User login
Mitchel is a reporter for MDedge based in the Philadelphia area. He started with the company in 1992, when it was International Medical News Group (IMNG), and has since covered a range of medical specialties. Mitchel trained as a virologist at Roswell Park Memorial Institute in Buffalo, and then worked briefly as a researcher at Boston Children's Hospital before pivoting to journalism as a AAAS Mass Media Fellow in 1980. His first reporting job was with Science Digest magazine, and from the mid-1980s to early-1990s he was a reporter with Medical World News. @mitchelzoler
Rheumatoid Arthritis Incidence Rises With Age, Peaks During 70s
LONDON – The incidence of rheumatoid arthritis rises with age in both men and women and shows the biggest jump during the sixth decade of life, when the incidence among adults in their 50s nearly doubles compared with those in their 40s, based on findings from an analysis of about 10,000 Swedish patients diagnosed for the first time during 2006-2008.
The nationwide data also showed that peak rheumatoid arthritis (RA) incidence occurs among men and women in their 70s, with a new onset rate of at least 73 cases per 100,000 population annually, Jonas Eriksson said at the Annual European Congress of Rheumatology.
The nationwide Swedish data that allowed analysis of about 10,000 cases far exceeded the scope of previous incidence estimates, enabling Mr. Eriksson and his associates in the clinical epidemiology unit at the Karolinska Institute, Stockholm, to estimate incidence rates by age and sex. They used data collected by the Swedish Rheumatology Quality Register, the National Patient Register, and the Prescribed Drug Register.
To assess incident RA cases they used three different definitions of new-onset disease. The most restrictive definition involved patients who met all of five separate defining criteria: a first-ever inpatient visit, a specialist outpatient visit, or inclusion in the Swedish Rheumatology Quality Register with a RA diagnosis during 2006-2008; at least one visit to a rheumatology or internal medicine department; at least two visits with a diagnosis of RA during 2006-2008; a second visit with a RA diagnosis within 1 year after a first visit; and exclusion of patients treated with a disease-modifying antirheumatic drug more than 6 months before the first visit with a RA diagnosis, pain in joints, or an unspecified diagnosis.
Applying these criteria to the databases for 2006-2008 identified 7,953 patients with a presumed first-time diagnosis of RA, which resulted in a calculated incidence rate of 35 cases/100,000 population per year. Broken down by gender, the rates were 22 cases/100,000 in men and 48 cases/100,000 in women. Mr. Eriksson also reported incidence rates among men and women broken down by age. The peak new-onset rates occurred in people aged 70-79 years, with rates of 60 cases/100,000 per year among men and 86 cases/100,000 per year in women.
To further broaden the analysis, the researchers calculated incidence rates using two less stringent definitions. They applied a "medium" definition that eliminated the exclusion portion of their initial, strict definition. This identified 9,133 new-onset cases during the 3 years studied, with an overall incidence rate of 41 cases/100,000 per year and rates of 25 cases/100,000 per year in men and 55 cases/100,000 per year in women.
A third, "liberal" definition of RA limited the identifying criteria to the first two elements from the original list of five: a first-ever inpatient visit, a specialist outpatient visit, or inclusion in the Swedish Rheumatology Quality Register during 2006-2008; and at least one visit to a rheumatology or internal medicine department. This identified 11,715 new-onset cases in 2006-2008, an overall rate of 52/100,000 per year, with rates of 33/100,000 per year in men and 71/100,000 per year in women, Mr. Eriksson said.
The range of overall annual incidence rates they calculated – 35/100,000, 41/100,000, and 52/100,00 – collectively matched the annual incidence rates in previously reported studies of much smaller numbers of patients in Sweden, the United States, and Finland with newly diagnosed RA, he noted.
Mr. Eriksson said that he had no disclosures.
LONDON – The incidence of rheumatoid arthritis rises with age in both men and women and shows the biggest jump during the sixth decade of life, when the incidence among adults in their 50s nearly doubles compared with those in their 40s, based on findings from an analysis of about 10,000 Swedish patients diagnosed for the first time during 2006-2008.
The nationwide data also showed that peak rheumatoid arthritis (RA) incidence occurs among men and women in their 70s, with a new onset rate of at least 73 cases per 100,000 population annually, Jonas Eriksson said at the Annual European Congress of Rheumatology.
The nationwide Swedish data that allowed analysis of about 10,000 cases far exceeded the scope of previous incidence estimates, enabling Mr. Eriksson and his associates in the clinical epidemiology unit at the Karolinska Institute, Stockholm, to estimate incidence rates by age and sex. They used data collected by the Swedish Rheumatology Quality Register, the National Patient Register, and the Prescribed Drug Register.
To assess incident RA cases they used three different definitions of new-onset disease. The most restrictive definition involved patients who met all of five separate defining criteria: a first-ever inpatient visit, a specialist outpatient visit, or inclusion in the Swedish Rheumatology Quality Register with a RA diagnosis during 2006-2008; at least one visit to a rheumatology or internal medicine department; at least two visits with a diagnosis of RA during 2006-2008; a second visit with a RA diagnosis within 1 year after a first visit; and exclusion of patients treated with a disease-modifying antirheumatic drug more than 6 months before the first visit with a RA diagnosis, pain in joints, or an unspecified diagnosis.
Applying these criteria to the databases for 2006-2008 identified 7,953 patients with a presumed first-time diagnosis of RA, which resulted in a calculated incidence rate of 35 cases/100,000 population per year. Broken down by gender, the rates were 22 cases/100,000 in men and 48 cases/100,000 in women. Mr. Eriksson also reported incidence rates among men and women broken down by age. The peak new-onset rates occurred in people aged 70-79 years, with rates of 60 cases/100,000 per year among men and 86 cases/100,000 per year in women.
To further broaden the analysis, the researchers calculated incidence rates using two less stringent definitions. They applied a "medium" definition that eliminated the exclusion portion of their initial, strict definition. This identified 9,133 new-onset cases during the 3 years studied, with an overall incidence rate of 41 cases/100,000 per year and rates of 25 cases/100,000 per year in men and 55 cases/100,000 per year in women.
A third, "liberal" definition of RA limited the identifying criteria to the first two elements from the original list of five: a first-ever inpatient visit, a specialist outpatient visit, or inclusion in the Swedish Rheumatology Quality Register during 2006-2008; and at least one visit to a rheumatology or internal medicine department. This identified 11,715 new-onset cases in 2006-2008, an overall rate of 52/100,000 per year, with rates of 33/100,000 per year in men and 71/100,000 per year in women, Mr. Eriksson said.
The range of overall annual incidence rates they calculated – 35/100,000, 41/100,000, and 52/100,00 – collectively matched the annual incidence rates in previously reported studies of much smaller numbers of patients in Sweden, the United States, and Finland with newly diagnosed RA, he noted.
Mr. Eriksson said that he had no disclosures.
LONDON – The incidence of rheumatoid arthritis rises with age in both men and women and shows the biggest jump during the sixth decade of life, when the incidence among adults in their 50s nearly doubles compared with those in their 40s, based on findings from an analysis of about 10,000 Swedish patients diagnosed for the first time during 2006-2008.
The nationwide data also showed that peak rheumatoid arthritis (RA) incidence occurs among men and women in their 70s, with a new onset rate of at least 73 cases per 100,000 population annually, Jonas Eriksson said at the Annual European Congress of Rheumatology.
The nationwide Swedish data that allowed analysis of about 10,000 cases far exceeded the scope of previous incidence estimates, enabling Mr. Eriksson and his associates in the clinical epidemiology unit at the Karolinska Institute, Stockholm, to estimate incidence rates by age and sex. They used data collected by the Swedish Rheumatology Quality Register, the National Patient Register, and the Prescribed Drug Register.
To assess incident RA cases they used three different definitions of new-onset disease. The most restrictive definition involved patients who met all of five separate defining criteria: a first-ever inpatient visit, a specialist outpatient visit, or inclusion in the Swedish Rheumatology Quality Register with a RA diagnosis during 2006-2008; at least one visit to a rheumatology or internal medicine department; at least two visits with a diagnosis of RA during 2006-2008; a second visit with a RA diagnosis within 1 year after a first visit; and exclusion of patients treated with a disease-modifying antirheumatic drug more than 6 months before the first visit with a RA diagnosis, pain in joints, or an unspecified diagnosis.
Applying these criteria to the databases for 2006-2008 identified 7,953 patients with a presumed first-time diagnosis of RA, which resulted in a calculated incidence rate of 35 cases/100,000 population per year. Broken down by gender, the rates were 22 cases/100,000 in men and 48 cases/100,000 in women. Mr. Eriksson also reported incidence rates among men and women broken down by age. The peak new-onset rates occurred in people aged 70-79 years, with rates of 60 cases/100,000 per year among men and 86 cases/100,000 per year in women.
To further broaden the analysis, the researchers calculated incidence rates using two less stringent definitions. They applied a "medium" definition that eliminated the exclusion portion of their initial, strict definition. This identified 9,133 new-onset cases during the 3 years studied, with an overall incidence rate of 41 cases/100,000 per year and rates of 25 cases/100,000 per year in men and 55 cases/100,000 per year in women.
A third, "liberal" definition of RA limited the identifying criteria to the first two elements from the original list of five: a first-ever inpatient visit, a specialist outpatient visit, or inclusion in the Swedish Rheumatology Quality Register during 2006-2008; and at least one visit to a rheumatology or internal medicine department. This identified 11,715 new-onset cases in 2006-2008, an overall rate of 52/100,000 per year, with rates of 33/100,000 per year in men and 71/100,000 per year in women, Mr. Eriksson said.
The range of overall annual incidence rates they calculated – 35/100,000, 41/100,000, and 52/100,00 – collectively matched the annual incidence rates in previously reported studies of much smaller numbers of patients in Sweden, the United States, and Finland with newly diagnosed RA, he noted.
Mr. Eriksson said that he had no disclosures.
FROM THE ANNUAL EUROPEAN CONGRESS OF RHEUMATOLOGY
Major Finding: The incidence rate of newly diagnosed rheumatoid arthritis rises with age, peaking among people in their 70s with an incidence of 73 new cases per 100,000 population annually.
Data Source: Review of Swedish national patient registers for 2006-2008, which identified about 10,000 newly diagnosed cases of RA.
Disclosures: Mr. Eriksson said he had no disclosures.
Bariatric Surgery Cuts Mortality, MIs, and Strokes in Morbidly Obese
ORLANDO – Patients undergoing bariatric surgery had a significantly reduced rate of subsequent myocardial infarctions and strokes and significantly increased survival, compared with similar, morbidly obese patients who had other types of surgery, in a retrospective cohort study of more than 9,000 U.S. patients.
The results "add to the growing evidence that bariatric surgery plays a role in temporizing the risk factors for major cardiovascular events. We believe our analysis builds on prior reports and takes them a step further by evaluating actual events," Dr. John D. Scott said at the annual meeting of the American Society for Metabolic and Bariatric Surgery.
In his study of bariatric surgery patients in South Carolina during 1996-2008, the combined rate of MIs, strokes, and deaths was 52% below the rate in patients undergoing gastrointestinal surgery, and 28% below the rate of those who had orthopedic surgery – both statistically significant differences. The results also showed significant drops in each component of the combined end point (MIs, strokes, and deaths).
"Previous literature demonstrated that cardiovascular risk declined after bariatric surgery. What this study did was look at the rate of actual cardiovascular events, which significantly declined after bariatric surgery," said Dr. Scott, a bariatric surgeon at University Medical Center Greenville (S.C.) Hospital System.
The new study used hospital in-patient records collected during 1996-2008 through the South Carolina Office of Research and Statistics, and death data collected by the South Carolina Department of Health and Environmental Control. The analysis included morbidly obese patients aged 40-79 years who underwent nonemergency surgery (4,747 patients who had any form of bariatric surgery, 3,066 patients who underwent joint replacement or spinal surgery, and 1,327 patients who had a cholecystectomy, hernia repair, or lysis of gastrointestinal adhesions). Those with a history of prior MI or stroke were excluded.
Patients were followed for an average of 14 months after bariatric surgery, 25 after orthopedic surgery, and 26 months after gastrointestinal surgery.
In a multivariate analysis that controlled for age, sex, race, hypertension, dyslipidemia, diabetes, coronary artery disease, obstructive sleep apnea, and a history of transient ischemic attack, patients undergoing bariatric surgery had a significant 41% reduced rate of first MI compared with the orthopedic surgery patients, and a significant 51% lower rate compared with the gastrointestinal surgery patients.
Mortality in the bariatric surgery patients dropped by a significant 19% and 55% relative to the orthopedic and gastrointestinal patients, respectively, and the stroke rate was also significantly lower following bariatric surgery compared with the rates in each control group. The magnitude of these event-rate reductions was consistent with prior reports of risk reduction, Dr. Scott said.
Notably, bariatric surgery "reduced cardiovascular events, as opposed to obesity-drug treatments that may actually increase the risk for cardiovascular events," he noted. "Bariatric surgery has been rigorously tested and [proved] over the past 20 years, and it has a dramatic effect on all aspects of patient health. [Most] medical treatments for obesity don’t have 20 years of data, and some medications actually cause heart problems. We don’t know how bariatric surgery reduced myocardial infarctions and strokes, but it’s probably several factors: weight loss and resolution of diabetes, hypertension, and sleep apnea. The spectrum of returning patients to a more normal, baseline state probably leads to less morbidity and mortality," Dr. Scott said.
Dr. Scott said that he has been a speaker for Gore.
Dr. Scott and his associates have attempted to address a quintessential question about bariatric surgery: Does it reduce the long-term mortality associated with obesity? About 10 prior reports in the literature have also attempted to address this, including one published in the same week that Dr. Scott presented his findings (JAMA 2011;305:2419-26). All of these studies have weaknesses, mostly involving the control group. Because nonsurgical patients who received medical management typically are used as the control group, this often raises the question of whether the control patients were sicker than the surgical patients.
Dr. Scott’s study avoided this weakness by comparing bariatric surgery patients with other surgery patients. This eliminated the bias of greater sickness, as all patients in the study were healthy enough to undergo elective surgery. It also eliminated any bias stemming from access to surgical and medical care.
Despite this, the bariatric surgery and control groups differed in demographics and comorbidities. It seems as though the between-group differences were too extensive to allow for adequate adjustment by a multivariate analysis. In addition, the study included no information on body mass index, so no adjustment was possible for this variable.
I believe the impact of bariatric surgery can only be reliably tested in a randomized, controlled trial. The biases embedded in databases cannot be fully eliminated; the only way to address this question objectively is with a randomized trial.
Philip Schauer, M.D., is director of the bariatric and metabolic institute at the Cleveland Clinic. He made these comments as the designated discussant of Dr. Scott’s paper. He said that he has received teaching grants from Allergan and Covidien; consulting fees as a member of the advisory board of and research support from Bard/Davol and Ethicon Endo-Surgery; consulting fees from Baxter Healthcare, Cardinal Health, and Stryker Endoscopy; and support from RemedyMD.
Dr. Scott and his associates have attempted to address a quintessential question about bariatric surgery: Does it reduce the long-term mortality associated with obesity? About 10 prior reports in the literature have also attempted to address this, including one published in the same week that Dr. Scott presented his findings (JAMA 2011;305:2419-26). All of these studies have weaknesses, mostly involving the control group. Because nonsurgical patients who received medical management typically are used as the control group, this often raises the question of whether the control patients were sicker than the surgical patients.
Dr. Scott’s study avoided this weakness by comparing bariatric surgery patients with other surgery patients. This eliminated the bias of greater sickness, as all patients in the study were healthy enough to undergo elective surgery. It also eliminated any bias stemming from access to surgical and medical care.
Despite this, the bariatric surgery and control groups differed in demographics and comorbidities. It seems as though the between-group differences were too extensive to allow for adequate adjustment by a multivariate analysis. In addition, the study included no information on body mass index, so no adjustment was possible for this variable.
I believe the impact of bariatric surgery can only be reliably tested in a randomized, controlled trial. The biases embedded in databases cannot be fully eliminated; the only way to address this question objectively is with a randomized trial.
Philip Schauer, M.D., is director of the bariatric and metabolic institute at the Cleveland Clinic. He made these comments as the designated discussant of Dr. Scott’s paper. He said that he has received teaching grants from Allergan and Covidien; consulting fees as a member of the advisory board of and research support from Bard/Davol and Ethicon Endo-Surgery; consulting fees from Baxter Healthcare, Cardinal Health, and Stryker Endoscopy; and support from RemedyMD.
Dr. Scott and his associates have attempted to address a quintessential question about bariatric surgery: Does it reduce the long-term mortality associated with obesity? About 10 prior reports in the literature have also attempted to address this, including one published in the same week that Dr. Scott presented his findings (JAMA 2011;305:2419-26). All of these studies have weaknesses, mostly involving the control group. Because nonsurgical patients who received medical management typically are used as the control group, this often raises the question of whether the control patients were sicker than the surgical patients.
Dr. Scott’s study avoided this weakness by comparing bariatric surgery patients with other surgery patients. This eliminated the bias of greater sickness, as all patients in the study were healthy enough to undergo elective surgery. It also eliminated any bias stemming from access to surgical and medical care.
Despite this, the bariatric surgery and control groups differed in demographics and comorbidities. It seems as though the between-group differences were too extensive to allow for adequate adjustment by a multivariate analysis. In addition, the study included no information on body mass index, so no adjustment was possible for this variable.
I believe the impact of bariatric surgery can only be reliably tested in a randomized, controlled trial. The biases embedded in databases cannot be fully eliminated; the only way to address this question objectively is with a randomized trial.
Philip Schauer, M.D., is director of the bariatric and metabolic institute at the Cleveland Clinic. He made these comments as the designated discussant of Dr. Scott’s paper. He said that he has received teaching grants from Allergan and Covidien; consulting fees as a member of the advisory board of and research support from Bard/Davol and Ethicon Endo-Surgery; consulting fees from Baxter Healthcare, Cardinal Health, and Stryker Endoscopy; and support from RemedyMD.
ORLANDO – Patients undergoing bariatric surgery had a significantly reduced rate of subsequent myocardial infarctions and strokes and significantly increased survival, compared with similar, morbidly obese patients who had other types of surgery, in a retrospective cohort study of more than 9,000 U.S. patients.
The results "add to the growing evidence that bariatric surgery plays a role in temporizing the risk factors for major cardiovascular events. We believe our analysis builds on prior reports and takes them a step further by evaluating actual events," Dr. John D. Scott said at the annual meeting of the American Society for Metabolic and Bariatric Surgery.
In his study of bariatric surgery patients in South Carolina during 1996-2008, the combined rate of MIs, strokes, and deaths was 52% below the rate in patients undergoing gastrointestinal surgery, and 28% below the rate of those who had orthopedic surgery – both statistically significant differences. The results also showed significant drops in each component of the combined end point (MIs, strokes, and deaths).
"Previous literature demonstrated that cardiovascular risk declined after bariatric surgery. What this study did was look at the rate of actual cardiovascular events, which significantly declined after bariatric surgery," said Dr. Scott, a bariatric surgeon at University Medical Center Greenville (S.C.) Hospital System.
The new study used hospital in-patient records collected during 1996-2008 through the South Carolina Office of Research and Statistics, and death data collected by the South Carolina Department of Health and Environmental Control. The analysis included morbidly obese patients aged 40-79 years who underwent nonemergency surgery (4,747 patients who had any form of bariatric surgery, 3,066 patients who underwent joint replacement or spinal surgery, and 1,327 patients who had a cholecystectomy, hernia repair, or lysis of gastrointestinal adhesions). Those with a history of prior MI or stroke were excluded.
Patients were followed for an average of 14 months after bariatric surgery, 25 after orthopedic surgery, and 26 months after gastrointestinal surgery.
In a multivariate analysis that controlled for age, sex, race, hypertension, dyslipidemia, diabetes, coronary artery disease, obstructive sleep apnea, and a history of transient ischemic attack, patients undergoing bariatric surgery had a significant 41% reduced rate of first MI compared with the orthopedic surgery patients, and a significant 51% lower rate compared with the gastrointestinal surgery patients.
Mortality in the bariatric surgery patients dropped by a significant 19% and 55% relative to the orthopedic and gastrointestinal patients, respectively, and the stroke rate was also significantly lower following bariatric surgery compared with the rates in each control group. The magnitude of these event-rate reductions was consistent with prior reports of risk reduction, Dr. Scott said.
Notably, bariatric surgery "reduced cardiovascular events, as opposed to obesity-drug treatments that may actually increase the risk for cardiovascular events," he noted. "Bariatric surgery has been rigorously tested and [proved] over the past 20 years, and it has a dramatic effect on all aspects of patient health. [Most] medical treatments for obesity don’t have 20 years of data, and some medications actually cause heart problems. We don’t know how bariatric surgery reduced myocardial infarctions and strokes, but it’s probably several factors: weight loss and resolution of diabetes, hypertension, and sleep apnea. The spectrum of returning patients to a more normal, baseline state probably leads to less morbidity and mortality," Dr. Scott said.
Dr. Scott said that he has been a speaker for Gore.
ORLANDO – Patients undergoing bariatric surgery had a significantly reduced rate of subsequent myocardial infarctions and strokes and significantly increased survival, compared with similar, morbidly obese patients who had other types of surgery, in a retrospective cohort study of more than 9,000 U.S. patients.
The results "add to the growing evidence that bariatric surgery plays a role in temporizing the risk factors for major cardiovascular events. We believe our analysis builds on prior reports and takes them a step further by evaluating actual events," Dr. John D. Scott said at the annual meeting of the American Society for Metabolic and Bariatric Surgery.
In his study of bariatric surgery patients in South Carolina during 1996-2008, the combined rate of MIs, strokes, and deaths was 52% below the rate in patients undergoing gastrointestinal surgery, and 28% below the rate of those who had orthopedic surgery – both statistically significant differences. The results also showed significant drops in each component of the combined end point (MIs, strokes, and deaths).
"Previous literature demonstrated that cardiovascular risk declined after bariatric surgery. What this study did was look at the rate of actual cardiovascular events, which significantly declined after bariatric surgery," said Dr. Scott, a bariatric surgeon at University Medical Center Greenville (S.C.) Hospital System.
The new study used hospital in-patient records collected during 1996-2008 through the South Carolina Office of Research and Statistics, and death data collected by the South Carolina Department of Health and Environmental Control. The analysis included morbidly obese patients aged 40-79 years who underwent nonemergency surgery (4,747 patients who had any form of bariatric surgery, 3,066 patients who underwent joint replacement or spinal surgery, and 1,327 patients who had a cholecystectomy, hernia repair, or lysis of gastrointestinal adhesions). Those with a history of prior MI or stroke were excluded.
Patients were followed for an average of 14 months after bariatric surgery, 25 after orthopedic surgery, and 26 months after gastrointestinal surgery.
In a multivariate analysis that controlled for age, sex, race, hypertension, dyslipidemia, diabetes, coronary artery disease, obstructive sleep apnea, and a history of transient ischemic attack, patients undergoing bariatric surgery had a significant 41% reduced rate of first MI compared with the orthopedic surgery patients, and a significant 51% lower rate compared with the gastrointestinal surgery patients.
Mortality in the bariatric surgery patients dropped by a significant 19% and 55% relative to the orthopedic and gastrointestinal patients, respectively, and the stroke rate was also significantly lower following bariatric surgery compared with the rates in each control group. The magnitude of these event-rate reductions was consistent with prior reports of risk reduction, Dr. Scott said.
Notably, bariatric surgery "reduced cardiovascular events, as opposed to obesity-drug treatments that may actually increase the risk for cardiovascular events," he noted. "Bariatric surgery has been rigorously tested and [proved] over the past 20 years, and it has a dramatic effect on all aspects of patient health. [Most] medical treatments for obesity don’t have 20 years of data, and some medications actually cause heart problems. We don’t know how bariatric surgery reduced myocardial infarctions and strokes, but it’s probably several factors: weight loss and resolution of diabetes, hypertension, and sleep apnea. The spectrum of returning patients to a more normal, baseline state probably leads to less morbidity and mortality," Dr. Scott said.
Dr. Scott said that he has been a speaker for Gore.
FROM THE ANNUAL MEETING OF THE AMERICAN SOCIETY FOR METABOLIC AND BARIATRIC SURGERY
Major Finding: Bariatric surgery patients had a statistically significant 28% reduced relative rate of death, MI, or stroke, compared with orthopedic surgery patients, and a significant 52% reduced relative rate of these end points, compared with gastrointestinal surgery patients, in an adjusted multivariate analysis.
Data Source: Retrospective cohort study of 9,140 morbidly obese patients who underwent elective bariatric, orthopedic, or gastrointestinal surgery in South Carolina during 1996-2008.
Disclosures: Dr. Scott said that he has been a speaker for Gore.
Crizotinib Boosts Overall Survival of ALK+ Lung Cancer
AMSTERDAM – Crizotinib treatment boosted overall survival of selected patients with advanced non–small cell lung cancer by about a year compared with patients on standard chemotherapy in a historical control analysis, adding to the growing body of evidence for the efficacy of this novel targeted therapy.
"Crizotinib may prolong overall survival and fundamentally alter the natural history" of NSCLC that features alterations in the anaplastic lymphoma kinase (ALK) gene, Dr. Alice T. Shaw said at the World Conference on Lung Cancer. Results from several recent studies indicated that about 7% of patients with advanced NSCLC have ALK-positive tumors in which the gene is rearranged.
Results from Dr. Shaw’s new analysis also indicated that the overall survival of patients with ALK-positive NSCLC closely tracked the survival rate of patients with normal ALK genes and advanced NSCLC, suggesting that the presence of ALK mutation does not change prognosis.
"ALK-positive patients do not intrinsically do better on their own, but you can make them live a lot longer if you give them this targeted therapy, crizotinib," said Dr. Shaw, an oncologist at Harvard Medical School and Massachusetts General Hospital, both in Boston.
In May, the Food and Drug Administration began a priority review of crizotinib, an ALK inhibitor, for an indication to treat patients with advanced, ALK-positive NSCLC.
"For regulatory approval, people look at overall survival, but you’ll never get [overall survival] from the large randomized studies because it would be unethical not to let patients [who were initially randomized to not receive crizotinib] cross over. That’s why this analysis is important, even with its flaws, because it shows – or at least strongly suggests – that this drug improves overall survival, that we are really making a difference for these patients," Dr. Shaw said in an interview. Prior reports from crizotinib studies in ALK-positive patients documented a response rate of 50%-60%, and a median progression-free survival of 10 months.
Dr. Shaw and her associates used data on patients who were treated with crizotinib from the first, phase I study of the drug, because those patients have had the longest follow-up on the drug, a median of 18 months for those who remained alive (N. Engl. J. Med. 2010;363:1693-703).
The phase I crizotinib study included 82 ALK-positive patients who received the drug. To better match these patients with a control group of ALK-positive patients who never got crizotinib, the researchers focused on the 56 patients who came from study centers in the United States and Australia, and specifically on the 30 patients within this subgroup who received crizotinib as their second or third chemotherapy agent.
They compared overall survival of these 30 patients with 21 ALK-positive patients from the United States or Australia who had been assessed for potential enrollment in the phase I study but never received crizotinib. In addition, during follow-up all of these control patients remained on second-line chemotherapy.
The new analysis showed that the 30 crizotinib-treated patients had an overall 1-year survival rate of 74%, and a 2-year rate of 54%, with median survival not yet reached during the median 18-month follow-up. The 21 matched control patients had a 1-year survival rate of 44% and a 2-year rate of 12%, and median survival duration of 6 months. Calculations showed a hazard ratio for overall survival of 0.36 for the patients who did not get crizotinib compared with those who did (P = .004).
"These results suggest that crizotinib may significantly improve survival outcomes in patients with advanced ALK-positive NSCLC," Dr. Shaw said.
To confirm that ALK positivity itself played no role in overall survival, Dr. Shaw and her associates compared overall survival in the 21 control patients who never received crizotinib vs. 48 patients who had advanced NSCLC without any ALK mutations, who never received crizotinib, and who had been treated with standard, second-line chemotherapy. In addition, all 48 control patients and all 21 ALK-positive patients had tumors with adenocarcinoma histology, and they all had a history of being never or light smokers. The two groups had virtually identical overall survival rates, Dr. Shaw reported at the meeting, which was sponsored by the International Association for the Study of Lung Cancer.
The crizotinib study that provided much of the data used in this analysis was funded by Pfizer, the company developing the drug. Dr. Shaw said that she has been a consultant to Pfizer, Ariad, Chugai, and Millennium. She has received research support from Novartis and AstraZeneca.
AMSTERDAM – Crizotinib treatment boosted overall survival of selected patients with advanced non–small cell lung cancer by about a year compared with patients on standard chemotherapy in a historical control analysis, adding to the growing body of evidence for the efficacy of this novel targeted therapy.
"Crizotinib may prolong overall survival and fundamentally alter the natural history" of NSCLC that features alterations in the anaplastic lymphoma kinase (ALK) gene, Dr. Alice T. Shaw said at the World Conference on Lung Cancer. Results from several recent studies indicated that about 7% of patients with advanced NSCLC have ALK-positive tumors in which the gene is rearranged.
Results from Dr. Shaw’s new analysis also indicated that the overall survival of patients with ALK-positive NSCLC closely tracked the survival rate of patients with normal ALK genes and advanced NSCLC, suggesting that the presence of ALK mutation does not change prognosis.
"ALK-positive patients do not intrinsically do better on their own, but you can make them live a lot longer if you give them this targeted therapy, crizotinib," said Dr. Shaw, an oncologist at Harvard Medical School and Massachusetts General Hospital, both in Boston.
In May, the Food and Drug Administration began a priority review of crizotinib, an ALK inhibitor, for an indication to treat patients with advanced, ALK-positive NSCLC.
"For regulatory approval, people look at overall survival, but you’ll never get [overall survival] from the large randomized studies because it would be unethical not to let patients [who were initially randomized to not receive crizotinib] cross over. That’s why this analysis is important, even with its flaws, because it shows – or at least strongly suggests – that this drug improves overall survival, that we are really making a difference for these patients," Dr. Shaw said in an interview. Prior reports from crizotinib studies in ALK-positive patients documented a response rate of 50%-60%, and a median progression-free survival of 10 months.
Dr. Shaw and her associates used data on patients who were treated with crizotinib from the first, phase I study of the drug, because those patients have had the longest follow-up on the drug, a median of 18 months for those who remained alive (N. Engl. J. Med. 2010;363:1693-703).
The phase I crizotinib study included 82 ALK-positive patients who received the drug. To better match these patients with a control group of ALK-positive patients who never got crizotinib, the researchers focused on the 56 patients who came from study centers in the United States and Australia, and specifically on the 30 patients within this subgroup who received crizotinib as their second or third chemotherapy agent.
They compared overall survival of these 30 patients with 21 ALK-positive patients from the United States or Australia who had been assessed for potential enrollment in the phase I study but never received crizotinib. In addition, during follow-up all of these control patients remained on second-line chemotherapy.
The new analysis showed that the 30 crizotinib-treated patients had an overall 1-year survival rate of 74%, and a 2-year rate of 54%, with median survival not yet reached during the median 18-month follow-up. The 21 matched control patients had a 1-year survival rate of 44% and a 2-year rate of 12%, and median survival duration of 6 months. Calculations showed a hazard ratio for overall survival of 0.36 for the patients who did not get crizotinib compared with those who did (P = .004).
"These results suggest that crizotinib may significantly improve survival outcomes in patients with advanced ALK-positive NSCLC," Dr. Shaw said.
To confirm that ALK positivity itself played no role in overall survival, Dr. Shaw and her associates compared overall survival in the 21 control patients who never received crizotinib vs. 48 patients who had advanced NSCLC without any ALK mutations, who never received crizotinib, and who had been treated with standard, second-line chemotherapy. In addition, all 48 control patients and all 21 ALK-positive patients had tumors with adenocarcinoma histology, and they all had a history of being never or light smokers. The two groups had virtually identical overall survival rates, Dr. Shaw reported at the meeting, which was sponsored by the International Association for the Study of Lung Cancer.
The crizotinib study that provided much of the data used in this analysis was funded by Pfizer, the company developing the drug. Dr. Shaw said that she has been a consultant to Pfizer, Ariad, Chugai, and Millennium. She has received research support from Novartis and AstraZeneca.
AMSTERDAM – Crizotinib treatment boosted overall survival of selected patients with advanced non–small cell lung cancer by about a year compared with patients on standard chemotherapy in a historical control analysis, adding to the growing body of evidence for the efficacy of this novel targeted therapy.
"Crizotinib may prolong overall survival and fundamentally alter the natural history" of NSCLC that features alterations in the anaplastic lymphoma kinase (ALK) gene, Dr. Alice T. Shaw said at the World Conference on Lung Cancer. Results from several recent studies indicated that about 7% of patients with advanced NSCLC have ALK-positive tumors in which the gene is rearranged.
Results from Dr. Shaw’s new analysis also indicated that the overall survival of patients with ALK-positive NSCLC closely tracked the survival rate of patients with normal ALK genes and advanced NSCLC, suggesting that the presence of ALK mutation does not change prognosis.
"ALK-positive patients do not intrinsically do better on their own, but you can make them live a lot longer if you give them this targeted therapy, crizotinib," said Dr. Shaw, an oncologist at Harvard Medical School and Massachusetts General Hospital, both in Boston.
In May, the Food and Drug Administration began a priority review of crizotinib, an ALK inhibitor, for an indication to treat patients with advanced, ALK-positive NSCLC.
"For regulatory approval, people look at overall survival, but you’ll never get [overall survival] from the large randomized studies because it would be unethical not to let patients [who were initially randomized to not receive crizotinib] cross over. That’s why this analysis is important, even with its flaws, because it shows – or at least strongly suggests – that this drug improves overall survival, that we are really making a difference for these patients," Dr. Shaw said in an interview. Prior reports from crizotinib studies in ALK-positive patients documented a response rate of 50%-60%, and a median progression-free survival of 10 months.
Dr. Shaw and her associates used data on patients who were treated with crizotinib from the first, phase I study of the drug, because those patients have had the longest follow-up on the drug, a median of 18 months for those who remained alive (N. Engl. J. Med. 2010;363:1693-703).
The phase I crizotinib study included 82 ALK-positive patients who received the drug. To better match these patients with a control group of ALK-positive patients who never got crizotinib, the researchers focused on the 56 patients who came from study centers in the United States and Australia, and specifically on the 30 patients within this subgroup who received crizotinib as their second or third chemotherapy agent.
They compared overall survival of these 30 patients with 21 ALK-positive patients from the United States or Australia who had been assessed for potential enrollment in the phase I study but never received crizotinib. In addition, during follow-up all of these control patients remained on second-line chemotherapy.
The new analysis showed that the 30 crizotinib-treated patients had an overall 1-year survival rate of 74%, and a 2-year rate of 54%, with median survival not yet reached during the median 18-month follow-up. The 21 matched control patients had a 1-year survival rate of 44% and a 2-year rate of 12%, and median survival duration of 6 months. Calculations showed a hazard ratio for overall survival of 0.36 for the patients who did not get crizotinib compared with those who did (P = .004).
"These results suggest that crizotinib may significantly improve survival outcomes in patients with advanced ALK-positive NSCLC," Dr. Shaw said.
To confirm that ALK positivity itself played no role in overall survival, Dr. Shaw and her associates compared overall survival in the 21 control patients who never received crizotinib vs. 48 patients who had advanced NSCLC without any ALK mutations, who never received crizotinib, and who had been treated with standard, second-line chemotherapy. In addition, all 48 control patients and all 21 ALK-positive patients had tumors with adenocarcinoma histology, and they all had a history of being never or light smokers. The two groups had virtually identical overall survival rates, Dr. Shaw reported at the meeting, which was sponsored by the International Association for the Study of Lung Cancer.
The crizotinib study that provided much of the data used in this analysis was funded by Pfizer, the company developing the drug. Dr. Shaw said that she has been a consultant to Pfizer, Ariad, Chugai, and Millennium. She has received research support from Novartis and AstraZeneca.
FROM THE WORLD CONFERENCE ON LUNG CANCER
Major Finding: Selected patients with ALK-positive, advanced NSCLC treated with crizotinib had a 1-year overall survival rate of 74% and a 2-year rate of 54%, compared with rates of 44% and 12%, respectively, in matched patients who did not receive crizotinib. The HR for survival among the patients not on crizotinib was 0.36, compared with those who got the drug (P = .004).
Data Source: The 18-month median follow-up data from a phase I study of crizotinib-treated patients, and follow-up on matched ALK-positive patients who had been evaluated for possible treatment in this trial but who never received crizotinib.
Disclosures: The crizotinib study that provided much of the data used in this analysis was funded by Pfizer, the company developing the drug. Dr. Shaw said that she has been a consultant to Pfizer, Ariad, Chugai, and Millennium. She has received research support from Novartis and AstraZeneca.
Rheumatoid Arthritis Drug Trials Often Lack Comparator Regimens
LONDON – Many recently performed rheumatology drug trials ran into the ethical trap of treating control patients with an ineffective regimen, with the result that some patients experienced ongoing pain and joint dysfunction and continued disease progression.
"I would propose that we change the trial design for the placebo control to use an active comparator against the [investigational] drug," Dr. Aaron Juche said while presenting a poster at the annual European Congress of Rheumatology.
In most cases for current studies testing a new drug aimed at controlling rheumatoid arthritis pain, dysfunction, and progression, "the standard of care would be a tumor necrosis factor [TNF] inhibitor as the active comparator," said Dr. Juche, a rheumatologist at Johanniter Hospital in Treuenbrietzen, Germany. Because TNF inhibitors are so effective, a study that uses this treatment in the comparator arm would likely have to be a noninferiority study and would also probably have to involve a relatively large number of patients, he said in an interview.
Dr. Juche said he first became interested in this issue because he "wondered whether placebo-treated patients [in recent drug trials] were being treated as I would treat a patient in standard practice." The standard approach for drug-trial design in patients with rheumatoid arthritis (RA) in recent years has been to follow a model that’s more than a decade old, dating back to the first studies on TNF inhibitors during the 1990s: "Patients who did not adequately respond to immunosuppressive drugs were randomly assigned to either an experimental condition under which they received the new substance, or to a control condition under which they continued their formerly inefficient treatment and received a placebo."
To more systematically assess the scope of the problem, he and his associate reviewed 17 recent, published clinical trials that drug companies used to document the safety and efficacy of three new drugs, abatacept, golimumab, and tocilizumab, to the European Medicines Agency. Dr. Juche said these studies fairly represented most recently performed drug efficacy trials for patients with RA.
Of the seven studies he reviewed that tested abatacept, none used a control therapy that effectively treated the patients’ disease. In all seven studies, patients remained on treatment with a disease-modifying antirheumatic drug (DMARD) that they had already failed on, most commonly methotrexate. During these studies, "patients experienced a persistent, high disease activity," Dr. Juche reported in his poster.
Among four pivotal studies involving golimumab, one enrolled methotrexate-naive patients and then used methotrexate as the control drug. The other three used control groups that either received placebo and nothing else, or placebo plus methotrexate for enrolled patients who had already failed methotrexate.
A similar pattern existed for the six studies of tocilizumab that Dr. Juche reviewed. One of the six studies used methotrexate as the comparator in a trial that enrolled methotrexate-naive patients. The other five studies used comparator groups on either placebo alone or placebo plus a DMARD to which the patient had already not responded.
Dr. Juche added that he did not believe that rheumatology was a unique medical specialty in having so many of its trials involve ineffective regimens in the control groups, but he did not systematically assess efficacy trials done in other specialties. As a rheumatologist, he focused his attention only on those studies from his specialty.
These designs run counter to the stipulations of the 2008 Declaration of Helsinki of the World Medical Association, Dr. Juche noted. The Declaration said: "The benefits, risks, burdens, and effectiveness of a new intervention must be tested against those of the best current proven intervention, except ... where no current proven intervention exists or where, for compelling and scientifically sound methodological reasons, the use of placebo is necessary to determine the efficacy of an intervention and the patients who receive placebo or no treatment will not be subject to any risk or serious or irreversible harm."
Dr. Juche said that he has received travel expense support from Actelion.
LONDON – Many recently performed rheumatology drug trials ran into the ethical trap of treating control patients with an ineffective regimen, with the result that some patients experienced ongoing pain and joint dysfunction and continued disease progression.
"I would propose that we change the trial design for the placebo control to use an active comparator against the [investigational] drug," Dr. Aaron Juche said while presenting a poster at the annual European Congress of Rheumatology.
In most cases for current studies testing a new drug aimed at controlling rheumatoid arthritis pain, dysfunction, and progression, "the standard of care would be a tumor necrosis factor [TNF] inhibitor as the active comparator," said Dr. Juche, a rheumatologist at Johanniter Hospital in Treuenbrietzen, Germany. Because TNF inhibitors are so effective, a study that uses this treatment in the comparator arm would likely have to be a noninferiority study and would also probably have to involve a relatively large number of patients, he said in an interview.
Dr. Juche said he first became interested in this issue because he "wondered whether placebo-treated patients [in recent drug trials] were being treated as I would treat a patient in standard practice." The standard approach for drug-trial design in patients with rheumatoid arthritis (RA) in recent years has been to follow a model that’s more than a decade old, dating back to the first studies on TNF inhibitors during the 1990s: "Patients who did not adequately respond to immunosuppressive drugs were randomly assigned to either an experimental condition under which they received the new substance, or to a control condition under which they continued their formerly inefficient treatment and received a placebo."
To more systematically assess the scope of the problem, he and his associate reviewed 17 recent, published clinical trials that drug companies used to document the safety and efficacy of three new drugs, abatacept, golimumab, and tocilizumab, to the European Medicines Agency. Dr. Juche said these studies fairly represented most recently performed drug efficacy trials for patients with RA.
Of the seven studies he reviewed that tested abatacept, none used a control therapy that effectively treated the patients’ disease. In all seven studies, patients remained on treatment with a disease-modifying antirheumatic drug (DMARD) that they had already failed on, most commonly methotrexate. During these studies, "patients experienced a persistent, high disease activity," Dr. Juche reported in his poster.
Among four pivotal studies involving golimumab, one enrolled methotrexate-naive patients and then used methotrexate as the control drug. The other three used control groups that either received placebo and nothing else, or placebo plus methotrexate for enrolled patients who had already failed methotrexate.
A similar pattern existed for the six studies of tocilizumab that Dr. Juche reviewed. One of the six studies used methotrexate as the comparator in a trial that enrolled methotrexate-naive patients. The other five studies used comparator groups on either placebo alone or placebo plus a DMARD to which the patient had already not responded.
Dr. Juche added that he did not believe that rheumatology was a unique medical specialty in having so many of its trials involve ineffective regimens in the control groups, but he did not systematically assess efficacy trials done in other specialties. As a rheumatologist, he focused his attention only on those studies from his specialty.
These designs run counter to the stipulations of the 2008 Declaration of Helsinki of the World Medical Association, Dr. Juche noted. The Declaration said: "The benefits, risks, burdens, and effectiveness of a new intervention must be tested against those of the best current proven intervention, except ... where no current proven intervention exists or where, for compelling and scientifically sound methodological reasons, the use of placebo is necessary to determine the efficacy of an intervention and the patients who receive placebo or no treatment will not be subject to any risk or serious or irreversible harm."
Dr. Juche said that he has received travel expense support from Actelion.
LONDON – Many recently performed rheumatology drug trials ran into the ethical trap of treating control patients with an ineffective regimen, with the result that some patients experienced ongoing pain and joint dysfunction and continued disease progression.
"I would propose that we change the trial design for the placebo control to use an active comparator against the [investigational] drug," Dr. Aaron Juche said while presenting a poster at the annual European Congress of Rheumatology.
In most cases for current studies testing a new drug aimed at controlling rheumatoid arthritis pain, dysfunction, and progression, "the standard of care would be a tumor necrosis factor [TNF] inhibitor as the active comparator," said Dr. Juche, a rheumatologist at Johanniter Hospital in Treuenbrietzen, Germany. Because TNF inhibitors are so effective, a study that uses this treatment in the comparator arm would likely have to be a noninferiority study and would also probably have to involve a relatively large number of patients, he said in an interview.
Dr. Juche said he first became interested in this issue because he "wondered whether placebo-treated patients [in recent drug trials] were being treated as I would treat a patient in standard practice." The standard approach for drug-trial design in patients with rheumatoid arthritis (RA) in recent years has been to follow a model that’s more than a decade old, dating back to the first studies on TNF inhibitors during the 1990s: "Patients who did not adequately respond to immunosuppressive drugs were randomly assigned to either an experimental condition under which they received the new substance, or to a control condition under which they continued their formerly inefficient treatment and received a placebo."
To more systematically assess the scope of the problem, he and his associate reviewed 17 recent, published clinical trials that drug companies used to document the safety and efficacy of three new drugs, abatacept, golimumab, and tocilizumab, to the European Medicines Agency. Dr. Juche said these studies fairly represented most recently performed drug efficacy trials for patients with RA.
Of the seven studies he reviewed that tested abatacept, none used a control therapy that effectively treated the patients’ disease. In all seven studies, patients remained on treatment with a disease-modifying antirheumatic drug (DMARD) that they had already failed on, most commonly methotrexate. During these studies, "patients experienced a persistent, high disease activity," Dr. Juche reported in his poster.
Among four pivotal studies involving golimumab, one enrolled methotrexate-naive patients and then used methotrexate as the control drug. The other three used control groups that either received placebo and nothing else, or placebo plus methotrexate for enrolled patients who had already failed methotrexate.
A similar pattern existed for the six studies of tocilizumab that Dr. Juche reviewed. One of the six studies used methotrexate as the comparator in a trial that enrolled methotrexate-naive patients. The other five studies used comparator groups on either placebo alone or placebo plus a DMARD to which the patient had already not responded.
Dr. Juche added that he did not believe that rheumatology was a unique medical specialty in having so many of its trials involve ineffective regimens in the control groups, but he did not systematically assess efficacy trials done in other specialties. As a rheumatologist, he focused his attention only on those studies from his specialty.
These designs run counter to the stipulations of the 2008 Declaration of Helsinki of the World Medical Association, Dr. Juche noted. The Declaration said: "The benefits, risks, burdens, and effectiveness of a new intervention must be tested against those of the best current proven intervention, except ... where no current proven intervention exists or where, for compelling and scientifically sound methodological reasons, the use of placebo is necessary to determine the efficacy of an intervention and the patients who receive placebo or no treatment will not be subject to any risk or serious or irreversible harm."
Dr. Juche said that he has received travel expense support from Actelion.
FROM THE ANNUAL EUROPEAN CONGRESS OF RHEUMATOLOGY
Major Finding: A review of 17 recent clinical trials for three new rheumatoid arthritis drugs showed that only two of the trials placed patients randomized into the comparator arms on active drug regimens.
Data Source: Review of publicly reported trial data.
Disclosures: Dr. Juche said that he has received travel support from Actelion.
Rheumatoid Arthritis Drug Trials Often Lack Comparator Regimens
LONDON – Many recently performed rheumatology drug trials ran into the ethical trap of treating control patients with an ineffective regimen, with the result that some patients experienced ongoing pain and joint dysfunction and continued disease progression.
"I would propose that we change the trial design for the placebo control to use an active comparator against the [investigational] drug," Dr. Aaron Juche said while presenting a poster at the annual European Congress of Rheumatology.
In most cases for current studies testing a new drug aimed at controlling rheumatoid arthritis pain, dysfunction, and progression, "the standard of care would be a tumor necrosis factor [TNF] inhibitor as the active comparator," said Dr. Juche, a rheumatologist at Johanniter Hospital in Treuenbrietzen, Germany. Because TNF inhibitors are so effective, a study that uses this treatment in the comparator arm would likely have to be a noninferiority study and would also probably have to involve a relatively large number of patients, he said in an interview.
Dr. Juche said he first became interested in this issue because he "wondered whether placebo-treated patients [in recent drug trials] were being treated as I would treat a patient in standard practice." The standard approach for drug-trial design in patients with rheumatoid arthritis (RA) in recent years has been to follow a model that’s more than a decade old, dating back to the first studies on TNF inhibitors during the 1990s: "Patients who did not adequately respond to immunosuppressive drugs were randomly assigned to either an experimental condition under which they received the new substance, or to a control condition under which they continued their formerly inefficient treatment and received a placebo."
To more systematically assess the scope of the problem, he and his associate reviewed 17 recent, published clinical trials that drug companies used to document the safety and efficacy of three new drugs, abatacept, golimumab, and tocilizumab, to the European Medicines Agency. Dr. Juche said these studies fairly represented most recently performed drug efficacy trials for patients with RA.
Of the seven studies he reviewed that tested abatacept, none used a control therapy that effectively treated the patients’ disease. In all seven studies, patients remained on treatment with a disease-modifying antirheumatic drug (DMARD) that they had already failed on, most commonly methotrexate. During these studies, "patients experienced a persistent, high disease activity," Dr. Juche reported in his poster.
Among four pivotal studies involving golimumab, one enrolled methotrexate-naive patients and then used methotrexate as the control drug. The other three used control groups that either received placebo and nothing else, or placebo plus methotrexate for enrolled patients who had already failed methotrexate.
A similar pattern existed for the six studies of tocilizumab that Dr. Juche reviewed. One of the six studies used methotrexate as the comparator in a trial that enrolled methotrexate-naive patients. The other five studies used comparator groups on either placebo alone or placebo plus a DMARD to which the patient had already not responded.
Dr. Juche added that he did not believe that rheumatology was a unique medical specialty in having so many of its trials involve ineffective regimens in the control groups, but he did not systematically assess efficacy trials done in other specialties. As a rheumatologist, he focused his attention only on those studies from his specialty.
These designs run counter to the stipulations of the 2008 Declaration of Helsinki of the World Medical Association, Dr. Juche noted. The Declaration said: "The benefits, risks, burdens, and effectiveness of a new intervention must be tested against those of the best current proven intervention, except ... where no current proven intervention exists or where, for compelling and scientifically sound methodological reasons, the use of placebo is necessary to determine the efficacy of an intervention and the patients who receive placebo or no treatment will not be subject to any risk or serious or irreversible harm."
Dr. Juche said that he has received travel expense support from Actelion.
LONDON – Many recently performed rheumatology drug trials ran into the ethical trap of treating control patients with an ineffective regimen, with the result that some patients experienced ongoing pain and joint dysfunction and continued disease progression.
"I would propose that we change the trial design for the placebo control to use an active comparator against the [investigational] drug," Dr. Aaron Juche said while presenting a poster at the annual European Congress of Rheumatology.
In most cases for current studies testing a new drug aimed at controlling rheumatoid arthritis pain, dysfunction, and progression, "the standard of care would be a tumor necrosis factor [TNF] inhibitor as the active comparator," said Dr. Juche, a rheumatologist at Johanniter Hospital in Treuenbrietzen, Germany. Because TNF inhibitors are so effective, a study that uses this treatment in the comparator arm would likely have to be a noninferiority study and would also probably have to involve a relatively large number of patients, he said in an interview.
Dr. Juche said he first became interested in this issue because he "wondered whether placebo-treated patients [in recent drug trials] were being treated as I would treat a patient in standard practice." The standard approach for drug-trial design in patients with rheumatoid arthritis (RA) in recent years has been to follow a model that’s more than a decade old, dating back to the first studies on TNF inhibitors during the 1990s: "Patients who did not adequately respond to immunosuppressive drugs were randomly assigned to either an experimental condition under which they received the new substance, or to a control condition under which they continued their formerly inefficient treatment and received a placebo."
To more systematically assess the scope of the problem, he and his associate reviewed 17 recent, published clinical trials that drug companies used to document the safety and efficacy of three new drugs, abatacept, golimumab, and tocilizumab, to the European Medicines Agency. Dr. Juche said these studies fairly represented most recently performed drug efficacy trials for patients with RA.
Of the seven studies he reviewed that tested abatacept, none used a control therapy that effectively treated the patients’ disease. In all seven studies, patients remained on treatment with a disease-modifying antirheumatic drug (DMARD) that they had already failed on, most commonly methotrexate. During these studies, "patients experienced a persistent, high disease activity," Dr. Juche reported in his poster.
Among four pivotal studies involving golimumab, one enrolled methotrexate-naive patients and then used methotrexate as the control drug. The other three used control groups that either received placebo and nothing else, or placebo plus methotrexate for enrolled patients who had already failed methotrexate.
A similar pattern existed for the six studies of tocilizumab that Dr. Juche reviewed. One of the six studies used methotrexate as the comparator in a trial that enrolled methotrexate-naive patients. The other five studies used comparator groups on either placebo alone or placebo plus a DMARD to which the patient had already not responded.
Dr. Juche added that he did not believe that rheumatology was a unique medical specialty in having so many of its trials involve ineffective regimens in the control groups, but he did not systematically assess efficacy trials done in other specialties. As a rheumatologist, he focused his attention only on those studies from his specialty.
These designs run counter to the stipulations of the 2008 Declaration of Helsinki of the World Medical Association, Dr. Juche noted. The Declaration said: "The benefits, risks, burdens, and effectiveness of a new intervention must be tested against those of the best current proven intervention, except ... where no current proven intervention exists or where, for compelling and scientifically sound methodological reasons, the use of placebo is necessary to determine the efficacy of an intervention and the patients who receive placebo or no treatment will not be subject to any risk or serious or irreversible harm."
Dr. Juche said that he has received travel expense support from Actelion.
LONDON – Many recently performed rheumatology drug trials ran into the ethical trap of treating control patients with an ineffective regimen, with the result that some patients experienced ongoing pain and joint dysfunction and continued disease progression.
"I would propose that we change the trial design for the placebo control to use an active comparator against the [investigational] drug," Dr. Aaron Juche said while presenting a poster at the annual European Congress of Rheumatology.
In most cases for current studies testing a new drug aimed at controlling rheumatoid arthritis pain, dysfunction, and progression, "the standard of care would be a tumor necrosis factor [TNF] inhibitor as the active comparator," said Dr. Juche, a rheumatologist at Johanniter Hospital in Treuenbrietzen, Germany. Because TNF inhibitors are so effective, a study that uses this treatment in the comparator arm would likely have to be a noninferiority study and would also probably have to involve a relatively large number of patients, he said in an interview.
Dr. Juche said he first became interested in this issue because he "wondered whether placebo-treated patients [in recent drug trials] were being treated as I would treat a patient in standard practice." The standard approach for drug-trial design in patients with rheumatoid arthritis (RA) in recent years has been to follow a model that’s more than a decade old, dating back to the first studies on TNF inhibitors during the 1990s: "Patients who did not adequately respond to immunosuppressive drugs were randomly assigned to either an experimental condition under which they received the new substance, or to a control condition under which they continued their formerly inefficient treatment and received a placebo."
To more systematically assess the scope of the problem, he and his associate reviewed 17 recent, published clinical trials that drug companies used to document the safety and efficacy of three new drugs, abatacept, golimumab, and tocilizumab, to the European Medicines Agency. Dr. Juche said these studies fairly represented most recently performed drug efficacy trials for patients with RA.
Of the seven studies he reviewed that tested abatacept, none used a control therapy that effectively treated the patients’ disease. In all seven studies, patients remained on treatment with a disease-modifying antirheumatic drug (DMARD) that they had already failed on, most commonly methotrexate. During these studies, "patients experienced a persistent, high disease activity," Dr. Juche reported in his poster.
Among four pivotal studies involving golimumab, one enrolled methotrexate-naive patients and then used methotrexate as the control drug. The other three used control groups that either received placebo and nothing else, or placebo plus methotrexate for enrolled patients who had already failed methotrexate.
A similar pattern existed for the six studies of tocilizumab that Dr. Juche reviewed. One of the six studies used methotrexate as the comparator in a trial that enrolled methotrexate-naive patients. The other five studies used comparator groups on either placebo alone or placebo plus a DMARD to which the patient had already not responded.
Dr. Juche added that he did not believe that rheumatology was a unique medical specialty in having so many of its trials involve ineffective regimens in the control groups, but he did not systematically assess efficacy trials done in other specialties. As a rheumatologist, he focused his attention only on those studies from his specialty.
These designs run counter to the stipulations of the 2008 Declaration of Helsinki of the World Medical Association, Dr. Juche noted. The Declaration said: "The benefits, risks, burdens, and effectiveness of a new intervention must be tested against those of the best current proven intervention, except ... where no current proven intervention exists or where, for compelling and scientifically sound methodological reasons, the use of placebo is necessary to determine the efficacy of an intervention and the patients who receive placebo or no treatment will not be subject to any risk or serious or irreversible harm."
Dr. Juche said that he has received travel expense support from Actelion.
FROM THE ANNUAL EUROPEAN CONGRESS OF RHEUMATOLOGY
Major Finding: A review of 17 recent clinical trials for three new rheumatoid arthritis drugs showed that only two of the trials placed patients randomized into the comparator arms on active drug regimens.
Data Source: Review of publicly reported trial data.
Disclosures: Dr. Juche said that he has received travel support from Actelion.
Hereditary Hemochromatosis Linked to Increased Arthropathies and Joint Surgery
LONDON – Patients with hereditary hemochromatosis have a significantly increased prevalence of various arthropathies and an elevated need for joint-replacement surgery, compared with the general population, according to findings from a study of Swedish national registry data.
The analysis also showed that first-degree relatives of people with hereditary hemochromatosis do not have an increased rate of arthropathies or need for joint replacement, even though genetic models predict that a majority of these relatives carry one copy of an autosomal recessive mutation that causes hereditary hemochromatosis.
"This dissociation between the genotype and the phenotype" relative to the risk for arthropathy and need for joint replacement "suggests to me that the gene itself is not involved. It suggests to me that you need more than just the gene" to boost the risk for arthropathy and joint failure, noted Dr. Johan Askling.
Arthropathy is a classic phenotypic feature of patients with hereditary hemochromatosis, a genetic disease in people who carry two mutated copies of the hemochromatosis gene (HFE) associated with iron overload. But the nature of the relationship between the disease and arthropathies remains poorly understood. The new finding that increased arthropathies occur only in homozygous, affected individuals suggests that the risk is linked to iron overload itself, rather than to the causative mutated genes.
Dr. Askling and his associates identified 3,531 patients with a diagnosis of hereditary hemochromatosis from Swedish national records for the period 1999-2006. The investigators also identified another 11,794 first-degree relatives of these patients. They then identified 37,369 people as matched controls for the patients from the general Swedish population and 196,628 people as matched controls for the first-degree relatives.
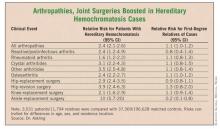
The researchers then tallied the incidence of consultations or hospitalizations for rheumatoid arthritis, osteoarthritis, and other arthritides in the cases, their first-degree relatives, and the controls during the study period. They calculated a relative risk for these complications in affected people and in their relatives, compared with the controls that adjusted for differences in age, sex, and residence location. The researchers also ran similar analyses for the incidence of various joint-replacement surgeries (see table).
The results showed that the patients with hereditary hemochromatosis had consistent, statistically significant increased rates of arthropathies. For example, for all arthropathies the rate was 2.4-fold higher in the patients than in the controls. But this increased rate did not exist among the first-degree relatives. For all arthropathies, their rate was just 10% higher than among the matched controls, a difference that was not significant, reported Dr. Askling, an epidemiologist at the Karolinska Institute in Stockholm.
A similar pattern existed for joint-replacement surgeries. Hip surgery, for example, was 2.9-fold more frequent among the hereditary hemochromatosis patients than among their matched controls, while among the first-degree relatives the incidence of hip-replacement surgery was 10% less common than among the matched controls, a difference that was not statistically significant.
Dr. Askling said that he had no disclosures.
LONDON – Patients with hereditary hemochromatosis have a significantly increased prevalence of various arthropathies and an elevated need for joint-replacement surgery, compared with the general population, according to findings from a study of Swedish national registry data.
The analysis also showed that first-degree relatives of people with hereditary hemochromatosis do not have an increased rate of arthropathies or need for joint replacement, even though genetic models predict that a majority of these relatives carry one copy of an autosomal recessive mutation that causes hereditary hemochromatosis.
"This dissociation between the genotype and the phenotype" relative to the risk for arthropathy and need for joint replacement "suggests to me that the gene itself is not involved. It suggests to me that you need more than just the gene" to boost the risk for arthropathy and joint failure, noted Dr. Johan Askling.
Arthropathy is a classic phenotypic feature of patients with hereditary hemochromatosis, a genetic disease in people who carry two mutated copies of the hemochromatosis gene (HFE) associated with iron overload. But the nature of the relationship between the disease and arthropathies remains poorly understood. The new finding that increased arthropathies occur only in homozygous, affected individuals suggests that the risk is linked to iron overload itself, rather than to the causative mutated genes.
Dr. Askling and his associates identified 3,531 patients with a diagnosis of hereditary hemochromatosis from Swedish national records for the period 1999-2006. The investigators also identified another 11,794 first-degree relatives of these patients. They then identified 37,369 people as matched controls for the patients from the general Swedish population and 196,628 people as matched controls for the first-degree relatives.
The researchers then tallied the incidence of consultations or hospitalizations for rheumatoid arthritis, osteoarthritis, and other arthritides in the cases, their first-degree relatives, and the controls during the study period. They calculated a relative risk for these complications in affected people and in their relatives, compared with the controls that adjusted for differences in age, sex, and residence location. The researchers also ran similar analyses for the incidence of various joint-replacement surgeries (see table).
The results showed that the patients with hereditary hemochromatosis had consistent, statistically significant increased rates of arthropathies. For example, for all arthropathies the rate was 2.4-fold higher in the patients than in the controls. But this increased rate did not exist among the first-degree relatives. For all arthropathies, their rate was just 10% higher than among the matched controls, a difference that was not significant, reported Dr. Askling, an epidemiologist at the Karolinska Institute in Stockholm.
A similar pattern existed for joint-replacement surgeries. Hip surgery, for example, was 2.9-fold more frequent among the hereditary hemochromatosis patients than among their matched controls, while among the first-degree relatives the incidence of hip-replacement surgery was 10% less common than among the matched controls, a difference that was not statistically significant.
Dr. Askling said that he had no disclosures.
LONDON – Patients with hereditary hemochromatosis have a significantly increased prevalence of various arthropathies and an elevated need for joint-replacement surgery, compared with the general population, according to findings from a study of Swedish national registry data.
The analysis also showed that first-degree relatives of people with hereditary hemochromatosis do not have an increased rate of arthropathies or need for joint replacement, even though genetic models predict that a majority of these relatives carry one copy of an autosomal recessive mutation that causes hereditary hemochromatosis.
"This dissociation between the genotype and the phenotype" relative to the risk for arthropathy and need for joint replacement "suggests to me that the gene itself is not involved. It suggests to me that you need more than just the gene" to boost the risk for arthropathy and joint failure, noted Dr. Johan Askling.
Arthropathy is a classic phenotypic feature of patients with hereditary hemochromatosis, a genetic disease in people who carry two mutated copies of the hemochromatosis gene (HFE) associated with iron overload. But the nature of the relationship between the disease and arthropathies remains poorly understood. The new finding that increased arthropathies occur only in homozygous, affected individuals suggests that the risk is linked to iron overload itself, rather than to the causative mutated genes.
Dr. Askling and his associates identified 3,531 patients with a diagnosis of hereditary hemochromatosis from Swedish national records for the period 1999-2006. The investigators also identified another 11,794 first-degree relatives of these patients. They then identified 37,369 people as matched controls for the patients from the general Swedish population and 196,628 people as matched controls for the first-degree relatives.
The researchers then tallied the incidence of consultations or hospitalizations for rheumatoid arthritis, osteoarthritis, and other arthritides in the cases, their first-degree relatives, and the controls during the study period. They calculated a relative risk for these complications in affected people and in their relatives, compared with the controls that adjusted for differences in age, sex, and residence location. The researchers also ran similar analyses for the incidence of various joint-replacement surgeries (see table).
The results showed that the patients with hereditary hemochromatosis had consistent, statistically significant increased rates of arthropathies. For example, for all arthropathies the rate was 2.4-fold higher in the patients than in the controls. But this increased rate did not exist among the first-degree relatives. For all arthropathies, their rate was just 10% higher than among the matched controls, a difference that was not significant, reported Dr. Askling, an epidemiologist at the Karolinska Institute in Stockholm.
A similar pattern existed for joint-replacement surgeries. Hip surgery, for example, was 2.9-fold more frequent among the hereditary hemochromatosis patients than among their matched controls, while among the first-degree relatives the incidence of hip-replacement surgery was 10% less common than among the matched controls, a difference that was not statistically significant.
Dr. Askling said that he had no disclosures.
FROM THE ANNUAL EUROPEAN CONGRESS OF RHEUMATOLOGY
Major Finding: Patients with hereditary hemochromatosis had a 2.4-fold increased prevalence of arthropathies and a 2.9-fold increased rate of hip surgery, compared with matched controls. In contrast, first-degree relatives of hereditary hemochromatosis patients had no significantly different rates for arthropathy or need for joint-replacement surgery, compared with controls.
Data Source: Case-control study of records from Swedish national registries during 1999-2006, with 3,531 patients diagnosed with hereditary hemochromatosis and 37,369 matched controls, and 11,794 first-degree relatives of the patients and 196,628 matched controls.
Disclosures: Dr. Askling said that he had no disclosures.
Hereditary Hemochromatosis Linked to Increased Arthropathies and Joint Surgery
LONDON – Patients with hereditary hemochromatosis have a significantly increased prevalence of various arthropathies and an elevated need for joint-replacement surgery, compared with the general population, according to findings from a study of Swedish national registry data.
The analysis also showed that first-degree relatives of people with hereditary hemochromatosis do not have an increased rate of arthropathies or need for joint replacement, even though genetic models predict that a majority of these relatives carry one copy of an autosomal recessive mutation that causes hereditary hemochromatosis.
"This dissociation between the genotype and the phenotype" relative to the risk for arthropathy and need for joint replacement "suggests to me that the gene itself is not involved. It suggests to me that you need more than just the gene" to boost the risk for arthropathy and joint failure, noted Dr. Johan Askling.
Arthropathy is a classic phenotypic feature of patients with hereditary hemochromatosis, a genetic disease in people who carry two mutated copies of the hemochromatosis gene (HFE) associated with iron overload. But the nature of the relationship between the disease and arthropathies remains poorly understood. The new finding that increased arthropathies occur only in homozygous, affected individuals suggests that the risk is linked to iron overload itself, rather than to the causative mutated genes.
Dr. Askling and his associates identified 3,531 patients with a diagnosis of hereditary hemochromatosis from Swedish national records for the period 1999-2006. The investigators also identified another 11,794 first-degree relatives of these patients. They then identified 37,369 people as matched controls for the patients from the general Swedish population and 196,628 people as matched controls for the first-degree relatives.
The researchers then tallied the incidence of consultations or hospitalizations for rheumatoid arthritis, osteoarthritis, and other arthritides in the cases, their first-degree relatives, and the controls during the study period. They calculated a relative risk for these complications in affected people and in their relatives, compared with the controls that adjusted for differences in age, sex, and residence location. The researchers also ran similar analyses for the incidence of various joint-replacement surgeries (see table).
The results showed that the patients with hereditary hemochromatosis had consistent, statistically significant increased rates of arthropathies. For example, for all arthropathies the rate was 2.4-fold higher in the patients than in the controls. But this increased rate did not exist among the first-degree relatives. For all arthropathies, their rate was just 10% higher than among the matched controls, a difference that was not significant, reported Dr. Askling, an epidemiologist at the Karolinska Institute in Stockholm.
A similar pattern existed for joint-replacement surgeries. Hip surgery, for example, was 2.9-fold more frequent among the hereditary hemochromatosis patients than among their matched controls, while among the first-degree relatives the incidence of hip-replacement surgery was 10% less common than among the matched controls, a difference that was not statistically significant.
Dr. Askling said that he had no disclosures.
LONDON – Patients with hereditary hemochromatosis have a significantly increased prevalence of various arthropathies and an elevated need for joint-replacement surgery, compared with the general population, according to findings from a study of Swedish national registry data.
The analysis also showed that first-degree relatives of people with hereditary hemochromatosis do not have an increased rate of arthropathies or need for joint replacement, even though genetic models predict that a majority of these relatives carry one copy of an autosomal recessive mutation that causes hereditary hemochromatosis.
"This dissociation between the genotype and the phenotype" relative to the risk for arthropathy and need for joint replacement "suggests to me that the gene itself is not involved. It suggests to me that you need more than just the gene" to boost the risk for arthropathy and joint failure, noted Dr. Johan Askling.
Arthropathy is a classic phenotypic feature of patients with hereditary hemochromatosis, a genetic disease in people who carry two mutated copies of the hemochromatosis gene (HFE) associated with iron overload. But the nature of the relationship between the disease and arthropathies remains poorly understood. The new finding that increased arthropathies occur only in homozygous, affected individuals suggests that the risk is linked to iron overload itself, rather than to the causative mutated genes.
Dr. Askling and his associates identified 3,531 patients with a diagnosis of hereditary hemochromatosis from Swedish national records for the period 1999-2006. The investigators also identified another 11,794 first-degree relatives of these patients. They then identified 37,369 people as matched controls for the patients from the general Swedish population and 196,628 people as matched controls for the first-degree relatives.
The researchers then tallied the incidence of consultations or hospitalizations for rheumatoid arthritis, osteoarthritis, and other arthritides in the cases, their first-degree relatives, and the controls during the study period. They calculated a relative risk for these complications in affected people and in their relatives, compared with the controls that adjusted for differences in age, sex, and residence location. The researchers also ran similar analyses for the incidence of various joint-replacement surgeries (see table).
The results showed that the patients with hereditary hemochromatosis had consistent, statistically significant increased rates of arthropathies. For example, for all arthropathies the rate was 2.4-fold higher in the patients than in the controls. But this increased rate did not exist among the first-degree relatives. For all arthropathies, their rate was just 10% higher than among the matched controls, a difference that was not significant, reported Dr. Askling, an epidemiologist at the Karolinska Institute in Stockholm.
A similar pattern existed for joint-replacement surgeries. Hip surgery, for example, was 2.9-fold more frequent among the hereditary hemochromatosis patients than among their matched controls, while among the first-degree relatives the incidence of hip-replacement surgery was 10% less common than among the matched controls, a difference that was not statistically significant.
Dr. Askling said that he had no disclosures.
LONDON – Patients with hereditary hemochromatosis have a significantly increased prevalence of various arthropathies and an elevated need for joint-replacement surgery, compared with the general population, according to findings from a study of Swedish national registry data.
The analysis also showed that first-degree relatives of people with hereditary hemochromatosis do not have an increased rate of arthropathies or need for joint replacement, even though genetic models predict that a majority of these relatives carry one copy of an autosomal recessive mutation that causes hereditary hemochromatosis.
"This dissociation between the genotype and the phenotype" relative to the risk for arthropathy and need for joint replacement "suggests to me that the gene itself is not involved. It suggests to me that you need more than just the gene" to boost the risk for arthropathy and joint failure, noted Dr. Johan Askling.
Arthropathy is a classic phenotypic feature of patients with hereditary hemochromatosis, a genetic disease in people who carry two mutated copies of the hemochromatosis gene (HFE) associated with iron overload. But the nature of the relationship between the disease and arthropathies remains poorly understood. The new finding that increased arthropathies occur only in homozygous, affected individuals suggests that the risk is linked to iron overload itself, rather than to the causative mutated genes.
Dr. Askling and his associates identified 3,531 patients with a diagnosis of hereditary hemochromatosis from Swedish national records for the period 1999-2006. The investigators also identified another 11,794 first-degree relatives of these patients. They then identified 37,369 people as matched controls for the patients from the general Swedish population and 196,628 people as matched controls for the first-degree relatives.
The researchers then tallied the incidence of consultations or hospitalizations for rheumatoid arthritis, osteoarthritis, and other arthritides in the cases, their first-degree relatives, and the controls during the study period. They calculated a relative risk for these complications in affected people and in their relatives, compared with the controls that adjusted for differences in age, sex, and residence location. The researchers also ran similar analyses for the incidence of various joint-replacement surgeries (see table).
The results showed that the patients with hereditary hemochromatosis had consistent, statistically significant increased rates of arthropathies. For example, for all arthropathies the rate was 2.4-fold higher in the patients than in the controls. But this increased rate did not exist among the first-degree relatives. For all arthropathies, their rate was just 10% higher than among the matched controls, a difference that was not significant, reported Dr. Askling, an epidemiologist at the Karolinska Institute in Stockholm.
A similar pattern existed for joint-replacement surgeries. Hip surgery, for example, was 2.9-fold more frequent among the hereditary hemochromatosis patients than among their matched controls, while among the first-degree relatives the incidence of hip-replacement surgery was 10% less common than among the matched controls, a difference that was not statistically significant.
Dr. Askling said that he had no disclosures.
FROM THE ANNUAL EUROPEAN CONGRESS OF RHEUMATOLOGY
Major Finding: Patients with hereditary hemochromatosis had a 2.4-fold increased prevalence of arthropathies and a 2.9-fold increased rate of hip surgery, compared with matched controls. In contrast, first-degree relatives of hereditary hemochromatosis patients had no significantly different rates for arthropathy or need for joint-replacement surgery, compared with controls.
Data Source: Case-control study of records from Swedish national registries during 1999-2006, with 3,531 patients diagnosed with hereditary hemochromatosis and 37,369 matched controls, and 11,794 first-degree relatives of the patients and 196,628 matched controls.
Disclosures: Dr. Askling said that he had no disclosures.
Tocilizumab Continues to Benefit sJIA Patients Over Time
LONDON – Children with systemic juvenile idiopathic arthritis continued to improve on treatment with the interleukin-6 inhibitor tocilizumab as their time on the drug extended out to 1 year, in follow-up of the open-label phase of the drug’s pivotal trial for this disease.
During continued tocilizumab treatment, the percent of systemic juvenile idiopathic arthritis (sJIA) patients who had an American College of Rheumatology (ACR) 90 response and no fever rose from 37% of the treated group after the end of the 12-week randomized trial, to about 55% after an additional 40 weeks of open-label treatment. There was no active joint disease in 49 of the 99 patients (49%) treated for 52 weeks; the children appeared to be in full remission, Dr. Fabrizio De Benedetti said at the meeting. In addition, 52 of the patients treated for 52 weeks fully withdrew from treatment with oral corticosteroids. At their entry onto tocilizumab treatment, their average corticosteroid dosage was 0.30 mg/kg per day.
Over 52 weeks, tocilizumab treatment also had an "acceptable" safety profile. Thirteen patients had a serious adverse event, and 6 had an adverse event leading to withdrawal from treatment. "There was no increase in the rate of serious adverse events between weeks 12 and 52. It is reassuring that there was no accumulation of safety issues with time. But it’s still only 1 year, so we still need more time" to fully assess safety, said Dr. De Benedetti, who is director of the division of rheumatology at Ospedale Pediatrico Bambino Gesù in Rome and lead investigator for the TENDER trial and extension phase.
Based on the results from the 12-week randomized phase III trial, Roche – the company that developed and markets tocilizumab (Actemra) – in April received approval from the Food and Drug Administration for an expanded indication for tocilizumab to treat sJIA. Tocilizumab received FDA approval last year for treatment of rheumatoid arthritis.
Tocilizumab "is very effective; it’s the best drug we have for sJIA. But the experience we have using it is still short" Dr. Patricia Woo, a collaborator on the TENDER trial, said in an interview. "We have 1-year experience, compared with [potentially] using it for many years" to treat children with sJIA. The next phase of the TENDER protocol is to attempt gradually to wean off the drug those children who achieve complete remission on tocilizumab for 6 months to see if they can remain in remission without ongoing treatment.
"We hope that patients will stay in remission. If we inhibit a mediator of inflammation, interleukin-6, you may give the system a chance to reset and end up with complete and durable remission," Dr. De Benedetti said in an interview.
The continued improvement that the sJIA patients showed as their duration on tocilizumab extended from 12 to 52 weeks didn’t surprise either Dr. Woo or Dr. De Benedetti.
"It takes time for these patients to get better," said Dr. Woo, emeritus professor of rheumatology at University College, London.
But the two differed in their current approach to starting tocilizumab treatment in children with sJIA, now that the drug is on the market and has a sJIA indication in both the United States and in Europe. Dr. Woo recommended a trial of methotrexate treatment first, for 2-3 months, and then a move to tocilizumab if patients don’t respond. In contrast, Dr. De Benedetti sees tocilizumab as a reasonable first-line agent.
Methotrexate has not shown efficacy in sJIA. Some patients may respond, but there is no reason to force people to use methotrexate before anything else," he said. However, another new treatment approach that warrants investigation for treating sJIA is the IL-1 inhibitors, such as anakinra (Kineret) and canakinumab (Ilaris), he added.
The original TENDER cohort included 112 children with an average age of 10 years who were randomized to treatment with tocilizumab or placebo for 12 weeks. Children weighing 30 kg or more received an 8 mg/kg tocilizumab infusion every 2 weeks; those weighing less than 30 kg received a 12-mg/kg dosage.
At the end of 12 weeks, 110 of the participants remained on or crossed over to tocilizumab, and 99 children completed either 52 weeks or 40 weeks (if they started in the placebo group) on the active drug. After 1 year, about 80%-90% of patients had ACR30 and ACR50 responses and no fever, roughly similar to the levels seen after 12 weeks. But the percent with ACR70 responses and no fever rose from about 65% after 12 weeks to about 80% after 1 year. The overall average oral corticosteroid dosage needed by the tocilizumab-treated patients after 1 year was 0.06 mg/kg per day, a significant drop from the average 0.30 mg/kg per day at baseline. The average number of active joints in patients at 1 year was about 3, compared with an average of about 6 active joints after 12 weeks and an average of 20 average joints in each patient at baseline.
The TENDER trial was sponsored by Roche, the company that markets tocilizumab. Dr. De Benedetti said he has been a consultant to Bristol-Myers Squibb, Hoffmann-La Roche, and Pfizer, and he has received research support from Hoffmann-La Roche. Dr. Woo said she had no disclosures.
LONDON – Children with systemic juvenile idiopathic arthritis continued to improve on treatment with the interleukin-6 inhibitor tocilizumab as their time on the drug extended out to 1 year, in follow-up of the open-label phase of the drug’s pivotal trial for this disease.
During continued tocilizumab treatment, the percent of systemic juvenile idiopathic arthritis (sJIA) patients who had an American College of Rheumatology (ACR) 90 response and no fever rose from 37% of the treated group after the end of the 12-week randomized trial, to about 55% after an additional 40 weeks of open-label treatment. There was no active joint disease in 49 of the 99 patients (49%) treated for 52 weeks; the children appeared to be in full remission, Dr. Fabrizio De Benedetti said at the meeting. In addition, 52 of the patients treated for 52 weeks fully withdrew from treatment with oral corticosteroids. At their entry onto tocilizumab treatment, their average corticosteroid dosage was 0.30 mg/kg per day.
Over 52 weeks, tocilizumab treatment also had an "acceptable" safety profile. Thirteen patients had a serious adverse event, and 6 had an adverse event leading to withdrawal from treatment. "There was no increase in the rate of serious adverse events between weeks 12 and 52. It is reassuring that there was no accumulation of safety issues with time. But it’s still only 1 year, so we still need more time" to fully assess safety, said Dr. De Benedetti, who is director of the division of rheumatology at Ospedale Pediatrico Bambino Gesù in Rome and lead investigator for the TENDER trial and extension phase.
Based on the results from the 12-week randomized phase III trial, Roche – the company that developed and markets tocilizumab (Actemra) – in April received approval from the Food and Drug Administration for an expanded indication for tocilizumab to treat sJIA. Tocilizumab received FDA approval last year for treatment of rheumatoid arthritis.
Tocilizumab "is very effective; it’s the best drug we have for sJIA. But the experience we have using it is still short" Dr. Patricia Woo, a collaborator on the TENDER trial, said in an interview. "We have 1-year experience, compared with [potentially] using it for many years" to treat children with sJIA. The next phase of the TENDER protocol is to attempt gradually to wean off the drug those children who achieve complete remission on tocilizumab for 6 months to see if they can remain in remission without ongoing treatment.
"We hope that patients will stay in remission. If we inhibit a mediator of inflammation, interleukin-6, you may give the system a chance to reset and end up with complete and durable remission," Dr. De Benedetti said in an interview.
The continued improvement that the sJIA patients showed as their duration on tocilizumab extended from 12 to 52 weeks didn’t surprise either Dr. Woo or Dr. De Benedetti.
"It takes time for these patients to get better," said Dr. Woo, emeritus professor of rheumatology at University College, London.
But the two differed in their current approach to starting tocilizumab treatment in children with sJIA, now that the drug is on the market and has a sJIA indication in both the United States and in Europe. Dr. Woo recommended a trial of methotrexate treatment first, for 2-3 months, and then a move to tocilizumab if patients don’t respond. In contrast, Dr. De Benedetti sees tocilizumab as a reasonable first-line agent.
Methotrexate has not shown efficacy in sJIA. Some patients may respond, but there is no reason to force people to use methotrexate before anything else," he said. However, another new treatment approach that warrants investigation for treating sJIA is the IL-1 inhibitors, such as anakinra (Kineret) and canakinumab (Ilaris), he added.
The original TENDER cohort included 112 children with an average age of 10 years who were randomized to treatment with tocilizumab or placebo for 12 weeks. Children weighing 30 kg or more received an 8 mg/kg tocilizumab infusion every 2 weeks; those weighing less than 30 kg received a 12-mg/kg dosage.
At the end of 12 weeks, 110 of the participants remained on or crossed over to tocilizumab, and 99 children completed either 52 weeks or 40 weeks (if they started in the placebo group) on the active drug. After 1 year, about 80%-90% of patients had ACR30 and ACR50 responses and no fever, roughly similar to the levels seen after 12 weeks. But the percent with ACR70 responses and no fever rose from about 65% after 12 weeks to about 80% after 1 year. The overall average oral corticosteroid dosage needed by the tocilizumab-treated patients after 1 year was 0.06 mg/kg per day, a significant drop from the average 0.30 mg/kg per day at baseline. The average number of active joints in patients at 1 year was about 3, compared with an average of about 6 active joints after 12 weeks and an average of 20 average joints in each patient at baseline.
The TENDER trial was sponsored by Roche, the company that markets tocilizumab. Dr. De Benedetti said he has been a consultant to Bristol-Myers Squibb, Hoffmann-La Roche, and Pfizer, and he has received research support from Hoffmann-La Roche. Dr. Woo said she had no disclosures.
LONDON – Children with systemic juvenile idiopathic arthritis continued to improve on treatment with the interleukin-6 inhibitor tocilizumab as their time on the drug extended out to 1 year, in follow-up of the open-label phase of the drug’s pivotal trial for this disease.
During continued tocilizumab treatment, the percent of systemic juvenile idiopathic arthritis (sJIA) patients who had an American College of Rheumatology (ACR) 90 response and no fever rose from 37% of the treated group after the end of the 12-week randomized trial, to about 55% after an additional 40 weeks of open-label treatment. There was no active joint disease in 49 of the 99 patients (49%) treated for 52 weeks; the children appeared to be in full remission, Dr. Fabrizio De Benedetti said at the meeting. In addition, 52 of the patients treated for 52 weeks fully withdrew from treatment with oral corticosteroids. At their entry onto tocilizumab treatment, their average corticosteroid dosage was 0.30 mg/kg per day.
Over 52 weeks, tocilizumab treatment also had an "acceptable" safety profile. Thirteen patients had a serious adverse event, and 6 had an adverse event leading to withdrawal from treatment. "There was no increase in the rate of serious adverse events between weeks 12 and 52. It is reassuring that there was no accumulation of safety issues with time. But it’s still only 1 year, so we still need more time" to fully assess safety, said Dr. De Benedetti, who is director of the division of rheumatology at Ospedale Pediatrico Bambino Gesù in Rome and lead investigator for the TENDER trial and extension phase.
Based on the results from the 12-week randomized phase III trial, Roche – the company that developed and markets tocilizumab (Actemra) – in April received approval from the Food and Drug Administration for an expanded indication for tocilizumab to treat sJIA. Tocilizumab received FDA approval last year for treatment of rheumatoid arthritis.
Tocilizumab "is very effective; it’s the best drug we have for sJIA. But the experience we have using it is still short" Dr. Patricia Woo, a collaborator on the TENDER trial, said in an interview. "We have 1-year experience, compared with [potentially] using it for many years" to treat children with sJIA. The next phase of the TENDER protocol is to attempt gradually to wean off the drug those children who achieve complete remission on tocilizumab for 6 months to see if they can remain in remission without ongoing treatment.
"We hope that patients will stay in remission. If we inhibit a mediator of inflammation, interleukin-6, you may give the system a chance to reset and end up with complete and durable remission," Dr. De Benedetti said in an interview.
The continued improvement that the sJIA patients showed as their duration on tocilizumab extended from 12 to 52 weeks didn’t surprise either Dr. Woo or Dr. De Benedetti.
"It takes time for these patients to get better," said Dr. Woo, emeritus professor of rheumatology at University College, London.
But the two differed in their current approach to starting tocilizumab treatment in children with sJIA, now that the drug is on the market and has a sJIA indication in both the United States and in Europe. Dr. Woo recommended a trial of methotrexate treatment first, for 2-3 months, and then a move to tocilizumab if patients don’t respond. In contrast, Dr. De Benedetti sees tocilizumab as a reasonable first-line agent.
Methotrexate has not shown efficacy in sJIA. Some patients may respond, but there is no reason to force people to use methotrexate before anything else," he said. However, another new treatment approach that warrants investigation for treating sJIA is the IL-1 inhibitors, such as anakinra (Kineret) and canakinumab (Ilaris), he added.
The original TENDER cohort included 112 children with an average age of 10 years who were randomized to treatment with tocilizumab or placebo for 12 weeks. Children weighing 30 kg or more received an 8 mg/kg tocilizumab infusion every 2 weeks; those weighing less than 30 kg received a 12-mg/kg dosage.
At the end of 12 weeks, 110 of the participants remained on or crossed over to tocilizumab, and 99 children completed either 52 weeks or 40 weeks (if they started in the placebo group) on the active drug. After 1 year, about 80%-90% of patients had ACR30 and ACR50 responses and no fever, roughly similar to the levels seen after 12 weeks. But the percent with ACR70 responses and no fever rose from about 65% after 12 weeks to about 80% after 1 year. The overall average oral corticosteroid dosage needed by the tocilizumab-treated patients after 1 year was 0.06 mg/kg per day, a significant drop from the average 0.30 mg/kg per day at baseline. The average number of active joints in patients at 1 year was about 3, compared with an average of about 6 active joints after 12 weeks and an average of 20 average joints in each patient at baseline.
The TENDER trial was sponsored by Roche, the company that markets tocilizumab. Dr. De Benedetti said he has been a consultant to Bristol-Myers Squibb, Hoffmann-La Roche, and Pfizer, and he has received research support from Hoffmann-La Roche. Dr. Woo said she had no disclosures.
FROM THE ANNUAL EUROPEAN CONGRESS OF RHEUMATOLOGY
Major Finding: Treatment with the interleukin-6 blocker tocilizumab led to ongoing improvements in 99 children with systemic juvenile idiopathic arthritis; 49% had no active joints, 53% required no treatment with an oral corticosteroid, and about 55% had no fever and an ACR90 response.
Data Source: Forty-week, open-label extension of the original 12-week TENDER trial.
Disclosures: The TENDER trial was sponsored by Roche, the company that markets tocilizumab. Dr. De Benedetti said he has been a consultant to Bristol-Myers Squibb, Hoffmann-La Roche, and Pfizer, and he has received research support from Hoffmann-La Roche. Dr. Woo said she had no disclosures.
Fulranumab Shows Efficacy for Osteoarthritis Pain
LONDON – An investigational nerve growth factor inhibitor, fulranumab, showed promising efficacy and safety as a pain reliever for patients with hip or knee osteoarthritis in 12-week results from a phase II study of 466 patients.
Further study of fulranumab in osteoarthritis had been on hold. The Food and Drug Administration issued a moratorium last December that halted clinical testing of fulranumab and most other investigational agents in the anti–nerve growth factor class, following reports that some of these drugs appeared to trigger episodes of rapid progression of hip or knee osteoarthritis (OA) that led to joint replacement and possible osteonecrosis. The FDA lifted that moratorium on research with fulranumab in cancer pain this month. The moratorium on research involving OA pain remains in place, according to investigators.
Whether or not osteoarthritis progressed rapidly in any patient treated with fulranumab remains unknown. "Cases of joint replacement reported during the entire trial are under investigation, and will be reported in a future publication," Dr. John Thipphawong said at the annual European Congress of Rheumatology.
The safety data Dr. Thipphawong presented for 12 weeks of treatment showed a well-tolerated profile, compared with placebo. Specifically, serious adverse events occurred in 1% of patients treated with fulranumab, compared with 2% of those on placebo. Adverse events led to discontinuation of the assigned drug in 2% of fulranumab recipients and 1% of those on placebo. Adverse events that occurred more often in fulranumab-treated patients were paresthesia, with a 6%-10% rate in the higher fulranumab dosage subgroups, compared with a 3% rate for patients on placebo, and a hypoesthesia rate of 5%-6% in the higher dosage fulranumab subgroups, compared with a 1% rate with placebo. The fulranumab-treated patients also had no significant changes in laboratory values, ECG, or vital signs at 12 weeks after treatment began.
The study enrolled patients with documented hip or knee osteoarthritis who met the diagnostic criteria of the American College of Rheumatology and showed radiographic evidence of the disease, with a Kellgren-Lawrence grade of 2 or greater. All patients also reported moderate to severe pain, with a painscore of at least 5 on a 0-10 numerical rating scale despite treatment with an opioid, a nonsteroidal anti-inflammatory drug, or both.
The study randomized patients to receive fulranumab or placebo once every 4 or 8 weeks as a subcutaneous injection in addition to standard pain medications. The protocol tested five different fulranumab dosages: 1 mg every 4 weeks, 3 mg every 4 weeks, 3 mg every 8 weeks, 6 mg every 8 weeks, or 10 mg every 8 weeks. Fulranumab is a fully human, recombinant monoclonal antibody that neutralizes the biological actions of human nerve growth factor. About 78 patients entered each of the five active-treatment arms as well as a placebo arm. The study’s primary efficacy end point was the change in average pain score from baseline to the end of week 12 of the study.
The patients’ average age was 61 years, 58% were women, and two-thirds were white. Their average body mass index was 32 kg/m2, and 60% weighed at least 85 kg. Knee OA predominated as the affected joint, in 77% of patients.
At 12 weeks after the start of treatment, average pain reduction with fulranumab significantly surpassed the placebo group in the 3 mg every 4 weeks, 6 mg every 8 weeks, and 10 mg every 8 weeks subgroups. In these three groups, pain scores fell by an average of 3.05, 2.64, and 2.65 points, respectively, compared with an average drop of 1.91 points in the placebo group, reported Dr. Thipphawong, who is senior director of clinical development, Johnson & Johnson Pharmaceutical Research & Development.
The study also included several secondary efficacy measures. The three highest-dosage subgroups, as well as the 3 mg every 8 weeks subgroup, showed statistically significant declines, compared with placebo after 12 weeks in the average levels of the Western Ontario and McMaster University Osteoarthritis Index (WOMAC) subscales for pain and global function. For the WOMAC subscales of physical function and stiffness, all five fulranumab dosage subgroups showed significant reductions, compared with placebo.
On the Brief Pain Inventory-Short Form, patients in the 3 mg every 4 weeks and 10 mg every 8 weeks subgroups had significant average reductions, compared with the placebo group for the subscales of pain intensity and pain interference with activities. The three highest-dosage subgroups also produced average drops in patient global assessment of disease status that were statistically significant, compared with the placebo group’s average.
In a separate poster at the meeting, Dr. Thipphawong and his associates also reported that several of the fulranumab subgroups showed statistically significant average improvements, with placebo in several subscale measures on the Short From-36, specifically bodily pain, vitality, and physical component. The four highest-dosage subgroups also had significant average improvements in pain interference with sleep, compared with placebo, and all five fulranumab dosage subgroups had significant average improvements in sleep adequacy, compared with the placebo group.
Dr. Thipphawong and several of his associates are employees of Johnson & Johnson, the company developing fulranumab.
LONDON – An investigational nerve growth factor inhibitor, fulranumab, showed promising efficacy and safety as a pain reliever for patients with hip or knee osteoarthritis in 12-week results from a phase II study of 466 patients.
Further study of fulranumab in osteoarthritis had been on hold. The Food and Drug Administration issued a moratorium last December that halted clinical testing of fulranumab and most other investigational agents in the anti–nerve growth factor class, following reports that some of these drugs appeared to trigger episodes of rapid progression of hip or knee osteoarthritis (OA) that led to joint replacement and possible osteonecrosis. The FDA lifted that moratorium on research with fulranumab in cancer pain this month. The moratorium on research involving OA pain remains in place, according to investigators.
Whether or not osteoarthritis progressed rapidly in any patient treated with fulranumab remains unknown. "Cases of joint replacement reported during the entire trial are under investigation, and will be reported in a future publication," Dr. John Thipphawong said at the annual European Congress of Rheumatology.
The safety data Dr. Thipphawong presented for 12 weeks of treatment showed a well-tolerated profile, compared with placebo. Specifically, serious adverse events occurred in 1% of patients treated with fulranumab, compared with 2% of those on placebo. Adverse events led to discontinuation of the assigned drug in 2% of fulranumab recipients and 1% of those on placebo. Adverse events that occurred more often in fulranumab-treated patients were paresthesia, with a 6%-10% rate in the higher fulranumab dosage subgroups, compared with a 3% rate for patients on placebo, and a hypoesthesia rate of 5%-6% in the higher dosage fulranumab subgroups, compared with a 1% rate with placebo. The fulranumab-treated patients also had no significant changes in laboratory values, ECG, or vital signs at 12 weeks after treatment began.
The study enrolled patients with documented hip or knee osteoarthritis who met the diagnostic criteria of the American College of Rheumatology and showed radiographic evidence of the disease, with a Kellgren-Lawrence grade of 2 or greater. All patients also reported moderate to severe pain, with a painscore of at least 5 on a 0-10 numerical rating scale despite treatment with an opioid, a nonsteroidal anti-inflammatory drug, or both.
The study randomized patients to receive fulranumab or placebo once every 4 or 8 weeks as a subcutaneous injection in addition to standard pain medications. The protocol tested five different fulranumab dosages: 1 mg every 4 weeks, 3 mg every 4 weeks, 3 mg every 8 weeks, 6 mg every 8 weeks, or 10 mg every 8 weeks. Fulranumab is a fully human, recombinant monoclonal antibody that neutralizes the biological actions of human nerve growth factor. About 78 patients entered each of the five active-treatment arms as well as a placebo arm. The study’s primary efficacy end point was the change in average pain score from baseline to the end of week 12 of the study.
The patients’ average age was 61 years, 58% were women, and two-thirds were white. Their average body mass index was 32 kg/m2, and 60% weighed at least 85 kg. Knee OA predominated as the affected joint, in 77% of patients.
At 12 weeks after the start of treatment, average pain reduction with fulranumab significantly surpassed the placebo group in the 3 mg every 4 weeks, 6 mg every 8 weeks, and 10 mg every 8 weeks subgroups. In these three groups, pain scores fell by an average of 3.05, 2.64, and 2.65 points, respectively, compared with an average drop of 1.91 points in the placebo group, reported Dr. Thipphawong, who is senior director of clinical development, Johnson & Johnson Pharmaceutical Research & Development.
The study also included several secondary efficacy measures. The three highest-dosage subgroups, as well as the 3 mg every 8 weeks subgroup, showed statistically significant declines, compared with placebo after 12 weeks in the average levels of the Western Ontario and McMaster University Osteoarthritis Index (WOMAC) subscales for pain and global function. For the WOMAC subscales of physical function and stiffness, all five fulranumab dosage subgroups showed significant reductions, compared with placebo.
On the Brief Pain Inventory-Short Form, patients in the 3 mg every 4 weeks and 10 mg every 8 weeks subgroups had significant average reductions, compared with the placebo group for the subscales of pain intensity and pain interference with activities. The three highest-dosage subgroups also produced average drops in patient global assessment of disease status that were statistically significant, compared with the placebo group’s average.
In a separate poster at the meeting, Dr. Thipphawong and his associates also reported that several of the fulranumab subgroups showed statistically significant average improvements, with placebo in several subscale measures on the Short From-36, specifically bodily pain, vitality, and physical component. The four highest-dosage subgroups also had significant average improvements in pain interference with sleep, compared with placebo, and all five fulranumab dosage subgroups had significant average improvements in sleep adequacy, compared with the placebo group.
Dr. Thipphawong and several of his associates are employees of Johnson & Johnson, the company developing fulranumab.
LONDON – An investigational nerve growth factor inhibitor, fulranumab, showed promising efficacy and safety as a pain reliever for patients with hip or knee osteoarthritis in 12-week results from a phase II study of 466 patients.
Further study of fulranumab in osteoarthritis had been on hold. The Food and Drug Administration issued a moratorium last December that halted clinical testing of fulranumab and most other investigational agents in the anti–nerve growth factor class, following reports that some of these drugs appeared to trigger episodes of rapid progression of hip or knee osteoarthritis (OA) that led to joint replacement and possible osteonecrosis. The FDA lifted that moratorium on research with fulranumab in cancer pain this month. The moratorium on research involving OA pain remains in place, according to investigators.
Whether or not osteoarthritis progressed rapidly in any patient treated with fulranumab remains unknown. "Cases of joint replacement reported during the entire trial are under investigation, and will be reported in a future publication," Dr. John Thipphawong said at the annual European Congress of Rheumatology.
The safety data Dr. Thipphawong presented for 12 weeks of treatment showed a well-tolerated profile, compared with placebo. Specifically, serious adverse events occurred in 1% of patients treated with fulranumab, compared with 2% of those on placebo. Adverse events led to discontinuation of the assigned drug in 2% of fulranumab recipients and 1% of those on placebo. Adverse events that occurred more often in fulranumab-treated patients were paresthesia, with a 6%-10% rate in the higher fulranumab dosage subgroups, compared with a 3% rate for patients on placebo, and a hypoesthesia rate of 5%-6% in the higher dosage fulranumab subgroups, compared with a 1% rate with placebo. The fulranumab-treated patients also had no significant changes in laboratory values, ECG, or vital signs at 12 weeks after treatment began.
The study enrolled patients with documented hip or knee osteoarthritis who met the diagnostic criteria of the American College of Rheumatology and showed radiographic evidence of the disease, with a Kellgren-Lawrence grade of 2 or greater. All patients also reported moderate to severe pain, with a painscore of at least 5 on a 0-10 numerical rating scale despite treatment with an opioid, a nonsteroidal anti-inflammatory drug, or both.
The study randomized patients to receive fulranumab or placebo once every 4 or 8 weeks as a subcutaneous injection in addition to standard pain medications. The protocol tested five different fulranumab dosages: 1 mg every 4 weeks, 3 mg every 4 weeks, 3 mg every 8 weeks, 6 mg every 8 weeks, or 10 mg every 8 weeks. Fulranumab is a fully human, recombinant monoclonal antibody that neutralizes the biological actions of human nerve growth factor. About 78 patients entered each of the five active-treatment arms as well as a placebo arm. The study’s primary efficacy end point was the change in average pain score from baseline to the end of week 12 of the study.
The patients’ average age was 61 years, 58% were women, and two-thirds were white. Their average body mass index was 32 kg/m2, and 60% weighed at least 85 kg. Knee OA predominated as the affected joint, in 77% of patients.
At 12 weeks after the start of treatment, average pain reduction with fulranumab significantly surpassed the placebo group in the 3 mg every 4 weeks, 6 mg every 8 weeks, and 10 mg every 8 weeks subgroups. In these three groups, pain scores fell by an average of 3.05, 2.64, and 2.65 points, respectively, compared with an average drop of 1.91 points in the placebo group, reported Dr. Thipphawong, who is senior director of clinical development, Johnson & Johnson Pharmaceutical Research & Development.
The study also included several secondary efficacy measures. The three highest-dosage subgroups, as well as the 3 mg every 8 weeks subgroup, showed statistically significant declines, compared with placebo after 12 weeks in the average levels of the Western Ontario and McMaster University Osteoarthritis Index (WOMAC) subscales for pain and global function. For the WOMAC subscales of physical function and stiffness, all five fulranumab dosage subgroups showed significant reductions, compared with placebo.
On the Brief Pain Inventory-Short Form, patients in the 3 mg every 4 weeks and 10 mg every 8 weeks subgroups had significant average reductions, compared with the placebo group for the subscales of pain intensity and pain interference with activities. The three highest-dosage subgroups also produced average drops in patient global assessment of disease status that were statistically significant, compared with the placebo group’s average.
In a separate poster at the meeting, Dr. Thipphawong and his associates also reported that several of the fulranumab subgroups showed statistically significant average improvements, with placebo in several subscale measures on the Short From-36, specifically bodily pain, vitality, and physical component. The four highest-dosage subgroups also had significant average improvements in pain interference with sleep, compared with placebo, and all five fulranumab dosage subgroups had significant average improvements in sleep adequacy, compared with the placebo group.
Dr. Thipphawong and several of his associates are employees of Johnson & Johnson, the company developing fulranumab.
FROM THE ANNUAL EUROPEAN CONGRESS OF RHEUMATOLOGY
Major Finding: Treatment with several different dosages of fulranumab led to statistically significant improvements in a number of efficacy measures and was well tolerated. The primary efficacy end point of change in average pain intensity at 12 weeks from the start of treatment showed significant drops, compared with the placebo group for the three largest dosages of fulranumab tested.
Data Source: Phase II randomized, placebo-controlled trial that assessed the efficacy and safety of five dosages of fulranumab after 12 weeks of treatment in patients with moderate to severely painful osteoarthritis of the hip or knee.
Disclosures: Dr. Thipphawong and several of his associates are employees of Johnson & Johnson, the company developing fulranumab.
Fulranumab Shows Efficacy for Osteoarthritis Pain
LONDON – An investigational nerve growth factor inhibitor, fulranumab, showed promising efficacy and safety as a pain reliever for patients with hip or knee osteoarthritis in 12-week results from a phase II study of 466 patients.
Further study of fulranumab in osteoarthritis had been on hold. The Food and Drug Administration issued a moratorium last December that halted clinical testing of fulranumab and most other investigational agents in the anti–nerve growth factor class, following reports that some of these drugs appeared to trigger episodes of rapid progression of hip or knee osteoarthritis (OA) that led to joint replacement and possible osteonecrosis. The FDA lifted that moratorium on research with fulranumab in cancer pain this month. The moratorium on research involving OA pain remains in place, according to investigators.
Whether or not osteoarthritis progressed rapidly in any patient treated with fulranumab remains unknown. "Cases of joint replacement reported during the entire trial are under investigation, and will be reported in a future publication," Dr. John Thipphawong said at the annual European Congress of Rheumatology.
The safety data Dr. Thipphawong presented for 12 weeks of treatment showed a well-tolerated profile, compared with placebo. Specifically, serious adverse events occurred in 1% of patients treated with fulranumab, compared with 2% of those on placebo. Adverse events led to discontinuation of the assigned drug in 2% of fulranumab recipients and 1% of those on placebo. Adverse events that occurred more often in fulranumab-treated patients were paresthesia, with a 6%-10% rate in the higher fulranumab dosage subgroups, compared with a 3% rate for patients on placebo, and a hypoesthesia rate of 5%-6% in the higher dosage fulranumab subgroups, compared with a 1% rate with placebo. The fulranumab-treated patients also had no significant changes in laboratory values, ECG, or vital signs at 12 weeks after treatment began.
The study enrolled patients with documented hip or knee osteoarthritis who met the diagnostic criteria of the American College of Rheumatology and showed radiographic evidence of the disease, with a Kellgren-Lawrence grade of 2 or greater. All patients also reported moderate to severe pain, with a painscore of at least 5 on a 0-10 numerical rating scale despite treatment with an opioid, a nonsteroidal anti-inflammatory drug, or both.
The study randomized patients to receive fulranumab or placebo once every 4 or 8 weeks as a subcutaneous injection in addition to standard pain medications. The protocol tested five different fulranumab dosages: 1 mg every 4 weeks, 3 mg every 4 weeks, 3 mg every 8 weeks, 6 mg every 8 weeks, or 10 mg every 8 weeks. Fulranumab is a fully human, recombinant monoclonal antibody that neutralizes the biological actions of human nerve growth factor. About 78 patients entered each of the five active-treatment arms as well as a placebo arm. The study’s primary efficacy end point was the change in average pain score from baseline to the end of week 12 of the study.
The patients’ average age was 61 years, 58% were women, and two-thirds were white. Their average body mass index was 32 kg/m2, and 60% weighed at least 85 kg. Knee OA predominated as the affected joint, in 77% of patients.
At 12 weeks after the start of treatment, average pain reduction with fulranumab significantly surpassed the placebo group in the 3 mg every 4 weeks, 6 mg every 8 weeks, and 10 mg every 8 weeks subgroups. In these three groups, pain scores fell by an average of 3.05, 2.64, and 2.65 points, respectively, compared with an average drop of 1.91 points in the placebo group, reported Dr. Thipphawong, who is senior director of clinical development, Johnson & Johnson Pharmaceutical Research & Development.
The study also included several secondary efficacy measures. The three highest-dosage subgroups, as well as the 3 mg every 8 weeks subgroup, showed statistically significant declines, compared with placebo after 12 weeks in the average levels of the Western Ontario and McMaster University Osteoarthritis Index (WOMAC) subscales for pain and global function. For the WOMAC subscales of physical function and stiffness, all five fulranumab dosage subgroups showed significant reductions, compared with placebo.
On the Brief Pain Inventory-Short Form, patients in the 3 mg every 4 weeks and 10 mg every 8 weeks subgroups had significant average reductions, compared with the placebo group for the subscales of pain intensity and pain interference with activities. The three highest-dosage subgroups also produced average drops in patient global assessment of disease status that were statistically significant, compared with the placebo group’s average.
In a separate poster at the meeting, Dr. Thipphawong and his associates also reported that several of the fulranumab subgroups showed statistically significant average improvements, with placebo in several subscale measures on the Short From-36, specifically bodily pain, vitality, and physical component. The four highest-dosage subgroups also had significant average improvements in pain interference with sleep, compared with placebo, and all five fulranumab dosage subgroups had significant average improvements in sleep adequacy, compared with the placebo group.
Dr. Thipphawong and several of his associates are employees of Johnson & Johnson, the company developing fulranumab.
LONDON – An investigational nerve growth factor inhibitor, fulranumab, showed promising efficacy and safety as a pain reliever for patients with hip or knee osteoarthritis in 12-week results from a phase II study of 466 patients.
Further study of fulranumab in osteoarthritis had been on hold. The Food and Drug Administration issued a moratorium last December that halted clinical testing of fulranumab and most other investigational agents in the anti–nerve growth factor class, following reports that some of these drugs appeared to trigger episodes of rapid progression of hip or knee osteoarthritis (OA) that led to joint replacement and possible osteonecrosis. The FDA lifted that moratorium on research with fulranumab in cancer pain this month. The moratorium on research involving OA pain remains in place, according to investigators.
Whether or not osteoarthritis progressed rapidly in any patient treated with fulranumab remains unknown. "Cases of joint replacement reported during the entire trial are under investigation, and will be reported in a future publication," Dr. John Thipphawong said at the annual European Congress of Rheumatology.
The safety data Dr. Thipphawong presented for 12 weeks of treatment showed a well-tolerated profile, compared with placebo. Specifically, serious adverse events occurred in 1% of patients treated with fulranumab, compared with 2% of those on placebo. Adverse events led to discontinuation of the assigned drug in 2% of fulranumab recipients and 1% of those on placebo. Adverse events that occurred more often in fulranumab-treated patients were paresthesia, with a 6%-10% rate in the higher fulranumab dosage subgroups, compared with a 3% rate for patients on placebo, and a hypoesthesia rate of 5%-6% in the higher dosage fulranumab subgroups, compared with a 1% rate with placebo. The fulranumab-treated patients also had no significant changes in laboratory values, ECG, or vital signs at 12 weeks after treatment began.
The study enrolled patients with documented hip or knee osteoarthritis who met the diagnostic criteria of the American College of Rheumatology and showed radiographic evidence of the disease, with a Kellgren-Lawrence grade of 2 or greater. All patients also reported moderate to severe pain, with a painscore of at least 5 on a 0-10 numerical rating scale despite treatment with an opioid, a nonsteroidal anti-inflammatory drug, or both.
The study randomized patients to receive fulranumab or placebo once every 4 or 8 weeks as a subcutaneous injection in addition to standard pain medications. The protocol tested five different fulranumab dosages: 1 mg every 4 weeks, 3 mg every 4 weeks, 3 mg every 8 weeks, 6 mg every 8 weeks, or 10 mg every 8 weeks. Fulranumab is a fully human, recombinant monoclonal antibody that neutralizes the biological actions of human nerve growth factor. About 78 patients entered each of the five active-treatment arms as well as a placebo arm. The study’s primary efficacy end point was the change in average pain score from baseline to the end of week 12 of the study.
The patients’ average age was 61 years, 58% were women, and two-thirds were white. Their average body mass index was 32 kg/m2, and 60% weighed at least 85 kg. Knee OA predominated as the affected joint, in 77% of patients.
At 12 weeks after the start of treatment, average pain reduction with fulranumab significantly surpassed the placebo group in the 3 mg every 4 weeks, 6 mg every 8 weeks, and 10 mg every 8 weeks subgroups. In these three groups, pain scores fell by an average of 3.05, 2.64, and 2.65 points, respectively, compared with an average drop of 1.91 points in the placebo group, reported Dr. Thipphawong, who is senior director of clinical development, Johnson & Johnson Pharmaceutical Research & Development.
The study also included several secondary efficacy measures. The three highest-dosage subgroups, as well as the 3 mg every 8 weeks subgroup, showed statistically significant declines, compared with placebo after 12 weeks in the average levels of the Western Ontario and McMaster University Osteoarthritis Index (WOMAC) subscales for pain and global function. For the WOMAC subscales of physical function and stiffness, all five fulranumab dosage subgroups showed significant reductions, compared with placebo.
On the Brief Pain Inventory-Short Form, patients in the 3 mg every 4 weeks and 10 mg every 8 weeks subgroups had significant average reductions, compared with the placebo group for the subscales of pain intensity and pain interference with activities. The three highest-dosage subgroups also produced average drops in patient global assessment of disease status that were statistically significant, compared with the placebo group’s average.
In a separate poster at the meeting, Dr. Thipphawong and his associates also reported that several of the fulranumab subgroups showed statistically significant average improvements, with placebo in several subscale measures on the Short From-36, specifically bodily pain, vitality, and physical component. The four highest-dosage subgroups also had significant average improvements in pain interference with sleep, compared with placebo, and all five fulranumab dosage subgroups had significant average improvements in sleep adequacy, compared with the placebo group.
Dr. Thipphawong and several of his associates are employees of Johnson & Johnson, the company developing fulranumab.
LONDON – An investigational nerve growth factor inhibitor, fulranumab, showed promising efficacy and safety as a pain reliever for patients with hip or knee osteoarthritis in 12-week results from a phase II study of 466 patients.
Further study of fulranumab in osteoarthritis had been on hold. The Food and Drug Administration issued a moratorium last December that halted clinical testing of fulranumab and most other investigational agents in the anti–nerve growth factor class, following reports that some of these drugs appeared to trigger episodes of rapid progression of hip or knee osteoarthritis (OA) that led to joint replacement and possible osteonecrosis. The FDA lifted that moratorium on research with fulranumab in cancer pain this month. The moratorium on research involving OA pain remains in place, according to investigators.
Whether or not osteoarthritis progressed rapidly in any patient treated with fulranumab remains unknown. "Cases of joint replacement reported during the entire trial are under investigation, and will be reported in a future publication," Dr. John Thipphawong said at the annual European Congress of Rheumatology.
The safety data Dr. Thipphawong presented for 12 weeks of treatment showed a well-tolerated profile, compared with placebo. Specifically, serious adverse events occurred in 1% of patients treated with fulranumab, compared with 2% of those on placebo. Adverse events led to discontinuation of the assigned drug in 2% of fulranumab recipients and 1% of those on placebo. Adverse events that occurred more often in fulranumab-treated patients were paresthesia, with a 6%-10% rate in the higher fulranumab dosage subgroups, compared with a 3% rate for patients on placebo, and a hypoesthesia rate of 5%-6% in the higher dosage fulranumab subgroups, compared with a 1% rate with placebo. The fulranumab-treated patients also had no significant changes in laboratory values, ECG, or vital signs at 12 weeks after treatment began.
The study enrolled patients with documented hip or knee osteoarthritis who met the diagnostic criteria of the American College of Rheumatology and showed radiographic evidence of the disease, with a Kellgren-Lawrence grade of 2 or greater. All patients also reported moderate to severe pain, with a painscore of at least 5 on a 0-10 numerical rating scale despite treatment with an opioid, a nonsteroidal anti-inflammatory drug, or both.
The study randomized patients to receive fulranumab or placebo once every 4 or 8 weeks as a subcutaneous injection in addition to standard pain medications. The protocol tested five different fulranumab dosages: 1 mg every 4 weeks, 3 mg every 4 weeks, 3 mg every 8 weeks, 6 mg every 8 weeks, or 10 mg every 8 weeks. Fulranumab is a fully human, recombinant monoclonal antibody that neutralizes the biological actions of human nerve growth factor. About 78 patients entered each of the five active-treatment arms as well as a placebo arm. The study’s primary efficacy end point was the change in average pain score from baseline to the end of week 12 of the study.
The patients’ average age was 61 years, 58% were women, and two-thirds were white. Their average body mass index was 32 kg/m2, and 60% weighed at least 85 kg. Knee OA predominated as the affected joint, in 77% of patients.
At 12 weeks after the start of treatment, average pain reduction with fulranumab significantly surpassed the placebo group in the 3 mg every 4 weeks, 6 mg every 8 weeks, and 10 mg every 8 weeks subgroups. In these three groups, pain scores fell by an average of 3.05, 2.64, and 2.65 points, respectively, compared with an average drop of 1.91 points in the placebo group, reported Dr. Thipphawong, who is senior director of clinical development, Johnson & Johnson Pharmaceutical Research & Development.
The study also included several secondary efficacy measures. The three highest-dosage subgroups, as well as the 3 mg every 8 weeks subgroup, showed statistically significant declines, compared with placebo after 12 weeks in the average levels of the Western Ontario and McMaster University Osteoarthritis Index (WOMAC) subscales for pain and global function. For the WOMAC subscales of physical function and stiffness, all five fulranumab dosage subgroups showed significant reductions, compared with placebo.
On the Brief Pain Inventory-Short Form, patients in the 3 mg every 4 weeks and 10 mg every 8 weeks subgroups had significant average reductions, compared with the placebo group for the subscales of pain intensity and pain interference with activities. The three highest-dosage subgroups also produced average drops in patient global assessment of disease status that were statistically significant, compared with the placebo group’s average.
In a separate poster at the meeting, Dr. Thipphawong and his associates also reported that several of the fulranumab subgroups showed statistically significant average improvements, with placebo in several subscale measures on the Short From-36, specifically bodily pain, vitality, and physical component. The four highest-dosage subgroups also had significant average improvements in pain interference with sleep, compared with placebo, and all five fulranumab dosage subgroups had significant average improvements in sleep adequacy, compared with the placebo group.
Dr. Thipphawong and several of his associates are employees of Johnson & Johnson, the company developing fulranumab.
FROM THE ANNUAL EUROPEAN CONGRESS OF RHEUMATOLOGY
Major Finding: Treatment with several different dosages of fulranumab led to statistically significant improvements in a number of efficacy measures and was well tolerated. The primary efficacy end point of change in average pain intensity at 12 weeks from the start of treatment showed significant drops, compared with the placebo group for the three largest dosages of fulranumab tested.
Data Source: Phase II randomized, placebo-controlled trial that assessed the efficacy and safety of five dosages of fulranumab after 12 weeks of treatment in patients with moderate to severely painful osteoarthritis of the hip or knee.
Disclosures: Dr. Thipphawong and several of his associates are employees of Johnson & Johnson, the company developing fulranumab.