User login
Untargeted CT scans leads to overdiagnoses in lung cancer
Such overdiagnosis was illustrated in a recent study from JAMA Internal Medicine of women in Taiwan who were screened for lung cancer using low-dose CT (LDCT).
The study, and the accompanying editorial, pointed out the potential for large databases of routine clinical data to track long-term outcomes, and potentially identify patient subgroups that could benefit from early diagnosis using digital technologies.
The Taiwanese findings echo a similar trend identified in a 2018 post hoc analysis of the Danish Lung Cancer Screening Trial, which estimated that 67.2% of cancers found during that CT screening program for current or former smokers were overdiagnosed. The authors recommended that researchers report rates of overdiagnosis in future screening studies.
The authors of the Taiwan study noted that LDCT is low cost and is frequently offered to individuals who are not considered at high risk of lung cancer, and advertisements in Taiwan often target women, who rarely smoke. The researchers examined data from the Taiwan National Cancer Registry. They looked for evidence of an increased incidence of early-stage detection and reduced incidence of late-stage diagnosis. They found that, from 2004 to 2018, there was an increase of lung cancer incidence from 2.3 to 14.4 per 100,000 (difference, 12.1; 95% confidence interval, 11.3-12.8), but no significant difference in the incidence of late-stage disease (from 18.7 to 19.3 per 100,000; difference, 0.6; 95% CI, –0.5 to 1.7).
“This combination of findings, an additional 12.1 early-stage cancers per 100,000 population and no reduction in late-stage cancers, is strongly suggestive of overdiagnosis,” the authors wrote.
It can be difficult to convince people of the potential harms of overdiagnosis, especially when patients have a nodule removed and remain healthy years later. “It’s very counterintuitive, but it’s a reality, and I think this paper paints the reality very, very clearly,” said Daniel Capurro, MD, PhD, deputy director of the Centre for the Digital Transformation of Health at University of Melbourne, and an author of the editorial.
The issue is that some lung cancers progress so slowly that they may never cause a problem clinically, and their removal can lead to unnecessary cost and risk. And it’s not just cancer. “There are a bunch of other conditions that are defined by specific criteria, but we don’t add the prognosis to that definition. At the individual patient level, we don’t know the prognosis,” Dr. Capurro said.
Dr. Capurro discussed the increasing use of digital technologies like smartphone apps. Machine learning can potentially use such data to diagnose conditions like sleep or mood disorders before they become clinically significant, allowing earlier intervention, but they could also lead to overdiagnosis. Dr. Capurro proposed using longitudinal databases to track patient outcomes, which could be applied to digital screening technologies.
“You might be able to find unknown patterns that help discriminate between these pathological definitions. You should be able to train (digital screens) with the pathological definition plus the disease trajectory as a way to improve that label,” he said.
The study was funded by the Taiwan Ministry of Health and Welfare Clinical Trial Center.
Such overdiagnosis was illustrated in a recent study from JAMA Internal Medicine of women in Taiwan who were screened for lung cancer using low-dose CT (LDCT).
The study, and the accompanying editorial, pointed out the potential for large databases of routine clinical data to track long-term outcomes, and potentially identify patient subgroups that could benefit from early diagnosis using digital technologies.
The Taiwanese findings echo a similar trend identified in a 2018 post hoc analysis of the Danish Lung Cancer Screening Trial, which estimated that 67.2% of cancers found during that CT screening program for current or former smokers were overdiagnosed. The authors recommended that researchers report rates of overdiagnosis in future screening studies.
The authors of the Taiwan study noted that LDCT is low cost and is frequently offered to individuals who are not considered at high risk of lung cancer, and advertisements in Taiwan often target women, who rarely smoke. The researchers examined data from the Taiwan National Cancer Registry. They looked for evidence of an increased incidence of early-stage detection and reduced incidence of late-stage diagnosis. They found that, from 2004 to 2018, there was an increase of lung cancer incidence from 2.3 to 14.4 per 100,000 (difference, 12.1; 95% confidence interval, 11.3-12.8), but no significant difference in the incidence of late-stage disease (from 18.7 to 19.3 per 100,000; difference, 0.6; 95% CI, –0.5 to 1.7).
“This combination of findings, an additional 12.1 early-stage cancers per 100,000 population and no reduction in late-stage cancers, is strongly suggestive of overdiagnosis,” the authors wrote.
It can be difficult to convince people of the potential harms of overdiagnosis, especially when patients have a nodule removed and remain healthy years later. “It’s very counterintuitive, but it’s a reality, and I think this paper paints the reality very, very clearly,” said Daniel Capurro, MD, PhD, deputy director of the Centre for the Digital Transformation of Health at University of Melbourne, and an author of the editorial.
The issue is that some lung cancers progress so slowly that they may never cause a problem clinically, and their removal can lead to unnecessary cost and risk. And it’s not just cancer. “There are a bunch of other conditions that are defined by specific criteria, but we don’t add the prognosis to that definition. At the individual patient level, we don’t know the prognosis,” Dr. Capurro said.
Dr. Capurro discussed the increasing use of digital technologies like smartphone apps. Machine learning can potentially use such data to diagnose conditions like sleep or mood disorders before they become clinically significant, allowing earlier intervention, but they could also lead to overdiagnosis. Dr. Capurro proposed using longitudinal databases to track patient outcomes, which could be applied to digital screening technologies.
“You might be able to find unknown patterns that help discriminate between these pathological definitions. You should be able to train (digital screens) with the pathological definition plus the disease trajectory as a way to improve that label,” he said.
The study was funded by the Taiwan Ministry of Health and Welfare Clinical Trial Center.
Such overdiagnosis was illustrated in a recent study from JAMA Internal Medicine of women in Taiwan who were screened for lung cancer using low-dose CT (LDCT).
The study, and the accompanying editorial, pointed out the potential for large databases of routine clinical data to track long-term outcomes, and potentially identify patient subgroups that could benefit from early diagnosis using digital technologies.
The Taiwanese findings echo a similar trend identified in a 2018 post hoc analysis of the Danish Lung Cancer Screening Trial, which estimated that 67.2% of cancers found during that CT screening program for current or former smokers were overdiagnosed. The authors recommended that researchers report rates of overdiagnosis in future screening studies.
The authors of the Taiwan study noted that LDCT is low cost and is frequently offered to individuals who are not considered at high risk of lung cancer, and advertisements in Taiwan often target women, who rarely smoke. The researchers examined data from the Taiwan National Cancer Registry. They looked for evidence of an increased incidence of early-stage detection and reduced incidence of late-stage diagnosis. They found that, from 2004 to 2018, there was an increase of lung cancer incidence from 2.3 to 14.4 per 100,000 (difference, 12.1; 95% confidence interval, 11.3-12.8), but no significant difference in the incidence of late-stage disease (from 18.7 to 19.3 per 100,000; difference, 0.6; 95% CI, –0.5 to 1.7).
“This combination of findings, an additional 12.1 early-stage cancers per 100,000 population and no reduction in late-stage cancers, is strongly suggestive of overdiagnosis,” the authors wrote.
It can be difficult to convince people of the potential harms of overdiagnosis, especially when patients have a nodule removed and remain healthy years later. “It’s very counterintuitive, but it’s a reality, and I think this paper paints the reality very, very clearly,” said Daniel Capurro, MD, PhD, deputy director of the Centre for the Digital Transformation of Health at University of Melbourne, and an author of the editorial.
The issue is that some lung cancers progress so slowly that they may never cause a problem clinically, and their removal can lead to unnecessary cost and risk. And it’s not just cancer. “There are a bunch of other conditions that are defined by specific criteria, but we don’t add the prognosis to that definition. At the individual patient level, we don’t know the prognosis,” Dr. Capurro said.
Dr. Capurro discussed the increasing use of digital technologies like smartphone apps. Machine learning can potentially use such data to diagnose conditions like sleep or mood disorders before they become clinically significant, allowing earlier intervention, but they could also lead to overdiagnosis. Dr. Capurro proposed using longitudinal databases to track patient outcomes, which could be applied to digital screening technologies.
“You might be able to find unknown patterns that help discriminate between these pathological definitions. You should be able to train (digital screens) with the pathological definition plus the disease trajectory as a way to improve that label,” he said.
The study was funded by the Taiwan Ministry of Health and Welfare Clinical Trial Center.
FROM JAMA INTERNAL MEDICINE
Physical exercise might contribute to increased BDNF levels in MS
Key clinical point: Physical activity increased peripheral levels of brain-derived neurotrophic factor (BDNF) in patients with multiple sclerosis (MS).
Major finding: Serum BDNF concentrations were significantly higher after exercise intervention compared with the preintervention levels (standardized mean difference 0.3309; P = .0275).
Study details: This was a meta-analysis of 13 exercise intervention clinical trials involving 271 patients with MS.
Disclosures: The authors did not receive any funding for this work. The authors declared no conflicts of interest.
Source: Shobeiri P et al. Exercise-induced increase in blood-based brain-derived neurotrophic factor (BDNF) in people with multiple sclerosis: A systematic review and meta-analysis of exercise intervention trials. PLoS One. 2022;17(3):e0264557 (Mar 3). Doi: 10.1371/journal.pone.0264557
Key clinical point: Physical activity increased peripheral levels of brain-derived neurotrophic factor (BDNF) in patients with multiple sclerosis (MS).
Major finding: Serum BDNF concentrations were significantly higher after exercise intervention compared with the preintervention levels (standardized mean difference 0.3309; P = .0275).
Study details: This was a meta-analysis of 13 exercise intervention clinical trials involving 271 patients with MS.
Disclosures: The authors did not receive any funding for this work. The authors declared no conflicts of interest.
Source: Shobeiri P et al. Exercise-induced increase in blood-based brain-derived neurotrophic factor (BDNF) in people with multiple sclerosis: A systematic review and meta-analysis of exercise intervention trials. PLoS One. 2022;17(3):e0264557 (Mar 3). Doi: 10.1371/journal.pone.0264557
Key clinical point: Physical activity increased peripheral levels of brain-derived neurotrophic factor (BDNF) in patients with multiple sclerosis (MS).
Major finding: Serum BDNF concentrations were significantly higher after exercise intervention compared with the preintervention levels (standardized mean difference 0.3309; P = .0275).
Study details: This was a meta-analysis of 13 exercise intervention clinical trials involving 271 patients with MS.
Disclosures: The authors did not receive any funding for this work. The authors declared no conflicts of interest.
Source: Shobeiri P et al. Exercise-induced increase in blood-based brain-derived neurotrophic factor (BDNF) in people with multiple sclerosis: A systematic review and meta-analysis of exercise intervention trials. PLoS One. 2022;17(3):e0264557 (Mar 3). Doi: 10.1371/journal.pone.0264557
Get the science right
Get the science right. I have spent years researching and reflecting on what makes the best physicians, the best medicine, the optimal organized medical system, and the best medical ethics and law to support all of it. I have traveled to almost innumerable conferences to discuss these topics with colleagues who have similar goals. Time and time again, I come back to the conclusion that, in the modern era, the second-most important thing to do is to get the science right.
The practice of medicine in my Western world can be traced back to Hippocrates and earlier. The practice of nursing has other milestones. The healing arts have different points of origin in other cultures, such as China. In a modern world of mass communication, these various historical paths are converging on scientific evidence. The science to support medicine has always had flaws, but it has fared better than the other options. Sometimes, the science was so sketchy that the key was to believe in whatever the shaman was providing. But for the past 100 years, science, rather than tradition and hierarchy, has been relied upon to guide policy and action. For the past 50 years, evidence-based medicine has ascended. Have we become better than the snake oil salesmen of the late 19th century?
Modern health care is far from perfect. The pandemic has been a major stressor to the health care system. The pandemic has revealed flaws and weaknesses, including inequity in access to care, health illiteracy, and a shaky moral compass balancing individual liberty and social good. Overall, despite multiple mistakes dealing with a novel threat, I think the institutions promoting science have performed well during the pandemic, especially when compared with the moral and governmental institutions encouraging ethical behavior and making policies to promote justice.
My highest praise would be for the professionalism of health care workers. Nurses and physicians have staffed the hospitals and clinics caring for people when the hallways were overflowing for days without end. Without the commitment, the teamwork, and the courage to provide that care, the death toll would have been much higher and the suffering unimaginable. My observation is that these people were not motivated by an abstract primum non nocere, first do no harm. It was the commitment to love one’s neighbor and care for the sick. This dedication is the first most important thing in professionalism.
Part of what fuels that commitment is a belief that what they are doing makes a difference. The belief is stronger when there is measurable, scientific evidence that a difference is being made. The scientific decisions have not been perfect, but at this point the evidence is clear that the shutdown flattened the curve. Vaccines saved lives and will continue to do so. Masks saved lives. Nursing care, particularly intensive care, reduced the case fatality rate and assuaged suffering and grief.
What lessons about training new providers can be gleaned from the past 2 years? Those who teach professionalism for physicians, nurses, and other health care workers should strengthen the common value systems that undergird the commitment people have to the patients and the professions. In the face of postmodern nihilism and relativism, virtues need to be clarified and reinforced. In the face of political polarization which seeks to make a political affiliation the locus of loyalty and commitment, emphasize the fellowship of the health care professions.
To me as a scientist, a key lesson is that we need to be better at getting the science right. Two years ago I was wiping some groceries with alcohol and quarantining cans in shopping bags in the corner of the kitchen for 24 hours before shelving them. I still push elevator buttons with my knuckles. The Centers for Disease Control and Prevention needs to revamp their policy making procedures.
Institutions must work to reestablish the public trust in science. That is a challenge because while many amazing scientific advances have occurred (i.e., my MRI last week showed far more going on than my orthopedist and physical therapist detected based on clinical exam). Imaging such as MR and ultrasound have been major advances in diagnostic medicine, but there are also repeated examples demonstrating where medicine has been wrong. In the past 6 months I have read new guidelines for ear tubes, for neonatal jaundice, for newborn sepsis, and for newborn hypoglycemia. All indicate to me that my training 30 years ago was on target and the interval “improvements” in practice have been worthless Brownian motion based on false scientific discoveries. My recommendation would be that pediatrics do one-third as much research but do that research three times better and get it right.
Dr. Powell is a retired pediatric hospitalist and clinical ethics consultant living in St. Louis. Email him at pdnews@mdedge.com.
Get the science right. I have spent years researching and reflecting on what makes the best physicians, the best medicine, the optimal organized medical system, and the best medical ethics and law to support all of it. I have traveled to almost innumerable conferences to discuss these topics with colleagues who have similar goals. Time and time again, I come back to the conclusion that, in the modern era, the second-most important thing to do is to get the science right.
The practice of medicine in my Western world can be traced back to Hippocrates and earlier. The practice of nursing has other milestones. The healing arts have different points of origin in other cultures, such as China. In a modern world of mass communication, these various historical paths are converging on scientific evidence. The science to support medicine has always had flaws, but it has fared better than the other options. Sometimes, the science was so sketchy that the key was to believe in whatever the shaman was providing. But for the past 100 years, science, rather than tradition and hierarchy, has been relied upon to guide policy and action. For the past 50 years, evidence-based medicine has ascended. Have we become better than the snake oil salesmen of the late 19th century?
Modern health care is far from perfect. The pandemic has been a major stressor to the health care system. The pandemic has revealed flaws and weaknesses, including inequity in access to care, health illiteracy, and a shaky moral compass balancing individual liberty and social good. Overall, despite multiple mistakes dealing with a novel threat, I think the institutions promoting science have performed well during the pandemic, especially when compared with the moral and governmental institutions encouraging ethical behavior and making policies to promote justice.
My highest praise would be for the professionalism of health care workers. Nurses and physicians have staffed the hospitals and clinics caring for people when the hallways were overflowing for days without end. Without the commitment, the teamwork, and the courage to provide that care, the death toll would have been much higher and the suffering unimaginable. My observation is that these people were not motivated by an abstract primum non nocere, first do no harm. It was the commitment to love one’s neighbor and care for the sick. This dedication is the first most important thing in professionalism.
Part of what fuels that commitment is a belief that what they are doing makes a difference. The belief is stronger when there is measurable, scientific evidence that a difference is being made. The scientific decisions have not been perfect, but at this point the evidence is clear that the shutdown flattened the curve. Vaccines saved lives and will continue to do so. Masks saved lives. Nursing care, particularly intensive care, reduced the case fatality rate and assuaged suffering and grief.
What lessons about training new providers can be gleaned from the past 2 years? Those who teach professionalism for physicians, nurses, and other health care workers should strengthen the common value systems that undergird the commitment people have to the patients and the professions. In the face of postmodern nihilism and relativism, virtues need to be clarified and reinforced. In the face of political polarization which seeks to make a political affiliation the locus of loyalty and commitment, emphasize the fellowship of the health care professions.
To me as a scientist, a key lesson is that we need to be better at getting the science right. Two years ago I was wiping some groceries with alcohol and quarantining cans in shopping bags in the corner of the kitchen for 24 hours before shelving them. I still push elevator buttons with my knuckles. The Centers for Disease Control and Prevention needs to revamp their policy making procedures.
Institutions must work to reestablish the public trust in science. That is a challenge because while many amazing scientific advances have occurred (i.e., my MRI last week showed far more going on than my orthopedist and physical therapist detected based on clinical exam). Imaging such as MR and ultrasound have been major advances in diagnostic medicine, but there are also repeated examples demonstrating where medicine has been wrong. In the past 6 months I have read new guidelines for ear tubes, for neonatal jaundice, for newborn sepsis, and for newborn hypoglycemia. All indicate to me that my training 30 years ago was on target and the interval “improvements” in practice have been worthless Brownian motion based on false scientific discoveries. My recommendation would be that pediatrics do one-third as much research but do that research three times better and get it right.
Dr. Powell is a retired pediatric hospitalist and clinical ethics consultant living in St. Louis. Email him at pdnews@mdedge.com.
Get the science right. I have spent years researching and reflecting on what makes the best physicians, the best medicine, the optimal organized medical system, and the best medical ethics and law to support all of it. I have traveled to almost innumerable conferences to discuss these topics with colleagues who have similar goals. Time and time again, I come back to the conclusion that, in the modern era, the second-most important thing to do is to get the science right.
The practice of medicine in my Western world can be traced back to Hippocrates and earlier. The practice of nursing has other milestones. The healing arts have different points of origin in other cultures, such as China. In a modern world of mass communication, these various historical paths are converging on scientific evidence. The science to support medicine has always had flaws, but it has fared better than the other options. Sometimes, the science was so sketchy that the key was to believe in whatever the shaman was providing. But for the past 100 years, science, rather than tradition and hierarchy, has been relied upon to guide policy and action. For the past 50 years, evidence-based medicine has ascended. Have we become better than the snake oil salesmen of the late 19th century?
Modern health care is far from perfect. The pandemic has been a major stressor to the health care system. The pandemic has revealed flaws and weaknesses, including inequity in access to care, health illiteracy, and a shaky moral compass balancing individual liberty and social good. Overall, despite multiple mistakes dealing with a novel threat, I think the institutions promoting science have performed well during the pandemic, especially when compared with the moral and governmental institutions encouraging ethical behavior and making policies to promote justice.
My highest praise would be for the professionalism of health care workers. Nurses and physicians have staffed the hospitals and clinics caring for people when the hallways were overflowing for days without end. Without the commitment, the teamwork, and the courage to provide that care, the death toll would have been much higher and the suffering unimaginable. My observation is that these people were not motivated by an abstract primum non nocere, first do no harm. It was the commitment to love one’s neighbor and care for the sick. This dedication is the first most important thing in professionalism.
Part of what fuels that commitment is a belief that what they are doing makes a difference. The belief is stronger when there is measurable, scientific evidence that a difference is being made. The scientific decisions have not been perfect, but at this point the evidence is clear that the shutdown flattened the curve. Vaccines saved lives and will continue to do so. Masks saved lives. Nursing care, particularly intensive care, reduced the case fatality rate and assuaged suffering and grief.
What lessons about training new providers can be gleaned from the past 2 years? Those who teach professionalism for physicians, nurses, and other health care workers should strengthen the common value systems that undergird the commitment people have to the patients and the professions. In the face of postmodern nihilism and relativism, virtues need to be clarified and reinforced. In the face of political polarization which seeks to make a political affiliation the locus of loyalty and commitment, emphasize the fellowship of the health care professions.
To me as a scientist, a key lesson is that we need to be better at getting the science right. Two years ago I was wiping some groceries with alcohol and quarantining cans in shopping bags in the corner of the kitchen for 24 hours before shelving them. I still push elevator buttons with my knuckles. The Centers for Disease Control and Prevention needs to revamp their policy making procedures.
Institutions must work to reestablish the public trust in science. That is a challenge because while many amazing scientific advances have occurred (i.e., my MRI last week showed far more going on than my orthopedist and physical therapist detected based on clinical exam). Imaging such as MR and ultrasound have been major advances in diagnostic medicine, but there are also repeated examples demonstrating where medicine has been wrong. In the past 6 months I have read new guidelines for ear tubes, for neonatal jaundice, for newborn sepsis, and for newborn hypoglycemia. All indicate to me that my training 30 years ago was on target and the interval “improvements” in practice have been worthless Brownian motion based on false scientific discoveries. My recommendation would be that pediatrics do one-third as much research but do that research three times better and get it right.
Dr. Powell is a retired pediatric hospitalist and clinical ethics consultant living in St. Louis. Email him at pdnews@mdedge.com.
Smoking cessation could prevent a large proportion of MS cases
Key clinical point: At least 13% of cases of multiple sclerosis (MS) can be prevented if tobacco smoking is avoided, indicating the need for integrated programs aimed not only at smoking cessation but also at smoking prevention.
Major finding: The overall attributable fraction (AF) of MS because of smoking was 13.1% (95% CI 10.7%-15.4%), with AF being 0.6% (95% CI 0%-2%) in ex-smokers, indicating the beneficial effects of smoking cessation. Ever-smokers were at a 41% (95% CI 1.33%-1.50%) increased risk for MS than never smokers.
Study details: This was a population-based matched case-control study including 9,419 patients with MS and 9,419 matched control individuals.
Disclosures: No external funding was received for this study. The authors declared no conflicts of interest.
Source: Manouchehrinia A et al. Smoking attributable risk in multiple sclerosis. Front Immunol. 2022;13:840158 (Mar 3). Doi: 10.3389/fimmu.2022.840158
Key clinical point: At least 13% of cases of multiple sclerosis (MS) can be prevented if tobacco smoking is avoided, indicating the need for integrated programs aimed not only at smoking cessation but also at smoking prevention.
Major finding: The overall attributable fraction (AF) of MS because of smoking was 13.1% (95% CI 10.7%-15.4%), with AF being 0.6% (95% CI 0%-2%) in ex-smokers, indicating the beneficial effects of smoking cessation. Ever-smokers were at a 41% (95% CI 1.33%-1.50%) increased risk for MS than never smokers.
Study details: This was a population-based matched case-control study including 9,419 patients with MS and 9,419 matched control individuals.
Disclosures: No external funding was received for this study. The authors declared no conflicts of interest.
Source: Manouchehrinia A et al. Smoking attributable risk in multiple sclerosis. Front Immunol. 2022;13:840158 (Mar 3). Doi: 10.3389/fimmu.2022.840158
Key clinical point: At least 13% of cases of multiple sclerosis (MS) can be prevented if tobacco smoking is avoided, indicating the need for integrated programs aimed not only at smoking cessation but also at smoking prevention.
Major finding: The overall attributable fraction (AF) of MS because of smoking was 13.1% (95% CI 10.7%-15.4%), with AF being 0.6% (95% CI 0%-2%) in ex-smokers, indicating the beneficial effects of smoking cessation. Ever-smokers were at a 41% (95% CI 1.33%-1.50%) increased risk for MS than never smokers.
Study details: This was a population-based matched case-control study including 9,419 patients with MS and 9,419 matched control individuals.
Disclosures: No external funding was received for this study. The authors declared no conflicts of interest.
Source: Manouchehrinia A et al. Smoking attributable risk in multiple sclerosis. Front Immunol. 2022;13:840158 (Mar 3). Doi: 10.3389/fimmu.2022.840158
RMS: Extended ofatumumab treatment presents favorable benefit-risk profile in ALITHIOS study
Key clinical point: Extended treatment with ofatumumab for up to 3.5 years was well tolerated without any new risks in patients with relapsing multiple sclerosis (RMS).
Major finding: Overall, 83.8% and 9.7% of patients experienced at least 1 adverse event (AE) and serious AE, respectively. Systemic injection-related reactions, infections, and malignancies were reported in 24.8%, 54.3%, and 0.3% of patients, respectively. In most patients, the mean serum immunoglobulin (Ig) G and IgM levels were stable and above the lower limit of normal and the risk for serious infections was low.
Study details: Findings are from the ongoing phase 3b ALITHIOS umbrella extension trial involving 1,969 patients with RMS who completed ASCLEPIOS I/II, APLIOS, or APOLITOS trial and continued or switched to ofatumumab in ALITHIOS.
Disclosures: This study was funded by Novartis Pharma AG (Basel, Switzerland). The authors declared receiving consultancy fees, personal compensation, travel reimbursement, research support, or serving on advisory boards for various sources including Novartis Pharma AG. Some authors declared being employees of Novartis Pharma AG.
Source: Hauser SL et al. Safety experience with continued exposure to ofatumumab in patients with relapsing forms of multiple sclerosis for up to 3.5 years. Mult Scler. 2022 (Mar 1). Doi: 10.1177/13524585221079731
Key clinical point: Extended treatment with ofatumumab for up to 3.5 years was well tolerated without any new risks in patients with relapsing multiple sclerosis (RMS).
Major finding: Overall, 83.8% and 9.7% of patients experienced at least 1 adverse event (AE) and serious AE, respectively. Systemic injection-related reactions, infections, and malignancies were reported in 24.8%, 54.3%, and 0.3% of patients, respectively. In most patients, the mean serum immunoglobulin (Ig) G and IgM levels were stable and above the lower limit of normal and the risk for serious infections was low.
Study details: Findings are from the ongoing phase 3b ALITHIOS umbrella extension trial involving 1,969 patients with RMS who completed ASCLEPIOS I/II, APLIOS, or APOLITOS trial and continued or switched to ofatumumab in ALITHIOS.
Disclosures: This study was funded by Novartis Pharma AG (Basel, Switzerland). The authors declared receiving consultancy fees, personal compensation, travel reimbursement, research support, or serving on advisory boards for various sources including Novartis Pharma AG. Some authors declared being employees of Novartis Pharma AG.
Source: Hauser SL et al. Safety experience with continued exposure to ofatumumab in patients with relapsing forms of multiple sclerosis for up to 3.5 years. Mult Scler. 2022 (Mar 1). Doi: 10.1177/13524585221079731
Key clinical point: Extended treatment with ofatumumab for up to 3.5 years was well tolerated without any new risks in patients with relapsing multiple sclerosis (RMS).
Major finding: Overall, 83.8% and 9.7% of patients experienced at least 1 adverse event (AE) and serious AE, respectively. Systemic injection-related reactions, infections, and malignancies were reported in 24.8%, 54.3%, and 0.3% of patients, respectively. In most patients, the mean serum immunoglobulin (Ig) G and IgM levels were stable and above the lower limit of normal and the risk for serious infections was low.
Study details: Findings are from the ongoing phase 3b ALITHIOS umbrella extension trial involving 1,969 patients with RMS who completed ASCLEPIOS I/II, APLIOS, or APOLITOS trial and continued or switched to ofatumumab in ALITHIOS.
Disclosures: This study was funded by Novartis Pharma AG (Basel, Switzerland). The authors declared receiving consultancy fees, personal compensation, travel reimbursement, research support, or serving on advisory boards for various sources including Novartis Pharma AG. Some authors declared being employees of Novartis Pharma AG.
Source: Hauser SL et al. Safety experience with continued exposure to ofatumumab in patients with relapsing forms of multiple sclerosis for up to 3.5 years. Mult Scler. 2022 (Mar 1). Doi: 10.1177/13524585221079731
Multiple sclerosis: Discontinuing fingolimod improves humoral response after SARS-CoV-2 vaccination
Key clinical point: Short-term fingolimod discontinuation until the absolute lymphocyte count increases to >1,000 cells/mm3 may improve the SARS-CoV-2 mRNA vaccine-specific humoral response in patients with multiple sclerosis (MS) but not the adaptive cellular response.
Major finding: Overall, 80% vs. 20% of patients in the fingolimod-discontinuation vs. fingolimod-continuation group developed a positive humoral response against SARS-CoV-2 1 month after the third vaccine dose, with a significantly higher median immunoglobulin (Ig) G titer in the fingolimod-discontinuation vs. fingolimod-continuation group (202.3 vs. 26.4 binding antibody units/mL; P = .022).
Study details: This was a prospective monocentric 3-month randomized clinical trial involving 20 patients with relapsing-remitting MS on fingolimod therapy who received the third dose of BNT162b2 vaccine after failing to develop a humoral IgG immune response to the previous 2 doses and were randomly assigned to the fingolimod-continuation or fingolimod-discontinuation group.
Disclosures: This study was supported by Sheba Multiple Sclerosis Research Grant. The authors declared no conflicts of interest.
Source: Achiron A et al. Immune response to the third COVID-19 vaccine dose is related to lymphocyte count in multiple sclerosis patients treated with fingolimod. J Neurol. 2022 (Mar 2). Doi: 10.1007/s00415-022-11030-0
Key clinical point: Short-term fingolimod discontinuation until the absolute lymphocyte count increases to >1,000 cells/mm3 may improve the SARS-CoV-2 mRNA vaccine-specific humoral response in patients with multiple sclerosis (MS) but not the adaptive cellular response.
Major finding: Overall, 80% vs. 20% of patients in the fingolimod-discontinuation vs. fingolimod-continuation group developed a positive humoral response against SARS-CoV-2 1 month after the third vaccine dose, with a significantly higher median immunoglobulin (Ig) G titer in the fingolimod-discontinuation vs. fingolimod-continuation group (202.3 vs. 26.4 binding antibody units/mL; P = .022).
Study details: This was a prospective monocentric 3-month randomized clinical trial involving 20 patients with relapsing-remitting MS on fingolimod therapy who received the third dose of BNT162b2 vaccine after failing to develop a humoral IgG immune response to the previous 2 doses and were randomly assigned to the fingolimod-continuation or fingolimod-discontinuation group.
Disclosures: This study was supported by Sheba Multiple Sclerosis Research Grant. The authors declared no conflicts of interest.
Source: Achiron A et al. Immune response to the third COVID-19 vaccine dose is related to lymphocyte count in multiple sclerosis patients treated with fingolimod. J Neurol. 2022 (Mar 2). Doi: 10.1007/s00415-022-11030-0
Key clinical point: Short-term fingolimod discontinuation until the absolute lymphocyte count increases to >1,000 cells/mm3 may improve the SARS-CoV-2 mRNA vaccine-specific humoral response in patients with multiple sclerosis (MS) but not the adaptive cellular response.
Major finding: Overall, 80% vs. 20% of patients in the fingolimod-discontinuation vs. fingolimod-continuation group developed a positive humoral response against SARS-CoV-2 1 month after the third vaccine dose, with a significantly higher median immunoglobulin (Ig) G titer in the fingolimod-discontinuation vs. fingolimod-continuation group (202.3 vs. 26.4 binding antibody units/mL; P = .022).
Study details: This was a prospective monocentric 3-month randomized clinical trial involving 20 patients with relapsing-remitting MS on fingolimod therapy who received the third dose of BNT162b2 vaccine after failing to develop a humoral IgG immune response to the previous 2 doses and were randomly assigned to the fingolimod-continuation or fingolimod-discontinuation group.
Disclosures: This study was supported by Sheba Multiple Sclerosis Research Grant. The authors declared no conflicts of interest.
Source: Achiron A et al. Immune response to the third COVID-19 vaccine dose is related to lymphocyte count in multiple sclerosis patients treated with fingolimod. J Neurol. 2022 (Mar 2). Doi: 10.1007/s00415-022-11030-0
Flu vaccination does not increase risk for infections or relapse in MS
Key clinical point: Vaccination against influenza was well tolerated in patients with multiple sclerosis (MS) who mainly experienced short-term nonserious adverse events following immunization (AEFI), with the risk for MS relapse not being significantly different than those who were not vaccinated.
Major finding: Overall, 60.2% of patients did not experience any vaccine-related AEFIs, with pain at the injection site (68.1%), headache (10.6%), flu-like symptoms (17%), and fatigue (4.3%) being the major nonserious short-term AEFIs. The long-term AEFIs included flu-like symptoms, COVID-19, and MS relapse, with incidences of infection or MS relapse (P = .65) and cumulative survival rate (P = .21) not being significantly different between the vaccinated and unvaccinated groups.
Study details: This was a single-center, prospective, vaccination-vigilance trial including 194 patients with MS, of whom 113 patients received any of the recommended flu vaccines and 81 did not.
Disclosures: The study received no external funding. GT Maniscalco declared serving on speaking and advisory boards and receiving speaker fees from various sources. Other authors declared no conflicts of interest.
Source: Maniscalco GT et al. Flu vaccination in multiple sclerosis patients: A monocentric prospective vaccine-vigilance study. Expert Opin Drug Saf. 2022 (Feb 22). Doi: 10.1080/14740338.2022.2044787
Key clinical point: Vaccination against influenza was well tolerated in patients with multiple sclerosis (MS) who mainly experienced short-term nonserious adverse events following immunization (AEFI), with the risk for MS relapse not being significantly different than those who were not vaccinated.
Major finding: Overall, 60.2% of patients did not experience any vaccine-related AEFIs, with pain at the injection site (68.1%), headache (10.6%), flu-like symptoms (17%), and fatigue (4.3%) being the major nonserious short-term AEFIs. The long-term AEFIs included flu-like symptoms, COVID-19, and MS relapse, with incidences of infection or MS relapse (P = .65) and cumulative survival rate (P = .21) not being significantly different between the vaccinated and unvaccinated groups.
Study details: This was a single-center, prospective, vaccination-vigilance trial including 194 patients with MS, of whom 113 patients received any of the recommended flu vaccines and 81 did not.
Disclosures: The study received no external funding. GT Maniscalco declared serving on speaking and advisory boards and receiving speaker fees from various sources. Other authors declared no conflicts of interest.
Source: Maniscalco GT et al. Flu vaccination in multiple sclerosis patients: A monocentric prospective vaccine-vigilance study. Expert Opin Drug Saf. 2022 (Feb 22). Doi: 10.1080/14740338.2022.2044787
Key clinical point: Vaccination against influenza was well tolerated in patients with multiple sclerosis (MS) who mainly experienced short-term nonserious adverse events following immunization (AEFI), with the risk for MS relapse not being significantly different than those who were not vaccinated.
Major finding: Overall, 60.2% of patients did not experience any vaccine-related AEFIs, with pain at the injection site (68.1%), headache (10.6%), flu-like symptoms (17%), and fatigue (4.3%) being the major nonserious short-term AEFIs. The long-term AEFIs included flu-like symptoms, COVID-19, and MS relapse, with incidences of infection or MS relapse (P = .65) and cumulative survival rate (P = .21) not being significantly different between the vaccinated and unvaccinated groups.
Study details: This was a single-center, prospective, vaccination-vigilance trial including 194 patients with MS, of whom 113 patients received any of the recommended flu vaccines and 81 did not.
Disclosures: The study received no external funding. GT Maniscalco declared serving on speaking and advisory boards and receiving speaker fees from various sources. Other authors declared no conflicts of interest.
Source: Maniscalco GT et al. Flu vaccination in multiple sclerosis patients: A monocentric prospective vaccine-vigilance study. Expert Opin Drug Saf. 2022 (Feb 22). Doi: 10.1080/14740338.2022.2044787
Hormone therapy use and disability accrual in women with MS
Key clinical point: Over 22 years of follow-up found no association between the use of hormone therapy (HT) and the risk for disability accrual in women with multiple sclerosis (MS) treated with a disease-modifying therapy (DMT) when used for <5 years.
Major finding: Overall, current HT use vs. no use was not associated with a significantly higher risk for disability accrual; however, the risk of reaching 6-month confirmed and sustained Expanded Disability Status Scale 4 increased from 0.6 (95% CI 0.3-1.2) after <1 year of use to 1.4 (95% CI 0.9-2.2) after >5 years of HT use vs. no use.
Study details: The data come from a nationwide, population-based cohort study of 3,325 women with relapsing-remitting MS treated with DMT.
Disclosures: This study received no external funding. TI Kopp revealed his role as an adviser for Novartis and received Biogen's sponsorship for congress participation. M Magyari declared serving as an advisor and receiving honoraria for lecturing and research support for congress participation from various sources. Ø Lidegaard had no conflicts of interest.
Source: Kopp TI et al. Hormone therapy and disease activity in Danish women with multiple sclerosis: A population-based cohort study. Eur J Neurol. 2022 (Feb 23). Doi: 10.1111/ene.15299
Key clinical point: Over 22 years of follow-up found no association between the use of hormone therapy (HT) and the risk for disability accrual in women with multiple sclerosis (MS) treated with a disease-modifying therapy (DMT) when used for <5 years.
Major finding: Overall, current HT use vs. no use was not associated with a significantly higher risk for disability accrual; however, the risk of reaching 6-month confirmed and sustained Expanded Disability Status Scale 4 increased from 0.6 (95% CI 0.3-1.2) after <1 year of use to 1.4 (95% CI 0.9-2.2) after >5 years of HT use vs. no use.
Study details: The data come from a nationwide, population-based cohort study of 3,325 women with relapsing-remitting MS treated with DMT.
Disclosures: This study received no external funding. TI Kopp revealed his role as an adviser for Novartis and received Biogen's sponsorship for congress participation. M Magyari declared serving as an advisor and receiving honoraria for lecturing and research support for congress participation from various sources. Ø Lidegaard had no conflicts of interest.
Source: Kopp TI et al. Hormone therapy and disease activity in Danish women with multiple sclerosis: A population-based cohort study. Eur J Neurol. 2022 (Feb 23). Doi: 10.1111/ene.15299
Key clinical point: Over 22 years of follow-up found no association between the use of hormone therapy (HT) and the risk for disability accrual in women with multiple sclerosis (MS) treated with a disease-modifying therapy (DMT) when used for <5 years.
Major finding: Overall, current HT use vs. no use was not associated with a significantly higher risk for disability accrual; however, the risk of reaching 6-month confirmed and sustained Expanded Disability Status Scale 4 increased from 0.6 (95% CI 0.3-1.2) after <1 year of use to 1.4 (95% CI 0.9-2.2) after >5 years of HT use vs. no use.
Study details: The data come from a nationwide, population-based cohort study of 3,325 women with relapsing-remitting MS treated with DMT.
Disclosures: This study received no external funding. TI Kopp revealed his role as an adviser for Novartis and received Biogen's sponsorship for congress participation. M Magyari declared serving as an advisor and receiving honoraria for lecturing and research support for congress participation from various sources. Ø Lidegaard had no conflicts of interest.
Source: Kopp TI et al. Hormone therapy and disease activity in Danish women with multiple sclerosis: A population-based cohort study. Eur J Neurol. 2022 (Feb 23). Doi: 10.1111/ene.15299
Purulent Nodule on the Mandible
The Diagnosis: Odontogenic Cutaneous Sinus Tract
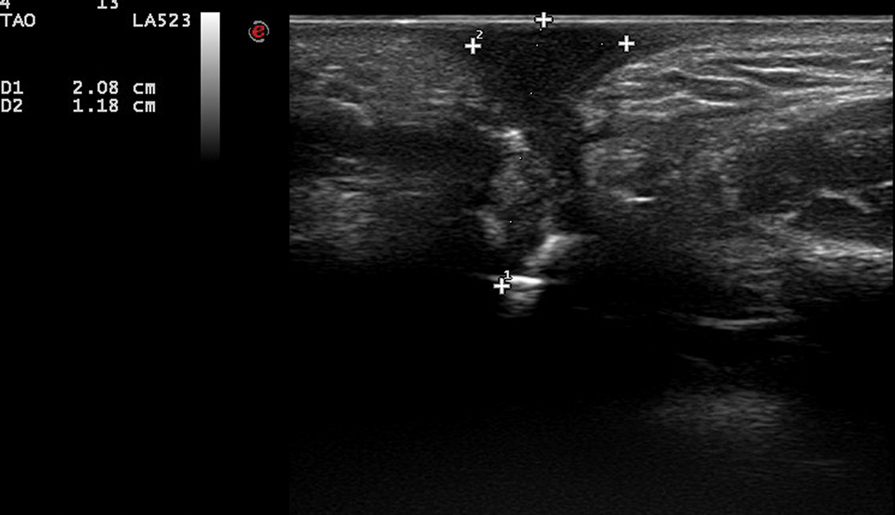
In our patient, panoramic radiography showed a radiolucency in the periapex of the mandibular first molar (Figure 1). Ultrasonography depicted a hypoechoic band that originated from the cutaneous lesion and extended through the subcutaneous tissue to the defective alveolar bone, suggesting odontogenic inflammation (Figure 2).1 The infected pulp was removed, and the purulent nodules then disappeared.
The dental etiology of odontogenic cutaneous sinus tracts can be confirmed by panoramic radiography and ultrasonography. The odontogenic sinus path can be clearly observed via radiography by injecting or inserting a radiopaque substance into the sinus tract.2 Effective treatment of the diseased tooth is removal of the infected pulp, performance of a root canal to eliminate infection, closure and filling of the root canal, and repair of the crown. Once the source of infection is eliminated, the sinus typically subsides within 2 weeks. When residual skin retreats or scars are present, cosmetic surgery can be performed to improve the appearance.3,4
Odontogenic cutaneous sinus tracts usually are caused by a route of drainage from a chronic apical abscess. They follow a path of least resistance through the alveolar bone and periosteum, spreading into the surrounding soft tissues. With the formation of abscesses, sinus tracts will erupt intraorally or cutaneously, depending on the relationship of the posterior tooth apices to the mandibular attachments of the mylohyoid and buccinator muscles and the maxillary attachment of the buccinator.2,5 Clinically, cutaneous lesions present as nodules, cysts, or dimples that have attached to deep tissues through the sinus tract. Half of patients may have no dental symptoms and often are misdiagnosed with nonodontogenic lesions. Subsequent improper treatments, such as repeated use of antibiotics, multiple biopsies, surgical excision, and chemotherapy, often are repeated and ineffective.6 The most common cause of chronic cutaneous sinus tracts in the face and neck is a chronically draining dental infection.2,5 A thorough history is necessary when odontogenic cutaneous sinuses are suspected. Toothache before the development of the sinus tract is an important diagnostic clue.
Pyogenic granuloma, syringocystadenoma papilliferum, osteomyelitis, infected epidermoid cyst, actinomycoses, and salivary gland fistula also should be considered in the differential diagnosis.7-10 Pyogenic granuloma (also known as lobular capillary hemangioma) is a benign overgrowth of capillaries showing a vascular phenotype that usually occurs as a response to different stimulating factors such as local stimuli, trauma, or hormonal factors. Clinically, pyogenic granuloma presents as a red, solitary, painless nodule on the face or distal extremities.11,12 Syringocystadenoma papilliferum is a benign adnexal proliferation with apocrine differentiation that usually presents as a hairless papillomatous plaque or nodule measuring 1 to 4 cm in diameter and often is first noted at birth or during early childhood.7 Osteomyelitis is progressive inflammation of the periosteum and bone marrow that rapidly breaks through the periosteum and spreads to surrounding areas. The mandible is the most susceptible bone for facial osteomyelitis.8 Epidermoid cysts are formed by the proliferation of epidermal cells within a circumscribed dermal space. Infection of the cysts is characterized by redness, swelling, heat, and pain. As the infection progresses, suppurative inflammation develops, leading to local liquefaction and abscesses.9
This case was initially misdiagnosed as infectious skin lesions by outside clinicians. Multiple surgical treatments and long-term antibiotic therapy were attempted before the correct diagnosis was made. The clinical diagnosis of odontogenic cutaneous sinus tracts is challenging due to the variety of affected sites and clinical signs. Ultrasonography should be performed as early as possible to identify the disease and avoid unnecessary surgery. For appropriate dental therapy, close liaison with the stomatology department is warranted.
- Shobatake C, Miyagawa F, Fukumoto T, et al. Usefulness of ultrasonography for rapidly diagnosing cutaneous sinus tracts of dental origin. Eur J Dermatol. 2014;24:683-687.
- Cioffi GA, Terezhalmy GT, Parlette HL. Cutaneous draining sinus tract: an odontogenic etiology. J Am Acad Dermatol. 1986;14:94-100.
- McWalter GM, Alexander JB, del Rio CE, et al. Cutaneous sinus tracts of dental etiology. Oral Surg Oral Med Oral Pathol. 1988;66:608-614.
- Spear KL, Sheridan PJ, Perry HO. Sinus tracts to the chin and jaw of dental origin. J Am Acad Dermatol. 1983;8:486-492.
- Lewin-Epstein J, Taicher S, Azaz B. Cutaneous sinus tracts of dental origin. Arch Dermatol. 1978;114:1158-1161.
- Mittal N, Gupta P. Management of extraoral sinus cases: a clinical dilemma. J Endod. 2004;30:541-547.
- Alegria-Landa V, Jo-Velasco M, Santonja C, et al. Syringocystadenoma papilliferum associated with verrucous carcinoma of the skin in the same lesion: report of four cases. J Cutan Pathol. 2020;47:12-16.
- Prasad KC, Prasad SC, Mouli N, et al. Osteomyelitis in the head and neck. Acta Otolaryngol. 2007;127:194-205.
- Hong SH, Chung HW, Choi JY, et al. MRI findings of subcutaneous epidermal cysts: emphasis on the presence of rupture. AJR Am J Roentgenol. 2006;186:961-966.
- Gefrerer L, Popowski W, Perek JN, et al. Recurrent pyogenic granuloma around dental implants: a rare case report. Int J Periodontics Restorative Dent. 2016;36:573-581.
- Chae JB, Park JT, Kim BR, et al. Agminated eruptive pyogenic granuloma on chin following redundant needle injections. J Dermatol. 2016;43:577-578.
- Thompson LD. Lobular capillary hemangioma (pyogenic granuloma) of the oral cavity. Ear Nose Throat J. 2017;96:240.
The Diagnosis: Odontogenic Cutaneous Sinus Tract
In our patient, panoramic radiography showed a radiolucency in the periapex of the mandibular first molar (Figure 1). Ultrasonography depicted a hypoechoic band that originated from the cutaneous lesion and extended through the subcutaneous tissue to the defective alveolar bone, suggesting odontogenic inflammation (Figure 2).1 The infected pulp was removed, and the purulent nodules then disappeared.
The dental etiology of odontogenic cutaneous sinus tracts can be confirmed by panoramic radiography and ultrasonography. The odontogenic sinus path can be clearly observed via radiography by injecting or inserting a radiopaque substance into the sinus tract.2 Effective treatment of the diseased tooth is removal of the infected pulp, performance of a root canal to eliminate infection, closure and filling of the root canal, and repair of the crown. Once the source of infection is eliminated, the sinus typically subsides within 2 weeks. When residual skin retreats or scars are present, cosmetic surgery can be performed to improve the appearance.3,4
Odontogenic cutaneous sinus tracts usually are caused by a route of drainage from a chronic apical abscess. They follow a path of least resistance through the alveolar bone and periosteum, spreading into the surrounding soft tissues. With the formation of abscesses, sinus tracts will erupt intraorally or cutaneously, depending on the relationship of the posterior tooth apices to the mandibular attachments of the mylohyoid and buccinator muscles and the maxillary attachment of the buccinator.2,5 Clinically, cutaneous lesions present as nodules, cysts, or dimples that have attached to deep tissues through the sinus tract. Half of patients may have no dental symptoms and often are misdiagnosed with nonodontogenic lesions. Subsequent improper treatments, such as repeated use of antibiotics, multiple biopsies, surgical excision, and chemotherapy, often are repeated and ineffective.6 The most common cause of chronic cutaneous sinus tracts in the face and neck is a chronically draining dental infection.2,5 A thorough history is necessary when odontogenic cutaneous sinuses are suspected. Toothache before the development of the sinus tract is an important diagnostic clue.
Pyogenic granuloma, syringocystadenoma papilliferum, osteomyelitis, infected epidermoid cyst, actinomycoses, and salivary gland fistula also should be considered in the differential diagnosis.7-10 Pyogenic granuloma (also known as lobular capillary hemangioma) is a benign overgrowth of capillaries showing a vascular phenotype that usually occurs as a response to different stimulating factors such as local stimuli, trauma, or hormonal factors. Clinically, pyogenic granuloma presents as a red, solitary, painless nodule on the face or distal extremities.11,12 Syringocystadenoma papilliferum is a benign adnexal proliferation with apocrine differentiation that usually presents as a hairless papillomatous plaque or nodule measuring 1 to 4 cm in diameter and often is first noted at birth or during early childhood.7 Osteomyelitis is progressive inflammation of the periosteum and bone marrow that rapidly breaks through the periosteum and spreads to surrounding areas. The mandible is the most susceptible bone for facial osteomyelitis.8 Epidermoid cysts are formed by the proliferation of epidermal cells within a circumscribed dermal space. Infection of the cysts is characterized by redness, swelling, heat, and pain. As the infection progresses, suppurative inflammation develops, leading to local liquefaction and abscesses.9
This case was initially misdiagnosed as infectious skin lesions by outside clinicians. Multiple surgical treatments and long-term antibiotic therapy were attempted before the correct diagnosis was made. The clinical diagnosis of odontogenic cutaneous sinus tracts is challenging due to the variety of affected sites and clinical signs. Ultrasonography should be performed as early as possible to identify the disease and avoid unnecessary surgery. For appropriate dental therapy, close liaison with the stomatology department is warranted.
The Diagnosis: Odontogenic Cutaneous Sinus Tract
In our patient, panoramic radiography showed a radiolucency in the periapex of the mandibular first molar (Figure 1). Ultrasonography depicted a hypoechoic band that originated from the cutaneous lesion and extended through the subcutaneous tissue to the defective alveolar bone, suggesting odontogenic inflammation (Figure 2).1 The infected pulp was removed, and the purulent nodules then disappeared.
The dental etiology of odontogenic cutaneous sinus tracts can be confirmed by panoramic radiography and ultrasonography. The odontogenic sinus path can be clearly observed via radiography by injecting or inserting a radiopaque substance into the sinus tract.2 Effective treatment of the diseased tooth is removal of the infected pulp, performance of a root canal to eliminate infection, closure and filling of the root canal, and repair of the crown. Once the source of infection is eliminated, the sinus typically subsides within 2 weeks. When residual skin retreats or scars are present, cosmetic surgery can be performed to improve the appearance.3,4
Odontogenic cutaneous sinus tracts usually are caused by a route of drainage from a chronic apical abscess. They follow a path of least resistance through the alveolar bone and periosteum, spreading into the surrounding soft tissues. With the formation of abscesses, sinus tracts will erupt intraorally or cutaneously, depending on the relationship of the posterior tooth apices to the mandibular attachments of the mylohyoid and buccinator muscles and the maxillary attachment of the buccinator.2,5 Clinically, cutaneous lesions present as nodules, cysts, or dimples that have attached to deep tissues through the sinus tract. Half of patients may have no dental symptoms and often are misdiagnosed with nonodontogenic lesions. Subsequent improper treatments, such as repeated use of antibiotics, multiple biopsies, surgical excision, and chemotherapy, often are repeated and ineffective.6 The most common cause of chronic cutaneous sinus tracts in the face and neck is a chronically draining dental infection.2,5 A thorough history is necessary when odontogenic cutaneous sinuses are suspected. Toothache before the development of the sinus tract is an important diagnostic clue.
Pyogenic granuloma, syringocystadenoma papilliferum, osteomyelitis, infected epidermoid cyst, actinomycoses, and salivary gland fistula also should be considered in the differential diagnosis.7-10 Pyogenic granuloma (also known as lobular capillary hemangioma) is a benign overgrowth of capillaries showing a vascular phenotype that usually occurs as a response to different stimulating factors such as local stimuli, trauma, or hormonal factors. Clinically, pyogenic granuloma presents as a red, solitary, painless nodule on the face or distal extremities.11,12 Syringocystadenoma papilliferum is a benign adnexal proliferation with apocrine differentiation that usually presents as a hairless papillomatous plaque or nodule measuring 1 to 4 cm in diameter and often is first noted at birth or during early childhood.7 Osteomyelitis is progressive inflammation of the periosteum and bone marrow that rapidly breaks through the periosteum and spreads to surrounding areas. The mandible is the most susceptible bone for facial osteomyelitis.8 Epidermoid cysts are formed by the proliferation of epidermal cells within a circumscribed dermal space. Infection of the cysts is characterized by redness, swelling, heat, and pain. As the infection progresses, suppurative inflammation develops, leading to local liquefaction and abscesses.9
This case was initially misdiagnosed as infectious skin lesions by outside clinicians. Multiple surgical treatments and long-term antibiotic therapy were attempted before the correct diagnosis was made. The clinical diagnosis of odontogenic cutaneous sinus tracts is challenging due to the variety of affected sites and clinical signs. Ultrasonography should be performed as early as possible to identify the disease and avoid unnecessary surgery. For appropriate dental therapy, close liaison with the stomatology department is warranted.
- Shobatake C, Miyagawa F, Fukumoto T, et al. Usefulness of ultrasonography for rapidly diagnosing cutaneous sinus tracts of dental origin. Eur J Dermatol. 2014;24:683-687.
- Cioffi GA, Terezhalmy GT, Parlette HL. Cutaneous draining sinus tract: an odontogenic etiology. J Am Acad Dermatol. 1986;14:94-100.
- McWalter GM, Alexander JB, del Rio CE, et al. Cutaneous sinus tracts of dental etiology. Oral Surg Oral Med Oral Pathol. 1988;66:608-614.
- Spear KL, Sheridan PJ, Perry HO. Sinus tracts to the chin and jaw of dental origin. J Am Acad Dermatol. 1983;8:486-492.
- Lewin-Epstein J, Taicher S, Azaz B. Cutaneous sinus tracts of dental origin. Arch Dermatol. 1978;114:1158-1161.
- Mittal N, Gupta P. Management of extraoral sinus cases: a clinical dilemma. J Endod. 2004;30:541-547.
- Alegria-Landa V, Jo-Velasco M, Santonja C, et al. Syringocystadenoma papilliferum associated with verrucous carcinoma of the skin in the same lesion: report of four cases. J Cutan Pathol. 2020;47:12-16.
- Prasad KC, Prasad SC, Mouli N, et al. Osteomyelitis in the head and neck. Acta Otolaryngol. 2007;127:194-205.
- Hong SH, Chung HW, Choi JY, et al. MRI findings of subcutaneous epidermal cysts: emphasis on the presence of rupture. AJR Am J Roentgenol. 2006;186:961-966.
- Gefrerer L, Popowski W, Perek JN, et al. Recurrent pyogenic granuloma around dental implants: a rare case report. Int J Periodontics Restorative Dent. 2016;36:573-581.
- Chae JB, Park JT, Kim BR, et al. Agminated eruptive pyogenic granuloma on chin following redundant needle injections. J Dermatol. 2016;43:577-578.
- Thompson LD. Lobular capillary hemangioma (pyogenic granuloma) of the oral cavity. Ear Nose Throat J. 2017;96:240.
- Shobatake C, Miyagawa F, Fukumoto T, et al. Usefulness of ultrasonography for rapidly diagnosing cutaneous sinus tracts of dental origin. Eur J Dermatol. 2014;24:683-687.
- Cioffi GA, Terezhalmy GT, Parlette HL. Cutaneous draining sinus tract: an odontogenic etiology. J Am Acad Dermatol. 1986;14:94-100.
- McWalter GM, Alexander JB, del Rio CE, et al. Cutaneous sinus tracts of dental etiology. Oral Surg Oral Med Oral Pathol. 1988;66:608-614.
- Spear KL, Sheridan PJ, Perry HO. Sinus tracts to the chin and jaw of dental origin. J Am Acad Dermatol. 1983;8:486-492.
- Lewin-Epstein J, Taicher S, Azaz B. Cutaneous sinus tracts of dental origin. Arch Dermatol. 1978;114:1158-1161.
- Mittal N, Gupta P. Management of extraoral sinus cases: a clinical dilemma. J Endod. 2004;30:541-547.
- Alegria-Landa V, Jo-Velasco M, Santonja C, et al. Syringocystadenoma papilliferum associated with verrucous carcinoma of the skin in the same lesion: report of four cases. J Cutan Pathol. 2020;47:12-16.
- Prasad KC, Prasad SC, Mouli N, et al. Osteomyelitis in the head and neck. Acta Otolaryngol. 2007;127:194-205.
- Hong SH, Chung HW, Choi JY, et al. MRI findings of subcutaneous epidermal cysts: emphasis on the presence of rupture. AJR Am J Roentgenol. 2006;186:961-966.
- Gefrerer L, Popowski W, Perek JN, et al. Recurrent pyogenic granuloma around dental implants: a rare case report. Int J Periodontics Restorative Dent. 2016;36:573-581.
- Chae JB, Park JT, Kim BR, et al. Agminated eruptive pyogenic granuloma on chin following redundant needle injections. J Dermatol. 2016;43:577-578.
- Thompson LD. Lobular capillary hemangioma (pyogenic granuloma) of the oral cavity. Ear Nose Throat J. 2017;96:240.
A 27-year-old man presented with a recurrent nodule with purulent discharge on the mandible of 3 months’ duration. He underwent several surgical excisions before he was referred to our outpatient clinic, but each time the lesion recurred. The patient was otherwise healthy with no associated discomfort. He denied exposure to animals or ticks, and he did not have a family history of similar lesions. He had a root canal treatment several years prior to the current presentation. Physical examination revealed 2 contiguous nodules with purulent secretions on the left mandible.
Masitinib at 4.5 mg/kg/day shows promise in progressive forms of multiple sclerosis
Key clinical point: Masitinib at a dose of 4.5 mg/kg/day may benefit patients with primary progressive multiple sclerosis (PPMS) or nonactive secondary progressive multiple sclerosis (nSPMS).
Major finding: The Expanded Disability Status Scale(EDSS)-based disability worsening was slower with 4.5 mg/kg/day masitinib 4.5 mg/kg/day vs. placebo (change in EDSS 0.001 vs. 0.098), with a between-group difference of −0.097 (P = .027). No new safety signals were identified.
Study details: The findings come from the 96-week, phase 3 Study AB07002 trial involving 611 patients with PPMS or nSPMS who were randomly assigned to parallel groups of either 4.5 mg/kg/day masitinib, 6 mg/kg/day uptitrated masitinib, or an equivalent placebo.
Disclosures: This study was funded by AB Science, Paris, France. A Moussy, C Mansfield, and O Hermine reported being employees and shareholders of AB Science, and the other authors reported receiving research support and nonfinancial support or personal fees from various sources, including AB Science.
Source: Vermersch P et al, on behalf of the AB07002 Study Group. Efficacy and safety of masitinib in progressive forms of multiple sclerosis: A randomized, phase 3, clinical trial. Neurol Neuroimmunol Neuroinflamm. 2022;9(3):e1148 (Feb 21). Doi: 10.1212/NXI.0000000000001148
Key clinical point: Masitinib at a dose of 4.5 mg/kg/day may benefit patients with primary progressive multiple sclerosis (PPMS) or nonactive secondary progressive multiple sclerosis (nSPMS).
Major finding: The Expanded Disability Status Scale(EDSS)-based disability worsening was slower with 4.5 mg/kg/day masitinib 4.5 mg/kg/day vs. placebo (change in EDSS 0.001 vs. 0.098), with a between-group difference of −0.097 (P = .027). No new safety signals were identified.
Study details: The findings come from the 96-week, phase 3 Study AB07002 trial involving 611 patients with PPMS or nSPMS who were randomly assigned to parallel groups of either 4.5 mg/kg/day masitinib, 6 mg/kg/day uptitrated masitinib, or an equivalent placebo.
Disclosures: This study was funded by AB Science, Paris, France. A Moussy, C Mansfield, and O Hermine reported being employees and shareholders of AB Science, and the other authors reported receiving research support and nonfinancial support or personal fees from various sources, including AB Science.
Source: Vermersch P et al, on behalf of the AB07002 Study Group. Efficacy and safety of masitinib in progressive forms of multiple sclerosis: A randomized, phase 3, clinical trial. Neurol Neuroimmunol Neuroinflamm. 2022;9(3):e1148 (Feb 21). Doi: 10.1212/NXI.0000000000001148
Key clinical point: Masitinib at a dose of 4.5 mg/kg/day may benefit patients with primary progressive multiple sclerosis (PPMS) or nonactive secondary progressive multiple sclerosis (nSPMS).
Major finding: The Expanded Disability Status Scale(EDSS)-based disability worsening was slower with 4.5 mg/kg/day masitinib 4.5 mg/kg/day vs. placebo (change in EDSS 0.001 vs. 0.098), with a between-group difference of −0.097 (P = .027). No new safety signals were identified.
Study details: The findings come from the 96-week, phase 3 Study AB07002 trial involving 611 patients with PPMS or nSPMS who were randomly assigned to parallel groups of either 4.5 mg/kg/day masitinib, 6 mg/kg/day uptitrated masitinib, or an equivalent placebo.
Disclosures: This study was funded by AB Science, Paris, France. A Moussy, C Mansfield, and O Hermine reported being employees and shareholders of AB Science, and the other authors reported receiving research support and nonfinancial support or personal fees from various sources, including AB Science.
Source: Vermersch P et al, on behalf of the AB07002 Study Group. Efficacy and safety of masitinib in progressive forms of multiple sclerosis: A randomized, phase 3, clinical trial. Neurol Neuroimmunol Neuroinflamm. 2022;9(3):e1148 (Feb 21). Doi: 10.1212/NXI.0000000000001148