User login
Mitchel is a reporter for MDedge based in the Philadelphia area. He started with the company in 1992, when it was International Medical News Group (IMNG), and has since covered a range of medical specialties. Mitchel trained as a virologist at Roswell Park Memorial Institute in Buffalo, and then worked briefly as a researcher at Boston Children's Hospital before pivoting to journalism as a AAAS Mass Media Fellow in 1980. His first reporting job was with Science Digest magazine, and from the mid-1980s to early-1990s he was a reporter with Medical World News. @mitchelzoler
Quick Statin Use After Stroke Cuts Mortality
LOS ANGELES – Starting or maintaining acute stroke patients on a statin during their initial hospitalization was linked with a dramatic improvement in 1-year survival in a retrospective review of medical records for more than 12,000 U.S. patients.
Based on the finding, Kaiser Permanente of Northern California will issue a revised order set that will recommend to physicians that they start acute stroke patients on 80-mg simvastatin as soon as possible on the first day of their hospitalization, Dr. Alexander C. Flint said at the International Stroke Conference.
"Based on results from the SPARCL [Stroke Prevention by Aggressive Reduction in Cholesterol Levels] trial, pretty much everyone in the stroke community believes that patients who have had an ischemic stroke should be treated with high-dose statin to prevent a second stroke (N. Engl. J. Med. 2006;355:549-59). In our study, the question wasn’t whether to treat, but the timing. What our results say is that you should not wait until the patient is discharged or is an outpatient, but that you should start the statin on day 1," Dr. Flint said in an interview.
The data he reported showed that stroke patients who started on a statin during their acute-phase hospitalization had a 15% absolute reduced rate of death during the first year following their stroke, compared with patients who did not start on a statin and did not receive a statin prior to their stroke (Stroke 2011;42:e-42-110). After adjustment for several possible confounding factors, including age; sex; race and ethnicity; year of stroke; and comorbidities such as hypertension and diabetes, stroke patients who started on a statin while hospitalized had a statistically significant (45%) relatively lower risk of death during the subsequent year, compared with patients who did not receive a statin.
The study involved 12,689 patients who received care from Kaiser Permanente of Northern California and had an ischemic stroke during 2000-2007. The total included 3,749 patients who were on steady statin treatment for at least 3 months before their stroke, and 8,940 patients who were not receiving a statin at all before their stroke.* Of the 3,749 patients who were on a statin before their stroke, most (3,280, or 87%) continued to receive a statin during their hospitalization. And among the 8,940 who did not receive regular statin treatment before their stroke, 3,013 (34%) began statin treatment while hospitalized.
Patients who received a statin prior to their stroke but did not continue while hospitalized had a statistically significant 15% relative reduction in their mortality during the following year, compared with patients who never received a statin.
The key element for mortality protection appeared to be treatment while hospitalized. Relative mortality reduction compared with nonstatin users was 41% among patients who were on a statin both before their stroke and while hospitalized, and 45% among those who started on a statin while hospitalized, said Dr. Flint, a neurointensivist and stroke specialist at Kaiser Redwood City (Calif.). Patients who received a statin before their stroke but discontinued the drug once hospitalized had the worst outcomes, with a mortality rate that was 2.5-fold higher than that of patients who never received a statin.
Further analysis highlighted the importance of an early start to statin treatment in hospitalized patients, and also showed a dose-response relationship. Patients who received at least 60 mg of their statin daily either before hospitalization or both before and during hospitalization had a significantly lower mortality rate, compared with patients who took less than 60 mg/day. Dr. Flint noted that about 70% of patients received lovastatin, and about 20% received simvastatin.
Regarding timing, patients who either began on a statin for the first time or restarted their treatment on their first hospitalized day had a significantly lower 1-year mortality, compared with patients who did not start or restart their statin until their third day in hospital.
Dr. Flint also reported an additional analysis that had been run to determine whether patients’ survival prognosis drove their statin treatment instead of their statin treatment’s driving their survival. To do this, he looked at patterns of care at each of the 17 Kaiser Permanente of Northern California hospitals that were involved in the study. This "grouped treatment analysis" showed that although the survival prognosis of patients who were withdrawn from prior statin treatment while hospitalized played some role in the relationship, it was unable to explain all of the survival effect, indicating that statin treatment itself during hospitalization played a significant role in subsequent survival.
The strong impact that early statin treatment during stroke hospitalization has on long-term survival probably depends on the pleiotropic effects of statins. The timing makes it less likely that the effect of statins on lipid levels can explain the observed survival benefits, Dr. Flint said.
Dr. Flint said that he had no disclosures.
* CORRECTION, 3/4/2011: An earlier version of this article stated that some study participants took statins intermittently prior to having a stroke. However, the study included only patients who were taking a statin for at least 3 months prior to the stroke or those not taking a statin at all. This version has been updated.
LOS ANGELES – Starting or maintaining acute stroke patients on a statin during their initial hospitalization was linked with a dramatic improvement in 1-year survival in a retrospective review of medical records for more than 12,000 U.S. patients.
Based on the finding, Kaiser Permanente of Northern California will issue a revised order set that will recommend to physicians that they start acute stroke patients on 80-mg simvastatin as soon as possible on the first day of their hospitalization, Dr. Alexander C. Flint said at the International Stroke Conference.
"Based on results from the SPARCL [Stroke Prevention by Aggressive Reduction in Cholesterol Levels] trial, pretty much everyone in the stroke community believes that patients who have had an ischemic stroke should be treated with high-dose statin to prevent a second stroke (N. Engl. J. Med. 2006;355:549-59). In our study, the question wasn’t whether to treat, but the timing. What our results say is that you should not wait until the patient is discharged or is an outpatient, but that you should start the statin on day 1," Dr. Flint said in an interview.
The data he reported showed that stroke patients who started on a statin during their acute-phase hospitalization had a 15% absolute reduced rate of death during the first year following their stroke, compared with patients who did not start on a statin and did not receive a statin prior to their stroke (Stroke 2011;42:e-42-110). After adjustment for several possible confounding factors, including age; sex; race and ethnicity; year of stroke; and comorbidities such as hypertension and diabetes, stroke patients who started on a statin while hospitalized had a statistically significant (45%) relatively lower risk of death during the subsequent year, compared with patients who did not receive a statin.
The study involved 12,689 patients who received care from Kaiser Permanente of Northern California and had an ischemic stroke during 2000-2007. The total included 3,749 patients who were on steady statin treatment for at least 3 months before their stroke, and 8,940 patients who were not receiving a statin at all before their stroke.* Of the 3,749 patients who were on a statin before their stroke, most (3,280, or 87%) continued to receive a statin during their hospitalization. And among the 8,940 who did not receive regular statin treatment before their stroke, 3,013 (34%) began statin treatment while hospitalized.
Patients who received a statin prior to their stroke but did not continue while hospitalized had a statistically significant 15% relative reduction in their mortality during the following year, compared with patients who never received a statin.
The key element for mortality protection appeared to be treatment while hospitalized. Relative mortality reduction compared with nonstatin users was 41% among patients who were on a statin both before their stroke and while hospitalized, and 45% among those who started on a statin while hospitalized, said Dr. Flint, a neurointensivist and stroke specialist at Kaiser Redwood City (Calif.). Patients who received a statin before their stroke but discontinued the drug once hospitalized had the worst outcomes, with a mortality rate that was 2.5-fold higher than that of patients who never received a statin.
Further analysis highlighted the importance of an early start to statin treatment in hospitalized patients, and also showed a dose-response relationship. Patients who received at least 60 mg of their statin daily either before hospitalization or both before and during hospitalization had a significantly lower mortality rate, compared with patients who took less than 60 mg/day. Dr. Flint noted that about 70% of patients received lovastatin, and about 20% received simvastatin.
Regarding timing, patients who either began on a statin for the first time or restarted their treatment on their first hospitalized day had a significantly lower 1-year mortality, compared with patients who did not start or restart their statin until their third day in hospital.
Dr. Flint also reported an additional analysis that had been run to determine whether patients’ survival prognosis drove their statin treatment instead of their statin treatment’s driving their survival. To do this, he looked at patterns of care at each of the 17 Kaiser Permanente of Northern California hospitals that were involved in the study. This "grouped treatment analysis" showed that although the survival prognosis of patients who were withdrawn from prior statin treatment while hospitalized played some role in the relationship, it was unable to explain all of the survival effect, indicating that statin treatment itself during hospitalization played a significant role in subsequent survival.
The strong impact that early statin treatment during stroke hospitalization has on long-term survival probably depends on the pleiotropic effects of statins. The timing makes it less likely that the effect of statins on lipid levels can explain the observed survival benefits, Dr. Flint said.
Dr. Flint said that he had no disclosures.
* CORRECTION, 3/4/2011: An earlier version of this article stated that some study participants took statins intermittently prior to having a stroke. However, the study included only patients who were taking a statin for at least 3 months prior to the stroke or those not taking a statin at all. This version has been updated.
LOS ANGELES – Starting or maintaining acute stroke patients on a statin during their initial hospitalization was linked with a dramatic improvement in 1-year survival in a retrospective review of medical records for more than 12,000 U.S. patients.
Based on the finding, Kaiser Permanente of Northern California will issue a revised order set that will recommend to physicians that they start acute stroke patients on 80-mg simvastatin as soon as possible on the first day of their hospitalization, Dr. Alexander C. Flint said at the International Stroke Conference.
"Based on results from the SPARCL [Stroke Prevention by Aggressive Reduction in Cholesterol Levels] trial, pretty much everyone in the stroke community believes that patients who have had an ischemic stroke should be treated with high-dose statin to prevent a second stroke (N. Engl. J. Med. 2006;355:549-59). In our study, the question wasn’t whether to treat, but the timing. What our results say is that you should not wait until the patient is discharged or is an outpatient, but that you should start the statin on day 1," Dr. Flint said in an interview.
The data he reported showed that stroke patients who started on a statin during their acute-phase hospitalization had a 15% absolute reduced rate of death during the first year following their stroke, compared with patients who did not start on a statin and did not receive a statin prior to their stroke (Stroke 2011;42:e-42-110). After adjustment for several possible confounding factors, including age; sex; race and ethnicity; year of stroke; and comorbidities such as hypertension and diabetes, stroke patients who started on a statin while hospitalized had a statistically significant (45%) relatively lower risk of death during the subsequent year, compared with patients who did not receive a statin.
The study involved 12,689 patients who received care from Kaiser Permanente of Northern California and had an ischemic stroke during 2000-2007. The total included 3,749 patients who were on steady statin treatment for at least 3 months before their stroke, and 8,940 patients who were not receiving a statin at all before their stroke.* Of the 3,749 patients who were on a statin before their stroke, most (3,280, or 87%) continued to receive a statin during their hospitalization. And among the 8,940 who did not receive regular statin treatment before their stroke, 3,013 (34%) began statin treatment while hospitalized.
Patients who received a statin prior to their stroke but did not continue while hospitalized had a statistically significant 15% relative reduction in their mortality during the following year, compared with patients who never received a statin.
The key element for mortality protection appeared to be treatment while hospitalized. Relative mortality reduction compared with nonstatin users was 41% among patients who were on a statin both before their stroke and while hospitalized, and 45% among those who started on a statin while hospitalized, said Dr. Flint, a neurointensivist and stroke specialist at Kaiser Redwood City (Calif.). Patients who received a statin before their stroke but discontinued the drug once hospitalized had the worst outcomes, with a mortality rate that was 2.5-fold higher than that of patients who never received a statin.
Further analysis highlighted the importance of an early start to statin treatment in hospitalized patients, and also showed a dose-response relationship. Patients who received at least 60 mg of their statin daily either before hospitalization or both before and during hospitalization had a significantly lower mortality rate, compared with patients who took less than 60 mg/day. Dr. Flint noted that about 70% of patients received lovastatin, and about 20% received simvastatin.
Regarding timing, patients who either began on a statin for the first time or restarted their treatment on their first hospitalized day had a significantly lower 1-year mortality, compared with patients who did not start or restart their statin until their third day in hospital.
Dr. Flint also reported an additional analysis that had been run to determine whether patients’ survival prognosis drove their statin treatment instead of their statin treatment’s driving their survival. To do this, he looked at patterns of care at each of the 17 Kaiser Permanente of Northern California hospitals that were involved in the study. This "grouped treatment analysis" showed that although the survival prognosis of patients who were withdrawn from prior statin treatment while hospitalized played some role in the relationship, it was unable to explain all of the survival effect, indicating that statin treatment itself during hospitalization played a significant role in subsequent survival.
The strong impact that early statin treatment during stroke hospitalization has on long-term survival probably depends on the pleiotropic effects of statins. The timing makes it less likely that the effect of statins on lipid levels can explain the observed survival benefits, Dr. Flint said.
Dr. Flint said that he had no disclosures.
* CORRECTION, 3/4/2011: An earlier version of this article stated that some study participants took statins intermittently prior to having a stroke. However, the study included only patients who were taking a statin for at least 3 months prior to the stroke or those not taking a statin at all. This version has been updated.
Quick Statin Use After Stroke Cuts Mortality
LOS ANGELES – Starting or maintaining acute stroke patients on a statin during their initial hospitalization was linked with a dramatic improvement in 1-year survival in a retrospective review of medical records for more than 12,000 U.S. patients.
Based on the finding, Kaiser Permanente of Northern California will issue a revised order set that will recommend to physicians that they start acute stroke patients on 80-mg simvastatin as soon as possible on the first day of their hospitalization, Dr. Alexander C. Flint said at the International Stroke Conference.
"Based on results from the SPARCL [Stroke Prevention by Aggressive Reduction in Cholesterol Levels] trial, pretty much everyone in the stroke community believes that patients who have had an ischemic stroke should be treated with high-dose statin to prevent a second stroke (N. Engl. J. Med. 2006;355:549-59). In our study, the question wasn’t whether to treat, but the timing. What our results say is that you should not wait until the patient is discharged or is an outpatient, but that you should start the statin on day 1," Dr. Flint said in an interview.
The data he reported showed that stroke patients who started on a statin during their acute-phase hospitalization had a 15% absolute reduced rate of death during the first year following their stroke, compared with patients who did not start on a statin and did not receive a statin prior to their stroke (Stroke 2011;42:e-42-110). After adjustment for several possible confounding factors, including age; sex; race and ethnicity; year of stroke; and comorbidities such as hypertension and diabetes, stroke patients who started on a statin while hospitalized had a statistically significant (45%) relatively lower risk of death during the subsequent year, compared with patients who did not receive a statin.
The study involved 12,689 patients who received care from Kaiser Permanente of Northern California and had an ischemic stroke during 2000-2007. The total included 3,749 patients who were on steady statin treatment for at least 3 months before their stroke, and 8,940 patients who were not receiving a statin at all before their stroke.* Of the 3,749 patients who were on a statin before their stroke, most (3,280, or 87%) continued to receive a statin during their hospitalization. And among the 8,940 who did not receive regular statin treatment before their stroke, 3,013 (34%) began statin treatment while hospitalized.
Patients who received a statin prior to their stroke but did not continue while hospitalized had a statistically significant 15% relative reduction in their mortality during the following year, compared with patients who never received a statin.
The key element for mortality protection appeared to be treatment while hospitalized. Relative mortality reduction compared with nonstatin users was 41% among patients who were on a statin both before their stroke and while hospitalized, and 45% among those who started on a statin while hospitalized, said Dr. Flint, a neurointensivist and stroke specialist at Kaiser Redwood City (Calif.). Patients who received a statin before their stroke but discontinued the drug once hospitalized had the worst outcomes, with a mortality rate that was 2.5-fold higher than that of patients who never received a statin.
Further analysis highlighted the importance of an early start to statin treatment in hospitalized patients, and also showed a dose-response relationship. Patients who received at least 60 mg of their statin daily either before hospitalization or both before and during hospitalization had a significantly lower mortality rate, compared with patients who took less than 60 mg/day. Dr. Flint noted that about 70% of patients received lovastatin, and about 20% received simvastatin.
Regarding timing, patients who either began on a statin for the first time or restarted their treatment on their first hospitalized day had a significantly lower 1-year mortality, compared with patients who did not start or restart their statin until their third day in hospital.
Dr. Flint also reported an additional analysis that had been run to determine whether patients’ survival prognosis drove their statin treatment instead of their statin treatment’s driving their survival. To do this, he looked at patterns of care at each of the 17 Kaiser Permanente of Northern California hospitals that were involved in the study. This "grouped treatment analysis" showed that although the survival prognosis of patients who were withdrawn from prior statin treatment while hospitalized played some role in the relationship, it was unable to explain all of the survival effect, indicating that statin treatment itself during hospitalization played a significant role in subsequent survival.
The strong impact that early statin treatment during stroke hospitalization has on long-term survival probably depends on the pleiotropic effects of statins. The timing makes it less likely that the effect of statins on lipid levels can explain the observed survival benefits, Dr. Flint said.
Dr. Flint said that he had no disclosures.
* CORRECTION, 3/4/2011: An earlier version of this article stated that some study participants took statins intermittently prior to having a stroke. However, the study included only patients who were taking a statin for at least 3 months prior to the stroke or those not taking a statin at all. This version has been updated.
LOS ANGELES – Starting or maintaining acute stroke patients on a statin during their initial hospitalization was linked with a dramatic improvement in 1-year survival in a retrospective review of medical records for more than 12,000 U.S. patients.
Based on the finding, Kaiser Permanente of Northern California will issue a revised order set that will recommend to physicians that they start acute stroke patients on 80-mg simvastatin as soon as possible on the first day of their hospitalization, Dr. Alexander C. Flint said at the International Stroke Conference.
"Based on results from the SPARCL [Stroke Prevention by Aggressive Reduction in Cholesterol Levels] trial, pretty much everyone in the stroke community believes that patients who have had an ischemic stroke should be treated with high-dose statin to prevent a second stroke (N. Engl. J. Med. 2006;355:549-59). In our study, the question wasn’t whether to treat, but the timing. What our results say is that you should not wait until the patient is discharged or is an outpatient, but that you should start the statin on day 1," Dr. Flint said in an interview.
The data he reported showed that stroke patients who started on a statin during their acute-phase hospitalization had a 15% absolute reduced rate of death during the first year following their stroke, compared with patients who did not start on a statin and did not receive a statin prior to their stroke (Stroke 2011;42:e-42-110). After adjustment for several possible confounding factors, including age; sex; race and ethnicity; year of stroke; and comorbidities such as hypertension and diabetes, stroke patients who started on a statin while hospitalized had a statistically significant (45%) relatively lower risk of death during the subsequent year, compared with patients who did not receive a statin.
The study involved 12,689 patients who received care from Kaiser Permanente of Northern California and had an ischemic stroke during 2000-2007. The total included 3,749 patients who were on steady statin treatment for at least 3 months before their stroke, and 8,940 patients who were not receiving a statin at all before their stroke.* Of the 3,749 patients who were on a statin before their stroke, most (3,280, or 87%) continued to receive a statin during their hospitalization. And among the 8,940 who did not receive regular statin treatment before their stroke, 3,013 (34%) began statin treatment while hospitalized.
Patients who received a statin prior to their stroke but did not continue while hospitalized had a statistically significant 15% relative reduction in their mortality during the following year, compared with patients who never received a statin.
The key element for mortality protection appeared to be treatment while hospitalized. Relative mortality reduction compared with nonstatin users was 41% among patients who were on a statin both before their stroke and while hospitalized, and 45% among those who started on a statin while hospitalized, said Dr. Flint, a neurointensivist and stroke specialist at Kaiser Redwood City (Calif.). Patients who received a statin before their stroke but discontinued the drug once hospitalized had the worst outcomes, with a mortality rate that was 2.5-fold higher than that of patients who never received a statin.
Further analysis highlighted the importance of an early start to statin treatment in hospitalized patients, and also showed a dose-response relationship. Patients who received at least 60 mg of their statin daily either before hospitalization or both before and during hospitalization had a significantly lower mortality rate, compared with patients who took less than 60 mg/day. Dr. Flint noted that about 70% of patients received lovastatin, and about 20% received simvastatin.
Regarding timing, patients who either began on a statin for the first time or restarted their treatment on their first hospitalized day had a significantly lower 1-year mortality, compared with patients who did not start or restart their statin until their third day in hospital.
Dr. Flint also reported an additional analysis that had been run to determine whether patients’ survival prognosis drove their statin treatment instead of their statin treatment’s driving their survival. To do this, he looked at patterns of care at each of the 17 Kaiser Permanente of Northern California hospitals that were involved in the study. This "grouped treatment analysis" showed that although the survival prognosis of patients who were withdrawn from prior statin treatment while hospitalized played some role in the relationship, it was unable to explain all of the survival effect, indicating that statin treatment itself during hospitalization played a significant role in subsequent survival.
The strong impact that early statin treatment during stroke hospitalization has on long-term survival probably depends on the pleiotropic effects of statins. The timing makes it less likely that the effect of statins on lipid levels can explain the observed survival benefits, Dr. Flint said.
Dr. Flint said that he had no disclosures.
* CORRECTION, 3/4/2011: An earlier version of this article stated that some study participants took statins intermittently prior to having a stroke. However, the study included only patients who were taking a statin for at least 3 months prior to the stroke or those not taking a statin at all. This version has been updated.
LOS ANGELES – Starting or maintaining acute stroke patients on a statin during their initial hospitalization was linked with a dramatic improvement in 1-year survival in a retrospective review of medical records for more than 12,000 U.S. patients.
Based on the finding, Kaiser Permanente of Northern California will issue a revised order set that will recommend to physicians that they start acute stroke patients on 80-mg simvastatin as soon as possible on the first day of their hospitalization, Dr. Alexander C. Flint said at the International Stroke Conference.
"Based on results from the SPARCL [Stroke Prevention by Aggressive Reduction in Cholesterol Levels] trial, pretty much everyone in the stroke community believes that patients who have had an ischemic stroke should be treated with high-dose statin to prevent a second stroke (N. Engl. J. Med. 2006;355:549-59). In our study, the question wasn’t whether to treat, but the timing. What our results say is that you should not wait until the patient is discharged or is an outpatient, but that you should start the statin on day 1," Dr. Flint said in an interview.
The data he reported showed that stroke patients who started on a statin during their acute-phase hospitalization had a 15% absolute reduced rate of death during the first year following their stroke, compared with patients who did not start on a statin and did not receive a statin prior to their stroke (Stroke 2011;42:e-42-110). After adjustment for several possible confounding factors, including age; sex; race and ethnicity; year of stroke; and comorbidities such as hypertension and diabetes, stroke patients who started on a statin while hospitalized had a statistically significant (45%) relatively lower risk of death during the subsequent year, compared with patients who did not receive a statin.
The study involved 12,689 patients who received care from Kaiser Permanente of Northern California and had an ischemic stroke during 2000-2007. The total included 3,749 patients who were on steady statin treatment for at least 3 months before their stroke, and 8,940 patients who were not receiving a statin at all before their stroke.* Of the 3,749 patients who were on a statin before their stroke, most (3,280, or 87%) continued to receive a statin during their hospitalization. And among the 8,940 who did not receive regular statin treatment before their stroke, 3,013 (34%) began statin treatment while hospitalized.
Patients who received a statin prior to their stroke but did not continue while hospitalized had a statistically significant 15% relative reduction in their mortality during the following year, compared with patients who never received a statin.
The key element for mortality protection appeared to be treatment while hospitalized. Relative mortality reduction compared with nonstatin users was 41% among patients who were on a statin both before their stroke and while hospitalized, and 45% among those who started on a statin while hospitalized, said Dr. Flint, a neurointensivist and stroke specialist at Kaiser Redwood City (Calif.). Patients who received a statin before their stroke but discontinued the drug once hospitalized had the worst outcomes, with a mortality rate that was 2.5-fold higher than that of patients who never received a statin.
Further analysis highlighted the importance of an early start to statin treatment in hospitalized patients, and also showed a dose-response relationship. Patients who received at least 60 mg of their statin daily either before hospitalization or both before and during hospitalization had a significantly lower mortality rate, compared with patients who took less than 60 mg/day. Dr. Flint noted that about 70% of patients received lovastatin, and about 20% received simvastatin.
Regarding timing, patients who either began on a statin for the first time or restarted their treatment on their first hospitalized day had a significantly lower 1-year mortality, compared with patients who did not start or restart their statin until their third day in hospital.
Dr. Flint also reported an additional analysis that had been run to determine whether patients’ survival prognosis drove their statin treatment instead of their statin treatment’s driving their survival. To do this, he looked at patterns of care at each of the 17 Kaiser Permanente of Northern California hospitals that were involved in the study. This "grouped treatment analysis" showed that although the survival prognosis of patients who were withdrawn from prior statin treatment while hospitalized played some role in the relationship, it was unable to explain all of the survival effect, indicating that statin treatment itself during hospitalization played a significant role in subsequent survival.
The strong impact that early statin treatment during stroke hospitalization has on long-term survival probably depends on the pleiotropic effects of statins. The timing makes it less likely that the effect of statins on lipid levels can explain the observed survival benefits, Dr. Flint said.
Dr. Flint said that he had no disclosures.
* CORRECTION, 3/4/2011: An earlier version of this article stated that some study participants took statins intermittently prior to having a stroke. However, the study included only patients who were taking a statin for at least 3 months prior to the stroke or those not taking a statin at all. This version has been updated.
FROM THE INTERNATIONAL STROKE CONFERENCE
Major Finding: Patients who began statin treatment while hospitalized following an acute ischemic stroke had a 45% reduced relative mortality rate, compared with patients never treated with a statin.
Data Source: Review of 12,689 patients enrolled in Kaiser Permanente of Northern California who had an acute ischemic stroke during 2000-2007.
Disclosures: Dr. Flint reported having no relevant disclosures.
Strokes Pose Long-Term Survival Risk in AF Patients
LOS ANGELES – Strokes in patients with atrial fibrillation have long-term consequences.
Patients with atrial fibrillation (AF) who had an ischemic stroke and survived for the first 30 days following the event still had a greater than threefold increased risk of death during the following 5 years, compared with AF patients who had no stroke, in a retrospective study.
"The effects of stroke on mortality in patients with atrial fibrillation persist far beyond the initial event," Dr. Margaret Fang said at the International Stroke Conference.
The findings also highlight the importance of using proper anticoagulation regimens in patients with AF, both to prevent strokes and to reduce the severity of the strokes that do occur.
"We talk about preventing in-hospital death and 30-day mortality" with anticoagulation treatment of patients with AF, "but by preventing stroke, we also reduce long-term mortality. And if strokes occur, they are milder, and milder strokes have better long-term mortality outcomes," Dr. Fang, a hospitalist and director of the anticoagulation clinic at the University of California, San Francisco, said in an interview.
Her study reviewed 13,559 patients with nonvalvular AF (average age, 71 years) who were enrolled in Kaiser Permanente of Northern California. At baseline, about 9% of the patients had a history of a prior stroke. During a median follow-up of 6 years, 1,025 patients had a new-onset ischemic stroke.
About half of the patients were on warfarin at baseline. During follow-up, the incidence of stroke was 1.2% per year among patients on warfarin and 2.0% per year in patients not on warfarin. Warfarin treatment also led to milder strokes: About 46% of the warfarin-treated patients who had a stroke had either no deficit or only minor sequelae from their stroke, compared with 39% in patients not on warfarin. Major or severe deficits or death occurred in 54% of those on warfarin and in 61% of those not receiving anticoagulant treatment. The 30-day mortality rate was 20% in patients on warfarin at the time of their stroke and 28% in those not on warfarin.
The mortality among AF patients who survived longer than 30 days after their stroke was a statistically-significant 3.4-fold higher than in AF patients who did not have a stroke, according to an analysis that controlled for age, sex, prior stroke, and comorbidities such as hypertension and diabetes. At the 5-year follow-up, more than 70% of the AF patients without a stroke remained alive, compared with fewer than 40% of patients who had a stroke during the study period.
Survival beyond 30 days after a stroke also depended on stroke severity. About 60% of patients without disability following their stroke were alive at 5 years. Patients with strokes that produced minor, major, or severe deficits had 5-year survival rates of roughly 50%, 30%, and 10%, respectively.
Dr. Fang said that she had no disclosures.
LOS ANGELES – Strokes in patients with atrial fibrillation have long-term consequences.
Patients with atrial fibrillation (AF) who had an ischemic stroke and survived for the first 30 days following the event still had a greater than threefold increased risk of death during the following 5 years, compared with AF patients who had no stroke, in a retrospective study.
"The effects of stroke on mortality in patients with atrial fibrillation persist far beyond the initial event," Dr. Margaret Fang said at the International Stroke Conference.
The findings also highlight the importance of using proper anticoagulation regimens in patients with AF, both to prevent strokes and to reduce the severity of the strokes that do occur.
"We talk about preventing in-hospital death and 30-day mortality" with anticoagulation treatment of patients with AF, "but by preventing stroke, we also reduce long-term mortality. And if strokes occur, they are milder, and milder strokes have better long-term mortality outcomes," Dr. Fang, a hospitalist and director of the anticoagulation clinic at the University of California, San Francisco, said in an interview.
Her study reviewed 13,559 patients with nonvalvular AF (average age, 71 years) who were enrolled in Kaiser Permanente of Northern California. At baseline, about 9% of the patients had a history of a prior stroke. During a median follow-up of 6 years, 1,025 patients had a new-onset ischemic stroke.
About half of the patients were on warfarin at baseline. During follow-up, the incidence of stroke was 1.2% per year among patients on warfarin and 2.0% per year in patients not on warfarin. Warfarin treatment also led to milder strokes: About 46% of the warfarin-treated patients who had a stroke had either no deficit or only minor sequelae from their stroke, compared with 39% in patients not on warfarin. Major or severe deficits or death occurred in 54% of those on warfarin and in 61% of those not receiving anticoagulant treatment. The 30-day mortality rate was 20% in patients on warfarin at the time of their stroke and 28% in those not on warfarin.
The mortality among AF patients who survived longer than 30 days after their stroke was a statistically-significant 3.4-fold higher than in AF patients who did not have a stroke, according to an analysis that controlled for age, sex, prior stroke, and comorbidities such as hypertension and diabetes. At the 5-year follow-up, more than 70% of the AF patients without a stroke remained alive, compared with fewer than 40% of patients who had a stroke during the study period.
Survival beyond 30 days after a stroke also depended on stroke severity. About 60% of patients without disability following their stroke were alive at 5 years. Patients with strokes that produced minor, major, or severe deficits had 5-year survival rates of roughly 50%, 30%, and 10%, respectively.
Dr. Fang said that she had no disclosures.
LOS ANGELES – Strokes in patients with atrial fibrillation have long-term consequences.
Patients with atrial fibrillation (AF) who had an ischemic stroke and survived for the first 30 days following the event still had a greater than threefold increased risk of death during the following 5 years, compared with AF patients who had no stroke, in a retrospective study.
"The effects of stroke on mortality in patients with atrial fibrillation persist far beyond the initial event," Dr. Margaret Fang said at the International Stroke Conference.
The findings also highlight the importance of using proper anticoagulation regimens in patients with AF, both to prevent strokes and to reduce the severity of the strokes that do occur.
"We talk about preventing in-hospital death and 30-day mortality" with anticoagulation treatment of patients with AF, "but by preventing stroke, we also reduce long-term mortality. And if strokes occur, they are milder, and milder strokes have better long-term mortality outcomes," Dr. Fang, a hospitalist and director of the anticoagulation clinic at the University of California, San Francisco, said in an interview.
Her study reviewed 13,559 patients with nonvalvular AF (average age, 71 years) who were enrolled in Kaiser Permanente of Northern California. At baseline, about 9% of the patients had a history of a prior stroke. During a median follow-up of 6 years, 1,025 patients had a new-onset ischemic stroke.
About half of the patients were on warfarin at baseline. During follow-up, the incidence of stroke was 1.2% per year among patients on warfarin and 2.0% per year in patients not on warfarin. Warfarin treatment also led to milder strokes: About 46% of the warfarin-treated patients who had a stroke had either no deficit or only minor sequelae from their stroke, compared with 39% in patients not on warfarin. Major or severe deficits or death occurred in 54% of those on warfarin and in 61% of those not receiving anticoagulant treatment. The 30-day mortality rate was 20% in patients on warfarin at the time of their stroke and 28% in those not on warfarin.
The mortality among AF patients who survived longer than 30 days after their stroke was a statistically-significant 3.4-fold higher than in AF patients who did not have a stroke, according to an analysis that controlled for age, sex, prior stroke, and comorbidities such as hypertension and diabetes. At the 5-year follow-up, more than 70% of the AF patients without a stroke remained alive, compared with fewer than 40% of patients who had a stroke during the study period.
Survival beyond 30 days after a stroke also depended on stroke severity. About 60% of patients without disability following their stroke were alive at 5 years. Patients with strokes that produced minor, major, or severe deficits had 5-year survival rates of roughly 50%, 30%, and 10%, respectively.
Dr. Fang said that she had no disclosures.
Major Finding: Patients with AF who had a stroke and survived for at least 30 days had a 3.4-fold increased risk of death at 5 years, compared with AF patients without a stroke.
Data Source: Review of 13,559 patients with AF treated through Kaiser Permanente of Northern California and followed for a median of 6 years.
Disclosures: Dr. Fang said that she had no disclosures.
Strokes Pose Long-Term Survival Risk in AF Patients
LOS ANGELES – Strokes in patients with atrial fibrillation have long-term consequences.
Patients with atrial fibrillation (AF) who had an ischemic stroke and survived for the first 30 days following the event still had a greater than threefold increased risk of death during the following 5 years, compared with AF patients who had no stroke, in a retrospective study.
"The effects of stroke on mortality in patients with atrial fibrillation persist far beyond the initial event," Dr. Margaret Fang said at the International Stroke Conference.
The findings also highlight the importance of using proper anticoagulation regimens in patients with AF, both to prevent strokes and to reduce the severity of the strokes that do occur.
"We talk about preventing in-hospital death and 30-day mortality" with anticoagulation treatment of patients with AF, "but by preventing stroke, we also reduce long-term mortality. And if strokes occur, they are milder, and milder strokes have better long-term mortality outcomes," Dr. Fang, a hospitalist and director of the anticoagulation clinic at the University of California, San Francisco, said in an interview.
Her study reviewed 13,559 patients with nonvalvular AF (average age, 71 years) who were enrolled in Kaiser Permanente of Northern California. At baseline, about 9% of the patients had a history of a prior stroke. During a median follow-up of 6 years, 1,025 patients had a new-onset ischemic stroke.
About half of the patients were on warfarin at baseline. During follow-up, the incidence of stroke was 1.2% per year among patients on warfarin and 2.0% per year in patients not on warfarin. Warfarin treatment also led to milder strokes: About 46% of the warfarin-treated patients who had a stroke had either no deficit or only minor sequelae from their stroke, compared with 39% in patients not on warfarin. Major or severe deficits or death occurred in 54% of those on warfarin and in 61% of those not receiving anticoagulant treatment. The 30-day mortality rate was 20% in patients on warfarin at the time of their stroke and 28% in those not on warfarin.
The mortality among AF patients who survived longer than 30 days after their stroke was a statistically-significant 3.4-fold higher than in AF patients who did not have a stroke, according to an analysis that controlled for age, sex, prior stroke, and comorbidities such as hypertension and diabetes. At the 5-year follow-up, more than 70% of the AF patients without a stroke remained alive, compared with fewer than 40% of patients who had a stroke during the study period.
Survival beyond 30 days after a stroke also depended on stroke severity. About 60% of patients without disability following their stroke were alive at 5 years. Patients with strokes that produced minor, major, or severe deficits had 5-year survival rates of roughly 50%, 30%, and 10%, respectively.
Dr. Fang said that she had no disclosures.
LOS ANGELES – Strokes in patients with atrial fibrillation have long-term consequences.
Patients with atrial fibrillation (AF) who had an ischemic stroke and survived for the first 30 days following the event still had a greater than threefold increased risk of death during the following 5 years, compared with AF patients who had no stroke, in a retrospective study.
"The effects of stroke on mortality in patients with atrial fibrillation persist far beyond the initial event," Dr. Margaret Fang said at the International Stroke Conference.
The findings also highlight the importance of using proper anticoagulation regimens in patients with AF, both to prevent strokes and to reduce the severity of the strokes that do occur.
"We talk about preventing in-hospital death and 30-day mortality" with anticoagulation treatment of patients with AF, "but by preventing stroke, we also reduce long-term mortality. And if strokes occur, they are milder, and milder strokes have better long-term mortality outcomes," Dr. Fang, a hospitalist and director of the anticoagulation clinic at the University of California, San Francisco, said in an interview.
Her study reviewed 13,559 patients with nonvalvular AF (average age, 71 years) who were enrolled in Kaiser Permanente of Northern California. At baseline, about 9% of the patients had a history of a prior stroke. During a median follow-up of 6 years, 1,025 patients had a new-onset ischemic stroke.
About half of the patients were on warfarin at baseline. During follow-up, the incidence of stroke was 1.2% per year among patients on warfarin and 2.0% per year in patients not on warfarin. Warfarin treatment also led to milder strokes: About 46% of the warfarin-treated patients who had a stroke had either no deficit or only minor sequelae from their stroke, compared with 39% in patients not on warfarin. Major or severe deficits or death occurred in 54% of those on warfarin and in 61% of those not receiving anticoagulant treatment. The 30-day mortality rate was 20% in patients on warfarin at the time of their stroke and 28% in those not on warfarin.
The mortality among AF patients who survived longer than 30 days after their stroke was a statistically-significant 3.4-fold higher than in AF patients who did not have a stroke, according to an analysis that controlled for age, sex, prior stroke, and comorbidities such as hypertension and diabetes. At the 5-year follow-up, more than 70% of the AF patients without a stroke remained alive, compared with fewer than 40% of patients who had a stroke during the study period.
Survival beyond 30 days after a stroke also depended on stroke severity. About 60% of patients without disability following their stroke were alive at 5 years. Patients with strokes that produced minor, major, or severe deficits had 5-year survival rates of roughly 50%, 30%, and 10%, respectively.
Dr. Fang said that she had no disclosures.
LOS ANGELES – Strokes in patients with atrial fibrillation have long-term consequences.
Patients with atrial fibrillation (AF) who had an ischemic stroke and survived for the first 30 days following the event still had a greater than threefold increased risk of death during the following 5 years, compared with AF patients who had no stroke, in a retrospective study.
"The effects of stroke on mortality in patients with atrial fibrillation persist far beyond the initial event," Dr. Margaret Fang said at the International Stroke Conference.
The findings also highlight the importance of using proper anticoagulation regimens in patients with AF, both to prevent strokes and to reduce the severity of the strokes that do occur.
"We talk about preventing in-hospital death and 30-day mortality" with anticoagulation treatment of patients with AF, "but by preventing stroke, we also reduce long-term mortality. And if strokes occur, they are milder, and milder strokes have better long-term mortality outcomes," Dr. Fang, a hospitalist and director of the anticoagulation clinic at the University of California, San Francisco, said in an interview.
Her study reviewed 13,559 patients with nonvalvular AF (average age, 71 years) who were enrolled in Kaiser Permanente of Northern California. At baseline, about 9% of the patients had a history of a prior stroke. During a median follow-up of 6 years, 1,025 patients had a new-onset ischemic stroke.
About half of the patients were on warfarin at baseline. During follow-up, the incidence of stroke was 1.2% per year among patients on warfarin and 2.0% per year in patients not on warfarin. Warfarin treatment also led to milder strokes: About 46% of the warfarin-treated patients who had a stroke had either no deficit or only minor sequelae from their stroke, compared with 39% in patients not on warfarin. Major or severe deficits or death occurred in 54% of those on warfarin and in 61% of those not receiving anticoagulant treatment. The 30-day mortality rate was 20% in patients on warfarin at the time of their stroke and 28% in those not on warfarin.
The mortality among AF patients who survived longer than 30 days after their stroke was a statistically-significant 3.4-fold higher than in AF patients who did not have a stroke, according to an analysis that controlled for age, sex, prior stroke, and comorbidities such as hypertension and diabetes. At the 5-year follow-up, more than 70% of the AF patients without a stroke remained alive, compared with fewer than 40% of patients who had a stroke during the study period.
Survival beyond 30 days after a stroke also depended on stroke severity. About 60% of patients without disability following their stroke were alive at 5 years. Patients with strokes that produced minor, major, or severe deficits had 5-year survival rates of roughly 50%, 30%, and 10%, respectively.
Dr. Fang said that she had no disclosures.
Major Finding: Patients with AF who had a stroke and survived for at least 30 days had a 3.4-fold increased risk of death at 5 years, compared with AF patients without a stroke.
Data Source: Review of 13,559 patients with AF treated through Kaiser Permanente of Northern California and followed for a median of 6 years.
Disclosures: Dr. Fang said that she had no disclosures.
Strokes Pose Long-Term Survival Risk in AF Patients
LOS ANGELES – Strokes in patients with atrial fibrillation have long-term consequences.
Patients with atrial fibrillation (AF) who had an ischemic stroke and survived for the first 30 days following the event still had a greater than threefold increased risk of death during the following 5 years, compared with AF patients who had no stroke, in a retrospective study.
"The effects of stroke on mortality in patients with atrial fibrillation persist far beyond the initial event," Dr. Margaret Fang said at the International Stroke Conference.
The findings also highlight the importance of using proper anticoagulation regimens in patients with AF, both to prevent strokes and to reduce the severity of the strokes that do occur.
"We talk about preventing in-hospital death and 30-day mortality" with anticoagulation treatment of patients with AF, "but by preventing stroke, we also reduce long-term mortality. And if strokes occur, they are milder, and milder strokes have better long-term mortality outcomes," Dr. Fang, a hospitalist and director of the anticoagulation clinic at the University of California, San Francisco, said in an interview.
Her study reviewed 13,559 patients with nonvalvular AF (average age, 71 years) who were enrolled in Kaiser Permanente of Northern California. At baseline, about 9% of the patients had a history of a prior stroke. During a median follow-up of 6 years, 1,025 patients had a new-onset ischemic stroke.
About half of the patients were on warfarin at baseline. During follow-up, the incidence of stroke was 1.2% per year among patients on warfarin and 2.0% per year in patients not on warfarin. Warfarin treatment also led to milder strokes: About 46% of the warfarin-treated patients who had a stroke had either no deficit or only minor sequelae from their stroke, compared with 39% in patients not on warfarin. Major or severe deficits or death occurred in 54% of those on warfarin and in 61% of those not receiving anticoagulant treatment. The 30-day mortality rate was 20% in patients on warfarin at the time of their stroke and 28% in those not on warfarin.
The mortality among AF patients who survived longer than 30 days after their stroke was a statistically-significant 3.4-fold higher than in AF patients who did not have a stroke, according to an analysis that controlled for age, sex, prior stroke, and comorbidities such as hypertension and diabetes. At the 5-year follow-up, more than 70% of the AF patients without a stroke remained alive, compared with fewer than 40% of patients who had a stroke during the study period.
Survival beyond 30 days after a stroke also depended on stroke severity. About 60% of patients without disability following their stroke were alive at 5 years. Patients with strokes that produced minor, major, or severe deficits had 5-year survival rates of roughly 50%, 30%, and 10%, respectively.
Dr. Fang said that she had no disclosures.
LOS ANGELES – Strokes in patients with atrial fibrillation have long-term consequences.
Patients with atrial fibrillation (AF) who had an ischemic stroke and survived for the first 30 days following the event still had a greater than threefold increased risk of death during the following 5 years, compared with AF patients who had no stroke, in a retrospective study.
"The effects of stroke on mortality in patients with atrial fibrillation persist far beyond the initial event," Dr. Margaret Fang said at the International Stroke Conference.
The findings also highlight the importance of using proper anticoagulation regimens in patients with AF, both to prevent strokes and to reduce the severity of the strokes that do occur.
"We talk about preventing in-hospital death and 30-day mortality" with anticoagulation treatment of patients with AF, "but by preventing stroke, we also reduce long-term mortality. And if strokes occur, they are milder, and milder strokes have better long-term mortality outcomes," Dr. Fang, a hospitalist and director of the anticoagulation clinic at the University of California, San Francisco, said in an interview.
Her study reviewed 13,559 patients with nonvalvular AF (average age, 71 years) who were enrolled in Kaiser Permanente of Northern California. At baseline, about 9% of the patients had a history of a prior stroke. During a median follow-up of 6 years, 1,025 patients had a new-onset ischemic stroke.
About half of the patients were on warfarin at baseline. During follow-up, the incidence of stroke was 1.2% per year among patients on warfarin and 2.0% per year in patients not on warfarin. Warfarin treatment also led to milder strokes: About 46% of the warfarin-treated patients who had a stroke had either no deficit or only minor sequelae from their stroke, compared with 39% in patients not on warfarin. Major or severe deficits or death occurred in 54% of those on warfarin and in 61% of those not receiving anticoagulant treatment. The 30-day mortality rate was 20% in patients on warfarin at the time of their stroke and 28% in those not on warfarin.
The mortality among AF patients who survived longer than 30 days after their stroke was a statistically-significant 3.4-fold higher than in AF patients who did not have a stroke, according to an analysis that controlled for age, sex, prior stroke, and comorbidities such as hypertension and diabetes. At the 5-year follow-up, more than 70% of the AF patients without a stroke remained alive, compared with fewer than 40% of patients who had a stroke during the study period.
Survival beyond 30 days after a stroke also depended on stroke severity. About 60% of patients without disability following their stroke were alive at 5 years. Patients with strokes that produced minor, major, or severe deficits had 5-year survival rates of roughly 50%, 30%, and 10%, respectively.
Dr. Fang said that she had no disclosures.
LOS ANGELES – Strokes in patients with atrial fibrillation have long-term consequences.
Patients with atrial fibrillation (AF) who had an ischemic stroke and survived for the first 30 days following the event still had a greater than threefold increased risk of death during the following 5 years, compared with AF patients who had no stroke, in a retrospective study.
"The effects of stroke on mortality in patients with atrial fibrillation persist far beyond the initial event," Dr. Margaret Fang said at the International Stroke Conference.
The findings also highlight the importance of using proper anticoagulation regimens in patients with AF, both to prevent strokes and to reduce the severity of the strokes that do occur.
"We talk about preventing in-hospital death and 30-day mortality" with anticoagulation treatment of patients with AF, "but by preventing stroke, we also reduce long-term mortality. And if strokes occur, they are milder, and milder strokes have better long-term mortality outcomes," Dr. Fang, a hospitalist and director of the anticoagulation clinic at the University of California, San Francisco, said in an interview.
Her study reviewed 13,559 patients with nonvalvular AF (average age, 71 years) who were enrolled in Kaiser Permanente of Northern California. At baseline, about 9% of the patients had a history of a prior stroke. During a median follow-up of 6 years, 1,025 patients had a new-onset ischemic stroke.
About half of the patients were on warfarin at baseline. During follow-up, the incidence of stroke was 1.2% per year among patients on warfarin and 2.0% per year in patients not on warfarin. Warfarin treatment also led to milder strokes: About 46% of the warfarin-treated patients who had a stroke had either no deficit or only minor sequelae from their stroke, compared with 39% in patients not on warfarin. Major or severe deficits or death occurred in 54% of those on warfarin and in 61% of those not receiving anticoagulant treatment. The 30-day mortality rate was 20% in patients on warfarin at the time of their stroke and 28% in those not on warfarin.
The mortality among AF patients who survived longer than 30 days after their stroke was a statistically-significant 3.4-fold higher than in AF patients who did not have a stroke, according to an analysis that controlled for age, sex, prior stroke, and comorbidities such as hypertension and diabetes. At the 5-year follow-up, more than 70% of the AF patients without a stroke remained alive, compared with fewer than 40% of patients who had a stroke during the study period.
Survival beyond 30 days after a stroke also depended on stroke severity. About 60% of patients without disability following their stroke were alive at 5 years. Patients with strokes that produced minor, major, or severe deficits had 5-year survival rates of roughly 50%, 30%, and 10%, respectively.
Dr. Fang said that she had no disclosures.
Major Finding: Patients with AF who had a stroke and survived for at least 30 days had a 3.4-fold increased risk of death at 5 years, compared with AF patients without a stroke.
Data Source: Review of 13,559 patients with AF treated through Kaiser Permanente of Northern California and followed for a median of 6 years.
Disclosures: Dr. Fang said that she had no disclosures.
Carotid Stents Caused Excess Strokes in Older Patients and Women
LOS ANGELES – Women, as well as all patients aged 65 years or older who have substantial carotid artery stenosis that needs revascularization, may prefer endarterectomy, and would want to steer clear of carotid stenting, according to new data from CREST, the largest randomized trial to compare these two carotid interventions.
All patients aged 65 or older who were randomized to treatment by carotid artery stenting had a statistically significant excess of strokes, compared with similar subgroups who were treated with endarterectomy during the periprocedural period and 4-year follow-up, George Howard, Dr.P.H., said at the International Stroke Conference. "Patient age should be an important factor in selecting the treatment option for carotid stenosis," said Dr. Howard, professor and chairman of biostatistics at the University of Alabama at Birmingham.
Analysis of the patients enrolled in CREST (Carotid Revascularization Endarterectomy vs. Stenting Trial) by sex showed that the treatment of carotid stenosis by stenting led to an excess rate of periprocedural strokes among women, but not in men, Virginia J. Howard, Ph.D., said in a separate talk at the conference. Women who underwent an endarterectomy also had no excess risk for myocardial infarctions, compared with women who received a carotid stent, unlike men who had a significantly increased rate of MIs following open surgery, compared with those who got stented, said Dr. Howard, an epidemiologist at the University of Alabama at Birmingham.
The primary results from CREST, first reported last year, showed that all patients who were enrolled in the study had similar rates of stroke, MI, or death regardless of whether they underwent carotid endarterectomy or stenting (N. Engl. J. Med. 2010;363:11-23). But these new details, which show an excess rate of periprocedural strokes in women undergoing stenting as well as the excess of all strokes in patients aged 65 or older undergoing stenting, may tip the balance away from stenting in these patient subgroups.
Another CREST analysis that was also reported at the conference showed that patients who had a stroke had significant decrements in several measures of their health status at 1 year following their intervention, whereas patients who had an MI generally had a much more average health status profile after 1 year.
Going into CREST, which began in 2000, "we thought the results would be the opposite. [At that time,] we preferred to take older patients to stenting," commented Dr. Thomas G. Brott, lead investigator for CREST and a professor of neurology and director or research at the Mayo Clinic in Jacksonville, Florida. "Our interventionalists believe that age is a surrogate marker for patients with calcified and tortuous vessels that might not be suitable for stenting." Regarding the sex-related finding, the implications "depend on how a woman would value [the risk of having] a stroke or a MI. If the woman is more concerned about a periprocedural stroke, then the results suggest there could be a preference for endarterectomy," Dr. Brott said in an interview.
In the sex-based analysis, the rate of periprocedural stroke was 5.5% in stented women and 2.2% in those who underwent endarterectomy, a statistically significant 2.6-fold increased rate with stenting, Dr. Virginia Howard reported. During the entire follow-up, which added the rate of ipsilateral strokes during 4 years following the intervention, stroke rates were 7.8% in stented women and 5.0% in those who had endarterectomy, a nonsignificant difference. The two treatment options produced no difference in stroke rates in men, either periprocedurally or after 4 years. MI rates were similar in women following either intervention, both periprocedurally and after 4 years. The periprocedural and 4-year MI rates in men were significantly higher with endarterectomy.
In the age-based analyses, a calculation that used age as a continuous variable showed that the number of strokes occurring with either endarterectomy or stenting was similar for patients aged 64 years. For those aged 65 or older, fewer strokes occurred with endarterectomy, a relationship that grew stronger with increasing age. For patients aged 63 or younger, stenting produced fewer strokes, and the relationship grew stronger with decreasing age.
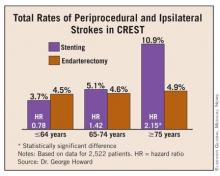
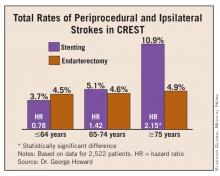
The age analysis also examined the data by dividing patients into three prespecified age group: younger than 65, 65-74 years, and 75 and older. (See box.) The most striking age effect occurred in patients aged 75 or older: In this subgroup, treatment with stenting more than doubled the total stroke risk, both periprocedural and long-term strokes, compared with patients who were treated with endarterectomy.
The incidence of MI showed a much weaker age effect, and patients who underwent stenting had a reduced rate of MI at all ages, compared with those who had endarterectomy. In addition, in the endarterectomy arm, age had no significant effect on the MI rate. Among patients treated with endarterectomy, the incidence of MI was 1.6% in patients younger than 65 years and 3.2% in those aged 75 or older, differences that were not statistically significant, Dr. George Howard said.
Dr. Christopher J. Moran said that a physician who wants to prevent strokes in patients with carotid artery disease would have to "think long and hard before treating a woman with carotid stenting." In some cases, endarterectomy may not be an option: The woman may be a poor operative candidate, or may not be a good candidate for anesthesia. "But if a woman is a good operative candidate, she should be treated with endarterectomy," he said.
Conventional angiography or CT angiography lets an operator assess the size of a woman’s arteries, explained Dr. Moran, a professor of radiology and neurological surgery at Washington University, St. Louis, who performs carotid artery stenting but did not participate in CREST. The smallest self-expanding stents available for treating carotid disease are 5 mm in diameter, and because these are ideally oversized to the artery, the smallest diameter carotid that should be stented is 4 mm, he said. "Many women have carotids that are smaller than 4 mm, and in those cases you should definitely think twice about stenting."
The same considerations apply to patients who are 70-80 years old, Dr. Moran added. "If they are good operative candidates, they should undergo endarterectomy." The assessment of calcification and tortuosity in patients – factors that may be causing the worse outcomes in elderly patients who are treated with carotid stenting – might not be easy preoperatively. CT angiography may be able to identify these features. MR angiography will reveal tortuosity but not calcification. "The best assessment is by conventional angiography, although this is done much less frequently today than in the past. It is critical to initially assess a patient’s anatomy to determine whether he or she is a good candidate for stenting before starting the procedure," he concluded.
CREST received its primary funding from the U.S. National Institutes of Health, but received supplemental funding from Abbott Vascular Solutions, the company that markets the carotid stents and embolic protection devices used in the study. Dr. Virginia J. Howard said that she had no disclosures. Dr. George Howard said that he has been a consultant to Abbott. Dr. Brott had no disclosures. Dr. Moran said that he has been a speaker and a proctor for, and a consultant to, Codman and EV3 Inc.
LOS ANGELES – Women, as well as all patients aged 65 years or older who have substantial carotid artery stenosis that needs revascularization, may prefer endarterectomy, and would want to steer clear of carotid stenting, according to new data from CREST, the largest randomized trial to compare these two carotid interventions.
All patients aged 65 or older who were randomized to treatment by carotid artery stenting had a statistically significant excess of strokes, compared with similar subgroups who were treated with endarterectomy during the periprocedural period and 4-year follow-up, George Howard, Dr.P.H., said at the International Stroke Conference. "Patient age should be an important factor in selecting the treatment option for carotid stenosis," said Dr. Howard, professor and chairman of biostatistics at the University of Alabama at Birmingham.
Analysis of the patients enrolled in CREST (Carotid Revascularization Endarterectomy vs. Stenting Trial) by sex showed that the treatment of carotid stenosis by stenting led to an excess rate of periprocedural strokes among women, but not in men, Virginia J. Howard, Ph.D., said in a separate talk at the conference. Women who underwent an endarterectomy also had no excess risk for myocardial infarctions, compared with women who received a carotid stent, unlike men who had a significantly increased rate of MIs following open surgery, compared with those who got stented, said Dr. Howard, an epidemiologist at the University of Alabama at Birmingham.
The primary results from CREST, first reported last year, showed that all patients who were enrolled in the study had similar rates of stroke, MI, or death regardless of whether they underwent carotid endarterectomy or stenting (N. Engl. J. Med. 2010;363:11-23). But these new details, which show an excess rate of periprocedural strokes in women undergoing stenting as well as the excess of all strokes in patients aged 65 or older undergoing stenting, may tip the balance away from stenting in these patient subgroups.
Another CREST analysis that was also reported at the conference showed that patients who had a stroke had significant decrements in several measures of their health status at 1 year following their intervention, whereas patients who had an MI generally had a much more average health status profile after 1 year.
Going into CREST, which began in 2000, "we thought the results would be the opposite. [At that time,] we preferred to take older patients to stenting," commented Dr. Thomas G. Brott, lead investigator for CREST and a professor of neurology and director or research at the Mayo Clinic in Jacksonville, Florida. "Our interventionalists believe that age is a surrogate marker for patients with calcified and tortuous vessels that might not be suitable for stenting." Regarding the sex-related finding, the implications "depend on how a woman would value [the risk of having] a stroke or a MI. If the woman is more concerned about a periprocedural stroke, then the results suggest there could be a preference for endarterectomy," Dr. Brott said in an interview.
In the sex-based analysis, the rate of periprocedural stroke was 5.5% in stented women and 2.2% in those who underwent endarterectomy, a statistically significant 2.6-fold increased rate with stenting, Dr. Virginia Howard reported. During the entire follow-up, which added the rate of ipsilateral strokes during 4 years following the intervention, stroke rates were 7.8% in stented women and 5.0% in those who had endarterectomy, a nonsignificant difference. The two treatment options produced no difference in stroke rates in men, either periprocedurally or after 4 years. MI rates were similar in women following either intervention, both periprocedurally and after 4 years. The periprocedural and 4-year MI rates in men were significantly higher with endarterectomy.
In the age-based analyses, a calculation that used age as a continuous variable showed that the number of strokes occurring with either endarterectomy or stenting was similar for patients aged 64 years. For those aged 65 or older, fewer strokes occurred with endarterectomy, a relationship that grew stronger with increasing age. For patients aged 63 or younger, stenting produced fewer strokes, and the relationship grew stronger with decreasing age.
The age analysis also examined the data by dividing patients into three prespecified age group: younger than 65, 65-74 years, and 75 and older. (See box.) The most striking age effect occurred in patients aged 75 or older: In this subgroup, treatment with stenting more than doubled the total stroke risk, both periprocedural and long-term strokes, compared with patients who were treated with endarterectomy.
The incidence of MI showed a much weaker age effect, and patients who underwent stenting had a reduced rate of MI at all ages, compared with those who had endarterectomy. In addition, in the endarterectomy arm, age had no significant effect on the MI rate. Among patients treated with endarterectomy, the incidence of MI was 1.6% in patients younger than 65 years and 3.2% in those aged 75 or older, differences that were not statistically significant, Dr. George Howard said.
Dr. Christopher J. Moran said that a physician who wants to prevent strokes in patients with carotid artery disease would have to "think long and hard before treating a woman with carotid stenting." In some cases, endarterectomy may not be an option: The woman may be a poor operative candidate, or may not be a good candidate for anesthesia. "But if a woman is a good operative candidate, she should be treated with endarterectomy," he said.
Conventional angiography or CT angiography lets an operator assess the size of a woman’s arteries, explained Dr. Moran, a professor of radiology and neurological surgery at Washington University, St. Louis, who performs carotid artery stenting but did not participate in CREST. The smallest self-expanding stents available for treating carotid disease are 5 mm in diameter, and because these are ideally oversized to the artery, the smallest diameter carotid that should be stented is 4 mm, he said. "Many women have carotids that are smaller than 4 mm, and in those cases you should definitely think twice about stenting."
The same considerations apply to patients who are 70-80 years old, Dr. Moran added. "If they are good operative candidates, they should undergo endarterectomy." The assessment of calcification and tortuosity in patients – factors that may be causing the worse outcomes in elderly patients who are treated with carotid stenting – might not be easy preoperatively. CT angiography may be able to identify these features. MR angiography will reveal tortuosity but not calcification. "The best assessment is by conventional angiography, although this is done much less frequently today than in the past. It is critical to initially assess a patient’s anatomy to determine whether he or she is a good candidate for stenting before starting the procedure," he concluded.
CREST received its primary funding from the U.S. National Institutes of Health, but received supplemental funding from Abbott Vascular Solutions, the company that markets the carotid stents and embolic protection devices used in the study. Dr. Virginia J. Howard said that she had no disclosures. Dr. George Howard said that he has been a consultant to Abbott. Dr. Brott had no disclosures. Dr. Moran said that he has been a speaker and a proctor for, and a consultant to, Codman and EV3 Inc.
LOS ANGELES – Women, as well as all patients aged 65 years or older who have substantial carotid artery stenosis that needs revascularization, may prefer endarterectomy, and would want to steer clear of carotid stenting, according to new data from CREST, the largest randomized trial to compare these two carotid interventions.
All patients aged 65 or older who were randomized to treatment by carotid artery stenting had a statistically significant excess of strokes, compared with similar subgroups who were treated with endarterectomy during the periprocedural period and 4-year follow-up, George Howard, Dr.P.H., said at the International Stroke Conference. "Patient age should be an important factor in selecting the treatment option for carotid stenosis," said Dr. Howard, professor and chairman of biostatistics at the University of Alabama at Birmingham.
Analysis of the patients enrolled in CREST (Carotid Revascularization Endarterectomy vs. Stenting Trial) by sex showed that the treatment of carotid stenosis by stenting led to an excess rate of periprocedural strokes among women, but not in men, Virginia J. Howard, Ph.D., said in a separate talk at the conference. Women who underwent an endarterectomy also had no excess risk for myocardial infarctions, compared with women who received a carotid stent, unlike men who had a significantly increased rate of MIs following open surgery, compared with those who got stented, said Dr. Howard, an epidemiologist at the University of Alabama at Birmingham.
The primary results from CREST, first reported last year, showed that all patients who were enrolled in the study had similar rates of stroke, MI, or death regardless of whether they underwent carotid endarterectomy or stenting (N. Engl. J. Med. 2010;363:11-23). But these new details, which show an excess rate of periprocedural strokes in women undergoing stenting as well as the excess of all strokes in patients aged 65 or older undergoing stenting, may tip the balance away from stenting in these patient subgroups.
Another CREST analysis that was also reported at the conference showed that patients who had a stroke had significant decrements in several measures of their health status at 1 year following their intervention, whereas patients who had an MI generally had a much more average health status profile after 1 year.
Going into CREST, which began in 2000, "we thought the results would be the opposite. [At that time,] we preferred to take older patients to stenting," commented Dr. Thomas G. Brott, lead investigator for CREST and a professor of neurology and director or research at the Mayo Clinic in Jacksonville, Florida. "Our interventionalists believe that age is a surrogate marker for patients with calcified and tortuous vessels that might not be suitable for stenting." Regarding the sex-related finding, the implications "depend on how a woman would value [the risk of having] a stroke or a MI. If the woman is more concerned about a periprocedural stroke, then the results suggest there could be a preference for endarterectomy," Dr. Brott said in an interview.
In the sex-based analysis, the rate of periprocedural stroke was 5.5% in stented women and 2.2% in those who underwent endarterectomy, a statistically significant 2.6-fold increased rate with stenting, Dr. Virginia Howard reported. During the entire follow-up, which added the rate of ipsilateral strokes during 4 years following the intervention, stroke rates were 7.8% in stented women and 5.0% in those who had endarterectomy, a nonsignificant difference. The two treatment options produced no difference in stroke rates in men, either periprocedurally or after 4 years. MI rates were similar in women following either intervention, both periprocedurally and after 4 years. The periprocedural and 4-year MI rates in men were significantly higher with endarterectomy.
In the age-based analyses, a calculation that used age as a continuous variable showed that the number of strokes occurring with either endarterectomy or stenting was similar for patients aged 64 years. For those aged 65 or older, fewer strokes occurred with endarterectomy, a relationship that grew stronger with increasing age. For patients aged 63 or younger, stenting produced fewer strokes, and the relationship grew stronger with decreasing age.
The age analysis also examined the data by dividing patients into three prespecified age group: younger than 65, 65-74 years, and 75 and older. (See box.) The most striking age effect occurred in patients aged 75 or older: In this subgroup, treatment with stenting more than doubled the total stroke risk, both periprocedural and long-term strokes, compared with patients who were treated with endarterectomy.
The incidence of MI showed a much weaker age effect, and patients who underwent stenting had a reduced rate of MI at all ages, compared with those who had endarterectomy. In addition, in the endarterectomy arm, age had no significant effect on the MI rate. Among patients treated with endarterectomy, the incidence of MI was 1.6% in patients younger than 65 years and 3.2% in those aged 75 or older, differences that were not statistically significant, Dr. George Howard said.
Dr. Christopher J. Moran said that a physician who wants to prevent strokes in patients with carotid artery disease would have to "think long and hard before treating a woman with carotid stenting." In some cases, endarterectomy may not be an option: The woman may be a poor operative candidate, or may not be a good candidate for anesthesia. "But if a woman is a good operative candidate, she should be treated with endarterectomy," he said.
Conventional angiography or CT angiography lets an operator assess the size of a woman’s arteries, explained Dr. Moran, a professor of radiology and neurological surgery at Washington University, St. Louis, who performs carotid artery stenting but did not participate in CREST. The smallest self-expanding stents available for treating carotid disease are 5 mm in diameter, and because these are ideally oversized to the artery, the smallest diameter carotid that should be stented is 4 mm, he said. "Many women have carotids that are smaller than 4 mm, and in those cases you should definitely think twice about stenting."
The same considerations apply to patients who are 70-80 years old, Dr. Moran added. "If they are good operative candidates, they should undergo endarterectomy." The assessment of calcification and tortuosity in patients – factors that may be causing the worse outcomes in elderly patients who are treated with carotid stenting – might not be easy preoperatively. CT angiography may be able to identify these features. MR angiography will reveal tortuosity but not calcification. "The best assessment is by conventional angiography, although this is done much less frequently today than in the past. It is critical to initially assess a patient’s anatomy to determine whether he or she is a good candidate for stenting before starting the procedure," he concluded.
CREST received its primary funding from the U.S. National Institutes of Health, but received supplemental funding from Abbott Vascular Solutions, the company that markets the carotid stents and embolic protection devices used in the study. Dr. Virginia J. Howard said that she had no disclosures. Dr. George Howard said that he has been a consultant to Abbott. Dr. Brott had no disclosures. Dr. Moran said that he has been a speaker and a proctor for, and a consultant to, Codman and EV3 Inc.
FROM THE INTERNATIONAL STROKE CONFERENCE
Major Finding: Carotid stenting led to a statistically significant excess of strokes in patients aged 65 and older, compared with carotid endarterectomy. Stenting also led to a significant excess of periprocedural strokes in women compared with endarterectomy.
Data Source: CREST, a randomized, multicenter study of 2,522 patients with carotid stenosis.
Disclosures: CREST received its primary funding from the NIH, but received supplemental funding from Abbott Vascular Solutions, the company that markets the carotid stents and embolic protection devices that were used in the study. Dr. Virginia J. Howard said that she had no disclosures. Dr. George Howard said that he has been a consultant to Abbott. Dr. Brott had no disclosures.
Carotid Stents Caused Excess Strokes in Older Patients and Women
LOS ANGELES – Women, as well as all patients aged 65 years or older who have substantial carotid artery stenosis that needs revascularization, may prefer endarterectomy, and would want to steer clear of carotid stenting, according to new data from CREST, the largest randomized trial to compare these two carotid interventions.
All patients aged 65 or older who were randomized to treatment by carotid artery stenting had a statistically significant excess of strokes, compared with similar subgroups who were treated with endarterectomy during the periprocedural period and 4-year follow-up, George Howard, Dr.P.H., said at the International Stroke Conference. "Patient age should be an important factor in selecting the treatment option for carotid stenosis," said Dr. Howard, professor and chairman of biostatistics at the University of Alabama at Birmingham.
Analysis of the patients enrolled in CREST (Carotid Revascularization Endarterectomy vs. Stenting Trial) by sex showed that the treatment of carotid stenosis by stenting led to an excess rate of periprocedural strokes among women, but not in men, Virginia J. Howard, Ph.D., said in a separate talk at the conference. Women who underwent an endarterectomy also had no excess risk for myocardial infarctions, compared with women who received a carotid stent, unlike men who had a significantly increased rate of MIs following open surgery, compared with those who got stented, said Dr. Howard, an epidemiologist at the University of Alabama at Birmingham.
The primary results from CREST, first reported last year, showed that all patients who were enrolled in the study had similar rates of stroke, MI, or death regardless of whether they underwent carotid endarterectomy or stenting (N. Engl. J. Med. 2010;363:11-23). But these new details, which show an excess rate of periprocedural strokes in women undergoing stenting as well as the excess of all strokes in patients aged 65 or older undergoing stenting, may tip the balance away from stenting in these patient subgroups.
Another CREST analysis that was also reported at the conference showed that patients who had a stroke had significant decrements in several measures of their health status at 1 year following their intervention, whereas patients who had an MI generally had a much more average health status profile after 1 year.
Going into CREST, which began in 2000, "we thought the results would be the opposite. [At that time,] we preferred to take older patients to stenting," commented Dr. Thomas G. Brott, lead investigator for CREST and a professor of neurology and director or research at the Mayo Clinic in Jacksonville, Florida. "Our interventionalists believe that age is a surrogate marker for patients with calcified and tortuous vessels that might not be suitable for stenting." Regarding the sex-related finding, the implications "depend on how a woman would value [the risk of having] a stroke or a MI. If the woman is more concerned about a periprocedural stroke, then the results suggest there could be a preference for endarterectomy," Dr. Brott said in an interview.
In the sex-based analysis, the rate of periprocedural stroke was 5.5% in stented women and 2.2% in those who underwent endarterectomy, a statistically significant 2.6-fold increased rate with stenting, Dr. Virginia Howard reported. During the entire follow-up, which added the rate of ipsilateral strokes during 4 years following the intervention, stroke rates were 7.8% in stented women and 5.0% in those who had endarterectomy, a nonsignificant difference. The two treatment options produced no difference in stroke rates in men, either periprocedurally or after 4 years. MI rates were similar in women following either intervention, both periprocedurally and after 4 years. The periprocedural and 4-year MI rates in men were significantly higher with endarterectomy.
In the age-based analyses, a calculation that used age as a continuous variable showed that the number of strokes occurring with either endarterectomy or stenting was similar for patients aged 64 years. For those aged 65 or older, fewer strokes occurred with endarterectomy, a relationship that grew stronger with increasing age. For patients aged 63 or younger, stenting produced fewer strokes, and the relationship grew stronger with decreasing age.
The age analysis also examined the data by dividing patients into three prespecified age group: younger than 65, 65-74 years, and 75 and older. (See box.) The most striking age effect occurred in patients aged 75 or older: In this subgroup, treatment with stenting more than doubled the total stroke risk, both periprocedural and long-term strokes, compared with patients who were treated with endarterectomy.
The incidence of MI showed a much weaker age effect, and patients who underwent stenting had a reduced rate of MI at all ages, compared with those who had endarterectomy. In addition, in the endarterectomy arm, age had no significant effect on the MI rate. Among patients treated with endarterectomy, the incidence of MI was 1.6% in patients younger than 65 years and 3.2% in those aged 75 or older, differences that were not statistically significant, Dr. George Howard said.
Dr. Christopher J. Moran said that a physician who wants to prevent strokes in patients with carotid artery disease would have to "think long and hard before treating a woman with carotid stenting." In some cases, endarterectomy may not be an option: The woman may be a poor operative candidate, or may not be a good candidate for anesthesia. "But if a woman is a good operative candidate, she should be treated with endarterectomy," he said.
Conventional angiography or CT angiography lets an operator assess the size of a woman’s arteries, explained Dr. Moran, a professor of radiology and neurological surgery at Washington University, St. Louis, who performs carotid artery stenting but did not participate in CREST. The smallest self-expanding stents available for treating carotid disease are 5 mm in diameter, and because these are ideally oversized to the artery, the smallest diameter carotid that should be stented is 4 mm, he said. "Many women have carotids that are smaller than 4 mm, and in those cases you should definitely think twice about stenting."
The same considerations apply to patients who are 70-80 years old, Dr. Moran added. "If they are good operative candidates, they should undergo endarterectomy." The assessment of calcification and tortuosity in patients – factors that may be causing the worse outcomes in elderly patients who are treated with carotid stenting – might not be easy preoperatively. CT angiography may be able to identify these features. MR angiography will reveal tortuosity but not calcification. "The best assessment is by conventional angiography, although this is done much less frequently today than in the past. It is critical to initially assess a patient’s anatomy to determine whether he or she is a good candidate for stenting before starting the procedure," he concluded.
CREST received its primary funding from the U.S. National Institutes of Health, but received supplemental funding from Abbott Vascular Solutions, the company that markets the carotid stents and embolic protection devices used in the study. Dr. Virginia J. Howard said that she had no disclosures. Dr. George Howard said that he has been a consultant to Abbott. Dr. Brott had no disclosures. Dr. Moran said that he has been a speaker and a proctor for, and a consultant to, Codman and EV3 Inc.
LOS ANGELES – Women, as well as all patients aged 65 years or older who have substantial carotid artery stenosis that needs revascularization, may prefer endarterectomy, and would want to steer clear of carotid stenting, according to new data from CREST, the largest randomized trial to compare these two carotid interventions.
All patients aged 65 or older who were randomized to treatment by carotid artery stenting had a statistically significant excess of strokes, compared with similar subgroups who were treated with endarterectomy during the periprocedural period and 4-year follow-up, George Howard, Dr.P.H., said at the International Stroke Conference. "Patient age should be an important factor in selecting the treatment option for carotid stenosis," said Dr. Howard, professor and chairman of biostatistics at the University of Alabama at Birmingham.
Analysis of the patients enrolled in CREST (Carotid Revascularization Endarterectomy vs. Stenting Trial) by sex showed that the treatment of carotid stenosis by stenting led to an excess rate of periprocedural strokes among women, but not in men, Virginia J. Howard, Ph.D., said in a separate talk at the conference. Women who underwent an endarterectomy also had no excess risk for myocardial infarctions, compared with women who received a carotid stent, unlike men who had a significantly increased rate of MIs following open surgery, compared with those who got stented, said Dr. Howard, an epidemiologist at the University of Alabama at Birmingham.
The primary results from CREST, first reported last year, showed that all patients who were enrolled in the study had similar rates of stroke, MI, or death regardless of whether they underwent carotid endarterectomy or stenting (N. Engl. J. Med. 2010;363:11-23). But these new details, which show an excess rate of periprocedural strokes in women undergoing stenting as well as the excess of all strokes in patients aged 65 or older undergoing stenting, may tip the balance away from stenting in these patient subgroups.
Another CREST analysis that was also reported at the conference showed that patients who had a stroke had significant decrements in several measures of their health status at 1 year following their intervention, whereas patients who had an MI generally had a much more average health status profile after 1 year.
Going into CREST, which began in 2000, "we thought the results would be the opposite. [At that time,] we preferred to take older patients to stenting," commented Dr. Thomas G. Brott, lead investigator for CREST and a professor of neurology and director or research at the Mayo Clinic in Jacksonville, Florida. "Our interventionalists believe that age is a surrogate marker for patients with calcified and tortuous vessels that might not be suitable for stenting." Regarding the sex-related finding, the implications "depend on how a woman would value [the risk of having] a stroke or a MI. If the woman is more concerned about a periprocedural stroke, then the results suggest there could be a preference for endarterectomy," Dr. Brott said in an interview.
In the sex-based analysis, the rate of periprocedural stroke was 5.5% in stented women and 2.2% in those who underwent endarterectomy, a statistically significant 2.6-fold increased rate with stenting, Dr. Virginia Howard reported. During the entire follow-up, which added the rate of ipsilateral strokes during 4 years following the intervention, stroke rates were 7.8% in stented women and 5.0% in those who had endarterectomy, a nonsignificant difference. The two treatment options produced no difference in stroke rates in men, either periprocedurally or after 4 years. MI rates were similar in women following either intervention, both periprocedurally and after 4 years. The periprocedural and 4-year MI rates in men were significantly higher with endarterectomy.
In the age-based analyses, a calculation that used age as a continuous variable showed that the number of strokes occurring with either endarterectomy or stenting was similar for patients aged 64 years. For those aged 65 or older, fewer strokes occurred with endarterectomy, a relationship that grew stronger with increasing age. For patients aged 63 or younger, stenting produced fewer strokes, and the relationship grew stronger with decreasing age.
The age analysis also examined the data by dividing patients into three prespecified age group: younger than 65, 65-74 years, and 75 and older. (See box.) The most striking age effect occurred in patients aged 75 or older: In this subgroup, treatment with stenting more than doubled the total stroke risk, both periprocedural and long-term strokes, compared with patients who were treated with endarterectomy.
The incidence of MI showed a much weaker age effect, and patients who underwent stenting had a reduced rate of MI at all ages, compared with those who had endarterectomy. In addition, in the endarterectomy arm, age had no significant effect on the MI rate. Among patients treated with endarterectomy, the incidence of MI was 1.6% in patients younger than 65 years and 3.2% in those aged 75 or older, differences that were not statistically significant, Dr. George Howard said.
Dr. Christopher J. Moran said that a physician who wants to prevent strokes in patients with carotid artery disease would have to "think long and hard before treating a woman with carotid stenting." In some cases, endarterectomy may not be an option: The woman may be a poor operative candidate, or may not be a good candidate for anesthesia. "But if a woman is a good operative candidate, she should be treated with endarterectomy," he said.
Conventional angiography or CT angiography lets an operator assess the size of a woman’s arteries, explained Dr. Moran, a professor of radiology and neurological surgery at Washington University, St. Louis, who performs carotid artery stenting but did not participate in CREST. The smallest self-expanding stents available for treating carotid disease are 5 mm in diameter, and because these are ideally oversized to the artery, the smallest diameter carotid that should be stented is 4 mm, he said. "Many women have carotids that are smaller than 4 mm, and in those cases you should definitely think twice about stenting."
The same considerations apply to patients who are 70-80 years old, Dr. Moran added. "If they are good operative candidates, they should undergo endarterectomy." The assessment of calcification and tortuosity in patients – factors that may be causing the worse outcomes in elderly patients who are treated with carotid stenting – might not be easy preoperatively. CT angiography may be able to identify these features. MR angiography will reveal tortuosity but not calcification. "The best assessment is by conventional angiography, although this is done much less frequently today than in the past. It is critical to initially assess a patient’s anatomy to determine whether he or she is a good candidate for stenting before starting the procedure," he concluded.
CREST received its primary funding from the U.S. National Institutes of Health, but received supplemental funding from Abbott Vascular Solutions, the company that markets the carotid stents and embolic protection devices used in the study. Dr. Virginia J. Howard said that she had no disclosures. Dr. George Howard said that he has been a consultant to Abbott. Dr. Brott had no disclosures. Dr. Moran said that he has been a speaker and a proctor for, and a consultant to, Codman and EV3 Inc.
LOS ANGELES – Women, as well as all patients aged 65 years or older who have substantial carotid artery stenosis that needs revascularization, may prefer endarterectomy, and would want to steer clear of carotid stenting, according to new data from CREST, the largest randomized trial to compare these two carotid interventions.
All patients aged 65 or older who were randomized to treatment by carotid artery stenting had a statistically significant excess of strokes, compared with similar subgroups who were treated with endarterectomy during the periprocedural period and 4-year follow-up, George Howard, Dr.P.H., said at the International Stroke Conference. "Patient age should be an important factor in selecting the treatment option for carotid stenosis," said Dr. Howard, professor and chairman of biostatistics at the University of Alabama at Birmingham.
Analysis of the patients enrolled in CREST (Carotid Revascularization Endarterectomy vs. Stenting Trial) by sex showed that the treatment of carotid stenosis by stenting led to an excess rate of periprocedural strokes among women, but not in men, Virginia J. Howard, Ph.D., said in a separate talk at the conference. Women who underwent an endarterectomy also had no excess risk for myocardial infarctions, compared with women who received a carotid stent, unlike men who had a significantly increased rate of MIs following open surgery, compared with those who got stented, said Dr. Howard, an epidemiologist at the University of Alabama at Birmingham.
The primary results from CREST, first reported last year, showed that all patients who were enrolled in the study had similar rates of stroke, MI, or death regardless of whether they underwent carotid endarterectomy or stenting (N. Engl. J. Med. 2010;363:11-23). But these new details, which show an excess rate of periprocedural strokes in women undergoing stenting as well as the excess of all strokes in patients aged 65 or older undergoing stenting, may tip the balance away from stenting in these patient subgroups.
Another CREST analysis that was also reported at the conference showed that patients who had a stroke had significant decrements in several measures of their health status at 1 year following their intervention, whereas patients who had an MI generally had a much more average health status profile after 1 year.
Going into CREST, which began in 2000, "we thought the results would be the opposite. [At that time,] we preferred to take older patients to stenting," commented Dr. Thomas G. Brott, lead investigator for CREST and a professor of neurology and director or research at the Mayo Clinic in Jacksonville, Florida. "Our interventionalists believe that age is a surrogate marker for patients with calcified and tortuous vessels that might not be suitable for stenting." Regarding the sex-related finding, the implications "depend on how a woman would value [the risk of having] a stroke or a MI. If the woman is more concerned about a periprocedural stroke, then the results suggest there could be a preference for endarterectomy," Dr. Brott said in an interview.
In the sex-based analysis, the rate of periprocedural stroke was 5.5% in stented women and 2.2% in those who underwent endarterectomy, a statistically significant 2.6-fold increased rate with stenting, Dr. Virginia Howard reported. During the entire follow-up, which added the rate of ipsilateral strokes during 4 years following the intervention, stroke rates were 7.8% in stented women and 5.0% in those who had endarterectomy, a nonsignificant difference. The two treatment options produced no difference in stroke rates in men, either periprocedurally or after 4 years. MI rates were similar in women following either intervention, both periprocedurally and after 4 years. The periprocedural and 4-year MI rates in men were significantly higher with endarterectomy.
In the age-based analyses, a calculation that used age as a continuous variable showed that the number of strokes occurring with either endarterectomy or stenting was similar for patients aged 64 years. For those aged 65 or older, fewer strokes occurred with endarterectomy, a relationship that grew stronger with increasing age. For patients aged 63 or younger, stenting produced fewer strokes, and the relationship grew stronger with decreasing age.
The age analysis also examined the data by dividing patients into three prespecified age group: younger than 65, 65-74 years, and 75 and older. (See box.) The most striking age effect occurred in patients aged 75 or older: In this subgroup, treatment with stenting more than doubled the total stroke risk, both periprocedural and long-term strokes, compared with patients who were treated with endarterectomy.
The incidence of MI showed a much weaker age effect, and patients who underwent stenting had a reduced rate of MI at all ages, compared with those who had endarterectomy. In addition, in the endarterectomy arm, age had no significant effect on the MI rate. Among patients treated with endarterectomy, the incidence of MI was 1.6% in patients younger than 65 years and 3.2% in those aged 75 or older, differences that were not statistically significant, Dr. George Howard said.
Dr. Christopher J. Moran said that a physician who wants to prevent strokes in patients with carotid artery disease would have to "think long and hard before treating a woman with carotid stenting." In some cases, endarterectomy may not be an option: The woman may be a poor operative candidate, or may not be a good candidate for anesthesia. "But if a woman is a good operative candidate, she should be treated with endarterectomy," he said.
Conventional angiography or CT angiography lets an operator assess the size of a woman’s arteries, explained Dr. Moran, a professor of radiology and neurological surgery at Washington University, St. Louis, who performs carotid artery stenting but did not participate in CREST. The smallest self-expanding stents available for treating carotid disease are 5 mm in diameter, and because these are ideally oversized to the artery, the smallest diameter carotid that should be stented is 4 mm, he said. "Many women have carotids that are smaller than 4 mm, and in those cases you should definitely think twice about stenting."
The same considerations apply to patients who are 70-80 years old, Dr. Moran added. "If they are good operative candidates, they should undergo endarterectomy." The assessment of calcification and tortuosity in patients – factors that may be causing the worse outcomes in elderly patients who are treated with carotid stenting – might not be easy preoperatively. CT angiography may be able to identify these features. MR angiography will reveal tortuosity but not calcification. "The best assessment is by conventional angiography, although this is done much less frequently today than in the past. It is critical to initially assess a patient’s anatomy to determine whether he or she is a good candidate for stenting before starting the procedure," he concluded.
CREST received its primary funding from the U.S. National Institutes of Health, but received supplemental funding from Abbott Vascular Solutions, the company that markets the carotid stents and embolic protection devices used in the study. Dr. Virginia J. Howard said that she had no disclosures. Dr. George Howard said that he has been a consultant to Abbott. Dr. Brott had no disclosures. Dr. Moran said that he has been a speaker and a proctor for, and a consultant to, Codman and EV3 Inc.
FROM THE INTERNATIONAL STROKE CONFERENCE
Major Finding: Carotid stenting led to a statistically significant excess of strokes in patients aged 65 and older, compared with carotid endarterectomy. Stenting also led to a significant excess of periprocedural strokes in women compared with endarterectomy.
Data Source: CREST, a randomized, multicenter study of 2,522 patients with carotid stenosis.
Disclosures: CREST received its primary funding from the NIH, but received supplemental funding from Abbott Vascular Solutions, the company that markets the carotid stents and embolic protection devices that were used in the study. Dr. Virginia J. Howard said that she had no disclosures. Dr. George Howard said that he has been a consultant to Abbott. Dr. Brott had no disclosures.
Carotid Stenting, Endarterectomy Yield Similar Quality-of-Life Outcomes
LOS ANGELES – Carotid stenting and carotid endarterectomy led to very similar health status outcomes a year after surgery, according to the quality-of-life analysis of the CREST trial.
Although patients with carotid artery stenosis randomized to the stenting arm of the study generally had better health status measures at 2 and 4 weeks following their intervention, by 1 year "all between-group differences had entirely resolved" when compared with the patients randomized to carotid endarterectomy, Dr. Joshua M. Stolker said at the International Stroke Conference.
The two treatment alternatives tested in the Carotid Revascularization Endarterectomy vs Stenting Trial (CREST) led to nearly identical long-term outcomes for quality-of-life despite an excess of strokes in the carotid stenting arm, and despite the finding in a new, exploratory analysis of health status outcomes that strokes produced a markedly larger decrement in health status than did myocardial infarctions or cranial nerve palsy. The worse outcomes with stroke probably did not affect the overall outcome of the stented patients because the number of strokes – and especially the number of major strokes – was relatively small in CREST.
Because of "the small absolute difference in stroke rates" between the stented and open-surgery patients and the fact that "most of the difference was in minor strokes, "Overall, there was no difference for the whole population despite the impact of stroke," said Dr. Stolker, a cardiologist at Saint Louis University.
In CREST, stented patients had a 1.8% higher rate of all strokes, compared with the endarterectomy patients, including a 0.5% excess rate of major strokes.
Stroke patients showed statistically significant impairments, compared with the patients who did not have a stroke, in seven of the eight health status outcome subscales measured using the Short Form (SF)-36: physical function, role physical, vitality, pain, social function, role emotional, and mental health. In contrast, after 1 year patients in CREST who had an MI following their surgery had a deficit only in the measure of general health, compared with the CREST patients who did not have an MI. And patients who developed cranial-nerve palsy after their surgery had no 1-year deficits for any health-status measure, compared with the patients who did not develop cranial-nerve palsy.
These results "confirmed what a lot of us already suspected, that periprocedural stroke had a significant impact on 1-year health status across multiple SF-36 outcomes, but periprocedural MI and cranial-nerve palsy did not," Dr. Stolker said.
The greatest impact on health status occurred in patients with major periprocedural strokes, who on average showed significant reductions in all eight subscales of the SF-36 at 1-year follow-up. Patients with minor periprocedural strokes had, on average, significant 1-year drops in "three or four" SF-36 subscales, compared with CREST patients who did not have strokes, he said in an interview.
CREST randomized more than 2,500 patients with symptomatic or substantial asymptomatic carotid disease to either endarterectomy or carotid stenting during 2000-2008. The study’s primary end point results – the periprocedural rate of stroke, MI, or death plus the 4-year rate of ipsilateral stroke – showed no significant between the two study arms, results reported last year (N. Engl. J. Med. 2010;363:11-23). Dr. Stolker’s new report focused on a prespecified analysis of health status outcomes.
In addition to the eight subscales of the SF-36, the researchers also measured changes in health status by six parameters measures by modified Likert scales: difficulty walking, difficulty eating and swallowing, difficulty driving, headaches, neck pain, and leg pain.
The new analysis showed that at 2 weeks after the interventions, patients who had undergone carotid stenting had, on average, significantly better health-status scores for five of the eight SF-36 subscales. But at 4 weeks after treatment, this fell to significantly better scores for stenting in three subscales: physical function, social function, and role physical. One year after the intervention, both the stented and open surgery arms showed, on average, essentially identical scores for all eight subscales.
The six additional parameters scored on a modified Likert scale showed a roughly similar pattern. After 2 weeks, the stented patients had significantly better scores for difficulty eating and swallowing, difficulty driving, headache, and neck pain, while the endarterectomy patients had a significant edge for difficulty walking and leg pain. These between-group differences began diminishing at 4 weeks and, at 1 year after the intervention, neither procedure had a significant difference for any of the six measures.
CREST was primarily funded by the National Institutes of Health. It also received supplemental support from Abbott Vascular Solutions, the company that markets the carotid stent and embolic protection device used in the study. Dr. Stolker said that he has been on the speakers bureau of AstraZeneca and Pfizer.
LOS ANGELES – Carotid stenting and carotid endarterectomy led to very similar health status outcomes a year after surgery, according to the quality-of-life analysis of the CREST trial.
Although patients with carotid artery stenosis randomized to the stenting arm of the study generally had better health status measures at 2 and 4 weeks following their intervention, by 1 year "all between-group differences had entirely resolved" when compared with the patients randomized to carotid endarterectomy, Dr. Joshua M. Stolker said at the International Stroke Conference.
The two treatment alternatives tested in the Carotid Revascularization Endarterectomy vs Stenting Trial (CREST) led to nearly identical long-term outcomes for quality-of-life despite an excess of strokes in the carotid stenting arm, and despite the finding in a new, exploratory analysis of health status outcomes that strokes produced a markedly larger decrement in health status than did myocardial infarctions or cranial nerve palsy. The worse outcomes with stroke probably did not affect the overall outcome of the stented patients because the number of strokes – and especially the number of major strokes – was relatively small in CREST.
Because of "the small absolute difference in stroke rates" between the stented and open-surgery patients and the fact that "most of the difference was in minor strokes, "Overall, there was no difference for the whole population despite the impact of stroke," said Dr. Stolker, a cardiologist at Saint Louis University.
In CREST, stented patients had a 1.8% higher rate of all strokes, compared with the endarterectomy patients, including a 0.5% excess rate of major strokes.
Stroke patients showed statistically significant impairments, compared with the patients who did not have a stroke, in seven of the eight health status outcome subscales measured using the Short Form (SF)-36: physical function, role physical, vitality, pain, social function, role emotional, and mental health. In contrast, after 1 year patients in CREST who had an MI following their surgery had a deficit only in the measure of general health, compared with the CREST patients who did not have an MI. And patients who developed cranial-nerve palsy after their surgery had no 1-year deficits for any health-status measure, compared with the patients who did not develop cranial-nerve palsy.
These results "confirmed what a lot of us already suspected, that periprocedural stroke had a significant impact on 1-year health status across multiple SF-36 outcomes, but periprocedural MI and cranial-nerve palsy did not," Dr. Stolker said.
The greatest impact on health status occurred in patients with major periprocedural strokes, who on average showed significant reductions in all eight subscales of the SF-36 at 1-year follow-up. Patients with minor periprocedural strokes had, on average, significant 1-year drops in "three or four" SF-36 subscales, compared with CREST patients who did not have strokes, he said in an interview.
CREST randomized more than 2,500 patients with symptomatic or substantial asymptomatic carotid disease to either endarterectomy or carotid stenting during 2000-2008. The study’s primary end point results – the periprocedural rate of stroke, MI, or death plus the 4-year rate of ipsilateral stroke – showed no significant between the two study arms, results reported last year (N. Engl. J. Med. 2010;363:11-23). Dr. Stolker’s new report focused on a prespecified analysis of health status outcomes.
In addition to the eight subscales of the SF-36, the researchers also measured changes in health status by six parameters measures by modified Likert scales: difficulty walking, difficulty eating and swallowing, difficulty driving, headaches, neck pain, and leg pain.
The new analysis showed that at 2 weeks after the interventions, patients who had undergone carotid stenting had, on average, significantly better health-status scores for five of the eight SF-36 subscales. But at 4 weeks after treatment, this fell to significantly better scores for stenting in three subscales: physical function, social function, and role physical. One year after the intervention, both the stented and open surgery arms showed, on average, essentially identical scores for all eight subscales.
The six additional parameters scored on a modified Likert scale showed a roughly similar pattern. After 2 weeks, the stented patients had significantly better scores for difficulty eating and swallowing, difficulty driving, headache, and neck pain, while the endarterectomy patients had a significant edge for difficulty walking and leg pain. These between-group differences began diminishing at 4 weeks and, at 1 year after the intervention, neither procedure had a significant difference for any of the six measures.
CREST was primarily funded by the National Institutes of Health. It also received supplemental support from Abbott Vascular Solutions, the company that markets the carotid stent and embolic protection device used in the study. Dr. Stolker said that he has been on the speakers bureau of AstraZeneca and Pfizer.
LOS ANGELES – Carotid stenting and carotid endarterectomy led to very similar health status outcomes a year after surgery, according to the quality-of-life analysis of the CREST trial.
Although patients with carotid artery stenosis randomized to the stenting arm of the study generally had better health status measures at 2 and 4 weeks following their intervention, by 1 year "all between-group differences had entirely resolved" when compared with the patients randomized to carotid endarterectomy, Dr. Joshua M. Stolker said at the International Stroke Conference.
The two treatment alternatives tested in the Carotid Revascularization Endarterectomy vs Stenting Trial (CREST) led to nearly identical long-term outcomes for quality-of-life despite an excess of strokes in the carotid stenting arm, and despite the finding in a new, exploratory analysis of health status outcomes that strokes produced a markedly larger decrement in health status than did myocardial infarctions or cranial nerve palsy. The worse outcomes with stroke probably did not affect the overall outcome of the stented patients because the number of strokes – and especially the number of major strokes – was relatively small in CREST.
Because of "the small absolute difference in stroke rates" between the stented and open-surgery patients and the fact that "most of the difference was in minor strokes, "Overall, there was no difference for the whole population despite the impact of stroke," said Dr. Stolker, a cardiologist at Saint Louis University.
In CREST, stented patients had a 1.8% higher rate of all strokes, compared with the endarterectomy patients, including a 0.5% excess rate of major strokes.
Stroke patients showed statistically significant impairments, compared with the patients who did not have a stroke, in seven of the eight health status outcome subscales measured using the Short Form (SF)-36: physical function, role physical, vitality, pain, social function, role emotional, and mental health. In contrast, after 1 year patients in CREST who had an MI following their surgery had a deficit only in the measure of general health, compared with the CREST patients who did not have an MI. And patients who developed cranial-nerve palsy after their surgery had no 1-year deficits for any health-status measure, compared with the patients who did not develop cranial-nerve palsy.
These results "confirmed what a lot of us already suspected, that periprocedural stroke had a significant impact on 1-year health status across multiple SF-36 outcomes, but periprocedural MI and cranial-nerve palsy did not," Dr. Stolker said.
The greatest impact on health status occurred in patients with major periprocedural strokes, who on average showed significant reductions in all eight subscales of the SF-36 at 1-year follow-up. Patients with minor periprocedural strokes had, on average, significant 1-year drops in "three or four" SF-36 subscales, compared with CREST patients who did not have strokes, he said in an interview.
CREST randomized more than 2,500 patients with symptomatic or substantial asymptomatic carotid disease to either endarterectomy or carotid stenting during 2000-2008. The study’s primary end point results – the periprocedural rate of stroke, MI, or death plus the 4-year rate of ipsilateral stroke – showed no significant between the two study arms, results reported last year (N. Engl. J. Med. 2010;363:11-23). Dr. Stolker’s new report focused on a prespecified analysis of health status outcomes.
In addition to the eight subscales of the SF-36, the researchers also measured changes in health status by six parameters measures by modified Likert scales: difficulty walking, difficulty eating and swallowing, difficulty driving, headaches, neck pain, and leg pain.
The new analysis showed that at 2 weeks after the interventions, patients who had undergone carotid stenting had, on average, significantly better health-status scores for five of the eight SF-36 subscales. But at 4 weeks after treatment, this fell to significantly better scores for stenting in three subscales: physical function, social function, and role physical. One year after the intervention, both the stented and open surgery arms showed, on average, essentially identical scores for all eight subscales.
The six additional parameters scored on a modified Likert scale showed a roughly similar pattern. After 2 weeks, the stented patients had significantly better scores for difficulty eating and swallowing, difficulty driving, headache, and neck pain, while the endarterectomy patients had a significant edge for difficulty walking and leg pain. These between-group differences began diminishing at 4 weeks and, at 1 year after the intervention, neither procedure had a significant difference for any of the six measures.
CREST was primarily funded by the National Institutes of Health. It also received supplemental support from Abbott Vascular Solutions, the company that markets the carotid stent and embolic protection device used in the study. Dr. Stolker said that he has been on the speakers bureau of AstraZeneca and Pfizer.
FROM THE INTERNATIONAL STROKE CONFERENCE
Carotid Stenting, Endarterectomy Yield Similar Quality-of-Life Outcomes
LOS ANGELES – Carotid stenting and carotid endarterectomy led to very similar health status outcomes a year after surgery, according to the quality-of-life analysis of the CREST trial.
Although patients with carotid artery stenosis randomized to the stenting arm of the study generally had better health status measures at 2 and 4 weeks following their intervention, by 1 year "all between-group differences had entirely resolved" when compared with the patients randomized to carotid endarterectomy, Dr. Joshua M. Stolker said at the International Stroke Conference.
The two treatment alternatives tested in the Carotid Revascularization Endarterectomy vs Stenting Trial (CREST) led to nearly identical long-term outcomes for quality-of-life despite an excess of strokes in the carotid stenting arm, and despite the finding in a new, exploratory analysis of health status outcomes that strokes produced a markedly larger decrement in health status than did myocardial infarctions or cranial nerve palsy. The worse outcomes with stroke probably did not affect the overall outcome of the stented patients because the number of strokes – and especially the number of major strokes – was relatively small in CREST.
Because of "the small absolute difference in stroke rates" between the stented and open-surgery patients and the fact that "most of the difference was in minor strokes, "Overall, there was no difference for the whole population despite the impact of stroke," said Dr. Stolker, a cardiologist at Saint Louis University.
In CREST, stented patients had a 1.8% higher rate of all strokes, compared with the endarterectomy patients, including a 0.5% excess rate of major strokes.
Stroke patients showed statistically significant impairments, compared with the patients who did not have a stroke, in seven of the eight health status outcome subscales measured using the Short Form (SF)-36: physical function, role physical, vitality, pain, social function, role emotional, and mental health. In contrast, after 1 year patients in CREST who had an MI following their surgery had a deficit only in the measure of general health, compared with the CREST patients who did not have an MI. And patients who developed cranial-nerve palsy after their surgery had no 1-year deficits for any health-status measure, compared with the patients who did not develop cranial-nerve palsy.
These results "confirmed what a lot of us already suspected, that periprocedural stroke had a significant impact on 1-year health status across multiple SF-36 outcomes, but periprocedural MI and cranial-nerve palsy did not," Dr. Stolker said.
The greatest impact on health status occurred in patients with major periprocedural strokes, who on average showed significant reductions in all eight subscales of the SF-36 at 1-year follow-up. Patients with minor periprocedural strokes had, on average, significant 1-year drops in "three or four" SF-36 subscales, compared with CREST patients who did not have strokes, he said in an interview.
CREST randomized more than 2,500 patients with symptomatic or substantial asymptomatic carotid disease to either endarterectomy or carotid stenting during 2000-2008. The study’s primary end point results – the periprocedural rate of stroke, MI, or death plus the 4-year rate of ipsilateral stroke – showed no significant between the two study arms, results reported last year (N. Engl. J. Med. 2010;363:11-23). Dr. Stolker’s new report focused on a prespecified analysis of health status outcomes.
In addition to the eight subscales of the SF-36, the researchers also measured changes in health status by six parameters measures by modified Likert scales: difficulty walking, difficulty eating and swallowing, difficulty driving, headaches, neck pain, and leg pain.
The new analysis showed that at 2 weeks after the interventions, patients who had undergone carotid stenting had, on average, significantly better health-status scores for five of the eight SF-36 subscales. But at 4 weeks after treatment, this fell to significantly better scores for stenting in three subscales: physical function, social function, and role physical. One year after the intervention, both the stented and open surgery arms showed, on average, essentially identical scores for all eight subscales.
The six additional parameters scored on a modified Likert scale showed a roughly similar pattern. After 2 weeks, the stented patients had significantly better scores for difficulty eating and swallowing, difficulty driving, headache, and neck pain, while the endarterectomy patients had a significant edge for difficulty walking and leg pain. These between-group differences began diminishing at 4 weeks and, at 1 year after the intervention, neither procedure had a significant difference for any of the six measures.
CREST was primarily funded by the National Institutes of Health. It also received supplemental support from Abbott Vascular Solutions, the company that markets the carotid stent and embolic protection device used in the study. Dr. Stolker said that he has been on the speakers bureau of AstraZeneca and Pfizer.
LOS ANGELES – Carotid stenting and carotid endarterectomy led to very similar health status outcomes a year after surgery, according to the quality-of-life analysis of the CREST trial.
Although patients with carotid artery stenosis randomized to the stenting arm of the study generally had better health status measures at 2 and 4 weeks following their intervention, by 1 year "all between-group differences had entirely resolved" when compared with the patients randomized to carotid endarterectomy, Dr. Joshua M. Stolker said at the International Stroke Conference.
The two treatment alternatives tested in the Carotid Revascularization Endarterectomy vs Stenting Trial (CREST) led to nearly identical long-term outcomes for quality-of-life despite an excess of strokes in the carotid stenting arm, and despite the finding in a new, exploratory analysis of health status outcomes that strokes produced a markedly larger decrement in health status than did myocardial infarctions or cranial nerve palsy. The worse outcomes with stroke probably did not affect the overall outcome of the stented patients because the number of strokes – and especially the number of major strokes – was relatively small in CREST.
Because of "the small absolute difference in stroke rates" between the stented and open-surgery patients and the fact that "most of the difference was in minor strokes, "Overall, there was no difference for the whole population despite the impact of stroke," said Dr. Stolker, a cardiologist at Saint Louis University.
In CREST, stented patients had a 1.8% higher rate of all strokes, compared with the endarterectomy patients, including a 0.5% excess rate of major strokes.
Stroke patients showed statistically significant impairments, compared with the patients who did not have a stroke, in seven of the eight health status outcome subscales measured using the Short Form (SF)-36: physical function, role physical, vitality, pain, social function, role emotional, and mental health. In contrast, after 1 year patients in CREST who had an MI following their surgery had a deficit only in the measure of general health, compared with the CREST patients who did not have an MI. And patients who developed cranial-nerve palsy after their surgery had no 1-year deficits for any health-status measure, compared with the patients who did not develop cranial-nerve palsy.
These results "confirmed what a lot of us already suspected, that periprocedural stroke had a significant impact on 1-year health status across multiple SF-36 outcomes, but periprocedural MI and cranial-nerve palsy did not," Dr. Stolker said.
The greatest impact on health status occurred in patients with major periprocedural strokes, who on average showed significant reductions in all eight subscales of the SF-36 at 1-year follow-up. Patients with minor periprocedural strokes had, on average, significant 1-year drops in "three or four" SF-36 subscales, compared with CREST patients who did not have strokes, he said in an interview.
CREST randomized more than 2,500 patients with symptomatic or substantial asymptomatic carotid disease to either endarterectomy or carotid stenting during 2000-2008. The study’s primary end point results – the periprocedural rate of stroke, MI, or death plus the 4-year rate of ipsilateral stroke – showed no significant between the two study arms, results reported last year (N. Engl. J. Med. 2010;363:11-23). Dr. Stolker’s new report focused on a prespecified analysis of health status outcomes.
In addition to the eight subscales of the SF-36, the researchers also measured changes in health status by six parameters measures by modified Likert scales: difficulty walking, difficulty eating and swallowing, difficulty driving, headaches, neck pain, and leg pain.
The new analysis showed that at 2 weeks after the interventions, patients who had undergone carotid stenting had, on average, significantly better health-status scores for five of the eight SF-36 subscales. But at 4 weeks after treatment, this fell to significantly better scores for stenting in three subscales: physical function, social function, and role physical. One year after the intervention, both the stented and open surgery arms showed, on average, essentially identical scores for all eight subscales.
The six additional parameters scored on a modified Likert scale showed a roughly similar pattern. After 2 weeks, the stented patients had significantly better scores for difficulty eating and swallowing, difficulty driving, headache, and neck pain, while the endarterectomy patients had a significant edge for difficulty walking and leg pain. These between-group differences began diminishing at 4 weeks and, at 1 year after the intervention, neither procedure had a significant difference for any of the six measures.
CREST was primarily funded by the National Institutes of Health. It also received supplemental support from Abbott Vascular Solutions, the company that markets the carotid stent and embolic protection device used in the study. Dr. Stolker said that he has been on the speakers bureau of AstraZeneca and Pfizer.
LOS ANGELES – Carotid stenting and carotid endarterectomy led to very similar health status outcomes a year after surgery, according to the quality-of-life analysis of the CREST trial.
Although patients with carotid artery stenosis randomized to the stenting arm of the study generally had better health status measures at 2 and 4 weeks following their intervention, by 1 year "all between-group differences had entirely resolved" when compared with the patients randomized to carotid endarterectomy, Dr. Joshua M. Stolker said at the International Stroke Conference.
The two treatment alternatives tested in the Carotid Revascularization Endarterectomy vs Stenting Trial (CREST) led to nearly identical long-term outcomes for quality-of-life despite an excess of strokes in the carotid stenting arm, and despite the finding in a new, exploratory analysis of health status outcomes that strokes produced a markedly larger decrement in health status than did myocardial infarctions or cranial nerve palsy. The worse outcomes with stroke probably did not affect the overall outcome of the stented patients because the number of strokes – and especially the number of major strokes – was relatively small in CREST.
Because of "the small absolute difference in stroke rates" between the stented and open-surgery patients and the fact that "most of the difference was in minor strokes, "Overall, there was no difference for the whole population despite the impact of stroke," said Dr. Stolker, a cardiologist at Saint Louis University.
In CREST, stented patients had a 1.8% higher rate of all strokes, compared with the endarterectomy patients, including a 0.5% excess rate of major strokes.
Stroke patients showed statistically significant impairments, compared with the patients who did not have a stroke, in seven of the eight health status outcome subscales measured using the Short Form (SF)-36: physical function, role physical, vitality, pain, social function, role emotional, and mental health. In contrast, after 1 year patients in CREST who had an MI following their surgery had a deficit only in the measure of general health, compared with the CREST patients who did not have an MI. And patients who developed cranial-nerve palsy after their surgery had no 1-year deficits for any health-status measure, compared with the patients who did not develop cranial-nerve palsy.
These results "confirmed what a lot of us already suspected, that periprocedural stroke had a significant impact on 1-year health status across multiple SF-36 outcomes, but periprocedural MI and cranial-nerve palsy did not," Dr. Stolker said.
The greatest impact on health status occurred in patients with major periprocedural strokes, who on average showed significant reductions in all eight subscales of the SF-36 at 1-year follow-up. Patients with minor periprocedural strokes had, on average, significant 1-year drops in "three or four" SF-36 subscales, compared with CREST patients who did not have strokes, he said in an interview.
CREST randomized more than 2,500 patients with symptomatic or substantial asymptomatic carotid disease to either endarterectomy or carotid stenting during 2000-2008. The study’s primary end point results – the periprocedural rate of stroke, MI, or death plus the 4-year rate of ipsilateral stroke – showed no significant between the two study arms, results reported last year (N. Engl. J. Med. 2010;363:11-23). Dr. Stolker’s new report focused on a prespecified analysis of health status outcomes.
In addition to the eight subscales of the SF-36, the researchers also measured changes in health status by six parameters measures by modified Likert scales: difficulty walking, difficulty eating and swallowing, difficulty driving, headaches, neck pain, and leg pain.
The new analysis showed that at 2 weeks after the interventions, patients who had undergone carotid stenting had, on average, significantly better health-status scores for five of the eight SF-36 subscales. But at 4 weeks after treatment, this fell to significantly better scores for stenting in three subscales: physical function, social function, and role physical. One year after the intervention, both the stented and open surgery arms showed, on average, essentially identical scores for all eight subscales.
The six additional parameters scored on a modified Likert scale showed a roughly similar pattern. After 2 weeks, the stented patients had significantly better scores for difficulty eating and swallowing, difficulty driving, headache, and neck pain, while the endarterectomy patients had a significant edge for difficulty walking and leg pain. These between-group differences began diminishing at 4 weeks and, at 1 year after the intervention, neither procedure had a significant difference for any of the six measures.
CREST was primarily funded by the National Institutes of Health. It also received supplemental support from Abbott Vascular Solutions, the company that markets the carotid stent and embolic protection device used in the study. Dr. Stolker said that he has been on the speakers bureau of AstraZeneca and Pfizer.
FROM THE INTERNATIONAL STROKE CONFERENCE
Major Finding: One year after randomization to carotid artery stenting or endarterectomy, patients in each treatment arm had on average very similar health status outcomes.
Data Source: CREST, a randomized, multicenter trial with 2,522 patients.
Disclosures: CREST was primarily funded by the National Institutes of Health. It also received supplemental support from Abbott Vascular Solutions, the company that markets the carotid stent and embolic protection device used in the study. Dr. Stolker said that he has been on the speakers bureau of AstraZeneca and Pfizer.
Percutaneous Hepatic Perfusion Boosts Melanoma Response
MIAMI BEACH – A novel percutaneous system for isolating hepatic blood flow allowed clinicians to treat hepatic melanoma metastases with a high concentration of melphalan and then filter out the drug to minimize its entry into the systemic circulation in a study of 93 patients.
This method for percutaneous hepatic perfusion (PHP) produced a more than fourfold increase in the average duration of hepatic progression-free survival in PHP patients compared with control patients in the phase III, randomized controlled trial, Dr. Charles W. Nutting said at ISET 2011, an international symposium on endovascular therapy.
Based on these results, the company that developed the percutaneous catheter system, Delcath Systems, filed a new drug application with the Food and Drug Administration.
"High-dose melphalan, delivered via intra-arterial administration with subsequent hepatic hemofiltration, is effective against hepatic metastases from ocular and cutaneous melanoma and provides improved disease control when compared with standard treatment regimens," said Dr. Nutting, an interventional radiologist at Swedish Medical Center in Denver.
"The FDA told us what result they would want to see" to approve PHP – an average duration of hepatic progression-free survival of 7.7 months in PHP patients and an average 4.0-month survival in control patients, Dr. Nutting said in an interview.
"The results exceeded that," he noted, with an average hepatic progression-free survival of 245 days (8.2 months) in the patients randomized to initial PHP and an average of 49 days (1.6 months) in control patients who received best alternative care. The hazard ratio for the PHP patients compared with the controls for this primary end point was 0.301 (P =.0001.)
PHP is "now one of the primary treatments" for inoperable melanoma liver metastases in patients whose most significant disease is in the liver, he added.
The clear success of PHP also suggested that the method might also help patients with other types of liver tumors, including primary cancers and other malignancies that often metastasize to the liver, such as colon cancer, Dr. Nutting said.
The researchers who developed PHP envisioned it as a potentially easier-to-tolerate variation on isolated hepatic perfusion, a method first used more than a decade ago that involved an open surgical procedure to isolate the hepatic circulation (J. Am. Coll. Surg. 2000;191:519-30). It was so invasive, however, that each patient could tolerate only a single treatment, Dr. Nutting said.
The percutaneous approach, developed as a more tolerable alternative, was applied serially one to six times to each patient in the PHP arm of the current trial with a 4-week interval between treatments.
The procedure involves inserting a double-balloon catheter from the patient’s groin through the hepatic artery and into the inferior vena cava. The superior balloon is then inflated and brought down to occlude the upper hepatic veins, while the second balloon is inflated below the hepatic veins to isolate hepatic venous return. A continuous infusion of melphalan enters the patient via a second catheter into the hepatic artery. After the drug distributes through the liver, the first catheter sucks out the hepatic venous blood (which is blocked by the two balloons from entering the systemic venous flow) via a set of holes and shunts it to an externally placed filter at a rate of 500 mL/min. After the blood is cleansed of the drug, it is returned to the patient.
The total melphalan dose delivered is 3.0 mg/kg ideal body weight of the patient, with the total dose diluted in 500 mL of fluid. The system takes 30 minutes to pump the entire dose into the patient, after which the balloons isolating the hepatic venous system and the filtration mechanism remain in place for another 30 minutes to continue to cleanse the drug from the patient’s liver. The system cuts systemic exposure to the melphalan by 80% compared with the intrahepatic dose delivered, Dr. Nutting said.
The study enrolled 44 patients into the PHP arm and 49 into the control arm at 12 U.S. centers. All patients had metastatic melanoma that primarily affected the liver and was judged too extensive for surgical removal. Patients had a median of 20 hepatic metastases (range, 4-100). In 88% of patients the primary tumor was ocular melanoma, and 12% had cutaneous melanoma. Their average age was 55 years.
Despite the high melphalan dose used, the 40 PHP patients included in the safety analysis had "minimal toxicity that was well within acceptable limits for the doses of medication we gave," he said.
During the 116 total treatments these patients received, grade 3 or 4 neutropenia occurred after 61% of treatments, thrombocytopenia after 74%, and anemia after 47%. Grade 5 neutropenia occurred following two treatments, but these episodes were usually transient and manageable. A total of three patients in the PHP group died, two from neutropenia sepsis and one from hepatic failure.
In a secondary efficacy analysis, no patient in either treatment arm had a complete response. The incidence of patient responses was 34% in the PHP patients and 2% in the controls. The combined rate of partial response or stable disease reached 86% in the PHP-treated patients and 28% in the control patients.
The trial was sponsored in part by Delcath, the company developing the PHP system. Dr. Notting said that he has received research support from, and has spoken on behalf of, Delcath.
MIAMI BEACH – A novel percutaneous system for isolating hepatic blood flow allowed clinicians to treat hepatic melanoma metastases with a high concentration of melphalan and then filter out the drug to minimize its entry into the systemic circulation in a study of 93 patients.
This method for percutaneous hepatic perfusion (PHP) produced a more than fourfold increase in the average duration of hepatic progression-free survival in PHP patients compared with control patients in the phase III, randomized controlled trial, Dr. Charles W. Nutting said at ISET 2011, an international symposium on endovascular therapy.
Based on these results, the company that developed the percutaneous catheter system, Delcath Systems, filed a new drug application with the Food and Drug Administration.
"High-dose melphalan, delivered via intra-arterial administration with subsequent hepatic hemofiltration, is effective against hepatic metastases from ocular and cutaneous melanoma and provides improved disease control when compared with standard treatment regimens," said Dr. Nutting, an interventional radiologist at Swedish Medical Center in Denver.
"The FDA told us what result they would want to see" to approve PHP – an average duration of hepatic progression-free survival of 7.7 months in PHP patients and an average 4.0-month survival in control patients, Dr. Nutting said in an interview.
"The results exceeded that," he noted, with an average hepatic progression-free survival of 245 days (8.2 months) in the patients randomized to initial PHP and an average of 49 days (1.6 months) in control patients who received best alternative care. The hazard ratio for the PHP patients compared with the controls for this primary end point was 0.301 (P =.0001.)
PHP is "now one of the primary treatments" for inoperable melanoma liver metastases in patients whose most significant disease is in the liver, he added.
The clear success of PHP also suggested that the method might also help patients with other types of liver tumors, including primary cancers and other malignancies that often metastasize to the liver, such as colon cancer, Dr. Nutting said.
The researchers who developed PHP envisioned it as a potentially easier-to-tolerate variation on isolated hepatic perfusion, a method first used more than a decade ago that involved an open surgical procedure to isolate the hepatic circulation (J. Am. Coll. Surg. 2000;191:519-30). It was so invasive, however, that each patient could tolerate only a single treatment, Dr. Nutting said.
The percutaneous approach, developed as a more tolerable alternative, was applied serially one to six times to each patient in the PHP arm of the current trial with a 4-week interval between treatments.
The procedure involves inserting a double-balloon catheter from the patient’s groin through the hepatic artery and into the inferior vena cava. The superior balloon is then inflated and brought down to occlude the upper hepatic veins, while the second balloon is inflated below the hepatic veins to isolate hepatic venous return. A continuous infusion of melphalan enters the patient via a second catheter into the hepatic artery. After the drug distributes through the liver, the first catheter sucks out the hepatic venous blood (which is blocked by the two balloons from entering the systemic venous flow) via a set of holes and shunts it to an externally placed filter at a rate of 500 mL/min. After the blood is cleansed of the drug, it is returned to the patient.
The total melphalan dose delivered is 3.0 mg/kg ideal body weight of the patient, with the total dose diluted in 500 mL of fluid. The system takes 30 minutes to pump the entire dose into the patient, after which the balloons isolating the hepatic venous system and the filtration mechanism remain in place for another 30 minutes to continue to cleanse the drug from the patient’s liver. The system cuts systemic exposure to the melphalan by 80% compared with the intrahepatic dose delivered, Dr. Nutting said.
The study enrolled 44 patients into the PHP arm and 49 into the control arm at 12 U.S. centers. All patients had metastatic melanoma that primarily affected the liver and was judged too extensive for surgical removal. Patients had a median of 20 hepatic metastases (range, 4-100). In 88% of patients the primary tumor was ocular melanoma, and 12% had cutaneous melanoma. Their average age was 55 years.
Despite the high melphalan dose used, the 40 PHP patients included in the safety analysis had "minimal toxicity that was well within acceptable limits for the doses of medication we gave," he said.
During the 116 total treatments these patients received, grade 3 or 4 neutropenia occurred after 61% of treatments, thrombocytopenia after 74%, and anemia after 47%. Grade 5 neutropenia occurred following two treatments, but these episodes were usually transient and manageable. A total of three patients in the PHP group died, two from neutropenia sepsis and one from hepatic failure.
In a secondary efficacy analysis, no patient in either treatment arm had a complete response. The incidence of patient responses was 34% in the PHP patients and 2% in the controls. The combined rate of partial response or stable disease reached 86% in the PHP-treated patients and 28% in the control patients.
The trial was sponsored in part by Delcath, the company developing the PHP system. Dr. Notting said that he has received research support from, and has spoken on behalf of, Delcath.
MIAMI BEACH – A novel percutaneous system for isolating hepatic blood flow allowed clinicians to treat hepatic melanoma metastases with a high concentration of melphalan and then filter out the drug to minimize its entry into the systemic circulation in a study of 93 patients.
This method for percutaneous hepatic perfusion (PHP) produced a more than fourfold increase in the average duration of hepatic progression-free survival in PHP patients compared with control patients in the phase III, randomized controlled trial, Dr. Charles W. Nutting said at ISET 2011, an international symposium on endovascular therapy.
Based on these results, the company that developed the percutaneous catheter system, Delcath Systems, filed a new drug application with the Food and Drug Administration.
"High-dose melphalan, delivered via intra-arterial administration with subsequent hepatic hemofiltration, is effective against hepatic metastases from ocular and cutaneous melanoma and provides improved disease control when compared with standard treatment regimens," said Dr. Nutting, an interventional radiologist at Swedish Medical Center in Denver.
"The FDA told us what result they would want to see" to approve PHP – an average duration of hepatic progression-free survival of 7.7 months in PHP patients and an average 4.0-month survival in control patients, Dr. Nutting said in an interview.
"The results exceeded that," he noted, with an average hepatic progression-free survival of 245 days (8.2 months) in the patients randomized to initial PHP and an average of 49 days (1.6 months) in control patients who received best alternative care. The hazard ratio for the PHP patients compared with the controls for this primary end point was 0.301 (P =.0001.)
PHP is "now one of the primary treatments" for inoperable melanoma liver metastases in patients whose most significant disease is in the liver, he added.
The clear success of PHP also suggested that the method might also help patients with other types of liver tumors, including primary cancers and other malignancies that often metastasize to the liver, such as colon cancer, Dr. Nutting said.
The researchers who developed PHP envisioned it as a potentially easier-to-tolerate variation on isolated hepatic perfusion, a method first used more than a decade ago that involved an open surgical procedure to isolate the hepatic circulation (J. Am. Coll. Surg. 2000;191:519-30). It was so invasive, however, that each patient could tolerate only a single treatment, Dr. Nutting said.
The percutaneous approach, developed as a more tolerable alternative, was applied serially one to six times to each patient in the PHP arm of the current trial with a 4-week interval between treatments.
The procedure involves inserting a double-balloon catheter from the patient’s groin through the hepatic artery and into the inferior vena cava. The superior balloon is then inflated and brought down to occlude the upper hepatic veins, while the second balloon is inflated below the hepatic veins to isolate hepatic venous return. A continuous infusion of melphalan enters the patient via a second catheter into the hepatic artery. After the drug distributes through the liver, the first catheter sucks out the hepatic venous blood (which is blocked by the two balloons from entering the systemic venous flow) via a set of holes and shunts it to an externally placed filter at a rate of 500 mL/min. After the blood is cleansed of the drug, it is returned to the patient.
The total melphalan dose delivered is 3.0 mg/kg ideal body weight of the patient, with the total dose diluted in 500 mL of fluid. The system takes 30 minutes to pump the entire dose into the patient, after which the balloons isolating the hepatic venous system and the filtration mechanism remain in place for another 30 minutes to continue to cleanse the drug from the patient’s liver. The system cuts systemic exposure to the melphalan by 80% compared with the intrahepatic dose delivered, Dr. Nutting said.
The study enrolled 44 patients into the PHP arm and 49 into the control arm at 12 U.S. centers. All patients had metastatic melanoma that primarily affected the liver and was judged too extensive for surgical removal. Patients had a median of 20 hepatic metastases (range, 4-100). In 88% of patients the primary tumor was ocular melanoma, and 12% had cutaneous melanoma. Their average age was 55 years.
Despite the high melphalan dose used, the 40 PHP patients included in the safety analysis had "minimal toxicity that was well within acceptable limits for the doses of medication we gave," he said.
During the 116 total treatments these patients received, grade 3 or 4 neutropenia occurred after 61% of treatments, thrombocytopenia after 74%, and anemia after 47%. Grade 5 neutropenia occurred following two treatments, but these episodes were usually transient and manageable. A total of three patients in the PHP group died, two from neutropenia sepsis and one from hepatic failure.
In a secondary efficacy analysis, no patient in either treatment arm had a complete response. The incidence of patient responses was 34% in the PHP patients and 2% in the controls. The combined rate of partial response or stable disease reached 86% in the PHP-treated patients and 28% in the control patients.
The trial was sponsored in part by Delcath, the company developing the PHP system. Dr. Notting said that he has received research support from, and has spoken on behalf of, Delcath.
FROM ISET 2011, AN INTERNATIONAL SYMPOSIUM ON ENDOVASCULAR THERAPY
Major Finding: A percutaneous method for targeting melphalan to treat liver metastases while filtering it out of patients' blood before it reached their systemic circulation, led to an average hepatic progression-free survival of 8.2 months in the drug arm and 1.6 months in the standard-treatment control arm (P =.0001).
Data Source: Phase III trial with 44 patients randomized to percutaneous hepatic perfusion and 49 control patients who received standard treatment.
Disclosures: The trial was sponsored in part by Delcath, the company developing the PHP system. Dr. Notting said that he has received research support from, and has spoken on behalf of, Delcath.