User login
Internists blame bureaucracy as top cause of burnout
Reported burnout among internal medicine physicians decreased over the past year based on data from Medscape’s annual survey of burnout and depression among physicians in the United States.
Approximately 80% of male internists and 85% of female internists said that their feelings of burnout and/or depression were driven by their jobs all or most of the time. The job-related stress and burnout come home with them — 76% of respondents overall said that burnout had negatively affected their personal relationships.
Too many bureaucratic tasks such as charting and paperwork were by far the top contributor to burnout, reported by 70% of respondents, with insufficient compensation and lack of respect from employers, colleagues, and staff as relatively distant second and third contributors (40% and 37%, respectively).
In addition, nearly half of the physicians said that their burnout was severe enough that they might leave medicine.
To help manage burnout, more internists reported positive coping strategies such as exercise (51%), talking with friends and family (47%), spending time alone (41%), and sleeping (40%), compared to less healthy strategies such as eating junk food, drinking alcohol, and using nicotine or cannabis products.
When asked what workplace measures would help with burnout, no one strategy rose to the top, but the top three were increased compensation (49%), additional support staff (48%), and more flexible work schedules (45%).
Notably, 62% of internists reported depression they defined as colloquial (feeling down or sad) and 27% described their depression as clinical. However, only 9% said they had sought professional help for depression, and 15% said they had sought help for burnout.
Staying in Practice Despite Burnout
The percentage of physicians across specialties who report depression and burnout worsened during the COVID-19 pandemic, said Noel Deep, MD, an internal medicine physician in group practice in Antigo, Wisconsin, in an interview.
Since the pandemic, newer stressors have replaced the pandemic-related stressors, and increasing bureaucratic burdens and paperwork continue to cause more physicians to report burnout, he said.
“If not assessed and addressed, this will lead to attrition in the physician workforce leading to increased burden on other physicians and impact patient access to healthcare,” he added.
The survey findings reflect Dr. Deep’s observations. “When talking to physicians across specialties, I have heard universally from many physicians about their experiences and ongoing struggles with potential burnout and mood-related issues,” he said. “While many of them feel that they are getting to the point of burnout, most of them also stoically continue to provide care to patients because they feel an obligation to them,” he said.
This feeling of obligation to patients is why less than one third of the physicians who consider retiring or leaving medicine because of burnout actually do, he said.
As for measures to reduce burnout, “I personally feel that increasing the compensation will not lead to decreased burnout,” Dr. Deep said. Although more money may provide temporary satisfaction, it will not yield long-term improvement in burnout, he said. “Based on personal experiences and my interactions with physicians, providing them more autonomy and control over their practices ... would contribute to decreasing the burnout,” Dr. Deep emphasized.
What Is to Be Done?
“I would favor having physician leaders in healthcare organizations take the time to talk to physicians [and] provide mentoring programs when new physicians are recruited, with ongoing discussions at operations and governance meetings about physician health and wellness,” Dr. Deep said. Providing frequent updates to physicians about wellness resources and encouraging them to seek out help anonymously through Employee Assistance Programs and other counseling services would be beneficial, he added.
“I would also consider peer mentoring when possible. Employers, healthcare organizations, and other key stakeholders should continue to work toward decreasing the stigma of depression and burnout,” Dr. Deep said.
Employers can help physicians manage and reduce burnout and depression by engaging with them, listening to their concerns, and trying to address them, said Dr. Deep. These actions will increase physicians’ trust in their administrations and promote a positive and healthy work environment, he said. “This will lead to reduced attrition in the workforce, retention of experienced physicians and support staff, and lead to increased patient satisfaction as well.”
The data come from Medscape’s annual report on Physician Burnout & Depression, which included 9226 practicing physicians in the United States across more than 29 specialties.
Dr. Deep had no financial conflicts to disclose; he serves on the Editorial Advisory Board of Internal Medicine News.
Reported burnout among internal medicine physicians decreased over the past year based on data from Medscape’s annual survey of burnout and depression among physicians in the United States.
Approximately 80% of male internists and 85% of female internists said that their feelings of burnout and/or depression were driven by their jobs all or most of the time. The job-related stress and burnout come home with them — 76% of respondents overall said that burnout had negatively affected their personal relationships.
Too many bureaucratic tasks such as charting and paperwork were by far the top contributor to burnout, reported by 70% of respondents, with insufficient compensation and lack of respect from employers, colleagues, and staff as relatively distant second and third contributors (40% and 37%, respectively).
In addition, nearly half of the physicians said that their burnout was severe enough that they might leave medicine.
To help manage burnout, more internists reported positive coping strategies such as exercise (51%), talking with friends and family (47%), spending time alone (41%), and sleeping (40%), compared to less healthy strategies such as eating junk food, drinking alcohol, and using nicotine or cannabis products.
When asked what workplace measures would help with burnout, no one strategy rose to the top, but the top three were increased compensation (49%), additional support staff (48%), and more flexible work schedules (45%).
Notably, 62% of internists reported depression they defined as colloquial (feeling down or sad) and 27% described their depression as clinical. However, only 9% said they had sought professional help for depression, and 15% said they had sought help for burnout.
Staying in Practice Despite Burnout
The percentage of physicians across specialties who report depression and burnout worsened during the COVID-19 pandemic, said Noel Deep, MD, an internal medicine physician in group practice in Antigo, Wisconsin, in an interview.
Since the pandemic, newer stressors have replaced the pandemic-related stressors, and increasing bureaucratic burdens and paperwork continue to cause more physicians to report burnout, he said.
“If not assessed and addressed, this will lead to attrition in the physician workforce leading to increased burden on other physicians and impact patient access to healthcare,” he added.
The survey findings reflect Dr. Deep’s observations. “When talking to physicians across specialties, I have heard universally from many physicians about their experiences and ongoing struggles with potential burnout and mood-related issues,” he said. “While many of them feel that they are getting to the point of burnout, most of them also stoically continue to provide care to patients because they feel an obligation to them,” he said.
This feeling of obligation to patients is why less than one third of the physicians who consider retiring or leaving medicine because of burnout actually do, he said.
As for measures to reduce burnout, “I personally feel that increasing the compensation will not lead to decreased burnout,” Dr. Deep said. Although more money may provide temporary satisfaction, it will not yield long-term improvement in burnout, he said. “Based on personal experiences and my interactions with physicians, providing them more autonomy and control over their practices ... would contribute to decreasing the burnout,” Dr. Deep emphasized.
What Is to Be Done?
“I would favor having physician leaders in healthcare organizations take the time to talk to physicians [and] provide mentoring programs when new physicians are recruited, with ongoing discussions at operations and governance meetings about physician health and wellness,” Dr. Deep said. Providing frequent updates to physicians about wellness resources and encouraging them to seek out help anonymously through Employee Assistance Programs and other counseling services would be beneficial, he added.
“I would also consider peer mentoring when possible. Employers, healthcare organizations, and other key stakeholders should continue to work toward decreasing the stigma of depression and burnout,” Dr. Deep said.
Employers can help physicians manage and reduce burnout and depression by engaging with them, listening to their concerns, and trying to address them, said Dr. Deep. These actions will increase physicians’ trust in their administrations and promote a positive and healthy work environment, he said. “This will lead to reduced attrition in the workforce, retention of experienced physicians and support staff, and lead to increased patient satisfaction as well.”
The data come from Medscape’s annual report on Physician Burnout & Depression, which included 9226 practicing physicians in the United States across more than 29 specialties.
Dr. Deep had no financial conflicts to disclose; he serves on the Editorial Advisory Board of Internal Medicine News.
Reported burnout among internal medicine physicians decreased over the past year based on data from Medscape’s annual survey of burnout and depression among physicians in the United States.
Approximately 80% of male internists and 85% of female internists said that their feelings of burnout and/or depression were driven by their jobs all or most of the time. The job-related stress and burnout come home with them — 76% of respondents overall said that burnout had negatively affected their personal relationships.
Too many bureaucratic tasks such as charting and paperwork were by far the top contributor to burnout, reported by 70% of respondents, with insufficient compensation and lack of respect from employers, colleagues, and staff as relatively distant second and third contributors (40% and 37%, respectively).
In addition, nearly half of the physicians said that their burnout was severe enough that they might leave medicine.
To help manage burnout, more internists reported positive coping strategies such as exercise (51%), talking with friends and family (47%), spending time alone (41%), and sleeping (40%), compared to less healthy strategies such as eating junk food, drinking alcohol, and using nicotine or cannabis products.
When asked what workplace measures would help with burnout, no one strategy rose to the top, but the top three were increased compensation (49%), additional support staff (48%), and more flexible work schedules (45%).
Notably, 62% of internists reported depression they defined as colloquial (feeling down or sad) and 27% described their depression as clinical. However, only 9% said they had sought professional help for depression, and 15% said they had sought help for burnout.
Staying in Practice Despite Burnout
The percentage of physicians across specialties who report depression and burnout worsened during the COVID-19 pandemic, said Noel Deep, MD, an internal medicine physician in group practice in Antigo, Wisconsin, in an interview.
Since the pandemic, newer stressors have replaced the pandemic-related stressors, and increasing bureaucratic burdens and paperwork continue to cause more physicians to report burnout, he said.
“If not assessed and addressed, this will lead to attrition in the physician workforce leading to increased burden on other physicians and impact patient access to healthcare,” he added.
The survey findings reflect Dr. Deep’s observations. “When talking to physicians across specialties, I have heard universally from many physicians about their experiences and ongoing struggles with potential burnout and mood-related issues,” he said. “While many of them feel that they are getting to the point of burnout, most of them also stoically continue to provide care to patients because they feel an obligation to them,” he said.
This feeling of obligation to patients is why less than one third of the physicians who consider retiring or leaving medicine because of burnout actually do, he said.
As for measures to reduce burnout, “I personally feel that increasing the compensation will not lead to decreased burnout,” Dr. Deep said. Although more money may provide temporary satisfaction, it will not yield long-term improvement in burnout, he said. “Based on personal experiences and my interactions with physicians, providing them more autonomy and control over their practices ... would contribute to decreasing the burnout,” Dr. Deep emphasized.
What Is to Be Done?
“I would favor having physician leaders in healthcare organizations take the time to talk to physicians [and] provide mentoring programs when new physicians are recruited, with ongoing discussions at operations and governance meetings about physician health and wellness,” Dr. Deep said. Providing frequent updates to physicians about wellness resources and encouraging them to seek out help anonymously through Employee Assistance Programs and other counseling services would be beneficial, he added.
“I would also consider peer mentoring when possible. Employers, healthcare organizations, and other key stakeholders should continue to work toward decreasing the stigma of depression and burnout,” Dr. Deep said.
Employers can help physicians manage and reduce burnout and depression by engaging with them, listening to their concerns, and trying to address them, said Dr. Deep. These actions will increase physicians’ trust in their administrations and promote a positive and healthy work environment, he said. “This will lead to reduced attrition in the workforce, retention of experienced physicians and support staff, and lead to increased patient satisfaction as well.”
The data come from Medscape’s annual report on Physician Burnout & Depression, which included 9226 practicing physicians in the United States across more than 29 specialties.
Dr. Deep had no financial conflicts to disclose; he serves on the Editorial Advisory Board of Internal Medicine News.
Sugar Substitutes Satisfy Appetite, Blunt Insulin Response
TOPLINE:
but decrease post-meal insulin and glucose levels in adults with overweight or obesity.
METHODOLOGY:
- In 2023, the World Health Organization issued a conditional recommendation that S&SE should not be used for weight control, apparently due to a lack of evidence for a clear benefit and weak evidence linking S&SE intake with excess weight and poorer health outcomes.
- This randomized crossover trial, conducted in England and France between 2021 and 2022, evaluated the acute (1 day) and repeated (daily for 2 weeks) effects of S&SEs vs sucrose in solid food on appetite and endocrine responses in adults with overweight or obesity.
- Overall, 53 adults (33 women, 20 men; aged 18-60 years) with overweight or obesity consumed biscuits with fruit filling containing either sucrose or reformulated with the S&SEs StRebM or neotame, daily for three 2-week intervention periods separated by a washout period of 14-21 days.
- Participants were required to fast for 12 hours before attending a laboratory session at the beginning (day 1) and end (day 14) of each consumption period.
- The primary endpoint was the composite appetite score, while secondary endpoints included food preferences, postprandial glucose and insulin response, and other satiety-related peptides, such as ghrelin, glucagon-like peptide 1, and pancreatic polypeptide.
TAKEAWAY:
- The composite appetite scores were comparable between the sucrose, StRebM, and neotame groups, with lower appetite suppression observed on day 14 than on day 1 for all three formulations.
- Neotame (P < .001) and StRebM (P < .001) lowered postprandial insulin levels compared with sucrose, while glucose levels saw a decline only with StRebM (and not with neotame) compared with sucrose (P < .05).
- The S&SEs had no effect on satiety levels, as any acute or repeated exposures to StRebM or neotame vs sucrose did not affect the ghrelin and glucagon-like peptide-1 responses.
- Gastrointestinal issues were more frequently reported in the neotame and StRebM groups than in the sucrose group.
IN PRACTICE:
“There is no detrimental impact of replacing sugar with S&SE in these endpoints,” the authors wrote. “Additionally, glucose and insulin responses were blunted after acute and repeated consumption of S&SE-reformulated biscuits, which may confer a benefit for blood glucose control, for example, in individuals at risk of developing type 2 diabetes.”
SOURCE:
This study was led by Catherine Gibbons, School of Psychology, Faculty of Medicine and Health, University of Leeds, England. It was published online in eBioMedicine.
LIMITATIONS:
The reformulated products required the addition of polyol bulking agents (8% maltitol and 8% sorbitol) to match the biscuits in sensory qualities as closely as possible. Gastrointestinal symptoms (initial bloating and flatulence) in the neotame and StRebM formulations may be due to the polyols, classed as low-digestible carbohydrates.
DISCLOSURES:
This study received funding from a European Union Horizon 2020 program, SWEET (Sweeteners and sweetness enhancers: Impact on health, obesity, safety, and sustainability). The authors reported receiving funding and honoraria from the food and beverage industry and trade groups from various entities.
A version of this article appeared on Medscape.com.
TOPLINE:
but decrease post-meal insulin and glucose levels in adults with overweight or obesity.
METHODOLOGY:
- In 2023, the World Health Organization issued a conditional recommendation that S&SE should not be used for weight control, apparently due to a lack of evidence for a clear benefit and weak evidence linking S&SE intake with excess weight and poorer health outcomes.
- This randomized crossover trial, conducted in England and France between 2021 and 2022, evaluated the acute (1 day) and repeated (daily for 2 weeks) effects of S&SEs vs sucrose in solid food on appetite and endocrine responses in adults with overweight or obesity.
- Overall, 53 adults (33 women, 20 men; aged 18-60 years) with overweight or obesity consumed biscuits with fruit filling containing either sucrose or reformulated with the S&SEs StRebM or neotame, daily for three 2-week intervention periods separated by a washout period of 14-21 days.
- Participants were required to fast for 12 hours before attending a laboratory session at the beginning (day 1) and end (day 14) of each consumption period.
- The primary endpoint was the composite appetite score, while secondary endpoints included food preferences, postprandial glucose and insulin response, and other satiety-related peptides, such as ghrelin, glucagon-like peptide 1, and pancreatic polypeptide.
TAKEAWAY:
- The composite appetite scores were comparable between the sucrose, StRebM, and neotame groups, with lower appetite suppression observed on day 14 than on day 1 for all three formulations.
- Neotame (P < .001) and StRebM (P < .001) lowered postprandial insulin levels compared with sucrose, while glucose levels saw a decline only with StRebM (and not with neotame) compared with sucrose (P < .05).
- The S&SEs had no effect on satiety levels, as any acute or repeated exposures to StRebM or neotame vs sucrose did not affect the ghrelin and glucagon-like peptide-1 responses.
- Gastrointestinal issues were more frequently reported in the neotame and StRebM groups than in the sucrose group.
IN PRACTICE:
“There is no detrimental impact of replacing sugar with S&SE in these endpoints,” the authors wrote. “Additionally, glucose and insulin responses were blunted after acute and repeated consumption of S&SE-reformulated biscuits, which may confer a benefit for blood glucose control, for example, in individuals at risk of developing type 2 diabetes.”
SOURCE:
This study was led by Catherine Gibbons, School of Psychology, Faculty of Medicine and Health, University of Leeds, England. It was published online in eBioMedicine.
LIMITATIONS:
The reformulated products required the addition of polyol bulking agents (8% maltitol and 8% sorbitol) to match the biscuits in sensory qualities as closely as possible. Gastrointestinal symptoms (initial bloating and flatulence) in the neotame and StRebM formulations may be due to the polyols, classed as low-digestible carbohydrates.
DISCLOSURES:
This study received funding from a European Union Horizon 2020 program, SWEET (Sweeteners and sweetness enhancers: Impact on health, obesity, safety, and sustainability). The authors reported receiving funding and honoraria from the food and beverage industry and trade groups from various entities.
A version of this article appeared on Medscape.com.
TOPLINE:
but decrease post-meal insulin and glucose levels in adults with overweight or obesity.
METHODOLOGY:
- In 2023, the World Health Organization issued a conditional recommendation that S&SE should not be used for weight control, apparently due to a lack of evidence for a clear benefit and weak evidence linking S&SE intake with excess weight and poorer health outcomes.
- This randomized crossover trial, conducted in England and France between 2021 and 2022, evaluated the acute (1 day) and repeated (daily for 2 weeks) effects of S&SEs vs sucrose in solid food on appetite and endocrine responses in adults with overweight or obesity.
- Overall, 53 adults (33 women, 20 men; aged 18-60 years) with overweight or obesity consumed biscuits with fruit filling containing either sucrose or reformulated with the S&SEs StRebM or neotame, daily for three 2-week intervention periods separated by a washout period of 14-21 days.
- Participants were required to fast for 12 hours before attending a laboratory session at the beginning (day 1) and end (day 14) of each consumption period.
- The primary endpoint was the composite appetite score, while secondary endpoints included food preferences, postprandial glucose and insulin response, and other satiety-related peptides, such as ghrelin, glucagon-like peptide 1, and pancreatic polypeptide.
TAKEAWAY:
- The composite appetite scores were comparable between the sucrose, StRebM, and neotame groups, with lower appetite suppression observed on day 14 than on day 1 for all three formulations.
- Neotame (P < .001) and StRebM (P < .001) lowered postprandial insulin levels compared with sucrose, while glucose levels saw a decline only with StRebM (and not with neotame) compared with sucrose (P < .05).
- The S&SEs had no effect on satiety levels, as any acute or repeated exposures to StRebM or neotame vs sucrose did not affect the ghrelin and glucagon-like peptide-1 responses.
- Gastrointestinal issues were more frequently reported in the neotame and StRebM groups than in the sucrose group.
IN PRACTICE:
“There is no detrimental impact of replacing sugar with S&SE in these endpoints,” the authors wrote. “Additionally, glucose and insulin responses were blunted after acute and repeated consumption of S&SE-reformulated biscuits, which may confer a benefit for blood glucose control, for example, in individuals at risk of developing type 2 diabetes.”
SOURCE:
This study was led by Catherine Gibbons, School of Psychology, Faculty of Medicine and Health, University of Leeds, England. It was published online in eBioMedicine.
LIMITATIONS:
The reformulated products required the addition of polyol bulking agents (8% maltitol and 8% sorbitol) to match the biscuits in sensory qualities as closely as possible. Gastrointestinal symptoms (initial bloating and flatulence) in the neotame and StRebM formulations may be due to the polyols, classed as low-digestible carbohydrates.
DISCLOSURES:
This study received funding from a European Union Horizon 2020 program, SWEET (Sweeteners and sweetness enhancers: Impact on health, obesity, safety, and sustainability). The authors reported receiving funding and honoraria from the food and beverage industry and trade groups from various entities.
A version of this article appeared on Medscape.com.
Children With ASD May Have Earlier Onset of Suicidal Thoughts, Behaviors
, according to a research letter in JAMA Pediatrics.
Suicide rates among all US children ages 10-14 years tripled between 2007 and 2021, becoming the second leading cause of death for this age bracket. Between 2018 and 2021, 315 suicides were reported among US children ages 5 to 11 years.
People with ASD show increased rates of STB, although prevalence estimates vary by study, which led the authors to study the issue.
Lead author Benjamin Joffe Schindel, MD, MPH, a fellow in neurodevelopmental medicine at the Kennedy Krieger Institute in Columbia, Maryland, and colleagues, analyzed responses from 968 caregivers of children ages 8-25 with ASD.
They found the following reported lifetime STB incidence:
- 392 (40.5%) reported wanting to die
- 187 (19.3%) reported wanting to end their own lives
- 72 (7.4%) reported having a suicide plan
Among those answering affirmatively to each of the above questions regarding STB, onset at 8 years or younger was reported in 142 (36.2%); 66 (35.3%); and 13 (18.1%) of the children, respectively. Included in the findings was one suicide attempt by cutting in an 8-year-old child.
Dr. Schindel said though there is no direct comparison with age of these thoughts among the general population, a previous study in 2013 showed that through age 10 prevalence of suicide ideation is very low (< 1%), then increases slowly through age 12 and then more rapidly until age 17.
Disturbing Findings
“The unexpectedly high frequency of STBs among children with ASD who were 8 years or younger is particularly disturbing given the lack of validated suicide risk screening tools and interventions for this age group,” the authors wrote. They added that early start of STB in children with ASD is important as this population has been underrepresented in suicide research and prevention efforts.
The average child age in this study was 13.4; 84.8% were White; and 81% were male. More than half of the children (54.8%) were taking medications for emotional, behavioral, or mood-related issues.
Data were collected from May to October 2017 from responses to the Mental Health and Suicidal Behaviors Questionnaire, an online caregiver-answered survey. The survey was created and distributed by the Interactive Autism Network (IAN), an international autism registry, from 2006 to 2019 with approximately 55, 000 participating families.
Thoughts Come at a ‘Shockingly Young Age’
Suzanne Rybczynski, MD, chief medical officer at East Tennessee Children’s Hospital in Knoxville, who was not part of the research, said the study was small but will help get the message out that “kids start thinking about suicide, especially kids with autism,” at a “shockingly young age.”
The results demonstrate the great demand for studying thoughts and behaviors especially in younger children and in children with neurodiversity — autism or other neurodevelopmental disabilities.
Studying children with ASD in relation to suicidal thoughts is difficult, Dr. Rybczynski said, because the way they think about death and how much is understood about the finality of suicide has not been well studied. It’s also uncertain how well the children understood the questions in this study, she added.
This retrospective study also asked for responses from caregivers who may remember or interpret a child’s thoughts and words differently from the child’s true intent, Dr. Rybczynski said.
“We need more studies like this asking questions to kids directly,” she said, so researchers can figure what children think it means to die.
Current Screening Recommendations
Current recommendations from the American Academy of Pediatrics (AAP) are to screen children universally for suicide risk at age 12 using a validated tool and if there are behavioral health concerns, screen as needed from ages 8 to 12.
This study suggests that screening needs to start earlier, Dr. Rybczynski said. “But we also need to know that we’re asking the right questions” and whether questions might be different for children with different abilities.
Children who are less verbal are often not included in screening. Screening studies often specifically exclude children with neurodisabilities, she explained. Getting these youngsters involved and making appropriate screening available “would be lifesaving,” she said.
“There are no validated (screening) tools down to age 8, which is not to say that some organizations don’t use them, but they’re not validated,” she said.
Dr. Rybczynski pointed out that most of the children were White and male and future work investigating these thoughts in girls and other racial/ethnic groups with ASD will be important as well. In addition, it will be important to revisit the issue post-pandemic with the rise in mental health issues with COVID-19.
Identifying children struggling with thoughts of suicide is the key to preventing tragedy, Dr. Rybczynski said, adding, “All those deaths are avoidable.”
Various study coauthors disclosed ties to the Simons Foundation, the Patient-Centered Outcomes Research Institute, the US Social Security Administration, American Foundation for Suicide Prevention, and Sarepta. No other disclosures were reported. Dr. Rybczynski, who provided commentary on the study, has no relevant financial relationships.
, according to a research letter in JAMA Pediatrics.
Suicide rates among all US children ages 10-14 years tripled between 2007 and 2021, becoming the second leading cause of death for this age bracket. Between 2018 and 2021, 315 suicides were reported among US children ages 5 to 11 years.
People with ASD show increased rates of STB, although prevalence estimates vary by study, which led the authors to study the issue.
Lead author Benjamin Joffe Schindel, MD, MPH, a fellow in neurodevelopmental medicine at the Kennedy Krieger Institute in Columbia, Maryland, and colleagues, analyzed responses from 968 caregivers of children ages 8-25 with ASD.
They found the following reported lifetime STB incidence:
- 392 (40.5%) reported wanting to die
- 187 (19.3%) reported wanting to end their own lives
- 72 (7.4%) reported having a suicide plan
Among those answering affirmatively to each of the above questions regarding STB, onset at 8 years or younger was reported in 142 (36.2%); 66 (35.3%); and 13 (18.1%) of the children, respectively. Included in the findings was one suicide attempt by cutting in an 8-year-old child.
Dr. Schindel said though there is no direct comparison with age of these thoughts among the general population, a previous study in 2013 showed that through age 10 prevalence of suicide ideation is very low (< 1%), then increases slowly through age 12 and then more rapidly until age 17.
Disturbing Findings
“The unexpectedly high frequency of STBs among children with ASD who were 8 years or younger is particularly disturbing given the lack of validated suicide risk screening tools and interventions for this age group,” the authors wrote. They added that early start of STB in children with ASD is important as this population has been underrepresented in suicide research and prevention efforts.
The average child age in this study was 13.4; 84.8% were White; and 81% were male. More than half of the children (54.8%) were taking medications for emotional, behavioral, or mood-related issues.
Data were collected from May to October 2017 from responses to the Mental Health and Suicidal Behaviors Questionnaire, an online caregiver-answered survey. The survey was created and distributed by the Interactive Autism Network (IAN), an international autism registry, from 2006 to 2019 with approximately 55, 000 participating families.
Thoughts Come at a ‘Shockingly Young Age’
Suzanne Rybczynski, MD, chief medical officer at East Tennessee Children’s Hospital in Knoxville, who was not part of the research, said the study was small but will help get the message out that “kids start thinking about suicide, especially kids with autism,” at a “shockingly young age.”
The results demonstrate the great demand for studying thoughts and behaviors especially in younger children and in children with neurodiversity — autism or other neurodevelopmental disabilities.
Studying children with ASD in relation to suicidal thoughts is difficult, Dr. Rybczynski said, because the way they think about death and how much is understood about the finality of suicide has not been well studied. It’s also uncertain how well the children understood the questions in this study, she added.
This retrospective study also asked for responses from caregivers who may remember or interpret a child’s thoughts and words differently from the child’s true intent, Dr. Rybczynski said.
“We need more studies like this asking questions to kids directly,” she said, so researchers can figure what children think it means to die.
Current Screening Recommendations
Current recommendations from the American Academy of Pediatrics (AAP) are to screen children universally for suicide risk at age 12 using a validated tool and if there are behavioral health concerns, screen as needed from ages 8 to 12.
This study suggests that screening needs to start earlier, Dr. Rybczynski said. “But we also need to know that we’re asking the right questions” and whether questions might be different for children with different abilities.
Children who are less verbal are often not included in screening. Screening studies often specifically exclude children with neurodisabilities, she explained. Getting these youngsters involved and making appropriate screening available “would be lifesaving,” she said.
“There are no validated (screening) tools down to age 8, which is not to say that some organizations don’t use them, but they’re not validated,” she said.
Dr. Rybczynski pointed out that most of the children were White and male and future work investigating these thoughts in girls and other racial/ethnic groups with ASD will be important as well. In addition, it will be important to revisit the issue post-pandemic with the rise in mental health issues with COVID-19.
Identifying children struggling with thoughts of suicide is the key to preventing tragedy, Dr. Rybczynski said, adding, “All those deaths are avoidable.”
Various study coauthors disclosed ties to the Simons Foundation, the Patient-Centered Outcomes Research Institute, the US Social Security Administration, American Foundation for Suicide Prevention, and Sarepta. No other disclosures were reported. Dr. Rybczynski, who provided commentary on the study, has no relevant financial relationships.
, according to a research letter in JAMA Pediatrics.
Suicide rates among all US children ages 10-14 years tripled between 2007 and 2021, becoming the second leading cause of death for this age bracket. Between 2018 and 2021, 315 suicides were reported among US children ages 5 to 11 years.
People with ASD show increased rates of STB, although prevalence estimates vary by study, which led the authors to study the issue.
Lead author Benjamin Joffe Schindel, MD, MPH, a fellow in neurodevelopmental medicine at the Kennedy Krieger Institute in Columbia, Maryland, and colleagues, analyzed responses from 968 caregivers of children ages 8-25 with ASD.
They found the following reported lifetime STB incidence:
- 392 (40.5%) reported wanting to die
- 187 (19.3%) reported wanting to end their own lives
- 72 (7.4%) reported having a suicide plan
Among those answering affirmatively to each of the above questions regarding STB, onset at 8 years or younger was reported in 142 (36.2%); 66 (35.3%); and 13 (18.1%) of the children, respectively. Included in the findings was one suicide attempt by cutting in an 8-year-old child.
Dr. Schindel said though there is no direct comparison with age of these thoughts among the general population, a previous study in 2013 showed that through age 10 prevalence of suicide ideation is very low (< 1%), then increases slowly through age 12 and then more rapidly until age 17.
Disturbing Findings
“The unexpectedly high frequency of STBs among children with ASD who were 8 years or younger is particularly disturbing given the lack of validated suicide risk screening tools and interventions for this age group,” the authors wrote. They added that early start of STB in children with ASD is important as this population has been underrepresented in suicide research and prevention efforts.
The average child age in this study was 13.4; 84.8% were White; and 81% were male. More than half of the children (54.8%) were taking medications for emotional, behavioral, or mood-related issues.
Data were collected from May to October 2017 from responses to the Mental Health and Suicidal Behaviors Questionnaire, an online caregiver-answered survey. The survey was created and distributed by the Interactive Autism Network (IAN), an international autism registry, from 2006 to 2019 with approximately 55, 000 participating families.
Thoughts Come at a ‘Shockingly Young Age’
Suzanne Rybczynski, MD, chief medical officer at East Tennessee Children’s Hospital in Knoxville, who was not part of the research, said the study was small but will help get the message out that “kids start thinking about suicide, especially kids with autism,” at a “shockingly young age.”
The results demonstrate the great demand for studying thoughts and behaviors especially in younger children and in children with neurodiversity — autism or other neurodevelopmental disabilities.
Studying children with ASD in relation to suicidal thoughts is difficult, Dr. Rybczynski said, because the way they think about death and how much is understood about the finality of suicide has not been well studied. It’s also uncertain how well the children understood the questions in this study, she added.
This retrospective study also asked for responses from caregivers who may remember or interpret a child’s thoughts and words differently from the child’s true intent, Dr. Rybczynski said.
“We need more studies like this asking questions to kids directly,” she said, so researchers can figure what children think it means to die.
Current Screening Recommendations
Current recommendations from the American Academy of Pediatrics (AAP) are to screen children universally for suicide risk at age 12 using a validated tool and if there are behavioral health concerns, screen as needed from ages 8 to 12.
This study suggests that screening needs to start earlier, Dr. Rybczynski said. “But we also need to know that we’re asking the right questions” and whether questions might be different for children with different abilities.
Children who are less verbal are often not included in screening. Screening studies often specifically exclude children with neurodisabilities, she explained. Getting these youngsters involved and making appropriate screening available “would be lifesaving,” she said.
“There are no validated (screening) tools down to age 8, which is not to say that some organizations don’t use them, but they’re not validated,” she said.
Dr. Rybczynski pointed out that most of the children were White and male and future work investigating these thoughts in girls and other racial/ethnic groups with ASD will be important as well. In addition, it will be important to revisit the issue post-pandemic with the rise in mental health issues with COVID-19.
Identifying children struggling with thoughts of suicide is the key to preventing tragedy, Dr. Rybczynski said, adding, “All those deaths are avoidable.”
Various study coauthors disclosed ties to the Simons Foundation, the Patient-Centered Outcomes Research Institute, the US Social Security Administration, American Foundation for Suicide Prevention, and Sarepta. No other disclosures were reported. Dr. Rybczynski, who provided commentary on the study, has no relevant financial relationships.
FROM JAMA PEDIATRICS
The Rise of Positive Psychiatry (and How Pediatrics Can Join the Effort)
Psychiatry, like all medical disciplines, changes over time. For many decades, psychiatrists were primarily psychotherapists. As medications slowly became available, these became a second tool for treatment — so much so that by the 21st century many, if not most, psychiatrists saw themselves primarily as psychopharmacologists and diagnosticians who were skilled at identifying various forms of mental illness and using medications in the hopes of inducing a clinically meaningful “response” in symptoms. While still belonging to the umbrella category of a mental health professional, more and more psychiatrists trained and practiced as mental illness professionals.
Slowly, however, there have been stirrings within the field by many who have found the identity of the psychiatrist as a “prescriber” to be too narrow, and the current “med check” model of treatment too confining. This change was partly inspired by our colleagues in clinical psychology who were challenged in the 1990s by then American Psychological Association President Martin Seligman, PhD, to develop knowledge and expertise not only in alleviating mental suffering but also in promoting true mental well-being, a construct that still was often vaguely defined. One framework of well-being that was advanced at the time was the PERMA model, representing the five well-being dimensions of Positive emotions, Engagement, Relationships, Meaning, and Accomplishment.1
While there have always been those in psychiatry who have advocated for a broad emphasis that incorporates the full spectrum of mental health, there has been a surge of interest in the past 10-15 years, urging a focus on well-being and the tools that can help a person achieve it. This trend has variably been referred to as positive psychiatry, lifestyle psychiatry, and other terms.2 As one might expect, child and adolescent psychiatry has been particularly fertile ground for such principles, and models such as the Vermont Family Based Approach have expanded the concept beyond the individual to the family and even community.3
It is important to note here that embracing the concept of well-being in treatment does not in any way require one to abandon the idea that genetic or environmental factors can lead to negative outcomes in brain development, nor does it mandate that one leaves behind important treatment modalities such as traditional psychotherapy and medication treatment. Further, this approach should not be confused with some “wellness” activities that offer quick fixes and lack scientific rigor. Positive psychiatry does, however, offer a third pathway to advance positive emotional behavioral growth, namely through health promotion activities ranging from exercise to good nutrition to positive parenting in ways that have been shown to benefit both those who are already doing fairly well as well as those who are actively struggling with significant psychiatric disorders.4
Primary care clinicians already have extensive familiarity talking about these kinds of health promoting activities with families. That said, it’s been my observation from many years of doing consultations and reviewing notes that these conversations happen almost exclusively during well-check visits and can get forgotten when a child presents with emotional behavioral challenges.
So how can the primary care clinician who is interested in more fully incorporating the burgeoning science on well-being work these principles into routine practice? Here are three suggestions.
Ask Some New Questions
It’s difficult to treat things that aren’t assessed. To best incorporate true mental health within one’s work with families, it can be very helpful to expand the regular questions one asks to include those that address some of the PERMA and health promotion areas described above. Some examples could include the following:
- Hopes. What would a perfect life look like for you when you’re older?
- Connection. Is there anything that you just love doing, so much so that time sometimes just seems to go away?
- Strengths. What are you good at? What good things would your friends say about you?
- Parenting. What are you most proud of as a parent, and where are your biggest challenges?
- Nutrition. What does a typical school day breakfast look like for you?
- Screens. Do you have any restrictions related to what you do on screens?
- Sleep. Tell me about your typical bedtime routine.
Add Some New Interventions
Counseling and medications can be powerful ways to bring improvement in a child’s life, but thinking about health promotion opens up a whole new avenue for intervention. This domain includes areas like physical activity, nutrition, sleep practices, parenting, participation in music and the arts, practicing kindness towards others, and mindfulness, among others.
For someone newly diagnosed with ADHD, for example, consider expanding your treatment plan to include not only medications but also specific guidance to exercise more, limit screen usage, practice good bedtime routines, eat a real breakfast, and reduce the helicopter parenting. Monitor these areas over time.
Another example relates to common sleep problems. Before making that melatonin recommendation, ask yourself if you understand what is happening in that child’s environment at night. Are they allowed to play video games until 2 a.m.? Are they taking naps during the day because they have nothing to do? Are they downing caffeinated drinks with dinner? Does the child get zero physical activity outside of the PE class? Maybe you still will need the melatonin, but perhaps other areas need to be addressed first.
Find Some New Colleagues
While it can be challenging sometimes to find anyone in mental health who sees new patients, there is value is finding out the approach and methodology that psychiatric clinicians and therapists apply in their practice. Working collaboratively with those who value a well-being orientation and who can work productively with the whole family to increase health promotion can yield benefits for a patient’s long-term physical and mental health.
The renewed interest and attention on well-being and health promotion activities that can optimize brain growth are a welcome and overdue development in mental health treatment. Pediatricians and other primary care clinicians can be a critical part of this growing initiative by gaining knowledge about youth well-being, applying this knowledge in day-to-day practice, and working collaboratively with those who share a similar perspective.
Dr. Rettew is a child & adolescent psychiatrist and medical director of Lane County Behavioral Health in Eugene, Oregon. He is on the psychiatry faculty at Oregon Health & Science University. You can follow him on Facebook and X @PediPsych. His latest book is Parenting Made Complicated: What Science Really Knows about the Greatest Debates of Early Childhood.
References
1. Seligman, MEP. Flourish: a visionary new understanding of happiness and well-being. New York: Simon & Schuster; 2011.
2. Jeste DV, Palmer BW. (Eds.). Positive psychiatry: a clinical handbook. Washington DC: American Psychiatric Publishing; 2015. doi: 10.1176/appi.books.9781615370818.
3. Hudziak J, Ivanova MY. The Vermont family based approach: Family based health promotion, illness prevention, and intervention. Child Adolesc Psychiatr Clin N Am. 2016 Apr;25(2):167-78. doi: 10.1016/j.chc.2015.11.002.
4. Rettew DC. Incorporating positive psychiatry with children and adolescents. Current Psychiatry. 2022 November;21(11):12-16,45. doi: 10.12788/cp.0303.
Psychiatry, like all medical disciplines, changes over time. For many decades, psychiatrists were primarily psychotherapists. As medications slowly became available, these became a second tool for treatment — so much so that by the 21st century many, if not most, psychiatrists saw themselves primarily as psychopharmacologists and diagnosticians who were skilled at identifying various forms of mental illness and using medications in the hopes of inducing a clinically meaningful “response” in symptoms. While still belonging to the umbrella category of a mental health professional, more and more psychiatrists trained and practiced as mental illness professionals.
Slowly, however, there have been stirrings within the field by many who have found the identity of the psychiatrist as a “prescriber” to be too narrow, and the current “med check” model of treatment too confining. This change was partly inspired by our colleagues in clinical psychology who were challenged in the 1990s by then American Psychological Association President Martin Seligman, PhD, to develop knowledge and expertise not only in alleviating mental suffering but also in promoting true mental well-being, a construct that still was often vaguely defined. One framework of well-being that was advanced at the time was the PERMA model, representing the five well-being dimensions of Positive emotions, Engagement, Relationships, Meaning, and Accomplishment.1
While there have always been those in psychiatry who have advocated for a broad emphasis that incorporates the full spectrum of mental health, there has been a surge of interest in the past 10-15 years, urging a focus on well-being and the tools that can help a person achieve it. This trend has variably been referred to as positive psychiatry, lifestyle psychiatry, and other terms.2 As one might expect, child and adolescent psychiatry has been particularly fertile ground for such principles, and models such as the Vermont Family Based Approach have expanded the concept beyond the individual to the family and even community.3
It is important to note here that embracing the concept of well-being in treatment does not in any way require one to abandon the idea that genetic or environmental factors can lead to negative outcomes in brain development, nor does it mandate that one leaves behind important treatment modalities such as traditional psychotherapy and medication treatment. Further, this approach should not be confused with some “wellness” activities that offer quick fixes and lack scientific rigor. Positive psychiatry does, however, offer a third pathway to advance positive emotional behavioral growth, namely through health promotion activities ranging from exercise to good nutrition to positive parenting in ways that have been shown to benefit both those who are already doing fairly well as well as those who are actively struggling with significant psychiatric disorders.4
Primary care clinicians already have extensive familiarity talking about these kinds of health promoting activities with families. That said, it’s been my observation from many years of doing consultations and reviewing notes that these conversations happen almost exclusively during well-check visits and can get forgotten when a child presents with emotional behavioral challenges.
So how can the primary care clinician who is interested in more fully incorporating the burgeoning science on well-being work these principles into routine practice? Here are three suggestions.
Ask Some New Questions
It’s difficult to treat things that aren’t assessed. To best incorporate true mental health within one’s work with families, it can be very helpful to expand the regular questions one asks to include those that address some of the PERMA and health promotion areas described above. Some examples could include the following:
- Hopes. What would a perfect life look like for you when you’re older?
- Connection. Is there anything that you just love doing, so much so that time sometimes just seems to go away?
- Strengths. What are you good at? What good things would your friends say about you?
- Parenting. What are you most proud of as a parent, and where are your biggest challenges?
- Nutrition. What does a typical school day breakfast look like for you?
- Screens. Do you have any restrictions related to what you do on screens?
- Sleep. Tell me about your typical bedtime routine.
Add Some New Interventions
Counseling and medications can be powerful ways to bring improvement in a child’s life, but thinking about health promotion opens up a whole new avenue for intervention. This domain includes areas like physical activity, nutrition, sleep practices, parenting, participation in music and the arts, practicing kindness towards others, and mindfulness, among others.
For someone newly diagnosed with ADHD, for example, consider expanding your treatment plan to include not only medications but also specific guidance to exercise more, limit screen usage, practice good bedtime routines, eat a real breakfast, and reduce the helicopter parenting. Monitor these areas over time.
Another example relates to common sleep problems. Before making that melatonin recommendation, ask yourself if you understand what is happening in that child’s environment at night. Are they allowed to play video games until 2 a.m.? Are they taking naps during the day because they have nothing to do? Are they downing caffeinated drinks with dinner? Does the child get zero physical activity outside of the PE class? Maybe you still will need the melatonin, but perhaps other areas need to be addressed first.
Find Some New Colleagues
While it can be challenging sometimes to find anyone in mental health who sees new patients, there is value is finding out the approach and methodology that psychiatric clinicians and therapists apply in their practice. Working collaboratively with those who value a well-being orientation and who can work productively with the whole family to increase health promotion can yield benefits for a patient’s long-term physical and mental health.
The renewed interest and attention on well-being and health promotion activities that can optimize brain growth are a welcome and overdue development in mental health treatment. Pediatricians and other primary care clinicians can be a critical part of this growing initiative by gaining knowledge about youth well-being, applying this knowledge in day-to-day practice, and working collaboratively with those who share a similar perspective.
Dr. Rettew is a child & adolescent psychiatrist and medical director of Lane County Behavioral Health in Eugene, Oregon. He is on the psychiatry faculty at Oregon Health & Science University. You can follow him on Facebook and X @PediPsych. His latest book is Parenting Made Complicated: What Science Really Knows about the Greatest Debates of Early Childhood.
References
1. Seligman, MEP. Flourish: a visionary new understanding of happiness and well-being. New York: Simon & Schuster; 2011.
2. Jeste DV, Palmer BW. (Eds.). Positive psychiatry: a clinical handbook. Washington DC: American Psychiatric Publishing; 2015. doi: 10.1176/appi.books.9781615370818.
3. Hudziak J, Ivanova MY. The Vermont family based approach: Family based health promotion, illness prevention, and intervention. Child Adolesc Psychiatr Clin N Am. 2016 Apr;25(2):167-78. doi: 10.1016/j.chc.2015.11.002.
4. Rettew DC. Incorporating positive psychiatry with children and adolescents. Current Psychiatry. 2022 November;21(11):12-16,45. doi: 10.12788/cp.0303.
Psychiatry, like all medical disciplines, changes over time. For many decades, psychiatrists were primarily psychotherapists. As medications slowly became available, these became a second tool for treatment — so much so that by the 21st century many, if not most, psychiatrists saw themselves primarily as psychopharmacologists and diagnosticians who were skilled at identifying various forms of mental illness and using medications in the hopes of inducing a clinically meaningful “response” in symptoms. While still belonging to the umbrella category of a mental health professional, more and more psychiatrists trained and practiced as mental illness professionals.
Slowly, however, there have been stirrings within the field by many who have found the identity of the psychiatrist as a “prescriber” to be too narrow, and the current “med check” model of treatment too confining. This change was partly inspired by our colleagues in clinical psychology who were challenged in the 1990s by then American Psychological Association President Martin Seligman, PhD, to develop knowledge and expertise not only in alleviating mental suffering but also in promoting true mental well-being, a construct that still was often vaguely defined. One framework of well-being that was advanced at the time was the PERMA model, representing the five well-being dimensions of Positive emotions, Engagement, Relationships, Meaning, and Accomplishment.1
While there have always been those in psychiatry who have advocated for a broad emphasis that incorporates the full spectrum of mental health, there has been a surge of interest in the past 10-15 years, urging a focus on well-being and the tools that can help a person achieve it. This trend has variably been referred to as positive psychiatry, lifestyle psychiatry, and other terms.2 As one might expect, child and adolescent psychiatry has been particularly fertile ground for such principles, and models such as the Vermont Family Based Approach have expanded the concept beyond the individual to the family and even community.3
It is important to note here that embracing the concept of well-being in treatment does not in any way require one to abandon the idea that genetic or environmental factors can lead to negative outcomes in brain development, nor does it mandate that one leaves behind important treatment modalities such as traditional psychotherapy and medication treatment. Further, this approach should not be confused with some “wellness” activities that offer quick fixes and lack scientific rigor. Positive psychiatry does, however, offer a third pathway to advance positive emotional behavioral growth, namely through health promotion activities ranging from exercise to good nutrition to positive parenting in ways that have been shown to benefit both those who are already doing fairly well as well as those who are actively struggling with significant psychiatric disorders.4
Primary care clinicians already have extensive familiarity talking about these kinds of health promoting activities with families. That said, it’s been my observation from many years of doing consultations and reviewing notes that these conversations happen almost exclusively during well-check visits and can get forgotten when a child presents with emotional behavioral challenges.
So how can the primary care clinician who is interested in more fully incorporating the burgeoning science on well-being work these principles into routine practice? Here are three suggestions.
Ask Some New Questions
It’s difficult to treat things that aren’t assessed. To best incorporate true mental health within one’s work with families, it can be very helpful to expand the regular questions one asks to include those that address some of the PERMA and health promotion areas described above. Some examples could include the following:
- Hopes. What would a perfect life look like for you when you’re older?
- Connection. Is there anything that you just love doing, so much so that time sometimes just seems to go away?
- Strengths. What are you good at? What good things would your friends say about you?
- Parenting. What are you most proud of as a parent, and where are your biggest challenges?
- Nutrition. What does a typical school day breakfast look like for you?
- Screens. Do you have any restrictions related to what you do on screens?
- Sleep. Tell me about your typical bedtime routine.
Add Some New Interventions
Counseling and medications can be powerful ways to bring improvement in a child’s life, but thinking about health promotion opens up a whole new avenue for intervention. This domain includes areas like physical activity, nutrition, sleep practices, parenting, participation in music and the arts, practicing kindness towards others, and mindfulness, among others.
For someone newly diagnosed with ADHD, for example, consider expanding your treatment plan to include not only medications but also specific guidance to exercise more, limit screen usage, practice good bedtime routines, eat a real breakfast, and reduce the helicopter parenting. Monitor these areas over time.
Another example relates to common sleep problems. Before making that melatonin recommendation, ask yourself if you understand what is happening in that child’s environment at night. Are they allowed to play video games until 2 a.m.? Are they taking naps during the day because they have nothing to do? Are they downing caffeinated drinks with dinner? Does the child get zero physical activity outside of the PE class? Maybe you still will need the melatonin, but perhaps other areas need to be addressed first.
Find Some New Colleagues
While it can be challenging sometimes to find anyone in mental health who sees new patients, there is value is finding out the approach and methodology that psychiatric clinicians and therapists apply in their practice. Working collaboratively with those who value a well-being orientation and who can work productively with the whole family to increase health promotion can yield benefits for a patient’s long-term physical and mental health.
The renewed interest and attention on well-being and health promotion activities that can optimize brain growth are a welcome and overdue development in mental health treatment. Pediatricians and other primary care clinicians can be a critical part of this growing initiative by gaining knowledge about youth well-being, applying this knowledge in day-to-day practice, and working collaboratively with those who share a similar perspective.
Dr. Rettew is a child & adolescent psychiatrist and medical director of Lane County Behavioral Health in Eugene, Oregon. He is on the psychiatry faculty at Oregon Health & Science University. You can follow him on Facebook and X @PediPsych. His latest book is Parenting Made Complicated: What Science Really Knows about the Greatest Debates of Early Childhood.
References
1. Seligman, MEP. Flourish: a visionary new understanding of happiness and well-being. New York: Simon & Schuster; 2011.
2. Jeste DV, Palmer BW. (Eds.). Positive psychiatry: a clinical handbook. Washington DC: American Psychiatric Publishing; 2015. doi: 10.1176/appi.books.9781615370818.
3. Hudziak J, Ivanova MY. The Vermont family based approach: Family based health promotion, illness prevention, and intervention. Child Adolesc Psychiatr Clin N Am. 2016 Apr;25(2):167-78. doi: 10.1016/j.chc.2015.11.002.
4. Rettew DC. Incorporating positive psychiatry with children and adolescents. Current Psychiatry. 2022 November;21(11):12-16,45. doi: 10.12788/cp.0303.
D-Mannose as UTI Treatment Offers No Benefit
TOPLINE:
A natural sugar used to treat recurring urinary tract infections (rUTIs) did not reduce future episodes, outpatient visits, the use of antibiotics, or symptoms compared with a placebo, according to a new study.
METHODOLOGY:
- D-Mannose is recommended as a natural alternative to antibiotics and sold as a dietary supplement; research showing the efficacy of D-mannose in treating UTIs is mixed.
- The double-blind, randomized controlled trial followed 598 women older than 18 years (median age, 61.3; range 18.2-93.5 years) with a history of rUTIs over 6 months from nearly 100 primary care clinics in the United Kingdom.
- Patients took 2 g of D-mannose or placebo powder daily and recorded their symptoms using a daily diary or through responses to health surveys, weekly questionnaires, and phone calls.
- Researchers checked medical records for urine culture results, antibiotic prescriptions, hospitalizations, and outpatient visits for UTIs.
TAKEAWAY:
- Approximately 51% of participants who took D-mannose and 55.7% of those who took a placebo contacted a healthcare professional reporting a UTI (relative risk, 0.92; 95% CI, 0.80-1.05; P = .22).
- Women in both groups reported similar durations of “moderately bad” or “worse” symptoms, and the number of antibiotic courses, instances of clinically suspected UTIs, and hospital admissions were similar between the two groups.
- Some studies have reported that synthetic mannosides are promising alternatives to D-mannose.
IN PRACTICE:
“D-Mannose should not be recommended to prevent future episodes of medically attended UTI in women with recurrent UTI in primary care,” the study authors wrote.
SOURCE:
The study was led by Gail Hayward, DPhil, associate professor at the Nuffield Department of Primary Care Health Sciences at the University of Oxford in England, and was published online in JAMA Internal Medicine.
LIMITATIONS:
Some participants may have taken less than 2 mg/d or skipped days. Because researchers used powder rather than capsules, dosing could have been inconsistent. Researchers did not obtain a microbiologic confirmation for each rUTI. A small percentage of women were taking antibiotics.
DISCLOSURES:
The study was funded by the National Institute for Health and Care Research (NIHR) School for Primary Care Research and the NIHR Oxford Biomedical Research Centre. Various authors reported receiving support from the NIHR Health Protection Research Unit on Healthcare-Associated Infections and Antimicrobial Resistance and were NIHR investigators.
A version of this article first appeared on Medscape.com.
TOPLINE:
A natural sugar used to treat recurring urinary tract infections (rUTIs) did not reduce future episodes, outpatient visits, the use of antibiotics, or symptoms compared with a placebo, according to a new study.
METHODOLOGY:
- D-Mannose is recommended as a natural alternative to antibiotics and sold as a dietary supplement; research showing the efficacy of D-mannose in treating UTIs is mixed.
- The double-blind, randomized controlled trial followed 598 women older than 18 years (median age, 61.3; range 18.2-93.5 years) with a history of rUTIs over 6 months from nearly 100 primary care clinics in the United Kingdom.
- Patients took 2 g of D-mannose or placebo powder daily and recorded their symptoms using a daily diary or through responses to health surveys, weekly questionnaires, and phone calls.
- Researchers checked medical records for urine culture results, antibiotic prescriptions, hospitalizations, and outpatient visits for UTIs.
TAKEAWAY:
- Approximately 51% of participants who took D-mannose and 55.7% of those who took a placebo contacted a healthcare professional reporting a UTI (relative risk, 0.92; 95% CI, 0.80-1.05; P = .22).
- Women in both groups reported similar durations of “moderately bad” or “worse” symptoms, and the number of antibiotic courses, instances of clinically suspected UTIs, and hospital admissions were similar between the two groups.
- Some studies have reported that synthetic mannosides are promising alternatives to D-mannose.
IN PRACTICE:
“D-Mannose should not be recommended to prevent future episodes of medically attended UTI in women with recurrent UTI in primary care,” the study authors wrote.
SOURCE:
The study was led by Gail Hayward, DPhil, associate professor at the Nuffield Department of Primary Care Health Sciences at the University of Oxford in England, and was published online in JAMA Internal Medicine.
LIMITATIONS:
Some participants may have taken less than 2 mg/d or skipped days. Because researchers used powder rather than capsules, dosing could have been inconsistent. Researchers did not obtain a microbiologic confirmation for each rUTI. A small percentage of women were taking antibiotics.
DISCLOSURES:
The study was funded by the National Institute for Health and Care Research (NIHR) School for Primary Care Research and the NIHR Oxford Biomedical Research Centre. Various authors reported receiving support from the NIHR Health Protection Research Unit on Healthcare-Associated Infections and Antimicrobial Resistance and were NIHR investigators.
A version of this article first appeared on Medscape.com.
TOPLINE:
A natural sugar used to treat recurring urinary tract infections (rUTIs) did not reduce future episodes, outpatient visits, the use of antibiotics, or symptoms compared with a placebo, according to a new study.
METHODOLOGY:
- D-Mannose is recommended as a natural alternative to antibiotics and sold as a dietary supplement; research showing the efficacy of D-mannose in treating UTIs is mixed.
- The double-blind, randomized controlled trial followed 598 women older than 18 years (median age, 61.3; range 18.2-93.5 years) with a history of rUTIs over 6 months from nearly 100 primary care clinics in the United Kingdom.
- Patients took 2 g of D-mannose or placebo powder daily and recorded their symptoms using a daily diary or through responses to health surveys, weekly questionnaires, and phone calls.
- Researchers checked medical records for urine culture results, antibiotic prescriptions, hospitalizations, and outpatient visits for UTIs.
TAKEAWAY:
- Approximately 51% of participants who took D-mannose and 55.7% of those who took a placebo contacted a healthcare professional reporting a UTI (relative risk, 0.92; 95% CI, 0.80-1.05; P = .22).
- Women in both groups reported similar durations of “moderately bad” or “worse” symptoms, and the number of antibiotic courses, instances of clinically suspected UTIs, and hospital admissions were similar between the two groups.
- Some studies have reported that synthetic mannosides are promising alternatives to D-mannose.
IN PRACTICE:
“D-Mannose should not be recommended to prevent future episodes of medically attended UTI in women with recurrent UTI in primary care,” the study authors wrote.
SOURCE:
The study was led by Gail Hayward, DPhil, associate professor at the Nuffield Department of Primary Care Health Sciences at the University of Oxford in England, and was published online in JAMA Internal Medicine.
LIMITATIONS:
Some participants may have taken less than 2 mg/d or skipped days. Because researchers used powder rather than capsules, dosing could have been inconsistent. Researchers did not obtain a microbiologic confirmation for each rUTI. A small percentage of women were taking antibiotics.
DISCLOSURES:
The study was funded by the National Institute for Health and Care Research (NIHR) School for Primary Care Research and the NIHR Oxford Biomedical Research Centre. Various authors reported receiving support from the NIHR Health Protection Research Unit on Healthcare-Associated Infections and Antimicrobial Resistance and were NIHR investigators.
A version of this article first appeared on Medscape.com.
Family Physician Burnout Rates Remain Stable, But Few Seek Help
Reported burnout among family physicians was down slightly in 2023 from the previous year, but burnout lasted longer, based on data from this news organization’s annual survey of burnout and depression among physicians in the United States.
Overall, 70% of internists surveyed said they had felt burned out for at least 13 months, compared with 60% in the 2023 survey. Of these, 41% said they had experienced feelings of burnout out for more than 2 years.
Overall, 82% of both male and female family physicians who reported feeling burned out or depressed attributed their burnout or depression to job stress rather than stress in their personal lives.
Bureaucratic tasks such as charting and paperwork were cited by 73% of respondents as the greatest contributor to family physicians’ burnout, followed by too many hours at work (39%) and lack of respect from administrators, colleagues, or staff.
Notably, 45% responded with either a 4 or 5 on a 1-5 scale that their burnout was severe enough that they might consider leaving practice, and 73% of respondents said that burnout was taking a negative toll on their personal relationships, up from 67% in last year’s survey.
Depression also remains a problem for family physicians, but fewer than 20% reported seeking help for either depression or burnout (15% and 16%, respectively)
Among the 27% of respondents who reported clinical depression, 69% cited job burnout as a significant contributor.
The top three strategies cited by respondents to reduce burnout were more support staff, more flexible work schedules, and lighter patient loads.
Take Needs for Support Seriously
The findings reflect the need not only of increased administrative support, but also personal and emotional support to reduce burnout among family physicians, Susan K. Fidler, MD, associate director of the Family Medicine Residency Program at Jefferson Health, Abington, Pennsylvania, said in an interview.
“Family physicians are a critically important societal resource to support the health of communities,” she said.
“It takes at least 7 years to train a family physician, and we need to create a culture in medicine to keep these highly-trained specialists engaged in their work to continue to provide continuity of care to their communities,” said Dr. Fidler. “Losing a family physician to burnout directly impacts the care that community receives and further worsens someone’s ability to access care,” she said.
Dr. Fidler was not surprised by the impact of administrative work on a physicians’ experience of burnout. “Physicians are energized by taking care of patients, and it is hard to feel like you are helping people by wading through the paperwork and administrative burden associated with our healthcare system,” she said.
However, she was surprised by the higher burnout rate in female physicians compared with males (55% vs. 45%, respectively). “As the proportion of the family physician workforce becomes increasing female, it becomes critical to understand this difference and provide support to address their specific needs,” she said.
Dr. Fidler said she agreed with the reported top three measures that might reduce burnout among family physicians. “In order to take care of the complex needs of our patients, more support staff and more time with patients can increase satisfaction with the practice of medicine,” she added.
Currently, physicians are often choosing between staying on time in short appointment slots and taking the necessary time to address patients’ needs, said Dr. Fidler.
“Longer appointments and more support staff allow family physicians to use their excellent training to provide whole-person care,” she said.
Previous research has shown that helping family physicians identify the most meaningful aspects of their work can reduce burnout, Dr. Fidler said. “It is up to healthcare administrators to allow physicians the flexibility to find their meaning in work and to support the systems that allow physicians to practice efficiently and effectively,” she said.
The data come from Medscape’s annual report on Physician Burnout & Depression, which included 9226 practicing physicians in the United States across more than 29 specialties.
Dr. Fidler had no financial conflicts to disclose.
Reported burnout among family physicians was down slightly in 2023 from the previous year, but burnout lasted longer, based on data from this news organization’s annual survey of burnout and depression among physicians in the United States.
Overall, 70% of internists surveyed said they had felt burned out for at least 13 months, compared with 60% in the 2023 survey. Of these, 41% said they had experienced feelings of burnout out for more than 2 years.
Overall, 82% of both male and female family physicians who reported feeling burned out or depressed attributed their burnout or depression to job stress rather than stress in their personal lives.
Bureaucratic tasks such as charting and paperwork were cited by 73% of respondents as the greatest contributor to family physicians’ burnout, followed by too many hours at work (39%) and lack of respect from administrators, colleagues, or staff.
Notably, 45% responded with either a 4 or 5 on a 1-5 scale that their burnout was severe enough that they might consider leaving practice, and 73% of respondents said that burnout was taking a negative toll on their personal relationships, up from 67% in last year’s survey.
Depression also remains a problem for family physicians, but fewer than 20% reported seeking help for either depression or burnout (15% and 16%, respectively)
Among the 27% of respondents who reported clinical depression, 69% cited job burnout as a significant contributor.
The top three strategies cited by respondents to reduce burnout were more support staff, more flexible work schedules, and lighter patient loads.
Take Needs for Support Seriously
The findings reflect the need not only of increased administrative support, but also personal and emotional support to reduce burnout among family physicians, Susan K. Fidler, MD, associate director of the Family Medicine Residency Program at Jefferson Health, Abington, Pennsylvania, said in an interview.
“Family physicians are a critically important societal resource to support the health of communities,” she said.
“It takes at least 7 years to train a family physician, and we need to create a culture in medicine to keep these highly-trained specialists engaged in their work to continue to provide continuity of care to their communities,” said Dr. Fidler. “Losing a family physician to burnout directly impacts the care that community receives and further worsens someone’s ability to access care,” she said.
Dr. Fidler was not surprised by the impact of administrative work on a physicians’ experience of burnout. “Physicians are energized by taking care of patients, and it is hard to feel like you are helping people by wading through the paperwork and administrative burden associated with our healthcare system,” she said.
However, she was surprised by the higher burnout rate in female physicians compared with males (55% vs. 45%, respectively). “As the proportion of the family physician workforce becomes increasing female, it becomes critical to understand this difference and provide support to address their specific needs,” she said.
Dr. Fidler said she agreed with the reported top three measures that might reduce burnout among family physicians. “In order to take care of the complex needs of our patients, more support staff and more time with patients can increase satisfaction with the practice of medicine,” she added.
Currently, physicians are often choosing between staying on time in short appointment slots and taking the necessary time to address patients’ needs, said Dr. Fidler.
“Longer appointments and more support staff allow family physicians to use their excellent training to provide whole-person care,” she said.
Previous research has shown that helping family physicians identify the most meaningful aspects of their work can reduce burnout, Dr. Fidler said. “It is up to healthcare administrators to allow physicians the flexibility to find their meaning in work and to support the systems that allow physicians to practice efficiently and effectively,” she said.
The data come from Medscape’s annual report on Physician Burnout & Depression, which included 9226 practicing physicians in the United States across more than 29 specialties.
Dr. Fidler had no financial conflicts to disclose.
Reported burnout among family physicians was down slightly in 2023 from the previous year, but burnout lasted longer, based on data from this news organization’s annual survey of burnout and depression among physicians in the United States.
Overall, 70% of internists surveyed said they had felt burned out for at least 13 months, compared with 60% in the 2023 survey. Of these, 41% said they had experienced feelings of burnout out for more than 2 years.
Overall, 82% of both male and female family physicians who reported feeling burned out or depressed attributed their burnout or depression to job stress rather than stress in their personal lives.
Bureaucratic tasks such as charting and paperwork were cited by 73% of respondents as the greatest contributor to family physicians’ burnout, followed by too many hours at work (39%) and lack of respect from administrators, colleagues, or staff.
Notably, 45% responded with either a 4 or 5 on a 1-5 scale that their burnout was severe enough that they might consider leaving practice, and 73% of respondents said that burnout was taking a negative toll on their personal relationships, up from 67% in last year’s survey.
Depression also remains a problem for family physicians, but fewer than 20% reported seeking help for either depression or burnout (15% and 16%, respectively)
Among the 27% of respondents who reported clinical depression, 69% cited job burnout as a significant contributor.
The top three strategies cited by respondents to reduce burnout were more support staff, more flexible work schedules, and lighter patient loads.
Take Needs for Support Seriously
The findings reflect the need not only of increased administrative support, but also personal and emotional support to reduce burnout among family physicians, Susan K. Fidler, MD, associate director of the Family Medicine Residency Program at Jefferson Health, Abington, Pennsylvania, said in an interview.
“Family physicians are a critically important societal resource to support the health of communities,” she said.
“It takes at least 7 years to train a family physician, and we need to create a culture in medicine to keep these highly-trained specialists engaged in their work to continue to provide continuity of care to their communities,” said Dr. Fidler. “Losing a family physician to burnout directly impacts the care that community receives and further worsens someone’s ability to access care,” she said.
Dr. Fidler was not surprised by the impact of administrative work on a physicians’ experience of burnout. “Physicians are energized by taking care of patients, and it is hard to feel like you are helping people by wading through the paperwork and administrative burden associated with our healthcare system,” she said.
However, she was surprised by the higher burnout rate in female physicians compared with males (55% vs. 45%, respectively). “As the proportion of the family physician workforce becomes increasing female, it becomes critical to understand this difference and provide support to address their specific needs,” she said.
Dr. Fidler said she agreed with the reported top three measures that might reduce burnout among family physicians. “In order to take care of the complex needs of our patients, more support staff and more time with patients can increase satisfaction with the practice of medicine,” she added.
Currently, physicians are often choosing between staying on time in short appointment slots and taking the necessary time to address patients’ needs, said Dr. Fidler.
“Longer appointments and more support staff allow family physicians to use their excellent training to provide whole-person care,” she said.
Previous research has shown that helping family physicians identify the most meaningful aspects of their work can reduce burnout, Dr. Fidler said. “It is up to healthcare administrators to allow physicians the flexibility to find their meaning in work and to support the systems that allow physicians to practice efficiently and effectively,” she said.
The data come from Medscape’s annual report on Physician Burnout & Depression, which included 9226 practicing physicians in the United States across more than 29 specialties.
Dr. Fidler had no financial conflicts to disclose.
Time Wasted to Avoid Penalties
Depression is a serious issue. I want to say that off the top, because nothing below is intended to minimize it.
But does everyone need to be tested for it?
A lot of general practices test for it with every patient and every visit. After all, mandates say you have to or you’ll get penalized a few bucks. Since no one wants to leave any money on the table in the razor-thin margins of running a medical practice, they ask these questions (I don’t blame them for that).
I can see where this might be useful, but does it really do much? Or is it just a mandatory waste of time?
Good question.
A recent review by the American College of Physicians found it was mostly a waste of time (which surprises no one). Only one of the eight measures involved in depression screening (suicide risk assessment) turned out to be useful. So, basically, 88% of the time spent on these questions contributed absolutely nothing of clinical relevance.
Of course, this isn’t unique to family medicine. Every time I see a Medicare or Medicare Advantage patient I have to document whether they’ve had flu and pneumonia vaccines. While there are occasional cases where asking about recent vaccines is critical to the history, for most it’s not. But I do it so I don’t get penalized, even though the answer changes nothing. It’s not like I give vaccines in my practice.
A fair number of people come to me for hospital follow-ups, so I go into the system and review the chart. The notes inevitably contain questions of sexual activity, fear of violence, fear of domestic abuse, food security, recent travel patterns, and so on. Some of them are useful in certain situations, but not in all, or even most. All they do is increase the length of the note until anything of relevance is obscured, and allow someone in coding to check the boxes to raise the billing level. Realistically, the ER staff involved probably didn’t ask any of them, and just clicked “no.”
Once this probably seemed like a good idea, but clearly most of it is now a waste of time. These “quality measures” have turned the art of taking a good history into a session of mouse and box clicking.
Does that really improve care?
Dr. Block has a solo neurology practice in Scottsdale, Arizona.
Depression is a serious issue. I want to say that off the top, because nothing below is intended to minimize it.
But does everyone need to be tested for it?
A lot of general practices test for it with every patient and every visit. After all, mandates say you have to or you’ll get penalized a few bucks. Since no one wants to leave any money on the table in the razor-thin margins of running a medical practice, they ask these questions (I don’t blame them for that).
I can see where this might be useful, but does it really do much? Or is it just a mandatory waste of time?
Good question.
A recent review by the American College of Physicians found it was mostly a waste of time (which surprises no one). Only one of the eight measures involved in depression screening (suicide risk assessment) turned out to be useful. So, basically, 88% of the time spent on these questions contributed absolutely nothing of clinical relevance.
Of course, this isn’t unique to family medicine. Every time I see a Medicare or Medicare Advantage patient I have to document whether they’ve had flu and pneumonia vaccines. While there are occasional cases where asking about recent vaccines is critical to the history, for most it’s not. But I do it so I don’t get penalized, even though the answer changes nothing. It’s not like I give vaccines in my practice.
A fair number of people come to me for hospital follow-ups, so I go into the system and review the chart. The notes inevitably contain questions of sexual activity, fear of violence, fear of domestic abuse, food security, recent travel patterns, and so on. Some of them are useful in certain situations, but not in all, or even most. All they do is increase the length of the note until anything of relevance is obscured, and allow someone in coding to check the boxes to raise the billing level. Realistically, the ER staff involved probably didn’t ask any of them, and just clicked “no.”
Once this probably seemed like a good idea, but clearly most of it is now a waste of time. These “quality measures” have turned the art of taking a good history into a session of mouse and box clicking.
Does that really improve care?
Dr. Block has a solo neurology practice in Scottsdale, Arizona.
Depression is a serious issue. I want to say that off the top, because nothing below is intended to minimize it.
But does everyone need to be tested for it?
A lot of general practices test for it with every patient and every visit. After all, mandates say you have to or you’ll get penalized a few bucks. Since no one wants to leave any money on the table in the razor-thin margins of running a medical practice, they ask these questions (I don’t blame them for that).
I can see where this might be useful, but does it really do much? Or is it just a mandatory waste of time?
Good question.
A recent review by the American College of Physicians found it was mostly a waste of time (which surprises no one). Only one of the eight measures involved in depression screening (suicide risk assessment) turned out to be useful. So, basically, 88% of the time spent on these questions contributed absolutely nothing of clinical relevance.
Of course, this isn’t unique to family medicine. Every time I see a Medicare or Medicare Advantage patient I have to document whether they’ve had flu and pneumonia vaccines. While there are occasional cases where asking about recent vaccines is critical to the history, for most it’s not. But I do it so I don’t get penalized, even though the answer changes nothing. It’s not like I give vaccines in my practice.
A fair number of people come to me for hospital follow-ups, so I go into the system and review the chart. The notes inevitably contain questions of sexual activity, fear of violence, fear of domestic abuse, food security, recent travel patterns, and so on. Some of them are useful in certain situations, but not in all, or even most. All they do is increase the length of the note until anything of relevance is obscured, and allow someone in coding to check the boxes to raise the billing level. Realistically, the ER staff involved probably didn’t ask any of them, and just clicked “no.”
Once this probably seemed like a good idea, but clearly most of it is now a waste of time. These “quality measures” have turned the art of taking a good history into a session of mouse and box clicking.
Does that really improve care?
Dr. Block has a solo neurology practice in Scottsdale, Arizona.
RA Flare Risk Rises Following DMARD Taper to Discontinuation With Conventional Synthetics or TNF Inhibitors
Patients with rheumatoid arthritis (RA) in remission who tapered and then fully stopped either conventional synthetic disease-modifying antirheumatic drug (csDMARD) or tumor necrosis factor (TNF)–inhibitor therapy experienced more disease flares than those who received stable dose treatment in an open-label, randomized trial.
In the 3-year trial, called ARCTIC REWIND, 80% of patients taking stable doses of only csMARDs remained flare-free compared with 38% in another treatment arm taking only csDMARDs who tapered to a half dose and then discontinued all after 1 year. In patients who continued to receive half-dose csDMARDs for the entire study period, 57% remained flare-free.
A separate two treatment arms of the study that assessed the effect of tapering TNF-inhibitor treatment to withdrawal showed that only 25% of patients who tapered TNF inhibitor to withdrawal remained flare-free over 3 years compared with 85% who remained on a stable TNF-inhibitor dose.
Though the risk for flare was higher in both the half-dose csDMARD and drug-free groups, the results also suggested that tapering medication “could be a realistic option for some patients with rheumatoid arthritis in sustained remission on csDMARDs,” wrote Kaja Kjørholt, MD, of the Center for Treatment of Rheumatic and Musculoskeletal Diseases at Diakonhjemmet Hospital in Oslo, Norway, and colleagues.
The 3-year results for the csDMARD-only arms of the trial were published in The Lancet Rheumatology. The 3-year results of the TNF-inhibitor arms of the study were presented as an abstract at the annual meeting of the American College of Rheumatology (ACR).
Don’t Avoid Tapering But Take an Individualized Approach
Many rheumatologists will taper patients with RA in remission to lower doses of medication, but the protocols for this study do not reflect clinical practice, noted James R. O’Dell, MD, chief of the Division of Rheumatology at the University of Nebraska Medical Center in Omaha, Nebraska. He was not involved with the research.
“I don’t know of any rheumatologist who would ever think that it was a good idea to taper somebody completely off of all DMARDs,” he told this news organization. “The only surprise is that more of them didn’t flare,” he continued, though he suspected that more patients would flare if they were followed for more time. Rheumatologists also would take a much more individualized approach when tapering to lower doses, he added, and do so at a much slower rate than what was observed in this study.
Both the ACR and the European Alliance of Associations for Rheumatology recommendations for the management of RA stated that tapering DMARDs can be considered for patients who have sustained remission, but they do not mention discontinuing medication entirely.
In the TNF-inhibitor arms of the trial, the tapering group received a half dose of a TNF inhibitor for 4 months before stopping therapy entirely, which Dr. O’Dell noted was a large dip in too short a period.
“Nobody should be surprised that these people flared a lot,” he said. However, tapering to lower doses of a TNF inhibitor can be successful, he noted, adding that more than half of his patients taking a TNF inhibitor are on less than their original dose. Completely tapering off a TNF inhibitor is less common and depends on what other DMARDs a patient is taking, he said, and complete drug-free remission in this population is highly unlikely.
Dr. O’Dell emphasized that the takeaway from these results should not be to avoid tapering medication because of flare risk but instead a tailored approach — something that is not possible with a study protocol — is needed.
“We want our patients to have all the medicine they need and no more,” he said. “That sweet spot is different for each individual patient for how much TNF inhibition or how much conventional therapy they need. If we’re thoughtful about that in the clinic, we can find that sweet spot,” he said.
Details of ARCTIC REWIND
The open-label ARCTIC REWIND trial enrolled patients with RA in sustained remission, determined via Disease Activity Score (DAS), from 10 different hospitals in Norway. Researchers enrolled 160 patients in the csDMARD-only arms and randomized them to receive stable dose csDMARDs for 3 years or half-dose csDMARDs for 1 year, followed by complete withdrawal for the next 2 years; withdrawal of csDMARDs was only done in patients who had not had a flare during the first year. Participants had scheduled clinic visits every 4 months, and full-dose csDMARD therapy was resumed in patients who experienced disease flares.
There was a total of 99 patients randomized in the TNF-inhibitor arms to continue stable TNF-inhibitor therapy or to taper to a half dose for 4 months before discontinuing therapy. Like the csDMARD study, clinic visits occurred every 4 months, and full-dose therapy was resumed if a flare occurred. Patients taking a TNF inhibitor could also take a csDMARD as needed.
Last year, 1-year results for the csDMARD arms were published in JAMA, and 1-year results for the TNF-inhibitor arms were reported in Annals of the Rheumatic Diseases.
At baseline, most patients across the three csDMARD groups (81%) had received methotrexate monotherapy. Triple therapy (methotrexate, sulfasalazine, and hydroxychloroquine) was used in 13% of the stable-dose group, 7% of the half-dose group, and 8% of the half-dose tapering to withdrawal group. Seven individuals in the stable-dose group, three individuals in the half-dose group, and three individuals the half-dose tapering to withdrawal group used other mono/duo therapies.
A total of 139 participants in the csDMARD-only arms completed 3 years of follow-up, with 68 in the stable-dose group, 36 in the half-dose group, and 35 in the half-dose tapering to withdrawal group.
Compared with the stable-dose group, the risk for flare was more than four times higher in the half-dose tapering to withdrawal group (hazard ratio [HR], 4.2; 95% CI, 2.2-8.2) and about three times higher in the half-dose group (HR, 2.9; 95% CI, 1.5-5.9). The flare risk between the half dose and half-dose tapering to withdrawal group was not statistically significant.
Most patients regained DAS remission status in the next clinic visit following a flare, the authors reported. Comparing the last visit to baseline, 10 patients in the taper-to-withdrawal group (27%) had increased treatment — either by adding a biologic or increasing csDMARD dose — compared with one patient (3%) in the half-dose group and 11 patients (14%) in the stable-dose group. Adverse events were common across all three groups, though were highest in the tapering to withdrawal group.
In the TNF-inhibitor arms, a total of 80 patients completed the 3-year follow-up. By the end of 3 years, 75% of the tapering group experienced a disease flare compared with 15% of the stable TNF-inhibitor group. Most patients regained DAS remission status in the next clinic visit following a flare, the authors reported. During the study, 23% of the tapering group and 13% of the stable TNF-inhibitor group used systemic glucocorticoids. Four patients in the tapering group and two patients in the stable TNF-inhibitor group switched to another TNF inhibitor during the study. An additional two patients in the stable TNF-inhibitor group switched to a Janus kinase inhibitor during the 3-year study.
Adverse events were similar in both treatment groups, but serious adverse events were more common in the tapering group (21%) than in the stable-dose group (11%).
The authors concluded that the findings did not support tapering a TNF inhibitor to withdrawal for patients in sustained remission, but they noted that additional research is needed to identify which patients would fare better or worse tapering csDMARDs.
ARCTIC REWIND was funded by grants from The Research Council of Norway and The South-Eastern Norway Regional Health Authorities. Many of the authors disclosed financial ties to pharmaceutical companies. Dr. O’Dell disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
Patients with rheumatoid arthritis (RA) in remission who tapered and then fully stopped either conventional synthetic disease-modifying antirheumatic drug (csDMARD) or tumor necrosis factor (TNF)–inhibitor therapy experienced more disease flares than those who received stable dose treatment in an open-label, randomized trial.
In the 3-year trial, called ARCTIC REWIND, 80% of patients taking stable doses of only csMARDs remained flare-free compared with 38% in another treatment arm taking only csDMARDs who tapered to a half dose and then discontinued all after 1 year. In patients who continued to receive half-dose csDMARDs for the entire study period, 57% remained flare-free.
A separate two treatment arms of the study that assessed the effect of tapering TNF-inhibitor treatment to withdrawal showed that only 25% of patients who tapered TNF inhibitor to withdrawal remained flare-free over 3 years compared with 85% who remained on a stable TNF-inhibitor dose.
Though the risk for flare was higher in both the half-dose csDMARD and drug-free groups, the results also suggested that tapering medication “could be a realistic option for some patients with rheumatoid arthritis in sustained remission on csDMARDs,” wrote Kaja Kjørholt, MD, of the Center for Treatment of Rheumatic and Musculoskeletal Diseases at Diakonhjemmet Hospital in Oslo, Norway, and colleagues.
The 3-year results for the csDMARD-only arms of the trial were published in The Lancet Rheumatology. The 3-year results of the TNF-inhibitor arms of the study were presented as an abstract at the annual meeting of the American College of Rheumatology (ACR).
Don’t Avoid Tapering But Take an Individualized Approach
Many rheumatologists will taper patients with RA in remission to lower doses of medication, but the protocols for this study do not reflect clinical practice, noted James R. O’Dell, MD, chief of the Division of Rheumatology at the University of Nebraska Medical Center in Omaha, Nebraska. He was not involved with the research.
“I don’t know of any rheumatologist who would ever think that it was a good idea to taper somebody completely off of all DMARDs,” he told this news organization. “The only surprise is that more of them didn’t flare,” he continued, though he suspected that more patients would flare if they were followed for more time. Rheumatologists also would take a much more individualized approach when tapering to lower doses, he added, and do so at a much slower rate than what was observed in this study.
Both the ACR and the European Alliance of Associations for Rheumatology recommendations for the management of RA stated that tapering DMARDs can be considered for patients who have sustained remission, but they do not mention discontinuing medication entirely.
In the TNF-inhibitor arms of the trial, the tapering group received a half dose of a TNF inhibitor for 4 months before stopping therapy entirely, which Dr. O’Dell noted was a large dip in too short a period.
“Nobody should be surprised that these people flared a lot,” he said. However, tapering to lower doses of a TNF inhibitor can be successful, he noted, adding that more than half of his patients taking a TNF inhibitor are on less than their original dose. Completely tapering off a TNF inhibitor is less common and depends on what other DMARDs a patient is taking, he said, and complete drug-free remission in this population is highly unlikely.
Dr. O’Dell emphasized that the takeaway from these results should not be to avoid tapering medication because of flare risk but instead a tailored approach — something that is not possible with a study protocol — is needed.
“We want our patients to have all the medicine they need and no more,” he said. “That sweet spot is different for each individual patient for how much TNF inhibition or how much conventional therapy they need. If we’re thoughtful about that in the clinic, we can find that sweet spot,” he said.
Details of ARCTIC REWIND
The open-label ARCTIC REWIND trial enrolled patients with RA in sustained remission, determined via Disease Activity Score (DAS), from 10 different hospitals in Norway. Researchers enrolled 160 patients in the csDMARD-only arms and randomized them to receive stable dose csDMARDs for 3 years or half-dose csDMARDs for 1 year, followed by complete withdrawal for the next 2 years; withdrawal of csDMARDs was only done in patients who had not had a flare during the first year. Participants had scheduled clinic visits every 4 months, and full-dose csDMARD therapy was resumed in patients who experienced disease flares.
There was a total of 99 patients randomized in the TNF-inhibitor arms to continue stable TNF-inhibitor therapy or to taper to a half dose for 4 months before discontinuing therapy. Like the csDMARD study, clinic visits occurred every 4 months, and full-dose therapy was resumed if a flare occurred. Patients taking a TNF inhibitor could also take a csDMARD as needed.
Last year, 1-year results for the csDMARD arms were published in JAMA, and 1-year results for the TNF-inhibitor arms were reported in Annals of the Rheumatic Diseases.
At baseline, most patients across the three csDMARD groups (81%) had received methotrexate monotherapy. Triple therapy (methotrexate, sulfasalazine, and hydroxychloroquine) was used in 13% of the stable-dose group, 7% of the half-dose group, and 8% of the half-dose tapering to withdrawal group. Seven individuals in the stable-dose group, three individuals in the half-dose group, and three individuals the half-dose tapering to withdrawal group used other mono/duo therapies.
A total of 139 participants in the csDMARD-only arms completed 3 years of follow-up, with 68 in the stable-dose group, 36 in the half-dose group, and 35 in the half-dose tapering to withdrawal group.
Compared with the stable-dose group, the risk for flare was more than four times higher in the half-dose tapering to withdrawal group (hazard ratio [HR], 4.2; 95% CI, 2.2-8.2) and about three times higher in the half-dose group (HR, 2.9; 95% CI, 1.5-5.9). The flare risk between the half dose and half-dose tapering to withdrawal group was not statistically significant.
Most patients regained DAS remission status in the next clinic visit following a flare, the authors reported. Comparing the last visit to baseline, 10 patients in the taper-to-withdrawal group (27%) had increased treatment — either by adding a biologic or increasing csDMARD dose — compared with one patient (3%) in the half-dose group and 11 patients (14%) in the stable-dose group. Adverse events were common across all three groups, though were highest in the tapering to withdrawal group.
In the TNF-inhibitor arms, a total of 80 patients completed the 3-year follow-up. By the end of 3 years, 75% of the tapering group experienced a disease flare compared with 15% of the stable TNF-inhibitor group. Most patients regained DAS remission status in the next clinic visit following a flare, the authors reported. During the study, 23% of the tapering group and 13% of the stable TNF-inhibitor group used systemic glucocorticoids. Four patients in the tapering group and two patients in the stable TNF-inhibitor group switched to another TNF inhibitor during the study. An additional two patients in the stable TNF-inhibitor group switched to a Janus kinase inhibitor during the 3-year study.
Adverse events were similar in both treatment groups, but serious adverse events were more common in the tapering group (21%) than in the stable-dose group (11%).
The authors concluded that the findings did not support tapering a TNF inhibitor to withdrawal for patients in sustained remission, but they noted that additional research is needed to identify which patients would fare better or worse tapering csDMARDs.
ARCTIC REWIND was funded by grants from The Research Council of Norway and The South-Eastern Norway Regional Health Authorities. Many of the authors disclosed financial ties to pharmaceutical companies. Dr. O’Dell disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
Patients with rheumatoid arthritis (RA) in remission who tapered and then fully stopped either conventional synthetic disease-modifying antirheumatic drug (csDMARD) or tumor necrosis factor (TNF)–inhibitor therapy experienced more disease flares than those who received stable dose treatment in an open-label, randomized trial.
In the 3-year trial, called ARCTIC REWIND, 80% of patients taking stable doses of only csMARDs remained flare-free compared with 38% in another treatment arm taking only csDMARDs who tapered to a half dose and then discontinued all after 1 year. In patients who continued to receive half-dose csDMARDs for the entire study period, 57% remained flare-free.
A separate two treatment arms of the study that assessed the effect of tapering TNF-inhibitor treatment to withdrawal showed that only 25% of patients who tapered TNF inhibitor to withdrawal remained flare-free over 3 years compared with 85% who remained on a stable TNF-inhibitor dose.
Though the risk for flare was higher in both the half-dose csDMARD and drug-free groups, the results also suggested that tapering medication “could be a realistic option for some patients with rheumatoid arthritis in sustained remission on csDMARDs,” wrote Kaja Kjørholt, MD, of the Center for Treatment of Rheumatic and Musculoskeletal Diseases at Diakonhjemmet Hospital in Oslo, Norway, and colleagues.
The 3-year results for the csDMARD-only arms of the trial were published in The Lancet Rheumatology. The 3-year results of the TNF-inhibitor arms of the study were presented as an abstract at the annual meeting of the American College of Rheumatology (ACR).
Don’t Avoid Tapering But Take an Individualized Approach
Many rheumatologists will taper patients with RA in remission to lower doses of medication, but the protocols for this study do not reflect clinical practice, noted James R. O’Dell, MD, chief of the Division of Rheumatology at the University of Nebraska Medical Center in Omaha, Nebraska. He was not involved with the research.
“I don’t know of any rheumatologist who would ever think that it was a good idea to taper somebody completely off of all DMARDs,” he told this news organization. “The only surprise is that more of them didn’t flare,” he continued, though he suspected that more patients would flare if they were followed for more time. Rheumatologists also would take a much more individualized approach when tapering to lower doses, he added, and do so at a much slower rate than what was observed in this study.
Both the ACR and the European Alliance of Associations for Rheumatology recommendations for the management of RA stated that tapering DMARDs can be considered for patients who have sustained remission, but they do not mention discontinuing medication entirely.
In the TNF-inhibitor arms of the trial, the tapering group received a half dose of a TNF inhibitor for 4 months before stopping therapy entirely, which Dr. O’Dell noted was a large dip in too short a period.
“Nobody should be surprised that these people flared a lot,” he said. However, tapering to lower doses of a TNF inhibitor can be successful, he noted, adding that more than half of his patients taking a TNF inhibitor are on less than their original dose. Completely tapering off a TNF inhibitor is less common and depends on what other DMARDs a patient is taking, he said, and complete drug-free remission in this population is highly unlikely.
Dr. O’Dell emphasized that the takeaway from these results should not be to avoid tapering medication because of flare risk but instead a tailored approach — something that is not possible with a study protocol — is needed.
“We want our patients to have all the medicine they need and no more,” he said. “That sweet spot is different for each individual patient for how much TNF inhibition or how much conventional therapy they need. If we’re thoughtful about that in the clinic, we can find that sweet spot,” he said.
Details of ARCTIC REWIND
The open-label ARCTIC REWIND trial enrolled patients with RA in sustained remission, determined via Disease Activity Score (DAS), from 10 different hospitals in Norway. Researchers enrolled 160 patients in the csDMARD-only arms and randomized them to receive stable dose csDMARDs for 3 years or half-dose csDMARDs for 1 year, followed by complete withdrawal for the next 2 years; withdrawal of csDMARDs was only done in patients who had not had a flare during the first year. Participants had scheduled clinic visits every 4 months, and full-dose csDMARD therapy was resumed in patients who experienced disease flares.
There was a total of 99 patients randomized in the TNF-inhibitor arms to continue stable TNF-inhibitor therapy or to taper to a half dose for 4 months before discontinuing therapy. Like the csDMARD study, clinic visits occurred every 4 months, and full-dose therapy was resumed if a flare occurred. Patients taking a TNF inhibitor could also take a csDMARD as needed.
Last year, 1-year results for the csDMARD arms were published in JAMA, and 1-year results for the TNF-inhibitor arms were reported in Annals of the Rheumatic Diseases.
At baseline, most patients across the three csDMARD groups (81%) had received methotrexate monotherapy. Triple therapy (methotrexate, sulfasalazine, and hydroxychloroquine) was used in 13% of the stable-dose group, 7% of the half-dose group, and 8% of the half-dose tapering to withdrawal group. Seven individuals in the stable-dose group, three individuals in the half-dose group, and three individuals the half-dose tapering to withdrawal group used other mono/duo therapies.
A total of 139 participants in the csDMARD-only arms completed 3 years of follow-up, with 68 in the stable-dose group, 36 in the half-dose group, and 35 in the half-dose tapering to withdrawal group.
Compared with the stable-dose group, the risk for flare was more than four times higher in the half-dose tapering to withdrawal group (hazard ratio [HR], 4.2; 95% CI, 2.2-8.2) and about three times higher in the half-dose group (HR, 2.9; 95% CI, 1.5-5.9). The flare risk between the half dose and half-dose tapering to withdrawal group was not statistically significant.
Most patients regained DAS remission status in the next clinic visit following a flare, the authors reported. Comparing the last visit to baseline, 10 patients in the taper-to-withdrawal group (27%) had increased treatment — either by adding a biologic or increasing csDMARD dose — compared with one patient (3%) in the half-dose group and 11 patients (14%) in the stable-dose group. Adverse events were common across all three groups, though were highest in the tapering to withdrawal group.
In the TNF-inhibitor arms, a total of 80 patients completed the 3-year follow-up. By the end of 3 years, 75% of the tapering group experienced a disease flare compared with 15% of the stable TNF-inhibitor group. Most patients regained DAS remission status in the next clinic visit following a flare, the authors reported. During the study, 23% of the tapering group and 13% of the stable TNF-inhibitor group used systemic glucocorticoids. Four patients in the tapering group and two patients in the stable TNF-inhibitor group switched to another TNF inhibitor during the study. An additional two patients in the stable TNF-inhibitor group switched to a Janus kinase inhibitor during the 3-year study.
Adverse events were similar in both treatment groups, but serious adverse events were more common in the tapering group (21%) than in the stable-dose group (11%).
The authors concluded that the findings did not support tapering a TNF inhibitor to withdrawal for patients in sustained remission, but they noted that additional research is needed to identify which patients would fare better or worse tapering csDMARDs.
ARCTIC REWIND was funded by grants from The Research Council of Norway and The South-Eastern Norway Regional Health Authorities. Many of the authors disclosed financial ties to pharmaceutical companies. Dr. O’Dell disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
Worldwide Uptick in Invasive Group A Streptococcus Disease Post Pandemic — What Should We Know?
Invasive group A streptococcus (iGAS) infections are rare (4-9 cases/100,000 US population annually) but potentially devastating (approximately 2,300 deaths annually in US), and affect all ages. Cases increase in winter-spring, paralleling the “season” of increased noninvasive GAS, e.g., pharyngitis and scarlet fever. iGAS case rates are lower in children than adults. That said, one well-known pediatric iGAS scenario has been deep cellulitis and necrotizing fasciitis during the healing phase of varicella. Other forms of iGAS include bacteremia, pneumonia (particularly when empyema is present), lymphangitis, erysipelas, and toxic shock syndrome. iGAS can occur with/after influenza but has also occurred concurrently with other viral respiratory infections.
Persons with underlying conditions (cancer or immune compromised status; chronic diseases of the heart, kidney or lung; diabetes mellitus) are at higher risk. Other subpopulations at risk for iGAS are illicit drug users, the elderly, homeless persons, nursing home residents, American Indian persons, and Alaska Native persons. Most experts feel that highly toxigenic strains of GAS are responsible for most iGAS. Indeed, most iGAS isolates produce (sometimes hyper-produce) superantigens that cause exaggerated innate immune responses, higher levels of inflammation, and often times tissue destruction, e.g., “flesh eating bacteria.” And who can forget that Jim Henson, creator of the Muppets, died of iGAS?
But why discuss iGAS in 2024? The pattern for iGAS has fluctuated more than usual in the last decade. So much so that the recent upsurge has caught the collective eye of the lay press. So, patients and friends may have questions about why and how iGAS is increasing lately. The bottom line is that no one knows for sure. However, the most recent 2 years of uptick may reflect GAS circulating at relatively high levels even when taking into account that GAS season occurs in winter-spring most years. Yet it seems likely that additional factors may have played a role in the fluctuations noted this past decade, e.g., temporary changes in societal behavior, a new GAS strain with over two dozen mutations, and possibly rapid waning of protection against GAS exotoxins.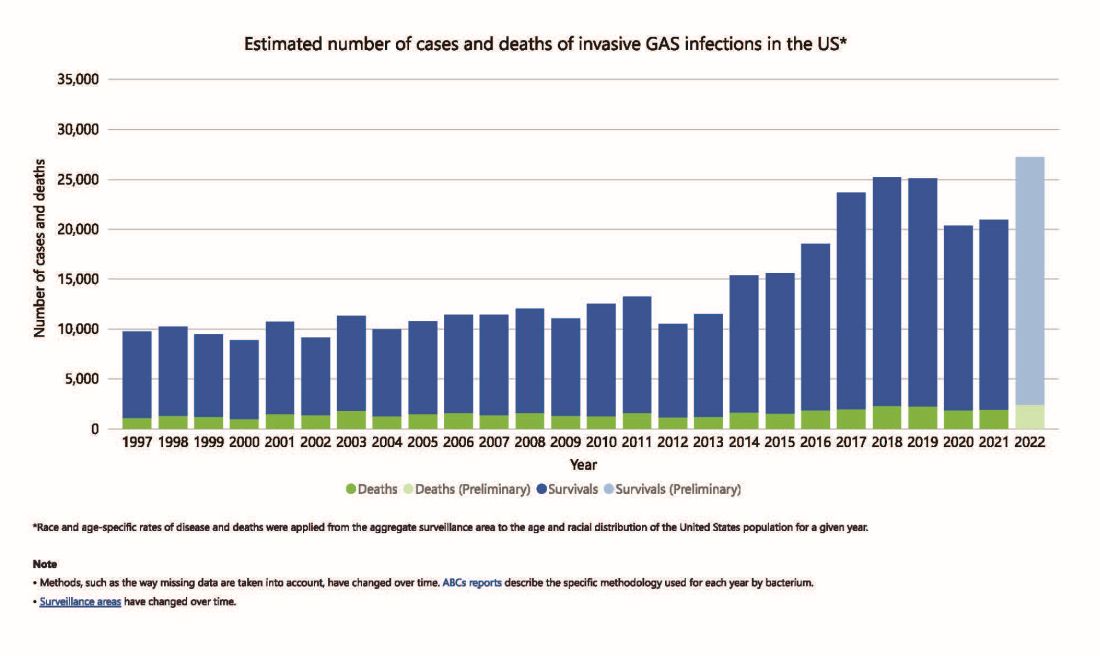
Social Behavior Factor
The SARS-CoV-2 pandemic brought extremes of disease and death to the world and dramatic changes in social behavior. A byproduct was dramatic decreases in nearly all infectious diseases, with numerous reports of near absence of many respiratory and gastrointestinal viruses in the 2020-2021 seasons. Interestingly, we did not see a drop in human rhinovirus infections, justifying its nickname as the cockroach of viruses. Reports also emerged about drops in bacterial diseases during 2020-2021 (although not so much for STIs), including noninvasive and invasive GAS disease, and also GAS-associated deaths (lowest since 2016).1 The drop in iGAS during social restrictions makes sense because GAS is spread by direct contact with infected persons or their secretions, and social contact had dramatically decreased particularly in the first 6 months of the pandemic.
However, since 2022 and the return to “normal” social behaviors, both viral diseases (e.g., RSV, influenza, and Norovirus), and some bacterial diseases have rebounded. That said, something else must be contributing, because iGAS rates had increased 4-5 years pre pandemic. In fact, the fluctuating pattern included “normal” annual rates in the early 2000s rising in ~2015 followed by the explainable pandemic drop (by nearly 25%), and not-too-unexpected 2-year postpandemic rise. But interestingly enough, the rebound is higher than might be expected for iGAS and children were overrepresented in first year’s rise (2022 rate for pediatric iGAS was the highest since 1997) while those older than 65 were overrepresented in second year (2023).1
Emergence of M1UK
One potential factor for the prepandemic rise in iGAS infections worldwide is the emergence and worldwide spread of a new GAS emm type variant designated M1UK.2 GAS isolates can be typed into categories designated as emm types based on DNA sequence. There are more than 240 emm types, with 6 being most common — M1, M3, and M28 (each up to 20% of GAS isolates) and M12, M82, and M89 (each up to 10%). M1, M3 and M28 have also been particularly associated with invasive disease. While emm types vary year to year and region by region, the overall emm type distribution among iGAS isolates in the United States had not been unusual since the turn of the century and the US M1 strain was the same as that which had been predominant worldwide (designated M1GLOBAL). This new M1UK sublineage had emerged around 2010 and had been increasing pre pandemic. The M1UK sequence contained a specific set of 27 SNPs (single nucleoside polymorphisms, i.e., single base mutations) and was associated with an uptick in scarlet fever in the United Kingdom starting around 2010. Its prevalence increased up to around 2015 while spreading internationally. It also had enhanced expression of SpeA, a phage-encoded superantigen. Some of the M1UK mutations also appear to alter GAS metabolic processes to allow better survival (better “fitness”) compared with other GAS. So, a more virulent hardier GAS had arisen and seems a reasonable candidate for contributing to the increased iGAS rates.
Waning Antibody to GAS As Potential Factor in Rebound
No consensus exists on correlates of protection from iGAS. However, adults seem to have less noninvasive GAS than children. One potential reason is that frequent GAS re-exposure, regardless of whether disease results, likely boosts anti-GAS antibodies. Pandemic social restrictions temporarily prevented such boosts. In children with developing antibody repertoires, anti-GAS antibodies may have waned below protective levels faster during a year without frequent boosting. Thus, children were iGAS susceptible soon after pandemic restrictions were dropped (2022). Increased iGAS rates in the elderly in 2023 may have occurred because of diminished GAS exposures accelerating immune senescence with anti-GAS antibodies dropping, but less quickly than in children. These speculations are simply hypotheses until future studies can test them.
All that said, how do we use information on increased iGAS in our daily practices? In addition to standard preventive strategies for viral coinfections (e.g., varicella and influenza vaccine), reminding families about rigorous attention to wound care is the one high-risk scenario we have not yet discussed. During 2024, a time of expected increased prevalence of iGAS, early wound care needs to be fastidious. Further, share warning signs with families (e.g., rapidly expanding painful erythema), “streaks” ascending from extremity wounds, fever and a highly painful wound, darkening almost purple color within cellulitis or soft tissue infection, or loss of sensation in the middle of an otherwise painful soft tissue infection. These presentations require immediate medical attention.
If such a patient presents, the Centers for Disease Control and Prevention (CDC) recommends admission along with blood and, where possible, wound cultures. If in the context of pneumonia with pleural effusion, culturing pleural fluid is also important. Remember, leading edge cultures are not often positive for GAS, seemingly because GAS exotoxins are found at erythema’s leading edge, not the bacteria. The bacteria are somewhere more central in the inflammatory process. Despite not being prominent among recent iGAS cases, another scenario that could sneak up on you is the infected surgical wound as nascent iGAS.
Finally, remember that nationally increasing numbers of iGAS isolates are resistant to erythromycin and clindamycin, the latter usually recommended to reduce tissue damage in iGAS.3 So, it is important to be aware of susceptibility patterns in your locale and consider an ID consultation. My hope is that you do not see an iGAS case this year, but we all need to remain alert. With a high index of suspicion and rapid diagnosis, you can minimize long-term sequelae and potential fatalities.
While it is too early to tell how the rest of 2024 will turn out, preliminary indications are that GAS is circulating at higher than usual levels (30%-35% GAS positive throat swabs in early April 2024 in Kansas City area) and iGAS rates will likely also be relatively high, particularly if Ontario, Canada, data are any indication.4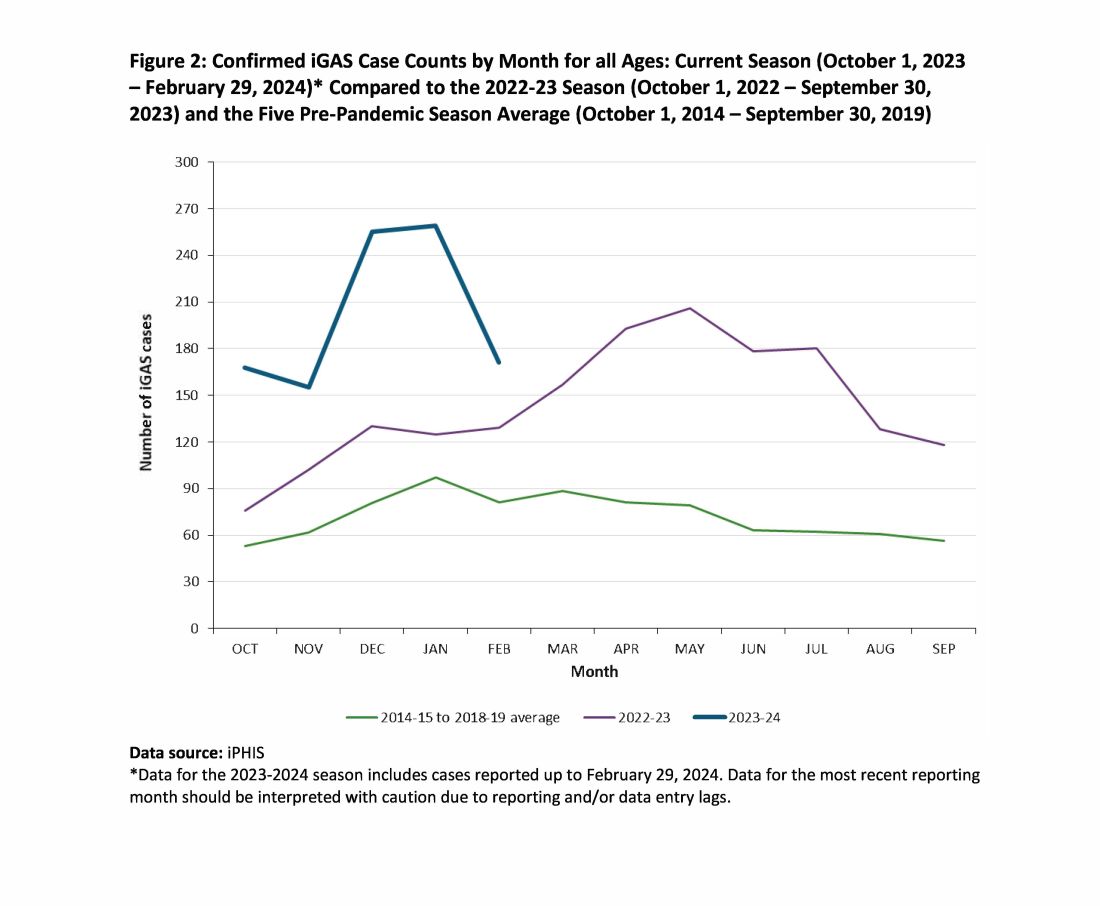
Dr. Harrison is professor of pediatrics and pediatric infectious diseases at Children’s Mercy Hospitals and Clinics, Kansas City, Mo. He said he had no relevant financial disclosures. Email him at pdnews@mdedge.com.
References
1. Current Group A Strep Activity, Centers for Disease Control and Prevention. April 2024. CDC webpage on current invasive GAS disease. April 2024.
2. Li Y et al. Expansion of Invasive Group A Streptococcus M1UK Lineage in Active Bacterial Core Surveillance, United States, 2019-2021 Emerg Infect Dis. 2023;29(10):2116-2120. doi: 10.3201/eid2910.230675.
3. Andreoni F et al. Clindamycin Affects Group A Streptococcus Virulence Factors and Improves Clinical Outcome. J Infect Dis. 2017 Jan 15;215(2):269-277. doi: 10.1093/infdis/jiw229.
4. Group A Streptococcal Disease, Invasive (iGAS), Public Health Ontario.
Invasive group A streptococcus (iGAS) infections are rare (4-9 cases/100,000 US population annually) but potentially devastating (approximately 2,300 deaths annually in US), and affect all ages. Cases increase in winter-spring, paralleling the “season” of increased noninvasive GAS, e.g., pharyngitis and scarlet fever. iGAS case rates are lower in children than adults. That said, one well-known pediatric iGAS scenario has been deep cellulitis and necrotizing fasciitis during the healing phase of varicella. Other forms of iGAS include bacteremia, pneumonia (particularly when empyema is present), lymphangitis, erysipelas, and toxic shock syndrome. iGAS can occur with/after influenza but has also occurred concurrently with other viral respiratory infections.
Persons with underlying conditions (cancer or immune compromised status; chronic diseases of the heart, kidney or lung; diabetes mellitus) are at higher risk. Other subpopulations at risk for iGAS are illicit drug users, the elderly, homeless persons, nursing home residents, American Indian persons, and Alaska Native persons. Most experts feel that highly toxigenic strains of GAS are responsible for most iGAS. Indeed, most iGAS isolates produce (sometimes hyper-produce) superantigens that cause exaggerated innate immune responses, higher levels of inflammation, and often times tissue destruction, e.g., “flesh eating bacteria.” And who can forget that Jim Henson, creator of the Muppets, died of iGAS?
But why discuss iGAS in 2024? The pattern for iGAS has fluctuated more than usual in the last decade. So much so that the recent upsurge has caught the collective eye of the lay press. So, patients and friends may have questions about why and how iGAS is increasing lately. The bottom line is that no one knows for sure. However, the most recent 2 years of uptick may reflect GAS circulating at relatively high levels even when taking into account that GAS season occurs in winter-spring most years. Yet it seems likely that additional factors may have played a role in the fluctuations noted this past decade, e.g., temporary changes in societal behavior, a new GAS strain with over two dozen mutations, and possibly rapid waning of protection against GAS exotoxins.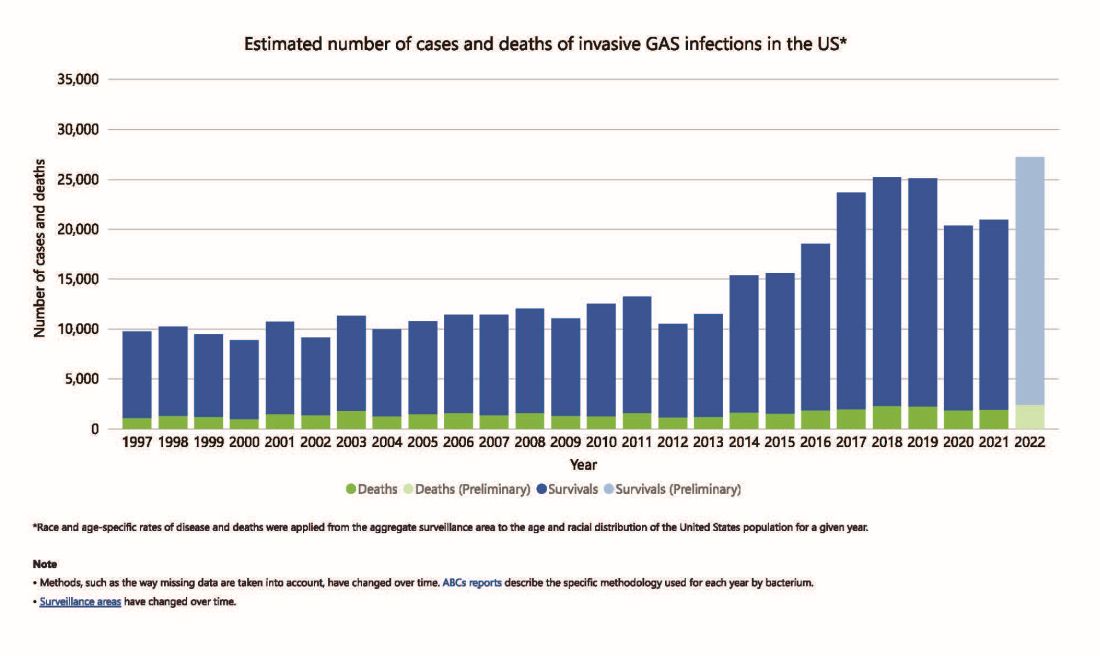
Social Behavior Factor
The SARS-CoV-2 pandemic brought extremes of disease and death to the world and dramatic changes in social behavior. A byproduct was dramatic decreases in nearly all infectious diseases, with numerous reports of near absence of many respiratory and gastrointestinal viruses in the 2020-2021 seasons. Interestingly, we did not see a drop in human rhinovirus infections, justifying its nickname as the cockroach of viruses. Reports also emerged about drops in bacterial diseases during 2020-2021 (although not so much for STIs), including noninvasive and invasive GAS disease, and also GAS-associated deaths (lowest since 2016).1 The drop in iGAS during social restrictions makes sense because GAS is spread by direct contact with infected persons or their secretions, and social contact had dramatically decreased particularly in the first 6 months of the pandemic.
However, since 2022 and the return to “normal” social behaviors, both viral diseases (e.g., RSV, influenza, and Norovirus), and some bacterial diseases have rebounded. That said, something else must be contributing, because iGAS rates had increased 4-5 years pre pandemic. In fact, the fluctuating pattern included “normal” annual rates in the early 2000s rising in ~2015 followed by the explainable pandemic drop (by nearly 25%), and not-too-unexpected 2-year postpandemic rise. But interestingly enough, the rebound is higher than might be expected for iGAS and children were overrepresented in first year’s rise (2022 rate for pediatric iGAS was the highest since 1997) while those older than 65 were overrepresented in second year (2023).1
Emergence of M1UK
One potential factor for the prepandemic rise in iGAS infections worldwide is the emergence and worldwide spread of a new GAS emm type variant designated M1UK.2 GAS isolates can be typed into categories designated as emm types based on DNA sequence. There are more than 240 emm types, with 6 being most common — M1, M3, and M28 (each up to 20% of GAS isolates) and M12, M82, and M89 (each up to 10%). M1, M3 and M28 have also been particularly associated with invasive disease. While emm types vary year to year and region by region, the overall emm type distribution among iGAS isolates in the United States had not been unusual since the turn of the century and the US M1 strain was the same as that which had been predominant worldwide (designated M1GLOBAL). This new M1UK sublineage had emerged around 2010 and had been increasing pre pandemic. The M1UK sequence contained a specific set of 27 SNPs (single nucleoside polymorphisms, i.e., single base mutations) and was associated with an uptick in scarlet fever in the United Kingdom starting around 2010. Its prevalence increased up to around 2015 while spreading internationally. It also had enhanced expression of SpeA, a phage-encoded superantigen. Some of the M1UK mutations also appear to alter GAS metabolic processes to allow better survival (better “fitness”) compared with other GAS. So, a more virulent hardier GAS had arisen and seems a reasonable candidate for contributing to the increased iGAS rates.
Waning Antibody to GAS As Potential Factor in Rebound
No consensus exists on correlates of protection from iGAS. However, adults seem to have less noninvasive GAS than children. One potential reason is that frequent GAS re-exposure, regardless of whether disease results, likely boosts anti-GAS antibodies. Pandemic social restrictions temporarily prevented such boosts. In children with developing antibody repertoires, anti-GAS antibodies may have waned below protective levels faster during a year without frequent boosting. Thus, children were iGAS susceptible soon after pandemic restrictions were dropped (2022). Increased iGAS rates in the elderly in 2023 may have occurred because of diminished GAS exposures accelerating immune senescence with anti-GAS antibodies dropping, but less quickly than in children. These speculations are simply hypotheses until future studies can test them.
All that said, how do we use information on increased iGAS in our daily practices? In addition to standard preventive strategies for viral coinfections (e.g., varicella and influenza vaccine), reminding families about rigorous attention to wound care is the one high-risk scenario we have not yet discussed. During 2024, a time of expected increased prevalence of iGAS, early wound care needs to be fastidious. Further, share warning signs with families (e.g., rapidly expanding painful erythema), “streaks” ascending from extremity wounds, fever and a highly painful wound, darkening almost purple color within cellulitis or soft tissue infection, or loss of sensation in the middle of an otherwise painful soft tissue infection. These presentations require immediate medical attention.
If such a patient presents, the Centers for Disease Control and Prevention (CDC) recommends admission along with blood and, where possible, wound cultures. If in the context of pneumonia with pleural effusion, culturing pleural fluid is also important. Remember, leading edge cultures are not often positive for GAS, seemingly because GAS exotoxins are found at erythema’s leading edge, not the bacteria. The bacteria are somewhere more central in the inflammatory process. Despite not being prominent among recent iGAS cases, another scenario that could sneak up on you is the infected surgical wound as nascent iGAS.
Finally, remember that nationally increasing numbers of iGAS isolates are resistant to erythromycin and clindamycin, the latter usually recommended to reduce tissue damage in iGAS.3 So, it is important to be aware of susceptibility patterns in your locale and consider an ID consultation. My hope is that you do not see an iGAS case this year, but we all need to remain alert. With a high index of suspicion and rapid diagnosis, you can minimize long-term sequelae and potential fatalities.
While it is too early to tell how the rest of 2024 will turn out, preliminary indications are that GAS is circulating at higher than usual levels (30%-35% GAS positive throat swabs in early April 2024 in Kansas City area) and iGAS rates will likely also be relatively high, particularly if Ontario, Canada, data are any indication.4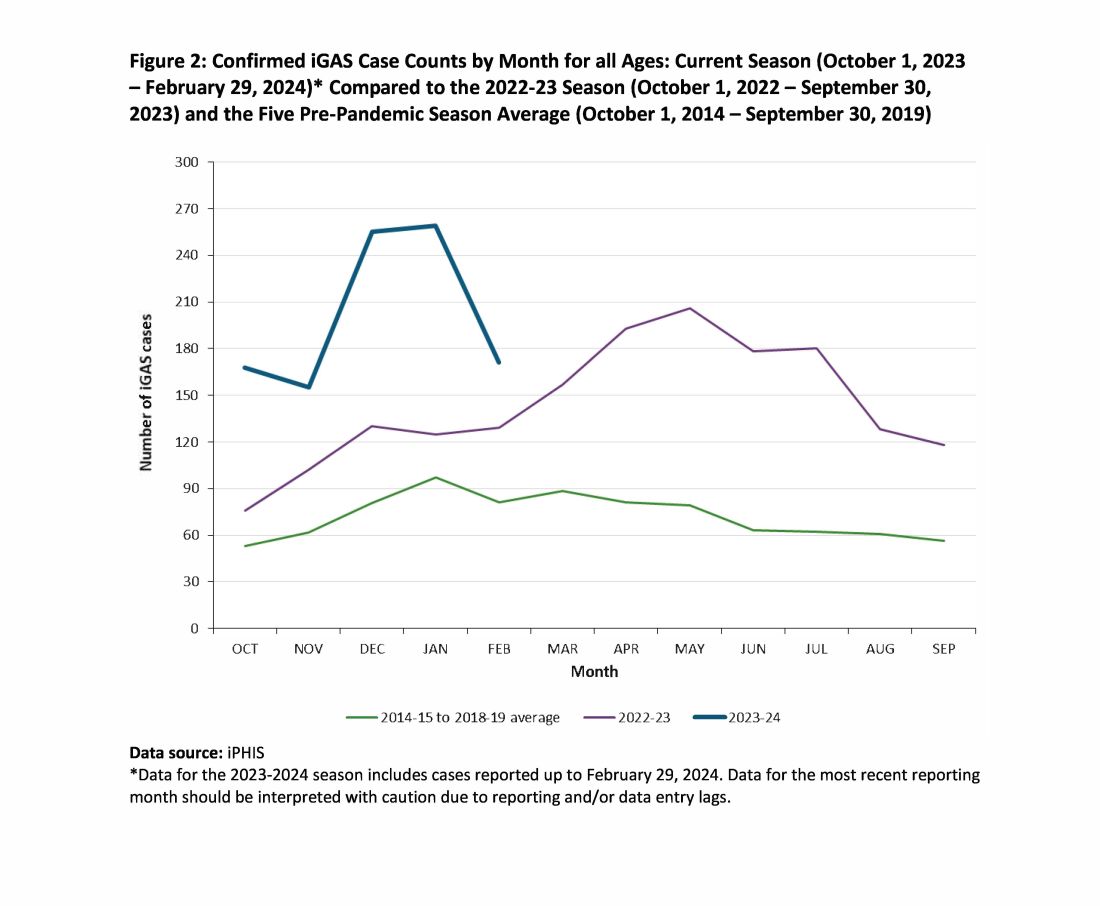
Dr. Harrison is professor of pediatrics and pediatric infectious diseases at Children’s Mercy Hospitals and Clinics, Kansas City, Mo. He said he had no relevant financial disclosures. Email him at pdnews@mdedge.com.
References
1. Current Group A Strep Activity, Centers for Disease Control and Prevention. April 2024. CDC webpage on current invasive GAS disease. April 2024.
2. Li Y et al. Expansion of Invasive Group A Streptococcus M1UK Lineage in Active Bacterial Core Surveillance, United States, 2019-2021 Emerg Infect Dis. 2023;29(10):2116-2120. doi: 10.3201/eid2910.230675.
3. Andreoni F et al. Clindamycin Affects Group A Streptococcus Virulence Factors and Improves Clinical Outcome. J Infect Dis. 2017 Jan 15;215(2):269-277. doi: 10.1093/infdis/jiw229.
4. Group A Streptococcal Disease, Invasive (iGAS), Public Health Ontario.
Invasive group A streptococcus (iGAS) infections are rare (4-9 cases/100,000 US population annually) but potentially devastating (approximately 2,300 deaths annually in US), and affect all ages. Cases increase in winter-spring, paralleling the “season” of increased noninvasive GAS, e.g., pharyngitis and scarlet fever. iGAS case rates are lower in children than adults. That said, one well-known pediatric iGAS scenario has been deep cellulitis and necrotizing fasciitis during the healing phase of varicella. Other forms of iGAS include bacteremia, pneumonia (particularly when empyema is present), lymphangitis, erysipelas, and toxic shock syndrome. iGAS can occur with/after influenza but has also occurred concurrently with other viral respiratory infections.
Persons with underlying conditions (cancer or immune compromised status; chronic diseases of the heart, kidney or lung; diabetes mellitus) are at higher risk. Other subpopulations at risk for iGAS are illicit drug users, the elderly, homeless persons, nursing home residents, American Indian persons, and Alaska Native persons. Most experts feel that highly toxigenic strains of GAS are responsible for most iGAS. Indeed, most iGAS isolates produce (sometimes hyper-produce) superantigens that cause exaggerated innate immune responses, higher levels of inflammation, and often times tissue destruction, e.g., “flesh eating bacteria.” And who can forget that Jim Henson, creator of the Muppets, died of iGAS?
But why discuss iGAS in 2024? The pattern for iGAS has fluctuated more than usual in the last decade. So much so that the recent upsurge has caught the collective eye of the lay press. So, patients and friends may have questions about why and how iGAS is increasing lately. The bottom line is that no one knows for sure. However, the most recent 2 years of uptick may reflect GAS circulating at relatively high levels even when taking into account that GAS season occurs in winter-spring most years. Yet it seems likely that additional factors may have played a role in the fluctuations noted this past decade, e.g., temporary changes in societal behavior, a new GAS strain with over two dozen mutations, and possibly rapid waning of protection against GAS exotoxins.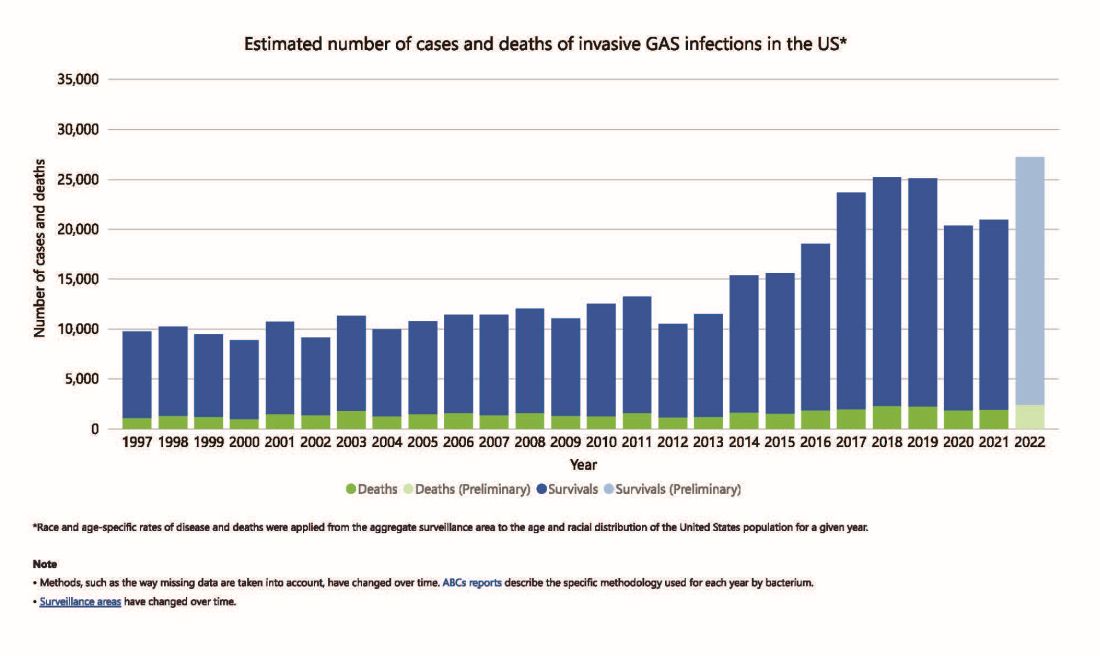
Social Behavior Factor
The SARS-CoV-2 pandemic brought extremes of disease and death to the world and dramatic changes in social behavior. A byproduct was dramatic decreases in nearly all infectious diseases, with numerous reports of near absence of many respiratory and gastrointestinal viruses in the 2020-2021 seasons. Interestingly, we did not see a drop in human rhinovirus infections, justifying its nickname as the cockroach of viruses. Reports also emerged about drops in bacterial diseases during 2020-2021 (although not so much for STIs), including noninvasive and invasive GAS disease, and also GAS-associated deaths (lowest since 2016).1 The drop in iGAS during social restrictions makes sense because GAS is spread by direct contact with infected persons or their secretions, and social contact had dramatically decreased particularly in the first 6 months of the pandemic.
However, since 2022 and the return to “normal” social behaviors, both viral diseases (e.g., RSV, influenza, and Norovirus), and some bacterial diseases have rebounded. That said, something else must be contributing, because iGAS rates had increased 4-5 years pre pandemic. In fact, the fluctuating pattern included “normal” annual rates in the early 2000s rising in ~2015 followed by the explainable pandemic drop (by nearly 25%), and not-too-unexpected 2-year postpandemic rise. But interestingly enough, the rebound is higher than might be expected for iGAS and children were overrepresented in first year’s rise (2022 rate for pediatric iGAS was the highest since 1997) while those older than 65 were overrepresented in second year (2023).1
Emergence of M1UK
One potential factor for the prepandemic rise in iGAS infections worldwide is the emergence and worldwide spread of a new GAS emm type variant designated M1UK.2 GAS isolates can be typed into categories designated as emm types based on DNA sequence. There are more than 240 emm types, with 6 being most common — M1, M3, and M28 (each up to 20% of GAS isolates) and M12, M82, and M89 (each up to 10%). M1, M3 and M28 have also been particularly associated with invasive disease. While emm types vary year to year and region by region, the overall emm type distribution among iGAS isolates in the United States had not been unusual since the turn of the century and the US M1 strain was the same as that which had been predominant worldwide (designated M1GLOBAL). This new M1UK sublineage had emerged around 2010 and had been increasing pre pandemic. The M1UK sequence contained a specific set of 27 SNPs (single nucleoside polymorphisms, i.e., single base mutations) and was associated with an uptick in scarlet fever in the United Kingdom starting around 2010. Its prevalence increased up to around 2015 while spreading internationally. It also had enhanced expression of SpeA, a phage-encoded superantigen. Some of the M1UK mutations also appear to alter GAS metabolic processes to allow better survival (better “fitness”) compared with other GAS. So, a more virulent hardier GAS had arisen and seems a reasonable candidate for contributing to the increased iGAS rates.
Waning Antibody to GAS As Potential Factor in Rebound
No consensus exists on correlates of protection from iGAS. However, adults seem to have less noninvasive GAS than children. One potential reason is that frequent GAS re-exposure, regardless of whether disease results, likely boosts anti-GAS antibodies. Pandemic social restrictions temporarily prevented such boosts. In children with developing antibody repertoires, anti-GAS antibodies may have waned below protective levels faster during a year without frequent boosting. Thus, children were iGAS susceptible soon after pandemic restrictions were dropped (2022). Increased iGAS rates in the elderly in 2023 may have occurred because of diminished GAS exposures accelerating immune senescence with anti-GAS antibodies dropping, but less quickly than in children. These speculations are simply hypotheses until future studies can test them.
All that said, how do we use information on increased iGAS in our daily practices? In addition to standard preventive strategies for viral coinfections (e.g., varicella and influenza vaccine), reminding families about rigorous attention to wound care is the one high-risk scenario we have not yet discussed. During 2024, a time of expected increased prevalence of iGAS, early wound care needs to be fastidious. Further, share warning signs with families (e.g., rapidly expanding painful erythema), “streaks” ascending from extremity wounds, fever and a highly painful wound, darkening almost purple color within cellulitis or soft tissue infection, or loss of sensation in the middle of an otherwise painful soft tissue infection. These presentations require immediate medical attention.
If such a patient presents, the Centers for Disease Control and Prevention (CDC) recommends admission along with blood and, where possible, wound cultures. If in the context of pneumonia with pleural effusion, culturing pleural fluid is also important. Remember, leading edge cultures are not often positive for GAS, seemingly because GAS exotoxins are found at erythema’s leading edge, not the bacteria. The bacteria are somewhere more central in the inflammatory process. Despite not being prominent among recent iGAS cases, another scenario that could sneak up on you is the infected surgical wound as nascent iGAS.
Finally, remember that nationally increasing numbers of iGAS isolates are resistant to erythromycin and clindamycin, the latter usually recommended to reduce tissue damage in iGAS.3 So, it is important to be aware of susceptibility patterns in your locale and consider an ID consultation. My hope is that you do not see an iGAS case this year, but we all need to remain alert. With a high index of suspicion and rapid diagnosis, you can minimize long-term sequelae and potential fatalities.
While it is too early to tell how the rest of 2024 will turn out, preliminary indications are that GAS is circulating at higher than usual levels (30%-35% GAS positive throat swabs in early April 2024 in Kansas City area) and iGAS rates will likely also be relatively high, particularly if Ontario, Canada, data are any indication.4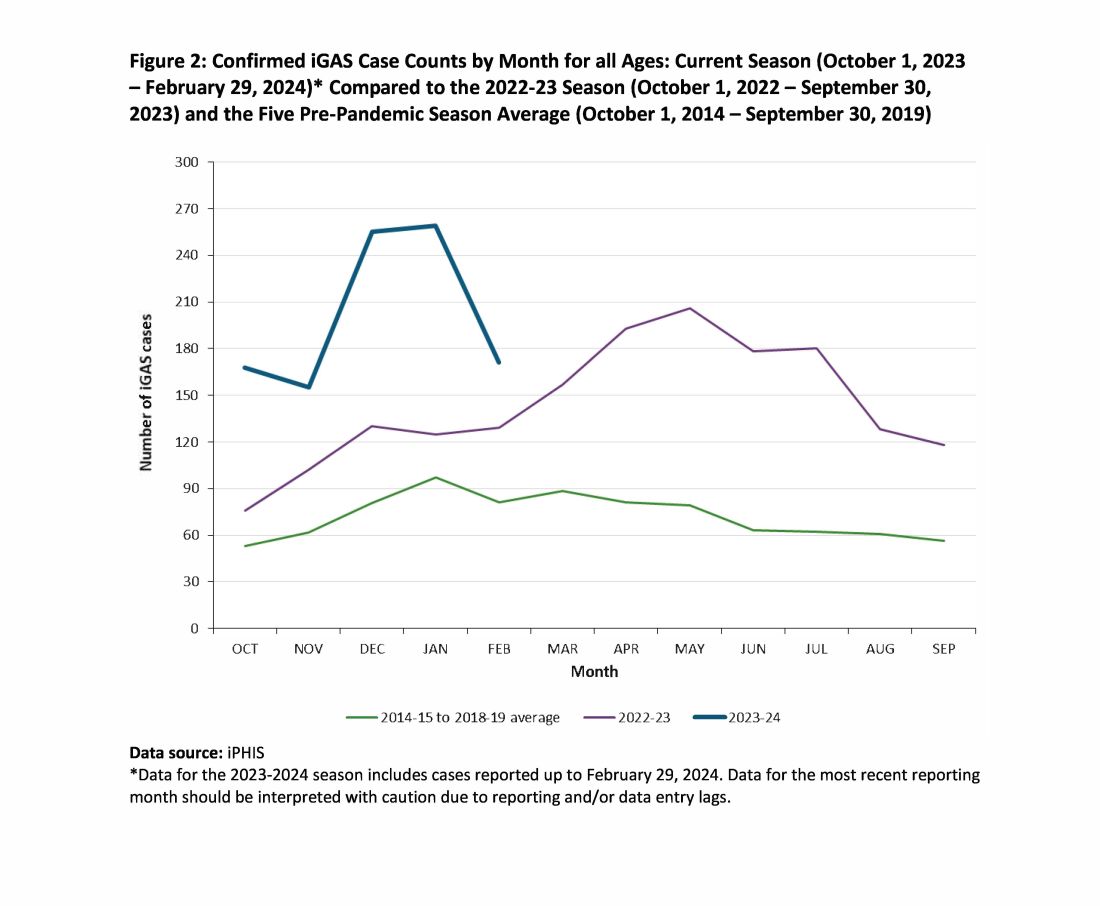
Dr. Harrison is professor of pediatrics and pediatric infectious diseases at Children’s Mercy Hospitals and Clinics, Kansas City, Mo. He said he had no relevant financial disclosures. Email him at pdnews@mdedge.com.
References
1. Current Group A Strep Activity, Centers for Disease Control and Prevention. April 2024. CDC webpage on current invasive GAS disease. April 2024.
2. Li Y et al. Expansion of Invasive Group A Streptococcus M1UK Lineage in Active Bacterial Core Surveillance, United States, 2019-2021 Emerg Infect Dis. 2023;29(10):2116-2120. doi: 10.3201/eid2910.230675.
3. Andreoni F et al. Clindamycin Affects Group A Streptococcus Virulence Factors and Improves Clinical Outcome. J Infect Dis. 2017 Jan 15;215(2):269-277. doi: 10.1093/infdis/jiw229.
4. Group A Streptococcal Disease, Invasive (iGAS), Public Health Ontario.
One-Minute Speech Test Could Help Assess Dementia Risk
BUDAPEST, HUNGARY — , suggests research.
János Kálmán, MD, PhD, and colleagues at the University of Szeged in Hungary have developed an automated speech analysis approach called the Speech-Gap Test (S-GAP Test) that is unique because it focuses on the temporal changes made when someone talks. This means it does not overcomplicate matters by also assessing the phonetics and semantics of speech, Dr. Kálmán said.
Dr. Kálmán presented his findings at the 32nd European Congress of Psychiatry.
Temporal Speech Parameters
The test analyzes parameters such as how quickly someone speaks, whether they hesitate when they talk, how long the hesitation lasts, and how many silent pauses they make. This can be done with a mere 60-second sample of speech, Dr. Kálmán said, noting that other automated speech and language tools currently in development need much longer audio samples.
“We tried different approaches and we finally ended up with the temporal speech parameters because these are not culture-dependent, not education-dependent, and could be more reliable than the semantic parts of [speech] analysis,” he explained.
The analysis of temporal speech parameters is also not language-dependent. Although the S-GAP Test was developed using audio samples from native Hungarian speakers, Dr. Kálmán and his collaborators have shown that it works just as well with samples from native English and German speakers. They now plan to validate the test further using samples from native Spanish speakers.
For Screening, Not Diagnosis
Currently, “the only purpose of this tool would be initial screening,” Dr. Kálmán said at the congress. It is not for diagnosis, and there is no intention to get it registered as a medical device.
A national survey of primary care physicians conducted by Dr. Kálmán and collaborators showed that there was little time for performing standard cognitive tests during the average consultation. Thus, the original idea was that the S-GAP Test would be an aid to help primary care physicians quickly flag whether a patient might have cognitive problems that needed further assessment at a memory clinic or by more specialist neurology services.
The goalposts have since been moved, from developing a pure telemedicine solution to a more widespread application that perhaps anyone could buy and download from the internet or using a smartphone.
Dr. Kálmán doesn’t discount developing a more sophisticated version of the S-GAP Test in the future that combines temporal speech parameters with biomarkers for mild cognitive impairment or Alzheimer’s disease and could be used in memory clinics and by neurologists for the purpose of diagnosis.
Detect to Prevent?
The big question is: What happens to all the people that could be flagged as needing further assessment using tools such as the S-GAP Test?
Tackling risk factors for dementia will probably be key, said Robert Perneckzy, MD, MBA, professor of translational dementia research at Ludwig Maximilian University of Munich, Imperial College London, and the University of Sheffield.
According to the Lancet Commission on dementia, there are 12 potentially modifiable risk factors for dementia. Their influence varies throughout the life course, but certain early events, such as the level of education attained, can’t be modified in an older patient.
That said, there are many risk factors that might still be influenced later in life, such as adequately treating comorbid conditions such as diabetes, and addressing alcohol consumption and smoking practices.
“We can do things in terms of personal risk, risk mitigation, which have a huge effect on dementia risk much later in life,” said Dr. Perneckzy.
“The speech-based assessments are another opportunity to save our time as doctors to do assessments before someone comes to the memory clinic,” he said.
The S-GAP Test is under development by the University of Szeged. Dr. Kálmán is a co-inventor. Dr. Perneckzy had no relevant conflicts of interest but has helped validate the S-GAP Test in the German language.
A version of this article appeared on Medscape.com.
BUDAPEST, HUNGARY — , suggests research.
János Kálmán, MD, PhD, and colleagues at the University of Szeged in Hungary have developed an automated speech analysis approach called the Speech-Gap Test (S-GAP Test) that is unique because it focuses on the temporal changes made when someone talks. This means it does not overcomplicate matters by also assessing the phonetics and semantics of speech, Dr. Kálmán said.
Dr. Kálmán presented his findings at the 32nd European Congress of Psychiatry.
Temporal Speech Parameters
The test analyzes parameters such as how quickly someone speaks, whether they hesitate when they talk, how long the hesitation lasts, and how many silent pauses they make. This can be done with a mere 60-second sample of speech, Dr. Kálmán said, noting that other automated speech and language tools currently in development need much longer audio samples.
“We tried different approaches and we finally ended up with the temporal speech parameters because these are not culture-dependent, not education-dependent, and could be more reliable than the semantic parts of [speech] analysis,” he explained.
The analysis of temporal speech parameters is also not language-dependent. Although the S-GAP Test was developed using audio samples from native Hungarian speakers, Dr. Kálmán and his collaborators have shown that it works just as well with samples from native English and German speakers. They now plan to validate the test further using samples from native Spanish speakers.
For Screening, Not Diagnosis
Currently, “the only purpose of this tool would be initial screening,” Dr. Kálmán said at the congress. It is not for diagnosis, and there is no intention to get it registered as a medical device.
A national survey of primary care physicians conducted by Dr. Kálmán and collaborators showed that there was little time for performing standard cognitive tests during the average consultation. Thus, the original idea was that the S-GAP Test would be an aid to help primary care physicians quickly flag whether a patient might have cognitive problems that needed further assessment at a memory clinic or by more specialist neurology services.
The goalposts have since been moved, from developing a pure telemedicine solution to a more widespread application that perhaps anyone could buy and download from the internet or using a smartphone.
Dr. Kálmán doesn’t discount developing a more sophisticated version of the S-GAP Test in the future that combines temporal speech parameters with biomarkers for mild cognitive impairment or Alzheimer’s disease and could be used in memory clinics and by neurologists for the purpose of diagnosis.
Detect to Prevent?
The big question is: What happens to all the people that could be flagged as needing further assessment using tools such as the S-GAP Test?
Tackling risk factors for dementia will probably be key, said Robert Perneckzy, MD, MBA, professor of translational dementia research at Ludwig Maximilian University of Munich, Imperial College London, and the University of Sheffield.
According to the Lancet Commission on dementia, there are 12 potentially modifiable risk factors for dementia. Their influence varies throughout the life course, but certain early events, such as the level of education attained, can’t be modified in an older patient.
That said, there are many risk factors that might still be influenced later in life, such as adequately treating comorbid conditions such as diabetes, and addressing alcohol consumption and smoking practices.
“We can do things in terms of personal risk, risk mitigation, which have a huge effect on dementia risk much later in life,” said Dr. Perneckzy.
“The speech-based assessments are another opportunity to save our time as doctors to do assessments before someone comes to the memory clinic,” he said.
The S-GAP Test is under development by the University of Szeged. Dr. Kálmán is a co-inventor. Dr. Perneckzy had no relevant conflicts of interest but has helped validate the S-GAP Test in the German language.
A version of this article appeared on Medscape.com.
BUDAPEST, HUNGARY — , suggests research.
János Kálmán, MD, PhD, and colleagues at the University of Szeged in Hungary have developed an automated speech analysis approach called the Speech-Gap Test (S-GAP Test) that is unique because it focuses on the temporal changes made when someone talks. This means it does not overcomplicate matters by also assessing the phonetics and semantics of speech, Dr. Kálmán said.
Dr. Kálmán presented his findings at the 32nd European Congress of Psychiatry.
Temporal Speech Parameters
The test analyzes parameters such as how quickly someone speaks, whether they hesitate when they talk, how long the hesitation lasts, and how many silent pauses they make. This can be done with a mere 60-second sample of speech, Dr. Kálmán said, noting that other automated speech and language tools currently in development need much longer audio samples.
“We tried different approaches and we finally ended up with the temporal speech parameters because these are not culture-dependent, not education-dependent, and could be more reliable than the semantic parts of [speech] analysis,” he explained.
The analysis of temporal speech parameters is also not language-dependent. Although the S-GAP Test was developed using audio samples from native Hungarian speakers, Dr. Kálmán and his collaborators have shown that it works just as well with samples from native English and German speakers. They now plan to validate the test further using samples from native Spanish speakers.
For Screening, Not Diagnosis
Currently, “the only purpose of this tool would be initial screening,” Dr. Kálmán said at the congress. It is not for diagnosis, and there is no intention to get it registered as a medical device.
A national survey of primary care physicians conducted by Dr. Kálmán and collaborators showed that there was little time for performing standard cognitive tests during the average consultation. Thus, the original idea was that the S-GAP Test would be an aid to help primary care physicians quickly flag whether a patient might have cognitive problems that needed further assessment at a memory clinic or by more specialist neurology services.
The goalposts have since been moved, from developing a pure telemedicine solution to a more widespread application that perhaps anyone could buy and download from the internet or using a smartphone.
Dr. Kálmán doesn’t discount developing a more sophisticated version of the S-GAP Test in the future that combines temporal speech parameters with biomarkers for mild cognitive impairment or Alzheimer’s disease and could be used in memory clinics and by neurologists for the purpose of diagnosis.
Detect to Prevent?
The big question is: What happens to all the people that could be flagged as needing further assessment using tools such as the S-GAP Test?
Tackling risk factors for dementia will probably be key, said Robert Perneckzy, MD, MBA, professor of translational dementia research at Ludwig Maximilian University of Munich, Imperial College London, and the University of Sheffield.
According to the Lancet Commission on dementia, there are 12 potentially modifiable risk factors for dementia. Their influence varies throughout the life course, but certain early events, such as the level of education attained, can’t be modified in an older patient.
That said, there are many risk factors that might still be influenced later in life, such as adequately treating comorbid conditions such as diabetes, and addressing alcohol consumption and smoking practices.
“We can do things in terms of personal risk, risk mitigation, which have a huge effect on dementia risk much later in life,” said Dr. Perneckzy.
“The speech-based assessments are another opportunity to save our time as doctors to do assessments before someone comes to the memory clinic,” he said.
The S-GAP Test is under development by the University of Szeged. Dr. Kálmán is a co-inventor. Dr. Perneckzy had no relevant conflicts of interest but has helped validate the S-GAP Test in the German language.
A version of this article appeared on Medscape.com.
FROM THE EUROPEAN CONGRESS OF PSYCHIATRY






