User login
M. Alexander Otto began his reporting career early in 1999 covering the pharmaceutical industry for a national pharmacists' magazine and freelancing for the Washington Post and other newspapers. He then joined BNA, now part of Bloomberg News, covering health law and the protection of people and animals in medical research. Alex next worked for the McClatchy Company. Based on his work, Alex won a year-long Knight Science Journalism Fellowship to MIT in 2008-2009. He joined the company shortly thereafter. Alex has a newspaper journalism degree from Syracuse (N.Y.) University and a master's degree in medical science -- a physician assistant degree -- from George Washington University. Alex is based in Seattle.
Despite VTE prophylaxis, more bleeds, no benefit in medical inpatients
VIDEO: Rethink the VTE
LAS VEGAS – Venous thromboembolism prophylaxis does not seem to prevent symptomatic deep vein thrombosis or pulmonary embolism in nonsurgical, non-ICU hospital patients, but it does seem to increase the risk of major bleeding, according to a series of large, observational studies from the Michigan Hospital Medicine Safety Consortium, a quality improvement program involving 40 Michigan hospitals.
Spurred by the Joint Commission and others, hospitalists across the United States have "put their foot on the gas to increase pharmacologic prophylaxis, and we’re using it in patients we think really should get it, but also in some patients who probably shouldn’t. We need more research to" distinguish between the two groups. "Many of us feel that the pendulum has swung too far, and that we need to bring it back to the middle," said investigator Dr. Scott Kaatz, chief quality officer and leader of the hospitalist program at Hurley Medical Center in Flint, Mich.
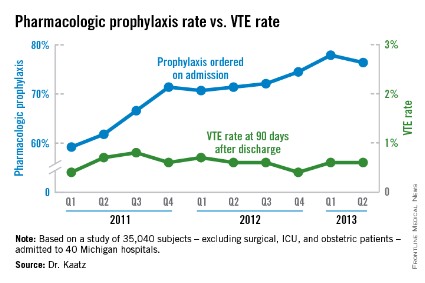
Among the Consortium’s findings, venous thromboembolism (VTE) prophylaxis – generally a subcutaneous shot with a heparin product – was ordered at admission for 59.2% of general adult inpatients in the first quarter of 2011, excluding surgical, ICU, and obstetric patients. By the second quarter of 2013, that had risen to 76.4%. Even so, among the 35,040 subjects included in the analysis, the rate of symptomatic VTEs averaged 0.56% throughout the observation period, and did not decrease as more patients were prophylaxed (P for trend = .114). The investigators followed their subjects in the hospital, and for 3 months afterward.
"We have not shown a good correlation between increasing prophylaxis and decreasing hospital-associated VTE," Dr. Kaatz said at the Society of Hospital Medicine annual meeting.
Meanwhile, in a second analysis of 26,205 prophylaxed medical inpatients, the rates of major bleeding tripled from 0.2% to 0.6% over the 2-plus years that prophylaxis was becoming more common (P = .052). Prophylaxis rates also climbed from 8.7% to 25.8% among a subset of 1,165 patients contraindicated because of their bleeding risks. The relationship between contraindications and the increased bleeding rate isn’t clear; some who bled had contraindications, but others did not.
"Five years ago, I was an advocate: prophylaxis everybody. [Now,] I’m really worried that I might be causing some bleeding. VTE rates are pretty low," and lower than once thought among general medical inpatients, may be caused by early mobilization and shorter hospital stays. "We are really spending a lot of effort to prophylaxis something that’s" uncommon, without clear benefit and possible harm. "I think several of us will take [these findings] back to our hospitals to change our prophylaxis protocols," Dr. Kaatz said.
Consortium members came up with their own list of contraindications because "there’s not a lot of literature, unfortunately," to help, he noted. The list included brain metastases; intracranial monitoring devices; severe head or spine trauma within 24 hours; gastrointestinal, genitourinary or other hemorrhages within 6 months; intracranial hemorrhage within a year; and platelet counts below 50,000/mm3.
The Caprini score is one of several proposed to distinguish high-risk VTE patients from others, but in a third study, investigators found that it "did not effectively discriminate populations for which pharmacologic prophylaxis was useful." Scores of 5 or higher did predict risk, but among high-scorers, 0.72% who received prophylaxis – and 0.86% who did not – developed VTEs, an insignificant difference (P = .26). Michigan researchers have found other scoring systems to be problematic, as well.
"The mantra for years now has been to prophylaxis for VTEs, so a lot of us are treating to prophylaxis everybody," even low Caprini-score patients. "Now, we’re taking a step back. There’s a movement toward weighing VTE and bleeding risks. If we can find the population that doesn’t warrant prophylaxis, that would be a big step," said investigator Dr. Paul Grant, a hospitalist who is with the internal medicine department at the University of Michigan in Ann Arbor.
The consortium is funded by Blue Cross/Blue Shield of Michigan and the Blue Care Network. Dr. Grant has no disclosures. Dr. Kaatz is a speaker for Boehringer Ingelheim, Janssen, Daiichi Sankyo, and Bristol-Myers Squibb.
It may be worth looking again at prophylaxis in the general medical inpatient who’s at low risk for VTE, and who’s going to be in the hospital for a short period of time. It’s been generally believed that hospitalized patients are at moderate risk, but as we are getting more data like these, we are realizing that there may be a population of hospitalized patients who are at lower risk than we thought. That raises a question: Do they really need prophylaxis?
In general, we need to be more thoughtful about VTE prophylaxis. It costs money, and may have adverse outcomes.
Dr. Eduard E. Vasilevskis is a hospitalist and is in the department of medicine at Vanderbilt University in Nashville, Tenn. He has no relevant disclosures.
It may be worth looking again at prophylaxis in the general medical inpatient who’s at low risk for VTE, and who’s going to be in the hospital for a short period of time. It’s been generally believed that hospitalized patients are at moderate risk, but as we are getting more data like these, we are realizing that there may be a population of hospitalized patients who are at lower risk than we thought. That raises a question: Do they really need prophylaxis?
In general, we need to be more thoughtful about VTE prophylaxis. It costs money, and may have adverse outcomes.
Dr. Eduard E. Vasilevskis is a hospitalist and is in the department of medicine at Vanderbilt University in Nashville, Tenn. He has no relevant disclosures.
It may be worth looking again at prophylaxis in the general medical inpatient who’s at low risk for VTE, and who’s going to be in the hospital for a short period of time. It’s been generally believed that hospitalized patients are at moderate risk, but as we are getting more data like these, we are realizing that there may be a population of hospitalized patients who are at lower risk than we thought. That raises a question: Do they really need prophylaxis?
In general, we need to be more thoughtful about VTE prophylaxis. It costs money, and may have adverse outcomes.
Dr. Eduard E. Vasilevskis is a hospitalist and is in the department of medicine at Vanderbilt University in Nashville, Tenn. He has no relevant disclosures.
VIDEO: Rethink the VTE
LAS VEGAS – Venous thromboembolism prophylaxis does not seem to prevent symptomatic deep vein thrombosis or pulmonary embolism in nonsurgical, non-ICU hospital patients, but it does seem to increase the risk of major bleeding, according to a series of large, observational studies from the Michigan Hospital Medicine Safety Consortium, a quality improvement program involving 40 Michigan hospitals.
Spurred by the Joint Commission and others, hospitalists across the United States have "put their foot on the gas to increase pharmacologic prophylaxis, and we’re using it in patients we think really should get it, but also in some patients who probably shouldn’t. We need more research to" distinguish between the two groups. "Many of us feel that the pendulum has swung too far, and that we need to bring it back to the middle," said investigator Dr. Scott Kaatz, chief quality officer and leader of the hospitalist program at Hurley Medical Center in Flint, Mich.
Among the Consortium’s findings, venous thromboembolism (VTE) prophylaxis – generally a subcutaneous shot with a heparin product – was ordered at admission for 59.2% of general adult inpatients in the first quarter of 2011, excluding surgical, ICU, and obstetric patients. By the second quarter of 2013, that had risen to 76.4%. Even so, among the 35,040 subjects included in the analysis, the rate of symptomatic VTEs averaged 0.56% throughout the observation period, and did not decrease as more patients were prophylaxed (P for trend = .114). The investigators followed their subjects in the hospital, and for 3 months afterward.
"We have not shown a good correlation between increasing prophylaxis and decreasing hospital-associated VTE," Dr. Kaatz said at the Society of Hospital Medicine annual meeting.
Meanwhile, in a second analysis of 26,205 prophylaxed medical inpatients, the rates of major bleeding tripled from 0.2% to 0.6% over the 2-plus years that prophylaxis was becoming more common (P = .052). Prophylaxis rates also climbed from 8.7% to 25.8% among a subset of 1,165 patients contraindicated because of their bleeding risks. The relationship between contraindications and the increased bleeding rate isn’t clear; some who bled had contraindications, but others did not.
"Five years ago, I was an advocate: prophylaxis everybody. [Now,] I’m really worried that I might be causing some bleeding. VTE rates are pretty low," and lower than once thought among general medical inpatients, may be caused by early mobilization and shorter hospital stays. "We are really spending a lot of effort to prophylaxis something that’s" uncommon, without clear benefit and possible harm. "I think several of us will take [these findings] back to our hospitals to change our prophylaxis protocols," Dr. Kaatz said.
Consortium members came up with their own list of contraindications because "there’s not a lot of literature, unfortunately," to help, he noted. The list included brain metastases; intracranial monitoring devices; severe head or spine trauma within 24 hours; gastrointestinal, genitourinary or other hemorrhages within 6 months; intracranial hemorrhage within a year; and platelet counts below 50,000/mm3.
The Caprini score is one of several proposed to distinguish high-risk VTE patients from others, but in a third study, investigators found that it "did not effectively discriminate populations for which pharmacologic prophylaxis was useful." Scores of 5 or higher did predict risk, but among high-scorers, 0.72% who received prophylaxis – and 0.86% who did not – developed VTEs, an insignificant difference (P = .26). Michigan researchers have found other scoring systems to be problematic, as well.
"The mantra for years now has been to prophylaxis for VTEs, so a lot of us are treating to prophylaxis everybody," even low Caprini-score patients. "Now, we’re taking a step back. There’s a movement toward weighing VTE and bleeding risks. If we can find the population that doesn’t warrant prophylaxis, that would be a big step," said investigator Dr. Paul Grant, a hospitalist who is with the internal medicine department at the University of Michigan in Ann Arbor.
The consortium is funded by Blue Cross/Blue Shield of Michigan and the Blue Care Network. Dr. Grant has no disclosures. Dr. Kaatz is a speaker for Boehringer Ingelheim, Janssen, Daiichi Sankyo, and Bristol-Myers Squibb.
VIDEO: Rethink the VTE
LAS VEGAS – Venous thromboembolism prophylaxis does not seem to prevent symptomatic deep vein thrombosis or pulmonary embolism in nonsurgical, non-ICU hospital patients, but it does seem to increase the risk of major bleeding, according to a series of large, observational studies from the Michigan Hospital Medicine Safety Consortium, a quality improvement program involving 40 Michigan hospitals.
Spurred by the Joint Commission and others, hospitalists across the United States have "put their foot on the gas to increase pharmacologic prophylaxis, and we’re using it in patients we think really should get it, but also in some patients who probably shouldn’t. We need more research to" distinguish between the two groups. "Many of us feel that the pendulum has swung too far, and that we need to bring it back to the middle," said investigator Dr. Scott Kaatz, chief quality officer and leader of the hospitalist program at Hurley Medical Center in Flint, Mich.
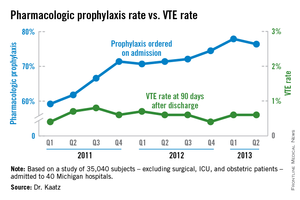
Among the Consortium’s findings, venous thromboembolism (VTE) prophylaxis – generally a subcutaneous shot with a heparin product – was ordered at admission for 59.2% of general adult inpatients in the first quarter of 2011, excluding surgical, ICU, and obstetric patients. By the second quarter of 2013, that had risen to 76.4%. Even so, among the 35,040 subjects included in the analysis, the rate of symptomatic VTEs averaged 0.56% throughout the observation period, and did not decrease as more patients were prophylaxed (P for trend = .114). The investigators followed their subjects in the hospital, and for 3 months afterward.
"We have not shown a good correlation between increasing prophylaxis and decreasing hospital-associated VTE," Dr. Kaatz said at the Society of Hospital Medicine annual meeting.
Meanwhile, in a second analysis of 26,205 prophylaxed medical inpatients, the rates of major bleeding tripled from 0.2% to 0.6% over the 2-plus years that prophylaxis was becoming more common (P = .052). Prophylaxis rates also climbed from 8.7% to 25.8% among a subset of 1,165 patients contraindicated because of their bleeding risks. The relationship between contraindications and the increased bleeding rate isn’t clear; some who bled had contraindications, but others did not.
"Five years ago, I was an advocate: prophylaxis everybody. [Now,] I’m really worried that I might be causing some bleeding. VTE rates are pretty low," and lower than once thought among general medical inpatients, may be caused by early mobilization and shorter hospital stays. "We are really spending a lot of effort to prophylaxis something that’s" uncommon, without clear benefit and possible harm. "I think several of us will take [these findings] back to our hospitals to change our prophylaxis protocols," Dr. Kaatz said.
Consortium members came up with their own list of contraindications because "there’s not a lot of literature, unfortunately," to help, he noted. The list included brain metastases; intracranial monitoring devices; severe head or spine trauma within 24 hours; gastrointestinal, genitourinary or other hemorrhages within 6 months; intracranial hemorrhage within a year; and platelet counts below 50,000/mm3.
The Caprini score is one of several proposed to distinguish high-risk VTE patients from others, but in a third study, investigators found that it "did not effectively discriminate populations for which pharmacologic prophylaxis was useful." Scores of 5 or higher did predict risk, but among high-scorers, 0.72% who received prophylaxis – and 0.86% who did not – developed VTEs, an insignificant difference (P = .26). Michigan researchers have found other scoring systems to be problematic, as well.
"The mantra for years now has been to prophylaxis for VTEs, so a lot of us are treating to prophylaxis everybody," even low Caprini-score patients. "Now, we’re taking a step back. There’s a movement toward weighing VTE and bleeding risks. If we can find the population that doesn’t warrant prophylaxis, that would be a big step," said investigator Dr. Paul Grant, a hospitalist who is with the internal medicine department at the University of Michigan in Ann Arbor.
The consortium is funded by Blue Cross/Blue Shield of Michigan and the Blue Care Network. Dr. Grant has no disclosures. Dr. Kaatz is a speaker for Boehringer Ingelheim, Janssen, Daiichi Sankyo, and Bristol-Myers Squibb.
AT HOSPITAL MEDICINE 2014
Major finding: As VTE prophylaxis climbed from 59.2% to 77.9% over 2-plus years, the rate of symptomatic VTEs held steady at 0.56%, but major bleeds associated with prophylaxis increased from 0.2% to 0.6%.
Data Source: Observational studies involving tens of thousands of nonsurgical, non-ICU adult inpatients in Michigan hospitals.
Disclosures: The work was funded by Blue Cross Blue Shield of Michigan and the Blue Care Network. A principal investigator reports ties to Boehringer Ingelheim, Janssen, Daiichi Sankyo, and Pfizer-Bristol-Myers Squibb.
VIDEO: Treat insomnia in depressed, even suicidal people
LOS ANGELES – The relationship between depression, suicidality, and insomnia is more complex than once thought. Insomnia might contribute to the other problems and make them worse, instead of simply being a symptom of depression.
Dr. Vaughn McCall, professor and chairman of the department of psychiatry and health behavior at the Medical College of Georgia, Augusta, is running a randomized trial to see whether the judicious use of zolpidem (Ambien CR) improves the moods and outlooks of depressed patients on SSRIs who have active suicidal ideation. The results are still a few years away. In the meantime, he explains in this video from the American Association of Suicidology annual meeting that new or worsening insomnia cannot be ignored in depression. He also describes how to safely prescribe sleeping pills when necessary.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
LOS ANGELES – The relationship between depression, suicidality, and insomnia is more complex than once thought. Insomnia might contribute to the other problems and make them worse, instead of simply being a symptom of depression.
Dr. Vaughn McCall, professor and chairman of the department of psychiatry and health behavior at the Medical College of Georgia, Augusta, is running a randomized trial to see whether the judicious use of zolpidem (Ambien CR) improves the moods and outlooks of depressed patients on SSRIs who have active suicidal ideation. The results are still a few years away. In the meantime, he explains in this video from the American Association of Suicidology annual meeting that new or worsening insomnia cannot be ignored in depression. He also describes how to safely prescribe sleeping pills when necessary.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
LOS ANGELES – The relationship between depression, suicidality, and insomnia is more complex than once thought. Insomnia might contribute to the other problems and make them worse, instead of simply being a symptom of depression.
Dr. Vaughn McCall, professor and chairman of the department of psychiatry and health behavior at the Medical College of Georgia, Augusta, is running a randomized trial to see whether the judicious use of zolpidem (Ambien CR) improves the moods and outlooks of depressed patients on SSRIs who have active suicidal ideation. The results are still a few years away. In the meantime, he explains in this video from the American Association of Suicidology annual meeting that new or worsening insomnia cannot be ignored in depression. He also describes how to safely prescribe sleeping pills when necessary.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
EXPERT ANALYSIS FROM THE AAS ANNUAL CONFERENCE
VIDEO: Stick to safety concerns when discussing guns with patients
LOS ANGELES – It’s something on many providers’ minds these days: how to talk to patients and families about household guns when safety is a concern. Some U.S. doctors have gotten into trouble for even broaching the subject.
It’s key to keep the conversation about safety and not to let it veer into Second Amendment issues, said Elaine Frank, founder and program director of the Counseling on Access to Lethal Means (CALM) project at Dartmouth-Hitchcock Medical Center, Lebanon, N.H. She and her colleagues train providers about how to handle the topic.
An independent study presented at the American Association of Suicidology annual meeting found that clinicians are more likely to discuss guns with patients after the training, and more confident about doing so. Ms. Frank was on hand to hear the results, and she took a few moments to share her tips and insights.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
LOS ANGELES – It’s something on many providers’ minds these days: how to talk to patients and families about household guns when safety is a concern. Some U.S. doctors have gotten into trouble for even broaching the subject.
It’s key to keep the conversation about safety and not to let it veer into Second Amendment issues, said Elaine Frank, founder and program director of the Counseling on Access to Lethal Means (CALM) project at Dartmouth-Hitchcock Medical Center, Lebanon, N.H. She and her colleagues train providers about how to handle the topic.
An independent study presented at the American Association of Suicidology annual meeting found that clinicians are more likely to discuss guns with patients after the training, and more confident about doing so. Ms. Frank was on hand to hear the results, and she took a few moments to share her tips and insights.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
LOS ANGELES – It’s something on many providers’ minds these days: how to talk to patients and families about household guns when safety is a concern. Some U.S. doctors have gotten into trouble for even broaching the subject.
It’s key to keep the conversation about safety and not to let it veer into Second Amendment issues, said Elaine Frank, founder and program director of the Counseling on Access to Lethal Means (CALM) project at Dartmouth-Hitchcock Medical Center, Lebanon, N.H. She and her colleagues train providers about how to handle the topic.
An independent study presented at the American Association of Suicidology annual meeting found that clinicians are more likely to discuss guns with patients after the training, and more confident about doing so. Ms. Frank was on hand to hear the results, and she took a few moments to share her tips and insights.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT THE ANNUAL AAS CONFERENCE
Phytoestrogens may be helpful in asthma and allergy
SAN DIEGO – Could increased consumption of phytoestrogens help prevent or treat asthma and allergy?
Dr. Jessica Savage, an allergist and immunologist at Brigham and Women’s Hospital, Boston, and her colleagues correlated one-time urinary phytoestrogen measurements from 7,909 subjects in the National Health and Nutrition Examination Survey, 2003-2010, with histories of physician-diagnosed asthma and self-reported wheezing.
The investigators also considered serum total and specific IgE levels obtained from a subset of 2,218 subjects. They defined atopy as having at least one positive IgE level (0.35 kU/L or above) to an aeroallergen.
Adjusting for a wide range of potential cofounders, including age, gender, race, urinary creatinine, poverty, body mass index, smoking, and smoke exposure, they found that, for every natural log increase in urinary enterolactone, the odds of asthma decreased by 8%.
Enterolactone also was significantly inversely associated with asthma prevalence and had the strongest inverse association with wheezing.
For every natural log increase in urinary o-desmethylangolensin (ODMA), there was a 7% decrease in the odds of wheeze. The odds of atopy significantly decreased with increasing ODMA levels.
"We can’t say anything about cause and effect" yet, but if the association holds up with further investigation, it might suggest a role for phytoestrogen probiotics to help treat the conditions, Dr. Savage said at the annual meeting of the American Academy of Allergy, Asthma, and Immunology.
Phytoestrogens are plant-derived compounds. Gut bacteria convert lignans, which are particularly plentiful in flax seeds, into enterolactone, and the isoflavone daidzein, particularly plentiful in soybeans, into ODMA.
"Increased consumption of sources of phytoestrogens or probiotics to increase precursor conversion may help prevent or treat asthma and allergic disease," Dr. Savage said. "I was really surprised that the enterolactone signal is very strong both for asthma and for wheezing."
Although soy-derived compounds have been associated with better lung function and decreased lung symptoms in the past, "there’s really not a lot known about enterolactone," she said. "The idea is that somehow these metabolites are anti-inflammatory. Urinary levels are partly due to your diet and partly to having the right bacterial flora in your gut. Our findings could be explained by people just having different diets; they could also be explained by people with asthma having lower levels of the right kind of bacteria."
About half the subjects were female, and about 80% were over age 18 years; 70% of the study population was white. Enterolactone tertiles were defined as 0.2-178; 179-644; and 645-122,000 ng/mL urine. ODMA tertiles were defined as 0.1-1.4; 1.5-12.8; and 12.9-18,500 ng/mL urine.
The study was funded by the National Institutes of Health. The investigators reported having no disclosures.
Dr. Jennifer Cox, FCCP, comments: It is a novel idea that phytoestrogens could prevent or treat allergy and asthma. However,the this study population had few pediatric subjects, the majority of patients were white, and it was a one-time measurement. Before we recommend to our patients to increase consumption of phytoestrogens, further research to include pediatric patients, a more diverse ethnic background, and frequent monitoring of urinary levels will be helpful to document if there is a true cause and effect.
SAN DIEGO – Could increased consumption of phytoestrogens help prevent or treat asthma and allergy?
Dr. Jessica Savage, an allergist and immunologist at Brigham and Women’s Hospital, Boston, and her colleagues correlated one-time urinary phytoestrogen measurements from 7,909 subjects in the National Health and Nutrition Examination Survey, 2003-2010, with histories of physician-diagnosed asthma and self-reported wheezing.
The investigators also considered serum total and specific IgE levels obtained from a subset of 2,218 subjects. They defined atopy as having at least one positive IgE level (0.35 kU/L or above) to an aeroallergen.
Adjusting for a wide range of potential cofounders, including age, gender, race, urinary creatinine, poverty, body mass index, smoking, and smoke exposure, they found that, for every natural log increase in urinary enterolactone, the odds of asthma decreased by 8%.
Enterolactone also was significantly inversely associated with asthma prevalence and had the strongest inverse association with wheezing.
For every natural log increase in urinary o-desmethylangolensin (ODMA), there was a 7% decrease in the odds of wheeze. The odds of atopy significantly decreased with increasing ODMA levels.
"We can’t say anything about cause and effect" yet, but if the association holds up with further investigation, it might suggest a role for phytoestrogen probiotics to help treat the conditions, Dr. Savage said at the annual meeting of the American Academy of Allergy, Asthma, and Immunology.
Phytoestrogens are plant-derived compounds. Gut bacteria convert lignans, which are particularly plentiful in flax seeds, into enterolactone, and the isoflavone daidzein, particularly plentiful in soybeans, into ODMA.
"Increased consumption of sources of phytoestrogens or probiotics to increase precursor conversion may help prevent or treat asthma and allergic disease," Dr. Savage said. "I was really surprised that the enterolactone signal is very strong both for asthma and for wheezing."
Although soy-derived compounds have been associated with better lung function and decreased lung symptoms in the past, "there’s really not a lot known about enterolactone," she said. "The idea is that somehow these metabolites are anti-inflammatory. Urinary levels are partly due to your diet and partly to having the right bacterial flora in your gut. Our findings could be explained by people just having different diets; they could also be explained by people with asthma having lower levels of the right kind of bacteria."
About half the subjects were female, and about 80% were over age 18 years; 70% of the study population was white. Enterolactone tertiles were defined as 0.2-178; 179-644; and 645-122,000 ng/mL urine. ODMA tertiles were defined as 0.1-1.4; 1.5-12.8; and 12.9-18,500 ng/mL urine.
The study was funded by the National Institutes of Health. The investigators reported having no disclosures.
Dr. Jennifer Cox, FCCP, comments: It is a novel idea that phytoestrogens could prevent or treat allergy and asthma. However,the this study population had few pediatric subjects, the majority of patients were white, and it was a one-time measurement. Before we recommend to our patients to increase consumption of phytoestrogens, further research to include pediatric patients, a more diverse ethnic background, and frequent monitoring of urinary levels will be helpful to document if there is a true cause and effect.
SAN DIEGO – Could increased consumption of phytoestrogens help prevent or treat asthma and allergy?
Dr. Jessica Savage, an allergist and immunologist at Brigham and Women’s Hospital, Boston, and her colleagues correlated one-time urinary phytoestrogen measurements from 7,909 subjects in the National Health and Nutrition Examination Survey, 2003-2010, with histories of physician-diagnosed asthma and self-reported wheezing.
The investigators also considered serum total and specific IgE levels obtained from a subset of 2,218 subjects. They defined atopy as having at least one positive IgE level (0.35 kU/L or above) to an aeroallergen.
Adjusting for a wide range of potential cofounders, including age, gender, race, urinary creatinine, poverty, body mass index, smoking, and smoke exposure, they found that, for every natural log increase in urinary enterolactone, the odds of asthma decreased by 8%.
Enterolactone also was significantly inversely associated with asthma prevalence and had the strongest inverse association with wheezing.
For every natural log increase in urinary o-desmethylangolensin (ODMA), there was a 7% decrease in the odds of wheeze. The odds of atopy significantly decreased with increasing ODMA levels.
"We can’t say anything about cause and effect" yet, but if the association holds up with further investigation, it might suggest a role for phytoestrogen probiotics to help treat the conditions, Dr. Savage said at the annual meeting of the American Academy of Allergy, Asthma, and Immunology.
Phytoestrogens are plant-derived compounds. Gut bacteria convert lignans, which are particularly plentiful in flax seeds, into enterolactone, and the isoflavone daidzein, particularly plentiful in soybeans, into ODMA.
"Increased consumption of sources of phytoestrogens or probiotics to increase precursor conversion may help prevent or treat asthma and allergic disease," Dr. Savage said. "I was really surprised that the enterolactone signal is very strong both for asthma and for wheezing."
Although soy-derived compounds have been associated with better lung function and decreased lung symptoms in the past, "there’s really not a lot known about enterolactone," she said. "The idea is that somehow these metabolites are anti-inflammatory. Urinary levels are partly due to your diet and partly to having the right bacterial flora in your gut. Our findings could be explained by people just having different diets; they could also be explained by people with asthma having lower levels of the right kind of bacteria."
About half the subjects were female, and about 80% were over age 18 years; 70% of the study population was white. Enterolactone tertiles were defined as 0.2-178; 179-644; and 645-122,000 ng/mL urine. ODMA tertiles were defined as 0.1-1.4; 1.5-12.8; and 12.9-18,500 ng/mL urine.
The study was funded by the National Institutes of Health. The investigators reported having no disclosures.
Dr. Jennifer Cox, FCCP, comments: It is a novel idea that phytoestrogens could prevent or treat allergy and asthma. However,the this study population had few pediatric subjects, the majority of patients were white, and it was a one-time measurement. Before we recommend to our patients to increase consumption of phytoestrogens, further research to include pediatric patients, a more diverse ethnic background, and frequent monitoring of urinary levels will be helpful to document if there is a true cause and effect.
Major finding: For every natural log increase in urinary enterolactone, the odds of asthma decrease by 8%.
Data Source: The National Health and Nutrition Examination Survey 2003-2010.
Disclosures: The study was funded by the National Institutes of Health. The investigators reported no relevant disclosures.
Manual aspiration removes blood clots in more than half of ischemic stroke patients
SAN DIEGO – Manual, endoscopic clot aspiration restored cerebral blood flow in 66 (58.9%) of 112 acute ischemic stroke patients at the University of Pittsburgh Medical Center, according to a retrospective review.
When it failed, trying again with a stentriever ultimately restored flow on the thrombolysis in cerebral infarction scale (TICI 2b/3) in 97 (86.6%) patients, about the same rate of success as if a stentriever had been used in the first place. Patients needed a median of two passes.
Stentrievers are "the new technology that everyone is using, and they work very well, but they’re expensive," in the range of $5,000-$7,000, said investigator and interventional neurologist Dr. Ashutosh P. Jadhav.
"Our local practice is to use manual aspiration thrombectomy as our first pass. We are [often] able to do the procedure with just the catheter alone, which is a fifth of the price. We like it because it’s cost effective, and we are comfortable doing it. If the clot is refractory, then we move onto stentrievers," he said at the International Stroke Conference, sponsored by the American Heart Association (Tech. Vasc. Interv. Radiol. 2012;15:68-77).
The median time from symptom onset to groin puncture was 267 minutes. When manual aspiration was used alone, the mean procedural time was 63 minutes. When the team had to try again with a stentriever, the mean procedural time was 97 minutes (P less than .0001).
"Maybe if we did a trial against stentriever" on first pass, "we might find" trying manual aspiration first "takes a little bit longer, but we don’t have evidence of that right now," Dr. Jadhav of the UMPC Stroke Institute said.
Large-bore catheters – 0.07 inches and above – were used in about a quarter of the cases, and medium-bore catheters – 0.054-0.058 inches – in the rest. "Primary manual aspiration thrombectomy was carried out with a preference for the largest catheter considered to be trackable into the target lesion." Catheter make and size were not associated with higher or faster recanalization rates, Dr. Jadhav and his team noted.
"When we get the catheter into the clot, we pull back [on the attached 20 cc syringe] in one movement, so we don’t see a high rate of embolism. We did get a 9.8% risk of parenchymal hematoma, and a 6.2% risk of symptomatic hemorrhage," but the rates are "comparable to what people have seen with other therapies," he said. Four patients (3.6%) had intracranial distal wire perforations.
The median age in the series was 67 years, and median NIH stroke scale score was 17. Seventy patients (62.5%) were occluded in the first branch of the middle cerebral artery, and nine (8.0%) were occluded in the second branch. Twenty-one (18.8%) were occluded in the terminus of the internal carotid artery, and 12 (10.7%) had vertebrobasilar occlusions.
Almost half of the patients had 90-day modified Rankin Scale scores of 2 or less, but 35 (31.3%) had died at 3 months. Manual aspiration alone was not associated with better outcomes.
The investigators did not report outside funding. Dr. Jadhav said he has no disclosures.
SAN DIEGO – Manual, endoscopic clot aspiration restored cerebral blood flow in 66 (58.9%) of 112 acute ischemic stroke patients at the University of Pittsburgh Medical Center, according to a retrospective review.
When it failed, trying again with a stentriever ultimately restored flow on the thrombolysis in cerebral infarction scale (TICI 2b/3) in 97 (86.6%) patients, about the same rate of success as if a stentriever had been used in the first place. Patients needed a median of two passes.
Stentrievers are "the new technology that everyone is using, and they work very well, but they’re expensive," in the range of $5,000-$7,000, said investigator and interventional neurologist Dr. Ashutosh P. Jadhav.
"Our local practice is to use manual aspiration thrombectomy as our first pass. We are [often] able to do the procedure with just the catheter alone, which is a fifth of the price. We like it because it’s cost effective, and we are comfortable doing it. If the clot is refractory, then we move onto stentrievers," he said at the International Stroke Conference, sponsored by the American Heart Association (Tech. Vasc. Interv. Radiol. 2012;15:68-77).
The median time from symptom onset to groin puncture was 267 minutes. When manual aspiration was used alone, the mean procedural time was 63 minutes. When the team had to try again with a stentriever, the mean procedural time was 97 minutes (P less than .0001).
"Maybe if we did a trial against stentriever" on first pass, "we might find" trying manual aspiration first "takes a little bit longer, but we don’t have evidence of that right now," Dr. Jadhav of the UMPC Stroke Institute said.
Large-bore catheters – 0.07 inches and above – were used in about a quarter of the cases, and medium-bore catheters – 0.054-0.058 inches – in the rest. "Primary manual aspiration thrombectomy was carried out with a preference for the largest catheter considered to be trackable into the target lesion." Catheter make and size were not associated with higher or faster recanalization rates, Dr. Jadhav and his team noted.
"When we get the catheter into the clot, we pull back [on the attached 20 cc syringe] in one movement, so we don’t see a high rate of embolism. We did get a 9.8% risk of parenchymal hematoma, and a 6.2% risk of symptomatic hemorrhage," but the rates are "comparable to what people have seen with other therapies," he said. Four patients (3.6%) had intracranial distal wire perforations.
The median age in the series was 67 years, and median NIH stroke scale score was 17. Seventy patients (62.5%) were occluded in the first branch of the middle cerebral artery, and nine (8.0%) were occluded in the second branch. Twenty-one (18.8%) were occluded in the terminus of the internal carotid artery, and 12 (10.7%) had vertebrobasilar occlusions.
Almost half of the patients had 90-day modified Rankin Scale scores of 2 or less, but 35 (31.3%) had died at 3 months. Manual aspiration alone was not associated with better outcomes.
The investigators did not report outside funding. Dr. Jadhav said he has no disclosures.
SAN DIEGO – Manual, endoscopic clot aspiration restored cerebral blood flow in 66 (58.9%) of 112 acute ischemic stroke patients at the University of Pittsburgh Medical Center, according to a retrospective review.
When it failed, trying again with a stentriever ultimately restored flow on the thrombolysis in cerebral infarction scale (TICI 2b/3) in 97 (86.6%) patients, about the same rate of success as if a stentriever had been used in the first place. Patients needed a median of two passes.
Stentrievers are "the new technology that everyone is using, and they work very well, but they’re expensive," in the range of $5,000-$7,000, said investigator and interventional neurologist Dr. Ashutosh P. Jadhav.
"Our local practice is to use manual aspiration thrombectomy as our first pass. We are [often] able to do the procedure with just the catheter alone, which is a fifth of the price. We like it because it’s cost effective, and we are comfortable doing it. If the clot is refractory, then we move onto stentrievers," he said at the International Stroke Conference, sponsored by the American Heart Association (Tech. Vasc. Interv. Radiol. 2012;15:68-77).
The median time from symptom onset to groin puncture was 267 minutes. When manual aspiration was used alone, the mean procedural time was 63 minutes. When the team had to try again with a stentriever, the mean procedural time was 97 minutes (P less than .0001).
"Maybe if we did a trial against stentriever" on first pass, "we might find" trying manual aspiration first "takes a little bit longer, but we don’t have evidence of that right now," Dr. Jadhav of the UMPC Stroke Institute said.
Large-bore catheters – 0.07 inches and above – were used in about a quarter of the cases, and medium-bore catheters – 0.054-0.058 inches – in the rest. "Primary manual aspiration thrombectomy was carried out with a preference for the largest catheter considered to be trackable into the target lesion." Catheter make and size were not associated with higher or faster recanalization rates, Dr. Jadhav and his team noted.
"When we get the catheter into the clot, we pull back [on the attached 20 cc syringe] in one movement, so we don’t see a high rate of embolism. We did get a 9.8% risk of parenchymal hematoma, and a 6.2% risk of symptomatic hemorrhage," but the rates are "comparable to what people have seen with other therapies," he said. Four patients (3.6%) had intracranial distal wire perforations.
The median age in the series was 67 years, and median NIH stroke scale score was 17. Seventy patients (62.5%) were occluded in the first branch of the middle cerebral artery, and nine (8.0%) were occluded in the second branch. Twenty-one (18.8%) were occluded in the terminus of the internal carotid artery, and 12 (10.7%) had vertebrobasilar occlusions.
Almost half of the patients had 90-day modified Rankin Scale scores of 2 or less, but 35 (31.3%) had died at 3 months. Manual aspiration alone was not associated with better outcomes.
The investigators did not report outside funding. Dr. Jadhav said he has no disclosures.
AT THE INTERNATIONAL STROKE CONFERENCE
Major finding: Manual aspiration – without the aid of a stentriever – restores TICI 2b/3 blood flow in 58.9% of ischemic stroke patients.
Data source: A retrospective review of 112 acute ischemic stroke patients.
Disclosures: The investigators did not report outside funding. The presenter has no disclosures.
Start rapid status epilepticus protocol when convulsions go past 2 minutes
LAS VEGAS – The treatment window for generalized, convulsive status epilepticus has been compressed in recent years, something that’s important for hospitalists to know, according to Dr. Andrew Josephson, medical director of inpatient neurology at the University of California, San Francisco.
"We’ve figured out that, for every minute that goes by, brain cells are dying and the seizure is becoming more resistant to treatment," he said at the annual meeting of the Society of Hospital Medicine.
Previously, general anesthetics didn’t come into play for maybe an hour or more. "That’s not how we do it nowadays. If a spell goes on for longer than 2 minutes, that’s status epilepticus and should be treated as such," he said.
Lorazepam 2 mg IV comes first, every 2 minutes "until you’re worried about their airway" – generally after 4-8 doses. If lorazepam doses don’t work, patients are "loaded with IV fosphenytoin," not phenytoin, which is limb threatening if it infiltrates from the peripheral intravenous line. The dose of fosphenytoin is 18-20 mg/kg; a gram is insufficient in most adults, Dr. Josephson said.
Fosphenytoin takes about 10 minutes to run in. If patients are still seizing, "we generally go right to intubation, putting the patient in a suppressive state with general anesthetics. The things that we use are IV midazolam or IV propofol," he said.
"Keep in mind, we generally paralyze someone to intubate them, so they will stop shaking. That does not mean they have stopped seizing. So at this point, it’s extremely important that EEGs are taken when the patient is under general anesthesia," he said.
Follow-up in the hospital depends on whether it’s the patient’s first seizure or if he or she is a known epileptic.
Most first-time seizures in adults have an obvious explanation. Drugs and alcohol are high on the differential, along with meningitis/encephalitis. If the attack started focally, the patient has a brain tumor until proven otherwise. Low glucose also could be to blame, or low sodium, low magnesium, or low or high calcium.
Breakthrough seizures in known epileptics generally mean that something’s wrong with their antiepileptic medications – either they aren’t taking them or a new drug is interfering with them – or that they have a urinary tract infection, pneumonia, or some other systemic infection, and not necessarily a CNS infection.
Intramuscular midazolam has been in the news recently after it was found in a trial that 10 mg delivered by paramedics to the thigh by auto-injector works at least as well as intravenous lorazepam for status epilepticus (N. Engl. J. Med. 2012;366:591-600). Approval might come in 2014, and when it does the auto-injector is likely to "become the standard of care and benzodiazepine of choice for status epilepticus outside of the hospital and probably inside the hospital" since it’s far less cumbersome than fumbling with intravenous lines in the middle of a neurologic emergency, Dr. Josephson said.
Dr. Josephson has no relevant disclosures.
LAS VEGAS – The treatment window for generalized, convulsive status epilepticus has been compressed in recent years, something that’s important for hospitalists to know, according to Dr. Andrew Josephson, medical director of inpatient neurology at the University of California, San Francisco.
"We’ve figured out that, for every minute that goes by, brain cells are dying and the seizure is becoming more resistant to treatment," he said at the annual meeting of the Society of Hospital Medicine.
Previously, general anesthetics didn’t come into play for maybe an hour or more. "That’s not how we do it nowadays. If a spell goes on for longer than 2 minutes, that’s status epilepticus and should be treated as such," he said.
Lorazepam 2 mg IV comes first, every 2 minutes "until you’re worried about their airway" – generally after 4-8 doses. If lorazepam doses don’t work, patients are "loaded with IV fosphenytoin," not phenytoin, which is limb threatening if it infiltrates from the peripheral intravenous line. The dose of fosphenytoin is 18-20 mg/kg; a gram is insufficient in most adults, Dr. Josephson said.
Fosphenytoin takes about 10 minutes to run in. If patients are still seizing, "we generally go right to intubation, putting the patient in a suppressive state with general anesthetics. The things that we use are IV midazolam or IV propofol," he said.
"Keep in mind, we generally paralyze someone to intubate them, so they will stop shaking. That does not mean they have stopped seizing. So at this point, it’s extremely important that EEGs are taken when the patient is under general anesthesia," he said.
Follow-up in the hospital depends on whether it’s the patient’s first seizure or if he or she is a known epileptic.
Most first-time seizures in adults have an obvious explanation. Drugs and alcohol are high on the differential, along with meningitis/encephalitis. If the attack started focally, the patient has a brain tumor until proven otherwise. Low glucose also could be to blame, or low sodium, low magnesium, or low or high calcium.
Breakthrough seizures in known epileptics generally mean that something’s wrong with their antiepileptic medications – either they aren’t taking them or a new drug is interfering with them – or that they have a urinary tract infection, pneumonia, or some other systemic infection, and not necessarily a CNS infection.
Intramuscular midazolam has been in the news recently after it was found in a trial that 10 mg delivered by paramedics to the thigh by auto-injector works at least as well as intravenous lorazepam for status epilepticus (N. Engl. J. Med. 2012;366:591-600). Approval might come in 2014, and when it does the auto-injector is likely to "become the standard of care and benzodiazepine of choice for status epilepticus outside of the hospital and probably inside the hospital" since it’s far less cumbersome than fumbling with intravenous lines in the middle of a neurologic emergency, Dr. Josephson said.
Dr. Josephson has no relevant disclosures.
LAS VEGAS – The treatment window for generalized, convulsive status epilepticus has been compressed in recent years, something that’s important for hospitalists to know, according to Dr. Andrew Josephson, medical director of inpatient neurology at the University of California, San Francisco.
"We’ve figured out that, for every minute that goes by, brain cells are dying and the seizure is becoming more resistant to treatment," he said at the annual meeting of the Society of Hospital Medicine.
Previously, general anesthetics didn’t come into play for maybe an hour or more. "That’s not how we do it nowadays. If a spell goes on for longer than 2 minutes, that’s status epilepticus and should be treated as such," he said.
Lorazepam 2 mg IV comes first, every 2 minutes "until you’re worried about their airway" – generally after 4-8 doses. If lorazepam doses don’t work, patients are "loaded with IV fosphenytoin," not phenytoin, which is limb threatening if it infiltrates from the peripheral intravenous line. The dose of fosphenytoin is 18-20 mg/kg; a gram is insufficient in most adults, Dr. Josephson said.
Fosphenytoin takes about 10 minutes to run in. If patients are still seizing, "we generally go right to intubation, putting the patient in a suppressive state with general anesthetics. The things that we use are IV midazolam or IV propofol," he said.
"Keep in mind, we generally paralyze someone to intubate them, so they will stop shaking. That does not mean they have stopped seizing. So at this point, it’s extremely important that EEGs are taken when the patient is under general anesthesia," he said.
Follow-up in the hospital depends on whether it’s the patient’s first seizure or if he or she is a known epileptic.
Most first-time seizures in adults have an obvious explanation. Drugs and alcohol are high on the differential, along with meningitis/encephalitis. If the attack started focally, the patient has a brain tumor until proven otherwise. Low glucose also could be to blame, or low sodium, low magnesium, or low or high calcium.
Breakthrough seizures in known epileptics generally mean that something’s wrong with their antiepileptic medications – either they aren’t taking them or a new drug is interfering with them – or that they have a urinary tract infection, pneumonia, or some other systemic infection, and not necessarily a CNS infection.
Intramuscular midazolam has been in the news recently after it was found in a trial that 10 mg delivered by paramedics to the thigh by auto-injector works at least as well as intravenous lorazepam for status epilepticus (N. Engl. J. Med. 2012;366:591-600). Approval might come in 2014, and when it does the auto-injector is likely to "become the standard of care and benzodiazepine of choice for status epilepticus outside of the hospital and probably inside the hospital" since it’s far less cumbersome than fumbling with intravenous lines in the middle of a neurologic emergency, Dr. Josephson said.
Dr. Josephson has no relevant disclosures.
AT HOSPITAL MEDICINE 14
VIDEO: Feeding elderly patients after hip surgery
LAS VEGAS – Among 100 hip fracture patients at Salem (Ore.) Hospital, those fed within 24 hours left the hospital sooner, and fewer of them died. Other patients went up to a week without being fed.
Doctors might have overlooked nutrition or been put off by the notion that gastronomy feeding tubes don’t help in end-stage dementia. The Salem patients, however, didn’t have end-stage dementia and were being fed by nasogastric tubes. In an interview, Dr. Cynthia Wallace, medical director of Vibra Specialty Hospital in nearby Portland, explained that it’s time to broaden who’s authorized to order nutritional consults, so that patients don’t fall through the cracks.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
LAS VEGAS – Among 100 hip fracture patients at Salem (Ore.) Hospital, those fed within 24 hours left the hospital sooner, and fewer of them died. Other patients went up to a week without being fed.
Doctors might have overlooked nutrition or been put off by the notion that gastronomy feeding tubes don’t help in end-stage dementia. The Salem patients, however, didn’t have end-stage dementia and were being fed by nasogastric tubes. In an interview, Dr. Cynthia Wallace, medical director of Vibra Specialty Hospital in nearby Portland, explained that it’s time to broaden who’s authorized to order nutritional consults, so that patients don’t fall through the cracks.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
LAS VEGAS – Among 100 hip fracture patients at Salem (Ore.) Hospital, those fed within 24 hours left the hospital sooner, and fewer of them died. Other patients went up to a week without being fed.
Doctors might have overlooked nutrition or been put off by the notion that gastronomy feeding tubes don’t help in end-stage dementia. The Salem patients, however, didn’t have end-stage dementia and were being fed by nasogastric tubes. In an interview, Dr. Cynthia Wallace, medical director of Vibra Specialty Hospital in nearby Portland, explained that it’s time to broaden who’s authorized to order nutritional consults, so that patients don’t fall through the cracks.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Plasma fluoride levels tied to voriconazole-induced periostitis
LAS VEGAS – Check fluoride levels in patients on long-term voriconazole who present with new-onset bone pain, researchers at St. Joseph Mercy Hospital in Ann Arbor, Mich., advised after a retrospective investigation of 28 patients who were on the antifungal for a couple of months.
Plasma fluoride levels above 8 micromol/L are 95% sensitive (95% CI, 0.76-0.99) and 100% specific (95% CI, 0.59-1.0) for periostitis triggered by the fluorine atoms in the voriconazole molecule. Stopping the antifungal – or switching to one that does not contain fluorine, like itraconazole – is likely to clear the bone pain in a few weeks or months.
If bone scans can’t be ordered – or are too expensive – in voriconazole patients with skeletal pain, "getting a fluoride level is worthwhile. It’s much cheaper, and is very predictive" for voriconazole periostitis, said lead investigator Dr. Woo Moon of St. Joseph’s.
"One hundred percent of the patients who had periostitis had either involvement of the rib or ulna, and both in almost half of the cases," he said, noting that this is puzzling because previous reports of fluoride periostitis have been in the lower extremities.
The findings come in the wake of CNS fungal infections and abscesses caused by contaminated methylprednisolone injections in 2012 and 2013; 195 patients were treated at the hospital with voriconazole, as suggested by the Centers for Disease Control & Prevention because of the drug’s superior CNS penetration and activity against suspected pathogens.
Up to 59 patients (30%) reported pain in the ribs and arms after a couple months of treatment. The current investigation involved the 28 adult patients who had both fluoride level measurements and full-body scans to check for periostitis.
Plasma fluoride levels were significantly higher in the 21 (75%) who turned out to have periostitis (12.78 vs. 3.61 micromol/L, P less than .001). They were also on significantly higher doses of voriconazole (780 vs. 450 mg/day; P less than .001) and had significantly higher serum alkaline phosphatase levels (273 vs. 117 IU/L; P = .02). There were no differences in alanine transaminase, bilirubin, or creatinine levels.
Pain "improved dramatically" from 2 weeks to 5 months after discontinuation in 17 of the 19 (89%) patients who had pain outcomes noted in their records. Pain did not improve in the two others, Dr. Moon said at the annual meeting of the Society of Hospital Medicine.
Each molecule of voriconazole contains three fluorine atoms. At the recommended maintenance dose of 200 mg twice daily, "you’re taking in 65 mg of fluoride per day, 15 times the United States Department of Agriculture’s daily allowance," he said.
Voriconazole periostitis has been reported before in case studies and small series. However, because of the rib and ulna involvement, quick resolution after discontinuation, and strong predictive value of fluoride measurements, "we thought it was worthwhile to report our findings," he said.
Dr. Moon said she has no relevant financial disclosures, and the work received no outside funding.
LAS VEGAS – Check fluoride levels in patients on long-term voriconazole who present with new-onset bone pain, researchers at St. Joseph Mercy Hospital in Ann Arbor, Mich., advised after a retrospective investigation of 28 patients who were on the antifungal for a couple of months.
Plasma fluoride levels above 8 micromol/L are 95% sensitive (95% CI, 0.76-0.99) and 100% specific (95% CI, 0.59-1.0) for periostitis triggered by the fluorine atoms in the voriconazole molecule. Stopping the antifungal – or switching to one that does not contain fluorine, like itraconazole – is likely to clear the bone pain in a few weeks or months.
If bone scans can’t be ordered – or are too expensive – in voriconazole patients with skeletal pain, "getting a fluoride level is worthwhile. It’s much cheaper, and is very predictive" for voriconazole periostitis, said lead investigator Dr. Woo Moon of St. Joseph’s.
"One hundred percent of the patients who had periostitis had either involvement of the rib or ulna, and both in almost half of the cases," he said, noting that this is puzzling because previous reports of fluoride periostitis have been in the lower extremities.
The findings come in the wake of CNS fungal infections and abscesses caused by contaminated methylprednisolone injections in 2012 and 2013; 195 patients were treated at the hospital with voriconazole, as suggested by the Centers for Disease Control & Prevention because of the drug’s superior CNS penetration and activity against suspected pathogens.
Up to 59 patients (30%) reported pain in the ribs and arms after a couple months of treatment. The current investigation involved the 28 adult patients who had both fluoride level measurements and full-body scans to check for periostitis.
Plasma fluoride levels were significantly higher in the 21 (75%) who turned out to have periostitis (12.78 vs. 3.61 micromol/L, P less than .001). They were also on significantly higher doses of voriconazole (780 vs. 450 mg/day; P less than .001) and had significantly higher serum alkaline phosphatase levels (273 vs. 117 IU/L; P = .02). There were no differences in alanine transaminase, bilirubin, or creatinine levels.
Pain "improved dramatically" from 2 weeks to 5 months after discontinuation in 17 of the 19 (89%) patients who had pain outcomes noted in their records. Pain did not improve in the two others, Dr. Moon said at the annual meeting of the Society of Hospital Medicine.
Each molecule of voriconazole contains three fluorine atoms. At the recommended maintenance dose of 200 mg twice daily, "you’re taking in 65 mg of fluoride per day, 15 times the United States Department of Agriculture’s daily allowance," he said.
Voriconazole periostitis has been reported before in case studies and small series. However, because of the rib and ulna involvement, quick resolution after discontinuation, and strong predictive value of fluoride measurements, "we thought it was worthwhile to report our findings," he said.
Dr. Moon said she has no relevant financial disclosures, and the work received no outside funding.
LAS VEGAS – Check fluoride levels in patients on long-term voriconazole who present with new-onset bone pain, researchers at St. Joseph Mercy Hospital in Ann Arbor, Mich., advised after a retrospective investigation of 28 patients who were on the antifungal for a couple of months.
Plasma fluoride levels above 8 micromol/L are 95% sensitive (95% CI, 0.76-0.99) and 100% specific (95% CI, 0.59-1.0) for periostitis triggered by the fluorine atoms in the voriconazole molecule. Stopping the antifungal – or switching to one that does not contain fluorine, like itraconazole – is likely to clear the bone pain in a few weeks or months.
If bone scans can’t be ordered – or are too expensive – in voriconazole patients with skeletal pain, "getting a fluoride level is worthwhile. It’s much cheaper, and is very predictive" for voriconazole periostitis, said lead investigator Dr. Woo Moon of St. Joseph’s.
"One hundred percent of the patients who had periostitis had either involvement of the rib or ulna, and both in almost half of the cases," he said, noting that this is puzzling because previous reports of fluoride periostitis have been in the lower extremities.
The findings come in the wake of CNS fungal infections and abscesses caused by contaminated methylprednisolone injections in 2012 and 2013; 195 patients were treated at the hospital with voriconazole, as suggested by the Centers for Disease Control & Prevention because of the drug’s superior CNS penetration and activity against suspected pathogens.
Up to 59 patients (30%) reported pain in the ribs and arms after a couple months of treatment. The current investigation involved the 28 adult patients who had both fluoride level measurements and full-body scans to check for periostitis.
Plasma fluoride levels were significantly higher in the 21 (75%) who turned out to have periostitis (12.78 vs. 3.61 micromol/L, P less than .001). They were also on significantly higher doses of voriconazole (780 vs. 450 mg/day; P less than .001) and had significantly higher serum alkaline phosphatase levels (273 vs. 117 IU/L; P = .02). There were no differences in alanine transaminase, bilirubin, or creatinine levels.
Pain "improved dramatically" from 2 weeks to 5 months after discontinuation in 17 of the 19 (89%) patients who had pain outcomes noted in their records. Pain did not improve in the two others, Dr. Moon said at the annual meeting of the Society of Hospital Medicine.
Each molecule of voriconazole contains three fluorine atoms. At the recommended maintenance dose of 200 mg twice daily, "you’re taking in 65 mg of fluoride per day, 15 times the United States Department of Agriculture’s daily allowance," he said.
Voriconazole periostitis has been reported before in case studies and small series. However, because of the rib and ulna involvement, quick resolution after discontinuation, and strong predictive value of fluoride measurements, "we thought it was worthwhile to report our findings," he said.
Dr. Moon said she has no relevant financial disclosures, and the work received no outside funding.
AT HOSPITAL MEDICINE 2014
Major finding: Plasma fluoride levels above 8 micromol/L are 95% sensitive (95% CI 0.76-0.99) and 100% specific (95% CI 0.59-1.0) for periostitis triggered by the fluorine atoms in voriconazole.
Data Source: A retrospective investigation of 28 adult patients who developed bone pain after a couple months on the antifungal.
Disclosures: The lead investigator said she has no relevant financial disclosures, and the work received no outside funding.
VIDEO: Rethink the VTE prophylaxis mantra
LAS VEGAS – Venous thromboembolism prophylaxis – a sine qua non of the Joint Commission and others – doesn’t seem to prevent deep vein thrombosis or pulmonary embolism in hospitalized medical patients, but it does make them more likely to bleed, according to investigators from the Michigan Hospital Medicine Safety Consortium.
The findings are prompting one of those investigators to reassess his own approach. In an interview at the Society of Hospital Medicine’s 2014 meeting, Dr. Scott Kaatz, chief quality officer at Hurley Medical Center in Flint, Mich., told us how he’s thinking a bit differently these days when it comes to VTE prophylaxis in medical inpatients.
LAS VEGAS – Venous thromboembolism prophylaxis – a sine qua non of the Joint Commission and others – doesn’t seem to prevent deep vein thrombosis or pulmonary embolism in hospitalized medical patients, but it does make them more likely to bleed, according to investigators from the Michigan Hospital Medicine Safety Consortium.
The findings are prompting one of those investigators to reassess his own approach. In an interview at the Society of Hospital Medicine’s 2014 meeting, Dr. Scott Kaatz, chief quality officer at Hurley Medical Center in Flint, Mich., told us how he’s thinking a bit differently these days when it comes to VTE prophylaxis in medical inpatients.
LAS VEGAS – Venous thromboembolism prophylaxis – a sine qua non of the Joint Commission and others – doesn’t seem to prevent deep vein thrombosis or pulmonary embolism in hospitalized medical patients, but it does make them more likely to bleed, according to investigators from the Michigan Hospital Medicine Safety Consortium.
The findings are prompting one of those investigators to reassess his own approach. In an interview at the Society of Hospital Medicine’s 2014 meeting, Dr. Scott Kaatz, chief quality officer at Hurley Medical Center in Flint, Mich., told us how he’s thinking a bit differently these days when it comes to VTE prophylaxis in medical inpatients.
AT HOSPITAL MEDICINE 2014
Challenge-test physical urticaria patients to verify triggers
SAN DIEGO – Approximately one-quarter of patients diagnosed with physical urticaria actually responded when challenged, based on data from a study conducted at the National Institutes of Health.
Before patients change their lives and start taking antihistamines for a physical urticaria, they need to be challenge tested to make sure they actually have one, the researchers noted.
"Some of these patients were taking a lot of medication for no reason," generally antihistamines, but, at least in one patient who tested negative, cyclosporine and methotrexate, said lead investigator Dr. Hirsh Komarow, a staff clinician at the NIH’s National Institute of Allergy and Infectious Diseases.
Among 73 patients diagnosed with a physical urticaria and referred to NIH by their allergist or dermatologist, 19 (26%) did not develop hives from their presumed trigger or any others after exhaustive challenge testing. The patients had been off antihistamines for at least a week to ensure that their reactions weren’t blunted.
Nine patients (12%) did not react to their presumed trigger but reacted to others, and 45 (62%) reacted to their presumed trigger.
The rate of negative challenges was low in cold-induced (8/32, 25%) and delayed-pressure urticaria and dermatographism (2/7, 29% in both cases), but high in cholinergic (14/21, 67%) and solar (2/3, 67%) urticaria. Negative challenges were more than twice as likely in women as in men. All of the five negative patients rechallenged a year later remained negative.
Because of the time and resources involved with challenge testing, "allergists often rely on a patient history for diagnosis and selection of intervention strategies," but the physical urticarias "should be verified ... particularly when severe" enough to require life-style changes and medication, the researchers noted. "Physicians that are unable to perform testing ... may consider referral to a tertiary center for evaluation."
Overall, patients reported symptoms for an average of 9 years. Patients who tested negative reported symptoms for a mean of 6 years. It’s possible that these patients had a physical urticaria at one point, but, "Maybe it went away. Most of these go away in 5 years," Dr. Komarow said at the annual meeting of the American Academy of Allergy, Asthma, and Immunology.
In general, physical urticaria patients change their lives to avoid triggers. "There are a million things they do. People who react to cold, for instance, won’t go skiing, they won’t go swimming, and they won’t go to the football game with their kids. They won’t go to the frozen foods section of the supermarket," Dr. Komarow said. Cholinergic urticaria patients "won’t exercise. They won’t go in the sauna; they won’t go in the hot tub. Once they find out they don’t have physical urticaria or that it’s very mild, they say ‘I feel free,’" he said.
The subjects had been referred to NIH for participation in a large, ongoing physical urticaria trial headed by Dr. Komarow.
Their median age was 31 years, and 48 (66 %) were women. The 19 challenge-negative patients were slightly younger, with a mean age of 28 years. The majority of subjects overall, and those who were challenge-negative, rated their symptoms as moderate to severe. About half the subjects in the study had atopic tendencies, detected by serum IgE and other measures.
Among other techniques, cold urticaria was challenged with beakers full of ice water, cholinergic urticaria with treadmill exercise, and solar urticaria with sun lamps. Patients were then observed over 24 hours.
The work was funded by NIH. Dr. Komarow has no relevant disclosures.
SAN DIEGO – Approximately one-quarter of patients diagnosed with physical urticaria actually responded when challenged, based on data from a study conducted at the National Institutes of Health.
Before patients change their lives and start taking antihistamines for a physical urticaria, they need to be challenge tested to make sure they actually have one, the researchers noted.
"Some of these patients were taking a lot of medication for no reason," generally antihistamines, but, at least in one patient who tested negative, cyclosporine and methotrexate, said lead investigator Dr. Hirsh Komarow, a staff clinician at the NIH’s National Institute of Allergy and Infectious Diseases.
Among 73 patients diagnosed with a physical urticaria and referred to NIH by their allergist or dermatologist, 19 (26%) did not develop hives from their presumed trigger or any others after exhaustive challenge testing. The patients had been off antihistamines for at least a week to ensure that their reactions weren’t blunted.
Nine patients (12%) did not react to their presumed trigger but reacted to others, and 45 (62%) reacted to their presumed trigger.
The rate of negative challenges was low in cold-induced (8/32, 25%) and delayed-pressure urticaria and dermatographism (2/7, 29% in both cases), but high in cholinergic (14/21, 67%) and solar (2/3, 67%) urticaria. Negative challenges were more than twice as likely in women as in men. All of the five negative patients rechallenged a year later remained negative.
Because of the time and resources involved with challenge testing, "allergists often rely on a patient history for diagnosis and selection of intervention strategies," but the physical urticarias "should be verified ... particularly when severe" enough to require life-style changes and medication, the researchers noted. "Physicians that are unable to perform testing ... may consider referral to a tertiary center for evaluation."
Overall, patients reported symptoms for an average of 9 years. Patients who tested negative reported symptoms for a mean of 6 years. It’s possible that these patients had a physical urticaria at one point, but, "Maybe it went away. Most of these go away in 5 years," Dr. Komarow said at the annual meeting of the American Academy of Allergy, Asthma, and Immunology.
In general, physical urticaria patients change their lives to avoid triggers. "There are a million things they do. People who react to cold, for instance, won’t go skiing, they won’t go swimming, and they won’t go to the football game with their kids. They won’t go to the frozen foods section of the supermarket," Dr. Komarow said. Cholinergic urticaria patients "won’t exercise. They won’t go in the sauna; they won’t go in the hot tub. Once they find out they don’t have physical urticaria or that it’s very mild, they say ‘I feel free,’" he said.
The subjects had been referred to NIH for participation in a large, ongoing physical urticaria trial headed by Dr. Komarow.
Their median age was 31 years, and 48 (66 %) were women. The 19 challenge-negative patients were slightly younger, with a mean age of 28 years. The majority of subjects overall, and those who were challenge-negative, rated their symptoms as moderate to severe. About half the subjects in the study had atopic tendencies, detected by serum IgE and other measures.
Among other techniques, cold urticaria was challenged with beakers full of ice water, cholinergic urticaria with treadmill exercise, and solar urticaria with sun lamps. Patients were then observed over 24 hours.
The work was funded by NIH. Dr. Komarow has no relevant disclosures.
SAN DIEGO – Approximately one-quarter of patients diagnosed with physical urticaria actually responded when challenged, based on data from a study conducted at the National Institutes of Health.
Before patients change their lives and start taking antihistamines for a physical urticaria, they need to be challenge tested to make sure they actually have one, the researchers noted.
"Some of these patients were taking a lot of medication for no reason," generally antihistamines, but, at least in one patient who tested negative, cyclosporine and methotrexate, said lead investigator Dr. Hirsh Komarow, a staff clinician at the NIH’s National Institute of Allergy and Infectious Diseases.
Among 73 patients diagnosed with a physical urticaria and referred to NIH by their allergist or dermatologist, 19 (26%) did not develop hives from their presumed trigger or any others after exhaustive challenge testing. The patients had been off antihistamines for at least a week to ensure that their reactions weren’t blunted.
Nine patients (12%) did not react to their presumed trigger but reacted to others, and 45 (62%) reacted to their presumed trigger.
The rate of negative challenges was low in cold-induced (8/32, 25%) and delayed-pressure urticaria and dermatographism (2/7, 29% in both cases), but high in cholinergic (14/21, 67%) and solar (2/3, 67%) urticaria. Negative challenges were more than twice as likely in women as in men. All of the five negative patients rechallenged a year later remained negative.
Because of the time and resources involved with challenge testing, "allergists often rely on a patient history for diagnosis and selection of intervention strategies," but the physical urticarias "should be verified ... particularly when severe" enough to require life-style changes and medication, the researchers noted. "Physicians that are unable to perform testing ... may consider referral to a tertiary center for evaluation."
Overall, patients reported symptoms for an average of 9 years. Patients who tested negative reported symptoms for a mean of 6 years. It’s possible that these patients had a physical urticaria at one point, but, "Maybe it went away. Most of these go away in 5 years," Dr. Komarow said at the annual meeting of the American Academy of Allergy, Asthma, and Immunology.
In general, physical urticaria patients change their lives to avoid triggers. "There are a million things they do. People who react to cold, for instance, won’t go skiing, they won’t go swimming, and they won’t go to the football game with their kids. They won’t go to the frozen foods section of the supermarket," Dr. Komarow said. Cholinergic urticaria patients "won’t exercise. They won’t go in the sauna; they won’t go in the hot tub. Once they find out they don’t have physical urticaria or that it’s very mild, they say ‘I feel free,’" he said.
The subjects had been referred to NIH for participation in a large, ongoing physical urticaria trial headed by Dr. Komarow.
Their median age was 31 years, and 48 (66 %) were women. The 19 challenge-negative patients were slightly younger, with a mean age of 28 years. The majority of subjects overall, and those who were challenge-negative, rated their symptoms as moderate to severe. About half the subjects in the study had atopic tendencies, detected by serum IgE and other measures.
Among other techniques, cold urticaria was challenged with beakers full of ice water, cholinergic urticaria with treadmill exercise, and solar urticaria with sun lamps. Patients were then observed over 24 hours.
The work was funded by NIH. Dr. Komarow has no relevant disclosures.
EXPERT ANALYSIS FROM THE 2014 AAAAI ANNUAL MEETING
Major finding: 26% of patients diagnosed with a physical urticaria and referred to NIH by their allergist or dermatologist did not develop hives from their presumed trigger or any others after exhaustive challenge testing.
Data source: Prospective study of 73 adults with diagnosed physical urticaria.
Disclosures: The work was funded by NIH. The lead investigator has no relevant disclosures.