User login
MMF may increase risk of CNS lymphoma
A new study has linked the immunosuppressive drug mycophenolate mofetil (MMF) to an increased risk of central nervous system (CNS) lymphoma in solid organ transplant recipients.
However, the research also suggests that calcineurin inhibitors (CNIs), when given alone or in combination with MMF, may protect transplant recipients from CNS lymphoma.
Researchers reported these findings in Oncotarget.
“MMF remains one of the best current medications for immunosuppression that we have,” said study author Amy Duffield, MD, PhD, of The Johns Hopkins Medical Institutions in Baltimore, Maryland.
“But a better understanding of its association with CNS lymphoproliferative disease will be crucial to further improving patients’ transplant regimens based on all of the risks these patients face.”
Dr Duffield and her colleagues noted that lymphomas and leukemias are known to be complications of solid organ transplants, but these malignancies rarely start in the CNS.
Still, in recent years, clinicians have begun to notice a rise in primary CNS lymphoproliferative disorders among transplant recipients. The current study is thought to be the first large enough to identify a link between MMF and these tumors.
For this work, Dr Duffield and her colleagues analyzed information on 177 patients with post-transplant lymphoproliferative disorder (PTLD) who were seen at Johns Hopkins Hospital between 1986 and 2014.
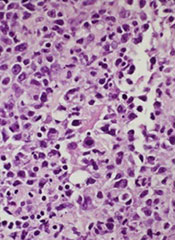
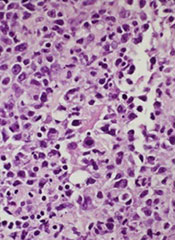
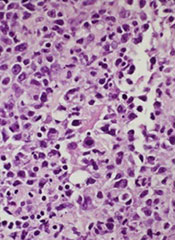
In that group, 29 patients—mostly kidney transplant recipients—were diagnosed with primary CNS lymphoproliferative disorders. The researchers said these were predominantly classified as monomorphic PTLD (72%), and most of the classifiable lymphomas were large B-cell lymphomas.
There were no cases of primary CNS PTLD diagnosed between 1986 and 1997, but the diagnosis increased markedly in the next decades.
The proportion of primary CNS PTLD cases compared to other PTLDs was 4.4-fold higher in the period from 2005 to 2014 than in the period from 1995 to 2004 (P<0.0001), even though the total number of PTLD cases remained relatively stable over time.
The researchers had prescription records on 16 of the patients who developed primary CNS lymphoproliferative disease.
Fifteen of the 16 patients had been taking MMF in the year prior to, or at the time of, their PTLD diagnosis. On the other hand, 37 of the 102 patients with PTLD outside the CNS had taken MMF (P<0.001).
The researchers also found that patients who took CNIs, either alone or in combination with MMF, seemed to be protected from developing primary CNS disease.
Primary CNS lymphoproliferative disease accounted for 66.7% of PTLDs among patients who took MMF but not a CNI (n=6), 23.9% of PTLDs among patients who took both an MMF and a CNI (n=46), and 1.7% of PTLDs among patients who took just a CNI (n=60).
The researchers found similar trends in a set of 6966 patients with PTLD. Those patients’ records were gleaned from an organ transplant database managed by the Organ Procurement and Transplantation Network and the United Network for Organ Sharing.
“More research needs to be done to confirm our results,” said Genevieve Crane, MD, PhD, of The Johns Hopkins Medical Institutions.
“But our work suggests that, at least in some patients, the combination of MMF and CNIs may be protective against CNS lymphoproliferative disease in a way that had not previously been appreciated.” ![]()
A new study has linked the immunosuppressive drug mycophenolate mofetil (MMF) to an increased risk of central nervous system (CNS) lymphoma in solid organ transplant recipients.
However, the research also suggests that calcineurin inhibitors (CNIs), when given alone or in combination with MMF, may protect transplant recipients from CNS lymphoma.
Researchers reported these findings in Oncotarget.
“MMF remains one of the best current medications for immunosuppression that we have,” said study author Amy Duffield, MD, PhD, of The Johns Hopkins Medical Institutions in Baltimore, Maryland.
“But a better understanding of its association with CNS lymphoproliferative disease will be crucial to further improving patients’ transplant regimens based on all of the risks these patients face.”
Dr Duffield and her colleagues noted that lymphomas and leukemias are known to be complications of solid organ transplants, but these malignancies rarely start in the CNS.
Still, in recent years, clinicians have begun to notice a rise in primary CNS lymphoproliferative disorders among transplant recipients. The current study is thought to be the first large enough to identify a link between MMF and these tumors.
For this work, Dr Duffield and her colleagues analyzed information on 177 patients with post-transplant lymphoproliferative disorder (PTLD) who were seen at Johns Hopkins Hospital between 1986 and 2014.
In that group, 29 patients—mostly kidney transplant recipients—were diagnosed with primary CNS lymphoproliferative disorders. The researchers said these were predominantly classified as monomorphic PTLD (72%), and most of the classifiable lymphomas were large B-cell lymphomas.
There were no cases of primary CNS PTLD diagnosed between 1986 and 1997, but the diagnosis increased markedly in the next decades.
The proportion of primary CNS PTLD cases compared to other PTLDs was 4.4-fold higher in the period from 2005 to 2014 than in the period from 1995 to 2004 (P<0.0001), even though the total number of PTLD cases remained relatively stable over time.
The researchers had prescription records on 16 of the patients who developed primary CNS lymphoproliferative disease.
Fifteen of the 16 patients had been taking MMF in the year prior to, or at the time of, their PTLD diagnosis. On the other hand, 37 of the 102 patients with PTLD outside the CNS had taken MMF (P<0.001).
The researchers also found that patients who took CNIs, either alone or in combination with MMF, seemed to be protected from developing primary CNS disease.
Primary CNS lymphoproliferative disease accounted for 66.7% of PTLDs among patients who took MMF but not a CNI (n=6), 23.9% of PTLDs among patients who took both an MMF and a CNI (n=46), and 1.7% of PTLDs among patients who took just a CNI (n=60).
The researchers found similar trends in a set of 6966 patients with PTLD. Those patients’ records were gleaned from an organ transplant database managed by the Organ Procurement and Transplantation Network and the United Network for Organ Sharing.
“More research needs to be done to confirm our results,” said Genevieve Crane, MD, PhD, of The Johns Hopkins Medical Institutions.
“But our work suggests that, at least in some patients, the combination of MMF and CNIs may be protective against CNS lymphoproliferative disease in a way that had not previously been appreciated.” ![]()
A new study has linked the immunosuppressive drug mycophenolate mofetil (MMF) to an increased risk of central nervous system (CNS) lymphoma in solid organ transplant recipients.
However, the research also suggests that calcineurin inhibitors (CNIs), when given alone or in combination with MMF, may protect transplant recipients from CNS lymphoma.
Researchers reported these findings in Oncotarget.
“MMF remains one of the best current medications for immunosuppression that we have,” said study author Amy Duffield, MD, PhD, of The Johns Hopkins Medical Institutions in Baltimore, Maryland.
“But a better understanding of its association with CNS lymphoproliferative disease will be crucial to further improving patients’ transplant regimens based on all of the risks these patients face.”
Dr Duffield and her colleagues noted that lymphomas and leukemias are known to be complications of solid organ transplants, but these malignancies rarely start in the CNS.
Still, in recent years, clinicians have begun to notice a rise in primary CNS lymphoproliferative disorders among transplant recipients. The current study is thought to be the first large enough to identify a link between MMF and these tumors.
For this work, Dr Duffield and her colleagues analyzed information on 177 patients with post-transplant lymphoproliferative disorder (PTLD) who were seen at Johns Hopkins Hospital between 1986 and 2014.
In that group, 29 patients—mostly kidney transplant recipients—were diagnosed with primary CNS lymphoproliferative disorders. The researchers said these were predominantly classified as monomorphic PTLD (72%), and most of the classifiable lymphomas were large B-cell lymphomas.
There were no cases of primary CNS PTLD diagnosed between 1986 and 1997, but the diagnosis increased markedly in the next decades.
The proportion of primary CNS PTLD cases compared to other PTLDs was 4.4-fold higher in the period from 2005 to 2014 than in the period from 1995 to 2004 (P<0.0001), even though the total number of PTLD cases remained relatively stable over time.
The researchers had prescription records on 16 of the patients who developed primary CNS lymphoproliferative disease.
Fifteen of the 16 patients had been taking MMF in the year prior to, or at the time of, their PTLD diagnosis. On the other hand, 37 of the 102 patients with PTLD outside the CNS had taken MMF (P<0.001).
The researchers also found that patients who took CNIs, either alone or in combination with MMF, seemed to be protected from developing primary CNS disease.
Primary CNS lymphoproliferative disease accounted for 66.7% of PTLDs among patients who took MMF but not a CNI (n=6), 23.9% of PTLDs among patients who took both an MMF and a CNI (n=46), and 1.7% of PTLDs among patients who took just a CNI (n=60).
The researchers found similar trends in a set of 6966 patients with PTLD. Those patients’ records were gleaned from an organ transplant database managed by the Organ Procurement and Transplantation Network and the United Network for Organ Sharing.
“More research needs to be done to confirm our results,” said Genevieve Crane, MD, PhD, of The Johns Hopkins Medical Institutions.
“But our work suggests that, at least in some patients, the combination of MMF and CNIs may be protective against CNS lymphoproliferative disease in a way that had not previously been appreciated.” ![]()
Malarial protein is basis for potential cancer therapy
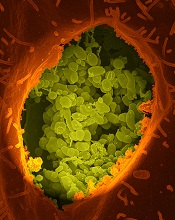
Photo by Vivian Sum
A protein expressed by the malaria parasite Plasmodium falciparum may prove useful for treating a range of cancers, according to research published in Cancer Cell.
This protein, VAR2CSA, binds a chondroitin sulfate (CS) that is found in placenta but is also present in many different cancer cells.
So investigators combined recombinant VAR2CSA (rVAR2) with 2 different toxins to create cancer-targeting treatments.
The treatments effectively targeted cancers in vitro and in vivo, impeding tumor growth and even eradicating cancer in some mice.
An idea is born
This research was born while the investigators were exploring why pregnant women are particularly susceptible to malaria. The team found that P falciparum produces VAR2CSA, which binds to a particular CS in the placenta, and that placenta-like CS (pl-CS) is found in most cancers.
This suggested the pl-CS could be a target for anticancer drugs, and VAR2CSA could provide the tool for carrying such drugs to tumors.
“Scientists have spent decades trying to find biochemical similarities between placenta tissue and cancer, but we just didn’t have the technology to find it,” said project leader Mads Daugaard, PhD, of the University of British Columbia in Vancouver, Canada.
“When my colleagues discovered how malaria uses VAR2CSA to embed itself in the placenta, we immediately saw its potential to deliver cancer drugs in a precise, controlled way to tumors.”
Testing rVAR2
After demonstrating that rVAR2 binds only to pl-CS, the investigators tested rVAR2 in patient-derived cancer cell lines of hematopoietic, epithelial, and mesenchymal origin. rVAR2 reacted with 95% (106/111) of these cell lines.
To determine whether rVAR2 could be used as a pl-CS-specific tumor-targeting system, the investigators fused the cytotoxic domain of diphtheria toxin (DT388) to rVAR2, creating a recombinant rDT388-VAR2 (rVAR2-DT) fusion protein.
The rVAR2-DT protein killed tumor cell lines of epithelial and mesenchymal origin, but it had no effect on normal primary human endothelial cells.
The investigators also tested rVAR2-DT in mouse models of prostate cancer and found that as few as 3 doses were enough to significantly inhibit tumor growth.
However, the team noted that clinical trials with DT fusions have shown that high drug concentrations are not well-tolerated.
So they chemically conjugated a hemiasterlin analog (KT886) to rVAR2 via a protease cleavable linker. The rVAR2-KT886 drug conjugate (VDC886) carried an average of 3 toxins per rVAR2 molecule.
The investigators tested VDC886 in 33 cancer cell lines and observed cytotoxicity in all cell lines.
So the team went on to test VDC886 in mouse models of non-Hodgkin lymphoma, prostate cancer, and metastatic breast cancer. VDC886 significantly inhibited tumor growth in all 3 models.
In mice with non-Hodgkin lymphoma, treated tumors were about a quarter the size of tumors in control mice. For the mice with prostate cancer, tumors completely disappeared in 2 of the 6 treated mice a month after they received the first dose of VDC886.
In mice with metastatic breast cancer, 5 of the 6 treated mice were cured and alive after almost 8 weeks. None of the control mice with metastatic breast cancer survived that long.
The investigators said they did not observe any adverse effects in the mice, and their organs were unharmed by the therapy.
“It appears that the malaria protein attaches itself to the tumor without any significant attachment to other tissue,” said Thomas Mandel Clausen, a PhD student at the University of Copenhagen in Denmark.
“And the mice that were given doses of protein and toxin showed far higher survival rates than the untreated mice. We have seen that 3 doses can arrest growth in a tumor and even make it shrink.”
Based on these results, 2 companies—Vancouver-based Kairos Therapeutics and Copenhagen-based VAR2 Pharmaceuticals—are developing the compound for clinical trials. The investigators believe this will take a few years. ![]()
Photo by Vivian Sum
A protein expressed by the malaria parasite Plasmodium falciparum may prove useful for treating a range of cancers, according to research published in Cancer Cell.
This protein, VAR2CSA, binds a chondroitin sulfate (CS) that is found in placenta but is also present in many different cancer cells.
So investigators combined recombinant VAR2CSA (rVAR2) with 2 different toxins to create cancer-targeting treatments.
The treatments effectively targeted cancers in vitro and in vivo, impeding tumor growth and even eradicating cancer in some mice.
An idea is born
This research was born while the investigators were exploring why pregnant women are particularly susceptible to malaria. The team found that P falciparum produces VAR2CSA, which binds to a particular CS in the placenta, and that placenta-like CS (pl-CS) is found in most cancers.
This suggested the pl-CS could be a target for anticancer drugs, and VAR2CSA could provide the tool for carrying such drugs to tumors.
“Scientists have spent decades trying to find biochemical similarities between placenta tissue and cancer, but we just didn’t have the technology to find it,” said project leader Mads Daugaard, PhD, of the University of British Columbia in Vancouver, Canada.
“When my colleagues discovered how malaria uses VAR2CSA to embed itself in the placenta, we immediately saw its potential to deliver cancer drugs in a precise, controlled way to tumors.”
Testing rVAR2
After demonstrating that rVAR2 binds only to pl-CS, the investigators tested rVAR2 in patient-derived cancer cell lines of hematopoietic, epithelial, and mesenchymal origin. rVAR2 reacted with 95% (106/111) of these cell lines.
To determine whether rVAR2 could be used as a pl-CS-specific tumor-targeting system, the investigators fused the cytotoxic domain of diphtheria toxin (DT388) to rVAR2, creating a recombinant rDT388-VAR2 (rVAR2-DT) fusion protein.
The rVAR2-DT protein killed tumor cell lines of epithelial and mesenchymal origin, but it had no effect on normal primary human endothelial cells.
The investigators also tested rVAR2-DT in mouse models of prostate cancer and found that as few as 3 doses were enough to significantly inhibit tumor growth.
However, the team noted that clinical trials with DT fusions have shown that high drug concentrations are not well-tolerated.
So they chemically conjugated a hemiasterlin analog (KT886) to rVAR2 via a protease cleavable linker. The rVAR2-KT886 drug conjugate (VDC886) carried an average of 3 toxins per rVAR2 molecule.
The investigators tested VDC886 in 33 cancer cell lines and observed cytotoxicity in all cell lines.
So the team went on to test VDC886 in mouse models of non-Hodgkin lymphoma, prostate cancer, and metastatic breast cancer. VDC886 significantly inhibited tumor growth in all 3 models.
In mice with non-Hodgkin lymphoma, treated tumors were about a quarter the size of tumors in control mice. For the mice with prostate cancer, tumors completely disappeared in 2 of the 6 treated mice a month after they received the first dose of VDC886.
In mice with metastatic breast cancer, 5 of the 6 treated mice were cured and alive after almost 8 weeks. None of the control mice with metastatic breast cancer survived that long.
The investigators said they did not observe any adverse effects in the mice, and their organs were unharmed by the therapy.
“It appears that the malaria protein attaches itself to the tumor without any significant attachment to other tissue,” said Thomas Mandel Clausen, a PhD student at the University of Copenhagen in Denmark.
“And the mice that were given doses of protein and toxin showed far higher survival rates than the untreated mice. We have seen that 3 doses can arrest growth in a tumor and even make it shrink.”
Based on these results, 2 companies—Vancouver-based Kairos Therapeutics and Copenhagen-based VAR2 Pharmaceuticals—are developing the compound for clinical trials. The investigators believe this will take a few years. ![]()
Photo by Vivian Sum
A protein expressed by the malaria parasite Plasmodium falciparum may prove useful for treating a range of cancers, according to research published in Cancer Cell.
This protein, VAR2CSA, binds a chondroitin sulfate (CS) that is found in placenta but is also present in many different cancer cells.
So investigators combined recombinant VAR2CSA (rVAR2) with 2 different toxins to create cancer-targeting treatments.
The treatments effectively targeted cancers in vitro and in vivo, impeding tumor growth and even eradicating cancer in some mice.
An idea is born
This research was born while the investigators were exploring why pregnant women are particularly susceptible to malaria. The team found that P falciparum produces VAR2CSA, which binds to a particular CS in the placenta, and that placenta-like CS (pl-CS) is found in most cancers.
This suggested the pl-CS could be a target for anticancer drugs, and VAR2CSA could provide the tool for carrying such drugs to tumors.
“Scientists have spent decades trying to find biochemical similarities between placenta tissue and cancer, but we just didn’t have the technology to find it,” said project leader Mads Daugaard, PhD, of the University of British Columbia in Vancouver, Canada.
“When my colleagues discovered how malaria uses VAR2CSA to embed itself in the placenta, we immediately saw its potential to deliver cancer drugs in a precise, controlled way to tumors.”
Testing rVAR2
After demonstrating that rVAR2 binds only to pl-CS, the investigators tested rVAR2 in patient-derived cancer cell lines of hematopoietic, epithelial, and mesenchymal origin. rVAR2 reacted with 95% (106/111) of these cell lines.
To determine whether rVAR2 could be used as a pl-CS-specific tumor-targeting system, the investigators fused the cytotoxic domain of diphtheria toxin (DT388) to rVAR2, creating a recombinant rDT388-VAR2 (rVAR2-DT) fusion protein.
The rVAR2-DT protein killed tumor cell lines of epithelial and mesenchymal origin, but it had no effect on normal primary human endothelial cells.
The investigators also tested rVAR2-DT in mouse models of prostate cancer and found that as few as 3 doses were enough to significantly inhibit tumor growth.
However, the team noted that clinical trials with DT fusions have shown that high drug concentrations are not well-tolerated.
So they chemically conjugated a hemiasterlin analog (KT886) to rVAR2 via a protease cleavable linker. The rVAR2-KT886 drug conjugate (VDC886) carried an average of 3 toxins per rVAR2 molecule.
The investigators tested VDC886 in 33 cancer cell lines and observed cytotoxicity in all cell lines.
So the team went on to test VDC886 in mouse models of non-Hodgkin lymphoma, prostate cancer, and metastatic breast cancer. VDC886 significantly inhibited tumor growth in all 3 models.
In mice with non-Hodgkin lymphoma, treated tumors were about a quarter the size of tumors in control mice. For the mice with prostate cancer, tumors completely disappeared in 2 of the 6 treated mice a month after they received the first dose of VDC886.
In mice with metastatic breast cancer, 5 of the 6 treated mice were cured and alive after almost 8 weeks. None of the control mice with metastatic breast cancer survived that long.
The investigators said they did not observe any adverse effects in the mice, and their organs were unharmed by the therapy.
“It appears that the malaria protein attaches itself to the tumor without any significant attachment to other tissue,” said Thomas Mandel Clausen, a PhD student at the University of Copenhagen in Denmark.
“And the mice that were given doses of protein and toxin showed far higher survival rates than the untreated mice. We have seen that 3 doses can arrest growth in a tumor and even make it shrink.”
Based on these results, 2 companies—Vancouver-based Kairos Therapeutics and Copenhagen-based VAR2 Pharmaceuticals—are developing the compound for clinical trials. The investigators believe this will take a few years. ![]()
Computerized cognitive training benefits childhood cancer survivors

Conklin and Jason Ashford
Photo courtesy of St. Jude
Children’s Research Hospital
and Peter Barta
Cognitive training presented as a video game can help improve cognitive skills in childhood cancer survivors (CCSs), new research suggests.
CCSs who completed 20 to 30 training sessions with this game experienced significant improvements in working memory, attention, and the speed at which their brains process information.
However, these improvements did not translate to improved math or reading performance.
Heather Conklin, PhD, of St. Jude Children’s Research Hospital in Memphis, Tennessee, and her colleagues conducted this research and described the results in the Journal of Clinical Oncology.
Study design
This study included 68 CCSs who had received cranial irradiation, intrathecal chemotherapy, or both for the treatment of acute lymphoblastic leukemia or brain tumors.
Participants were 8 to 16 years old, had completed treatment, and had been disease-free for at least a year. Prior to joining the study, all scored below expectations on measures of working memory.
The computerized intervention the CCSs used is called Cogmed (http://www.cogmed.com). It’s a working memory intervention that has previously demonstrated efficacy for individuals with developmental and acquired attention disorders as well as for healthy adults.
For this study, half the CCSs were randomized to begin using Cogmed immediately. The remaining survivors, who served as the control group, were given the opportunity to use Cogmed about 6 months later.
The CCSs assigned to Cogmed first were asked to complete 25 training sessions at home, along with weekly, telephone-based coaching. The training sessions lasted 30 to 45 minutes and included verbal and visual-spatial exercises that were presented as games and are designed to improve working memory.
CCSs who began training immediately underwent functional brain MRI before and soon after completing the intervention. The imaging tracked brain activity as the survivors completed a working memory exercise.
Results
CCSs who completed the intervention (n=30) showed greater improvements than controls on measures of working memory (P=0.002), attention (P=0.01), and processing speed (P=0.02).
The researchers said the benefits to working memory and attention were comparable to gains reported in previous studies of stimulant medications. And the gains from cognitive training moved the CCSs’ performance into the normal range.
Caregivers also reported significant improvement in the attention and executive functioning of CCSs who completed the training. (Executive functioning includes skills like planning and focus needed to juggle multiple tasks and get things done.)
“These results suggest that computerized cognitive training may help fill a void in management of cognitive late effects that impact quality of life for childhood cancer survivors, such as the likelihood they will complete school and live independently,” Dr Conklin said.
In addition, post-intervention brain imaging showed decreased activation of left lateral prefrontal and bilateral medial frontal areas.
“That suggests the intervention exercised and strengthened the well-established working memory network,” Dr Conklin said. “The implication is that the brain may operate more efficiently and have less need for compensatory strategies. Such training-induced neuroplasticity suggests the benefits might be sustained going forward.”
The researchers are now studying the possible benefits of starting brain training during treatment or combining it with other interventions. The team is also tracking whether the cognitive benefits are sustained and might eventually translate to the improved academic performance reported for other populations. ![]()

Conklin and Jason Ashford
Photo courtesy of St. Jude
Children’s Research Hospital
and Peter Barta
Cognitive training presented as a video game can help improve cognitive skills in childhood cancer survivors (CCSs), new research suggests.
CCSs who completed 20 to 30 training sessions with this game experienced significant improvements in working memory, attention, and the speed at which their brains process information.
However, these improvements did not translate to improved math or reading performance.
Heather Conklin, PhD, of St. Jude Children’s Research Hospital in Memphis, Tennessee, and her colleagues conducted this research and described the results in the Journal of Clinical Oncology.
Study design
This study included 68 CCSs who had received cranial irradiation, intrathecal chemotherapy, or both for the treatment of acute lymphoblastic leukemia or brain tumors.
Participants were 8 to 16 years old, had completed treatment, and had been disease-free for at least a year. Prior to joining the study, all scored below expectations on measures of working memory.
The computerized intervention the CCSs used is called Cogmed (http://www.cogmed.com). It’s a working memory intervention that has previously demonstrated efficacy for individuals with developmental and acquired attention disorders as well as for healthy adults.
For this study, half the CCSs were randomized to begin using Cogmed immediately. The remaining survivors, who served as the control group, were given the opportunity to use Cogmed about 6 months later.
The CCSs assigned to Cogmed first were asked to complete 25 training sessions at home, along with weekly, telephone-based coaching. The training sessions lasted 30 to 45 minutes and included verbal and visual-spatial exercises that were presented as games and are designed to improve working memory.
CCSs who began training immediately underwent functional brain MRI before and soon after completing the intervention. The imaging tracked brain activity as the survivors completed a working memory exercise.
Results
CCSs who completed the intervention (n=30) showed greater improvements than controls on measures of working memory (P=0.002), attention (P=0.01), and processing speed (P=0.02).
The researchers said the benefits to working memory and attention were comparable to gains reported in previous studies of stimulant medications. And the gains from cognitive training moved the CCSs’ performance into the normal range.
Caregivers also reported significant improvement in the attention and executive functioning of CCSs who completed the training. (Executive functioning includes skills like planning and focus needed to juggle multiple tasks and get things done.)
“These results suggest that computerized cognitive training may help fill a void in management of cognitive late effects that impact quality of life for childhood cancer survivors, such as the likelihood they will complete school and live independently,” Dr Conklin said.
In addition, post-intervention brain imaging showed decreased activation of left lateral prefrontal and bilateral medial frontal areas.
“That suggests the intervention exercised and strengthened the well-established working memory network,” Dr Conklin said. “The implication is that the brain may operate more efficiently and have less need for compensatory strategies. Such training-induced neuroplasticity suggests the benefits might be sustained going forward.”
The researchers are now studying the possible benefits of starting brain training during treatment or combining it with other interventions. The team is also tracking whether the cognitive benefits are sustained and might eventually translate to the improved academic performance reported for other populations. ![]()

Conklin and Jason Ashford
Photo courtesy of St. Jude
Children’s Research Hospital
and Peter Barta
Cognitive training presented as a video game can help improve cognitive skills in childhood cancer survivors (CCSs), new research suggests.
CCSs who completed 20 to 30 training sessions with this game experienced significant improvements in working memory, attention, and the speed at which their brains process information.
However, these improvements did not translate to improved math or reading performance.
Heather Conklin, PhD, of St. Jude Children’s Research Hospital in Memphis, Tennessee, and her colleagues conducted this research and described the results in the Journal of Clinical Oncology.
Study design
This study included 68 CCSs who had received cranial irradiation, intrathecal chemotherapy, or both for the treatment of acute lymphoblastic leukemia or brain tumors.
Participants were 8 to 16 years old, had completed treatment, and had been disease-free for at least a year. Prior to joining the study, all scored below expectations on measures of working memory.
The computerized intervention the CCSs used is called Cogmed (http://www.cogmed.com). It’s a working memory intervention that has previously demonstrated efficacy for individuals with developmental and acquired attention disorders as well as for healthy adults.
For this study, half the CCSs were randomized to begin using Cogmed immediately. The remaining survivors, who served as the control group, were given the opportunity to use Cogmed about 6 months later.
The CCSs assigned to Cogmed first were asked to complete 25 training sessions at home, along with weekly, telephone-based coaching. The training sessions lasted 30 to 45 minutes and included verbal and visual-spatial exercises that were presented as games and are designed to improve working memory.
CCSs who began training immediately underwent functional brain MRI before and soon after completing the intervention. The imaging tracked brain activity as the survivors completed a working memory exercise.
Results
CCSs who completed the intervention (n=30) showed greater improvements than controls on measures of working memory (P=0.002), attention (P=0.01), and processing speed (P=0.02).
The researchers said the benefits to working memory and attention were comparable to gains reported in previous studies of stimulant medications. And the gains from cognitive training moved the CCSs’ performance into the normal range.
Caregivers also reported significant improvement in the attention and executive functioning of CCSs who completed the training. (Executive functioning includes skills like planning and focus needed to juggle multiple tasks and get things done.)
“These results suggest that computerized cognitive training may help fill a void in management of cognitive late effects that impact quality of life for childhood cancer survivors, such as the likelihood they will complete school and live independently,” Dr Conklin said.
In addition, post-intervention brain imaging showed decreased activation of left lateral prefrontal and bilateral medial frontal areas.
“That suggests the intervention exercised and strengthened the well-established working memory network,” Dr Conklin said. “The implication is that the brain may operate more efficiently and have less need for compensatory strategies. Such training-induced neuroplasticity suggests the benefits might be sustained going forward.”
The researchers are now studying the possible benefits of starting brain training during treatment or combining it with other interventions. The team is also tracking whether the cognitive benefits are sustained and might eventually translate to the improved academic performance reported for other populations. ![]()
Targeting a protein to improve AML treatment

Photo courtesy of VCU
Massey Cancer Center
Preclinical experiments have shown that blocking production of the protein CHD4 may help increase the effectiveness of first-line treatments for acute myeloid leukemia (AML).
Researchers found that depleting AML cells of CHD4 makes them more susceptible to standard chemotherapeutic agents by reducing the cells’ ability to repair DNA damage.
Depleting CHD4 also decreased AML cells’ ability to form colonies in vitro and tumors in vivo.
On the other hand, CHD4 depletion did not have detrimental effects on healthy bone marrow cells. The cells were no more sensitive to chemotherapy, and their growth was not affected.
Researchers reported these results in Blood.
“We are very encouraged by these findings,” said study author Gordon Ginder, MD, of Virginia Commonwealth University in Richmond.
“Targeting the CHD4 protein could allow us to reduce chemotherapy doses, which could potentially mean more effective first- and second-line treatments with fewer serious side effects.”
CHD4 is involved in silencing tumor suppressor genes in cancer cells. Recently, it has been shown to play a role in repairing DNA damage.
With their experiments, Dr Ginder and his colleagues found that CHD4 depletion severely restricted the ability of AML cells to develop colonies in soft agar models and establish tumors in mouse models.
In addition, blocking the production of CHD4 rendered AML cells more sensitive to daunorubicin and cytarabine, both in vitro and in vivo.
“This study builds on our team’s efforts to understand the molecular processes through which epigenetic regulators impact gene expression,” Dr Ginder said.
“Future studies will attempt to uncover the detailed mechanism through which CHD4 decreases the ability of AML cells to initiate leukemia and will look for potential ways to target this important protein. The fact that it functions as an enzyme suggests it may be druggable.” ![]()

Photo courtesy of VCU
Massey Cancer Center
Preclinical experiments have shown that blocking production of the protein CHD4 may help increase the effectiveness of first-line treatments for acute myeloid leukemia (AML).
Researchers found that depleting AML cells of CHD4 makes them more susceptible to standard chemotherapeutic agents by reducing the cells’ ability to repair DNA damage.
Depleting CHD4 also decreased AML cells’ ability to form colonies in vitro and tumors in vivo.
On the other hand, CHD4 depletion did not have detrimental effects on healthy bone marrow cells. The cells were no more sensitive to chemotherapy, and their growth was not affected.
Researchers reported these results in Blood.
“We are very encouraged by these findings,” said study author Gordon Ginder, MD, of Virginia Commonwealth University in Richmond.
“Targeting the CHD4 protein could allow us to reduce chemotherapy doses, which could potentially mean more effective first- and second-line treatments with fewer serious side effects.”
CHD4 is involved in silencing tumor suppressor genes in cancer cells. Recently, it has been shown to play a role in repairing DNA damage.
With their experiments, Dr Ginder and his colleagues found that CHD4 depletion severely restricted the ability of AML cells to develop colonies in soft agar models and establish tumors in mouse models.
In addition, blocking the production of CHD4 rendered AML cells more sensitive to daunorubicin and cytarabine, both in vitro and in vivo.
“This study builds on our team’s efforts to understand the molecular processes through which epigenetic regulators impact gene expression,” Dr Ginder said.
“Future studies will attempt to uncover the detailed mechanism through which CHD4 decreases the ability of AML cells to initiate leukemia and will look for potential ways to target this important protein. The fact that it functions as an enzyme suggests it may be druggable.” ![]()

Photo courtesy of VCU
Massey Cancer Center
Preclinical experiments have shown that blocking production of the protein CHD4 may help increase the effectiveness of first-line treatments for acute myeloid leukemia (AML).
Researchers found that depleting AML cells of CHD4 makes them more susceptible to standard chemotherapeutic agents by reducing the cells’ ability to repair DNA damage.
Depleting CHD4 also decreased AML cells’ ability to form colonies in vitro and tumors in vivo.
On the other hand, CHD4 depletion did not have detrimental effects on healthy bone marrow cells. The cells were no more sensitive to chemotherapy, and their growth was not affected.
Researchers reported these results in Blood.
“We are very encouraged by these findings,” said study author Gordon Ginder, MD, of Virginia Commonwealth University in Richmond.
“Targeting the CHD4 protein could allow us to reduce chemotherapy doses, which could potentially mean more effective first- and second-line treatments with fewer serious side effects.”
CHD4 is involved in silencing tumor suppressor genes in cancer cells. Recently, it has been shown to play a role in repairing DNA damage.
With their experiments, Dr Ginder and his colleagues found that CHD4 depletion severely restricted the ability of AML cells to develop colonies in soft agar models and establish tumors in mouse models.
In addition, blocking the production of CHD4 rendered AML cells more sensitive to daunorubicin and cytarabine, both in vitro and in vivo.
“This study builds on our team’s efforts to understand the molecular processes through which epigenetic regulators impact gene expression,” Dr Ginder said.
“Future studies will attempt to uncover the detailed mechanism through which CHD4 decreases the ability of AML cells to initiate leukemia and will look for potential ways to target this important protein. The fact that it functions as an enzyme suggests it may be druggable.” ![]()
Donor’s lack of sleep may impact HSCT

Sleep-deprived mice make poor donors for hematopoietic stem cell transplants (HSCTs), according to a study published in Nature Communications.
The research showed that a sleep deficit of just 4 hours can reduce—by more than 50%—the ability of HSCs to engraft and reconstitute the blood and bone marrow of an irradiated recipient mouse.
Researchers believe these findings may also apply to humans.
“Considering how little attention we typically pay to sleep in the hospital setting, this finding is troubling,” said study author Asya Rolls, PhD, of Technion–Israel Institute of Technology in Haifa.
“We go to all this trouble to find a matching donor, but this research suggests that, if the donor is not well-rested, it can impact the outcome of the transplantation. However, it’s heartening to think that this is not an insurmountable obstacle. A short period of recovery sleep before transplant can restore the donor’s cells’ ability to function normally.”
Dr Rolls and her colleagues studied mice that had been gently handled for 4 hours to prevent them from sleeping while control mice dozed. The team then collected HSCs from the sleep-deprived and well-rested mice and injected the cells into 12 irradiated mice.
The recipient mice also received an injection of their own HSCs collected prior to radiation so the researchers could quantify the relative abilities of the donated HSCs to engraft successfully.
The team then assessed the prevalence of myeloid cells derived from donated HSCs at 8 weeks and 16 weeks after transplant. At 16 weeks, donor myeloid chimerism was about 26% in HSCT recipients with well-rested donors and about 12% in recipients with sleep-deprived donors (P<0.0001).
Dr Rolls and her colleagues also compared the ability of fluorescently labeled HSCs from sleep-deprived mice and rested mice to home to the bone marrow. After 12 hours, 3.3% percent of HSCs from rested mice were found in the bone marrow, compared to 1.7% of HSCs from sleep-deprived mice (P<0.05).
Further investigation revealed that sleep deprivation downregulates the expression of miR-19b, a negative regulator of the suppressor of cytokine signaling (SOCS) genes, which inhibit HSC migration and homing.
Finally, Dr Rolls and her colleagues found the effects of sleep deprivation on HSCs could be reversed by letting mice catch up on sleep. Even 2 hours of recovery sleep restored the HSCs’ ability to function normally in transplantation tests.
“We still don’t know how sleep deprivation affects us all, not just bone marrow donors,” Dr Rolls said. “The fact that recovery sleep is so helpful only emphasizes how important it is to pay attention to sleep.” ![]()

Sleep-deprived mice make poor donors for hematopoietic stem cell transplants (HSCTs), according to a study published in Nature Communications.
The research showed that a sleep deficit of just 4 hours can reduce—by more than 50%—the ability of HSCs to engraft and reconstitute the blood and bone marrow of an irradiated recipient mouse.
Researchers believe these findings may also apply to humans.
“Considering how little attention we typically pay to sleep in the hospital setting, this finding is troubling,” said study author Asya Rolls, PhD, of Technion–Israel Institute of Technology in Haifa.
“We go to all this trouble to find a matching donor, but this research suggests that, if the donor is not well-rested, it can impact the outcome of the transplantation. However, it’s heartening to think that this is not an insurmountable obstacle. A short period of recovery sleep before transplant can restore the donor’s cells’ ability to function normally.”
Dr Rolls and her colleagues studied mice that had been gently handled for 4 hours to prevent them from sleeping while control mice dozed. The team then collected HSCs from the sleep-deprived and well-rested mice and injected the cells into 12 irradiated mice.
The recipient mice also received an injection of their own HSCs collected prior to radiation so the researchers could quantify the relative abilities of the donated HSCs to engraft successfully.
The team then assessed the prevalence of myeloid cells derived from donated HSCs at 8 weeks and 16 weeks after transplant. At 16 weeks, donor myeloid chimerism was about 26% in HSCT recipients with well-rested donors and about 12% in recipients with sleep-deprived donors (P<0.0001).
Dr Rolls and her colleagues also compared the ability of fluorescently labeled HSCs from sleep-deprived mice and rested mice to home to the bone marrow. After 12 hours, 3.3% percent of HSCs from rested mice were found in the bone marrow, compared to 1.7% of HSCs from sleep-deprived mice (P<0.05).
Further investigation revealed that sleep deprivation downregulates the expression of miR-19b, a negative regulator of the suppressor of cytokine signaling (SOCS) genes, which inhibit HSC migration and homing.
Finally, Dr Rolls and her colleagues found the effects of sleep deprivation on HSCs could be reversed by letting mice catch up on sleep. Even 2 hours of recovery sleep restored the HSCs’ ability to function normally in transplantation tests.
“We still don’t know how sleep deprivation affects us all, not just bone marrow donors,” Dr Rolls said. “The fact that recovery sleep is so helpful only emphasizes how important it is to pay attention to sleep.” ![]()

Sleep-deprived mice make poor donors for hematopoietic stem cell transplants (HSCTs), according to a study published in Nature Communications.
The research showed that a sleep deficit of just 4 hours can reduce—by more than 50%—the ability of HSCs to engraft and reconstitute the blood and bone marrow of an irradiated recipient mouse.
Researchers believe these findings may also apply to humans.
“Considering how little attention we typically pay to sleep in the hospital setting, this finding is troubling,” said study author Asya Rolls, PhD, of Technion–Israel Institute of Technology in Haifa.
“We go to all this trouble to find a matching donor, but this research suggests that, if the donor is not well-rested, it can impact the outcome of the transplantation. However, it’s heartening to think that this is not an insurmountable obstacle. A short period of recovery sleep before transplant can restore the donor’s cells’ ability to function normally.”
Dr Rolls and her colleagues studied mice that had been gently handled for 4 hours to prevent them from sleeping while control mice dozed. The team then collected HSCs from the sleep-deprived and well-rested mice and injected the cells into 12 irradiated mice.
The recipient mice also received an injection of their own HSCs collected prior to radiation so the researchers could quantify the relative abilities of the donated HSCs to engraft successfully.
The team then assessed the prevalence of myeloid cells derived from donated HSCs at 8 weeks and 16 weeks after transplant. At 16 weeks, donor myeloid chimerism was about 26% in HSCT recipients with well-rested donors and about 12% in recipients with sleep-deprived donors (P<0.0001).
Dr Rolls and her colleagues also compared the ability of fluorescently labeled HSCs from sleep-deprived mice and rested mice to home to the bone marrow. After 12 hours, 3.3% percent of HSCs from rested mice were found in the bone marrow, compared to 1.7% of HSCs from sleep-deprived mice (P<0.05).
Further investigation revealed that sleep deprivation downregulates the expression of miR-19b, a negative regulator of the suppressor of cytokine signaling (SOCS) genes, which inhibit HSC migration and homing.
Finally, Dr Rolls and her colleagues found the effects of sleep deprivation on HSCs could be reversed by letting mice catch up on sleep. Even 2 hours of recovery sleep restored the HSCs’ ability to function normally in transplantation tests.
“We still don’t know how sleep deprivation affects us all, not just bone marrow donors,” Dr Rolls said. “The fact that recovery sleep is so helpful only emphasizes how important it is to pay attention to sleep.” ![]()
Bacterium may increase risk of DLBCL, FL
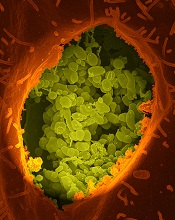
Coxiella burnetii
Image courtesy of NIAID
The bacterium that causes Q fever may confer an increased risk of diffuse large B-cell lymphoma (DLBCL) and follicular lymphoma (FL), according to a study published in Blood.
Q fever is an infectious disease caused by Coxiella burnetii, a bacterium primarily transmitted through the excrements of cattle, sheep, and goats.
Because some patients with Q fever develop lymphoma, researchers believed the malignancy could be a risk factor for Q fever.
However, the experience of 1 patient prompted a group of researchers in France to consider the opposite—that the infection might cause the lymphoma.
“During a follow-up scan in a patient we had successfully treated for Q fever, we observed a tumor close to the location of the previous infection,” said study author Didier Raoult, MD, PhD, of Aix-Marseille University in Marseille, France.
“The discovery that it was a lymphoma tumor containing C burnetii encouraged us to consider that the infection might have contributed to the development of the cancer.”
To better understand the association between C burnetii and lymphoma, Dr Raoult and his colleagues screened 1468 patients treated at the French National Referral Center for Q Fever from 2004 to 2014.
The researchers imaged patient tissue samples and identified 7 people, including the initial patient, who developed lymphoma after C burnetii infection. Six patients were diagnosed with DLBCL and 1 with FL.
To determine if patients with Q fever have a higher risk of lymphoma than the general population, the researchers compared the incidence of lymphoma in the Q fever registry to the incidence reported in France’s general population.
This revealed an excess risk of DLBCL and FL in the Q fever population, with standardized incidence ratios of 25.4 for DLBCL and 6.7 for FL.
In addition, the odds of developing lymphoma were higher in patients with persistent, concentrated infections than in those with other forms of Q fever. The hazard ratio for patients with persistent, concentrated infection was 9.35.
Finally, the researchers observed interleukin-10 overproduction in Q fever patients with lymphoma. The team said this suggests that suppression of the immune system may have allowed the lymphoma cells to evade immune detection and multiply.
“As we continue to learn more about the association between C burnetii and lymphoma, these results should encourage clinicians to survey high-risk patients as early as possible for potential cancer,” Dr Raoult said.
“Ultimately, this early diagnosis and treatment would improve outcomes for Q fever patients who subsequently develop lymphoma, particularly those with B-cell non-Hodgkin lymphoma.” ![]()
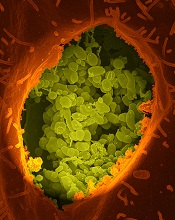
Coxiella burnetii
Image courtesy of NIAID
The bacterium that causes Q fever may confer an increased risk of diffuse large B-cell lymphoma (DLBCL) and follicular lymphoma (FL), according to a study published in Blood.
Q fever is an infectious disease caused by Coxiella burnetii, a bacterium primarily transmitted through the excrements of cattle, sheep, and goats.
Because some patients with Q fever develop lymphoma, researchers believed the malignancy could be a risk factor for Q fever.
However, the experience of 1 patient prompted a group of researchers in France to consider the opposite—that the infection might cause the lymphoma.
“During a follow-up scan in a patient we had successfully treated for Q fever, we observed a tumor close to the location of the previous infection,” said study author Didier Raoult, MD, PhD, of Aix-Marseille University in Marseille, France.
“The discovery that it was a lymphoma tumor containing C burnetii encouraged us to consider that the infection might have contributed to the development of the cancer.”
To better understand the association between C burnetii and lymphoma, Dr Raoult and his colleagues screened 1468 patients treated at the French National Referral Center for Q Fever from 2004 to 2014.
The researchers imaged patient tissue samples and identified 7 people, including the initial patient, who developed lymphoma after C burnetii infection. Six patients were diagnosed with DLBCL and 1 with FL.
To determine if patients with Q fever have a higher risk of lymphoma than the general population, the researchers compared the incidence of lymphoma in the Q fever registry to the incidence reported in France’s general population.
This revealed an excess risk of DLBCL and FL in the Q fever population, with standardized incidence ratios of 25.4 for DLBCL and 6.7 for FL.
In addition, the odds of developing lymphoma were higher in patients with persistent, concentrated infections than in those with other forms of Q fever. The hazard ratio for patients with persistent, concentrated infection was 9.35.
Finally, the researchers observed interleukin-10 overproduction in Q fever patients with lymphoma. The team said this suggests that suppression of the immune system may have allowed the lymphoma cells to evade immune detection and multiply.
“As we continue to learn more about the association between C burnetii and lymphoma, these results should encourage clinicians to survey high-risk patients as early as possible for potential cancer,” Dr Raoult said.
“Ultimately, this early diagnosis and treatment would improve outcomes for Q fever patients who subsequently develop lymphoma, particularly those with B-cell non-Hodgkin lymphoma.” ![]()
Coxiella burnetii
Image courtesy of NIAID
The bacterium that causes Q fever may confer an increased risk of diffuse large B-cell lymphoma (DLBCL) and follicular lymphoma (FL), according to a study published in Blood.
Q fever is an infectious disease caused by Coxiella burnetii, a bacterium primarily transmitted through the excrements of cattle, sheep, and goats.
Because some patients with Q fever develop lymphoma, researchers believed the malignancy could be a risk factor for Q fever.
However, the experience of 1 patient prompted a group of researchers in France to consider the opposite—that the infection might cause the lymphoma.
“During a follow-up scan in a patient we had successfully treated for Q fever, we observed a tumor close to the location of the previous infection,” said study author Didier Raoult, MD, PhD, of Aix-Marseille University in Marseille, France.
“The discovery that it was a lymphoma tumor containing C burnetii encouraged us to consider that the infection might have contributed to the development of the cancer.”
To better understand the association between C burnetii and lymphoma, Dr Raoult and his colleagues screened 1468 patients treated at the French National Referral Center for Q Fever from 2004 to 2014.
The researchers imaged patient tissue samples and identified 7 people, including the initial patient, who developed lymphoma after C burnetii infection. Six patients were diagnosed with DLBCL and 1 with FL.
To determine if patients with Q fever have a higher risk of lymphoma than the general population, the researchers compared the incidence of lymphoma in the Q fever registry to the incidence reported in France’s general population.
This revealed an excess risk of DLBCL and FL in the Q fever population, with standardized incidence ratios of 25.4 for DLBCL and 6.7 for FL.
In addition, the odds of developing lymphoma were higher in patients with persistent, concentrated infections than in those with other forms of Q fever. The hazard ratio for patients with persistent, concentrated infection was 9.35.
Finally, the researchers observed interleukin-10 overproduction in Q fever patients with lymphoma. The team said this suggests that suppression of the immune system may have allowed the lymphoma cells to evade immune detection and multiply.
“As we continue to learn more about the association between C burnetii and lymphoma, these results should encourage clinicians to survey high-risk patients as early as possible for potential cancer,” Dr Raoult said.
“Ultimately, this early diagnosis and treatment would improve outcomes for Q fever patients who subsequently develop lymphoma, particularly those with B-cell non-Hodgkin lymphoma.” ![]()
Report: Many cancer patients may be dying of VTE

chemotherapy
Photo by Rhoda Baer
Thousands of annual deaths among cancer patients in England and Wales may be caused by venous thromboembolism (VTE), according to a report from the All-Party Parliamentary Thrombosis Group (APPTG).
The report showed that, of the patients who died of cancer from 2012 through 2014, about 2.6% also had VTE listed on their death certificate as a cause of death.
This percentage corresponds to nearly 4000 deaths annually.
The report also indicated that many hospitals are not taking appropriate action to reduce the risk of VTE in cancer patients.
The APPTG conducted this research to determine awareness about VTE risk in cancer patients within the National Health Service (NHS). So the group requested data from 150 NHS hospitals in England and 7 in Wales.
The researchers received responses from 92 hospitals—28 in North England, 21 in South England, 25 in the Midlands and East England, 13 in London, and 5 in Wales. The responses included data spanning the period from 2012 through 2014.
On average, 7% of cancer patients in England and Wales were also diagnosed with VTE during the 3-year period.
The incidence of VTE in cancer patients varied by region. For example, it was 2% in the South of England and 3.6% in Wales.
The yearly incidences of cancer and VTE among all hospitals studied were as follows:
| Patients diagnosed with cancer and VTE in England and Wales | ||
| Year | Patients treated
for cancer |
Cancer patients
diagnosed with VTE |
| 2014 | 363,692 | 6301 (1.7%) |
| 2013 | 353,614 | 6506 (1.8%) |
| 2012 | 339,125 | 5716 (1.7%) |
Mortality rates among these patients were as follows:
| Mortality rates involving cancer and VTE in England and Wales | ||
| Year | Cancer deaths | Cancer deaths where VTE
was also listed as cause of death |
| 2014 | 159,187 | 4088 (2.6%) |
| 2013 | 157,848 | 4028 (2.6%) |
| 2012 | 157,293 | 3848 (2.5%) |
The researchers also found that only 41% of the hospitals studied have a dedicated policy or pathway for the management of suspected VTE in patients receiving chemotherapy.
Slightly less than half of the hospitals provide patients with both written and verbal information about the risk of developing VTE during chemotherapy, what symptoms to look out for, and what action patients should take if they suspect a VTE.
“It is a tragedy that, in today’s NHS, a patient can beat their cancer, only to then die of a clot,” said Andrew Gwynne, chair of the APPTG.
“We hope that by raising awareness of this overlooked issue, we can drive up patient safety and provide better outcomes for patients.” ![]()

chemotherapy
Photo by Rhoda Baer
Thousands of annual deaths among cancer patients in England and Wales may be caused by venous thromboembolism (VTE), according to a report from the All-Party Parliamentary Thrombosis Group (APPTG).
The report showed that, of the patients who died of cancer from 2012 through 2014, about 2.6% also had VTE listed on their death certificate as a cause of death.
This percentage corresponds to nearly 4000 deaths annually.
The report also indicated that many hospitals are not taking appropriate action to reduce the risk of VTE in cancer patients.
The APPTG conducted this research to determine awareness about VTE risk in cancer patients within the National Health Service (NHS). So the group requested data from 150 NHS hospitals in England and 7 in Wales.
The researchers received responses from 92 hospitals—28 in North England, 21 in South England, 25 in the Midlands and East England, 13 in London, and 5 in Wales. The responses included data spanning the period from 2012 through 2014.
On average, 7% of cancer patients in England and Wales were also diagnosed with VTE during the 3-year period.
The incidence of VTE in cancer patients varied by region. For example, it was 2% in the South of England and 3.6% in Wales.
The yearly incidences of cancer and VTE among all hospitals studied were as follows:
| Patients diagnosed with cancer and VTE in England and Wales | ||
| Year | Patients treated
for cancer |
Cancer patients
diagnosed with VTE |
| 2014 | 363,692 | 6301 (1.7%) |
| 2013 | 353,614 | 6506 (1.8%) |
| 2012 | 339,125 | 5716 (1.7%) |
Mortality rates among these patients were as follows:
| Mortality rates involving cancer and VTE in England and Wales | ||
| Year | Cancer deaths | Cancer deaths where VTE
was also listed as cause of death |
| 2014 | 159,187 | 4088 (2.6%) |
| 2013 | 157,848 | 4028 (2.6%) |
| 2012 | 157,293 | 3848 (2.5%) |
The researchers also found that only 41% of the hospitals studied have a dedicated policy or pathway for the management of suspected VTE in patients receiving chemotherapy.
Slightly less than half of the hospitals provide patients with both written and verbal information about the risk of developing VTE during chemotherapy, what symptoms to look out for, and what action patients should take if they suspect a VTE.
“It is a tragedy that, in today’s NHS, a patient can beat their cancer, only to then die of a clot,” said Andrew Gwynne, chair of the APPTG.
“We hope that by raising awareness of this overlooked issue, we can drive up patient safety and provide better outcomes for patients.” ![]()

chemotherapy
Photo by Rhoda Baer
Thousands of annual deaths among cancer patients in England and Wales may be caused by venous thromboembolism (VTE), according to a report from the All-Party Parliamentary Thrombosis Group (APPTG).
The report showed that, of the patients who died of cancer from 2012 through 2014, about 2.6% also had VTE listed on their death certificate as a cause of death.
This percentage corresponds to nearly 4000 deaths annually.
The report also indicated that many hospitals are not taking appropriate action to reduce the risk of VTE in cancer patients.
The APPTG conducted this research to determine awareness about VTE risk in cancer patients within the National Health Service (NHS). So the group requested data from 150 NHS hospitals in England and 7 in Wales.
The researchers received responses from 92 hospitals—28 in North England, 21 in South England, 25 in the Midlands and East England, 13 in London, and 5 in Wales. The responses included data spanning the period from 2012 through 2014.
On average, 7% of cancer patients in England and Wales were also diagnosed with VTE during the 3-year period.
The incidence of VTE in cancer patients varied by region. For example, it was 2% in the South of England and 3.6% in Wales.
The yearly incidences of cancer and VTE among all hospitals studied were as follows:
| Patients diagnosed with cancer and VTE in England and Wales | ||
| Year | Patients treated
for cancer |
Cancer patients
diagnosed with VTE |
| 2014 | 363,692 | 6301 (1.7%) |
| 2013 | 353,614 | 6506 (1.8%) |
| 2012 | 339,125 | 5716 (1.7%) |
Mortality rates among these patients were as follows:
| Mortality rates involving cancer and VTE in England and Wales | ||
| Year | Cancer deaths | Cancer deaths where VTE
was also listed as cause of death |
| 2014 | 159,187 | 4088 (2.6%) |
| 2013 | 157,848 | 4028 (2.6%) |
| 2012 | 157,293 | 3848 (2.5%) |
The researchers also found that only 41% of the hospitals studied have a dedicated policy or pathway for the management of suspected VTE in patients receiving chemotherapy.
Slightly less than half of the hospitals provide patients with both written and verbal information about the risk of developing VTE during chemotherapy, what symptoms to look out for, and what action patients should take if they suspect a VTE.
“It is a tragedy that, in today’s NHS, a patient can beat their cancer, only to then die of a clot,” said Andrew Gwynne, chair of the APPTG.
“We hope that by raising awareness of this overlooked issue, we can drive up patient safety and provide better outcomes for patients.”
Explaining treatment-related anemia

Research conducted in mice suggests that genomic screening might reveal cancer patients who are likely to develop treatment-related anemia.
The study showed that mice lacking Pten and Shp2—enzymes targeted by certain anticancer therapies—can’t produce and sustain enough red blood cells.
Investigators said this helps explain why anemia is a common side effect of anticancer drugs that target enzymes involved in tumor growth.
“Based on this unexpected finding, we might want to think about screening cancer patients’ genetic backgrounds for loss of Pten or Pten-regulated signals before prescribing anticancer drugs that might do more harm than good,” said Gen-Sheng Feng, PhD, of the University of California San Diego School of Medicine.
Dr Feng and his colleagues described their research in PNAS.
First, the team genetically engineered mice to lack Pten, Shp2, or both enzymes. The Pten-deficient mice had elevated white blood cells counts, consistent with myeloproliferative neoplasms (MPNs).
The Shp2-deficient mice experienced the opposite—lower white blood cell counts. And mice lacking both Pten and Shp2 had relatively normal white blood cell counts, suggesting that loss of Shp2 suppresses MPNs induced by Pten loss.
However, the investigators also discovered that mice lacking both enzymes had shorter lifespans than wild-type mice or mice lacking 1 of the enzymes.
This was because the combined deficiency of Shp2 and Pten induced lethal anemia. And this anemia was a result of 2 factors: red blood cells failed to develop properly and those that did form had a shortened lifespan.
To build upon these findings, the investigators treated Pten-deficient mice with the Shp2 inhibitor 11a-1 or with the MEK inhibitor trametinib. (MEK belongs to the same cellular communication network as Shp2.)
As with genetic deletion of Shp2, pharmacologic inhibition of Shp2 suppressed MPN induced by Pten loss and induced severe anemia in the mice.
Trametinib treatment had a similar effect, inducing anemia in Pten-deficient mice but not wild-type mice.
“What we’ve learned is that even if we know a lot about how individual molecules function in a cell, designing effective therapeutics that target them will require a more comprehensive understanding of the cross-talk between molecules in a particular cell type and in the context of disease,” Dr Feng concluded.

Research conducted in mice suggests that genomic screening might reveal cancer patients who are likely to develop treatment-related anemia.
The study showed that mice lacking Pten and Shp2—enzymes targeted by certain anticancer therapies—can’t produce and sustain enough red blood cells.
Investigators said this helps explain why anemia is a common side effect of anticancer drugs that target enzymes involved in tumor growth.
“Based on this unexpected finding, we might want to think about screening cancer patients’ genetic backgrounds for loss of Pten or Pten-regulated signals before prescribing anticancer drugs that might do more harm than good,” said Gen-Sheng Feng, PhD, of the University of California San Diego School of Medicine.
Dr Feng and his colleagues described their research in PNAS.
First, the team genetically engineered mice to lack Pten, Shp2, or both enzymes. The Pten-deficient mice had elevated white blood cells counts, consistent with myeloproliferative neoplasms (MPNs).
The Shp2-deficient mice experienced the opposite—lower white blood cell counts. And mice lacking both Pten and Shp2 had relatively normal white blood cell counts, suggesting that loss of Shp2 suppresses MPNs induced by Pten loss.
However, the investigators also discovered that mice lacking both enzymes had shorter lifespans than wild-type mice or mice lacking 1 of the enzymes.
This was because the combined deficiency of Shp2 and Pten induced lethal anemia. And this anemia was a result of 2 factors: red blood cells failed to develop properly and those that did form had a shortened lifespan.
To build upon these findings, the investigators treated Pten-deficient mice with the Shp2 inhibitor 11a-1 or with the MEK inhibitor trametinib. (MEK belongs to the same cellular communication network as Shp2.)
As with genetic deletion of Shp2, pharmacologic inhibition of Shp2 suppressed MPN induced by Pten loss and induced severe anemia in the mice.
Trametinib treatment had a similar effect, inducing anemia in Pten-deficient mice but not wild-type mice.
“What we’ve learned is that even if we know a lot about how individual molecules function in a cell, designing effective therapeutics that target them will require a more comprehensive understanding of the cross-talk between molecules in a particular cell type and in the context of disease,” Dr Feng concluded.

Research conducted in mice suggests that genomic screening might reveal cancer patients who are likely to develop treatment-related anemia.
The study showed that mice lacking Pten and Shp2—enzymes targeted by certain anticancer therapies—can’t produce and sustain enough red blood cells.
Investigators said this helps explain why anemia is a common side effect of anticancer drugs that target enzymes involved in tumor growth.
“Based on this unexpected finding, we might want to think about screening cancer patients’ genetic backgrounds for loss of Pten or Pten-regulated signals before prescribing anticancer drugs that might do more harm than good,” said Gen-Sheng Feng, PhD, of the University of California San Diego School of Medicine.
Dr Feng and his colleagues described their research in PNAS.
First, the team genetically engineered mice to lack Pten, Shp2, or both enzymes. The Pten-deficient mice had elevated white blood cells counts, consistent with myeloproliferative neoplasms (MPNs).
The Shp2-deficient mice experienced the opposite—lower white blood cell counts. And mice lacking both Pten and Shp2 had relatively normal white blood cell counts, suggesting that loss of Shp2 suppresses MPNs induced by Pten loss.
However, the investigators also discovered that mice lacking both enzymes had shorter lifespans than wild-type mice or mice lacking 1 of the enzymes.
This was because the combined deficiency of Shp2 and Pten induced lethal anemia. And this anemia was a result of 2 factors: red blood cells failed to develop properly and those that did form had a shortened lifespan.
To build upon these findings, the investigators treated Pten-deficient mice with the Shp2 inhibitor 11a-1 or with the MEK inhibitor trametinib. (MEK belongs to the same cellular communication network as Shp2.)
As with genetic deletion of Shp2, pharmacologic inhibition of Shp2 suppressed MPN induced by Pten loss and induced severe anemia in the mice.
Trametinib treatment had a similar effect, inducing anemia in Pten-deficient mice but not wild-type mice.
“What we’ve learned is that even if we know a lot about how individual molecules function in a cell, designing effective therapeutics that target them will require a more comprehensive understanding of the cross-talk between molecules in a particular cell type and in the context of disease,” Dr Feng concluded.
Anticoagulant granted fast track designation

Image by Kevin MacKenzie
The US Food and Drug Administration (FDA) has granted fast track designation to betrixaban as extended-duration venous thromboembolism (VTE) prophylaxis for acute medically ill patients.
This includes patients who are hospitalized for serious medical conditions such as heart failure, stroke, infection, and pulmonary disease.
Betrixaban is an investigational oral anticoagulant that directly inhibits the activity of factor Xa.
According to Portola Pharmaceuticals, the company developing betrixaban, the drug has distinct properties that may allow it to demonstrate clinical benefit without significantly increasing the risk of fatal bleeding and certain other serious side effects.
These benefits include a 19- to 25-hour half-life for once-daily dosing, a low peak-to-trough drug concentration ratio that minimizes anticoagulant variability, low renal clearance, and no significant CYP3A4 metabolism, which may reduce the risk of drug-drug interactions.
Betrixaban trials
In the phase 2 Explore-Xa trial, researchers compared betrixaban and warfarin in patients with atrial fibrillation. The team randomized 508 patients to 1 of 3 blinded doses of betrixaban (40 mg, 60 mg, or 80 mg once daily) or unblinded warfarin, adjusted to an international normalized ratio of 2.0-3.0.
The primary outcome was major or clinically relevant non-major bleeding. At a mean follow-up of 147 days, the primary outcome had been met by 1 patient in the 40 mg betrixaban arm, 5 each in the 60 mg and 80 mg betrixaban arms, and 7 in the warfarin arm.
One patient each in the 60 mg and 80 mg arms experienced an ischemic stroke. And there were 2 vascular deaths, 1 each in the 40 mg arm and the warfarin arm.
In the phase 2 EXPERT trial, researchers compared betrixaban and enoxaparin as VTE prophylaxis in patients who underwent total knee replacement.
The team enrolled 215 patients and assigned them to 1 of 3 post-operative prophylaxis regimens: betrixaban at 15 mg twice daily, betrixaban at 40 mg twice daily, or enoxaparin at 30 mg every 12 hours—all for 10 to 14 days.
The primary efficacy outcome was the incidence of VTE during the dosing period, and 175 patients were evaluable for this outcome. VTE occurred in 20% of patients in the 15 mg betrixaban arm (14/70), 15% in the 40 mg betrixaban arm (10/65), and 10% (4/40) in the enoxaparin arm.
Safety outcomes included major and clinically significant non-major bleeds through 48 hours after treatment. There were no bleeds in the 15 mg betrixaban arm, 2 (2.4%) clinically significant non-major bleeds in the 40 mg betrixaban arm, and 1 (2.3%) major bleed and 2 (4.6%) clinically significant non-major bleeds in the enoxaparin arm.
Betrixaban is currently being tested in the phase 3 APEX trial for the prevention of VTE in acute medically ill patients. Portola said it expects to complete enrollment in APEX by the end of this year and report top-line data in the first quarter of 2016.
If the trial is successful, the company plans to submit a new drug application to the FDA later in 2016 under the fast track designation.
About fast track designation
The FDA’s fast track program is designed to facilitate and expedite the development and review of new drugs intended to treat serious or life-threatening conditions and address unmet medical need.
Through the fast track program, a product may be eligible for priority review. In addition, the company developing the drug may be allowed to submit sections of the biologic license application or new drug application on a rolling basis as data become available.
Fast track designation also provides the company with opportunities for more frequent meetings with the FDA to discuss the drug’s development plan and ensure collection of the appropriate data needed to support drug approval. And the designation allows for more frequent written communication from the FDA about things such as the design of proposed clinical trials and the use of biomarkers.

Image by Kevin MacKenzie
The US Food and Drug Administration (FDA) has granted fast track designation to betrixaban as extended-duration venous thromboembolism (VTE) prophylaxis for acute medically ill patients.
This includes patients who are hospitalized for serious medical conditions such as heart failure, stroke, infection, and pulmonary disease.
Betrixaban is an investigational oral anticoagulant that directly inhibits the activity of factor Xa.
According to Portola Pharmaceuticals, the company developing betrixaban, the drug has distinct properties that may allow it to demonstrate clinical benefit without significantly increasing the risk of fatal bleeding and certain other serious side effects.
These benefits include a 19- to 25-hour half-life for once-daily dosing, a low peak-to-trough drug concentration ratio that minimizes anticoagulant variability, low renal clearance, and no significant CYP3A4 metabolism, which may reduce the risk of drug-drug interactions.
Betrixaban trials
In the phase 2 Explore-Xa trial, researchers compared betrixaban and warfarin in patients with atrial fibrillation. The team randomized 508 patients to 1 of 3 blinded doses of betrixaban (40 mg, 60 mg, or 80 mg once daily) or unblinded warfarin, adjusted to an international normalized ratio of 2.0-3.0.
The primary outcome was major or clinically relevant non-major bleeding. At a mean follow-up of 147 days, the primary outcome had been met by 1 patient in the 40 mg betrixaban arm, 5 each in the 60 mg and 80 mg betrixaban arms, and 7 in the warfarin arm.
One patient each in the 60 mg and 80 mg arms experienced an ischemic stroke. And there were 2 vascular deaths, 1 each in the 40 mg arm and the warfarin arm.
In the phase 2 EXPERT trial, researchers compared betrixaban and enoxaparin as VTE prophylaxis in patients who underwent total knee replacement.
The team enrolled 215 patients and assigned them to 1 of 3 post-operative prophylaxis regimens: betrixaban at 15 mg twice daily, betrixaban at 40 mg twice daily, or enoxaparin at 30 mg every 12 hours—all for 10 to 14 days.
The primary efficacy outcome was the incidence of VTE during the dosing period, and 175 patients were evaluable for this outcome. VTE occurred in 20% of patients in the 15 mg betrixaban arm (14/70), 15% in the 40 mg betrixaban arm (10/65), and 10% (4/40) in the enoxaparin arm.
Safety outcomes included major and clinically significant non-major bleeds through 48 hours after treatment. There were no bleeds in the 15 mg betrixaban arm, 2 (2.4%) clinically significant non-major bleeds in the 40 mg betrixaban arm, and 1 (2.3%) major bleed and 2 (4.6%) clinically significant non-major bleeds in the enoxaparin arm.
Betrixaban is currently being tested in the phase 3 APEX trial for the prevention of VTE in acute medically ill patients. Portola said it expects to complete enrollment in APEX by the end of this year and report top-line data in the first quarter of 2016.
If the trial is successful, the company plans to submit a new drug application to the FDA later in 2016 under the fast track designation.
About fast track designation
The FDA’s fast track program is designed to facilitate and expedite the development and review of new drugs intended to treat serious or life-threatening conditions and address unmet medical need.
Through the fast track program, a product may be eligible for priority review. In addition, the company developing the drug may be allowed to submit sections of the biologic license application or new drug application on a rolling basis as data become available.
Fast track designation also provides the company with opportunities for more frequent meetings with the FDA to discuss the drug’s development plan and ensure collection of the appropriate data needed to support drug approval. And the designation allows for more frequent written communication from the FDA about things such as the design of proposed clinical trials and the use of biomarkers.

Image by Kevin MacKenzie
The US Food and Drug Administration (FDA) has granted fast track designation to betrixaban as extended-duration venous thromboembolism (VTE) prophylaxis for acute medically ill patients.
This includes patients who are hospitalized for serious medical conditions such as heart failure, stroke, infection, and pulmonary disease.
Betrixaban is an investigational oral anticoagulant that directly inhibits the activity of factor Xa.
According to Portola Pharmaceuticals, the company developing betrixaban, the drug has distinct properties that may allow it to demonstrate clinical benefit without significantly increasing the risk of fatal bleeding and certain other serious side effects.
These benefits include a 19- to 25-hour half-life for once-daily dosing, a low peak-to-trough drug concentration ratio that minimizes anticoagulant variability, low renal clearance, and no significant CYP3A4 metabolism, which may reduce the risk of drug-drug interactions.
Betrixaban trials
In the phase 2 Explore-Xa trial, researchers compared betrixaban and warfarin in patients with atrial fibrillation. The team randomized 508 patients to 1 of 3 blinded doses of betrixaban (40 mg, 60 mg, or 80 mg once daily) or unblinded warfarin, adjusted to an international normalized ratio of 2.0-3.0.
The primary outcome was major or clinically relevant non-major bleeding. At a mean follow-up of 147 days, the primary outcome had been met by 1 patient in the 40 mg betrixaban arm, 5 each in the 60 mg and 80 mg betrixaban arms, and 7 in the warfarin arm.
One patient each in the 60 mg and 80 mg arms experienced an ischemic stroke. And there were 2 vascular deaths, 1 each in the 40 mg arm and the warfarin arm.
In the phase 2 EXPERT trial, researchers compared betrixaban and enoxaparin as VTE prophylaxis in patients who underwent total knee replacement.
The team enrolled 215 patients and assigned them to 1 of 3 post-operative prophylaxis regimens: betrixaban at 15 mg twice daily, betrixaban at 40 mg twice daily, or enoxaparin at 30 mg every 12 hours—all for 10 to 14 days.
The primary efficacy outcome was the incidence of VTE during the dosing period, and 175 patients were evaluable for this outcome. VTE occurred in 20% of patients in the 15 mg betrixaban arm (14/70), 15% in the 40 mg betrixaban arm (10/65), and 10% (4/40) in the enoxaparin arm.
Safety outcomes included major and clinically significant non-major bleeds through 48 hours after treatment. There were no bleeds in the 15 mg betrixaban arm, 2 (2.4%) clinically significant non-major bleeds in the 40 mg betrixaban arm, and 1 (2.3%) major bleed and 2 (4.6%) clinically significant non-major bleeds in the enoxaparin arm.
Betrixaban is currently being tested in the phase 3 APEX trial for the prevention of VTE in acute medically ill patients. Portola said it expects to complete enrollment in APEX by the end of this year and report top-line data in the first quarter of 2016.
If the trial is successful, the company plans to submit a new drug application to the FDA later in 2016 under the fast track designation.
About fast track designation
The FDA’s fast track program is designed to facilitate and expedite the development and review of new drugs intended to treat serious or life-threatening conditions and address unmet medical need.
Through the fast track program, a product may be eligible for priority review. In addition, the company developing the drug may be allowed to submit sections of the biologic license application or new drug application on a rolling basis as data become available.
Fast track designation also provides the company with opportunities for more frequent meetings with the FDA to discuss the drug’s development plan and ensure collection of the appropriate data needed to support drug approval. And the designation allows for more frequent written communication from the FDA about things such as the design of proposed clinical trials and the use of biomarkers.
Cancer survivors have poor diets, study suggests

New research suggests that cancer survivors in the US may need dietary interventions to improve their health.
The study showed that, overall, cancer survivors did not adhere to federal dietary guidelines as well as a matched control population.
Cancer survivors tended to consume more empty calories and less fiber than controls.
Fang Fang Zhang, MD, PhD, of Tufts University in Boston, Massachusetts, and his colleagues reported these findings in Cancer.
The team evaluated the diets of 1533 adult cancer survivors who participated in the National Health and Nutrition Examination Survey from 1999 to 2010. The investigators also assessed the diets of 3075 individuals who had no history of cancer and were matched to the cancer survivors by age, sex, and race/ethnicity.
The goal was to determine how subjects’ diets aligned with advice from the 2010 Dietary Guidelines for Americans, which was jointly issued by the Department of Agriculture and the Department of Health and Human Services.
Cancer survivors had poor adherence to the guidelines, with a total Healthy Eating Index score of 47.2 out of 100, compared with a score of 48.3 in the adults without a history of cancer (P=0.03).
Cancer survivors had a significantly lower mean score for empty calories compared to the noncancer group—13.6 and 14.4, respectively (P=0.001). This suggested the cancer group had a higher consumption of calories from solid fats, alcohol, and added sugars.
Cancer survivors also had significantly lower dietary intake of fiber than the noncancer group—15.0 and 15.9 g per day, respectively (P=0.02).
Compared to recommended values, cancer survivors had low dietary intakes of vitamin D (31% of the recommended intake), vitamin E (47%), potassium (55%), and calcium (73%) but high intakes of saturated fat (112%) and sodium (133%).
The investigators noted that diet quality in cancer survivors increased linearly with age. The older the age, the better the diet quality.
Survivors with lower education (high school or less) had significantly worse diet quality than those with higher education. And survivors who were current smokers had significantly worse diet quality than non-smokers or former smokers.
For the 4 major cancer types in the US (breast, prostate, lung, and colorectal), breast cancer survivors had the best diet quality, and lung cancer survivors had the worst diet quality.
The investigators said that knowing how well cancer survivors adhere to federal dietary guidelines can help inform evidence-based priorities for improving their nutritional intake.
“Dietary changes that include more fiber, fruit, and vegetables in the diet and less fat, sodium, and added sugar would be important for cancer survivors,” Dr Zhang said.
“Oncology care providers can play critical roles in reinforcing the importance of a healthful diet and can refer patients to registered dietitians who are experts in oncology care or to other reputable sources in order to improve survivors’ overall health.”

New research suggests that cancer survivors in the US may need dietary interventions to improve their health.
The study showed that, overall, cancer survivors did not adhere to federal dietary guidelines as well as a matched control population.
Cancer survivors tended to consume more empty calories and less fiber than controls.
Fang Fang Zhang, MD, PhD, of Tufts University in Boston, Massachusetts, and his colleagues reported these findings in Cancer.
The team evaluated the diets of 1533 adult cancer survivors who participated in the National Health and Nutrition Examination Survey from 1999 to 2010. The investigators also assessed the diets of 3075 individuals who had no history of cancer and were matched to the cancer survivors by age, sex, and race/ethnicity.
The goal was to determine how subjects’ diets aligned with advice from the 2010 Dietary Guidelines for Americans, which was jointly issued by the Department of Agriculture and the Department of Health and Human Services.
Cancer survivors had poor adherence to the guidelines, with a total Healthy Eating Index score of 47.2 out of 100, compared with a score of 48.3 in the adults without a history of cancer (P=0.03).
Cancer survivors had a significantly lower mean score for empty calories compared to the noncancer group—13.6 and 14.4, respectively (P=0.001). This suggested the cancer group had a higher consumption of calories from solid fats, alcohol, and added sugars.
Cancer survivors also had significantly lower dietary intake of fiber than the noncancer group—15.0 and 15.9 g per day, respectively (P=0.02).
Compared to recommended values, cancer survivors had low dietary intakes of vitamin D (31% of the recommended intake), vitamin E (47%), potassium (55%), and calcium (73%) but high intakes of saturated fat (112%) and sodium (133%).
The investigators noted that diet quality in cancer survivors increased linearly with age. The older the age, the better the diet quality.
Survivors with lower education (high school or less) had significantly worse diet quality than those with higher education. And survivors who were current smokers had significantly worse diet quality than non-smokers or former smokers.
For the 4 major cancer types in the US (breast, prostate, lung, and colorectal), breast cancer survivors had the best diet quality, and lung cancer survivors had the worst diet quality.
The investigators said that knowing how well cancer survivors adhere to federal dietary guidelines can help inform evidence-based priorities for improving their nutritional intake.
“Dietary changes that include more fiber, fruit, and vegetables in the diet and less fat, sodium, and added sugar would be important for cancer survivors,” Dr Zhang said.
“Oncology care providers can play critical roles in reinforcing the importance of a healthful diet and can refer patients to registered dietitians who are experts in oncology care or to other reputable sources in order to improve survivors’ overall health.”

New research suggests that cancer survivors in the US may need dietary interventions to improve their health.
The study showed that, overall, cancer survivors did not adhere to federal dietary guidelines as well as a matched control population.
Cancer survivors tended to consume more empty calories and less fiber than controls.
Fang Fang Zhang, MD, PhD, of Tufts University in Boston, Massachusetts, and his colleagues reported these findings in Cancer.
The team evaluated the diets of 1533 adult cancer survivors who participated in the National Health and Nutrition Examination Survey from 1999 to 2010. The investigators also assessed the diets of 3075 individuals who had no history of cancer and were matched to the cancer survivors by age, sex, and race/ethnicity.
The goal was to determine how subjects’ diets aligned with advice from the 2010 Dietary Guidelines for Americans, which was jointly issued by the Department of Agriculture and the Department of Health and Human Services.
Cancer survivors had poor adherence to the guidelines, with a total Healthy Eating Index score of 47.2 out of 100, compared with a score of 48.3 in the adults without a history of cancer (P=0.03).
Cancer survivors had a significantly lower mean score for empty calories compared to the noncancer group—13.6 and 14.4, respectively (P=0.001). This suggested the cancer group had a higher consumption of calories from solid fats, alcohol, and added sugars.
Cancer survivors also had significantly lower dietary intake of fiber than the noncancer group—15.0 and 15.9 g per day, respectively (P=0.02).
Compared to recommended values, cancer survivors had low dietary intakes of vitamin D (31% of the recommended intake), vitamin E (47%), potassium (55%), and calcium (73%) but high intakes of saturated fat (112%) and sodium (133%).
The investigators noted that diet quality in cancer survivors increased linearly with age. The older the age, the better the diet quality.
Survivors with lower education (high school or less) had significantly worse diet quality than those with higher education. And survivors who were current smokers had significantly worse diet quality than non-smokers or former smokers.
For the 4 major cancer types in the US (breast, prostate, lung, and colorectal), breast cancer survivors had the best diet quality, and lung cancer survivors had the worst diet quality.
The investigators said that knowing how well cancer survivors adhere to federal dietary guidelines can help inform evidence-based priorities for improving their nutritional intake.
“Dietary changes that include more fiber, fruit, and vegetables in the diet and less fat, sodium, and added sugar would be important for cancer survivors,” Dr Zhang said.
“Oncology care providers can play critical roles in reinforcing the importance of a healthful diet and can refer patients to registered dietitians who are experts in oncology care or to other reputable sources in order to improve survivors’ overall health.”