User login
Mediterranean diet linked to lower risk for preeclampsia
Pregnant women who had a higher adherence to a Mediterranean-style diet had a lower risk of preeclampsia, according to the results of a new study.
“As an observational study, it obviously has limitations that need to be considered, but these results build on other evidence that Mediterranean diet reduces cardiovascular risk and extends those findings to pregnancy as preeclampsia is a cardiovascular outcome,” senior author Noel T. Mueller, PhD, associate professor at Johns Hopkins Bloomberg School of Public Health, Baltimore, said in an interview.
The study was published online April 20 in the Journal of the American Heart Association.
The authors noted that preeclampsia, characterized by a range of symptoms including hypertension, proteinuria, and end-organ dysfunction, is a disorder that occurs in up to 5%-10% of all pregnant women worldwide, and is more common in Black women. It is a major cause of maternal and fetal morbidity and raises the risk for long-term cardiovascular disease (CVD), including chronic hypertension, coronary artery disease, ischemic stroke, and heart failure.
Children born to mothers with preeclampsia are at an elevated risk of having higher blood pressure and other abnormal cardiometabolic parameters.
The authors noted that multiple studies have demonstrated the benefit of the Mediterranean diet – characterized primarily by high intake of vegetables, fruits, and unsaturated fats – in reducing cardiovascular risk in the nonpregnant population. The current study was conducted to investigate whether benefits could also be seen in pregnant women in the form of a reduced risk of preeclampsia.
For the study, which used data from the Boston Birth Cohort, maternal sociodemographic and dietary data were obtained from 8,507 women via interview and food frequency questionnaire within 24-72 hours of giving birth. A Mediterranean-style diet score was calculated from the food frequency questionnaire. Additional clinical information, including physician diagnoses of preexisting conditions and preeclampsia, were extracted from medical records.
Of the women in the sample, 848 developed preeclampsia, of whom 47% were Black, and 28% were Hispanic.
After multivariable adjustment, the greatest adherence to a Mediterranean-style diet was associated with lower odds of developing preeclampsia (adjusted odds ratio comparing tertile 3 to tertile 1, 0.78; 95% confidence interval [CI], 0.64-0.96).
A subgroup analysis of Black women demonstrated a similar benefit with an adjusted odds ratio comparing tertile 3 to tertile 1 of 0.74 (95% CI, 0.76-0.96).
“In this racially and ethnically diverse cohort, women who had greater adherence to a Mediterranean-style diet during pregnancy had a greater than 20% lower odds of developing preeclampsia, after [adjustment] for potential confounders. In addition, the evidence for the protective effect of a Mediterranean-style diet against the odds of developing preeclampsia remained present in a subgroup analysis of Black women,” the researchers concluded.
Asked whether this would be enough evidence to recommend a Mediterranean diet to pregnant women, Dr. Mueller said that the organizations that issue dietary guidelines would probably require replication of these results and also possibly a randomized trial in a diverse population group before advocating such a diet.
“That is something we would like to do but this will take time and money,” he added.
Lead study author Anum Minhas, MD, Johns Hopkins University, Baltimore, said that in the meantime she would be recommending a Mediterranean diet to her pregnant patients.
“The Mediterranean diet is a very healthy way of eating. I can’t see any downside of following such a diet in pregnancy, especially for high-risk women – those with obesity, hypertension or gestational diabetes, and there are likely other potential benefits such as reduced weight gain and reduced gestational diabetes,” she said.
Dr. Mueller said he appreciated this pragmatic approach. “Sometimes there can be hesitation on making recommendations from observational studies, but the alternative to recommending this diet is either no recommendations on diet or recommending an alternative diet,” he said. “The Mediterranean diet or the DASH diet, which is quite similar, have shown by far the most evidence of cardioprotection of any diets. They have been shown to reduce blood pressure and lipids and improve cardiovascular risk, and I think we can now assume that that likely extends to pregnancy. I feel comfortable for this diet to be recommended to pregnant women.”
But he added: “Having said that, there is still a need for a randomized trial in pregnancy. We think it works but until we have a randomized trial we won’t know for sure, and we won’t know how much of a benefit we can get.”
Commenting on the study, JoAnn Manson, MD, chief of the division of preventive medicine at Brigham and Women’s Hospital, Boston, pointed out that this type of observational study is important for hypothesis generation but cannot prove cause and effect relationships.
“The evidence is promising enough,” said Dr. Manson, who was not involved with this study. But she added that to move forward, a randomized trial in women at elevated risk of preeclampsia would be needed, beginning in early pregnancy, if not earlier.
“In the meantime,” she noted, “several large-scale cohorts could be leveraged to look at diet assessed before or during pregnancy to see if this dietary pattern is prospectively related to lower risk of preeclampsia.
“With additional supportive data, and in view of the diet’s safety and general cardiovascular benefits, it could become a major tool for preventing adverse pregnancy outcomes.”
The Boston Birth Cohort study was supported in part by grants from the March of Dimes, the National Institutes of Health, and the Health Resources and Services Administration of the U.S. Department of Health and Human Services. The authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Pregnant women who had a higher adherence to a Mediterranean-style diet had a lower risk of preeclampsia, according to the results of a new study.
“As an observational study, it obviously has limitations that need to be considered, but these results build on other evidence that Mediterranean diet reduces cardiovascular risk and extends those findings to pregnancy as preeclampsia is a cardiovascular outcome,” senior author Noel T. Mueller, PhD, associate professor at Johns Hopkins Bloomberg School of Public Health, Baltimore, said in an interview.
The study was published online April 20 in the Journal of the American Heart Association.
The authors noted that preeclampsia, characterized by a range of symptoms including hypertension, proteinuria, and end-organ dysfunction, is a disorder that occurs in up to 5%-10% of all pregnant women worldwide, and is more common in Black women. It is a major cause of maternal and fetal morbidity and raises the risk for long-term cardiovascular disease (CVD), including chronic hypertension, coronary artery disease, ischemic stroke, and heart failure.
Children born to mothers with preeclampsia are at an elevated risk of having higher blood pressure and other abnormal cardiometabolic parameters.
The authors noted that multiple studies have demonstrated the benefit of the Mediterranean diet – characterized primarily by high intake of vegetables, fruits, and unsaturated fats – in reducing cardiovascular risk in the nonpregnant population. The current study was conducted to investigate whether benefits could also be seen in pregnant women in the form of a reduced risk of preeclampsia.
For the study, which used data from the Boston Birth Cohort, maternal sociodemographic and dietary data were obtained from 8,507 women via interview and food frequency questionnaire within 24-72 hours of giving birth. A Mediterranean-style diet score was calculated from the food frequency questionnaire. Additional clinical information, including physician diagnoses of preexisting conditions and preeclampsia, were extracted from medical records.
Of the women in the sample, 848 developed preeclampsia, of whom 47% were Black, and 28% were Hispanic.
After multivariable adjustment, the greatest adherence to a Mediterranean-style diet was associated with lower odds of developing preeclampsia (adjusted odds ratio comparing tertile 3 to tertile 1, 0.78; 95% confidence interval [CI], 0.64-0.96).
A subgroup analysis of Black women demonstrated a similar benefit with an adjusted odds ratio comparing tertile 3 to tertile 1 of 0.74 (95% CI, 0.76-0.96).
“In this racially and ethnically diverse cohort, women who had greater adherence to a Mediterranean-style diet during pregnancy had a greater than 20% lower odds of developing preeclampsia, after [adjustment] for potential confounders. In addition, the evidence for the protective effect of a Mediterranean-style diet against the odds of developing preeclampsia remained present in a subgroup analysis of Black women,” the researchers concluded.
Asked whether this would be enough evidence to recommend a Mediterranean diet to pregnant women, Dr. Mueller said that the organizations that issue dietary guidelines would probably require replication of these results and also possibly a randomized trial in a diverse population group before advocating such a diet.
“That is something we would like to do but this will take time and money,” he added.
Lead study author Anum Minhas, MD, Johns Hopkins University, Baltimore, said that in the meantime she would be recommending a Mediterranean diet to her pregnant patients.
“The Mediterranean diet is a very healthy way of eating. I can’t see any downside of following such a diet in pregnancy, especially for high-risk women – those with obesity, hypertension or gestational diabetes, and there are likely other potential benefits such as reduced weight gain and reduced gestational diabetes,” she said.
Dr. Mueller said he appreciated this pragmatic approach. “Sometimes there can be hesitation on making recommendations from observational studies, but the alternative to recommending this diet is either no recommendations on diet or recommending an alternative diet,” he said. “The Mediterranean diet or the DASH diet, which is quite similar, have shown by far the most evidence of cardioprotection of any diets. They have been shown to reduce blood pressure and lipids and improve cardiovascular risk, and I think we can now assume that that likely extends to pregnancy. I feel comfortable for this diet to be recommended to pregnant women.”
But he added: “Having said that, there is still a need for a randomized trial in pregnancy. We think it works but until we have a randomized trial we won’t know for sure, and we won’t know how much of a benefit we can get.”
Commenting on the study, JoAnn Manson, MD, chief of the division of preventive medicine at Brigham and Women’s Hospital, Boston, pointed out that this type of observational study is important for hypothesis generation but cannot prove cause and effect relationships.
“The evidence is promising enough,” said Dr. Manson, who was not involved with this study. But she added that to move forward, a randomized trial in women at elevated risk of preeclampsia would be needed, beginning in early pregnancy, if not earlier.
“In the meantime,” she noted, “several large-scale cohorts could be leveraged to look at diet assessed before or during pregnancy to see if this dietary pattern is prospectively related to lower risk of preeclampsia.
“With additional supportive data, and in view of the diet’s safety and general cardiovascular benefits, it could become a major tool for preventing adverse pregnancy outcomes.”
The Boston Birth Cohort study was supported in part by grants from the March of Dimes, the National Institutes of Health, and the Health Resources and Services Administration of the U.S. Department of Health and Human Services. The authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Pregnant women who had a higher adherence to a Mediterranean-style diet had a lower risk of preeclampsia, according to the results of a new study.
“As an observational study, it obviously has limitations that need to be considered, but these results build on other evidence that Mediterranean diet reduces cardiovascular risk and extends those findings to pregnancy as preeclampsia is a cardiovascular outcome,” senior author Noel T. Mueller, PhD, associate professor at Johns Hopkins Bloomberg School of Public Health, Baltimore, said in an interview.
The study was published online April 20 in the Journal of the American Heart Association.
The authors noted that preeclampsia, characterized by a range of symptoms including hypertension, proteinuria, and end-organ dysfunction, is a disorder that occurs in up to 5%-10% of all pregnant women worldwide, and is more common in Black women. It is a major cause of maternal and fetal morbidity and raises the risk for long-term cardiovascular disease (CVD), including chronic hypertension, coronary artery disease, ischemic stroke, and heart failure.
Children born to mothers with preeclampsia are at an elevated risk of having higher blood pressure and other abnormal cardiometabolic parameters.
The authors noted that multiple studies have demonstrated the benefit of the Mediterranean diet – characterized primarily by high intake of vegetables, fruits, and unsaturated fats – in reducing cardiovascular risk in the nonpregnant population. The current study was conducted to investigate whether benefits could also be seen in pregnant women in the form of a reduced risk of preeclampsia.
For the study, which used data from the Boston Birth Cohort, maternal sociodemographic and dietary data were obtained from 8,507 women via interview and food frequency questionnaire within 24-72 hours of giving birth. A Mediterranean-style diet score was calculated from the food frequency questionnaire. Additional clinical information, including physician diagnoses of preexisting conditions and preeclampsia, were extracted from medical records.
Of the women in the sample, 848 developed preeclampsia, of whom 47% were Black, and 28% were Hispanic.
After multivariable adjustment, the greatest adherence to a Mediterranean-style diet was associated with lower odds of developing preeclampsia (adjusted odds ratio comparing tertile 3 to tertile 1, 0.78; 95% confidence interval [CI], 0.64-0.96).
A subgroup analysis of Black women demonstrated a similar benefit with an adjusted odds ratio comparing tertile 3 to tertile 1 of 0.74 (95% CI, 0.76-0.96).
“In this racially and ethnically diverse cohort, women who had greater adherence to a Mediterranean-style diet during pregnancy had a greater than 20% lower odds of developing preeclampsia, after [adjustment] for potential confounders. In addition, the evidence for the protective effect of a Mediterranean-style diet against the odds of developing preeclampsia remained present in a subgroup analysis of Black women,” the researchers concluded.
Asked whether this would be enough evidence to recommend a Mediterranean diet to pregnant women, Dr. Mueller said that the organizations that issue dietary guidelines would probably require replication of these results and also possibly a randomized trial in a diverse population group before advocating such a diet.
“That is something we would like to do but this will take time and money,” he added.
Lead study author Anum Minhas, MD, Johns Hopkins University, Baltimore, said that in the meantime she would be recommending a Mediterranean diet to her pregnant patients.
“The Mediterranean diet is a very healthy way of eating. I can’t see any downside of following such a diet in pregnancy, especially for high-risk women – those with obesity, hypertension or gestational diabetes, and there are likely other potential benefits such as reduced weight gain and reduced gestational diabetes,” she said.
Dr. Mueller said he appreciated this pragmatic approach. “Sometimes there can be hesitation on making recommendations from observational studies, but the alternative to recommending this diet is either no recommendations on diet or recommending an alternative diet,” he said. “The Mediterranean diet or the DASH diet, which is quite similar, have shown by far the most evidence of cardioprotection of any diets. They have been shown to reduce blood pressure and lipids and improve cardiovascular risk, and I think we can now assume that that likely extends to pregnancy. I feel comfortable for this diet to be recommended to pregnant women.”
But he added: “Having said that, there is still a need for a randomized trial in pregnancy. We think it works but until we have a randomized trial we won’t know for sure, and we won’t know how much of a benefit we can get.”
Commenting on the study, JoAnn Manson, MD, chief of the division of preventive medicine at Brigham and Women’s Hospital, Boston, pointed out that this type of observational study is important for hypothesis generation but cannot prove cause and effect relationships.
“The evidence is promising enough,” said Dr. Manson, who was not involved with this study. But she added that to move forward, a randomized trial in women at elevated risk of preeclampsia would be needed, beginning in early pregnancy, if not earlier.
“In the meantime,” she noted, “several large-scale cohorts could be leveraged to look at diet assessed before or during pregnancy to see if this dietary pattern is prospectively related to lower risk of preeclampsia.
“With additional supportive data, and in view of the diet’s safety and general cardiovascular benefits, it could become a major tool for preventing adverse pregnancy outcomes.”
The Boston Birth Cohort study was supported in part by grants from the March of Dimes, the National Institutes of Health, and the Health Resources and Services Administration of the U.S. Department of Health and Human Services. The authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM THE JOURNAL OF THE AMERICAN HEART ASSOCIATION
Majority of pandemic pediatric visits managed with telemedicine
Approximately two-thirds of pediatric acute care concerns managed in telemedicine visits required no additional visits or follow-up, based on data from more than 600 visits.
The increase in use of telemedicine during the first year of the COVID-19 pandemic enabled access to care and connection to doctors for many pediatric patients, said Kristina Kissiova, MD, of Children’s National Health System, Washington, and colleagues. Some advantages of telemedicine include enhanced medical homes, reduced health care costs, and less crowding and wait time for patients in offices and emergency departments; however, the optimal use of telemedicine for acute primary care has not been examined, they said.
In a study presented at the annual meeting of the Pediatric Academic Societies, the researchers conducted a retrospective chart review of 638 acute care telemedicine visits conducted by 21 health care providers at a single practice in Washington in October 2020 and November 2020. Approximately half of the patients were male, 65% were white, and 89% had commercial insurance. The most common age group was 6-12 years (23%), followed by 2-3 years (16%), 3-6 years (15%), and 12-18 years (14%).
The primary outcome was the number and nature of visits completed via telemedicine without the need for referral or a subsequent in-person visit. Telemedicine visits for well-child checks and follow-up visits were excluded.
Overall, 60% of the visits (384 of 638) were completed over telemedicine with no need for additional visits or referrals. The most common acute complaints were upper respiratory infections, dermatologic issues, gastrointestinal issues, COVID-19 related issues, and fever (18.7%, 16.3%, 12.9%, 11.9%, and 10.3%, respectively).
Of these, dermatologic and GI concerns were most often completed via telemedicine (93.3% and 81.7%, respectively), while upper respiratory tract infections and fever issues were the least likely to be completed via telemedicine (22.7% and 13.6%), mainly because of the need to report for in-person COVID-19 testing, the researchers said.
Among other less common chief complaints, 100% of breathing concerns, behavior/mental health concerns, and head trauma or falls were addressed via telemedicine without additional referrals or follow-up visits. In addition, 90.9% of urgent care or emergency department follow-ups, 88.9% of ear concerns, and 87.5% of eye concerns were completely resolved via telemedicine visits.
Overall, 3% of patients who were not referred after a telemedicine visit presented in person for worsening symptoms. Of these who were referred after a telemedicine visit, 90% were seen in person within 48 hours.
The study findings were limited by the inclusion of data from only a single center. However, “These early findings provide insight into the utility of telehealth in the primary care setting for a broad array of urgent concerns,” the researchers concluded.
Pandemic propelled telemedicine to improve patient care
The widespread adoption of telemedicine in primary care has been a beneficial side effect of the COVID-19 pandemic, said Tim Joos, MD, a Seattle-based clinician with a combination internal medicine/pediatrics practice, in an interview.
“Toward the end of World War II and in the push to form the United Nations, Winston Churchill was credited with the saying, ‘Never let a good crisis go to waste,’” said Dr. Joos, who was not connected with the study.
“As awful as this pandemic has been, it has propelled health care delivery at an unprecedented pace into the digital age,” he noted.
The current study is important because it highlights the number of complaints that can be successfully resolved through telemedicine, offering patients and families quicker access and more options for care, Dr. Joos said.
“I feel that giving patients and families an open choice for either telemedicine or in-person visits improves the likelihood that the issue will be resolved efficiently and satisfactorily with fewer visits,” he added.
Approximately two-thirds of pediatric acute care concerns managed in telemedicine visits required no additional visits or follow-up, based on data from more than 600 visits.
The increase in use of telemedicine during the first year of the COVID-19 pandemic enabled access to care and connection to doctors for many pediatric patients, said Kristina Kissiova, MD, of Children’s National Health System, Washington, and colleagues. Some advantages of telemedicine include enhanced medical homes, reduced health care costs, and less crowding and wait time for patients in offices and emergency departments; however, the optimal use of telemedicine for acute primary care has not been examined, they said.
In a study presented at the annual meeting of the Pediatric Academic Societies, the researchers conducted a retrospective chart review of 638 acute care telemedicine visits conducted by 21 health care providers at a single practice in Washington in October 2020 and November 2020. Approximately half of the patients were male, 65% were white, and 89% had commercial insurance. The most common age group was 6-12 years (23%), followed by 2-3 years (16%), 3-6 years (15%), and 12-18 years (14%).
The primary outcome was the number and nature of visits completed via telemedicine without the need for referral or a subsequent in-person visit. Telemedicine visits for well-child checks and follow-up visits were excluded.
Overall, 60% of the visits (384 of 638) were completed over telemedicine with no need for additional visits or referrals. The most common acute complaints were upper respiratory infections, dermatologic issues, gastrointestinal issues, COVID-19 related issues, and fever (18.7%, 16.3%, 12.9%, 11.9%, and 10.3%, respectively).
Of these, dermatologic and GI concerns were most often completed via telemedicine (93.3% and 81.7%, respectively), while upper respiratory tract infections and fever issues were the least likely to be completed via telemedicine (22.7% and 13.6%), mainly because of the need to report for in-person COVID-19 testing, the researchers said.
Among other less common chief complaints, 100% of breathing concerns, behavior/mental health concerns, and head trauma or falls were addressed via telemedicine without additional referrals or follow-up visits. In addition, 90.9% of urgent care or emergency department follow-ups, 88.9% of ear concerns, and 87.5% of eye concerns were completely resolved via telemedicine visits.
Overall, 3% of patients who were not referred after a telemedicine visit presented in person for worsening symptoms. Of these who were referred after a telemedicine visit, 90% were seen in person within 48 hours.
The study findings were limited by the inclusion of data from only a single center. However, “These early findings provide insight into the utility of telehealth in the primary care setting for a broad array of urgent concerns,” the researchers concluded.
Pandemic propelled telemedicine to improve patient care
The widespread adoption of telemedicine in primary care has been a beneficial side effect of the COVID-19 pandemic, said Tim Joos, MD, a Seattle-based clinician with a combination internal medicine/pediatrics practice, in an interview.
“Toward the end of World War II and in the push to form the United Nations, Winston Churchill was credited with the saying, ‘Never let a good crisis go to waste,’” said Dr. Joos, who was not connected with the study.
“As awful as this pandemic has been, it has propelled health care delivery at an unprecedented pace into the digital age,” he noted.
The current study is important because it highlights the number of complaints that can be successfully resolved through telemedicine, offering patients and families quicker access and more options for care, Dr. Joos said.
“I feel that giving patients and families an open choice for either telemedicine or in-person visits improves the likelihood that the issue will be resolved efficiently and satisfactorily with fewer visits,” he added.
Approximately two-thirds of pediatric acute care concerns managed in telemedicine visits required no additional visits or follow-up, based on data from more than 600 visits.
The increase in use of telemedicine during the first year of the COVID-19 pandemic enabled access to care and connection to doctors for many pediatric patients, said Kristina Kissiova, MD, of Children’s National Health System, Washington, and colleagues. Some advantages of telemedicine include enhanced medical homes, reduced health care costs, and less crowding and wait time for patients in offices and emergency departments; however, the optimal use of telemedicine for acute primary care has not been examined, they said.
In a study presented at the annual meeting of the Pediatric Academic Societies, the researchers conducted a retrospective chart review of 638 acute care telemedicine visits conducted by 21 health care providers at a single practice in Washington in October 2020 and November 2020. Approximately half of the patients were male, 65% were white, and 89% had commercial insurance. The most common age group was 6-12 years (23%), followed by 2-3 years (16%), 3-6 years (15%), and 12-18 years (14%).
The primary outcome was the number and nature of visits completed via telemedicine without the need for referral or a subsequent in-person visit. Telemedicine visits for well-child checks and follow-up visits were excluded.
Overall, 60% of the visits (384 of 638) were completed over telemedicine with no need for additional visits or referrals. The most common acute complaints were upper respiratory infections, dermatologic issues, gastrointestinal issues, COVID-19 related issues, and fever (18.7%, 16.3%, 12.9%, 11.9%, and 10.3%, respectively).
Of these, dermatologic and GI concerns were most often completed via telemedicine (93.3% and 81.7%, respectively), while upper respiratory tract infections and fever issues were the least likely to be completed via telemedicine (22.7% and 13.6%), mainly because of the need to report for in-person COVID-19 testing, the researchers said.
Among other less common chief complaints, 100% of breathing concerns, behavior/mental health concerns, and head trauma or falls were addressed via telemedicine without additional referrals or follow-up visits. In addition, 90.9% of urgent care or emergency department follow-ups, 88.9% of ear concerns, and 87.5% of eye concerns were completely resolved via telemedicine visits.
Overall, 3% of patients who were not referred after a telemedicine visit presented in person for worsening symptoms. Of these who were referred after a telemedicine visit, 90% were seen in person within 48 hours.
The study findings were limited by the inclusion of data from only a single center. However, “These early findings provide insight into the utility of telehealth in the primary care setting for a broad array of urgent concerns,” the researchers concluded.
Pandemic propelled telemedicine to improve patient care
The widespread adoption of telemedicine in primary care has been a beneficial side effect of the COVID-19 pandemic, said Tim Joos, MD, a Seattle-based clinician with a combination internal medicine/pediatrics practice, in an interview.
“Toward the end of World War II and in the push to form the United Nations, Winston Churchill was credited with the saying, ‘Never let a good crisis go to waste,’” said Dr. Joos, who was not connected with the study.
“As awful as this pandemic has been, it has propelled health care delivery at an unprecedented pace into the digital age,” he noted.
The current study is important because it highlights the number of complaints that can be successfully resolved through telemedicine, offering patients and families quicker access and more options for care, Dr. Joos said.
“I feel that giving patients and families an open choice for either telemedicine or in-person visits improves the likelihood that the issue will be resolved efficiently and satisfactorily with fewer visits,” he added.
FROM PAS 2022
Myocarditis higher with Moderna COVID vax in young men
One of the largest studies to date on myocarditis after COVID-19 vaccination confirms an increased risk with both the Pfizer and Moderna vaccines in young men and shows that the risk is higher with the Moderna than with the Pfizer vaccine.
The study also suggests for the first time that in young men 16 to 24 years of age, the risk for myocarditis after vaccination with either the Pfizer or Moderna vaccine is higher than the risk for myocarditis after COVID-19 infection.
The population-based study involved data on 23.1 million residents across four Scandinavian countries – Denmark, Finland, Norway, and Sweden – 74% of whom had received two vaccine doses and 7% of whom had received one dose.
By linking data from high-quality nationwide health registers on COVID-19 vaccination, infection rates, and myocarditis diagnoses, the researchers were able to evaluate the risk for myocarditis by vaccine product, vaccination dose number, sex, and age.
The study was published online in JAMA Cardiology.
The results confirm that the risk for myocarditis after COVID-19 mRNA vaccines is highest in young men 16 to 24 years of age after the second dose.
For men in this age group who received two doses of the same vaccine, data were compatible, with between four and seven excess myocarditis events in 28 days per 100,000 individuals after the second dose of the Pfizer vaccine, and between nine and 28 per 100,000 individuals after the second dose of the Moderna vaccine.
“This is one of the largest studies on this topic to date. The first population studies were in Israel, with 5 million individuals, and looked at just the Pfizer vaccine. We have data on 23 million people from Scandinavia that include both the Pfizer and Moderna vaccines,” senior author Rickard Ljung, MD, Swedish Medical Products Agency, told this news organization.
“We show a clearly higher risk of myocarditis after the Moderna vaccine than after the Pfizer vaccine. This has been suggested before, but our data confirm definitively that the Moderna vaccine has a higher risk of myocarditis than the Pfizer vaccine,” he added.
“In the group at highest risk of myocarditis after COVID vaccination – young men aged 16 to 24 – the Pfizer vaccine shows a five times higher risk of myocarditis versus the unvaccinated cohort, while the Moderna vaccine shows a 15 times higher risk,” Dr. Ljung noted.
After seeing these data, the Swedish regulatory authority is no longer recommending use of the Moderna vaccine for people younger than 30 years, Dr. Ljung said. Similar recommendations have been made in Norway and Finland.
The researchers report that their finding of a higher risk for myocarditis after the Moderna vaccine than after the Pfizer vaccine in young men is in line with data from the Canada, France, the United Kingdom, and the United States. But they point out that, compared with previous studies, the current study had the advantage of data analyzed according to a common protocol from four different countries and that showed similar directions of associations, despite considerable differences in previous COVID-19 infection levels and lockdown policies.
Risk higher with vaccination than infection?
For what is believed to be the first time, the Scandinavian data also suggest a higher risk for myocarditis after COVID-19 vaccination with both the Pfizer and Moderna vaccines than after COVID-19 infection in young men 16 to 24 years.
Although previous studies have shown that males in this age group have the highest risk for myocarditis after vaccination, it has always been suggested that the risk after vaccination is lower than the risk after infection. The Scandinavian data suggest otherwise for this age group.
Dr. Ljung explained that the myocarditis risk after COVID infection is very hard to study.
“It is highly dependent on the testing strategy,” he said. “For example, in the first half of 2020, the only people being tested were those admitted to hospital, so studies would have included the sickest patients and would therefore likely have found a higher rate of myocarditis. But this current Scandinavian dataset only included individuals with a positive COVID test after August 2020, reflecting a broader range of people.”
The researchers found an excess rate of myocarditis of 3.26 per 100,000 individuals within 28 days of a positive COVID-19 test among all males, and 1.37 per 100,000 individuals among males 16 to 24 years of age.
“We show that the risk of myocarditis after COVID infection is lower in younger people and higher in older people, but the opposite is true after COVID vaccination, where the risk of myocarditis is higher in younger people and lower in older people,” Dr. Ljung said.
The study was not able to look at severity of myocarditis but did record length of hospital stay, which was similar in patients who developed myocarditis after vaccination and those in the unvaccinated cohort (4 to 5 days). Deaths were rare, with no deaths in people younger than 40 years.
“I think we can say that in people aged over 40, the risk of myocarditis is greater with infection than with vaccination, but in those under 40, it is not so clear. And our data suggest that for young men aged 16 to 24 years, the risk of myocarditis after COVID vaccination with either the Pfizer or Moderna vaccine is higher than after COVID infection,” Dr. Ljung commented.
Although the Swedish regulatory agency has already stopped recommending use of Moderna vaccine in those younger than 30 years on the basis of these data, Dr. Ljung was reluctant to make any recommendations regarding the use of the Pfizer vaccine in young males, saying it was up to individual public-health agencies to makes these decisions.
But he pointed out that the current study only looked at myocarditis, and COVID infection can result in many other complications that can lead to hospitalization and death, which needs to be taken into account when assessing the risk and benefit of vaccination.
Dr. Ljung noted that the current data only applied to the first two doses of the vaccines; data after booster injections have not been included, although the researchers are looking at that now.
What to advise patients?
In an accompanying Editor’s Note, Ann Marie Navar, MD, University of Texas Southwestern Medical Center, Dallas, who is editor of JAMA Cardiology, and Robert Bonow, MD, Northwestern University Feinberg School of Medicine, Chicago, who is deputy editor of JAMA Cardiology, try to explain how these data can inform the way health care professionals communicate with their patients about vaccination.
They point out the “good news,” that older adults who are at highest risk for COVID-19 complications appear to be at extremely low risk for vaccine-associated myocarditis.
They note that for both men and women older than 40 years, the excess number of cases of myocarditis after vaccination was fewer than two in 100,000 vaccinees across all vaccines studied, and the death toll from COVID-19 in the United States as of March was more than 200 per 100,000 population.
“Given the high rates of morbidity and mortality from COVID-19 infection in older adults and the efficacy of the vaccine in preventing severe infection and death, the benefits of immunization in those older than 40 years clearly outweigh the risks,” the editors say.
But given these data in young men, they suggest that health care professionals consider recommending the Pfizer vaccine over the Moderna vaccine for certain populations, including young men and other individuals for whom concerns about myocarditis present a barrier to immunization.
The editors also point out that although the risk for myocarditis after COVID-19 immunization is real, this low risk must be considered in the context of the overall benefit of the vaccine.
“At the individual level, immunization prevents not only COVID-19-related myocarditis but also severe disease, hospitalization, long-term complications after COVID-19 infection, and death. At the population level, immunization helps to decrease community spread, decrease the chances of new variants emerging, protect people who are immunocompromised, and ensure our health care system can continue to provide for our communities,” they conclude.
Dr. Ljung reports grants from Sanofi Aventis paid to his institution outside the submitted work and personal fees from Pfizer outside the submitted work. Dr. Navar reports personal fees from Pfizer and AstraZeneca, outside the scope of this work.
A version of this article first appeared on Medscape.com.
One of the largest studies to date on myocarditis after COVID-19 vaccination confirms an increased risk with both the Pfizer and Moderna vaccines in young men and shows that the risk is higher with the Moderna than with the Pfizer vaccine.
The study also suggests for the first time that in young men 16 to 24 years of age, the risk for myocarditis after vaccination with either the Pfizer or Moderna vaccine is higher than the risk for myocarditis after COVID-19 infection.
The population-based study involved data on 23.1 million residents across four Scandinavian countries – Denmark, Finland, Norway, and Sweden – 74% of whom had received two vaccine doses and 7% of whom had received one dose.
By linking data from high-quality nationwide health registers on COVID-19 vaccination, infection rates, and myocarditis diagnoses, the researchers were able to evaluate the risk for myocarditis by vaccine product, vaccination dose number, sex, and age.
The study was published online in JAMA Cardiology.
The results confirm that the risk for myocarditis after COVID-19 mRNA vaccines is highest in young men 16 to 24 years of age after the second dose.
For men in this age group who received two doses of the same vaccine, data were compatible, with between four and seven excess myocarditis events in 28 days per 100,000 individuals after the second dose of the Pfizer vaccine, and between nine and 28 per 100,000 individuals after the second dose of the Moderna vaccine.
“This is one of the largest studies on this topic to date. The first population studies were in Israel, with 5 million individuals, and looked at just the Pfizer vaccine. We have data on 23 million people from Scandinavia that include both the Pfizer and Moderna vaccines,” senior author Rickard Ljung, MD, Swedish Medical Products Agency, told this news organization.
“We show a clearly higher risk of myocarditis after the Moderna vaccine than after the Pfizer vaccine. This has been suggested before, but our data confirm definitively that the Moderna vaccine has a higher risk of myocarditis than the Pfizer vaccine,” he added.
“In the group at highest risk of myocarditis after COVID vaccination – young men aged 16 to 24 – the Pfizer vaccine shows a five times higher risk of myocarditis versus the unvaccinated cohort, while the Moderna vaccine shows a 15 times higher risk,” Dr. Ljung noted.
After seeing these data, the Swedish regulatory authority is no longer recommending use of the Moderna vaccine for people younger than 30 years, Dr. Ljung said. Similar recommendations have been made in Norway and Finland.
The researchers report that their finding of a higher risk for myocarditis after the Moderna vaccine than after the Pfizer vaccine in young men is in line with data from the Canada, France, the United Kingdom, and the United States. But they point out that, compared with previous studies, the current study had the advantage of data analyzed according to a common protocol from four different countries and that showed similar directions of associations, despite considerable differences in previous COVID-19 infection levels and lockdown policies.
Risk higher with vaccination than infection?
For what is believed to be the first time, the Scandinavian data also suggest a higher risk for myocarditis after COVID-19 vaccination with both the Pfizer and Moderna vaccines than after COVID-19 infection in young men 16 to 24 years.
Although previous studies have shown that males in this age group have the highest risk for myocarditis after vaccination, it has always been suggested that the risk after vaccination is lower than the risk after infection. The Scandinavian data suggest otherwise for this age group.
Dr. Ljung explained that the myocarditis risk after COVID infection is very hard to study.
“It is highly dependent on the testing strategy,” he said. “For example, in the first half of 2020, the only people being tested were those admitted to hospital, so studies would have included the sickest patients and would therefore likely have found a higher rate of myocarditis. But this current Scandinavian dataset only included individuals with a positive COVID test after August 2020, reflecting a broader range of people.”
The researchers found an excess rate of myocarditis of 3.26 per 100,000 individuals within 28 days of a positive COVID-19 test among all males, and 1.37 per 100,000 individuals among males 16 to 24 years of age.
“We show that the risk of myocarditis after COVID infection is lower in younger people and higher in older people, but the opposite is true after COVID vaccination, where the risk of myocarditis is higher in younger people and lower in older people,” Dr. Ljung said.
The study was not able to look at severity of myocarditis but did record length of hospital stay, which was similar in patients who developed myocarditis after vaccination and those in the unvaccinated cohort (4 to 5 days). Deaths were rare, with no deaths in people younger than 40 years.
“I think we can say that in people aged over 40, the risk of myocarditis is greater with infection than with vaccination, but in those under 40, it is not so clear. And our data suggest that for young men aged 16 to 24 years, the risk of myocarditis after COVID vaccination with either the Pfizer or Moderna vaccine is higher than after COVID infection,” Dr. Ljung commented.
Although the Swedish regulatory agency has already stopped recommending use of Moderna vaccine in those younger than 30 years on the basis of these data, Dr. Ljung was reluctant to make any recommendations regarding the use of the Pfizer vaccine in young males, saying it was up to individual public-health agencies to makes these decisions.
But he pointed out that the current study only looked at myocarditis, and COVID infection can result in many other complications that can lead to hospitalization and death, which needs to be taken into account when assessing the risk and benefit of vaccination.
Dr. Ljung noted that the current data only applied to the first two doses of the vaccines; data after booster injections have not been included, although the researchers are looking at that now.
What to advise patients?
In an accompanying Editor’s Note, Ann Marie Navar, MD, University of Texas Southwestern Medical Center, Dallas, who is editor of JAMA Cardiology, and Robert Bonow, MD, Northwestern University Feinberg School of Medicine, Chicago, who is deputy editor of JAMA Cardiology, try to explain how these data can inform the way health care professionals communicate with their patients about vaccination.
They point out the “good news,” that older adults who are at highest risk for COVID-19 complications appear to be at extremely low risk for vaccine-associated myocarditis.
They note that for both men and women older than 40 years, the excess number of cases of myocarditis after vaccination was fewer than two in 100,000 vaccinees across all vaccines studied, and the death toll from COVID-19 in the United States as of March was more than 200 per 100,000 population.
“Given the high rates of morbidity and mortality from COVID-19 infection in older adults and the efficacy of the vaccine in preventing severe infection and death, the benefits of immunization in those older than 40 years clearly outweigh the risks,” the editors say.
But given these data in young men, they suggest that health care professionals consider recommending the Pfizer vaccine over the Moderna vaccine for certain populations, including young men and other individuals for whom concerns about myocarditis present a barrier to immunization.
The editors also point out that although the risk for myocarditis after COVID-19 immunization is real, this low risk must be considered in the context of the overall benefit of the vaccine.
“At the individual level, immunization prevents not only COVID-19-related myocarditis but also severe disease, hospitalization, long-term complications after COVID-19 infection, and death. At the population level, immunization helps to decrease community spread, decrease the chances of new variants emerging, protect people who are immunocompromised, and ensure our health care system can continue to provide for our communities,” they conclude.
Dr. Ljung reports grants from Sanofi Aventis paid to his institution outside the submitted work and personal fees from Pfizer outside the submitted work. Dr. Navar reports personal fees from Pfizer and AstraZeneca, outside the scope of this work.
A version of this article first appeared on Medscape.com.
One of the largest studies to date on myocarditis after COVID-19 vaccination confirms an increased risk with both the Pfizer and Moderna vaccines in young men and shows that the risk is higher with the Moderna than with the Pfizer vaccine.
The study also suggests for the first time that in young men 16 to 24 years of age, the risk for myocarditis after vaccination with either the Pfizer or Moderna vaccine is higher than the risk for myocarditis after COVID-19 infection.
The population-based study involved data on 23.1 million residents across four Scandinavian countries – Denmark, Finland, Norway, and Sweden – 74% of whom had received two vaccine doses and 7% of whom had received one dose.
By linking data from high-quality nationwide health registers on COVID-19 vaccination, infection rates, and myocarditis diagnoses, the researchers were able to evaluate the risk for myocarditis by vaccine product, vaccination dose number, sex, and age.
The study was published online in JAMA Cardiology.
The results confirm that the risk for myocarditis after COVID-19 mRNA vaccines is highest in young men 16 to 24 years of age after the second dose.
For men in this age group who received two doses of the same vaccine, data were compatible, with between four and seven excess myocarditis events in 28 days per 100,000 individuals after the second dose of the Pfizer vaccine, and between nine and 28 per 100,000 individuals after the second dose of the Moderna vaccine.
“This is one of the largest studies on this topic to date. The first population studies were in Israel, with 5 million individuals, and looked at just the Pfizer vaccine. We have data on 23 million people from Scandinavia that include both the Pfizer and Moderna vaccines,” senior author Rickard Ljung, MD, Swedish Medical Products Agency, told this news organization.
“We show a clearly higher risk of myocarditis after the Moderna vaccine than after the Pfizer vaccine. This has been suggested before, but our data confirm definitively that the Moderna vaccine has a higher risk of myocarditis than the Pfizer vaccine,” he added.
“In the group at highest risk of myocarditis after COVID vaccination – young men aged 16 to 24 – the Pfizer vaccine shows a five times higher risk of myocarditis versus the unvaccinated cohort, while the Moderna vaccine shows a 15 times higher risk,” Dr. Ljung noted.
After seeing these data, the Swedish regulatory authority is no longer recommending use of the Moderna vaccine for people younger than 30 years, Dr. Ljung said. Similar recommendations have been made in Norway and Finland.
The researchers report that their finding of a higher risk for myocarditis after the Moderna vaccine than after the Pfizer vaccine in young men is in line with data from the Canada, France, the United Kingdom, and the United States. But they point out that, compared with previous studies, the current study had the advantage of data analyzed according to a common protocol from four different countries and that showed similar directions of associations, despite considerable differences in previous COVID-19 infection levels and lockdown policies.
Risk higher with vaccination than infection?
For what is believed to be the first time, the Scandinavian data also suggest a higher risk for myocarditis after COVID-19 vaccination with both the Pfizer and Moderna vaccines than after COVID-19 infection in young men 16 to 24 years.
Although previous studies have shown that males in this age group have the highest risk for myocarditis after vaccination, it has always been suggested that the risk after vaccination is lower than the risk after infection. The Scandinavian data suggest otherwise for this age group.
Dr. Ljung explained that the myocarditis risk after COVID infection is very hard to study.
“It is highly dependent on the testing strategy,” he said. “For example, in the first half of 2020, the only people being tested were those admitted to hospital, so studies would have included the sickest patients and would therefore likely have found a higher rate of myocarditis. But this current Scandinavian dataset only included individuals with a positive COVID test after August 2020, reflecting a broader range of people.”
The researchers found an excess rate of myocarditis of 3.26 per 100,000 individuals within 28 days of a positive COVID-19 test among all males, and 1.37 per 100,000 individuals among males 16 to 24 years of age.
“We show that the risk of myocarditis after COVID infection is lower in younger people and higher in older people, but the opposite is true after COVID vaccination, where the risk of myocarditis is higher in younger people and lower in older people,” Dr. Ljung said.
The study was not able to look at severity of myocarditis but did record length of hospital stay, which was similar in patients who developed myocarditis after vaccination and those in the unvaccinated cohort (4 to 5 days). Deaths were rare, with no deaths in people younger than 40 years.
“I think we can say that in people aged over 40, the risk of myocarditis is greater with infection than with vaccination, but in those under 40, it is not so clear. And our data suggest that for young men aged 16 to 24 years, the risk of myocarditis after COVID vaccination with either the Pfizer or Moderna vaccine is higher than after COVID infection,” Dr. Ljung commented.
Although the Swedish regulatory agency has already stopped recommending use of Moderna vaccine in those younger than 30 years on the basis of these data, Dr. Ljung was reluctant to make any recommendations regarding the use of the Pfizer vaccine in young males, saying it was up to individual public-health agencies to makes these decisions.
But he pointed out that the current study only looked at myocarditis, and COVID infection can result in many other complications that can lead to hospitalization and death, which needs to be taken into account when assessing the risk and benefit of vaccination.
Dr. Ljung noted that the current data only applied to the first two doses of the vaccines; data after booster injections have not been included, although the researchers are looking at that now.
What to advise patients?
In an accompanying Editor’s Note, Ann Marie Navar, MD, University of Texas Southwestern Medical Center, Dallas, who is editor of JAMA Cardiology, and Robert Bonow, MD, Northwestern University Feinberg School of Medicine, Chicago, who is deputy editor of JAMA Cardiology, try to explain how these data can inform the way health care professionals communicate with their patients about vaccination.
They point out the “good news,” that older adults who are at highest risk for COVID-19 complications appear to be at extremely low risk for vaccine-associated myocarditis.
They note that for both men and women older than 40 years, the excess number of cases of myocarditis after vaccination was fewer than two in 100,000 vaccinees across all vaccines studied, and the death toll from COVID-19 in the United States as of March was more than 200 per 100,000 population.
“Given the high rates of morbidity and mortality from COVID-19 infection in older adults and the efficacy of the vaccine in preventing severe infection and death, the benefits of immunization in those older than 40 years clearly outweigh the risks,” the editors say.
But given these data in young men, they suggest that health care professionals consider recommending the Pfizer vaccine over the Moderna vaccine for certain populations, including young men and other individuals for whom concerns about myocarditis present a barrier to immunization.
The editors also point out that although the risk for myocarditis after COVID-19 immunization is real, this low risk must be considered in the context of the overall benefit of the vaccine.
“At the individual level, immunization prevents not only COVID-19-related myocarditis but also severe disease, hospitalization, long-term complications after COVID-19 infection, and death. At the population level, immunization helps to decrease community spread, decrease the chances of new variants emerging, protect people who are immunocompromised, and ensure our health care system can continue to provide for our communities,” they conclude.
Dr. Ljung reports grants from Sanofi Aventis paid to his institution outside the submitted work and personal fees from Pfizer outside the submitted work. Dr. Navar reports personal fees from Pfizer and AstraZeneca, outside the scope of this work.
A version of this article first appeared on Medscape.com.
FROM JAMA CARDIOLOGY
How gender-affirming care is provided to adolescents in the United States
“Texas investigates parents of transgender teen.” “Court did not force dad to allow chemical castration of son.” Headlines such as these are becoming more common as transgender adolescents and young adults, as well as their families, continue to come under attack from state and local governments. In the 2021 state legislative sessions, more than 100 anti-trans bills were filed across 35 state legislatures. Texas alone saw 13 anti-trans bills, covering everything from sports participation to criminalization of best-practice medical care.1 Many of these bills are introduced under the guise of “protecting” these adolescents and young adults but are detrimental to their health. They also contain descriptions of gender-affirming care that do not reflect the evidence-based standards of care followed by clinicians across the country. Below is scientifically accurate information on gender-affirming care.
Gender identity development
Trajectories of gender identity are diverse. In a large sample of transgender adults (n = 27,715), 10% started to realize they were transgender at age 5 or younger, 16% between ages 6 and 10, 28% between 11 and 15, 29% between 16 and 20, and 18% at age 21 or older.2 In childhood, cross-gender play and preferences are a normal part of gender expression and many gender-nonconforming children will go on to identify with the sex they were assigned at birth (labeled cisgender). However, some children explicitly identify with a gender different than the sex they were assigned at birth (labeled transgender). Children who are consistent, insistent, and persistent in this identity appear likely to remain so into adolescence and adulthood. It is important to note that there is no evidence that discouraging gender nonconformity decreases the likelihood that a child will identify as transgender. In fact, this practice is no longer considered ethical, as it can have damaging effects on self-esteem and mental health. In addition, not all transgender people are noticeably gender nonconforming in childhood and that lack of childhood gender nonconformity does not invalidate someone’s transgender identity.
Gender-affirming care
For youth who identify as transgender, all steps in transition prior to puberty are social. This includes steps like changing hairstyles or clothing and using a different (affirmed) name and/or pronouns. This time period allows youth to explore their gender identity and expression. In one large study of 10,000 LGBTQ youth, among youth who reported “all or most people” used their affirmed pronoun, 12% reported a history of suicide attempt.3 In comparison, among those who reported that “no one” used their affirmed pronoun, the suicide attempt rate was 28%. Further, 14% of youth who reported that they were able to make changes in their clothing and appearance reported a past suicide attempt in comparison to 26% of those who were not able to. Many of these youth also are under the care of mental health professionals during this time.
At the onset of puberty, transgender youth are eligible for medical management, if needed, to address gender dysphoria (i.e., distress with one’s sex characteristics that is consistent and impairing). It is important to recognize that not all people who identify as transgender experience gender dysphoria or desire a medical transition. For those who do seek medical care, puberty must be confirmed either by breast/testicular exam or checking gonadotropin levels. Standards of care suggest that prior to pubertal suppression with GnRH agonists, such as leuprolide or histrelin, adolescents undergo a thorough psychosocial evaluation by a qualified, licensed clinician. After this evaluation, pubertal suppression may be initiated. These adolescents are monitored by their physicians every 3-6 months for side effects and continuing evaluation of their gender identity. GnRH agonists pause any further pubertal development while the adolescent continues to explore his/her/their gender identity. GnRH agonists are fully reversible and if they are stopped, the child’s natal puberty would recommence.
If an adolescent desires to start gender-affirming hormones, these are started as early as age 14, depending on their maturity, when they desire to start, and/or their ability to obtain parental consent. If a patient has not begun GnRH agonists and undergone a previous psychosocial evaluation, a thorough psychosocial evaluation by a qualified, licensed clinician would take place prior to initiating gender-affirming hormones. Prior to initiating hormones, a thorough informed-consent process occurs between the clinician, patient, and family. This process reviews reversible versus irreversible effects, as well of any side effects of the medication(s). Adolescents who begin hormonal treatment are then monitored every 3-6 months for medication side effects, efficacy, satisfaction with treatment, and by continued mental health assessments. Engagement in mental health therapy is not required beyond the initial evaluation (as many adolescents are well adjusted), but it is encouraged for support during the adolescent’s transition.4 It is important to note that the decision to begin hormones, or not, as well as how to adjust dosing over time, is nuanced and is individualized to each patient’s particular goals for his/her/their transition.
Care for transmasculine identified adolescents (those who were assigned female at birth) typically involves testosterone, delivered via subcutaneous injection, transdermal patch, or transdermal gel. Care for transfeminine individuals (those who were assigned male at birth) typically involves estradiol, delivered via daily pill, weekly or twice weekly transdermal patch, or intramuscular injection, as well as an androgen blocker. This is because estradiol by itself is a weak androgen inhibitor. Antiandrogen medication is delivered by daily oral spironolactone, daily oral bicalutamide (an androgen receptor blocker), or GnRH agonists similar to those used for puberty blockade.
Outcomes
At least 13 studies have documented an improvement in gender dysphoria and/or mental health for adolescents and young adults after beginning gender affirming medical care.5 A recent study by Turban et al. showed that access to gender affirming hormones during adolescence or early adulthood was associated with decreased odds of past month suicidal ideation than for those who did not have access to gender-affirming hormones.6 Tordoff et al. found that receipt of gender-affirming care, including medications, led to a 60% decrease in depressive symptoms and a 73% decrease in suicidality.7 One other question that often arises is whether youth who undergo medical treatment for their transition regret their transition or retransition back to the sex they were assigned at birth. In a large study at a gender clinic in the United Kingdom, they found a regret rate of only 0.47% (16 of 3,398 adolescents aged 13-20).8 This is similar to other studies that have also found low rates of regret. Regret is often due to lack of acceptance in society rather than lack of transgender identity.
The care of gender diverse youth takes place on a spectrum, including options that do not include medical treatment. By supporting youth where they are on their gender journey, there is a significant reduction in adverse mental health outcomes. Gender-affirming hormonal treatment is individualized and a thorough multidisciplinary evaluation and informed consent are obtained prior to initiation. There are careful, nuanced discussions with patients and their families to individualize care based on individual goals. By following established evidence-based standards of care, physicians can support their gender-diverse patients throughout their gender journey. Just like other medical treatments, procedures, or surgeries, gender-affirming care should be undertaken in the context of the sacred patient-physician relationship.
Dr. Cooper is assistant professor of pediatrics at University of Texas Southwestern, Dallas, and an adolescent medicine specialist at Children’s Medical Center Dallas.
References
1. Equality Texas. Legislative Bill Tracker.
2. James SE et al. The Report of the 2015 U.S. Transgender Survey. 2016. Washington, DC: National Center for Transgender Equality.
3. The Trevor Project. 2020. National Survey on LGBTQ Mental Health.
4. Lopez X et al. Curr Opin Pediatrics. 2017;29(4):475-80.
5. Turban J. The evidence for trans youth gender-affirming medical care. Psychology Today. 2022 Jan 24.
6. Turban J et al. Access to gender-affirming hormones during adolescence and mental health outcomes among transgender adults. PLOS ONE. 2022;17(1).
7. Tordoff DM et al. Mental health outcomes in transgender and nonbinary youths receiving gender-affirming care. JAMA Network Open. 2022;5(2).
8. Davies S et al. Detransition rates in a national UK gender identity clinic. Inside Matters. On Law, Ethics, and Religion. 2019 Apr 11.
“Texas investigates parents of transgender teen.” “Court did not force dad to allow chemical castration of son.” Headlines such as these are becoming more common as transgender adolescents and young adults, as well as their families, continue to come under attack from state and local governments. In the 2021 state legislative sessions, more than 100 anti-trans bills were filed across 35 state legislatures. Texas alone saw 13 anti-trans bills, covering everything from sports participation to criminalization of best-practice medical care.1 Many of these bills are introduced under the guise of “protecting” these adolescents and young adults but are detrimental to their health. They also contain descriptions of gender-affirming care that do not reflect the evidence-based standards of care followed by clinicians across the country. Below is scientifically accurate information on gender-affirming care.
Gender identity development
Trajectories of gender identity are diverse. In a large sample of transgender adults (n = 27,715), 10% started to realize they were transgender at age 5 or younger, 16% between ages 6 and 10, 28% between 11 and 15, 29% between 16 and 20, and 18% at age 21 or older.2 In childhood, cross-gender play and preferences are a normal part of gender expression and many gender-nonconforming children will go on to identify with the sex they were assigned at birth (labeled cisgender). However, some children explicitly identify with a gender different than the sex they were assigned at birth (labeled transgender). Children who are consistent, insistent, and persistent in this identity appear likely to remain so into adolescence and adulthood. It is important to note that there is no evidence that discouraging gender nonconformity decreases the likelihood that a child will identify as transgender. In fact, this practice is no longer considered ethical, as it can have damaging effects on self-esteem and mental health. In addition, not all transgender people are noticeably gender nonconforming in childhood and that lack of childhood gender nonconformity does not invalidate someone’s transgender identity.
Gender-affirming care
For youth who identify as transgender, all steps in transition prior to puberty are social. This includes steps like changing hairstyles or clothing and using a different (affirmed) name and/or pronouns. This time period allows youth to explore their gender identity and expression. In one large study of 10,000 LGBTQ youth, among youth who reported “all or most people” used their affirmed pronoun, 12% reported a history of suicide attempt.3 In comparison, among those who reported that “no one” used their affirmed pronoun, the suicide attempt rate was 28%. Further, 14% of youth who reported that they were able to make changes in their clothing and appearance reported a past suicide attempt in comparison to 26% of those who were not able to. Many of these youth also are under the care of mental health professionals during this time.
At the onset of puberty, transgender youth are eligible for medical management, if needed, to address gender dysphoria (i.e., distress with one’s sex characteristics that is consistent and impairing). It is important to recognize that not all people who identify as transgender experience gender dysphoria or desire a medical transition. For those who do seek medical care, puberty must be confirmed either by breast/testicular exam or checking gonadotropin levels. Standards of care suggest that prior to pubertal suppression with GnRH agonists, such as leuprolide or histrelin, adolescents undergo a thorough psychosocial evaluation by a qualified, licensed clinician. After this evaluation, pubertal suppression may be initiated. These adolescents are monitored by their physicians every 3-6 months for side effects and continuing evaluation of their gender identity. GnRH agonists pause any further pubertal development while the adolescent continues to explore his/her/their gender identity. GnRH agonists are fully reversible and if they are stopped, the child’s natal puberty would recommence.
If an adolescent desires to start gender-affirming hormones, these are started as early as age 14, depending on their maturity, when they desire to start, and/or their ability to obtain parental consent. If a patient has not begun GnRH agonists and undergone a previous psychosocial evaluation, a thorough psychosocial evaluation by a qualified, licensed clinician would take place prior to initiating gender-affirming hormones. Prior to initiating hormones, a thorough informed-consent process occurs between the clinician, patient, and family. This process reviews reversible versus irreversible effects, as well of any side effects of the medication(s). Adolescents who begin hormonal treatment are then monitored every 3-6 months for medication side effects, efficacy, satisfaction with treatment, and by continued mental health assessments. Engagement in mental health therapy is not required beyond the initial evaluation (as many adolescents are well adjusted), but it is encouraged for support during the adolescent’s transition.4 It is important to note that the decision to begin hormones, or not, as well as how to adjust dosing over time, is nuanced and is individualized to each patient’s particular goals for his/her/their transition.
Care for transmasculine identified adolescents (those who were assigned female at birth) typically involves testosterone, delivered via subcutaneous injection, transdermal patch, or transdermal gel. Care for transfeminine individuals (those who were assigned male at birth) typically involves estradiol, delivered via daily pill, weekly or twice weekly transdermal patch, or intramuscular injection, as well as an androgen blocker. This is because estradiol by itself is a weak androgen inhibitor. Antiandrogen medication is delivered by daily oral spironolactone, daily oral bicalutamide (an androgen receptor blocker), or GnRH agonists similar to those used for puberty blockade.
Outcomes
At least 13 studies have documented an improvement in gender dysphoria and/or mental health for adolescents and young adults after beginning gender affirming medical care.5 A recent study by Turban et al. showed that access to gender affirming hormones during adolescence or early adulthood was associated with decreased odds of past month suicidal ideation than for those who did not have access to gender-affirming hormones.6 Tordoff et al. found that receipt of gender-affirming care, including medications, led to a 60% decrease in depressive symptoms and a 73% decrease in suicidality.7 One other question that often arises is whether youth who undergo medical treatment for their transition regret their transition or retransition back to the sex they were assigned at birth. In a large study at a gender clinic in the United Kingdom, they found a regret rate of only 0.47% (16 of 3,398 adolescents aged 13-20).8 This is similar to other studies that have also found low rates of regret. Regret is often due to lack of acceptance in society rather than lack of transgender identity.
The care of gender diverse youth takes place on a spectrum, including options that do not include medical treatment. By supporting youth where they are on their gender journey, there is a significant reduction in adverse mental health outcomes. Gender-affirming hormonal treatment is individualized and a thorough multidisciplinary evaluation and informed consent are obtained prior to initiation. There are careful, nuanced discussions with patients and their families to individualize care based on individual goals. By following established evidence-based standards of care, physicians can support their gender-diverse patients throughout their gender journey. Just like other medical treatments, procedures, or surgeries, gender-affirming care should be undertaken in the context of the sacred patient-physician relationship.
Dr. Cooper is assistant professor of pediatrics at University of Texas Southwestern, Dallas, and an adolescent medicine specialist at Children’s Medical Center Dallas.
References
1. Equality Texas. Legislative Bill Tracker.
2. James SE et al. The Report of the 2015 U.S. Transgender Survey. 2016. Washington, DC: National Center for Transgender Equality.
3. The Trevor Project. 2020. National Survey on LGBTQ Mental Health.
4. Lopez X et al. Curr Opin Pediatrics. 2017;29(4):475-80.
5. Turban J. The evidence for trans youth gender-affirming medical care. Psychology Today. 2022 Jan 24.
6. Turban J et al. Access to gender-affirming hormones during adolescence and mental health outcomes among transgender adults. PLOS ONE. 2022;17(1).
7. Tordoff DM et al. Mental health outcomes in transgender and nonbinary youths receiving gender-affirming care. JAMA Network Open. 2022;5(2).
8. Davies S et al. Detransition rates in a national UK gender identity clinic. Inside Matters. On Law, Ethics, and Religion. 2019 Apr 11.
“Texas investigates parents of transgender teen.” “Court did not force dad to allow chemical castration of son.” Headlines such as these are becoming more common as transgender adolescents and young adults, as well as their families, continue to come under attack from state and local governments. In the 2021 state legislative sessions, more than 100 anti-trans bills were filed across 35 state legislatures. Texas alone saw 13 anti-trans bills, covering everything from sports participation to criminalization of best-practice medical care.1 Many of these bills are introduced under the guise of “protecting” these adolescents and young adults but are detrimental to their health. They also contain descriptions of gender-affirming care that do not reflect the evidence-based standards of care followed by clinicians across the country. Below is scientifically accurate information on gender-affirming care.
Gender identity development
Trajectories of gender identity are diverse. In a large sample of transgender adults (n = 27,715), 10% started to realize they were transgender at age 5 or younger, 16% between ages 6 and 10, 28% between 11 and 15, 29% between 16 and 20, and 18% at age 21 or older.2 In childhood, cross-gender play and preferences are a normal part of gender expression and many gender-nonconforming children will go on to identify with the sex they were assigned at birth (labeled cisgender). However, some children explicitly identify with a gender different than the sex they were assigned at birth (labeled transgender). Children who are consistent, insistent, and persistent in this identity appear likely to remain so into adolescence and adulthood. It is important to note that there is no evidence that discouraging gender nonconformity decreases the likelihood that a child will identify as transgender. In fact, this practice is no longer considered ethical, as it can have damaging effects on self-esteem and mental health. In addition, not all transgender people are noticeably gender nonconforming in childhood and that lack of childhood gender nonconformity does not invalidate someone’s transgender identity.
Gender-affirming care
For youth who identify as transgender, all steps in transition prior to puberty are social. This includes steps like changing hairstyles or clothing and using a different (affirmed) name and/or pronouns. This time period allows youth to explore their gender identity and expression. In one large study of 10,000 LGBTQ youth, among youth who reported “all or most people” used their affirmed pronoun, 12% reported a history of suicide attempt.3 In comparison, among those who reported that “no one” used their affirmed pronoun, the suicide attempt rate was 28%. Further, 14% of youth who reported that they were able to make changes in their clothing and appearance reported a past suicide attempt in comparison to 26% of those who were not able to. Many of these youth also are under the care of mental health professionals during this time.
At the onset of puberty, transgender youth are eligible for medical management, if needed, to address gender dysphoria (i.e., distress with one’s sex characteristics that is consistent and impairing). It is important to recognize that not all people who identify as transgender experience gender dysphoria or desire a medical transition. For those who do seek medical care, puberty must be confirmed either by breast/testicular exam or checking gonadotropin levels. Standards of care suggest that prior to pubertal suppression with GnRH agonists, such as leuprolide or histrelin, adolescents undergo a thorough psychosocial evaluation by a qualified, licensed clinician. After this evaluation, pubertal suppression may be initiated. These adolescents are monitored by their physicians every 3-6 months for side effects and continuing evaluation of their gender identity. GnRH agonists pause any further pubertal development while the adolescent continues to explore his/her/their gender identity. GnRH agonists are fully reversible and if they are stopped, the child’s natal puberty would recommence.
If an adolescent desires to start gender-affirming hormones, these are started as early as age 14, depending on their maturity, when they desire to start, and/or their ability to obtain parental consent. If a patient has not begun GnRH agonists and undergone a previous psychosocial evaluation, a thorough psychosocial evaluation by a qualified, licensed clinician would take place prior to initiating gender-affirming hormones. Prior to initiating hormones, a thorough informed-consent process occurs between the clinician, patient, and family. This process reviews reversible versus irreversible effects, as well of any side effects of the medication(s). Adolescents who begin hormonal treatment are then monitored every 3-6 months for medication side effects, efficacy, satisfaction with treatment, and by continued mental health assessments. Engagement in mental health therapy is not required beyond the initial evaluation (as many adolescents are well adjusted), but it is encouraged for support during the adolescent’s transition.4 It is important to note that the decision to begin hormones, or not, as well as how to adjust dosing over time, is nuanced and is individualized to each patient’s particular goals for his/her/their transition.
Care for transmasculine identified adolescents (those who were assigned female at birth) typically involves testosterone, delivered via subcutaneous injection, transdermal patch, or transdermal gel. Care for transfeminine individuals (those who were assigned male at birth) typically involves estradiol, delivered via daily pill, weekly or twice weekly transdermal patch, or intramuscular injection, as well as an androgen blocker. This is because estradiol by itself is a weak androgen inhibitor. Antiandrogen medication is delivered by daily oral spironolactone, daily oral bicalutamide (an androgen receptor blocker), or GnRH agonists similar to those used for puberty blockade.
Outcomes
At least 13 studies have documented an improvement in gender dysphoria and/or mental health for adolescents and young adults after beginning gender affirming medical care.5 A recent study by Turban et al. showed that access to gender affirming hormones during adolescence or early adulthood was associated with decreased odds of past month suicidal ideation than for those who did not have access to gender-affirming hormones.6 Tordoff et al. found that receipt of gender-affirming care, including medications, led to a 60% decrease in depressive symptoms and a 73% decrease in suicidality.7 One other question that often arises is whether youth who undergo medical treatment for their transition regret their transition or retransition back to the sex they were assigned at birth. In a large study at a gender clinic in the United Kingdom, they found a regret rate of only 0.47% (16 of 3,398 adolescents aged 13-20).8 This is similar to other studies that have also found low rates of regret. Regret is often due to lack of acceptance in society rather than lack of transgender identity.
The care of gender diverse youth takes place on a spectrum, including options that do not include medical treatment. By supporting youth where they are on their gender journey, there is a significant reduction in adverse mental health outcomes. Gender-affirming hormonal treatment is individualized and a thorough multidisciplinary evaluation and informed consent are obtained prior to initiation. There are careful, nuanced discussions with patients and their families to individualize care based on individual goals. By following established evidence-based standards of care, physicians can support their gender-diverse patients throughout their gender journey. Just like other medical treatments, procedures, or surgeries, gender-affirming care should be undertaken in the context of the sacred patient-physician relationship.
Dr. Cooper is assistant professor of pediatrics at University of Texas Southwestern, Dallas, and an adolescent medicine specialist at Children’s Medical Center Dallas.
References
1. Equality Texas. Legislative Bill Tracker.
2. James SE et al. The Report of the 2015 U.S. Transgender Survey. 2016. Washington, DC: National Center for Transgender Equality.
3. The Trevor Project. 2020. National Survey on LGBTQ Mental Health.
4. Lopez X et al. Curr Opin Pediatrics. 2017;29(4):475-80.
5. Turban J. The evidence for trans youth gender-affirming medical care. Psychology Today. 2022 Jan 24.
6. Turban J et al. Access to gender-affirming hormones during adolescence and mental health outcomes among transgender adults. PLOS ONE. 2022;17(1).
7. Tordoff DM et al. Mental health outcomes in transgender and nonbinary youths receiving gender-affirming care. JAMA Network Open. 2022;5(2).
8. Davies S et al. Detransition rates in a national UK gender identity clinic. Inside Matters. On Law, Ethics, and Religion. 2019 Apr 11.
How are maternal and neonatal outcomes impacted by the contemporary practice of operative vaginal delivery?
Muraca GM, Boutin A, Razaz N, et al. Maternal and neonatal trauma following operative vaginal delivery. CMAJ. 2022;194:E1-E12. doi: 10.1503/cmaj.210841.
EXPERT COMMENTARY
Operative vaginal delivery is used to achieve and expedite safe vaginal birth while avoiding CD and its associated morbidities.1,2 Despite support from the American College of Obstetricians and Gynecologists (ACOG) for the use of OVD as an alternative to CD, OVD was used in only 3% of all US births in 2013, a shift from approximately 30% in 1987.1,3 Reported complications of OVD are biased by the level of experience of the operator, changes in practice, and by misinterpretation of the counterfactual.1
Outcomes of OVD should be compared with appropriate reference groups, namely, with second-stage CD births rather than with spontaneous vaginal births.4 With decreasing rates of OVD, evidence of contemporary data is needed on appropriately compared perinatal outcomes.4
Details of the study
Muraca and colleagues conducted an observational cohort study of births in Canada between 2013 and 2019 to assess the incidence of maternal and neonatal trauma following OVD. They used composites defined a priori— stratified by instrument, region, level of obstetric care, and institutional OVD volume.
Results. Among 1,326,191 live or stillbirths, 2.9% were attempted forceps deliveries and 8.4% were attempted vacuum deliveries. Following forceps delivery, the maternal trauma rate was 25.3% (95% confidence interval [CI], 24.8%–25.7%), and the neonatal trauma rate was 9.6 per 1,000 live births (95% CI, 8.6–10.6). Following vacuum delivery, maternal and neonatal trauma rates were 13.2% (95% CI, 13.0%–13.4%) and 9.6 per 1,000 live births (95% CI, 9.0–10.2), respectively. Maternal trauma was driven by higher order perineal lacerations. Some association was seen between increased forceps volume and decreased maternal trauma rates.
The authors concluded that in Canada, rates of maternal and neonatal trauma following OVD are higher than previously reported in consensus statements.
Study strengths and limitations
This large contemporary study uniquely stratified perinatal outcomes following OVD. The outcomes are well defined and meaningful, but some limitations affect the generalizability of the findings.
First, stillbirths were included for the maternal composite outcome, yet the incidence of this within the study population is not reported. Operative vaginal deliveries that involve stillbirths can be complex; a subgroup analysis excluding these would aid in interpretation.
Second, complicated OVDs, including sequential use of forceps and vacuum and OVDs from midpelvic station, were included; ACOG recommends against both these practices in routine circumstances due to known increases in maternal and neonatal morbidity.1 As such, the inclusion of these OVDs may bias results away from the null.
Finally, despite discussing the role of episiotomy, the episiotomy rate in this cohort is not reported.
Despite these limitations, the study by Muraca and colleagues is a positive step forward toward understanding the role of OVD in contemporary obstetric practice, and it uniquely ascertains the impact of OVD volume outcomes that previously had been an elusive exposure ●
While it is important to understand perinatal outcomes following OVD in a contemporary cohort, utilizing the correct cohort and reference group is critical.4 Risks for maternal and neonatal trauma follow OVD; however, outcomes vary based on appropriate selection of OVD candidates and adherence to recommended national guidelines.1,4 The infrequency of OVD raises concerns regarding adequate training for obstetricians, which should be prioritized so that they can offer OVD as a safe alternative to CD birth.3
HAYLEY E. MILLER, MD, AND DANIELLE M. PANELLI, MD
- American College of Obstetricians and Gynecologists. Operative vaginal birth: ACOG practice bulletin, number 219. Obstet Gynecol. 2020;135:e149-e159.
- Spong CY, Berghella V, Wenstrom KD, et al. Preventing the first cesarean delivery: summary of a joint Eunice Kennedy Shriver National Institute of Child Health and Human Development, Society for Maternal-Fetal Medicine, and American College of Obstetricians and Gynecologists workshop. Obstet Gynecol. 2012;120:1181-1193.
- Zahniser SC, Kendrick JS, Franks AL, et al. Trends in obstetric operative procedures, 1980 to 1987. Am J Public Health. 1992;82:1340-1344.
- Panelli DM, Leonard SA, Joudi N, et al. Severe maternal and neonatal morbidity after attempted operative vaginal delivery. Am J Obstet Gynecol MFM. 2021;3: 100339.
Muraca GM, Boutin A, Razaz N, et al. Maternal and neonatal trauma following operative vaginal delivery. CMAJ. 2022;194:E1-E12. doi: 10.1503/cmaj.210841.
EXPERT COMMENTARY
Operative vaginal delivery is used to achieve and expedite safe vaginal birth while avoiding CD and its associated morbidities.1,2 Despite support from the American College of Obstetricians and Gynecologists (ACOG) for the use of OVD as an alternative to CD, OVD was used in only 3% of all US births in 2013, a shift from approximately 30% in 1987.1,3 Reported complications of OVD are biased by the level of experience of the operator, changes in practice, and by misinterpretation of the counterfactual.1
Outcomes of OVD should be compared with appropriate reference groups, namely, with second-stage CD births rather than with spontaneous vaginal births.4 With decreasing rates of OVD, evidence of contemporary data is needed on appropriately compared perinatal outcomes.4
Details of the study
Muraca and colleagues conducted an observational cohort study of births in Canada between 2013 and 2019 to assess the incidence of maternal and neonatal trauma following OVD. They used composites defined a priori— stratified by instrument, region, level of obstetric care, and institutional OVD volume.
Results. Among 1,326,191 live or stillbirths, 2.9% were attempted forceps deliveries and 8.4% were attempted vacuum deliveries. Following forceps delivery, the maternal trauma rate was 25.3% (95% confidence interval [CI], 24.8%–25.7%), and the neonatal trauma rate was 9.6 per 1,000 live births (95% CI, 8.6–10.6). Following vacuum delivery, maternal and neonatal trauma rates were 13.2% (95% CI, 13.0%–13.4%) and 9.6 per 1,000 live births (95% CI, 9.0–10.2), respectively. Maternal trauma was driven by higher order perineal lacerations. Some association was seen between increased forceps volume and decreased maternal trauma rates.
The authors concluded that in Canada, rates of maternal and neonatal trauma following OVD are higher than previously reported in consensus statements.
Study strengths and limitations
This large contemporary study uniquely stratified perinatal outcomes following OVD. The outcomes are well defined and meaningful, but some limitations affect the generalizability of the findings.
First, stillbirths were included for the maternal composite outcome, yet the incidence of this within the study population is not reported. Operative vaginal deliveries that involve stillbirths can be complex; a subgroup analysis excluding these would aid in interpretation.
Second, complicated OVDs, including sequential use of forceps and vacuum and OVDs from midpelvic station, were included; ACOG recommends against both these practices in routine circumstances due to known increases in maternal and neonatal morbidity.1 As such, the inclusion of these OVDs may bias results away from the null.
Finally, despite discussing the role of episiotomy, the episiotomy rate in this cohort is not reported.
Despite these limitations, the study by Muraca and colleagues is a positive step forward toward understanding the role of OVD in contemporary obstetric practice, and it uniquely ascertains the impact of OVD volume outcomes that previously had been an elusive exposure ●
While it is important to understand perinatal outcomes following OVD in a contemporary cohort, utilizing the correct cohort and reference group is critical.4 Risks for maternal and neonatal trauma follow OVD; however, outcomes vary based on appropriate selection of OVD candidates and adherence to recommended national guidelines.1,4 The infrequency of OVD raises concerns regarding adequate training for obstetricians, which should be prioritized so that they can offer OVD as a safe alternative to CD birth.3
HAYLEY E. MILLER, MD, AND DANIELLE M. PANELLI, MD
Muraca GM, Boutin A, Razaz N, et al. Maternal and neonatal trauma following operative vaginal delivery. CMAJ. 2022;194:E1-E12. doi: 10.1503/cmaj.210841.
EXPERT COMMENTARY
Operative vaginal delivery is used to achieve and expedite safe vaginal birth while avoiding CD and its associated morbidities.1,2 Despite support from the American College of Obstetricians and Gynecologists (ACOG) for the use of OVD as an alternative to CD, OVD was used in only 3% of all US births in 2013, a shift from approximately 30% in 1987.1,3 Reported complications of OVD are biased by the level of experience of the operator, changes in practice, and by misinterpretation of the counterfactual.1
Outcomes of OVD should be compared with appropriate reference groups, namely, with second-stage CD births rather than with spontaneous vaginal births.4 With decreasing rates of OVD, evidence of contemporary data is needed on appropriately compared perinatal outcomes.4
Details of the study
Muraca and colleagues conducted an observational cohort study of births in Canada between 2013 and 2019 to assess the incidence of maternal and neonatal trauma following OVD. They used composites defined a priori— stratified by instrument, region, level of obstetric care, and institutional OVD volume.
Results. Among 1,326,191 live or stillbirths, 2.9% were attempted forceps deliveries and 8.4% were attempted vacuum deliveries. Following forceps delivery, the maternal trauma rate was 25.3% (95% confidence interval [CI], 24.8%–25.7%), and the neonatal trauma rate was 9.6 per 1,000 live births (95% CI, 8.6–10.6). Following vacuum delivery, maternal and neonatal trauma rates were 13.2% (95% CI, 13.0%–13.4%) and 9.6 per 1,000 live births (95% CI, 9.0–10.2), respectively. Maternal trauma was driven by higher order perineal lacerations. Some association was seen between increased forceps volume and decreased maternal trauma rates.
The authors concluded that in Canada, rates of maternal and neonatal trauma following OVD are higher than previously reported in consensus statements.
Study strengths and limitations
This large contemporary study uniquely stratified perinatal outcomes following OVD. The outcomes are well defined and meaningful, but some limitations affect the generalizability of the findings.
First, stillbirths were included for the maternal composite outcome, yet the incidence of this within the study population is not reported. Operative vaginal deliveries that involve stillbirths can be complex; a subgroup analysis excluding these would aid in interpretation.
Second, complicated OVDs, including sequential use of forceps and vacuum and OVDs from midpelvic station, were included; ACOG recommends against both these practices in routine circumstances due to known increases in maternal and neonatal morbidity.1 As such, the inclusion of these OVDs may bias results away from the null.
Finally, despite discussing the role of episiotomy, the episiotomy rate in this cohort is not reported.
Despite these limitations, the study by Muraca and colleagues is a positive step forward toward understanding the role of OVD in contemporary obstetric practice, and it uniquely ascertains the impact of OVD volume outcomes that previously had been an elusive exposure ●
While it is important to understand perinatal outcomes following OVD in a contemporary cohort, utilizing the correct cohort and reference group is critical.4 Risks for maternal and neonatal trauma follow OVD; however, outcomes vary based on appropriate selection of OVD candidates and adherence to recommended national guidelines.1,4 The infrequency of OVD raises concerns regarding adequate training for obstetricians, which should be prioritized so that they can offer OVD as a safe alternative to CD birth.3
HAYLEY E. MILLER, MD, AND DANIELLE M. PANELLI, MD
- American College of Obstetricians and Gynecologists. Operative vaginal birth: ACOG practice bulletin, number 219. Obstet Gynecol. 2020;135:e149-e159.
- Spong CY, Berghella V, Wenstrom KD, et al. Preventing the first cesarean delivery: summary of a joint Eunice Kennedy Shriver National Institute of Child Health and Human Development, Society for Maternal-Fetal Medicine, and American College of Obstetricians and Gynecologists workshop. Obstet Gynecol. 2012;120:1181-1193.
- Zahniser SC, Kendrick JS, Franks AL, et al. Trends in obstetric operative procedures, 1980 to 1987. Am J Public Health. 1992;82:1340-1344.
- Panelli DM, Leonard SA, Joudi N, et al. Severe maternal and neonatal morbidity after attempted operative vaginal delivery. Am J Obstet Gynecol MFM. 2021;3: 100339.
- American College of Obstetricians and Gynecologists. Operative vaginal birth: ACOG practice bulletin, number 219. Obstet Gynecol. 2020;135:e149-e159.
- Spong CY, Berghella V, Wenstrom KD, et al. Preventing the first cesarean delivery: summary of a joint Eunice Kennedy Shriver National Institute of Child Health and Human Development, Society for Maternal-Fetal Medicine, and American College of Obstetricians and Gynecologists workshop. Obstet Gynecol. 2012;120:1181-1193.
- Zahniser SC, Kendrick JS, Franks AL, et al. Trends in obstetric operative procedures, 1980 to 1987. Am J Public Health. 1992;82:1340-1344.
- Panelli DM, Leonard SA, Joudi N, et al. Severe maternal and neonatal morbidity after attempted operative vaginal delivery. Am J Obstet Gynecol MFM. 2021;3: 100339.
Depression strikes more than half of obese adolescents
More than 50% of obese adolescents met criteria for depression, which also was associated with several components of metabolic syndrome, based on data from 160 individuals.
Previous research shows that the metabolic consequences of obesity are worsened with the coexistence of depression in adults, but a similar relationship in obese adolescents has not been explored, according to Nisha Gupta, a medical student at the University of Texas Health Science Center, Houston, and colleagues.
“This relationship is explained by an overactive stress response and adoption of unhealthy lifestyle habits,” both of which increased during the COVID-19 pandemic, the researchers noted in their abstract.
In a study presented at the Pediatric Academic Societies annual meeting, the researchers reviewed data from 160 obese adolescents seen at a pediatric weight management clinic between July 1, 2018, and Dec. 3, 2021. The data included anthropometric, clinical, and laboratory information. Depression was assessed using the Patient Health Questionnaire–9 (PHQ-9). The goal of the study was to compare the prevalence of metabolic syndrome components in obese youth with and without diagnosed depression.
Overall, 46% of the patients had PHQ-9 scores less than 5, which was defined as no clinically significant depression. A total of 26% had current or prior diagnoses of depression, and 25% met the criteria for moderate to severe depression, with PHQ-9 scores of 10 or higher. Notably, 18% of individuals with no prior history of depression met criteria for moderate to severe depression, the researchers wrote.
Teens who reported daytime fatigue or trouble sleeping, and those who reported eating out seven or more times a week had higher scores than those without these reports.
In laboratory analyses, higher PHQ-9 scores were significantly associated with increasing weight, body mass index, body fat percentage, diastolic blood pressure, and fasting blood insulin (P < .02 for all).
The study findings were limited by the relatively small sample size, the researchers noted. However, the results suggest that depression is common, but often underdiagnosed in obese adolescents, and depression screening should be part of obesity management.
Study highlights need to screen
The current study is important because of the overall increase in obesity in the United States, which extends to children and teens, Tim Joos, MD, a Seattle-based clinician with a combination internal medicine/pediatrics practice, said in an interview.
“With skyrocketing rates of obesity among children and teens over the last decades, we are seeing more ‘adult’ diseases seep into the younger ages, including type 2 diabetes, high blood pressure and now, depression,” he said.
“The results are a wake-up call for the need for better system-wide prevention and management of obesity in adolescents and the importance of screening and managing depression in obese teenagers,” he emphasized.
The study received no outside funding. The researchers had no financial conflicts to disclose. Dr. Joos had no financial conflicts to disclose and serves on the editorial advisory board of Pediatric News.
More than 50% of obese adolescents met criteria for depression, which also was associated with several components of metabolic syndrome, based on data from 160 individuals.
Previous research shows that the metabolic consequences of obesity are worsened with the coexistence of depression in adults, but a similar relationship in obese adolescents has not been explored, according to Nisha Gupta, a medical student at the University of Texas Health Science Center, Houston, and colleagues.
“This relationship is explained by an overactive stress response and adoption of unhealthy lifestyle habits,” both of which increased during the COVID-19 pandemic, the researchers noted in their abstract.
In a study presented at the Pediatric Academic Societies annual meeting, the researchers reviewed data from 160 obese adolescents seen at a pediatric weight management clinic between July 1, 2018, and Dec. 3, 2021. The data included anthropometric, clinical, and laboratory information. Depression was assessed using the Patient Health Questionnaire–9 (PHQ-9). The goal of the study was to compare the prevalence of metabolic syndrome components in obese youth with and without diagnosed depression.
Overall, 46% of the patients had PHQ-9 scores less than 5, which was defined as no clinically significant depression. A total of 26% had current or prior diagnoses of depression, and 25% met the criteria for moderate to severe depression, with PHQ-9 scores of 10 or higher. Notably, 18% of individuals with no prior history of depression met criteria for moderate to severe depression, the researchers wrote.
Teens who reported daytime fatigue or trouble sleeping, and those who reported eating out seven or more times a week had higher scores than those without these reports.
In laboratory analyses, higher PHQ-9 scores were significantly associated with increasing weight, body mass index, body fat percentage, diastolic blood pressure, and fasting blood insulin (P < .02 for all).
The study findings were limited by the relatively small sample size, the researchers noted. However, the results suggest that depression is common, but often underdiagnosed in obese adolescents, and depression screening should be part of obesity management.
Study highlights need to screen
The current study is important because of the overall increase in obesity in the United States, which extends to children and teens, Tim Joos, MD, a Seattle-based clinician with a combination internal medicine/pediatrics practice, said in an interview.
“With skyrocketing rates of obesity among children and teens over the last decades, we are seeing more ‘adult’ diseases seep into the younger ages, including type 2 diabetes, high blood pressure and now, depression,” he said.
“The results are a wake-up call for the need for better system-wide prevention and management of obesity in adolescents and the importance of screening and managing depression in obese teenagers,” he emphasized.
The study received no outside funding. The researchers had no financial conflicts to disclose. Dr. Joos had no financial conflicts to disclose and serves on the editorial advisory board of Pediatric News.
More than 50% of obese adolescents met criteria for depression, which also was associated with several components of metabolic syndrome, based on data from 160 individuals.
Previous research shows that the metabolic consequences of obesity are worsened with the coexistence of depression in adults, but a similar relationship in obese adolescents has not been explored, according to Nisha Gupta, a medical student at the University of Texas Health Science Center, Houston, and colleagues.
“This relationship is explained by an overactive stress response and adoption of unhealthy lifestyle habits,” both of which increased during the COVID-19 pandemic, the researchers noted in their abstract.
In a study presented at the Pediatric Academic Societies annual meeting, the researchers reviewed data from 160 obese adolescents seen at a pediatric weight management clinic between July 1, 2018, and Dec. 3, 2021. The data included anthropometric, clinical, and laboratory information. Depression was assessed using the Patient Health Questionnaire–9 (PHQ-9). The goal of the study was to compare the prevalence of metabolic syndrome components in obese youth with and without diagnosed depression.
Overall, 46% of the patients had PHQ-9 scores less than 5, which was defined as no clinically significant depression. A total of 26% had current or prior diagnoses of depression, and 25% met the criteria for moderate to severe depression, with PHQ-9 scores of 10 or higher. Notably, 18% of individuals with no prior history of depression met criteria for moderate to severe depression, the researchers wrote.
Teens who reported daytime fatigue or trouble sleeping, and those who reported eating out seven or more times a week had higher scores than those without these reports.
In laboratory analyses, higher PHQ-9 scores were significantly associated with increasing weight, body mass index, body fat percentage, diastolic blood pressure, and fasting blood insulin (P < .02 for all).
The study findings were limited by the relatively small sample size, the researchers noted. However, the results suggest that depression is common, but often underdiagnosed in obese adolescents, and depression screening should be part of obesity management.
Study highlights need to screen
The current study is important because of the overall increase in obesity in the United States, which extends to children and teens, Tim Joos, MD, a Seattle-based clinician with a combination internal medicine/pediatrics practice, said in an interview.
“With skyrocketing rates of obesity among children and teens over the last decades, we are seeing more ‘adult’ diseases seep into the younger ages, including type 2 diabetes, high blood pressure and now, depression,” he said.
“The results are a wake-up call for the need for better system-wide prevention and management of obesity in adolescents and the importance of screening and managing depression in obese teenagers,” he emphasized.
The study received no outside funding. The researchers had no financial conflicts to disclose. Dr. Joos had no financial conflicts to disclose and serves on the editorial advisory board of Pediatric News.
FROM PAS 2022
Restrictive, vegan-based diet linked to fewer RA symptoms
A . After 16 weeks, the mean Disease Activity Score in 28 joints (DAS28) decreased from 4.5 to 2.5 (P < .001), and the mean number of swollen joints dipped from 7.0 to 3.3 (P = .03).
The study was published in the American Journal of Lifestyle Medicine. It’s not clear whether the vegan diet or the restriction of trigger foods – or both or neither – was helpful. Significant weight loss in the diet group could have played a role in reducing symptoms.
Still, the dietary strategy is “a life-changing experience for people,” lead author Neal D. Barnard, MD, an internal medicine specialist and adjunct professor of medicine at George Washington University, Washington, D.C, and president of the Physicians Committee for Responsible Medicine, said in an interview. “Doctors should know about it, and they should try it themselves.”
The researchers launched the study to determine the feasibility of a “practical and easy-to-prescribe diet” without caloric limits, Dr. Barnard said. “People have done a variety of studies where they’ve looked at diet changes, often with fasting, and the quality has been variable.”
There’s no consensus in the medical literature on which dietary approach is best for patients with RA. A 2021 systematic review by Philippa and colleagues found positive results for the Mediterranean diet, high doses of omega-3 fatty acids, vitamin D supplementation, and sodium restriction. Fasting had significant but temporary effects, and the reviewers noted “outcomes from vegetarian, elimination, peptide, or elemental diets suggested that responses are very individualized.”
For the new randomized, crossover study, researchers assigned 44 women to one of two diet phases. After 16 weeks, they had a 4-week washout period, then began the other 16-week phase. A total of 32 patients completed the study, and they had a mean age of 57 years. Overall, 66% were White, 16% were Black, and 79% held a college degree or graduate degree.
In the 16-week intervention phase, participants went on a low-fat vegan diet. After 4 weeks, they eliminated common RA trigger foods such as grains with gluten, nuts, citrus fruits, and chocolate. After week 7, the subjects added back the trigger foods one by one, keeping them in their diet if they didn’t seem to cause pain.
In the 16-week placebo phase, the women took a supplement that they were told contained omega-3 oils and vitamin E. However, the amounts of omega-3 and vitamin E were very low and had no apparent effect.
Participants in the diet phase attended weekly 1-hour dietary support-group sessions. Thirty-two women completed the full study.
Average DAS28 scores fell in the diet phase, compared with the supplement phase (treatment effect, 1.8 [95% confidence interval [CI], 3.2 to 0.4]; P = .01), as did swollen joints (treatment effect, –4.2 [95% CI, –8.3 to –0.1], P = .047).
While the researchers reported dips in the DAS28 score and swollen joints, “the reductions in the number of painful and tender joints did not reach statistical significance (treatment effects, –4.1 [95% CI, –8.7 to +0.5]; P = .08; and –1.8 [95% CI, –5.5 to +1.9]; P = .41, respectively).”
Mean body weight fell by 6.5 kg among those in the diet group, while those in the placebo group gained 0.8 kg (treatment effect, –7.3 kg [95% CI, –9.4 to –5.1]; P < .001).
The researchers noted “the presumed mechanisms by which diets such [as this intervention strategy] reduce joint symptoms relate to the removal of inflammatory elements of an omnivorous diet, the presence of anti-inflammatory constituents in a plant-based diet, and diet-induced reductions in gut permeability that may, in turn, reduce the passage of antigens into circulation.”
Patients tolerate the diet well, Dr. Barnard said. “It’s practical for day-to-day life, and you don’t have to check into a fasting hospital.”
The message for physicians, he said, is to encourage patients to try changing their eating patterns before turning to medication. “It’s a good idea for anyone to have a chance to try a diet change,” he said. “You’ll know within a matter of weeks whether it will work.”
Vegan diets are also cheaper than diets with meat and dairy, he added.
The study has various limitations. It began with 44 participants, but 12 failed to complete it for various reasons. Four participants who were assigned to the diet phase first refused to resume their regular diets during the next phase. It’s not clear if the lost weight is most responsible for the diet’s benefits, Harvard Medical School rheumatologist Daniel H. Solomon, MD, MPH, said in an interview. In his review of the study findings, Dr. Solomon said that another possibility is that certain aspects of the diet – and not the full diet – were responsible.
“I am sure that motivated patients could follow such a diet,” he said, “but first we should determine if the specific diet was the key issue or whether weight loss was more important.”
The study was funded by the Physicians Committee for Responsible Medicine. Dr. Barnard disclosed royalties and honoraria from books, articles, and lectures on nutrition and health.
A . After 16 weeks, the mean Disease Activity Score in 28 joints (DAS28) decreased from 4.5 to 2.5 (P < .001), and the mean number of swollen joints dipped from 7.0 to 3.3 (P = .03).
The study was published in the American Journal of Lifestyle Medicine. It’s not clear whether the vegan diet or the restriction of trigger foods – or both or neither – was helpful. Significant weight loss in the diet group could have played a role in reducing symptoms.
Still, the dietary strategy is “a life-changing experience for people,” lead author Neal D. Barnard, MD, an internal medicine specialist and adjunct professor of medicine at George Washington University, Washington, D.C, and president of the Physicians Committee for Responsible Medicine, said in an interview. “Doctors should know about it, and they should try it themselves.”
The researchers launched the study to determine the feasibility of a “practical and easy-to-prescribe diet” without caloric limits, Dr. Barnard said. “People have done a variety of studies where they’ve looked at diet changes, often with fasting, and the quality has been variable.”
There’s no consensus in the medical literature on which dietary approach is best for patients with RA. A 2021 systematic review by Philippa and colleagues found positive results for the Mediterranean diet, high doses of omega-3 fatty acids, vitamin D supplementation, and sodium restriction. Fasting had significant but temporary effects, and the reviewers noted “outcomes from vegetarian, elimination, peptide, or elemental diets suggested that responses are very individualized.”
For the new randomized, crossover study, researchers assigned 44 women to one of two diet phases. After 16 weeks, they had a 4-week washout period, then began the other 16-week phase. A total of 32 patients completed the study, and they had a mean age of 57 years. Overall, 66% were White, 16% were Black, and 79% held a college degree or graduate degree.
In the 16-week intervention phase, participants went on a low-fat vegan diet. After 4 weeks, they eliminated common RA trigger foods such as grains with gluten, nuts, citrus fruits, and chocolate. After week 7, the subjects added back the trigger foods one by one, keeping them in their diet if they didn’t seem to cause pain.
In the 16-week placebo phase, the women took a supplement that they were told contained omega-3 oils and vitamin E. However, the amounts of omega-3 and vitamin E were very low and had no apparent effect.
Participants in the diet phase attended weekly 1-hour dietary support-group sessions. Thirty-two women completed the full study.
Average DAS28 scores fell in the diet phase, compared with the supplement phase (treatment effect, 1.8 [95% confidence interval [CI], 3.2 to 0.4]; P = .01), as did swollen joints (treatment effect, –4.2 [95% CI, –8.3 to –0.1], P = .047).
While the researchers reported dips in the DAS28 score and swollen joints, “the reductions in the number of painful and tender joints did not reach statistical significance (treatment effects, –4.1 [95% CI, –8.7 to +0.5]; P = .08; and –1.8 [95% CI, –5.5 to +1.9]; P = .41, respectively).”
Mean body weight fell by 6.5 kg among those in the diet group, while those in the placebo group gained 0.8 kg (treatment effect, –7.3 kg [95% CI, –9.4 to –5.1]; P < .001).
The researchers noted “the presumed mechanisms by which diets such [as this intervention strategy] reduce joint symptoms relate to the removal of inflammatory elements of an omnivorous diet, the presence of anti-inflammatory constituents in a plant-based diet, and diet-induced reductions in gut permeability that may, in turn, reduce the passage of antigens into circulation.”
Patients tolerate the diet well, Dr. Barnard said. “It’s practical for day-to-day life, and you don’t have to check into a fasting hospital.”
The message for physicians, he said, is to encourage patients to try changing their eating patterns before turning to medication. “It’s a good idea for anyone to have a chance to try a diet change,” he said. “You’ll know within a matter of weeks whether it will work.”
Vegan diets are also cheaper than diets with meat and dairy, he added.
The study has various limitations. It began with 44 participants, but 12 failed to complete it for various reasons. Four participants who were assigned to the diet phase first refused to resume their regular diets during the next phase. It’s not clear if the lost weight is most responsible for the diet’s benefits, Harvard Medical School rheumatologist Daniel H. Solomon, MD, MPH, said in an interview. In his review of the study findings, Dr. Solomon said that another possibility is that certain aspects of the diet – and not the full diet – were responsible.
“I am sure that motivated patients could follow such a diet,” he said, “but first we should determine if the specific diet was the key issue or whether weight loss was more important.”
The study was funded by the Physicians Committee for Responsible Medicine. Dr. Barnard disclosed royalties and honoraria from books, articles, and lectures on nutrition and health.
A . After 16 weeks, the mean Disease Activity Score in 28 joints (DAS28) decreased from 4.5 to 2.5 (P < .001), and the mean number of swollen joints dipped from 7.0 to 3.3 (P = .03).
The study was published in the American Journal of Lifestyle Medicine. It’s not clear whether the vegan diet or the restriction of trigger foods – or both or neither – was helpful. Significant weight loss in the diet group could have played a role in reducing symptoms.
Still, the dietary strategy is “a life-changing experience for people,” lead author Neal D. Barnard, MD, an internal medicine specialist and adjunct professor of medicine at George Washington University, Washington, D.C, and president of the Physicians Committee for Responsible Medicine, said in an interview. “Doctors should know about it, and they should try it themselves.”
The researchers launched the study to determine the feasibility of a “practical and easy-to-prescribe diet” without caloric limits, Dr. Barnard said. “People have done a variety of studies where they’ve looked at diet changes, often with fasting, and the quality has been variable.”
There’s no consensus in the medical literature on which dietary approach is best for patients with RA. A 2021 systematic review by Philippa and colleagues found positive results for the Mediterranean diet, high doses of omega-3 fatty acids, vitamin D supplementation, and sodium restriction. Fasting had significant but temporary effects, and the reviewers noted “outcomes from vegetarian, elimination, peptide, or elemental diets suggested that responses are very individualized.”
For the new randomized, crossover study, researchers assigned 44 women to one of two diet phases. After 16 weeks, they had a 4-week washout period, then began the other 16-week phase. A total of 32 patients completed the study, and they had a mean age of 57 years. Overall, 66% were White, 16% were Black, and 79% held a college degree or graduate degree.
In the 16-week intervention phase, participants went on a low-fat vegan diet. After 4 weeks, they eliminated common RA trigger foods such as grains with gluten, nuts, citrus fruits, and chocolate. After week 7, the subjects added back the trigger foods one by one, keeping them in their diet if they didn’t seem to cause pain.
In the 16-week placebo phase, the women took a supplement that they were told contained omega-3 oils and vitamin E. However, the amounts of omega-3 and vitamin E were very low and had no apparent effect.
Participants in the diet phase attended weekly 1-hour dietary support-group sessions. Thirty-two women completed the full study.
Average DAS28 scores fell in the diet phase, compared with the supplement phase (treatment effect, 1.8 [95% confidence interval [CI], 3.2 to 0.4]; P = .01), as did swollen joints (treatment effect, –4.2 [95% CI, –8.3 to –0.1], P = .047).
While the researchers reported dips in the DAS28 score and swollen joints, “the reductions in the number of painful and tender joints did not reach statistical significance (treatment effects, –4.1 [95% CI, –8.7 to +0.5]; P = .08; and –1.8 [95% CI, –5.5 to +1.9]; P = .41, respectively).”
Mean body weight fell by 6.5 kg among those in the diet group, while those in the placebo group gained 0.8 kg (treatment effect, –7.3 kg [95% CI, –9.4 to –5.1]; P < .001).
The researchers noted “the presumed mechanisms by which diets such [as this intervention strategy] reduce joint symptoms relate to the removal of inflammatory elements of an omnivorous diet, the presence of anti-inflammatory constituents in a plant-based diet, and diet-induced reductions in gut permeability that may, in turn, reduce the passage of antigens into circulation.”
Patients tolerate the diet well, Dr. Barnard said. “It’s practical for day-to-day life, and you don’t have to check into a fasting hospital.”
The message for physicians, he said, is to encourage patients to try changing their eating patterns before turning to medication. “It’s a good idea for anyone to have a chance to try a diet change,” he said. “You’ll know within a matter of weeks whether it will work.”
Vegan diets are also cheaper than diets with meat and dairy, he added.
The study has various limitations. It began with 44 participants, but 12 failed to complete it for various reasons. Four participants who were assigned to the diet phase first refused to resume their regular diets during the next phase. It’s not clear if the lost weight is most responsible for the diet’s benefits, Harvard Medical School rheumatologist Daniel H. Solomon, MD, MPH, said in an interview. In his review of the study findings, Dr. Solomon said that another possibility is that certain aspects of the diet – and not the full diet – were responsible.
“I am sure that motivated patients could follow such a diet,” he said, “but first we should determine if the specific diet was the key issue or whether weight loss was more important.”
The study was funded by the Physicians Committee for Responsible Medicine. Dr. Barnard disclosed royalties and honoraria from books, articles, and lectures on nutrition and health.
FROM THE AMERICAN JOURNAL OF LIFESTYLE MEDICINE
Psychiatric illness associated with eosinophilic esophagitis
People with eosinophilic esophagitis (EoE) may run an increased risk of mood disorders, anxiety, and ADHD and should be screened for those conditions, researchers say.
“It’s important to know that there is an elevated risk of those diagnoses, so you have that in mind when you treat your patients. You can assess their quality of life and the status of their mental state,” said lead author Lovisa Röjler, MD, a pediatrician and doctoral student at Örebro (Sweden) University Hospital.
“Psychiatric disorders are not found with a blood sample or radiology examination,” she said in an interview.
The study was published online in the American Journal of Gastroenterology.
Elevated risk found
Previous studies into the relationship between EoE and anxiety and depression have conflicting conclusions.
In the hope of shedding further light, Dr. Röjler and colleagues analyzed data from Sweden’s ESPRESSO cohort, which consists of more than 6 million biopsy samples from the gastrointestinal tract that were collected from throughout the country during the years 1965-2017.
They identified 1,458 people with EoE who had not experienced psychiatric events before being diagnosed with EoE. Of these, 70% had dysphagia, and 58% had food impaction.
In the study, up to 5 reference persons (6,436 people) without EoE who were identified from the Swedish Total Population Register were matched to the patients with EoE by age, sex, county, and year of diagnosis.
Among the people with EoE, there were 106 events of psychiatric disease, at an incidence of 15.96 per 1,000 person-years versus 10.93 per 1,000 person-years (331 events) among those without EoE. This 50% increased risk for psychiatric illness for people with EoE was statistically significant (hazard ratio, 1.50; 95% confidence interval, 1.20-1.87).
To adjust for genetic and environmental confounding factors, the researchers compared the rate of psychiatric events among 1,055 people with EoE with that of siblings who did not have EoE (1,699 people). There were 74 events of psychiatric disease among the siblings (8.99 per 1000 person-years). From this the researchers calculated a 62% increased risk of psychiatric events for those with EoE (HR, 1.62; 95% CI, 1.14-2.31).
There was no difference in risk for psychiatric disorders by educational attainment, though people for whom there were no data on education were at increased risk.
There was also no difference in psychiatric risk associated with the use of steroids or proton pump inhibitors for EoE, though these medications have sometimes been linked to psychiatric disorders.
After adjusting for inflammatory bowel disease, celiac disease, and asthma, the researchers still found an increased risk of psychiatric events. Also, the people who had EoE were no more likely than the reference persons to have had psychiatric events before their diagnosis, suggesting that EoE caused the psychiatric events rather than the other way around.
Previous researchers have found a similar association with psychiatric illness in people with celiac disease and inflammatory bowel disease. The researchers speculated that people with EoE might develop psychiatric illnesses because their symptoms and treatments, such as restrictive diets, cause stress and chronic pain and thereby cause problems with education, work, and social and economic status.
Dr. Röjler recommended that clinicians use questionnaires to identify mood disorders and ADHD in their patients and then refer them to a mental health professional.
Screen for psychiatric disorders
Tiffany Taft, PsyD, a research associate professor of medicine at Northwestern University, Chicago, who was not involved in the study, agreed that patients with EoE should be screened more often for psychiatric disorders.
“We’ve found that symptom-specific anxiety is prevalent and associated with other outcomes, like quality of life, so it may not be the typical anxiety that you would diagnose from the Diagnostic and Statistical Manual of Mental Disorders,” Dr. Taft said in an interview.
While anxiety is not likely to trigger EoE, it can worsen the symptoms, she said. Sometimes helping patients make the connection between their mental health and EoE can address the anxiety itself.
“Education is good enough for a certain chunk of patients,” Dr. Taft said.
Other patients benefit from cognitive-behavioral therapy, which gives them a more realistic understanding of their situation.
“We also add in relaxation, deep breathing, and guided imagery to calm down the stress response in the body, which is part of that brain-gut connection that enhances symptom severity,” she said.
Some patients prefer medications, or they rely on medication because that is what their insurance provides, she said, adding that most patients do best with a combination of medication and talk therapy.
Ideally, people with these disorders would be referred to someone such as herself, a psychotherapist with a specialty in gastroenterology, Dr. Taft said. But there are not many people in that subspecialty, so if a gastroenterology psychologist is not available, a psychologist who specializes in treating mental illness associated with chronic diseases is a good second choice.
The study was funded by Örebro County Council and Karolinska Institutet. Dr. Röjler and Dr. Taft reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
People with eosinophilic esophagitis (EoE) may run an increased risk of mood disorders, anxiety, and ADHD and should be screened for those conditions, researchers say.
“It’s important to know that there is an elevated risk of those diagnoses, so you have that in mind when you treat your patients. You can assess their quality of life and the status of their mental state,” said lead author Lovisa Röjler, MD, a pediatrician and doctoral student at Örebro (Sweden) University Hospital.
“Psychiatric disorders are not found with a blood sample or radiology examination,” she said in an interview.
The study was published online in the American Journal of Gastroenterology.
Elevated risk found
Previous studies into the relationship between EoE and anxiety and depression have conflicting conclusions.
In the hope of shedding further light, Dr. Röjler and colleagues analyzed data from Sweden’s ESPRESSO cohort, which consists of more than 6 million biopsy samples from the gastrointestinal tract that were collected from throughout the country during the years 1965-2017.
They identified 1,458 people with EoE who had not experienced psychiatric events before being diagnosed with EoE. Of these, 70% had dysphagia, and 58% had food impaction.
In the study, up to 5 reference persons (6,436 people) without EoE who were identified from the Swedish Total Population Register were matched to the patients with EoE by age, sex, county, and year of diagnosis.
Among the people with EoE, there were 106 events of psychiatric disease, at an incidence of 15.96 per 1,000 person-years versus 10.93 per 1,000 person-years (331 events) among those without EoE. This 50% increased risk for psychiatric illness for people with EoE was statistically significant (hazard ratio, 1.50; 95% confidence interval, 1.20-1.87).
To adjust for genetic and environmental confounding factors, the researchers compared the rate of psychiatric events among 1,055 people with EoE with that of siblings who did not have EoE (1,699 people). There were 74 events of psychiatric disease among the siblings (8.99 per 1000 person-years). From this the researchers calculated a 62% increased risk of psychiatric events for those with EoE (HR, 1.62; 95% CI, 1.14-2.31).
There was no difference in risk for psychiatric disorders by educational attainment, though people for whom there were no data on education were at increased risk.
There was also no difference in psychiatric risk associated with the use of steroids or proton pump inhibitors for EoE, though these medications have sometimes been linked to psychiatric disorders.
After adjusting for inflammatory bowel disease, celiac disease, and asthma, the researchers still found an increased risk of psychiatric events. Also, the people who had EoE were no more likely than the reference persons to have had psychiatric events before their diagnosis, suggesting that EoE caused the psychiatric events rather than the other way around.
Previous researchers have found a similar association with psychiatric illness in people with celiac disease and inflammatory bowel disease. The researchers speculated that people with EoE might develop psychiatric illnesses because their symptoms and treatments, such as restrictive diets, cause stress and chronic pain and thereby cause problems with education, work, and social and economic status.
Dr. Röjler recommended that clinicians use questionnaires to identify mood disorders and ADHD in their patients and then refer them to a mental health professional.
Screen for psychiatric disorders
Tiffany Taft, PsyD, a research associate professor of medicine at Northwestern University, Chicago, who was not involved in the study, agreed that patients with EoE should be screened more often for psychiatric disorders.
“We’ve found that symptom-specific anxiety is prevalent and associated with other outcomes, like quality of life, so it may not be the typical anxiety that you would diagnose from the Diagnostic and Statistical Manual of Mental Disorders,” Dr. Taft said in an interview.
While anxiety is not likely to trigger EoE, it can worsen the symptoms, she said. Sometimes helping patients make the connection between their mental health and EoE can address the anxiety itself.
“Education is good enough for a certain chunk of patients,” Dr. Taft said.
Other patients benefit from cognitive-behavioral therapy, which gives them a more realistic understanding of their situation.
“We also add in relaxation, deep breathing, and guided imagery to calm down the stress response in the body, which is part of that brain-gut connection that enhances symptom severity,” she said.
Some patients prefer medications, or they rely on medication because that is what their insurance provides, she said, adding that most patients do best with a combination of medication and talk therapy.
Ideally, people with these disorders would be referred to someone such as herself, a psychotherapist with a specialty in gastroenterology, Dr. Taft said. But there are not many people in that subspecialty, so if a gastroenterology psychologist is not available, a psychologist who specializes in treating mental illness associated with chronic diseases is a good second choice.
The study was funded by Örebro County Council and Karolinska Institutet. Dr. Röjler and Dr. Taft reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
People with eosinophilic esophagitis (EoE) may run an increased risk of mood disorders, anxiety, and ADHD and should be screened for those conditions, researchers say.
“It’s important to know that there is an elevated risk of those diagnoses, so you have that in mind when you treat your patients. You can assess their quality of life and the status of their mental state,” said lead author Lovisa Röjler, MD, a pediatrician and doctoral student at Örebro (Sweden) University Hospital.
“Psychiatric disorders are not found with a blood sample or radiology examination,” she said in an interview.
The study was published online in the American Journal of Gastroenterology.
Elevated risk found
Previous studies into the relationship between EoE and anxiety and depression have conflicting conclusions.
In the hope of shedding further light, Dr. Röjler and colleagues analyzed data from Sweden’s ESPRESSO cohort, which consists of more than 6 million biopsy samples from the gastrointestinal tract that were collected from throughout the country during the years 1965-2017.
They identified 1,458 people with EoE who had not experienced psychiatric events before being diagnosed with EoE. Of these, 70% had dysphagia, and 58% had food impaction.
In the study, up to 5 reference persons (6,436 people) without EoE who were identified from the Swedish Total Population Register were matched to the patients with EoE by age, sex, county, and year of diagnosis.
Among the people with EoE, there were 106 events of psychiatric disease, at an incidence of 15.96 per 1,000 person-years versus 10.93 per 1,000 person-years (331 events) among those without EoE. This 50% increased risk for psychiatric illness for people with EoE was statistically significant (hazard ratio, 1.50; 95% confidence interval, 1.20-1.87).
To adjust for genetic and environmental confounding factors, the researchers compared the rate of psychiatric events among 1,055 people with EoE with that of siblings who did not have EoE (1,699 people). There were 74 events of psychiatric disease among the siblings (8.99 per 1000 person-years). From this the researchers calculated a 62% increased risk of psychiatric events for those with EoE (HR, 1.62; 95% CI, 1.14-2.31).
There was no difference in risk for psychiatric disorders by educational attainment, though people for whom there were no data on education were at increased risk.
There was also no difference in psychiatric risk associated with the use of steroids or proton pump inhibitors for EoE, though these medications have sometimes been linked to psychiatric disorders.
After adjusting for inflammatory bowel disease, celiac disease, and asthma, the researchers still found an increased risk of psychiatric events. Also, the people who had EoE were no more likely than the reference persons to have had psychiatric events before their diagnosis, suggesting that EoE caused the psychiatric events rather than the other way around.
Previous researchers have found a similar association with psychiatric illness in people with celiac disease and inflammatory bowel disease. The researchers speculated that people with EoE might develop psychiatric illnesses because their symptoms and treatments, such as restrictive diets, cause stress and chronic pain and thereby cause problems with education, work, and social and economic status.
Dr. Röjler recommended that clinicians use questionnaires to identify mood disorders and ADHD in their patients and then refer them to a mental health professional.
Screen for psychiatric disorders
Tiffany Taft, PsyD, a research associate professor of medicine at Northwestern University, Chicago, who was not involved in the study, agreed that patients with EoE should be screened more often for psychiatric disorders.
“We’ve found that symptom-specific anxiety is prevalent and associated with other outcomes, like quality of life, so it may not be the typical anxiety that you would diagnose from the Diagnostic and Statistical Manual of Mental Disorders,” Dr. Taft said in an interview.
While anxiety is not likely to trigger EoE, it can worsen the symptoms, she said. Sometimes helping patients make the connection between their mental health and EoE can address the anxiety itself.
“Education is good enough for a certain chunk of patients,” Dr. Taft said.
Other patients benefit from cognitive-behavioral therapy, which gives them a more realistic understanding of their situation.
“We also add in relaxation, deep breathing, and guided imagery to calm down the stress response in the body, which is part of that brain-gut connection that enhances symptom severity,” she said.
Some patients prefer medications, or they rely on medication because that is what their insurance provides, she said, adding that most patients do best with a combination of medication and talk therapy.
Ideally, people with these disorders would be referred to someone such as herself, a psychotherapist with a specialty in gastroenterology, Dr. Taft said. But there are not many people in that subspecialty, so if a gastroenterology psychologist is not available, a psychologist who specializes in treating mental illness associated with chronic diseases is a good second choice.
The study was funded by Örebro County Council and Karolinska Institutet. Dr. Röjler and Dr. Taft reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM THE AMERICAN JOURNAL OF GASTROENTEROLOGY
Trans women in female sports: A sports scientist’s take
An interview with Ross Tucker, PhD
When Lia Thomas won the women’s 500-yard freestyle at the 2022 NCAA Division 1 swimming championships, the issue of trans women’s participation in female sports ignited national headlines.
which prohibit trans women’s participation.
This interview has been edited for length and clarity.
Let’s start with the proinclusion argument that there are always advantages in sports.
That’s true. The whole point of sports is to recognize people who have advantages and reward them for it. By the time this argument comes out, people have already accepted that males have advantages, right?
Some do, some don’t.
If someone uses this argument to say that we should allow trans women, basically biological males, to compete in women’s sports, they’ve implicitly accepted that there are advantages. Otherwise, what advantage are you talking about?
They would say it’s like the advantage Michael Phelps has because of his wingspan.
To answer that, you have to start by asking why women’s sports exist.
Women’s sports exist because we recognize that male physiology has biological differences that create performance advantages. Women’s sports exist to ensure that male advantages are excluded. If you allow male advantage in, you’re allowing something to cross into a category that specifically tries to exclude it. That makes the advantage possessed by trans women conceptually and substantively different from an advantage that’s possessed by Michael Phelps because his advantage doesn’t cross a category boundary line.
If someone wants to allow natural advantages to be celebrated in sports, they’re arguing against the existence of any categories, because every single category in sports is trying to filter out certain advantages.
Weight categories in boxing exist to get rid of the advantage of being stronger, taller, with greater reach. Paralympic categories filter out the natural advantage that someone has if, for example, they are only mildly affected by cerebral palsy, compared with more severely affected.
If someone wants to allow natural advantages, they’re making an argument for all advantages to be eliminated from regulation, and we would end up with sports dominated by males between the ages of 20 and 28.
There are some people suggesting open categories by height and weight.
The problem is that for any height, males will be stronger, faster, more powerful than females. For any mass, and we know this because weightlifting has categories by mass, males lift about 30% heavier than females. They’ll be about 10%-15% faster at the same height and weight.
There’d be one or two sports where you might have some women, like gymnastics. Otherwise you would have to create categories that are so small – say, under 100 pounds. But in every other category, most sports would be completely dominated by males.
It’s not a viable solution for me unless we as a society are satisfied with filtering out women.
Another argument is that if trans women have an advantage, then they would be dominating.
That one misunderstands how you assess advantage. For a trans woman to win, she still has to be good enough at the base level without the advantage, in order to parlay that advantage into winning the women’s events.
If I was in the Tour de France and you gave me a bicycle with a 100-watt motor, I wouldn’t win the Tour de France. I’d do better than I would have done without it, but I wouldn’t win. Does my failure to win prove that motors don’t give an advantage? Of course not. My failure says more about my base level of performance than it does about the motor.
In terms of trans athletes, the retention of biological attributes creates the retention of performance advantages, which means that the person’s ranking relative to their peers’ will go up when they compare themselves to women rather than men. Someone who’s ranked 500 might improve to the 250s, but you still won’t see them on a podium.
It’s the change in performance that matters, not the final outcome.
Wasn’t Lia Thomas ranked in the 500s in the men’s division?
There’s some dispute as to whether it was 460 or 550 in the 200- and 65th in the 500-yard freestyle. But the concept is the same and we can use that case because we know the percentage performance change.
As Will Thomas, the performance was 4:18 in the 500-yard freestyle. As Lia Thomas, it’s 4:33. Ms. Thomas has slowed by 5.8% as a result of testosterone suppression. That’s fairly typical; most studies so far suggest performance impairments in that range.
The thing is that the male-female gap in swimming times is 10%-12% on average. That means that Ms. Thomas has retained about half the male advantage.
In strength events, for instance, weightlifting, where the gap is 30% or more, if you lost 10%, you’d still retain a 20% advantage and you’d jump more ranking places.
The retention of about half the male advantage is enough for No. 1 in the NCAA, but it’s not enough to move Ms. Thomas to No. 1 in the world.
The record set by Katie Ledecky in the 500 freestyle is 4:24. Thomas swam 4:18 as a man so could only afford to lose about 1% to be the record holder in women’s swimming.
When Ms. Thomas was beaten by cisgender women in other events, your point is that’s just because her baseline (pretransition) time wasn’t good enough.
Exactly. Are your performances in men’s sports close enough to the best woman such that you can turn that retained advantage into dominance, winning in women’s sports?
If the answer to that is yes, then you get Thomas in the 500. If the answer to that is not quite, then you get Thomas in the other distances.
On your podcast, you expressed frustration at having to keep debunking these arguments. Why do you think they persist?
There are a few things in play. There are nuances around the idea of advantage that people from outside sports don’t always appreciate.
But then the second thing comes into play and that’s the fact that this is an emotive issue. If you come to this debate wanting trans inclusion, then you reject the idea that it’s unfair. You will dismiss everything I’ve just said.
There’s a third thing. When people invoke the Phelps wingspan argument, they haven’t thought through the implications. If you could sit them down and say: “Okay. If you want to get rid of regulating natural advantages, then we would get rid of male and female categories,” what do you think would happen then?
They may still support inclusion because that’s their world view, but at least they’re honest now and understand the implications. But most people don’t go through that process.
I get that men are faster but I was shocked at how many are faster than elite women – for example, Allyson Felix.
There’s an amazing visual representation of that.
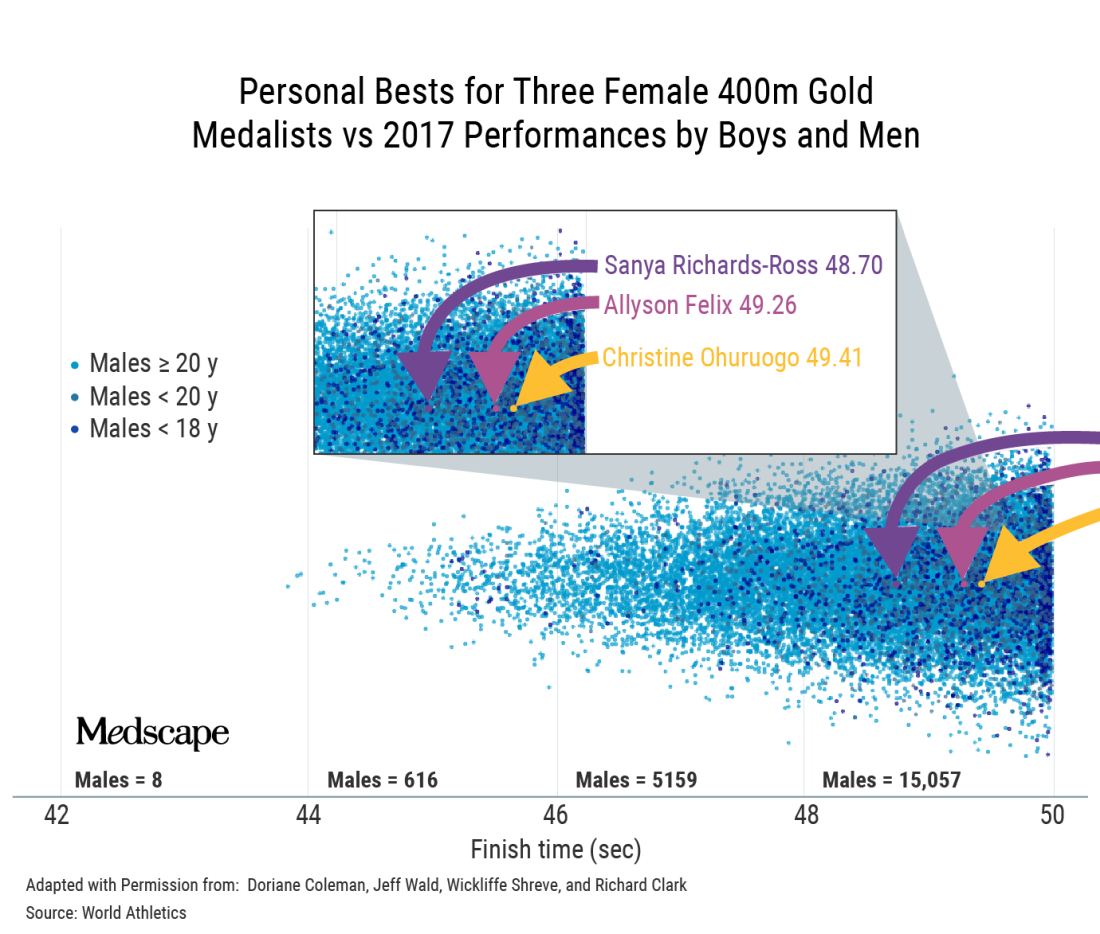
That’s a classic example where, if you’re immersed in sports, it becomes intuitive. If you’re not, you do a double-take and think, is that right? Position determines perspective.
Do you think some of it is because we’re constantly told that girls and women can do anything?
It’s a paradox that is difficult for people to get their minds around because in most walks of life, we can say that women can do anything. Of course, it’s arguably more difficult for women to become CEOs of Fortune 500 companies. This is a work in progress.
But sports are different. In sports, it’s not possible to directly compare male and female, and then tell girls they can be the best at whatever in the whole human race. That’s the uniqueness of sports and the reason categories exist in the first place. The biology does matter.
Speaking of biology, you’ve said that the focus on testosterone levels is a bit of a red herring.
Yes. The authorities were looking for a solution.
They grabbed onto the idea that lowering testosterone was the solution and perpetuated that as the mechanism by which we would ensure fairness. The problem is that my concentration of testosterone today is only a tiny part of the story.
I’ve been exposed to testosterone my whole life. My twin sister has not. There are many differences between us, but in terms of sports, the main biological difference is not that my testosterone is higher today; it’s that my testosterone has been higher my whole life. It’s the work done by that hormone over many years that makes a difference.
The key issue is, has this body, this physiology, been exposed to and benefited in the sports context, from male hormones – yes or no?
If your answer is yes, then that body belongs in male sports. With gender identity, we want to accommodate as far as possible, but we can’t take away that difference. That’s where we create this collision of rights between trans women and women.
Ultimately, your point is that we can’t have both fairness and inclusion.
When we sat down to do the World Rugby trans guidance, we had an epiphany: It doesn’t matter which way we go; we’re going to face hostility.
Once you accept that there are two parties that are affected and one of them will always be unhappy, then you start to see that fairness and inclusion can’t be balanced.
What about Joanna Harper’s proposal to make rules case by case and sport by sport?
First, it could be tricky legally because you’re effectively discriminating against some people within a subset of a subset. You’re going to end up saying to some trans women: “You can play because you don’t pose a safety or fairness issue.” But to another: “You can’t because you’re too strong.”
Then the problem is, how do you do that screening? It’s not like you can measure half a dozen variables and then have an algorithm spit out a performance level that tells you that this trans woman can compete here safely and fairly. It’s a theoretical solution that is practically impossible.
At a conference in Boston recently, Joanna said that when there are no medals, prize money, scholarships, or record times, we should allow inclusion. But just because a woman isn’t winning medals or going to the Olympics doesn’t mean there’s not considerable value for her if she were to make her school team, for instance.
There are only 11 places on the soccer field, eight lanes in a swimming pool. The moment you allow someone in, you potentially exclude someone else. And that happens everywhere, not only at the elite level.
Would you ever make a distinction between elite and subelite?
One of the beauties of sports is that it’s a meritocracy; it functions on a pathway system. I don’t think the level matters if you can track that this person’s presence denied a place on the team or a place at the competition to someone else.
With Lia Thomas, it’s not only denying the silver medalist gold or fourth place a bronze; it’s also the fact that there are only so many places at that meet. For some, that was their ambition and they weren’t able to realize it.
Now, a lot of sports are played outside that pathway. Say your local tennis club has a social league. There is little there to stand in the way of inclusion. Although I’m mindful that there may be a women’s league where it does matter to them.
We can try to accommodate trans women when the stakes are not high, provided that two requirements are met: One is that there’s no disruption to the selection/meritocracy pathway; and the second key point is that women must be okay with that inclusion, particularly if there are safety considerations, but even if it’s just a fairness consideration.
That’s where it gets tricky, because there are bigoted people in the world. Unfortunately, sometimes it’s difficult to tell whether people are using scientific arguments to prop up bigotry or whether they are genuine.
Joanna Harper has said that if you support inclusion, you have to be okay with trans women winning.
Winning the summer tennis league is not winning in the same sense as winning at the NCAA.
But the moment winning means selection and performance pathways, then I think we have to draw a line. The moment participation disrupts the natural order in sports, then it’s a problem.
In World Rugby, we proposed open competitions lower in contact to deal with the safety concerns. That was rejected by the trans community because they felt it was othering – that we were trying to squeeze them off to the side.
If you offered me one of two choices: no participation, or inclusion and they have to be able to win, I’d go for the former.
How did you get involved in this topic?
I got involved because I testified in the Caster Semenya case at the Court of Arbitration for Sport.
That is not a transgender issue; it’s a difference of sex development issue. What it has in common is the question of what to do with male-bodied biological advantage in sports.
When World Rugby joined the Olympic Games, we followed the IOC transgender policy. In 2019, it became apparent from the latest research that male advantage isn’t removed by testosterone suppression. We decided to delete the previous policy and make a new one.
The latest IOC policy is kind of no policy; it leaves it up to the governing bodies for each sport.
The one element of progress in what the IOC released, and it really is the only one, is that they’ve recognized that sports have to manage three imperatives: fairness, inclusion, and safety.
The 2015 IOC document says something like “sports should strive to be as inclusive as possible, but the overriding objective remains to guarantee a fair competition.” Basically, fair competition was nonnegotiable and must be guaranteed.
Of course, that policy allowed for testosterone suppression, and you’d have a difficult time convincing a physiologist that lowering testosterone guarantees fair competition.
Where there is merit in the current policy is that it’s clear that sports like rugby, boxing, taekwondo, and judo have a different equation with respect to safety, fairness, and inclusion than sports like equestrian, shooting, and archery. I think that’s wise to acknowledge.
However, the IOC policy doesn’t do anything to lead. In fact, what they said was extraordinary: There should be no presumption of advantage. If there’s no presumption of advantage for male-bodied athletes, then why do they persist with two categories? If there’s no presumption of advantage for trans women, are they saying that gender identity removes the advantage? We know that’s not true. We know that at the very least, you should presume that there is some advantage. How you manage it is up to you, but you can’t say that it’s not there.
This is a hostile debate. Have you ever thought: Maybe I’ll just shut up and stick to other sports topics?
Big time. The Lia Thomas case brought out a lot of vitriol. From about 2017, the situation we had with Ms. Thomas was predictable. The problem is that 95% of the world didn’t know this was happening and were taken by surprise.
The number of people who have opinions has exploded. A lot wade in without much thought. I’ve seen people question Lia Thomas’s motives. Presumably, Lia Thomas is trans, identifies as a woman, and therefore thinks she belongs in women’s sports. But I’ve seen people saying she only wants to swim in women’s sports because she knows she’ll win. And that’s not the worst of it. I’ve seen people saying Lia Thomas is only identifying as a woman so she can get into women’s changing rooms.
I don’t see how that helps the conversation. It just polarizes to the point that neither side is listening to the other. Before it was the trans community that wasn’t interested in talking about the idea of advantage, fairness, and safety. Their position is that trans women are women; how do you even have a discussion when they’ve got that dogma as their foundation?
Now, unfortunately, on the other side, we’re seeing unnecessary offensive tactics. For example, I’ve referred to Lia Thomas as “she.” I’ll have people shouting at me for using “she.” You’ve got to pick your battles, and that’s not the one you want to be fighting, in my opinion.
A version of this article first appeared on Medscape.com.
An interview with Ross Tucker, PhD
An interview with Ross Tucker, PhD
When Lia Thomas won the women’s 500-yard freestyle at the 2022 NCAA Division 1 swimming championships, the issue of trans women’s participation in female sports ignited national headlines.
which prohibit trans women’s participation.
This interview has been edited for length and clarity.
Let’s start with the proinclusion argument that there are always advantages in sports.
That’s true. The whole point of sports is to recognize people who have advantages and reward them for it. By the time this argument comes out, people have already accepted that males have advantages, right?
Some do, some don’t.
If someone uses this argument to say that we should allow trans women, basically biological males, to compete in women’s sports, they’ve implicitly accepted that there are advantages. Otherwise, what advantage are you talking about?
They would say it’s like the advantage Michael Phelps has because of his wingspan.
To answer that, you have to start by asking why women’s sports exist.
Women’s sports exist because we recognize that male physiology has biological differences that create performance advantages. Women’s sports exist to ensure that male advantages are excluded. If you allow male advantage in, you’re allowing something to cross into a category that specifically tries to exclude it. That makes the advantage possessed by trans women conceptually and substantively different from an advantage that’s possessed by Michael Phelps because his advantage doesn’t cross a category boundary line.
If someone wants to allow natural advantages to be celebrated in sports, they’re arguing against the existence of any categories, because every single category in sports is trying to filter out certain advantages.
Weight categories in boxing exist to get rid of the advantage of being stronger, taller, with greater reach. Paralympic categories filter out the natural advantage that someone has if, for example, they are only mildly affected by cerebral palsy, compared with more severely affected.
If someone wants to allow natural advantages, they’re making an argument for all advantages to be eliminated from regulation, and we would end up with sports dominated by males between the ages of 20 and 28.
There are some people suggesting open categories by height and weight.
The problem is that for any height, males will be stronger, faster, more powerful than females. For any mass, and we know this because weightlifting has categories by mass, males lift about 30% heavier than females. They’ll be about 10%-15% faster at the same height and weight.
There’d be one or two sports where you might have some women, like gymnastics. Otherwise you would have to create categories that are so small – say, under 100 pounds. But in every other category, most sports would be completely dominated by males.
It’s not a viable solution for me unless we as a society are satisfied with filtering out women.
Another argument is that if trans women have an advantage, then they would be dominating.
That one misunderstands how you assess advantage. For a trans woman to win, she still has to be good enough at the base level without the advantage, in order to parlay that advantage into winning the women’s events.
If I was in the Tour de France and you gave me a bicycle with a 100-watt motor, I wouldn’t win the Tour de France. I’d do better than I would have done without it, but I wouldn’t win. Does my failure to win prove that motors don’t give an advantage? Of course not. My failure says more about my base level of performance than it does about the motor.
In terms of trans athletes, the retention of biological attributes creates the retention of performance advantages, which means that the person’s ranking relative to their peers’ will go up when they compare themselves to women rather than men. Someone who’s ranked 500 might improve to the 250s, but you still won’t see them on a podium.
It’s the change in performance that matters, not the final outcome.
Wasn’t Lia Thomas ranked in the 500s in the men’s division?
There’s some dispute as to whether it was 460 or 550 in the 200- and 65th in the 500-yard freestyle. But the concept is the same and we can use that case because we know the percentage performance change.
As Will Thomas, the performance was 4:18 in the 500-yard freestyle. As Lia Thomas, it’s 4:33. Ms. Thomas has slowed by 5.8% as a result of testosterone suppression. That’s fairly typical; most studies so far suggest performance impairments in that range.
The thing is that the male-female gap in swimming times is 10%-12% on average. That means that Ms. Thomas has retained about half the male advantage.
In strength events, for instance, weightlifting, where the gap is 30% or more, if you lost 10%, you’d still retain a 20% advantage and you’d jump more ranking places.
The retention of about half the male advantage is enough for No. 1 in the NCAA, but it’s not enough to move Ms. Thomas to No. 1 in the world.
The record set by Katie Ledecky in the 500 freestyle is 4:24. Thomas swam 4:18 as a man so could only afford to lose about 1% to be the record holder in women’s swimming.
When Ms. Thomas was beaten by cisgender women in other events, your point is that’s just because her baseline (pretransition) time wasn’t good enough.
Exactly. Are your performances in men’s sports close enough to the best woman such that you can turn that retained advantage into dominance, winning in women’s sports?
If the answer to that is yes, then you get Thomas in the 500. If the answer to that is not quite, then you get Thomas in the other distances.
On your podcast, you expressed frustration at having to keep debunking these arguments. Why do you think they persist?
There are a few things in play. There are nuances around the idea of advantage that people from outside sports don’t always appreciate.
But then the second thing comes into play and that’s the fact that this is an emotive issue. If you come to this debate wanting trans inclusion, then you reject the idea that it’s unfair. You will dismiss everything I’ve just said.
There’s a third thing. When people invoke the Phelps wingspan argument, they haven’t thought through the implications. If you could sit them down and say: “Okay. If you want to get rid of regulating natural advantages, then we would get rid of male and female categories,” what do you think would happen then?
They may still support inclusion because that’s their world view, but at least they’re honest now and understand the implications. But most people don’t go through that process.
I get that men are faster but I was shocked at how many are faster than elite women – for example, Allyson Felix.
There’s an amazing visual representation of that.
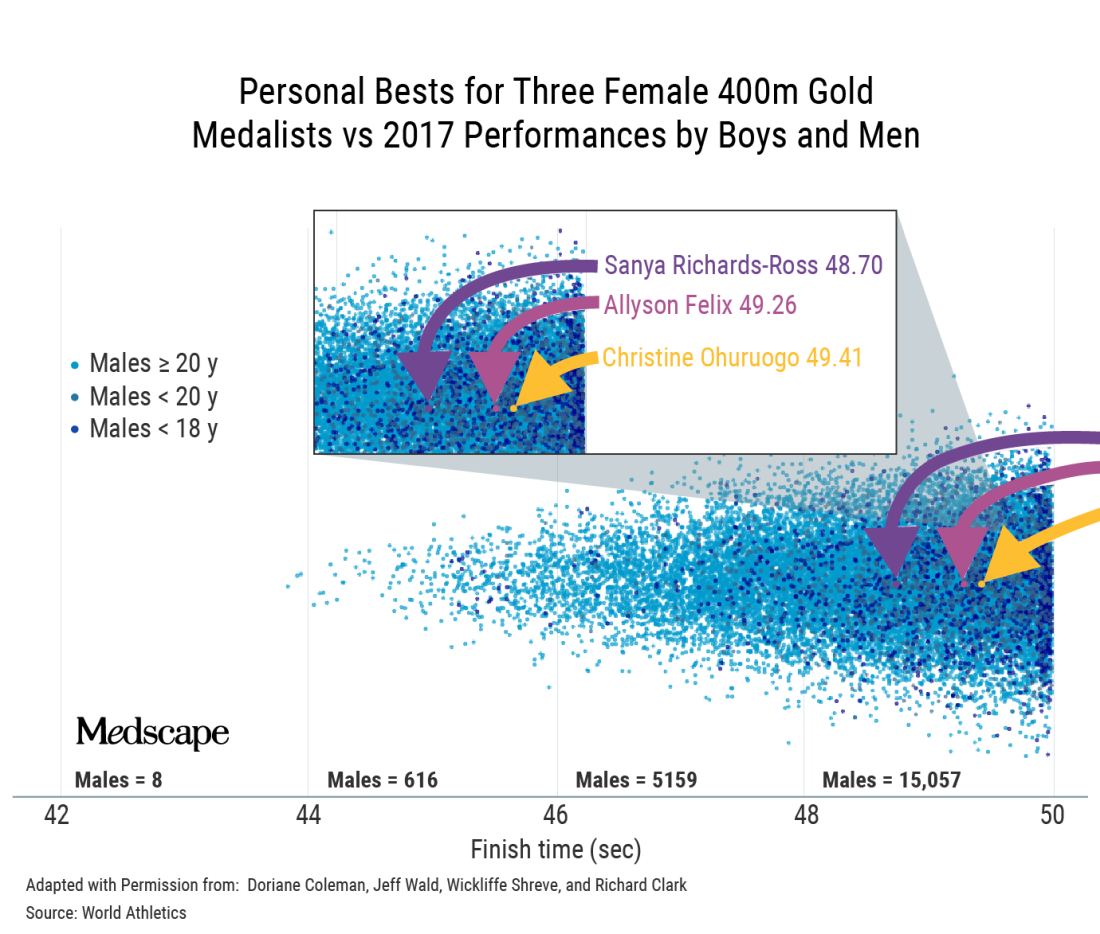
That’s a classic example where, if you’re immersed in sports, it becomes intuitive. If you’re not, you do a double-take and think, is that right? Position determines perspective.
Do you think some of it is because we’re constantly told that girls and women can do anything?
It’s a paradox that is difficult for people to get their minds around because in most walks of life, we can say that women can do anything. Of course, it’s arguably more difficult for women to become CEOs of Fortune 500 companies. This is a work in progress.
But sports are different. In sports, it’s not possible to directly compare male and female, and then tell girls they can be the best at whatever in the whole human race. That’s the uniqueness of sports and the reason categories exist in the first place. The biology does matter.
Speaking of biology, you’ve said that the focus on testosterone levels is a bit of a red herring.
Yes. The authorities were looking for a solution.
They grabbed onto the idea that lowering testosterone was the solution and perpetuated that as the mechanism by which we would ensure fairness. The problem is that my concentration of testosterone today is only a tiny part of the story.
I’ve been exposed to testosterone my whole life. My twin sister has not. There are many differences between us, but in terms of sports, the main biological difference is not that my testosterone is higher today; it’s that my testosterone has been higher my whole life. It’s the work done by that hormone over many years that makes a difference.
The key issue is, has this body, this physiology, been exposed to and benefited in the sports context, from male hormones – yes or no?
If your answer is yes, then that body belongs in male sports. With gender identity, we want to accommodate as far as possible, but we can’t take away that difference. That’s where we create this collision of rights between trans women and women.
Ultimately, your point is that we can’t have both fairness and inclusion.
When we sat down to do the World Rugby trans guidance, we had an epiphany: It doesn’t matter which way we go; we’re going to face hostility.
Once you accept that there are two parties that are affected and one of them will always be unhappy, then you start to see that fairness and inclusion can’t be balanced.
What about Joanna Harper’s proposal to make rules case by case and sport by sport?
First, it could be tricky legally because you’re effectively discriminating against some people within a subset of a subset. You’re going to end up saying to some trans women: “You can play because you don’t pose a safety or fairness issue.” But to another: “You can’t because you’re too strong.”
Then the problem is, how do you do that screening? It’s not like you can measure half a dozen variables and then have an algorithm spit out a performance level that tells you that this trans woman can compete here safely and fairly. It’s a theoretical solution that is practically impossible.
At a conference in Boston recently, Joanna said that when there are no medals, prize money, scholarships, or record times, we should allow inclusion. But just because a woman isn’t winning medals or going to the Olympics doesn’t mean there’s not considerable value for her if she were to make her school team, for instance.
There are only 11 places on the soccer field, eight lanes in a swimming pool. The moment you allow someone in, you potentially exclude someone else. And that happens everywhere, not only at the elite level.
Would you ever make a distinction between elite and subelite?
One of the beauties of sports is that it’s a meritocracy; it functions on a pathway system. I don’t think the level matters if you can track that this person’s presence denied a place on the team or a place at the competition to someone else.
With Lia Thomas, it’s not only denying the silver medalist gold or fourth place a bronze; it’s also the fact that there are only so many places at that meet. For some, that was their ambition and they weren’t able to realize it.
Now, a lot of sports are played outside that pathway. Say your local tennis club has a social league. There is little there to stand in the way of inclusion. Although I’m mindful that there may be a women’s league where it does matter to them.
We can try to accommodate trans women when the stakes are not high, provided that two requirements are met: One is that there’s no disruption to the selection/meritocracy pathway; and the second key point is that women must be okay with that inclusion, particularly if there are safety considerations, but even if it’s just a fairness consideration.
That’s where it gets tricky, because there are bigoted people in the world. Unfortunately, sometimes it’s difficult to tell whether people are using scientific arguments to prop up bigotry or whether they are genuine.
Joanna Harper has said that if you support inclusion, you have to be okay with trans women winning.
Winning the summer tennis league is not winning in the same sense as winning at the NCAA.
But the moment winning means selection and performance pathways, then I think we have to draw a line. The moment participation disrupts the natural order in sports, then it’s a problem.
In World Rugby, we proposed open competitions lower in contact to deal with the safety concerns. That was rejected by the trans community because they felt it was othering – that we were trying to squeeze them off to the side.
If you offered me one of two choices: no participation, or inclusion and they have to be able to win, I’d go for the former.
How did you get involved in this topic?
I got involved because I testified in the Caster Semenya case at the Court of Arbitration for Sport.
That is not a transgender issue; it’s a difference of sex development issue. What it has in common is the question of what to do with male-bodied biological advantage in sports.
When World Rugby joined the Olympic Games, we followed the IOC transgender policy. In 2019, it became apparent from the latest research that male advantage isn’t removed by testosterone suppression. We decided to delete the previous policy and make a new one.
The latest IOC policy is kind of no policy; it leaves it up to the governing bodies for each sport.
The one element of progress in what the IOC released, and it really is the only one, is that they’ve recognized that sports have to manage three imperatives: fairness, inclusion, and safety.
The 2015 IOC document says something like “sports should strive to be as inclusive as possible, but the overriding objective remains to guarantee a fair competition.” Basically, fair competition was nonnegotiable and must be guaranteed.
Of course, that policy allowed for testosterone suppression, and you’d have a difficult time convincing a physiologist that lowering testosterone guarantees fair competition.
Where there is merit in the current policy is that it’s clear that sports like rugby, boxing, taekwondo, and judo have a different equation with respect to safety, fairness, and inclusion than sports like equestrian, shooting, and archery. I think that’s wise to acknowledge.
However, the IOC policy doesn’t do anything to lead. In fact, what they said was extraordinary: There should be no presumption of advantage. If there’s no presumption of advantage for male-bodied athletes, then why do they persist with two categories? If there’s no presumption of advantage for trans women, are they saying that gender identity removes the advantage? We know that’s not true. We know that at the very least, you should presume that there is some advantage. How you manage it is up to you, but you can’t say that it’s not there.
This is a hostile debate. Have you ever thought: Maybe I’ll just shut up and stick to other sports topics?
Big time. The Lia Thomas case brought out a lot of vitriol. From about 2017, the situation we had with Ms. Thomas was predictable. The problem is that 95% of the world didn’t know this was happening and were taken by surprise.
The number of people who have opinions has exploded. A lot wade in without much thought. I’ve seen people question Lia Thomas’s motives. Presumably, Lia Thomas is trans, identifies as a woman, and therefore thinks she belongs in women’s sports. But I’ve seen people saying she only wants to swim in women’s sports because she knows she’ll win. And that’s not the worst of it. I’ve seen people saying Lia Thomas is only identifying as a woman so she can get into women’s changing rooms.
I don’t see how that helps the conversation. It just polarizes to the point that neither side is listening to the other. Before it was the trans community that wasn’t interested in talking about the idea of advantage, fairness, and safety. Their position is that trans women are women; how do you even have a discussion when they’ve got that dogma as their foundation?
Now, unfortunately, on the other side, we’re seeing unnecessary offensive tactics. For example, I’ve referred to Lia Thomas as “she.” I’ll have people shouting at me for using “she.” You’ve got to pick your battles, and that’s not the one you want to be fighting, in my opinion.
A version of this article first appeared on Medscape.com.
When Lia Thomas won the women’s 500-yard freestyle at the 2022 NCAA Division 1 swimming championships, the issue of trans women’s participation in female sports ignited national headlines.
which prohibit trans women’s participation.
This interview has been edited for length and clarity.
Let’s start with the proinclusion argument that there are always advantages in sports.
That’s true. The whole point of sports is to recognize people who have advantages and reward them for it. By the time this argument comes out, people have already accepted that males have advantages, right?
Some do, some don’t.
If someone uses this argument to say that we should allow trans women, basically biological males, to compete in women’s sports, they’ve implicitly accepted that there are advantages. Otherwise, what advantage are you talking about?
They would say it’s like the advantage Michael Phelps has because of his wingspan.
To answer that, you have to start by asking why women’s sports exist.
Women’s sports exist because we recognize that male physiology has biological differences that create performance advantages. Women’s sports exist to ensure that male advantages are excluded. If you allow male advantage in, you’re allowing something to cross into a category that specifically tries to exclude it. That makes the advantage possessed by trans women conceptually and substantively different from an advantage that’s possessed by Michael Phelps because his advantage doesn’t cross a category boundary line.
If someone wants to allow natural advantages to be celebrated in sports, they’re arguing against the existence of any categories, because every single category in sports is trying to filter out certain advantages.
Weight categories in boxing exist to get rid of the advantage of being stronger, taller, with greater reach. Paralympic categories filter out the natural advantage that someone has if, for example, they are only mildly affected by cerebral palsy, compared with more severely affected.
If someone wants to allow natural advantages, they’re making an argument for all advantages to be eliminated from regulation, and we would end up with sports dominated by males between the ages of 20 and 28.
There are some people suggesting open categories by height and weight.
The problem is that for any height, males will be stronger, faster, more powerful than females. For any mass, and we know this because weightlifting has categories by mass, males lift about 30% heavier than females. They’ll be about 10%-15% faster at the same height and weight.
There’d be one or two sports where you might have some women, like gymnastics. Otherwise you would have to create categories that are so small – say, under 100 pounds. But in every other category, most sports would be completely dominated by males.
It’s not a viable solution for me unless we as a society are satisfied with filtering out women.
Another argument is that if trans women have an advantage, then they would be dominating.
That one misunderstands how you assess advantage. For a trans woman to win, she still has to be good enough at the base level without the advantage, in order to parlay that advantage into winning the women’s events.
If I was in the Tour de France and you gave me a bicycle with a 100-watt motor, I wouldn’t win the Tour de France. I’d do better than I would have done without it, but I wouldn’t win. Does my failure to win prove that motors don’t give an advantage? Of course not. My failure says more about my base level of performance than it does about the motor.
In terms of trans athletes, the retention of biological attributes creates the retention of performance advantages, which means that the person’s ranking relative to their peers’ will go up when they compare themselves to women rather than men. Someone who’s ranked 500 might improve to the 250s, but you still won’t see them on a podium.
It’s the change in performance that matters, not the final outcome.
Wasn’t Lia Thomas ranked in the 500s in the men’s division?
There’s some dispute as to whether it was 460 or 550 in the 200- and 65th in the 500-yard freestyle. But the concept is the same and we can use that case because we know the percentage performance change.
As Will Thomas, the performance was 4:18 in the 500-yard freestyle. As Lia Thomas, it’s 4:33. Ms. Thomas has slowed by 5.8% as a result of testosterone suppression. That’s fairly typical; most studies so far suggest performance impairments in that range.
The thing is that the male-female gap in swimming times is 10%-12% on average. That means that Ms. Thomas has retained about half the male advantage.
In strength events, for instance, weightlifting, where the gap is 30% or more, if you lost 10%, you’d still retain a 20% advantage and you’d jump more ranking places.
The retention of about half the male advantage is enough for No. 1 in the NCAA, but it’s not enough to move Ms. Thomas to No. 1 in the world.
The record set by Katie Ledecky in the 500 freestyle is 4:24. Thomas swam 4:18 as a man so could only afford to lose about 1% to be the record holder in women’s swimming.
When Ms. Thomas was beaten by cisgender women in other events, your point is that’s just because her baseline (pretransition) time wasn’t good enough.
Exactly. Are your performances in men’s sports close enough to the best woman such that you can turn that retained advantage into dominance, winning in women’s sports?
If the answer to that is yes, then you get Thomas in the 500. If the answer to that is not quite, then you get Thomas in the other distances.
On your podcast, you expressed frustration at having to keep debunking these arguments. Why do you think they persist?
There are a few things in play. There are nuances around the idea of advantage that people from outside sports don’t always appreciate.
But then the second thing comes into play and that’s the fact that this is an emotive issue. If you come to this debate wanting trans inclusion, then you reject the idea that it’s unfair. You will dismiss everything I’ve just said.
There’s a third thing. When people invoke the Phelps wingspan argument, they haven’t thought through the implications. If you could sit them down and say: “Okay. If you want to get rid of regulating natural advantages, then we would get rid of male and female categories,” what do you think would happen then?
They may still support inclusion because that’s their world view, but at least they’re honest now and understand the implications. But most people don’t go through that process.
I get that men are faster but I was shocked at how many are faster than elite women – for example, Allyson Felix.
There’s an amazing visual representation of that.
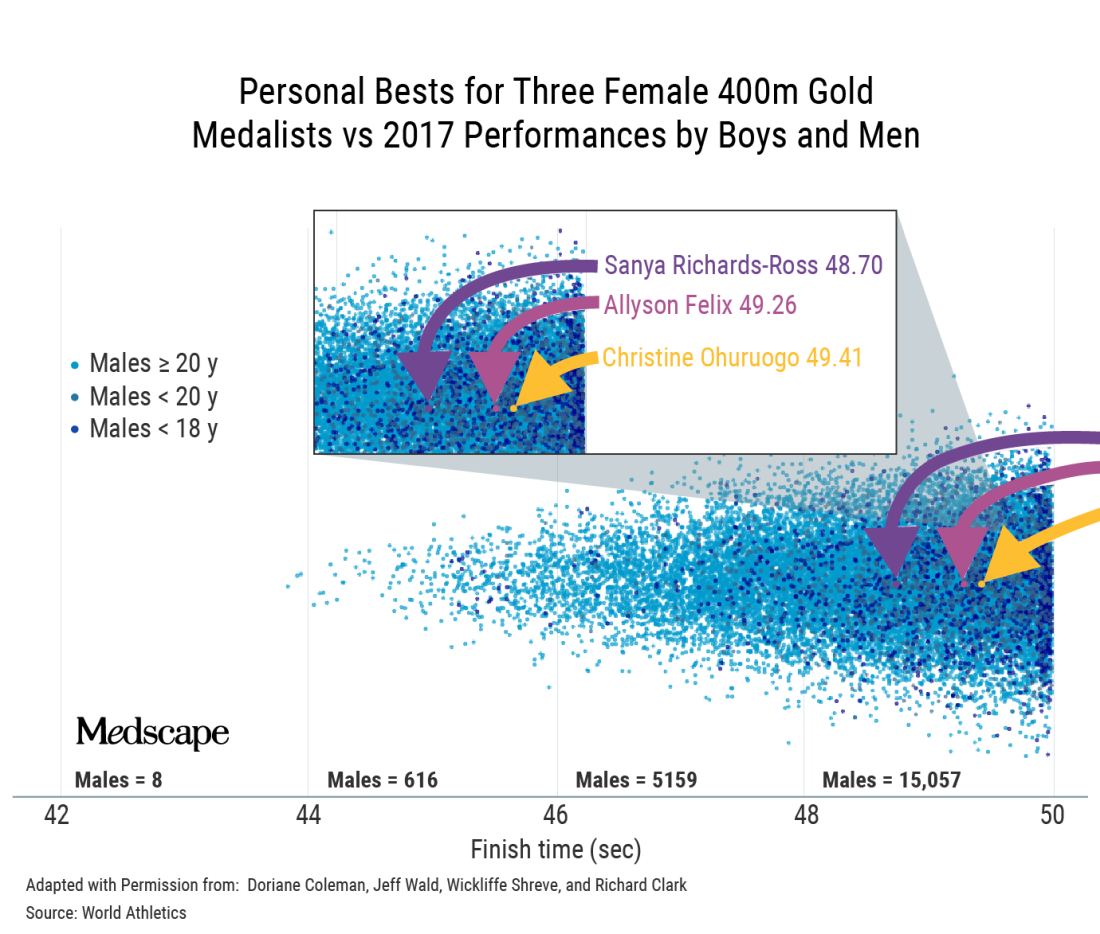
That’s a classic example where, if you’re immersed in sports, it becomes intuitive. If you’re not, you do a double-take and think, is that right? Position determines perspective.
Do you think some of it is because we’re constantly told that girls and women can do anything?
It’s a paradox that is difficult for people to get their minds around because in most walks of life, we can say that women can do anything. Of course, it’s arguably more difficult for women to become CEOs of Fortune 500 companies. This is a work in progress.
But sports are different. In sports, it’s not possible to directly compare male and female, and then tell girls they can be the best at whatever in the whole human race. That’s the uniqueness of sports and the reason categories exist in the first place. The biology does matter.
Speaking of biology, you’ve said that the focus on testosterone levels is a bit of a red herring.
Yes. The authorities were looking for a solution.
They grabbed onto the idea that lowering testosterone was the solution and perpetuated that as the mechanism by which we would ensure fairness. The problem is that my concentration of testosterone today is only a tiny part of the story.
I’ve been exposed to testosterone my whole life. My twin sister has not. There are many differences between us, but in terms of sports, the main biological difference is not that my testosterone is higher today; it’s that my testosterone has been higher my whole life. It’s the work done by that hormone over many years that makes a difference.
The key issue is, has this body, this physiology, been exposed to and benefited in the sports context, from male hormones – yes or no?
If your answer is yes, then that body belongs in male sports. With gender identity, we want to accommodate as far as possible, but we can’t take away that difference. That’s where we create this collision of rights between trans women and women.
Ultimately, your point is that we can’t have both fairness and inclusion.
When we sat down to do the World Rugby trans guidance, we had an epiphany: It doesn’t matter which way we go; we’re going to face hostility.
Once you accept that there are two parties that are affected and one of them will always be unhappy, then you start to see that fairness and inclusion can’t be balanced.
What about Joanna Harper’s proposal to make rules case by case and sport by sport?
First, it could be tricky legally because you’re effectively discriminating against some people within a subset of a subset. You’re going to end up saying to some trans women: “You can play because you don’t pose a safety or fairness issue.” But to another: “You can’t because you’re too strong.”
Then the problem is, how do you do that screening? It’s not like you can measure half a dozen variables and then have an algorithm spit out a performance level that tells you that this trans woman can compete here safely and fairly. It’s a theoretical solution that is practically impossible.
At a conference in Boston recently, Joanna said that when there are no medals, prize money, scholarships, or record times, we should allow inclusion. But just because a woman isn’t winning medals or going to the Olympics doesn’t mean there’s not considerable value for her if she were to make her school team, for instance.
There are only 11 places on the soccer field, eight lanes in a swimming pool. The moment you allow someone in, you potentially exclude someone else. And that happens everywhere, not only at the elite level.
Would you ever make a distinction between elite and subelite?
One of the beauties of sports is that it’s a meritocracy; it functions on a pathway system. I don’t think the level matters if you can track that this person’s presence denied a place on the team or a place at the competition to someone else.
With Lia Thomas, it’s not only denying the silver medalist gold or fourth place a bronze; it’s also the fact that there are only so many places at that meet. For some, that was their ambition and they weren’t able to realize it.
Now, a lot of sports are played outside that pathway. Say your local tennis club has a social league. There is little there to stand in the way of inclusion. Although I’m mindful that there may be a women’s league where it does matter to them.
We can try to accommodate trans women when the stakes are not high, provided that two requirements are met: One is that there’s no disruption to the selection/meritocracy pathway; and the second key point is that women must be okay with that inclusion, particularly if there are safety considerations, but even if it’s just a fairness consideration.
That’s where it gets tricky, because there are bigoted people in the world. Unfortunately, sometimes it’s difficult to tell whether people are using scientific arguments to prop up bigotry or whether they are genuine.
Joanna Harper has said that if you support inclusion, you have to be okay with trans women winning.
Winning the summer tennis league is not winning in the same sense as winning at the NCAA.
But the moment winning means selection and performance pathways, then I think we have to draw a line. The moment participation disrupts the natural order in sports, then it’s a problem.
In World Rugby, we proposed open competitions lower in contact to deal with the safety concerns. That was rejected by the trans community because they felt it was othering – that we were trying to squeeze them off to the side.
If you offered me one of two choices: no participation, or inclusion and they have to be able to win, I’d go for the former.
How did you get involved in this topic?
I got involved because I testified in the Caster Semenya case at the Court of Arbitration for Sport.
That is not a transgender issue; it’s a difference of sex development issue. What it has in common is the question of what to do with male-bodied biological advantage in sports.
When World Rugby joined the Olympic Games, we followed the IOC transgender policy. In 2019, it became apparent from the latest research that male advantage isn’t removed by testosterone suppression. We decided to delete the previous policy and make a new one.
The latest IOC policy is kind of no policy; it leaves it up to the governing bodies for each sport.
The one element of progress in what the IOC released, and it really is the only one, is that they’ve recognized that sports have to manage three imperatives: fairness, inclusion, and safety.
The 2015 IOC document says something like “sports should strive to be as inclusive as possible, but the overriding objective remains to guarantee a fair competition.” Basically, fair competition was nonnegotiable and must be guaranteed.
Of course, that policy allowed for testosterone suppression, and you’d have a difficult time convincing a physiologist that lowering testosterone guarantees fair competition.
Where there is merit in the current policy is that it’s clear that sports like rugby, boxing, taekwondo, and judo have a different equation with respect to safety, fairness, and inclusion than sports like equestrian, shooting, and archery. I think that’s wise to acknowledge.
However, the IOC policy doesn’t do anything to lead. In fact, what they said was extraordinary: There should be no presumption of advantage. If there’s no presumption of advantage for male-bodied athletes, then why do they persist with two categories? If there’s no presumption of advantage for trans women, are they saying that gender identity removes the advantage? We know that’s not true. We know that at the very least, you should presume that there is some advantage. How you manage it is up to you, but you can’t say that it’s not there.
This is a hostile debate. Have you ever thought: Maybe I’ll just shut up and stick to other sports topics?
Big time. The Lia Thomas case brought out a lot of vitriol. From about 2017, the situation we had with Ms. Thomas was predictable. The problem is that 95% of the world didn’t know this was happening and were taken by surprise.
The number of people who have opinions has exploded. A lot wade in without much thought. I’ve seen people question Lia Thomas’s motives. Presumably, Lia Thomas is trans, identifies as a woman, and therefore thinks she belongs in women’s sports. But I’ve seen people saying she only wants to swim in women’s sports because she knows she’ll win. And that’s not the worst of it. I’ve seen people saying Lia Thomas is only identifying as a woman so she can get into women’s changing rooms.
I don’t see how that helps the conversation. It just polarizes to the point that neither side is listening to the other. Before it was the trans community that wasn’t interested in talking about the idea of advantage, fairness, and safety. Their position is that trans women are women; how do you even have a discussion when they’ve got that dogma as their foundation?
Now, unfortunately, on the other side, we’re seeing unnecessary offensive tactics. For example, I’ve referred to Lia Thomas as “she.” I’ll have people shouting at me for using “she.” You’ve got to pick your battles, and that’s not the one you want to be fighting, in my opinion.
A version of this article first appeared on Medscape.com.
Age, skin cancer risks for ICI-induced bullous pemphigoid identified
that may result in treatment interruption or cessation.
Investigators in Boston report that among patients receiving ICIs, being aged 70 years or older and having skin cancer are both significant risk factors for bullous pemphigoid. On the plus side, ICI-induced bullous pemphigoid also appears to be a marker for improved tumor responses to therapy.
In a nested case-control study of 5,636 patients with cancer who received either a programmed death 1 inhibitor such as pembrolizumab (Keytruda) or nivolumab (Opdivo) or a cytotoxic T-lymphocyte–associated protein 4 inhibitor such as ipilimumab (Yervoy), 35 patients (0.6%) developed bullous pemphigoid. The study by Nicole R. LeBoeuf, MD, MPH, from Brigham and Women’s Hospital in Boston and colleagues was published online in JAMA Dermatology.
“What is interesting is that 0.6 is a small number, but we’re seeing bullous pemphigoid at considerably higher frequency than is expected in the general population,” Dr. LeBoeuf said in an interview.
And although bullous pemphigoid has the potential to disrupt ICI therapy, it also appears to be a marker for a favorable tumor response, the investigators found.
Their findings suggest that management of bullous pemphigoid for patients receiving ICIs should focus on early identification and management with therapies directed at the specific toxicity, Dr. LeBoeuf said.
“When you make a specific diagnosis like bullous pemphigoid, then you can treat that specific disease with very targeted therapies, such as omalizumab or dupilumab or rituximab – things that are not globally immune suppressing like steroid or other T-cell–depleting agents. Studies have shown that depleting B cells with anti-CD20 agents is not detrimental to immune checkpoint inhibitor therapy,” she said.
Dermatologic AEs common
About 40% of patients with cancer treated with ICIs experience immune-related dermatologic adverse events (AEs) that can range from mild rashes and hair and nail changes to uncommon but life-threatening complications, such as Stevens-Johnson syndrome, a form of toxic epidermal necrolysis, according to members of a European Academy of Dermatology and Venereology task force.
“The desirable, immune-mediated oncologic response is often achieved at the cost of immune-related adverse events (irAEs) that may potentially affect any organ system,” they wrote in a position statement on the management of ICI-derived dermatologic adverse events.
Dr. LeBoeuf and colleagues note that, while reported risk factors for idiopathic bullous pemphigoid include advanced age, type 2 diabetes, use of dipeptidyl peptidase-4 inhibitors, cerebrovascular disease, and neurocognitive disease, risk factors for bullous pemphigoid and other adverse dermatologic events associated with ICIs are less well known.
Study details
To identify risk factors for bullous pemphigoid in patients receiving ICI, the investigators performed a case-control study nested within a retrospective cohort study.
They evaluated records for all patients in the three Harvard-affiliated hospitals to identify patients with ICI-associated bullous pemphigoid from October 2014 through December 2020. Control persons were all patients in the Dana-Farber cancer registry who received ICIs during the study period.
The investigators chose age at ICI initiation (69 years and younger or 70 years and older), sex, ICI agents, and cancer type as potential risk factors.
They used propensity score matching based on age, cancer type, ICI agent, and number of ICI cycles to match two control persons with each case patient.
Of the 5,636 patients treated with ICIs during the study period, 35 (0.6%) developed bullous pemphigoid. The median age was 72.8 years, and 71.4% were men.
In a multivariate logistic regression model that included 2,955 patients with complete data in the cancer registry, factors significantly associated with developing bullous pemphigoid included age 70 years or older (odds ratio, 2.32; P = .01), having melanoma (OR, 3.21; P < .001), and having nonmelanoma skin cancer (OR, 8.32; P < .001).
In comparing the 35 case patients with their matched control patients, a complete or partial response at first restaging imaging was significantly associated with developing bullous pemphigoid (OR, 3.37; P = .01). In addition, there was a higher likelihood of tumor responses to ICIs among patients with bullous pemphigoid, compared with matched control patients (objective response rate, 82.9% vs. 61.4%; P = .03).
Prudent toxicity management
Ryan Sullivan, MD, who treats patients with skin cancer at Massachusetts General Hospital Cancer Center, Boston, but was not involved in the study, commented that the findings raise questions about the relationship between skin cancers and immune-related adverse events.
“It is compelling that bullous pemphigoid is a skin toxicity and is more common to happen in skin cancer patients,” he noted. “That’s a very interesting finding, and the reason that it’s interesting is that it’s harder to understand why a presumably antibody-mediated side effect would be more likely to have that cross-reactivity where the tumor started and where the toxicity happened,” he said in an interview.
He noted that the benefits of ICIs for patients with skin cancers far outweigh the risks of dermatologic adverse events such as bullous pemphigoid and that ICI-associated events require judicious management.
“This is true across the spectrum of toxicities: There are clear manifestations of toxicity that we should be more thoughtful about what’s driving them, more thoughtful about what it is, and more thoughtful about treating them, other than just pouring steroids into patients in industrial doses and hoping that everything’s going to be OK,” he said.
No funding source for the study was reported. Dr. LeBoeuf reported receiving grants from the National Institutes of Health National Cancer Institute during the conduct of the study and personal fees for serving as a consultant for several companies outside the study. Coauthor Arash Mostaghimi, MD, MPA, MPH, is associate editor of JAMA Dermatology but was not involved in study selection or evaluation for publication. Dr. Sullivan disclosed consulting for ICI makers Bristol-Myers Squibb and Merck.
A version of this article first appeared on Medscape.com.
that may result in treatment interruption or cessation.
Investigators in Boston report that among patients receiving ICIs, being aged 70 years or older and having skin cancer are both significant risk factors for bullous pemphigoid. On the plus side, ICI-induced bullous pemphigoid also appears to be a marker for improved tumor responses to therapy.
In a nested case-control study of 5,636 patients with cancer who received either a programmed death 1 inhibitor such as pembrolizumab (Keytruda) or nivolumab (Opdivo) or a cytotoxic T-lymphocyte–associated protein 4 inhibitor such as ipilimumab (Yervoy), 35 patients (0.6%) developed bullous pemphigoid. The study by Nicole R. LeBoeuf, MD, MPH, from Brigham and Women’s Hospital in Boston and colleagues was published online in JAMA Dermatology.
“What is interesting is that 0.6 is a small number, but we’re seeing bullous pemphigoid at considerably higher frequency than is expected in the general population,” Dr. LeBoeuf said in an interview.
And although bullous pemphigoid has the potential to disrupt ICI therapy, it also appears to be a marker for a favorable tumor response, the investigators found.
Their findings suggest that management of bullous pemphigoid for patients receiving ICIs should focus on early identification and management with therapies directed at the specific toxicity, Dr. LeBoeuf said.
“When you make a specific diagnosis like bullous pemphigoid, then you can treat that specific disease with very targeted therapies, such as omalizumab or dupilumab or rituximab – things that are not globally immune suppressing like steroid or other T-cell–depleting agents. Studies have shown that depleting B cells with anti-CD20 agents is not detrimental to immune checkpoint inhibitor therapy,” she said.
Dermatologic AEs common
About 40% of patients with cancer treated with ICIs experience immune-related dermatologic adverse events (AEs) that can range from mild rashes and hair and nail changes to uncommon but life-threatening complications, such as Stevens-Johnson syndrome, a form of toxic epidermal necrolysis, according to members of a European Academy of Dermatology and Venereology task force.
“The desirable, immune-mediated oncologic response is often achieved at the cost of immune-related adverse events (irAEs) that may potentially affect any organ system,” they wrote in a position statement on the management of ICI-derived dermatologic adverse events.
Dr. LeBoeuf and colleagues note that, while reported risk factors for idiopathic bullous pemphigoid include advanced age, type 2 diabetes, use of dipeptidyl peptidase-4 inhibitors, cerebrovascular disease, and neurocognitive disease, risk factors for bullous pemphigoid and other adverse dermatologic events associated with ICIs are less well known.
Study details
To identify risk factors for bullous pemphigoid in patients receiving ICI, the investigators performed a case-control study nested within a retrospective cohort study.
They evaluated records for all patients in the three Harvard-affiliated hospitals to identify patients with ICI-associated bullous pemphigoid from October 2014 through December 2020. Control persons were all patients in the Dana-Farber cancer registry who received ICIs during the study period.
The investigators chose age at ICI initiation (69 years and younger or 70 years and older), sex, ICI agents, and cancer type as potential risk factors.
They used propensity score matching based on age, cancer type, ICI agent, and number of ICI cycles to match two control persons with each case patient.
Of the 5,636 patients treated with ICIs during the study period, 35 (0.6%) developed bullous pemphigoid. The median age was 72.8 years, and 71.4% were men.
In a multivariate logistic regression model that included 2,955 patients with complete data in the cancer registry, factors significantly associated with developing bullous pemphigoid included age 70 years or older (odds ratio, 2.32; P = .01), having melanoma (OR, 3.21; P < .001), and having nonmelanoma skin cancer (OR, 8.32; P < .001).
In comparing the 35 case patients with their matched control patients, a complete or partial response at first restaging imaging was significantly associated with developing bullous pemphigoid (OR, 3.37; P = .01). In addition, there was a higher likelihood of tumor responses to ICIs among patients with bullous pemphigoid, compared with matched control patients (objective response rate, 82.9% vs. 61.4%; P = .03).
Prudent toxicity management
Ryan Sullivan, MD, who treats patients with skin cancer at Massachusetts General Hospital Cancer Center, Boston, but was not involved in the study, commented that the findings raise questions about the relationship between skin cancers and immune-related adverse events.
“It is compelling that bullous pemphigoid is a skin toxicity and is more common to happen in skin cancer patients,” he noted. “That’s a very interesting finding, and the reason that it’s interesting is that it’s harder to understand why a presumably antibody-mediated side effect would be more likely to have that cross-reactivity where the tumor started and where the toxicity happened,” he said in an interview.
He noted that the benefits of ICIs for patients with skin cancers far outweigh the risks of dermatologic adverse events such as bullous pemphigoid and that ICI-associated events require judicious management.
“This is true across the spectrum of toxicities: There are clear manifestations of toxicity that we should be more thoughtful about what’s driving them, more thoughtful about what it is, and more thoughtful about treating them, other than just pouring steroids into patients in industrial doses and hoping that everything’s going to be OK,” he said.
No funding source for the study was reported. Dr. LeBoeuf reported receiving grants from the National Institutes of Health National Cancer Institute during the conduct of the study and personal fees for serving as a consultant for several companies outside the study. Coauthor Arash Mostaghimi, MD, MPA, MPH, is associate editor of JAMA Dermatology but was not involved in study selection or evaluation for publication. Dr. Sullivan disclosed consulting for ICI makers Bristol-Myers Squibb and Merck.
A version of this article first appeared on Medscape.com.
that may result in treatment interruption or cessation.
Investigators in Boston report that among patients receiving ICIs, being aged 70 years or older and having skin cancer are both significant risk factors for bullous pemphigoid. On the plus side, ICI-induced bullous pemphigoid also appears to be a marker for improved tumor responses to therapy.
In a nested case-control study of 5,636 patients with cancer who received either a programmed death 1 inhibitor such as pembrolizumab (Keytruda) or nivolumab (Opdivo) or a cytotoxic T-lymphocyte–associated protein 4 inhibitor such as ipilimumab (Yervoy), 35 patients (0.6%) developed bullous pemphigoid. The study by Nicole R. LeBoeuf, MD, MPH, from Brigham and Women’s Hospital in Boston and colleagues was published online in JAMA Dermatology.
“What is interesting is that 0.6 is a small number, but we’re seeing bullous pemphigoid at considerably higher frequency than is expected in the general population,” Dr. LeBoeuf said in an interview.
And although bullous pemphigoid has the potential to disrupt ICI therapy, it also appears to be a marker for a favorable tumor response, the investigators found.
Their findings suggest that management of bullous pemphigoid for patients receiving ICIs should focus on early identification and management with therapies directed at the specific toxicity, Dr. LeBoeuf said.
“When you make a specific diagnosis like bullous pemphigoid, then you can treat that specific disease with very targeted therapies, such as omalizumab or dupilumab or rituximab – things that are not globally immune suppressing like steroid or other T-cell–depleting agents. Studies have shown that depleting B cells with anti-CD20 agents is not detrimental to immune checkpoint inhibitor therapy,” she said.
Dermatologic AEs common
About 40% of patients with cancer treated with ICIs experience immune-related dermatologic adverse events (AEs) that can range from mild rashes and hair and nail changes to uncommon but life-threatening complications, such as Stevens-Johnson syndrome, a form of toxic epidermal necrolysis, according to members of a European Academy of Dermatology and Venereology task force.
“The desirable, immune-mediated oncologic response is often achieved at the cost of immune-related adverse events (irAEs) that may potentially affect any organ system,” they wrote in a position statement on the management of ICI-derived dermatologic adverse events.
Dr. LeBoeuf and colleagues note that, while reported risk factors for idiopathic bullous pemphigoid include advanced age, type 2 diabetes, use of dipeptidyl peptidase-4 inhibitors, cerebrovascular disease, and neurocognitive disease, risk factors for bullous pemphigoid and other adverse dermatologic events associated with ICIs are less well known.
Study details
To identify risk factors for bullous pemphigoid in patients receiving ICI, the investigators performed a case-control study nested within a retrospective cohort study.
They evaluated records for all patients in the three Harvard-affiliated hospitals to identify patients with ICI-associated bullous pemphigoid from October 2014 through December 2020. Control persons were all patients in the Dana-Farber cancer registry who received ICIs during the study period.
The investigators chose age at ICI initiation (69 years and younger or 70 years and older), sex, ICI agents, and cancer type as potential risk factors.
They used propensity score matching based on age, cancer type, ICI agent, and number of ICI cycles to match two control persons with each case patient.
Of the 5,636 patients treated with ICIs during the study period, 35 (0.6%) developed bullous pemphigoid. The median age was 72.8 years, and 71.4% were men.
In a multivariate logistic regression model that included 2,955 patients with complete data in the cancer registry, factors significantly associated with developing bullous pemphigoid included age 70 years or older (odds ratio, 2.32; P = .01), having melanoma (OR, 3.21; P < .001), and having nonmelanoma skin cancer (OR, 8.32; P < .001).
In comparing the 35 case patients with their matched control patients, a complete or partial response at first restaging imaging was significantly associated with developing bullous pemphigoid (OR, 3.37; P = .01). In addition, there was a higher likelihood of tumor responses to ICIs among patients with bullous pemphigoid, compared with matched control patients (objective response rate, 82.9% vs. 61.4%; P = .03).
Prudent toxicity management
Ryan Sullivan, MD, who treats patients with skin cancer at Massachusetts General Hospital Cancer Center, Boston, but was not involved in the study, commented that the findings raise questions about the relationship between skin cancers and immune-related adverse events.
“It is compelling that bullous pemphigoid is a skin toxicity and is more common to happen in skin cancer patients,” he noted. “That’s a very interesting finding, and the reason that it’s interesting is that it’s harder to understand why a presumably antibody-mediated side effect would be more likely to have that cross-reactivity where the tumor started and where the toxicity happened,” he said in an interview.
He noted that the benefits of ICIs for patients with skin cancers far outweigh the risks of dermatologic adverse events such as bullous pemphigoid and that ICI-associated events require judicious management.
“This is true across the spectrum of toxicities: There are clear manifestations of toxicity that we should be more thoughtful about what’s driving them, more thoughtful about what it is, and more thoughtful about treating them, other than just pouring steroids into patients in industrial doses and hoping that everything’s going to be OK,” he said.
No funding source for the study was reported. Dr. LeBoeuf reported receiving grants from the National Institutes of Health National Cancer Institute during the conduct of the study and personal fees for serving as a consultant for several companies outside the study. Coauthor Arash Mostaghimi, MD, MPA, MPH, is associate editor of JAMA Dermatology but was not involved in study selection or evaluation for publication. Dr. Sullivan disclosed consulting for ICI makers Bristol-Myers Squibb and Merck.
A version of this article first appeared on Medscape.com.
FROM JAMA DERMATOLOGY