up. One was recorded as having maintained this weight at year 1 and the other at year 4, but no further measurements were available for either.
“Given the low number of patients achieving BMI of less than 25 kg/m2, we also wanted to focus on another important clinical goal of obesity remission (BMI less than 30),” wrote Corey J. Lager, MD, of the University of Michigan, Brehm Center for Diabetes, Ann Arbor, and his coauthors. “Taking into account that the mean BMI prior to surgery in our cohort was 47.1 kg/m2, this target is associated with significant estimated health benefits and likely brings a mortality benefit for patients undergoing gastric bypass.”
The authors said that a conservative estimate of the probability of achieving and sustaining BMI 25 or less after Roux-en-Y gastric bypass was just 2.3%. However, they offered a more liberal estimate – based on the number of patients who were at BMI 25 or under at the last available data point – of 6.8%.
Achieving weight loss to a BMI less than 30 was significantly influenced by age. The group who achieved this weight were on average 3 years younger at baseline than those who did not.
Similarly, initial BMI played a role in outcomes. The women who achieved a BMI below 30 had an initial mean BMI of 43.5, compared with 50.4 in the women who did not achieve this weight (P less than .0001). In males, the mean baseline BMI in those who got their weight below 30 was 44.6, compared with 48.1 in those who did not (P = .18).
Roux-en-Y gastric bypass was also associated with significant and sustained decreases in both systolic and diastolic blood pressure that was similar for both sexes. The maximum mean decrease of 14 ± 7 mm Hg was achieved at 1 year after surgery, and, at 5 years, the mean decrease was 11 ± 3 mm Hg.
The authors commented that, despite “excellent” weight loss being achieved by a majority of patients, the findings show the challenge of weight loss and maintenance in patients with a very high BMI. However, they also pointed to the encouragingly low rates of significant weight regain and the fact that fewer than 1% of patients returned to a weight greater than their preoperative weight. Higher preoperative BMI was correlated with greater weight loss but also negatively correlated with achieving BMI under 30.
The authors concluded with two takeaway messages. First, realistic goals should be set for patients undergoing gastric bypass surgery, with an emphasis on remission of obesity and with a reduced expectation of achievement of BMI under 25 over the long run. In addition, because the higher the initial BMI, the less likely that weight loss will not be maintained, “we should also carefully examine the option of pursuing surgery at lower BMI cutoffs, at which point patients have a greater likelihood of obesity remission.”
The study was supported by the University of Michigan Health System, the National Institutes of Health, and the Nutrition Obesity Research Centers. One author declared grant support and advisory positions with pharmaceutical companies and intellectual property unrelated to the study. Another author is an investigator on a sponsored clinical study. No other conflicts of interest were declared.
Around one-quarter of obese individuals who undergo Roux-en-Y gastric bypass had sustained, long-term remission of obesity, but far fewer achieved body mass index of under 25 kg/m2 or maintained it over 5 years, new research suggests.
Researchers reported on the outcomes of a retrospective cohort study of 219 patients who underwent Roux-en-Y gastric bypass surgery at a single center between 2008 and 2010 and were followed for up to 7 years after the procedure.
Only 16.9% of female patients achieved a BMI of under 25 kg/m2 – during the study period, and only 2.7% reached this BMI by year 2 and sustained it at least to year 5 of follow-up.
Two males in the study achieved BMI of under 25 during follow-up. One was recorded as having maintained this weight at year 1 and the other at year 4, but no further measurements were available for either.
“Given the low number of patients achieving BMI of less than 25 kg/m2, we also wanted to focus on another important clinical goal of obesity remission (BMI less than 30),” wrote Corey J. Lager, MD, of the University of Michigan, Brehm Center for Diabetes, Ann Arbor, and his coauthors. “Taking into account that the mean BMI prior to surgery in our cohort was 47.1 kg/m2, this target is associated with significant estimated health benefits and likely brings a mortality benefit for patients undergoing gastric bypass.”
The authors said that a conservative estimate of the probability of achieving and sustaining BMI 25 or less after Roux-en-Y gastric bypass was just 2.3%. However, they offered a more liberal estimate – based on the number of patients who were at BMI 25 or under at the last available data point – of 6.8%.
Achieving weight loss to a BMI less than 30 was significantly influenced by age. The group who achieved this weight were on average 3 years younger at baseline than those who did not.
Similarly, initial BMI played a role in outcomes. The women who achieved a BMI below 30 had an initial mean BMI of 43.5, compared with 50.4 in the women who did not achieve this weight (P less than .0001). In males, the mean baseline BMI in those who got their weight below 30 was 44.6, compared with 48.1 in those who did not (P = .18).
Roux-en-Y gastric bypass was also associated with significant and sustained decreases in both systolic and diastolic blood pressure that was similar for both sexes. The maximum mean decrease of 14 ± 7 mm Hg was achieved at 1 year after surgery, and, at 5 years, the mean decrease was 11 ± 3 mm Hg.
The authors commented that, despite “excellent” weight loss being achieved by a majority of patients, the findings show the challenge of weight loss and maintenance in patients with a very high BMI. However, they also pointed to the encouragingly low rates of significant weight regain and the fact that fewer than 1% of patients returned to a weight greater than their preoperative weight. Higher preoperative BMI was correlated with greater weight loss but also negatively correlated with achieving BMI under 30.
The authors concluded with two takeaway messages. First, realistic goals should be set for patients undergoing gastric bypass surgery, with an emphasis on remission of obesity and with a reduced expectation of achievement of BMI under 25 over the long run. In addition, because the higher the initial BMI, the less likely that weight loss will not be maintained, “we should also carefully examine the option of pursuing surgery at lower BMI cutoffs, at which point patients have a greater likelihood of obesity remission.”
The study was supported by the University of Michigan Health System, the National Institutes of Health, and the Nutrition Obesity Research Centers. One author declared grant support and advisory positions with pharmaceutical companies and intellectual property unrelated to the study. Another author is an investigator on a sponsored clinical study. No other conflicts of interest were declared.
FROM OBESITY SURGERY
Key clinical point: Roux-en-Y gastric bypass is associated with sustained, long-term remission of obesity in around one-quarter of patients.
Major finding: Nearly one-quarter of patients who underwent Roux-en-Y gastric bypass achieved a BMI below 30 kg/m2 that was sustained at their last follow-up, but healthy weight was sustained at 5 years’ follow-up in far fewer patients.
Data source: Retrospective cohort study of 219 patients.
Disclosures: The study was supported by the University of Michigan Health System, the National Institutes of Health, and the Nutrition Obesity Research Centers. One author declared grant support and advisory positions with pharmaceutical companies and intellectual property unrelated to the study. Another author is an investigator on a sponsored clinical study. No other conflicts of interest were declared.
Physical treatment plus antifungal best for chromoblastomycosis, review finds
SYDNEY – Chromoblastomycosis is best managed with a combination of surgery or cryotherapy, with an antifungal, based on a systematic review of 37 studies.
The results of these studies, none of which was randomized or controlled, highlighted challenges in the management of chromoblastomycosis, such as low cure rates and high relapse rates, particularly with chronic and extensive disease. “This is due to the indolent nature of the disease, which leads to a delayed diagnosis, so then the patient develops lymphedema and fibrosis, and the drug isn’t able to penetrate the sites of the lesion,” said Antonia Laino, MD, of the dermatology research center, University of Queensland (Australia).
Noncompliance was also found to be an issue because of side effects and the cost of long-term treatment.
Surgical and pharmacologic options were among the treatments used. Based on the results, Dr. Laino said surgery was recommended as the best treatment for small lesions, and could achieve cure rates of 100% for very small lesions. Cryotherapy was also used to treat chromoblastomycosis lesions, with variable success rates that were dependent on the size of the lesion and the frequency of freezing cycles. However, she suggested that larger lesions should be treated in serial sections, and warned of the risk of retractile scars with treatment over joints.
The most commonly reported drug therapies for chromoblastomycosis were itraconazole and terbinafine. With itraconazole, cure rates ranged from 15% to 80% over an average of 8.5 months of treatment. Pulsed itraconazole therapy, involving 1 week on and 3 weeks off treatment, achieved cure rates of 67%-100% across the studies. With terbinafine treatment, cure rates ranged from 40% to 75% over an average of 9 months of treatment.
In an interview, Dr. Laino said randomized controlled trials were needed to establish best practices for the treatment of chromoblastomycosis.
“I would also say that an antifungal plus a physical method [surgery or cryotherapy] is the way to go,” she said in the interview. As for pharmacotherapy, currently, “there’s the most support for use of itraconazole,” she said, but other antifungals that are being developed will also probably become good options, as studies of those become available. Refractory cases and very severe disease could be treated with a combination of itraconazole and terbinafine.
Chromoblastomycosis is a subcutaneous mycotic infection that is endemic worldwide, but is more common in tropical regions. It usually develops after injury to the skin, which allows entry of any one of several fungal pathogens including Fonsecaea pedrosoi, Phialophora verrucosa, and Cladophialophora carrionii. “Chromoblastomycosis can present with many different lesions, but the early lesions usually resemble a dermatophyte infection or begin as a papule,” Dr. Laino said. “Over time, the lesions will progress into the nodular, tumorous verrucous, cicatricial, and plaque types, and in advanced cases … you’ll see a lot of different lesions in one patient.”
No conflicts of interest were declared.
SYDNEY – Chromoblastomycosis is best managed with a combination of surgery or cryotherapy, with an antifungal, based on a systematic review of 37 studies.
The results of these studies, none of which was randomized or controlled, highlighted challenges in the management of chromoblastomycosis, such as low cure rates and high relapse rates, particularly with chronic and extensive disease. “This is due to the indolent nature of the disease, which leads to a delayed diagnosis, so then the patient develops lymphedema and fibrosis, and the drug isn’t able to penetrate the sites of the lesion,” said Antonia Laino, MD, of the dermatology research center, University of Queensland (Australia).
Noncompliance was also found to be an issue because of side effects and the cost of long-term treatment.
Surgical and pharmacologic options were among the treatments used. Based on the results, Dr. Laino said surgery was recommended as the best treatment for small lesions, and could achieve cure rates of 100% for very small lesions. Cryotherapy was also used to treat chromoblastomycosis lesions, with variable success rates that were dependent on the size of the lesion and the frequency of freezing cycles. However, she suggested that larger lesions should be treated in serial sections, and warned of the risk of retractile scars with treatment over joints.
The most commonly reported drug therapies for chromoblastomycosis were itraconazole and terbinafine. With itraconazole, cure rates ranged from 15% to 80% over an average of 8.5 months of treatment. Pulsed itraconazole therapy, involving 1 week on and 3 weeks off treatment, achieved cure rates of 67%-100% across the studies. With terbinafine treatment, cure rates ranged from 40% to 75% over an average of 9 months of treatment.
In an interview, Dr. Laino said randomized controlled trials were needed to establish best practices for the treatment of chromoblastomycosis.
“I would also say that an antifungal plus a physical method [surgery or cryotherapy] is the way to go,” she said in the interview. As for pharmacotherapy, currently, “there’s the most support for use of itraconazole,” she said, but other antifungals that are being developed will also probably become good options, as studies of those become available. Refractory cases and very severe disease could be treated with a combination of itraconazole and terbinafine.
Chromoblastomycosis is a subcutaneous mycotic infection that is endemic worldwide, but is more common in tropical regions. It usually develops after injury to the skin, which allows entry of any one of several fungal pathogens including Fonsecaea pedrosoi, Phialophora verrucosa, and Cladophialophora carrionii. “Chromoblastomycosis can present with many different lesions, but the early lesions usually resemble a dermatophyte infection or begin as a papule,” Dr. Laino said. “Over time, the lesions will progress into the nodular, tumorous verrucous, cicatricial, and plaque types, and in advanced cases … you’ll see a lot of different lesions in one patient.”
No conflicts of interest were declared.
SYDNEY – Chromoblastomycosis is best managed with a combination of surgery or cryotherapy, with an antifungal, based on a systematic review of 37 studies.
The results of these studies, none of which was randomized or controlled, highlighted challenges in the management of chromoblastomycosis, such as low cure rates and high relapse rates, particularly with chronic and extensive disease. “This is due to the indolent nature of the disease, which leads to a delayed diagnosis, so then the patient develops lymphedema and fibrosis, and the drug isn’t able to penetrate the sites of the lesion,” said Antonia Laino, MD, of the dermatology research center, University of Queensland (Australia).
Noncompliance was also found to be an issue because of side effects and the cost of long-term treatment.
Surgical and pharmacologic options were among the treatments used. Based on the results, Dr. Laino said surgery was recommended as the best treatment for small lesions, and could achieve cure rates of 100% for very small lesions. Cryotherapy was also used to treat chromoblastomycosis lesions, with variable success rates that were dependent on the size of the lesion and the frequency of freezing cycles. However, she suggested that larger lesions should be treated in serial sections, and warned of the risk of retractile scars with treatment over joints.
The most commonly reported drug therapies for chromoblastomycosis were itraconazole and terbinafine. With itraconazole, cure rates ranged from 15% to 80% over an average of 8.5 months of treatment. Pulsed itraconazole therapy, involving 1 week on and 3 weeks off treatment, achieved cure rates of 67%-100% across the studies. With terbinafine treatment, cure rates ranged from 40% to 75% over an average of 9 months of treatment.
In an interview, Dr. Laino said randomized controlled trials were needed to establish best practices for the treatment of chromoblastomycosis.
“I would also say that an antifungal plus a physical method [surgery or cryotherapy] is the way to go,” she said in the interview. As for pharmacotherapy, currently, “there’s the most support for use of itraconazole,” she said, but other antifungals that are being developed will also probably become good options, as studies of those become available. Refractory cases and very severe disease could be treated with a combination of itraconazole and terbinafine.
Chromoblastomycosis is a subcutaneous mycotic infection that is endemic worldwide, but is more common in tropical regions. It usually develops after injury to the skin, which allows entry of any one of several fungal pathogens including Fonsecaea pedrosoi, Phialophora verrucosa, and Cladophialophora carrionii. “Chromoblastomycosis can present with many different lesions, but the early lesions usually resemble a dermatophyte infection or begin as a papule,” Dr. Laino said. “Over time, the lesions will progress into the nodular, tumorous verrucous, cicatricial, and plaque types, and in advanced cases … you’ll see a lot of different lesions in one patient.”
No conflicts of interest were declared.
AT ACDASM 2017
Key clinical point:
Major finding: Surgery in combination with an antifungal was the most effective management approach for chromoblastomycosis.
Data source: A systematic review of 37 studies of patients with chromoblastomycosis.
Disclosures: No conflicts of interest were declared.
Treatment challenges for lichen planopilaris
SYDNEY – Responses to treatments for lichen planopilaris varied widely, and decreased with second- and third-line therapies, in a retrospective study, Karolina Kerkemeyer, MD, said at the annual meeting of the Australasian College of Dermatologists.
An analysis of computerized medical records for 32 patients who had been treated for lichen planopilaris at a tertiary referral hair center in Australia was conducted from 2012 to 2016 by Dr. Kerkemeyer of the University of Notre Dame Australia, Werribee, and Jack Green, MD, of the Skin and Cancer Foundation and St. Vincent’s Hospital in Melbourne. The study excluded patients with a dual diagnosis, or those followed for less than 12 months.
The most common treatment was topical steroids, used to treat 31 patients, followed by tetracyclines – minocycline or doxycycline – used to treat 21 patients, and hydroxychloroquine, used to treat 18 patients. Some patients were also treated with steroid-sparing immunosuppressants, including methotrexate, mycophenolate, and cyclosporine. Fourteen patients were also treated with intralesional steroids, and seven were treated with topical tacrolimus.
The researchers used a graded four-point scale to assess patients’ response to treatment, which corresponded to remission, partial improvement, no change, and worsening of disease, based on patients’ clinical signs, symptoms, and extent of alopecia.
Only a small proportion – about 15% – of patients achieved remission, which was seen with topical steroids, hydroxychloroquine, and doxycycline. About one-third of patients treated with doxycycline actually showed a worsening of symptoms.
The greatest proportion (75%) of patients with partial remission was among those treated with systemic acitretin, although the numbers were low (three of four patients who received this therapy).
In addition, one of the seven patients treated with minocycline achieved partial remission during this therapy, one showed a worsening of the condition, and the remaining five were unchanged. Among those treated with an immunosuppressant, the 3 patients treated with mycophenolate had no change in the condition; 4 of the 10 patients treated with methotrexate achieved partial remission, 4 were unchanged, and 2 experienced a worsening of the condition. One of the three patients treated with cyclosporine achieved partial remission while the other two remained unchanged. With topical tacrolimus, two patients achieved partial remission, two showed a worsening of the condition, and the remaining three were unchanged.
The response rates to treatment significantly decreased with subsequent therapies: 18 of the 32 patients responded to first-line treatments, compared with 7 of 19 who received second-line treatment and only 1 of 9 patients who received third-line treatment. “Many patients were not responsive to therapy, highlighting the difficulty of treating this scarring alopecia,” Dr. Kerkemeyer said.
In an interview, she said that topical or intralesional steroids seemed to be the best first-line option because they are associated with fewer side effects than other options. “They were easier to start off in patients first,” and for those who do not respond, switching to another treatment, such as topical tacrolimus, if they wanted a topical option, or an oral treatment, such as an immunosuppressant like methotrexate, she noted.
No conflicts of interest were declared.
SYDNEY – Responses to treatments for lichen planopilaris varied widely, and decreased with second- and third-line therapies, in a retrospective study, Karolina Kerkemeyer, MD, said at the annual meeting of the Australasian College of Dermatologists.
An analysis of computerized medical records for 32 patients who had been treated for lichen planopilaris at a tertiary referral hair center in Australia was conducted from 2012 to 2016 by Dr. Kerkemeyer of the University of Notre Dame Australia, Werribee, and Jack Green, MD, of the Skin and Cancer Foundation and St. Vincent’s Hospital in Melbourne. The study excluded patients with a dual diagnosis, or those followed for less than 12 months.
The most common treatment was topical steroids, used to treat 31 patients, followed by tetracyclines – minocycline or doxycycline – used to treat 21 patients, and hydroxychloroquine, used to treat 18 patients. Some patients were also treated with steroid-sparing immunosuppressants, including methotrexate, mycophenolate, and cyclosporine. Fourteen patients were also treated with intralesional steroids, and seven were treated with topical tacrolimus.
The researchers used a graded four-point scale to assess patients’ response to treatment, which corresponded to remission, partial improvement, no change, and worsening of disease, based on patients’ clinical signs, symptoms, and extent of alopecia.
Only a small proportion – about 15% – of patients achieved remission, which was seen with topical steroids, hydroxychloroquine, and doxycycline. About one-third of patients treated with doxycycline actually showed a worsening of symptoms.
The greatest proportion (75%) of patients with partial remission was among those treated with systemic acitretin, although the numbers were low (three of four patients who received this therapy).
In addition, one of the seven patients treated with minocycline achieved partial remission during this therapy, one showed a worsening of the condition, and the remaining five were unchanged. Among those treated with an immunosuppressant, the 3 patients treated with mycophenolate had no change in the condition; 4 of the 10 patients treated with methotrexate achieved partial remission, 4 were unchanged, and 2 experienced a worsening of the condition. One of the three patients treated with cyclosporine achieved partial remission while the other two remained unchanged. With topical tacrolimus, two patients achieved partial remission, two showed a worsening of the condition, and the remaining three were unchanged.
The response rates to treatment significantly decreased with subsequent therapies: 18 of the 32 patients responded to first-line treatments, compared with 7 of 19 who received second-line treatment and only 1 of 9 patients who received third-line treatment. “Many patients were not responsive to therapy, highlighting the difficulty of treating this scarring alopecia,” Dr. Kerkemeyer said.
In an interview, she said that topical or intralesional steroids seemed to be the best first-line option because they are associated with fewer side effects than other options. “They were easier to start off in patients first,” and for those who do not respond, switching to another treatment, such as topical tacrolimus, if they wanted a topical option, or an oral treatment, such as an immunosuppressant like methotrexate, she noted.
No conflicts of interest were declared.
SYDNEY – Responses to treatments for lichen planopilaris varied widely, and decreased with second- and third-line therapies, in a retrospective study, Karolina Kerkemeyer, MD, said at the annual meeting of the Australasian College of Dermatologists.
An analysis of computerized medical records for 32 patients who had been treated for lichen planopilaris at a tertiary referral hair center in Australia was conducted from 2012 to 2016 by Dr. Kerkemeyer of the University of Notre Dame Australia, Werribee, and Jack Green, MD, of the Skin and Cancer Foundation and St. Vincent’s Hospital in Melbourne. The study excluded patients with a dual diagnosis, or those followed for less than 12 months.
The most common treatment was topical steroids, used to treat 31 patients, followed by tetracyclines – minocycline or doxycycline – used to treat 21 patients, and hydroxychloroquine, used to treat 18 patients. Some patients were also treated with steroid-sparing immunosuppressants, including methotrexate, mycophenolate, and cyclosporine. Fourteen patients were also treated with intralesional steroids, and seven were treated with topical tacrolimus.
The researchers used a graded four-point scale to assess patients’ response to treatment, which corresponded to remission, partial improvement, no change, and worsening of disease, based on patients’ clinical signs, symptoms, and extent of alopecia.
Only a small proportion – about 15% – of patients achieved remission, which was seen with topical steroids, hydroxychloroquine, and doxycycline. About one-third of patients treated with doxycycline actually showed a worsening of symptoms.
The greatest proportion (75%) of patients with partial remission was among those treated with systemic acitretin, although the numbers were low (three of four patients who received this therapy).
In addition, one of the seven patients treated with minocycline achieved partial remission during this therapy, one showed a worsening of the condition, and the remaining five were unchanged. Among those treated with an immunosuppressant, the 3 patients treated with mycophenolate had no change in the condition; 4 of the 10 patients treated with methotrexate achieved partial remission, 4 were unchanged, and 2 experienced a worsening of the condition. One of the three patients treated with cyclosporine achieved partial remission while the other two remained unchanged. With topical tacrolimus, two patients achieved partial remission, two showed a worsening of the condition, and the remaining three were unchanged.
The response rates to treatment significantly decreased with subsequent therapies: 18 of the 32 patients responded to first-line treatments, compared with 7 of 19 who received second-line treatment and only 1 of 9 patients who received third-line treatment. “Many patients were not responsive to therapy, highlighting the difficulty of treating this scarring alopecia,” Dr. Kerkemeyer said.
In an interview, she said that topical or intralesional steroids seemed to be the best first-line option because they are associated with fewer side effects than other options. “They were easier to start off in patients first,” and for those who do not respond, switching to another treatment, such as topical tacrolimus, if they wanted a topical option, or an oral treatment, such as an immunosuppressant like methotrexate, she noted.
No conflicts of interest were declared.
Key clinical point: Lichen planopilaris is a scarring alopecia that is particularly difficult to treat, and a significant number of patients may have refractory disease.
Major finding:
Data source: A retrospective analysis of 32 patients with lichen planopilaris.
Disclosures: No conflicts of interest were declared.
Skin cancer risk similar for liver and kidney transplant recipients
SYDNEY – The risk of developing nonmelanoma skin cancer among liver transplant recipients is similar to that among kidney transplant recipients, but the former tend to have more skin cancer risk factors at baseline, according to a longitudinal cohort study reported at the annual meeting of the Australasian College of Dermatologists.
Liver transplant recipients have been thought to be at a lower risk of developing nonmelanoma skin cancers than are other solid organ transplant recipients, said Ludi Ge, MD, of the department of dermatology at the University of Sydney and Royal Prince Alfred Hospital, Sydney. However, data from a longitudinal cohort study of 230 kidney or liver transplant patients suggest the risk of nonmelanoma skin cancer is similar – if not greater – among liver transplant recipients, compared with kidney transplant recipients.
Over a 5-year period, 47% of liver transplant recipients developed at least one nonmelanoma skin cancer, compared with 33% of renal transplant recipients, representing a 78% greater risk among liver transplant recipients. However, Dr. Ge said the confidence intervals were wide, and the difference lost statistical significance in the multivariate analysis.
The researchers also noted that the liver transplant recipients in the study tended to be older at baseline, with a history of more sun exposure and more previous skin cancers, and were more likely to have a high risk skin type that sunburns easily.
In an interview, Dr. Ge said the findings had implications for the screening and follow-up of liver transplant recipients.
“Previously, we always thought that liver transplant recipients were at lower risk, and, possibly, they’re not screened as much so not followed up as much,” she said. “I think they really should be thought ... as high risk as renal transplant patients and the heart and lung transplant patients.”
The study showed that, while the renal transplant patients developed fewer skin cancers, they developed 1.9 lesions per year on average, compared with liver transplant patients, who developed 1.4 lesions per year.
The majority of skin cancers in both groups were squamous cell carcinomas and basal cell carcinomas, with a small number of keratoacanthomas. There was a similar ratio of squamous cell carcinomas to basal cell carcinomas between the two groups of transplant recipients – 1.7:1 in renal transplant recipients and 1.6:1 in liver recipients – which differed from the previously reported ratios of about 3:1, Dr. Ge said at the meeting.
She noted that this may have been because not every squamous cell carcinoma in situ was biopsied because of the sheer number of tumors, so many were treated empirically and, therefore, not entered into the clinic database.
Dr. Ge also pointed out that the evidence for the 3:1 ratio was around 10 years old.
“I think there’s been quite a change in the immunosuppressants that are used by transplant physicians, so, more and more, we’re seeing the use of sirolimus and everolimus, which are antiangiogenic,” she said.
Dr. Ge also strongly recommended that dermatology clinics specifically manage organ transplant recipients and commented that this could revolutionize the management of these patients, who tend to get lost to follow-up in standard dermatology clinics. “They’re very difficult to look after, they develop innumerable skin cancers that can result in death, and you need to intervene quite early,” she said in the interview.
No conflicts of interest were declared.
SYDNEY – The risk of developing nonmelanoma skin cancer among liver transplant recipients is similar to that among kidney transplant recipients, but the former tend to have more skin cancer risk factors at baseline, according to a longitudinal cohort study reported at the annual meeting of the Australasian College of Dermatologists.
Liver transplant recipients have been thought to be at a lower risk of developing nonmelanoma skin cancers than are other solid organ transplant recipients, said Ludi Ge, MD, of the department of dermatology at the University of Sydney and Royal Prince Alfred Hospital, Sydney. However, data from a longitudinal cohort study of 230 kidney or liver transplant patients suggest the risk of nonmelanoma skin cancer is similar – if not greater – among liver transplant recipients, compared with kidney transplant recipients.
Over a 5-year period, 47% of liver transplant recipients developed at least one nonmelanoma skin cancer, compared with 33% of renal transplant recipients, representing a 78% greater risk among liver transplant recipients. However, Dr. Ge said the confidence intervals were wide, and the difference lost statistical significance in the multivariate analysis.
The researchers also noted that the liver transplant recipients in the study tended to be older at baseline, with a history of more sun exposure and more previous skin cancers, and were more likely to have a high risk skin type that sunburns easily.
In an interview, Dr. Ge said the findings had implications for the screening and follow-up of liver transplant recipients.
“Previously, we always thought that liver transplant recipients were at lower risk, and, possibly, they’re not screened as much so not followed up as much,” she said. “I think they really should be thought ... as high risk as renal transplant patients and the heart and lung transplant patients.”
The study showed that, while the renal transplant patients developed fewer skin cancers, they developed 1.9 lesions per year on average, compared with liver transplant patients, who developed 1.4 lesions per year.
The majority of skin cancers in both groups were squamous cell carcinomas and basal cell carcinomas, with a small number of keratoacanthomas. There was a similar ratio of squamous cell carcinomas to basal cell carcinomas between the two groups of transplant recipients – 1.7:1 in renal transplant recipients and 1.6:1 in liver recipients – which differed from the previously reported ratios of about 3:1, Dr. Ge said at the meeting.
She noted that this may have been because not every squamous cell carcinoma in situ was biopsied because of the sheer number of tumors, so many were treated empirically and, therefore, not entered into the clinic database.
Dr. Ge also pointed out that the evidence for the 3:1 ratio was around 10 years old.
“I think there’s been quite a change in the immunosuppressants that are used by transplant physicians, so, more and more, we’re seeing the use of sirolimus and everolimus, which are antiangiogenic,” she said.
Dr. Ge also strongly recommended that dermatology clinics specifically manage organ transplant recipients and commented that this could revolutionize the management of these patients, who tend to get lost to follow-up in standard dermatology clinics. “They’re very difficult to look after, they develop innumerable skin cancers that can result in death, and you need to intervene quite early,” she said in the interview.
No conflicts of interest were declared.
SYDNEY – The risk of developing nonmelanoma skin cancer among liver transplant recipients is similar to that among kidney transplant recipients, but the former tend to have more skin cancer risk factors at baseline, according to a longitudinal cohort study reported at the annual meeting of the Australasian College of Dermatologists.
Liver transplant recipients have been thought to be at a lower risk of developing nonmelanoma skin cancers than are other solid organ transplant recipients, said Ludi Ge, MD, of the department of dermatology at the University of Sydney and Royal Prince Alfred Hospital, Sydney. However, data from a longitudinal cohort study of 230 kidney or liver transplant patients suggest the risk of nonmelanoma skin cancer is similar – if not greater – among liver transplant recipients, compared with kidney transplant recipients.
Over a 5-year period, 47% of liver transplant recipients developed at least one nonmelanoma skin cancer, compared with 33% of renal transplant recipients, representing a 78% greater risk among liver transplant recipients. However, Dr. Ge said the confidence intervals were wide, and the difference lost statistical significance in the multivariate analysis.
The researchers also noted that the liver transplant recipients in the study tended to be older at baseline, with a history of more sun exposure and more previous skin cancers, and were more likely to have a high risk skin type that sunburns easily.
In an interview, Dr. Ge said the findings had implications for the screening and follow-up of liver transplant recipients.
“Previously, we always thought that liver transplant recipients were at lower risk, and, possibly, they’re not screened as much so not followed up as much,” she said. “I think they really should be thought ... as high risk as renal transplant patients and the heart and lung transplant patients.”
The study showed that, while the renal transplant patients developed fewer skin cancers, they developed 1.9 lesions per year on average, compared with liver transplant patients, who developed 1.4 lesions per year.
The majority of skin cancers in both groups were squamous cell carcinomas and basal cell carcinomas, with a small number of keratoacanthomas. There was a similar ratio of squamous cell carcinomas to basal cell carcinomas between the two groups of transplant recipients – 1.7:1 in renal transplant recipients and 1.6:1 in liver recipients – which differed from the previously reported ratios of about 3:1, Dr. Ge said at the meeting.
She noted that this may have been because not every squamous cell carcinoma in situ was biopsied because of the sheer number of tumors, so many were treated empirically and, therefore, not entered into the clinic database.
Dr. Ge also pointed out that the evidence for the 3:1 ratio was around 10 years old.
“I think there’s been quite a change in the immunosuppressants that are used by transplant physicians, so, more and more, we’re seeing the use of sirolimus and everolimus, which are antiangiogenic,” she said.
Dr. Ge also strongly recommended that dermatology clinics specifically manage organ transplant recipients and commented that this could revolutionize the management of these patients, who tend to get lost to follow-up in standard dermatology clinics. “They’re very difficult to look after, they develop innumerable skin cancers that can result in death, and you need to intervene quite early,” she said in the interview.
No conflicts of interest were declared.
AT ACDASM 2017
Key clinical point: Liver transplant recipients should be screened and followed for the development of nonmelanoma skin cancers as closely as are kidney transplant recipients.
Major finding: Over 5 years, 47% of liver transplant recipients developed at least one nonmelanoma skin cancer, compared with 33% of renal transplant recipients, a difference that was not statistically significant after a multivariate analysis was done.
Data source: A longitudinal cohort study of 230 kidney or liver transplant recipients attending a dermatology clinic affiliated with an organ transplant unit.
Disclosures: No conflicts of interest were disclosed.