User login
FDG-PET Performs Poorly in Lung Cancer Diagnosis
CHICAGO – The diagnostic accuracy of FDG-PET in lung cancer performed below levels described in previous reports and varied widely among U.S. centers in a secondary analysis of a large phase III clinical trial.
"FDG-PET performed poorly for diagnosing non–small cell lung cancer in a national sample of clinical stage 1 patients," Dr. Eric L. Grogan said at the annnual meeting of the of the American Society of Clinical Oncology.
The current National Comprehensive Cancer Network guidelines recommend the use of fluorodeoxyglucose positron emission tomography (FDG-PET) for the diagnosis of NSCLC based on studies showing a high degree of accuracy for this diagnostic tool, notably a sensitivity of 94% and a median specificity of 83% in a meta-analysis of 40 studies (JAMA 2001;285:914-24).
Others have reported, however, that FDG-PET performs poorly at single institutions in regions of endemic fungal lung diseases (Ann. Thor. Surg. 2011;92:428-32 and Lung Cancer 2002;36:297-301), observed Dr. Grogan, of Vanderbilt-Ingram Cancer Center in Nashville, Tenn.
Among 682 patients in the American College of Surgeons Oncology Group (ACOSOG) Z4031 trial, the overall accuracy of FDG-PET was 73%, the sensitivity 82%, and the specificity only 31%.
The series is the largest to date evaluating the accuracy of FDG-PET in patients with known or suspected clinical stage 1 NSCLC. In addition, it is generalizable to clinical practice because multiple FDG-PET scanners were used and the scans were performed in community and academic centers and interpreted by multiple radiologists, Dr. Grogan said.
"Results of PET scans in this population should be interpreted cautiously, and reasons for the poor test performance should be explored in other studies," he said.
Discussant Dr. Tetsuya Mitsudomi, who is the chief of thoracic surgery at Aichi Cancer Center Hospital in Nagoya, Japan, said FDG-PET shows reasonable sensitivity, but very low specificity compared with previous studies.
"I think this reflects the real world," he said. "So, the lung cancer diagnosis cannot be made on the basis of PET positivity alone."
Investigators at 51 sites in 39 cities enrolled 969 patients with known or clinically suspicious stage 1 lesions between 2004 and 2006 to evaluate the value of proteomic analysis in diagnosing NSCLC (the results were presented at ASCO 2010). FDG-PET scans were available for 682 patients. All underwent surgical resection. Analyses were performed for all patients and for sites with more than 25 patients.
PET avidity was determined by the radiologist’s description of lesion activity or by the reported maximum standard uptake value (SUV). Avidity was classified in four categories: category 1 was no avidity/not cancer (SUV = 0), category 2 was low avidity/not likely cancer (SUV 0 to less than 2.5), category 3 was avidity/possibly cancer (SUV 2.5 to less than 5.0), and category 4 was high avidity/likely cancer (SUV 5.0 or more).
Among the 682 patients, there were 566 cancers and 116 benign cases. In all, 82% of the cancerous lesions were PET avid, and "surprisingly, 69% of the benign lesions were avid," Dr. Grogan said.
Patients with cancer were significantly older (67 vs. 61 years; P less than .001) and had larger lesions (26 mm vs. 20 mm; P less than .001).
The positive predictive value of FDG-PET was 85% and negative predictive value 26%. This translates into 80 false positives and 101 false negatives. The majority of false positives were found to be granulomas (69%), he observed. Eleven of the false negatives were 10 mm or less.
Not surprising, FDG-PET accuracy improved with lesion size, Dr. Grogan said. The accuracy was less than 50% for lesions less than 20 mm, but greater than 80% for lesions larger than 30 mm. "Above 30 mm, the accuracy did not seem to improve," he observed.
In the eight cities that had more than 25 patients, the sensitivity varied significantly, from a low of 67% in Los Angeles to a high of 91% in Durham, N.C. (P = .03), Dr. Grogan said, without explanation. Specificity ranged from 15% in Birmingham, Ala., to 46% in Philadelphia, but this did not reach statistical significance because of the small number of benign cases at each institution (P = .72).
Dr. Mitsudomi said he could not explain the reason for the heterogeneity, especially in terms of the specificity, between centers.
"It’s not possible to remove all the false positives if you use FDG, but newer tracers are being developed and they may increase the specificity rate," he added.
Dr. Grogan reported no disclosures. Dr. Mitsudomi reported having a consulting/advisory role with Boehringer Ingelheim, Kyowa Hakko Kirin, Lilly, and Pfizer, and receiving honoraria from AstraZeneca, Chugai Pharma, Lilly, and Roche.☐
CHICAGO – The diagnostic accuracy of FDG-PET in lung cancer performed below levels described in previous reports and varied widely among U.S. centers in a secondary analysis of a large phase III clinical trial.
"FDG-PET performed poorly for diagnosing non–small cell lung cancer in a national sample of clinical stage 1 patients," Dr. Eric L. Grogan said at the annnual meeting of the of the American Society of Clinical Oncology.
The current National Comprehensive Cancer Network guidelines recommend the use of fluorodeoxyglucose positron emission tomography (FDG-PET) for the diagnosis of NSCLC based on studies showing a high degree of accuracy for this diagnostic tool, notably a sensitivity of 94% and a median specificity of 83% in a meta-analysis of 40 studies (JAMA 2001;285:914-24).
Others have reported, however, that FDG-PET performs poorly at single institutions in regions of endemic fungal lung diseases (Ann. Thor. Surg. 2011;92:428-32 and Lung Cancer 2002;36:297-301), observed Dr. Grogan, of Vanderbilt-Ingram Cancer Center in Nashville, Tenn.
Among 682 patients in the American College of Surgeons Oncology Group (ACOSOG) Z4031 trial, the overall accuracy of FDG-PET was 73%, the sensitivity 82%, and the specificity only 31%.
The series is the largest to date evaluating the accuracy of FDG-PET in patients with known or suspected clinical stage 1 NSCLC. In addition, it is generalizable to clinical practice because multiple FDG-PET scanners were used and the scans were performed in community and academic centers and interpreted by multiple radiologists, Dr. Grogan said.
"Results of PET scans in this population should be interpreted cautiously, and reasons for the poor test performance should be explored in other studies," he said.
Discussant Dr. Tetsuya Mitsudomi, who is the chief of thoracic surgery at Aichi Cancer Center Hospital in Nagoya, Japan, said FDG-PET shows reasonable sensitivity, but very low specificity compared with previous studies.
"I think this reflects the real world," he said. "So, the lung cancer diagnosis cannot be made on the basis of PET positivity alone."
Investigators at 51 sites in 39 cities enrolled 969 patients with known or clinically suspicious stage 1 lesions between 2004 and 2006 to evaluate the value of proteomic analysis in diagnosing NSCLC (the results were presented at ASCO 2010). FDG-PET scans were available for 682 patients. All underwent surgical resection. Analyses were performed for all patients and for sites with more than 25 patients.
PET avidity was determined by the radiologist’s description of lesion activity or by the reported maximum standard uptake value (SUV). Avidity was classified in four categories: category 1 was no avidity/not cancer (SUV = 0), category 2 was low avidity/not likely cancer (SUV 0 to less than 2.5), category 3 was avidity/possibly cancer (SUV 2.5 to less than 5.0), and category 4 was high avidity/likely cancer (SUV 5.0 or more).
Among the 682 patients, there were 566 cancers and 116 benign cases. In all, 82% of the cancerous lesions were PET avid, and "surprisingly, 69% of the benign lesions were avid," Dr. Grogan said.
Patients with cancer were significantly older (67 vs. 61 years; P less than .001) and had larger lesions (26 mm vs. 20 mm; P less than .001).
The positive predictive value of FDG-PET was 85% and negative predictive value 26%. This translates into 80 false positives and 101 false negatives. The majority of false positives were found to be granulomas (69%), he observed. Eleven of the false negatives were 10 mm or less.
Not surprising, FDG-PET accuracy improved with lesion size, Dr. Grogan said. The accuracy was less than 50% for lesions less than 20 mm, but greater than 80% for lesions larger than 30 mm. "Above 30 mm, the accuracy did not seem to improve," he observed.
In the eight cities that had more than 25 patients, the sensitivity varied significantly, from a low of 67% in Los Angeles to a high of 91% in Durham, N.C. (P = .03), Dr. Grogan said, without explanation. Specificity ranged from 15% in Birmingham, Ala., to 46% in Philadelphia, but this did not reach statistical significance because of the small number of benign cases at each institution (P = .72).
Dr. Mitsudomi said he could not explain the reason for the heterogeneity, especially in terms of the specificity, between centers.
"It’s not possible to remove all the false positives if you use FDG, but newer tracers are being developed and they may increase the specificity rate," he added.
Dr. Grogan reported no disclosures. Dr. Mitsudomi reported having a consulting/advisory role with Boehringer Ingelheim, Kyowa Hakko Kirin, Lilly, and Pfizer, and receiving honoraria from AstraZeneca, Chugai Pharma, Lilly, and Roche.☐
CHICAGO – The diagnostic accuracy of FDG-PET in lung cancer performed below levels described in previous reports and varied widely among U.S. centers in a secondary analysis of a large phase III clinical trial.
"FDG-PET performed poorly for diagnosing non–small cell lung cancer in a national sample of clinical stage 1 patients," Dr. Eric L. Grogan said at the annnual meeting of the of the American Society of Clinical Oncology.
The current National Comprehensive Cancer Network guidelines recommend the use of fluorodeoxyglucose positron emission tomography (FDG-PET) for the diagnosis of NSCLC based on studies showing a high degree of accuracy for this diagnostic tool, notably a sensitivity of 94% and a median specificity of 83% in a meta-analysis of 40 studies (JAMA 2001;285:914-24).
Others have reported, however, that FDG-PET performs poorly at single institutions in regions of endemic fungal lung diseases (Ann. Thor. Surg. 2011;92:428-32 and Lung Cancer 2002;36:297-301), observed Dr. Grogan, of Vanderbilt-Ingram Cancer Center in Nashville, Tenn.
Among 682 patients in the American College of Surgeons Oncology Group (ACOSOG) Z4031 trial, the overall accuracy of FDG-PET was 73%, the sensitivity 82%, and the specificity only 31%.
The series is the largest to date evaluating the accuracy of FDG-PET in patients with known or suspected clinical stage 1 NSCLC. In addition, it is generalizable to clinical practice because multiple FDG-PET scanners were used and the scans were performed in community and academic centers and interpreted by multiple radiologists, Dr. Grogan said.
"Results of PET scans in this population should be interpreted cautiously, and reasons for the poor test performance should be explored in other studies," he said.
Discussant Dr. Tetsuya Mitsudomi, who is the chief of thoracic surgery at Aichi Cancer Center Hospital in Nagoya, Japan, said FDG-PET shows reasonable sensitivity, but very low specificity compared with previous studies.
"I think this reflects the real world," he said. "So, the lung cancer diagnosis cannot be made on the basis of PET positivity alone."
Investigators at 51 sites in 39 cities enrolled 969 patients with known or clinically suspicious stage 1 lesions between 2004 and 2006 to evaluate the value of proteomic analysis in diagnosing NSCLC (the results were presented at ASCO 2010). FDG-PET scans were available for 682 patients. All underwent surgical resection. Analyses were performed for all patients and for sites with more than 25 patients.
PET avidity was determined by the radiologist’s description of lesion activity or by the reported maximum standard uptake value (SUV). Avidity was classified in four categories: category 1 was no avidity/not cancer (SUV = 0), category 2 was low avidity/not likely cancer (SUV 0 to less than 2.5), category 3 was avidity/possibly cancer (SUV 2.5 to less than 5.0), and category 4 was high avidity/likely cancer (SUV 5.0 or more).
Among the 682 patients, there were 566 cancers and 116 benign cases. In all, 82% of the cancerous lesions were PET avid, and "surprisingly, 69% of the benign lesions were avid," Dr. Grogan said.
Patients with cancer were significantly older (67 vs. 61 years; P less than .001) and had larger lesions (26 mm vs. 20 mm; P less than .001).
The positive predictive value of FDG-PET was 85% and negative predictive value 26%. This translates into 80 false positives and 101 false negatives. The majority of false positives were found to be granulomas (69%), he observed. Eleven of the false negatives were 10 mm or less.
Not surprising, FDG-PET accuracy improved with lesion size, Dr. Grogan said. The accuracy was less than 50% for lesions less than 20 mm, but greater than 80% for lesions larger than 30 mm. "Above 30 mm, the accuracy did not seem to improve," he observed.
In the eight cities that had more than 25 patients, the sensitivity varied significantly, from a low of 67% in Los Angeles to a high of 91% in Durham, N.C. (P = .03), Dr. Grogan said, without explanation. Specificity ranged from 15% in Birmingham, Ala., to 46% in Philadelphia, but this did not reach statistical significance because of the small number of benign cases at each institution (P = .72).
Dr. Mitsudomi said he could not explain the reason for the heterogeneity, especially in terms of the specificity, between centers.
"It’s not possible to remove all the false positives if you use FDG, but newer tracers are being developed and they may increase the specificity rate," he added.
Dr. Grogan reported no disclosures. Dr. Mitsudomi reported having a consulting/advisory role with Boehringer Ingelheim, Kyowa Hakko Kirin, Lilly, and Pfizer, and receiving honoraria from AstraZeneca, Chugai Pharma, Lilly, and Roche.☐
Major Finding: The overall accuracy of FDG-PET was 73%, the sensitivity 82%, and the specificity only 31%.
Data Source: Secondary analysis of 682 patients with FDG-PET scans in the ACOSOG Z4031 trial of 969 patients with a clinically suspicious stage I lung lesion.
Disclosures: Dr. Grogan reported no disclosures. Dr. Mitsudomi reported having a consulting/advisory role with Boehringer Ingelheim, Kyowa Hakko Kirin, Lilly, and Pfizer, and receiving honoraria from AstraZeneca, Chugai Pharma, Lilly, and Roche.
Night Pediatric Curriculum Emerges Amid Restricted Residency Hours
COVINGTON, KY. – A national pediatric nighttime curriculum is feasible and improves resident learning and confidence, data from a national field test have shown.
The Web- and case-based curriculum was created through a massive collaborative effort and fills a global need in the wake of the 2011 Accreditation Council for Graduate Medical Education resident work-hour restrictions. Those restrictions led to a substantial increase in nighttime rotations for interns and second- and third-year residents.

Despite this shift, only 30% of residency programs had a formal nighttime curriculum by November 2010.
Nighttime rotations bring a unique challenge of delivering resident education in "an environment where there isn’t the traditional morning report, noon conference, and postcall rounds," Dr. Rebecca Blankenburg said at Pediatric Hospital Medicine 2012.
Through a collaboration of the Academic Pediatric Association, American Academy of Pediatrics, Society of Hospital Medicine, and the Association of Pediatric Program Directors, educators nationally created 30 modules based on topics determined through a literature review, a needs assessment of residency program directors, and an expert consensus.
Each module contains one case geared toward interns and one case geared toward residents, a brief 15-minute PowerPoint presentation with and without voiceover, a 1- to 2-page topic summary, and five pre- and posttest questions, said Dr. Blankenburg, a hospitalist with Lucile Packard Children’s Hospital at Stanford (Calif.) University.
A preliminary pilot test was conducted at Stanford from February to June 2011, followed by the national field test of 10 modules from July to December 2011.
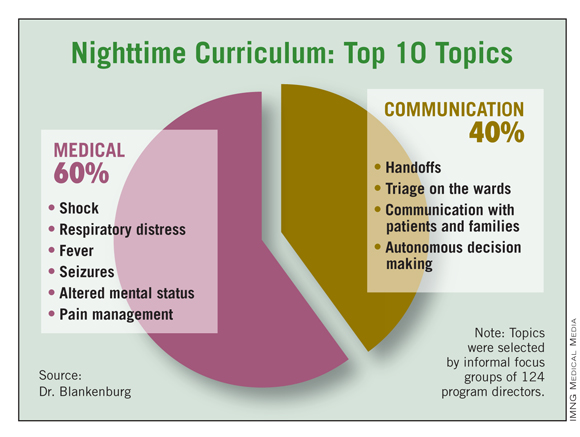
The top 10 topics, selected by informal focus groups of 124 program directors, were 60% medical and 40% communication. They covered shock, respiratory distress, fever, seizures, altered mental status, pain management, handoffs, triage on the wards, communication with patients and families, and autonomous decision making.
"The focus groups felt really strongly that at nighttime, we shouldn’t be teaching things that could be taught by a content expert during the day, but rather emphasizing those teachable moments at night," Dr. Blankenburg said.
In all, 89 pediatric and combined internal medicine–pediatric residency programs participated, representing 46% of all programs nationally and involving more than 2,000 learners. Prior to the study, 84% of participating programs had no nighttime curriculum.
Although program directors anticipated that the curriculum would be taught equally between self-study computer modules, resident-led modules, and faculty-led modules, in actuality, those percentages were 47%, 29%, and 20%, respectively, with the remaining 4% conducted via other means including Skype, she said.
During their nighttime rotation, 64% of residents completed at least six modules (average, 6.8).
"The curriculum was implemented in a variety of ways, which we felt was a potential limitation in that it was a more difficult study design, but it also makes it more practical in that we will be applying this broadly," Dr. Blankenburg said.
Residents responding to confidential online pre- and postcurriculum surveys believed that the curriculum significantly improved their nighttime learning (4.7 vs. 6.4 on a 10-point scale). Confidence also increased significantly for all 10 topics and all levels of learners, she said.
Among 493 respondents, pre- and postcurriculum knowledge scores increased significantly for first-year residents (6.11 vs. 7.24) and second-year residents (6.84 vs. 7.22), but not among those in their third year (7.16 vs. 7.31).
Though there were rich comments expressing a desire for residents or faculty to facilitate the sessions, an analysis of variance revealed no significant differences in attitudes, confidence, or knowledge across teaching methods, Dr. Blankenburg said.
Some residents described the curriculum as focused, quick, effective, and pertinent to night-shift concerns. Others suggested it could be improved by having higher levels of discussion for higher-level residents, using a facilitator, and adding more topics, questions, and cases to practice the knowledge learned in the sessions. The survey indicated that "77% of residents believed the modules were most geared towards interns," but that’s not necessarily a fatal flaw. " ‘[It’s] probably more helpful in terms of knowledge for earlier in residency. The formatting, however, helped with passing info along to my PGY1 counterpart,’ " Dr. Blankenburg quoted a third-year resident as saying.
The collaborative is already at work improving the curriculum based on feedback and has funding to place version 2 of the curriculum on the interactive Web-based platform Moodle by Aug. 15, Dr. Blankenburg said. There are also plans to join forces in the coming year with educational and design students to make the curriculum more interactive.
"We’re really interested in the idea of a flipped classroom and how to have these be learning modules that residents can do on their own, perhaps, but really have applied learning activities that bring it to a higher level," she added.
Dr. Blankenburg reported having no relevant financial conflicts. The research was funded through an APPD grant and the 2012 APA Ray E. Helfer Award for Innovation in Medical Education
**This story was updated and a collaborator's name corrected on Aug. 3, 2012.
COVINGTON, KY. – A national pediatric nighttime curriculum is feasible and improves resident learning and confidence, data from a national field test have shown.
The Web- and case-based curriculum was created through a massive collaborative effort and fills a global need in the wake of the 2011 Accreditation Council for Graduate Medical Education resident work-hour restrictions. Those restrictions led to a substantial increase in nighttime rotations for interns and second- and third-year residents.

Despite this shift, only 30% of residency programs had a formal nighttime curriculum by November 2010.
Nighttime rotations bring a unique challenge of delivering resident education in "an environment where there isn’t the traditional morning report, noon conference, and postcall rounds," Dr. Rebecca Blankenburg said at Pediatric Hospital Medicine 2012.
Through a collaboration of the Academic Pediatric Association, American Academy of Pediatrics, Society of Hospital Medicine, and the Association of Pediatric Program Directors, educators nationally created 30 modules based on topics determined through a literature review, a needs assessment of residency program directors, and an expert consensus.
Each module contains one case geared toward interns and one case geared toward residents, a brief 15-minute PowerPoint presentation with and without voiceover, a 1- to 2-page topic summary, and five pre- and posttest questions, said Dr. Blankenburg, a hospitalist with Lucile Packard Children’s Hospital at Stanford (Calif.) University.
A preliminary pilot test was conducted at Stanford from February to June 2011, followed by the national field test of 10 modules from July to December 2011.
The top 10 topics, selected by informal focus groups of 124 program directors, were 60% medical and 40% communication. They covered shock, respiratory distress, fever, seizures, altered mental status, pain management, handoffs, triage on the wards, communication with patients and families, and autonomous decision making.
"The focus groups felt really strongly that at nighttime, we shouldn’t be teaching things that could be taught by a content expert during the day, but rather emphasizing those teachable moments at night," Dr. Blankenburg said.
In all, 89 pediatric and combined internal medicine–pediatric residency programs participated, representing 46% of all programs nationally and involving more than 2,000 learners. Prior to the study, 84% of participating programs had no nighttime curriculum.
Although program directors anticipated that the curriculum would be taught equally between self-study computer modules, resident-led modules, and faculty-led modules, in actuality, those percentages were 47%, 29%, and 20%, respectively, with the remaining 4% conducted via other means including Skype, she said.
During their nighttime rotation, 64% of residents completed at least six modules (average, 6.8).
"The curriculum was implemented in a variety of ways, which we felt was a potential limitation in that it was a more difficult study design, but it also makes it more practical in that we will be applying this broadly," Dr. Blankenburg said.
Residents responding to confidential online pre- and postcurriculum surveys believed that the curriculum significantly improved their nighttime learning (4.7 vs. 6.4 on a 10-point scale). Confidence also increased significantly for all 10 topics and all levels of learners, she said.
Among 493 respondents, pre- and postcurriculum knowledge scores increased significantly for first-year residents (6.11 vs. 7.24) and second-year residents (6.84 vs. 7.22), but not among those in their third year (7.16 vs. 7.31).
Though there were rich comments expressing a desire for residents or faculty to facilitate the sessions, an analysis of variance revealed no significant differences in attitudes, confidence, or knowledge across teaching methods, Dr. Blankenburg said.
Some residents described the curriculum as focused, quick, effective, and pertinent to night-shift concerns. Others suggested it could be improved by having higher levels of discussion for higher-level residents, using a facilitator, and adding more topics, questions, and cases to practice the knowledge learned in the sessions. The survey indicated that "77% of residents believed the modules were most geared towards interns," but that’s not necessarily a fatal flaw. " ‘[It’s] probably more helpful in terms of knowledge for earlier in residency. The formatting, however, helped with passing info along to my PGY1 counterpart,’ " Dr. Blankenburg quoted a third-year resident as saying.
The collaborative is already at work improving the curriculum based on feedback and has funding to place version 2 of the curriculum on the interactive Web-based platform Moodle by Aug. 15, Dr. Blankenburg said. There are also plans to join forces in the coming year with educational and design students to make the curriculum more interactive.
"We’re really interested in the idea of a flipped classroom and how to have these be learning modules that residents can do on their own, perhaps, but really have applied learning activities that bring it to a higher level," she added.
Dr. Blankenburg reported having no relevant financial conflicts. The research was funded through an APPD grant and the 2012 APA Ray E. Helfer Award for Innovation in Medical Education
**This story was updated and a collaborator's name corrected on Aug. 3, 2012.
COVINGTON, KY. – A national pediatric nighttime curriculum is feasible and improves resident learning and confidence, data from a national field test have shown.
The Web- and case-based curriculum was created through a massive collaborative effort and fills a global need in the wake of the 2011 Accreditation Council for Graduate Medical Education resident work-hour restrictions. Those restrictions led to a substantial increase in nighttime rotations for interns and second- and third-year residents.

Despite this shift, only 30% of residency programs had a formal nighttime curriculum by November 2010.
Nighttime rotations bring a unique challenge of delivering resident education in "an environment where there isn’t the traditional morning report, noon conference, and postcall rounds," Dr. Rebecca Blankenburg said at Pediatric Hospital Medicine 2012.
Through a collaboration of the Academic Pediatric Association, American Academy of Pediatrics, Society of Hospital Medicine, and the Association of Pediatric Program Directors, educators nationally created 30 modules based on topics determined through a literature review, a needs assessment of residency program directors, and an expert consensus.
Each module contains one case geared toward interns and one case geared toward residents, a brief 15-minute PowerPoint presentation with and without voiceover, a 1- to 2-page topic summary, and five pre- and posttest questions, said Dr. Blankenburg, a hospitalist with Lucile Packard Children’s Hospital at Stanford (Calif.) University.
A preliminary pilot test was conducted at Stanford from February to June 2011, followed by the national field test of 10 modules from July to December 2011.
The top 10 topics, selected by informal focus groups of 124 program directors, were 60% medical and 40% communication. They covered shock, respiratory distress, fever, seizures, altered mental status, pain management, handoffs, triage on the wards, communication with patients and families, and autonomous decision making.
"The focus groups felt really strongly that at nighttime, we shouldn’t be teaching things that could be taught by a content expert during the day, but rather emphasizing those teachable moments at night," Dr. Blankenburg said.
In all, 89 pediatric and combined internal medicine–pediatric residency programs participated, representing 46% of all programs nationally and involving more than 2,000 learners. Prior to the study, 84% of participating programs had no nighttime curriculum.
Although program directors anticipated that the curriculum would be taught equally between self-study computer modules, resident-led modules, and faculty-led modules, in actuality, those percentages were 47%, 29%, and 20%, respectively, with the remaining 4% conducted via other means including Skype, she said.
During their nighttime rotation, 64% of residents completed at least six modules (average, 6.8).
"The curriculum was implemented in a variety of ways, which we felt was a potential limitation in that it was a more difficult study design, but it also makes it more practical in that we will be applying this broadly," Dr. Blankenburg said.
Residents responding to confidential online pre- and postcurriculum surveys believed that the curriculum significantly improved their nighttime learning (4.7 vs. 6.4 on a 10-point scale). Confidence also increased significantly for all 10 topics and all levels of learners, she said.
Among 493 respondents, pre- and postcurriculum knowledge scores increased significantly for first-year residents (6.11 vs. 7.24) and second-year residents (6.84 vs. 7.22), but not among those in their third year (7.16 vs. 7.31).
Though there were rich comments expressing a desire for residents or faculty to facilitate the sessions, an analysis of variance revealed no significant differences in attitudes, confidence, or knowledge across teaching methods, Dr. Blankenburg said.
Some residents described the curriculum as focused, quick, effective, and pertinent to night-shift concerns. Others suggested it could be improved by having higher levels of discussion for higher-level residents, using a facilitator, and adding more topics, questions, and cases to practice the knowledge learned in the sessions. The survey indicated that "77% of residents believed the modules were most geared towards interns," but that’s not necessarily a fatal flaw. " ‘[It’s] probably more helpful in terms of knowledge for earlier in residency. The formatting, however, helped with passing info along to my PGY1 counterpart,’ " Dr. Blankenburg quoted a third-year resident as saying.
The collaborative is already at work improving the curriculum based on feedback and has funding to place version 2 of the curriculum on the interactive Web-based platform Moodle by Aug. 15, Dr. Blankenburg said. There are also plans to join forces in the coming year with educational and design students to make the curriculum more interactive.
"We’re really interested in the idea of a flipped classroom and how to have these be learning modules that residents can do on their own, perhaps, but really have applied learning activities that bring it to a higher level," she added.
Dr. Blankenburg reported having no relevant financial conflicts. The research was funded through an APPD grant and the 2012 APA Ray E. Helfer Award for Innovation in Medical Education
**This story was updated and a collaborator's name corrected on Aug. 3, 2012.
AT PEDIATRIC HOSPITAL MEDICINE 2012
Major Finding: Residents responding to confidential online pre- and postcurriculum surveys believed that a pediatric nighttime curriculum significantly improved their nighttime learning (4.7 vs. 6.4 on a 10-point scale).
Data Source: A national field test of the curriculum was conducted at 89 pediatric and combined internal medicine–pediatric residency programs, representing 46% of all programs nationally.
Disclosures: Dr. Blankenburg reported no relevant financial conflicts.
Blacks Using IVF Face Greatest Preterm Birth Risk
MINNEAPOLIS – Black women who conceive using in vitro fertilization are at a markedly increased risk of any type of preterm birth, compared with other races, a retrospective cohort study indicates.
Hispanic women had a significantly lower rate of preterm births than did black women, and similar or slightly higher rates than did white women.
Native American women were not at an increased risk of any type of preterm birth, compared with whites, whereas Asians were at a reduced risk of preterm twin births.
"There exist notable racial and ethnic disparities in preterm births in infants conceived by IVF, with the highest rate in black women," Dr. Xu Xiong of the school of public health and tropical medicine at Tulane University in New Orleans reported at the annual meeting of the Society for Pediatric and Perinatal Epidemiologic Research.
Racial disparities in preterm birth may reflect biological differences resulting from genetic background or from variations in social demographics, socioeconomic status (SES), environmental exposures, lifestyles, cultural factors, and access to care and treatment, he said. SES factors (such as income, education, and occupation) were not available in the data set, although all of the women were able to finance expensive and time-consuming IVF treatment.
"In this study of relatively higher income women [who] conceived by IVF, our findings of an even greater difference in preterm births between black and white women than in the general population indicate that SES may not be as solely important a determinant for the racial gaps of preterm birth than previously postulated," Dr. Xiong said in an interview.
The investigators conducted a retrospective cohort study of 56,465 singleton and 23,748 twin pregnancies resulting from fresh nondonor IVF cycles in 82,519 women, using 2006-2008 data from the SART CORS (Society for Assisted Reproductive Technology Clinic Outcome Reporting System).
Among singleton births, 3.3% of black women had a very early preterm birth at less than 28 weeks, compared with 0.7% of white women, 1% of Hispanics, 0.7% of Asians, and 1% of Native Americans (P less than .05).
The pattern was similar for early preterm birth at less than 32 weeks (5.8% vs. 1.6%, 2.2%, 1.4%, and 1.4%, respectively), and for preterm birth at less than 37 weeks (13.3% vs. 6.6%, 8%, 6%, and 8%, respectively) (both P less than .05), Dr. Xiong reported.
In multivariate analysis with adjustment for confounding variables including maternal age; gravida status; smoking status; day of embryo transfer; number of embryos transferred; number of gestational sacs with heart rate; body mass index; prior spontaneous abortions; and infertility diagnosis, black women remained at significantly increased risk of very early preterm birth (odds ratio, 4.5), early preterm birth (OR, 3.7) and preterm birth (OR, 2.0), compared with white women (all P less than .05).
As expected, twin pregnancies increased preterm births for all groups, but once again, blacks had the highest rate of very early preterm birth at 7.7%, compared with 2.5% of whites, 3.7% of Hispanics, 2.3% of Asians, and 3% of Native Americans (P less than .05), he said.
Rates were also significantly higher for black women for early preterm twin birth (13.6% vs. 6.6%, 7%, 5.8%, and 5.8%, respectively) and for preterm twin birth (46.5% vs. 37.6%, 37.5%, 33%, and 41%, respectively; P less than .05).
In the adjusted analysis, black women delivering twins had a significantly increased risk of very early preterm twin births (OR, 3.3), early preterm birth (OR, 2.2) and preterm birth (OR, 1.4), compared with whites (P less than .05), reported Dr. Xiong and his coauthors.
At baseline, black women were more likely to be at least 40 years of age than were whites, Hispanics, Asians, and Native Americans (10.3% vs. 7.4%, 6.3%, 6.7%, and 6.6%, respectively), more likely to be obese (14.6%, 7.5%, 7.5%, 3%, and 9.5%, respectively), and more likely to report a prior preterm birth (69% vs. 59%, 60%, 58%, and 55.4%, respectively).
Roughly 7% of blacks and Native Americans and 6% of Asians smoked, compared with nearly 10% of white and Hispanic mothers. The majority of all women (57%) had two fresh embryos transferred, and 63.5% reported no prior use of IVF/assisted reproductive technology, with rates comparable across racial groups.
Dr. Xiong and his coauthors reported no conflicts of interest.
MINNEAPOLIS – Black women who conceive using in vitro fertilization are at a markedly increased risk of any type of preterm birth, compared with other races, a retrospective cohort study indicates.
Hispanic women had a significantly lower rate of preterm births than did black women, and similar or slightly higher rates than did white women.
Native American women were not at an increased risk of any type of preterm birth, compared with whites, whereas Asians were at a reduced risk of preterm twin births.
"There exist notable racial and ethnic disparities in preterm births in infants conceived by IVF, with the highest rate in black women," Dr. Xu Xiong of the school of public health and tropical medicine at Tulane University in New Orleans reported at the annual meeting of the Society for Pediatric and Perinatal Epidemiologic Research.
Racial disparities in preterm birth may reflect biological differences resulting from genetic background or from variations in social demographics, socioeconomic status (SES), environmental exposures, lifestyles, cultural factors, and access to care and treatment, he said. SES factors (such as income, education, and occupation) were not available in the data set, although all of the women were able to finance expensive and time-consuming IVF treatment.
"In this study of relatively higher income women [who] conceived by IVF, our findings of an even greater difference in preterm births between black and white women than in the general population indicate that SES may not be as solely important a determinant for the racial gaps of preterm birth than previously postulated," Dr. Xiong said in an interview.
The investigators conducted a retrospective cohort study of 56,465 singleton and 23,748 twin pregnancies resulting from fresh nondonor IVF cycles in 82,519 women, using 2006-2008 data from the SART CORS (Society for Assisted Reproductive Technology Clinic Outcome Reporting System).
Among singleton births, 3.3% of black women had a very early preterm birth at less than 28 weeks, compared with 0.7% of white women, 1% of Hispanics, 0.7% of Asians, and 1% of Native Americans (P less than .05).
The pattern was similar for early preterm birth at less than 32 weeks (5.8% vs. 1.6%, 2.2%, 1.4%, and 1.4%, respectively), and for preterm birth at less than 37 weeks (13.3% vs. 6.6%, 8%, 6%, and 8%, respectively) (both P less than .05), Dr. Xiong reported.
In multivariate analysis with adjustment for confounding variables including maternal age; gravida status; smoking status; day of embryo transfer; number of embryos transferred; number of gestational sacs with heart rate; body mass index; prior spontaneous abortions; and infertility diagnosis, black women remained at significantly increased risk of very early preterm birth (odds ratio, 4.5), early preterm birth (OR, 3.7) and preterm birth (OR, 2.0), compared with white women (all P less than .05).
As expected, twin pregnancies increased preterm births for all groups, but once again, blacks had the highest rate of very early preterm birth at 7.7%, compared with 2.5% of whites, 3.7% of Hispanics, 2.3% of Asians, and 3% of Native Americans (P less than .05), he said.
Rates were also significantly higher for black women for early preterm twin birth (13.6% vs. 6.6%, 7%, 5.8%, and 5.8%, respectively) and for preterm twin birth (46.5% vs. 37.6%, 37.5%, 33%, and 41%, respectively; P less than .05).
In the adjusted analysis, black women delivering twins had a significantly increased risk of very early preterm twin births (OR, 3.3), early preterm birth (OR, 2.2) and preterm birth (OR, 1.4), compared with whites (P less than .05), reported Dr. Xiong and his coauthors.
At baseline, black women were more likely to be at least 40 years of age than were whites, Hispanics, Asians, and Native Americans (10.3% vs. 7.4%, 6.3%, 6.7%, and 6.6%, respectively), more likely to be obese (14.6%, 7.5%, 7.5%, 3%, and 9.5%, respectively), and more likely to report a prior preterm birth (69% vs. 59%, 60%, 58%, and 55.4%, respectively).
Roughly 7% of blacks and Native Americans and 6% of Asians smoked, compared with nearly 10% of white and Hispanic mothers. The majority of all women (57%) had two fresh embryos transferred, and 63.5% reported no prior use of IVF/assisted reproductive technology, with rates comparable across racial groups.
Dr. Xiong and his coauthors reported no conflicts of interest.
MINNEAPOLIS – Black women who conceive using in vitro fertilization are at a markedly increased risk of any type of preterm birth, compared with other races, a retrospective cohort study indicates.
Hispanic women had a significantly lower rate of preterm births than did black women, and similar or slightly higher rates than did white women.
Native American women were not at an increased risk of any type of preterm birth, compared with whites, whereas Asians were at a reduced risk of preterm twin births.
"There exist notable racial and ethnic disparities in preterm births in infants conceived by IVF, with the highest rate in black women," Dr. Xu Xiong of the school of public health and tropical medicine at Tulane University in New Orleans reported at the annual meeting of the Society for Pediatric and Perinatal Epidemiologic Research.
Racial disparities in preterm birth may reflect biological differences resulting from genetic background or from variations in social demographics, socioeconomic status (SES), environmental exposures, lifestyles, cultural factors, and access to care and treatment, he said. SES factors (such as income, education, and occupation) were not available in the data set, although all of the women were able to finance expensive and time-consuming IVF treatment.
"In this study of relatively higher income women [who] conceived by IVF, our findings of an even greater difference in preterm births between black and white women than in the general population indicate that SES may not be as solely important a determinant for the racial gaps of preterm birth than previously postulated," Dr. Xiong said in an interview.
The investigators conducted a retrospective cohort study of 56,465 singleton and 23,748 twin pregnancies resulting from fresh nondonor IVF cycles in 82,519 women, using 2006-2008 data from the SART CORS (Society for Assisted Reproductive Technology Clinic Outcome Reporting System).
Among singleton births, 3.3% of black women had a very early preterm birth at less than 28 weeks, compared with 0.7% of white women, 1% of Hispanics, 0.7% of Asians, and 1% of Native Americans (P less than .05).
The pattern was similar for early preterm birth at less than 32 weeks (5.8% vs. 1.6%, 2.2%, 1.4%, and 1.4%, respectively), and for preterm birth at less than 37 weeks (13.3% vs. 6.6%, 8%, 6%, and 8%, respectively) (both P less than .05), Dr. Xiong reported.
In multivariate analysis with adjustment for confounding variables including maternal age; gravida status; smoking status; day of embryo transfer; number of embryos transferred; number of gestational sacs with heart rate; body mass index; prior spontaneous abortions; and infertility diagnosis, black women remained at significantly increased risk of very early preterm birth (odds ratio, 4.5), early preterm birth (OR, 3.7) and preterm birth (OR, 2.0), compared with white women (all P less than .05).
As expected, twin pregnancies increased preterm births for all groups, but once again, blacks had the highest rate of very early preterm birth at 7.7%, compared with 2.5% of whites, 3.7% of Hispanics, 2.3% of Asians, and 3% of Native Americans (P less than .05), he said.
Rates were also significantly higher for black women for early preterm twin birth (13.6% vs. 6.6%, 7%, 5.8%, and 5.8%, respectively) and for preterm twin birth (46.5% vs. 37.6%, 37.5%, 33%, and 41%, respectively; P less than .05).
In the adjusted analysis, black women delivering twins had a significantly increased risk of very early preterm twin births (OR, 3.3), early preterm birth (OR, 2.2) and preterm birth (OR, 1.4), compared with whites (P less than .05), reported Dr. Xiong and his coauthors.
At baseline, black women were more likely to be at least 40 years of age than were whites, Hispanics, Asians, and Native Americans (10.3% vs. 7.4%, 6.3%, 6.7%, and 6.6%, respectively), more likely to be obese (14.6%, 7.5%, 7.5%, 3%, and 9.5%, respectively), and more likely to report a prior preterm birth (69% vs. 59%, 60%, 58%, and 55.4%, respectively).
Roughly 7% of blacks and Native Americans and 6% of Asians smoked, compared with nearly 10% of white and Hispanic mothers. The majority of all women (57%) had two fresh embryos transferred, and 63.5% reported no prior use of IVF/assisted reproductive technology, with rates comparable across racial groups.
Dr. Xiong and his coauthors reported no conflicts of interest.
AT THE ANNUAL MEETING OF THE SOCIETY FOR PEDIATRIC AND PERINATAL EPIDEMIOLOGIC RESEARCH
Two Fastidious Bacteria Linked to Pelvic Inflammatory Disease
MINNEAPOLIS – Evidence suggests that two novel fastidious bacteria linked to bacterial vaginosis are also associated with pelvic inflammatory disease.
Ureaplasma urealyticum biovar 2 (UU-2) and Leptotrichia sanguiengens/Leptotrichia amnionii (LS/LA) were significantly associated with PID after adjustment for age, race, chlamydia, and gonorrhea.
Ureaplasma parvum (UP), however, was not associated with PID in a substudy of women participating in the PEACH (PID Evaluation and Clinical Health) study.
"This is the first study to demonstrate that [LS/LA] and UU-2, but not UP, are associated with PID," lead author Catherine Haggerty, Ph.D., said at the annual meeting of the Society for Pediatric and Perinatal Epidemiologic Research.
The results are consistent with studies showing that UU-2 is associated with nongonococcal urethritis in men, whereas UP is not. UU-2 and UP, also known as biovar 1, were recently designated as two distinct biovars. UP has not been consistently associated with bacterial vaginosis (BV) or PID.
The investigators used polymerase chain reaction (PCR) to measure select BV-associated, fastidious bacteria in cervical and endometrial specimens from 607 of 831 women recruited from emergency department and outpatient clinics during 1996-1999 for PEACH. The multicenter, randomized study compared the effectiveness of inpatient and outpatient treatment for PID.
The PEACH cohort was largely (75%) African-American, 40% were aged 20-24 years, half had an upper genital infection or inflammation, and 35% had gonorrhea or chlamydia.
Among the women in the subset, 22% had LS/LA only, 17% UP, 4% UU-2, 46% were coinfected with two or more bacteria, and 11% had no infection, said Dr. Haggerty, a reproductive epidemiologist with the University of Pittsburgh.
In adjusted logistic regression analysis, women who tested positive for LS/LA, UP, or UU-2 in the lower genital tract (cervix) were approximately 10, 13, and 20 times as likely, respectively, to test positive in the upper genital tract (endometrium).
Contamination during sampling is one possible explanation, but "still, the data provide intriguing evidence that there may be an upward transmission of these bacteria that may lead to the development of [PID]," she said.
Indeed, the likelihood of a woman having endometritis was significantly increased if she tested positive for UU-2 (adjusted odds ratio, 1.4) or LS/LA (OR, 2.2) in the endometrium, but not UP (OR, 0.8).
Among those women without gonorrheal or chlamydial infection, the risk of PID (histologically confirmed endometritis) was further increased with UU-2 (OR, 2.5) and LS/LA (OR, 2.7), but not UP (OR, 0.8).
The results may be important in guiding PID treatment, which currently consists of broad-spectrum antibiotics that may not target all the bacteria associated with the disorder, Dr. Haggerty said. UU-2 expresses tetracycline resistance in up to 45% of patients, while antimicrobial resistance to Leptotrichia is largely unknown because of the difficulty in culturing fastidious bacteria in vitro.
In addition, resistance to vaginal metronidazole has been reported among pregnant women with BV who carry the Leptotrichia or Sneathia species or BV-associated bacterium 1 (BVAB1) (BMC Infect. Dis. 2009;9:89). Metronidazole is a mainstay of BV treatment, but the Centers for Disease Control and Prevention still lists it as optional for PID, despite the frequent coexistence of the two conditions, Dr. Haggerty said.
"Studies are needed to determine treatment of these bacteria in general, as well as among PID patients," she said.
During a discussion of the study, an audience member questioned whether PCR is taking over as the diagnostic criterion for PID because many of the bacteria cannot be identified without it. Dr. Haggerty replied that we are moving in that direction, as a result of the "landmark study" by Dr. David Fredricks et al., reporting high sensitivities and specificities for several bacteria or combinations of bacteria identified using targeted PCR versus the Amsel (clinical) or Nugent (Gram stain) criteria (J. Clin. Microbiol. 2007;45:3270-6).
Dr. Haggerty and her coauthors reported no conflicts of interest. The substudy was funded by the National Institutes of Health/National Institute of Allergy and Infectious Diseases. PEACH was funded by the Agency for Health Care Policy and Research, now known as the Agency for Healthcare Research and Quality.
MINNEAPOLIS – Evidence suggests that two novel fastidious bacteria linked to bacterial vaginosis are also associated with pelvic inflammatory disease.
Ureaplasma urealyticum biovar 2 (UU-2) and Leptotrichia sanguiengens/Leptotrichia amnionii (LS/LA) were significantly associated with PID after adjustment for age, race, chlamydia, and gonorrhea.
Ureaplasma parvum (UP), however, was not associated with PID in a substudy of women participating in the PEACH (PID Evaluation and Clinical Health) study.
"This is the first study to demonstrate that [LS/LA] and UU-2, but not UP, are associated with PID," lead author Catherine Haggerty, Ph.D., said at the annual meeting of the Society for Pediatric and Perinatal Epidemiologic Research.
The results are consistent with studies showing that UU-2 is associated with nongonococcal urethritis in men, whereas UP is not. UU-2 and UP, also known as biovar 1, were recently designated as two distinct biovars. UP has not been consistently associated with bacterial vaginosis (BV) or PID.
The investigators used polymerase chain reaction (PCR) to measure select BV-associated, fastidious bacteria in cervical and endometrial specimens from 607 of 831 women recruited from emergency department and outpatient clinics during 1996-1999 for PEACH. The multicenter, randomized study compared the effectiveness of inpatient and outpatient treatment for PID.
The PEACH cohort was largely (75%) African-American, 40% were aged 20-24 years, half had an upper genital infection or inflammation, and 35% had gonorrhea or chlamydia.
Among the women in the subset, 22% had LS/LA only, 17% UP, 4% UU-2, 46% were coinfected with two or more bacteria, and 11% had no infection, said Dr. Haggerty, a reproductive epidemiologist with the University of Pittsburgh.
In adjusted logistic regression analysis, women who tested positive for LS/LA, UP, or UU-2 in the lower genital tract (cervix) were approximately 10, 13, and 20 times as likely, respectively, to test positive in the upper genital tract (endometrium).
Contamination during sampling is one possible explanation, but "still, the data provide intriguing evidence that there may be an upward transmission of these bacteria that may lead to the development of [PID]," she said.
Indeed, the likelihood of a woman having endometritis was significantly increased if she tested positive for UU-2 (adjusted odds ratio, 1.4) or LS/LA (OR, 2.2) in the endometrium, but not UP (OR, 0.8).
Among those women without gonorrheal or chlamydial infection, the risk of PID (histologically confirmed endometritis) was further increased with UU-2 (OR, 2.5) and LS/LA (OR, 2.7), but not UP (OR, 0.8).
The results may be important in guiding PID treatment, which currently consists of broad-spectrum antibiotics that may not target all the bacteria associated with the disorder, Dr. Haggerty said. UU-2 expresses tetracycline resistance in up to 45% of patients, while antimicrobial resistance to Leptotrichia is largely unknown because of the difficulty in culturing fastidious bacteria in vitro.
In addition, resistance to vaginal metronidazole has been reported among pregnant women with BV who carry the Leptotrichia or Sneathia species or BV-associated bacterium 1 (BVAB1) (BMC Infect. Dis. 2009;9:89). Metronidazole is a mainstay of BV treatment, but the Centers for Disease Control and Prevention still lists it as optional for PID, despite the frequent coexistence of the two conditions, Dr. Haggerty said.
"Studies are needed to determine treatment of these bacteria in general, as well as among PID patients," she said.
During a discussion of the study, an audience member questioned whether PCR is taking over as the diagnostic criterion for PID because many of the bacteria cannot be identified without it. Dr. Haggerty replied that we are moving in that direction, as a result of the "landmark study" by Dr. David Fredricks et al., reporting high sensitivities and specificities for several bacteria or combinations of bacteria identified using targeted PCR versus the Amsel (clinical) or Nugent (Gram stain) criteria (J. Clin. Microbiol. 2007;45:3270-6).
Dr. Haggerty and her coauthors reported no conflicts of interest. The substudy was funded by the National Institutes of Health/National Institute of Allergy and Infectious Diseases. PEACH was funded by the Agency for Health Care Policy and Research, now known as the Agency for Healthcare Research and Quality.
MINNEAPOLIS – Evidence suggests that two novel fastidious bacteria linked to bacterial vaginosis are also associated with pelvic inflammatory disease.
Ureaplasma urealyticum biovar 2 (UU-2) and Leptotrichia sanguiengens/Leptotrichia amnionii (LS/LA) were significantly associated with PID after adjustment for age, race, chlamydia, and gonorrhea.
Ureaplasma parvum (UP), however, was not associated with PID in a substudy of women participating in the PEACH (PID Evaluation and Clinical Health) study.
"This is the first study to demonstrate that [LS/LA] and UU-2, but not UP, are associated with PID," lead author Catherine Haggerty, Ph.D., said at the annual meeting of the Society for Pediatric and Perinatal Epidemiologic Research.
The results are consistent with studies showing that UU-2 is associated with nongonococcal urethritis in men, whereas UP is not. UU-2 and UP, also known as biovar 1, were recently designated as two distinct biovars. UP has not been consistently associated with bacterial vaginosis (BV) or PID.
The investigators used polymerase chain reaction (PCR) to measure select BV-associated, fastidious bacteria in cervical and endometrial specimens from 607 of 831 women recruited from emergency department and outpatient clinics during 1996-1999 for PEACH. The multicenter, randomized study compared the effectiveness of inpatient and outpatient treatment for PID.
The PEACH cohort was largely (75%) African-American, 40% were aged 20-24 years, half had an upper genital infection or inflammation, and 35% had gonorrhea or chlamydia.
Among the women in the subset, 22% had LS/LA only, 17% UP, 4% UU-2, 46% were coinfected with two or more bacteria, and 11% had no infection, said Dr. Haggerty, a reproductive epidemiologist with the University of Pittsburgh.
In adjusted logistic regression analysis, women who tested positive for LS/LA, UP, or UU-2 in the lower genital tract (cervix) were approximately 10, 13, and 20 times as likely, respectively, to test positive in the upper genital tract (endometrium).
Contamination during sampling is one possible explanation, but "still, the data provide intriguing evidence that there may be an upward transmission of these bacteria that may lead to the development of [PID]," she said.
Indeed, the likelihood of a woman having endometritis was significantly increased if she tested positive for UU-2 (adjusted odds ratio, 1.4) or LS/LA (OR, 2.2) in the endometrium, but not UP (OR, 0.8).
Among those women without gonorrheal or chlamydial infection, the risk of PID (histologically confirmed endometritis) was further increased with UU-2 (OR, 2.5) and LS/LA (OR, 2.7), but not UP (OR, 0.8).
The results may be important in guiding PID treatment, which currently consists of broad-spectrum antibiotics that may not target all the bacteria associated with the disorder, Dr. Haggerty said. UU-2 expresses tetracycline resistance in up to 45% of patients, while antimicrobial resistance to Leptotrichia is largely unknown because of the difficulty in culturing fastidious bacteria in vitro.
In addition, resistance to vaginal metronidazole has been reported among pregnant women with BV who carry the Leptotrichia or Sneathia species or BV-associated bacterium 1 (BVAB1) (BMC Infect. Dis. 2009;9:89). Metronidazole is a mainstay of BV treatment, but the Centers for Disease Control and Prevention still lists it as optional for PID, despite the frequent coexistence of the two conditions, Dr. Haggerty said.
"Studies are needed to determine treatment of these bacteria in general, as well as among PID patients," she said.
During a discussion of the study, an audience member questioned whether PCR is taking over as the diagnostic criterion for PID because many of the bacteria cannot be identified without it. Dr. Haggerty replied that we are moving in that direction, as a result of the "landmark study" by Dr. David Fredricks et al., reporting high sensitivities and specificities for several bacteria or combinations of bacteria identified using targeted PCR versus the Amsel (clinical) or Nugent (Gram stain) criteria (J. Clin. Microbiol. 2007;45:3270-6).
Dr. Haggerty and her coauthors reported no conflicts of interest. The substudy was funded by the National Institutes of Health/National Institute of Allergy and Infectious Diseases. PEACH was funded by the Agency for Health Care Policy and Research, now known as the Agency for Healthcare Research and Quality.
AT THE ANNUAL MEETING OF THE SOCIETY FOR PEDIATRIC AND PERINATAL EPIDEMIOLOGIC RESEARCH
Obesity Especially Impairs Fertility in Black Women
MINNEAPOLIS – Young black women who are obese or heavy through the hips were less likely to become pregnant, according to a substudy of the ongoing, prospective Black Women’s Health Study.
Fecundity was significantly reduced in a dose-response fashion for women who were overweight (fecundity ratio, 0.89), obese (FR, 0.75) and very obese (FR, 0.68) after adjustment for age, education, smoking history, alcohol intake, physical activity, parity, region, and waist-to-hip ratio.
A large waist-to-hip ratio (defined as 0.8 or greater), also was significantly associated with lower fecundity (FR, 0.73), with fecundity ratios less than 1 indicating reduced fecundity or longer time to pregnancy (TTP).
"Overall and central adiposity are associated with reduced fecundability in black women," Lauren Wise, Sc.D., said at the annual meeting of the Society for Pediatric and Perinatal Epidemiologic Research.
The substudy is the first TTP study in black women, and its results largely agree with previous studies consistently linking high body mass index and reduced fertility in white women.
Little is known about the determinants of fertility in black women, who are disproportionately affected by the obesity epidemic in the United States. Studies of central adiposity and fertility in whites have been inconclusive, with some suggesting that adiposity may interfere with estrogen metabolism, increase insulin resistance, and change the quality and pH of cervical mucus, said Dr. Wise of the Slone Epidemiology Center at Boston University.
The substudy cohort was drawn from 59,000 women in the Black Women’s Health Study, the largest study of U.S. black women’s health yet conducted and now in its 17th year of follow-up. A total of 15,500 women completed a Web-based survey in 2011 reporting the TTP for each planned pregnancy. There were 10,272 births, of which only 4,315 births (43%) were planned. The researchers excluded both the unplanned pregnancies and women who had incomplete data, a history of infertility, and age older than 40 years either in 1995 or while they attempted pregnancy; the final sample included 2,084 births and 209 unsuccessful pregnancy attempts among 1,706 women, aged 21-40 years.
The average age was 34 years for all BMI groups including those classified as overweight (BMI, 25-29 kg/m2), obese (BMI, 30-34) and very obese (BMI, 35 or greater).
BMI was inversely associated with education and vigorous exercise, and was positively associated with waist-to-hip ratio, waist circumference, and current smoking status, reported Dr. Wise and her colleagues.
After adjusting for all previous covariates plus BMI, researchers found that a waist circumference of 33-35 inches – but not beyond – was significantly associated with lower fecundity.
Fecundity was not lower in women who were underweight (BMI less than 18.5; FR, 1.11).
During a discussion of the results, one attendee pointed out that asking participants about marital status, which the investigators did, is not the same as asking about relationship status or frequency of intercourse.
Another audience member observed that male obesity is proving to be just as important as female obesity in terms of a couple’s inability to conceive.
Indeed, a recent systematic review involving 14 studies and 9,779 men reported that overweight and obese men are at increased risk of oligozoospermia or azoospermia, compared with normal-weight men (Arch. Intern. Med. 2012;172:440-2). Possible hypotheses for this relationship include hypogonadotropic hyperestrogenic hypogonadism due to aromatization of steroids in estrogens in peripheral tissue; direct alterations of spermatogenesis and Sertoli cell function; hip, abdominal and scrotal fat-tissue accumulation, leading to increased scrotal temperature; and accumulation of toxins and liposoluble endocrine disruptors in fatty tissue.
The analysis and the Black Women’s Health Study are sponsored by the National Institutes of Health. Dr. Wise and her coauthors reported no disclosures.
MINNEAPOLIS – Young black women who are obese or heavy through the hips were less likely to become pregnant, according to a substudy of the ongoing, prospective Black Women’s Health Study.
Fecundity was significantly reduced in a dose-response fashion for women who were overweight (fecundity ratio, 0.89), obese (FR, 0.75) and very obese (FR, 0.68) after adjustment for age, education, smoking history, alcohol intake, physical activity, parity, region, and waist-to-hip ratio.
A large waist-to-hip ratio (defined as 0.8 or greater), also was significantly associated with lower fecundity (FR, 0.73), with fecundity ratios less than 1 indicating reduced fecundity or longer time to pregnancy (TTP).
"Overall and central adiposity are associated with reduced fecundability in black women," Lauren Wise, Sc.D., said at the annual meeting of the Society for Pediatric and Perinatal Epidemiologic Research.
The substudy is the first TTP study in black women, and its results largely agree with previous studies consistently linking high body mass index and reduced fertility in white women.
Little is known about the determinants of fertility in black women, who are disproportionately affected by the obesity epidemic in the United States. Studies of central adiposity and fertility in whites have been inconclusive, with some suggesting that adiposity may interfere with estrogen metabolism, increase insulin resistance, and change the quality and pH of cervical mucus, said Dr. Wise of the Slone Epidemiology Center at Boston University.
The substudy cohort was drawn from 59,000 women in the Black Women’s Health Study, the largest study of U.S. black women’s health yet conducted and now in its 17th year of follow-up. A total of 15,500 women completed a Web-based survey in 2011 reporting the TTP for each planned pregnancy. There were 10,272 births, of which only 4,315 births (43%) were planned. The researchers excluded both the unplanned pregnancies and women who had incomplete data, a history of infertility, and age older than 40 years either in 1995 or while they attempted pregnancy; the final sample included 2,084 births and 209 unsuccessful pregnancy attempts among 1,706 women, aged 21-40 years.
The average age was 34 years for all BMI groups including those classified as overweight (BMI, 25-29 kg/m2), obese (BMI, 30-34) and very obese (BMI, 35 or greater).
BMI was inversely associated with education and vigorous exercise, and was positively associated with waist-to-hip ratio, waist circumference, and current smoking status, reported Dr. Wise and her colleagues.
After adjusting for all previous covariates plus BMI, researchers found that a waist circumference of 33-35 inches – but not beyond – was significantly associated with lower fecundity.
Fecundity was not lower in women who were underweight (BMI less than 18.5; FR, 1.11).
During a discussion of the results, one attendee pointed out that asking participants about marital status, which the investigators did, is not the same as asking about relationship status or frequency of intercourse.
Another audience member observed that male obesity is proving to be just as important as female obesity in terms of a couple’s inability to conceive.
Indeed, a recent systematic review involving 14 studies and 9,779 men reported that overweight and obese men are at increased risk of oligozoospermia or azoospermia, compared with normal-weight men (Arch. Intern. Med. 2012;172:440-2). Possible hypotheses for this relationship include hypogonadotropic hyperestrogenic hypogonadism due to aromatization of steroids in estrogens in peripheral tissue; direct alterations of spermatogenesis and Sertoli cell function; hip, abdominal and scrotal fat-tissue accumulation, leading to increased scrotal temperature; and accumulation of toxins and liposoluble endocrine disruptors in fatty tissue.
The analysis and the Black Women’s Health Study are sponsored by the National Institutes of Health. Dr. Wise and her coauthors reported no disclosures.
MINNEAPOLIS – Young black women who are obese or heavy through the hips were less likely to become pregnant, according to a substudy of the ongoing, prospective Black Women’s Health Study.
Fecundity was significantly reduced in a dose-response fashion for women who were overweight (fecundity ratio, 0.89), obese (FR, 0.75) and very obese (FR, 0.68) after adjustment for age, education, smoking history, alcohol intake, physical activity, parity, region, and waist-to-hip ratio.
A large waist-to-hip ratio (defined as 0.8 or greater), also was significantly associated with lower fecundity (FR, 0.73), with fecundity ratios less than 1 indicating reduced fecundity or longer time to pregnancy (TTP).
"Overall and central adiposity are associated with reduced fecundability in black women," Lauren Wise, Sc.D., said at the annual meeting of the Society for Pediatric and Perinatal Epidemiologic Research.
The substudy is the first TTP study in black women, and its results largely agree with previous studies consistently linking high body mass index and reduced fertility in white women.
Little is known about the determinants of fertility in black women, who are disproportionately affected by the obesity epidemic in the United States. Studies of central adiposity and fertility in whites have been inconclusive, with some suggesting that adiposity may interfere with estrogen metabolism, increase insulin resistance, and change the quality and pH of cervical mucus, said Dr. Wise of the Slone Epidemiology Center at Boston University.
The substudy cohort was drawn from 59,000 women in the Black Women’s Health Study, the largest study of U.S. black women’s health yet conducted and now in its 17th year of follow-up. A total of 15,500 women completed a Web-based survey in 2011 reporting the TTP for each planned pregnancy. There were 10,272 births, of which only 4,315 births (43%) were planned. The researchers excluded both the unplanned pregnancies and women who had incomplete data, a history of infertility, and age older than 40 years either in 1995 or while they attempted pregnancy; the final sample included 2,084 births and 209 unsuccessful pregnancy attempts among 1,706 women, aged 21-40 years.
The average age was 34 years for all BMI groups including those classified as overweight (BMI, 25-29 kg/m2), obese (BMI, 30-34) and very obese (BMI, 35 or greater).
BMI was inversely associated with education and vigorous exercise, and was positively associated with waist-to-hip ratio, waist circumference, and current smoking status, reported Dr. Wise and her colleagues.
After adjusting for all previous covariates plus BMI, researchers found that a waist circumference of 33-35 inches – but not beyond – was significantly associated with lower fecundity.
Fecundity was not lower in women who were underweight (BMI less than 18.5; FR, 1.11).
During a discussion of the results, one attendee pointed out that asking participants about marital status, which the investigators did, is not the same as asking about relationship status or frequency of intercourse.
Another audience member observed that male obesity is proving to be just as important as female obesity in terms of a couple’s inability to conceive.
Indeed, a recent systematic review involving 14 studies and 9,779 men reported that overweight and obese men are at increased risk of oligozoospermia or azoospermia, compared with normal-weight men (Arch. Intern. Med. 2012;172:440-2). Possible hypotheses for this relationship include hypogonadotropic hyperestrogenic hypogonadism due to aromatization of steroids in estrogens in peripheral tissue; direct alterations of spermatogenesis and Sertoli cell function; hip, abdominal and scrotal fat-tissue accumulation, leading to increased scrotal temperature; and accumulation of toxins and liposoluble endocrine disruptors in fatty tissue.
The analysis and the Black Women’s Health Study are sponsored by the National Institutes of Health. Dr. Wise and her coauthors reported no disclosures.
AT THE ANNUAL MEETING OF THE SOCIETY FOR PEDIATRIC AND PERINATAL EPIDEMIOLOGIC RESEARCH
Major Finding: Fecundity was significantly reduced in women who were overweight (FR, 0.89), obese (FR, 0.75) and very obese (FR, 0.68), even after adjustment for important confounders.
Data Source: This was a retrospective analysis of 1,706 women attempting pregnancy in the prospective Black Women’s Health Study.
Disclosures: The analysis and the Black Women’s Health Study are sponsored by the National Institutes of Health. Dr. Wise and her coauthors reported no disclosures.
Probiotic Prescribing Skyrockets for Pediatric Gastroenteritis
COVINGTON, KY. – A multifaceted intervention propelled probiotic prescriptions within 18 hours of admission from 1% to 100% among children admitted for acute gastroenteritis with diarrhea.
This was true regardless of their insurance status.
Moreover, the 100% prescribing rate was achieved within 6 weeks and has been sustained for 7 months, lead author Dr. Michelle Parker reported at Pediatric Hospital Medicine 2012.
"It’s definitely become culture," she said during the poster presentation.
A multidisciplinary team of hospital medicine attending physicians, nurse representative, and a research assistant at Cincinnati Children’s Hospital identified six key drivers they felt would increase inpatient prescribing of Lactobacillus rhamnosus GG (LGG) at admission. They were identification of eligible patients; adequate staff knowledge; prescriber buy-in; available and appropriate administration of LGG; immediate response to failure of prescribing; and process standardization.
One of the biggest game changers was to incorporate LGG as a default order within the acute gastroenteritis electronic order set, with the appropriate dose and frequency preselected, Dr. Parker said. The default order did not just happen, without the physician being aware, as prescribing physicians still had to click, enter LGG, and save the indication for its use.
The second key element was monitoring the electronic medical records each weekday for children with acute gastroenteritis, aged 2 months to 18 years, who were not prescribed LGG, and e-mailing their care team.
"We engaged them in a dialogue, not told them they had to [prescribe]," said Dr. Parker, with Cincinnati Children’s division of hospital medicine. "That gave them a chance to prescribe it if that was their intention and it was just forgotten, and it was also a good chance to further the education."
Education included reviewing the evidence on LGG and appropriate prescribing with hospital medicine attending physicians, residents and medical students, brief monthly reminders to residents and a campaign to private pediatricians with admitting privileges that included electronic information and signage in key areas of the hospital.
Before the intervention, however, the hospital had published its own evidence-based guideline in 2007, recommending consideration of probiotics. A Cochrane review of 63 studies in 8,014 infants and young children had also been published, showing that probiotics were safe and had a clear benefit in reducing the duration of diarrhea, although the size of the effect varied between studies (Cochrane Database Syst. Rev. 2010 [doi:10.1002/14651858.CD003048.pub3]).
So why then did the hospital have a 1% preintervention prescribing rate?
Dr. Parker admits the 1% rate is "far less than ideal" but said other hospitals are likely in the same predicament because it’s very hard for people to put evidence and guidelines into practice.
"I think this is all around the country," she said. "There’s evidence that it takes 17 years of solid evidence to change practice, for it to become the expert recommendation."
The intervention also removed a logistic barrier, with the help of its pharmacy, which began supplying the community hospital inpatient unit with LGG, specifically adult Culturelle because it has the most evidence behind it, she said.
The labor-intensive identification and mitigation process was discontinued after the system stabilized and the focus of the initiative shifted more towards shared decision-making with families.
"Instead of saying you have to do this in all kids, we tell them it’s something they have to pay for out of pocket and that it’s a modest benefit of 24 hours of less stool," Dr. Parker said. "So, is that something you’re interested in doing?"
A separate analysis found that there was no difference in prescription fill rates based on insurance status. One explanation for this is that the pharmacy will dispense only the number of capsules prescribed, rather than having families pay for the entire bottle, which can cost between $17 and $30, she said.
The chart review excluded children with known or presumed bacterial gastroenteritis, major comorbid conditions, and former premature infants not yet 2 months corrected gestational age. Specific demographics on the cohort were not provided.
The authors acknowledged that the James M. Anderson Center for Health Systems Excellence in Cincinnati collaborated in the project.
COVINGTON, KY. – A multifaceted intervention propelled probiotic prescriptions within 18 hours of admission from 1% to 100% among children admitted for acute gastroenteritis with diarrhea.
This was true regardless of their insurance status.
Moreover, the 100% prescribing rate was achieved within 6 weeks and has been sustained for 7 months, lead author Dr. Michelle Parker reported at Pediatric Hospital Medicine 2012.
"It’s definitely become culture," she said during the poster presentation.
A multidisciplinary team of hospital medicine attending physicians, nurse representative, and a research assistant at Cincinnati Children’s Hospital identified six key drivers they felt would increase inpatient prescribing of Lactobacillus rhamnosus GG (LGG) at admission. They were identification of eligible patients; adequate staff knowledge; prescriber buy-in; available and appropriate administration of LGG; immediate response to failure of prescribing; and process standardization.
One of the biggest game changers was to incorporate LGG as a default order within the acute gastroenteritis electronic order set, with the appropriate dose and frequency preselected, Dr. Parker said. The default order did not just happen, without the physician being aware, as prescribing physicians still had to click, enter LGG, and save the indication for its use.
The second key element was monitoring the electronic medical records each weekday for children with acute gastroenteritis, aged 2 months to 18 years, who were not prescribed LGG, and e-mailing their care team.
"We engaged them in a dialogue, not told them they had to [prescribe]," said Dr. Parker, with Cincinnati Children’s division of hospital medicine. "That gave them a chance to prescribe it if that was their intention and it was just forgotten, and it was also a good chance to further the education."
Education included reviewing the evidence on LGG and appropriate prescribing with hospital medicine attending physicians, residents and medical students, brief monthly reminders to residents and a campaign to private pediatricians with admitting privileges that included electronic information and signage in key areas of the hospital.
Before the intervention, however, the hospital had published its own evidence-based guideline in 2007, recommending consideration of probiotics. A Cochrane review of 63 studies in 8,014 infants and young children had also been published, showing that probiotics were safe and had a clear benefit in reducing the duration of diarrhea, although the size of the effect varied between studies (Cochrane Database Syst. Rev. 2010 [doi:10.1002/14651858.CD003048.pub3]).
So why then did the hospital have a 1% preintervention prescribing rate?
Dr. Parker admits the 1% rate is "far less than ideal" but said other hospitals are likely in the same predicament because it’s very hard for people to put evidence and guidelines into practice.
"I think this is all around the country," she said. "There’s evidence that it takes 17 years of solid evidence to change practice, for it to become the expert recommendation."
The intervention also removed a logistic barrier, with the help of its pharmacy, which began supplying the community hospital inpatient unit with LGG, specifically adult Culturelle because it has the most evidence behind it, she said.
The labor-intensive identification and mitigation process was discontinued after the system stabilized and the focus of the initiative shifted more towards shared decision-making with families.
"Instead of saying you have to do this in all kids, we tell them it’s something they have to pay for out of pocket and that it’s a modest benefit of 24 hours of less stool," Dr. Parker said. "So, is that something you’re interested in doing?"
A separate analysis found that there was no difference in prescription fill rates based on insurance status. One explanation for this is that the pharmacy will dispense only the number of capsules prescribed, rather than having families pay for the entire bottle, which can cost between $17 and $30, she said.
The chart review excluded children with known or presumed bacterial gastroenteritis, major comorbid conditions, and former premature infants not yet 2 months corrected gestational age. Specific demographics on the cohort were not provided.
The authors acknowledged that the James M. Anderson Center for Health Systems Excellence in Cincinnati collaborated in the project.
COVINGTON, KY. – A multifaceted intervention propelled probiotic prescriptions within 18 hours of admission from 1% to 100% among children admitted for acute gastroenteritis with diarrhea.
This was true regardless of their insurance status.
Moreover, the 100% prescribing rate was achieved within 6 weeks and has been sustained for 7 months, lead author Dr. Michelle Parker reported at Pediatric Hospital Medicine 2012.
"It’s definitely become culture," she said during the poster presentation.
A multidisciplinary team of hospital medicine attending physicians, nurse representative, and a research assistant at Cincinnati Children’s Hospital identified six key drivers they felt would increase inpatient prescribing of Lactobacillus rhamnosus GG (LGG) at admission. They were identification of eligible patients; adequate staff knowledge; prescriber buy-in; available and appropriate administration of LGG; immediate response to failure of prescribing; and process standardization.
One of the biggest game changers was to incorporate LGG as a default order within the acute gastroenteritis electronic order set, with the appropriate dose and frequency preselected, Dr. Parker said. The default order did not just happen, without the physician being aware, as prescribing physicians still had to click, enter LGG, and save the indication for its use.
The second key element was monitoring the electronic medical records each weekday for children with acute gastroenteritis, aged 2 months to 18 years, who were not prescribed LGG, and e-mailing their care team.
"We engaged them in a dialogue, not told them they had to [prescribe]," said Dr. Parker, with Cincinnati Children’s division of hospital medicine. "That gave them a chance to prescribe it if that was their intention and it was just forgotten, and it was also a good chance to further the education."
Education included reviewing the evidence on LGG and appropriate prescribing with hospital medicine attending physicians, residents and medical students, brief monthly reminders to residents and a campaign to private pediatricians with admitting privileges that included electronic information and signage in key areas of the hospital.
Before the intervention, however, the hospital had published its own evidence-based guideline in 2007, recommending consideration of probiotics. A Cochrane review of 63 studies in 8,014 infants and young children had also been published, showing that probiotics were safe and had a clear benefit in reducing the duration of diarrhea, although the size of the effect varied between studies (Cochrane Database Syst. Rev. 2010 [doi:10.1002/14651858.CD003048.pub3]).
So why then did the hospital have a 1% preintervention prescribing rate?
Dr. Parker admits the 1% rate is "far less than ideal" but said other hospitals are likely in the same predicament because it’s very hard for people to put evidence and guidelines into practice.
"I think this is all around the country," she said. "There’s evidence that it takes 17 years of solid evidence to change practice, for it to become the expert recommendation."
The intervention also removed a logistic barrier, with the help of its pharmacy, which began supplying the community hospital inpatient unit with LGG, specifically adult Culturelle because it has the most evidence behind it, she said.
The labor-intensive identification and mitigation process was discontinued after the system stabilized and the focus of the initiative shifted more towards shared decision-making with families.
"Instead of saying you have to do this in all kids, we tell them it’s something they have to pay for out of pocket and that it’s a modest benefit of 24 hours of less stool," Dr. Parker said. "So, is that something you’re interested in doing?"
A separate analysis found that there was no difference in prescription fill rates based on insurance status. One explanation for this is that the pharmacy will dispense only the number of capsules prescribed, rather than having families pay for the entire bottle, which can cost between $17 and $30, she said.
The chart review excluded children with known or presumed bacterial gastroenteritis, major comorbid conditions, and former premature infants not yet 2 months corrected gestational age. Specific demographics on the cohort were not provided.
The authors acknowledged that the James M. Anderson Center for Health Systems Excellence in Cincinnati collaborated in the project.
AT PEDIATRIC HOSPITAL MEDICINE 2012
Major Finding: Inpatient prescriptions of Lactobacillus rhamnosus GG among children admitted for acute gastroenteritis with diarrhea rose from 1% to 100% within 6 weeks.
Data Source: Retrospective chart review of a single-hospital intervention.
Disclosures: The authors disclosed that the James M. Anderson Center for Health Systems Excellence collaborated in the project.
Redefining Apparent Life-Threatening Events in Kids
COVINGTON, KY. – Evaluation and management of apparent life-threatening events should start with a clear, concise definition and an understanding of the risk for a serious underlying disorder, but so far this has proved elusive.
Despite a deluge of testing, nearly 50% of children leave the hospital with a diagnosis of idiopathic or gastroesophageal reflux, Dr. Joel Tieder said at the Pediatric Hospital Medicine 2012 meeting.
National efforts by an expert panel of hospitalist researchers and policy makers are underway to standardize inpatient care for an apparent life-threatening event (ALTE), a condition that evokes high anxiety in parents and providers alike and is defined by a loose constellation of symptoms.
The rallying cry for many pediatric hospitalists proved to be the largest multicenter study of ALTE to date (J. Pediatr. 2008;152:629-35). This study identified the frequent use of nonindicated testing – including pH probes, chest x-rays, and EKGs – and inconsistent hospital outcomes among infants admitted with ALTE.
"People really coalesced around this idea that hospitalists should own this disorder and fix it," explained Dr. Tieder, who led the study and sits on the expert panel. "There was just too much variability around the diagnosis and management, and we felt that this might be the first disorder we could tackle with guidelines."
The panel, sponsored by the Society for Hospital Medicine, has summarized and submitted for publication the sparse science there is on ALTE in hopes of soliciting comment and consensus.
Redefinition in Action
The panel also took the ambitious and somewhat unorthodox step of holding workshops at the Pediatric Hospital Medicine 2012 meeting for attendees to pen their own definition of ALTE. The discourse was dynamic and at times deafening, and despite the agreed upon goal among an audience of pediatric hospitalists, consensus on the content was conspicuously absent, which speaks to the difficulty of the task. Common themes did emerge and will be folded into the ongoing dialogue, said Dr. Tieder of Seattle Children’s Hospital.
Currently, clinicians diagnose ALTE using the National Institutes of Health’s definition that was put forth in 1986: an episode in the first year of life that appears potentially life threatening to the observer and is characterized by some combination of color change, apnea, alteration in muscle tone, and choking or gagging.
The crux of the problem is that this definition does not distinguish ALTE as a constellation of symptoms vs. ALTE as a diagnosis, he said. The term is loosely applied when testing proves to be unfruitful, or it is kept as the diagnosis despite an identification of the underlying cause of the event.
The new definition should also make very clear that – despite previous misnomers such as "near-miss SIDS" or "aborted crib deaths" –an ALTE is very different from SIDS, Dr. Tieder said. The two conditions have different risk factors, and interventions to reduce SIDS (such as the "Back to Sleep" campaign) have not reduced ALTEs.
The broad subjective definition of ALTE, the low prevalence of underlying disease, and the anxiety induced by ALTE combine to make "a recipe for testing cascade," Dr. Tieder said. "These are beautiful, healthy-appearing infants, and yet we do all these potentially harmful things to them with little evidence that the results will improve their outcomes."
Importantly, the yield for routine diagnostic testing for ALTE is low. In one study of 243 consecutive infants who experienced an ALTE, only 17.7% of 3,776 tests ordered were positive; even worse, just 6% contributed to the diagnosis (Pediatrics 2005;115:885-93).
Common discharge diagnoses for ALTE – such as idiopathic gastroesophageal reflux, respiratory infections (8%-11%), and seizures (9-11%) – are largely self-limiting and nonrecurring. It’s with the less common causes that clinicians start seeing the problem with managing an ALTE, Dr. Tieder said. These include pertussis (0.05%-9%), cardiac arrhythmias (fewer than 1%), bacterial infection (0%-8%), metabolic disorder (1.5%), and – increasingly and especially in infants with recurrent ALTE – child maltreatment (fewer than 1%).
"You need to have a high index of suspicion for child maltreatment," he said. A recent study involving 563 children, average age 2.3 months, who presented to the emergency department following an ALTE found a mortality rate of 9% in victims of child abuse (Pediatr. Emerg. Care 2011;27:591-5).
An Unfunded Conundrum
Despite the potential risk for serious underlying conditions and death, research funding has been lacking. Again, the problem lies with ALTE’s being defined as a constellation of symptoms, not as a disease (which is how government typically allocates research dollars), Dr. Tieder explained.
"We’re really stuck without a research source," he said. In the conventional mechanism, government funders "might fund child maltreatment, but [ALTE represents] only a minority of these patients. So when they start to rank priorities in this current austere environment, ALTEs don’t have a lot of cachet."
Grasping the Risks
A better understanding of life-threatening risk in infants with an ALTE, however, could revolutionize the work-up of these infants, just as greater understanding of the risk of myocardial infarction has revolutionized the way adult hospitalists stage the evaluation and management of adults presenting with chest pain.
Based on the current evidence, the panel has concluded that certain features can be used to assess risk and guide diagnostic testing. Factors that may define lower-risk infants are age older than 2 months; a first ALTE; a previously healthy status on no medications; no social concerns; no family history of SIDS or ALTE; and an obstructive event (such as choking, gagging, breath holding, or having a vasovagal episode) that was secondary to emesis, coughing, or crying, Dr. Tieder said. Although this is not set in stone, the panel suggests that routine screening is not indicated in low-risk infants, he added.
Key elements for higher-risk infants are age younger than 2 months, especially with upper respiratory symptoms or exposure; more than one ALTE; a history of prematurity, central apnea, comorbid conditions, or medication use; pertussis exposure/risk; social concerns; family history of SIDS; or unexplained death with physical findings of bruising or bleeding, particularly in the mouth.
Groups that are most likely to benefit from hospital admission include high-risk infants, infants younger than 37 weeks post-conceptual age, those younger than 2 months of age in whom pertussis and respiratory syncytial virus testing is pending, or cases where maltreatment is a concern, he said.
A Gap Filled
No definite timeline has been established for the panel to complete its task, but hospitalists are uniquely qualified to define ALTE and to establish a national standard for inpatient care for ALTEs, according to panel member and pediatric hospitalist Dr. Jack Percelay, who holds the newly created pediatrics seat on the SHM board of directors.
"It’s very multidisciplinary, so everybody looks at it from their own scope," he said in an interview. "The GI people look at it and say it’s got to be reflux; the neurology people say it looks like it’s going to be seizures. Or it could be trauma. We have that global view, so that’s why we’re the best people for it.
"I’m not sure that we want to be the experts, but no one else has really looked at it, so it was an opportunity for us. It was an orphan disease."
Dr. Tieder reported a relationship with Child Hospital Association, which provides grant support to the Pediatric Research in Inpatient Settings Network. Dr. Percelay reported no conflicts of interest.
COVINGTON, KY. – Evaluation and management of apparent life-threatening events should start with a clear, concise definition and an understanding of the risk for a serious underlying disorder, but so far this has proved elusive.
Despite a deluge of testing, nearly 50% of children leave the hospital with a diagnosis of idiopathic or gastroesophageal reflux, Dr. Joel Tieder said at the Pediatric Hospital Medicine 2012 meeting.
National efforts by an expert panel of hospitalist researchers and policy makers are underway to standardize inpatient care for an apparent life-threatening event (ALTE), a condition that evokes high anxiety in parents and providers alike and is defined by a loose constellation of symptoms.
The rallying cry for many pediatric hospitalists proved to be the largest multicenter study of ALTE to date (J. Pediatr. 2008;152:629-35). This study identified the frequent use of nonindicated testing – including pH probes, chest x-rays, and EKGs – and inconsistent hospital outcomes among infants admitted with ALTE.
"People really coalesced around this idea that hospitalists should own this disorder and fix it," explained Dr. Tieder, who led the study and sits on the expert panel. "There was just too much variability around the diagnosis and management, and we felt that this might be the first disorder we could tackle with guidelines."
The panel, sponsored by the Society for Hospital Medicine, has summarized and submitted for publication the sparse science there is on ALTE in hopes of soliciting comment and consensus.
Redefinition in Action
The panel also took the ambitious and somewhat unorthodox step of holding workshops at the Pediatric Hospital Medicine 2012 meeting for attendees to pen their own definition of ALTE. The discourse was dynamic and at times deafening, and despite the agreed upon goal among an audience of pediatric hospitalists, consensus on the content was conspicuously absent, which speaks to the difficulty of the task. Common themes did emerge and will be folded into the ongoing dialogue, said Dr. Tieder of Seattle Children’s Hospital.
Currently, clinicians diagnose ALTE using the National Institutes of Health’s definition that was put forth in 1986: an episode in the first year of life that appears potentially life threatening to the observer and is characterized by some combination of color change, apnea, alteration in muscle tone, and choking or gagging.
The crux of the problem is that this definition does not distinguish ALTE as a constellation of symptoms vs. ALTE as a diagnosis, he said. The term is loosely applied when testing proves to be unfruitful, or it is kept as the diagnosis despite an identification of the underlying cause of the event.
The new definition should also make very clear that – despite previous misnomers such as "near-miss SIDS" or "aborted crib deaths" –an ALTE is very different from SIDS, Dr. Tieder said. The two conditions have different risk factors, and interventions to reduce SIDS (such as the "Back to Sleep" campaign) have not reduced ALTEs.
The broad subjective definition of ALTE, the low prevalence of underlying disease, and the anxiety induced by ALTE combine to make "a recipe for testing cascade," Dr. Tieder said. "These are beautiful, healthy-appearing infants, and yet we do all these potentially harmful things to them with little evidence that the results will improve their outcomes."
Importantly, the yield for routine diagnostic testing for ALTE is low. In one study of 243 consecutive infants who experienced an ALTE, only 17.7% of 3,776 tests ordered were positive; even worse, just 6% contributed to the diagnosis (Pediatrics 2005;115:885-93).
Common discharge diagnoses for ALTE – such as idiopathic gastroesophageal reflux, respiratory infections (8%-11%), and seizures (9-11%) – are largely self-limiting and nonrecurring. It’s with the less common causes that clinicians start seeing the problem with managing an ALTE, Dr. Tieder said. These include pertussis (0.05%-9%), cardiac arrhythmias (fewer than 1%), bacterial infection (0%-8%), metabolic disorder (1.5%), and – increasingly and especially in infants with recurrent ALTE – child maltreatment (fewer than 1%).
"You need to have a high index of suspicion for child maltreatment," he said. A recent study involving 563 children, average age 2.3 months, who presented to the emergency department following an ALTE found a mortality rate of 9% in victims of child abuse (Pediatr. Emerg. Care 2011;27:591-5).
An Unfunded Conundrum
Despite the potential risk for serious underlying conditions and death, research funding has been lacking. Again, the problem lies with ALTE’s being defined as a constellation of symptoms, not as a disease (which is how government typically allocates research dollars), Dr. Tieder explained.
"We’re really stuck without a research source," he said. In the conventional mechanism, government funders "might fund child maltreatment, but [ALTE represents] only a minority of these patients. So when they start to rank priorities in this current austere environment, ALTEs don’t have a lot of cachet."
Grasping the Risks
A better understanding of life-threatening risk in infants with an ALTE, however, could revolutionize the work-up of these infants, just as greater understanding of the risk of myocardial infarction has revolutionized the way adult hospitalists stage the evaluation and management of adults presenting with chest pain.
Based on the current evidence, the panel has concluded that certain features can be used to assess risk and guide diagnostic testing. Factors that may define lower-risk infants are age older than 2 months; a first ALTE; a previously healthy status on no medications; no social concerns; no family history of SIDS or ALTE; and an obstructive event (such as choking, gagging, breath holding, or having a vasovagal episode) that was secondary to emesis, coughing, or crying, Dr. Tieder said. Although this is not set in stone, the panel suggests that routine screening is not indicated in low-risk infants, he added.
Key elements for higher-risk infants are age younger than 2 months, especially with upper respiratory symptoms or exposure; more than one ALTE; a history of prematurity, central apnea, comorbid conditions, or medication use; pertussis exposure/risk; social concerns; family history of SIDS; or unexplained death with physical findings of bruising or bleeding, particularly in the mouth.
Groups that are most likely to benefit from hospital admission include high-risk infants, infants younger than 37 weeks post-conceptual age, those younger than 2 months of age in whom pertussis and respiratory syncytial virus testing is pending, or cases where maltreatment is a concern, he said.
A Gap Filled
No definite timeline has been established for the panel to complete its task, but hospitalists are uniquely qualified to define ALTE and to establish a national standard for inpatient care for ALTEs, according to panel member and pediatric hospitalist Dr. Jack Percelay, who holds the newly created pediatrics seat on the SHM board of directors.
"It’s very multidisciplinary, so everybody looks at it from their own scope," he said in an interview. "The GI people look at it and say it’s got to be reflux; the neurology people say it looks like it’s going to be seizures. Or it could be trauma. We have that global view, so that’s why we’re the best people for it.
"I’m not sure that we want to be the experts, but no one else has really looked at it, so it was an opportunity for us. It was an orphan disease."
Dr. Tieder reported a relationship with Child Hospital Association, which provides grant support to the Pediatric Research in Inpatient Settings Network. Dr. Percelay reported no conflicts of interest.
COVINGTON, KY. – Evaluation and management of apparent life-threatening events should start with a clear, concise definition and an understanding of the risk for a serious underlying disorder, but so far this has proved elusive.
Despite a deluge of testing, nearly 50% of children leave the hospital with a diagnosis of idiopathic or gastroesophageal reflux, Dr. Joel Tieder said at the Pediatric Hospital Medicine 2012 meeting.
National efforts by an expert panel of hospitalist researchers and policy makers are underway to standardize inpatient care for an apparent life-threatening event (ALTE), a condition that evokes high anxiety in parents and providers alike and is defined by a loose constellation of symptoms.
The rallying cry for many pediatric hospitalists proved to be the largest multicenter study of ALTE to date (J. Pediatr. 2008;152:629-35). This study identified the frequent use of nonindicated testing – including pH probes, chest x-rays, and EKGs – and inconsistent hospital outcomes among infants admitted with ALTE.
"People really coalesced around this idea that hospitalists should own this disorder and fix it," explained Dr. Tieder, who led the study and sits on the expert panel. "There was just too much variability around the diagnosis and management, and we felt that this might be the first disorder we could tackle with guidelines."
The panel, sponsored by the Society for Hospital Medicine, has summarized and submitted for publication the sparse science there is on ALTE in hopes of soliciting comment and consensus.
Redefinition in Action
The panel also took the ambitious and somewhat unorthodox step of holding workshops at the Pediatric Hospital Medicine 2012 meeting for attendees to pen their own definition of ALTE. The discourse was dynamic and at times deafening, and despite the agreed upon goal among an audience of pediatric hospitalists, consensus on the content was conspicuously absent, which speaks to the difficulty of the task. Common themes did emerge and will be folded into the ongoing dialogue, said Dr. Tieder of Seattle Children’s Hospital.
Currently, clinicians diagnose ALTE using the National Institutes of Health’s definition that was put forth in 1986: an episode in the first year of life that appears potentially life threatening to the observer and is characterized by some combination of color change, apnea, alteration in muscle tone, and choking or gagging.
The crux of the problem is that this definition does not distinguish ALTE as a constellation of symptoms vs. ALTE as a diagnosis, he said. The term is loosely applied when testing proves to be unfruitful, or it is kept as the diagnosis despite an identification of the underlying cause of the event.
The new definition should also make very clear that – despite previous misnomers such as "near-miss SIDS" or "aborted crib deaths" –an ALTE is very different from SIDS, Dr. Tieder said. The two conditions have different risk factors, and interventions to reduce SIDS (such as the "Back to Sleep" campaign) have not reduced ALTEs.
The broad subjective definition of ALTE, the low prevalence of underlying disease, and the anxiety induced by ALTE combine to make "a recipe for testing cascade," Dr. Tieder said. "These are beautiful, healthy-appearing infants, and yet we do all these potentially harmful things to them with little evidence that the results will improve their outcomes."
Importantly, the yield for routine diagnostic testing for ALTE is low. In one study of 243 consecutive infants who experienced an ALTE, only 17.7% of 3,776 tests ordered were positive; even worse, just 6% contributed to the diagnosis (Pediatrics 2005;115:885-93).
Common discharge diagnoses for ALTE – such as idiopathic gastroesophageal reflux, respiratory infections (8%-11%), and seizures (9-11%) – are largely self-limiting and nonrecurring. It’s with the less common causes that clinicians start seeing the problem with managing an ALTE, Dr. Tieder said. These include pertussis (0.05%-9%), cardiac arrhythmias (fewer than 1%), bacterial infection (0%-8%), metabolic disorder (1.5%), and – increasingly and especially in infants with recurrent ALTE – child maltreatment (fewer than 1%).
"You need to have a high index of suspicion for child maltreatment," he said. A recent study involving 563 children, average age 2.3 months, who presented to the emergency department following an ALTE found a mortality rate of 9% in victims of child abuse (Pediatr. Emerg. Care 2011;27:591-5).
An Unfunded Conundrum
Despite the potential risk for serious underlying conditions and death, research funding has been lacking. Again, the problem lies with ALTE’s being defined as a constellation of symptoms, not as a disease (which is how government typically allocates research dollars), Dr. Tieder explained.
"We’re really stuck without a research source," he said. In the conventional mechanism, government funders "might fund child maltreatment, but [ALTE represents] only a minority of these patients. So when they start to rank priorities in this current austere environment, ALTEs don’t have a lot of cachet."
Grasping the Risks
A better understanding of life-threatening risk in infants with an ALTE, however, could revolutionize the work-up of these infants, just as greater understanding of the risk of myocardial infarction has revolutionized the way adult hospitalists stage the evaluation and management of adults presenting with chest pain.
Based on the current evidence, the panel has concluded that certain features can be used to assess risk and guide diagnostic testing. Factors that may define lower-risk infants are age older than 2 months; a first ALTE; a previously healthy status on no medications; no social concerns; no family history of SIDS or ALTE; and an obstructive event (such as choking, gagging, breath holding, or having a vasovagal episode) that was secondary to emesis, coughing, or crying, Dr. Tieder said. Although this is not set in stone, the panel suggests that routine screening is not indicated in low-risk infants, he added.
Key elements for higher-risk infants are age younger than 2 months, especially with upper respiratory symptoms or exposure; more than one ALTE; a history of prematurity, central apnea, comorbid conditions, or medication use; pertussis exposure/risk; social concerns; family history of SIDS; or unexplained death with physical findings of bruising or bleeding, particularly in the mouth.
Groups that are most likely to benefit from hospital admission include high-risk infants, infants younger than 37 weeks post-conceptual age, those younger than 2 months of age in whom pertussis and respiratory syncytial virus testing is pending, or cases where maltreatment is a concern, he said.
A Gap Filled
No definite timeline has been established for the panel to complete its task, but hospitalists are uniquely qualified to define ALTE and to establish a national standard for inpatient care for ALTEs, according to panel member and pediatric hospitalist Dr. Jack Percelay, who holds the newly created pediatrics seat on the SHM board of directors.
"It’s very multidisciplinary, so everybody looks at it from their own scope," he said in an interview. "The GI people look at it and say it’s got to be reflux; the neurology people say it looks like it’s going to be seizures. Or it could be trauma. We have that global view, so that’s why we’re the best people for it.
"I’m not sure that we want to be the experts, but no one else has really looked at it, so it was an opportunity for us. It was an orphan disease."
Dr. Tieder reported a relationship with Child Hospital Association, which provides grant support to the Pediatric Research in Inpatient Settings Network. Dr. Percelay reported no conflicts of interest.
AT THE PEDIATRIC HOSPITAL MEDICINE 2012 MEETING
Disclosures: Dr. Tieder reported a relationship with Child Hospital Association, which provides grant support to the Pediatric Research in Inpatient Settings Network. Dr. Percelay reported no conflicts of interest.
H1N1 Swine Flu Outbreak Identified in Indiana
Two- and four-legged visitors to an Indiana county fair picked up an unwelcome diagnosis of H1N1 influenza A.
The Centers for Disease Control and Prevention has confirmed four human cases of H3N2v virus with the influenza A(H1N1)pdm09 virus M gene. The viruses are similar to 12 cases identified in 2011 and 1 detected earlier this year (MMWR 2012;61:561).
Two people sought emergency care for respiratory illness on July 12 (the first day of the 5-day fair), and two others were identified as part of the subsequent public health investigation.
All four persons were swine exhibitors or their family members who had close contact with the pigs, and all have fully recovered without hospitalization.
In addition, respiratory specimens from a sample of 12 pigs at the fair were positive for influenza A(H3N2) virus. Preliminary genetic analysis has shown a very high level of similarity between the gene sequences of H3N2v viruses from humans and the H3N2 viruses from pigs, the CDC reported. There was no word on the subsequent health of the pigs.
The CDC is recommending that clinicians who suspect influenza in patients with recent exposure to pigs should obtain nasopharyngeal swab or aspirate in viral transport medium, and contact their state or local health department and request a timely diagnosis at a state public health laboratory.
Antiviral treatment with oral oseltamivir or inhaled zanamivir in suspected cases is recommended.
Health officials also advise that persons who raise pigs or come into close contact with them at fairs or other such summer venues should be aware of the potential risk for influenza transmission between swine and humans.
The four human Indiana cases bring the total of reported H1N1 influenza cases to 17 since August 2011.
Additional information is available at the CDC’s H3N2v website.
Two- and four-legged visitors to an Indiana county fair picked up an unwelcome diagnosis of H1N1 influenza A.
The Centers for Disease Control and Prevention has confirmed four human cases of H3N2v virus with the influenza A(H1N1)pdm09 virus M gene. The viruses are similar to 12 cases identified in 2011 and 1 detected earlier this year (MMWR 2012;61:561).
Two people sought emergency care for respiratory illness on July 12 (the first day of the 5-day fair), and two others were identified as part of the subsequent public health investigation.
All four persons were swine exhibitors or their family members who had close contact with the pigs, and all have fully recovered without hospitalization.
In addition, respiratory specimens from a sample of 12 pigs at the fair were positive for influenza A(H3N2) virus. Preliminary genetic analysis has shown a very high level of similarity between the gene sequences of H3N2v viruses from humans and the H3N2 viruses from pigs, the CDC reported. There was no word on the subsequent health of the pigs.
The CDC is recommending that clinicians who suspect influenza in patients with recent exposure to pigs should obtain nasopharyngeal swab or aspirate in viral transport medium, and contact their state or local health department and request a timely diagnosis at a state public health laboratory.
Antiviral treatment with oral oseltamivir or inhaled zanamivir in suspected cases is recommended.
Health officials also advise that persons who raise pigs or come into close contact with them at fairs or other such summer venues should be aware of the potential risk for influenza transmission between swine and humans.
The four human Indiana cases bring the total of reported H1N1 influenza cases to 17 since August 2011.
Additional information is available at the CDC’s H3N2v website.
Two- and four-legged visitors to an Indiana county fair picked up an unwelcome diagnosis of H1N1 influenza A.
The Centers for Disease Control and Prevention has confirmed four human cases of H3N2v virus with the influenza A(H1N1)pdm09 virus M gene. The viruses are similar to 12 cases identified in 2011 and 1 detected earlier this year (MMWR 2012;61:561).
Two people sought emergency care for respiratory illness on July 12 (the first day of the 5-day fair), and two others were identified as part of the subsequent public health investigation.
All four persons were swine exhibitors or their family members who had close contact with the pigs, and all have fully recovered without hospitalization.
In addition, respiratory specimens from a sample of 12 pigs at the fair were positive for influenza A(H3N2) virus. Preliminary genetic analysis has shown a very high level of similarity between the gene sequences of H3N2v viruses from humans and the H3N2 viruses from pigs, the CDC reported. There was no word on the subsequent health of the pigs.
The CDC is recommending that clinicians who suspect influenza in patients with recent exposure to pigs should obtain nasopharyngeal swab or aspirate in viral transport medium, and contact their state or local health department and request a timely diagnosis at a state public health laboratory.
Antiviral treatment with oral oseltamivir or inhaled zanamivir in suspected cases is recommended.
Health officials also advise that persons who raise pigs or come into close contact with them at fairs or other such summer venues should be aware of the potential risk for influenza transmission between swine and humans.
The four human Indiana cases bring the total of reported H1N1 influenza cases to 17 since August 2011.
Additional information is available at the CDC’s H3N2v website.
Single-Stick Approach Slashes Blood Culture Contamination
COVINGTON, KY. – Peripheral blood culture contamination can be reduced by more than half with little to no cost and without a dreaded second venipuncture for the patient, new research shows.
The contamination rate at in the pediatric emergency department at Vanderbilt University Medical Center in Nashville, Tenn., fell 60% from 4% to 1.6% after an intervention that focused on establishing a sterile bedside field, staff education and using a single-site intravenous insertion, Dr. Paul Hain said at Pediatric Hospital Medicine 2012.
The American Society of Microbiology currently recommends that contamination rates should not exceed 3% for the hospital setting.
Akron (Ohio) Children’s Hospital and Kansas City (Mo.) Children’s Hospital have both reported reducing false-positive blood culture rates from 9% to 2.8% and from 6.7% to 2.3%, respectively, but they did so by drawing culture specimens from a site separate from the inserted IV catheters, he explained.
The tipping point at Vanderbilt centered on a 7-week-old admitted with a diagnosis of apparent life-threatening event who, as a result of blood culture contamination, underwent an unnecessary lumbar puncture, received 2 days of unneeded antibiotics and antiviral therapy, spent 2 extra days in the hospital because of concerns for a serious bacterial infection and, ultimately, needed a plastic surgeon consult for an infiltration wound, he said.
A preintervention analysis revealed several opportunities during the process that could contribute to contamination. They were:
• The top of the culture bottle, clearly labeled as being nonsterile, was not sterilized with alcohol or chlorhexidine.
• Chlorhexidine solution was not allowed to completely dry on the skin prior to catheter insertion.
• The catheter site was palpated with a gloveless, nonsterile finger prior to insertion, but after cleansing.
• The blood sample was injected into a nonsterile container before injection into a sterile blood culture bottle or was placed on a nonsterile surface, bed, or sheets.
• The blood culture was drawn from peripheral intravenous catheter placed at the transferring hospital.
Based on these observations, lead author Dr. Randon T. Hall created a kit that included an IV catheter, transfer device, syringe, T-connector, clave, sterile tape and gloves, and an IV needle to help set up a sterile field.
A webinar was created to educate day and night shift nurses and the blood draw procedure was standardized, explained Dr. Hain, who recently became vice president and medical director for population health and network development at Children’s Medical Center, Dallas.
The procedure requires cleaning the top of the blood culture bottle with alcohol or chlorhexidine, placing extra tape on the side of the stand for later use in securing the IV, and having a holder ready the patient and position the sterile field kit for easy access.
The nurse dons sterile gloves, attaches the syringe to the T-connector and leaves it on the sterile field before cleansing the IV site thoroughly with a chlorhexidine swab, and creating a generous sterile area above and below the injection site, he said.
A tourniquet is then applied, the IV catheter placed, the blood drawn, and the sample put directly into a blood culture bottle. If working alone, the syringe has to be placed on the sterile glove field before securing the catheter, Dr. Hain said.
"It seems like this should have been the old procedure, I realize that, but it wasn’t," he added. "The old procedure was: If you learned how to draw blood in nursing school, good."
Contamination rates began falling within a month of the intervention began in July 2009, and hit a low of about 0.5% in early 2011 before reaching an average of 1.6% at the time of the analysis in December 2011.
From July 2009 to June 2010, there were 149 contaminations, costing the hospital $416,243, Dr. Hain said. That’s not counting the additional 53 calls made to families for repeat cultures, two needle sticks, one IV infiltrate and, on two occasions, police being sent to the home to retrieve a child when parents could not be reached by phone.
A 60% reduction in $417,000 yearly costs is $250,000 in approximate savings or $2,800/contamination. If one calculates the true cost, which current dogma places at approximately 50% of costs, then the true cost savings per year in the pediatric ED is $125,000, Dr. Hain said.
"This costs nothing to do, except Dr. Hall’s time," he said. "And the interesting part is that the [pediatric ED] collects only about 30% of our blood cultures, so we think there is the opportunity to double or triple our return on investment of zero dollars, if we can get this to spread to the rest of the hospital."
When asked by the audience how the intervention got buy-in from nurses, Dr. Hain said that Dr. Hall, who is now with Cincinnati Children’s Hospital Medical Center, acknowledged each month that the contamination rate remained below 4%, thanking each nurse for keeping children safe.
"It was much more of a positive thing, than if you drew a bad blood culture," he added.
Dr. Hall said in an interview that he’s discussed implementing the intervention into daily practice and potential savings with the executive board at Vanderbilt Children’s Hospital and the NICU educator and also has met with the current chief resident to continue surveillance and reporting to the ED.
Dr. Hall and Dr. Hain report no conflicts of interest. A coauthor disclosed research funding from CareFusion, bioMérieux and Affinium Pharmaceuticals.
COVINGTON, KY. – Peripheral blood culture contamination can be reduced by more than half with little to no cost and without a dreaded second venipuncture for the patient, new research shows.
The contamination rate at in the pediatric emergency department at Vanderbilt University Medical Center in Nashville, Tenn., fell 60% from 4% to 1.6% after an intervention that focused on establishing a sterile bedside field, staff education and using a single-site intravenous insertion, Dr. Paul Hain said at Pediatric Hospital Medicine 2012.
The American Society of Microbiology currently recommends that contamination rates should not exceed 3% for the hospital setting.
Akron (Ohio) Children’s Hospital and Kansas City (Mo.) Children’s Hospital have both reported reducing false-positive blood culture rates from 9% to 2.8% and from 6.7% to 2.3%, respectively, but they did so by drawing culture specimens from a site separate from the inserted IV catheters, he explained.
The tipping point at Vanderbilt centered on a 7-week-old admitted with a diagnosis of apparent life-threatening event who, as a result of blood culture contamination, underwent an unnecessary lumbar puncture, received 2 days of unneeded antibiotics and antiviral therapy, spent 2 extra days in the hospital because of concerns for a serious bacterial infection and, ultimately, needed a plastic surgeon consult for an infiltration wound, he said.
A preintervention analysis revealed several opportunities during the process that could contribute to contamination. They were:
• The top of the culture bottle, clearly labeled as being nonsterile, was not sterilized with alcohol or chlorhexidine.
• Chlorhexidine solution was not allowed to completely dry on the skin prior to catheter insertion.
• The catheter site was palpated with a gloveless, nonsterile finger prior to insertion, but after cleansing.
• The blood sample was injected into a nonsterile container before injection into a sterile blood culture bottle or was placed on a nonsterile surface, bed, or sheets.
• The blood culture was drawn from peripheral intravenous catheter placed at the transferring hospital.
Based on these observations, lead author Dr. Randon T. Hall created a kit that included an IV catheter, transfer device, syringe, T-connector, clave, sterile tape and gloves, and an IV needle to help set up a sterile field.
A webinar was created to educate day and night shift nurses and the blood draw procedure was standardized, explained Dr. Hain, who recently became vice president and medical director for population health and network development at Children’s Medical Center, Dallas.
The procedure requires cleaning the top of the blood culture bottle with alcohol or chlorhexidine, placing extra tape on the side of the stand for later use in securing the IV, and having a holder ready the patient and position the sterile field kit for easy access.
The nurse dons sterile gloves, attaches the syringe to the T-connector and leaves it on the sterile field before cleansing the IV site thoroughly with a chlorhexidine swab, and creating a generous sterile area above and below the injection site, he said.
A tourniquet is then applied, the IV catheter placed, the blood drawn, and the sample put directly into a blood culture bottle. If working alone, the syringe has to be placed on the sterile glove field before securing the catheter, Dr. Hain said.
"It seems like this should have been the old procedure, I realize that, but it wasn’t," he added. "The old procedure was: If you learned how to draw blood in nursing school, good."
Contamination rates began falling within a month of the intervention began in July 2009, and hit a low of about 0.5% in early 2011 before reaching an average of 1.6% at the time of the analysis in December 2011.
From July 2009 to June 2010, there were 149 contaminations, costing the hospital $416,243, Dr. Hain said. That’s not counting the additional 53 calls made to families for repeat cultures, two needle sticks, one IV infiltrate and, on two occasions, police being sent to the home to retrieve a child when parents could not be reached by phone.
A 60% reduction in $417,000 yearly costs is $250,000 in approximate savings or $2,800/contamination. If one calculates the true cost, which current dogma places at approximately 50% of costs, then the true cost savings per year in the pediatric ED is $125,000, Dr. Hain said.
"This costs nothing to do, except Dr. Hall’s time," he said. "And the interesting part is that the [pediatric ED] collects only about 30% of our blood cultures, so we think there is the opportunity to double or triple our return on investment of zero dollars, if we can get this to spread to the rest of the hospital."
When asked by the audience how the intervention got buy-in from nurses, Dr. Hain said that Dr. Hall, who is now with Cincinnati Children’s Hospital Medical Center, acknowledged each month that the contamination rate remained below 4%, thanking each nurse for keeping children safe.
"It was much more of a positive thing, than if you drew a bad blood culture," he added.
Dr. Hall said in an interview that he’s discussed implementing the intervention into daily practice and potential savings with the executive board at Vanderbilt Children’s Hospital and the NICU educator and also has met with the current chief resident to continue surveillance and reporting to the ED.
Dr. Hall and Dr. Hain report no conflicts of interest. A coauthor disclosed research funding from CareFusion, bioMérieux and Affinium Pharmaceuticals.
COVINGTON, KY. – Peripheral blood culture contamination can be reduced by more than half with little to no cost and without a dreaded second venipuncture for the patient, new research shows.
The contamination rate at in the pediatric emergency department at Vanderbilt University Medical Center in Nashville, Tenn., fell 60% from 4% to 1.6% after an intervention that focused on establishing a sterile bedside field, staff education and using a single-site intravenous insertion, Dr. Paul Hain said at Pediatric Hospital Medicine 2012.
The American Society of Microbiology currently recommends that contamination rates should not exceed 3% for the hospital setting.
Akron (Ohio) Children’s Hospital and Kansas City (Mo.) Children’s Hospital have both reported reducing false-positive blood culture rates from 9% to 2.8% and from 6.7% to 2.3%, respectively, but they did so by drawing culture specimens from a site separate from the inserted IV catheters, he explained.
The tipping point at Vanderbilt centered on a 7-week-old admitted with a diagnosis of apparent life-threatening event who, as a result of blood culture contamination, underwent an unnecessary lumbar puncture, received 2 days of unneeded antibiotics and antiviral therapy, spent 2 extra days in the hospital because of concerns for a serious bacterial infection and, ultimately, needed a plastic surgeon consult for an infiltration wound, he said.
A preintervention analysis revealed several opportunities during the process that could contribute to contamination. They were:
• The top of the culture bottle, clearly labeled as being nonsterile, was not sterilized with alcohol or chlorhexidine.
• Chlorhexidine solution was not allowed to completely dry on the skin prior to catheter insertion.
• The catheter site was palpated with a gloveless, nonsterile finger prior to insertion, but after cleansing.
• The blood sample was injected into a nonsterile container before injection into a sterile blood culture bottle or was placed on a nonsterile surface, bed, or sheets.
• The blood culture was drawn from peripheral intravenous catheter placed at the transferring hospital.
Based on these observations, lead author Dr. Randon T. Hall created a kit that included an IV catheter, transfer device, syringe, T-connector, clave, sterile tape and gloves, and an IV needle to help set up a sterile field.
A webinar was created to educate day and night shift nurses and the blood draw procedure was standardized, explained Dr. Hain, who recently became vice president and medical director for population health and network development at Children’s Medical Center, Dallas.
The procedure requires cleaning the top of the blood culture bottle with alcohol or chlorhexidine, placing extra tape on the side of the stand for later use in securing the IV, and having a holder ready the patient and position the sterile field kit for easy access.
The nurse dons sterile gloves, attaches the syringe to the T-connector and leaves it on the sterile field before cleansing the IV site thoroughly with a chlorhexidine swab, and creating a generous sterile area above and below the injection site, he said.
A tourniquet is then applied, the IV catheter placed, the blood drawn, and the sample put directly into a blood culture bottle. If working alone, the syringe has to be placed on the sterile glove field before securing the catheter, Dr. Hain said.
"It seems like this should have been the old procedure, I realize that, but it wasn’t," he added. "The old procedure was: If you learned how to draw blood in nursing school, good."
Contamination rates began falling within a month of the intervention began in July 2009, and hit a low of about 0.5% in early 2011 before reaching an average of 1.6% at the time of the analysis in December 2011.
From July 2009 to June 2010, there were 149 contaminations, costing the hospital $416,243, Dr. Hain said. That’s not counting the additional 53 calls made to families for repeat cultures, two needle sticks, one IV infiltrate and, on two occasions, police being sent to the home to retrieve a child when parents could not be reached by phone.
A 60% reduction in $417,000 yearly costs is $250,000 in approximate savings or $2,800/contamination. If one calculates the true cost, which current dogma places at approximately 50% of costs, then the true cost savings per year in the pediatric ED is $125,000, Dr. Hain said.
"This costs nothing to do, except Dr. Hall’s time," he said. "And the interesting part is that the [pediatric ED] collects only about 30% of our blood cultures, so we think there is the opportunity to double or triple our return on investment of zero dollars, if we can get this to spread to the rest of the hospital."
When asked by the audience how the intervention got buy-in from nurses, Dr. Hain said that Dr. Hall, who is now with Cincinnati Children’s Hospital Medical Center, acknowledged each month that the contamination rate remained below 4%, thanking each nurse for keeping children safe.
"It was much more of a positive thing, than if you drew a bad blood culture," he added.
Dr. Hall said in an interview that he’s discussed implementing the intervention into daily practice and potential savings with the executive board at Vanderbilt Children’s Hospital and the NICU educator and also has met with the current chief resident to continue surveillance and reporting to the ED.
Dr. Hall and Dr. Hain report no conflicts of interest. A coauthor disclosed research funding from CareFusion, bioMérieux and Affinium Pharmaceuticals.
AT PEDIATRIC HOSPITAL MEDICINE 2012
Major Finding: The blood culture contamination rate fell 60% from 4% to 1.6% after an intervention that focused on establishing a sterile bedside field, staff education, and use of a single-site intravenous insertion.
Data Source: Data are from an single-center observational study conducted July 2009-December 2011 in a hospital setting.
Disclosures: Dr. Hall and Dr. Hain report no conflicts of interest. A coauthor disclosed research funding from CareFusion, bioMérieux, and Affinium Pharmaceuticals.
Traffic-Related Toxins Linked to Childhood Kidney Cancer
MINNEAPOLIS – Prenatal exposure to traffic-related toxins may increase the risk for Wilms tumor, the most common form of childhood kidney cancer, the results of a study suggest.
Furthermore, findings suggest that different toxins may be potent at different pregnancy periods, Anshu Shrestha reported in a poster presentation at the annual meeting of the Society for Pediatric and Perinatal Epidemiologic Research.
The main culprits – formaldehyde, lead, and chromium VI – all have been shown to increase the risk of kidney cancer in adults, but little is known about their relationship to childhood renal cancers.
Wilms tumor occurs in 1 in 200,000-250,000 children, typically striking at about 3 years and rarely developing after age 8 years. The cure rate is about 90%, if the tumor has not metastasized.
The population-based, case-control study included 84 children in the California Cancer Registry who were aged 5 years and younger at the time of diagnosis with Wilms tumor, and 25,222 controls who were randomly selected from a birth registry and matched by birth year. Cases and controls lived within a 5-mile radius of a California Air Resources Board monitoring site, which measures 24-hour averages of air toxic concentrations every 12 days. Trimester-specific averages were calculated for 20 air toxins that were selected for carcinogenic property and sufficient sample size. Logistic regression analysis was adjusted for birth year, maternal age, maternal race/ethnicity and census-based socioeconomic status.
Third-trimester exposure to formaldehyde increased the risk of Wilms tumor by nearly 1.5-fold (odds ratio, 1.43), said Ms. Shrestha, an epidemiology doctoral student at the school of public health, University of California, Los Angeles.
Exposure to chromium VI in the first trimester and to lead in the second trimester also increased the odds of Wilms tumor, although to a lesser degree (OR, 1.10 and 1.27).
Positive associations were suggested for first-trimester exposure to lead, selenium, and benzene, but not for 1,3-butadiene, styrene, and ortho-dichlorobenzene.
Ms. Shrestha said that the data are preliminary and require more work to confirm that they are not due to chance alone.
Nearly half (47.6%) of the cases were Hispanic, 52.4% lived at the two lowest socioeconomic levels, and 55% had mothers aged 20-29 years at the time of their birth. Only 10.7% of cases lived at the highest socioeconomic level (defined by a combination of seven census indicators, including education and median household income).
The study was supported by grants from the National Institute of Environmental Health Sciences. Ms. Shrestha did not provide conflict of interest information.
MINNEAPOLIS – Prenatal exposure to traffic-related toxins may increase the risk for Wilms tumor, the most common form of childhood kidney cancer, the results of a study suggest.
Furthermore, findings suggest that different toxins may be potent at different pregnancy periods, Anshu Shrestha reported in a poster presentation at the annual meeting of the Society for Pediatric and Perinatal Epidemiologic Research.
The main culprits – formaldehyde, lead, and chromium VI – all have been shown to increase the risk of kidney cancer in adults, but little is known about their relationship to childhood renal cancers.
Wilms tumor occurs in 1 in 200,000-250,000 children, typically striking at about 3 years and rarely developing after age 8 years. The cure rate is about 90%, if the tumor has not metastasized.
The population-based, case-control study included 84 children in the California Cancer Registry who were aged 5 years and younger at the time of diagnosis with Wilms tumor, and 25,222 controls who were randomly selected from a birth registry and matched by birth year. Cases and controls lived within a 5-mile radius of a California Air Resources Board monitoring site, which measures 24-hour averages of air toxic concentrations every 12 days. Trimester-specific averages were calculated for 20 air toxins that were selected for carcinogenic property and sufficient sample size. Logistic regression analysis was adjusted for birth year, maternal age, maternal race/ethnicity and census-based socioeconomic status.
Third-trimester exposure to formaldehyde increased the risk of Wilms tumor by nearly 1.5-fold (odds ratio, 1.43), said Ms. Shrestha, an epidemiology doctoral student at the school of public health, University of California, Los Angeles.
Exposure to chromium VI in the first trimester and to lead in the second trimester also increased the odds of Wilms tumor, although to a lesser degree (OR, 1.10 and 1.27).
Positive associations were suggested for first-trimester exposure to lead, selenium, and benzene, but not for 1,3-butadiene, styrene, and ortho-dichlorobenzene.
Ms. Shrestha said that the data are preliminary and require more work to confirm that they are not due to chance alone.
Nearly half (47.6%) of the cases were Hispanic, 52.4% lived at the two lowest socioeconomic levels, and 55% had mothers aged 20-29 years at the time of their birth. Only 10.7% of cases lived at the highest socioeconomic level (defined by a combination of seven census indicators, including education and median household income).
The study was supported by grants from the National Institute of Environmental Health Sciences. Ms. Shrestha did not provide conflict of interest information.
MINNEAPOLIS – Prenatal exposure to traffic-related toxins may increase the risk for Wilms tumor, the most common form of childhood kidney cancer, the results of a study suggest.
Furthermore, findings suggest that different toxins may be potent at different pregnancy periods, Anshu Shrestha reported in a poster presentation at the annual meeting of the Society for Pediatric and Perinatal Epidemiologic Research.
The main culprits – formaldehyde, lead, and chromium VI – all have been shown to increase the risk of kidney cancer in adults, but little is known about their relationship to childhood renal cancers.
Wilms tumor occurs in 1 in 200,000-250,000 children, typically striking at about 3 years and rarely developing after age 8 years. The cure rate is about 90%, if the tumor has not metastasized.
The population-based, case-control study included 84 children in the California Cancer Registry who were aged 5 years and younger at the time of diagnosis with Wilms tumor, and 25,222 controls who were randomly selected from a birth registry and matched by birth year. Cases and controls lived within a 5-mile radius of a California Air Resources Board monitoring site, which measures 24-hour averages of air toxic concentrations every 12 days. Trimester-specific averages were calculated for 20 air toxins that were selected for carcinogenic property and sufficient sample size. Logistic regression analysis was adjusted for birth year, maternal age, maternal race/ethnicity and census-based socioeconomic status.
Third-trimester exposure to formaldehyde increased the risk of Wilms tumor by nearly 1.5-fold (odds ratio, 1.43), said Ms. Shrestha, an epidemiology doctoral student at the school of public health, University of California, Los Angeles.
Exposure to chromium VI in the first trimester and to lead in the second trimester also increased the odds of Wilms tumor, although to a lesser degree (OR, 1.10 and 1.27).
Positive associations were suggested for first-trimester exposure to lead, selenium, and benzene, but not for 1,3-butadiene, styrene, and ortho-dichlorobenzene.
Ms. Shrestha said that the data are preliminary and require more work to confirm that they are not due to chance alone.
Nearly half (47.6%) of the cases were Hispanic, 52.4% lived at the two lowest socioeconomic levels, and 55% had mothers aged 20-29 years at the time of their birth. Only 10.7% of cases lived at the highest socioeconomic level (defined by a combination of seven census indicators, including education and median household income).
The study was supported by grants from the National Institute of Environmental Health Sciences. Ms. Shrestha did not provide conflict of interest information.
AT THE ANNUAL MEETING OF THE SOCIETY FOR PEDIATRIC AND PERINATAL EPIDEMIOLOGIC RESEARCH
Major Finding: Third-trimester exposure to formaldehyde increased the risk of Wilms tumor by nearly 1.5-fold (OR, 1.43).
Data Source: This was a population-based, case-control study involving 84 children with Wilms tumor and 25,222 controls.
Disclosures: The study was supported by grants from the National Institute of Environmental Health Sciences. Ms. Shrestha did not provide conflict of interest information.