User login
High ER expression + high RS spells high risk for late distant recurrence
The combination of a 21-gene recurrence score and quantitative estrogen receptor expression may help clinicians identify patients with estrogen receptor–positive breast cancer who are most likely to benefit from hormonal therapy extended beyond the customary 5 years, according to researchers.
Long-term follow-up of patients with recurrence score information from two National Surgical Adjuvant Breast and Bowel Project (NSABP) studies showed that recurrence score is strongly prognostic for late distant recurrences among patients with higher quantitative estrogen receptor expression (ESR1) levels, reported Dr. Norman Wolmark and colleagues from the NSABP Operations Centers and other institutions.
“These results suggest the value of extended tamoxifen therapy merits evaluation in patients with intermediate and high [recurrence score] with higher ESR1 expression at initial diagnosis,” they wrote (J Clin Oncol. 2016 May 23. doi: 10.1200/JCO.2015.62.6630).
The authors looked at data on patients with recurrence score information who were enrolled in the tamoxifen-only arm of the NSABP B-14 trial and in the B-28 trial, which compared four cycles of doxorubicin plus cyclophosphamide (AC) with four cycles of AC followed by four cycles of paclitaxel plus 5 years of tamoxifen for hormone receptor–positive patients. The recurrence score cohorts for the studies included 668 and 1,065 patients, respectively.
After a median follow-up of 11.2 years in B-28, recurrence score was associated with both early (0 to 5 years) and distant recurrence (P less than .001 and P = .02, respectively), regardless of ESR1 expression.
The investigators then used B-28 to establish a quantitative ESR1 cut-point to identify patients for whom recurrence scores predicted late distant recurrences. They determined it to be 9.1 normalized expression cycle threshold units (CT), and then validated this cutoff in B-14.
In the B-14 cohort, a recurrence score of less than 18 CT was associated with a distant recurrence rate in years 5 through 15 of 6.8%, a score from 18 to 30 was associated with a 11.2% rate, and a score of 31 or greater was associated with a 16.4% rate (P less than .01).
The results “confirm studies of other molecular assays in postmenopausal patients and extend these findings to premenopausal women: at-risk patients have varying rates of [late distant recurrence], and a low-risk group with less than a 5% risk of recurrence in the second [5 years] can be identified,” the researchers wrote.
The data also confirm and extend results of foundational gene expression studies showing that highly proliferative, high-ER-gene–expressing tumors are at the greatest risk of late relapse, they said.
However, additional studies are needed before clinicians can rely on genomic factors to predict which patients require only 5 years of hormonal therapy, they cautioned.
The study was supported by National Cancer Institute grants, Susan G. Komen for the Cure grants, Bristol-Myers Squibb, Pharmaceutical Research Institute, AstraZeneca, and Genomic Health. Several authors disclosed relationships with various pharmaceutical companies, and five are employed by Genomic Health.
The combination of a 21-gene recurrence score and quantitative estrogen receptor expression may help clinicians identify patients with estrogen receptor–positive breast cancer who are most likely to benefit from hormonal therapy extended beyond the customary 5 years, according to researchers.
Long-term follow-up of patients with recurrence score information from two National Surgical Adjuvant Breast and Bowel Project (NSABP) studies showed that recurrence score is strongly prognostic for late distant recurrences among patients with higher quantitative estrogen receptor expression (ESR1) levels, reported Dr. Norman Wolmark and colleagues from the NSABP Operations Centers and other institutions.
“These results suggest the value of extended tamoxifen therapy merits evaluation in patients with intermediate and high [recurrence score] with higher ESR1 expression at initial diagnosis,” they wrote (J Clin Oncol. 2016 May 23. doi: 10.1200/JCO.2015.62.6630).
The authors looked at data on patients with recurrence score information who were enrolled in the tamoxifen-only arm of the NSABP B-14 trial and in the B-28 trial, which compared four cycles of doxorubicin plus cyclophosphamide (AC) with four cycles of AC followed by four cycles of paclitaxel plus 5 years of tamoxifen for hormone receptor–positive patients. The recurrence score cohorts for the studies included 668 and 1,065 patients, respectively.
After a median follow-up of 11.2 years in B-28, recurrence score was associated with both early (0 to 5 years) and distant recurrence (P less than .001 and P = .02, respectively), regardless of ESR1 expression.
The investigators then used B-28 to establish a quantitative ESR1 cut-point to identify patients for whom recurrence scores predicted late distant recurrences. They determined it to be 9.1 normalized expression cycle threshold units (CT), and then validated this cutoff in B-14.
In the B-14 cohort, a recurrence score of less than 18 CT was associated with a distant recurrence rate in years 5 through 15 of 6.8%, a score from 18 to 30 was associated with a 11.2% rate, and a score of 31 or greater was associated with a 16.4% rate (P less than .01).
The results “confirm studies of other molecular assays in postmenopausal patients and extend these findings to premenopausal women: at-risk patients have varying rates of [late distant recurrence], and a low-risk group with less than a 5% risk of recurrence in the second [5 years] can be identified,” the researchers wrote.
The data also confirm and extend results of foundational gene expression studies showing that highly proliferative, high-ER-gene–expressing tumors are at the greatest risk of late relapse, they said.
However, additional studies are needed before clinicians can rely on genomic factors to predict which patients require only 5 years of hormonal therapy, they cautioned.
The study was supported by National Cancer Institute grants, Susan G. Komen for the Cure grants, Bristol-Myers Squibb, Pharmaceutical Research Institute, AstraZeneca, and Genomic Health. Several authors disclosed relationships with various pharmaceutical companies, and five are employed by Genomic Health.
The combination of a 21-gene recurrence score and quantitative estrogen receptor expression may help clinicians identify patients with estrogen receptor–positive breast cancer who are most likely to benefit from hormonal therapy extended beyond the customary 5 years, according to researchers.
Long-term follow-up of patients with recurrence score information from two National Surgical Adjuvant Breast and Bowel Project (NSABP) studies showed that recurrence score is strongly prognostic for late distant recurrences among patients with higher quantitative estrogen receptor expression (ESR1) levels, reported Dr. Norman Wolmark and colleagues from the NSABP Operations Centers and other institutions.
“These results suggest the value of extended tamoxifen therapy merits evaluation in patients with intermediate and high [recurrence score] with higher ESR1 expression at initial diagnosis,” they wrote (J Clin Oncol. 2016 May 23. doi: 10.1200/JCO.2015.62.6630).
The authors looked at data on patients with recurrence score information who were enrolled in the tamoxifen-only arm of the NSABP B-14 trial and in the B-28 trial, which compared four cycles of doxorubicin plus cyclophosphamide (AC) with four cycles of AC followed by four cycles of paclitaxel plus 5 years of tamoxifen for hormone receptor–positive patients. The recurrence score cohorts for the studies included 668 and 1,065 patients, respectively.
After a median follow-up of 11.2 years in B-28, recurrence score was associated with both early (0 to 5 years) and distant recurrence (P less than .001 and P = .02, respectively), regardless of ESR1 expression.
The investigators then used B-28 to establish a quantitative ESR1 cut-point to identify patients for whom recurrence scores predicted late distant recurrences. They determined it to be 9.1 normalized expression cycle threshold units (CT), and then validated this cutoff in B-14.
In the B-14 cohort, a recurrence score of less than 18 CT was associated with a distant recurrence rate in years 5 through 15 of 6.8%, a score from 18 to 30 was associated with a 11.2% rate, and a score of 31 or greater was associated with a 16.4% rate (P less than .01).
The results “confirm studies of other molecular assays in postmenopausal patients and extend these findings to premenopausal women: at-risk patients have varying rates of [late distant recurrence], and a low-risk group with less than a 5% risk of recurrence in the second [5 years] can be identified,” the researchers wrote.
The data also confirm and extend results of foundational gene expression studies showing that highly proliferative, high-ER-gene–expressing tumors are at the greatest risk of late relapse, they said.
However, additional studies are needed before clinicians can rely on genomic factors to predict which patients require only 5 years of hormonal therapy, they cautioned.
The study was supported by National Cancer Institute grants, Susan G. Komen for the Cure grants, Bristol-Myers Squibb, Pharmaceutical Research Institute, AstraZeneca, and Genomic Health. Several authors disclosed relationships with various pharmaceutical companies, and five are employed by Genomic Health.
FROM JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: A 21-gene recurrence score is strongly prognostic for late distant recurrence of breast cancer in patients with higher quantitative estrogen receptor expression (ESR1).
Major finding: Above an ESR1 expression cut point of 9.1 CT, a recurrence score of less than 18 CT was associated with a distant recurrence rate in years 5 through 15 of 6.8%, a score from 18 to 30 was associated with a 11.2% rate, and a score of 31 or greater was associated with a 16.4% rate (P less than .01).
Data source: Analyses of 668 patients in NSABP B-14, and 1065 in NSABP B-28.
Disclosures: The study was supported by National Cancer Institute grants, Susan G. Komen for the Cure grants, Bristol-Myers Squibb, Pharmaceutical Research Institute, AstraZeneca, and Genomic Health. Several authors disclosed relationships with various pharmaceutical companies, and five are employed by Genomic Health.
Novel combination delays progression of recurrent gynecologic tumors
A novel strategy of knocking down tumor vasculature and keeping it from getting back up significantly reduced the risk of tumor progression among women with recurrent ovarian, tubal or peritoneal cancers, investigators reported.
Among 107 women enrolled in a randomized phase II trial, the combination of the experimental vascular-disrupting agent fosbretabulin with the angiogenesis inhibitor bevacizumab (Avastin) was associated with a median progression-free survival (PFS, the primary endpoint) of 7.3 months, compared with 4.8 months for bevacizumab alone. The hazard ratio (HR) for the combination was 0.69 (P = .05), reported Dr. Bradley J. Monk of Creighton University, Omaha, Neb., and Dignity Health St. Joseph’s Hospital and Medical Center, Phoenix, and his colleagues.
“This randomized phase II trial comparing bevacizumab plus fosbretabulin to bevacizumab alone provides further evidence regarding the safety and efficacy of nonchemotherapy-containing antivascular combinations,” they wrote (J Clin Oncol. 2016 May 23. doi: 10.1200/JCO.2015.65.8153).
Combining a vascular-disrupting agent such as fosbretabulin with an agent targeted against vascular endothelial growth factor (VEGF) such as bevacizumab allows for more selective disruption of tumor vessels and inhibition of tumor neovascularization, while largely sparing cells with normal vasculature.
The regimen has the theoretical advantage of lower toxicity than more conventional combinations of an anti-VEGF agent and cytotoxic chemotherapy compounds. In a phase I trial of fosbretabulin and becavizumab, hypertension appeared to be the major dose-limiting toxicity, the authors noted.
In this phase II study, women with recurrent or persistent epithelial ovarian, tubal, or peritoneal carcinoma were randomly assigned to receive bevacizumab 15 mg/kg IV once every 3 weeks or the same dose and schedule of bevacizumab plus fosbretabulin 60 mg/m2 IV until disease progression or intolerable toxicity.
As noted before, the study met its primary endpoint of an improvement in PFS with the combination. Among patients with measurable disease, the overall response rate to the combination was 35.7%, compared with 28.2% for bevacizumab alone.
The only grade 3 or greater adverse event occurring more frequently with the combination than with single-agent bevacizumab was hypertension, which occurred in 35% vs. 20%, respectively. One patient in the combination arm had a grade 3 thromboembolic event and one patient in the bevacizumab-only arm had an intestinal fistula.
“On the basis of the PFS, overall response rate, and tolerability of these two antivascular therapies, further evaluation is warranted for this chemotherapy-free regimen,” Dr. Monk and his associates said.
The study was supported by grants from the National Cancer Institute. Dr. Monk and several coauthors disclosed consulting/advisory roles, speaker’s bureau participation, research funding, or travel reimbursements from multiple pharmaceutical companies.
A novel strategy of knocking down tumor vasculature and keeping it from getting back up significantly reduced the risk of tumor progression among women with recurrent ovarian, tubal or peritoneal cancers, investigators reported.
Among 107 women enrolled in a randomized phase II trial, the combination of the experimental vascular-disrupting agent fosbretabulin with the angiogenesis inhibitor bevacizumab (Avastin) was associated with a median progression-free survival (PFS, the primary endpoint) of 7.3 months, compared with 4.8 months for bevacizumab alone. The hazard ratio (HR) for the combination was 0.69 (P = .05), reported Dr. Bradley J. Monk of Creighton University, Omaha, Neb., and Dignity Health St. Joseph’s Hospital and Medical Center, Phoenix, and his colleagues.
“This randomized phase II trial comparing bevacizumab plus fosbretabulin to bevacizumab alone provides further evidence regarding the safety and efficacy of nonchemotherapy-containing antivascular combinations,” they wrote (J Clin Oncol. 2016 May 23. doi: 10.1200/JCO.2015.65.8153).
Combining a vascular-disrupting agent such as fosbretabulin with an agent targeted against vascular endothelial growth factor (VEGF) such as bevacizumab allows for more selective disruption of tumor vessels and inhibition of tumor neovascularization, while largely sparing cells with normal vasculature.
The regimen has the theoretical advantage of lower toxicity than more conventional combinations of an anti-VEGF agent and cytotoxic chemotherapy compounds. In a phase I trial of fosbretabulin and becavizumab, hypertension appeared to be the major dose-limiting toxicity, the authors noted.
In this phase II study, women with recurrent or persistent epithelial ovarian, tubal, or peritoneal carcinoma were randomly assigned to receive bevacizumab 15 mg/kg IV once every 3 weeks or the same dose and schedule of bevacizumab plus fosbretabulin 60 mg/m2 IV until disease progression or intolerable toxicity.
As noted before, the study met its primary endpoint of an improvement in PFS with the combination. Among patients with measurable disease, the overall response rate to the combination was 35.7%, compared with 28.2% for bevacizumab alone.
The only grade 3 or greater adverse event occurring more frequently with the combination than with single-agent bevacizumab was hypertension, which occurred in 35% vs. 20%, respectively. One patient in the combination arm had a grade 3 thromboembolic event and one patient in the bevacizumab-only arm had an intestinal fistula.
“On the basis of the PFS, overall response rate, and tolerability of these two antivascular therapies, further evaluation is warranted for this chemotherapy-free regimen,” Dr. Monk and his associates said.
The study was supported by grants from the National Cancer Institute. Dr. Monk and several coauthors disclosed consulting/advisory roles, speaker’s bureau participation, research funding, or travel reimbursements from multiple pharmaceutical companies.
A novel strategy of knocking down tumor vasculature and keeping it from getting back up significantly reduced the risk of tumor progression among women with recurrent ovarian, tubal or peritoneal cancers, investigators reported.
Among 107 women enrolled in a randomized phase II trial, the combination of the experimental vascular-disrupting agent fosbretabulin with the angiogenesis inhibitor bevacizumab (Avastin) was associated with a median progression-free survival (PFS, the primary endpoint) of 7.3 months, compared with 4.8 months for bevacizumab alone. The hazard ratio (HR) for the combination was 0.69 (P = .05), reported Dr. Bradley J. Monk of Creighton University, Omaha, Neb., and Dignity Health St. Joseph’s Hospital and Medical Center, Phoenix, and his colleagues.
“This randomized phase II trial comparing bevacizumab plus fosbretabulin to bevacizumab alone provides further evidence regarding the safety and efficacy of nonchemotherapy-containing antivascular combinations,” they wrote (J Clin Oncol. 2016 May 23. doi: 10.1200/JCO.2015.65.8153).
Combining a vascular-disrupting agent such as fosbretabulin with an agent targeted against vascular endothelial growth factor (VEGF) such as bevacizumab allows for more selective disruption of tumor vessels and inhibition of tumor neovascularization, while largely sparing cells with normal vasculature.
The regimen has the theoretical advantage of lower toxicity than more conventional combinations of an anti-VEGF agent and cytotoxic chemotherapy compounds. In a phase I trial of fosbretabulin and becavizumab, hypertension appeared to be the major dose-limiting toxicity, the authors noted.
In this phase II study, women with recurrent or persistent epithelial ovarian, tubal, or peritoneal carcinoma were randomly assigned to receive bevacizumab 15 mg/kg IV once every 3 weeks or the same dose and schedule of bevacizumab plus fosbretabulin 60 mg/m2 IV until disease progression or intolerable toxicity.
As noted before, the study met its primary endpoint of an improvement in PFS with the combination. Among patients with measurable disease, the overall response rate to the combination was 35.7%, compared with 28.2% for bevacizumab alone.
The only grade 3 or greater adverse event occurring more frequently with the combination than with single-agent bevacizumab was hypertension, which occurred in 35% vs. 20%, respectively. One patient in the combination arm had a grade 3 thromboembolic event and one patient in the bevacizumab-only arm had an intestinal fistula.
“On the basis of the PFS, overall response rate, and tolerability of these two antivascular therapies, further evaluation is warranted for this chemotherapy-free regimen,” Dr. Monk and his associates said.
The study was supported by grants from the National Cancer Institute. Dr. Monk and several coauthors disclosed consulting/advisory roles, speaker’s bureau participation, research funding, or travel reimbursements from multiple pharmaceutical companies.
FROM THE JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: The combination of a vascular disrupter and antiangiogenic agent improved progression-free survival in epithelial cancers of the female reproductive tract.
Major finding: Median PFS was 7.3 months with fosbretabulin plus bevacizumab vs. 4.8 months for bevacizumab alone.
Data source: Randomized phase II trial involving 107 women with recurrent or persistent epithelial ovarian, tubal, or peritoneal carcinomas.
Disclosures: The study was supported by grants from the National Cancer Institute. Dr. Monk and several coauthors disclosed consulting/advisory roles, speaker’s bureau participation, research funding, or travel reimbursements from multiple pharmaceutical companies.
Enzastaurin flops as maintenance in treated DLBCL
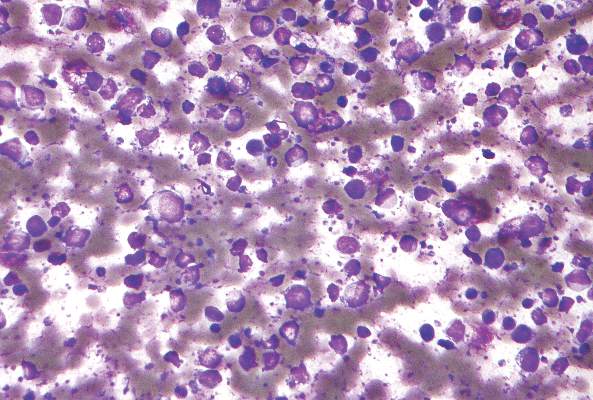
Maintenance therapy with enzastaurin, an experimental agent directed against B-cell malignancies, did not improve disease-free survival among patients with high-risk diffuse large B-cell lymphomas following complete responses to chemotherapy with rituximab.
In a randomized, double-blind trial, after a median follow-up of 48 months, the hazard ratio for disease-free survival with enzastaurin vs. placebo, the primary endpoint, was 0.92 (P = .541), reported Dr. Michael Crump of Princess Margaret Cancer Centre in Toronto, and colleagues.
“The risk of treatment failure, however defined, is likely to be different in the subpopulation of patients who achieve remission after that treatment. Furthermore, identifying the value of specific biomarkers in predicting therapeutic response to novel targeted agents may be necessary in guiding future trials within defined subgroups of patients with DLBCL,” they wrote in the study, published online May 23 in Journal of Clinical Oncology.
Enzastaurin is a selective inhibitor of the protein kinase C-beta isoform (PKC-beta) expressed in both normal and malignant B cells. It has been shown to decrease tumor proliferation and induced apoptosis in cancer cells, and has been shown to have activity against relapsed or refractory DLBCL, mantle cell lymphoma, and follicular lymphoma, the authors explained.
Dr. Crump and colleagues conducted a phase III study to determine whether enzastaurin could be effective as maintenance therapy in patients with DLBCL at high risk for relapse after having had complete responses to first-line therapy with rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone (R-CHOP).
They enrolled 758 patients with stage II bulky DLBCL or stage III-IV disease who had three or more International Prognostic Index risk factors at diagnosis, and who had achieved either a confirmed or unconfirmed complete response after six to eight cycles of R-CHOP.
The patients were randomly assigned on a 2:1 basis to receive either oral enzastaurin 500 mg daily or placebo for 3 years, or until disease progression or unacceptable toxicity,
As noted, there was no significant difference in DFS with the active drug vs. placebo. In addition, in correlative analyses looking for biomarkers of response by cell of origin (i.e., germinal-center or non–germinal-center B cell) or by PKC-beta protein expression, the authors found no significant associations with either DFS or overall survival.
Enzastaurin was generally safe, with minor and manageable adverse events. More patients in the enzastaurin arm had episodes of QTc prolongation, but these did not require discontinuation of the drug.
Dr. Crump and coauthors disclosed consulting, advising, research funding and other relationships with various companies, including Eli Lilly. Five coauthors are Lilly employees.
Maintenance therapy with enzastaurin, an experimental agent directed against B-cell malignancies, did not improve disease-free survival among patients with high-risk diffuse large B-cell lymphomas following complete responses to chemotherapy with rituximab.
In a randomized, double-blind trial, after a median follow-up of 48 months, the hazard ratio for disease-free survival with enzastaurin vs. placebo, the primary endpoint, was 0.92 (P = .541), reported Dr. Michael Crump of Princess Margaret Cancer Centre in Toronto, and colleagues.
“The risk of treatment failure, however defined, is likely to be different in the subpopulation of patients who achieve remission after that treatment. Furthermore, identifying the value of specific biomarkers in predicting therapeutic response to novel targeted agents may be necessary in guiding future trials within defined subgroups of patients with DLBCL,” they wrote in the study, published online May 23 in Journal of Clinical Oncology.
Enzastaurin is a selective inhibitor of the protein kinase C-beta isoform (PKC-beta) expressed in both normal and malignant B cells. It has been shown to decrease tumor proliferation and induced apoptosis in cancer cells, and has been shown to have activity against relapsed or refractory DLBCL, mantle cell lymphoma, and follicular lymphoma, the authors explained.
Dr. Crump and colleagues conducted a phase III study to determine whether enzastaurin could be effective as maintenance therapy in patients with DLBCL at high risk for relapse after having had complete responses to first-line therapy with rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone (R-CHOP).
They enrolled 758 patients with stage II bulky DLBCL or stage III-IV disease who had three or more International Prognostic Index risk factors at diagnosis, and who had achieved either a confirmed or unconfirmed complete response after six to eight cycles of R-CHOP.
The patients were randomly assigned on a 2:1 basis to receive either oral enzastaurin 500 mg daily or placebo for 3 years, or until disease progression or unacceptable toxicity,
As noted, there was no significant difference in DFS with the active drug vs. placebo. In addition, in correlative analyses looking for biomarkers of response by cell of origin (i.e., germinal-center or non–germinal-center B cell) or by PKC-beta protein expression, the authors found no significant associations with either DFS or overall survival.
Enzastaurin was generally safe, with minor and manageable adverse events. More patients in the enzastaurin arm had episodes of QTc prolongation, but these did not require discontinuation of the drug.
Dr. Crump and coauthors disclosed consulting, advising, research funding and other relationships with various companies, including Eli Lilly. Five coauthors are Lilly employees.
Maintenance therapy with enzastaurin, an experimental agent directed against B-cell malignancies, did not improve disease-free survival among patients with high-risk diffuse large B-cell lymphomas following complete responses to chemotherapy with rituximab.
In a randomized, double-blind trial, after a median follow-up of 48 months, the hazard ratio for disease-free survival with enzastaurin vs. placebo, the primary endpoint, was 0.92 (P = .541), reported Dr. Michael Crump of Princess Margaret Cancer Centre in Toronto, and colleagues.
“The risk of treatment failure, however defined, is likely to be different in the subpopulation of patients who achieve remission after that treatment. Furthermore, identifying the value of specific biomarkers in predicting therapeutic response to novel targeted agents may be necessary in guiding future trials within defined subgroups of patients with DLBCL,” they wrote in the study, published online May 23 in Journal of Clinical Oncology.
Enzastaurin is a selective inhibitor of the protein kinase C-beta isoform (PKC-beta) expressed in both normal and malignant B cells. It has been shown to decrease tumor proliferation and induced apoptosis in cancer cells, and has been shown to have activity against relapsed or refractory DLBCL, mantle cell lymphoma, and follicular lymphoma, the authors explained.
Dr. Crump and colleagues conducted a phase III study to determine whether enzastaurin could be effective as maintenance therapy in patients with DLBCL at high risk for relapse after having had complete responses to first-line therapy with rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone (R-CHOP).
They enrolled 758 patients with stage II bulky DLBCL or stage III-IV disease who had three or more International Prognostic Index risk factors at diagnosis, and who had achieved either a confirmed or unconfirmed complete response after six to eight cycles of R-CHOP.
The patients were randomly assigned on a 2:1 basis to receive either oral enzastaurin 500 mg daily or placebo for 3 years, or until disease progression or unacceptable toxicity,
As noted, there was no significant difference in DFS with the active drug vs. placebo. In addition, in correlative analyses looking for biomarkers of response by cell of origin (i.e., germinal-center or non–germinal-center B cell) or by PKC-beta protein expression, the authors found no significant associations with either DFS or overall survival.
Enzastaurin was generally safe, with minor and manageable adverse events. More patients in the enzastaurin arm had episodes of QTc prolongation, but these did not require discontinuation of the drug.
Dr. Crump and coauthors disclosed consulting, advising, research funding and other relationships with various companies, including Eli Lilly. Five coauthors are Lilly employees.
FROM JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: The experimental agent enzastaurin was no better than placebo as maintenance therapy in patients who had achieved a complete response to R-CHOP.
Major finding: At 48 months median follow-up, the hazard ratio for enzastaurin was 0.92 (P = ns).
Data source: Randomized, double-blind, placebo controlled trial of 758 patients with diffuse large B-cell lymphoma in complete remission after first-line therapy with R-CHOP.
Disclosures: Dr. Crump and coauthors disclosed consulting, advising, research funding and other relationships with various companies, including Eli Lilly. Five coauthors are Lilly employees.
Full course of AI keeps disease at bay longer
It’s common sense that adherence to a therapy with proven efficacy can result in better outcomes, and now there’s good scientific evidence to back it up.
A retrospective study of patients enrolled in a seminal clinical trial shows that postmenopausal women with early hormone receptor–positive breast cancer who stopped taking the aromatase inhibitor letrozole (Femara) before 5 years were up had an approximately 50% reduction in disease-free survival (DFS) compared with women who took the drug as prescribed, reported Dr. Jacquie H. Chirgwin of the Maroondah Breast Clinic in Ringwood East, Victoria, Australia, and colleagues (J Clin Oncol. 2016 May 23 doi: 10.1200/JCO.2015.63.8619).
“These results reinforce the importance of optimizing adherence by educating and supporting patients about the prognostic importance of adherence, the possible [adverse events] associated with switching treatment, and effective toxicity management,” they said.
The authors looked at data on 6,144 women who took part in the Breast International Group 1-98 (BIG 1-98) trial, which showed that 5 years of letrozole was associated with better overall survival (OS) than 5 years of tamoxifen, that sequential tamoxifen and letrozole were adequate for intermediate-risk patients, and that 5 years of either drug or a sequence were equally effective for low-risk patients.
To see whether shorter duration of therapy or less-than-ideal adherence to dosing had an adverse effect on outcomes, the investigators conducted regression analyses examining the relationship between DFS and both persistence (duration) of therapy, and compliance (adherence to dose and regularity of dosing).
They found that early cessation of letrozole was associated with a multivariable model hazard ratio (HR) for DFS of 1.45 (P = .01) and that a compliance score of less than 90% was associated with an HR of 1.61 (P = .02).
About 20% of women who took sequential therapy were nonpersistent, compared with 16.9% of women who took tamoxifen, and 17.6% of those who took letrozole.
In the large majority of cases (82.7%) adverse events were the primary reason for early discontinuation of therapy.
Patients who were older, smoked, had node-negative disease or had a prior thromboembolic event were less likely to be adherent, the investigators found.
It should be noted that all of the patients in this clinical trial had the medications provided to them and agreed to be participants in a randomized clinical treatment trial. Therefore, the rate of nonpersistence and noncompliance may underestimate the rates in the general population, where behavior, access, and financial factors may have a larger effect. In a prior study by our group, we found that higher copayment amounts were inversely associated with adherence to adjuvant AI therapy. Others have found a similar association with imatinib in patients with chronic myeloid leukemia. The introduction of generic aromatase inhibitors has also resulted in decreased discontinuation and increased adherence to hormonal therapy. These studies and others suggest that medication compliance may be improved if financial barriers are removed. Therefore, public policy efforts are needed to assure access to curative therapies.
Dr. Dawn L. Hershman of Herbert Irving Comprehensive Cancer Center and Columbia University Medical Center, New York, made this comments in an editorial accompanying the study by Chirgwin et al. (J Clin Oncol. 2016 May 23. doi: 10.1200/JCO.2016.67.7336).
It should be noted that all of the patients in this clinical trial had the medications provided to them and agreed to be participants in a randomized clinical treatment trial. Therefore, the rate of nonpersistence and noncompliance may underestimate the rates in the general population, where behavior, access, and financial factors may have a larger effect. In a prior study by our group, we found that higher copayment amounts were inversely associated with adherence to adjuvant AI therapy. Others have found a similar association with imatinib in patients with chronic myeloid leukemia. The introduction of generic aromatase inhibitors has also resulted in decreased discontinuation and increased adherence to hormonal therapy. These studies and others suggest that medication compliance may be improved if financial barriers are removed. Therefore, public policy efforts are needed to assure access to curative therapies.
Dr. Dawn L. Hershman of Herbert Irving Comprehensive Cancer Center and Columbia University Medical Center, New York, made this comments in an editorial accompanying the study by Chirgwin et al. (J Clin Oncol. 2016 May 23. doi: 10.1200/JCO.2016.67.7336).
It should be noted that all of the patients in this clinical trial had the medications provided to them and agreed to be participants in a randomized clinical treatment trial. Therefore, the rate of nonpersistence and noncompliance may underestimate the rates in the general population, where behavior, access, and financial factors may have a larger effect. In a prior study by our group, we found that higher copayment amounts were inversely associated with adherence to adjuvant AI therapy. Others have found a similar association with imatinib in patients with chronic myeloid leukemia. The introduction of generic aromatase inhibitors has also resulted in decreased discontinuation and increased adherence to hormonal therapy. These studies and others suggest that medication compliance may be improved if financial barriers are removed. Therefore, public policy efforts are needed to assure access to curative therapies.
Dr. Dawn L. Hershman of Herbert Irving Comprehensive Cancer Center and Columbia University Medical Center, New York, made this comments in an editorial accompanying the study by Chirgwin et al. (J Clin Oncol. 2016 May 23. doi: 10.1200/JCO.2016.67.7336).
It’s common sense that adherence to a therapy with proven efficacy can result in better outcomes, and now there’s good scientific evidence to back it up.
A retrospective study of patients enrolled in a seminal clinical trial shows that postmenopausal women with early hormone receptor–positive breast cancer who stopped taking the aromatase inhibitor letrozole (Femara) before 5 years were up had an approximately 50% reduction in disease-free survival (DFS) compared with women who took the drug as prescribed, reported Dr. Jacquie H. Chirgwin of the Maroondah Breast Clinic in Ringwood East, Victoria, Australia, and colleagues (J Clin Oncol. 2016 May 23 doi: 10.1200/JCO.2015.63.8619).
“These results reinforce the importance of optimizing adherence by educating and supporting patients about the prognostic importance of adherence, the possible [adverse events] associated with switching treatment, and effective toxicity management,” they said.
The authors looked at data on 6,144 women who took part in the Breast International Group 1-98 (BIG 1-98) trial, which showed that 5 years of letrozole was associated with better overall survival (OS) than 5 years of tamoxifen, that sequential tamoxifen and letrozole were adequate for intermediate-risk patients, and that 5 years of either drug or a sequence were equally effective for low-risk patients.
To see whether shorter duration of therapy or less-than-ideal adherence to dosing had an adverse effect on outcomes, the investigators conducted regression analyses examining the relationship between DFS and both persistence (duration) of therapy, and compliance (adherence to dose and regularity of dosing).
They found that early cessation of letrozole was associated with a multivariable model hazard ratio (HR) for DFS of 1.45 (P = .01) and that a compliance score of less than 90% was associated with an HR of 1.61 (P = .02).
About 20% of women who took sequential therapy were nonpersistent, compared with 16.9% of women who took tamoxifen, and 17.6% of those who took letrozole.
In the large majority of cases (82.7%) adverse events were the primary reason for early discontinuation of therapy.
Patients who were older, smoked, had node-negative disease or had a prior thromboembolic event were less likely to be adherent, the investigators found.
It’s common sense that adherence to a therapy with proven efficacy can result in better outcomes, and now there’s good scientific evidence to back it up.
A retrospective study of patients enrolled in a seminal clinical trial shows that postmenopausal women with early hormone receptor–positive breast cancer who stopped taking the aromatase inhibitor letrozole (Femara) before 5 years were up had an approximately 50% reduction in disease-free survival (DFS) compared with women who took the drug as prescribed, reported Dr. Jacquie H. Chirgwin of the Maroondah Breast Clinic in Ringwood East, Victoria, Australia, and colleagues (J Clin Oncol. 2016 May 23 doi: 10.1200/JCO.2015.63.8619).
“These results reinforce the importance of optimizing adherence by educating and supporting patients about the prognostic importance of adherence, the possible [adverse events] associated with switching treatment, and effective toxicity management,” they said.
The authors looked at data on 6,144 women who took part in the Breast International Group 1-98 (BIG 1-98) trial, which showed that 5 years of letrozole was associated with better overall survival (OS) than 5 years of tamoxifen, that sequential tamoxifen and letrozole were adequate for intermediate-risk patients, and that 5 years of either drug or a sequence were equally effective for low-risk patients.
To see whether shorter duration of therapy or less-than-ideal adherence to dosing had an adverse effect on outcomes, the investigators conducted regression analyses examining the relationship between DFS and both persistence (duration) of therapy, and compliance (adherence to dose and regularity of dosing).
They found that early cessation of letrozole was associated with a multivariable model hazard ratio (HR) for DFS of 1.45 (P = .01) and that a compliance score of less than 90% was associated with an HR of 1.61 (P = .02).
About 20% of women who took sequential therapy were nonpersistent, compared with 16.9% of women who took tamoxifen, and 17.6% of those who took letrozole.
In the large majority of cases (82.7%) adverse events were the primary reason for early discontinuation of therapy.
Patients who were older, smoked, had node-negative disease or had a prior thromboembolic event were less likely to be adherent, the investigators found.
FROM JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: Early cessation of aromatase inhibitor therapy is associated with reduced disease-free survival in postmenopausal women with early hormone receptor–positive breast cancer.
Major finding: Hazard ratios for worse disease-free survival with shorter duration therapy and poor compliance were 1.45 and 1.61, respectively.
Data source: Retrospective regression analysis of data on 6,144 women in the BIG 1-98 trial.
Disclosures: BIG 1-98 was supported by Novartis. Four coauthors disclosed receiving research funding or honoraria from the company. Dr. Hershman reported no relevant disclosures.
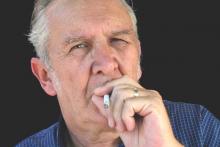
Smoking gun: DNA methylation in prostate cancer
More reason, if any is needed, to encourage patients to kick the habit comes from a study showing an association between cigarette smoking and tumor DNA methylation changes.
In a study of tumor tissue from men with prostate cancer (PCa) who underwent radical prostatectomy, smoking was associated with differential methylation across 40 genetic regions, and at least 10 of the regions significantly correlated with levels of messenger RNA (mRNA) expression in corresponding genes.
Men whose tumors had the highest levels of smoking-associated methylation were more likely to have higher Gleason grade tumors or regional vs. local stage disease, reported Dr. Irene M. Shui of the Fred Hutchinson Cancer Research Center in Seattle and her colleagues.
“[O]ur results provide support for the hypothesis that smoking-induced changes in DNA methylation may underlie the association of smoking with PCa recurrence and mortality,” they wrote (Cancer 2016 May 3. doi: 10.1002/cncr.30045).
To see whether DNA methylation could at least partly explain the association of smoking with increased PCa progression and mortality, the investigators looked at tumor methylation and long-term follow-up data on 523 patients, 469 of whom (90%) had matched tumor gene expression data available. In all, 43% of the men were never smokers, 47% were former smokers, and 10% were current smokers.
The investigators examined tumor methylation profiles by smoking status, with the goals of determining whether smoking-associated changes in methylation are linked to mRNA expression, and whether they are related to disease prognosis.
They found that 40 DNA methylation regions were associated with smoking, and that 10 of the regions were strongly correlated with mRNA expression. They then used these 10 regions to create a smoking-related methylation score.
As noted before, the score was associated with adverse outcomes, with men in the highest third having an odds ratio (OR) for disease recurrence of 2.29 (P = .0007), and an OR of 4.21 for death from prostate cancer (P = .004)
The associations between smoking-related methylation scores and worse outcomes were slightly less strong but still significant after adjustment for Gleason score and pathologic stage.
“Importantly, there is evidence that smoking-related methylation changes in blood may be reversible; men who quit smoking for longer periods of time have methylation profiles similar to those of never-smokers,” the authors wrote.
More reason, if any is needed, to encourage patients to kick the habit comes from a study showing an association between cigarette smoking and tumor DNA methylation changes.
In a study of tumor tissue from men with prostate cancer (PCa) who underwent radical prostatectomy, smoking was associated with differential methylation across 40 genetic regions, and at least 10 of the regions significantly correlated with levels of messenger RNA (mRNA) expression in corresponding genes.
Men whose tumors had the highest levels of smoking-associated methylation were more likely to have higher Gleason grade tumors or regional vs. local stage disease, reported Dr. Irene M. Shui of the Fred Hutchinson Cancer Research Center in Seattle and her colleagues.
“[O]ur results provide support for the hypothesis that smoking-induced changes in DNA methylation may underlie the association of smoking with PCa recurrence and mortality,” they wrote (Cancer 2016 May 3. doi: 10.1002/cncr.30045).
To see whether DNA methylation could at least partly explain the association of smoking with increased PCa progression and mortality, the investigators looked at tumor methylation and long-term follow-up data on 523 patients, 469 of whom (90%) had matched tumor gene expression data available. In all, 43% of the men were never smokers, 47% were former smokers, and 10% were current smokers.
The investigators examined tumor methylation profiles by smoking status, with the goals of determining whether smoking-associated changes in methylation are linked to mRNA expression, and whether they are related to disease prognosis.
They found that 40 DNA methylation regions were associated with smoking, and that 10 of the regions were strongly correlated with mRNA expression. They then used these 10 regions to create a smoking-related methylation score.
As noted before, the score was associated with adverse outcomes, with men in the highest third having an odds ratio (OR) for disease recurrence of 2.29 (P = .0007), and an OR of 4.21 for death from prostate cancer (P = .004)
The associations between smoking-related methylation scores and worse outcomes were slightly less strong but still significant after adjustment for Gleason score and pathologic stage.
“Importantly, there is evidence that smoking-related methylation changes in blood may be reversible; men who quit smoking for longer periods of time have methylation profiles similar to those of never-smokers,” the authors wrote.
More reason, if any is needed, to encourage patients to kick the habit comes from a study showing an association between cigarette smoking and tumor DNA methylation changes.
In a study of tumor tissue from men with prostate cancer (PCa) who underwent radical prostatectomy, smoking was associated with differential methylation across 40 genetic regions, and at least 10 of the regions significantly correlated with levels of messenger RNA (mRNA) expression in corresponding genes.
Men whose tumors had the highest levels of smoking-associated methylation were more likely to have higher Gleason grade tumors or regional vs. local stage disease, reported Dr. Irene M. Shui of the Fred Hutchinson Cancer Research Center in Seattle and her colleagues.
“[O]ur results provide support for the hypothesis that smoking-induced changes in DNA methylation may underlie the association of smoking with PCa recurrence and mortality,” they wrote (Cancer 2016 May 3. doi: 10.1002/cncr.30045).
To see whether DNA methylation could at least partly explain the association of smoking with increased PCa progression and mortality, the investigators looked at tumor methylation and long-term follow-up data on 523 patients, 469 of whom (90%) had matched tumor gene expression data available. In all, 43% of the men were never smokers, 47% were former smokers, and 10% were current smokers.
The investigators examined tumor methylation profiles by smoking status, with the goals of determining whether smoking-associated changes in methylation are linked to mRNA expression, and whether they are related to disease prognosis.
They found that 40 DNA methylation regions were associated with smoking, and that 10 of the regions were strongly correlated with mRNA expression. They then used these 10 regions to create a smoking-related methylation score.
As noted before, the score was associated with adverse outcomes, with men in the highest third having an odds ratio (OR) for disease recurrence of 2.29 (P = .0007), and an OR of 4.21 for death from prostate cancer (P = .004)
The associations between smoking-related methylation scores and worse outcomes were slightly less strong but still significant after adjustment for Gleason score and pathologic stage.
“Importantly, there is evidence that smoking-related methylation changes in blood may be reversible; men who quit smoking for longer periods of time have methylation profiles similar to those of never-smokers,” the authors wrote.
FROM CANCER
Key clinical point: This study demonstrates an association between smoking, DNA methylation, and potentially pathogenic genetic changes.
Major finding: Men with the highest smoking-related methylation scores were at increased risk for worse prostate cancer outcomes.
Data source: A retrospective study of tumor methylation and the association with outcomes in 523 men who underwent radical prostatectomy for adenocarcinoma of the prostate.
Disclosures: The study was supported by grants from the National Institutes of Health, Fred Hutchinson Cancer Research Center, and Prostate Cancer Foundation. The authors made no conflict of interest disclosures.
Aspirin lowers bile duct cancer risk
Regular aspirin use is associated with an approximately threefold reduction in risk for the three major subtypes of cholangiocarcinoma, results of a case-control study indicate.
In a study comparing patients with bile duct cancers with matched controls, aspirin use was associated with a 65% reduction in risk for intrahepatic cholangiocarcinoma (CCA), 66% reduction in risk for perihilar CCA, and 71% reduction in risk for distal CCA, reported Dr. Jonggi Choi and colleagues from the Mayo Medical School in Rochester, Minn.
“This is one of the largest hospital-based case-control studies evaluating risk factors for CCA in Western populations. We found that aspirin use had a significant inverse association with CCA development,” they wrote in Hepatology (2016. doi: 10.1002/hep.28529).
They also found that other disorders, including primary sclerosing cholangitis (PSC), non–PSC related cirrhosis, biliary tract diseases, hepatitis B infections, and diabetes, as well as smoking, were associated with varying magnitudes of risk for different CCA subtypes.
“This supports the hypothesis that the three CCA subtypes are distinct diseases and that each subtype thus has its own susceptibility to risk factors,” they wrote.
The investigators conducted a case-control study to look at various risk factors for CCA using data on all patients seen for CCA at the Mayo Clinic in Rochester from 2000 through 2014. Each case was matched by age, race, sex, and residence to two controls, chosen from among patients enrolled in the Mayo Clinic Biobank.
There were a total of 2,395 cases (1,169 with intrahepatic CCA, 995 with perihilar CCA, and 231 with distal CCA) and 4,769 controls. In all, 24.7% of cases and 44.6% of controls had used aspirin.
In multivariate logistic regression analysis controlling for demographic factors, obesity, hypertension, diabetes, stroke, coronary artery disease, peripheral vascular disease, atrial fibrillation, nonalcoholic fatty liver disease/nonalcoholic steatohepatitis, PSC, cirrhosis, irritable bowel disease, and smoking status, aspirin was significantly associated with a reduction in risk for all CCA subtypes with adjusted odds ratios (AOR) of 0.35 for intrahepatic CCA, 0.34 for perihilar cancer, and 0.29 for distal CCA (P for all less than .001).
In addition, they found that PSC was strongly associated with risk for perihilar CCA (AOR 453; P less than .001), intrahepatic CCA (AOR 93.4, P less than .001), and distal CCA (AOR 34.0, P = .002).
Cirrhosis not related to PSC was also associated with intrahepatic and perihilar CCA (AOR 13.8 and 14.1, respectively, P less than .001 for each), but not with distal CCA. Isolated inflammatory bowel disease without PSC was not associated with elevated risk of any CCA subtype.
Regular aspirin use is associated with an approximately threefold reduction in risk for the three major subtypes of cholangiocarcinoma, results of a case-control study indicate.
In a study comparing patients with bile duct cancers with matched controls, aspirin use was associated with a 65% reduction in risk for intrahepatic cholangiocarcinoma (CCA), 66% reduction in risk for perihilar CCA, and 71% reduction in risk for distal CCA, reported Dr. Jonggi Choi and colleagues from the Mayo Medical School in Rochester, Minn.
“This is one of the largest hospital-based case-control studies evaluating risk factors for CCA in Western populations. We found that aspirin use had a significant inverse association with CCA development,” they wrote in Hepatology (2016. doi: 10.1002/hep.28529).
They also found that other disorders, including primary sclerosing cholangitis (PSC), non–PSC related cirrhosis, biliary tract diseases, hepatitis B infections, and diabetes, as well as smoking, were associated with varying magnitudes of risk for different CCA subtypes.
“This supports the hypothesis that the three CCA subtypes are distinct diseases and that each subtype thus has its own susceptibility to risk factors,” they wrote.
The investigators conducted a case-control study to look at various risk factors for CCA using data on all patients seen for CCA at the Mayo Clinic in Rochester from 2000 through 2014. Each case was matched by age, race, sex, and residence to two controls, chosen from among patients enrolled in the Mayo Clinic Biobank.
There were a total of 2,395 cases (1,169 with intrahepatic CCA, 995 with perihilar CCA, and 231 with distal CCA) and 4,769 controls. In all, 24.7% of cases and 44.6% of controls had used aspirin.
In multivariate logistic regression analysis controlling for demographic factors, obesity, hypertension, diabetes, stroke, coronary artery disease, peripheral vascular disease, atrial fibrillation, nonalcoholic fatty liver disease/nonalcoholic steatohepatitis, PSC, cirrhosis, irritable bowel disease, and smoking status, aspirin was significantly associated with a reduction in risk for all CCA subtypes with adjusted odds ratios (AOR) of 0.35 for intrahepatic CCA, 0.34 for perihilar cancer, and 0.29 for distal CCA (P for all less than .001).
In addition, they found that PSC was strongly associated with risk for perihilar CCA (AOR 453; P less than .001), intrahepatic CCA (AOR 93.4, P less than .001), and distal CCA (AOR 34.0, P = .002).
Cirrhosis not related to PSC was also associated with intrahepatic and perihilar CCA (AOR 13.8 and 14.1, respectively, P less than .001 for each), but not with distal CCA. Isolated inflammatory bowel disease without PSC was not associated with elevated risk of any CCA subtype.
Regular aspirin use is associated with an approximately threefold reduction in risk for the three major subtypes of cholangiocarcinoma, results of a case-control study indicate.
In a study comparing patients with bile duct cancers with matched controls, aspirin use was associated with a 65% reduction in risk for intrahepatic cholangiocarcinoma (CCA), 66% reduction in risk for perihilar CCA, and 71% reduction in risk for distal CCA, reported Dr. Jonggi Choi and colleagues from the Mayo Medical School in Rochester, Minn.
“This is one of the largest hospital-based case-control studies evaluating risk factors for CCA in Western populations. We found that aspirin use had a significant inverse association with CCA development,” they wrote in Hepatology (2016. doi: 10.1002/hep.28529).
They also found that other disorders, including primary sclerosing cholangitis (PSC), non–PSC related cirrhosis, biliary tract diseases, hepatitis B infections, and diabetes, as well as smoking, were associated with varying magnitudes of risk for different CCA subtypes.
“This supports the hypothesis that the three CCA subtypes are distinct diseases and that each subtype thus has its own susceptibility to risk factors,” they wrote.
The investigators conducted a case-control study to look at various risk factors for CCA using data on all patients seen for CCA at the Mayo Clinic in Rochester from 2000 through 2014. Each case was matched by age, race, sex, and residence to two controls, chosen from among patients enrolled in the Mayo Clinic Biobank.
There were a total of 2,395 cases (1,169 with intrahepatic CCA, 995 with perihilar CCA, and 231 with distal CCA) and 4,769 controls. In all, 24.7% of cases and 44.6% of controls had used aspirin.
In multivariate logistic regression analysis controlling for demographic factors, obesity, hypertension, diabetes, stroke, coronary artery disease, peripheral vascular disease, atrial fibrillation, nonalcoholic fatty liver disease/nonalcoholic steatohepatitis, PSC, cirrhosis, irritable bowel disease, and smoking status, aspirin was significantly associated with a reduction in risk for all CCA subtypes with adjusted odds ratios (AOR) of 0.35 for intrahepatic CCA, 0.34 for perihilar cancer, and 0.29 for distal CCA (P for all less than .001).
In addition, they found that PSC was strongly associated with risk for perihilar CCA (AOR 453; P less than .001), intrahepatic CCA (AOR 93.4, P less than .001), and distal CCA (AOR 34.0, P = .002).
Cirrhosis not related to PSC was also associated with intrahepatic and perihilar CCA (AOR 13.8 and 14.1, respectively, P less than .001 for each), but not with distal CCA. Isolated inflammatory bowel disease without PSC was not associated with elevated risk of any CCA subtype.
FROM HEPATOLOGY
Key clinical point: Aspirin use is associated with an approximately threefold reduction in risk for the three cholangiocarcinoma (CCA) subtypes.
Major finding: Respective adjusted odds ratios for aspirin and intrahepatic, perihilar, and distal CCA were 0.35, 0.34, and 0.29.
Data source: Case-control study including 2,395 patients with CCA and 4,769 controls.
Disclosures: The study was supported by the National Institutes of Health, Mayo Clinic, Mayo Foundation, and the Cholangiocarcinoma Foundation. The authors reported no conflicts of interest.
Pembrolizumab shows activity against advanced TNBC
Early data from a phase Ib trial suggest that the immune checkpoint inhibitor pembrolizumab has modest activity against heavily pretreated metastatic triple-negative breast cancer (mTNBC).
Among 27 women with advanced triple-negative breast cancer (tumors lacking HER2, estrogen, and progesterone receptors) enrolled in a basket trial for cancers expressing the programmed death-1 ligand (PD-L1), the overall response rate to biweekly pembrolizumab (Keytruda) was 18.5%, reported Dr. Rita Nanda of the University of Chicago and colleagues (J Clin Oncol. 2016 May 2. doi: 10.1200/JCO.2015.64.8931).
“Overall, these results support further development of pembrolizumab for the treatment of mTNBC,” they said.
The TNBC study was included in the open-label, multicohort Keynote 012 study looking at the use of pembrolizumab in patients with advanced solid tumors expressing PD-L1.
The investigators evaluated PD-L1 status in 111 women with mTNBC, and identified 65 with tumors expressing the target, 32 of whom were enrolled in the trial.
The patients were treated with pembrolizumab 10 mg/kg intravenously every 2 weeks until unacceptable toxicity or disease progression, or at the discretion of the investigator. Clinically stable patients with first radiologic evidence of disease progression according to Response Evaluation Criteria for Solid Tumors (RECIST) could be continued on the checkpoint inhibitor until evidence of progression could be shown on a second scan 4 or more weeks later.
The patients received a median of five doses (range, 1-36). After a median follow-up of 10 months, the overall response rate among 27 patients evaluable for response was 18.5%, consisting of one complete response, four partial responses, and seven cases of stable disease. Thirteen patients had disease progression on pembrolizumab, and two patients discontinued therapy before the first scan.
The median time to response was 17.9 weeks; the median duration of response had not been reached by the time of data cut-off on March 25, 2015.
The adverse event profile was similar to that seen with pembrolizumab in the other study cohorts (gastric, urothelial, and head and neck cancers), with generally mild arthralgia, fatigue, myalgia, and nausea. However, there were five grade 3 or greater toxicities, including anemia, aseptic meningitis, lymphopenia, headache, and pyrexia, and one patient died from treatment-related disseminated intravascular coagulation accompanied by a grade 4 decrease in blood fibrinogen.
The investigators noted that the overall response rate seen in the TNBC cohort “makes it the first published report showing clinical activity for an immune checkpoint inhibitor in a heavily pretreated mTNBC population.”
Overall response rates for the other cohorts in the study were 21.4% for patients with head and neck cancers, 22.2% for those with gastric cancers, and 27.6% for those with urothelial cancers.
The study was sponsored by Merck & Co. Dr. Nanda and several coauthors disclosed consulting, research funding, and/or honoraria from the company, and four of the 12 coauthors are employees.
Early data from a phase Ib trial suggest that the immune checkpoint inhibitor pembrolizumab has modest activity against heavily pretreated metastatic triple-negative breast cancer (mTNBC).
Among 27 women with advanced triple-negative breast cancer (tumors lacking HER2, estrogen, and progesterone receptors) enrolled in a basket trial for cancers expressing the programmed death-1 ligand (PD-L1), the overall response rate to biweekly pembrolizumab (Keytruda) was 18.5%, reported Dr. Rita Nanda of the University of Chicago and colleagues (J Clin Oncol. 2016 May 2. doi: 10.1200/JCO.2015.64.8931).
“Overall, these results support further development of pembrolizumab for the treatment of mTNBC,” they said.
The TNBC study was included in the open-label, multicohort Keynote 012 study looking at the use of pembrolizumab in patients with advanced solid tumors expressing PD-L1.
The investigators evaluated PD-L1 status in 111 women with mTNBC, and identified 65 with tumors expressing the target, 32 of whom were enrolled in the trial.
The patients were treated with pembrolizumab 10 mg/kg intravenously every 2 weeks until unacceptable toxicity or disease progression, or at the discretion of the investigator. Clinically stable patients with first radiologic evidence of disease progression according to Response Evaluation Criteria for Solid Tumors (RECIST) could be continued on the checkpoint inhibitor until evidence of progression could be shown on a second scan 4 or more weeks later.
The patients received a median of five doses (range, 1-36). After a median follow-up of 10 months, the overall response rate among 27 patients evaluable for response was 18.5%, consisting of one complete response, four partial responses, and seven cases of stable disease. Thirteen patients had disease progression on pembrolizumab, and two patients discontinued therapy before the first scan.
The median time to response was 17.9 weeks; the median duration of response had not been reached by the time of data cut-off on March 25, 2015.
The adverse event profile was similar to that seen with pembrolizumab in the other study cohorts (gastric, urothelial, and head and neck cancers), with generally mild arthralgia, fatigue, myalgia, and nausea. However, there were five grade 3 or greater toxicities, including anemia, aseptic meningitis, lymphopenia, headache, and pyrexia, and one patient died from treatment-related disseminated intravascular coagulation accompanied by a grade 4 decrease in blood fibrinogen.
The investigators noted that the overall response rate seen in the TNBC cohort “makes it the first published report showing clinical activity for an immune checkpoint inhibitor in a heavily pretreated mTNBC population.”
Overall response rates for the other cohorts in the study were 21.4% for patients with head and neck cancers, 22.2% for those with gastric cancers, and 27.6% for those with urothelial cancers.
The study was sponsored by Merck & Co. Dr. Nanda and several coauthors disclosed consulting, research funding, and/or honoraria from the company, and four of the 12 coauthors are employees.
Early data from a phase Ib trial suggest that the immune checkpoint inhibitor pembrolizumab has modest activity against heavily pretreated metastatic triple-negative breast cancer (mTNBC).
Among 27 women with advanced triple-negative breast cancer (tumors lacking HER2, estrogen, and progesterone receptors) enrolled in a basket trial for cancers expressing the programmed death-1 ligand (PD-L1), the overall response rate to biweekly pembrolizumab (Keytruda) was 18.5%, reported Dr. Rita Nanda of the University of Chicago and colleagues (J Clin Oncol. 2016 May 2. doi: 10.1200/JCO.2015.64.8931).
“Overall, these results support further development of pembrolizumab for the treatment of mTNBC,” they said.
The TNBC study was included in the open-label, multicohort Keynote 012 study looking at the use of pembrolizumab in patients with advanced solid tumors expressing PD-L1.
The investigators evaluated PD-L1 status in 111 women with mTNBC, and identified 65 with tumors expressing the target, 32 of whom were enrolled in the trial.
The patients were treated with pembrolizumab 10 mg/kg intravenously every 2 weeks until unacceptable toxicity or disease progression, or at the discretion of the investigator. Clinically stable patients with first radiologic evidence of disease progression according to Response Evaluation Criteria for Solid Tumors (RECIST) could be continued on the checkpoint inhibitor until evidence of progression could be shown on a second scan 4 or more weeks later.
The patients received a median of five doses (range, 1-36). After a median follow-up of 10 months, the overall response rate among 27 patients evaluable for response was 18.5%, consisting of one complete response, four partial responses, and seven cases of stable disease. Thirteen patients had disease progression on pembrolizumab, and two patients discontinued therapy before the first scan.
The median time to response was 17.9 weeks; the median duration of response had not been reached by the time of data cut-off on March 25, 2015.
The adverse event profile was similar to that seen with pembrolizumab in the other study cohorts (gastric, urothelial, and head and neck cancers), with generally mild arthralgia, fatigue, myalgia, and nausea. However, there were five grade 3 or greater toxicities, including anemia, aseptic meningitis, lymphopenia, headache, and pyrexia, and one patient died from treatment-related disseminated intravascular coagulation accompanied by a grade 4 decrease in blood fibrinogen.
The investigators noted that the overall response rate seen in the TNBC cohort “makes it the first published report showing clinical activity for an immune checkpoint inhibitor in a heavily pretreated mTNBC population.”
Overall response rates for the other cohorts in the study were 21.4% for patients with head and neck cancers, 22.2% for those with gastric cancers, and 27.6% for those with urothelial cancers.
The study was sponsored by Merck & Co. Dr. Nanda and several coauthors disclosed consulting, research funding, and/or honoraria from the company, and four of the 12 coauthors are employees.
FROM JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: The immune checkpoint inhibitor pembrolizumab may be effective against metastatic triple-negative breast cancer.
Major finding: The overall response rate to pembrolizumab therapy among 27 women with metastatic TNBC evaluable for response was 18.5%.
Data source: Open-label, multicohort, phase Ib study in patients with solid tumors expressing PD-L1.
Disclosures: The study was sponsored by Merck & Co. Dr. Nanda and several coauthors disclosed consulting, research funding, and/or honoraria from the company, and four of the 12 coauthors are employees.
Physician, know thy patient before recommending treatment
Hollywood, FLA. – Although patients and physicians should always be partners in medical decision making, guiding patients into making medically sound choices may involve a lot of listening and empathy, often followed by a little friendly persuasion, suggests an expert in health care decision making,
“Even when you get to a situation where the clinical practice guideline would point toward shared decision making, we’ve got to do shared decision making right or the guideline just doesn’t do the work for us. We clinicians have to know how to partner with our patients to make decisions when their values matter,” said Dr. Peter A Ubel, professor of business, public policy, and medicine at Duke University, Durham, N.H.
Dr. Ubel discussed how to understand and use patient preferences in cancer treatment decisions at the annual conference of the National Comprehensive Cancer Network.
In the case of early-stage prostate cancer, for example, treatment options include surveillance or active treatment with surgery or radiation, but the risk/benefit trade-offs require careful discussion.
“The different approaches have different pros and cons: If you get active treatment, there’s a pretty good chance you’ll experience incontinence or erectile dysfunction, whereas if you undergo surveillance you won’t experience those as side effects of the surveillance strategy, but you will live with a cancer inside your body, the accompanying anxiety, and wondering every 6 months whether it has advanced,” Dr. Ubel said.
“The question is how do we go figure out which treatment is best for which patient?” he added.
What doctors say not always what patients hear
To examine how decisions are made, Dr. Ubel and his colleagues conducted a study in which patients scheduled for biopsy for suspicion of prostate cancer were approached at the time of their clinic visits and asked to participate in a study about prostate cancer decision making. Patients were given a booklet aimed at the seventh-grade reading level describing prostate cancer and its treatment, and were asked, once they had finished, what course of therapy they might pursue if the diagnosis turned out to be positive, and why. They also were asked if it was important to them to maintain natural sexual function.
The encounter between the patients and their urologists at the time of diagnosis were audio recorded, so that investigators could see whether physicians recommend specific treatments and why.
“One of the things that really jumped out in this study was just how much language, how much explanation urologists use to help patients understand their diagnosis,” Dr. Ubel said.
In one encounter, the urologist explained to the patient that 3 out of 12 biopsy cores had less than 30% cancer involvement, suggesting moderately low-risk disease, but then went on to talk about Gleason scores, tumor grades and patterns, and risk categories.
“When a patient just finds out he has prostate cancer, it’s a tough time to put a whole bunch of information in front of him for him to absorb and make a decision,” Dr. Ubel said. Patients need time to absorb the shock of a cancer diagnosis first – even a diagnosis of an early, easily treated cancer – and information overload may actually reduce their ability to comprehend their choices or retain the information, he added. The urologist in this scenario is making a very earnest effort to tell the patient that he doesn’t have the kind of cancer that’s ever going to kill him, or that it is highly unlikely to cause any problems for the next 10-15 years, and there is ample time to decide how to treat it.
“But the doctor kind of forgets that the patient doesn’t speak medicalese, and the doctor feels like you really have to give them thorough informed consent, after all. So you need to inform the heck out of patients with all of the medical detail you believe is necessary to understand the decision, instead of the translation of the medical detail into terms the patient can understand,” he said.
An important part of shared decision making, therefore, is to make sure that patients can understand their alternatives, but not to overwhelm them with detail, because they may give up and ask the physician, “What do you think I should do?” which can introduce physician bias that may not always lead to the right choice for that patient.
“I actually morally don’t recommend that. I think instead we should give the right amount of information at the right time so they can actually get engaged in the choice,” Dr. Ubel said.
Discussion informs choices
The investigators looked at how prediagnosis education materials and discussions with urologists shaped patient decisions about treatment choice. Patients were called before their appointments to ensure that they had read the booklet, and then just before the appointment were asked which way they were leaning if the diagnosis turned out to be positive.
The investigators found that of 44 patients who expressed a preference for active surveillance before the appointment, 55% actually went on to receive active treatment. Among 119 patients with no expressed preference for surveillance or active therapy, 46% went on to treatment, and of 118 expressing previsit preference only for active surveillance, 54% went on to receive it.
“The leaning that they had before seeing the doctor had no influence on what treatment they got,” Dr. Ubel said. Instead, physicians’ recommendations had a strong influence on treatment choice. Recommendations are an essential part of the discussion, “but I don’t think we often do them well,” he said.
Ask patients to think out loud about what they have read or have been told, and ask them to repeat in their own words what they heard the doctor say, Dr. Ubel suggested. It’s incumbent on the physician to try to understand the patient’s preferences, and say something like, “I’m the expert on medical facts, but you’re the expert on you,” or “What sounds good and bad to you about that treatment alternative?”
Finally, physicians need to make recommendations based on patient preferences, he said.
For example, in one recorded encounter, the physician asked the patient, “Are you the kind of person where the idea of just watching your PSA is that unsettling to you?” When the patient replied “Yeah, I think I would be,” the physician was able to make an informed recommendation, saying “then I don’t think you’d be a good candidate for surveillance.”
“This doctor did not just make a recommendation; he tried to find out something about the patient first, and that’s critical to giving good advice,” Dr. Ubel said.
Hollywood, FLA. – Although patients and physicians should always be partners in medical decision making, guiding patients into making medically sound choices may involve a lot of listening and empathy, often followed by a little friendly persuasion, suggests an expert in health care decision making,
“Even when you get to a situation where the clinical practice guideline would point toward shared decision making, we’ve got to do shared decision making right or the guideline just doesn’t do the work for us. We clinicians have to know how to partner with our patients to make decisions when their values matter,” said Dr. Peter A Ubel, professor of business, public policy, and medicine at Duke University, Durham, N.H.
Dr. Ubel discussed how to understand and use patient preferences in cancer treatment decisions at the annual conference of the National Comprehensive Cancer Network.
In the case of early-stage prostate cancer, for example, treatment options include surveillance or active treatment with surgery or radiation, but the risk/benefit trade-offs require careful discussion.
“The different approaches have different pros and cons: If you get active treatment, there’s a pretty good chance you’ll experience incontinence or erectile dysfunction, whereas if you undergo surveillance you won’t experience those as side effects of the surveillance strategy, but you will live with a cancer inside your body, the accompanying anxiety, and wondering every 6 months whether it has advanced,” Dr. Ubel said.
“The question is how do we go figure out which treatment is best for which patient?” he added.
What doctors say not always what patients hear
To examine how decisions are made, Dr. Ubel and his colleagues conducted a study in which patients scheduled for biopsy for suspicion of prostate cancer were approached at the time of their clinic visits and asked to participate in a study about prostate cancer decision making. Patients were given a booklet aimed at the seventh-grade reading level describing prostate cancer and its treatment, and were asked, once they had finished, what course of therapy they might pursue if the diagnosis turned out to be positive, and why. They also were asked if it was important to them to maintain natural sexual function.
The encounter between the patients and their urologists at the time of diagnosis were audio recorded, so that investigators could see whether physicians recommend specific treatments and why.
“One of the things that really jumped out in this study was just how much language, how much explanation urologists use to help patients understand their diagnosis,” Dr. Ubel said.
In one encounter, the urologist explained to the patient that 3 out of 12 biopsy cores had less than 30% cancer involvement, suggesting moderately low-risk disease, but then went on to talk about Gleason scores, tumor grades and patterns, and risk categories.
“When a patient just finds out he has prostate cancer, it’s a tough time to put a whole bunch of information in front of him for him to absorb and make a decision,” Dr. Ubel said. Patients need time to absorb the shock of a cancer diagnosis first – even a diagnosis of an early, easily treated cancer – and information overload may actually reduce their ability to comprehend their choices or retain the information, he added. The urologist in this scenario is making a very earnest effort to tell the patient that he doesn’t have the kind of cancer that’s ever going to kill him, or that it is highly unlikely to cause any problems for the next 10-15 years, and there is ample time to decide how to treat it.
“But the doctor kind of forgets that the patient doesn’t speak medicalese, and the doctor feels like you really have to give them thorough informed consent, after all. So you need to inform the heck out of patients with all of the medical detail you believe is necessary to understand the decision, instead of the translation of the medical detail into terms the patient can understand,” he said.
An important part of shared decision making, therefore, is to make sure that patients can understand their alternatives, but not to overwhelm them with detail, because they may give up and ask the physician, “What do you think I should do?” which can introduce physician bias that may not always lead to the right choice for that patient.
“I actually morally don’t recommend that. I think instead we should give the right amount of information at the right time so they can actually get engaged in the choice,” Dr. Ubel said.
Discussion informs choices
The investigators looked at how prediagnosis education materials and discussions with urologists shaped patient decisions about treatment choice. Patients were called before their appointments to ensure that they had read the booklet, and then just before the appointment were asked which way they were leaning if the diagnosis turned out to be positive.
The investigators found that of 44 patients who expressed a preference for active surveillance before the appointment, 55% actually went on to receive active treatment. Among 119 patients with no expressed preference for surveillance or active therapy, 46% went on to treatment, and of 118 expressing previsit preference only for active surveillance, 54% went on to receive it.
“The leaning that they had before seeing the doctor had no influence on what treatment they got,” Dr. Ubel said. Instead, physicians’ recommendations had a strong influence on treatment choice. Recommendations are an essential part of the discussion, “but I don’t think we often do them well,” he said.
Ask patients to think out loud about what they have read or have been told, and ask them to repeat in their own words what they heard the doctor say, Dr. Ubel suggested. It’s incumbent on the physician to try to understand the patient’s preferences, and say something like, “I’m the expert on medical facts, but you’re the expert on you,” or “What sounds good and bad to you about that treatment alternative?”
Finally, physicians need to make recommendations based on patient preferences, he said.
For example, in one recorded encounter, the physician asked the patient, “Are you the kind of person where the idea of just watching your PSA is that unsettling to you?” When the patient replied “Yeah, I think I would be,” the physician was able to make an informed recommendation, saying “then I don’t think you’d be a good candidate for surveillance.”
“This doctor did not just make a recommendation; he tried to find out something about the patient first, and that’s critical to giving good advice,” Dr. Ubel said.
Hollywood, FLA. – Although patients and physicians should always be partners in medical decision making, guiding patients into making medically sound choices may involve a lot of listening and empathy, often followed by a little friendly persuasion, suggests an expert in health care decision making,
“Even when you get to a situation where the clinical practice guideline would point toward shared decision making, we’ve got to do shared decision making right or the guideline just doesn’t do the work for us. We clinicians have to know how to partner with our patients to make decisions when their values matter,” said Dr. Peter A Ubel, professor of business, public policy, and medicine at Duke University, Durham, N.H.
Dr. Ubel discussed how to understand and use patient preferences in cancer treatment decisions at the annual conference of the National Comprehensive Cancer Network.
In the case of early-stage prostate cancer, for example, treatment options include surveillance or active treatment with surgery or radiation, but the risk/benefit trade-offs require careful discussion.
“The different approaches have different pros and cons: If you get active treatment, there’s a pretty good chance you’ll experience incontinence or erectile dysfunction, whereas if you undergo surveillance you won’t experience those as side effects of the surveillance strategy, but you will live with a cancer inside your body, the accompanying anxiety, and wondering every 6 months whether it has advanced,” Dr. Ubel said.
“The question is how do we go figure out which treatment is best for which patient?” he added.
What doctors say not always what patients hear
To examine how decisions are made, Dr. Ubel and his colleagues conducted a study in which patients scheduled for biopsy for suspicion of prostate cancer were approached at the time of their clinic visits and asked to participate in a study about prostate cancer decision making. Patients were given a booklet aimed at the seventh-grade reading level describing prostate cancer and its treatment, and were asked, once they had finished, what course of therapy they might pursue if the diagnosis turned out to be positive, and why. They also were asked if it was important to them to maintain natural sexual function.
The encounter between the patients and their urologists at the time of diagnosis were audio recorded, so that investigators could see whether physicians recommend specific treatments and why.
“One of the things that really jumped out in this study was just how much language, how much explanation urologists use to help patients understand their diagnosis,” Dr. Ubel said.
In one encounter, the urologist explained to the patient that 3 out of 12 biopsy cores had less than 30% cancer involvement, suggesting moderately low-risk disease, but then went on to talk about Gleason scores, tumor grades and patterns, and risk categories.
“When a patient just finds out he has prostate cancer, it’s a tough time to put a whole bunch of information in front of him for him to absorb and make a decision,” Dr. Ubel said. Patients need time to absorb the shock of a cancer diagnosis first – even a diagnosis of an early, easily treated cancer – and information overload may actually reduce their ability to comprehend their choices or retain the information, he added. The urologist in this scenario is making a very earnest effort to tell the patient that he doesn’t have the kind of cancer that’s ever going to kill him, or that it is highly unlikely to cause any problems for the next 10-15 years, and there is ample time to decide how to treat it.
“But the doctor kind of forgets that the patient doesn’t speak medicalese, and the doctor feels like you really have to give them thorough informed consent, after all. So you need to inform the heck out of patients with all of the medical detail you believe is necessary to understand the decision, instead of the translation of the medical detail into terms the patient can understand,” he said.
An important part of shared decision making, therefore, is to make sure that patients can understand their alternatives, but not to overwhelm them with detail, because they may give up and ask the physician, “What do you think I should do?” which can introduce physician bias that may not always lead to the right choice for that patient.
“I actually morally don’t recommend that. I think instead we should give the right amount of information at the right time so they can actually get engaged in the choice,” Dr. Ubel said.
Discussion informs choices
The investigators looked at how prediagnosis education materials and discussions with urologists shaped patient decisions about treatment choice. Patients were called before their appointments to ensure that they had read the booklet, and then just before the appointment were asked which way they were leaning if the diagnosis turned out to be positive.
The investigators found that of 44 patients who expressed a preference for active surveillance before the appointment, 55% actually went on to receive active treatment. Among 119 patients with no expressed preference for surveillance or active therapy, 46% went on to treatment, and of 118 expressing previsit preference only for active surveillance, 54% went on to receive it.
“The leaning that they had before seeing the doctor had no influence on what treatment they got,” Dr. Ubel said. Instead, physicians’ recommendations had a strong influence on treatment choice. Recommendations are an essential part of the discussion, “but I don’t think we often do them well,” he said.
Ask patients to think out loud about what they have read or have been told, and ask them to repeat in their own words what they heard the doctor say, Dr. Ubel suggested. It’s incumbent on the physician to try to understand the patient’s preferences, and say something like, “I’m the expert on medical facts, but you’re the expert on you,” or “What sounds good and bad to you about that treatment alternative?”
Finally, physicians need to make recommendations based on patient preferences, he said.
For example, in one recorded encounter, the physician asked the patient, “Are you the kind of person where the idea of just watching your PSA is that unsettling to you?” When the patient replied “Yeah, I think I would be,” the physician was able to make an informed recommendation, saying “then I don’t think you’d be a good candidate for surveillance.”
“This doctor did not just make a recommendation; he tried to find out something about the patient first, and that’s critical to giving good advice,” Dr. Ubel said.
AT THE NCCN ANNUAL CONFERENCE
Key clinical point: Clinicians should understand patients’ coping styles and personalities before making recommendations about comparable treatment options.
Major finding: Physician recommendations were the strongest determining factor in patient choices of prostate cancer therapies.
Data source: Study of 281 prostate cancer patients and their treatment-decision encounters with urologists.
Disclosures: Dr. Ubel reported having no relevant disclosures.
Prostate cancer’s future seen in molecular tests
HOLLYWOOD, FLA. – Current evidence suggests that molecular tests for prostate cancer are prognostic and can help clinicians and patients with difficult treatment decisions. In the not-too-distant future, gene tests could also guide choice of therapies.
“I think that the largest impact is going to come in areas of both the greatest treatment uncertainty and areas where we can be predictive about the response to treatment,” said Dr. Ashley Ross, a urologic oncologist and pathologist at the Sidney Kimmel Comprehensive Cancer Center at Johns Hopkins University, Baltimore.
Multigene panels may soon be able help identify which patients might benefit more from radical prostatectomy or radiation therapy, whether radiation therapy effects could be enhanced with the addition of androgen-deprivation therapy, and whether early use of docetaxel might add therapeutic benefit, he said at the annual conference of the National Comprehensive Cancer Network.
The 2016 iteration of the NCCN guidelines for the treatment of prostate cancer include a note stating that “men with clinically localized disease may consider the use of tumor-based molecular assays. Retrospective case cohort studies have shown that molecular assays performed on biopsy or prostatectomy specimens provide prognostic information independent of NCCN risk groups.”
The use of molecular assays may inform treatment decisions by helping to predict the likelihood of death if a patient is managed conservatively, risks for biochemical progression after radical prostatectomy or external beam therapy, and the likelihood that a patient could develop metastatic disease after radical prostatectomy or salvage radiotherapy, the guidelines say.
Dr. Ross reviewed the molecular biology of localized prostate cancer and the benefits and risks of currently available molecular tests.
“We’ve had an increased ability to get molecular information or genomic information from very limited amounts of routinely-stored pathologic tissue, and that’s resulted in the generation of many molecular-based tissue tests in prostate cancer. With the emergence of those tests and a lot of aggressive marketing, there has been a lot of confusion for patients and providers about whether we should use them or not and in what context,” he said.
Prostate cancer is genomically complex, even in the localized stage, with copy number alterations, deletions, and amplifications; chromosomal rearrangements; and point mutations, he said.
One of the best characterized genomic events is the early loss of the tumor suppressor gene PTEN (phosphatase and tensin homolog). This gene works within the PI3 kinase (PI3K)/AKT pathway. PI3K pathway mutations have been identified in up to 40% of all primary prostate cancers and 100% of mutations, Dr. Ross explained.
Loss of PTEN itself has been detected in about 15%-40% of primary prostate cancers and 50% of metastases, and the loss correlates with disease stage and tumor grade.
The NCCN guidelines list six available tissue-based tests for prostate cancer prognosis, including tests based on general cancer features such as cell-cycle proliferation, and those based on specific molecular features of cancer.
An example of the general type of test is the Ki-67 immunohistochemistry (IHC) test, which looks for a cellular marker of proliferation, and has been shown to have independent prognostic significance after radiation therapy or radical prostatectomy. This test is not currently recommended by the Medicare Molecular Diagnostic Services (MolDx) program, however.
Another general-type test is the Polaris quantitative reverse-transcriptase polymerase chain reaction (RT-PCR) panel, which tests for 31 cell-cycle-related genes and 15 “housekeeping” controls. This test is recommended for post-biopsy evaluation of men with very-low-risk or low-risk prostate cancer who at the time of diagnosis have at least 10 years of life expectancy. It has been shown to independently predict prostate cancer–specific mortality, biochemical failure/recurrence, and metastasis, the guidelines say.
Tests based on molecular features include:
• PTEN/ERG, an IHC or fluorescent in situ hybridization test that has been shown to predict prostate cancer–specific mortality, upgrading to Gleason pattern 4 on radical prostatectomy, and biochemical recurrence (not MolDx recommended).
• Decipher, a whole-transcriptome 1.4M RNA expression oligonucleotide microarray shown to predict biochemical failure, metastasis, and prostate cancer–specific mortality (recommended for postradical prostatectomy for patients with pT2 tumors with positive margins, and pT3 disease, and rising PSA above nadir);
• Oncotype DX, an RT-PCR assay for 12 prostate cancer genes and five housekeeping controls (recommended for post-biopsy evaluation of men with very-low-risk or low-risk prostate cancer who at the time of diagnosis have at least 10 years of life expectancy).
• ProMark, multiplex immunofluorescent staining of eight proteins, which has been shown to independently predict non–organ-confined pT3 disease or Gleason pattern 4 disease on radical prostatectomy (not reviewed).
Dr. Ross said that in his practice, he generally does not order molecular testing for surveillance of men older than 65 who have very-low-risk disease. For men with low-risk disease, however, molecular testing may help in clinical decision making to predict upgrading or disease progression.
“There’s limited data from surveillance populations, but these tests can be used in this context with retrospective data available, realizing that in most cases the tests will be confirmative, or another way of thinking about it is ‘noninformative,’ so there are some considerations about cost in that context,” he said. For men with intermediate or high-risk disease, however, currently available tests are not good at predicting what an individual patient’s response would be to a specific type of therapy, whether surgery, radiation, androgen deprivation, chemotherapy, or a combination.
“This is an area where predictive biomarkers would be very informative. There is ongoing research, and I think this is an area of potentially large advancement in how we risk-stratify our patients,” Dr. Ross said.
HOLLYWOOD, FLA. – Current evidence suggests that molecular tests for prostate cancer are prognostic and can help clinicians and patients with difficult treatment decisions. In the not-too-distant future, gene tests could also guide choice of therapies.
“I think that the largest impact is going to come in areas of both the greatest treatment uncertainty and areas where we can be predictive about the response to treatment,” said Dr. Ashley Ross, a urologic oncologist and pathologist at the Sidney Kimmel Comprehensive Cancer Center at Johns Hopkins University, Baltimore.
Multigene panels may soon be able help identify which patients might benefit more from radical prostatectomy or radiation therapy, whether radiation therapy effects could be enhanced with the addition of androgen-deprivation therapy, and whether early use of docetaxel might add therapeutic benefit, he said at the annual conference of the National Comprehensive Cancer Network.
The 2016 iteration of the NCCN guidelines for the treatment of prostate cancer include a note stating that “men with clinically localized disease may consider the use of tumor-based molecular assays. Retrospective case cohort studies have shown that molecular assays performed on biopsy or prostatectomy specimens provide prognostic information independent of NCCN risk groups.”
The use of molecular assays may inform treatment decisions by helping to predict the likelihood of death if a patient is managed conservatively, risks for biochemical progression after radical prostatectomy or external beam therapy, and the likelihood that a patient could develop metastatic disease after radical prostatectomy or salvage radiotherapy, the guidelines say.
Dr. Ross reviewed the molecular biology of localized prostate cancer and the benefits and risks of currently available molecular tests.
“We’ve had an increased ability to get molecular information or genomic information from very limited amounts of routinely-stored pathologic tissue, and that’s resulted in the generation of many molecular-based tissue tests in prostate cancer. With the emergence of those tests and a lot of aggressive marketing, there has been a lot of confusion for patients and providers about whether we should use them or not and in what context,” he said.
Prostate cancer is genomically complex, even in the localized stage, with copy number alterations, deletions, and amplifications; chromosomal rearrangements; and point mutations, he said.
One of the best characterized genomic events is the early loss of the tumor suppressor gene PTEN (phosphatase and tensin homolog). This gene works within the PI3 kinase (PI3K)/AKT pathway. PI3K pathway mutations have been identified in up to 40% of all primary prostate cancers and 100% of mutations, Dr. Ross explained.
Loss of PTEN itself has been detected in about 15%-40% of primary prostate cancers and 50% of metastases, and the loss correlates with disease stage and tumor grade.
The NCCN guidelines list six available tissue-based tests for prostate cancer prognosis, including tests based on general cancer features such as cell-cycle proliferation, and those based on specific molecular features of cancer.
An example of the general type of test is the Ki-67 immunohistochemistry (IHC) test, which looks for a cellular marker of proliferation, and has been shown to have independent prognostic significance after radiation therapy or radical prostatectomy. This test is not currently recommended by the Medicare Molecular Diagnostic Services (MolDx) program, however.
Another general-type test is the Polaris quantitative reverse-transcriptase polymerase chain reaction (RT-PCR) panel, which tests for 31 cell-cycle-related genes and 15 “housekeeping” controls. This test is recommended for post-biopsy evaluation of men with very-low-risk or low-risk prostate cancer who at the time of diagnosis have at least 10 years of life expectancy. It has been shown to independently predict prostate cancer–specific mortality, biochemical failure/recurrence, and metastasis, the guidelines say.
Tests based on molecular features include:
• PTEN/ERG, an IHC or fluorescent in situ hybridization test that has been shown to predict prostate cancer–specific mortality, upgrading to Gleason pattern 4 on radical prostatectomy, and biochemical recurrence (not MolDx recommended).
• Decipher, a whole-transcriptome 1.4M RNA expression oligonucleotide microarray shown to predict biochemical failure, metastasis, and prostate cancer–specific mortality (recommended for postradical prostatectomy for patients with pT2 tumors with positive margins, and pT3 disease, and rising PSA above nadir);
• Oncotype DX, an RT-PCR assay for 12 prostate cancer genes and five housekeeping controls (recommended for post-biopsy evaluation of men with very-low-risk or low-risk prostate cancer who at the time of diagnosis have at least 10 years of life expectancy).
• ProMark, multiplex immunofluorescent staining of eight proteins, which has been shown to independently predict non–organ-confined pT3 disease or Gleason pattern 4 disease on radical prostatectomy (not reviewed).
Dr. Ross said that in his practice, he generally does not order molecular testing for surveillance of men older than 65 who have very-low-risk disease. For men with low-risk disease, however, molecular testing may help in clinical decision making to predict upgrading or disease progression.
“There’s limited data from surveillance populations, but these tests can be used in this context with retrospective data available, realizing that in most cases the tests will be confirmative, or another way of thinking about it is ‘noninformative,’ so there are some considerations about cost in that context,” he said. For men with intermediate or high-risk disease, however, currently available tests are not good at predicting what an individual patient’s response would be to a specific type of therapy, whether surgery, radiation, androgen deprivation, chemotherapy, or a combination.
“This is an area where predictive biomarkers would be very informative. There is ongoing research, and I think this is an area of potentially large advancement in how we risk-stratify our patients,” Dr. Ross said.
HOLLYWOOD, FLA. – Current evidence suggests that molecular tests for prostate cancer are prognostic and can help clinicians and patients with difficult treatment decisions. In the not-too-distant future, gene tests could also guide choice of therapies.
“I think that the largest impact is going to come in areas of both the greatest treatment uncertainty and areas where we can be predictive about the response to treatment,” said Dr. Ashley Ross, a urologic oncologist and pathologist at the Sidney Kimmel Comprehensive Cancer Center at Johns Hopkins University, Baltimore.
Multigene panels may soon be able help identify which patients might benefit more from radical prostatectomy or radiation therapy, whether radiation therapy effects could be enhanced with the addition of androgen-deprivation therapy, and whether early use of docetaxel might add therapeutic benefit, he said at the annual conference of the National Comprehensive Cancer Network.
The 2016 iteration of the NCCN guidelines for the treatment of prostate cancer include a note stating that “men with clinically localized disease may consider the use of tumor-based molecular assays. Retrospective case cohort studies have shown that molecular assays performed on biopsy or prostatectomy specimens provide prognostic information independent of NCCN risk groups.”
The use of molecular assays may inform treatment decisions by helping to predict the likelihood of death if a patient is managed conservatively, risks for biochemical progression after radical prostatectomy or external beam therapy, and the likelihood that a patient could develop metastatic disease after radical prostatectomy or salvage radiotherapy, the guidelines say.
Dr. Ross reviewed the molecular biology of localized prostate cancer and the benefits and risks of currently available molecular tests.
“We’ve had an increased ability to get molecular information or genomic information from very limited amounts of routinely-stored pathologic tissue, and that’s resulted in the generation of many molecular-based tissue tests in prostate cancer. With the emergence of those tests and a lot of aggressive marketing, there has been a lot of confusion for patients and providers about whether we should use them or not and in what context,” he said.
Prostate cancer is genomically complex, even in the localized stage, with copy number alterations, deletions, and amplifications; chromosomal rearrangements; and point mutations, he said.
One of the best characterized genomic events is the early loss of the tumor suppressor gene PTEN (phosphatase and tensin homolog). This gene works within the PI3 kinase (PI3K)/AKT pathway. PI3K pathway mutations have been identified in up to 40% of all primary prostate cancers and 100% of mutations, Dr. Ross explained.
Loss of PTEN itself has been detected in about 15%-40% of primary prostate cancers and 50% of metastases, and the loss correlates with disease stage and tumor grade.
The NCCN guidelines list six available tissue-based tests for prostate cancer prognosis, including tests based on general cancer features such as cell-cycle proliferation, and those based on specific molecular features of cancer.
An example of the general type of test is the Ki-67 immunohistochemistry (IHC) test, which looks for a cellular marker of proliferation, and has been shown to have independent prognostic significance after radiation therapy or radical prostatectomy. This test is not currently recommended by the Medicare Molecular Diagnostic Services (MolDx) program, however.
Another general-type test is the Polaris quantitative reverse-transcriptase polymerase chain reaction (RT-PCR) panel, which tests for 31 cell-cycle-related genes and 15 “housekeeping” controls. This test is recommended for post-biopsy evaluation of men with very-low-risk or low-risk prostate cancer who at the time of diagnosis have at least 10 years of life expectancy. It has been shown to independently predict prostate cancer–specific mortality, biochemical failure/recurrence, and metastasis, the guidelines say.
Tests based on molecular features include:
• PTEN/ERG, an IHC or fluorescent in situ hybridization test that has been shown to predict prostate cancer–specific mortality, upgrading to Gleason pattern 4 on radical prostatectomy, and biochemical recurrence (not MolDx recommended).
• Decipher, a whole-transcriptome 1.4M RNA expression oligonucleotide microarray shown to predict biochemical failure, metastasis, and prostate cancer–specific mortality (recommended for postradical prostatectomy for patients with pT2 tumors with positive margins, and pT3 disease, and rising PSA above nadir);
• Oncotype DX, an RT-PCR assay for 12 prostate cancer genes and five housekeeping controls (recommended for post-biopsy evaluation of men with very-low-risk or low-risk prostate cancer who at the time of diagnosis have at least 10 years of life expectancy).
• ProMark, multiplex immunofluorescent staining of eight proteins, which has been shown to independently predict non–organ-confined pT3 disease or Gleason pattern 4 disease on radical prostatectomy (not reviewed).
Dr. Ross said that in his practice, he generally does not order molecular testing for surveillance of men older than 65 who have very-low-risk disease. For men with low-risk disease, however, molecular testing may help in clinical decision making to predict upgrading or disease progression.
“There’s limited data from surveillance populations, but these tests can be used in this context with retrospective data available, realizing that in most cases the tests will be confirmative, or another way of thinking about it is ‘noninformative,’ so there are some considerations about cost in that context,” he said. For men with intermediate or high-risk disease, however, currently available tests are not good at predicting what an individual patient’s response would be to a specific type of therapy, whether surgery, radiation, androgen deprivation, chemotherapy, or a combination.
“This is an area where predictive biomarkers would be very informative. There is ongoing research, and I think this is an area of potentially large advancement in how we risk-stratify our patients,” Dr. Ross said.
EXPERT ANALYSIS FROM THE NCCN ANNUAL CONFERENCE
Prostate cancer’s future seen in molecular tests
HOLLYWOOD, FLA. – Current evidence suggests that molecular tests for prostate cancer are prognostic and can help clinicians and patients with difficult treatment decisions. In the not-too-distant future, gene tests could also guide choice of therapies.
“I think that the largest impact is going to come in areas of both the greatest treatment uncertainty and areas where we can be predictive about the response to treatment,” said Dr. Ashley Ross, a urologic oncologist and pathologist at the Sidney Kimmel Comprehensive Cancer Center at Johns Hopkins University, Baltimore.
Multigene panels may soon be able help identify which patients might benefit more from radical prostatectomy or radiation therapy, whether radiation therapy effects could be enhanced with the addition of androgen-deprivation therapy, and whether early use of docetaxel might add therapeutic benefit, he said at the annual conference of the National Comprehensive Cancer Network.
The 2016 iteration of the NCCN guidelines for the treatment of prostate cancer include a note stating that “men with clinically localized disease may consider the use of tumor-based molecular assays. Retrospective case cohort studies have shown that molecular assays performed on biopsy or prostatectomy specimens provide prognostic information independent of NCCN risk groups.”
The use of molecular assays may inform treatment decisions by helping to predict the likelihood of death if a patient is managed conservatively, risks for biochemical progression after radical prostatectomy or external beam therapy, and the likelihood that a patient could develop metastatic disease after radical prostatectomy or salvage radiotherapy, the guidelines say.
Dr. Ross reviewed the molecular biology of localized prostate cancer and the benefits and risks of currently available molecular tests.
“We’ve had an increased ability to get molecular information or genomic information from very limited amounts of routinely-stored pathologic tissue, and that’s resulted in the generation of many molecular-based tissue tests in prostate cancer. With the emergence of those tests and a lot of aggressive marketing, there has been a lot of confusion for patients and providers about whether we should use them or not and in what context,” he said.
Prostate cancer is genomically complex, even in the localized stage, with copy number alterations, deletions, and amplifications; chromosomal rearrangements; and point mutations, he said.
One of the best characterized genomic events is the early loss of the tumor suppressor gene PTEN (phosphatase and tensin homolog). This gene works within the PI3 kinase (PI3K)/AKT pathway. PI3K pathway mutations have been identified in up to 40% of all primary prostate cancers and 100% of mutations, Dr. Ross explained.
Loss of PTEN itself has been detected in about 15%-40% of primary prostate cancers and 50% of metastases, and the loss correlates with disease stage and tumor grade.
The NCCN guidelines list six available tissue-based tests for prostate cancer prognosis, including tests based on general cancer features such as cell-cycle proliferation, and those based on specific molecular features of cancer.
An example of the general type of test is the Ki-67 immunohistochemistry (IHC) test, which looks for a cellular marker of proliferation, and has been shown to have independent prognostic significance after radiation therapy or radical prostatectomy. This test is not currently recommended by the Medicare Molecular Diagnostic Services (MolDx) program, however.
Another general-type test is the Polaris quantitative reverse-transcriptase polymerase chain reaction (RT-PCR) panel, which tests for 31 cell-cycle-related genes and 15 “housekeeping” controls. This test is recommended for post-biopsy evaluation of men with very-low-risk or low-risk prostate cancer who at the time of diagnosis have at least 10 years of life expectancy. It has been shown to independently predict prostate cancer–specific mortality, biochemical failure/recurrence, and metastasis, the guidelines say.
Tests based on molecular features include:
• PTEN/ERG, an IHC or fluorescent in situ hybridization test that has been shown to predict prostate cancer–specific mortality, upgrading to Gleason pattern 4 on radical prostatectomy, and biochemical recurrence (not MolDx recommended).
• Decipher, a whole-transcriptome 1.4M RNA expression oligonucleotide microarray shown to predict biochemical failure, metastasis, and prostate cancer–specific mortality (recommended for postradical prostatectomy for patients with pT2 tumors with positive margins, and pT3 disease, and rising PSA above nadir);
• Oncotype DX, an RT-PCR assay for 12 prostate cancer genes and five housekeeping controls (recommended for post-biopsy evaluation of men with very-low-risk or low-risk prostate cancer who at the time of diagnosis have at least 10 years of life expectancy).
• ProMark, multiplex immunofluorescent staining of eight proteins, which has been shown to independently predict non–organ-confined pT3 disease or Gleason pattern 4 disease on radical prostatectomy (not reviewed).
Dr. Ross said that in his practice, he generally does not order molecular testing for surveillance of men older than 65 who have very-low-risk disease. For men with low-risk disease, however, molecular testing may help in clinical decision making to predict upgrading or disease progression.
“There’s limited data from surveillance populations, but these tests can be used in this context with retrospective data available, realizing that in most cases the tests will be confirmative, or another way of thinking about it is ‘noninformative,’ so there are some considerations about cost in that context,” he said. For men with intermediate or high-risk disease, however, currently available tests are not good at predicting what an individual patient’s response would be to a specific type of therapy, whether surgery, radiation, androgen deprivation, chemotherapy, or a combination.
“This is an area where predictive biomarkers would be very informative. There is ongoing research, and I think this is an area of potentially large advancement in how we risk-stratify our patients,” Dr. Ross said.
HOLLYWOOD, FLA. – Current evidence suggests that molecular tests for prostate cancer are prognostic and can help clinicians and patients with difficult treatment decisions. In the not-too-distant future, gene tests could also guide choice of therapies.
“I think that the largest impact is going to come in areas of both the greatest treatment uncertainty and areas where we can be predictive about the response to treatment,” said Dr. Ashley Ross, a urologic oncologist and pathologist at the Sidney Kimmel Comprehensive Cancer Center at Johns Hopkins University, Baltimore.
Multigene panels may soon be able help identify which patients might benefit more from radical prostatectomy or radiation therapy, whether radiation therapy effects could be enhanced with the addition of androgen-deprivation therapy, and whether early use of docetaxel might add therapeutic benefit, he said at the annual conference of the National Comprehensive Cancer Network.
The 2016 iteration of the NCCN guidelines for the treatment of prostate cancer include a note stating that “men with clinically localized disease may consider the use of tumor-based molecular assays. Retrospective case cohort studies have shown that molecular assays performed on biopsy or prostatectomy specimens provide prognostic information independent of NCCN risk groups.”
The use of molecular assays may inform treatment decisions by helping to predict the likelihood of death if a patient is managed conservatively, risks for biochemical progression after radical prostatectomy or external beam therapy, and the likelihood that a patient could develop metastatic disease after radical prostatectomy or salvage radiotherapy, the guidelines say.
Dr. Ross reviewed the molecular biology of localized prostate cancer and the benefits and risks of currently available molecular tests.
“We’ve had an increased ability to get molecular information or genomic information from very limited amounts of routinely-stored pathologic tissue, and that’s resulted in the generation of many molecular-based tissue tests in prostate cancer. With the emergence of those tests and a lot of aggressive marketing, there has been a lot of confusion for patients and providers about whether we should use them or not and in what context,” he said.
Prostate cancer is genomically complex, even in the localized stage, with copy number alterations, deletions, and amplifications; chromosomal rearrangements; and point mutations, he said.
One of the best characterized genomic events is the early loss of the tumor suppressor gene PTEN (phosphatase and tensin homolog). This gene works within the PI3 kinase (PI3K)/AKT pathway. PI3K pathway mutations have been identified in up to 40% of all primary prostate cancers and 100% of mutations, Dr. Ross explained.
Loss of PTEN itself has been detected in about 15%-40% of primary prostate cancers and 50% of metastases, and the loss correlates with disease stage and tumor grade.
The NCCN guidelines list six available tissue-based tests for prostate cancer prognosis, including tests based on general cancer features such as cell-cycle proliferation, and those based on specific molecular features of cancer.
An example of the general type of test is the Ki-67 immunohistochemistry (IHC) test, which looks for a cellular marker of proliferation, and has been shown to have independent prognostic significance after radiation therapy or radical prostatectomy. This test is not currently recommended by the Medicare Molecular Diagnostic Services (MolDx) program, however.
Another general-type test is the Polaris quantitative reverse-transcriptase polymerase chain reaction (RT-PCR) panel, which tests for 31 cell-cycle-related genes and 15 “housekeeping” controls. This test is recommended for post-biopsy evaluation of men with very-low-risk or low-risk prostate cancer who at the time of diagnosis have at least 10 years of life expectancy. It has been shown to independently predict prostate cancer–specific mortality, biochemical failure/recurrence, and metastasis, the guidelines say.
Tests based on molecular features include:
• PTEN/ERG, an IHC or fluorescent in situ hybridization test that has been shown to predict prostate cancer–specific mortality, upgrading to Gleason pattern 4 on radical prostatectomy, and biochemical recurrence (not MolDx recommended).
• Decipher, a whole-transcriptome 1.4M RNA expression oligonucleotide microarray shown to predict biochemical failure, metastasis, and prostate cancer–specific mortality (recommended for postradical prostatectomy for patients with pT2 tumors with positive margins, and pT3 disease, and rising PSA above nadir);
• Oncotype DX, an RT-PCR assay for 12 prostate cancer genes and five housekeeping controls (recommended for post-biopsy evaluation of men with very-low-risk or low-risk prostate cancer who at the time of diagnosis have at least 10 years of life expectancy).
• ProMark, multiplex immunofluorescent staining of eight proteins, which has been shown to independently predict non–organ-confined pT3 disease or Gleason pattern 4 disease on radical prostatectomy (not reviewed).
Dr. Ross said that in his practice, he generally does not order molecular testing for surveillance of men older than 65 who have very-low-risk disease. For men with low-risk disease, however, molecular testing may help in clinical decision making to predict upgrading or disease progression.
“There’s limited data from surveillance populations, but these tests can be used in this context with retrospective data available, realizing that in most cases the tests will be confirmative, or another way of thinking about it is ‘noninformative,’ so there are some considerations about cost in that context,” he said. For men with intermediate or high-risk disease, however, currently available tests are not good at predicting what an individual patient’s response would be to a specific type of therapy, whether surgery, radiation, androgen deprivation, chemotherapy, or a combination.
“This is an area where predictive biomarkers would be very informative. There is ongoing research, and I think this is an area of potentially large advancement in how we risk-stratify our patients,” Dr. Ross said.
HOLLYWOOD, FLA. – Current evidence suggests that molecular tests for prostate cancer are prognostic and can help clinicians and patients with difficult treatment decisions. In the not-too-distant future, gene tests could also guide choice of therapies.
“I think that the largest impact is going to come in areas of both the greatest treatment uncertainty and areas where we can be predictive about the response to treatment,” said Dr. Ashley Ross, a urologic oncologist and pathologist at the Sidney Kimmel Comprehensive Cancer Center at Johns Hopkins University, Baltimore.
Multigene panels may soon be able help identify which patients might benefit more from radical prostatectomy or radiation therapy, whether radiation therapy effects could be enhanced with the addition of androgen-deprivation therapy, and whether early use of docetaxel might add therapeutic benefit, he said at the annual conference of the National Comprehensive Cancer Network.
The 2016 iteration of the NCCN guidelines for the treatment of prostate cancer include a note stating that “men with clinically localized disease may consider the use of tumor-based molecular assays. Retrospective case cohort studies have shown that molecular assays performed on biopsy or prostatectomy specimens provide prognostic information independent of NCCN risk groups.”
The use of molecular assays may inform treatment decisions by helping to predict the likelihood of death if a patient is managed conservatively, risks for biochemical progression after radical prostatectomy or external beam therapy, and the likelihood that a patient could develop metastatic disease after radical prostatectomy or salvage radiotherapy, the guidelines say.
Dr. Ross reviewed the molecular biology of localized prostate cancer and the benefits and risks of currently available molecular tests.
“We’ve had an increased ability to get molecular information or genomic information from very limited amounts of routinely-stored pathologic tissue, and that’s resulted in the generation of many molecular-based tissue tests in prostate cancer. With the emergence of those tests and a lot of aggressive marketing, there has been a lot of confusion for patients and providers about whether we should use them or not and in what context,” he said.
Prostate cancer is genomically complex, even in the localized stage, with copy number alterations, deletions, and amplifications; chromosomal rearrangements; and point mutations, he said.
One of the best characterized genomic events is the early loss of the tumor suppressor gene PTEN (phosphatase and tensin homolog). This gene works within the PI3 kinase (PI3K)/AKT pathway. PI3K pathway mutations have been identified in up to 40% of all primary prostate cancers and 100% of mutations, Dr. Ross explained.
Loss of PTEN itself has been detected in about 15%-40% of primary prostate cancers and 50% of metastases, and the loss correlates with disease stage and tumor grade.
The NCCN guidelines list six available tissue-based tests for prostate cancer prognosis, including tests based on general cancer features such as cell-cycle proliferation, and those based on specific molecular features of cancer.
An example of the general type of test is the Ki-67 immunohistochemistry (IHC) test, which looks for a cellular marker of proliferation, and has been shown to have independent prognostic significance after radiation therapy or radical prostatectomy. This test is not currently recommended by the Medicare Molecular Diagnostic Services (MolDx) program, however.
Another general-type test is the Polaris quantitative reverse-transcriptase polymerase chain reaction (RT-PCR) panel, which tests for 31 cell-cycle-related genes and 15 “housekeeping” controls. This test is recommended for post-biopsy evaluation of men with very-low-risk or low-risk prostate cancer who at the time of diagnosis have at least 10 years of life expectancy. It has been shown to independently predict prostate cancer–specific mortality, biochemical failure/recurrence, and metastasis, the guidelines say.
Tests based on molecular features include:
• PTEN/ERG, an IHC or fluorescent in situ hybridization test that has been shown to predict prostate cancer–specific mortality, upgrading to Gleason pattern 4 on radical prostatectomy, and biochemical recurrence (not MolDx recommended).
• Decipher, a whole-transcriptome 1.4M RNA expression oligonucleotide microarray shown to predict biochemical failure, metastasis, and prostate cancer–specific mortality (recommended for postradical prostatectomy for patients with pT2 tumors with positive margins, and pT3 disease, and rising PSA above nadir);
• Oncotype DX, an RT-PCR assay for 12 prostate cancer genes and five housekeeping controls (recommended for post-biopsy evaluation of men with very-low-risk or low-risk prostate cancer who at the time of diagnosis have at least 10 years of life expectancy).
• ProMark, multiplex immunofluorescent staining of eight proteins, which has been shown to independently predict non–organ-confined pT3 disease or Gleason pattern 4 disease on radical prostatectomy (not reviewed).
Dr. Ross said that in his practice, he generally does not order molecular testing for surveillance of men older than 65 who have very-low-risk disease. For men with low-risk disease, however, molecular testing may help in clinical decision making to predict upgrading or disease progression.
“There’s limited data from surveillance populations, but these tests can be used in this context with retrospective data available, realizing that in most cases the tests will be confirmative, or another way of thinking about it is ‘noninformative,’ so there are some considerations about cost in that context,” he said. For men with intermediate or high-risk disease, however, currently available tests are not good at predicting what an individual patient’s response would be to a specific type of therapy, whether surgery, radiation, androgen deprivation, chemotherapy, or a combination.
“This is an area where predictive biomarkers would be very informative. There is ongoing research, and I think this is an area of potentially large advancement in how we risk-stratify our patients,” Dr. Ross said.
EXPERT ANALYSIS FROM THE NCCN ANNUAL CONFERENCE