User login
Risk of Steep SGR Cut Looms Again
Physicians are once again waiting for Congress to avert a 27% Medicare physician fee cut scheduled to take effect on March 1.
The pay cut was originally scheduled to begin Jan. 1, but after much back-and-forth in Congress, the House and Senate passed the Temporary Payroll Tax Cut Continuation Act of 2011 on Dec. 23, which included an extension of 2011 Medicare physician-payment rates through the end of February. President Obama quickly signed the bill into law.
Lawmakers also agreed to appoint a 20-member House-Senate committee to work on a longer-term plan to address the Medicare physician pay issue, along with a full-year extension of the Social Security payroll tax holiday and federally funded unemployment insurance benefits.
The agreement followed several days of brinksmanship by leaders in the House and Senate. It started on Dec. 13, when the House passed a bill that would have replaced the 27% Medicare fee cut with a 1% pay raise for physicians for 2 years. Despite bipartisan support for the so-called doc fix, other controversial provisions in the bill kept it from gaining traction in the Senate. A few days later, the Senate approved their own version of the bill, which extended the payroll tax holiday and unemployment benefits for 2 months and postponed any Medicare cuts until the end of February.
The House initially rejected a short-term fix, and even passed a resolution to formally disagree with the legislation passed by the Senate. But intense public criticism led House leaders to agree to the short-term plan and use the first 2 months of this year to negotiate a compromise.
Physicians remain furious with Congress for its inability to find a long-term solution in 2011. "There’s a tremendous degree of frustration out there," said Robert Doherty, senior vice president for government affairs and public policy at the American College of Physicians. "If Congress is expecting physicians to applaud them for agreeing to a 2-month extension, they’re going to find a lot of silence from the physician community."
Frustration is especially high because members of Congress had signaled early in 2011 that they were interested in crafting a long-term solution to replace the Sustainable Growth Rate formula, the statutory formula that ties spending on physicians’ services to the gross domestic product. In March 2011, leaders in the House Energy and Commerce Committee wrote to several physicians’ groups asking for proposals on how to reform the physician payment system and move to a new system that "reduces spending, pays providers fairly, and pays for services according to their value to the beneficiary."
The letter emphasized the need to act quickly in developing a long-term solution, or risk the "unwanted choice of extending a fundamentally broken payment system or jeopardizing access to care" for Medicare beneficiaries. "We cannot let either happen," the lawmakers wrote.
It’s too soon to tell what Congress will do next, but Mr. Doherty agreed that a long-term solution that would replace the SGR is unlikely right now.
In a worse-case scenario, physicians could be facing a situation similar to 2010, when Congress passed a series of temporary patches during the first half of the year, Mr. Doherty said. That situation could become a reality if lawmakers once again are deadlocked on the larger legislative package. "To a great extent, we’re once again going to be held hostage to negotiations over a broader package on issues that really have nothing to do with the SGR."☐
Physicians are once again waiting for Congress to avert a 27% Medicare physician fee cut scheduled to take effect on March 1.
The pay cut was originally scheduled to begin Jan. 1, but after much back-and-forth in Congress, the House and Senate passed the Temporary Payroll Tax Cut Continuation Act of 2011 on Dec. 23, which included an extension of 2011 Medicare physician-payment rates through the end of February. President Obama quickly signed the bill into law.
Lawmakers also agreed to appoint a 20-member House-Senate committee to work on a longer-term plan to address the Medicare physician pay issue, along with a full-year extension of the Social Security payroll tax holiday and federally funded unemployment insurance benefits.
The agreement followed several days of brinksmanship by leaders in the House and Senate. It started on Dec. 13, when the House passed a bill that would have replaced the 27% Medicare fee cut with a 1% pay raise for physicians for 2 years. Despite bipartisan support for the so-called doc fix, other controversial provisions in the bill kept it from gaining traction in the Senate. A few days later, the Senate approved their own version of the bill, which extended the payroll tax holiday and unemployment benefits for 2 months and postponed any Medicare cuts until the end of February.
The House initially rejected a short-term fix, and even passed a resolution to formally disagree with the legislation passed by the Senate. But intense public criticism led House leaders to agree to the short-term plan and use the first 2 months of this year to negotiate a compromise.
Physicians remain furious with Congress for its inability to find a long-term solution in 2011. "There’s a tremendous degree of frustration out there," said Robert Doherty, senior vice president for government affairs and public policy at the American College of Physicians. "If Congress is expecting physicians to applaud them for agreeing to a 2-month extension, they’re going to find a lot of silence from the physician community."
Frustration is especially high because members of Congress had signaled early in 2011 that they were interested in crafting a long-term solution to replace the Sustainable Growth Rate formula, the statutory formula that ties spending on physicians’ services to the gross domestic product. In March 2011, leaders in the House Energy and Commerce Committee wrote to several physicians’ groups asking for proposals on how to reform the physician payment system and move to a new system that "reduces spending, pays providers fairly, and pays for services according to their value to the beneficiary."
The letter emphasized the need to act quickly in developing a long-term solution, or risk the "unwanted choice of extending a fundamentally broken payment system or jeopardizing access to care" for Medicare beneficiaries. "We cannot let either happen," the lawmakers wrote.
It’s too soon to tell what Congress will do next, but Mr. Doherty agreed that a long-term solution that would replace the SGR is unlikely right now.
In a worse-case scenario, physicians could be facing a situation similar to 2010, when Congress passed a series of temporary patches during the first half of the year, Mr. Doherty said. That situation could become a reality if lawmakers once again are deadlocked on the larger legislative package. "To a great extent, we’re once again going to be held hostage to negotiations over a broader package on issues that really have nothing to do with the SGR."☐
Physicians are once again waiting for Congress to avert a 27% Medicare physician fee cut scheduled to take effect on March 1.
The pay cut was originally scheduled to begin Jan. 1, but after much back-and-forth in Congress, the House and Senate passed the Temporary Payroll Tax Cut Continuation Act of 2011 on Dec. 23, which included an extension of 2011 Medicare physician-payment rates through the end of February. President Obama quickly signed the bill into law.
Lawmakers also agreed to appoint a 20-member House-Senate committee to work on a longer-term plan to address the Medicare physician pay issue, along with a full-year extension of the Social Security payroll tax holiday and federally funded unemployment insurance benefits.
The agreement followed several days of brinksmanship by leaders in the House and Senate. It started on Dec. 13, when the House passed a bill that would have replaced the 27% Medicare fee cut with a 1% pay raise for physicians for 2 years. Despite bipartisan support for the so-called doc fix, other controversial provisions in the bill kept it from gaining traction in the Senate. A few days later, the Senate approved their own version of the bill, which extended the payroll tax holiday and unemployment benefits for 2 months and postponed any Medicare cuts until the end of February.
The House initially rejected a short-term fix, and even passed a resolution to formally disagree with the legislation passed by the Senate. But intense public criticism led House leaders to agree to the short-term plan and use the first 2 months of this year to negotiate a compromise.
Physicians remain furious with Congress for its inability to find a long-term solution in 2011. "There’s a tremendous degree of frustration out there," said Robert Doherty, senior vice president for government affairs and public policy at the American College of Physicians. "If Congress is expecting physicians to applaud them for agreeing to a 2-month extension, they’re going to find a lot of silence from the physician community."
Frustration is especially high because members of Congress had signaled early in 2011 that they were interested in crafting a long-term solution to replace the Sustainable Growth Rate formula, the statutory formula that ties spending on physicians’ services to the gross domestic product. In March 2011, leaders in the House Energy and Commerce Committee wrote to several physicians’ groups asking for proposals on how to reform the physician payment system and move to a new system that "reduces spending, pays providers fairly, and pays for services according to their value to the beneficiary."
The letter emphasized the need to act quickly in developing a long-term solution, or risk the "unwanted choice of extending a fundamentally broken payment system or jeopardizing access to care" for Medicare beneficiaries. "We cannot let either happen," the lawmakers wrote.
It’s too soon to tell what Congress will do next, but Mr. Doherty agreed that a long-term solution that would replace the SGR is unlikely right now.
In a worse-case scenario, physicians could be facing a situation similar to 2010, when Congress passed a series of temporary patches during the first half of the year, Mr. Doherty said. That situation could become a reality if lawmakers once again are deadlocked on the larger legislative package. "To a great extent, we’re once again going to be held hostage to negotiations over a broader package on issues that really have nothing to do with the SGR."☐
Safety Improvements Needed in Health IT
As physicians and hospitals gear up to implement electronic health records and other health information technology products, the federal government should increase its scrutiny of these products to ensure that they don’t actually contribute to medical errors.
That was the conclusion of an Institute of Medicine panel, which called on the Health and Human Services Department to assess potential safety risks associated with health IT and come up with a plan to minimize those risks. The plan should be published in 2012, with new reports each year, according to the panel’s recommendations.
But if the HHS secretary determines that the industry is falling short of the safety goals, the Food and Drug Administration should be tasked with regulating electronic health records, personal health records, and health information exchanges, the IOM committee recommended. The IOM study was sponsored by HHS.
The report http://www.iom.edu/Reports/2011/Health-IT-and-Patient-Safety-Building-Safer-Systems-for-Better-Care.aspx comes as physicians and hospitals strive to qualify for federal incentive payments for the use of health IT products to meet certain quality benchmarks. The program includes bonus payments in the early years, followed later by penalties if they fail to adopt health IT.
"Based on the literature, HIT certainly has clear and demonstrated potential to improve the safety and the quality of patient care, but it also can cause harm. We’ve heard about that," said Dr. Paul C. Tang, a member of the IOM committee and vice president and chief innovation and technology officer at Palo Alto (Calif.) Medical Foundation.
Although evidence demonstrates that health IT systems have helped to improve medication safety in some places, the literature is inconclusive about IT’s safety benefits in other areas, Dr. Tang said. And there are reports of harm associated with using these systems, from dosing errors to delays in treatment, according to the report.
But right now it’s difficult to quantify the safety issues because unlike drugs or devices, health IT software is installed and used differently from institution to institution, said Dr. Tang, who also serves as the vice chair on the HIT Policy Committee, which advises the federal government on the development of a nationwide health information infrastructure.
In addition, there is a wide array of different types of health IT products on the market. There are also contractual issues, such as confidentiality clauses, that may make it difficult for users to share safety concerns about the products, according to the IOM report. The IOM panel made a series of recommendations aimed at improving the information available on the safety risks and benefits associated with health IT use.
For instance, the panel called on HHS to develop a way for health IT users and vendors to report adverse events related to health IT. And the panel members urged Congress to establish an independent federal entity charged with investigating those adverse events. The body could be modeled on the National Transportation Safety Board, he said. ☐
As physicians and hospitals gear up to implement electronic health records and other health information technology products, the federal government should increase its scrutiny of these products to ensure that they don’t actually contribute to medical errors.
That was the conclusion of an Institute of Medicine panel, which called on the Health and Human Services Department to assess potential safety risks associated with health IT and come up with a plan to minimize those risks. The plan should be published in 2012, with new reports each year, according to the panel’s recommendations.
But if the HHS secretary determines that the industry is falling short of the safety goals, the Food and Drug Administration should be tasked with regulating electronic health records, personal health records, and health information exchanges, the IOM committee recommended. The IOM study was sponsored by HHS.
The report http://www.iom.edu/Reports/2011/Health-IT-and-Patient-Safety-Building-Safer-Systems-for-Better-Care.aspx comes as physicians and hospitals strive to qualify for federal incentive payments for the use of health IT products to meet certain quality benchmarks. The program includes bonus payments in the early years, followed later by penalties if they fail to adopt health IT.
"Based on the literature, HIT certainly has clear and demonstrated potential to improve the safety and the quality of patient care, but it also can cause harm. We’ve heard about that," said Dr. Paul C. Tang, a member of the IOM committee and vice president and chief innovation and technology officer at Palo Alto (Calif.) Medical Foundation.
Although evidence demonstrates that health IT systems have helped to improve medication safety in some places, the literature is inconclusive about IT’s safety benefits in other areas, Dr. Tang said. And there are reports of harm associated with using these systems, from dosing errors to delays in treatment, according to the report.
But right now it’s difficult to quantify the safety issues because unlike drugs or devices, health IT software is installed and used differently from institution to institution, said Dr. Tang, who also serves as the vice chair on the HIT Policy Committee, which advises the federal government on the development of a nationwide health information infrastructure.
In addition, there is a wide array of different types of health IT products on the market. There are also contractual issues, such as confidentiality clauses, that may make it difficult for users to share safety concerns about the products, according to the IOM report. The IOM panel made a series of recommendations aimed at improving the information available on the safety risks and benefits associated with health IT use.
For instance, the panel called on HHS to develop a way for health IT users and vendors to report adverse events related to health IT. And the panel members urged Congress to establish an independent federal entity charged with investigating those adverse events. The body could be modeled on the National Transportation Safety Board, he said. ☐
As physicians and hospitals gear up to implement electronic health records and other health information technology products, the federal government should increase its scrutiny of these products to ensure that they don’t actually contribute to medical errors.
That was the conclusion of an Institute of Medicine panel, which called on the Health and Human Services Department to assess potential safety risks associated with health IT and come up with a plan to minimize those risks. The plan should be published in 2012, with new reports each year, according to the panel’s recommendations.
But if the HHS secretary determines that the industry is falling short of the safety goals, the Food and Drug Administration should be tasked with regulating electronic health records, personal health records, and health information exchanges, the IOM committee recommended. The IOM study was sponsored by HHS.
The report http://www.iom.edu/Reports/2011/Health-IT-and-Patient-Safety-Building-Safer-Systems-for-Better-Care.aspx comes as physicians and hospitals strive to qualify for federal incentive payments for the use of health IT products to meet certain quality benchmarks. The program includes bonus payments in the early years, followed later by penalties if they fail to adopt health IT.
"Based on the literature, HIT certainly has clear and demonstrated potential to improve the safety and the quality of patient care, but it also can cause harm. We’ve heard about that," said Dr. Paul C. Tang, a member of the IOM committee and vice president and chief innovation and technology officer at Palo Alto (Calif.) Medical Foundation.
Although evidence demonstrates that health IT systems have helped to improve medication safety in some places, the literature is inconclusive about IT’s safety benefits in other areas, Dr. Tang said. And there are reports of harm associated with using these systems, from dosing errors to delays in treatment, according to the report.
But right now it’s difficult to quantify the safety issues because unlike drugs or devices, health IT software is installed and used differently from institution to institution, said Dr. Tang, who also serves as the vice chair on the HIT Policy Committee, which advises the federal government on the development of a nationwide health information infrastructure.
In addition, there is a wide array of different types of health IT products on the market. There are also contractual issues, such as confidentiality clauses, that may make it difficult for users to share safety concerns about the products, according to the IOM report. The IOM panel made a series of recommendations aimed at improving the information available on the safety risks and benefits associated with health IT use.
For instance, the panel called on HHS to develop a way for health IT users and vendors to report adverse events related to health IT. And the panel members urged Congress to establish an independent federal entity charged with investigating those adverse events. The body could be modeled on the National Transportation Safety Board, he said. ☐
Physicians Lack Time, Tools for Medicare's Cognitive Screening Benefit
Primary care physicians have one more item on their to-do lists: screening for cognitive impairment among Medicare beneficiaries.
Under section 4103 of the Affordable Care Act, Congress added a new benefit that provides full coverage for an Annual Wellness Visit for all Medicare beneficiaries. The visit is designed not as an annual physical, but as a preventive checkup, where the physician can design and update a long-range care plan and monitor the patient’s individual risk factors. As part of this visit, physicians are required by Medicare to assess the patient’s cognitive function using a combination of direct observation and patient and family reports.
But 1 year after the new Medicare benefit went into effect, Jan. 1, 2011, physicians aren’t spending a lot of time performing cognitive screening. Part of the reason is that they aren’t performing these annual wellness visits all that often.
"If you don’t have a half an hour to obtain a history from an informant and do a mental status exam, it’s not going to get done."
"A lot of patients don’t ask for that exam, at least not in our neck of the woods," said Dr. Eric Tangalos, an internist and professor of medicine at the Mayo Clinic in Rochester, Minn.
And he said physicians aren’t likely to suggest scheduling the Medicare Annual Wellness Visit starting at age 65, because some of the testing doesn’t have much clinical relevance that would aid in the care of patients. "The science behind an annual wellness examination is minimal," he said.
Another problem with the exam requirements is that the provider must develop a personalized prevention plan that includes a written screening schedule for the next 5-10 years. That requirement is not only time consuming, but could be difficult for practices that don’t use electronic health records, Dr. Tangalos said.
But if the Medicare Annual Wellness Visit does become more common, physicians and other providers are likely to need more guidance on what to do as part of the cognitive screening. Officials at the Centers for Medicare and Medicaid Services have instructed providers to assess cognitive function based on their direct observation, the patient’s own reports, and information from family members, friends, and caregivers. But they haven’t recommended any specific screening instruments or set other parameters for the testing.
CMS turned to the National Institute on Aging (NIA) to look into the issue. Officials at the NIA have been working on the project for the last year, meeting with experts and evaluating published brief cognitive screening instruments. Some of the issues they are looking at include the cost of the screens and how long they take to perform, said Molly Wagster, Ph.D., chief of the Behavioral and Systems Neuroscience of Aging Branch at the NIA. They are also looking into whether the screening instruments are valid and reliable and if they are appropriate for racial and ethnic minority groups.
NIA officials also are considering whether it makes sense to conduct the assessments in a targeted way. For example, they are looking at whether or not individuals aged 65 to 75 should be automatically screened and what risk factors might be appropriate in triggering a formal screening test. NIA officials expect to complete their work this year, Dr. Wagster said.
Dr. Tangalos, who also serves as codirector for education at the Mayo Alzheimer’s Disease Research Center, said he doesn’t view routine cognitive impairment screening among 65-year-olds as beneficial because the incidence of disease is still low in that age group. Dr. Tangalos prefers to focus on at-risk populations, such as anyone moving into an assisted living facility, or moving from their home to another city. "Those things just don’t happen by accident," he said. "That, by definition, is someone at risk."
Prioritizing patients for screening based on age and other risk factors makes sense, said Dr. Howard Fillit, executive director of the Alzheimer’s Drug Discovery Foundation. The organization has been a proponent of including the cognitive assessment in the annual wellness visit, but Dr. Fillit, who is a geriatrician, said they also understand that the busy primary care physician is being asked to do a lot of things in that exam. It may make sense to screen patients annually starting around age 70 or 75 instead, he said, when the exponential increase in prevalence makes it a greater priority within the wellness exam.
The CMS language requiring cognitive impairment screening in the annual wellness exam is fairly vague, Dr. Fillit said, which gives physicians some leeway in whether or not to do formalized screening in every patient receiving the exam. If a patient is 65 years old, plays tennis everyday, continues to run a business, and his wife has no concerns about his memory, that’s probably not the best candidate for performing a cognitive impairment screen, he said.
Time is likely to be the biggest problem for primary care physicians trying to add cognitive screening to their exams, said Dr. David Knopman, professor of neurology at the Mayo Clinic in Rochester, Minn. "If you don’t have a half an hour to obtain a history from an informant and do a mental status exam, it’s not going to get done," he said.
To do the screening properly, Dr. Knopman said physicians need to set aside enough time to perform the standardized screening tests and to speak with an informant, usually a spouse or adult child who knows the patient well. He advises practices to arrange in advance to have the informant present whenever a cognitive assessment is being performed.
Dr. Jacobo Mintzer, professor of neuroscience at the Medical University of South Carolina, Charleston, and chair of the scientific advisory committee at the Alzheimer’s Foundation of America, said he thinks that as time goes on cognitive impairment screening will become a standard part of the exam for all older adults, much like a blood pressure check. "At some point it becomes part of the basic consult that the patient receives," he said.
But not all primary care physicians will be comfortable diagnosing and treating dementia patients, he said, just as some physicians prefer to refer patients for cardiology conditions. His advice: "Know what you don’t know."
Dr. Marwan Sabbagh, a geriatric neurologist and director of the Banner Sun Health Research Institute in Sun City, Ariz., agrees that many primary care physicians aren’t comfortable making a diagnosis of Alzheimer’s disease, disclosing that diagnosis, and recommending treatment. The problem, he said, is that there just aren’t enough neurologists to go around.
There is a shortage of general neurologists, but when it comes to subspecialist neurologists who are specially trained to deal with issues of aging, the situation is even worse. The United Council for Neurologic Subspecialties have developed a certification pathway for geriatric neurologists and more fellowships in dementia and geriatric neurology are being created, Dr. Sabbagh said, but it will take years for those efforts to produce more physicians trained to care for dementia patients. "There is a huge gap," he said.
Primary care physicians have one more item on their to-do lists: screening for cognitive impairment among Medicare beneficiaries.
Under section 4103 of the Affordable Care Act, Congress added a new benefit that provides full coverage for an Annual Wellness Visit for all Medicare beneficiaries. The visit is designed not as an annual physical, but as a preventive checkup, where the physician can design and update a long-range care plan and monitor the patient’s individual risk factors. As part of this visit, physicians are required by Medicare to assess the patient’s cognitive function using a combination of direct observation and patient and family reports.
But 1 year after the new Medicare benefit went into effect, Jan. 1, 2011, physicians aren’t spending a lot of time performing cognitive screening. Part of the reason is that they aren’t performing these annual wellness visits all that often.
"If you don’t have a half an hour to obtain a history from an informant and do a mental status exam, it’s not going to get done."
"A lot of patients don’t ask for that exam, at least not in our neck of the woods," said Dr. Eric Tangalos, an internist and professor of medicine at the Mayo Clinic in Rochester, Minn.
And he said physicians aren’t likely to suggest scheduling the Medicare Annual Wellness Visit starting at age 65, because some of the testing doesn’t have much clinical relevance that would aid in the care of patients. "The science behind an annual wellness examination is minimal," he said.
Another problem with the exam requirements is that the provider must develop a personalized prevention plan that includes a written screening schedule for the next 5-10 years. That requirement is not only time consuming, but could be difficult for practices that don’t use electronic health records, Dr. Tangalos said.
But if the Medicare Annual Wellness Visit does become more common, physicians and other providers are likely to need more guidance on what to do as part of the cognitive screening. Officials at the Centers for Medicare and Medicaid Services have instructed providers to assess cognitive function based on their direct observation, the patient’s own reports, and information from family members, friends, and caregivers. But they haven’t recommended any specific screening instruments or set other parameters for the testing.
CMS turned to the National Institute on Aging (NIA) to look into the issue. Officials at the NIA have been working on the project for the last year, meeting with experts and evaluating published brief cognitive screening instruments. Some of the issues they are looking at include the cost of the screens and how long they take to perform, said Molly Wagster, Ph.D., chief of the Behavioral and Systems Neuroscience of Aging Branch at the NIA. They are also looking into whether the screening instruments are valid and reliable and if they are appropriate for racial and ethnic minority groups.
NIA officials also are considering whether it makes sense to conduct the assessments in a targeted way. For example, they are looking at whether or not individuals aged 65 to 75 should be automatically screened and what risk factors might be appropriate in triggering a formal screening test. NIA officials expect to complete their work this year, Dr. Wagster said.
Dr. Tangalos, who also serves as codirector for education at the Mayo Alzheimer’s Disease Research Center, said he doesn’t view routine cognitive impairment screening among 65-year-olds as beneficial because the incidence of disease is still low in that age group. Dr. Tangalos prefers to focus on at-risk populations, such as anyone moving into an assisted living facility, or moving from their home to another city. "Those things just don’t happen by accident," he said. "That, by definition, is someone at risk."
Prioritizing patients for screening based on age and other risk factors makes sense, said Dr. Howard Fillit, executive director of the Alzheimer’s Drug Discovery Foundation. The organization has been a proponent of including the cognitive assessment in the annual wellness visit, but Dr. Fillit, who is a geriatrician, said they also understand that the busy primary care physician is being asked to do a lot of things in that exam. It may make sense to screen patients annually starting around age 70 or 75 instead, he said, when the exponential increase in prevalence makes it a greater priority within the wellness exam.
The CMS language requiring cognitive impairment screening in the annual wellness exam is fairly vague, Dr. Fillit said, which gives physicians some leeway in whether or not to do formalized screening in every patient receiving the exam. If a patient is 65 years old, plays tennis everyday, continues to run a business, and his wife has no concerns about his memory, that’s probably not the best candidate for performing a cognitive impairment screen, he said.
Time is likely to be the biggest problem for primary care physicians trying to add cognitive screening to their exams, said Dr. David Knopman, professor of neurology at the Mayo Clinic in Rochester, Minn. "If you don’t have a half an hour to obtain a history from an informant and do a mental status exam, it’s not going to get done," he said.
To do the screening properly, Dr. Knopman said physicians need to set aside enough time to perform the standardized screening tests and to speak with an informant, usually a spouse or adult child who knows the patient well. He advises practices to arrange in advance to have the informant present whenever a cognitive assessment is being performed.
Dr. Jacobo Mintzer, professor of neuroscience at the Medical University of South Carolina, Charleston, and chair of the scientific advisory committee at the Alzheimer’s Foundation of America, said he thinks that as time goes on cognitive impairment screening will become a standard part of the exam for all older adults, much like a blood pressure check. "At some point it becomes part of the basic consult that the patient receives," he said.
But not all primary care physicians will be comfortable diagnosing and treating dementia patients, he said, just as some physicians prefer to refer patients for cardiology conditions. His advice: "Know what you don’t know."
Dr. Marwan Sabbagh, a geriatric neurologist and director of the Banner Sun Health Research Institute in Sun City, Ariz., agrees that many primary care physicians aren’t comfortable making a diagnosis of Alzheimer’s disease, disclosing that diagnosis, and recommending treatment. The problem, he said, is that there just aren’t enough neurologists to go around.
There is a shortage of general neurologists, but when it comes to subspecialist neurologists who are specially trained to deal with issues of aging, the situation is even worse. The United Council for Neurologic Subspecialties have developed a certification pathway for geriatric neurologists and more fellowships in dementia and geriatric neurology are being created, Dr. Sabbagh said, but it will take years for those efforts to produce more physicians trained to care for dementia patients. "There is a huge gap," he said.
Primary care physicians have one more item on their to-do lists: screening for cognitive impairment among Medicare beneficiaries.
Under section 4103 of the Affordable Care Act, Congress added a new benefit that provides full coverage for an Annual Wellness Visit for all Medicare beneficiaries. The visit is designed not as an annual physical, but as a preventive checkup, where the physician can design and update a long-range care plan and monitor the patient’s individual risk factors. As part of this visit, physicians are required by Medicare to assess the patient’s cognitive function using a combination of direct observation and patient and family reports.
But 1 year after the new Medicare benefit went into effect, Jan. 1, 2011, physicians aren’t spending a lot of time performing cognitive screening. Part of the reason is that they aren’t performing these annual wellness visits all that often.
"If you don’t have a half an hour to obtain a history from an informant and do a mental status exam, it’s not going to get done."
"A lot of patients don’t ask for that exam, at least not in our neck of the woods," said Dr. Eric Tangalos, an internist and professor of medicine at the Mayo Clinic in Rochester, Minn.
And he said physicians aren’t likely to suggest scheduling the Medicare Annual Wellness Visit starting at age 65, because some of the testing doesn’t have much clinical relevance that would aid in the care of patients. "The science behind an annual wellness examination is minimal," he said.
Another problem with the exam requirements is that the provider must develop a personalized prevention plan that includes a written screening schedule for the next 5-10 years. That requirement is not only time consuming, but could be difficult for practices that don’t use electronic health records, Dr. Tangalos said.
But if the Medicare Annual Wellness Visit does become more common, physicians and other providers are likely to need more guidance on what to do as part of the cognitive screening. Officials at the Centers for Medicare and Medicaid Services have instructed providers to assess cognitive function based on their direct observation, the patient’s own reports, and information from family members, friends, and caregivers. But they haven’t recommended any specific screening instruments or set other parameters for the testing.
CMS turned to the National Institute on Aging (NIA) to look into the issue. Officials at the NIA have been working on the project for the last year, meeting with experts and evaluating published brief cognitive screening instruments. Some of the issues they are looking at include the cost of the screens and how long they take to perform, said Molly Wagster, Ph.D., chief of the Behavioral and Systems Neuroscience of Aging Branch at the NIA. They are also looking into whether the screening instruments are valid and reliable and if they are appropriate for racial and ethnic minority groups.
NIA officials also are considering whether it makes sense to conduct the assessments in a targeted way. For example, they are looking at whether or not individuals aged 65 to 75 should be automatically screened and what risk factors might be appropriate in triggering a formal screening test. NIA officials expect to complete their work this year, Dr. Wagster said.
Dr. Tangalos, who also serves as codirector for education at the Mayo Alzheimer’s Disease Research Center, said he doesn’t view routine cognitive impairment screening among 65-year-olds as beneficial because the incidence of disease is still low in that age group. Dr. Tangalos prefers to focus on at-risk populations, such as anyone moving into an assisted living facility, or moving from their home to another city. "Those things just don’t happen by accident," he said. "That, by definition, is someone at risk."
Prioritizing patients for screening based on age and other risk factors makes sense, said Dr. Howard Fillit, executive director of the Alzheimer’s Drug Discovery Foundation. The organization has been a proponent of including the cognitive assessment in the annual wellness visit, but Dr. Fillit, who is a geriatrician, said they also understand that the busy primary care physician is being asked to do a lot of things in that exam. It may make sense to screen patients annually starting around age 70 or 75 instead, he said, when the exponential increase in prevalence makes it a greater priority within the wellness exam.
The CMS language requiring cognitive impairment screening in the annual wellness exam is fairly vague, Dr. Fillit said, which gives physicians some leeway in whether or not to do formalized screening in every patient receiving the exam. If a patient is 65 years old, plays tennis everyday, continues to run a business, and his wife has no concerns about his memory, that’s probably not the best candidate for performing a cognitive impairment screen, he said.
Time is likely to be the biggest problem for primary care physicians trying to add cognitive screening to their exams, said Dr. David Knopman, professor of neurology at the Mayo Clinic in Rochester, Minn. "If you don’t have a half an hour to obtain a history from an informant and do a mental status exam, it’s not going to get done," he said.
To do the screening properly, Dr. Knopman said physicians need to set aside enough time to perform the standardized screening tests and to speak with an informant, usually a spouse or adult child who knows the patient well. He advises practices to arrange in advance to have the informant present whenever a cognitive assessment is being performed.
Dr. Jacobo Mintzer, professor of neuroscience at the Medical University of South Carolina, Charleston, and chair of the scientific advisory committee at the Alzheimer’s Foundation of America, said he thinks that as time goes on cognitive impairment screening will become a standard part of the exam for all older adults, much like a blood pressure check. "At some point it becomes part of the basic consult that the patient receives," he said.
But not all primary care physicians will be comfortable diagnosing and treating dementia patients, he said, just as some physicians prefer to refer patients for cardiology conditions. His advice: "Know what you don’t know."
Dr. Marwan Sabbagh, a geriatric neurologist and director of the Banner Sun Health Research Institute in Sun City, Ariz., agrees that many primary care physicians aren’t comfortable making a diagnosis of Alzheimer’s disease, disclosing that diagnosis, and recommending treatment. The problem, he said, is that there just aren’t enough neurologists to go around.
There is a shortage of general neurologists, but when it comes to subspecialist neurologists who are specially trained to deal with issues of aging, the situation is even worse. The United Council for Neurologic Subspecialties have developed a certification pathway for geriatric neurologists and more fellowships in dementia and geriatric neurology are being created, Dr. Sabbagh said, but it will take years for those efforts to produce more physicians trained to care for dementia patients. "There is a huge gap," he said.
Baby Can Wait: Hospitals Curb Early Elective Deliveries
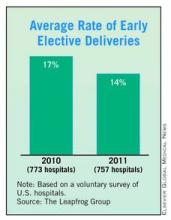
Hospitals appear to be making progress in keeping down the number of elective deliveries performed before 39 weeks’ gestation, according to data from the Leapfrog Group's annual hospital survey.
The survey of 757 hospitals found that 39% of reporting hospitals had early elective delivery rates of 5% or less in 2011, compared with 30% the previous year. And the average rate for early elective deliveries among these hospitals dropped from 17% to 14% between 2010 and 2011.
But there is still wide variation, with rates ranging from a low of less than 5% to more than 40%, according to the Leapfrog data.
"Of the hospitals that reported an elective delivery rate in 2010 and 2011, 65% improved their performance. This is extremely promising news. We are making a difference in the lives of women and newborns," Leapfrog CEO Leah Binder said in a written statement. "But there is still work to be done. We are seeing far too many newborns delivered early and without a medical reason, and there are still a number of hospitals who refuse to make this information public."
The Leapfrog Group, a coalition of public and private purchasers of employee health benefits that works on health care quality improvement, began collecting data on early elective deliveries in 2009 and first publicly reported hospital data in 2010. The group has identified the trend toward early deliveries as both a safety and economic issue. For instance, women who are induced in weeks 37 and 38 have a higher risk of needing a cesarean section than women who go into labor on their own.
Studies have also linked early elective deliveries to postpartum complications such as hematoma, wound dehiscence, anemia, endometriosis, urinary tract infections, and sepsis, according to the Leapfrog Group. On the economic side, early deliveries tend to be more costly. One estimate published in 2010 finds that nearly $1 billion in U.S. health care costs could be saved each year by reducing the early delivery rate by 1.7%. Those savings would be achieved mainly by reducing the number of days newborns spend in neonatal intensive care units (Am. J. Obstet. Gynecol. 2010;203:e1-6).
As part of the Leapfrog survey, hospitals were asked to report on the percentage of nonmedically indicated deliveries by induction or cesarean section between 37 and 39 completed weeks of gestation. These are deliveries in which the mothers had not already gone into active labor or experienced a spontaneous rupture of membranes.
Hospitals appear to be making progress in keeping down the number of elective deliveries performed before 39 weeks’ gestation, according to data from the Leapfrog Group's annual hospital survey.
The survey of 757 hospitals found that 39% of reporting hospitals had early elective delivery rates of 5% or less in 2011, compared with 30% the previous year. And the average rate for early elective deliveries among these hospitals dropped from 17% to 14% between 2010 and 2011.
But there is still wide variation, with rates ranging from a low of less than 5% to more than 40%, according to the Leapfrog data.
"Of the hospitals that reported an elective delivery rate in 2010 and 2011, 65% improved their performance. This is extremely promising news. We are making a difference in the lives of women and newborns," Leapfrog CEO Leah Binder said in a written statement. "But there is still work to be done. We are seeing far too many newborns delivered early and without a medical reason, and there are still a number of hospitals who refuse to make this information public."
The Leapfrog Group, a coalition of public and private purchasers of employee health benefits that works on health care quality improvement, began collecting data on early elective deliveries in 2009 and first publicly reported hospital data in 2010. The group has identified the trend toward early deliveries as both a safety and economic issue. For instance, women who are induced in weeks 37 and 38 have a higher risk of needing a cesarean section than women who go into labor on their own.
Studies have also linked early elective deliveries to postpartum complications such as hematoma, wound dehiscence, anemia, endometriosis, urinary tract infections, and sepsis, according to the Leapfrog Group. On the economic side, early deliveries tend to be more costly. One estimate published in 2010 finds that nearly $1 billion in U.S. health care costs could be saved each year by reducing the early delivery rate by 1.7%. Those savings would be achieved mainly by reducing the number of days newborns spend in neonatal intensive care units (Am. J. Obstet. Gynecol. 2010;203:e1-6).
As part of the Leapfrog survey, hospitals were asked to report on the percentage of nonmedically indicated deliveries by induction or cesarean section between 37 and 39 completed weeks of gestation. These are deliveries in which the mothers had not already gone into active labor or experienced a spontaneous rupture of membranes.
Hospitals appear to be making progress in keeping down the number of elective deliveries performed before 39 weeks’ gestation, according to data from the Leapfrog Group's annual hospital survey.
The survey of 757 hospitals found that 39% of reporting hospitals had early elective delivery rates of 5% or less in 2011, compared with 30% the previous year. And the average rate for early elective deliveries among these hospitals dropped from 17% to 14% between 2010 and 2011.
But there is still wide variation, with rates ranging from a low of less than 5% to more than 40%, according to the Leapfrog data.
"Of the hospitals that reported an elective delivery rate in 2010 and 2011, 65% improved their performance. This is extremely promising news. We are making a difference in the lives of women and newborns," Leapfrog CEO Leah Binder said in a written statement. "But there is still work to be done. We are seeing far too many newborns delivered early and without a medical reason, and there are still a number of hospitals who refuse to make this information public."
The Leapfrog Group, a coalition of public and private purchasers of employee health benefits that works on health care quality improvement, began collecting data on early elective deliveries in 2009 and first publicly reported hospital data in 2010. The group has identified the trend toward early deliveries as both a safety and economic issue. For instance, women who are induced in weeks 37 and 38 have a higher risk of needing a cesarean section than women who go into labor on their own.
Studies have also linked early elective deliveries to postpartum complications such as hematoma, wound dehiscence, anemia, endometriosis, urinary tract infections, and sepsis, according to the Leapfrog Group. On the economic side, early deliveries tend to be more costly. One estimate published in 2010 finds that nearly $1 billion in U.S. health care costs could be saved each year by reducing the early delivery rate by 1.7%. Those savings would be achieved mainly by reducing the number of days newborns spend in neonatal intensive care units (Am. J. Obstet. Gynecol. 2010;203:e1-6).
As part of the Leapfrog survey, hospitals were asked to report on the percentage of nonmedically indicated deliveries by induction or cesarean section between 37 and 39 completed weeks of gestation. These are deliveries in which the mothers had not already gone into active labor or experienced a spontaneous rupture of membranes.
FROM THE LEAPFROG GROUP
Leaders: Preventing Hemorrhage Through Research, Team Care
Dr. Margaret Fang, the medical director of the Anticoagulation Clinic at the University of California, San Francisco, has spent the past several years studying ways to prevent hemorrhage in older Americans through proper anticoagulation therapy. As a member of the Kaiser Permanente of North California ATRIA (Anticoagulation and Risk Factors in Atrial Fibrillation) Study Group, she is investigating thromboembolic and hemorrhagic outcomes among more than 13,000 atrial fibrillation patients. Most recently, she and her research collaborators developed and evaluated a new risk stratification scoring system to assess the likelihood of anticoagulant-related bleeding in atrial fibrillation patients. (J. Am. Coll. Cardiol. 2011; 58: 395-401).
In an interview with Hospitalist News, Dr. Fang explained some of the recent findings from the ATRIA Study Group and offered her views on the best role for hospitalists in assuring proper anticoagulation therapy.
Hospitalist News: In a recent study, your team evaluated a tool to assess the risk of bleeding in atrial fibrillation patients. How would that tool be used clinically?
DR. FANG: We developed a bleeding risk score called the ATRIA bleed score. It’s specifically designed to be used in patients who are taking anticoagulants. Our goal was to try to use clinical factors to help clinicians and patients estimate the risk of having a major bleeding event while taking an anticoagulant.
There are stroke risk–stratification schemes out there that I think are more widely used in patients who have atrial fibrillation. These are based on their clinical factors and can estimate their annual risk of stroke. Anticoagulants have complications of bleeding too, so it’s important to describe what we think a patient’s risk of bleeding is while on therapy. This score used five fairly easily available clinical factors. Based on whether patients have these risk factors or not, we can counsel them about what their likelihood of having a bleed is in a given year. The range can be as low as less than 1% to nearly 18% per year. Depending on where a patient falls in that risk spectrum and their estimated risk of stroke, you can then decide whether or not it’s worth proceeding with taking anticoagulants.
HN: Do clinicians tend to overestimate bleeding risk?
DR. FANG: I think so. If you look at practice patterns of whether patients with atrial fibrillation are prescribed anticoagulants or not, it shows that almost half of eligible patients are not taking anticoagulants. When you survey physicians as to whether that’s because of a knowledge deficit or something else that’s keeping them from prescribing anticoagulants, the dominant reason is that they think the patient has too high of a bleeding risk or it’s too hard to control or manage the anticoagulants for a given patient. Even though a lot of studies have shown that the consequences of having a stroke are much more severe than the consequences of having a bleed on therapy, a significant proportion of patients with atrial fibrillation are not prescribed anticoagulants.
HN: If the ATRIA bleed score were widely used, would there be more patients who could take advantage of anticoagulation therapy?
DR. FANG: By using this tool, clinicians can find not only the very high-risk patients, but also may be reassured that on average their patients have a lower risk of bleed than what they may have anticipated. They may find that the bleeding risk is not as high as they thought, especially when used in conjunction with a stroke risk scheme.
The other thing to consider is that prescribing anticoagulants will always be a decision that is made with a great deal of patient involvement. So, tools like a stroke risk calculator or a bleeding risk calculator facilitate that discussion and help the patient understand the risks and benefits of therapy.
HN: What does the Anticoagulation Clinic at UCSF do, and how is this different from how anticoagulation is managed at other hospitals?
DR. FANG: Our anticoagulation clinic manages about 600 patients taking chronic anticoagulants. It’s staffed by nurse practitioners and pharmacists who are all trained in anticoagulant management and in our anticoagulation protocols. As the medical director, I’m the only physician who is part of this clinic, and I serve in more of a supervisory role in which I can provide clinical input where needed and help develop standardized protocols and practice patterns. Many of the anticoagulation clinics are built in similar ways.
In the past, much of the anticoagulation management was handled by individual practitioners, such as primary care physicians. But there was an increasing body of literature to support the use of anticoagulation clinics, so now many larger institutions have an anticoagulation management service and an anticoagulation clinic. Some may have physicians working there, but I think that the majority have an interdisciplinary team with pharmacists and nurse practitioners managing most of the patients.
HN: What’s the role of the hospitalist in anticoagulation management?
DR. FANG: Hospitalists pay quite a lot of attention to transitions of care. Attending on the medical service, I understand a little bit about both what people know and what they don’t know about the referral and transitions processes when moving someone to an outpatient anticoagulation clinic. I serve as a liaison and try to think of ways to smooth that transition.
HN: What are the future research areas that are ripe to explore in the anticoagulation field?
DR. FANG: One of the most exciting areas is the development of newer anticoagulants that do not require the frequent blood tests and monitoring that warfarin does. Right now, our anticoagulation clinic exists because warfarin is very challenging to manage and requires very frequent visits. There are newer anticoagulants such as dabigatran and rivaroxaban and several others that are in the pipeline that may obviate the need for warfarin and therefore for anticoagulation clinics.
We know these newer agents seem as good as, if not better than, warfarin in very controlled settings and clinical trials, but we don’t know how they work in the potentially sicker, more difficult to manage populations that we see in the real world. There are certain indications and certain comorbidities that should make clinicians really cautious about using these agents. For instance, we don’t know these agents would perform in older individuals or in those who have renal disease. It’s important to figure out how clinicians are prescribing and using these medications, who they are using them in, and whether the outcomes in the real world are as good as those we’ve seen in clinical trials.
Take us to your leader. Nominate a hospitalist whose work inspires you. E-mail suggestions to m.schneider@elsevier.com. Read previous columns at ehospitalistnews.com.
Dr. Margaret Fang, the medical director of the Anticoagulation Clinic at the University of California, San Francisco, has spent the past several years studying ways to prevent hemorrhage in older Americans through proper anticoagulation therapy. As a member of the Kaiser Permanente of North California ATRIA (Anticoagulation and Risk Factors in Atrial Fibrillation) Study Group, she is investigating thromboembolic and hemorrhagic outcomes among more than 13,000 atrial fibrillation patients. Most recently, she and her research collaborators developed and evaluated a new risk stratification scoring system to assess the likelihood of anticoagulant-related bleeding in atrial fibrillation patients. (J. Am. Coll. Cardiol. 2011; 58: 395-401).
In an interview with Hospitalist News, Dr. Fang explained some of the recent findings from the ATRIA Study Group and offered her views on the best role for hospitalists in assuring proper anticoagulation therapy.
Hospitalist News: In a recent study, your team evaluated a tool to assess the risk of bleeding in atrial fibrillation patients. How would that tool be used clinically?
DR. FANG: We developed a bleeding risk score called the ATRIA bleed score. It’s specifically designed to be used in patients who are taking anticoagulants. Our goal was to try to use clinical factors to help clinicians and patients estimate the risk of having a major bleeding event while taking an anticoagulant.
There are stroke risk–stratification schemes out there that I think are more widely used in patients who have atrial fibrillation. These are based on their clinical factors and can estimate their annual risk of stroke. Anticoagulants have complications of bleeding too, so it’s important to describe what we think a patient’s risk of bleeding is while on therapy. This score used five fairly easily available clinical factors. Based on whether patients have these risk factors or not, we can counsel them about what their likelihood of having a bleed is in a given year. The range can be as low as less than 1% to nearly 18% per year. Depending on where a patient falls in that risk spectrum and their estimated risk of stroke, you can then decide whether or not it’s worth proceeding with taking anticoagulants.
HN: Do clinicians tend to overestimate bleeding risk?
DR. FANG: I think so. If you look at practice patterns of whether patients with atrial fibrillation are prescribed anticoagulants or not, it shows that almost half of eligible patients are not taking anticoagulants. When you survey physicians as to whether that’s because of a knowledge deficit or something else that’s keeping them from prescribing anticoagulants, the dominant reason is that they think the patient has too high of a bleeding risk or it’s too hard to control or manage the anticoagulants for a given patient. Even though a lot of studies have shown that the consequences of having a stroke are much more severe than the consequences of having a bleed on therapy, a significant proportion of patients with atrial fibrillation are not prescribed anticoagulants.
HN: If the ATRIA bleed score were widely used, would there be more patients who could take advantage of anticoagulation therapy?
DR. FANG: By using this tool, clinicians can find not only the very high-risk patients, but also may be reassured that on average their patients have a lower risk of bleed than what they may have anticipated. They may find that the bleeding risk is not as high as they thought, especially when used in conjunction with a stroke risk scheme.
The other thing to consider is that prescribing anticoagulants will always be a decision that is made with a great deal of patient involvement. So, tools like a stroke risk calculator or a bleeding risk calculator facilitate that discussion and help the patient understand the risks and benefits of therapy.
HN: What does the Anticoagulation Clinic at UCSF do, and how is this different from how anticoagulation is managed at other hospitals?
DR. FANG: Our anticoagulation clinic manages about 600 patients taking chronic anticoagulants. It’s staffed by nurse practitioners and pharmacists who are all trained in anticoagulant management and in our anticoagulation protocols. As the medical director, I’m the only physician who is part of this clinic, and I serve in more of a supervisory role in which I can provide clinical input where needed and help develop standardized protocols and practice patterns. Many of the anticoagulation clinics are built in similar ways.
In the past, much of the anticoagulation management was handled by individual practitioners, such as primary care physicians. But there was an increasing body of literature to support the use of anticoagulation clinics, so now many larger institutions have an anticoagulation management service and an anticoagulation clinic. Some may have physicians working there, but I think that the majority have an interdisciplinary team with pharmacists and nurse practitioners managing most of the patients.
HN: What’s the role of the hospitalist in anticoagulation management?
DR. FANG: Hospitalists pay quite a lot of attention to transitions of care. Attending on the medical service, I understand a little bit about both what people know and what they don’t know about the referral and transitions processes when moving someone to an outpatient anticoagulation clinic. I serve as a liaison and try to think of ways to smooth that transition.
HN: What are the future research areas that are ripe to explore in the anticoagulation field?
DR. FANG: One of the most exciting areas is the development of newer anticoagulants that do not require the frequent blood tests and monitoring that warfarin does. Right now, our anticoagulation clinic exists because warfarin is very challenging to manage and requires very frequent visits. There are newer anticoagulants such as dabigatran and rivaroxaban and several others that are in the pipeline that may obviate the need for warfarin and therefore for anticoagulation clinics.
We know these newer agents seem as good as, if not better than, warfarin in very controlled settings and clinical trials, but we don’t know how they work in the potentially sicker, more difficult to manage populations that we see in the real world. There are certain indications and certain comorbidities that should make clinicians really cautious about using these agents. For instance, we don’t know these agents would perform in older individuals or in those who have renal disease. It’s important to figure out how clinicians are prescribing and using these medications, who they are using them in, and whether the outcomes in the real world are as good as those we’ve seen in clinical trials.
Take us to your leader. Nominate a hospitalist whose work inspires you. E-mail suggestions to m.schneider@elsevier.com. Read previous columns at ehospitalistnews.com.
Dr. Margaret Fang, the medical director of the Anticoagulation Clinic at the University of California, San Francisco, has spent the past several years studying ways to prevent hemorrhage in older Americans through proper anticoagulation therapy. As a member of the Kaiser Permanente of North California ATRIA (Anticoagulation and Risk Factors in Atrial Fibrillation) Study Group, she is investigating thromboembolic and hemorrhagic outcomes among more than 13,000 atrial fibrillation patients. Most recently, she and her research collaborators developed and evaluated a new risk stratification scoring system to assess the likelihood of anticoagulant-related bleeding in atrial fibrillation patients. (J. Am. Coll. Cardiol. 2011; 58: 395-401).
In an interview with Hospitalist News, Dr. Fang explained some of the recent findings from the ATRIA Study Group and offered her views on the best role for hospitalists in assuring proper anticoagulation therapy.
Hospitalist News: In a recent study, your team evaluated a tool to assess the risk of bleeding in atrial fibrillation patients. How would that tool be used clinically?
DR. FANG: We developed a bleeding risk score called the ATRIA bleed score. It’s specifically designed to be used in patients who are taking anticoagulants. Our goal was to try to use clinical factors to help clinicians and patients estimate the risk of having a major bleeding event while taking an anticoagulant.
There are stroke risk–stratification schemes out there that I think are more widely used in patients who have atrial fibrillation. These are based on their clinical factors and can estimate their annual risk of stroke. Anticoagulants have complications of bleeding too, so it’s important to describe what we think a patient’s risk of bleeding is while on therapy. This score used five fairly easily available clinical factors. Based on whether patients have these risk factors or not, we can counsel them about what their likelihood of having a bleed is in a given year. The range can be as low as less than 1% to nearly 18% per year. Depending on where a patient falls in that risk spectrum and their estimated risk of stroke, you can then decide whether or not it’s worth proceeding with taking anticoagulants.
HN: Do clinicians tend to overestimate bleeding risk?
DR. FANG: I think so. If you look at practice patterns of whether patients with atrial fibrillation are prescribed anticoagulants or not, it shows that almost half of eligible patients are not taking anticoagulants. When you survey physicians as to whether that’s because of a knowledge deficit or something else that’s keeping them from prescribing anticoagulants, the dominant reason is that they think the patient has too high of a bleeding risk or it’s too hard to control or manage the anticoagulants for a given patient. Even though a lot of studies have shown that the consequences of having a stroke are much more severe than the consequences of having a bleed on therapy, a significant proportion of patients with atrial fibrillation are not prescribed anticoagulants.
HN: If the ATRIA bleed score were widely used, would there be more patients who could take advantage of anticoagulation therapy?
DR. FANG: By using this tool, clinicians can find not only the very high-risk patients, but also may be reassured that on average their patients have a lower risk of bleed than what they may have anticipated. They may find that the bleeding risk is not as high as they thought, especially when used in conjunction with a stroke risk scheme.
The other thing to consider is that prescribing anticoagulants will always be a decision that is made with a great deal of patient involvement. So, tools like a stroke risk calculator or a bleeding risk calculator facilitate that discussion and help the patient understand the risks and benefits of therapy.
HN: What does the Anticoagulation Clinic at UCSF do, and how is this different from how anticoagulation is managed at other hospitals?
DR. FANG: Our anticoagulation clinic manages about 600 patients taking chronic anticoagulants. It’s staffed by nurse practitioners and pharmacists who are all trained in anticoagulant management and in our anticoagulation protocols. As the medical director, I’m the only physician who is part of this clinic, and I serve in more of a supervisory role in which I can provide clinical input where needed and help develop standardized protocols and practice patterns. Many of the anticoagulation clinics are built in similar ways.
In the past, much of the anticoagulation management was handled by individual practitioners, such as primary care physicians. But there was an increasing body of literature to support the use of anticoagulation clinics, so now many larger institutions have an anticoagulation management service and an anticoagulation clinic. Some may have physicians working there, but I think that the majority have an interdisciplinary team with pharmacists and nurse practitioners managing most of the patients.
HN: What’s the role of the hospitalist in anticoagulation management?
DR. FANG: Hospitalists pay quite a lot of attention to transitions of care. Attending on the medical service, I understand a little bit about both what people know and what they don’t know about the referral and transitions processes when moving someone to an outpatient anticoagulation clinic. I serve as a liaison and try to think of ways to smooth that transition.
HN: What are the future research areas that are ripe to explore in the anticoagulation field?
DR. FANG: One of the most exciting areas is the development of newer anticoagulants that do not require the frequent blood tests and monitoring that warfarin does. Right now, our anticoagulation clinic exists because warfarin is very challenging to manage and requires very frequent visits. There are newer anticoagulants such as dabigatran and rivaroxaban and several others that are in the pipeline that may obviate the need for warfarin and therefore for anticoagulation clinics.
We know these newer agents seem as good as, if not better than, warfarin in very controlled settings and clinical trials, but we don’t know how they work in the potentially sicker, more difficult to manage populations that we see in the real world. There are certain indications and certain comorbidities that should make clinicians really cautious about using these agents. For instance, we don’t know these agents would perform in older individuals or in those who have renal disease. It’s important to figure out how clinicians are prescribing and using these medications, who they are using them in, and whether the outcomes in the real world are as good as those we’ve seen in clinical trials.
Take us to your leader. Nominate a hospitalist whose work inspires you. E-mail suggestions to m.schneider@elsevier.com. Read previous columns at ehospitalistnews.com.
GOP Candidates Go West; Health Reform Looms as Issue
As the GOP presidential candidates begin campaigning in Minnesota this week, they will face the critical health policy debate going on in many states – what to do about the Affordable Care Act.
Minnesota Gov. Mark Dayton (D), who was elected in a tight race in 2010, supports the federal health reform law and has been working to set up a state-run health exchange where residents can go to shop for health insurance beginning in 2014. But the work has been controversial. Although some traditional GOP constituencies like the Minnesota Chamber of Commerce support the efforts of Gov. Dayton, legislation to approve the exchange has so far failed to gain traction in the Republican-controlled state legislature.
Just a week before the Feb. 7 GOP caucus in Minnesota, Gov. Dayton announced further progress on the exchange, releasing recommendations from a 15-member task force. Meanwhile, Republicans in the legislature, who did not participate in the governor’s task force, began hearings on the issue.
It’s against that backdrop that the GOP presidential hopefuls will need to make their case to caucus voters. All of the Republican candidates have come out against the health law and vowed to repeal it. But in the run-up to the Jan. 31 Florida primary, the front runners – former Massachusetts Gov. Mitt Romney and former House Speaker Newt Gingrich – launched a series of attacks, accusing each other of supporting the controversial individual mandate requiring Americans to purchase health insurance.
Lawrence Jacobs, Ph.D., a professor of political science at the University of Minnesota’s Humphrey School of Public Affairs, said he expects that the candidates will continue to hit each other hard on the Affordable Care Act (ACA).
"It’s a major issue to conservative voters that are participating in the caucuses and the primaries. The candidates are trying to curry favor with the conservatives by proving that they are more hostile [to the ACA] than the other," Dr. Jacobs said. "I think we’re going to see a continuation of the same ballet steps we saw in Florida and South Carolina and New Hampshire and Iowa."
Dr. Philip Stoyke, the legislative chair for the Minnesota Academy of Family Physicians, which supports the ACA, said he’ll be watching the Republican candidates to see if they give any further details on their alternatives to the health law.
The candidates have said they favor free market alternatives, but have been short on specifics. "We have some concerns about that," Dr. Stoyke said.
Republicans will also be casting their votes in Colorado, which holds its caucus on Feb. 7. That state has a mixed track record when it comes to the ACA.
The state’s attorney general, John W. Suthers (R), has joined a multistate lawsuit challenging the law, which will be considered by the U.S. Supreme Court in March.
But in 2010, Colorado voters rejected a ballot measure that would have barred the state from complying with the rules of the ACA. And the state’s Governor, John Hickenlooper (D), has been working with both parties in the state legislature to design a state-run health exchange.
Dr. Robert Brockmann, president-elect of the Colorado Academy of Family Physicians, said he will be watching to see if the candidates talk about the health exchanges, an issue that he said is likely to be important to the large number of small businesses operating in the state. Another issue of importance to Colorado physicians is Medicaid provider payments. He said payments need to be higher to ensure that the influx of new Medicaid patients can gain access to care.
But despite the interest surrounding the health law, experts said health care is unlikely to play a major role in the GOP caucus there.
"My sense is that health care is just not prominent right now in the political agenda," said E. Scott Adler, associate professor of political science at the University of Colorado, Boulder.
Officials at the Colorado Medical Society agreed, saying that they didn’t know of any pressing health policy issues likely to be addressed during the upcoming GOP caucus.
This is the second in a series of articles looking at the Republican presidential primaries through the eyes of physicians. Next up: The Super Tuesday states cast their ballots March 6.
As the GOP presidential candidates begin campaigning in Minnesota this week, they will face the critical health policy debate going on in many states – what to do about the Affordable Care Act.
Minnesota Gov. Mark Dayton (D), who was elected in a tight race in 2010, supports the federal health reform law and has been working to set up a state-run health exchange where residents can go to shop for health insurance beginning in 2014. But the work has been controversial. Although some traditional GOP constituencies like the Minnesota Chamber of Commerce support the efforts of Gov. Dayton, legislation to approve the exchange has so far failed to gain traction in the Republican-controlled state legislature.
Just a week before the Feb. 7 GOP caucus in Minnesota, Gov. Dayton announced further progress on the exchange, releasing recommendations from a 15-member task force. Meanwhile, Republicans in the legislature, who did not participate in the governor’s task force, began hearings on the issue.
It’s against that backdrop that the GOP presidential hopefuls will need to make their case to caucus voters. All of the Republican candidates have come out against the health law and vowed to repeal it. But in the run-up to the Jan. 31 Florida primary, the front runners – former Massachusetts Gov. Mitt Romney and former House Speaker Newt Gingrich – launched a series of attacks, accusing each other of supporting the controversial individual mandate requiring Americans to purchase health insurance.
Lawrence Jacobs, Ph.D., a professor of political science at the University of Minnesota’s Humphrey School of Public Affairs, said he expects that the candidates will continue to hit each other hard on the Affordable Care Act (ACA).
"It’s a major issue to conservative voters that are participating in the caucuses and the primaries. The candidates are trying to curry favor with the conservatives by proving that they are more hostile [to the ACA] than the other," Dr. Jacobs said. "I think we’re going to see a continuation of the same ballet steps we saw in Florida and South Carolina and New Hampshire and Iowa."
Dr. Philip Stoyke, the legislative chair for the Minnesota Academy of Family Physicians, which supports the ACA, said he’ll be watching the Republican candidates to see if they give any further details on their alternatives to the health law.
The candidates have said they favor free market alternatives, but have been short on specifics. "We have some concerns about that," Dr. Stoyke said.
Republicans will also be casting their votes in Colorado, which holds its caucus on Feb. 7. That state has a mixed track record when it comes to the ACA.
The state’s attorney general, John W. Suthers (R), has joined a multistate lawsuit challenging the law, which will be considered by the U.S. Supreme Court in March.
But in 2010, Colorado voters rejected a ballot measure that would have barred the state from complying with the rules of the ACA. And the state’s Governor, John Hickenlooper (D), has been working with both parties in the state legislature to design a state-run health exchange.
Dr. Robert Brockmann, president-elect of the Colorado Academy of Family Physicians, said he will be watching to see if the candidates talk about the health exchanges, an issue that he said is likely to be important to the large number of small businesses operating in the state. Another issue of importance to Colorado physicians is Medicaid provider payments. He said payments need to be higher to ensure that the influx of new Medicaid patients can gain access to care.
But despite the interest surrounding the health law, experts said health care is unlikely to play a major role in the GOP caucus there.
"My sense is that health care is just not prominent right now in the political agenda," said E. Scott Adler, associate professor of political science at the University of Colorado, Boulder.
Officials at the Colorado Medical Society agreed, saying that they didn’t know of any pressing health policy issues likely to be addressed during the upcoming GOP caucus.
This is the second in a series of articles looking at the Republican presidential primaries through the eyes of physicians. Next up: The Super Tuesday states cast their ballots March 6.
As the GOP presidential candidates begin campaigning in Minnesota this week, they will face the critical health policy debate going on in many states – what to do about the Affordable Care Act.
Minnesota Gov. Mark Dayton (D), who was elected in a tight race in 2010, supports the federal health reform law and has been working to set up a state-run health exchange where residents can go to shop for health insurance beginning in 2014. But the work has been controversial. Although some traditional GOP constituencies like the Minnesota Chamber of Commerce support the efforts of Gov. Dayton, legislation to approve the exchange has so far failed to gain traction in the Republican-controlled state legislature.
Just a week before the Feb. 7 GOP caucus in Minnesota, Gov. Dayton announced further progress on the exchange, releasing recommendations from a 15-member task force. Meanwhile, Republicans in the legislature, who did not participate in the governor’s task force, began hearings on the issue.
It’s against that backdrop that the GOP presidential hopefuls will need to make their case to caucus voters. All of the Republican candidates have come out against the health law and vowed to repeal it. But in the run-up to the Jan. 31 Florida primary, the front runners – former Massachusetts Gov. Mitt Romney and former House Speaker Newt Gingrich – launched a series of attacks, accusing each other of supporting the controversial individual mandate requiring Americans to purchase health insurance.
Lawrence Jacobs, Ph.D., a professor of political science at the University of Minnesota’s Humphrey School of Public Affairs, said he expects that the candidates will continue to hit each other hard on the Affordable Care Act (ACA).
"It’s a major issue to conservative voters that are participating in the caucuses and the primaries. The candidates are trying to curry favor with the conservatives by proving that they are more hostile [to the ACA] than the other," Dr. Jacobs said. "I think we’re going to see a continuation of the same ballet steps we saw in Florida and South Carolina and New Hampshire and Iowa."
Dr. Philip Stoyke, the legislative chair for the Minnesota Academy of Family Physicians, which supports the ACA, said he’ll be watching the Republican candidates to see if they give any further details on their alternatives to the health law.
The candidates have said they favor free market alternatives, but have been short on specifics. "We have some concerns about that," Dr. Stoyke said.
Republicans will also be casting their votes in Colorado, which holds its caucus on Feb. 7. That state has a mixed track record when it comes to the ACA.
The state’s attorney general, John W. Suthers (R), has joined a multistate lawsuit challenging the law, which will be considered by the U.S. Supreme Court in March.
But in 2010, Colorado voters rejected a ballot measure that would have barred the state from complying with the rules of the ACA. And the state’s Governor, John Hickenlooper (D), has been working with both parties in the state legislature to design a state-run health exchange.
Dr. Robert Brockmann, president-elect of the Colorado Academy of Family Physicians, said he will be watching to see if the candidates talk about the health exchanges, an issue that he said is likely to be important to the large number of small businesses operating in the state. Another issue of importance to Colorado physicians is Medicaid provider payments. He said payments need to be higher to ensure that the influx of new Medicaid patients can gain access to care.
But despite the interest surrounding the health law, experts said health care is unlikely to play a major role in the GOP caucus there.
"My sense is that health care is just not prominent right now in the political agenda," said E. Scott Adler, associate professor of political science at the University of Colorado, Boulder.
Officials at the Colorado Medical Society agreed, saying that they didn’t know of any pressing health policy issues likely to be addressed during the upcoming GOP caucus.
This is the second in a series of articles looking at the Republican presidential primaries through the eyes of physicians. Next up: The Super Tuesday states cast their ballots March 6.
Tanning Salons Mislead Teens, Congressional Probe Finds
Many tanning salons are downplaying the health risks associated with indoor tanning while claiming that time in a tanning bed offers an array of health benefits, according to an investigative report from Democrats on the House Energy and Commerce Committee.
Committee investigators, posing as fair-skinned teenage girls, called 300 tanning salons across the country, and found that 90% said that the use of tanning beds did not pose a health risk. When pressed about skin cancer risks, some salon employees said the link to indoor tanning was "hype" or "a big myth."
"I think it validates what we’ve been saying as dermatologists for many years," said Dr. Bruce A. Brod of the University of Pennsylvania, Philadelphia. "Unfortunately, the indoor tanning industry does not responsibly regulate [itself]."
Dr. Brod said he’s not surprised by the report’s findings. "I hear those stories all the time" from patients who have used tanning salons, he said.
The American Academy of Dermatology Association called on Congress and the states to better regulate indoor tanning. In a statement, the AADA said states should follow California’s example and ban indoor tanning among young adults under the age of 18. The organization also urged Congress to pass H.R. 1676, the Tanning Bed Cancer Control Act, which instructs the Food and Drug Administration to reexamine the way it regulates tanning beds.
The congressional investigation was requested by Rep. Carolyn Maloney (D- N.Y.), sponsor of H.R. 1676, along with other top Democrats on the House Energy and Commerce Committee.
The Indoor Tanning Association (ITA) criticized the way the investigation was conducted. Association spokesman John Overstreet said the study was flawed because it was constructed by people who already have an unfavorable opinion of the industry. It was also "unfair" for committee investigators to rely on information given over the phone to undercover investigators.
The experience would be far different if a teenager came into a tanning salon accompanied by a parent, he said, adding that in such a situation the information provided likely would be much more comprehensive and would include a discussion about potential risks.
But while the ITA disputes the findings, the organization acknowledged the need to reevaluate how the tanning salon industry could better ensure that salons provide accurate and consistent information to all consumers.
Congressional investigators also found that 78% of the tanning salons they contacted touted some type of health benefits from indoor tanning, ranging from the treatment of depression to weight loss. Salon employees also told investigators that young people were not at risk for developing skin cancer and that the rising rates of cancer were linked to the increased use of sunscreen.
The report also took the tanning industry to task for targeting teenage girls in their marketing materials. The investigators found that tanning salons often offered student discounts or other promotions for prom, homecoming, and back-to-school.
Many tanning salons are downplaying the health risks associated with indoor tanning while claiming that time in a tanning bed offers an array of health benefits, according to an investigative report from Democrats on the House Energy and Commerce Committee.
Committee investigators, posing as fair-skinned teenage girls, called 300 tanning salons across the country, and found that 90% said that the use of tanning beds did not pose a health risk. When pressed about skin cancer risks, some salon employees said the link to indoor tanning was "hype" or "a big myth."
"I think it validates what we’ve been saying as dermatologists for many years," said Dr. Bruce A. Brod of the University of Pennsylvania, Philadelphia. "Unfortunately, the indoor tanning industry does not responsibly regulate [itself]."
Dr. Brod said he’s not surprised by the report’s findings. "I hear those stories all the time" from patients who have used tanning salons, he said.
The American Academy of Dermatology Association called on Congress and the states to better regulate indoor tanning. In a statement, the AADA said states should follow California’s example and ban indoor tanning among young adults under the age of 18. The organization also urged Congress to pass H.R. 1676, the Tanning Bed Cancer Control Act, which instructs the Food and Drug Administration to reexamine the way it regulates tanning beds.
The congressional investigation was requested by Rep. Carolyn Maloney (D- N.Y.), sponsor of H.R. 1676, along with other top Democrats on the House Energy and Commerce Committee.
The Indoor Tanning Association (ITA) criticized the way the investigation was conducted. Association spokesman John Overstreet said the study was flawed because it was constructed by people who already have an unfavorable opinion of the industry. It was also "unfair" for committee investigators to rely on information given over the phone to undercover investigators.
The experience would be far different if a teenager came into a tanning salon accompanied by a parent, he said, adding that in such a situation the information provided likely would be much more comprehensive and would include a discussion about potential risks.
But while the ITA disputes the findings, the organization acknowledged the need to reevaluate how the tanning salon industry could better ensure that salons provide accurate and consistent information to all consumers.
Congressional investigators also found that 78% of the tanning salons they contacted touted some type of health benefits from indoor tanning, ranging from the treatment of depression to weight loss. Salon employees also told investigators that young people were not at risk for developing skin cancer and that the rising rates of cancer were linked to the increased use of sunscreen.
The report also took the tanning industry to task for targeting teenage girls in their marketing materials. The investigators found that tanning salons often offered student discounts or other promotions for prom, homecoming, and back-to-school.
Many tanning salons are downplaying the health risks associated with indoor tanning while claiming that time in a tanning bed offers an array of health benefits, according to an investigative report from Democrats on the House Energy and Commerce Committee.
Committee investigators, posing as fair-skinned teenage girls, called 300 tanning salons across the country, and found that 90% said that the use of tanning beds did not pose a health risk. When pressed about skin cancer risks, some salon employees said the link to indoor tanning was "hype" or "a big myth."
"I think it validates what we’ve been saying as dermatologists for many years," said Dr. Bruce A. Brod of the University of Pennsylvania, Philadelphia. "Unfortunately, the indoor tanning industry does not responsibly regulate [itself]."
Dr. Brod said he’s not surprised by the report’s findings. "I hear those stories all the time" from patients who have used tanning salons, he said.
The American Academy of Dermatology Association called on Congress and the states to better regulate indoor tanning. In a statement, the AADA said states should follow California’s example and ban indoor tanning among young adults under the age of 18. The organization also urged Congress to pass H.R. 1676, the Tanning Bed Cancer Control Act, which instructs the Food and Drug Administration to reexamine the way it regulates tanning beds.
The congressional investigation was requested by Rep. Carolyn Maloney (D- N.Y.), sponsor of H.R. 1676, along with other top Democrats on the House Energy and Commerce Committee.
The Indoor Tanning Association (ITA) criticized the way the investigation was conducted. Association spokesman John Overstreet said the study was flawed because it was constructed by people who already have an unfavorable opinion of the industry. It was also "unfair" for committee investigators to rely on information given over the phone to undercover investigators.
The experience would be far different if a teenager came into a tanning salon accompanied by a parent, he said, adding that in such a situation the information provided likely would be much more comprehensive and would include a discussion about potential risks.
But while the ITA disputes the findings, the organization acknowledged the need to reevaluate how the tanning salon industry could better ensure that salons provide accurate and consistent information to all consumers.
Congressional investigators also found that 78% of the tanning salons they contacted touted some type of health benefits from indoor tanning, ranging from the treatment of depression to weight loss. Salon employees also told investigators that young people were not at risk for developing skin cancer and that the rising rates of cancer were linked to the increased use of sunscreen.
The report also took the tanning industry to task for targeting teenage girls in their marketing materials. The investigators found that tanning salons often offered student discounts or other promotions for prom, homecoming, and back-to-school.
Here We Go Again: Steep SGR Cut Looms : Frustration runs high among physicians as temporary fix of Medicare payment system ends.
Physicians are once again waiting for Congress to avert a 27% Medicare physician fee cut scheduled to take effect on March 1.
The pay cut was originally scheduled to begin Jan. 1, but after much back-and-forth in Congress, the House and Senate passed the Temporary Payroll Tax Cut Continuation Act of 2011 on Dec. 23, which included an extension of 2011 Medicare physician-payment rates through the end of February. President Obama quickly signed the bill into law.
Lawmakers also agreed to appoint a 20-member House-Senate conference committee to work on a longer-term plan to address the Medicare physician pay issue, along with a full-year extension of the Social Security payroll tax holiday and federally funded unemployment insurance benefits.
The agreement followed several days of brinksmanship by leaders in the House and Senate. It started on Dec. 13, when the House passed a bill that would have replaced the 27% Medicare fee cut with a 1% pay raise for physicians for 2 years. Despite bipartisan support for the so-called doc fix, other controversial provisions in the bill kept it from gaining traction in the Senate. A few days later, the Senate approved their own version of the bill, which extended the payroll tax holiday and unemployment benefits for 2 months and postponed any Medicare pay cuts until the end of February.
The House initially rejected the idea of a short-term fix, and even passed a resolution to formally disagree with the legislation passed by the Senate. But intense public criticism led House leaders to agree to the short-term plan and use the first 2 months of this year to negotiate a compromise.
Physicians remain furious with Congress for its inability to find a long-term solution in 2011.
“There's a tremendous degree of frustration out there,” said Robert Doherty, senior vice president for government affairs and public policy at the American College of Physicians. “If Congress is expecting physicians to applaud them for agreeing to a 2-month extension, they're going to find a lot of silence from the physician community.”
Dr. Jeffrey Cain, a Denver family physician and president-elect of the American Academy of Family Physicians, said that the last-minute legislation was no way to conduct the nation's business, and that it failed to meet the needs of physicians and patients. “Every time we kick the can down the road and we fail to address the issue, we put family medicine and – more importantly – the health of millions of Americans at risk,” Dr. Cain said.
Frustration is especially high because members of Congress had signaled early in 2011 that they were interested in crafting a long-term solution to replace the Sustainable Growth Rate formula, the statutory formula that ties spending on physicians' services to the gross domestic product. In March 2011, leaders in the House Energy and Commerce Committee wrote to several physicians' groups asking for proposals on how to reform the physician payment system and move to a new system that “reduces spending, pays providers fairly, and pays for services according to their value to the beneficiary.”
The letter emphasized the need to act quickly in developing a long-term solution, or risk the “unwanted choice of extending a fundamentally broken payment system or jeopardizing access to care” for Medicare beneficiaries. “We cannot let either happen,” the lawmakers wrote.
It's too soon to tell what Congress will do next, but both Mr. Doherty and Dr. Cain agreed that a long-term solution that would replace the SGR is unlikely right now. Instead, AAFP officials are pushing for a 2- to 3-year patch that would give lawmakers time to enact a permanent SGR fix.
In a worse-case scenario, physicians could be facing a situation similar to what happened in 2010, when Congress passed a series of temporary patches during the first half of the year, Mr. Doherty said. That situation could become a reality if lawmakers once again are deadlocked on the larger legislative package. “To a great extent, we're once again going to be held hostage to negotiations over a broader package on issues that really have nothing to do with the SGR.”
Every time we kick the can down the road, we put the health of millions of Americans at risk.
Source DR. CAIN
Physicians are once again waiting for Congress to avert a 27% Medicare physician fee cut scheduled to take effect on March 1.
The pay cut was originally scheduled to begin Jan. 1, but after much back-and-forth in Congress, the House and Senate passed the Temporary Payroll Tax Cut Continuation Act of 2011 on Dec. 23, which included an extension of 2011 Medicare physician-payment rates through the end of February. President Obama quickly signed the bill into law.
Lawmakers also agreed to appoint a 20-member House-Senate conference committee to work on a longer-term plan to address the Medicare physician pay issue, along with a full-year extension of the Social Security payroll tax holiday and federally funded unemployment insurance benefits.
The agreement followed several days of brinksmanship by leaders in the House and Senate. It started on Dec. 13, when the House passed a bill that would have replaced the 27% Medicare fee cut with a 1% pay raise for physicians for 2 years. Despite bipartisan support for the so-called doc fix, other controversial provisions in the bill kept it from gaining traction in the Senate. A few days later, the Senate approved their own version of the bill, which extended the payroll tax holiday and unemployment benefits for 2 months and postponed any Medicare pay cuts until the end of February.
The House initially rejected the idea of a short-term fix, and even passed a resolution to formally disagree with the legislation passed by the Senate. But intense public criticism led House leaders to agree to the short-term plan and use the first 2 months of this year to negotiate a compromise.
Physicians remain furious with Congress for its inability to find a long-term solution in 2011.
“There's a tremendous degree of frustration out there,” said Robert Doherty, senior vice president for government affairs and public policy at the American College of Physicians. “If Congress is expecting physicians to applaud them for agreeing to a 2-month extension, they're going to find a lot of silence from the physician community.”
Dr. Jeffrey Cain, a Denver family physician and president-elect of the American Academy of Family Physicians, said that the last-minute legislation was no way to conduct the nation's business, and that it failed to meet the needs of physicians and patients. “Every time we kick the can down the road and we fail to address the issue, we put family medicine and – more importantly – the health of millions of Americans at risk,” Dr. Cain said.
Frustration is especially high because members of Congress had signaled early in 2011 that they were interested in crafting a long-term solution to replace the Sustainable Growth Rate formula, the statutory formula that ties spending on physicians' services to the gross domestic product. In March 2011, leaders in the House Energy and Commerce Committee wrote to several physicians' groups asking for proposals on how to reform the physician payment system and move to a new system that “reduces spending, pays providers fairly, and pays for services according to their value to the beneficiary.”
The letter emphasized the need to act quickly in developing a long-term solution, or risk the “unwanted choice of extending a fundamentally broken payment system or jeopardizing access to care” for Medicare beneficiaries. “We cannot let either happen,” the lawmakers wrote.
It's too soon to tell what Congress will do next, but both Mr. Doherty and Dr. Cain agreed that a long-term solution that would replace the SGR is unlikely right now. Instead, AAFP officials are pushing for a 2- to 3-year patch that would give lawmakers time to enact a permanent SGR fix.
In a worse-case scenario, physicians could be facing a situation similar to what happened in 2010, when Congress passed a series of temporary patches during the first half of the year, Mr. Doherty said. That situation could become a reality if lawmakers once again are deadlocked on the larger legislative package. “To a great extent, we're once again going to be held hostage to negotiations over a broader package on issues that really have nothing to do with the SGR.”
Every time we kick the can down the road, we put the health of millions of Americans at risk.
Source DR. CAIN
Physicians are once again waiting for Congress to avert a 27% Medicare physician fee cut scheduled to take effect on March 1.
The pay cut was originally scheduled to begin Jan. 1, but after much back-and-forth in Congress, the House and Senate passed the Temporary Payroll Tax Cut Continuation Act of 2011 on Dec. 23, which included an extension of 2011 Medicare physician-payment rates through the end of February. President Obama quickly signed the bill into law.
Lawmakers also agreed to appoint a 20-member House-Senate conference committee to work on a longer-term plan to address the Medicare physician pay issue, along with a full-year extension of the Social Security payroll tax holiday and federally funded unemployment insurance benefits.
The agreement followed several days of brinksmanship by leaders in the House and Senate. It started on Dec. 13, when the House passed a bill that would have replaced the 27% Medicare fee cut with a 1% pay raise for physicians for 2 years. Despite bipartisan support for the so-called doc fix, other controversial provisions in the bill kept it from gaining traction in the Senate. A few days later, the Senate approved their own version of the bill, which extended the payroll tax holiday and unemployment benefits for 2 months and postponed any Medicare pay cuts until the end of February.
The House initially rejected the idea of a short-term fix, and even passed a resolution to formally disagree with the legislation passed by the Senate. But intense public criticism led House leaders to agree to the short-term plan and use the first 2 months of this year to negotiate a compromise.
Physicians remain furious with Congress for its inability to find a long-term solution in 2011.
“There's a tremendous degree of frustration out there,” said Robert Doherty, senior vice president for government affairs and public policy at the American College of Physicians. “If Congress is expecting physicians to applaud them for agreeing to a 2-month extension, they're going to find a lot of silence from the physician community.”
Dr. Jeffrey Cain, a Denver family physician and president-elect of the American Academy of Family Physicians, said that the last-minute legislation was no way to conduct the nation's business, and that it failed to meet the needs of physicians and patients. “Every time we kick the can down the road and we fail to address the issue, we put family medicine and – more importantly – the health of millions of Americans at risk,” Dr. Cain said.
Frustration is especially high because members of Congress had signaled early in 2011 that they were interested in crafting a long-term solution to replace the Sustainable Growth Rate formula, the statutory formula that ties spending on physicians' services to the gross domestic product. In March 2011, leaders in the House Energy and Commerce Committee wrote to several physicians' groups asking for proposals on how to reform the physician payment system and move to a new system that “reduces spending, pays providers fairly, and pays for services according to their value to the beneficiary.”
The letter emphasized the need to act quickly in developing a long-term solution, or risk the “unwanted choice of extending a fundamentally broken payment system or jeopardizing access to care” for Medicare beneficiaries. “We cannot let either happen,” the lawmakers wrote.
It's too soon to tell what Congress will do next, but both Mr. Doherty and Dr. Cain agreed that a long-term solution that would replace the SGR is unlikely right now. Instead, AAFP officials are pushing for a 2- to 3-year patch that would give lawmakers time to enact a permanent SGR fix.
In a worse-case scenario, physicians could be facing a situation similar to what happened in 2010, when Congress passed a series of temporary patches during the first half of the year, Mr. Doherty said. That situation could become a reality if lawmakers once again are deadlocked on the larger legislative package. “To a great extent, we're once again going to be held hostage to negotiations over a broader package on issues that really have nothing to do with the SGR.”
Every time we kick the can down the road, we put the health of millions of Americans at risk.
Source DR. CAIN
Medicare Demos Fall Short on Savings
Over the last 2 decades, policymakers have proposed a number of ways to change how health care is delivered in the Medicare program, but a new analysis from the nonpartisan Congressional Budget Office shows that so far those efforts have failed to yield significant savings.
The CBO analyzed 10 major Medicare demonstrations involving either disease management and care coordination or some type of value-based payments and found that most of the projects didn’t save the government money.
The analysis has clear implications for health policy going forward. Under the Affordable Care Act, Congress required the Centers for Medicare and Medicaid Services to pursue new payment and care delivery models including accountable care organizations (ACOs) and bundled payments. Congress also created a new Innovation Center within CMS to test other models of care. The idea behind the newly formed Innovation Center is that Medicare officials will be able to expand successful projects without having to return to Congress for approval.
Dr. Glen R. Stream, president of the American Academy of Family Physicians, said he expects that the leadership within Medicare will use the CBO analysis to improve future pilot projects. He said he’s hopeful that the work that the Innovation Center is undertaking will yield better results because its projects focus on broader care delivery concepts, such as the patient-centered medical home, rather than targeting only certain chronic conditions, as was done in several past demonstrations.
Looking at the six disease management and care coordination projects that Medicare had already undertaken, CBO analysts found that on average there was little to no effect on hospital admissions or regular Medicare spending. The demonstrations were more likely to reduce costs if they used care managers who had significant, direct contact with physicians and patients. However, those programs generally didn’t save enough money to cover the cost of the extra services provided. For example, in programs with significant in-person or telephone interaction between care management and patients there was an average 7% drop in hospital admissions and a 3% reduction in regular Medicare spending. However, in order to offset the cost of the care management fees, the programs would have had to reduce regular Medicare expenditures by 13%.
In the four demonstrations that focused on changing the financial incentives for health care providers, only one project produced significant savings. A project that offered bundled payments to physicians and hospitals for heart bypass surgery reduced Medicare expenditures related to heart bypass by about 10% without an adverse impact on patient outcomes. Medicare was able to achieve those savings in large part because officials negotiated bundled payments that were lower than the traditional fee-for-service payments, according to CBO. The other projects, which offered bonuses for meeting quality standards or reducing spending, did not achieve significant savings for the Medicare program, CBO wrote.
Over the last 2 decades, policymakers have proposed a number of ways to change how health care is delivered in the Medicare program, but a new analysis from the nonpartisan Congressional Budget Office shows that so far those efforts have failed to yield significant savings.
The CBO analyzed 10 major Medicare demonstrations involving either disease management and care coordination or some type of value-based payments and found that most of the projects didn’t save the government money.
The analysis has clear implications for health policy going forward. Under the Affordable Care Act, Congress required the Centers for Medicare and Medicaid Services to pursue new payment and care delivery models including accountable care organizations (ACOs) and bundled payments. Congress also created a new Innovation Center within CMS to test other models of care. The idea behind the newly formed Innovation Center is that Medicare officials will be able to expand successful projects without having to return to Congress for approval.
Dr. Glen R. Stream, president of the American Academy of Family Physicians, said he expects that the leadership within Medicare will use the CBO analysis to improve future pilot projects. He said he’s hopeful that the work that the Innovation Center is undertaking will yield better results because its projects focus on broader care delivery concepts, such as the patient-centered medical home, rather than targeting only certain chronic conditions, as was done in several past demonstrations.
Looking at the six disease management and care coordination projects that Medicare had already undertaken, CBO analysts found that on average there was little to no effect on hospital admissions or regular Medicare spending. The demonstrations were more likely to reduce costs if they used care managers who had significant, direct contact with physicians and patients. However, those programs generally didn’t save enough money to cover the cost of the extra services provided. For example, in programs with significant in-person or telephone interaction between care management and patients there was an average 7% drop in hospital admissions and a 3% reduction in regular Medicare spending. However, in order to offset the cost of the care management fees, the programs would have had to reduce regular Medicare expenditures by 13%.
In the four demonstrations that focused on changing the financial incentives for health care providers, only one project produced significant savings. A project that offered bundled payments to physicians and hospitals for heart bypass surgery reduced Medicare expenditures related to heart bypass by about 10% without an adverse impact on patient outcomes. Medicare was able to achieve those savings in large part because officials negotiated bundled payments that were lower than the traditional fee-for-service payments, according to CBO. The other projects, which offered bonuses for meeting quality standards or reducing spending, did not achieve significant savings for the Medicare program, CBO wrote.
Over the last 2 decades, policymakers have proposed a number of ways to change how health care is delivered in the Medicare program, but a new analysis from the nonpartisan Congressional Budget Office shows that so far those efforts have failed to yield significant savings.
The CBO analyzed 10 major Medicare demonstrations involving either disease management and care coordination or some type of value-based payments and found that most of the projects didn’t save the government money.
The analysis has clear implications for health policy going forward. Under the Affordable Care Act, Congress required the Centers for Medicare and Medicaid Services to pursue new payment and care delivery models including accountable care organizations (ACOs) and bundled payments. Congress also created a new Innovation Center within CMS to test other models of care. The idea behind the newly formed Innovation Center is that Medicare officials will be able to expand successful projects without having to return to Congress for approval.
Dr. Glen R. Stream, president of the American Academy of Family Physicians, said he expects that the leadership within Medicare will use the CBO analysis to improve future pilot projects. He said he’s hopeful that the work that the Innovation Center is undertaking will yield better results because its projects focus on broader care delivery concepts, such as the patient-centered medical home, rather than targeting only certain chronic conditions, as was done in several past demonstrations.
Looking at the six disease management and care coordination projects that Medicare had already undertaken, CBO analysts found that on average there was little to no effect on hospital admissions or regular Medicare spending. The demonstrations were more likely to reduce costs if they used care managers who had significant, direct contact with physicians and patients. However, those programs generally didn’t save enough money to cover the cost of the extra services provided. For example, in programs with significant in-person or telephone interaction between care management and patients there was an average 7% drop in hospital admissions and a 3% reduction in regular Medicare spending. However, in order to offset the cost of the care management fees, the programs would have had to reduce regular Medicare expenditures by 13%.
In the four demonstrations that focused on changing the financial incentives for health care providers, only one project produced significant savings. A project that offered bundled payments to physicians and hospitals for heart bypass surgery reduced Medicare expenditures related to heart bypass by about 10% without an adverse impact on patient outcomes. Medicare was able to achieve those savings in large part because officials negotiated bundled payments that were lower than the traditional fee-for-service payments, according to CBO. The other projects, which offered bonuses for meeting quality standards or reducing spending, did not achieve significant savings for the Medicare program, CBO wrote.
Steep SGR Cut Looms Again
Physicians are once again waiting for Congress to avert a 27% Medicare physician fee cut scheduled to take effect on March 1.
The pay cut was originally scheduled to begin Jan. 1, but after much back-and-forth in Congress, the House and Senate passed the Temporary Payroll Tax Cut Continuation Act of 2011 on Dec. 23, which included an extension of 2011 Medicare physician-payment rates through the end of February. President Obama quickly signed the bill into law.
Lawmakers also agreed to appoint a 20-member House-Senate conference committee to work on a longer-term plan to address the Medicare physician pay issue, along with a full-year extension of the Social Security payroll tax holiday and federally funded unemployment insurance benefits.
The agreement followed several days of brinksmanship by leaders in the House and Senate. It started on Dec. 13, when the House passed a bill that would have replaced the 27% Medicare fee cut with a 1% pay raise for physicians for 2 years. Despite bipartisan support for the so-called doc fix, other controversial provisions in the bill kept it from gaining traction in the Senate. A few days later, the Senate approved their own version of the bill, which extended the payroll tax holiday and unemployment benefits for 2 months and postponed any Medicare pay cuts until the end of February.
The House initially rejected the idea of a short-term fix, and even passed a resolution to formally disagree with the legislation passed by the Senate. But intense public criticism led House leaders to agree to the short-term plan and use the first 2 months of this year to negotiate a compromise.
"There’s a tremendous degree of frustration out there," said Robert Doherty, senior vice president for government affairs and public policy at the American College of Physicians. "If Congress is expecting physicians to applaud them for agreeing to a 2-month extension, they’re going to find a lot of silence from the physician community."
Frustration is especially high because members of Congress had signaled early in 2011 that they were interested in crafting a long-term solution to replace the Sustainable Growth Rate formula, the statutory formula that ties spending on physicians’ services to the Gross Domestic Product. In March 2011, leaders in the House Energy and Commerce Committee wrote to several physicians’ groups asking for proposals on how to reform the physician payment system and move to a new system that "reduces spending, pays providers fairly, and pays for services according to their value to the beneficiary."
The letter emphasized the need to act quickly in developing a long-term solution, or risk the "unwanted choice of extending a fundamentally broken payment system or jeopardizing access to care" for Medicare beneficiaries. "We cannot let either happen," the lawmakers wrote.
It’s too soon to tell what Congress will do next, but a long-term solution that would replace the SGR is unlikely now.
In a worse-case scenario, physicians could be facing a situation similar to what happened in 2010, when Congress passed a series of temporary patches during the first half of the year, Mr. Doherty said. That situation could become a reality if lawmakers once again are deadlocked on the larger legislative package. "To a great extent, we’re once again going to be held hostage to negotiations over a broader package on issues that really have nothing to do with the SGR."☐
Physicians are once again waiting for Congress to avert a 27% Medicare physician fee cut scheduled to take effect on March 1.
The pay cut was originally scheduled to begin Jan. 1, but after much back-and-forth in Congress, the House and Senate passed the Temporary Payroll Tax Cut Continuation Act of 2011 on Dec. 23, which included an extension of 2011 Medicare physician-payment rates through the end of February. President Obama quickly signed the bill into law.
Lawmakers also agreed to appoint a 20-member House-Senate conference committee to work on a longer-term plan to address the Medicare physician pay issue, along with a full-year extension of the Social Security payroll tax holiday and federally funded unemployment insurance benefits.
The agreement followed several days of brinksmanship by leaders in the House and Senate. It started on Dec. 13, when the House passed a bill that would have replaced the 27% Medicare fee cut with a 1% pay raise for physicians for 2 years. Despite bipartisan support for the so-called doc fix, other controversial provisions in the bill kept it from gaining traction in the Senate. A few days later, the Senate approved their own version of the bill, which extended the payroll tax holiday and unemployment benefits for 2 months and postponed any Medicare pay cuts until the end of February.
The House initially rejected the idea of a short-term fix, and even passed a resolution to formally disagree with the legislation passed by the Senate. But intense public criticism led House leaders to agree to the short-term plan and use the first 2 months of this year to negotiate a compromise.
"There’s a tremendous degree of frustration out there," said Robert Doherty, senior vice president for government affairs and public policy at the American College of Physicians. "If Congress is expecting physicians to applaud them for agreeing to a 2-month extension, they’re going to find a lot of silence from the physician community."
Frustration is especially high because members of Congress had signaled early in 2011 that they were interested in crafting a long-term solution to replace the Sustainable Growth Rate formula, the statutory formula that ties spending on physicians’ services to the Gross Domestic Product. In March 2011, leaders in the House Energy and Commerce Committee wrote to several physicians’ groups asking for proposals on how to reform the physician payment system and move to a new system that "reduces spending, pays providers fairly, and pays for services according to their value to the beneficiary."
The letter emphasized the need to act quickly in developing a long-term solution, or risk the "unwanted choice of extending a fundamentally broken payment system or jeopardizing access to care" for Medicare beneficiaries. "We cannot let either happen," the lawmakers wrote.
It’s too soon to tell what Congress will do next, but a long-term solution that would replace the SGR is unlikely now.
In a worse-case scenario, physicians could be facing a situation similar to what happened in 2010, when Congress passed a series of temporary patches during the first half of the year, Mr. Doherty said. That situation could become a reality if lawmakers once again are deadlocked on the larger legislative package. "To a great extent, we’re once again going to be held hostage to negotiations over a broader package on issues that really have nothing to do with the SGR."☐
Physicians are once again waiting for Congress to avert a 27% Medicare physician fee cut scheduled to take effect on March 1.
The pay cut was originally scheduled to begin Jan. 1, but after much back-and-forth in Congress, the House and Senate passed the Temporary Payroll Tax Cut Continuation Act of 2011 on Dec. 23, which included an extension of 2011 Medicare physician-payment rates through the end of February. President Obama quickly signed the bill into law.
Lawmakers also agreed to appoint a 20-member House-Senate conference committee to work on a longer-term plan to address the Medicare physician pay issue, along with a full-year extension of the Social Security payroll tax holiday and federally funded unemployment insurance benefits.
The agreement followed several days of brinksmanship by leaders in the House and Senate. It started on Dec. 13, when the House passed a bill that would have replaced the 27% Medicare fee cut with a 1% pay raise for physicians for 2 years. Despite bipartisan support for the so-called doc fix, other controversial provisions in the bill kept it from gaining traction in the Senate. A few days later, the Senate approved their own version of the bill, which extended the payroll tax holiday and unemployment benefits for 2 months and postponed any Medicare pay cuts until the end of February.
The House initially rejected the idea of a short-term fix, and even passed a resolution to formally disagree with the legislation passed by the Senate. But intense public criticism led House leaders to agree to the short-term plan and use the first 2 months of this year to negotiate a compromise.
"There’s a tremendous degree of frustration out there," said Robert Doherty, senior vice president for government affairs and public policy at the American College of Physicians. "If Congress is expecting physicians to applaud them for agreeing to a 2-month extension, they’re going to find a lot of silence from the physician community."
Frustration is especially high because members of Congress had signaled early in 2011 that they were interested in crafting a long-term solution to replace the Sustainable Growth Rate formula, the statutory formula that ties spending on physicians’ services to the Gross Domestic Product. In March 2011, leaders in the House Energy and Commerce Committee wrote to several physicians’ groups asking for proposals on how to reform the physician payment system and move to a new system that "reduces spending, pays providers fairly, and pays for services according to their value to the beneficiary."
The letter emphasized the need to act quickly in developing a long-term solution, or risk the "unwanted choice of extending a fundamentally broken payment system or jeopardizing access to care" for Medicare beneficiaries. "We cannot let either happen," the lawmakers wrote.
It’s too soon to tell what Congress will do next, but a long-term solution that would replace the SGR is unlikely now.
In a worse-case scenario, physicians could be facing a situation similar to what happened in 2010, when Congress passed a series of temporary patches during the first half of the year, Mr. Doherty said. That situation could become a reality if lawmakers once again are deadlocked on the larger legislative package. "To a great extent, we’re once again going to be held hostage to negotiations over a broader package on issues that really have nothing to do with the SGR."☐