User login
Child of The New Gastroenterologist
Staying financially well in the time of COVID-19
As COVID-19 continues to threaten the United States and the world, individuals in every profession have been challenged to examine their financial situation. At Fidelity Investments, we recently conducted a national survey asking people how current events have affected their opinions and behaviors when it comes to their money. The results showed that six in 10 Americans are concerned about household finances over the next 6 months. Unfortunately, we’ve seen that even health care professionals have not been financially spared, with salaries or benefits cut or, worse, furloughs and layoffs as hospital systems struggle. I work with many physicians, including gastroenterologists, in my role as a wealth planner for Fidelity Investments and have received quite a few questions related to shoring up family finances during these difficult times.
Luckily, the financial best practices that I share in “good” times ring true even in today’s world, with a few additions given the health and economic risks created by COVID-19.
1. Review your budget. It’s one thing to know that your budget is generally balanced (the dollars you spend are less than the dollars you earn). But it’s worth taking a closer look to see just where those dollars are going. In times of uncertainty, cutting back on expenses that aren’t necessary or don’t provide meaningful value to your life can be worthwhile. If you or your family have lost income because of the pandemic, you might consider these seven simple tips to help boost your cash flow.
2. Tackle (or find relief from) student loan debt. Doctors today graduate medical school with a median debt of just under $195,000.1 Repaying these loans is daunting, particularly during the COVID-19 crisis. The recent passing of the CARES Act recognizes these difficult times: in fact, it automatically suspended required minimum loan payments and interest accrual on federal student loans until Sept. 30, 2020. This only applies to federal student loans, not private student loans. Beyond this period, if you are still struggling with payments, you may explore the possibility of refinancing, by taking out a lower-interest private loan and using that to pay off student loans (although this may extend the life of your loan). Borrowers could also consider other programs, such as REPAYE (Revised Pay As You Earn) through which your monthly payment tops out at 10% of your monthly income, or Public Service Loan Forgiveness (PSLF) if you work for a not-for-profit hospital or other qualifying employer. This program forgives the remaining balance on your direct loans after you have made 120 qualifying monthly payments while working full-time for a qualifying employer.
Additionally, borrowers could look for opportunities to reduce accrued interest, either by refinancing to a lower rate or making payments every 2 weeks rather than once each month.
3. Evaluate your emergency fund. It’s a good idea to keep 3-6 months’ of essential expenses in cash or cash-like investments. If you don’t yet have this 3- to 6-month cushion saved, now is a good time to work to reduce your expenses and stash away any extra cash.
4. Save early and often for retirement. You can borrow money to support many of life’s needs, from housing, to cars, to college. But you can’t borrow for retirement. That is why I encourage clients to put retirement savings at the top of the list, after accounting for day-to-day needs of their families. People often ask me whether it makes sense to continue saving for retirement, often a far-off goal for younger doctors, especially in these uncertain times. My answer? Yes. If you are able to save, continue to save: the earlier you begin to make contributions to your retirement account, and the longer you continue to do so, the more your retirement account(s) have the potential to grow over time.
Another question I receive is whether to take distributions from a retirement account early if you find yourself in a precarious financial situation because of the COVID-19 crisis. The CARES Act provides options allowing Americans to take a withdrawal or loan from a participating retirement plan if you, your spouse, or your dependent have a COVID-19 related illness or you’re experiencing a loss of income related to the COVID-19 pandemic. Try to look at alternative sources of income before tapping your hard-earned retirement savings. If you can find a way to continue saving and avoid drawing down your retirement accounts, your future self will thank you.
5. If you have a high-deductible health plan that offers it, explore a Health Savings Account (HSA). One of the most important factors in a solid financial plan is knowing how to pay for health care expenses, both now and as we age. HSAs are a tax-advantaged account that can be used to save money for qualified medical expenses. They are considered to provide a “triple-tax advantage” since contributions, qualified withdrawals, and investment growth are all tax-free.2 The dollars in these accounts can stay there over time, so in years with low expenses you could use these to save for health care in retirement, while in other years they can be used to pay necessary medical bills. HSAs require the participant to be enrolled in a high-deductible health plan, so you would first need to verify that your employer provides this option.
6. Be prepared to protect yourself, your practice, and your family. Typically, I encourage the medical professionals I work with to review their current insurance plans (such as disability, life, and malpractice) to determine whether they have the right levels of coverage for their situation. With COVID-19 layered on top of the usual level of risk, it’s important to consider reviewing or updating other key elements of your family’s plan, like your health care proxies and a living will.
7. Put your income to work. When your disposable income grows, and you’ve covered all of the foundational elements of a financial plan (a rainy-day fund, contingency planning for health care costs, and so on), it might be the right time to consider investing for something other than retirement. As you do that, be sure you are invested in a diversified strategy with a balance of risk and return that is comfortable for you.
Recent market volatility can bring nerves that make it difficult to stay invested. However, as long as your risk tolerance and time horizon reflect your asset allocation – the mix of stock, bonds, and cash (which a financial planner can help with) – you can take comfort in knowing that historically every severe downturn has eventually given way to further growth.
During uncertain times like these, I think the best guidance is to focus on what you can control. The considerations above are a great place to start building a financial plan to solidify you and your family’s future. A Fidelity survey found that 44% of Americans are now working to build up their emergency savings, and one-third (34%) are rethinking how they manage their money because of the COVID-19 crisis.3 Despite the stresses we all face, there is no time like the present to start or revisit your financial plan.
Footnotes
1. Barron D. Why Doctors Are Drowning in Medical School Debt. Scientific American. July 15, 2019.
2. With respect to federal taxation only. Contributions, investment earnings, and distributions may or may not be subject to state taxation. The triple tax advantages are only applicable if the money is used to pay for qualified medical expenses as described in IRS Publication 969.
3. Fidelity Market Sentiment Study presents the findings of a nationwide online survey consisting of 3,012 adults, at least 18 years of age, from which 1,591 respondents qualified as having at least one investment account. The study was fielded April 1-8, 2020, by ENGINE INSIGHTS, an independent research firm not affiliated with Fidelity Investments. The results of this survey may not be representative of all adults meeting the same criteria as those surveyed for this study. For the purposes of this study, the generations are defined as follows: Millennials (aged 24-39 years); Generation X (aged 40-55 years); Baby Boomers (aged 56-74 years).
Mr. Tudor is Vice President, Wealth Planning Consultant at Fidelity Investments.
As COVID-19 continues to threaten the United States and the world, individuals in every profession have been challenged to examine their financial situation. At Fidelity Investments, we recently conducted a national survey asking people how current events have affected their opinions and behaviors when it comes to their money. The results showed that six in 10 Americans are concerned about household finances over the next 6 months. Unfortunately, we’ve seen that even health care professionals have not been financially spared, with salaries or benefits cut or, worse, furloughs and layoffs as hospital systems struggle. I work with many physicians, including gastroenterologists, in my role as a wealth planner for Fidelity Investments and have received quite a few questions related to shoring up family finances during these difficult times.
Luckily, the financial best practices that I share in “good” times ring true even in today’s world, with a few additions given the health and economic risks created by COVID-19.
1. Review your budget. It’s one thing to know that your budget is generally balanced (the dollars you spend are less than the dollars you earn). But it’s worth taking a closer look to see just where those dollars are going. In times of uncertainty, cutting back on expenses that aren’t necessary or don’t provide meaningful value to your life can be worthwhile. If you or your family have lost income because of the pandemic, you might consider these seven simple tips to help boost your cash flow.
2. Tackle (or find relief from) student loan debt. Doctors today graduate medical school with a median debt of just under $195,000.1 Repaying these loans is daunting, particularly during the COVID-19 crisis. The recent passing of the CARES Act recognizes these difficult times: in fact, it automatically suspended required minimum loan payments and interest accrual on federal student loans until Sept. 30, 2020. This only applies to federal student loans, not private student loans. Beyond this period, if you are still struggling with payments, you may explore the possibility of refinancing, by taking out a lower-interest private loan and using that to pay off student loans (although this may extend the life of your loan). Borrowers could also consider other programs, such as REPAYE (Revised Pay As You Earn) through which your monthly payment tops out at 10% of your monthly income, or Public Service Loan Forgiveness (PSLF) if you work for a not-for-profit hospital or other qualifying employer. This program forgives the remaining balance on your direct loans after you have made 120 qualifying monthly payments while working full-time for a qualifying employer.
Additionally, borrowers could look for opportunities to reduce accrued interest, either by refinancing to a lower rate or making payments every 2 weeks rather than once each month.
3. Evaluate your emergency fund. It’s a good idea to keep 3-6 months’ of essential expenses in cash or cash-like investments. If you don’t yet have this 3- to 6-month cushion saved, now is a good time to work to reduce your expenses and stash away any extra cash.
4. Save early and often for retirement. You can borrow money to support many of life’s needs, from housing, to cars, to college. But you can’t borrow for retirement. That is why I encourage clients to put retirement savings at the top of the list, after accounting for day-to-day needs of their families. People often ask me whether it makes sense to continue saving for retirement, often a far-off goal for younger doctors, especially in these uncertain times. My answer? Yes. If you are able to save, continue to save: the earlier you begin to make contributions to your retirement account, and the longer you continue to do so, the more your retirement account(s) have the potential to grow over time.
Another question I receive is whether to take distributions from a retirement account early if you find yourself in a precarious financial situation because of the COVID-19 crisis. The CARES Act provides options allowing Americans to take a withdrawal or loan from a participating retirement plan if you, your spouse, or your dependent have a COVID-19 related illness or you’re experiencing a loss of income related to the COVID-19 pandemic. Try to look at alternative sources of income before tapping your hard-earned retirement savings. If you can find a way to continue saving and avoid drawing down your retirement accounts, your future self will thank you.
5. If you have a high-deductible health plan that offers it, explore a Health Savings Account (HSA). One of the most important factors in a solid financial plan is knowing how to pay for health care expenses, both now and as we age. HSAs are a tax-advantaged account that can be used to save money for qualified medical expenses. They are considered to provide a “triple-tax advantage” since contributions, qualified withdrawals, and investment growth are all tax-free.2 The dollars in these accounts can stay there over time, so in years with low expenses you could use these to save for health care in retirement, while in other years they can be used to pay necessary medical bills. HSAs require the participant to be enrolled in a high-deductible health plan, so you would first need to verify that your employer provides this option.
6. Be prepared to protect yourself, your practice, and your family. Typically, I encourage the medical professionals I work with to review their current insurance plans (such as disability, life, and malpractice) to determine whether they have the right levels of coverage for their situation. With COVID-19 layered on top of the usual level of risk, it’s important to consider reviewing or updating other key elements of your family’s plan, like your health care proxies and a living will.
7. Put your income to work. When your disposable income grows, and you’ve covered all of the foundational elements of a financial plan (a rainy-day fund, contingency planning for health care costs, and so on), it might be the right time to consider investing for something other than retirement. As you do that, be sure you are invested in a diversified strategy with a balance of risk and return that is comfortable for you.
Recent market volatility can bring nerves that make it difficult to stay invested. However, as long as your risk tolerance and time horizon reflect your asset allocation – the mix of stock, bonds, and cash (which a financial planner can help with) – you can take comfort in knowing that historically every severe downturn has eventually given way to further growth.
During uncertain times like these, I think the best guidance is to focus on what you can control. The considerations above are a great place to start building a financial plan to solidify you and your family’s future. A Fidelity survey found that 44% of Americans are now working to build up their emergency savings, and one-third (34%) are rethinking how they manage their money because of the COVID-19 crisis.3 Despite the stresses we all face, there is no time like the present to start or revisit your financial plan.
Footnotes
1. Barron D. Why Doctors Are Drowning in Medical School Debt. Scientific American. July 15, 2019.
2. With respect to federal taxation only. Contributions, investment earnings, and distributions may or may not be subject to state taxation. The triple tax advantages are only applicable if the money is used to pay for qualified medical expenses as described in IRS Publication 969.
3. Fidelity Market Sentiment Study presents the findings of a nationwide online survey consisting of 3,012 adults, at least 18 years of age, from which 1,591 respondents qualified as having at least one investment account. The study was fielded April 1-8, 2020, by ENGINE INSIGHTS, an independent research firm not affiliated with Fidelity Investments. The results of this survey may not be representative of all adults meeting the same criteria as those surveyed for this study. For the purposes of this study, the generations are defined as follows: Millennials (aged 24-39 years); Generation X (aged 40-55 years); Baby Boomers (aged 56-74 years).
Mr. Tudor is Vice President, Wealth Planning Consultant at Fidelity Investments.
As COVID-19 continues to threaten the United States and the world, individuals in every profession have been challenged to examine their financial situation. At Fidelity Investments, we recently conducted a national survey asking people how current events have affected their opinions and behaviors when it comes to their money. The results showed that six in 10 Americans are concerned about household finances over the next 6 months. Unfortunately, we’ve seen that even health care professionals have not been financially spared, with salaries or benefits cut or, worse, furloughs and layoffs as hospital systems struggle. I work with many physicians, including gastroenterologists, in my role as a wealth planner for Fidelity Investments and have received quite a few questions related to shoring up family finances during these difficult times.
Luckily, the financial best practices that I share in “good” times ring true even in today’s world, with a few additions given the health and economic risks created by COVID-19.
1. Review your budget. It’s one thing to know that your budget is generally balanced (the dollars you spend are less than the dollars you earn). But it’s worth taking a closer look to see just where those dollars are going. In times of uncertainty, cutting back on expenses that aren’t necessary or don’t provide meaningful value to your life can be worthwhile. If you or your family have lost income because of the pandemic, you might consider these seven simple tips to help boost your cash flow.
2. Tackle (or find relief from) student loan debt. Doctors today graduate medical school with a median debt of just under $195,000.1 Repaying these loans is daunting, particularly during the COVID-19 crisis. The recent passing of the CARES Act recognizes these difficult times: in fact, it automatically suspended required minimum loan payments and interest accrual on federal student loans until Sept. 30, 2020. This only applies to federal student loans, not private student loans. Beyond this period, if you are still struggling with payments, you may explore the possibility of refinancing, by taking out a lower-interest private loan and using that to pay off student loans (although this may extend the life of your loan). Borrowers could also consider other programs, such as REPAYE (Revised Pay As You Earn) through which your monthly payment tops out at 10% of your monthly income, or Public Service Loan Forgiveness (PSLF) if you work for a not-for-profit hospital or other qualifying employer. This program forgives the remaining balance on your direct loans after you have made 120 qualifying monthly payments while working full-time for a qualifying employer.
Additionally, borrowers could look for opportunities to reduce accrued interest, either by refinancing to a lower rate or making payments every 2 weeks rather than once each month.
3. Evaluate your emergency fund. It’s a good idea to keep 3-6 months’ of essential expenses in cash or cash-like investments. If you don’t yet have this 3- to 6-month cushion saved, now is a good time to work to reduce your expenses and stash away any extra cash.
4. Save early and often for retirement. You can borrow money to support many of life’s needs, from housing, to cars, to college. But you can’t borrow for retirement. That is why I encourage clients to put retirement savings at the top of the list, after accounting for day-to-day needs of their families. People often ask me whether it makes sense to continue saving for retirement, often a far-off goal for younger doctors, especially in these uncertain times. My answer? Yes. If you are able to save, continue to save: the earlier you begin to make contributions to your retirement account, and the longer you continue to do so, the more your retirement account(s) have the potential to grow over time.
Another question I receive is whether to take distributions from a retirement account early if you find yourself in a precarious financial situation because of the COVID-19 crisis. The CARES Act provides options allowing Americans to take a withdrawal or loan from a participating retirement plan if you, your spouse, or your dependent have a COVID-19 related illness or you’re experiencing a loss of income related to the COVID-19 pandemic. Try to look at alternative sources of income before tapping your hard-earned retirement savings. If you can find a way to continue saving and avoid drawing down your retirement accounts, your future self will thank you.
5. If you have a high-deductible health plan that offers it, explore a Health Savings Account (HSA). One of the most important factors in a solid financial plan is knowing how to pay for health care expenses, both now and as we age. HSAs are a tax-advantaged account that can be used to save money for qualified medical expenses. They are considered to provide a “triple-tax advantage” since contributions, qualified withdrawals, and investment growth are all tax-free.2 The dollars in these accounts can stay there over time, so in years with low expenses you could use these to save for health care in retirement, while in other years they can be used to pay necessary medical bills. HSAs require the participant to be enrolled in a high-deductible health plan, so you would first need to verify that your employer provides this option.
6. Be prepared to protect yourself, your practice, and your family. Typically, I encourage the medical professionals I work with to review their current insurance plans (such as disability, life, and malpractice) to determine whether they have the right levels of coverage for their situation. With COVID-19 layered on top of the usual level of risk, it’s important to consider reviewing or updating other key elements of your family’s plan, like your health care proxies and a living will.
7. Put your income to work. When your disposable income grows, and you’ve covered all of the foundational elements of a financial plan (a rainy-day fund, contingency planning for health care costs, and so on), it might be the right time to consider investing for something other than retirement. As you do that, be sure you are invested in a diversified strategy with a balance of risk and return that is comfortable for you.
Recent market volatility can bring nerves that make it difficult to stay invested. However, as long as your risk tolerance and time horizon reflect your asset allocation – the mix of stock, bonds, and cash (which a financial planner can help with) – you can take comfort in knowing that historically every severe downturn has eventually given way to further growth.
During uncertain times like these, I think the best guidance is to focus on what you can control. The considerations above are a great place to start building a financial plan to solidify you and your family’s future. A Fidelity survey found that 44% of Americans are now working to build up their emergency savings, and one-third (34%) are rethinking how they manage their money because of the COVID-19 crisis.3 Despite the stresses we all face, there is no time like the present to start or revisit your financial plan.
Footnotes
1. Barron D. Why Doctors Are Drowning in Medical School Debt. Scientific American. July 15, 2019.
2. With respect to federal taxation only. Contributions, investment earnings, and distributions may or may not be subject to state taxation. The triple tax advantages are only applicable if the money is used to pay for qualified medical expenses as described in IRS Publication 969.
3. Fidelity Market Sentiment Study presents the findings of a nationwide online survey consisting of 3,012 adults, at least 18 years of age, from which 1,591 respondents qualified as having at least one investment account. The study was fielded April 1-8, 2020, by ENGINE INSIGHTS, an independent research firm not affiliated with Fidelity Investments. The results of this survey may not be representative of all adults meeting the same criteria as those surveyed for this study. For the purposes of this study, the generations are defined as follows: Millennials (aged 24-39 years); Generation X (aged 40-55 years); Baby Boomers (aged 56-74 years).
Mr. Tudor is Vice President, Wealth Planning Consultant at Fidelity Investments.
So you want to be an expert witness?
Acting as an expert witness in a legal matter can be a nice way to compliment your practice. However, it is important to understand the role of experts, as well as their duties and obligations. Expert witnesses are called to testify on the basis of their specialized knowledge, not necessarily their direct knowledge of events and issues in the case.
Medical experts often play an important role in the evaluation, development, and preparation of a case long before it ever goes to trial. In some states, to even file a medical malpractice complaint a plaintiff is required to have the case evaluated by an expert and obtain a written report outlining why the plaintiff has a reasonable and meritorious cause for filing such an action.
There are different types of expert witness testimony. Experts can give opinion testimony as a physician who provided treatment to the plaintiff and whose conduct is not at issue. The second type of expert witness is a retained or controlled expert witness. This is a person giving opinion testimony after being retained by a lawyer on behalf of one of the parties to the lawsuit.
Before you give deposition or trial testimony, your opinions must be disclosed in writing and provided to the other parties in the case. In federal court, this is governed by Federal Rule of Civil Procedure 26. If the case is pending in state court, your written opinions are governed by local court rules. In both cases, the written opinions should be thorough and complete because you will not be allowed to testify to new opinions at the time of trial but will generally be allowed to expand upon those disclosed in writing at your deposition trial.
In order for a jury to hear your opinions at trial, your opinions must be reliable. In federal court, expert testimony is governed by Federal Rule of Evidence 702, which states:
A witness who is qualified as an expert by knowledge, skill, experience, training, or education may testify in the form of an opinion or otherwise if:
a) the expert’s scientific, technical, or other specialized knowledge will help the trier of fact to understand the evidence or to determine a fact in issue;
b) the testimony is based on sufficient facts or data;
c) the testimony is the product of reliable principles and methods; and
d) the expert has reliably applied the principles and methods to the facts of the case.
This means, that if a fact or evidence at issue involves scientific, technical, or specialized knowledge that is outside the scope of an ordinary layman’s experience, or involves complex issues challenging a layman’s comprehension, expert testimony is required. The scientific evidence must not just be relevant but also reliable. Expert opinions will be scrutinized to see if they are based on scientific testing or review of scientific data rather than just assumptions or speculation. Additionally, the experts must be qualified by their knowledge, skill, experience, training, or education. Given these parameters, it should come as no surprise that expert trial testimony is required for all medical malpractice cases.
Some states follow the “new or novel rule” which dictates that expert testimony is only admissible if the methodology or scientific principal on which the opinion is based is sufficiently established to have gained general acceptance in the particular field in which it belongs. This means that the evidence must be generally accepted as reliable in the relevant scientific community. New or novel techniques will be placed under the scrutiny of this standard. Courts will look at papers, books, journals, and case law to make a determination as to the reliability and general acceptance. Failure to meet the requisite standards may render a physician ineligible to testify.
If you are considering acting as an expert witness there are a few basic dos and don’ts to keep in mind:
Do be mindful of your criticism. If testifying in a medical malpractice case, you will be giving sworn testimony as to whether another physician deviated from the standard of care. Be aware that your testimony can later be used against you if your conduct is ever at issue, or if you contradict yourself in another case. Attorneys often look for prior testimony to use when questioning you at deposition and trial.
Do be aware of any applicable professional society guidelines. Many professional societies publish ethical guidelines as it relates to expert medical testimony. Be aware of those and know that you may be asked about them, especially if you are a member of that society.
Do be prepared for basic areas of cross-examination. There are a few tried and true areas that will always be the subject of cross-examination. Any perceived bias you may have, your fees, and whether you do more work for plaintiffs versus defendants are a just few examples. You should also be prepared to be cross-examined on the differences between personal practice (what you do) and an actual deviation from the standard of care.
Do keep written communication to a minimum. All communication between the expert physician and the attorney is potentially discoverable by the other side. The rules differ for state and federal courts. Emails, draft reports, and written questions all cause the creation of unnecessary side issues and areas of cross-examination. The best practice is for all substantive communication to be done by phone.
Do be clear in what you are charging. It is not unusual for an expert to charge one hourly rate for record review, and a different rate for testimony. Your fee schedule should also note that any travel expenses you incur will also be invoiced. Your hourly rate should be appropriate for your area of practice. In our experience, gastroenterologists typically charge $400.00-$600.00 an hour for record review, and $550.00-$700.00 an hour for testimony.
Do not submit an invoice until after your deposition. Submitting invoices before your deposition creates unnecessary cross-examination issues. At the time of retention, speak to the attorney and ask if you will be able to submit invoices as you work. Most attorneys prefer invoices be submitted after your deposition. Because the wheels of justice often turn slowly, you could be waiting an equally long time to submit an invoice and get paid. One way to avoid this dilemma is to require a retainer at the time of retention.
Do not sign up with an expert finder service. Resist the urge to sign up with an expert finder service. The best medical experts come from referrals from other attorneys or physicians. Expert retention via an expert finder service creates the impression that you are a “hired gun” in the business of being a professional expert and can diminish your credibility. The finder services also charge a commission or fee.
As a gastroenterologist, you have the specialized knowledge to provide expert testimony regarding the cause of an injury and extent of damages in cases where you have treated a patient. You also have the type of education and training necessary to serve as an independent expert. Doing so is a serious task that can be time consuming and stressful. However, it can also be rewarding and allow you to make sure a fair and just outcome occurs.
This article is for general informational purposes only. Please consult your own attorney if you have questions. This information is not intended to create an attorney-client relationship.
Mr. Mills is an equity partner at Cunningham, Meyer & Vedrine PC in Chicago. Ms. Lindbert is a partner at Cunningham, Meyer & Vedrine PC. Both focus their practices on defending doctors and hospitals in medical malpractice actions.
Acting as an expert witness in a legal matter can be a nice way to compliment your practice. However, it is important to understand the role of experts, as well as their duties and obligations. Expert witnesses are called to testify on the basis of their specialized knowledge, not necessarily their direct knowledge of events and issues in the case.
Medical experts often play an important role in the evaluation, development, and preparation of a case long before it ever goes to trial. In some states, to even file a medical malpractice complaint a plaintiff is required to have the case evaluated by an expert and obtain a written report outlining why the plaintiff has a reasonable and meritorious cause for filing such an action.
There are different types of expert witness testimony. Experts can give opinion testimony as a physician who provided treatment to the plaintiff and whose conduct is not at issue. The second type of expert witness is a retained or controlled expert witness. This is a person giving opinion testimony after being retained by a lawyer on behalf of one of the parties to the lawsuit.
Before you give deposition or trial testimony, your opinions must be disclosed in writing and provided to the other parties in the case. In federal court, this is governed by Federal Rule of Civil Procedure 26. If the case is pending in state court, your written opinions are governed by local court rules. In both cases, the written opinions should be thorough and complete because you will not be allowed to testify to new opinions at the time of trial but will generally be allowed to expand upon those disclosed in writing at your deposition trial.
In order for a jury to hear your opinions at trial, your opinions must be reliable. In federal court, expert testimony is governed by Federal Rule of Evidence 702, which states:
A witness who is qualified as an expert by knowledge, skill, experience, training, or education may testify in the form of an opinion or otherwise if:
a) the expert’s scientific, technical, or other specialized knowledge will help the trier of fact to understand the evidence or to determine a fact in issue;
b) the testimony is based on sufficient facts or data;
c) the testimony is the product of reliable principles and methods; and
d) the expert has reliably applied the principles and methods to the facts of the case.
This means, that if a fact or evidence at issue involves scientific, technical, or specialized knowledge that is outside the scope of an ordinary layman’s experience, or involves complex issues challenging a layman’s comprehension, expert testimony is required. The scientific evidence must not just be relevant but also reliable. Expert opinions will be scrutinized to see if they are based on scientific testing or review of scientific data rather than just assumptions or speculation. Additionally, the experts must be qualified by their knowledge, skill, experience, training, or education. Given these parameters, it should come as no surprise that expert trial testimony is required for all medical malpractice cases.
Some states follow the “new or novel rule” which dictates that expert testimony is only admissible if the methodology or scientific principal on which the opinion is based is sufficiently established to have gained general acceptance in the particular field in which it belongs. This means that the evidence must be generally accepted as reliable in the relevant scientific community. New or novel techniques will be placed under the scrutiny of this standard. Courts will look at papers, books, journals, and case law to make a determination as to the reliability and general acceptance. Failure to meet the requisite standards may render a physician ineligible to testify.
If you are considering acting as an expert witness there are a few basic dos and don’ts to keep in mind:
Do be mindful of your criticism. If testifying in a medical malpractice case, you will be giving sworn testimony as to whether another physician deviated from the standard of care. Be aware that your testimony can later be used against you if your conduct is ever at issue, or if you contradict yourself in another case. Attorneys often look for prior testimony to use when questioning you at deposition and trial.
Do be aware of any applicable professional society guidelines. Many professional societies publish ethical guidelines as it relates to expert medical testimony. Be aware of those and know that you may be asked about them, especially if you are a member of that society.
Do be prepared for basic areas of cross-examination. There are a few tried and true areas that will always be the subject of cross-examination. Any perceived bias you may have, your fees, and whether you do more work for plaintiffs versus defendants are a just few examples. You should also be prepared to be cross-examined on the differences between personal practice (what you do) and an actual deviation from the standard of care.
Do keep written communication to a minimum. All communication between the expert physician and the attorney is potentially discoverable by the other side. The rules differ for state and federal courts. Emails, draft reports, and written questions all cause the creation of unnecessary side issues and areas of cross-examination. The best practice is for all substantive communication to be done by phone.
Do be clear in what you are charging. It is not unusual for an expert to charge one hourly rate for record review, and a different rate for testimony. Your fee schedule should also note that any travel expenses you incur will also be invoiced. Your hourly rate should be appropriate for your area of practice. In our experience, gastroenterologists typically charge $400.00-$600.00 an hour for record review, and $550.00-$700.00 an hour for testimony.
Do not submit an invoice until after your deposition. Submitting invoices before your deposition creates unnecessary cross-examination issues. At the time of retention, speak to the attorney and ask if you will be able to submit invoices as you work. Most attorneys prefer invoices be submitted after your deposition. Because the wheels of justice often turn slowly, you could be waiting an equally long time to submit an invoice and get paid. One way to avoid this dilemma is to require a retainer at the time of retention.
Do not sign up with an expert finder service. Resist the urge to sign up with an expert finder service. The best medical experts come from referrals from other attorneys or physicians. Expert retention via an expert finder service creates the impression that you are a “hired gun” in the business of being a professional expert and can diminish your credibility. The finder services also charge a commission or fee.
As a gastroenterologist, you have the specialized knowledge to provide expert testimony regarding the cause of an injury and extent of damages in cases where you have treated a patient. You also have the type of education and training necessary to serve as an independent expert. Doing so is a serious task that can be time consuming and stressful. However, it can also be rewarding and allow you to make sure a fair and just outcome occurs.
This article is for general informational purposes only. Please consult your own attorney if you have questions. This information is not intended to create an attorney-client relationship.
Mr. Mills is an equity partner at Cunningham, Meyer & Vedrine PC in Chicago. Ms. Lindbert is a partner at Cunningham, Meyer & Vedrine PC. Both focus their practices on defending doctors and hospitals in medical malpractice actions.
Acting as an expert witness in a legal matter can be a nice way to compliment your practice. However, it is important to understand the role of experts, as well as their duties and obligations. Expert witnesses are called to testify on the basis of their specialized knowledge, not necessarily their direct knowledge of events and issues in the case.
Medical experts often play an important role in the evaluation, development, and preparation of a case long before it ever goes to trial. In some states, to even file a medical malpractice complaint a plaintiff is required to have the case evaluated by an expert and obtain a written report outlining why the plaintiff has a reasonable and meritorious cause for filing such an action.
There are different types of expert witness testimony. Experts can give opinion testimony as a physician who provided treatment to the plaintiff and whose conduct is not at issue. The second type of expert witness is a retained or controlled expert witness. This is a person giving opinion testimony after being retained by a lawyer on behalf of one of the parties to the lawsuit.
Before you give deposition or trial testimony, your opinions must be disclosed in writing and provided to the other parties in the case. In federal court, this is governed by Federal Rule of Civil Procedure 26. If the case is pending in state court, your written opinions are governed by local court rules. In both cases, the written opinions should be thorough and complete because you will not be allowed to testify to new opinions at the time of trial but will generally be allowed to expand upon those disclosed in writing at your deposition trial.
In order for a jury to hear your opinions at trial, your opinions must be reliable. In federal court, expert testimony is governed by Federal Rule of Evidence 702, which states:
A witness who is qualified as an expert by knowledge, skill, experience, training, or education may testify in the form of an opinion or otherwise if:
a) the expert’s scientific, technical, or other specialized knowledge will help the trier of fact to understand the evidence or to determine a fact in issue;
b) the testimony is based on sufficient facts or data;
c) the testimony is the product of reliable principles and methods; and
d) the expert has reliably applied the principles and methods to the facts of the case.
This means, that if a fact or evidence at issue involves scientific, technical, or specialized knowledge that is outside the scope of an ordinary layman’s experience, or involves complex issues challenging a layman’s comprehension, expert testimony is required. The scientific evidence must not just be relevant but also reliable. Expert opinions will be scrutinized to see if they are based on scientific testing or review of scientific data rather than just assumptions or speculation. Additionally, the experts must be qualified by their knowledge, skill, experience, training, or education. Given these parameters, it should come as no surprise that expert trial testimony is required for all medical malpractice cases.
Some states follow the “new or novel rule” which dictates that expert testimony is only admissible if the methodology or scientific principal on which the opinion is based is sufficiently established to have gained general acceptance in the particular field in which it belongs. This means that the evidence must be generally accepted as reliable in the relevant scientific community. New or novel techniques will be placed under the scrutiny of this standard. Courts will look at papers, books, journals, and case law to make a determination as to the reliability and general acceptance. Failure to meet the requisite standards may render a physician ineligible to testify.
If you are considering acting as an expert witness there are a few basic dos and don’ts to keep in mind:
Do be mindful of your criticism. If testifying in a medical malpractice case, you will be giving sworn testimony as to whether another physician deviated from the standard of care. Be aware that your testimony can later be used against you if your conduct is ever at issue, or if you contradict yourself in another case. Attorneys often look for prior testimony to use when questioning you at deposition and trial.
Do be aware of any applicable professional society guidelines. Many professional societies publish ethical guidelines as it relates to expert medical testimony. Be aware of those and know that you may be asked about them, especially if you are a member of that society.
Do be prepared for basic areas of cross-examination. There are a few tried and true areas that will always be the subject of cross-examination. Any perceived bias you may have, your fees, and whether you do more work for plaintiffs versus defendants are a just few examples. You should also be prepared to be cross-examined on the differences between personal practice (what you do) and an actual deviation from the standard of care.
Do keep written communication to a minimum. All communication between the expert physician and the attorney is potentially discoverable by the other side. The rules differ for state and federal courts. Emails, draft reports, and written questions all cause the creation of unnecessary side issues and areas of cross-examination. The best practice is for all substantive communication to be done by phone.
Do be clear in what you are charging. It is not unusual for an expert to charge one hourly rate for record review, and a different rate for testimony. Your fee schedule should also note that any travel expenses you incur will also be invoiced. Your hourly rate should be appropriate for your area of practice. In our experience, gastroenterologists typically charge $400.00-$600.00 an hour for record review, and $550.00-$700.00 an hour for testimony.
Do not submit an invoice until after your deposition. Submitting invoices before your deposition creates unnecessary cross-examination issues. At the time of retention, speak to the attorney and ask if you will be able to submit invoices as you work. Most attorneys prefer invoices be submitted after your deposition. Because the wheels of justice often turn slowly, you could be waiting an equally long time to submit an invoice and get paid. One way to avoid this dilemma is to require a retainer at the time of retention.
Do not sign up with an expert finder service. Resist the urge to sign up with an expert finder service. The best medical experts come from referrals from other attorneys or physicians. Expert retention via an expert finder service creates the impression that you are a “hired gun” in the business of being a professional expert and can diminish your credibility. The finder services also charge a commission or fee.
As a gastroenterologist, you have the specialized knowledge to provide expert testimony regarding the cause of an injury and extent of damages in cases where you have treated a patient. You also have the type of education and training necessary to serve as an independent expert. Doing so is a serious task that can be time consuming and stressful. However, it can also be rewarding and allow you to make sure a fair and just outcome occurs.
This article is for general informational purposes only. Please consult your own attorney if you have questions. This information is not intended to create an attorney-client relationship.
Mr. Mills is an equity partner at Cunningham, Meyer & Vedrine PC in Chicago. Ms. Lindbert is a partner at Cunningham, Meyer & Vedrine PC. Both focus their practices on defending doctors and hospitals in medical malpractice actions.
Student loan management: An introduction for the young gastroenterologist
The young gastroenterologist has no shortage of personal finance topics to juggle, ranging from investments, to life and disability coverage, and planning for retirement. But the elephant in the room is student loan management. Average medical student debt today is approximately $240,000, and debt burdens greater than $300,000 are becoming common.1,2 With this staggering amount of debt, it is understandable why student loans are a major source of anxiety. Here, I will provide a brief introduction to student loan management for gastroenterologists.
Student loans: Basic strategy
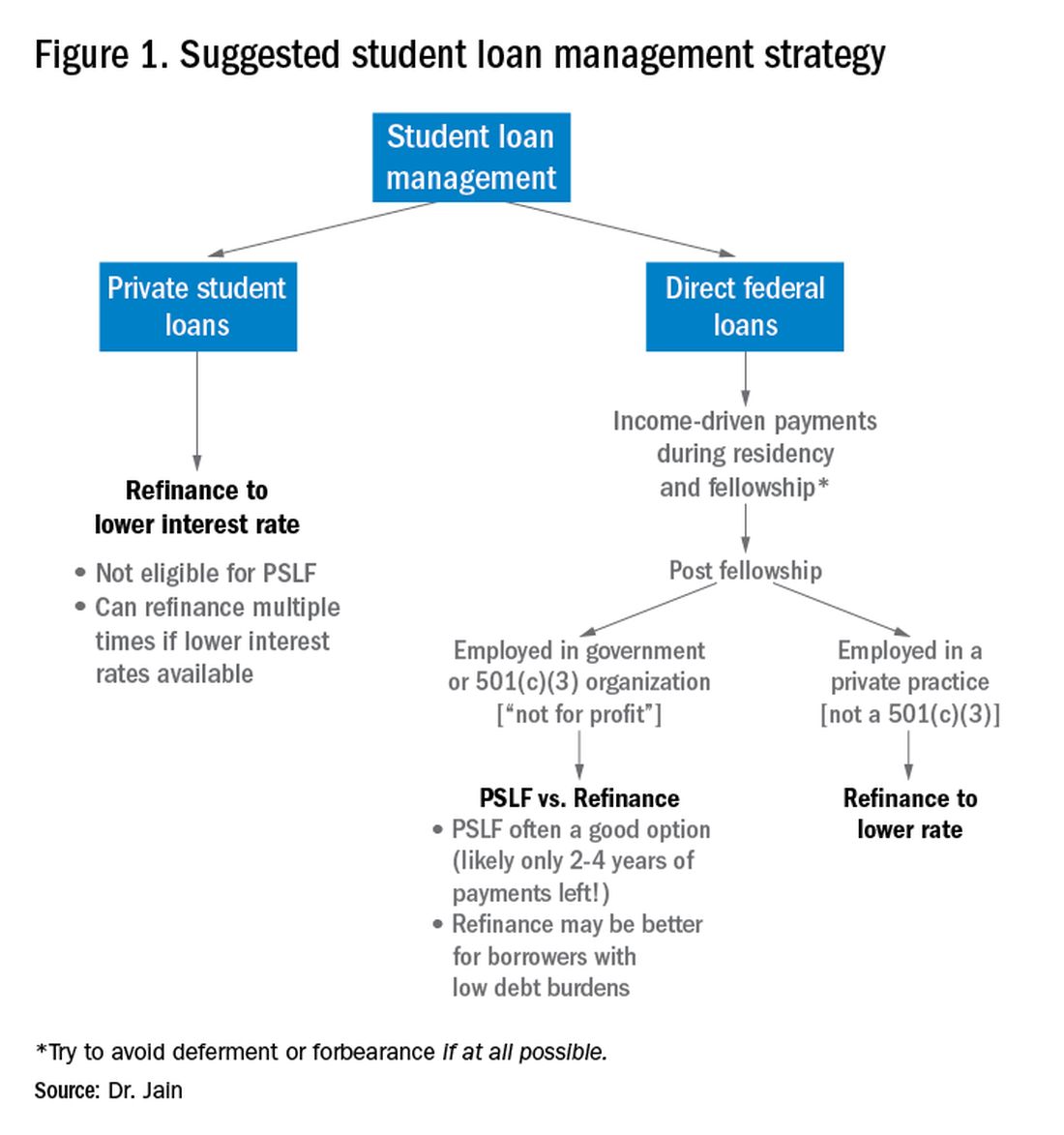
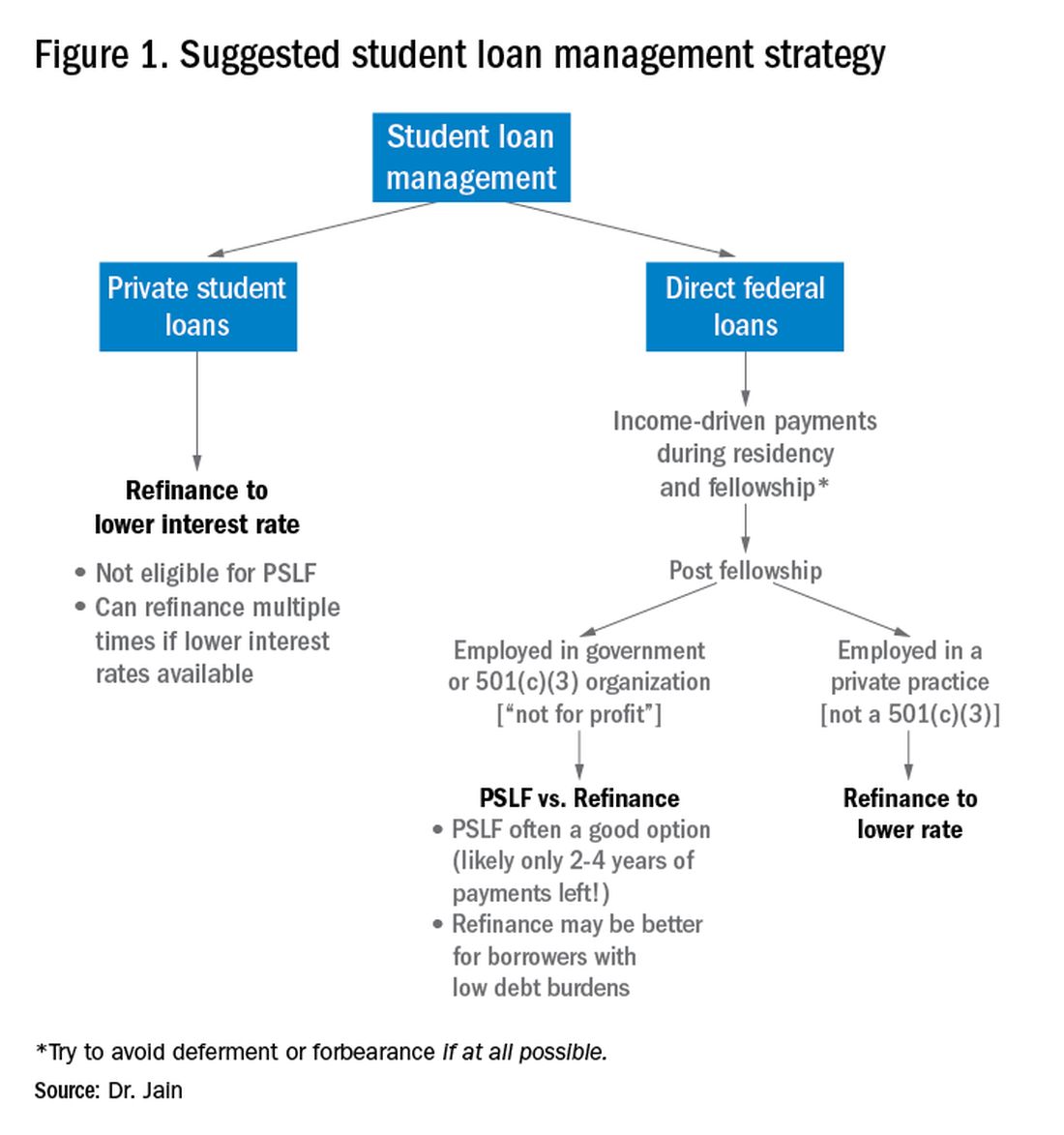
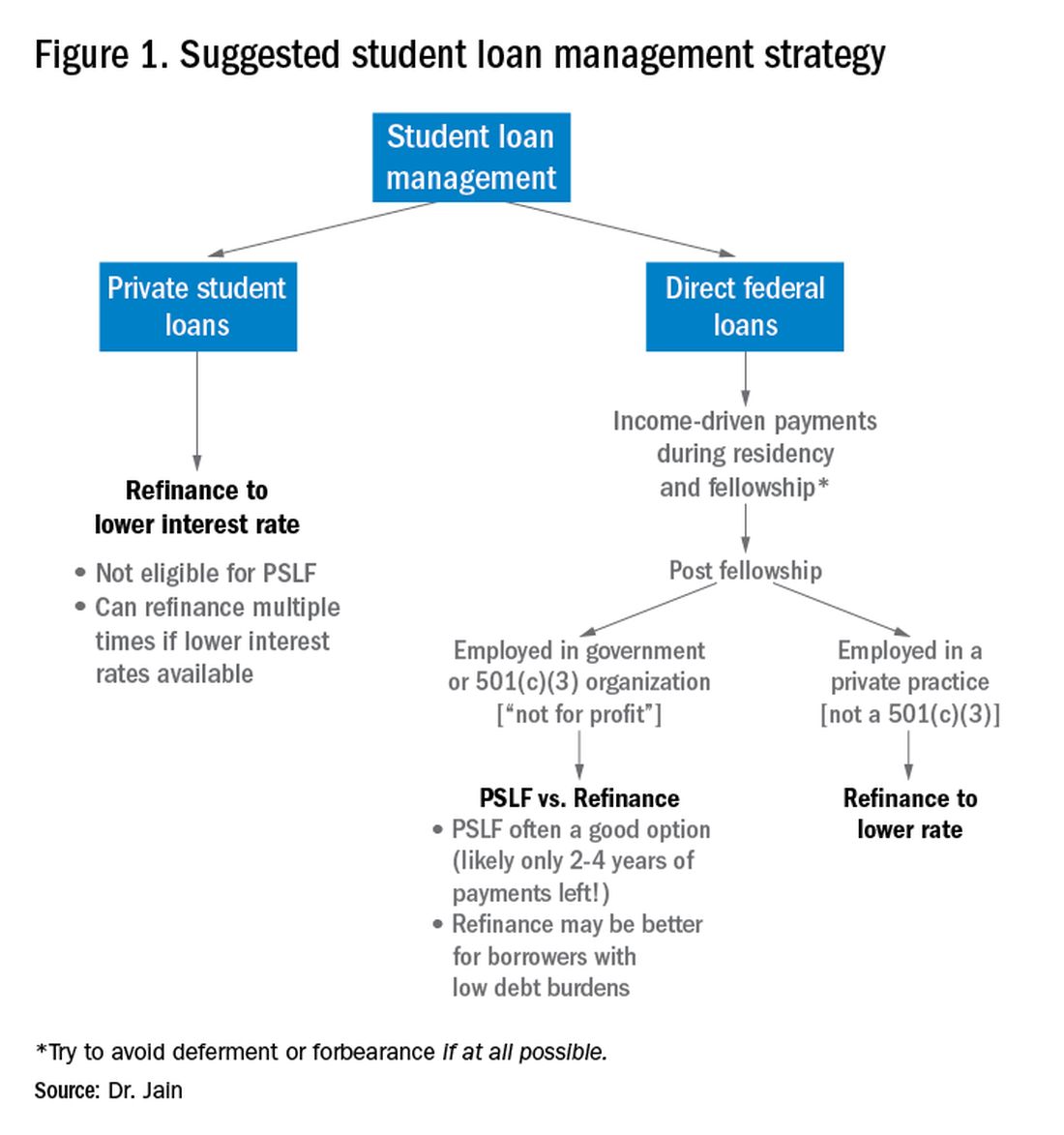
It is important to distinguish between two major types of loans: private student loans and direct federal loans. With private student loans the best strategy in most cases is to refinance to a lower interest rate. For direct federal loans, however, the decision making is more complex. There are two major approaches to these federal loans – either 1) refinance, or 2) go for public service loan forgiveness (PSLF). See Figure 1 for a flowchart summarizing my general approach to student loan management.
Refinance basics
One potential approach is to refinance your federal loans. Most federal loans today are at a relatively high interest rate of 6%-8%.3 Private refinancing can yield rates in the 3%-5% range, depending on the type of loan and other factors. For a loan balance of $200,000, the savings by refinancing could be approximately $2,000-$10,000 per year in interest alone. However, refinancing your loans with a private company eliminates the possibility of PSLF. Hence, you should only refinance federal loans once you are sure that you will not be pursuing PSLF. You may refinance your private loans anytime since they do not qualify for PSLF. There are multiple companies that provide student loan refinancing. The process can be done online, sometimes in as little as 30 minutes. There is generally little or no cost to refinancing, and many companies even provide a small cash-back incentive to refinance.
PSLF basics
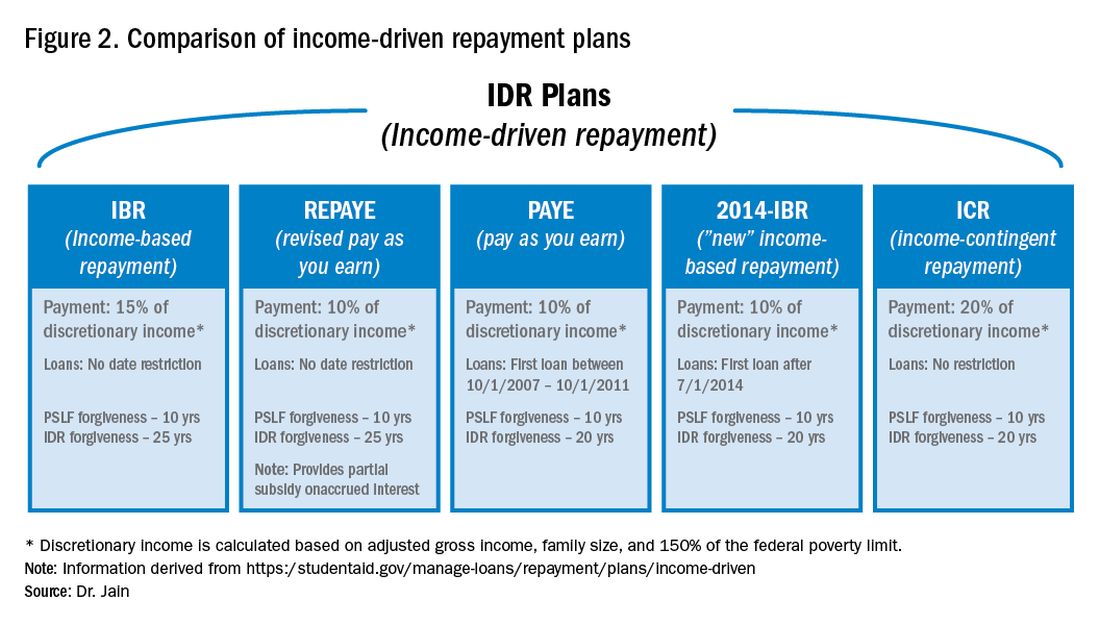
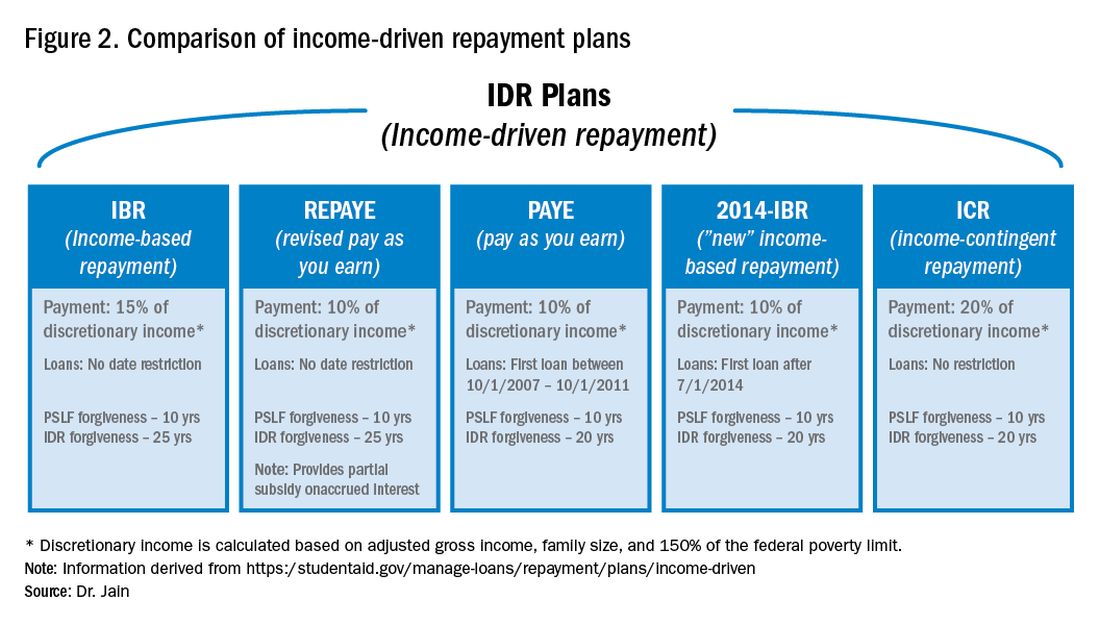
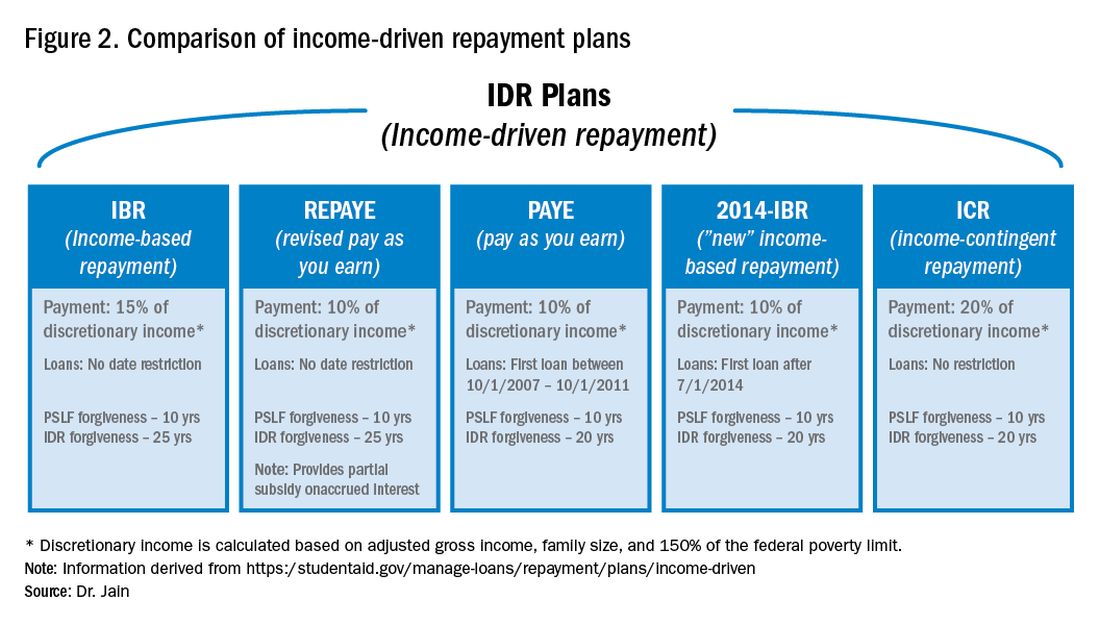
The PSLF program allows borrowers to have the remainder of their direct loans forgiven after 10 years (120 monthly payments) under a qualifying income-driven repayment (IDR) plan.4 Figure 2 shows an overview of the various IDR plans. During the 120 payments, the borrower must work full time for a qualifying employer, which includes a government employer or a not-for-profit 501(c)(3) organization. Loan forgiveness with PSLF is completely tax free. Importantly, the PSLF program only applies to direct federal loans. You can see your federal loan types and balances by visiting https://studentaid.gov/.
To PSLF or not to PSLF?
With direct federal loans, the decision to refinance or go for PSLF is a major fork in the road. PSLF can be a good option for borrowers with long training programs and with high student loan burdens (e.g., loan-to-income ratios of 1:1, 2:1 or higher). By contrast, borrowers with short training programs or relatively small loan burdens may be better off refinancing to a low interest rate and paying off loans quickly. Virtually all institutions that train residents and fellows are qualified government or 501(c)(3) organizations. Hence, a gastroenterology graduate generally will have completed at least 6 out of 10 years of payments by the end of training. Trainees who did a chief resident year or gastroenterology research track may have completed 7 or 8 years of qualifying payments already.
For trainees who are already planning an academic career, PSLF is often a good option. While PSLF can be a nice benefit, I would not advise making a career decision purely based on PSLF. Private practice jobs generally come with substantially higher salaries than academic and government jobs. This salary differential typically more than compensates for the loss of access to PSLF. Hence, I advise trainees to choose the practice setting that is best for their personal and career satisfaction, and then build a student loan management plan around that. The exception may be the trainee who has a very large student loan burden (e.g., loan-to-income ratio of 2:1 or 3:1).
Caveats with PSLF
There have been well publicized concerns about the future of PSLF, including proposals to eliminate or cap the program.5,6 However, most proposed legislation has only recommended changes to PSLF for new borrowers. If you currently have existing federal loans, you would very likely be grandfathered into the existing PSLF terms. All federal master promissory notes since 2007 have cited PSLF as a loan repayment option.7 Hence, eliminating PSLF for existing borrowers seems unlikely since it would be changing the terms of an executed contract.8
There have also been widespread reports of high numbers of borrowers being denied applications for PSLF.9,10 However, the majority of these applicants did not have correct types of loans, had not worked full time for qualifying employers or had not made the full 120 payments.11 Yet some denials have apparently resulted from errors in tracking qualifying payments by FedLoan servicing.12 Therefore it would be prudent to keep your own careful records of all qualifying payments towards PSLF.
The nuclear option: 20- to 25-year IDR-based forgiveness
An additional option allows borrowers to make IDRs for 20-25 years (details in Figure 2) and then having their remaining loan balance forgiven.13 This option is completely independent of PSLF. Borrowers can work full time or part time and can work for any employer, including private employers.
One additional option: NIH loan repayment programs
One additional solution to consider are the NIH Loan Repayment Programs (LRPs). These programs can provide substantial loan repayment (up to $50,000 annually) for trainees and attendings engaged in research that aligns with NIH priorities, including clinical research or health disparities research.14 Notably, the applicant’s research does not have to be NIH sponsored research.
Getting more information
The approach above is a general overview of student loan concepts for gastroenterologists. However, there are countless nuances and tactics that are beyond the scope of this introductory article. I encourage everyone to get additional information and advice when making your own loan management plan. There are many helpful online resources, podcasts, and books discussing the topic. Several companies provide detailed consultation on managing student loans. Such services may cost a few hundred dollars but could potentially save tens of thousands of dollars on student loan costs.
Dr. Jain is assistant professor of medicine, division of gastroenterology & hepatology, department of medicine, University of North Carolina School of Medicine, Chapel Hill. Dr. Jain has no conflicts of interest and no funding source.
References
1. https://nces.ed.gov/programs/digest/d18/tables/dt18_332.45.asp
2. https://www.credible.com/blog/statistics/average-medical-school-debt/
3. https://studentaid.gov/understand-aid/types/loans/interest-rates
4. https://studentaid.gov/manage-loans/forgiveness-cancellation/public-service
5. https://www.forbes.com/sites/robertfarrington/2019/09/24/how-to-get-your-public-service-loan-forgiveness-qualifying-payments-recounted/#18567f061f5d
6. https://www.cbo.gov/budget-options/2018/54721
7. https://static.studentloans.gov/images/ApplicationAndPromissoryNote.pdf
8. https://www.biglawinvestor.com/pslf-promissory-note/
9. https://bostonstudentloanlawyer.com/scary-stats-for-public-service-loan-forgiveness/
10. https://www.marketwatch.com/story/this-government-loan-forgiveness-program-has-rejected-99-of-borrowers-so-far-2018-09-20
11. https://studentaid.gov/data-center/student/loan-forgiveness/pslf-data
12. https://www.nytimes.com/2019/04/12/your-money/public-service-loan-forgiveness.html
13. https://studentaid.gov/manage-loans/repayment/plans/income-driven
14. https://www.lrp.nih.gov/eligibility-programs
The young gastroenterologist has no shortage of personal finance topics to juggle, ranging from investments, to life and disability coverage, and planning for retirement. But the elephant in the room is student loan management. Average medical student debt today is approximately $240,000, and debt burdens greater than $300,000 are becoming common.1,2 With this staggering amount of debt, it is understandable why student loans are a major source of anxiety. Here, I will provide a brief introduction to student loan management for gastroenterologists.
Student loans: Basic strategy
It is important to distinguish between two major types of loans: private student loans and direct federal loans. With private student loans the best strategy in most cases is to refinance to a lower interest rate. For direct federal loans, however, the decision making is more complex. There are two major approaches to these federal loans – either 1) refinance, or 2) go for public service loan forgiveness (PSLF). See Figure 1 for a flowchart summarizing my general approach to student loan management.
Refinance basics
One potential approach is to refinance your federal loans. Most federal loans today are at a relatively high interest rate of 6%-8%.3 Private refinancing can yield rates in the 3%-5% range, depending on the type of loan and other factors. For a loan balance of $200,000, the savings by refinancing could be approximately $2,000-$10,000 per year in interest alone. However, refinancing your loans with a private company eliminates the possibility of PSLF. Hence, you should only refinance federal loans once you are sure that you will not be pursuing PSLF. You may refinance your private loans anytime since they do not qualify for PSLF. There are multiple companies that provide student loan refinancing. The process can be done online, sometimes in as little as 30 minutes. There is generally little or no cost to refinancing, and many companies even provide a small cash-back incentive to refinance.
PSLF basics
The PSLF program allows borrowers to have the remainder of their direct loans forgiven after 10 years (120 monthly payments) under a qualifying income-driven repayment (IDR) plan.4 Figure 2 shows an overview of the various IDR plans. During the 120 payments, the borrower must work full time for a qualifying employer, which includes a government employer or a not-for-profit 501(c)(3) organization. Loan forgiveness with PSLF is completely tax free. Importantly, the PSLF program only applies to direct federal loans. You can see your federal loan types and balances by visiting https://studentaid.gov/.
To PSLF or not to PSLF?
With direct federal loans, the decision to refinance or go for PSLF is a major fork in the road. PSLF can be a good option for borrowers with long training programs and with high student loan burdens (e.g., loan-to-income ratios of 1:1, 2:1 or higher). By contrast, borrowers with short training programs or relatively small loan burdens may be better off refinancing to a low interest rate and paying off loans quickly. Virtually all institutions that train residents and fellows are qualified government or 501(c)(3) organizations. Hence, a gastroenterology graduate generally will have completed at least 6 out of 10 years of payments by the end of training. Trainees who did a chief resident year or gastroenterology research track may have completed 7 or 8 years of qualifying payments already.
For trainees who are already planning an academic career, PSLF is often a good option. While PSLF can be a nice benefit, I would not advise making a career decision purely based on PSLF. Private practice jobs generally come with substantially higher salaries than academic and government jobs. This salary differential typically more than compensates for the loss of access to PSLF. Hence, I advise trainees to choose the practice setting that is best for their personal and career satisfaction, and then build a student loan management plan around that. The exception may be the trainee who has a very large student loan burden (e.g., loan-to-income ratio of 2:1 or 3:1).
Caveats with PSLF
There have been well publicized concerns about the future of PSLF, including proposals to eliminate or cap the program.5,6 However, most proposed legislation has only recommended changes to PSLF for new borrowers. If you currently have existing federal loans, you would very likely be grandfathered into the existing PSLF terms. All federal master promissory notes since 2007 have cited PSLF as a loan repayment option.7 Hence, eliminating PSLF for existing borrowers seems unlikely since it would be changing the terms of an executed contract.8
There have also been widespread reports of high numbers of borrowers being denied applications for PSLF.9,10 However, the majority of these applicants did not have correct types of loans, had not worked full time for qualifying employers or had not made the full 120 payments.11 Yet some denials have apparently resulted from errors in tracking qualifying payments by FedLoan servicing.12 Therefore it would be prudent to keep your own careful records of all qualifying payments towards PSLF.
The nuclear option: 20- to 25-year IDR-based forgiveness
An additional option allows borrowers to make IDRs for 20-25 years (details in Figure 2) and then having their remaining loan balance forgiven.13 This option is completely independent of PSLF. Borrowers can work full time or part time and can work for any employer, including private employers.
One additional option: NIH loan repayment programs
One additional solution to consider are the NIH Loan Repayment Programs (LRPs). These programs can provide substantial loan repayment (up to $50,000 annually) for trainees and attendings engaged in research that aligns with NIH priorities, including clinical research or health disparities research.14 Notably, the applicant’s research does not have to be NIH sponsored research.
Getting more information
The approach above is a general overview of student loan concepts for gastroenterologists. However, there are countless nuances and tactics that are beyond the scope of this introductory article. I encourage everyone to get additional information and advice when making your own loan management plan. There are many helpful online resources, podcasts, and books discussing the topic. Several companies provide detailed consultation on managing student loans. Such services may cost a few hundred dollars but could potentially save tens of thousands of dollars on student loan costs.
Dr. Jain is assistant professor of medicine, division of gastroenterology & hepatology, department of medicine, University of North Carolina School of Medicine, Chapel Hill. Dr. Jain has no conflicts of interest and no funding source.
References
1. https://nces.ed.gov/programs/digest/d18/tables/dt18_332.45.asp
2. https://www.credible.com/blog/statistics/average-medical-school-debt/
3. https://studentaid.gov/understand-aid/types/loans/interest-rates
4. https://studentaid.gov/manage-loans/forgiveness-cancellation/public-service
5. https://www.forbes.com/sites/robertfarrington/2019/09/24/how-to-get-your-public-service-loan-forgiveness-qualifying-payments-recounted/#18567f061f5d
6. https://www.cbo.gov/budget-options/2018/54721
7. https://static.studentloans.gov/images/ApplicationAndPromissoryNote.pdf
8. https://www.biglawinvestor.com/pslf-promissory-note/
9. https://bostonstudentloanlawyer.com/scary-stats-for-public-service-loan-forgiveness/
10. https://www.marketwatch.com/story/this-government-loan-forgiveness-program-has-rejected-99-of-borrowers-so-far-2018-09-20
11. https://studentaid.gov/data-center/student/loan-forgiveness/pslf-data
12. https://www.nytimes.com/2019/04/12/your-money/public-service-loan-forgiveness.html
13. https://studentaid.gov/manage-loans/repayment/plans/income-driven
14. https://www.lrp.nih.gov/eligibility-programs
The young gastroenterologist has no shortage of personal finance topics to juggle, ranging from investments, to life and disability coverage, and planning for retirement. But the elephant in the room is student loan management. Average medical student debt today is approximately $240,000, and debt burdens greater than $300,000 are becoming common.1,2 With this staggering amount of debt, it is understandable why student loans are a major source of anxiety. Here, I will provide a brief introduction to student loan management for gastroenterologists.
Student loans: Basic strategy
It is important to distinguish between two major types of loans: private student loans and direct federal loans. With private student loans the best strategy in most cases is to refinance to a lower interest rate. For direct federal loans, however, the decision making is more complex. There are two major approaches to these federal loans – either 1) refinance, or 2) go for public service loan forgiveness (PSLF). See Figure 1 for a flowchart summarizing my general approach to student loan management.
Refinance basics
One potential approach is to refinance your federal loans. Most federal loans today are at a relatively high interest rate of 6%-8%.3 Private refinancing can yield rates in the 3%-5% range, depending on the type of loan and other factors. For a loan balance of $200,000, the savings by refinancing could be approximately $2,000-$10,000 per year in interest alone. However, refinancing your loans with a private company eliminates the possibility of PSLF. Hence, you should only refinance federal loans once you are sure that you will not be pursuing PSLF. You may refinance your private loans anytime since they do not qualify for PSLF. There are multiple companies that provide student loan refinancing. The process can be done online, sometimes in as little as 30 minutes. There is generally little or no cost to refinancing, and many companies even provide a small cash-back incentive to refinance.
PSLF basics
The PSLF program allows borrowers to have the remainder of their direct loans forgiven after 10 years (120 monthly payments) under a qualifying income-driven repayment (IDR) plan.4 Figure 2 shows an overview of the various IDR plans. During the 120 payments, the borrower must work full time for a qualifying employer, which includes a government employer or a not-for-profit 501(c)(3) organization. Loan forgiveness with PSLF is completely tax free. Importantly, the PSLF program only applies to direct federal loans. You can see your federal loan types and balances by visiting https://studentaid.gov/.
To PSLF or not to PSLF?
With direct federal loans, the decision to refinance or go for PSLF is a major fork in the road. PSLF can be a good option for borrowers with long training programs and with high student loan burdens (e.g., loan-to-income ratios of 1:1, 2:1 or higher). By contrast, borrowers with short training programs or relatively small loan burdens may be better off refinancing to a low interest rate and paying off loans quickly. Virtually all institutions that train residents and fellows are qualified government or 501(c)(3) organizations. Hence, a gastroenterology graduate generally will have completed at least 6 out of 10 years of payments by the end of training. Trainees who did a chief resident year or gastroenterology research track may have completed 7 or 8 years of qualifying payments already.
For trainees who are already planning an academic career, PSLF is often a good option. While PSLF can be a nice benefit, I would not advise making a career decision purely based on PSLF. Private practice jobs generally come with substantially higher salaries than academic and government jobs. This salary differential typically more than compensates for the loss of access to PSLF. Hence, I advise trainees to choose the practice setting that is best for their personal and career satisfaction, and then build a student loan management plan around that. The exception may be the trainee who has a very large student loan burden (e.g., loan-to-income ratio of 2:1 or 3:1).
Caveats with PSLF
There have been well publicized concerns about the future of PSLF, including proposals to eliminate or cap the program.5,6 However, most proposed legislation has only recommended changes to PSLF for new borrowers. If you currently have existing federal loans, you would very likely be grandfathered into the existing PSLF terms. All federal master promissory notes since 2007 have cited PSLF as a loan repayment option.7 Hence, eliminating PSLF for existing borrowers seems unlikely since it would be changing the terms of an executed contract.8
There have also been widespread reports of high numbers of borrowers being denied applications for PSLF.9,10 However, the majority of these applicants did not have correct types of loans, had not worked full time for qualifying employers or had not made the full 120 payments.11 Yet some denials have apparently resulted from errors in tracking qualifying payments by FedLoan servicing.12 Therefore it would be prudent to keep your own careful records of all qualifying payments towards PSLF.
The nuclear option: 20- to 25-year IDR-based forgiveness
An additional option allows borrowers to make IDRs for 20-25 years (details in Figure 2) and then having their remaining loan balance forgiven.13 This option is completely independent of PSLF. Borrowers can work full time or part time and can work for any employer, including private employers.
One additional option: NIH loan repayment programs
One additional solution to consider are the NIH Loan Repayment Programs (LRPs). These programs can provide substantial loan repayment (up to $50,000 annually) for trainees and attendings engaged in research that aligns with NIH priorities, including clinical research or health disparities research.14 Notably, the applicant’s research does not have to be NIH sponsored research.
Getting more information
The approach above is a general overview of student loan concepts for gastroenterologists. However, there are countless nuances and tactics that are beyond the scope of this introductory article. I encourage everyone to get additional information and advice when making your own loan management plan. There are many helpful online resources, podcasts, and books discussing the topic. Several companies provide detailed consultation on managing student loans. Such services may cost a few hundred dollars but could potentially save tens of thousands of dollars on student loan costs.
Dr. Jain is assistant professor of medicine, division of gastroenterology & hepatology, department of medicine, University of North Carolina School of Medicine, Chapel Hill. Dr. Jain has no conflicts of interest and no funding source.
References
1. https://nces.ed.gov/programs/digest/d18/tables/dt18_332.45.asp
2. https://www.credible.com/blog/statistics/average-medical-school-debt/
3. https://studentaid.gov/understand-aid/types/loans/interest-rates
4. https://studentaid.gov/manage-loans/forgiveness-cancellation/public-service
5. https://www.forbes.com/sites/robertfarrington/2019/09/24/how-to-get-your-public-service-loan-forgiveness-qualifying-payments-recounted/#18567f061f5d
6. https://www.cbo.gov/budget-options/2018/54721
7. https://static.studentloans.gov/images/ApplicationAndPromissoryNote.pdf
8. https://www.biglawinvestor.com/pslf-promissory-note/
9. https://bostonstudentloanlawyer.com/scary-stats-for-public-service-loan-forgiveness/
10. https://www.marketwatch.com/story/this-government-loan-forgiveness-program-has-rejected-99-of-borrowers-so-far-2018-09-20
11. https://studentaid.gov/data-center/student/loan-forgiveness/pslf-data
12. https://www.nytimes.com/2019/04/12/your-money/public-service-loan-forgiveness.html
13. https://studentaid.gov/manage-loans/repayment/plans/income-driven
14. https://www.lrp.nih.gov/eligibility-programs
Pitfalls in physician-patient communication via patient access support portals
Technology can be used to enhance communication, increase patient safety, and improve overall patient care. For example, many physicians have arranged for remote access to medical records and established a unique system of communication via a patient access support portal. A patient portal is a secure online website that provides patients 24-hour, on-demand access to their health information. Patient portals, while popular and oftentimes quite helpful, are not without drawbacks. Communication by electronic means with your patient can be viewed by some as impersonal and can make patients less tolerant to what they perceive to be a mistake, error, or unwanted outcome. A decrease in face-to-face contact and communication with your patient also gives you less time to resolve any conflict or disagreement. While communication via a patient access support portal has the potential to free up medical staff for direct patient care, such communication also carries liability risk.
Patient access support portal
A physician’s legal responsibility to communicate in a timely and accurate manner does not change, irrespective of the form of communication. However, communication via a patient access portal does have some unique features that must be considered by the practitioner. Practitioners must remember that any communication via the patient portal creates a permanent record, which can and will be used in the event of litigation. For example, when responding to a patient inquiry about a specific complaint, treatment provided, or test result, it will be presumed that the physician had access to the patient’s full medical record and that the full record will be utilized in making a response. Accessing the patient’s chart will leave an audit trail that will provide what is known as metadata, which in the context of electronic medical records, is what allows technicians to verify that the patient record was accessed, and it provides details as to when, and for how long it was accessed. These records are frequently pursued in litigation, so you must understand that parties can often re-create an intricate and accurate timeline of events. While state courts are divided on the issue of whether metadata contained within electronic medical records is discoverable, recent federal court decisions have held that such data is discoverable pursuant to the Federal Rules of Civil Procedure. Thus, once a patient has communicated with you via the portal, you will be responsible for responding in an appropriate and prompt fashion. For these reasons, it is imperative that you create an agreement with your patients as to how the portal will be used and clearly set forth the rules for such use.
Patient portal policies and procedures
In creating patient portal user agreements (See "Sample User Agreement," attached below), it is crucial that an agreement clearly identify the policies and procedures for use. A patient portal user agreement should:
- Set forth the rules and regulations for portal use.
- Include a verification procedure that requires the patients to confirm that they have the legal capacity to consent to the terms of use. This is especially important when treating patients with mental disability, elderly patients with dementia, minors, and any other individuals who may not legally consent.
- Include a verification procedure that requires the patients to confirm that they understand and agree to abide by the user agreement rules.
- Include a detailed list that informs users of the risks and benefits of communicating via the patient portal.
- Stress that communication through the patient portal is for nonemergent matters only.
- Set forth permissible topics for use, such as communicating with the physician or staff, obtaining test results or records, and setting, changing, or canceling appointments.
- Clearly indicate certain topics that should not be discussed via the patient portal, including mental health issues.
- Reiterate that communication via the patient portal is only one option, and that all other standard methods of communication remain available. In doing so, provide office telephone numbers, hotlines, and email addresses for convenience.
- Inform the patients that they should call the office with any questions or concerns regarding use of the patient portal.
- Include a statement that the patient should call 911 or proceed directly to the nearest hospital for any and all urgent or emergent medical matters.
Other considerations
There are, however, equally critical considerations to be made that go beyond the core details of the user agreement. For instance, use of the patient access portal should be limited to only current or active patients, and you should stress to patients the importance of keeping their contact information updated and accurate. This is especially vital in situations in which a patient is unresponsive to communication via the portal, as your staff will need to follow up via other means of communication. It is also imperative to ensure the patient portal is programmed to promptly alert you or your staff following an inquiry from the patient as the patient will likely expect an immediate response.
Notably, communication via the patient portal must still comply with the Health Insurance Portability and Accountability Act (HIPAA). This means that only authorized users are able to access records within the patient portal. To ensure compliance with HIPAA, all users should be instructed in the appropriate practices of maintaining patient privacy. This includes barring the use of shared passwords amongst multiple individuals, requiring that users enable an auto log-off setting, and programming work stations to turn off automatically after brief periods of nonuse. Further, all communications in the patient portal should be encrypted to prevent the patient’s sensitive information from being accessed in the event of an attempted security breach.
Finally, depending upon the practice, there may be instances in which someone other than the patient’s physician would be reading and responding to patient queries. In these situations, the patient should be informed of such potential. This way, if the communication is intended only for the physician, the patient will be afforded the opportunity to call the physician directly rather than communicate via the patient portal.
While the use of patient access portals is becoming far more prevalent, as they offer many practical benefits ranging from increased convenience and efficiency to enhanced patient care, they also carry the potential for increased liability exposure. As such, it is vital that physicians weigh all potential risks and benefits that are inherent in the use of patient access portals prior to making the decision to implement such technology.
Mr. Mills is an equity partner in Cunningham, Meyer & Vedrine, Chicago.
Technology can be used to enhance communication, increase patient safety, and improve overall patient care. For example, many physicians have arranged for remote access to medical records and established a unique system of communication via a patient access support portal. A patient portal is a secure online website that provides patients 24-hour, on-demand access to their health information. Patient portals, while popular and oftentimes quite helpful, are not without drawbacks. Communication by electronic means with your patient can be viewed by some as impersonal and can make patients less tolerant to what they perceive to be a mistake, error, or unwanted outcome. A decrease in face-to-face contact and communication with your patient also gives you less time to resolve any conflict or disagreement. While communication via a patient access support portal has the potential to free up medical staff for direct patient care, such communication also carries liability risk.
Patient access support portal
A physician’s legal responsibility to communicate in a timely and accurate manner does not change, irrespective of the form of communication. However, communication via a patient access portal does have some unique features that must be considered by the practitioner. Practitioners must remember that any communication via the patient portal creates a permanent record, which can and will be used in the event of litigation. For example, when responding to a patient inquiry about a specific complaint, treatment provided, or test result, it will be presumed that the physician had access to the patient’s full medical record and that the full record will be utilized in making a response. Accessing the patient’s chart will leave an audit trail that will provide what is known as metadata, which in the context of electronic medical records, is what allows technicians to verify that the patient record was accessed, and it provides details as to when, and for how long it was accessed. These records are frequently pursued in litigation, so you must understand that parties can often re-create an intricate and accurate timeline of events. While state courts are divided on the issue of whether metadata contained within electronic medical records is discoverable, recent federal court decisions have held that such data is discoverable pursuant to the Federal Rules of Civil Procedure. Thus, once a patient has communicated with you via the portal, you will be responsible for responding in an appropriate and prompt fashion. For these reasons, it is imperative that you create an agreement with your patients as to how the portal will be used and clearly set forth the rules for such use.
Patient portal policies and procedures
In creating patient portal user agreements (See "Sample User Agreement," attached below), it is crucial that an agreement clearly identify the policies and procedures for use. A patient portal user agreement should:
- Set forth the rules and regulations for portal use.
- Include a verification procedure that requires the patients to confirm that they have the legal capacity to consent to the terms of use. This is especially important when treating patients with mental disability, elderly patients with dementia, minors, and any other individuals who may not legally consent.
- Include a verification procedure that requires the patients to confirm that they understand and agree to abide by the user agreement rules.
- Include a detailed list that informs users of the risks and benefits of communicating via the patient portal.
- Stress that communication through the patient portal is for nonemergent matters only.
- Set forth permissible topics for use, such as communicating with the physician or staff, obtaining test results or records, and setting, changing, or canceling appointments.
- Clearly indicate certain topics that should not be discussed via the patient portal, including mental health issues.
- Reiterate that communication via the patient portal is only one option, and that all other standard methods of communication remain available. In doing so, provide office telephone numbers, hotlines, and email addresses for convenience.
- Inform the patients that they should call the office with any questions or concerns regarding use of the patient portal.
- Include a statement that the patient should call 911 or proceed directly to the nearest hospital for any and all urgent or emergent medical matters.
Other considerations
There are, however, equally critical considerations to be made that go beyond the core details of the user agreement. For instance, use of the patient access portal should be limited to only current or active patients, and you should stress to patients the importance of keeping their contact information updated and accurate. This is especially vital in situations in which a patient is unresponsive to communication via the portal, as your staff will need to follow up via other means of communication. It is also imperative to ensure the patient portal is programmed to promptly alert you or your staff following an inquiry from the patient as the patient will likely expect an immediate response.
Notably, communication via the patient portal must still comply with the Health Insurance Portability and Accountability Act (HIPAA). This means that only authorized users are able to access records within the patient portal. To ensure compliance with HIPAA, all users should be instructed in the appropriate practices of maintaining patient privacy. This includes barring the use of shared passwords amongst multiple individuals, requiring that users enable an auto log-off setting, and programming work stations to turn off automatically after brief periods of nonuse. Further, all communications in the patient portal should be encrypted to prevent the patient’s sensitive information from being accessed in the event of an attempted security breach.
Finally, depending upon the practice, there may be instances in which someone other than the patient’s physician would be reading and responding to patient queries. In these situations, the patient should be informed of such potential. This way, if the communication is intended only for the physician, the patient will be afforded the opportunity to call the physician directly rather than communicate via the patient portal.
While the use of patient access portals is becoming far more prevalent, as they offer many practical benefits ranging from increased convenience and efficiency to enhanced patient care, they also carry the potential for increased liability exposure. As such, it is vital that physicians weigh all potential risks and benefits that are inherent in the use of patient access portals prior to making the decision to implement such technology.
Mr. Mills is an equity partner in Cunningham, Meyer & Vedrine, Chicago.
Technology can be used to enhance communication, increase patient safety, and improve overall patient care. For example, many physicians have arranged for remote access to medical records and established a unique system of communication via a patient access support portal. A patient portal is a secure online website that provides patients 24-hour, on-demand access to their health information. Patient portals, while popular and oftentimes quite helpful, are not without drawbacks. Communication by electronic means with your patient can be viewed by some as impersonal and can make patients less tolerant to what they perceive to be a mistake, error, or unwanted outcome. A decrease in face-to-face contact and communication with your patient also gives you less time to resolve any conflict or disagreement. While communication via a patient access support portal has the potential to free up medical staff for direct patient care, such communication also carries liability risk.
Patient access support portal
A physician’s legal responsibility to communicate in a timely and accurate manner does not change, irrespective of the form of communication. However, communication via a patient access portal does have some unique features that must be considered by the practitioner. Practitioners must remember that any communication via the patient portal creates a permanent record, which can and will be used in the event of litigation. For example, when responding to a patient inquiry about a specific complaint, treatment provided, or test result, it will be presumed that the physician had access to the patient’s full medical record and that the full record will be utilized in making a response. Accessing the patient’s chart will leave an audit trail that will provide what is known as metadata, which in the context of electronic medical records, is what allows technicians to verify that the patient record was accessed, and it provides details as to when, and for how long it was accessed. These records are frequently pursued in litigation, so you must understand that parties can often re-create an intricate and accurate timeline of events. While state courts are divided on the issue of whether metadata contained within electronic medical records is discoverable, recent federal court decisions have held that such data is discoverable pursuant to the Federal Rules of Civil Procedure. Thus, once a patient has communicated with you via the portal, you will be responsible for responding in an appropriate and prompt fashion. For these reasons, it is imperative that you create an agreement with your patients as to how the portal will be used and clearly set forth the rules for such use.
Patient portal policies and procedures
In creating patient portal user agreements (See "Sample User Agreement," attached below), it is crucial that an agreement clearly identify the policies and procedures for use. A patient portal user agreement should:
- Set forth the rules and regulations for portal use.
- Include a verification procedure that requires the patients to confirm that they have the legal capacity to consent to the terms of use. This is especially important when treating patients with mental disability, elderly patients with dementia, minors, and any other individuals who may not legally consent.
- Include a verification procedure that requires the patients to confirm that they understand and agree to abide by the user agreement rules.
- Include a detailed list that informs users of the risks and benefits of communicating via the patient portal.
- Stress that communication through the patient portal is for nonemergent matters only.
- Set forth permissible topics for use, such as communicating with the physician or staff, obtaining test results or records, and setting, changing, or canceling appointments.
- Clearly indicate certain topics that should not be discussed via the patient portal, including mental health issues.
- Reiterate that communication via the patient portal is only one option, and that all other standard methods of communication remain available. In doing so, provide office telephone numbers, hotlines, and email addresses for convenience.
- Inform the patients that they should call the office with any questions or concerns regarding use of the patient portal.
- Include a statement that the patient should call 911 or proceed directly to the nearest hospital for any and all urgent or emergent medical matters.
Other considerations
There are, however, equally critical considerations to be made that go beyond the core details of the user agreement. For instance, use of the patient access portal should be limited to only current or active patients, and you should stress to patients the importance of keeping their contact information updated and accurate. This is especially vital in situations in which a patient is unresponsive to communication via the portal, as your staff will need to follow up via other means of communication. It is also imperative to ensure the patient portal is programmed to promptly alert you or your staff following an inquiry from the patient as the patient will likely expect an immediate response.
Notably, communication via the patient portal must still comply with the Health Insurance Portability and Accountability Act (HIPAA). This means that only authorized users are able to access records within the patient portal. To ensure compliance with HIPAA, all users should be instructed in the appropriate practices of maintaining patient privacy. This includes barring the use of shared passwords amongst multiple individuals, requiring that users enable an auto log-off setting, and programming work stations to turn off automatically after brief periods of nonuse. Further, all communications in the patient portal should be encrypted to prevent the patient’s sensitive information from being accessed in the event of an attempted security breach.
Finally, depending upon the practice, there may be instances in which someone other than the patient’s physician would be reading and responding to patient queries. In these situations, the patient should be informed of such potential. This way, if the communication is intended only for the physician, the patient will be afforded the opportunity to call the physician directly rather than communicate via the patient portal.
While the use of patient access portals is becoming far more prevalent, as they offer many practical benefits ranging from increased convenience and efficiency to enhanced patient care, they also carry the potential for increased liability exposure. As such, it is vital that physicians weigh all potential risks and benefits that are inherent in the use of patient access portals prior to making the decision to implement such technology.
Mr. Mills is an equity partner in Cunningham, Meyer & Vedrine, Chicago.
Estate planning: A must-do for all medical professionals
As medical professionals, you may have encountered patients with serious illnesses and asked yourself the following questions: What if I was in that situation? Where will my assets go when I die? What will happen to my loved ones, and will they be taken care of? Who would handle my affairs if I became ill? These important questions can only be addressed through effective estate planning.
Everyone needs an estate plan regardless of age, health, and financial or family situation. An effective estate plan provides for the orderly management and disposition of your assets upon your death. In addition, as medical professionals may appreciate, an effective estate plan appoints individuals to manage your financial affairs and make health care decisions for you in the event that you become physically or mentally incapacitated.
The most common estate planning tool is a will, which dictates how your assets pass at death. In addition, a will identifies the personal representative of your estate (that is, the person who will see that your assets pass in accordance with your wishes) and, in many states, identifies the guardian of any minor children. Although a court will make the ultimate determination of who is appointed as the guardian, courts typically give significant weight to the person named in a will.
If you die “intestate,” meaning that you died without a valid will, your assets will be distributed in accordance with your state’s intestacy statutes, and any interested person (as opposed to the individual of your choice) may be appointed as the personal representative of your estate. Therefore, to ensure that your property goes to the individuals of your choice and that your final affairs are handled by the person you trust, a will is essential.
In many states, a revocable living trust can be equally beneficial. Like a will, a revocable living trust will dictate how your property passes at death and appoints a trustee to see that the property is distributed in accordance with your wishes. Revocable living trusts can be great tools for incapacity planning and, unlike a will, are not required to be recorded, so the trust agreement can remain private. The assets that are held in a revocable living trust also avoid the often lengthy and expensive probate process, which generally includes the preparation and filing of a petition to open the estate, an inventory identifying the assets of the estate, and an accounting that details all assets received and distributed, followed by the payment of fees based upon the value of the probate estate.
In many situations, leaving assets to young, disabled, or troubled children would result in catastrophic consequences, such as disqualification for government benefits, dissipation of assets for inappropriate uses, or attachment by creditors. Further, for wealthy individuals, outright distributions to spouses could lead to unnecessary estate tax. Wills and revocable trusts can protect against these issues by requiring that, at death, the decedent’s assets are held in further trust for these individuals.
There are various types of trusts that can help ensure that your assets are used for the benefit of your loved one while avoiding any unintended consequences, some of which include the following:
- Special needs trusts, which allow the trustee to use the trust funds for the benefit of the disabled beneficiary without disqualifying the beneficiary from important government benefits.
- Spendthrift trusts, which can protect the trust assets from claims of creditors or property division in a divorce action.
- Marital trusts, which can be used to reduce taxes and ensure that property will be distributed pursuant to your wishes upon the death of your spouse.
- Dynasty trusts, which can be used to protect assets for many generations and, in doing so, reduce the amount of federal and state transfer taxes.
Whether you use a will or revocable living trust, it is critical to coordinate the beneficiary designations of assets such as retirement accounts and life insurance policies, as well as any other account that passes by beneficiary designation. These beneficiary designations trump the provisions of your will and revocable living trust. Likewise, property owned jointly with another person as joint tenants with the right of survivorship, or with a spouse as tenants by the entirety, will pass directly to the joint owner and not pursuant to the terms of your will or revocable trust.
An effective estate plan involves not just planning for death, but also for your incapacity. A durable power of attorney allows you to select an agent or agents to manage your property during your lifetime. The power of attorney can become effective immediately so that the agent can act on your behalf upon execution of the document or the power of attorney can become effective only if and when you become incapacitated.
A durable power of attorney for health care (or advance health care directive) permits you to appoint an agent to make health care decisions on your behalf in the event that you cannot make your own decisions. In addition, should you become permanently unconscious or in a terminal condition, it permits you to appoint an agent who can withhold or withdraw life-sustaining treatment. With a living will, you can express in writing the circumstances under which you do or do not want artificial life-sustaining measures.
With respect to these powers of attorney, the persons that you appoint as your agents should be people that you trust. It is also important to have conversations with your designated agents to ensure that they understand their responsibilities and your wishes. Without these powers of attorney, in the event of your incapacitation, a court will appoint a guardian. The guardian may not be the person you would have appointed, and it will result in annual, and burdensome, court filings.
As busy medical professionals, it may be difficult to find time to develop an estate plan and you may believe that there is plenty of time to do it in the future. It is important to begin thinking about your estate-planning goals and to speak with an attorney to help develop and draft your estate-planning documents. If you already have estate-planning documents, it is important to review those documents periodically to ensure that your estate-planning objectives have remained the same and, if they have changed, to update your documents.
No one knows what the future will hold, so it is important to consult with a local attorney to establish or review your estate plan now. If you do, you will be comforted by the fact that you and your loved ones will be taken care of in accordance with your wishes if you are unable to do so in the future.
Mr. D’Emilio is a managing member and Mr. Riley is an associate at McCollom D’Emilio Smith Uebler, Wilmington, Del.
As medical professionals, you may have encountered patients with serious illnesses and asked yourself the following questions: What if I was in that situation? Where will my assets go when I die? What will happen to my loved ones, and will they be taken care of? Who would handle my affairs if I became ill? These important questions can only be addressed through effective estate planning.
Everyone needs an estate plan regardless of age, health, and financial or family situation. An effective estate plan provides for the orderly management and disposition of your assets upon your death. In addition, as medical professionals may appreciate, an effective estate plan appoints individuals to manage your financial affairs and make health care decisions for you in the event that you become physically or mentally incapacitated.
The most common estate planning tool is a will, which dictates how your assets pass at death. In addition, a will identifies the personal representative of your estate (that is, the person who will see that your assets pass in accordance with your wishes) and, in many states, identifies the guardian of any minor children. Although a court will make the ultimate determination of who is appointed as the guardian, courts typically give significant weight to the person named in a will.
If you die “intestate,” meaning that you died without a valid will, your assets will be distributed in accordance with your state’s intestacy statutes, and any interested person (as opposed to the individual of your choice) may be appointed as the personal representative of your estate. Therefore, to ensure that your property goes to the individuals of your choice and that your final affairs are handled by the person you trust, a will is essential.
In many states, a revocable living trust can be equally beneficial. Like a will, a revocable living trust will dictate how your property passes at death and appoints a trustee to see that the property is distributed in accordance with your wishes. Revocable living trusts can be great tools for incapacity planning and, unlike a will, are not required to be recorded, so the trust agreement can remain private. The assets that are held in a revocable living trust also avoid the often lengthy and expensive probate process, which generally includes the preparation and filing of a petition to open the estate, an inventory identifying the assets of the estate, and an accounting that details all assets received and distributed, followed by the payment of fees based upon the value of the probate estate.
In many situations, leaving assets to young, disabled, or troubled children would result in catastrophic consequences, such as disqualification for government benefits, dissipation of assets for inappropriate uses, or attachment by creditors. Further, for wealthy individuals, outright distributions to spouses could lead to unnecessary estate tax. Wills and revocable trusts can protect against these issues by requiring that, at death, the decedent’s assets are held in further trust for these individuals.
There are various types of trusts that can help ensure that your assets are used for the benefit of your loved one while avoiding any unintended consequences, some of which include the following:
- Special needs trusts, which allow the trustee to use the trust funds for the benefit of the disabled beneficiary without disqualifying the beneficiary from important government benefits.
- Spendthrift trusts, which can protect the trust assets from claims of creditors or property division in a divorce action.
- Marital trusts, which can be used to reduce taxes and ensure that property will be distributed pursuant to your wishes upon the death of your spouse.
- Dynasty trusts, which can be used to protect assets for many generations and, in doing so, reduce the amount of federal and state transfer taxes.
Whether you use a will or revocable living trust, it is critical to coordinate the beneficiary designations of assets such as retirement accounts and life insurance policies, as well as any other account that passes by beneficiary designation. These beneficiary designations trump the provisions of your will and revocable living trust. Likewise, property owned jointly with another person as joint tenants with the right of survivorship, or with a spouse as tenants by the entirety, will pass directly to the joint owner and not pursuant to the terms of your will or revocable trust.
An effective estate plan involves not just planning for death, but also for your incapacity. A durable power of attorney allows you to select an agent or agents to manage your property during your lifetime. The power of attorney can become effective immediately so that the agent can act on your behalf upon execution of the document or the power of attorney can become effective only if and when you become incapacitated.
A durable power of attorney for health care (or advance health care directive) permits you to appoint an agent to make health care decisions on your behalf in the event that you cannot make your own decisions. In addition, should you become permanently unconscious or in a terminal condition, it permits you to appoint an agent who can withhold or withdraw life-sustaining treatment. With a living will, you can express in writing the circumstances under which you do or do not want artificial life-sustaining measures.
With respect to these powers of attorney, the persons that you appoint as your agents should be people that you trust. It is also important to have conversations with your designated agents to ensure that they understand their responsibilities and your wishes. Without these powers of attorney, in the event of your incapacitation, a court will appoint a guardian. The guardian may not be the person you would have appointed, and it will result in annual, and burdensome, court filings.
As busy medical professionals, it may be difficult to find time to develop an estate plan and you may believe that there is plenty of time to do it in the future. It is important to begin thinking about your estate-planning goals and to speak with an attorney to help develop and draft your estate-planning documents. If you already have estate-planning documents, it is important to review those documents periodically to ensure that your estate-planning objectives have remained the same and, if they have changed, to update your documents.
No one knows what the future will hold, so it is important to consult with a local attorney to establish or review your estate plan now. If you do, you will be comforted by the fact that you and your loved ones will be taken care of in accordance with your wishes if you are unable to do so in the future.
Mr. D’Emilio is a managing member and Mr. Riley is an associate at McCollom D’Emilio Smith Uebler, Wilmington, Del.
As medical professionals, you may have encountered patients with serious illnesses and asked yourself the following questions: What if I was in that situation? Where will my assets go when I die? What will happen to my loved ones, and will they be taken care of? Who would handle my affairs if I became ill? These important questions can only be addressed through effective estate planning.
Everyone needs an estate plan regardless of age, health, and financial or family situation. An effective estate plan provides for the orderly management and disposition of your assets upon your death. In addition, as medical professionals may appreciate, an effective estate plan appoints individuals to manage your financial affairs and make health care decisions for you in the event that you become physically or mentally incapacitated.
The most common estate planning tool is a will, which dictates how your assets pass at death. In addition, a will identifies the personal representative of your estate (that is, the person who will see that your assets pass in accordance with your wishes) and, in many states, identifies the guardian of any minor children. Although a court will make the ultimate determination of who is appointed as the guardian, courts typically give significant weight to the person named in a will.
If you die “intestate,” meaning that you died without a valid will, your assets will be distributed in accordance with your state’s intestacy statutes, and any interested person (as opposed to the individual of your choice) may be appointed as the personal representative of your estate. Therefore, to ensure that your property goes to the individuals of your choice and that your final affairs are handled by the person you trust, a will is essential.
In many states, a revocable living trust can be equally beneficial. Like a will, a revocable living trust will dictate how your property passes at death and appoints a trustee to see that the property is distributed in accordance with your wishes. Revocable living trusts can be great tools for incapacity planning and, unlike a will, are not required to be recorded, so the trust agreement can remain private. The assets that are held in a revocable living trust also avoid the often lengthy and expensive probate process, which generally includes the preparation and filing of a petition to open the estate, an inventory identifying the assets of the estate, and an accounting that details all assets received and distributed, followed by the payment of fees based upon the value of the probate estate.
In many situations, leaving assets to young, disabled, or troubled children would result in catastrophic consequences, such as disqualification for government benefits, dissipation of assets for inappropriate uses, or attachment by creditors. Further, for wealthy individuals, outright distributions to spouses could lead to unnecessary estate tax. Wills and revocable trusts can protect against these issues by requiring that, at death, the decedent’s assets are held in further trust for these individuals.
There are various types of trusts that can help ensure that your assets are used for the benefit of your loved one while avoiding any unintended consequences, some of which include the following:
- Special needs trusts, which allow the trustee to use the trust funds for the benefit of the disabled beneficiary without disqualifying the beneficiary from important government benefits.
- Spendthrift trusts, which can protect the trust assets from claims of creditors or property division in a divorce action.
- Marital trusts, which can be used to reduce taxes and ensure that property will be distributed pursuant to your wishes upon the death of your spouse.
- Dynasty trusts, which can be used to protect assets for many generations and, in doing so, reduce the amount of federal and state transfer taxes.
Whether you use a will or revocable living trust, it is critical to coordinate the beneficiary designations of assets such as retirement accounts and life insurance policies, as well as any other account that passes by beneficiary designation. These beneficiary designations trump the provisions of your will and revocable living trust. Likewise, property owned jointly with another person as joint tenants with the right of survivorship, or with a spouse as tenants by the entirety, will pass directly to the joint owner and not pursuant to the terms of your will or revocable trust.
An effective estate plan involves not just planning for death, but also for your incapacity. A durable power of attorney allows you to select an agent or agents to manage your property during your lifetime. The power of attorney can become effective immediately so that the agent can act on your behalf upon execution of the document or the power of attorney can become effective only if and when you become incapacitated.
A durable power of attorney for health care (or advance health care directive) permits you to appoint an agent to make health care decisions on your behalf in the event that you cannot make your own decisions. In addition, should you become permanently unconscious or in a terminal condition, it permits you to appoint an agent who can withhold or withdraw life-sustaining treatment. With a living will, you can express in writing the circumstances under which you do or do not want artificial life-sustaining measures.
With respect to these powers of attorney, the persons that you appoint as your agents should be people that you trust. It is also important to have conversations with your designated agents to ensure that they understand their responsibilities and your wishes. Without these powers of attorney, in the event of your incapacitation, a court will appoint a guardian. The guardian may not be the person you would have appointed, and it will result in annual, and burdensome, court filings.
As busy medical professionals, it may be difficult to find time to develop an estate plan and you may believe that there is plenty of time to do it in the future. It is important to begin thinking about your estate-planning goals and to speak with an attorney to help develop and draft your estate-planning documents. If you already have estate-planning documents, it is important to review those documents periodically to ensure that your estate-planning objectives have remained the same and, if they have changed, to update your documents.
No one knows what the future will hold, so it is important to consult with a local attorney to establish or review your estate plan now. If you do, you will be comforted by the fact that you and your loved ones will be taken care of in accordance with your wishes if you are unable to do so in the future.
Mr. D’Emilio is a managing member and Mr. Riley is an associate at McCollom D’Emilio Smith Uebler, Wilmington, Del.
Gastroenterology billing and coding: Just the basics
Understanding the business side of medicine helps physicians run a successful practice. However, the business side of medicine is not part of the normal curriculum in training and fellowship programs. Physicians come out of training with the knowledge to treat patients but with little or no knowledge of how to get reimbursed for their services. Gastroenterologists provide both medical and surgical services.
Listed below are some of the basic principles for both documentation and reimbursement policies. All reimbursement is based upon Relative Value Units (RVUs) assigned to every service provided. The services are based upon three factors: physician work value, malpractice cost, and practice expense. Those factors added together and multiplied by a conversion factor assigned by the Centers for Medicare & Medicaid Services (CMS) creates the national physician fee schedule. Each Medicare carrier has localities, and there is another percentage that is multiplied based upon geographic location, which will finalize the approved amount for each service. Your Medicare carrier has the actual approved amounts available on their websites with an effective date of Jan. 1. Commercial payers most commonly base contracts on the Medicare Fee Schedule, but each practice and payer relationship is different. For a better understanding, please contact your practice manager for more specific information based on your payer contracts.
Medical necessity is the key to success. If medical necessity is not demonstrated, payers can deny a claim, deny authorization for a lab test and/or diagnostic study, or recoup previously paid claims. Medicare and commercial payers will often have local coverage determinations (LCDs) for procedures and testing that include indications and restrictions along with approved diagnosis codes. Listed below are the four primary services that GI providers perform and provide interpretation for:
1. Evaluation and management (E&M) services: There are three criteria that have to be met to support any initial visit with patients: the history obtained, the examination performed, and the development of the treatment plan. There are five levels of service for office visits and three levels for inpatient visits, respectively. The levels are chosen based on the decision-making element of the visit, provided the documentation requirements are met for the level chosen. This is often not an easy selection unless the providers are educated on the E&M criteria. Auditors often see that visits are chosen by “guessing” the level, which leads to choosing either a lower or higher level of service than what was actually provided. Some providers have been instructed that E&M services are not that important since procedures are the major source of revenue for the practice. However, GI practices are visit-driven practices, and the initial visits are often worth more RVUs than some procedures. The E&M visit is truly vital and often the backbone for the medical necessity of any additional procedures and diagnostic services required in order for successful treatment of the patient.
2. Endoscopy and procedural billing: Here, medical necessity must be documented in order to submit charges for what was done. Gastroenterologists will often use multiple techniques when treating different areas within the gastrointestinal tract. Documentation has to include the location of lesions/abnormalities, method of treatment/removal, and the reason(s)/indication(s) for those procedures. There may be different instruments used in the colon (for example, snare in the sigmoid colon or biopsy forceps in the transverse colon). These may be separately reported with an appropriate modifier to indicate that these services were performed to different lesions/abnormalities. However, in order to bill for each of the procedures, all of this has to be documented in the endoscopy report. The physician is responsible for accurate and specific documentation and bringing charges back to the billing staff for claim submission. For a successful practice, a team approach is vital. Physicians and coding staff need to have an open line of communication to make sure that everything is submitted appropriately according to payer policies. Billing staff need to communicate any significant changes to the physicians/providers as these changes occur. Ignorance of payer policy is not considered an appropriate excuse when a payer investigates a claim and potential recoupment of moneys paid.
3. Diagnostic studies: Medical necessity/indication for the testing must be documented in order to submit charges for diagnostic studies. The terms “rule out” and “suspect” don’t completely give coders the reason why a physician suspects the patient might have a condition. Usually, abnormal lab tests, signs, and symptoms will often warrant the need for further investigation, and these are the most crucial indications for testing. Not only is this important for diagnostic studies but also for procedures. Make sure that the interpretation of the test results is clear along with a plan/recommendation(s).
4. Diagnosis codes: Assignment of codes per the International Classification of Diseases, 10th revision, Clinical Modification (ICD-10-CM) is the next and most important step after a visit, diagnostic study, and/or procedure. These codes support medical necessity for the services provided, and specificity of the diagnosis code is vital to successful submission and payment of a claim. Signs and symptoms are valid code choices when ruling out a more significant disease/diagnosis because these support medical necessity for a work-up to determine etiology. Comorbidities that impact the provider’s decision making should also be added as additional diagnoses to support the higher level of decision making. Up to 12 diagnosis codes can be assigned to any type of service provided. This also applies to preauthorization of all services, such as lab tests, radiology studies, GI diagnostic studies, and procedures. If specific information is not in the documentation for your staff to access, payers will often deny certain lab and radiology studies, as well as some procedures. There are 71,932 ICD-10-CM codes to choose from, and it is often difficult to find the “specific” code when doing a search in the electronic health record and billing system. Education and training are essential during the orientation sessions prior to active employment, as well as any time the system is upgraded. The providers should be willing to work with the IT representative(s) in the practice to help make the information easier to access. In other words, what “buzz” words would they like included in the description of the ICD-10-CM code in the practice’s list of favorites? For example, Crohn’s disease and ulcerative colitis have over a hundred choices. The choices are based on the location of the disease and whether the disease is without or with complications. If you are going to choose to provide a higher level of E&M service for a patient with Crohn’s disease of the large intestine because of exacerbation of the disease with bleeding, then the appropriate diagnosis code would be one of the following:
- K50.10 Crohn’s disease of large intestine without complications.
- K50.111 Crohn’s disease of large intestine with rectal bleeding.
- K50.112 Crohn’s disease of large intestine with intestinal obstruction.
- K50.113 Crohn’s disease of large intestine with fistula.
- K50.114 Crohn’s disease of large intestine with abscess.
- K50.118 Crohn’s disease of large intestine with other complication.
- K50.119 Crohn’s disease of large intestine with unspecified complications.
Getting paid for your provided services requires attention to detail and communication with your entire staffing team, including all providers. Make sure that your team is educated on all current issues and services pertaining to gastroenterology practices. If there is ever a question when reviewing a procedure note or any service, ask the provider who performed that service. Often, there will have to be legal corrections to the note before services can be billed. Making sure that the claim you are submitting is “clean” is essential for prompt payment. There are multiple resources available through the AGA that will help guide you with coding and billing. There are webinars, training sessions, and onsite services available via http://agau.gastro.org/diweb/catalog that can be provided for all providers, coding and billing staff, administrators, and clinical staff. Everyone needs to take an active role.
Ms. Mueller is a health care consultant with more than 35 years of experience in health care, including ICU/CCU nursing, physician office administration, GI claims submission and adjudication, and seminar instruction. She is president and owner of AskMueller Consulting in Lenzburg, Ill., which provides consulting services for physicians nationwide. Ms. Mueller is a nationally known speaker and the author of many multispecialty medical and surgical coding workbooks. She has a great amount of experience in gastroenterology, surgical subspecialties, and pediatric subspecialties. Her presentations have had audiences with the American Gastroenterological Association (AGA), North American Society for Pediatric Gastroenterology and Nutrition (NASPGAN), Society of Gastroenterology Nurses and Associates, Digestive Disease Week, American Pediatric Surgical Associations, and Decision Health and the Coding Institute. Ms. Mueller has written coding columns for ASGE, NASPGHAN, and AGA. She is the coeditor of the ASGE Coding Primer and also answers the coding hotline for the ASGE.
Understanding the business side of medicine helps physicians run a successful practice. However, the business side of medicine is not part of the normal curriculum in training and fellowship programs. Physicians come out of training with the knowledge to treat patients but with little or no knowledge of how to get reimbursed for their services. Gastroenterologists provide both medical and surgical services.
Listed below are some of the basic principles for both documentation and reimbursement policies. All reimbursement is based upon Relative Value Units (RVUs) assigned to every service provided. The services are based upon three factors: physician work value, malpractice cost, and practice expense. Those factors added together and multiplied by a conversion factor assigned by the Centers for Medicare & Medicaid Services (CMS) creates the national physician fee schedule. Each Medicare carrier has localities, and there is another percentage that is multiplied based upon geographic location, which will finalize the approved amount for each service. Your Medicare carrier has the actual approved amounts available on their websites with an effective date of Jan. 1. Commercial payers most commonly base contracts on the Medicare Fee Schedule, but each practice and payer relationship is different. For a better understanding, please contact your practice manager for more specific information based on your payer contracts.
Medical necessity is the key to success. If medical necessity is not demonstrated, payers can deny a claim, deny authorization for a lab test and/or diagnostic study, or recoup previously paid claims. Medicare and commercial payers will often have local coverage determinations (LCDs) for procedures and testing that include indications and restrictions along with approved diagnosis codes. Listed below are the four primary services that GI providers perform and provide interpretation for:
1. Evaluation and management (E&M) services: There are three criteria that have to be met to support any initial visit with patients: the history obtained, the examination performed, and the development of the treatment plan. There are five levels of service for office visits and three levels for inpatient visits, respectively. The levels are chosen based on the decision-making element of the visit, provided the documentation requirements are met for the level chosen. This is often not an easy selection unless the providers are educated on the E&M criteria. Auditors often see that visits are chosen by “guessing” the level, which leads to choosing either a lower or higher level of service than what was actually provided. Some providers have been instructed that E&M services are not that important since procedures are the major source of revenue for the practice. However, GI practices are visit-driven practices, and the initial visits are often worth more RVUs than some procedures. The E&M visit is truly vital and often the backbone for the medical necessity of any additional procedures and diagnostic services required in order for successful treatment of the patient.
2. Endoscopy and procedural billing: Here, medical necessity must be documented in order to submit charges for what was done. Gastroenterologists will often use multiple techniques when treating different areas within the gastrointestinal tract. Documentation has to include the location of lesions/abnormalities, method of treatment/removal, and the reason(s)/indication(s) for those procedures. There may be different instruments used in the colon (for example, snare in the sigmoid colon or biopsy forceps in the transverse colon). These may be separately reported with an appropriate modifier to indicate that these services were performed to different lesions/abnormalities. However, in order to bill for each of the procedures, all of this has to be documented in the endoscopy report. The physician is responsible for accurate and specific documentation and bringing charges back to the billing staff for claim submission. For a successful practice, a team approach is vital. Physicians and coding staff need to have an open line of communication to make sure that everything is submitted appropriately according to payer policies. Billing staff need to communicate any significant changes to the physicians/providers as these changes occur. Ignorance of payer policy is not considered an appropriate excuse when a payer investigates a claim and potential recoupment of moneys paid.
3. Diagnostic studies: Medical necessity/indication for the testing must be documented in order to submit charges for diagnostic studies. The terms “rule out” and “suspect” don’t completely give coders the reason why a physician suspects the patient might have a condition. Usually, abnormal lab tests, signs, and symptoms will often warrant the need for further investigation, and these are the most crucial indications for testing. Not only is this important for diagnostic studies but also for procedures. Make sure that the interpretation of the test results is clear along with a plan/recommendation(s).
4. Diagnosis codes: Assignment of codes per the International Classification of Diseases, 10th revision, Clinical Modification (ICD-10-CM) is the next and most important step after a visit, diagnostic study, and/or procedure. These codes support medical necessity for the services provided, and specificity of the diagnosis code is vital to successful submission and payment of a claim. Signs and symptoms are valid code choices when ruling out a more significant disease/diagnosis because these support medical necessity for a work-up to determine etiology. Comorbidities that impact the provider’s decision making should also be added as additional diagnoses to support the higher level of decision making. Up to 12 diagnosis codes can be assigned to any type of service provided. This also applies to preauthorization of all services, such as lab tests, radiology studies, GI diagnostic studies, and procedures. If specific information is not in the documentation for your staff to access, payers will often deny certain lab and radiology studies, as well as some procedures. There are 71,932 ICD-10-CM codes to choose from, and it is often difficult to find the “specific” code when doing a search in the electronic health record and billing system. Education and training are essential during the orientation sessions prior to active employment, as well as any time the system is upgraded. The providers should be willing to work with the IT representative(s) in the practice to help make the information easier to access. In other words, what “buzz” words would they like included in the description of the ICD-10-CM code in the practice’s list of favorites? For example, Crohn’s disease and ulcerative colitis have over a hundred choices. The choices are based on the location of the disease and whether the disease is without or with complications. If you are going to choose to provide a higher level of E&M service for a patient with Crohn’s disease of the large intestine because of exacerbation of the disease with bleeding, then the appropriate diagnosis code would be one of the following:
- K50.10 Crohn’s disease of large intestine without complications.
- K50.111 Crohn’s disease of large intestine with rectal bleeding.
- K50.112 Crohn’s disease of large intestine with intestinal obstruction.
- K50.113 Crohn’s disease of large intestine with fistula.
- K50.114 Crohn’s disease of large intestine with abscess.
- K50.118 Crohn’s disease of large intestine with other complication.
- K50.119 Crohn’s disease of large intestine with unspecified complications.
Getting paid for your provided services requires attention to detail and communication with your entire staffing team, including all providers. Make sure that your team is educated on all current issues and services pertaining to gastroenterology practices. If there is ever a question when reviewing a procedure note or any service, ask the provider who performed that service. Often, there will have to be legal corrections to the note before services can be billed. Making sure that the claim you are submitting is “clean” is essential for prompt payment. There are multiple resources available through the AGA that will help guide you with coding and billing. There are webinars, training sessions, and onsite services available via http://agau.gastro.org/diweb/catalog that can be provided for all providers, coding and billing staff, administrators, and clinical staff. Everyone needs to take an active role.
Ms. Mueller is a health care consultant with more than 35 years of experience in health care, including ICU/CCU nursing, physician office administration, GI claims submission and adjudication, and seminar instruction. She is president and owner of AskMueller Consulting in Lenzburg, Ill., which provides consulting services for physicians nationwide. Ms. Mueller is a nationally known speaker and the author of many multispecialty medical and surgical coding workbooks. She has a great amount of experience in gastroenterology, surgical subspecialties, and pediatric subspecialties. Her presentations have had audiences with the American Gastroenterological Association (AGA), North American Society for Pediatric Gastroenterology and Nutrition (NASPGAN), Society of Gastroenterology Nurses and Associates, Digestive Disease Week, American Pediatric Surgical Associations, and Decision Health and the Coding Institute. Ms. Mueller has written coding columns for ASGE, NASPGHAN, and AGA. She is the coeditor of the ASGE Coding Primer and also answers the coding hotline for the ASGE.
Understanding the business side of medicine helps physicians run a successful practice. However, the business side of medicine is not part of the normal curriculum in training and fellowship programs. Physicians come out of training with the knowledge to treat patients but with little or no knowledge of how to get reimbursed for their services. Gastroenterologists provide both medical and surgical services.
Listed below are some of the basic principles for both documentation and reimbursement policies. All reimbursement is based upon Relative Value Units (RVUs) assigned to every service provided. The services are based upon three factors: physician work value, malpractice cost, and practice expense. Those factors added together and multiplied by a conversion factor assigned by the Centers for Medicare & Medicaid Services (CMS) creates the national physician fee schedule. Each Medicare carrier has localities, and there is another percentage that is multiplied based upon geographic location, which will finalize the approved amount for each service. Your Medicare carrier has the actual approved amounts available on their websites with an effective date of Jan. 1. Commercial payers most commonly base contracts on the Medicare Fee Schedule, but each practice and payer relationship is different. For a better understanding, please contact your practice manager for more specific information based on your payer contracts.
Medical necessity is the key to success. If medical necessity is not demonstrated, payers can deny a claim, deny authorization for a lab test and/or diagnostic study, or recoup previously paid claims. Medicare and commercial payers will often have local coverage determinations (LCDs) for procedures and testing that include indications and restrictions along with approved diagnosis codes. Listed below are the four primary services that GI providers perform and provide interpretation for:
1. Evaluation and management (E&M) services: There are three criteria that have to be met to support any initial visit with patients: the history obtained, the examination performed, and the development of the treatment plan. There are five levels of service for office visits and three levels for inpatient visits, respectively. The levels are chosen based on the decision-making element of the visit, provided the documentation requirements are met for the level chosen. This is often not an easy selection unless the providers are educated on the E&M criteria. Auditors often see that visits are chosen by “guessing” the level, which leads to choosing either a lower or higher level of service than what was actually provided. Some providers have been instructed that E&M services are not that important since procedures are the major source of revenue for the practice. However, GI practices are visit-driven practices, and the initial visits are often worth more RVUs than some procedures. The E&M visit is truly vital and often the backbone for the medical necessity of any additional procedures and diagnostic services required in order for successful treatment of the patient.
2. Endoscopy and procedural billing: Here, medical necessity must be documented in order to submit charges for what was done. Gastroenterologists will often use multiple techniques when treating different areas within the gastrointestinal tract. Documentation has to include the location of lesions/abnormalities, method of treatment/removal, and the reason(s)/indication(s) for those procedures. There may be different instruments used in the colon (for example, snare in the sigmoid colon or biopsy forceps in the transverse colon). These may be separately reported with an appropriate modifier to indicate that these services were performed to different lesions/abnormalities. However, in order to bill for each of the procedures, all of this has to be documented in the endoscopy report. The physician is responsible for accurate and specific documentation and bringing charges back to the billing staff for claim submission. For a successful practice, a team approach is vital. Physicians and coding staff need to have an open line of communication to make sure that everything is submitted appropriately according to payer policies. Billing staff need to communicate any significant changes to the physicians/providers as these changes occur. Ignorance of payer policy is not considered an appropriate excuse when a payer investigates a claim and potential recoupment of moneys paid.
3. Diagnostic studies: Medical necessity/indication for the testing must be documented in order to submit charges for diagnostic studies. The terms “rule out” and “suspect” don’t completely give coders the reason why a physician suspects the patient might have a condition. Usually, abnormal lab tests, signs, and symptoms will often warrant the need for further investigation, and these are the most crucial indications for testing. Not only is this important for diagnostic studies but also for procedures. Make sure that the interpretation of the test results is clear along with a plan/recommendation(s).
4. Diagnosis codes: Assignment of codes per the International Classification of Diseases, 10th revision, Clinical Modification (ICD-10-CM) is the next and most important step after a visit, diagnostic study, and/or procedure. These codes support medical necessity for the services provided, and specificity of the diagnosis code is vital to successful submission and payment of a claim. Signs and symptoms are valid code choices when ruling out a more significant disease/diagnosis because these support medical necessity for a work-up to determine etiology. Comorbidities that impact the provider’s decision making should also be added as additional diagnoses to support the higher level of decision making. Up to 12 diagnosis codes can be assigned to any type of service provided. This also applies to preauthorization of all services, such as lab tests, radiology studies, GI diagnostic studies, and procedures. If specific information is not in the documentation for your staff to access, payers will often deny certain lab and radiology studies, as well as some procedures. There are 71,932 ICD-10-CM codes to choose from, and it is often difficult to find the “specific” code when doing a search in the electronic health record and billing system. Education and training are essential during the orientation sessions prior to active employment, as well as any time the system is upgraded. The providers should be willing to work with the IT representative(s) in the practice to help make the information easier to access. In other words, what “buzz” words would they like included in the description of the ICD-10-CM code in the practice’s list of favorites? For example, Crohn’s disease and ulcerative colitis have over a hundred choices. The choices are based on the location of the disease and whether the disease is without or with complications. If you are going to choose to provide a higher level of E&M service for a patient with Crohn’s disease of the large intestine because of exacerbation of the disease with bleeding, then the appropriate diagnosis code would be one of the following:
- K50.10 Crohn’s disease of large intestine without complications.
- K50.111 Crohn’s disease of large intestine with rectal bleeding.
- K50.112 Crohn’s disease of large intestine with intestinal obstruction.
- K50.113 Crohn’s disease of large intestine with fistula.
- K50.114 Crohn’s disease of large intestine with abscess.
- K50.118 Crohn’s disease of large intestine with other complication.
- K50.119 Crohn’s disease of large intestine with unspecified complications.
Getting paid for your provided services requires attention to detail and communication with your entire staffing team, including all providers. Make sure that your team is educated on all current issues and services pertaining to gastroenterology practices. If there is ever a question when reviewing a procedure note or any service, ask the provider who performed that service. Often, there will have to be legal corrections to the note before services can be billed. Making sure that the claim you are submitting is “clean” is essential for prompt payment. There are multiple resources available through the AGA that will help guide you with coding and billing. There are webinars, training sessions, and onsite services available via http://agau.gastro.org/diweb/catalog that can be provided for all providers, coding and billing staff, administrators, and clinical staff. Everyone needs to take an active role.
Ms. Mueller is a health care consultant with more than 35 years of experience in health care, including ICU/CCU nursing, physician office administration, GI claims submission and adjudication, and seminar instruction. She is president and owner of AskMueller Consulting in Lenzburg, Ill., which provides consulting services for physicians nationwide. Ms. Mueller is a nationally known speaker and the author of many multispecialty medical and surgical coding workbooks. She has a great amount of experience in gastroenterology, surgical subspecialties, and pediatric subspecialties. Her presentations have had audiences with the American Gastroenterological Association (AGA), North American Society for Pediatric Gastroenterology and Nutrition (NASPGAN), Society of Gastroenterology Nurses and Associates, Digestive Disease Week, American Pediatric Surgical Associations, and Decision Health and the Coding Institute. Ms. Mueller has written coding columns for ASGE, NASPGHAN, and AGA. She is the coeditor of the ASGE Coding Primer and also answers the coding hotline for the ASGE.
Planning for future college expenses with 529 accounts
Financial planning for families can involve multiple investment goals. The big ones usually are investing for retirement and for your children’s college expenses. With any investment strategy, once you have identified an investment goal, you will want to utilize the right investment account to achieve that goal. If investing for future college expenses is your goal, then one of the investment accounts you will want to utilize is called a 529 plan.
What is a 529 plan?
A 529 plan is a tax-favored account authorized by Section 529 of the Internal Revenue Code and sponsored by a state or educational institution. These plans have specific tax-saving features to them, compared with other taxable accounts, which are listed below. To begin with, there are two types of 529 plans: prepaid tuition plans and education savings plans. Every state has at least one type of 529 plan. Additionally, some private colleges sponsor a prepaid tuition plan.
Prepaid tuition plan
The first type of 529 account is a prepaid tuition plan. These let an account owner purchase college credits (or units) for participating colleges or universities at today’s prices to be used for the student’s future tuition charges. The states that sponsor prepaid plans do so primarily for the benefit of their in-state public colleges and universities. Things to know about the prepaid plans: States may or may not guarantee that the prepaid units keep up with increases in tuition charges. The plan also may have a state residency requirement. If the student decides not to attend one of the eligible schools, the equivalent payout may be less than had the student attended one of the participating institutions. There are no federal guarantees on the state prepaid plans and they are not available for private elementary and high school programs.
Education savings plan
The second type of 529 account is an education savings plan, an investment account into which you can invest your after-tax dollars. The intent with these accounts is to grow the balance for use at a future date. These are tax-deferred accounts, which means each year the interest, dividends, and capital gains created within the account do not show up on your tax return. If the funds are used for a “qualified” higher-education expense, then gains on the account are not taxed upon withdrawal.
As with most investments, the longer your money is invested, the more time it has to grow via accumulated interest, dividends, and appreciation. The larger the growth, the larger the tax benefits. This offers a tremendous advantage for a high-income and high-tax bracket household to invest for future goals (such as private school tuition or college expenses). By contrast, if you had invested in a fully taxable account, you would be subject to taxes each year on the interest, dividends, and capital gain distributions. Also, with taxable accounts, your investments would be subject to capital gains tax on the growth when they are sold to pay for those future expenses.
An account owner may choose among a range of investment options that the 529 plan provides. These are typically individual mutual funds or preformed mutual fund portfolios. The portfolios may have a fixed allocation percentage that stays the same over time or come “age-weighted,” meaning the investment allocation becomes more conservative the closer the student gets to college age when withdrawals would occur. This is a similar approach to the “target retirement date” offerings one sees in retirement accounts.
If one is using the 529 account for the student’s elementary or high school years, the investment time frame may be shorter and necessitate a more conservative approach, as the time for withdrawals would be nearer than the college years. As with most investments, the account can lose value based on investment performance.
Owner versus beneficiary
There are two parties to any 529 plan account: The account owner, who has control over the account and can name the beneficiary to the account, and the beneficiary (the student). The account owner can change beneficiaries on the account and can even name themselves as the beneficiary. One can name anyone as the beneficiary (e.g., child, friend, relative, yourself). You can be proactive by creating an account and naming yourself the beneficiary now, before switching to your child in the future. The account owner can live in one state with the beneficiary in another and invest in the 529 from a third state, and the student may eventually go to an educational institution in a fourth state. The 529 education savings account is not limited to any specific college, as a prepaid plan may be.
Withdrawals from 529s
If a 529 account withdrawal is for qualified higher education expenses or tuition for elementary or secondary schools, earnings are not subject to federal income tax or, in many cases, state income tax. Qualified withdrawals need to take place in the same tax year as the qualified expense.
Withdrawals not used for qualified higher education expenses in that year are considered “nonqualified” and would be subject to tax and 10% penalty on the earnings. State and local taxes may apply as well.
You can use the proceeds from the account free of taxes for the following qualified higher-education expenses:
- Tuition and school fees for both full and part time students at an eligible college, university, trade, or vocational institution.
- Room and board if the student is enrolled at more than half-time status. The amount up to the school’s room and board charges are eligible if paid directly to the school or to a landlord if living in nonschool housing. If actual charges to the landlord exceed the schools’ charges, then the amount above the school’s charges would be considered an excess withdrawal.
- Required books, supplies, and equipment for the academic program. Computer and technology equipment, printers, and required software, and such related services as Internet access also are qualified expenses.
- Private elementary or secondary school tuition up to $10,000 annually also is a qualified expense for 529 withdrawals.
Health insurance for the student and transportation-related costs to and from the school are not qualified expenses.
Contributions and fees
Like all investments, the fees associated with a 529 account need to be considered, as excess fees lower the investment returns. Prepaid tuition plans may charge initial application, transaction, and ongoing administrative fees. Investment 529 accounts may also have administrative costs such as program management fees, per-transaction fees, and the underlying investment expense ratios. Some states have broker-sold plans as well as direct-sold plans. Broker-sold plans can be purchased only through a broker and have the additional expenses associated with that either in the form of a load (sales charge) or higher expense ratio.
Contributions to a 529 plan can only be made in cash. If you currently have other investments, they need to be liquidated first (with the associated tax consequence) and then the proceeds invested into the 529 plan. Establishing the account and ongoing contributions are subject to gift tax limits ($15,000 for 2019). A married couple may make a “joint gift” to the account to double the limit. The 529 plans also allow the owner to front-load the account in 1 year with up to 5 years’ worth of gift limit contributions all at once. This lump sum is treated for tax reasons as a pro-rata 5 consecutive years of contributions all at once. Any additional gifts to that beneficiary during that year and the remaining four would be subject to gift tax issues if it means the annual gift limits were exceeded. Contributions are considered a “completed gift” for gift- and estate-tax purposes even though the account owner retains an element of control. The up-front 5-year gift election is available only on 529 accounts and is a great way for parents and grandparents (hint-hint) to reduce their estates and get a significant initial balance into the account. This can come in handy for those who may have procrastinated working toward this investment goal and need to catch up.
If the beneficiary does not need all or some of the funds for qualified higher education expenses, the account owner has options: One can change beneficiary to another relative who may need the funds or keep the account going and eventually add a grandchild as a beneficiary. Graduate school expenses also are eligible. A student can have multiple 529 accounts set up in their name.
Additional tax considerations
Education Tax Credits like the American Opportunity Tax Credit and the Lifetime Learning Credit have income phase-outs that you may or may not be eligible for based on your income. Education expenses used to qualify for the tax-free withdrawal from a 529 plan cannot be used to claim these tax credits. Several states offer state income tax deductions for contributions to a 529 plan but may have eligibility limited to the in-state plan only. It is wise to look to your own state’s plan first to see if that is the case and consider that as a factor when you choose a plan right for you. Refer to your tax professional for your eligibility.
In conclusion, 529 savings plans represent a tax-free way to grow your investments for future education expenses down the road, even if you don’t have a child yet. Speak to your financial adviser to learn about plans and contribution schedules that work with your current and future investing goals.
Good sources for further information include:
- www.savingforcollege.com.
- www.irs.gov/forms-pubs/about-publication-970.
- www.finra.org/investors/saving-college.
Mr. Clancy is director of financial planning, Drexel University College of Medicine.
Financial planning for families can involve multiple investment goals. The big ones usually are investing for retirement and for your children’s college expenses. With any investment strategy, once you have identified an investment goal, you will want to utilize the right investment account to achieve that goal. If investing for future college expenses is your goal, then one of the investment accounts you will want to utilize is called a 529 plan.
What is a 529 plan?
A 529 plan is a tax-favored account authorized by Section 529 of the Internal Revenue Code and sponsored by a state or educational institution. These plans have specific tax-saving features to them, compared with other taxable accounts, which are listed below. To begin with, there are two types of 529 plans: prepaid tuition plans and education savings plans. Every state has at least one type of 529 plan. Additionally, some private colleges sponsor a prepaid tuition plan.
Prepaid tuition plan
The first type of 529 account is a prepaid tuition plan. These let an account owner purchase college credits (or units) for participating colleges or universities at today’s prices to be used for the student’s future tuition charges. The states that sponsor prepaid plans do so primarily for the benefit of their in-state public colleges and universities. Things to know about the prepaid plans: States may or may not guarantee that the prepaid units keep up with increases in tuition charges. The plan also may have a state residency requirement. If the student decides not to attend one of the eligible schools, the equivalent payout may be less than had the student attended one of the participating institutions. There are no federal guarantees on the state prepaid plans and they are not available for private elementary and high school programs.
Education savings plan
The second type of 529 account is an education savings plan, an investment account into which you can invest your after-tax dollars. The intent with these accounts is to grow the balance for use at a future date. These are tax-deferred accounts, which means each year the interest, dividends, and capital gains created within the account do not show up on your tax return. If the funds are used for a “qualified” higher-education expense, then gains on the account are not taxed upon withdrawal.
As with most investments, the longer your money is invested, the more time it has to grow via accumulated interest, dividends, and appreciation. The larger the growth, the larger the tax benefits. This offers a tremendous advantage for a high-income and high-tax bracket household to invest for future goals (such as private school tuition or college expenses). By contrast, if you had invested in a fully taxable account, you would be subject to taxes each year on the interest, dividends, and capital gain distributions. Also, with taxable accounts, your investments would be subject to capital gains tax on the growth when they are sold to pay for those future expenses.
An account owner may choose among a range of investment options that the 529 plan provides. These are typically individual mutual funds or preformed mutual fund portfolios. The portfolios may have a fixed allocation percentage that stays the same over time or come “age-weighted,” meaning the investment allocation becomes more conservative the closer the student gets to college age when withdrawals would occur. This is a similar approach to the “target retirement date” offerings one sees in retirement accounts.
If one is using the 529 account for the student’s elementary or high school years, the investment time frame may be shorter and necessitate a more conservative approach, as the time for withdrawals would be nearer than the college years. As with most investments, the account can lose value based on investment performance.
Owner versus beneficiary
There are two parties to any 529 plan account: The account owner, who has control over the account and can name the beneficiary to the account, and the beneficiary (the student). The account owner can change beneficiaries on the account and can even name themselves as the beneficiary. One can name anyone as the beneficiary (e.g., child, friend, relative, yourself). You can be proactive by creating an account and naming yourself the beneficiary now, before switching to your child in the future. The account owner can live in one state with the beneficiary in another and invest in the 529 from a third state, and the student may eventually go to an educational institution in a fourth state. The 529 education savings account is not limited to any specific college, as a prepaid plan may be.
Withdrawals from 529s
If a 529 account withdrawal is for qualified higher education expenses or tuition for elementary or secondary schools, earnings are not subject to federal income tax or, in many cases, state income tax. Qualified withdrawals need to take place in the same tax year as the qualified expense.
Withdrawals not used for qualified higher education expenses in that year are considered “nonqualified” and would be subject to tax and 10% penalty on the earnings. State and local taxes may apply as well.
You can use the proceeds from the account free of taxes for the following qualified higher-education expenses:
- Tuition and school fees for both full and part time students at an eligible college, university, trade, or vocational institution.
- Room and board if the student is enrolled at more than half-time status. The amount up to the school’s room and board charges are eligible if paid directly to the school or to a landlord if living in nonschool housing. If actual charges to the landlord exceed the schools’ charges, then the amount above the school’s charges would be considered an excess withdrawal.
- Required books, supplies, and equipment for the academic program. Computer and technology equipment, printers, and required software, and such related services as Internet access also are qualified expenses.
- Private elementary or secondary school tuition up to $10,000 annually also is a qualified expense for 529 withdrawals.
Health insurance for the student and transportation-related costs to and from the school are not qualified expenses.
Contributions and fees
Like all investments, the fees associated with a 529 account need to be considered, as excess fees lower the investment returns. Prepaid tuition plans may charge initial application, transaction, and ongoing administrative fees. Investment 529 accounts may also have administrative costs such as program management fees, per-transaction fees, and the underlying investment expense ratios. Some states have broker-sold plans as well as direct-sold plans. Broker-sold plans can be purchased only through a broker and have the additional expenses associated with that either in the form of a load (sales charge) or higher expense ratio.
Contributions to a 529 plan can only be made in cash. If you currently have other investments, they need to be liquidated first (with the associated tax consequence) and then the proceeds invested into the 529 plan. Establishing the account and ongoing contributions are subject to gift tax limits ($15,000 for 2019). A married couple may make a “joint gift” to the account to double the limit. The 529 plans also allow the owner to front-load the account in 1 year with up to 5 years’ worth of gift limit contributions all at once. This lump sum is treated for tax reasons as a pro-rata 5 consecutive years of contributions all at once. Any additional gifts to that beneficiary during that year and the remaining four would be subject to gift tax issues if it means the annual gift limits were exceeded. Contributions are considered a “completed gift” for gift- and estate-tax purposes even though the account owner retains an element of control. The up-front 5-year gift election is available only on 529 accounts and is a great way for parents and grandparents (hint-hint) to reduce their estates and get a significant initial balance into the account. This can come in handy for those who may have procrastinated working toward this investment goal and need to catch up.
If the beneficiary does not need all or some of the funds for qualified higher education expenses, the account owner has options: One can change beneficiary to another relative who may need the funds or keep the account going and eventually add a grandchild as a beneficiary. Graduate school expenses also are eligible. A student can have multiple 529 accounts set up in their name.
Additional tax considerations
Education Tax Credits like the American Opportunity Tax Credit and the Lifetime Learning Credit have income phase-outs that you may or may not be eligible for based on your income. Education expenses used to qualify for the tax-free withdrawal from a 529 plan cannot be used to claim these tax credits. Several states offer state income tax deductions for contributions to a 529 plan but may have eligibility limited to the in-state plan only. It is wise to look to your own state’s plan first to see if that is the case and consider that as a factor when you choose a plan right for you. Refer to your tax professional for your eligibility.
In conclusion, 529 savings plans represent a tax-free way to grow your investments for future education expenses down the road, even if you don’t have a child yet. Speak to your financial adviser to learn about plans and contribution schedules that work with your current and future investing goals.
Good sources for further information include:
- www.savingforcollege.com.
- www.irs.gov/forms-pubs/about-publication-970.
- www.finra.org/investors/saving-college.
Mr. Clancy is director of financial planning, Drexel University College of Medicine.
Financial planning for families can involve multiple investment goals. The big ones usually are investing for retirement and for your children’s college expenses. With any investment strategy, once you have identified an investment goal, you will want to utilize the right investment account to achieve that goal. If investing for future college expenses is your goal, then one of the investment accounts you will want to utilize is called a 529 plan.
What is a 529 plan?
A 529 plan is a tax-favored account authorized by Section 529 of the Internal Revenue Code and sponsored by a state or educational institution. These plans have specific tax-saving features to them, compared with other taxable accounts, which are listed below. To begin with, there are two types of 529 plans: prepaid tuition plans and education savings plans. Every state has at least one type of 529 plan. Additionally, some private colleges sponsor a prepaid tuition plan.
Prepaid tuition plan
The first type of 529 account is a prepaid tuition plan. These let an account owner purchase college credits (or units) for participating colleges or universities at today’s prices to be used for the student’s future tuition charges. The states that sponsor prepaid plans do so primarily for the benefit of their in-state public colleges and universities. Things to know about the prepaid plans: States may or may not guarantee that the prepaid units keep up with increases in tuition charges. The plan also may have a state residency requirement. If the student decides not to attend one of the eligible schools, the equivalent payout may be less than had the student attended one of the participating institutions. There are no federal guarantees on the state prepaid plans and they are not available for private elementary and high school programs.
Education savings plan
The second type of 529 account is an education savings plan, an investment account into which you can invest your after-tax dollars. The intent with these accounts is to grow the balance for use at a future date. These are tax-deferred accounts, which means each year the interest, dividends, and capital gains created within the account do not show up on your tax return. If the funds are used for a “qualified” higher-education expense, then gains on the account are not taxed upon withdrawal.
As with most investments, the longer your money is invested, the more time it has to grow via accumulated interest, dividends, and appreciation. The larger the growth, the larger the tax benefits. This offers a tremendous advantage for a high-income and high-tax bracket household to invest for future goals (such as private school tuition or college expenses). By contrast, if you had invested in a fully taxable account, you would be subject to taxes each year on the interest, dividends, and capital gain distributions. Also, with taxable accounts, your investments would be subject to capital gains tax on the growth when they are sold to pay for those future expenses.
An account owner may choose among a range of investment options that the 529 plan provides. These are typically individual mutual funds or preformed mutual fund portfolios. The portfolios may have a fixed allocation percentage that stays the same over time or come “age-weighted,” meaning the investment allocation becomes more conservative the closer the student gets to college age when withdrawals would occur. This is a similar approach to the “target retirement date” offerings one sees in retirement accounts.
If one is using the 529 account for the student’s elementary or high school years, the investment time frame may be shorter and necessitate a more conservative approach, as the time for withdrawals would be nearer than the college years. As with most investments, the account can lose value based on investment performance.
Owner versus beneficiary
There are two parties to any 529 plan account: The account owner, who has control over the account and can name the beneficiary to the account, and the beneficiary (the student). The account owner can change beneficiaries on the account and can even name themselves as the beneficiary. One can name anyone as the beneficiary (e.g., child, friend, relative, yourself). You can be proactive by creating an account and naming yourself the beneficiary now, before switching to your child in the future. The account owner can live in one state with the beneficiary in another and invest in the 529 from a third state, and the student may eventually go to an educational institution in a fourth state. The 529 education savings account is not limited to any specific college, as a prepaid plan may be.
Withdrawals from 529s
If a 529 account withdrawal is for qualified higher education expenses or tuition for elementary or secondary schools, earnings are not subject to federal income tax or, in many cases, state income tax. Qualified withdrawals need to take place in the same tax year as the qualified expense.
Withdrawals not used for qualified higher education expenses in that year are considered “nonqualified” and would be subject to tax and 10% penalty on the earnings. State and local taxes may apply as well.
You can use the proceeds from the account free of taxes for the following qualified higher-education expenses:
- Tuition and school fees for both full and part time students at an eligible college, university, trade, or vocational institution.
- Room and board if the student is enrolled at more than half-time status. The amount up to the school’s room and board charges are eligible if paid directly to the school or to a landlord if living in nonschool housing. If actual charges to the landlord exceed the schools’ charges, then the amount above the school’s charges would be considered an excess withdrawal.
- Required books, supplies, and equipment for the academic program. Computer and technology equipment, printers, and required software, and such related services as Internet access also are qualified expenses.
- Private elementary or secondary school tuition up to $10,000 annually also is a qualified expense for 529 withdrawals.
Health insurance for the student and transportation-related costs to and from the school are not qualified expenses.
Contributions and fees
Like all investments, the fees associated with a 529 account need to be considered, as excess fees lower the investment returns. Prepaid tuition plans may charge initial application, transaction, and ongoing administrative fees. Investment 529 accounts may also have administrative costs such as program management fees, per-transaction fees, and the underlying investment expense ratios. Some states have broker-sold plans as well as direct-sold plans. Broker-sold plans can be purchased only through a broker and have the additional expenses associated with that either in the form of a load (sales charge) or higher expense ratio.
Contributions to a 529 plan can only be made in cash. If you currently have other investments, they need to be liquidated first (with the associated tax consequence) and then the proceeds invested into the 529 plan. Establishing the account and ongoing contributions are subject to gift tax limits ($15,000 for 2019). A married couple may make a “joint gift” to the account to double the limit. The 529 plans also allow the owner to front-load the account in 1 year with up to 5 years’ worth of gift limit contributions all at once. This lump sum is treated for tax reasons as a pro-rata 5 consecutive years of contributions all at once. Any additional gifts to that beneficiary during that year and the remaining four would be subject to gift tax issues if it means the annual gift limits were exceeded. Contributions are considered a “completed gift” for gift- and estate-tax purposes even though the account owner retains an element of control. The up-front 5-year gift election is available only on 529 accounts and is a great way for parents and grandparents (hint-hint) to reduce their estates and get a significant initial balance into the account. This can come in handy for those who may have procrastinated working toward this investment goal and need to catch up.
If the beneficiary does not need all or some of the funds for qualified higher education expenses, the account owner has options: One can change beneficiary to another relative who may need the funds or keep the account going and eventually add a grandchild as a beneficiary. Graduate school expenses also are eligible. A student can have multiple 529 accounts set up in their name.
Additional tax considerations
Education Tax Credits like the American Opportunity Tax Credit and the Lifetime Learning Credit have income phase-outs that you may or may not be eligible for based on your income. Education expenses used to qualify for the tax-free withdrawal from a 529 plan cannot be used to claim these tax credits. Several states offer state income tax deductions for contributions to a 529 plan but may have eligibility limited to the in-state plan only. It is wise to look to your own state’s plan first to see if that is the case and consider that as a factor when you choose a plan right for you. Refer to your tax professional for your eligibility.
In conclusion, 529 savings plans represent a tax-free way to grow your investments for future education expenses down the road, even if you don’t have a child yet. Speak to your financial adviser to learn about plans and contribution schedules that work with your current and future investing goals.
Good sources for further information include:
- www.savingforcollege.com.
- www.irs.gov/forms-pubs/about-publication-970.
- www.finra.org/investors/saving-college.
Mr. Clancy is director of financial planning, Drexel University College of Medicine.
Don’t let the mortgage preapproval process give you a stomachache
You are trying to buy your first home. Maybe you have heard stories from family, friends, and colleagues about nightmare scenarios when purchasing a home. There are many facets to the home-financing process, and a little bit of planning can reduce a significant amount of time and stress. Where do you begin? What do lenders look for when preapproving a borrower? What steps do I take to get preapproved for a mortgage loan? This article will help guide you through these initial stages to ultimately guide you to settlement on your new home.
Where to begin?
- Start by drafting a budget. How much of a monthly housing payment can you afford? Planning a budget is an extremely valuable exercise at any point in life, not just when buying a home. Often, borrowers will ask the question “How much can I afford?” The better question to ask is “Can I qualify for a home that meets the maximum monthly payment I have budgeted for?”
- What funds would I use for purchasing a home? Down payments and closing costs can add up quickly. Do you have funds readily available in an account you hold? Will you be obtaining a gift from a family member? Generally, funds for down payment are not allowed to be borrowed, unless the money is coming from an account secured by your own assets (for instance, borrowing from your own retirement account). Don’t think you necessarily need to put 20% down. Some loan programs offer little or no down payment options, while other programs may offer down payment assistance options.
- If you are not aware of your credit standing, run a free credit report to verify accurate information. Federal law allows consumers to access one free credit report annually with each of the three credit bureaus (Equifax, Experian, TransUnion). Knowing your credit history and data on your credit report is very important. If there are known or unknown issues on your credit report, it’s always best to at least be informed. You can access your free report at www.annualcreditreport.com.
- Start planning ahead with some of the documentation you will need for a loan approval. Lenders will request items such as tax returns and W-2s from the past 2 years, your recent pay stubs covering a 30-day period, most recent 2 months asset account statements (bank accounts, investment accounts, retirement accounts, etc.), as well as other documentation, depending on your specific scenario.
What are lenders looking at when preapproving an applicant?
Many people will often start to search for homes without having prepared for the preapproval process. This is not necessarily an issue and it doesn’t mean you will not be preapproved. Planning ahead could help you avoid any unforeseen problems and avoid rushing into the mortgage application process when trying to place an offer on a home.
In addition to supplying information on residence and employment/student history for the past 2 years, there are three primary components to a borrower’s credit portfolio:
1) Debt-to-income ratio: What monthly expenses will show on your credit report (car loans/leases, student loans, credit card payments, personal loans/lines of credit, and mortgages for other properties owned)? Do you own any other real estate? Do you have other required obligations, such as alimony or child support payments? To calculate, first combine these liabilities on a monthly expense basis along with the new proposed monthly housing payment. Take these monthly liabilities and divide by monthly income. Gross income (pretax) for employees of a company they do not own is typically utilized (bonus or commission income can have some alternate rules to be allowed as qualifying income); for self-employed borrowers, tax returns will be required to be reviewed; tax write offs could reduce qualifying income. Self-employed individuals will typically need to show a 2-year income history via personal tax returns (as well as business tax returns if applicable). See Figure 1 for an example of a debt-to-income ratio calculation. Many loan programs will require a debt-to-income ratio of 45% or less. There are various loan programs that will be more or less restrictive than this percentage. A lender will be able to guide you to the proper program for your scenario.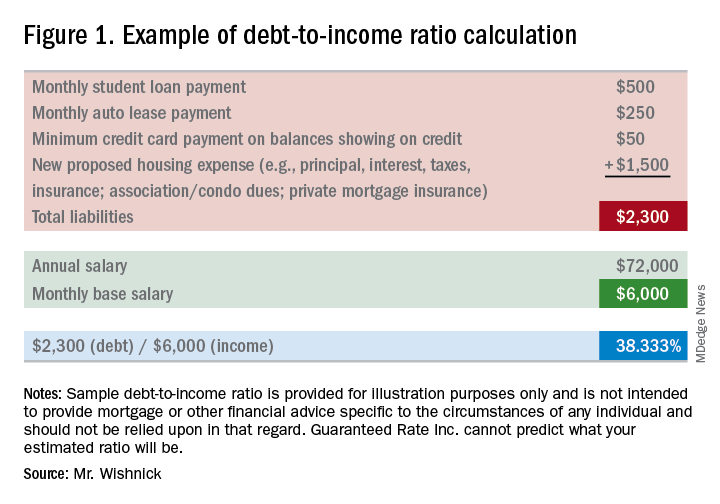
2) Liquid assets: Lenders will review the amount of liquid funds you have available for down payment, closing costs, and any necessary reserves. These may include, but are not limited to, checking/savings/money market accounts, investment accounts (stocks, bonds, mutual funds), and retirement funds. Are there enough allowable funds available for the down payment and closing costs, as well as any required reserves needed for qualification? Large non–payroll deposits can be required to be sourced to make sure the funds are from an allowable source.
3) Credit history/scores: Buying a home will be one of the largest purchases you will make in a lifetime. Credit scores have a major impact on the cost of credit (the interest rate you will obtain). Having higher scores could result in a lower interest rate, as well as open up certain loan programs that may be more advantageous for you. Oftentimes, lenders will take the middle of the three scores as your mortgage score (one score from each of the three credit bureaus). In most cases, if applying jointly, the lowest of the middle scores for all borrowers is the score that is used as the score for the applicants. In general, a 740 middle credit score is considered to be excellent for mortgage financing but is not a requirement for all programs.
**You may have heard about specific mortgage programs for physicians. These programs are intended for use for lesser down payments, and/or not calculating student loan payments when qualifying for home financing. As future income potential is typically not considered when determining debt-to-income ratios, not counting these liabilities potentially increases borrowing power.
You are now ready to be preapproved for mortgage financing. What should you do next?
- Talk to a trusted lender. Ask your real estate agent, family, friends, or colleagues for local lender recommendations. Real estate agents will want to make sure you have spoken with a lender and completed a preapproval application to ensure that you can be preapproved for financing before showing you homes. If you need a loan to purchase a home, a preapproval letter will be required to submit with an offer letter. The application contains questions such as your address and employment history for the past 2 years, income and asset information, as well as a series of other financial information. A hard credit inquiry will need to be performed in order for the lender to issue a preapproval. What should you expect from a lender in addition to competitive rates and an array of programs? Some people prefer more of a hands-on approach. Working with a lender who provides regular status updates and makes him/herself easily accessible for all of your questions can certainly be an attractive feature. Working with a local lender also may be reassuring, as he or she should have plenty of experience with the market in which you are purchasing.
- Search for homes. Upon being given the green light for your preapproval and a price range within your comfort zone, connect with your local real estate professional to search for homes. Plan to spend time with your agent discussing all your needs for your new home.
- Submit an offer. Your lender will be able to provide an estimate of closing costs and monthly payments for homes that you are considering buying before you make an offer. You will want to be sure you are comfortable with the financial obligation prior to making your offer. With your offer, an initial good faith deposit (earnest money deposit) will be required. Your real estate agent will guide you on the proper amount of the deposit.
Conclusion
Once you and the seller have come to terms, you will look to discuss with your lender the rate and program options to secure (locking in an interest rate and program), as well as to complete the formal mortgage application. The lender will request additional documentation, if you have not already provided documents, in order for you to obtain a conditional mortgage commitment. The lender also will order an appraisal to ensure the property value supports the price you have agreed to pay for it. Your real estate agent will guide you through the various deadlines and requirements in the contract for items like home inspections, ordering a title search to obtain title insurance, and other nonfinancing contingencies. Some areas may require attorneys for contract review and closing, which your agent will discuss with you. As you can see, buying a home is not an instant process. Taking the appropriate steps to prepare for your mortgage preapproval could save you a lot of time and stress.
Mr. Wishnick is a 15-year mortgage industry veteran, vice president of mortgage lending with Guaranteed Rate (NMLS #2611) and was ranked as a Top 1% mortgage originator by Mortgage Executive Magazine. He can be reached at rob.wishnick@rate.com.
All information provided in this publication is for informational and educational purposes only, and in no way is any of the content contained herein to be construed as financial, investment, or legal advice or instruction. Guaranteed Rate does not guarantee the quality, accuracy, completeness or timelines of the information in this publication.
You are trying to buy your first home. Maybe you have heard stories from family, friends, and colleagues about nightmare scenarios when purchasing a home. There are many facets to the home-financing process, and a little bit of planning can reduce a significant amount of time and stress. Where do you begin? What do lenders look for when preapproving a borrower? What steps do I take to get preapproved for a mortgage loan? This article will help guide you through these initial stages to ultimately guide you to settlement on your new home.
Where to begin?
- Start by drafting a budget. How much of a monthly housing payment can you afford? Planning a budget is an extremely valuable exercise at any point in life, not just when buying a home. Often, borrowers will ask the question “How much can I afford?” The better question to ask is “Can I qualify for a home that meets the maximum monthly payment I have budgeted for?”
- What funds would I use for purchasing a home? Down payments and closing costs can add up quickly. Do you have funds readily available in an account you hold? Will you be obtaining a gift from a family member? Generally, funds for down payment are not allowed to be borrowed, unless the money is coming from an account secured by your own assets (for instance, borrowing from your own retirement account). Don’t think you necessarily need to put 20% down. Some loan programs offer little or no down payment options, while other programs may offer down payment assistance options.
- If you are not aware of your credit standing, run a free credit report to verify accurate information. Federal law allows consumers to access one free credit report annually with each of the three credit bureaus (Equifax, Experian, TransUnion). Knowing your credit history and data on your credit report is very important. If there are known or unknown issues on your credit report, it’s always best to at least be informed. You can access your free report at www.annualcreditreport.com.
- Start planning ahead with some of the documentation you will need for a loan approval. Lenders will request items such as tax returns and W-2s from the past 2 years, your recent pay stubs covering a 30-day period, most recent 2 months asset account statements (bank accounts, investment accounts, retirement accounts, etc.), as well as other documentation, depending on your specific scenario.
What are lenders looking at when preapproving an applicant?
Many people will often start to search for homes without having prepared for the preapproval process. This is not necessarily an issue and it doesn’t mean you will not be preapproved. Planning ahead could help you avoid any unforeseen problems and avoid rushing into the mortgage application process when trying to place an offer on a home.
In addition to supplying information on residence and employment/student history for the past 2 years, there are three primary components to a borrower’s credit portfolio:
1) Debt-to-income ratio: What monthly expenses will show on your credit report (car loans/leases, student loans, credit card payments, personal loans/lines of credit, and mortgages for other properties owned)? Do you own any other real estate? Do you have other required obligations, such as alimony or child support payments? To calculate, first combine these liabilities on a monthly expense basis along with the new proposed monthly housing payment. Take these monthly liabilities and divide by monthly income. Gross income (pretax) for employees of a company they do not own is typically utilized (bonus or commission income can have some alternate rules to be allowed as qualifying income); for self-employed borrowers, tax returns will be required to be reviewed; tax write offs could reduce qualifying income. Self-employed individuals will typically need to show a 2-year income history via personal tax returns (as well as business tax returns if applicable). See Figure 1 for an example of a debt-to-income ratio calculation. Many loan programs will require a debt-to-income ratio of 45% or less. There are various loan programs that will be more or less restrictive than this percentage. A lender will be able to guide you to the proper program for your scenario.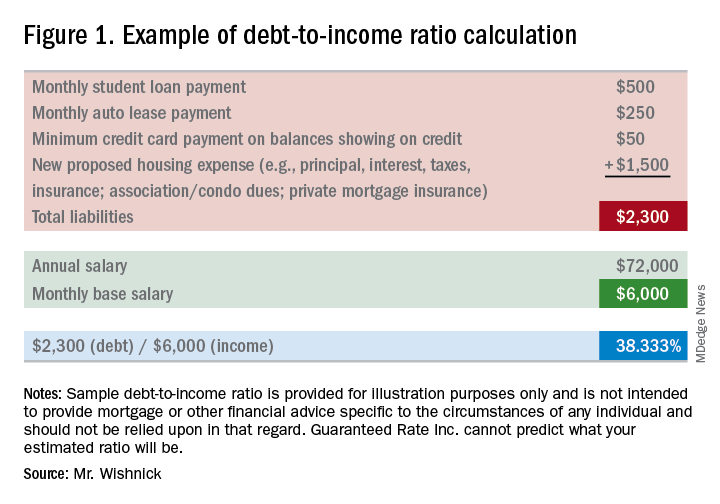
2) Liquid assets: Lenders will review the amount of liquid funds you have available for down payment, closing costs, and any necessary reserves. These may include, but are not limited to, checking/savings/money market accounts, investment accounts (stocks, bonds, mutual funds), and retirement funds. Are there enough allowable funds available for the down payment and closing costs, as well as any required reserves needed for qualification? Large non–payroll deposits can be required to be sourced to make sure the funds are from an allowable source.
3) Credit history/scores: Buying a home will be one of the largest purchases you will make in a lifetime. Credit scores have a major impact on the cost of credit (the interest rate you will obtain). Having higher scores could result in a lower interest rate, as well as open up certain loan programs that may be more advantageous for you. Oftentimes, lenders will take the middle of the three scores as your mortgage score (one score from each of the three credit bureaus). In most cases, if applying jointly, the lowest of the middle scores for all borrowers is the score that is used as the score for the applicants. In general, a 740 middle credit score is considered to be excellent for mortgage financing but is not a requirement for all programs.
**You may have heard about specific mortgage programs for physicians. These programs are intended for use for lesser down payments, and/or not calculating student loan payments when qualifying for home financing. As future income potential is typically not considered when determining debt-to-income ratios, not counting these liabilities potentially increases borrowing power.
You are now ready to be preapproved for mortgage financing. What should you do next?
- Talk to a trusted lender. Ask your real estate agent, family, friends, or colleagues for local lender recommendations. Real estate agents will want to make sure you have spoken with a lender and completed a preapproval application to ensure that you can be preapproved for financing before showing you homes. If you need a loan to purchase a home, a preapproval letter will be required to submit with an offer letter. The application contains questions such as your address and employment history for the past 2 years, income and asset information, as well as a series of other financial information. A hard credit inquiry will need to be performed in order for the lender to issue a preapproval. What should you expect from a lender in addition to competitive rates and an array of programs? Some people prefer more of a hands-on approach. Working with a lender who provides regular status updates and makes him/herself easily accessible for all of your questions can certainly be an attractive feature. Working with a local lender also may be reassuring, as he or she should have plenty of experience with the market in which you are purchasing.
- Search for homes. Upon being given the green light for your preapproval and a price range within your comfort zone, connect with your local real estate professional to search for homes. Plan to spend time with your agent discussing all your needs for your new home.
- Submit an offer. Your lender will be able to provide an estimate of closing costs and monthly payments for homes that you are considering buying before you make an offer. You will want to be sure you are comfortable with the financial obligation prior to making your offer. With your offer, an initial good faith deposit (earnest money deposit) will be required. Your real estate agent will guide you on the proper amount of the deposit.
Conclusion
Once you and the seller have come to terms, you will look to discuss with your lender the rate and program options to secure (locking in an interest rate and program), as well as to complete the formal mortgage application. The lender will request additional documentation, if you have not already provided documents, in order for you to obtain a conditional mortgage commitment. The lender also will order an appraisal to ensure the property value supports the price you have agreed to pay for it. Your real estate agent will guide you through the various deadlines and requirements in the contract for items like home inspections, ordering a title search to obtain title insurance, and other nonfinancing contingencies. Some areas may require attorneys for contract review and closing, which your agent will discuss with you. As you can see, buying a home is not an instant process. Taking the appropriate steps to prepare for your mortgage preapproval could save you a lot of time and stress.
Mr. Wishnick is a 15-year mortgage industry veteran, vice president of mortgage lending with Guaranteed Rate (NMLS #2611) and was ranked as a Top 1% mortgage originator by Mortgage Executive Magazine. He can be reached at rob.wishnick@rate.com.
All information provided in this publication is for informational and educational purposes only, and in no way is any of the content contained herein to be construed as financial, investment, or legal advice or instruction. Guaranteed Rate does not guarantee the quality, accuracy, completeness or timelines of the information in this publication.
You are trying to buy your first home. Maybe you have heard stories from family, friends, and colleagues about nightmare scenarios when purchasing a home. There are many facets to the home-financing process, and a little bit of planning can reduce a significant amount of time and stress. Where do you begin? What do lenders look for when preapproving a borrower? What steps do I take to get preapproved for a mortgage loan? This article will help guide you through these initial stages to ultimately guide you to settlement on your new home.
Where to begin?
- Start by drafting a budget. How much of a monthly housing payment can you afford? Planning a budget is an extremely valuable exercise at any point in life, not just when buying a home. Often, borrowers will ask the question “How much can I afford?” The better question to ask is “Can I qualify for a home that meets the maximum monthly payment I have budgeted for?”
- What funds would I use for purchasing a home? Down payments and closing costs can add up quickly. Do you have funds readily available in an account you hold? Will you be obtaining a gift from a family member? Generally, funds for down payment are not allowed to be borrowed, unless the money is coming from an account secured by your own assets (for instance, borrowing from your own retirement account). Don’t think you necessarily need to put 20% down. Some loan programs offer little or no down payment options, while other programs may offer down payment assistance options.
- If you are not aware of your credit standing, run a free credit report to verify accurate information. Federal law allows consumers to access one free credit report annually with each of the three credit bureaus (Equifax, Experian, TransUnion). Knowing your credit history and data on your credit report is very important. If there are known or unknown issues on your credit report, it’s always best to at least be informed. You can access your free report at www.annualcreditreport.com.
- Start planning ahead with some of the documentation you will need for a loan approval. Lenders will request items such as tax returns and W-2s from the past 2 years, your recent pay stubs covering a 30-day period, most recent 2 months asset account statements (bank accounts, investment accounts, retirement accounts, etc.), as well as other documentation, depending on your specific scenario.
What are lenders looking at when preapproving an applicant?
Many people will often start to search for homes without having prepared for the preapproval process. This is not necessarily an issue and it doesn’t mean you will not be preapproved. Planning ahead could help you avoid any unforeseen problems and avoid rushing into the mortgage application process when trying to place an offer on a home.
In addition to supplying information on residence and employment/student history for the past 2 years, there are three primary components to a borrower’s credit portfolio:
1) Debt-to-income ratio: What monthly expenses will show on your credit report (car loans/leases, student loans, credit card payments, personal loans/lines of credit, and mortgages for other properties owned)? Do you own any other real estate? Do you have other required obligations, such as alimony or child support payments? To calculate, first combine these liabilities on a monthly expense basis along with the new proposed monthly housing payment. Take these monthly liabilities and divide by monthly income. Gross income (pretax) for employees of a company they do not own is typically utilized (bonus or commission income can have some alternate rules to be allowed as qualifying income); for self-employed borrowers, tax returns will be required to be reviewed; tax write offs could reduce qualifying income. Self-employed individuals will typically need to show a 2-year income history via personal tax returns (as well as business tax returns if applicable). See Figure 1 for an example of a debt-to-income ratio calculation. Many loan programs will require a debt-to-income ratio of 45% or less. There are various loan programs that will be more or less restrictive than this percentage. A lender will be able to guide you to the proper program for your scenario.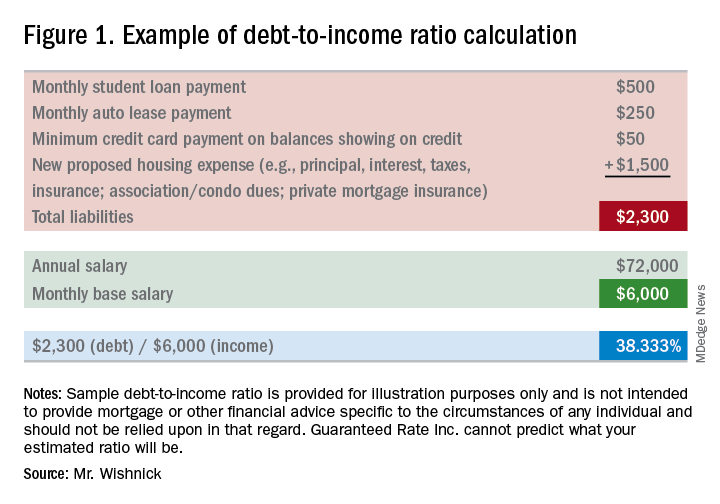
2) Liquid assets: Lenders will review the amount of liquid funds you have available for down payment, closing costs, and any necessary reserves. These may include, but are not limited to, checking/savings/money market accounts, investment accounts (stocks, bonds, mutual funds), and retirement funds. Are there enough allowable funds available for the down payment and closing costs, as well as any required reserves needed for qualification? Large non–payroll deposits can be required to be sourced to make sure the funds are from an allowable source.
3) Credit history/scores: Buying a home will be one of the largest purchases you will make in a lifetime. Credit scores have a major impact on the cost of credit (the interest rate you will obtain). Having higher scores could result in a lower interest rate, as well as open up certain loan programs that may be more advantageous for you. Oftentimes, lenders will take the middle of the three scores as your mortgage score (one score from each of the three credit bureaus). In most cases, if applying jointly, the lowest of the middle scores for all borrowers is the score that is used as the score for the applicants. In general, a 740 middle credit score is considered to be excellent for mortgage financing but is not a requirement for all programs.
**You may have heard about specific mortgage programs for physicians. These programs are intended for use for lesser down payments, and/or not calculating student loan payments when qualifying for home financing. As future income potential is typically not considered when determining debt-to-income ratios, not counting these liabilities potentially increases borrowing power.
You are now ready to be preapproved for mortgage financing. What should you do next?
- Talk to a trusted lender. Ask your real estate agent, family, friends, or colleagues for local lender recommendations. Real estate agents will want to make sure you have spoken with a lender and completed a preapproval application to ensure that you can be preapproved for financing before showing you homes. If you need a loan to purchase a home, a preapproval letter will be required to submit with an offer letter. The application contains questions such as your address and employment history for the past 2 years, income and asset information, as well as a series of other financial information. A hard credit inquiry will need to be performed in order for the lender to issue a preapproval. What should you expect from a lender in addition to competitive rates and an array of programs? Some people prefer more of a hands-on approach. Working with a lender who provides regular status updates and makes him/herself easily accessible for all of your questions can certainly be an attractive feature. Working with a local lender also may be reassuring, as he or she should have plenty of experience with the market in which you are purchasing.
- Search for homes. Upon being given the green light for your preapproval and a price range within your comfort zone, connect with your local real estate professional to search for homes. Plan to spend time with your agent discussing all your needs for your new home.
- Submit an offer. Your lender will be able to provide an estimate of closing costs and monthly payments for homes that you are considering buying before you make an offer. You will want to be sure you are comfortable with the financial obligation prior to making your offer. With your offer, an initial good faith deposit (earnest money deposit) will be required. Your real estate agent will guide you on the proper amount of the deposit.
Conclusion
Once you and the seller have come to terms, you will look to discuss with your lender the rate and program options to secure (locking in an interest rate and program), as well as to complete the formal mortgage application. The lender will request additional documentation, if you have not already provided documents, in order for you to obtain a conditional mortgage commitment. The lender also will order an appraisal to ensure the property value supports the price you have agreed to pay for it. Your real estate agent will guide you through the various deadlines and requirements in the contract for items like home inspections, ordering a title search to obtain title insurance, and other nonfinancing contingencies. Some areas may require attorneys for contract review and closing, which your agent will discuss with you. As you can see, buying a home is not an instant process. Taking the appropriate steps to prepare for your mortgage preapproval could save you a lot of time and stress.
Mr. Wishnick is a 15-year mortgage industry veteran, vice president of mortgage lending with Guaranteed Rate (NMLS #2611) and was ranked as a Top 1% mortgage originator by Mortgage Executive Magazine. He can be reached at rob.wishnick@rate.com.
All information provided in this publication is for informational and educational purposes only, and in no way is any of the content contained herein to be construed as financial, investment, or legal advice or instruction. Guaranteed Rate does not guarantee the quality, accuracy, completeness or timelines of the information in this publication.
Foundations for financial security: Get out of student debt and on the fast track to financial prosperity
Approaching the concept of retirement savings is particularly unique for medical professionals: Balancing a tremendously demanding career with family life and personal time allows few to have the luxury of extra time to address financial planning. Many in the field have higher priorities than saving for retirement on their minds, which compounds the issue.
According to the Association of American Medical Colleges, 76% of medical students will have student debt by the time they graduate. Among those students, the average debt is a staggering $190,000. The average American couple has only about $163,000 in savings by the time they are about 60 years old, so coming out of school, the average doctor will have more in debt than most have saved in their lifetimes. This means that many doctors can’t really start saving significantly until the latter half of their careers. With that in mind, consider these tips to help you on your journey to financial security.
Pay off debt or start saving for retirement?
When it comes to the decision of investing toward retirement or paying off debt more aggressively, there is really only one question that needs to be answered: “Can I make more investing than the loan is costing me?” Given the fact that Direct Graduate Plus Loans are now sitting at about 7% interest rates, an investment would have to make more than 7% per year to make sense. While we can look back at the historical performance of the stock market over time, it is pretty safe to say that in this scenario paying off the student loans as aggressively as possible is the best choice. The reason being is that the loans have a guaranteed cost of 7% per year in accrued interest, whereas an investment is never fully guaranteed to grow.
Make no mistake: High-interest debt is a financial dead weight; the longer it sits, the more it will attempt to sink you financially. A general rule of thumb is that the higher the interest rate on the loan, the more aggressively it should be paid off. Once the high interest loans are taken care of, saving for retirement can reenter the equation.
The company match
That being said, there is one caveat to this rule that you should strongly consider if the opportunity exists: the 401(k) or 403(b) company match. If you work in a position that offers a match on retirement plan contributions, taking advantage of this could substantially benefit you. In a typical safe harbor retirement plan, you will see something like a 3.5% company match for a 6% salary contribution. While there is no one formula that applies to every situation, an opportunity such as this shouldn’t be passed up.
Saving for retirement can be difficult enough. Why not take advantage of a situation in which you are getting free money? You should think about contributing enough to get the maximum match and putting the rest toward student debt. If you are unsure about your particular course of action, I’d suggest speaking to your financial professional to assist in coming up with a suitable game plan.
Roth deferral option
While many folks understand the general ins and outs of how retirement plans work, they fail to realize that there are actually two different types of contributions that can be made in most 401(k)s and 403(b)s: traditional deferrals and Roth deferrals. A traditional deferral is the standard pretax contribution option that lets you skip paying taxes now. Instead, you get taxed at your normal income tax bracket when the money is withdrawn in retirement. This is the option that most people use.
Roth deferrals are posttax contributions. Every dollar contributed gets taxed as ordinary income. Why would one do this, you ask? While there are a variety of different benefits, the primary advantage is that you never have to pay taxes on this money again. To reiterate, you pay taxes on this money now and never have to pay any taxes on it again. This can be extraordinarily helpful in retirement because it gives you the flexibility to choose between taxable and tax-free income.
While you can contribute to personal Roth IRAs to the tune of $5,500 a year if you are under 50 years old and $6,500 if you are 50 years and older, high income earners can be hampered by income limits. For instance, if you make over $135,000 a year as a single person or over $199,000 as a married couple, you are ineligible to make Roth IRA contributions. However, a benefit to Roth contributions in your company 401(k) or 403(b) plan is that these income limits don’t apply. Regardless of your level of income, you can make Roth deferrals in company sponsored retirement plans that allow them.
This strategy is best fit for, but not limited to, those who are earlier on in their careers and can reasonably expect to make much more in the future than they do now. Younger investors have the benefit of time: The more time an investment has to grow, the more it should be worth later on. Also, younger professionals are probably going to be paying the least amount of taxes early in their careers. While not all retirement plans allow for Roth deferrals, if the option is available, why not get taxes out of the way while it’s still relatively cheaper to do so?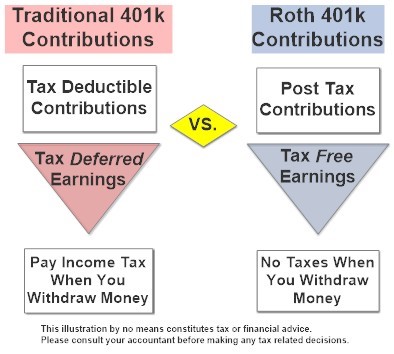
More aggressive strategies for those who need to “catch up” on retirement savings
Because many in the medical field have burdensome student loans, saving for retirement is often something that is pushed off by necessity. That being said, there are different ways to start saving more aggressively the closer you get toward retirement.
Catch up contributions. 401(k)s, 403(b)s, and IRAs all have built in “catch up” contributions that allow those aged 50 or older to save more. For instance, up to age 49 years, the maximum annual contribution in a 401(k) or 403(b) is $18,500 for 2018. At age 50 years, you are allowed to add an additional $6000 “catch up” contribution for a total of $24,500 per year. Likewise, IRAs allow for an additional $1000 per year contribution at age 50 years for a $6500 total yearly contribution.
Spousal IRAs. If you have a nonworking spouse, you may be able to contribute to an IRA on his or her behalf. To be eligible for a spousal IRA contribution, you must be married, file a joint income tax return, and have an earned income of at least what is being contributed to the IRAs. This would allow an additional $5,500 to $6,500 in retirement savings per year depending on your spouse’s age.
Simplified Employee Pension IRAs. For those who are self-employed, it could be worthwhile to look into opening up a Simplified Employee Pension (SEP) IRA. These types of retirement plans are similar to traditional IRAs except that they can only be opened up by an employer. The benefit of a SEP IRA is that it allows for a maximum pretax contribution of up to $54,000 or 25% of your total income, whichever is less.
Cash balance plans. For very-high-earning business owners or sole proprietors, saving $24,500 a year pretax in a 401(k) isn’t necessarily going to move the needle all that much. However, there is a plan available that may help tremendously. The cash balance plan is a little known hybrid retirement plan that allows high-earning practices and business owners to put away a serious amount of money in a short amount of time. For instance, an optimally set up cash balance plan would allow a 59 year old to save up to $278,000 in qualified pretax dollars in a single year. Undoubtedly, such plans are one of the most effective and efficient ways to save money for retirement for those who qualify.
Check out the maximum contributions limits of some retirement strategies below based on your age group.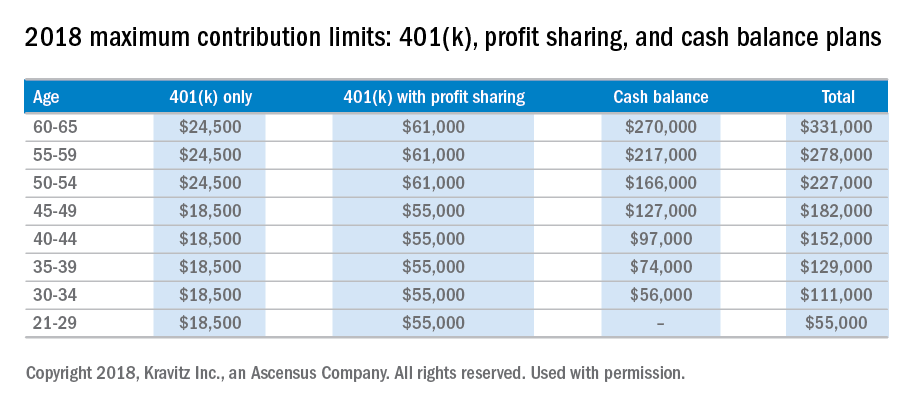
It’s important to realize that it is time that makes money, not timing. Establishing a smart investment plan early in your career will pay huge dividends and save mountains of heartache in your future. If you are unsure about which retirement plan works best for you, I’d recommend speaking to a qualified financial professional to assist you in the process. When it comes to planning for retirement, sooner is always better than later. The financial sacrifices of starting early are never as great as most young professionals fear.
Disclaimer:
This material has been prepared for educational purposes only and is not intended to provide, and should not be relied on for tax, legal, accounting advice, or financial advice. You should consult your own tax, legal, accounting, and financial advisors before engaging in any transaction. Securities offered through Capitol Securities Management Member FINRA, SIPC
Mr. Bellamah is a registered investment advisor with BNB Wealth Management http://www.bnbinc.com/.
Approaching the concept of retirement savings is particularly unique for medical professionals: Balancing a tremendously demanding career with family life and personal time allows few to have the luxury of extra time to address financial planning. Many in the field have higher priorities than saving for retirement on their minds, which compounds the issue.
According to the Association of American Medical Colleges, 76% of medical students will have student debt by the time they graduate. Among those students, the average debt is a staggering $190,000. The average American couple has only about $163,000 in savings by the time they are about 60 years old, so coming out of school, the average doctor will have more in debt than most have saved in their lifetimes. This means that many doctors can’t really start saving significantly until the latter half of their careers. With that in mind, consider these tips to help you on your journey to financial security.
Pay off debt or start saving for retirement?
When it comes to the decision of investing toward retirement or paying off debt more aggressively, there is really only one question that needs to be answered: “Can I make more investing than the loan is costing me?” Given the fact that Direct Graduate Plus Loans are now sitting at about 7% interest rates, an investment would have to make more than 7% per year to make sense. While we can look back at the historical performance of the stock market over time, it is pretty safe to say that in this scenario paying off the student loans as aggressively as possible is the best choice. The reason being is that the loans have a guaranteed cost of 7% per year in accrued interest, whereas an investment is never fully guaranteed to grow.
Make no mistake: High-interest debt is a financial dead weight; the longer it sits, the more it will attempt to sink you financially. A general rule of thumb is that the higher the interest rate on the loan, the more aggressively it should be paid off. Once the high interest loans are taken care of, saving for retirement can reenter the equation.
The company match
That being said, there is one caveat to this rule that you should strongly consider if the opportunity exists: the 401(k) or 403(b) company match. If you work in a position that offers a match on retirement plan contributions, taking advantage of this could substantially benefit you. In a typical safe harbor retirement plan, you will see something like a 3.5% company match for a 6% salary contribution. While there is no one formula that applies to every situation, an opportunity such as this shouldn’t be passed up.
Saving for retirement can be difficult enough. Why not take advantage of a situation in which you are getting free money? You should think about contributing enough to get the maximum match and putting the rest toward student debt. If you are unsure about your particular course of action, I’d suggest speaking to your financial professional to assist in coming up with a suitable game plan.
Roth deferral option
While many folks understand the general ins and outs of how retirement plans work, they fail to realize that there are actually two different types of contributions that can be made in most 401(k)s and 403(b)s: traditional deferrals and Roth deferrals. A traditional deferral is the standard pretax contribution option that lets you skip paying taxes now. Instead, you get taxed at your normal income tax bracket when the money is withdrawn in retirement. This is the option that most people use.
Roth deferrals are posttax contributions. Every dollar contributed gets taxed as ordinary income. Why would one do this, you ask? While there are a variety of different benefits, the primary advantage is that you never have to pay taxes on this money again. To reiterate, you pay taxes on this money now and never have to pay any taxes on it again. This can be extraordinarily helpful in retirement because it gives you the flexibility to choose between taxable and tax-free income.
While you can contribute to personal Roth IRAs to the tune of $5,500 a year if you are under 50 years old and $6,500 if you are 50 years and older, high income earners can be hampered by income limits. For instance, if you make over $135,000 a year as a single person or over $199,000 as a married couple, you are ineligible to make Roth IRA contributions. However, a benefit to Roth contributions in your company 401(k) or 403(b) plan is that these income limits don’t apply. Regardless of your level of income, you can make Roth deferrals in company sponsored retirement plans that allow them.
This strategy is best fit for, but not limited to, those who are earlier on in their careers and can reasonably expect to make much more in the future than they do now. Younger investors have the benefit of time: The more time an investment has to grow, the more it should be worth later on. Also, younger professionals are probably going to be paying the least amount of taxes early in their careers. While not all retirement plans allow for Roth deferrals, if the option is available, why not get taxes out of the way while it’s still relatively cheaper to do so?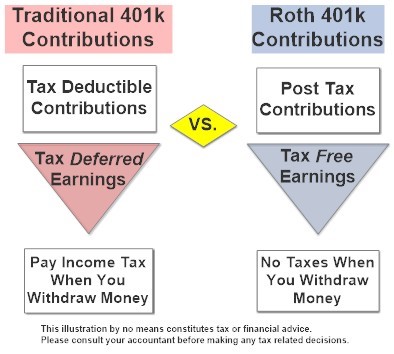
More aggressive strategies for those who need to “catch up” on retirement savings
Because many in the medical field have burdensome student loans, saving for retirement is often something that is pushed off by necessity. That being said, there are different ways to start saving more aggressively the closer you get toward retirement.
Catch up contributions. 401(k)s, 403(b)s, and IRAs all have built in “catch up” contributions that allow those aged 50 or older to save more. For instance, up to age 49 years, the maximum annual contribution in a 401(k) or 403(b) is $18,500 for 2018. At age 50 years, you are allowed to add an additional $6000 “catch up” contribution for a total of $24,500 per year. Likewise, IRAs allow for an additional $1000 per year contribution at age 50 years for a $6500 total yearly contribution.
Spousal IRAs. If you have a nonworking spouse, you may be able to contribute to an IRA on his or her behalf. To be eligible for a spousal IRA contribution, you must be married, file a joint income tax return, and have an earned income of at least what is being contributed to the IRAs. This would allow an additional $5,500 to $6,500 in retirement savings per year depending on your spouse’s age.
Simplified Employee Pension IRAs. For those who are self-employed, it could be worthwhile to look into opening up a Simplified Employee Pension (SEP) IRA. These types of retirement plans are similar to traditional IRAs except that they can only be opened up by an employer. The benefit of a SEP IRA is that it allows for a maximum pretax contribution of up to $54,000 or 25% of your total income, whichever is less.
Cash balance plans. For very-high-earning business owners or sole proprietors, saving $24,500 a year pretax in a 401(k) isn’t necessarily going to move the needle all that much. However, there is a plan available that may help tremendously. The cash balance plan is a little known hybrid retirement plan that allows high-earning practices and business owners to put away a serious amount of money in a short amount of time. For instance, an optimally set up cash balance plan would allow a 59 year old to save up to $278,000 in qualified pretax dollars in a single year. Undoubtedly, such plans are one of the most effective and efficient ways to save money for retirement for those who qualify.
Check out the maximum contributions limits of some retirement strategies below based on your age group.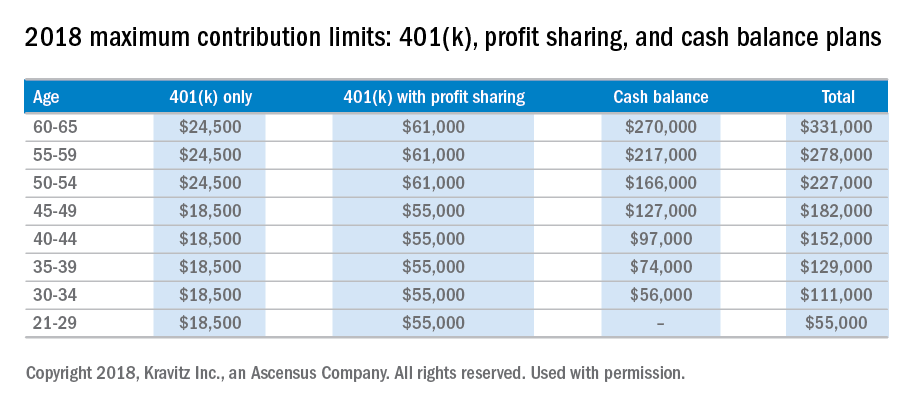
It’s important to realize that it is time that makes money, not timing. Establishing a smart investment plan early in your career will pay huge dividends and save mountains of heartache in your future. If you are unsure about which retirement plan works best for you, I’d recommend speaking to a qualified financial professional to assist you in the process. When it comes to planning for retirement, sooner is always better than later. The financial sacrifices of starting early are never as great as most young professionals fear.
Disclaimer:
This material has been prepared for educational purposes only and is not intended to provide, and should not be relied on for tax, legal, accounting advice, or financial advice. You should consult your own tax, legal, accounting, and financial advisors before engaging in any transaction. Securities offered through Capitol Securities Management Member FINRA, SIPC
Mr. Bellamah is a registered investment advisor with BNB Wealth Management http://www.bnbinc.com/.
Approaching the concept of retirement savings is particularly unique for medical professionals: Balancing a tremendously demanding career with family life and personal time allows few to have the luxury of extra time to address financial planning. Many in the field have higher priorities than saving for retirement on their minds, which compounds the issue.
According to the Association of American Medical Colleges, 76% of medical students will have student debt by the time they graduate. Among those students, the average debt is a staggering $190,000. The average American couple has only about $163,000 in savings by the time they are about 60 years old, so coming out of school, the average doctor will have more in debt than most have saved in their lifetimes. This means that many doctors can’t really start saving significantly until the latter half of their careers. With that in mind, consider these tips to help you on your journey to financial security.
Pay off debt or start saving for retirement?
When it comes to the decision of investing toward retirement or paying off debt more aggressively, there is really only one question that needs to be answered: “Can I make more investing than the loan is costing me?” Given the fact that Direct Graduate Plus Loans are now sitting at about 7% interest rates, an investment would have to make more than 7% per year to make sense. While we can look back at the historical performance of the stock market over time, it is pretty safe to say that in this scenario paying off the student loans as aggressively as possible is the best choice. The reason being is that the loans have a guaranteed cost of 7% per year in accrued interest, whereas an investment is never fully guaranteed to grow.
Make no mistake: High-interest debt is a financial dead weight; the longer it sits, the more it will attempt to sink you financially. A general rule of thumb is that the higher the interest rate on the loan, the more aggressively it should be paid off. Once the high interest loans are taken care of, saving for retirement can reenter the equation.
The company match
That being said, there is one caveat to this rule that you should strongly consider if the opportunity exists: the 401(k) or 403(b) company match. If you work in a position that offers a match on retirement plan contributions, taking advantage of this could substantially benefit you. In a typical safe harbor retirement plan, you will see something like a 3.5% company match for a 6% salary contribution. While there is no one formula that applies to every situation, an opportunity such as this shouldn’t be passed up.
Saving for retirement can be difficult enough. Why not take advantage of a situation in which you are getting free money? You should think about contributing enough to get the maximum match and putting the rest toward student debt. If you are unsure about your particular course of action, I’d suggest speaking to your financial professional to assist in coming up with a suitable game plan.
Roth deferral option
While many folks understand the general ins and outs of how retirement plans work, they fail to realize that there are actually two different types of contributions that can be made in most 401(k)s and 403(b)s: traditional deferrals and Roth deferrals. A traditional deferral is the standard pretax contribution option that lets you skip paying taxes now. Instead, you get taxed at your normal income tax bracket when the money is withdrawn in retirement. This is the option that most people use.
Roth deferrals are posttax contributions. Every dollar contributed gets taxed as ordinary income. Why would one do this, you ask? While there are a variety of different benefits, the primary advantage is that you never have to pay taxes on this money again. To reiterate, you pay taxes on this money now and never have to pay any taxes on it again. This can be extraordinarily helpful in retirement because it gives you the flexibility to choose between taxable and tax-free income.
While you can contribute to personal Roth IRAs to the tune of $5,500 a year if you are under 50 years old and $6,500 if you are 50 years and older, high income earners can be hampered by income limits. For instance, if you make over $135,000 a year as a single person or over $199,000 as a married couple, you are ineligible to make Roth IRA contributions. However, a benefit to Roth contributions in your company 401(k) or 403(b) plan is that these income limits don’t apply. Regardless of your level of income, you can make Roth deferrals in company sponsored retirement plans that allow them.
This strategy is best fit for, but not limited to, those who are earlier on in their careers and can reasonably expect to make much more in the future than they do now. Younger investors have the benefit of time: The more time an investment has to grow, the more it should be worth later on. Also, younger professionals are probably going to be paying the least amount of taxes early in their careers. While not all retirement plans allow for Roth deferrals, if the option is available, why not get taxes out of the way while it’s still relatively cheaper to do so?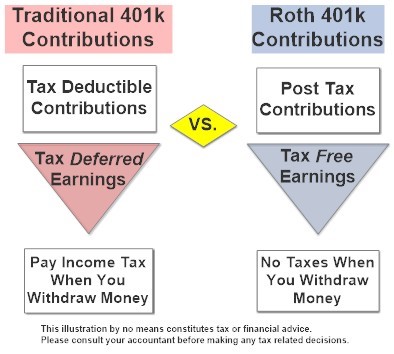
More aggressive strategies for those who need to “catch up” on retirement savings
Because many in the medical field have burdensome student loans, saving for retirement is often something that is pushed off by necessity. That being said, there are different ways to start saving more aggressively the closer you get toward retirement.
Catch up contributions. 401(k)s, 403(b)s, and IRAs all have built in “catch up” contributions that allow those aged 50 or older to save more. For instance, up to age 49 years, the maximum annual contribution in a 401(k) or 403(b) is $18,500 for 2018. At age 50 years, you are allowed to add an additional $6000 “catch up” contribution for a total of $24,500 per year. Likewise, IRAs allow for an additional $1000 per year contribution at age 50 years for a $6500 total yearly contribution.
Spousal IRAs. If you have a nonworking spouse, you may be able to contribute to an IRA on his or her behalf. To be eligible for a spousal IRA contribution, you must be married, file a joint income tax return, and have an earned income of at least what is being contributed to the IRAs. This would allow an additional $5,500 to $6,500 in retirement savings per year depending on your spouse’s age.
Simplified Employee Pension IRAs. For those who are self-employed, it could be worthwhile to look into opening up a Simplified Employee Pension (SEP) IRA. These types of retirement plans are similar to traditional IRAs except that they can only be opened up by an employer. The benefit of a SEP IRA is that it allows for a maximum pretax contribution of up to $54,000 or 25% of your total income, whichever is less.
Cash balance plans. For very-high-earning business owners or sole proprietors, saving $24,500 a year pretax in a 401(k) isn’t necessarily going to move the needle all that much. However, there is a plan available that may help tremendously. The cash balance plan is a little known hybrid retirement plan that allows high-earning practices and business owners to put away a serious amount of money in a short amount of time. For instance, an optimally set up cash balance plan would allow a 59 year old to save up to $278,000 in qualified pretax dollars in a single year. Undoubtedly, such plans are one of the most effective and efficient ways to save money for retirement for those who qualify.
Check out the maximum contributions limits of some retirement strategies below based on your age group.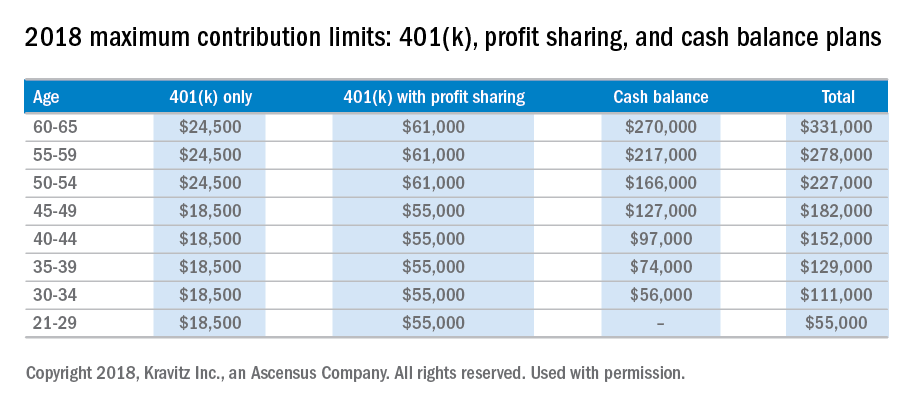
It’s important to realize that it is time that makes money, not timing. Establishing a smart investment plan early in your career will pay huge dividends and save mountains of heartache in your future. If you are unsure about which retirement plan works best for you, I’d recommend speaking to a qualified financial professional to assist you in the process. When it comes to planning for retirement, sooner is always better than later. The financial sacrifices of starting early are never as great as most young professionals fear.
Disclaimer:
This material has been prepared for educational purposes only and is not intended to provide, and should not be relied on for tax, legal, accounting advice, or financial advice. You should consult your own tax, legal, accounting, and financial advisors before engaging in any transaction. Securities offered through Capitol Securities Management Member FINRA, SIPC
Mr. Bellamah is a registered investment advisor with BNB Wealth Management http://www.bnbinc.com/.
Legal Issues for the Gastroenterologist: Part II
In the previous issue of The New Gastroenterologist, we discussed statistics and the basis on which most gastroenterologists are sued as well as what you can do to minimize this risk. In this second article, we discuss steps to assist in your defense in the event you have been sued. The following suggestions are based on our experience as defense attorneys who practice in the arena of medical malpractice.
Do not, under any circumstances, add or alter the plaintiff’s medical records. Although you have continued access to electronic medical records, accessing or altering these documents leaves an electronic trail. Attorneys are now frequently requesting an “audit trail” during discovery, which shows who and when someone accessed or altered relevant medical records. Additionally, it is likely that the plaintiff’s counsel has already obtained and reviewed records for their client. As such, counsel will notice any alterations and will require an explanation as to the same. If you did alter any medical records, it is important that you notify your attorney about the specifics of such.
After you have secured an attorney, it is critical that you arrange a meeting to develop a positive relationship early in the litigation process. This is important for many reasons. A medical malpractice case can be a long and arduous process which requires that you be involved with your attorney during the course of the litigation. For the attorney-client relationship to be successful, it is imperative that you know and feel comfortable with your attorney and develop confidence and trust in her. Without this trust, it will be difficult for you to accept various decisions or suggestions that the attorney believes are in your best interest. Conversely, the attorney should get to know you and understand your background, as this will assist in your representation.
A good relationship with you will also aid your attorney in educating herself on medical concepts relating to your case. Remember, your attorney most likely has not attended medical school and many of the medical concepts will initially be new to her. By the time trial arrives, however, your attorney will be very familiar with the medical issues in your case. This learning process can be expedited with your assistance and research.
Your deposition
At some point during the lawsuit, the plaintiff’s attorney will take your deposition. The plaintiff’s attorney will strive to obtain concessions that establish the standard of care, breach of the standard, causation, and damages. Your deposition is not the time for you to provide explanations. It is the time for you to concisely answer specific questions posed by counsel without volunteering any additional information. Ultimately, trials build on what occurs during depositions. Preparation is key. Be open to advice or criticisms from your lawyer. Try to eliminate any quirks or habits that interfere with the substance of your testimony or perceived credibility. A deposition is not a casual conversation, nor is it a test of your memory. Limit your answers to personal knowledge; never guess or speculate. If you do not know the answer to a question, or do not remember something, it is perfectly acceptable for you to say so. Only answer questions that you understand. You are allowed to ask the plaintiff’s counsel to repeat or rephrase questions.
Finally, and most importantly, always tell the truth. Discuss any anticipated issues or concerns with your lawyer before your deposition.
Preparing for trial
Conclusion
In summary, remember that there are things you can do both before and after you are sued to minimize litigation and its impact. As mentioned previously, before a lawsuit, and as a regular part of your practice, it is important that you stay current with medical advances, that you take the time to create a relationship with your patients involving quality communication, and that you thoroughly and legibly document all aspects of care provided. After a suit is filed against you, make sure you notify your insurer immediately, do not alter any records or discuss the case with anyone other than your lawyer or spouse, and do all you can to create a productive and honest relationship with your lawyer. This relationship will be invaluable as you do the difficult and time-consuming work of preparing for your deposition and trial, and it can help you endure and successfully navigate the litigation process.
The Importance of Follow-Up: Further Advice on How to Decrease the Risk of Being Sued
A common basis for establishing a malpractice liability claim against a physician is the failure to follow-up or track a patient’s test results. In today’s world, there is an increasing number of moving parts involved in any given patient’s care. A particular patient may treat with numerous physicians, all of whom use different record systems. Electronic medical record systems have made records more accessible and easier to track, but they also present a new set of challenges.
Every physician needs to determine how they plan to track test results. The ideal system would allow a physician to quickly get back any lab or diagnostic test that he or she orders. All staff members should know how the physician’s system works. Otherwise, test results might accidentally be filed before the physician reviews them or a miscommunication could prevent test results from being delivered. Whatever choice of system, it is key to follow and effectively use the program every time.
Additionally, it can be beneficial to let the patient know when he or she can expect to hear about their results, as failure to keep the patient reasonably informed can create a new set of patient concerns and anxiety. Ultimately, establishing a well-defined system for record-tracking can help physicians avoid malpractice liability claims because of a failure to follow-up.
In the previous issue of The New Gastroenterologist, we discussed statistics and the basis on which most gastroenterologists are sued as well as what you can do to minimize this risk. In this second article, we discuss steps to assist in your defense in the event you have been sued. The following suggestions are based on our experience as defense attorneys who practice in the arena of medical malpractice.
Do not, under any circumstances, add or alter the plaintiff’s medical records. Although you have continued access to electronic medical records, accessing or altering these documents leaves an electronic trail. Attorneys are now frequently requesting an “audit trail” during discovery, which shows who and when someone accessed or altered relevant medical records. Additionally, it is likely that the plaintiff’s counsel has already obtained and reviewed records for their client. As such, counsel will notice any alterations and will require an explanation as to the same. If you did alter any medical records, it is important that you notify your attorney about the specifics of such.
After you have secured an attorney, it is critical that you arrange a meeting to develop a positive relationship early in the litigation process. This is important for many reasons. A medical malpractice case can be a long and arduous process which requires that you be involved with your attorney during the course of the litigation. For the attorney-client relationship to be successful, it is imperative that you know and feel comfortable with your attorney and develop confidence and trust in her. Without this trust, it will be difficult for you to accept various decisions or suggestions that the attorney believes are in your best interest. Conversely, the attorney should get to know you and understand your background, as this will assist in your representation.
A good relationship with you will also aid your attorney in educating herself on medical concepts relating to your case. Remember, your attorney most likely has not attended medical school and many of the medical concepts will initially be new to her. By the time trial arrives, however, your attorney will be very familiar with the medical issues in your case. This learning process can be expedited with your assistance and research.
Your deposition
At some point during the lawsuit, the plaintiff’s attorney will take your deposition. The plaintiff’s attorney will strive to obtain concessions that establish the standard of care, breach of the standard, causation, and damages. Your deposition is not the time for you to provide explanations. It is the time for you to concisely answer specific questions posed by counsel without volunteering any additional information. Ultimately, trials build on what occurs during depositions. Preparation is key. Be open to advice or criticisms from your lawyer. Try to eliminate any quirks or habits that interfere with the substance of your testimony or perceived credibility. A deposition is not a casual conversation, nor is it a test of your memory. Limit your answers to personal knowledge; never guess or speculate. If you do not know the answer to a question, or do not remember something, it is perfectly acceptable for you to say so. Only answer questions that you understand. You are allowed to ask the plaintiff’s counsel to repeat or rephrase questions.
Finally, and most importantly, always tell the truth. Discuss any anticipated issues or concerns with your lawyer before your deposition.
Preparing for trial
Conclusion
In summary, remember that there are things you can do both before and after you are sued to minimize litigation and its impact. As mentioned previously, before a lawsuit, and as a regular part of your practice, it is important that you stay current with medical advances, that you take the time to create a relationship with your patients involving quality communication, and that you thoroughly and legibly document all aspects of care provided. After a suit is filed against you, make sure you notify your insurer immediately, do not alter any records or discuss the case with anyone other than your lawyer or spouse, and do all you can to create a productive and honest relationship with your lawyer. This relationship will be invaluable as you do the difficult and time-consuming work of preparing for your deposition and trial, and it can help you endure and successfully navigate the litigation process.
The Importance of Follow-Up: Further Advice on How to Decrease the Risk of Being Sued
A common basis for establishing a malpractice liability claim against a physician is the failure to follow-up or track a patient’s test results. In today’s world, there is an increasing number of moving parts involved in any given patient’s care. A particular patient may treat with numerous physicians, all of whom use different record systems. Electronic medical record systems have made records more accessible and easier to track, but they also present a new set of challenges.
Every physician needs to determine how they plan to track test results. The ideal system would allow a physician to quickly get back any lab or diagnostic test that he or she orders. All staff members should know how the physician’s system works. Otherwise, test results might accidentally be filed before the physician reviews them or a miscommunication could prevent test results from being delivered. Whatever choice of system, it is key to follow and effectively use the program every time.
Additionally, it can be beneficial to let the patient know when he or she can expect to hear about their results, as failure to keep the patient reasonably informed can create a new set of patient concerns and anxiety. Ultimately, establishing a well-defined system for record-tracking can help physicians avoid malpractice liability claims because of a failure to follow-up.
In the previous issue of The New Gastroenterologist, we discussed statistics and the basis on which most gastroenterologists are sued as well as what you can do to minimize this risk. In this second article, we discuss steps to assist in your defense in the event you have been sued. The following suggestions are based on our experience as defense attorneys who practice in the arena of medical malpractice.
Do not, under any circumstances, add or alter the plaintiff’s medical records. Although you have continued access to electronic medical records, accessing or altering these documents leaves an electronic trail. Attorneys are now frequently requesting an “audit trail” during discovery, which shows who and when someone accessed or altered relevant medical records. Additionally, it is likely that the plaintiff’s counsel has already obtained and reviewed records for their client. As such, counsel will notice any alterations and will require an explanation as to the same. If you did alter any medical records, it is important that you notify your attorney about the specifics of such.
After you have secured an attorney, it is critical that you arrange a meeting to develop a positive relationship early in the litigation process. This is important for many reasons. A medical malpractice case can be a long and arduous process which requires that you be involved with your attorney during the course of the litigation. For the attorney-client relationship to be successful, it is imperative that you know and feel comfortable with your attorney and develop confidence and trust in her. Without this trust, it will be difficult for you to accept various decisions or suggestions that the attorney believes are in your best interest. Conversely, the attorney should get to know you and understand your background, as this will assist in your representation.
A good relationship with you will also aid your attorney in educating herself on medical concepts relating to your case. Remember, your attorney most likely has not attended medical school and many of the medical concepts will initially be new to her. By the time trial arrives, however, your attorney will be very familiar with the medical issues in your case. This learning process can be expedited with your assistance and research.
Your deposition
At some point during the lawsuit, the plaintiff’s attorney will take your deposition. The plaintiff’s attorney will strive to obtain concessions that establish the standard of care, breach of the standard, causation, and damages. Your deposition is not the time for you to provide explanations. It is the time for you to concisely answer specific questions posed by counsel without volunteering any additional information. Ultimately, trials build on what occurs during depositions. Preparation is key. Be open to advice or criticisms from your lawyer. Try to eliminate any quirks or habits that interfere with the substance of your testimony or perceived credibility. A deposition is not a casual conversation, nor is it a test of your memory. Limit your answers to personal knowledge; never guess or speculate. If you do not know the answer to a question, or do not remember something, it is perfectly acceptable for you to say so. Only answer questions that you understand. You are allowed to ask the plaintiff’s counsel to repeat or rephrase questions.
Finally, and most importantly, always tell the truth. Discuss any anticipated issues or concerns with your lawyer before your deposition.
Preparing for trial
Conclusion
In summary, remember that there are things you can do both before and after you are sued to minimize litigation and its impact. As mentioned previously, before a lawsuit, and as a regular part of your practice, it is important that you stay current with medical advances, that you take the time to create a relationship with your patients involving quality communication, and that you thoroughly and legibly document all aspects of care provided. After a suit is filed against you, make sure you notify your insurer immediately, do not alter any records or discuss the case with anyone other than your lawyer or spouse, and do all you can to create a productive and honest relationship with your lawyer. This relationship will be invaluable as you do the difficult and time-consuming work of preparing for your deposition and trial, and it can help you endure and successfully navigate the litigation process.
The Importance of Follow-Up: Further Advice on How to Decrease the Risk of Being Sued
A common basis for establishing a malpractice liability claim against a physician is the failure to follow-up or track a patient’s test results. In today’s world, there is an increasing number of moving parts involved in any given patient’s care. A particular patient may treat with numerous physicians, all of whom use different record systems. Electronic medical record systems have made records more accessible and easier to track, but they also present a new set of challenges.
Every physician needs to determine how they plan to track test results. The ideal system would allow a physician to quickly get back any lab or diagnostic test that he or she orders. All staff members should know how the physician’s system works. Otherwise, test results might accidentally be filed before the physician reviews them or a miscommunication could prevent test results from being delivered. Whatever choice of system, it is key to follow and effectively use the program every time.
Additionally, it can be beneficial to let the patient know when he or she can expect to hear about their results, as failure to keep the patient reasonably informed can create a new set of patient concerns and anxiety. Ultimately, establishing a well-defined system for record-tracking can help physicians avoid malpractice liability claims because of a failure to follow-up.























