User login
Sleep: The new frontier in cardiovascular prevention
MUNICH – Getting less than 6 hours of sleep nightly on a regular basis or waking up multiple times was independently associated with increased risk of subclinical atherosclerosis in the Spanish PESA study, Fernando Dominguez, MD, reported at the annual congress of the European Society of Cardiology.
Moreover, a graded response was evident in PESA (Progression of Early Subclinical Atherosclerosis): The more times an individual typically awoke per night, the greater the number of atherosclerotic carotid or femoral artery territories documented on three-dimensional vascular ultrasound, added Dr. Dominguez of the Spanish National Center for Cardiovascular Research in Madrid.
the cardiologist said.
The cross-sectional PESA study, whose principal investigator was Valentin Fuster, MD, PhD, included 3,974 middle-aged Madrid bank employees free of known heart disease or history of stroke who wore a waistband activity monitor for a week to record sleep quantity and quality. They also underwent three-dimensional vascular ultrasound and measurement of coronary artery calcium.
PESA was one of several large studies presented at the meeting that focused on deviations from normal sleep as a marker for increased risk of cardiovascular disease and/or mortality. Of note, however, PESA was the only one to use activity monitoring technology to track sleep.
“It was essential to use objectively measured sleep variables, because they showed huge disparity with patients’ self-reports on sleep questionnaires,” Dr. Dominguez explained.
Indeed, while 10.7% of PESA participants self-reported sleeping less than 6 hours per night on the Sleep Habits Questionnaire, actigraphy showed the true rate was 27.1%.
Based on actigraphic findings, subjects were divided into tertiles based upon average hours of sleep per night, ranging from less than 6 to more than 8. They were also grouped in quintiles based upon their extent of fragmented sleep.
Subjects with short sleep were significantly older and more likely to have high blood pressure, a higher body mass index, and metabolic syndrome than those who averaged 7-8 hours of sleep. Individuals in the top quintile for sleep awakening were older and had higher prevalences of smoking and hypertension than those in the lowest quintile.
In multivariate analyses adjusted for these differences as well as for physical activity, depression, obstructive sleep apnea, daily calorie consumption, alcohol intake, and other potential confounders, subjects who slept less than 6 hours per night had a 27% greater volume of noncoronary plaque than those who slept 7-8 hours. They also had 21% more vascular territories laden with subclinical atherosclerosis. The risk of subclinical noncoronary atherosclerosis was greater among women who averaged less than 6 hours of sleep per night, representing a 48% relative risk increase in plaque volume, versus 21% in men.
At the other extreme, women who slept more than 8 hours per night had an 83% increased plaque volume, while men who slept that much had no increase in risk, compared with men who slept for 7-8 hours.
Subjects in the top quintile for sleep fragmentation had 34% more vascular territories affected by atherosclerosis than those in the lowest quintile. Their noncoronary plaque burden was 23% greater as well.
An 11-study meta-analysis
Epameinondas Fountas, MD, of the Onassis Cardiac Surgery Center in Athens, presented a meta-analysis of 11 prospective studies of the relationship between daily sleep duration and cardiovascular disease morbidity and mortality published within the past 5 years, reflecting burgeoning interest in this hot-button topic. Collectively, the meta-analysis totaled 1,000,541 adults without baseline cardiovascular disease who were followed for an average of 9.3 years.
In an analysis adjusted for numerous known cardiovascular risk factors, the Greek investigators found that short sleep duration as defined by a self-reported average of less than 6 hours per night was independently associated with a statistically significant and clinically meaningful 11% increase in the risk of diagnosis of fatal or nonfatal cardiovascular disease, compared with individuals who averaged 6-8 hours nightly. Moreover, those who averaged more than 8 hours of sleep per night were also at risk: they averaged a 32% increased risk in fatal or nonfatal cardiovascular events compared to normal 6- to 8-hour sleepers. Thus, 6-8 hours of sleep per night appears to be the sweet spot in terms of cardioprotection.
“Our message to patients is simple: Sleep well, not too long, nor too short, and be active,” Dr. Fountas said.
Numerous investigators have highlighted the pathophysiologic changes related to sleep deprivation that likely boost cardiovascular risk. These include activation of the sympathetic nervous system, increased inflammation, and disrupted glucose metabolism, he noted.
Swedes weigh in
Moa Bengtsson, a combined medical/PhD student at the University of Gothenburg (Sweden), presented a prospective study of 798 men who were 50 years old in 1993, when they underwent a physical examination and completed extensive lifestyle questionnaires that included average self-reported sleep duration. Among the 759 men still available for evaluation after 21 years, or nearly 15,000 person-years of followup, those who reported sleeping an average of 5 hours or less per night back at age 50 were 93% more likely to have experienced a major cardiovascular event by age 71 -- acute MI, stroke, coronary revascularization, heart failure hospitalization, or cardiovascular death -- compared with those who averaged 7-8 hours of shut eye.
The short sleepers had a higher prevalence of obesity, diabetes, hypertension, smoking, and physical inactivity than the men who slept 7-8 hours per night. However, these and other confounders were adjusted for in the multivariate analysis.
To place sleep abnormalities in context, Ms. Bengtssen observed that short sleep in the Gothenburg men was numerically a stronger independent risk factor for future cardiovascular events than obesity, which was associated with an 82% increase in risk, or even smoking, with a 70% increase in risk.
Men who averaged either 6 hours of sleep per night or more than 8 hours were not at increased cardiovascular risk over 21 years of followup, compared with those who slept 7-8 hours.
Like the other investigators, she noted that the studies presented at the meeting, despite their extensive adjustments for potential confounders, don’t prove a direct causal relationship between short sleep and increased cardiovascular risk. An informative next step in research, albeit a challenging one, would be to show whether improved long-term sleep habits favorably alter cardiovascular risk.
All three study investigators reported having no financial conflicts regarding their research, which was conducted free of commercial support.
MUNICH – Getting less than 6 hours of sleep nightly on a regular basis or waking up multiple times was independently associated with increased risk of subclinical atherosclerosis in the Spanish PESA study, Fernando Dominguez, MD, reported at the annual congress of the European Society of Cardiology.
Moreover, a graded response was evident in PESA (Progression of Early Subclinical Atherosclerosis): The more times an individual typically awoke per night, the greater the number of atherosclerotic carotid or femoral artery territories documented on three-dimensional vascular ultrasound, added Dr. Dominguez of the Spanish National Center for Cardiovascular Research in Madrid.
the cardiologist said.
The cross-sectional PESA study, whose principal investigator was Valentin Fuster, MD, PhD, included 3,974 middle-aged Madrid bank employees free of known heart disease or history of stroke who wore a waistband activity monitor for a week to record sleep quantity and quality. They also underwent three-dimensional vascular ultrasound and measurement of coronary artery calcium.
PESA was one of several large studies presented at the meeting that focused on deviations from normal sleep as a marker for increased risk of cardiovascular disease and/or mortality. Of note, however, PESA was the only one to use activity monitoring technology to track sleep.
“It was essential to use objectively measured sleep variables, because they showed huge disparity with patients’ self-reports on sleep questionnaires,” Dr. Dominguez explained.
Indeed, while 10.7% of PESA participants self-reported sleeping less than 6 hours per night on the Sleep Habits Questionnaire, actigraphy showed the true rate was 27.1%.
Based on actigraphic findings, subjects were divided into tertiles based upon average hours of sleep per night, ranging from less than 6 to more than 8. They were also grouped in quintiles based upon their extent of fragmented sleep.
Subjects with short sleep were significantly older and more likely to have high blood pressure, a higher body mass index, and metabolic syndrome than those who averaged 7-8 hours of sleep. Individuals in the top quintile for sleep awakening were older and had higher prevalences of smoking and hypertension than those in the lowest quintile.
In multivariate analyses adjusted for these differences as well as for physical activity, depression, obstructive sleep apnea, daily calorie consumption, alcohol intake, and other potential confounders, subjects who slept less than 6 hours per night had a 27% greater volume of noncoronary plaque than those who slept 7-8 hours. They also had 21% more vascular territories laden with subclinical atherosclerosis. The risk of subclinical noncoronary atherosclerosis was greater among women who averaged less than 6 hours of sleep per night, representing a 48% relative risk increase in plaque volume, versus 21% in men.
At the other extreme, women who slept more than 8 hours per night had an 83% increased plaque volume, while men who slept that much had no increase in risk, compared with men who slept for 7-8 hours.
Subjects in the top quintile for sleep fragmentation had 34% more vascular territories affected by atherosclerosis than those in the lowest quintile. Their noncoronary plaque burden was 23% greater as well.
An 11-study meta-analysis
Epameinondas Fountas, MD, of the Onassis Cardiac Surgery Center in Athens, presented a meta-analysis of 11 prospective studies of the relationship between daily sleep duration and cardiovascular disease morbidity and mortality published within the past 5 years, reflecting burgeoning interest in this hot-button topic. Collectively, the meta-analysis totaled 1,000,541 adults without baseline cardiovascular disease who were followed for an average of 9.3 years.
In an analysis adjusted for numerous known cardiovascular risk factors, the Greek investigators found that short sleep duration as defined by a self-reported average of less than 6 hours per night was independently associated with a statistically significant and clinically meaningful 11% increase in the risk of diagnosis of fatal or nonfatal cardiovascular disease, compared with individuals who averaged 6-8 hours nightly. Moreover, those who averaged more than 8 hours of sleep per night were also at risk: they averaged a 32% increased risk in fatal or nonfatal cardiovascular events compared to normal 6- to 8-hour sleepers. Thus, 6-8 hours of sleep per night appears to be the sweet spot in terms of cardioprotection.
“Our message to patients is simple: Sleep well, not too long, nor too short, and be active,” Dr. Fountas said.
Numerous investigators have highlighted the pathophysiologic changes related to sleep deprivation that likely boost cardiovascular risk. These include activation of the sympathetic nervous system, increased inflammation, and disrupted glucose metabolism, he noted.
Swedes weigh in
Moa Bengtsson, a combined medical/PhD student at the University of Gothenburg (Sweden), presented a prospective study of 798 men who were 50 years old in 1993, when they underwent a physical examination and completed extensive lifestyle questionnaires that included average self-reported sleep duration. Among the 759 men still available for evaluation after 21 years, or nearly 15,000 person-years of followup, those who reported sleeping an average of 5 hours or less per night back at age 50 were 93% more likely to have experienced a major cardiovascular event by age 71 -- acute MI, stroke, coronary revascularization, heart failure hospitalization, or cardiovascular death -- compared with those who averaged 7-8 hours of shut eye.
The short sleepers had a higher prevalence of obesity, diabetes, hypertension, smoking, and physical inactivity than the men who slept 7-8 hours per night. However, these and other confounders were adjusted for in the multivariate analysis.
To place sleep abnormalities in context, Ms. Bengtssen observed that short sleep in the Gothenburg men was numerically a stronger independent risk factor for future cardiovascular events than obesity, which was associated with an 82% increase in risk, or even smoking, with a 70% increase in risk.
Men who averaged either 6 hours of sleep per night or more than 8 hours were not at increased cardiovascular risk over 21 years of followup, compared with those who slept 7-8 hours.
Like the other investigators, she noted that the studies presented at the meeting, despite their extensive adjustments for potential confounders, don’t prove a direct causal relationship between short sleep and increased cardiovascular risk. An informative next step in research, albeit a challenging one, would be to show whether improved long-term sleep habits favorably alter cardiovascular risk.
All three study investigators reported having no financial conflicts regarding their research, which was conducted free of commercial support.
MUNICH – Getting less than 6 hours of sleep nightly on a regular basis or waking up multiple times was independently associated with increased risk of subclinical atherosclerosis in the Spanish PESA study, Fernando Dominguez, MD, reported at the annual congress of the European Society of Cardiology.
Moreover, a graded response was evident in PESA (Progression of Early Subclinical Atherosclerosis): The more times an individual typically awoke per night, the greater the number of atherosclerotic carotid or femoral artery territories documented on three-dimensional vascular ultrasound, added Dr. Dominguez of the Spanish National Center for Cardiovascular Research in Madrid.
the cardiologist said.
The cross-sectional PESA study, whose principal investigator was Valentin Fuster, MD, PhD, included 3,974 middle-aged Madrid bank employees free of known heart disease or history of stroke who wore a waistband activity monitor for a week to record sleep quantity and quality. They also underwent three-dimensional vascular ultrasound and measurement of coronary artery calcium.
PESA was one of several large studies presented at the meeting that focused on deviations from normal sleep as a marker for increased risk of cardiovascular disease and/or mortality. Of note, however, PESA was the only one to use activity monitoring technology to track sleep.
“It was essential to use objectively measured sleep variables, because they showed huge disparity with patients’ self-reports on sleep questionnaires,” Dr. Dominguez explained.
Indeed, while 10.7% of PESA participants self-reported sleeping less than 6 hours per night on the Sleep Habits Questionnaire, actigraphy showed the true rate was 27.1%.
Based on actigraphic findings, subjects were divided into tertiles based upon average hours of sleep per night, ranging from less than 6 to more than 8. They were also grouped in quintiles based upon their extent of fragmented sleep.
Subjects with short sleep were significantly older and more likely to have high blood pressure, a higher body mass index, and metabolic syndrome than those who averaged 7-8 hours of sleep. Individuals in the top quintile for sleep awakening were older and had higher prevalences of smoking and hypertension than those in the lowest quintile.
In multivariate analyses adjusted for these differences as well as for physical activity, depression, obstructive sleep apnea, daily calorie consumption, alcohol intake, and other potential confounders, subjects who slept less than 6 hours per night had a 27% greater volume of noncoronary plaque than those who slept 7-8 hours. They also had 21% more vascular territories laden with subclinical atherosclerosis. The risk of subclinical noncoronary atherosclerosis was greater among women who averaged less than 6 hours of sleep per night, representing a 48% relative risk increase in plaque volume, versus 21% in men.
At the other extreme, women who slept more than 8 hours per night had an 83% increased plaque volume, while men who slept that much had no increase in risk, compared with men who slept for 7-8 hours.
Subjects in the top quintile for sleep fragmentation had 34% more vascular territories affected by atherosclerosis than those in the lowest quintile. Their noncoronary plaque burden was 23% greater as well.
An 11-study meta-analysis
Epameinondas Fountas, MD, of the Onassis Cardiac Surgery Center in Athens, presented a meta-analysis of 11 prospective studies of the relationship between daily sleep duration and cardiovascular disease morbidity and mortality published within the past 5 years, reflecting burgeoning interest in this hot-button topic. Collectively, the meta-analysis totaled 1,000,541 adults without baseline cardiovascular disease who were followed for an average of 9.3 years.
In an analysis adjusted for numerous known cardiovascular risk factors, the Greek investigators found that short sleep duration as defined by a self-reported average of less than 6 hours per night was independently associated with a statistically significant and clinically meaningful 11% increase in the risk of diagnosis of fatal or nonfatal cardiovascular disease, compared with individuals who averaged 6-8 hours nightly. Moreover, those who averaged more than 8 hours of sleep per night were also at risk: they averaged a 32% increased risk in fatal or nonfatal cardiovascular events compared to normal 6- to 8-hour sleepers. Thus, 6-8 hours of sleep per night appears to be the sweet spot in terms of cardioprotection.
“Our message to patients is simple: Sleep well, not too long, nor too short, and be active,” Dr. Fountas said.
Numerous investigators have highlighted the pathophysiologic changes related to sleep deprivation that likely boost cardiovascular risk. These include activation of the sympathetic nervous system, increased inflammation, and disrupted glucose metabolism, he noted.
Swedes weigh in
Moa Bengtsson, a combined medical/PhD student at the University of Gothenburg (Sweden), presented a prospective study of 798 men who were 50 years old in 1993, when they underwent a physical examination and completed extensive lifestyle questionnaires that included average self-reported sleep duration. Among the 759 men still available for evaluation after 21 years, or nearly 15,000 person-years of followup, those who reported sleeping an average of 5 hours or less per night back at age 50 were 93% more likely to have experienced a major cardiovascular event by age 71 -- acute MI, stroke, coronary revascularization, heart failure hospitalization, or cardiovascular death -- compared with those who averaged 7-8 hours of shut eye.
The short sleepers had a higher prevalence of obesity, diabetes, hypertension, smoking, and physical inactivity than the men who slept 7-8 hours per night. However, these and other confounders were adjusted for in the multivariate analysis.
To place sleep abnormalities in context, Ms. Bengtssen observed that short sleep in the Gothenburg men was numerically a stronger independent risk factor for future cardiovascular events than obesity, which was associated with an 82% increase in risk, or even smoking, with a 70% increase in risk.
Men who averaged either 6 hours of sleep per night or more than 8 hours were not at increased cardiovascular risk over 21 years of followup, compared with those who slept 7-8 hours.
Like the other investigators, she noted that the studies presented at the meeting, despite their extensive adjustments for potential confounders, don’t prove a direct causal relationship between short sleep and increased cardiovascular risk. An informative next step in research, albeit a challenging one, would be to show whether improved long-term sleep habits favorably alter cardiovascular risk.
All three study investigators reported having no financial conflicts regarding their research, which was conducted free of commercial support.
REPORTING FROM THE ESC CONGRESS 2018
Four predictors confirmed for treatment-resistant depression
BARCELONA – Four potent clinical predictors of treatment-resistant depression have been confirmed in a validation study that showed the four factors collectively have a predictive accuracy of 87%, Alexander Kautzky, MD, reported at the annual congress of the European College of Neuropsychopharmacology.
The four predictors – all easily assessed – are symptom severity, which was independently associated with a 3.3-fold increased likelihood of treatment-resistant depression (TRD) in a study of 916 patients with major depression at 10 referral centers in eight European countries; suicidal risk, with a 1.74-fold increased risk; comorbid anxiety disorder, with a 1.68-fold increased risk; and the lifetime number of major depressive episodes, for which the associated TRD risk climbs by 15% per prior episode, according to Dr. Kautzky of the Medical University of Vienna.
When these four predictors were put to the test in an independent validation cohort of 314 patients with major depression, the four clinical markers of TRD exhibited a sensitivity of 86%, a specificity of 88%, and an overall predictive accuracy of 87%.
In these studies, Response was defined as at least a 50% drop in MADRS score to below 22 points.
The validation of these clinical predictors of TRD is a welcome development in psychiatry. The World Health Organization ranks major depressive disorder as the No. 4 cause of disease burden worldwide, and an impressive number of antidepressant medications are available, but up to 60% of patients do not respond sufficiently to their first round of antidepressant therapy. And there is a notable absence of biological markers to aid in selecting the best initial antidepressant for a given individual, Dr. Kautzky observed.
The validation study was supported by an unrestricted research grant from Lundbeck to a European research consortium known as the Group for the Study of Resistant Depression. Dr. Kautzky reported having no financial conflicts of interest.
BARCELONA – Four potent clinical predictors of treatment-resistant depression have been confirmed in a validation study that showed the four factors collectively have a predictive accuracy of 87%, Alexander Kautzky, MD, reported at the annual congress of the European College of Neuropsychopharmacology.
The four predictors – all easily assessed – are symptom severity, which was independently associated with a 3.3-fold increased likelihood of treatment-resistant depression (TRD) in a study of 916 patients with major depression at 10 referral centers in eight European countries; suicidal risk, with a 1.74-fold increased risk; comorbid anxiety disorder, with a 1.68-fold increased risk; and the lifetime number of major depressive episodes, for which the associated TRD risk climbs by 15% per prior episode, according to Dr. Kautzky of the Medical University of Vienna.
When these four predictors were put to the test in an independent validation cohort of 314 patients with major depression, the four clinical markers of TRD exhibited a sensitivity of 86%, a specificity of 88%, and an overall predictive accuracy of 87%.
In these studies, Response was defined as at least a 50% drop in MADRS score to below 22 points.
The validation of these clinical predictors of TRD is a welcome development in psychiatry. The World Health Organization ranks major depressive disorder as the No. 4 cause of disease burden worldwide, and an impressive number of antidepressant medications are available, but up to 60% of patients do not respond sufficiently to their first round of antidepressant therapy. And there is a notable absence of biological markers to aid in selecting the best initial antidepressant for a given individual, Dr. Kautzky observed.
The validation study was supported by an unrestricted research grant from Lundbeck to a European research consortium known as the Group for the Study of Resistant Depression. Dr. Kautzky reported having no financial conflicts of interest.
BARCELONA – Four potent clinical predictors of treatment-resistant depression have been confirmed in a validation study that showed the four factors collectively have a predictive accuracy of 87%, Alexander Kautzky, MD, reported at the annual congress of the European College of Neuropsychopharmacology.
The four predictors – all easily assessed – are symptom severity, which was independently associated with a 3.3-fold increased likelihood of treatment-resistant depression (TRD) in a study of 916 patients with major depression at 10 referral centers in eight European countries; suicidal risk, with a 1.74-fold increased risk; comorbid anxiety disorder, with a 1.68-fold increased risk; and the lifetime number of major depressive episodes, for which the associated TRD risk climbs by 15% per prior episode, according to Dr. Kautzky of the Medical University of Vienna.
When these four predictors were put to the test in an independent validation cohort of 314 patients with major depression, the four clinical markers of TRD exhibited a sensitivity of 86%, a specificity of 88%, and an overall predictive accuracy of 87%.
In these studies, Response was defined as at least a 50% drop in MADRS score to below 22 points.
The validation of these clinical predictors of TRD is a welcome development in psychiatry. The World Health Organization ranks major depressive disorder as the No. 4 cause of disease burden worldwide, and an impressive number of antidepressant medications are available, but up to 60% of patients do not respond sufficiently to their first round of antidepressant therapy. And there is a notable absence of biological markers to aid in selecting the best initial antidepressant for a given individual, Dr. Kautzky observed.
The validation study was supported by an unrestricted research grant from Lundbeck to a European research consortium known as the Group for the Study of Resistant Depression. Dr. Kautzky reported having no financial conflicts of interest.
REPORTING FROM THE ECNP CONGRESS
Key clinical point: Patients with major depressive disorder at high risk for treatment-resistant depression are now readily identifiable.
Major finding: Four easily collected clinical variables predict treatment-resistant depression with 87% accuracy.
Study details: This project identified clinical predictors of treatment-resistant depression in a cohort of 916 patients with major depressive disorder then validated the predictors in a separate cohort of 314 patients.
Disclosures: The presenter reported having no financial conflicts regarding this study, which was supported by an unrestricted research grant from Lundbeck.
Delusional infestation: not so rare
PARIS – Ever wonder, when encountering an occasional patient afflicted with delusional infestation, just how common this mental disorder is?
John J. Kohorst, MD, and his coinvestigators at the Mayo Clinic in Rochester, Minn., have the evidence-based answer.
The age- and sex-adjusted point prevalence of delusional infestation among Olmsted County, Minn., residents on the final day of 2010 was 27.3 cases per 100,000 person-years, he reported at the annual congress of the European Academy of Dermatology and Venereology.
“This is the than previously suspected,” according to the dermatologist.
He and his coinvestigators retrospectively analyzed data from the Rochester Epidemiology Project. They identified 22 female and 13 male county residents with a firm diagnosis of delusional infestation, also known as delusional parasitosis. This disorder is marked by a patient’s fixed false belief that they are infested with insects, worms, or other pathogens.
The prevalence was similar in men and women. The most striking study finding was how heavily age-dependent delusional infestation was. Before age 40, the prevalence was a mere 1.2 cases per 100,000 person-years. Among 40- to 59-year-old Olmsted County residents, it was 35/100,000, jumping to 64.5/100,000 in the 60- to 79-year-old age bracket, then doubling to 130.1 cases per 100,000 person-years in individuals aged 80 or older.
Dr. Kohorst reported having no financial conflicts regarding his study, conducted free of commercial support.
PARIS – Ever wonder, when encountering an occasional patient afflicted with delusional infestation, just how common this mental disorder is?
John J. Kohorst, MD, and his coinvestigators at the Mayo Clinic in Rochester, Minn., have the evidence-based answer.
The age- and sex-adjusted point prevalence of delusional infestation among Olmsted County, Minn., residents on the final day of 2010 was 27.3 cases per 100,000 person-years, he reported at the annual congress of the European Academy of Dermatology and Venereology.
“This is the than previously suspected,” according to the dermatologist.
He and his coinvestigators retrospectively analyzed data from the Rochester Epidemiology Project. They identified 22 female and 13 male county residents with a firm diagnosis of delusional infestation, also known as delusional parasitosis. This disorder is marked by a patient’s fixed false belief that they are infested with insects, worms, or other pathogens.
The prevalence was similar in men and women. The most striking study finding was how heavily age-dependent delusional infestation was. Before age 40, the prevalence was a mere 1.2 cases per 100,000 person-years. Among 40- to 59-year-old Olmsted County residents, it was 35/100,000, jumping to 64.5/100,000 in the 60- to 79-year-old age bracket, then doubling to 130.1 cases per 100,000 person-years in individuals aged 80 or older.
Dr. Kohorst reported having no financial conflicts regarding his study, conducted free of commercial support.
PARIS – Ever wonder, when encountering an occasional patient afflicted with delusional infestation, just how common this mental disorder is?
John J. Kohorst, MD, and his coinvestigators at the Mayo Clinic in Rochester, Minn., have the evidence-based answer.
The age- and sex-adjusted point prevalence of delusional infestation among Olmsted County, Minn., residents on the final day of 2010 was 27.3 cases per 100,000 person-years, he reported at the annual congress of the European Academy of Dermatology and Venereology.
“This is the than previously suspected,” according to the dermatologist.
He and his coinvestigators retrospectively analyzed data from the Rochester Epidemiology Project. They identified 22 female and 13 male county residents with a firm diagnosis of delusional infestation, also known as delusional parasitosis. This disorder is marked by a patient’s fixed false belief that they are infested with insects, worms, or other pathogens.
The prevalence was similar in men and women. The most striking study finding was how heavily age-dependent delusional infestation was. Before age 40, the prevalence was a mere 1.2 cases per 100,000 person-years. Among 40- to 59-year-old Olmsted County residents, it was 35/100,000, jumping to 64.5/100,000 in the 60- to 79-year-old age bracket, then doubling to 130.1 cases per 100,000 person-years in individuals aged 80 or older.
Dr. Kohorst reported having no financial conflicts regarding his study, conducted free of commercial support.
REPORTING FROM THE EADV CONGRESS
Key clinical point: Delusional infestation may be more common than previously suspected, particularly among older age groups.
Major finding: The age- and sex-adjusted point prevalence of delusional infestation among residents of one county in southeastern Minnesota is 27.3 cases per 100,000 person-years.
Study details: This was a retrospective analysis of data from the Rochester (Minn.) Epidemiology Project.
Disclosures: The presenter reported having no financial conflicts regarding his study, conducted free of commercial support.
Adult ADHD? Screen for hoarding symptoms
BARCELONA – Clinically meaningful hoarding symptoms are present in roughly one in four adults with attention-deficit/hyperactivity disorder, Sharon Morein-Zamir, PhD, reported at the annual congress of the European College of Neuropsychopharmacology.
Her message to her fellow clinicians: “Nobody tends to ask about hoarding problems in adult ADHD clinics. Ask your ADHD patients carefully and routinely about hoarding symptoms. Screen them for it, ask their family members about it, and see whether it could be a problem contributing to daily impairment,” urged Dr. Morein-Zamir, a senior lecturer in clinical psychology at Anglia Ruskin University in Cambridge, England.
The clinician must broach the subject, because hoarding often is characterized by lack of insight.
“Patients don’t complain about it. You’ll have family members complain about it, neighbors complain about it, maybe social services, but the individuals themselves often don’t think they have a problem. And if they acknowledge it, they don’t seek treatment for it. So you really need to actively ask about the issue. They won’t raise it themselves,” she said.
Hoarding disorder and ADHD are considered two separate entities. But her study demonstrated that they share a common link: inattention symptoms.
the psychologist continued.
Indeed, one of the reasons why hoarding disorder is no longer grouped with obsessive-compulsive disorder in diagnostic schema is that inattention symptoms are not characteristic of OCD.
Dr. Morein-Zamir presented a cross-sectional study of 50 patients in an adult ADHD clinic and 46 age- and sex-matched controls. A total of 22 of the ADHD patients were on methylphenidate, 15 on selective serotonin reuptake inhibitors, 6 on amphetamine, and 7 were unmedicated.
Participants were assessed for hoarding using two validated measures well-suited for screening in daily practice: the Saving Inventory–Revised (SIR) and the Clutter Image Rating (CIR). Clinically meaningful hoarding symptoms – a designation requiring both a score of at least 42 on the SIR and 12 on the CIR – were present in 11 of 50 adult ADHD patients and none of the controls.
The group with clinically meaningful hoarding symptoms differed from the 39 ADHD patients without hoarding most noticeably in their more pronounced inattention symptoms as scored on the Adult ADHD Self-Report Scale (ASRS): a mean score of 32.8, compared with 28.8 in ADHD patients without clinically important hoarding. In contrast, the two groups scored similarly for hyperactivity/impulsivity on the patient-completed 18-item ASRS, as well as for depression and anxiety on the Depression Anxiety Stress Scales (DASS).
Within the ADHD group, only inattention as measured on the ASRS predicted hoarding severity on the SIR. In a multivariate regression analysis controlling for age, sex, hyperactivity/impulsivity on the ASRS, and DASS scores, inattention correlated strongly with all of the key hoarding dimensions: clutter, excessive acquisition, and difficulty discarding. Hyperactivity/impulsivity showed a modest correlation with clutter but not with the other hoarding dimensions.
Dr. Morein-Zamir observed that, while the last 3 or so years have seen booming interest in the development of manualized cognitive-behavioral therapy strategies for hoarding disorder, it’s not yet known whether those tools will be effective for treating high-level hoarding symptoms in patients with ADHD.
She reported having no financial conflicts regarding her study, which was funded by the British Academy.
BARCELONA – Clinically meaningful hoarding symptoms are present in roughly one in four adults with attention-deficit/hyperactivity disorder, Sharon Morein-Zamir, PhD, reported at the annual congress of the European College of Neuropsychopharmacology.
Her message to her fellow clinicians: “Nobody tends to ask about hoarding problems in adult ADHD clinics. Ask your ADHD patients carefully and routinely about hoarding symptoms. Screen them for it, ask their family members about it, and see whether it could be a problem contributing to daily impairment,” urged Dr. Morein-Zamir, a senior lecturer in clinical psychology at Anglia Ruskin University in Cambridge, England.
The clinician must broach the subject, because hoarding often is characterized by lack of insight.
“Patients don’t complain about it. You’ll have family members complain about it, neighbors complain about it, maybe social services, but the individuals themselves often don’t think they have a problem. And if they acknowledge it, they don’t seek treatment for it. So you really need to actively ask about the issue. They won’t raise it themselves,” she said.
Hoarding disorder and ADHD are considered two separate entities. But her study demonstrated that they share a common link: inattention symptoms.
the psychologist continued.
Indeed, one of the reasons why hoarding disorder is no longer grouped with obsessive-compulsive disorder in diagnostic schema is that inattention symptoms are not characteristic of OCD.
Dr. Morein-Zamir presented a cross-sectional study of 50 patients in an adult ADHD clinic and 46 age- and sex-matched controls. A total of 22 of the ADHD patients were on methylphenidate, 15 on selective serotonin reuptake inhibitors, 6 on amphetamine, and 7 were unmedicated.
Participants were assessed for hoarding using two validated measures well-suited for screening in daily practice: the Saving Inventory–Revised (SIR) and the Clutter Image Rating (CIR). Clinically meaningful hoarding symptoms – a designation requiring both a score of at least 42 on the SIR and 12 on the CIR – were present in 11 of 50 adult ADHD patients and none of the controls.
The group with clinically meaningful hoarding symptoms differed from the 39 ADHD patients without hoarding most noticeably in their more pronounced inattention symptoms as scored on the Adult ADHD Self-Report Scale (ASRS): a mean score of 32.8, compared with 28.8 in ADHD patients without clinically important hoarding. In contrast, the two groups scored similarly for hyperactivity/impulsivity on the patient-completed 18-item ASRS, as well as for depression and anxiety on the Depression Anxiety Stress Scales (DASS).
Within the ADHD group, only inattention as measured on the ASRS predicted hoarding severity on the SIR. In a multivariate regression analysis controlling for age, sex, hyperactivity/impulsivity on the ASRS, and DASS scores, inattention correlated strongly with all of the key hoarding dimensions: clutter, excessive acquisition, and difficulty discarding. Hyperactivity/impulsivity showed a modest correlation with clutter but not with the other hoarding dimensions.
Dr. Morein-Zamir observed that, while the last 3 or so years have seen booming interest in the development of manualized cognitive-behavioral therapy strategies for hoarding disorder, it’s not yet known whether those tools will be effective for treating high-level hoarding symptoms in patients with ADHD.
She reported having no financial conflicts regarding her study, which was funded by the British Academy.
BARCELONA – Clinically meaningful hoarding symptoms are present in roughly one in four adults with attention-deficit/hyperactivity disorder, Sharon Morein-Zamir, PhD, reported at the annual congress of the European College of Neuropsychopharmacology.
Her message to her fellow clinicians: “Nobody tends to ask about hoarding problems in adult ADHD clinics. Ask your ADHD patients carefully and routinely about hoarding symptoms. Screen them for it, ask their family members about it, and see whether it could be a problem contributing to daily impairment,” urged Dr. Morein-Zamir, a senior lecturer in clinical psychology at Anglia Ruskin University in Cambridge, England.
The clinician must broach the subject, because hoarding often is characterized by lack of insight.
“Patients don’t complain about it. You’ll have family members complain about it, neighbors complain about it, maybe social services, but the individuals themselves often don’t think they have a problem. And if they acknowledge it, they don’t seek treatment for it. So you really need to actively ask about the issue. They won’t raise it themselves,” she said.
Hoarding disorder and ADHD are considered two separate entities. But her study demonstrated that they share a common link: inattention symptoms.
the psychologist continued.
Indeed, one of the reasons why hoarding disorder is no longer grouped with obsessive-compulsive disorder in diagnostic schema is that inattention symptoms are not characteristic of OCD.
Dr. Morein-Zamir presented a cross-sectional study of 50 patients in an adult ADHD clinic and 46 age- and sex-matched controls. A total of 22 of the ADHD patients were on methylphenidate, 15 on selective serotonin reuptake inhibitors, 6 on amphetamine, and 7 were unmedicated.
Participants were assessed for hoarding using two validated measures well-suited for screening in daily practice: the Saving Inventory–Revised (SIR) and the Clutter Image Rating (CIR). Clinically meaningful hoarding symptoms – a designation requiring both a score of at least 42 on the SIR and 12 on the CIR – were present in 11 of 50 adult ADHD patients and none of the controls.
The group with clinically meaningful hoarding symptoms differed from the 39 ADHD patients without hoarding most noticeably in their more pronounced inattention symptoms as scored on the Adult ADHD Self-Report Scale (ASRS): a mean score of 32.8, compared with 28.8 in ADHD patients without clinically important hoarding. In contrast, the two groups scored similarly for hyperactivity/impulsivity on the patient-completed 18-item ASRS, as well as for depression and anxiety on the Depression Anxiety Stress Scales (DASS).
Within the ADHD group, only inattention as measured on the ASRS predicted hoarding severity on the SIR. In a multivariate regression analysis controlling for age, sex, hyperactivity/impulsivity on the ASRS, and DASS scores, inattention correlated strongly with all of the key hoarding dimensions: clutter, excessive acquisition, and difficulty discarding. Hyperactivity/impulsivity showed a modest correlation with clutter but not with the other hoarding dimensions.
Dr. Morein-Zamir observed that, while the last 3 or so years have seen booming interest in the development of manualized cognitive-behavioral therapy strategies for hoarding disorder, it’s not yet known whether those tools will be effective for treating high-level hoarding symptoms in patients with ADHD.
She reported having no financial conflicts regarding her study, which was funded by the British Academy.
REPORTING FROM THE ECNP CONGRESS
Key clinical point: Routinely screen adults with ADHD for hoarding disorder.
Major finding: Eleven of 50 (22%) unselected adults with ADHD displayed clinically meaningful hoarding symptoms.
Study details: This cross-sectional study included 50 adult ADHD patients and 46 matched controls who were assessed for hoarding symptoms and inattention.
Disclosures: The presenter reported having no financial conflicts regarding this study, which was funded by the British Academy.
Data support revising ASCVD cardiovascular risk threshold
MUNICH – Revising the threshold for actionable high cardiovascular risk from the current 7.5% or greater risk of an event within 10 years as defined in American College of Cardiology/American Heart Association guidelines using the Atherosclerotic Cardiovascular Disease (ASCVD ) Risk Calculator to a 10% or greater 10-year risk would provide the optimal balance of sensitivity and specificity for discriminating future risk of cardiovascular events, according to Robert S. Rosenman, MD.
“I think this is very important from a public health policy perspective,” Dr. Rosenman, a cardiologist who is professor of medicine at Mount Sinai School of Medicine in New York, said at the annual congress of the European Society of Cardiology.
He elaborated: “This would eliminate 11.4 million people who are currently candidates for a statin but may not be getting the benefits of statin therapy. We feel that this information is actually quite important for the primary prevention population because there’s been a lot of pushback from our primary care physician colleagues about the overtreatment of low-risk individuals” under the current guidelines (Circulation. 2014 Jun 24;129[25 Suppl 2]:S49-73).
Dr. Rosenman and his coinvestigators conducted a secondary analysis of data on 21,343 adults in the REGARDS (Reasons for Geographic and Racial Differences in Stroke) study. All participants were free of a baseline history of heart disease or stroke. During a median 8.5 years of follow-up, 1,717 of them experienced adjudicated coronary heart disease or stroke events.
In multivariate analyses adjusted for standard cardiovascular risk factors, socioeconomic and demographic factors, and the use of statins and/or antihypertensive drugs, the higher the baseline 10-year predicted risk using the ACC/AHA ASCVD Risk Calculator based on the Pooled Cohort risk equations, the higher the incidence rate of cardiovascular events. No surprise there.
What was impressive, however, was that the optimal combination of sensitivity and specificity as captured in a statistic known as Youden’s index occurred at a 10-year predicted risk of 10%-12%. The biggest net improvement obtained through reclassification resulted from moving the threshold for elevated 10-year cardiovascular risk warranting statin therapy from 7.5% or greater to 10% or more, rather than using thresholds of 15% or 20%.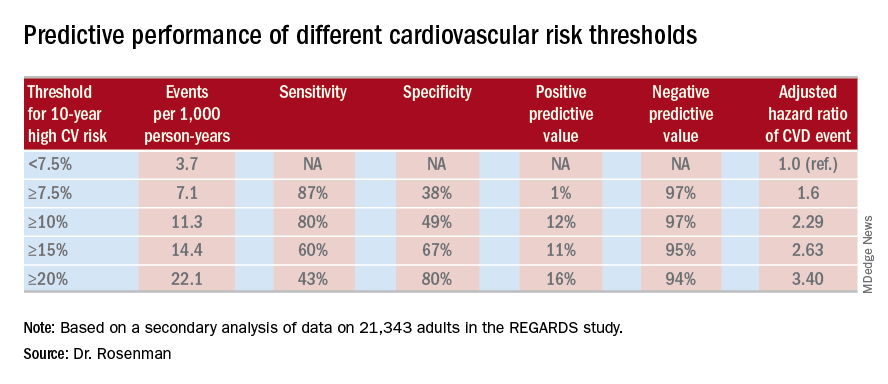
He cited data from the 2011-2014 National Health and Nutrition Examination Survey in support of his estimate that switching to a 10% threshold from the current 7.5% threshold would reduce the number of Americans deemed at high cardiovascular risk from 57.1 million to 45.8 million.
“This cutoff value of 10%, by the way, is the same cutoff value used in the recently published ACC/AHA guideline on hypertension. And it’s also the same cutoff value used for antiplatelet therapy in looking at the benefit/risk ratio. So this value of 10% is, I think, really the right number. Our study is the first effort that has been shown to validate that number, and it brings the cutoff values in the various guidelines in line,” the cardiologist observed.
Asked if these new findings are likely to result in a revision of the ACC/AHA cardiovascular risk assessment guidelines, Dr. Rosenman replied that the guidelines are under revision, with the draft update now circulating for comment. So the timing is dicey: His study is now in prepublication peer review, but hasn’t yet been published and thus may not carry persuasive weight.
“Hopefully, the guideline panel is going to make an adjustment to make the 10% figure in line with the blood pressure guidelines,” he said.
The new analysis of the REGARDS study was funded by a collaboration between Amgen, Mount Sinai School of Medicine, and the University of Alabama. Dr. Rosenman reported receiving research funding from and serving as an advisor to Amgen and a handful of other companies.
MUNICH – Revising the threshold for actionable high cardiovascular risk from the current 7.5% or greater risk of an event within 10 years as defined in American College of Cardiology/American Heart Association guidelines using the Atherosclerotic Cardiovascular Disease (ASCVD ) Risk Calculator to a 10% or greater 10-year risk would provide the optimal balance of sensitivity and specificity for discriminating future risk of cardiovascular events, according to Robert S. Rosenman, MD.
“I think this is very important from a public health policy perspective,” Dr. Rosenman, a cardiologist who is professor of medicine at Mount Sinai School of Medicine in New York, said at the annual congress of the European Society of Cardiology.
He elaborated: “This would eliminate 11.4 million people who are currently candidates for a statin but may not be getting the benefits of statin therapy. We feel that this information is actually quite important for the primary prevention population because there’s been a lot of pushback from our primary care physician colleagues about the overtreatment of low-risk individuals” under the current guidelines (Circulation. 2014 Jun 24;129[25 Suppl 2]:S49-73).
Dr. Rosenman and his coinvestigators conducted a secondary analysis of data on 21,343 adults in the REGARDS (Reasons for Geographic and Racial Differences in Stroke) study. All participants were free of a baseline history of heart disease or stroke. During a median 8.5 years of follow-up, 1,717 of them experienced adjudicated coronary heart disease or stroke events.
In multivariate analyses adjusted for standard cardiovascular risk factors, socioeconomic and demographic factors, and the use of statins and/or antihypertensive drugs, the higher the baseline 10-year predicted risk using the ACC/AHA ASCVD Risk Calculator based on the Pooled Cohort risk equations, the higher the incidence rate of cardiovascular events. No surprise there.
What was impressive, however, was that the optimal combination of sensitivity and specificity as captured in a statistic known as Youden’s index occurred at a 10-year predicted risk of 10%-12%. The biggest net improvement obtained through reclassification resulted from moving the threshold for elevated 10-year cardiovascular risk warranting statin therapy from 7.5% or greater to 10% or more, rather than using thresholds of 15% or 20%.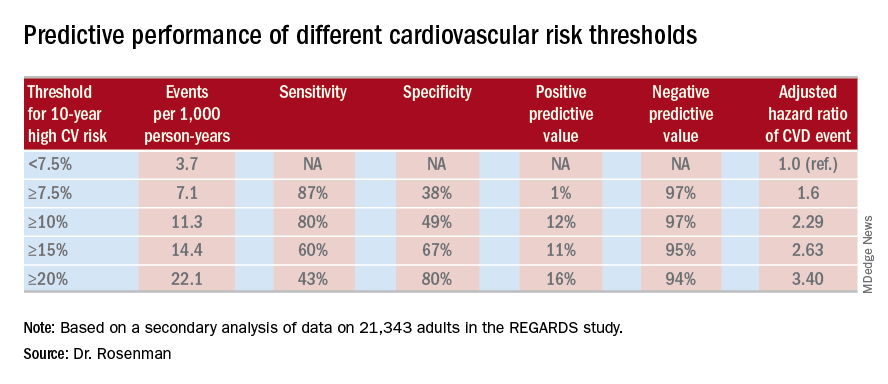
He cited data from the 2011-2014 National Health and Nutrition Examination Survey in support of his estimate that switching to a 10% threshold from the current 7.5% threshold would reduce the number of Americans deemed at high cardiovascular risk from 57.1 million to 45.8 million.
“This cutoff value of 10%, by the way, is the same cutoff value used in the recently published ACC/AHA guideline on hypertension. And it’s also the same cutoff value used for antiplatelet therapy in looking at the benefit/risk ratio. So this value of 10% is, I think, really the right number. Our study is the first effort that has been shown to validate that number, and it brings the cutoff values in the various guidelines in line,” the cardiologist observed.
Asked if these new findings are likely to result in a revision of the ACC/AHA cardiovascular risk assessment guidelines, Dr. Rosenman replied that the guidelines are under revision, with the draft update now circulating for comment. So the timing is dicey: His study is now in prepublication peer review, but hasn’t yet been published and thus may not carry persuasive weight.
“Hopefully, the guideline panel is going to make an adjustment to make the 10% figure in line with the blood pressure guidelines,” he said.
The new analysis of the REGARDS study was funded by a collaboration between Amgen, Mount Sinai School of Medicine, and the University of Alabama. Dr. Rosenman reported receiving research funding from and serving as an advisor to Amgen and a handful of other companies.
MUNICH – Revising the threshold for actionable high cardiovascular risk from the current 7.5% or greater risk of an event within 10 years as defined in American College of Cardiology/American Heart Association guidelines using the Atherosclerotic Cardiovascular Disease (ASCVD ) Risk Calculator to a 10% or greater 10-year risk would provide the optimal balance of sensitivity and specificity for discriminating future risk of cardiovascular events, according to Robert S. Rosenman, MD.
“I think this is very important from a public health policy perspective,” Dr. Rosenman, a cardiologist who is professor of medicine at Mount Sinai School of Medicine in New York, said at the annual congress of the European Society of Cardiology.
He elaborated: “This would eliminate 11.4 million people who are currently candidates for a statin but may not be getting the benefits of statin therapy. We feel that this information is actually quite important for the primary prevention population because there’s been a lot of pushback from our primary care physician colleagues about the overtreatment of low-risk individuals” under the current guidelines (Circulation. 2014 Jun 24;129[25 Suppl 2]:S49-73).
Dr. Rosenman and his coinvestigators conducted a secondary analysis of data on 21,343 adults in the REGARDS (Reasons for Geographic and Racial Differences in Stroke) study. All participants were free of a baseline history of heart disease or stroke. During a median 8.5 years of follow-up, 1,717 of them experienced adjudicated coronary heart disease or stroke events.
In multivariate analyses adjusted for standard cardiovascular risk factors, socioeconomic and demographic factors, and the use of statins and/or antihypertensive drugs, the higher the baseline 10-year predicted risk using the ACC/AHA ASCVD Risk Calculator based on the Pooled Cohort risk equations, the higher the incidence rate of cardiovascular events. No surprise there.
What was impressive, however, was that the optimal combination of sensitivity and specificity as captured in a statistic known as Youden’s index occurred at a 10-year predicted risk of 10%-12%. The biggest net improvement obtained through reclassification resulted from moving the threshold for elevated 10-year cardiovascular risk warranting statin therapy from 7.5% or greater to 10% or more, rather than using thresholds of 15% or 20%.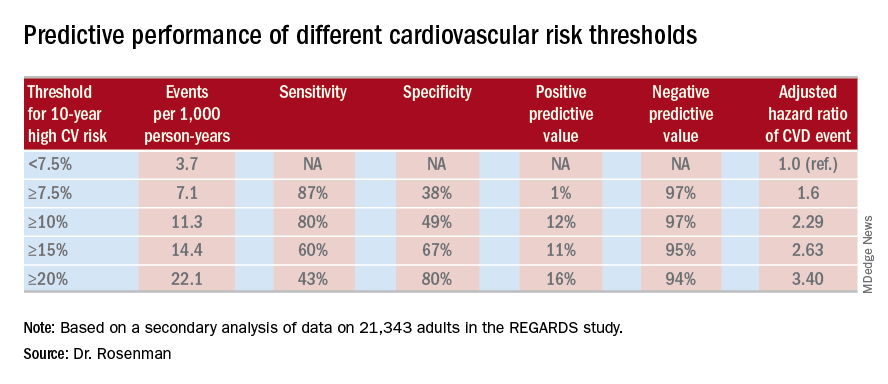
He cited data from the 2011-2014 National Health and Nutrition Examination Survey in support of his estimate that switching to a 10% threshold from the current 7.5% threshold would reduce the number of Americans deemed at high cardiovascular risk from 57.1 million to 45.8 million.
“This cutoff value of 10%, by the way, is the same cutoff value used in the recently published ACC/AHA guideline on hypertension. And it’s also the same cutoff value used for antiplatelet therapy in looking at the benefit/risk ratio. So this value of 10% is, I think, really the right number. Our study is the first effort that has been shown to validate that number, and it brings the cutoff values in the various guidelines in line,” the cardiologist observed.
Asked if these new findings are likely to result in a revision of the ACC/AHA cardiovascular risk assessment guidelines, Dr. Rosenman replied that the guidelines are under revision, with the draft update now circulating for comment. So the timing is dicey: His study is now in prepublication peer review, but hasn’t yet been published and thus may not carry persuasive weight.
“Hopefully, the guideline panel is going to make an adjustment to make the 10% figure in line with the blood pressure guidelines,” he said.
The new analysis of the REGARDS study was funded by a collaboration between Amgen, Mount Sinai School of Medicine, and the University of Alabama. Dr. Rosenman reported receiving research funding from and serving as an advisor to Amgen and a handful of other companies.
REPORTING FROM THE ESC CONGRESS 2018
Key clinical point:
Major finding: Redefining the threshold for high 10-year cardiovascular risk from the current 7.5% to 10% would reduce the number of Americans warranting statin therapy by 11.4 million.
Study details: This was a secondary analysis of data on 21,343 adults in the REGARDS study, 1,717 of whom experienced coronary heart disease or stroke events during a median 8.5 years of prospective follow-up.
Disclosures: The new analysis of the REGARDS study was funded by a collaboration between Amgen, Mount Sinai School of Medicine, and the University of Alabama. The presenter reported ties to Amgen and a handful of other companies.
The year’s top studies in child/adolescent psychiatry
BARCELONA – Prenatal exposure to selective serotonin reuptake inhibitors late in pregnancy was associated with a significantly increased risk of anxious and/or depressed behaviors at 5 years of age in the prospective Norwegian Mother and Child Cohort Study.
Other than that specific red flag, however, the outcomes of in utero exposure to maternal SSRIs were reassuringly benign. Prenatal exposure during early- or mid-pregnancy was not associated with increased risk of anxious/depressed behaviors, compared with nonexposure; that adverse effect was restricted to exposure at week 29 of pregnancy or later. Nor did in utero exposure to maternal SSRIs during any time in pregnancy pose an increased risk for pediatric externalizing, emotional, or social problems in this observational study of 8,359 Norwegian mother-child dyads, Josefina Castro-Fornieles, MD, PhD, observed at the annual congress of the European College of Neuropsychopharmacology.
The huge Norwegian study was among what she considers the four most important studies in child/adolescent psychiatry published through the first three quarters of 2018. The others she highlighted were a large longitudinal observational study that demonstrated that persistent maternal postnatal depression was strongly associated with a variety of pediatric behavioral disturbances documented during assessments at ages 3.5, 16, and 18 years; a Philadelphia study showing that multiple traumatic stressful events or any assaultive trauma experienced by children or adolescents were independently associated with significant psychopathology and neurocognitive deficits; and a Dutch brain MRI study that pinpointed a reduction in gray matter volume in the anterior cingulate cortex as a potential key mediator of the neurobiologic aftereffects of childhood sexual abuse.
She selected those studies because they shared a common theme, one that constituted her key take-home message: “When recording antecedents during a clinical assessment, both with adults and children, it is clear that we have to ask in a more detailed way – using validated scales and interviews if possible – about the mother’s prenatal problems, including psychopharmacological treatment. That is something we often don’t do in a sufficiently detailed way in our clinical practice. And it’s also important to ask about life events; abuse during childhood and adolescence can be really important. We can modulate our treatment depending upon whether there is an influence of any of these aspects,” said Dr. Castro-Fornieles, director of the Clinical Institute of Neuroscience at the Hospital Clinic of Barcelona and a recent past-president of the Spanish Society for Child and Adolescent Psychiatry.
The following are her Top 4 studies:
The Norwegian Mother and Child Cohort Study
The increased risk of anxious and/or depressed behaviors in children exposed to selective serotonin reuptake inhibitors (SSRIs) late in pregnancy did not emerge until the year-5 assessment; it wasn’t evident at the 1.5- or 3-year evaluations.
The investigators emphasized a key lesson from their study: The importance of following children with late-pregnancy exposure to maternal SSRI therapy for development of symptoms of anxiety and/or depression (J Am Acad Child Adolesc Psychiatry. 2018 Mar;57[3]:200-8). Dr. Castro-Fornieles strongly endorsed that recommendation. However, she noted what she considers an important limitation to the study: even though the University of Oslo investigators adjusted for numerous potential confounders in their risk models – including maternal body mass index, parity, education, smoking, substance use, breastfeeding, folic acid use, and other medications used during pregnancy – it’s not possible in a study such as this to control for genetic and environmental risk factors, which she suspects also were at work.
The Avon Longitudinal Study of Parents and Children in the United Kingdom
Maternal postnatal depression is common, affecting roughly 10% of mothers. But it is not invariably associated with adverse mental health outcomes in their children. This study of nearly 10,000 mothers and their children sought to identify which children were at most risk. Using the Edinburgh Postnatal Depression Scale, the international team of investigators categorized maternal postnatal depression as moderate, marked, or severe. The affective disorder was deemed persistent if scores on the Edinburgh scale were elevated at both 2 and 8 months after delivery.
Postnatal depression, whether persistent or not, was associated with roughly a 2- to 2.4-fold increase for child behavioral disturbances when assessed at age 3.5 years using the Rutter Total Problems Scale. But postnatal depression that was persistent was the real difference maker: It carried a much higher risk of adverse behavioral outcomes and cognitive deficits than did the nonpersistent version. Indeed, persistent severe postnatal depression was associated a 4.8-fold increased risk of behavioral problems at age 3.5 years, a 2.65-fold greater risk of markedly lower grades in mathematics at age 16 years, and a 7.4-fold increased prevalence of depression at 18 years of age. The investigators advised screening mothers during the first postpartum year in order to identify those with persistent postpartum depression (JAMA Psychiatry. 2018 Mar 1;75[3]:247-53).
Dr. Castro-Fornieles said an important shortcoming of the Avon study was that it did not record paternal data.
“The study didn’t consider depression or other functional measures in the father, his commitment to childrearing, and whether the family was together or divorced. I feel this is an important limitation in many studies. For me, it’s really important to consider what’s happening with the fathers,” she said.
Traumatic stress load, psychopathology, and cognition
An eye-opening report from the Philadelphia Neurodevelopmental Cohort documented a surprisingly high level of lifetime exposure to traumatic events among 9,498 youth aged 8-21 years, and the stepwise manner by which a greater traumatic stress load was associated with increasing severity of psychopathology and cognitive deficits. Notably, the study participants were recruited from general pediatric clinics in the Children’s Hospital of Philadelphia health care network; they were not patients seeking psychiatric help. And yet, extensive structured psychiatric evaluation showed that 23% of them had a history of one traumatic stressful event, 12% had two, and 1% had three or more.
In analyses adjusted for lifetime history of depression or PTSD, a higher traumatic event load was associated with increased risk of externalizing behaviors, mood/anxiety disorders, psychosis spectrum, and fear. Moreover, a high trauma stress load was associated with a 5.3-fold increased risk of suicidal thoughts and a 3.2-fold increased likelihood of cannabis use, compared with youth who had never been exposed to a traumatic event. Increased stress load also was associated with worse cognitive performance on tests of executive functioning, social cognition, and complex reasoning.
A history of assaultive trauma – being badly beaten, threatened with a weapon, or sexually abused – was associated with more severe psychopathology than in subjects with a history of nonassaultive traumatic events (Psychol Med. 2018 Apr 15:1-10).
Session moderator Carmen Moreno, MD, a child and adolescent psychiatrist at Gregorio Marañón University Hospital in Madrid, commented, “It was striking to me that the prevalence of childhood traumatic events was so high in a pediatric community sample. Is the measure the investigators chose the right measure?”
Dr. Castro-Fornieles replied that it was a very sensitive measure, in that an event many would consider part of normal life – for example, seeing a relative’s body on display in a funeral home – was scored as a traumatic exposure.
“Only one exposure is not that important,” she said. “The impact increases as you increase the number of traumatic events. And also the assaultive ones.”
Sexual abuse leaves a fingerprint
Investigators at Leiden (the Netherlands) University performed neuroimaging that looked at numerous brain regions of interest in 21 adolescents with childhood sexual abuse–related PTSD and 25 matched healthy controls. The standout finding was that the dorsal gray matter volume of the anterior cingulate cortex was significantly smaller in the teens with PTSD and a history of childhood sexual abuse (Eur Neuropsychopharmacol. 2017 Nov;27[11]:1163-71).
The investigators wanted a pure sample of patients with PTSD after childhood sexual abuse, so they excluded individuals who had experienced childhood sexual abuse and had a diagnosis of attention-deficit/hyperactivity disorder, oppositional defiant disorder, obsessive-compulsive disorder, conduct disorder, pervasive developmental disorder, bipolar disorder, or a psychotic disorder. That is both a strength and a limitation of the study, in Dr. Castro-Fornieles’ view.
“To me, that excludes too many of the children we see in our clinical settings. This work needs to be corroborated in a bigger sample, including patients with other diagnoses,” she said.
She reported having no financial conflicts regarding her presentation.
BARCELONA – Prenatal exposure to selective serotonin reuptake inhibitors late in pregnancy was associated with a significantly increased risk of anxious and/or depressed behaviors at 5 years of age in the prospective Norwegian Mother and Child Cohort Study.
Other than that specific red flag, however, the outcomes of in utero exposure to maternal SSRIs were reassuringly benign. Prenatal exposure during early- or mid-pregnancy was not associated with increased risk of anxious/depressed behaviors, compared with nonexposure; that adverse effect was restricted to exposure at week 29 of pregnancy or later. Nor did in utero exposure to maternal SSRIs during any time in pregnancy pose an increased risk for pediatric externalizing, emotional, or social problems in this observational study of 8,359 Norwegian mother-child dyads, Josefina Castro-Fornieles, MD, PhD, observed at the annual congress of the European College of Neuropsychopharmacology.
The huge Norwegian study was among what she considers the four most important studies in child/adolescent psychiatry published through the first three quarters of 2018. The others she highlighted were a large longitudinal observational study that demonstrated that persistent maternal postnatal depression was strongly associated with a variety of pediatric behavioral disturbances documented during assessments at ages 3.5, 16, and 18 years; a Philadelphia study showing that multiple traumatic stressful events or any assaultive trauma experienced by children or adolescents were independently associated with significant psychopathology and neurocognitive deficits; and a Dutch brain MRI study that pinpointed a reduction in gray matter volume in the anterior cingulate cortex as a potential key mediator of the neurobiologic aftereffects of childhood sexual abuse.
She selected those studies because they shared a common theme, one that constituted her key take-home message: “When recording antecedents during a clinical assessment, both with adults and children, it is clear that we have to ask in a more detailed way – using validated scales and interviews if possible – about the mother’s prenatal problems, including psychopharmacological treatment. That is something we often don’t do in a sufficiently detailed way in our clinical practice. And it’s also important to ask about life events; abuse during childhood and adolescence can be really important. We can modulate our treatment depending upon whether there is an influence of any of these aspects,” said Dr. Castro-Fornieles, director of the Clinical Institute of Neuroscience at the Hospital Clinic of Barcelona and a recent past-president of the Spanish Society for Child and Adolescent Psychiatry.
The following are her Top 4 studies:
The Norwegian Mother and Child Cohort Study
The increased risk of anxious and/or depressed behaviors in children exposed to selective serotonin reuptake inhibitors (SSRIs) late in pregnancy did not emerge until the year-5 assessment; it wasn’t evident at the 1.5- or 3-year evaluations.
The investigators emphasized a key lesson from their study: The importance of following children with late-pregnancy exposure to maternal SSRI therapy for development of symptoms of anxiety and/or depression (J Am Acad Child Adolesc Psychiatry. 2018 Mar;57[3]:200-8). Dr. Castro-Fornieles strongly endorsed that recommendation. However, she noted what she considers an important limitation to the study: even though the University of Oslo investigators adjusted for numerous potential confounders in their risk models – including maternal body mass index, parity, education, smoking, substance use, breastfeeding, folic acid use, and other medications used during pregnancy – it’s not possible in a study such as this to control for genetic and environmental risk factors, which she suspects also were at work.
The Avon Longitudinal Study of Parents and Children in the United Kingdom
Maternal postnatal depression is common, affecting roughly 10% of mothers. But it is not invariably associated with adverse mental health outcomes in their children. This study of nearly 10,000 mothers and their children sought to identify which children were at most risk. Using the Edinburgh Postnatal Depression Scale, the international team of investigators categorized maternal postnatal depression as moderate, marked, or severe. The affective disorder was deemed persistent if scores on the Edinburgh scale were elevated at both 2 and 8 months after delivery.
Postnatal depression, whether persistent or not, was associated with roughly a 2- to 2.4-fold increase for child behavioral disturbances when assessed at age 3.5 years using the Rutter Total Problems Scale. But postnatal depression that was persistent was the real difference maker: It carried a much higher risk of adverse behavioral outcomes and cognitive deficits than did the nonpersistent version. Indeed, persistent severe postnatal depression was associated a 4.8-fold increased risk of behavioral problems at age 3.5 years, a 2.65-fold greater risk of markedly lower grades in mathematics at age 16 years, and a 7.4-fold increased prevalence of depression at 18 years of age. The investigators advised screening mothers during the first postpartum year in order to identify those with persistent postpartum depression (JAMA Psychiatry. 2018 Mar 1;75[3]:247-53).
Dr. Castro-Fornieles said an important shortcoming of the Avon study was that it did not record paternal data.
“The study didn’t consider depression or other functional measures in the father, his commitment to childrearing, and whether the family was together or divorced. I feel this is an important limitation in many studies. For me, it’s really important to consider what’s happening with the fathers,” she said.
Traumatic stress load, psychopathology, and cognition
An eye-opening report from the Philadelphia Neurodevelopmental Cohort documented a surprisingly high level of lifetime exposure to traumatic events among 9,498 youth aged 8-21 years, and the stepwise manner by which a greater traumatic stress load was associated with increasing severity of psychopathology and cognitive deficits. Notably, the study participants were recruited from general pediatric clinics in the Children’s Hospital of Philadelphia health care network; they were not patients seeking psychiatric help. And yet, extensive structured psychiatric evaluation showed that 23% of them had a history of one traumatic stressful event, 12% had two, and 1% had three or more.
In analyses adjusted for lifetime history of depression or PTSD, a higher traumatic event load was associated with increased risk of externalizing behaviors, mood/anxiety disorders, psychosis spectrum, and fear. Moreover, a high trauma stress load was associated with a 5.3-fold increased risk of suicidal thoughts and a 3.2-fold increased likelihood of cannabis use, compared with youth who had never been exposed to a traumatic event. Increased stress load also was associated with worse cognitive performance on tests of executive functioning, social cognition, and complex reasoning.
A history of assaultive trauma – being badly beaten, threatened with a weapon, or sexually abused – was associated with more severe psychopathology than in subjects with a history of nonassaultive traumatic events (Psychol Med. 2018 Apr 15:1-10).
Session moderator Carmen Moreno, MD, a child and adolescent psychiatrist at Gregorio Marañón University Hospital in Madrid, commented, “It was striking to me that the prevalence of childhood traumatic events was so high in a pediatric community sample. Is the measure the investigators chose the right measure?”
Dr. Castro-Fornieles replied that it was a very sensitive measure, in that an event many would consider part of normal life – for example, seeing a relative’s body on display in a funeral home – was scored as a traumatic exposure.
“Only one exposure is not that important,” she said. “The impact increases as you increase the number of traumatic events. And also the assaultive ones.”
Sexual abuse leaves a fingerprint
Investigators at Leiden (the Netherlands) University performed neuroimaging that looked at numerous brain regions of interest in 21 adolescents with childhood sexual abuse–related PTSD and 25 matched healthy controls. The standout finding was that the dorsal gray matter volume of the anterior cingulate cortex was significantly smaller in the teens with PTSD and a history of childhood sexual abuse (Eur Neuropsychopharmacol. 2017 Nov;27[11]:1163-71).
The investigators wanted a pure sample of patients with PTSD after childhood sexual abuse, so they excluded individuals who had experienced childhood sexual abuse and had a diagnosis of attention-deficit/hyperactivity disorder, oppositional defiant disorder, obsessive-compulsive disorder, conduct disorder, pervasive developmental disorder, bipolar disorder, or a psychotic disorder. That is both a strength and a limitation of the study, in Dr. Castro-Fornieles’ view.
“To me, that excludes too many of the children we see in our clinical settings. This work needs to be corroborated in a bigger sample, including patients with other diagnoses,” she said.
She reported having no financial conflicts regarding her presentation.
BARCELONA – Prenatal exposure to selective serotonin reuptake inhibitors late in pregnancy was associated with a significantly increased risk of anxious and/or depressed behaviors at 5 years of age in the prospective Norwegian Mother and Child Cohort Study.
Other than that specific red flag, however, the outcomes of in utero exposure to maternal SSRIs were reassuringly benign. Prenatal exposure during early- or mid-pregnancy was not associated with increased risk of anxious/depressed behaviors, compared with nonexposure; that adverse effect was restricted to exposure at week 29 of pregnancy or later. Nor did in utero exposure to maternal SSRIs during any time in pregnancy pose an increased risk for pediatric externalizing, emotional, or social problems in this observational study of 8,359 Norwegian mother-child dyads, Josefina Castro-Fornieles, MD, PhD, observed at the annual congress of the European College of Neuropsychopharmacology.
The huge Norwegian study was among what she considers the four most important studies in child/adolescent psychiatry published through the first three quarters of 2018. The others she highlighted were a large longitudinal observational study that demonstrated that persistent maternal postnatal depression was strongly associated with a variety of pediatric behavioral disturbances documented during assessments at ages 3.5, 16, and 18 years; a Philadelphia study showing that multiple traumatic stressful events or any assaultive trauma experienced by children or adolescents were independently associated with significant psychopathology and neurocognitive deficits; and a Dutch brain MRI study that pinpointed a reduction in gray matter volume in the anterior cingulate cortex as a potential key mediator of the neurobiologic aftereffects of childhood sexual abuse.
She selected those studies because they shared a common theme, one that constituted her key take-home message: “When recording antecedents during a clinical assessment, both with adults and children, it is clear that we have to ask in a more detailed way – using validated scales and interviews if possible – about the mother’s prenatal problems, including psychopharmacological treatment. That is something we often don’t do in a sufficiently detailed way in our clinical practice. And it’s also important to ask about life events; abuse during childhood and adolescence can be really important. We can modulate our treatment depending upon whether there is an influence of any of these aspects,” said Dr. Castro-Fornieles, director of the Clinical Institute of Neuroscience at the Hospital Clinic of Barcelona and a recent past-president of the Spanish Society for Child and Adolescent Psychiatry.
The following are her Top 4 studies:
The Norwegian Mother and Child Cohort Study
The increased risk of anxious and/or depressed behaviors in children exposed to selective serotonin reuptake inhibitors (SSRIs) late in pregnancy did not emerge until the year-5 assessment; it wasn’t evident at the 1.5- or 3-year evaluations.
The investigators emphasized a key lesson from their study: The importance of following children with late-pregnancy exposure to maternal SSRI therapy for development of symptoms of anxiety and/or depression (J Am Acad Child Adolesc Psychiatry. 2018 Mar;57[3]:200-8). Dr. Castro-Fornieles strongly endorsed that recommendation. However, she noted what she considers an important limitation to the study: even though the University of Oslo investigators adjusted for numerous potential confounders in their risk models – including maternal body mass index, parity, education, smoking, substance use, breastfeeding, folic acid use, and other medications used during pregnancy – it’s not possible in a study such as this to control for genetic and environmental risk factors, which she suspects also were at work.
The Avon Longitudinal Study of Parents and Children in the United Kingdom
Maternal postnatal depression is common, affecting roughly 10% of mothers. But it is not invariably associated with adverse mental health outcomes in their children. This study of nearly 10,000 mothers and their children sought to identify which children were at most risk. Using the Edinburgh Postnatal Depression Scale, the international team of investigators categorized maternal postnatal depression as moderate, marked, or severe. The affective disorder was deemed persistent if scores on the Edinburgh scale were elevated at both 2 and 8 months after delivery.
Postnatal depression, whether persistent or not, was associated with roughly a 2- to 2.4-fold increase for child behavioral disturbances when assessed at age 3.5 years using the Rutter Total Problems Scale. But postnatal depression that was persistent was the real difference maker: It carried a much higher risk of adverse behavioral outcomes and cognitive deficits than did the nonpersistent version. Indeed, persistent severe postnatal depression was associated a 4.8-fold increased risk of behavioral problems at age 3.5 years, a 2.65-fold greater risk of markedly lower grades in mathematics at age 16 years, and a 7.4-fold increased prevalence of depression at 18 years of age. The investigators advised screening mothers during the first postpartum year in order to identify those with persistent postpartum depression (JAMA Psychiatry. 2018 Mar 1;75[3]:247-53).
Dr. Castro-Fornieles said an important shortcoming of the Avon study was that it did not record paternal data.
“The study didn’t consider depression or other functional measures in the father, his commitment to childrearing, and whether the family was together or divorced. I feel this is an important limitation in many studies. For me, it’s really important to consider what’s happening with the fathers,” she said.
Traumatic stress load, psychopathology, and cognition
An eye-opening report from the Philadelphia Neurodevelopmental Cohort documented a surprisingly high level of lifetime exposure to traumatic events among 9,498 youth aged 8-21 years, and the stepwise manner by which a greater traumatic stress load was associated with increasing severity of psychopathology and cognitive deficits. Notably, the study participants were recruited from general pediatric clinics in the Children’s Hospital of Philadelphia health care network; they were not patients seeking psychiatric help. And yet, extensive structured psychiatric evaluation showed that 23% of them had a history of one traumatic stressful event, 12% had two, and 1% had three or more.
In analyses adjusted for lifetime history of depression or PTSD, a higher traumatic event load was associated with increased risk of externalizing behaviors, mood/anxiety disorders, psychosis spectrum, and fear. Moreover, a high trauma stress load was associated with a 5.3-fold increased risk of suicidal thoughts and a 3.2-fold increased likelihood of cannabis use, compared with youth who had never been exposed to a traumatic event. Increased stress load also was associated with worse cognitive performance on tests of executive functioning, social cognition, and complex reasoning.
A history of assaultive trauma – being badly beaten, threatened with a weapon, or sexually abused – was associated with more severe psychopathology than in subjects with a history of nonassaultive traumatic events (Psychol Med. 2018 Apr 15:1-10).
Session moderator Carmen Moreno, MD, a child and adolescent psychiatrist at Gregorio Marañón University Hospital in Madrid, commented, “It was striking to me that the prevalence of childhood traumatic events was so high in a pediatric community sample. Is the measure the investigators chose the right measure?”
Dr. Castro-Fornieles replied that it was a very sensitive measure, in that an event many would consider part of normal life – for example, seeing a relative’s body on display in a funeral home – was scored as a traumatic exposure.
“Only one exposure is not that important,” she said. “The impact increases as you increase the number of traumatic events. And also the assaultive ones.”
Sexual abuse leaves a fingerprint
Investigators at Leiden (the Netherlands) University performed neuroimaging that looked at numerous brain regions of interest in 21 adolescents with childhood sexual abuse–related PTSD and 25 matched healthy controls. The standout finding was that the dorsal gray matter volume of the anterior cingulate cortex was significantly smaller in the teens with PTSD and a history of childhood sexual abuse (Eur Neuropsychopharmacol. 2017 Nov;27[11]:1163-71).
The investigators wanted a pure sample of patients with PTSD after childhood sexual abuse, so they excluded individuals who had experienced childhood sexual abuse and had a diagnosis of attention-deficit/hyperactivity disorder, oppositional defiant disorder, obsessive-compulsive disorder, conduct disorder, pervasive developmental disorder, bipolar disorder, or a psychotic disorder. That is both a strength and a limitation of the study, in Dr. Castro-Fornieles’ view.
“To me, that excludes too many of the children we see in our clinical settings. This work needs to be corroborated in a bigger sample, including patients with other diagnoses,” she said.
She reported having no financial conflicts regarding her presentation.
REPORTING FROM THE ECNP CONGRESS
Brisk walking may decrease TKR risk in OA
CHICAGO – according to a new analysis of data from the National Institutes of Health-sponsored Osteoarthritis Initiative.

Whether walking increases or decreases the risk of structural deterioration and total knee replacement (TKR) in patients with knee osteoarthritis has been a controversial topic marked by conflicting data. That’s probably because prior studies haven’t taken into account walking intensity, Hiral Master said at the annual meeting of the American College of Rheumatology.
Ms. Master, a PhD candidate in physical therapy at the University of Delaware, Newark, presented a study of 1,854 patients with knee osteoarthritis who participated in the Osteoarthritis Initiative, all of whom had worn an accelerometer. This permitted calculation of time spent walking at various intensities. Subjects spent an average of 459 minutes per day not walking and 8 minutes walking at moderate to vigorous intensity, defined as a cadence of more than 100 steps per minute.
During 5 years of follow-up, the incidence of TKR was 6%. In this video interview, Ms. Master explains that patients who replaced 5 minutes of not walking with 5 minutes of brisk walking daily had an adjusted 14% reduction in the risk of TKR. A dose-response was evident, with more minutes of moderate to vigorous walking being associated with progressively larger reductions in the risk of this major surgery. Walking at a cadence of less than 100 steps per minute, regardless of duration, was nonprotective.
SOURCE: Master H et al. Arthritis Rheumatol. 2018;70(Suppl 10), Abstract 1166.
CHICAGO – according to a new analysis of data from the National Institutes of Health-sponsored Osteoarthritis Initiative.

Whether walking increases or decreases the risk of structural deterioration and total knee replacement (TKR) in patients with knee osteoarthritis has been a controversial topic marked by conflicting data. That’s probably because prior studies haven’t taken into account walking intensity, Hiral Master said at the annual meeting of the American College of Rheumatology.
Ms. Master, a PhD candidate in physical therapy at the University of Delaware, Newark, presented a study of 1,854 patients with knee osteoarthritis who participated in the Osteoarthritis Initiative, all of whom had worn an accelerometer. This permitted calculation of time spent walking at various intensities. Subjects spent an average of 459 minutes per day not walking and 8 minutes walking at moderate to vigorous intensity, defined as a cadence of more than 100 steps per minute.
During 5 years of follow-up, the incidence of TKR was 6%. In this video interview, Ms. Master explains that patients who replaced 5 minutes of not walking with 5 minutes of brisk walking daily had an adjusted 14% reduction in the risk of TKR. A dose-response was evident, with more minutes of moderate to vigorous walking being associated with progressively larger reductions in the risk of this major surgery. Walking at a cadence of less than 100 steps per minute, regardless of duration, was nonprotective.
SOURCE: Master H et al. Arthritis Rheumatol. 2018;70(Suppl 10), Abstract 1166.
CHICAGO – according to a new analysis of data from the National Institutes of Health-sponsored Osteoarthritis Initiative.

Whether walking increases or decreases the risk of structural deterioration and total knee replacement (TKR) in patients with knee osteoarthritis has been a controversial topic marked by conflicting data. That’s probably because prior studies haven’t taken into account walking intensity, Hiral Master said at the annual meeting of the American College of Rheumatology.
Ms. Master, a PhD candidate in physical therapy at the University of Delaware, Newark, presented a study of 1,854 patients with knee osteoarthritis who participated in the Osteoarthritis Initiative, all of whom had worn an accelerometer. This permitted calculation of time spent walking at various intensities. Subjects spent an average of 459 minutes per day not walking and 8 minutes walking at moderate to vigorous intensity, defined as a cadence of more than 100 steps per minute.
During 5 years of follow-up, the incidence of TKR was 6%. In this video interview, Ms. Master explains that patients who replaced 5 minutes of not walking with 5 minutes of brisk walking daily had an adjusted 14% reduction in the risk of TKR. A dose-response was evident, with more minutes of moderate to vigorous walking being associated with progressively larger reductions in the risk of this major surgery. Walking at a cadence of less than 100 steps per minute, regardless of duration, was nonprotective.
SOURCE: Master H et al. Arthritis Rheumatol. 2018;70(Suppl 10), Abstract 1166.
REPORTING FROM THE ACR ANNUAL MEETING
Antiphospholipid antibodies are surprisingly common in first-MI patients
CHICAGO – Patients with a first MI were nearly nine times more likely to have detectable IgG antiphospholipid antibodies than were matched controls in a cross-sectional cohort study, Elisabet Svenungsson, MD, PhD, reported at the annual meeting of the American College of Rheumatology.
Her case-control study included 805 Swedish patients tested for antiphospholipid antibodies 6-10 weeks after experiencing their first MI and an equal number of age-, sex-, and location-matched controls. Prior to their MIs, none of the patients had been diagnosed with antiphospholipid syndrome, which requires both positive antiphospholipid antibodies and a vascular thrombotic event or obstetric morbidity.
A positive test for IgG anti-cardiolipin antibody was present in 10.9% of the first-MI patients, compared with 0.9% of controls. Similarly, 10.4% of acute MI patients and 0.9% of controls were positive for anti-beta2-glycoprotein-1 antibodies. Most patients who tested positive for one were positive for both. Thus, it’s possible that IgG antiphospholipid antibody positivity is an important silent risk factor that’s present in 1 in 10 MI patients, according to Dr. Svenungsson, professor of rheumatology at the Karolinska Institute in Stockholm.
If these results are confirmed and expanded upon in additional studies, testing for antiphospholipid antibodies could become part of the routine care in patients with an acute MI. Those who test positive would meet the criteria for antiphospholipid syndrome and qualify for long-term oral anticoagulation to reduce their elevated risk of further vascular events, she explained in this video interview.
The study was published in Annals of Internal Medicine simultaneously with the presentation at the ACR annual meeting (Ann Int Med. 2018 Oct 23. doi: 10.7326/M18-2130).
SOURCE: Grosso G et al. Arthritis Rheumatol. 2018;70(Suppl 10): Abstract 855.
CHICAGO – Patients with a first MI were nearly nine times more likely to have detectable IgG antiphospholipid antibodies than were matched controls in a cross-sectional cohort study, Elisabet Svenungsson, MD, PhD, reported at the annual meeting of the American College of Rheumatology.
Her case-control study included 805 Swedish patients tested for antiphospholipid antibodies 6-10 weeks after experiencing their first MI and an equal number of age-, sex-, and location-matched controls. Prior to their MIs, none of the patients had been diagnosed with antiphospholipid syndrome, which requires both positive antiphospholipid antibodies and a vascular thrombotic event or obstetric morbidity.
A positive test for IgG anti-cardiolipin antibody was present in 10.9% of the first-MI patients, compared with 0.9% of controls. Similarly, 10.4% of acute MI patients and 0.9% of controls were positive for anti-beta2-glycoprotein-1 antibodies. Most patients who tested positive for one were positive for both. Thus, it’s possible that IgG antiphospholipid antibody positivity is an important silent risk factor that’s present in 1 in 10 MI patients, according to Dr. Svenungsson, professor of rheumatology at the Karolinska Institute in Stockholm.
If these results are confirmed and expanded upon in additional studies, testing for antiphospholipid antibodies could become part of the routine care in patients with an acute MI. Those who test positive would meet the criteria for antiphospholipid syndrome and qualify for long-term oral anticoagulation to reduce their elevated risk of further vascular events, she explained in this video interview.
The study was published in Annals of Internal Medicine simultaneously with the presentation at the ACR annual meeting (Ann Int Med. 2018 Oct 23. doi: 10.7326/M18-2130).
SOURCE: Grosso G et al. Arthritis Rheumatol. 2018;70(Suppl 10): Abstract 855.
CHICAGO – Patients with a first MI were nearly nine times more likely to have detectable IgG antiphospholipid antibodies than were matched controls in a cross-sectional cohort study, Elisabet Svenungsson, MD, PhD, reported at the annual meeting of the American College of Rheumatology.
Her case-control study included 805 Swedish patients tested for antiphospholipid antibodies 6-10 weeks after experiencing their first MI and an equal number of age-, sex-, and location-matched controls. Prior to their MIs, none of the patients had been diagnosed with antiphospholipid syndrome, which requires both positive antiphospholipid antibodies and a vascular thrombotic event or obstetric morbidity.
A positive test for IgG anti-cardiolipin antibody was present in 10.9% of the first-MI patients, compared with 0.9% of controls. Similarly, 10.4% of acute MI patients and 0.9% of controls were positive for anti-beta2-glycoprotein-1 antibodies. Most patients who tested positive for one were positive for both. Thus, it’s possible that IgG antiphospholipid antibody positivity is an important silent risk factor that’s present in 1 in 10 MI patients, according to Dr. Svenungsson, professor of rheumatology at the Karolinska Institute in Stockholm.
If these results are confirmed and expanded upon in additional studies, testing for antiphospholipid antibodies could become part of the routine care in patients with an acute MI. Those who test positive would meet the criteria for antiphospholipid syndrome and qualify for long-term oral anticoagulation to reduce their elevated risk of further vascular events, she explained in this video interview.
The study was published in Annals of Internal Medicine simultaneously with the presentation at the ACR annual meeting (Ann Int Med. 2018 Oct 23. doi: 10.7326/M18-2130).
SOURCE: Grosso G et al. Arthritis Rheumatol. 2018;70(Suppl 10): Abstract 855.
REPORTING FROM THE ACR ANNUAL MEETING
Primary care holds key to curbing early-onset colorectal cancer
ESTES PARK, CO – , said gastroenterologist Swati G. Patel, MD, at a conference on internal medicine sponsored by the University of Colorado.
The startling rise in the incidence of colorectal cancer (CRC) in younger individuals in recent decades has generated much media coverage and considerable public concern. Reliable national data document a steady decline in CRC incidence over the past several decades in every age group 50 years and older – but a steady rise in incidence in those under age 50.
“The overall decline in CRC incidence and mortality beginning in the mid-1980s is an extremely amazing success story in cancer prevention. But there is still substantial work to be done,” observed Dr. Patel, who directs the Gastrointestinal Cancer Risk and Prevention Center at the university and is a staff physician at the Denver Veterans Affairs Medical Center.
Toward that end, in May 2018 the American Cancer Society issued updated guidelines recommending that people at average risk for CRC should now start undergoing regular screening for the disease at age 45. Models show that starting at age 45 rather than 50 would result in a 6.2% boost in life-years gained and a 17% increase in colonoscopies (CA Cancer J Clin. 2018 Jul;68(4):250-281).
“A different clinical and pathological entity”
Compared to CRC with onset at age 50 or later, early-onset disease is more often symptomatic at presentation. It is also significantly more likely to be located in the left colon or rectum, have a mucinous or signet ring histology, and be Stage III or IV.
“The disease seems to be a different clinical and pathological entity in younger patients,” Dr. Patel said.
The incidence of CRC before age 50 increased by 51% from 1994 to 2014. Mortality due to early-onset CRC rose by 11% during 2005-2015. Up to 90% of cases of early-onset CRC are diagnosed in individuals in their 40s. At the current rate of increase, early-onset CRC is projected to account for 20% of all cases of CRC by the year 2030.
The steadily rising incidence of early-onset CRC can’t be explained away as being due to earlier detection through greater availability of colonoscopy, in Dr. Patel’s view.
Numerous hypotheses have been put forth regarding the etiology of the rise in early-onset CRC. Correlations have variously been noted with the obesity epidemic, red meat consumption, diabetes, metabolic syndrome, increased early childhood exposure to antibiotics with resultant changes in gut microbiota in recent decades, and atopy.
“These are all fascinating hypotheses that will take decades to answer,” she said. “But in the meantime, what can we do about it now?”
Vital role for primary care
It’s going to take time to unravel the etiologies of early-onset CRC, both genetic and non-genetic. In the interim, opportunities abound for prevention and earlier detection. These opportunities are most available to primary care clinicians, since they provide continuity of care and are best positioned to detect red flags for patients at high risk for hereditary cancers.
“This is a time when we should concentrate our efforts on picking the low-hanging fruit,” Dr. Patel advised. She explained that this will entail a three-pronged approach: doing a better job of promptly evaluating potential symptoms of CRC, casting a wider net in search of patients with a hereditary cancer syndrome, and initiating earlier screening, especially in high-risk patients – a category that she said should include all African-Americans.
Prompt evaluation of symptoms
In one major study, the average time from symptom onset – bleeding, unexplained abdominal pain, changes in bowel habits, and/or iron deficiency – to diagnosis of CRC was 217 days in those with early-onset CRC, compared with 29.5 days in patients age 50 or older.
This huge disparity in time to diagnosis occurs largely because physicians typically assume that scant blood present in the stool of younger patients is due to hemorrhoids. Also frequently overlooked is the fact that the presence of hemorrhoids on physical examination can obscure an upstream malignant lesion.
“The initial plan is often to treat assumed benign pathology and only if symptoms persist to consider other causes,” Dr. Patel noted. That practice, she said, has to change: “The tools that we rely on in the clinic for this particular complaint – history and physical examination – are just not as reliable as we need them to be.”
Assessing for increased genetic/familial risk
The best estimate is that 16%-25% of early-onset CRC may be due to a high- or moderate-penetrance genetic mutation. Another 35% or so of cases are associated with a positive family history for CRC without a defined genetic condition.
In a 2011 study a mere 1.2% of Americans carrying a Lynch mutation were aware of it. “I suspect today it’s still less than 10%. We’re still not doing a very good job of identifying high-risk patients,” Dr. Patel said.
The National Comprehensive Cancer Network has published a guideline for assessment of genetic/familial high risk for CRC, but it’s far too complex and detailed for practical use in a busy primary care practice, in her view.
“You don’t have to remember all the detailed branching algorithms and criteria in the NCCN guideline. I propose a gut check. Increased risk boils down to three key points: any patient with onset of advanced neoplasia before age 50, or a personal history of multiple cancers, whether synchronous or metachronous, or with a strong family history of cancer on one side of the family should be sent on for a detailed risk assessment,” she said.
Similarly, don’t sweat trying to remember all the types of cancer associated with Lynch syndrome.
“We’re learning that the true answer is that it could be any kind of cancer,” Dr. Patel said.
It’s worth bearing in mind, however, that just because a patient doesn’t have a positive family history doesn’t mean that a hereditary cancer syndrome can be ruled out. Incomplete penetrance is characteristic of all of these hereditary syndromes. Indeed, 2 out of 10 patients with Lynch syndrome will never develop CRC.
Multiple gastroenterology societies now recommend routine PCR screening of all colon cancers for microsatellite instability markers – the hallmark of Lynch syndrome tumors – even if the cancer occurs in an 88-year-old. And if the screen is positive, genetic testing is appropriate. The University of Colorado is among a growing number of medical centers that have implemented this policy.
Dr. Patel noted that the American Cancer Society characterized its start-screening-at-45 guideline for average-risk patients as “conditional” rather than a “strong” recommendation. She advised applying it without reservation – and in some instances even starting at age 40 – for three groups clearly at high risk for early-onset CRC: African Americans, patients with a family history of CRC, and those with a family history of advanced adenoma, such as a tubular adenoma, which if not removed has an 80% chance of progressing to cancer.
She reported having no financial conflicts regarding her presentation.
ESTES PARK, CO – , said gastroenterologist Swati G. Patel, MD, at a conference on internal medicine sponsored by the University of Colorado.
The startling rise in the incidence of colorectal cancer (CRC) in younger individuals in recent decades has generated much media coverage and considerable public concern. Reliable national data document a steady decline in CRC incidence over the past several decades in every age group 50 years and older – but a steady rise in incidence in those under age 50.
“The overall decline in CRC incidence and mortality beginning in the mid-1980s is an extremely amazing success story in cancer prevention. But there is still substantial work to be done,” observed Dr. Patel, who directs the Gastrointestinal Cancer Risk and Prevention Center at the university and is a staff physician at the Denver Veterans Affairs Medical Center.
Toward that end, in May 2018 the American Cancer Society issued updated guidelines recommending that people at average risk for CRC should now start undergoing regular screening for the disease at age 45. Models show that starting at age 45 rather than 50 would result in a 6.2% boost in life-years gained and a 17% increase in colonoscopies (CA Cancer J Clin. 2018 Jul;68(4):250-281).
“A different clinical and pathological entity”
Compared to CRC with onset at age 50 or later, early-onset disease is more often symptomatic at presentation. It is also significantly more likely to be located in the left colon or rectum, have a mucinous or signet ring histology, and be Stage III or IV.
“The disease seems to be a different clinical and pathological entity in younger patients,” Dr. Patel said.
The incidence of CRC before age 50 increased by 51% from 1994 to 2014. Mortality due to early-onset CRC rose by 11% during 2005-2015. Up to 90% of cases of early-onset CRC are diagnosed in individuals in their 40s. At the current rate of increase, early-onset CRC is projected to account for 20% of all cases of CRC by the year 2030.
The steadily rising incidence of early-onset CRC can’t be explained away as being due to earlier detection through greater availability of colonoscopy, in Dr. Patel’s view.
Numerous hypotheses have been put forth regarding the etiology of the rise in early-onset CRC. Correlations have variously been noted with the obesity epidemic, red meat consumption, diabetes, metabolic syndrome, increased early childhood exposure to antibiotics with resultant changes in gut microbiota in recent decades, and atopy.
“These are all fascinating hypotheses that will take decades to answer,” she said. “But in the meantime, what can we do about it now?”
Vital role for primary care
It’s going to take time to unravel the etiologies of early-onset CRC, both genetic and non-genetic. In the interim, opportunities abound for prevention and earlier detection. These opportunities are most available to primary care clinicians, since they provide continuity of care and are best positioned to detect red flags for patients at high risk for hereditary cancers.
“This is a time when we should concentrate our efforts on picking the low-hanging fruit,” Dr. Patel advised. She explained that this will entail a three-pronged approach: doing a better job of promptly evaluating potential symptoms of CRC, casting a wider net in search of patients with a hereditary cancer syndrome, and initiating earlier screening, especially in high-risk patients – a category that she said should include all African-Americans.
Prompt evaluation of symptoms
In one major study, the average time from symptom onset – bleeding, unexplained abdominal pain, changes in bowel habits, and/or iron deficiency – to diagnosis of CRC was 217 days in those with early-onset CRC, compared with 29.5 days in patients age 50 or older.
This huge disparity in time to diagnosis occurs largely because physicians typically assume that scant blood present in the stool of younger patients is due to hemorrhoids. Also frequently overlooked is the fact that the presence of hemorrhoids on physical examination can obscure an upstream malignant lesion.
“The initial plan is often to treat assumed benign pathology and only if symptoms persist to consider other causes,” Dr. Patel noted. That practice, she said, has to change: “The tools that we rely on in the clinic for this particular complaint – history and physical examination – are just not as reliable as we need them to be.”
Assessing for increased genetic/familial risk
The best estimate is that 16%-25% of early-onset CRC may be due to a high- or moderate-penetrance genetic mutation. Another 35% or so of cases are associated with a positive family history for CRC without a defined genetic condition.
In a 2011 study a mere 1.2% of Americans carrying a Lynch mutation were aware of it. “I suspect today it’s still less than 10%. We’re still not doing a very good job of identifying high-risk patients,” Dr. Patel said.
The National Comprehensive Cancer Network has published a guideline for assessment of genetic/familial high risk for CRC, but it’s far too complex and detailed for practical use in a busy primary care practice, in her view.
“You don’t have to remember all the detailed branching algorithms and criteria in the NCCN guideline. I propose a gut check. Increased risk boils down to three key points: any patient with onset of advanced neoplasia before age 50, or a personal history of multiple cancers, whether synchronous or metachronous, or with a strong family history of cancer on one side of the family should be sent on for a detailed risk assessment,” she said.
Similarly, don’t sweat trying to remember all the types of cancer associated with Lynch syndrome.
“We’re learning that the true answer is that it could be any kind of cancer,” Dr. Patel said.
It’s worth bearing in mind, however, that just because a patient doesn’t have a positive family history doesn’t mean that a hereditary cancer syndrome can be ruled out. Incomplete penetrance is characteristic of all of these hereditary syndromes. Indeed, 2 out of 10 patients with Lynch syndrome will never develop CRC.
Multiple gastroenterology societies now recommend routine PCR screening of all colon cancers for microsatellite instability markers – the hallmark of Lynch syndrome tumors – even if the cancer occurs in an 88-year-old. And if the screen is positive, genetic testing is appropriate. The University of Colorado is among a growing number of medical centers that have implemented this policy.
Dr. Patel noted that the American Cancer Society characterized its start-screening-at-45 guideline for average-risk patients as “conditional” rather than a “strong” recommendation. She advised applying it without reservation – and in some instances even starting at age 40 – for three groups clearly at high risk for early-onset CRC: African Americans, patients with a family history of CRC, and those with a family history of advanced adenoma, such as a tubular adenoma, which if not removed has an 80% chance of progressing to cancer.
She reported having no financial conflicts regarding her presentation.
ESTES PARK, CO – , said gastroenterologist Swati G. Patel, MD, at a conference on internal medicine sponsored by the University of Colorado.
The startling rise in the incidence of colorectal cancer (CRC) in younger individuals in recent decades has generated much media coverage and considerable public concern. Reliable national data document a steady decline in CRC incidence over the past several decades in every age group 50 years and older – but a steady rise in incidence in those under age 50.
“The overall decline in CRC incidence and mortality beginning in the mid-1980s is an extremely amazing success story in cancer prevention. But there is still substantial work to be done,” observed Dr. Patel, who directs the Gastrointestinal Cancer Risk and Prevention Center at the university and is a staff physician at the Denver Veterans Affairs Medical Center.
Toward that end, in May 2018 the American Cancer Society issued updated guidelines recommending that people at average risk for CRC should now start undergoing regular screening for the disease at age 45. Models show that starting at age 45 rather than 50 would result in a 6.2% boost in life-years gained and a 17% increase in colonoscopies (CA Cancer J Clin. 2018 Jul;68(4):250-281).
“A different clinical and pathological entity”
Compared to CRC with onset at age 50 or later, early-onset disease is more often symptomatic at presentation. It is also significantly more likely to be located in the left colon or rectum, have a mucinous or signet ring histology, and be Stage III or IV.
“The disease seems to be a different clinical and pathological entity in younger patients,” Dr. Patel said.
The incidence of CRC before age 50 increased by 51% from 1994 to 2014. Mortality due to early-onset CRC rose by 11% during 2005-2015. Up to 90% of cases of early-onset CRC are diagnosed in individuals in their 40s. At the current rate of increase, early-onset CRC is projected to account for 20% of all cases of CRC by the year 2030.
The steadily rising incidence of early-onset CRC can’t be explained away as being due to earlier detection through greater availability of colonoscopy, in Dr. Patel’s view.
Numerous hypotheses have been put forth regarding the etiology of the rise in early-onset CRC. Correlations have variously been noted with the obesity epidemic, red meat consumption, diabetes, metabolic syndrome, increased early childhood exposure to antibiotics with resultant changes in gut microbiota in recent decades, and atopy.
“These are all fascinating hypotheses that will take decades to answer,” she said. “But in the meantime, what can we do about it now?”
Vital role for primary care
It’s going to take time to unravel the etiologies of early-onset CRC, both genetic and non-genetic. In the interim, opportunities abound for prevention and earlier detection. These opportunities are most available to primary care clinicians, since they provide continuity of care and are best positioned to detect red flags for patients at high risk for hereditary cancers.
“This is a time when we should concentrate our efforts on picking the low-hanging fruit,” Dr. Patel advised. She explained that this will entail a three-pronged approach: doing a better job of promptly evaluating potential symptoms of CRC, casting a wider net in search of patients with a hereditary cancer syndrome, and initiating earlier screening, especially in high-risk patients – a category that she said should include all African-Americans.
Prompt evaluation of symptoms
In one major study, the average time from symptom onset – bleeding, unexplained abdominal pain, changes in bowel habits, and/or iron deficiency – to diagnosis of CRC was 217 days in those with early-onset CRC, compared with 29.5 days in patients age 50 or older.
This huge disparity in time to diagnosis occurs largely because physicians typically assume that scant blood present in the stool of younger patients is due to hemorrhoids. Also frequently overlooked is the fact that the presence of hemorrhoids on physical examination can obscure an upstream malignant lesion.
“The initial plan is often to treat assumed benign pathology and only if symptoms persist to consider other causes,” Dr. Patel noted. That practice, she said, has to change: “The tools that we rely on in the clinic for this particular complaint – history and physical examination – are just not as reliable as we need them to be.”
Assessing for increased genetic/familial risk
The best estimate is that 16%-25% of early-onset CRC may be due to a high- or moderate-penetrance genetic mutation. Another 35% or so of cases are associated with a positive family history for CRC without a defined genetic condition.
In a 2011 study a mere 1.2% of Americans carrying a Lynch mutation were aware of it. “I suspect today it’s still less than 10%. We’re still not doing a very good job of identifying high-risk patients,” Dr. Patel said.
The National Comprehensive Cancer Network has published a guideline for assessment of genetic/familial high risk for CRC, but it’s far too complex and detailed for practical use in a busy primary care practice, in her view.
“You don’t have to remember all the detailed branching algorithms and criteria in the NCCN guideline. I propose a gut check. Increased risk boils down to three key points: any patient with onset of advanced neoplasia before age 50, or a personal history of multiple cancers, whether synchronous or metachronous, or with a strong family history of cancer on one side of the family should be sent on for a detailed risk assessment,” she said.
Similarly, don’t sweat trying to remember all the types of cancer associated with Lynch syndrome.
“We’re learning that the true answer is that it could be any kind of cancer,” Dr. Patel said.
It’s worth bearing in mind, however, that just because a patient doesn’t have a positive family history doesn’t mean that a hereditary cancer syndrome can be ruled out. Incomplete penetrance is characteristic of all of these hereditary syndromes. Indeed, 2 out of 10 patients with Lynch syndrome will never develop CRC.
Multiple gastroenterology societies now recommend routine PCR screening of all colon cancers for microsatellite instability markers – the hallmark of Lynch syndrome tumors – even if the cancer occurs in an 88-year-old. And if the screen is positive, genetic testing is appropriate. The University of Colorado is among a growing number of medical centers that have implemented this policy.
Dr. Patel noted that the American Cancer Society characterized its start-screening-at-45 guideline for average-risk patients as “conditional” rather than a “strong” recommendation. She advised applying it without reservation – and in some instances even starting at age 40 – for three groups clearly at high risk for early-onset CRC: African Americans, patients with a family history of CRC, and those with a family history of advanced adenoma, such as a tubular adenoma, which if not removed has an 80% chance of progressing to cancer.
She reported having no financial conflicts regarding her presentation.
REPORTING FROM COLORADO IM
ACR readies first-ever guidelines on managing reproductive health in rheumatology
CHICAGO – Help is on the way for rheumatologists who may feel out of their depth regarding reproductive health issues in their patients.
for internal review in draft form. Lisa R. Sammaritano, MD, a leader of the expert panel that developed the evidence-based recommendations, shared highlights of the forthcoming guidelines at the annual meeting of the American College of Rheumatology.
“Our patients, fortunately, are pursuing pregnancy more often now than in years past. One of the key messages of the guidelines is that patients really do want to discuss these topics with their rheumatologist, even though that often does not happen now. What patients told us [in the guideline-development process] is their rheumatologist knows them better than their gynecologist or any of their other doctors because we have followed them for a long period of time and we understand their disease and their symptoms. They really want our input on questions about contraception, when to plan a pregnancy, and medication use,” said Dr. Sammaritano of the Hospital for Special Surgery and Cornell University in New York.
The guidelines were created over the course of a year and a half with extensive input from ob.gyns., as well as a patient panel. The project included a systematic review of more than 300 published studies in which guideline panelists attempt to find answers to an initial list of 370 questions. Dr. Sammaritano predicted that the guidelines will prove to be useful not only for rheumatologists, but for their colleagues in ob.gyn. as well. Just as rheumatologists likely haven’t kept up with the sea changes that have occurred in ob.gyn. since their medical school days, most ob.gyns. know little about rheumatic diseases.
“There’s room for education on both sides,” she observed in an interview. “I have had to write letters to gynecologists to get them to put my patients with antiphospholipid antibodies on a contraceptive that includes a progestin because the labeling says, ‘May increase risk of thrombosis.’ And yet if you look at the literature, most of the progestins do not increase the risk of thrombosis, even in patients who are already at increased risk because of a genetic prothrombotic abnormality. I practically had to sign my life away to get a gynecologist to put a progestin-containing IUD in my patient, whereas the risk of thrombosis to my patient with an unplanned pregnancy would have been 10-fold or 100-fold higher. Unplanned pregnancy is dangerous for patients with our diseases.”
And yet, she noted, half of all pregnancies in the United States are unplanned. Among women with rheumatic diseases, the proportion may well be even higher in light of their documented low rate of utilization of effective contraception.
A publication date for the guidelines won’t be set until the review is completed, but the plan is to issue three separate documents. One will address reproductive health outside of pregnancy, with key topics to include contraception, fertility preservation, menopause, and hormone replacement therapy. The second document will focus on pregnancy management, with special attention devoted to women with lupus or antiphospholipid antibodies because they are at particularly high risk of adverse pregnancy outcomes. The third document will be devoted to medications, covering issues including which medications can be continued during pregnancy and when to safely stop the ones that can’t. This section will address both maternal and paternal use of rheumatologic medications, the latter being a topic below the radar of ob.gyns.
The three medications whose paternal use in pregnancy generate the most questions in clinical practice are methotrexate, cyclophosphamide, and sulfasalazine.
“I cannot tell you how many times I’ve been asked whether male patients with rheumatic diseases need to stop their methotrexate before they plan to father a child – that’s been a big one. The answer is they don’t need to stop, but that’s a conditional recommendation because the product label still says to stop it 3 months before. But that’s based on theoretical concerns, and all the data support a lack of teratogenicity for men using methotrexate prior to and during pregnancy,” Dr. Sammaritano said.
Men on cyclophosphamide absolutely have to stop the drug 3 months before pregnancy because the drug causes DNA fragmentation in the sperm. Sulfasalazine is known to impair male fertility. The ACR guidelines will recommend that men continue the drug, but if pregnancy doesn’t occur within a reasonable time, then it’s appropriate to get a semen analysis rather than stopping sulfasalazine unnecessarily.
American College of Obstetricians and Gynecologists guidelines now recommend long-acting reversible contraception, including IUDs and progestin implants, as first-line contraception for all women. The ACR draft guidelines strongly recommend the same.
“That is new. The use of this form of contraception in women with rheumatic diseases is quite low. In general, our patients don’t use contraception as often as other women, and when they do, they don’t use effective contraception. There are many theories as to why that may be: perhaps it’s a focus on the more immediate issues of their rheumatic disease that doesn’t allow their rheumatologist to get to the point of discussing contraception,” according to Dr. Sammaritano.
Many rheumatologists will be pleasantly surprised to learn that the problem of increased risk of pelvic inflammatory disease associated with earlier-generation IUDs is no longer an issue with the current devices. And contrary to a misconception among some ob.gyns., autoimmune disease will not cause a woman to reject her IUD.
The ACR guidelines recommend continuing hydroxychloroquine in lupus patients during pregnancy – and considering starting the drug in those not already on it – because of strong evidence supporting both safety and benefit for mother and baby.
“We are recommending the use of low-dose aspirin for patients with lupus and antiphospholipid antibodies because those two conditions increase the risk for preeclampsia, and the ob.gyns. routinely use low-dose aspirin starting toward the end of the first trimester as preventive therapy. Large studies show that it reduces the risk,” she continued.
Dr. Sammaritano cautioned that the literature on the use of rheumatologic medications in pregnancy and breast feeding is generally weak – and in the case of the new oral small molecule JAK inhibitors, essentially nonexistent.
“A lot of our recommendations are conditional because we did not feel that the data support a strong recommendation. But you have to do something. As long as you communicate the idea that we’re doing the best we can with what information is available, I think patients will respond to that,” the rheumatologist said.
She reported having no financial conflicts regarding her presentation.
CHICAGO – Help is on the way for rheumatologists who may feel out of their depth regarding reproductive health issues in their patients.
for internal review in draft form. Lisa R. Sammaritano, MD, a leader of the expert panel that developed the evidence-based recommendations, shared highlights of the forthcoming guidelines at the annual meeting of the American College of Rheumatology.
“Our patients, fortunately, are pursuing pregnancy more often now than in years past. One of the key messages of the guidelines is that patients really do want to discuss these topics with their rheumatologist, even though that often does not happen now. What patients told us [in the guideline-development process] is their rheumatologist knows them better than their gynecologist or any of their other doctors because we have followed them for a long period of time and we understand their disease and their symptoms. They really want our input on questions about contraception, when to plan a pregnancy, and medication use,” said Dr. Sammaritano of the Hospital for Special Surgery and Cornell University in New York.
The guidelines were created over the course of a year and a half with extensive input from ob.gyns., as well as a patient panel. The project included a systematic review of more than 300 published studies in which guideline panelists attempt to find answers to an initial list of 370 questions. Dr. Sammaritano predicted that the guidelines will prove to be useful not only for rheumatologists, but for their colleagues in ob.gyn. as well. Just as rheumatologists likely haven’t kept up with the sea changes that have occurred in ob.gyn. since their medical school days, most ob.gyns. know little about rheumatic diseases.
“There’s room for education on both sides,” she observed in an interview. “I have had to write letters to gynecologists to get them to put my patients with antiphospholipid antibodies on a contraceptive that includes a progestin because the labeling says, ‘May increase risk of thrombosis.’ And yet if you look at the literature, most of the progestins do not increase the risk of thrombosis, even in patients who are already at increased risk because of a genetic prothrombotic abnormality. I practically had to sign my life away to get a gynecologist to put a progestin-containing IUD in my patient, whereas the risk of thrombosis to my patient with an unplanned pregnancy would have been 10-fold or 100-fold higher. Unplanned pregnancy is dangerous for patients with our diseases.”
And yet, she noted, half of all pregnancies in the United States are unplanned. Among women with rheumatic diseases, the proportion may well be even higher in light of their documented low rate of utilization of effective contraception.
A publication date for the guidelines won’t be set until the review is completed, but the plan is to issue three separate documents. One will address reproductive health outside of pregnancy, with key topics to include contraception, fertility preservation, menopause, and hormone replacement therapy. The second document will focus on pregnancy management, with special attention devoted to women with lupus or antiphospholipid antibodies because they are at particularly high risk of adverse pregnancy outcomes. The third document will be devoted to medications, covering issues including which medications can be continued during pregnancy and when to safely stop the ones that can’t. This section will address both maternal and paternal use of rheumatologic medications, the latter being a topic below the radar of ob.gyns.
The three medications whose paternal use in pregnancy generate the most questions in clinical practice are methotrexate, cyclophosphamide, and sulfasalazine.
“I cannot tell you how many times I’ve been asked whether male patients with rheumatic diseases need to stop their methotrexate before they plan to father a child – that’s been a big one. The answer is they don’t need to stop, but that’s a conditional recommendation because the product label still says to stop it 3 months before. But that’s based on theoretical concerns, and all the data support a lack of teratogenicity for men using methotrexate prior to and during pregnancy,” Dr. Sammaritano said.
Men on cyclophosphamide absolutely have to stop the drug 3 months before pregnancy because the drug causes DNA fragmentation in the sperm. Sulfasalazine is known to impair male fertility. The ACR guidelines will recommend that men continue the drug, but if pregnancy doesn’t occur within a reasonable time, then it’s appropriate to get a semen analysis rather than stopping sulfasalazine unnecessarily.
American College of Obstetricians and Gynecologists guidelines now recommend long-acting reversible contraception, including IUDs and progestin implants, as first-line contraception for all women. The ACR draft guidelines strongly recommend the same.
“That is new. The use of this form of contraception in women with rheumatic diseases is quite low. In general, our patients don’t use contraception as often as other women, and when they do, they don’t use effective contraception. There are many theories as to why that may be: perhaps it’s a focus on the more immediate issues of their rheumatic disease that doesn’t allow their rheumatologist to get to the point of discussing contraception,” according to Dr. Sammaritano.
Many rheumatologists will be pleasantly surprised to learn that the problem of increased risk of pelvic inflammatory disease associated with earlier-generation IUDs is no longer an issue with the current devices. And contrary to a misconception among some ob.gyns., autoimmune disease will not cause a woman to reject her IUD.
The ACR guidelines recommend continuing hydroxychloroquine in lupus patients during pregnancy – and considering starting the drug in those not already on it – because of strong evidence supporting both safety and benefit for mother and baby.
“We are recommending the use of low-dose aspirin for patients with lupus and antiphospholipid antibodies because those two conditions increase the risk for preeclampsia, and the ob.gyns. routinely use low-dose aspirin starting toward the end of the first trimester as preventive therapy. Large studies show that it reduces the risk,” she continued.
Dr. Sammaritano cautioned that the literature on the use of rheumatologic medications in pregnancy and breast feeding is generally weak – and in the case of the new oral small molecule JAK inhibitors, essentially nonexistent.
“A lot of our recommendations are conditional because we did not feel that the data support a strong recommendation. But you have to do something. As long as you communicate the idea that we’re doing the best we can with what information is available, I think patients will respond to that,” the rheumatologist said.
She reported having no financial conflicts regarding her presentation.
CHICAGO – Help is on the way for rheumatologists who may feel out of their depth regarding reproductive health issues in their patients.
for internal review in draft form. Lisa R. Sammaritano, MD, a leader of the expert panel that developed the evidence-based recommendations, shared highlights of the forthcoming guidelines at the annual meeting of the American College of Rheumatology.
“Our patients, fortunately, are pursuing pregnancy more often now than in years past. One of the key messages of the guidelines is that patients really do want to discuss these topics with their rheumatologist, even though that often does not happen now. What patients told us [in the guideline-development process] is their rheumatologist knows them better than their gynecologist or any of their other doctors because we have followed them for a long period of time and we understand their disease and their symptoms. They really want our input on questions about contraception, when to plan a pregnancy, and medication use,” said Dr. Sammaritano of the Hospital for Special Surgery and Cornell University in New York.
The guidelines were created over the course of a year and a half with extensive input from ob.gyns., as well as a patient panel. The project included a systematic review of more than 300 published studies in which guideline panelists attempt to find answers to an initial list of 370 questions. Dr. Sammaritano predicted that the guidelines will prove to be useful not only for rheumatologists, but for their colleagues in ob.gyn. as well. Just as rheumatologists likely haven’t kept up with the sea changes that have occurred in ob.gyn. since their medical school days, most ob.gyns. know little about rheumatic diseases.
“There’s room for education on both sides,” she observed in an interview. “I have had to write letters to gynecologists to get them to put my patients with antiphospholipid antibodies on a contraceptive that includes a progestin because the labeling says, ‘May increase risk of thrombosis.’ And yet if you look at the literature, most of the progestins do not increase the risk of thrombosis, even in patients who are already at increased risk because of a genetic prothrombotic abnormality. I practically had to sign my life away to get a gynecologist to put a progestin-containing IUD in my patient, whereas the risk of thrombosis to my patient with an unplanned pregnancy would have been 10-fold or 100-fold higher. Unplanned pregnancy is dangerous for patients with our diseases.”
And yet, she noted, half of all pregnancies in the United States are unplanned. Among women with rheumatic diseases, the proportion may well be even higher in light of their documented low rate of utilization of effective contraception.
A publication date for the guidelines won’t be set until the review is completed, but the plan is to issue three separate documents. One will address reproductive health outside of pregnancy, with key topics to include contraception, fertility preservation, menopause, and hormone replacement therapy. The second document will focus on pregnancy management, with special attention devoted to women with lupus or antiphospholipid antibodies because they are at particularly high risk of adverse pregnancy outcomes. The third document will be devoted to medications, covering issues including which medications can be continued during pregnancy and when to safely stop the ones that can’t. This section will address both maternal and paternal use of rheumatologic medications, the latter being a topic below the radar of ob.gyns.
The three medications whose paternal use in pregnancy generate the most questions in clinical practice are methotrexate, cyclophosphamide, and sulfasalazine.
“I cannot tell you how many times I’ve been asked whether male patients with rheumatic diseases need to stop their methotrexate before they plan to father a child – that’s been a big one. The answer is they don’t need to stop, but that’s a conditional recommendation because the product label still says to stop it 3 months before. But that’s based on theoretical concerns, and all the data support a lack of teratogenicity for men using methotrexate prior to and during pregnancy,” Dr. Sammaritano said.
Men on cyclophosphamide absolutely have to stop the drug 3 months before pregnancy because the drug causes DNA fragmentation in the sperm. Sulfasalazine is known to impair male fertility. The ACR guidelines will recommend that men continue the drug, but if pregnancy doesn’t occur within a reasonable time, then it’s appropriate to get a semen analysis rather than stopping sulfasalazine unnecessarily.
American College of Obstetricians and Gynecologists guidelines now recommend long-acting reversible contraception, including IUDs and progestin implants, as first-line contraception for all women. The ACR draft guidelines strongly recommend the same.
“That is new. The use of this form of contraception in women with rheumatic diseases is quite low. In general, our patients don’t use contraception as often as other women, and when they do, they don’t use effective contraception. There are many theories as to why that may be: perhaps it’s a focus on the more immediate issues of their rheumatic disease that doesn’t allow their rheumatologist to get to the point of discussing contraception,” according to Dr. Sammaritano.
Many rheumatologists will be pleasantly surprised to learn that the problem of increased risk of pelvic inflammatory disease associated with earlier-generation IUDs is no longer an issue with the current devices. And contrary to a misconception among some ob.gyns., autoimmune disease will not cause a woman to reject her IUD.
The ACR guidelines recommend continuing hydroxychloroquine in lupus patients during pregnancy – and considering starting the drug in those not already on it – because of strong evidence supporting both safety and benefit for mother and baby.
“We are recommending the use of low-dose aspirin for patients with lupus and antiphospholipid antibodies because those two conditions increase the risk for preeclampsia, and the ob.gyns. routinely use low-dose aspirin starting toward the end of the first trimester as preventive therapy. Large studies show that it reduces the risk,” she continued.
Dr. Sammaritano cautioned that the literature on the use of rheumatologic medications in pregnancy and breast feeding is generally weak – and in the case of the new oral small molecule JAK inhibitors, essentially nonexistent.
“A lot of our recommendations are conditional because we did not feel that the data support a strong recommendation. But you have to do something. As long as you communicate the idea that we’re doing the best we can with what information is available, I think patients will respond to that,” the rheumatologist said.
She reported having no financial conflicts regarding her presentation.
REPORTING FROM THE ACR ANNUAL MEETING