User login
Are Breast Cancer Patients Satisfied With Their Care?
Japan has a universal health care system with low copays and short wait times for appointments, including those with specialists. Yet patient satisfaction scores are low compared with those of other countries. Researchers from Juntendo Urayasu Hospital, a university hospital in a Tokyo suburb, conducted a study of 214 patients with breast cancer to find out which aspects of radiation oncology care might affect patient satisfaction. The survey included questions about overall treatment, time from diagnosis to treatment start, wait times in the hospital, and length of consultations.
In general, levels of satisfaction were high. However, wait time was significantly negatively associated with both overall satisfaction and satisfaction with the radiation oncologist. Wait time was just under an hour for an average 11-minute consultation. Although this was longer than the “notorious” Japanese situation of a “3 hours wait and 3 minutes consultation,” the researchers say, “We expect that an international audience will appreciate that even 11 minutes is an exceptionally short duration for a consultation visit with a specialist in radiation oncology.”
They note, though, a reasonable caveat. Anyone can walk into their hospital and, for an additional fee, see a specialist on the day they want, which can lead to extended wait times from sheer congestion. Their hospital’s chief breast cancer surgeon sees 60 to 70 patients a day; the radiation oncologist treats 500 to 600 patients a year without resident or trainee support. This situation is typical of Japanese university hospitals, the researchers add.
Related: Breast Cancer Treatment Among Rural and Urban Women at the Veterans Health Administration
Importantly, for Japanese patients, the researchers also included questions to measure patients’ opinions about sharing how they felt with their physicians. The level of sharing correlated with satisfaction, but the researchers point out that in Japan sharing feelings remains “challenging.” Their findings suggest, they say, that if this were improved, patients’ satisfaction might increase.
Japan has a universal health care system with low copays and short wait times for appointments, including those with specialists. Yet patient satisfaction scores are low compared with those of other countries. Researchers from Juntendo Urayasu Hospital, a university hospital in a Tokyo suburb, conducted a study of 214 patients with breast cancer to find out which aspects of radiation oncology care might affect patient satisfaction. The survey included questions about overall treatment, time from diagnosis to treatment start, wait times in the hospital, and length of consultations.
In general, levels of satisfaction were high. However, wait time was significantly negatively associated with both overall satisfaction and satisfaction with the radiation oncologist. Wait time was just under an hour for an average 11-minute consultation. Although this was longer than the “notorious” Japanese situation of a “3 hours wait and 3 minutes consultation,” the researchers say, “We expect that an international audience will appreciate that even 11 minutes is an exceptionally short duration for a consultation visit with a specialist in radiation oncology.”
They note, though, a reasonable caveat. Anyone can walk into their hospital and, for an additional fee, see a specialist on the day they want, which can lead to extended wait times from sheer congestion. Their hospital’s chief breast cancer surgeon sees 60 to 70 patients a day; the radiation oncologist treats 500 to 600 patients a year without resident or trainee support. This situation is typical of Japanese university hospitals, the researchers add.
Related: Breast Cancer Treatment Among Rural and Urban Women at the Veterans Health Administration
Importantly, for Japanese patients, the researchers also included questions to measure patients’ opinions about sharing how they felt with their physicians. The level of sharing correlated with satisfaction, but the researchers point out that in Japan sharing feelings remains “challenging.” Their findings suggest, they say, that if this were improved, patients’ satisfaction might increase.
Japan has a universal health care system with low copays and short wait times for appointments, including those with specialists. Yet patient satisfaction scores are low compared with those of other countries. Researchers from Juntendo Urayasu Hospital, a university hospital in a Tokyo suburb, conducted a study of 214 patients with breast cancer to find out which aspects of radiation oncology care might affect patient satisfaction. The survey included questions about overall treatment, time from diagnosis to treatment start, wait times in the hospital, and length of consultations.
In general, levels of satisfaction were high. However, wait time was significantly negatively associated with both overall satisfaction and satisfaction with the radiation oncologist. Wait time was just under an hour for an average 11-minute consultation. Although this was longer than the “notorious” Japanese situation of a “3 hours wait and 3 minutes consultation,” the researchers say, “We expect that an international audience will appreciate that even 11 minutes is an exceptionally short duration for a consultation visit with a specialist in radiation oncology.”
They note, though, a reasonable caveat. Anyone can walk into their hospital and, for an additional fee, see a specialist on the day they want, which can lead to extended wait times from sheer congestion. Their hospital’s chief breast cancer surgeon sees 60 to 70 patients a day; the radiation oncologist treats 500 to 600 patients a year without resident or trainee support. This situation is typical of Japanese university hospitals, the researchers add.
Related: Breast Cancer Treatment Among Rural and Urban Women at the Veterans Health Administration
Importantly, for Japanese patients, the researchers also included questions to measure patients’ opinions about sharing how they felt with their physicians. The level of sharing correlated with satisfaction, but the researchers point out that in Japan sharing feelings remains “challenging.” Their findings suggest, they say, that if this were improved, patients’ satisfaction might increase.
The Long Legacy of Agent Orange
For some veterans, exposure to Agent Orange and its many health ramifications is an ongoing concern—even though they might have been exposed more than 50 years ago. Clinicians from Sinai Hospital of Baltimore in Maryland report on a patient who reminded them that a current illness could be related to that long-ago exposure.
Related: Bladder Cancer and Hyperthyroidism Linked to Agent Orange
The 69-year-old man came to their clinic with a painful, enlarging mass of the right lateral thigh, which ultrasound revealed as a myxofibrosarcoma. He underwent radical excision of the sarcoma with adjuvant radiotherapy. Histologic examination revealed an 8.3 cm, grade 3 pleomorphic liposarcoma. The patient asked, “Was it related to Agent Orange?” It may have been, the clinicians decided.
Agent Orange tends to accumulate in the liver and adipose tissue; it also affects lipid metabolism and may lead to hyperlipidemia. Although in the early days after the Vietnam War, many pathologies were labeled as “stress induced,” a number of illnesses have since been linked to Agent Orange, including B-cell leukemia, Hodgkin and non-Hodgkin lymphoma, prostate cancer, and, perhaps, multiple myeloma. But the authors say the toxin’s role in sarcomagenesis has been controversial in part because of conflicting case-control studies and because large-scale clinical trials are not feasible.
Related: Link Found Between Agent Orange Exposure and Multiple Myeloma
There has been no well-established precipitating factor for liposarcoma, the authors note. But they suggest that clinicians should have a high degree of suspicion for persistent and evolving soft tissue masses in patients with a previous military background, which should prompt the search for a possible toxin exposure.
Their patient experienced the enlarging soft tissue mass over the course of a year. A simple question: “Have you ever been in the military or had any previous wartime toxin exposure?” early on would have impelled the physicians to do a swifter workup, the authors say, particularly in a case with high risk of metastasis and poor prognosis. The patient will continue to be monitored “for years,” the authors say.
“While these days we have access to a vast amount of diagnostic tests and imaging,” the authors conclude, “one cannot underestimate the importance of understanding a patient’s past history.”
Source:
Khan K, Wozniak SE, Coleman J, Didolkar MS. BMJ Case Rep. 2016;2016. pii: bcr2016217438.
doi: 10.1136/bcr-2016-217438.
For some veterans, exposure to Agent Orange and its many health ramifications is an ongoing concern—even though they might have been exposed more than 50 years ago. Clinicians from Sinai Hospital of Baltimore in Maryland report on a patient who reminded them that a current illness could be related to that long-ago exposure.
Related: Bladder Cancer and Hyperthyroidism Linked to Agent Orange
The 69-year-old man came to their clinic with a painful, enlarging mass of the right lateral thigh, which ultrasound revealed as a myxofibrosarcoma. He underwent radical excision of the sarcoma with adjuvant radiotherapy. Histologic examination revealed an 8.3 cm, grade 3 pleomorphic liposarcoma. The patient asked, “Was it related to Agent Orange?” It may have been, the clinicians decided.
Agent Orange tends to accumulate in the liver and adipose tissue; it also affects lipid metabolism and may lead to hyperlipidemia. Although in the early days after the Vietnam War, many pathologies were labeled as “stress induced,” a number of illnesses have since been linked to Agent Orange, including B-cell leukemia, Hodgkin and non-Hodgkin lymphoma, prostate cancer, and, perhaps, multiple myeloma. But the authors say the toxin’s role in sarcomagenesis has been controversial in part because of conflicting case-control studies and because large-scale clinical trials are not feasible.
Related: Link Found Between Agent Orange Exposure and Multiple Myeloma
There has been no well-established precipitating factor for liposarcoma, the authors note. But they suggest that clinicians should have a high degree of suspicion for persistent and evolving soft tissue masses in patients with a previous military background, which should prompt the search for a possible toxin exposure.
Their patient experienced the enlarging soft tissue mass over the course of a year. A simple question: “Have you ever been in the military or had any previous wartime toxin exposure?” early on would have impelled the physicians to do a swifter workup, the authors say, particularly in a case with high risk of metastasis and poor prognosis. The patient will continue to be monitored “for years,” the authors say.
“While these days we have access to a vast amount of diagnostic tests and imaging,” the authors conclude, “one cannot underestimate the importance of understanding a patient’s past history.”
Source:
Khan K, Wozniak SE, Coleman J, Didolkar MS. BMJ Case Rep. 2016;2016. pii: bcr2016217438.
doi: 10.1136/bcr-2016-217438.
For some veterans, exposure to Agent Orange and its many health ramifications is an ongoing concern—even though they might have been exposed more than 50 years ago. Clinicians from Sinai Hospital of Baltimore in Maryland report on a patient who reminded them that a current illness could be related to that long-ago exposure.
Related: Bladder Cancer and Hyperthyroidism Linked to Agent Orange
The 69-year-old man came to their clinic with a painful, enlarging mass of the right lateral thigh, which ultrasound revealed as a myxofibrosarcoma. He underwent radical excision of the sarcoma with adjuvant radiotherapy. Histologic examination revealed an 8.3 cm, grade 3 pleomorphic liposarcoma. The patient asked, “Was it related to Agent Orange?” It may have been, the clinicians decided.
Agent Orange tends to accumulate in the liver and adipose tissue; it also affects lipid metabolism and may lead to hyperlipidemia. Although in the early days after the Vietnam War, many pathologies were labeled as “stress induced,” a number of illnesses have since been linked to Agent Orange, including B-cell leukemia, Hodgkin and non-Hodgkin lymphoma, prostate cancer, and, perhaps, multiple myeloma. But the authors say the toxin’s role in sarcomagenesis has been controversial in part because of conflicting case-control studies and because large-scale clinical trials are not feasible.
Related: Link Found Between Agent Orange Exposure and Multiple Myeloma
There has been no well-established precipitating factor for liposarcoma, the authors note. But they suggest that clinicians should have a high degree of suspicion for persistent and evolving soft tissue masses in patients with a previous military background, which should prompt the search for a possible toxin exposure.
Their patient experienced the enlarging soft tissue mass over the course of a year. A simple question: “Have you ever been in the military or had any previous wartime toxin exposure?” early on would have impelled the physicians to do a swifter workup, the authors say, particularly in a case with high risk of metastasis and poor prognosis. The patient will continue to be monitored “for years,” the authors say.
“While these days we have access to a vast amount of diagnostic tests and imaging,” the authors conclude, “one cannot underestimate the importance of understanding a patient’s past history.”
Source:
Khan K, Wozniak SE, Coleman J, Didolkar MS. BMJ Case Rep. 2016;2016. pii: bcr2016217438.
doi: 10.1136/bcr-2016-217438.
Patient Knowledge and Attitudes About Fecal Microbiota Therapy for Clostridium difficile Infection
Clostridium difficile (C difficile) infection (CDI) is a leading cause of infectious diarrhea among hospitalized patients and, increasingly, in ambulatory patients.1,2 The high prevalence of CDI and the high recurrence rates (15%-30%) led the CDC to categorize C difficile as an "urgent" threat (the highest category) in its 2013 Antimicrobial Resistance Threat Report.3-5 The Infectious Diseases Society of America guideline recommended treatment for CDI is vancomycin or metronidazole; more recent studies also support fidaxomicin use.4,6,7
Patients experiencing recurrent CDI are at risk for further recurrences, such that after the third CDI episode, the risk of subsequent recurrences exceeds 50%.8 This recurrence rate has stimulated research into other treatments, including fecal microbiota transplantation (FMT). A recent systematic review of FMT reports that 85% of patients have resolution of symptoms without recurrence after FMT, although this is based on data from case series and 2 small randomized clinical trials.9
A commonly cited barrier to FMT is patient acceptance. In response to this concern, a previous survey demonstrated that 81% of respondents would opt for FMT to treat a hypothetical case of recurrent CDI.10 However, the surveyed population did not have CDI, and the 48% response rate is concerning, since those with a favorable opinion of FMT might be more willing to complete a survey than would other patients. Accordingly, the authors systematically surveyed hospitalized veterans with active CDI to assess their knowledge, attitudes, and opinions about FMT as a treatment for CDI.
Methods
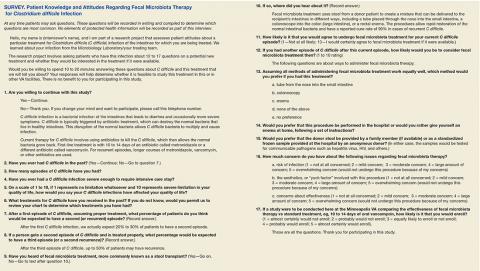
In-person patient interviews were conducted by one of the study authors at the Minneapolis VA Health Care System (MVAHCS), consisting of 13 to 18 questions. Questions addressed any prior CDI episodes and knowledge of the following: CDI, recurrence risk, and FMT; preferred route and location of FMT administration; concerns regarding FMT; likelihood of agreeing to undergo FMT (if available); and likelihood of enrollment in a hypothetical study comparing FMT to standard antibiotic treatment. The survey was developed internally and was not validated. Questions used the Likert-scale (Survey).
Patients with CDI were identified by monitoring for positive C difficile polymerase chain reaction (PCR) stool tests and then screened for inclusion by medical record review. Inclusion criteria were (1) MVAHCS hospitalization; and (2) written informed consent. Exclusion criteria were the inability to communicate or participate in an interview. Patient responses regarding their likelihood of agreeing to FMT for CDI treatment under different circumstances were compared using Wilcoxon rank sum test. These circumstances included FMT for their current episode of CDI, FMT for a subsequent episode, and FMT if recommended by their physician. Possible concerns regarding FMT also were solicited, including infection risk, effectiveness, and procedural aesthetics. The MVAHCS institutional review board approved the study.
Results
Stool PCR tests for CDI were monitored for 158 days from 2013 to 2014 (based on availability of study staff), yielding 106 positive results. Of those, 31 (29%) were from outpatients and not addressed further. Of the 75 positive CDI tests from 66 hospitalized patients (9 patients had duplicate tests), 18 of 66 (27%) were not able to provide consent and were excluded, leaving 48 eligible patients. Six (13%) were missed for logistic reasons (patient at a test or procedure, discharged before approached, etc), leaving 42 patients who were approached for participation. Among these, 34 (81%) consented to participate in the survey. Two subjects (6%) found the topic so unappealing that they terminated the interview.
The majority of enrolled subjects were men (32/34, 94%), with a mean age of 65.3 years (range, 31-89). Eleven subjects (32%) reported a prior CDI episode, with 10 reporting 1 such episode, and the other 2 episodes. Those with prior CDI reported the effect of CDI on their overall quality of life as 5.1 (1 = no limitation, 10 = severe limitation). Respondents were fairly accurate regarding the risk of recurrence after an initial episode of CDI, with the average expectedrecurrence rate estimated at 33%. In contrast, their estimation of the risk of recurrence after a second CDI episode was lower (28%), although the risk of recurrent episodes increases with each CDI recurrence.
Regarding FMT, 5 subjects indicated awareness of the procedure: 2 learning of it from a news source, 1 from family, 1 from a health care provider, and 1 was unsure of the source. After subjects received a description of FMT, their opinions regarding the procedure were elicited. When asked which route of delivery they would prefer if they were to undergo FMT, the 33 subjects who provided a response indicated a strong preference for either enema (15, 45%) or colonoscopy (10, 30%), compared with just 4 (12%) indicating no preference, 2 (6%) choosing nasogastric tube administration, and 2 (6%) indicating that they would not undergo FMT by any route (P < .001).
Regarding the location of FMT administration (hospital setting vs self-administered at home), 31 of 33 respondents (94%) indicated they would prefer FMT to occur in the hospital vs 2 (6%) preferring self-administration at home (P < .001). The preferred source of donor stool was more evenly distributed, with 14 of 32 respondents (44%) indicating a preference for an anonymous donor, 11 preferring a family member (34%), and 7 (21%) with no preference (P = .21).
Subjects were asked about concerns regarding FMT, and asked to rate each on a 5-point Likert scale (1 = not at all concerning; 5 = overwhelming concern). Concerns regarding risk of infection and effectiveness received an average score of 2.74 and 2.72, respectively, whereas concern regarding the aesthetics, or "yuck factor" was slightly lower (2.1: P = NS for all comparisons). Subjects also were asked to rate the likelihood of undergoing FMT, if it were available, for their current episode of CDI, a subsequent episode of CDI, or if their physician recommended undergoing FMT (10 point scale: 1 = not at all likely; 10 = certainly agree to FMT). The mean scores (SD) for agreeing to FMT for the current or a subsequent episode were 4.8 (SD 2.7) and 5.6 (SD 3.0); P = .12, but increased to 7.1 (SD 3.23) if FMT were recommended by their physician (P < .001 for FMT if physician recommended vs FMT for current episode; P = .001 for FMT if physician recommended vs FMT for a subsequent episode). Finally, subjects were asked about the likelihood of enrolling in a study comparing FMT to standard antimicrobial treatment, with answers ranging from 1 (almost certainly would not enroll) to 5 (almost certainly would enroll). Among the 32 respondents to this question, 17 (53%) answered either "probably would enroll" or "almost certainly would enroll," with a mean score of 3.2.
Discussion
Overall, VA patients with a current episode of CDI were not aware of FMT, with just 15% knowing about the procedure. However, after learning about FMT, patients expressed clear opinions regarding the route and setting of FMT administration, with enema or colonoscopy being the preferred routes, and a hospital the preferred setting. In contrast, subjects expressed ambivalence with regard to the source of donor stool, with no clear preference for stool from an anonymous donor vs from a family member.
When asked about concerns regarding FMT, none of the presented options (risk of infection, uncertain effectiveness, or procedural aesthetics) emerged as significantly more important than did others, although the oft-cited concern regarding FMT aesthetics engendered the lowest overall level of concern. In terms of FMT acceptance, 4 subjects (12%) were opposed to the procedure, indicating that they were not at all likely to agree to FMT for all scenarios (defined as a score of 1 or 2 on the 10-point Likert scale) or by terminating the survey because of the questions. However, 15 (44%) indicated that they would certainly agree to FMT (defined as a score of 9 or 10 on the 10-point Likert scale) if their physician recommended it. Physician recommendation for FMT resulted in the highest overall likelihood of agreeing to FMT, a finding in agreement with a previous survey of FMT for CDI.10 Most subjects indicated likely enrollment in a potential study comparing FMT with standard antimicrobial therapy.
Strengths/Limitations
Study strengths included surveying patients with current CDI, such that patients had personal experience with the disease in question. Use of in-person interviews also resulted in a robust response rate of 81% and allowed subjects to clarify any unclear questions with study personnel. Weaknesses included a relatively small sample size, underrepresentation of women, and lack of detail regarding respondent characteristics. Additionally, capsule delivery of FMT was not assessed since this method of delivery had not been published at the time of survey administration.
Conclusion
This survey of VA patients with CDI suggests that aesthetic concerns are not a critical deterrent for this population, and interest in FMT for the treatment of recurrent CDI exists. Physician recommendation to undergo FMT seems to be the most influential factor affecting the likelihood of agreeing to undergo FMT. These results support the feasibility of conducting clinical trials of FMT in the VA system.
1. Miller BA, Chen LF, Sexton DJ, Anderson DJ. Comparison of the burdens of hospital-onset, healthcare facility-associated Clostridium difficile Infection and of healthcare-associated infection due to methicillin-resistant Staphylococcus aureus in community hospitals. Infect Control Hosp Epidemiol. 2011;32(4):387-390.
2. Centers for Disease Control and Prevention. Severe Clostridium difficile-associated disease in populations previously at low risk--four states, 2005. MMWR Morb Mortal Wkly Rep. 2005;54(47):1201-1205.
3. Johnson S, Louie TJ, Gerding DN, et al; Polymer Alternative for CDI Treatment (PACT) investigators. Vancomycin, metronidazole, or tolevamer for Clostridium difficile infection: results from two multinational, randomized, controlled trials. Clin Infect Dis. 2014;59(3):345-354.
4. Louie TJ, Miller MA, Mullane KM, et al; OPT-80-003 Clinical Study Group. Fidaxomicin versus vancomycin for Clostridium difficile infection. N Engl J Med. 2011;364(5):422-431.
5. Centers for Disease Control and Prevention. Antibiotic resistance threats in the United States, 2013. http://www.cdc.gov/drugresistance/threat-report-2013. Updated July 17, 2014. Accessed November 16.2016.
6. Cohen SH, Gerding DN, Johnson S, et al; Society for Healthcare Epidemiology of America; Infectious Diseases Society of America. Clinical practice guidelines for Clostridium difficile infection in adults: 2010 update by the society for healthcare epidemiology of America (SHEA) and the Infectious Diseases Society of America (IDSA). Infect Control Hosp Epidemiol. 2010;31(5):431-455.
7. Cornely OA, Crook DW, Esposito R, et al; OPT-80-004 Clinical Study Group. Fidaxomicin versus vancomycin for infection with Clostridium difficile in Europe, Canada, and the USA: a double-blind, non-inferiority, randomised controlled trial. Lancet Infect Dis. 2012;12(4):281-289.
8. Johnson S. Recurrent Clostridium difficile infection: a review of risk factors, treatments, and outcomes. J Infect. 2009;58(6):403-410.
9. Drekonja DM, Reich J, Gezahegn S, et al. Fecal microbiota transplantation for Clostridium difficile infection--a systematic review. Ann Intern Med. 2015;162(9):630-638.
10. Zipursky JS, Sidorsky TI, Freedman CA, Sidorsky MN, Kirkland KB. Patient attitudes toward the use of fecal microbiota transplantation in the treatment of recurrent Clostridium difficile infection. Clin Infect Dis. 2012;55(12):1652-1658.
Clostridium difficile (C difficile) infection (CDI) is a leading cause of infectious diarrhea among hospitalized patients and, increasingly, in ambulatory patients.1,2 The high prevalence of CDI and the high recurrence rates (15%-30%) led the CDC to categorize C difficile as an "urgent" threat (the highest category) in its 2013 Antimicrobial Resistance Threat Report.3-5 The Infectious Diseases Society of America guideline recommended treatment for CDI is vancomycin or metronidazole; more recent studies also support fidaxomicin use.4,6,7
Patients experiencing recurrent CDI are at risk for further recurrences, such that after the third CDI episode, the risk of subsequent recurrences exceeds 50%.8 This recurrence rate has stimulated research into other treatments, including fecal microbiota transplantation (FMT). A recent systematic review of FMT reports that 85% of patients have resolution of symptoms without recurrence after FMT, although this is based on data from case series and 2 small randomized clinical trials.9
A commonly cited barrier to FMT is patient acceptance. In response to this concern, a previous survey demonstrated that 81% of respondents would opt for FMT to treat a hypothetical case of recurrent CDI.10 However, the surveyed population did not have CDI, and the 48% response rate is concerning, since those with a favorable opinion of FMT might be more willing to complete a survey than would other patients. Accordingly, the authors systematically surveyed hospitalized veterans with active CDI to assess their knowledge, attitudes, and opinions about FMT as a treatment for CDI.
Methods
In-person patient interviews were conducted by one of the study authors at the Minneapolis VA Health Care System (MVAHCS), consisting of 13 to 18 questions. Questions addressed any prior CDI episodes and knowledge of the following: CDI, recurrence risk, and FMT; preferred route and location of FMT administration; concerns regarding FMT; likelihood of agreeing to undergo FMT (if available); and likelihood of enrollment in a hypothetical study comparing FMT to standard antibiotic treatment. The survey was developed internally and was not validated. Questions used the Likert-scale (Survey).
Patients with CDI were identified by monitoring for positive C difficile polymerase chain reaction (PCR) stool tests and then screened for inclusion by medical record review. Inclusion criteria were (1) MVAHCS hospitalization; and (2) written informed consent. Exclusion criteria were the inability to communicate or participate in an interview. Patient responses regarding their likelihood of agreeing to FMT for CDI treatment under different circumstances were compared using Wilcoxon rank sum test. These circumstances included FMT for their current episode of CDI, FMT for a subsequent episode, and FMT if recommended by their physician. Possible concerns regarding FMT also were solicited, including infection risk, effectiveness, and procedural aesthetics. The MVAHCS institutional review board approved the study.
Results
Stool PCR tests for CDI were monitored for 158 days from 2013 to 2014 (based on availability of study staff), yielding 106 positive results. Of those, 31 (29%) were from outpatients and not addressed further. Of the 75 positive CDI tests from 66 hospitalized patients (9 patients had duplicate tests), 18 of 66 (27%) were not able to provide consent and were excluded, leaving 48 eligible patients. Six (13%) were missed for logistic reasons (patient at a test or procedure, discharged before approached, etc), leaving 42 patients who were approached for participation. Among these, 34 (81%) consented to participate in the survey. Two subjects (6%) found the topic so unappealing that they terminated the interview.
The majority of enrolled subjects were men (32/34, 94%), with a mean age of 65.3 years (range, 31-89). Eleven subjects (32%) reported a prior CDI episode, with 10 reporting 1 such episode, and the other 2 episodes. Those with prior CDI reported the effect of CDI on their overall quality of life as 5.1 (1 = no limitation, 10 = severe limitation). Respondents were fairly accurate regarding the risk of recurrence after an initial episode of CDI, with the average expectedrecurrence rate estimated at 33%. In contrast, their estimation of the risk of recurrence after a second CDI episode was lower (28%), although the risk of recurrent episodes increases with each CDI recurrence.
Regarding FMT, 5 subjects indicated awareness of the procedure: 2 learning of it from a news source, 1 from family, 1 from a health care provider, and 1 was unsure of the source. After subjects received a description of FMT, their opinions regarding the procedure were elicited. When asked which route of delivery they would prefer if they were to undergo FMT, the 33 subjects who provided a response indicated a strong preference for either enema (15, 45%) or colonoscopy (10, 30%), compared with just 4 (12%) indicating no preference, 2 (6%) choosing nasogastric tube administration, and 2 (6%) indicating that they would not undergo FMT by any route (P < .001).
Regarding the location of FMT administration (hospital setting vs self-administered at home), 31 of 33 respondents (94%) indicated they would prefer FMT to occur in the hospital vs 2 (6%) preferring self-administration at home (P < .001). The preferred source of donor stool was more evenly distributed, with 14 of 32 respondents (44%) indicating a preference for an anonymous donor, 11 preferring a family member (34%), and 7 (21%) with no preference (P = .21).
Subjects were asked about concerns regarding FMT, and asked to rate each on a 5-point Likert scale (1 = not at all concerning; 5 = overwhelming concern). Concerns regarding risk of infection and effectiveness received an average score of 2.74 and 2.72, respectively, whereas concern regarding the aesthetics, or "yuck factor" was slightly lower (2.1: P = NS for all comparisons). Subjects also were asked to rate the likelihood of undergoing FMT, if it were available, for their current episode of CDI, a subsequent episode of CDI, or if their physician recommended undergoing FMT (10 point scale: 1 = not at all likely; 10 = certainly agree to FMT). The mean scores (SD) for agreeing to FMT for the current or a subsequent episode were 4.8 (SD 2.7) and 5.6 (SD 3.0); P = .12, but increased to 7.1 (SD 3.23) if FMT were recommended by their physician (P < .001 for FMT if physician recommended vs FMT for current episode; P = .001 for FMT if physician recommended vs FMT for a subsequent episode). Finally, subjects were asked about the likelihood of enrolling in a study comparing FMT to standard antimicrobial treatment, with answers ranging from 1 (almost certainly would not enroll) to 5 (almost certainly would enroll). Among the 32 respondents to this question, 17 (53%) answered either "probably would enroll" or "almost certainly would enroll," with a mean score of 3.2.
Discussion
Overall, VA patients with a current episode of CDI were not aware of FMT, with just 15% knowing about the procedure. However, after learning about FMT, patients expressed clear opinions regarding the route and setting of FMT administration, with enema or colonoscopy being the preferred routes, and a hospital the preferred setting. In contrast, subjects expressed ambivalence with regard to the source of donor stool, with no clear preference for stool from an anonymous donor vs from a family member.
When asked about concerns regarding FMT, none of the presented options (risk of infection, uncertain effectiveness, or procedural aesthetics) emerged as significantly more important than did others, although the oft-cited concern regarding FMT aesthetics engendered the lowest overall level of concern. In terms of FMT acceptance, 4 subjects (12%) were opposed to the procedure, indicating that they were not at all likely to agree to FMT for all scenarios (defined as a score of 1 or 2 on the 10-point Likert scale) or by terminating the survey because of the questions. However, 15 (44%) indicated that they would certainly agree to FMT (defined as a score of 9 or 10 on the 10-point Likert scale) if their physician recommended it. Physician recommendation for FMT resulted in the highest overall likelihood of agreeing to FMT, a finding in agreement with a previous survey of FMT for CDI.10 Most subjects indicated likely enrollment in a potential study comparing FMT with standard antimicrobial therapy.
Strengths/Limitations
Study strengths included surveying patients with current CDI, such that patients had personal experience with the disease in question. Use of in-person interviews also resulted in a robust response rate of 81% and allowed subjects to clarify any unclear questions with study personnel. Weaknesses included a relatively small sample size, underrepresentation of women, and lack of detail regarding respondent characteristics. Additionally, capsule delivery of FMT was not assessed since this method of delivery had not been published at the time of survey administration.
Conclusion
This survey of VA patients with CDI suggests that aesthetic concerns are not a critical deterrent for this population, and interest in FMT for the treatment of recurrent CDI exists. Physician recommendation to undergo FMT seems to be the most influential factor affecting the likelihood of agreeing to undergo FMT. These results support the feasibility of conducting clinical trials of FMT in the VA system.
Clostridium difficile (C difficile) infection (CDI) is a leading cause of infectious diarrhea among hospitalized patients and, increasingly, in ambulatory patients.1,2 The high prevalence of CDI and the high recurrence rates (15%-30%) led the CDC to categorize C difficile as an "urgent" threat (the highest category) in its 2013 Antimicrobial Resistance Threat Report.3-5 The Infectious Diseases Society of America guideline recommended treatment for CDI is vancomycin or metronidazole; more recent studies also support fidaxomicin use.4,6,7
Patients experiencing recurrent CDI are at risk for further recurrences, such that after the third CDI episode, the risk of subsequent recurrences exceeds 50%.8 This recurrence rate has stimulated research into other treatments, including fecal microbiota transplantation (FMT). A recent systematic review of FMT reports that 85% of patients have resolution of symptoms without recurrence after FMT, although this is based on data from case series and 2 small randomized clinical trials.9
A commonly cited barrier to FMT is patient acceptance. In response to this concern, a previous survey demonstrated that 81% of respondents would opt for FMT to treat a hypothetical case of recurrent CDI.10 However, the surveyed population did not have CDI, and the 48% response rate is concerning, since those with a favorable opinion of FMT might be more willing to complete a survey than would other patients. Accordingly, the authors systematically surveyed hospitalized veterans with active CDI to assess their knowledge, attitudes, and opinions about FMT as a treatment for CDI.
Methods
In-person patient interviews were conducted by one of the study authors at the Minneapolis VA Health Care System (MVAHCS), consisting of 13 to 18 questions. Questions addressed any prior CDI episodes and knowledge of the following: CDI, recurrence risk, and FMT; preferred route and location of FMT administration; concerns regarding FMT; likelihood of agreeing to undergo FMT (if available); and likelihood of enrollment in a hypothetical study comparing FMT to standard antibiotic treatment. The survey was developed internally and was not validated. Questions used the Likert-scale (Survey).
Patients with CDI were identified by monitoring for positive C difficile polymerase chain reaction (PCR) stool tests and then screened for inclusion by medical record review. Inclusion criteria were (1) MVAHCS hospitalization; and (2) written informed consent. Exclusion criteria were the inability to communicate or participate in an interview. Patient responses regarding their likelihood of agreeing to FMT for CDI treatment under different circumstances were compared using Wilcoxon rank sum test. These circumstances included FMT for their current episode of CDI, FMT for a subsequent episode, and FMT if recommended by their physician. Possible concerns regarding FMT also were solicited, including infection risk, effectiveness, and procedural aesthetics. The MVAHCS institutional review board approved the study.
Results
Stool PCR tests for CDI were monitored for 158 days from 2013 to 2014 (based on availability of study staff), yielding 106 positive results. Of those, 31 (29%) were from outpatients and not addressed further. Of the 75 positive CDI tests from 66 hospitalized patients (9 patients had duplicate tests), 18 of 66 (27%) were not able to provide consent and were excluded, leaving 48 eligible patients. Six (13%) were missed for logistic reasons (patient at a test or procedure, discharged before approached, etc), leaving 42 patients who were approached for participation. Among these, 34 (81%) consented to participate in the survey. Two subjects (6%) found the topic so unappealing that they terminated the interview.
The majority of enrolled subjects were men (32/34, 94%), with a mean age of 65.3 years (range, 31-89). Eleven subjects (32%) reported a prior CDI episode, with 10 reporting 1 such episode, and the other 2 episodes. Those with prior CDI reported the effect of CDI on their overall quality of life as 5.1 (1 = no limitation, 10 = severe limitation). Respondents were fairly accurate regarding the risk of recurrence after an initial episode of CDI, with the average expectedrecurrence rate estimated at 33%. In contrast, their estimation of the risk of recurrence after a second CDI episode was lower (28%), although the risk of recurrent episodes increases with each CDI recurrence.
Regarding FMT, 5 subjects indicated awareness of the procedure: 2 learning of it from a news source, 1 from family, 1 from a health care provider, and 1 was unsure of the source. After subjects received a description of FMT, their opinions regarding the procedure were elicited. When asked which route of delivery they would prefer if they were to undergo FMT, the 33 subjects who provided a response indicated a strong preference for either enema (15, 45%) or colonoscopy (10, 30%), compared with just 4 (12%) indicating no preference, 2 (6%) choosing nasogastric tube administration, and 2 (6%) indicating that they would not undergo FMT by any route (P < .001).
Regarding the location of FMT administration (hospital setting vs self-administered at home), 31 of 33 respondents (94%) indicated they would prefer FMT to occur in the hospital vs 2 (6%) preferring self-administration at home (P < .001). The preferred source of donor stool was more evenly distributed, with 14 of 32 respondents (44%) indicating a preference for an anonymous donor, 11 preferring a family member (34%), and 7 (21%) with no preference (P = .21).
Subjects were asked about concerns regarding FMT, and asked to rate each on a 5-point Likert scale (1 = not at all concerning; 5 = overwhelming concern). Concerns regarding risk of infection and effectiveness received an average score of 2.74 and 2.72, respectively, whereas concern regarding the aesthetics, or "yuck factor" was slightly lower (2.1: P = NS for all comparisons). Subjects also were asked to rate the likelihood of undergoing FMT, if it were available, for their current episode of CDI, a subsequent episode of CDI, or if their physician recommended undergoing FMT (10 point scale: 1 = not at all likely; 10 = certainly agree to FMT). The mean scores (SD) for agreeing to FMT for the current or a subsequent episode were 4.8 (SD 2.7) and 5.6 (SD 3.0); P = .12, but increased to 7.1 (SD 3.23) if FMT were recommended by their physician (P < .001 for FMT if physician recommended vs FMT for current episode; P = .001 for FMT if physician recommended vs FMT for a subsequent episode). Finally, subjects were asked about the likelihood of enrolling in a study comparing FMT to standard antimicrobial treatment, with answers ranging from 1 (almost certainly would not enroll) to 5 (almost certainly would enroll). Among the 32 respondents to this question, 17 (53%) answered either "probably would enroll" or "almost certainly would enroll," with a mean score of 3.2.
Discussion
Overall, VA patients with a current episode of CDI were not aware of FMT, with just 15% knowing about the procedure. However, after learning about FMT, patients expressed clear opinions regarding the route and setting of FMT administration, with enema or colonoscopy being the preferred routes, and a hospital the preferred setting. In contrast, subjects expressed ambivalence with regard to the source of donor stool, with no clear preference for stool from an anonymous donor vs from a family member.
When asked about concerns regarding FMT, none of the presented options (risk of infection, uncertain effectiveness, or procedural aesthetics) emerged as significantly more important than did others, although the oft-cited concern regarding FMT aesthetics engendered the lowest overall level of concern. In terms of FMT acceptance, 4 subjects (12%) were opposed to the procedure, indicating that they were not at all likely to agree to FMT for all scenarios (defined as a score of 1 or 2 on the 10-point Likert scale) or by terminating the survey because of the questions. However, 15 (44%) indicated that they would certainly agree to FMT (defined as a score of 9 or 10 on the 10-point Likert scale) if their physician recommended it. Physician recommendation for FMT resulted in the highest overall likelihood of agreeing to FMT, a finding in agreement with a previous survey of FMT for CDI.10 Most subjects indicated likely enrollment in a potential study comparing FMT with standard antimicrobial therapy.
Strengths/Limitations
Study strengths included surveying patients with current CDI, such that patients had personal experience with the disease in question. Use of in-person interviews also resulted in a robust response rate of 81% and allowed subjects to clarify any unclear questions with study personnel. Weaknesses included a relatively small sample size, underrepresentation of women, and lack of detail regarding respondent characteristics. Additionally, capsule delivery of FMT was not assessed since this method of delivery had not been published at the time of survey administration.
Conclusion
This survey of VA patients with CDI suggests that aesthetic concerns are not a critical deterrent for this population, and interest in FMT for the treatment of recurrent CDI exists. Physician recommendation to undergo FMT seems to be the most influential factor affecting the likelihood of agreeing to undergo FMT. These results support the feasibility of conducting clinical trials of FMT in the VA system.
1. Miller BA, Chen LF, Sexton DJ, Anderson DJ. Comparison of the burdens of hospital-onset, healthcare facility-associated Clostridium difficile Infection and of healthcare-associated infection due to methicillin-resistant Staphylococcus aureus in community hospitals. Infect Control Hosp Epidemiol. 2011;32(4):387-390.
2. Centers for Disease Control and Prevention. Severe Clostridium difficile-associated disease in populations previously at low risk--four states, 2005. MMWR Morb Mortal Wkly Rep. 2005;54(47):1201-1205.
3. Johnson S, Louie TJ, Gerding DN, et al; Polymer Alternative for CDI Treatment (PACT) investigators. Vancomycin, metronidazole, or tolevamer for Clostridium difficile infection: results from two multinational, randomized, controlled trials. Clin Infect Dis. 2014;59(3):345-354.
4. Louie TJ, Miller MA, Mullane KM, et al; OPT-80-003 Clinical Study Group. Fidaxomicin versus vancomycin for Clostridium difficile infection. N Engl J Med. 2011;364(5):422-431.
5. Centers for Disease Control and Prevention. Antibiotic resistance threats in the United States, 2013. http://www.cdc.gov/drugresistance/threat-report-2013. Updated July 17, 2014. Accessed November 16.2016.
6. Cohen SH, Gerding DN, Johnson S, et al; Society for Healthcare Epidemiology of America; Infectious Diseases Society of America. Clinical practice guidelines for Clostridium difficile infection in adults: 2010 update by the society for healthcare epidemiology of America (SHEA) and the Infectious Diseases Society of America (IDSA). Infect Control Hosp Epidemiol. 2010;31(5):431-455.
7. Cornely OA, Crook DW, Esposito R, et al; OPT-80-004 Clinical Study Group. Fidaxomicin versus vancomycin for infection with Clostridium difficile in Europe, Canada, and the USA: a double-blind, non-inferiority, randomised controlled trial. Lancet Infect Dis. 2012;12(4):281-289.
8. Johnson S. Recurrent Clostridium difficile infection: a review of risk factors, treatments, and outcomes. J Infect. 2009;58(6):403-410.
9. Drekonja DM, Reich J, Gezahegn S, et al. Fecal microbiota transplantation for Clostridium difficile infection--a systematic review. Ann Intern Med. 2015;162(9):630-638.
10. Zipursky JS, Sidorsky TI, Freedman CA, Sidorsky MN, Kirkland KB. Patient attitudes toward the use of fecal microbiota transplantation in the treatment of recurrent Clostridium difficile infection. Clin Infect Dis. 2012;55(12):1652-1658.
1. Miller BA, Chen LF, Sexton DJ, Anderson DJ. Comparison of the burdens of hospital-onset, healthcare facility-associated Clostridium difficile Infection and of healthcare-associated infection due to methicillin-resistant Staphylococcus aureus in community hospitals. Infect Control Hosp Epidemiol. 2011;32(4):387-390.
2. Centers for Disease Control and Prevention. Severe Clostridium difficile-associated disease in populations previously at low risk--four states, 2005. MMWR Morb Mortal Wkly Rep. 2005;54(47):1201-1205.
3. Johnson S, Louie TJ, Gerding DN, et al; Polymer Alternative for CDI Treatment (PACT) investigators. Vancomycin, metronidazole, or tolevamer for Clostridium difficile infection: results from two multinational, randomized, controlled trials. Clin Infect Dis. 2014;59(3):345-354.
4. Louie TJ, Miller MA, Mullane KM, et al; OPT-80-003 Clinical Study Group. Fidaxomicin versus vancomycin for Clostridium difficile infection. N Engl J Med. 2011;364(5):422-431.
5. Centers for Disease Control and Prevention. Antibiotic resistance threats in the United States, 2013. http://www.cdc.gov/drugresistance/threat-report-2013. Updated July 17, 2014. Accessed November 16.2016.
6. Cohen SH, Gerding DN, Johnson S, et al; Society for Healthcare Epidemiology of America; Infectious Diseases Society of America. Clinical practice guidelines for Clostridium difficile infection in adults: 2010 update by the society for healthcare epidemiology of America (SHEA) and the Infectious Diseases Society of America (IDSA). Infect Control Hosp Epidemiol. 2010;31(5):431-455.
7. Cornely OA, Crook DW, Esposito R, et al; OPT-80-004 Clinical Study Group. Fidaxomicin versus vancomycin for infection with Clostridium difficile in Europe, Canada, and the USA: a double-blind, non-inferiority, randomised controlled trial. Lancet Infect Dis. 2012;12(4):281-289.
8. Johnson S. Recurrent Clostridium difficile infection: a review of risk factors, treatments, and outcomes. J Infect. 2009;58(6):403-410.
9. Drekonja DM, Reich J, Gezahegn S, et al. Fecal microbiota transplantation for Clostridium difficile infection--a systematic review. Ann Intern Med. 2015;162(9):630-638.
10. Zipursky JS, Sidorsky TI, Freedman CA, Sidorsky MN, Kirkland KB. Patient attitudes toward the use of fecal microbiota transplantation in the treatment of recurrent Clostridium difficile infection. Clin Infect Dis. 2012;55(12):1652-1658.
Leadership Initiatives in Patient-Centered Transgender Care
Patient-centered care is of fundamental importance when caring for the transgender population due to the well-established history of social stigma and systemic discrimination. Therefore, nursing education is mandated to equip graduates with culturally competent patient-centered care skills.1 In 2009, the Institute of Medicine (IOM) in partnership with the Robert Wood Johnson Foundation (RWJF) launched The Future of Nursing initiative, which outlined the major role nursing should play in transforming the health care system to meet the health care needs of diverse U.S. populations.
The initiative produced a blueprint of action-focused institutional recommendations at the local, state, and national levels that would facilitate the reforms necessary to transform the U.S. health care system. One of the recommendations of the IOM report was to increase opportunities for nurses to manage and lead collaborative efforts with physicians and other health care team members in the areas of systems redesign and research, to improve practice environments and health systems.2
The VHA is the largest integrated health care system in the U.S., serving more than 8.76 million veterans at more than 1,700 facilities. The VHA has an organizational structure that uses centralized control in Washington, DC, and branches out to 18 regional networks that are divided into local facilities in 50 states, the District of Columbia, Puerto Rico, the U.S. Virgin Islands, Guam, American Samoa, and the Philippines. This type of structure is known for promoting efficient standardization of processes and procedures across an organization.3
The VHA Blueprint for Excellence envisions the promotion of a positive culture of service and the advancement of health care innovations necessary to create an environment that all veterans deserve.4 To that end, the VHA can be a promising health care institution through which patient-centered initiatives can be standardized, promulgated nationally, and replicated as a model for the country and international health systems. However, it is important to note that the bureaucratic organizational structure of the VHA's national integrated system of care is based on a systemwide standardization effort.5 Therefore, more time may be required to implement organizational changes.
Transgender populations face significant social stigmatization, discrimination, and marginalization that contribute to negative patient outcomes. Consequently, this population experiences high rates of suicide, HIV/AIDS, substance use disorder, poverty, and homelessness.6 Due to the growing evidence of health disparities and negative health outcomes affecting transgender populations, the federal government has identified transgender patient care and outcomes as a major health concern and priority in the Healthy People Initiative 2020.2,7,8
In 2012, the VHA issued a directive mandating services for transgender veterans.9 Nevertheless, health care staff significantly lack the knowledge, skills, and cultural competencies that are vital in transgender care.
This article reviews the prevalence and demographics of the transgender population, social challenges, global health concerns, and public health policies. The article also examines how the doctor of nursing practice (DNP)-prepared nurse leader can provide transformational nursing leadership to facilitate culturally competent, patient-centered initiatives to improve access and services for transgender individuals in the VHA and provide a model for change in transgender population health.
Definitions
Gender is a behavioral, cultural, or psychological trait assigned by society that is associated with male or female sex. Sex denotes the biologic differences between males and females. Transgender is an umbrella term used to describe people whose gender identity or gender expression is different from that of their sex assigned at birth. Transsexualism is a subset of transgender persons who have taken steps to self-identify or transition to look like their preferred gender.
Demographics
Estimates of the prevalence of transgenderism are roughly drawn from less rigorous methods, such as the combination of parents who report transgenderism in children, the number of adults reportedly seeking clinical care (such as cross-sex or gender-affirming hormone therapy), and the number of surgical interventions reported in different countries.10 A meta-analysis of 21 studies concluded that the ratio of transsexuals (individuals who are altering or have already altered their birth sex) was predominantly 1:14,705 adult males and 1:38,461 adult females.11 Since all transgender persons do not identify as transsexual, these figures do not provide a precise estimation of the number of transgender persons worldwide.
About 700,000, or 0.3%, of the adult population in the U.S. identify themselves as transgender, and an estimated 134,300 identify as transgender veterans.6,12 The transgender population in the U.S. is estimated to be 55% white, 16% African American, 21% Hispanic, and 8% other races.13 The U.S. census data noted that the transgender population was geographically located across the nation. Transgender persons are more likely to be single, never married, divorced, and more educated but with significantly less household income.2 Data to provide an accurate reflection of the number of transgender people in the U.S. are lacking. Some transgender individuals also may identify as lesbian, gay, or bisexual, making population-based estimation even more challenging and difficult.
Transgender persons who have transitioned may not have changed their names or changed their identified sex on official Social Security records, which the Social Security Administration allows only if there is evidence that genital sexual reassignment surgery was performed.14 The number of transgender adults requesting treatment continues to rise.10
Social and Health Challenges
Transgender people face many challenges because of their gender identity. Surveys assessing the living conditions of transgender people have found that 43% to 60% report high levels of physical violence.15 By comparison, the National Intimate Partner and Sexual Violence Survey found that interpersonal violence and sexual violence were reported by lesbian and gay individuals at equal or higher levels than that reported by heterosexuals. Forty-four percent of lesbian women, 35% of heterosexual women, 29% of heterosexual men, and 26% of gay men reported experiencing rape or physical violence.16 A study in Spain reported 59% of transgender people experienced patterns of harassment, and in Canada, 34% of transgender people lived below the poverty level.17,18
In the U.S., the National Transgender Discrimination Survey of 6,450 transgender and nonconforming participants provided extensive data on challenges experienced by transgender people.6 Discrimination was frequently experienced in accessing health care. Due to transgender status, 19% were denied care, and 28% postponed care due to perceived harassment and violence within a health care setting.6 The same study also reported that as many as 41% live in extreme poverty with incomes of less than $10,000 per year reported. Twenty-six percent were physically assaulted, and 10% experienced sexual violence. More than 25% of the transgender population misused drugs or alcohol to cope with mistreatment.6
In the U.S., HIV infection rates for transgender individuals were more than 4 times (2.64%) the rate of the general population (0.6%).6 Internationally, there is a high prevalence of HIV in transgender women. The prevalence rate of HIV in U.S. transgender women was 21.74% of the estimated U.S. adult transgender population of about 700,000.19 One in 4 people living with HIV in the U.S. are women.20
Suicide attempt rates are extremely high among transgender people. A suicide rate of 22% to 43% has been reported across Europe, Canada, and the U.S.21 Depression and anxiety were commonly noted as a result of discrimination and social stigma. In the U.S., transgender persons reported high rates of depression, with 41% reporting attempted suicide compared with 1.6% of the general population.6 Access to health care services, such as mental health, psychosocial support, and stress management are critical for this vulnerable population.22
Health Policies
Since 1994, the UK has instituted legal employment protections for the transgender population. In the UK, transgender persons, including military and prisoners, have health care coverage that includes sexual reassignment surgery as part of the UK's National Health Service.23
In the U.S., the federal policy of "Don't Ask, Don't Tell" barring transgender persons from serving openly in the military was repealed in June 2016. This policy historically has had a silencing effect on perpetuating institutionalized biases.24 This remains problematic even after veterans have transitioned from military service to the VA for civilian care.
Between 2006 and 2013, the reported prevalence and incidence of transgender-related diagnoses in the VA have steadily increased with 40% of new diagnoses occurring since 2011.25 In fiscal year 2013, there were 32.9 per 100,000 veterans with transgender-related diagnoses.25 Health care staff, in particular health care providers (HCPs), can play a critical role in reducing health disparities and unequal treatment.26
With the passage of the U.S. Affordable Care Act (ACA), health insurance coverage for transgender persons is now guaranteed by law, and health disparities within the transgender population can begin to be properly addressed. The ACA offers the ability to purchase health insurance, possibly qualify for Medicaid, or obtain subsidies to purchase health insurance. Insurance coverage is accessible without regard to discrimination or preexisting conditions.27 As of May 2014, the Medicare program covered medically necessary hormone therapy and sex reassignment surgery.13 While VA benefits cover hormone therapy for transgender veterans, sex reassignment surgery is not currently a covered benefit.28 The ACA now increases access to primary care, preventative care, mental health services, and community health programs not previously available in the transgender community.
Healthy People 2020 Goals
One of the Healthy People 2020 stated goals is to improve the health and wellness of transgender people.29 The objective is to increase the number of population-based data collection systems used to monitor transgender people from the baseline of 2 to a total of 4 by 2020. The data systems would be assigned to collect relevant data, such as mental health; HIV status; illicit drug, alcohol, and tobacco use; cervical and breast cancer screening; health insurance coverage; and access to health care.
Health Care Staff Readiness
Transgender persons face health care challenges with major health disparities due to their gender identity. Transgender persons as a defined population are not well understood by HCPs. In a survey, 50% of transgender respondents reported that they had to teach their medical provider about transgender care.6 Negative perceptions of transgender persons are well established and have contribute to the poor health care access and services that transgender persons receive. Transgender persons are often denied access to care, denied visitation rights, and are hesitant to share information for fear of bureaucratic exclusion or isolation.
There is a lack of evidence-based studies to guide care and help HCPs gain greater understanding of this population's unique needs.30 Additionally, a significant lack of knowledge, skills, cultural competence, and awareness exist in providing transgender care. Research on nursing attitudes concerning transgender care consistently found negative attitudes, and physicians also frequently reported witnessing derogatory comments and discriminatory care from colleagues.31,32 The study by Carabez and colleagues found that practicing nurses rarely received the proper education or training in transgender health issues, and many were unaware of the needs of this population.33 In addition, many HCPs were uncomfortable working with transgender patients. Physicians also expressed knowledge deficits on gender identity disorders due to a lack of training and ethical concerns about their roles in providing gender-transitioning treatment.26
Although the VHA directive states that transgender services and treatment should be standardized, the VHA has not approved, defined, or endorsed specific standards of care or clinical guidelines within the organization for transgender care, further heightening HCP concerns.9 The clinical practice guidelines available for addressing preventive care for transgender patients are primarily based on consensus of expert opinion.34 Expert opinion has produced the Standards of Care (SOC) for the Health of Transsexual, Transgender, and Gender Nonconforming People, published by the World Professional Association for Transgender Health (WPATH) and cited by the IOM as the major clinical practice guidelines for providing care to transgender individuals.2 Transgender care at the VHA is guided by the WPATH standards of care.35
The VHA has created national educational programs and policies with targeted goals to provide uniform, culturally competent, patient-centered care. Online transgender health presentations are available, and at least 15 VHA facilities have transgender support groups.30 While the VHA supports a patient-centered philosophy for transgender patient care, many facilities do not currently have organizational initiatives that enhance clinical preparation of HCPs or have sufficiently modified the environment to better accommodate the health care needs of transgender veterans.
DNP Preparation
The DNP terminal degree provides nurses with doctoral-level training in organizational and systems leadership, leading quality improvement, and implementing systemwide initiatives by using scientific findings to drive processes that improve quality of care for a changing patient population.36 Preparation in research analysis of evidence-based interventions also is essential to evaluating practice patterns, patient outcomes, and systems of care that can identify gaps in practice. Training in health care policy and advocacy, information systems, patient care technology, and population health also is provided so that DNPs are competent to develop system strategies to transform health care through clinical prevention and health promotion.
QSEN Framework
In keeping with the IOM's Future of Nursing initiative recommendations that graduate nurses be prepared as leaders in education, practice, administration, and research, there is an increasing focus on providing graduate-level nursing education and training to ensure quality and efficiency of health outcomes.37 The Quality and Safety Education in Nursing (QSEN) project, initiated at the RWJF by Linda Cronenwett, PhD, RN, identifies a framework for knowledge, skills, and attitudes that defines the competencies that nurses need to deliver effective care to improve quality and safety within health care systems.38 These core competencies include quality improvement, safety, teamwork and collaboration, patient-centered care, evidence-based practice, and informatics. The RWJF and the American Association of Colleges of Nursing later expanded the project initiative to prepare nursing faculty to teach the QSEN competencies in graduate nursing programs.36
The DNP nurse leader is ideally suited to manage this project by applying competencies from the QSEN framework. Using open communication and mutual respect, the nurse leader is poised to effectively develop interprofessional teams to collaborate and initiate transformational changes that improve quality and patient-centered care delivered within the health care organization.
Public Health Resources
Public health resources addressing transgender patient care advocacy, public policy, community education, standards of care, cultural competency, mental health, hormone therapy, surgical interventions, reproductive health, primary care, preventative care, and research are available. For example, WPATH is an international multidisciplinary organization that has published comprehensive SOC for transgender, transsexual, and gender-nonconforming people. The seventh version of the SOC contains evidence-based guidelines for treatment.39 Additional online resources for transgender health are available from the CDC, the Center of Excellence for Transgender Health at the University of California, San Francisco; Department of Family and Community Medicine; and the National Center for Transgender Equality.13,40,41
Patient-Centered Transgender Care
The QSEN framework outlines competencies that provide applicable solutions that help prepare organizations to deliver culturally competent, patient-centered transgender care. The first step to creating patient-centered transgender care is to "analyze factors that create barriers to patient-centered care."42 The magnitude of the barriers to providing patient-centered transgender care also must be identified and understood. An assessment of individual values, beliefs, and attitudes can help to identify cultural characteristics and eliminate stereotypes that impact health practices.43
The nurse leader should solicit support from stakeholders to assess barriers to providing patient-centered transgender care at the system level. Stakeholders would include staff directly involved in patient care, such as physicians, nurse practitioners, physician assistants, registered nurses, nurse managers, nurse educators, licensed practical nurses, medical support assistants, psychologists, dieticians, and social workers. Other ancillary stakeholders with an interest in creating a patient-centered environment with positive patient outcomes include the executive leadership team of the organization, which consists of the chief of staff, director, administrative officers, and nurse executive.
The nurse leader should consult with experts in transgender care and present evidence-based research showing how deficits in staff knowledge, skills, and cultural competence negatively impact the quality of care provided to transgender persons. National data on the consequential health disparities and negative impacts on patient outcomes also should be discussed and presented to all stakeholders. The nurse leader in collaboration with the VA Office of Research and Development is ideally suited to obtain institutional review board approval of a proposal to conduct a needs assessment survey of health care staff barriers to providing patient-centered transgender care. Thereafter, the nurse leader would analyze, extract, and synthesize the data and evaluate the resources and technology available to translate this research knowledge into a clinical practice setting at the system level.44
The second solution uses the results of the survey to develop staff competency training within the organization. The nurse leader can facilitate collaboration and team building to develop practice guidelines and SOC. Competency training will prepare the staff to assist in developing strategies to improve the quality of care for transgender persons. Educationconcerning existing evidence-based clinical guidelines and SOC as well as anecdotal evidence of the needs of transgender patients should be included in competency training.45 One approach to competency training would be to trainintegrated multidisciplinary teams with expertise in transgender care to promote wellness and disease prevention.9 The nurse leader should collaborate with multiple disciplines to facilitate the development of interdisciplinary teams from nursing, medicine, social work, pharmacy, primary care, mental health, women's health, and endocrinology to participate in the Specialty Care Access Network Extension of Community Healthcare outcomes (SCAN-ECHO) training. Training can be offered by videoconferencing over several months and provides cost-effective, efficient training of providers in patient-centered transgender care.46,47 After the SCAN-ECHO program is completed, trained nursing experts could then develop a cultural sensitivity training program for nursing organizations to be offered to educate health care staff on an annual basis.
The third solution addresses the QSEN competency to "Analyze institutional features of the facilities that support or pose barriers to patient-centered care."42 Many veterans do not perceive VA environments as welcoming. In a study by Sherman and colleagues, less than one-third of veterans believed the VA environment was welcoming to sexual or gender minorities, and sexual orientation or gender identity was disclosed by only about 25% of veterans.48 Many veterans in this study felt uncomfortable disclosing their gender or sexual orientation. The majority felt that providers should not routinely ask about sexual orientation or gender identity, and 24% said they were very or somewhat uncomfortable discussing the issue. In another study, 202 VA providers were asked if they viewed the VA as welcoming, and 32% said the VA was somewhat or very unwelcoming.48
The nurse leader is trained in the essentials of health care policy advocacy, which is central to nursing practice.49 Nursing as a profession values social justice and equality, which are linked to fewer health disparities and more stable health indicators.50 Therefore, nursing can ideally provide organizational leaders by developing a culture wherein stable, patient-centered relationships can develop and thrive.
Organizational Culture
Strategies must be deployed to create an organizational culture that is welcoming, respectful, and supportive of transgender patients and family preferences. VA should develop support groups for transgender veterans in VA facilities. Support groups are helpful in diminishing stress, improving self-esteem, building confidence, and improving social relationships.51 Additionally, VA should develop community-based partnerships with other organizations that already provide institutional care and support from HCPs who support transgender persons' right to self-determination.52 These partnerships can foster environmental influences over time and lead to the development of trusting relationships between transgender veterans and the VA organization.
Another community partnership of importance for the nurse leader to develop is an alliance with local universities to train nursing students in cultural competencies in transgender care at VA facilities. The U.S. population continues to diversify in race and ethnicity and cultural influences; therefore, nurses must be prepared in cultural competencies in order to provide quality care that reduces health disparities.53
Under federal law, the VHA has a data sharing agreement with the DoD. Despite the repeal of the "Don't Ask, Don't Tell" federal law, which cleared the way for transgender persons to openly serve in the military, many transgender persons may remain fearful of reprisals, such as judgment, denial of care, or loss of benefits if gender identity is disclosed.54 Given the bureaucratic structure of the VHA, the implementation of cultural changes at the system level will require a collaborative effort between multidisciplinary teams and community partnerships to transform the VA environment over time. The authors believe that on this issue, external forces must guide and lead changes within the VA system in order to develop sustainable and trusting relationships with transgender veterans.
The fourth solution is implementation of policies that "empower patients or families in all aspects of the health care process."42 Again, the nurse leader is trained and prepared to advocate for a policy that implements a Patient Bill of Rights that explicitly guarantees health care and prohibits discrimination of gender-minority veterans. This change would foster trust and confidence from transgender individuals. A study found that 83% of providers and 83% of lesbian, gay, bisexual, and transgender veterans believe that this policy change would make the VHA environment more welcoming.48 Providing transgender-affirming materials and language on standard forms also would eliminate barriers, promote patient-centered care, and empower transgender patients by creating an environment that is more inclusive of everyone.48
Conclusion
The nurse leader is well positioned to implement the QSEN framework to integrate research, practice, and policy to create a more inclusive, patient-centered health care system for transgender veterans. By using the essential principles of doctoral education for advanced nursing practice, the nurse leader is prepared to advocate for changing the organization at the systems level. The nurse leader also is equipped to direct the implementation of patient-centered transgender care initiatives by ensuring the integration of the nursing organization as a partner in strategic planning as well as the development of solutions.
The VHA Blueprint of Excellence envisions organization and collaboration to promote new relationships that serve and benefit veterans. The DNP preparation allows the nurse leader to demonstrate the ability to collaborate with VHA stakeholders and develop alliances within and outside the organization by advocating for policy changes that will be transformational in improving health care delivery and patient outcomes to vulnerable transgender veteran populations. The IOM has tasked nurse executives with creating a health care infrastructure of doctorally prepared nurses to provide patient care that is increasingly growing more complex. With an increasing number of veterans using services, VHA has prioritized an expansion in the number of doctorally prepared nurses.55
As the largest integrated health care system in the U.S., the VHA provides an ideal setting for initiating these organizational changes as a result of having developed an integrated infrastructure to collect evidence-based data at the regional (network) and state facilities and make comparisons with national benchmarks. Therefore, changes are less difficult to disseminate throughout the hierarchy of the VHA. Consequently, the VHA has been a leader in the U.S. for equity in the health care arena and provides a model for international health care systems. Finally, these changes address an urgent need to reduce health disparities, morbidity, and mortality by improving quality care and health care delivery to a vulnerable transgender population.
1. Greiner AC, Knebel E, eds. Health Professions Education: A Bridge to Quality. Washington, DC: National Academies Press; 2003.
2. Institute of Medicine. Bisexual, and Transgender People: Building a Foundation for Better Understanding. Washington, DC: National Academy of Sciences; 2011.
3. Mintzberg H. The structuring of organizations: a synthesis of the research. https://papers.ssrn.com/sol3/papers.cfm?abstract_id=1496182 1979. Posted November 4, 2009. Accessed November 30, 2016.
4. U.S. Department of Veterans Affairs. VHA blue print for excellence. https://www.va.gov/health/docs/VHA_Blueprint_for_Excellence.pdf. Published September 21, 2014. Accessed November 30, 2016.
5. Morgan RO, Teal CR, Reddy SG, Ford ME, Ashton CM. Measurement in Veterans Affairs Health Services Research: veterans as a special population. Health Serv Res. 2005;40(5, part 2):1573-1583.
6. Grant JM, Mottet L, Tanis JE, Harrison J, Herman J, Keisling M. Injustice at every turn: a report of the National Transgender Discrimination Survey. http://www.thetaskforce.org/static_html/downloads /reports/reports/ntds_full.pdf. Published 2011. Accessed November 30, 2016.
7. Office of Disease Prevention and Health Promotion. Lesbian, gay, bisexual, and transgender health. http://www.healthypeople.gov/2020/topics-objec tives/topic/lesbian-gay-bisexual-and-transgender -health. Updated November 16, 2016. Accessed November 16, 2016.
8. Institute of Medicine Committee on Lesbian Gay, Bisexual, and Transgender Health Issues and Research Gaps and Opportunities. The Health of Lesbian, Gay, Bisexual, and Transgender People: Building a Foundation for Better Understanding. Washington, DC: National Academy of Sciences; 2011.
9. U.S. Department of Veterans Affairs. VHA Directive 2013-003: Providing Health Care for Transgender and Intersex Veterans. Washington, DC: U.S. Department of Veterans Affairs; 2013.
10. Zucker KJ, Lawrence AA. Epidemiology of gender identity disorder: recommendations for the Standards of Care of the World Professional Association for Transgender Health. Int J Transgenderism. 2009;11(1):8-18.
11. Arcelus J, Bouman WP, Van Den Noortgate W, Claes L, Witcomb G, Fernandez-Aranda F. Systematic review and meta-analysis of prevalence studies in transsexualism. Eur Psychiatry. 2015;30(6):807-815.
12. Gates GJ, Herman JL. Transgender military service in the United States. http://williamsinstitute.law.ucla.edu/wp-content/uploads/Transgender-Military -Service-May-2014.pdf. Published May 2014. Accessed November 30, 2016.
13. Flores AR, Brown TNT, and Herman JL. Race and ethnicity of adults who identify as transgender in the United States. http://williamsinstitute.law.ucla .edu/wp-content/uploads/Race-and-Ethnicity-of -Transgender-Identified-Adults-in-the-US.pdf. Published October 2016. Accessed December 13, 2016.
14. Harris BC. Likely Transgender individuals in US federal administrative records and the 2010 census. https://www.census.gov/srd/carra/15_03_Likely_Transgender_Individuals_in_ARs_and_2010Census.pdf. Published May 4, 2015. Accessed November 30, 2016.
15. Kenagy GP, Bostwick WB. Health and social service needs of transgender people in Chicago. Int J Transgenderism. 2005;8(2-3):57-66.
16. Centers for Disease Control and Prevention. National intimate partner and sexual violence survey, 2010 summary report. https://www.cdc.gov/viole nceprevention/pdf/nisvs_report2010-a.pdf. Published November 2011. Accessed December 12, 2016.
17. Bauer GR, Travers R, Scanlon K, Coleman TA. High heterogeneity of HIV-related sexual risk among transgender people in Ontario, Canada: a province-wide respondent-driven sampling survey. BMC Public Health. 2012;12(1):292-291.
18. Devis-Devis J, Pereira-Garcia S, Valencia-Peris A, Fuentes-Miguel J, López-Cañada E, Pérez-Samaniego V. Harassment patterns and risk profile in Spanish trans persons. J Homosex. 2016. [Epub ahead of print.]
19. Gates GJ. How many people are lesbian, gay, bisexual, and transgender? http://williamsinstitute.law.ucla.edu/wp-content/uploads/Gates-How-Many -People-LGBT-Apr-2011.pdf. Published April 2011. Accessed December 1, 2016.
20. Center for Disease Control and Prevention. HIV Among Women. http://www.cdc.gov/hiv/group/gender/women/index.html. Accessed December 10, 2016.
21. Bauer GR, Scheim AI, Pyne J, Travers R, Hammond R. Intervenable factors associated with suicide risk in transgender persons: a respondent driven sampling study in Ontario, Canada. BMC Public Health. 2015;15(1):525.
22. McCann E. People who are transgender: mental health concerns. J Psychiatr Ment Health Nurs. 2015;22(1):76-81.
23. Green R. Transsexual legal rights in the United States and United Kingdom: employment, medical treatment, and civil status. Arch Sex Behav. 2010;39(1):153-160.
24. Sharpe VA, Uchendu US. Ensuring appropriate care for LGBT veterans in the Veterans Health Administration. Hastings Cent Rep. 2014;44(suppl 4):S53-S55.
25. Kauth MR, Shipherd JC, Lindsay J, Blosnich JR, Brown GR, Jones KT. Access to care for transgender veterans in the Veterans Health Administration: 2006-2013. Am J Public Health. 2014;104(suppl 4):S532-S534.
26. Snelgrove JW, Jasudavisius AM, Rowe BW, Head EM, Bauer GR. "Completely out-at-sea" with "two-gender medicine": a qualitative analysis of physician-side barriers to providing healthcare for transgender patients. BMC Health Serv Res. 2012;12(1):110.
27. U.S. Department of Health and Human Services. Key features of the affordable care act. http://www .hhs.gov/healthcare/facts-and-features/key-features -of-aca/index.html. Last reviewed November 18, 2014. Accessed December 1, 2016.
28. U.S. Department of Veterans Affairs. Federal benefits for veterans, dependents, and survivors. https://www.va.gov/opa/publications/benefits_book/Chapter_1_Health_Care_Benefits.asp. Accessed December 1, 2016.
29. HealthyPeople.gov. Lesbian, gay, bisexual, and transgender health. https://www.healthypeople.gov/2020/topics-objectives/topic/lesbian-gay-bi sexual-and-transgender-health. Updated December 1, 2016. Accessed December 1, 2016.
30. Lutwak N, Byne W, Erickson-Schroth L, et al. Transgender veterans are inadequately understood by health care providers. Mil Med. 2014;179(5):483-485.
31. Dorsen C. An integrative review of nurse attitudes towards lesbian, gay, bisexual, and transgender patients. Can J Nurs Res. 2012;44(3):18-43.
32. Eliason MJ, Dibble SL, Robertson PA. Lesbian, gay, bisexual, and transgender (LGBT) physicians' experiences in the workplace. J Homosex. 2011;58(10):1355-1371.
33. Carabez R, Pellegrini M, Mankovitz A, Eliason M, Ciano M, Scott M. "Never in All My Years...": Nurses' education about LGBT health. J Prof Nurs. 2015;31(4):323-329
34. Buchholz L. Transgender care moves into the mainstream. JAMA. 2015;314(17):1785-1787.
35. VA Boston Healthcare System. Patient Care Memorandum-11-046-LM. Management of transgender veteran patients. http://www.boston.va.gov/services/images/lgbt_patient_care_memo_transgender_care.pdf. Published May 2011. Accessed December 1, 2016.
36. Cronenwett L, Sherwood G, Pohl J, et al. Quality and safety education for advanced nursing practice. Nurs Outlook. 2009;57(6):338-348.
37. Institute of Medicine. Committee on the Robert Wood Johnson Foundation Initiative on the Future of Nursing. The Future of Nursing: Leading Change, Advancing Health. Washington, DC: National Academies Press; 2011.
38. Smith EL, Cronenwett L, Sherwood G. Current assessments of quality and safety education in nursing. Nurs Outlook. 2007;55(3):132-137.
39. World Professional Association for Transgender Health (WPATH).The standards of care. http://www.wpath.org/site_page.cfm?pk_association _webpage_menu=1351&pk_association_web page=4655. Accessed December 1, 2016.
40. University of California San Francisco Department of Family and Community Medicine. Center of Excellence for Transgender Health. http://www.tran shealth.ucsf.edu/trans?page=home-00-00 Accessed December 1, 2016.
41. Center for Disease Control and Prevention. Lesbian, gay, bisexual and transgender health. http://www.cdc.gov/lgbthealth/transgender.htm. Accessed December 1, 2016.
42. American Association of Colleges of Nursing. QSEN education consortium: graduate-level QSEN competencies, knowledge, skills and attitudes. http://www.aacn.nche.edu/faculty/qsen/competen cies.pdf. Accessed December 1, 2016.
43. Andrews MM, Boyle JS. Transcultural Concepts in Nursing Care. Philadelphia, PA: Lippincott Williams & Wilkins; 2008.
44. Moran KJ, Burson R, Conrad D. The Doctor of Nursing Practice Scholarly Project: A Framework for Success. Burlington, MA: Jones & Bartlett; 2013.
45. Hanssmann C, Morrison D, Russian E, Shiu-Thornton S, Bowen D. A community-based program evaluation of community competency trainings. J Assoc Nurses AIDS Care.
46. Knapp H, Fletcher M, Taylor A, Chan K, Goetz MB. No clinic left behind: providing cost-effective in-services via distance learning. J Healthc Qual. 2011;33(5):17-24.
47. Kauth MR, Shipherd JC, Lindsay JA, Kirsh S, Knapp H, Matza L. Teleconsultation and training of VHA providers on transgender care: implementation of a multisite hub system. Telemed J E Health. 2015;21(12):1012-1018.
48. Sherman MD, Kauth MR, Ridener L, Shipherd JC, Bratkovich K, Beaulieu G. An empirical investigation of challenges and recommendations for welcoming sexual and gender minority veterans into VA care. Prof Psychol: Res Pract. 2014;45(6):433-442.
49. American Association of Colleges of Nursing. The essentials of doctoral education for advanced nursing practice. http://www.aacn.nche.edu/pub lications/position/DNPEssentials.pdf. Published October 2006. Accessed December 1, 2016.
50. Boutain DM. Social justice as a framework for professional nursing. J Nurs Educ. 2005;44(9):404-408.
51. Poteat T, German D, Kerrigan D. Managing uncertainty: a grounded theory of stigma in transgender health care encounters. Soc Sci Med. 2013;84:22-29.
52. Thornhill L, Klein P. Creating environments of care with transgender communities. J Assoc Nurs AIDS Care. 2010;21(3):230-239.
53. Collins J. Nursing cultural competencies: Improving patient care quality and satisfaction. Ohio Nurses Rev. 2015;90(1):10-11.
54. Sherman MD, Kauth MR, Shipherd JC, Street RL Jr. Communication between VA providers and sexual and gender minority veterans: a pilot study. Psychol Serv. 2014;11(2):235-242.
55. Cowan L, Fasoli DR, Hagle ME, et al. Creating an infrastructure to advance nursing practice and care for veterans. Nurse Leader. 2013;11(5):33-36.
Patient-centered care is of fundamental importance when caring for the transgender population due to the well-established history of social stigma and systemic discrimination. Therefore, nursing education is mandated to equip graduates with culturally competent patient-centered care skills.1 In 2009, the Institute of Medicine (IOM) in partnership with the Robert Wood Johnson Foundation (RWJF) launched The Future of Nursing initiative, which outlined the major role nursing should play in transforming the health care system to meet the health care needs of diverse U.S. populations.
The initiative produced a blueprint of action-focused institutional recommendations at the local, state, and national levels that would facilitate the reforms necessary to transform the U.S. health care system. One of the recommendations of the IOM report was to increase opportunities for nurses to manage and lead collaborative efforts with physicians and other health care team members in the areas of systems redesign and research, to improve practice environments and health systems.2
The VHA is the largest integrated health care system in the U.S., serving more than 8.76 million veterans at more than 1,700 facilities. The VHA has an organizational structure that uses centralized control in Washington, DC, and branches out to 18 regional networks that are divided into local facilities in 50 states, the District of Columbia, Puerto Rico, the U.S. Virgin Islands, Guam, American Samoa, and the Philippines. This type of structure is known for promoting efficient standardization of processes and procedures across an organization.3
The VHA Blueprint for Excellence envisions the promotion of a positive culture of service and the advancement of health care innovations necessary to create an environment that all veterans deserve.4 To that end, the VHA can be a promising health care institution through which patient-centered initiatives can be standardized, promulgated nationally, and replicated as a model for the country and international health systems. However, it is important to note that the bureaucratic organizational structure of the VHA's national integrated system of care is based on a systemwide standardization effort.5 Therefore, more time may be required to implement organizational changes.
Transgender populations face significant social stigmatization, discrimination, and marginalization that contribute to negative patient outcomes. Consequently, this population experiences high rates of suicide, HIV/AIDS, substance use disorder, poverty, and homelessness.6 Due to the growing evidence of health disparities and negative health outcomes affecting transgender populations, the federal government has identified transgender patient care and outcomes as a major health concern and priority in the Healthy People Initiative 2020.2,7,8
In 2012, the VHA issued a directive mandating services for transgender veterans.9 Nevertheless, health care staff significantly lack the knowledge, skills, and cultural competencies that are vital in transgender care.
This article reviews the prevalence and demographics of the transgender population, social challenges, global health concerns, and public health policies. The article also examines how the doctor of nursing practice (DNP)-prepared nurse leader can provide transformational nursing leadership to facilitate culturally competent, patient-centered initiatives to improve access and services for transgender individuals in the VHA and provide a model for change in transgender population health.
Definitions
Gender is a behavioral, cultural, or psychological trait assigned by society that is associated with male or female sex. Sex denotes the biologic differences between males and females. Transgender is an umbrella term used to describe people whose gender identity or gender expression is different from that of their sex assigned at birth. Transsexualism is a subset of transgender persons who have taken steps to self-identify or transition to look like their preferred gender.
Demographics
Estimates of the prevalence of transgenderism are roughly drawn from less rigorous methods, such as the combination of parents who report transgenderism in children, the number of adults reportedly seeking clinical care (such as cross-sex or gender-affirming hormone therapy), and the number of surgical interventions reported in different countries.10 A meta-analysis of 21 studies concluded that the ratio of transsexuals (individuals who are altering or have already altered their birth sex) was predominantly 1:14,705 adult males and 1:38,461 adult females.11 Since all transgender persons do not identify as transsexual, these figures do not provide a precise estimation of the number of transgender persons worldwide.
About 700,000, or 0.3%, of the adult population in the U.S. identify themselves as transgender, and an estimated 134,300 identify as transgender veterans.6,12 The transgender population in the U.S. is estimated to be 55% white, 16% African American, 21% Hispanic, and 8% other races.13 The U.S. census data noted that the transgender population was geographically located across the nation. Transgender persons are more likely to be single, never married, divorced, and more educated but with significantly less household income.2 Data to provide an accurate reflection of the number of transgender people in the U.S. are lacking. Some transgender individuals also may identify as lesbian, gay, or bisexual, making population-based estimation even more challenging and difficult.
Transgender persons who have transitioned may not have changed their names or changed their identified sex on official Social Security records, which the Social Security Administration allows only if there is evidence that genital sexual reassignment surgery was performed.14 The number of transgender adults requesting treatment continues to rise.10
Social and Health Challenges
Transgender people face many challenges because of their gender identity. Surveys assessing the living conditions of transgender people have found that 43% to 60% report high levels of physical violence.15 By comparison, the National Intimate Partner and Sexual Violence Survey found that interpersonal violence and sexual violence were reported by lesbian and gay individuals at equal or higher levels than that reported by heterosexuals. Forty-four percent of lesbian women, 35% of heterosexual women, 29% of heterosexual men, and 26% of gay men reported experiencing rape or physical violence.16 A study in Spain reported 59% of transgender people experienced patterns of harassment, and in Canada, 34% of transgender people lived below the poverty level.17,18
In the U.S., the National Transgender Discrimination Survey of 6,450 transgender and nonconforming participants provided extensive data on challenges experienced by transgender people.6 Discrimination was frequently experienced in accessing health care. Due to transgender status, 19% were denied care, and 28% postponed care due to perceived harassment and violence within a health care setting.6 The same study also reported that as many as 41% live in extreme poverty with incomes of less than $10,000 per year reported. Twenty-six percent were physically assaulted, and 10% experienced sexual violence. More than 25% of the transgender population misused drugs or alcohol to cope with mistreatment.6
In the U.S., HIV infection rates for transgender individuals were more than 4 times (2.64%) the rate of the general population (0.6%).6 Internationally, there is a high prevalence of HIV in transgender women. The prevalence rate of HIV in U.S. transgender women was 21.74% of the estimated U.S. adult transgender population of about 700,000.19 One in 4 people living with HIV in the U.S. are women.20
Suicide attempt rates are extremely high among transgender people. A suicide rate of 22% to 43% has been reported across Europe, Canada, and the U.S.21 Depression and anxiety were commonly noted as a result of discrimination and social stigma. In the U.S., transgender persons reported high rates of depression, with 41% reporting attempted suicide compared with 1.6% of the general population.6 Access to health care services, such as mental health, psychosocial support, and stress management are critical for this vulnerable population.22
Health Policies
Since 1994, the UK has instituted legal employment protections for the transgender population. In the UK, transgender persons, including military and prisoners, have health care coverage that includes sexual reassignment surgery as part of the UK's National Health Service.23
In the U.S., the federal policy of "Don't Ask, Don't Tell" barring transgender persons from serving openly in the military was repealed in June 2016. This policy historically has had a silencing effect on perpetuating institutionalized biases.24 This remains problematic even after veterans have transitioned from military service to the VA for civilian care.
Between 2006 and 2013, the reported prevalence and incidence of transgender-related diagnoses in the VA have steadily increased with 40% of new diagnoses occurring since 2011.25 In fiscal year 2013, there were 32.9 per 100,000 veterans with transgender-related diagnoses.25 Health care staff, in particular health care providers (HCPs), can play a critical role in reducing health disparities and unequal treatment.26
With the passage of the U.S. Affordable Care Act (ACA), health insurance coverage for transgender persons is now guaranteed by law, and health disparities within the transgender population can begin to be properly addressed. The ACA offers the ability to purchase health insurance, possibly qualify for Medicaid, or obtain subsidies to purchase health insurance. Insurance coverage is accessible without regard to discrimination or preexisting conditions.27 As of May 2014, the Medicare program covered medically necessary hormone therapy and sex reassignment surgery.13 While VA benefits cover hormone therapy for transgender veterans, sex reassignment surgery is not currently a covered benefit.28 The ACA now increases access to primary care, preventative care, mental health services, and community health programs not previously available in the transgender community.
Healthy People 2020 Goals
One of the Healthy People 2020 stated goals is to improve the health and wellness of transgender people.29 The objective is to increase the number of population-based data collection systems used to monitor transgender people from the baseline of 2 to a total of 4 by 2020. The data systems would be assigned to collect relevant data, such as mental health; HIV status; illicit drug, alcohol, and tobacco use; cervical and breast cancer screening; health insurance coverage; and access to health care.
Health Care Staff Readiness
Transgender persons face health care challenges with major health disparities due to their gender identity. Transgender persons as a defined population are not well understood by HCPs. In a survey, 50% of transgender respondents reported that they had to teach their medical provider about transgender care.6 Negative perceptions of transgender persons are well established and have contribute to the poor health care access and services that transgender persons receive. Transgender persons are often denied access to care, denied visitation rights, and are hesitant to share information for fear of bureaucratic exclusion or isolation.
There is a lack of evidence-based studies to guide care and help HCPs gain greater understanding of this population's unique needs.30 Additionally, a significant lack of knowledge, skills, cultural competence, and awareness exist in providing transgender care. Research on nursing attitudes concerning transgender care consistently found negative attitudes, and physicians also frequently reported witnessing derogatory comments and discriminatory care from colleagues.31,32 The study by Carabez and colleagues found that practicing nurses rarely received the proper education or training in transgender health issues, and many were unaware of the needs of this population.33 In addition, many HCPs were uncomfortable working with transgender patients. Physicians also expressed knowledge deficits on gender identity disorders due to a lack of training and ethical concerns about their roles in providing gender-transitioning treatment.26
Although the VHA directive states that transgender services and treatment should be standardized, the VHA has not approved, defined, or endorsed specific standards of care or clinical guidelines within the organization for transgender care, further heightening HCP concerns.9 The clinical practice guidelines available for addressing preventive care for transgender patients are primarily based on consensus of expert opinion.34 Expert opinion has produced the Standards of Care (SOC) for the Health of Transsexual, Transgender, and Gender Nonconforming People, published by the World Professional Association for Transgender Health (WPATH) and cited by the IOM as the major clinical practice guidelines for providing care to transgender individuals.2 Transgender care at the VHA is guided by the WPATH standards of care.35
The VHA has created national educational programs and policies with targeted goals to provide uniform, culturally competent, patient-centered care. Online transgender health presentations are available, and at least 15 VHA facilities have transgender support groups.30 While the VHA supports a patient-centered philosophy for transgender patient care, many facilities do not currently have organizational initiatives that enhance clinical preparation of HCPs or have sufficiently modified the environment to better accommodate the health care needs of transgender veterans.
DNP Preparation
The DNP terminal degree provides nurses with doctoral-level training in organizational and systems leadership, leading quality improvement, and implementing systemwide initiatives by using scientific findings to drive processes that improve quality of care for a changing patient population.36 Preparation in research analysis of evidence-based interventions also is essential to evaluating practice patterns, patient outcomes, and systems of care that can identify gaps in practice. Training in health care policy and advocacy, information systems, patient care technology, and population health also is provided so that DNPs are competent to develop system strategies to transform health care through clinical prevention and health promotion.
QSEN Framework
In keeping with the IOM's Future of Nursing initiative recommendations that graduate nurses be prepared as leaders in education, practice, administration, and research, there is an increasing focus on providing graduate-level nursing education and training to ensure quality and efficiency of health outcomes.37 The Quality and Safety Education in Nursing (QSEN) project, initiated at the RWJF by Linda Cronenwett, PhD, RN, identifies a framework for knowledge, skills, and attitudes that defines the competencies that nurses need to deliver effective care to improve quality and safety within health care systems.38 These core competencies include quality improvement, safety, teamwork and collaboration, patient-centered care, evidence-based practice, and informatics. The RWJF and the American Association of Colleges of Nursing later expanded the project initiative to prepare nursing faculty to teach the QSEN competencies in graduate nursing programs.36
The DNP nurse leader is ideally suited to manage this project by applying competencies from the QSEN framework. Using open communication and mutual respect, the nurse leader is poised to effectively develop interprofessional teams to collaborate and initiate transformational changes that improve quality and patient-centered care delivered within the health care organization.
Public Health Resources
Public health resources addressing transgender patient care advocacy, public policy, community education, standards of care, cultural competency, mental health, hormone therapy, surgical interventions, reproductive health, primary care, preventative care, and research are available. For example, WPATH is an international multidisciplinary organization that has published comprehensive SOC for transgender, transsexual, and gender-nonconforming people. The seventh version of the SOC contains evidence-based guidelines for treatment.39 Additional online resources for transgender health are available from the CDC, the Center of Excellence for Transgender Health at the University of California, San Francisco; Department of Family and Community Medicine; and the National Center for Transgender Equality.13,40,41
Patient-Centered Transgender Care
The QSEN framework outlines competencies that provide applicable solutions that help prepare organizations to deliver culturally competent, patient-centered transgender care. The first step to creating patient-centered transgender care is to "analyze factors that create barriers to patient-centered care."42 The magnitude of the barriers to providing patient-centered transgender care also must be identified and understood. An assessment of individual values, beliefs, and attitudes can help to identify cultural characteristics and eliminate stereotypes that impact health practices.43
The nurse leader should solicit support from stakeholders to assess barriers to providing patient-centered transgender care at the system level. Stakeholders would include staff directly involved in patient care, such as physicians, nurse practitioners, physician assistants, registered nurses, nurse managers, nurse educators, licensed practical nurses, medical support assistants, psychologists, dieticians, and social workers. Other ancillary stakeholders with an interest in creating a patient-centered environment with positive patient outcomes include the executive leadership team of the organization, which consists of the chief of staff, director, administrative officers, and nurse executive.
The nurse leader should consult with experts in transgender care and present evidence-based research showing how deficits in staff knowledge, skills, and cultural competence negatively impact the quality of care provided to transgender persons. National data on the consequential health disparities and negative impacts on patient outcomes also should be discussed and presented to all stakeholders. The nurse leader in collaboration with the VA Office of Research and Development is ideally suited to obtain institutional review board approval of a proposal to conduct a needs assessment survey of health care staff barriers to providing patient-centered transgender care. Thereafter, the nurse leader would analyze, extract, and synthesize the data and evaluate the resources and technology available to translate this research knowledge into a clinical practice setting at the system level.44
The second solution uses the results of the survey to develop staff competency training within the organization. The nurse leader can facilitate collaboration and team building to develop practice guidelines and SOC. Competency training will prepare the staff to assist in developing strategies to improve the quality of care for transgender persons. Educationconcerning existing evidence-based clinical guidelines and SOC as well as anecdotal evidence of the needs of transgender patients should be included in competency training.45 One approach to competency training would be to trainintegrated multidisciplinary teams with expertise in transgender care to promote wellness and disease prevention.9 The nurse leader should collaborate with multiple disciplines to facilitate the development of interdisciplinary teams from nursing, medicine, social work, pharmacy, primary care, mental health, women's health, and endocrinology to participate in the Specialty Care Access Network Extension of Community Healthcare outcomes (SCAN-ECHO) training. Training can be offered by videoconferencing over several months and provides cost-effective, efficient training of providers in patient-centered transgender care.46,47 After the SCAN-ECHO program is completed, trained nursing experts could then develop a cultural sensitivity training program for nursing organizations to be offered to educate health care staff on an annual basis.
The third solution addresses the QSEN competency to "Analyze institutional features of the facilities that support or pose barriers to patient-centered care."42 Many veterans do not perceive VA environments as welcoming. In a study by Sherman and colleagues, less than one-third of veterans believed the VA environment was welcoming to sexual or gender minorities, and sexual orientation or gender identity was disclosed by only about 25% of veterans.48 Many veterans in this study felt uncomfortable disclosing their gender or sexual orientation. The majority felt that providers should not routinely ask about sexual orientation or gender identity, and 24% said they were very or somewhat uncomfortable discussing the issue. In another study, 202 VA providers were asked if they viewed the VA as welcoming, and 32% said the VA was somewhat or very unwelcoming.48
The nurse leader is trained in the essentials of health care policy advocacy, which is central to nursing practice.49 Nursing as a profession values social justice and equality, which are linked to fewer health disparities and more stable health indicators.50 Therefore, nursing can ideally provide organizational leaders by developing a culture wherein stable, patient-centered relationships can develop and thrive.
Organizational Culture
Strategies must be deployed to create an organizational culture that is welcoming, respectful, and supportive of transgender patients and family preferences. VA should develop support groups for transgender veterans in VA facilities. Support groups are helpful in diminishing stress, improving self-esteem, building confidence, and improving social relationships.51 Additionally, VA should develop community-based partnerships with other organizations that already provide institutional care and support from HCPs who support transgender persons' right to self-determination.52 These partnerships can foster environmental influences over time and lead to the development of trusting relationships between transgender veterans and the VA organization.
Another community partnership of importance for the nurse leader to develop is an alliance with local universities to train nursing students in cultural competencies in transgender care at VA facilities. The U.S. population continues to diversify in race and ethnicity and cultural influences; therefore, nurses must be prepared in cultural competencies in order to provide quality care that reduces health disparities.53
Under federal law, the VHA has a data sharing agreement with the DoD. Despite the repeal of the "Don't Ask, Don't Tell" federal law, which cleared the way for transgender persons to openly serve in the military, many transgender persons may remain fearful of reprisals, such as judgment, denial of care, or loss of benefits if gender identity is disclosed.54 Given the bureaucratic structure of the VHA, the implementation of cultural changes at the system level will require a collaborative effort between multidisciplinary teams and community partnerships to transform the VA environment over time. The authors believe that on this issue, external forces must guide and lead changes within the VA system in order to develop sustainable and trusting relationships with transgender veterans.
The fourth solution is implementation of policies that "empower patients or families in all aspects of the health care process."42 Again, the nurse leader is trained and prepared to advocate for a policy that implements a Patient Bill of Rights that explicitly guarantees health care and prohibits discrimination of gender-minority veterans. This change would foster trust and confidence from transgender individuals. A study found that 83% of providers and 83% of lesbian, gay, bisexual, and transgender veterans believe that this policy change would make the VHA environment more welcoming.48 Providing transgender-affirming materials and language on standard forms also would eliminate barriers, promote patient-centered care, and empower transgender patients by creating an environment that is more inclusive of everyone.48
Conclusion
The nurse leader is well positioned to implement the QSEN framework to integrate research, practice, and policy to create a more inclusive, patient-centered health care system for transgender veterans. By using the essential principles of doctoral education for advanced nursing practice, the nurse leader is prepared to advocate for changing the organization at the systems level. The nurse leader also is equipped to direct the implementation of patient-centered transgender care initiatives by ensuring the integration of the nursing organization as a partner in strategic planning as well as the development of solutions.
The VHA Blueprint of Excellence envisions organization and collaboration to promote new relationships that serve and benefit veterans. The DNP preparation allows the nurse leader to demonstrate the ability to collaborate with VHA stakeholders and develop alliances within and outside the organization by advocating for policy changes that will be transformational in improving health care delivery and patient outcomes to vulnerable transgender veteran populations. The IOM has tasked nurse executives with creating a health care infrastructure of doctorally prepared nurses to provide patient care that is increasingly growing more complex. With an increasing number of veterans using services, VHA has prioritized an expansion in the number of doctorally prepared nurses.55
As the largest integrated health care system in the U.S., the VHA provides an ideal setting for initiating these organizational changes as a result of having developed an integrated infrastructure to collect evidence-based data at the regional (network) and state facilities and make comparisons with national benchmarks. Therefore, changes are less difficult to disseminate throughout the hierarchy of the VHA. Consequently, the VHA has been a leader in the U.S. for equity in the health care arena and provides a model for international health care systems. Finally, these changes address an urgent need to reduce health disparities, morbidity, and mortality by improving quality care and health care delivery to a vulnerable transgender population.
Patient-centered care is of fundamental importance when caring for the transgender population due to the well-established history of social stigma and systemic discrimination. Therefore, nursing education is mandated to equip graduates with culturally competent patient-centered care skills.1 In 2009, the Institute of Medicine (IOM) in partnership with the Robert Wood Johnson Foundation (RWJF) launched The Future of Nursing initiative, which outlined the major role nursing should play in transforming the health care system to meet the health care needs of diverse U.S. populations.
The initiative produced a blueprint of action-focused institutional recommendations at the local, state, and national levels that would facilitate the reforms necessary to transform the U.S. health care system. One of the recommendations of the IOM report was to increase opportunities for nurses to manage and lead collaborative efforts with physicians and other health care team members in the areas of systems redesign and research, to improve practice environments and health systems.2
The VHA is the largest integrated health care system in the U.S., serving more than 8.76 million veterans at more than 1,700 facilities. The VHA has an organizational structure that uses centralized control in Washington, DC, and branches out to 18 regional networks that are divided into local facilities in 50 states, the District of Columbia, Puerto Rico, the U.S. Virgin Islands, Guam, American Samoa, and the Philippines. This type of structure is known for promoting efficient standardization of processes and procedures across an organization.3
The VHA Blueprint for Excellence envisions the promotion of a positive culture of service and the advancement of health care innovations necessary to create an environment that all veterans deserve.4 To that end, the VHA can be a promising health care institution through which patient-centered initiatives can be standardized, promulgated nationally, and replicated as a model for the country and international health systems. However, it is important to note that the bureaucratic organizational structure of the VHA's national integrated system of care is based on a systemwide standardization effort.5 Therefore, more time may be required to implement organizational changes.
Transgender populations face significant social stigmatization, discrimination, and marginalization that contribute to negative patient outcomes. Consequently, this population experiences high rates of suicide, HIV/AIDS, substance use disorder, poverty, and homelessness.6 Due to the growing evidence of health disparities and negative health outcomes affecting transgender populations, the federal government has identified transgender patient care and outcomes as a major health concern and priority in the Healthy People Initiative 2020.2,7,8
In 2012, the VHA issued a directive mandating services for transgender veterans.9 Nevertheless, health care staff significantly lack the knowledge, skills, and cultural competencies that are vital in transgender care.
This article reviews the prevalence and demographics of the transgender population, social challenges, global health concerns, and public health policies. The article also examines how the doctor of nursing practice (DNP)-prepared nurse leader can provide transformational nursing leadership to facilitate culturally competent, patient-centered initiatives to improve access and services for transgender individuals in the VHA and provide a model for change in transgender population health.
Definitions
Gender is a behavioral, cultural, or psychological trait assigned by society that is associated with male or female sex. Sex denotes the biologic differences between males and females. Transgender is an umbrella term used to describe people whose gender identity or gender expression is different from that of their sex assigned at birth. Transsexualism is a subset of transgender persons who have taken steps to self-identify or transition to look like their preferred gender.
Demographics
Estimates of the prevalence of transgenderism are roughly drawn from less rigorous methods, such as the combination of parents who report transgenderism in children, the number of adults reportedly seeking clinical care (such as cross-sex or gender-affirming hormone therapy), and the number of surgical interventions reported in different countries.10 A meta-analysis of 21 studies concluded that the ratio of transsexuals (individuals who are altering or have already altered their birth sex) was predominantly 1:14,705 adult males and 1:38,461 adult females.11 Since all transgender persons do not identify as transsexual, these figures do not provide a precise estimation of the number of transgender persons worldwide.
About 700,000, or 0.3%, of the adult population in the U.S. identify themselves as transgender, and an estimated 134,300 identify as transgender veterans.6,12 The transgender population in the U.S. is estimated to be 55% white, 16% African American, 21% Hispanic, and 8% other races.13 The U.S. census data noted that the transgender population was geographically located across the nation. Transgender persons are more likely to be single, never married, divorced, and more educated but with significantly less household income.2 Data to provide an accurate reflection of the number of transgender people in the U.S. are lacking. Some transgender individuals also may identify as lesbian, gay, or bisexual, making population-based estimation even more challenging and difficult.
Transgender persons who have transitioned may not have changed their names or changed their identified sex on official Social Security records, which the Social Security Administration allows only if there is evidence that genital sexual reassignment surgery was performed.14 The number of transgender adults requesting treatment continues to rise.10
Social and Health Challenges
Transgender people face many challenges because of their gender identity. Surveys assessing the living conditions of transgender people have found that 43% to 60% report high levels of physical violence.15 By comparison, the National Intimate Partner and Sexual Violence Survey found that interpersonal violence and sexual violence were reported by lesbian and gay individuals at equal or higher levels than that reported by heterosexuals. Forty-four percent of lesbian women, 35% of heterosexual women, 29% of heterosexual men, and 26% of gay men reported experiencing rape or physical violence.16 A study in Spain reported 59% of transgender people experienced patterns of harassment, and in Canada, 34% of transgender people lived below the poverty level.17,18
In the U.S., the National Transgender Discrimination Survey of 6,450 transgender and nonconforming participants provided extensive data on challenges experienced by transgender people.6 Discrimination was frequently experienced in accessing health care. Due to transgender status, 19% were denied care, and 28% postponed care due to perceived harassment and violence within a health care setting.6 The same study also reported that as many as 41% live in extreme poverty with incomes of less than $10,000 per year reported. Twenty-six percent were physically assaulted, and 10% experienced sexual violence. More than 25% of the transgender population misused drugs or alcohol to cope with mistreatment.6
In the U.S., HIV infection rates for transgender individuals were more than 4 times (2.64%) the rate of the general population (0.6%).6 Internationally, there is a high prevalence of HIV in transgender women. The prevalence rate of HIV in U.S. transgender women was 21.74% of the estimated U.S. adult transgender population of about 700,000.19 One in 4 people living with HIV in the U.S. are women.20
Suicide attempt rates are extremely high among transgender people. A suicide rate of 22% to 43% has been reported across Europe, Canada, and the U.S.21 Depression and anxiety were commonly noted as a result of discrimination and social stigma. In the U.S., transgender persons reported high rates of depression, with 41% reporting attempted suicide compared with 1.6% of the general population.6 Access to health care services, such as mental health, psychosocial support, and stress management are critical for this vulnerable population.22
Health Policies
Since 1994, the UK has instituted legal employment protections for the transgender population. In the UK, transgender persons, including military and prisoners, have health care coverage that includes sexual reassignment surgery as part of the UK's National Health Service.23
In the U.S., the federal policy of "Don't Ask, Don't Tell" barring transgender persons from serving openly in the military was repealed in June 2016. This policy historically has had a silencing effect on perpetuating institutionalized biases.24 This remains problematic even after veterans have transitioned from military service to the VA for civilian care.
Between 2006 and 2013, the reported prevalence and incidence of transgender-related diagnoses in the VA have steadily increased with 40% of new diagnoses occurring since 2011.25 In fiscal year 2013, there were 32.9 per 100,000 veterans with transgender-related diagnoses.25 Health care staff, in particular health care providers (HCPs), can play a critical role in reducing health disparities and unequal treatment.26
With the passage of the U.S. Affordable Care Act (ACA), health insurance coverage for transgender persons is now guaranteed by law, and health disparities within the transgender population can begin to be properly addressed. The ACA offers the ability to purchase health insurance, possibly qualify for Medicaid, or obtain subsidies to purchase health insurance. Insurance coverage is accessible without regard to discrimination or preexisting conditions.27 As of May 2014, the Medicare program covered medically necessary hormone therapy and sex reassignment surgery.13 While VA benefits cover hormone therapy for transgender veterans, sex reassignment surgery is not currently a covered benefit.28 The ACA now increases access to primary care, preventative care, mental health services, and community health programs not previously available in the transgender community.
Healthy People 2020 Goals
One of the Healthy People 2020 stated goals is to improve the health and wellness of transgender people.29 The objective is to increase the number of population-based data collection systems used to monitor transgender people from the baseline of 2 to a total of 4 by 2020. The data systems would be assigned to collect relevant data, such as mental health; HIV status; illicit drug, alcohol, and tobacco use; cervical and breast cancer screening; health insurance coverage; and access to health care.
Health Care Staff Readiness
Transgender persons face health care challenges with major health disparities due to their gender identity. Transgender persons as a defined population are not well understood by HCPs. In a survey, 50% of transgender respondents reported that they had to teach their medical provider about transgender care.6 Negative perceptions of transgender persons are well established and have contribute to the poor health care access and services that transgender persons receive. Transgender persons are often denied access to care, denied visitation rights, and are hesitant to share information for fear of bureaucratic exclusion or isolation.
There is a lack of evidence-based studies to guide care and help HCPs gain greater understanding of this population's unique needs.30 Additionally, a significant lack of knowledge, skills, cultural competence, and awareness exist in providing transgender care. Research on nursing attitudes concerning transgender care consistently found negative attitudes, and physicians also frequently reported witnessing derogatory comments and discriminatory care from colleagues.31,32 The study by Carabez and colleagues found that practicing nurses rarely received the proper education or training in transgender health issues, and many were unaware of the needs of this population.33 In addition, many HCPs were uncomfortable working with transgender patients. Physicians also expressed knowledge deficits on gender identity disorders due to a lack of training and ethical concerns about their roles in providing gender-transitioning treatment.26
Although the VHA directive states that transgender services and treatment should be standardized, the VHA has not approved, defined, or endorsed specific standards of care or clinical guidelines within the organization for transgender care, further heightening HCP concerns.9 The clinical practice guidelines available for addressing preventive care for transgender patients are primarily based on consensus of expert opinion.34 Expert opinion has produced the Standards of Care (SOC) for the Health of Transsexual, Transgender, and Gender Nonconforming People, published by the World Professional Association for Transgender Health (WPATH) and cited by the IOM as the major clinical practice guidelines for providing care to transgender individuals.2 Transgender care at the VHA is guided by the WPATH standards of care.35
The VHA has created national educational programs and policies with targeted goals to provide uniform, culturally competent, patient-centered care. Online transgender health presentations are available, and at least 15 VHA facilities have transgender support groups.30 While the VHA supports a patient-centered philosophy for transgender patient care, many facilities do not currently have organizational initiatives that enhance clinical preparation of HCPs or have sufficiently modified the environment to better accommodate the health care needs of transgender veterans.
DNP Preparation
The DNP terminal degree provides nurses with doctoral-level training in organizational and systems leadership, leading quality improvement, and implementing systemwide initiatives by using scientific findings to drive processes that improve quality of care for a changing patient population.36 Preparation in research analysis of evidence-based interventions also is essential to evaluating practice patterns, patient outcomes, and systems of care that can identify gaps in practice. Training in health care policy and advocacy, information systems, patient care technology, and population health also is provided so that DNPs are competent to develop system strategies to transform health care through clinical prevention and health promotion.
QSEN Framework
In keeping with the IOM's Future of Nursing initiative recommendations that graduate nurses be prepared as leaders in education, practice, administration, and research, there is an increasing focus on providing graduate-level nursing education and training to ensure quality and efficiency of health outcomes.37 The Quality and Safety Education in Nursing (QSEN) project, initiated at the RWJF by Linda Cronenwett, PhD, RN, identifies a framework for knowledge, skills, and attitudes that defines the competencies that nurses need to deliver effective care to improve quality and safety within health care systems.38 These core competencies include quality improvement, safety, teamwork and collaboration, patient-centered care, evidence-based practice, and informatics. The RWJF and the American Association of Colleges of Nursing later expanded the project initiative to prepare nursing faculty to teach the QSEN competencies in graduate nursing programs.36
The DNP nurse leader is ideally suited to manage this project by applying competencies from the QSEN framework. Using open communication and mutual respect, the nurse leader is poised to effectively develop interprofessional teams to collaborate and initiate transformational changes that improve quality and patient-centered care delivered within the health care organization.
Public Health Resources
Public health resources addressing transgender patient care advocacy, public policy, community education, standards of care, cultural competency, mental health, hormone therapy, surgical interventions, reproductive health, primary care, preventative care, and research are available. For example, WPATH is an international multidisciplinary organization that has published comprehensive SOC for transgender, transsexual, and gender-nonconforming people. The seventh version of the SOC contains evidence-based guidelines for treatment.39 Additional online resources for transgender health are available from the CDC, the Center of Excellence for Transgender Health at the University of California, San Francisco; Department of Family and Community Medicine; and the National Center for Transgender Equality.13,40,41
Patient-Centered Transgender Care
The QSEN framework outlines competencies that provide applicable solutions that help prepare organizations to deliver culturally competent, patient-centered transgender care. The first step to creating patient-centered transgender care is to "analyze factors that create barriers to patient-centered care."42 The magnitude of the barriers to providing patient-centered transgender care also must be identified and understood. An assessment of individual values, beliefs, and attitudes can help to identify cultural characteristics and eliminate stereotypes that impact health practices.43
The nurse leader should solicit support from stakeholders to assess barriers to providing patient-centered transgender care at the system level. Stakeholders would include staff directly involved in patient care, such as physicians, nurse practitioners, physician assistants, registered nurses, nurse managers, nurse educators, licensed practical nurses, medical support assistants, psychologists, dieticians, and social workers. Other ancillary stakeholders with an interest in creating a patient-centered environment with positive patient outcomes include the executive leadership team of the organization, which consists of the chief of staff, director, administrative officers, and nurse executive.
The nurse leader should consult with experts in transgender care and present evidence-based research showing how deficits in staff knowledge, skills, and cultural competence negatively impact the quality of care provided to transgender persons. National data on the consequential health disparities and negative impacts on patient outcomes also should be discussed and presented to all stakeholders. The nurse leader in collaboration with the VA Office of Research and Development is ideally suited to obtain institutional review board approval of a proposal to conduct a needs assessment survey of health care staff barriers to providing patient-centered transgender care. Thereafter, the nurse leader would analyze, extract, and synthesize the data and evaluate the resources and technology available to translate this research knowledge into a clinical practice setting at the system level.44
The second solution uses the results of the survey to develop staff competency training within the organization. The nurse leader can facilitate collaboration and team building to develop practice guidelines and SOC. Competency training will prepare the staff to assist in developing strategies to improve the quality of care for transgender persons. Educationconcerning existing evidence-based clinical guidelines and SOC as well as anecdotal evidence of the needs of transgender patients should be included in competency training.45 One approach to competency training would be to trainintegrated multidisciplinary teams with expertise in transgender care to promote wellness and disease prevention.9 The nurse leader should collaborate with multiple disciplines to facilitate the development of interdisciplinary teams from nursing, medicine, social work, pharmacy, primary care, mental health, women's health, and endocrinology to participate in the Specialty Care Access Network Extension of Community Healthcare outcomes (SCAN-ECHO) training. Training can be offered by videoconferencing over several months and provides cost-effective, efficient training of providers in patient-centered transgender care.46,47 After the SCAN-ECHO program is completed, trained nursing experts could then develop a cultural sensitivity training program for nursing organizations to be offered to educate health care staff on an annual basis.
The third solution addresses the QSEN competency to "Analyze institutional features of the facilities that support or pose barriers to patient-centered care."42 Many veterans do not perceive VA environments as welcoming. In a study by Sherman and colleagues, less than one-third of veterans believed the VA environment was welcoming to sexual or gender minorities, and sexual orientation or gender identity was disclosed by only about 25% of veterans.48 Many veterans in this study felt uncomfortable disclosing their gender or sexual orientation. The majority felt that providers should not routinely ask about sexual orientation or gender identity, and 24% said they were very or somewhat uncomfortable discussing the issue. In another study, 202 VA providers were asked if they viewed the VA as welcoming, and 32% said the VA was somewhat or very unwelcoming.48
The nurse leader is trained in the essentials of health care policy advocacy, which is central to nursing practice.49 Nursing as a profession values social justice and equality, which are linked to fewer health disparities and more stable health indicators.50 Therefore, nursing can ideally provide organizational leaders by developing a culture wherein stable, patient-centered relationships can develop and thrive.
Organizational Culture
Strategies must be deployed to create an organizational culture that is welcoming, respectful, and supportive of transgender patients and family preferences. VA should develop support groups for transgender veterans in VA facilities. Support groups are helpful in diminishing stress, improving self-esteem, building confidence, and improving social relationships.51 Additionally, VA should develop community-based partnerships with other organizations that already provide institutional care and support from HCPs who support transgender persons' right to self-determination.52 These partnerships can foster environmental influences over time and lead to the development of trusting relationships between transgender veterans and the VA organization.
Another community partnership of importance for the nurse leader to develop is an alliance with local universities to train nursing students in cultural competencies in transgender care at VA facilities. The U.S. population continues to diversify in race and ethnicity and cultural influences; therefore, nurses must be prepared in cultural competencies in order to provide quality care that reduces health disparities.53
Under federal law, the VHA has a data sharing agreement with the DoD. Despite the repeal of the "Don't Ask, Don't Tell" federal law, which cleared the way for transgender persons to openly serve in the military, many transgender persons may remain fearful of reprisals, such as judgment, denial of care, or loss of benefits if gender identity is disclosed.54 Given the bureaucratic structure of the VHA, the implementation of cultural changes at the system level will require a collaborative effort between multidisciplinary teams and community partnerships to transform the VA environment over time. The authors believe that on this issue, external forces must guide and lead changes within the VA system in order to develop sustainable and trusting relationships with transgender veterans.
The fourth solution is implementation of policies that "empower patients or families in all aspects of the health care process."42 Again, the nurse leader is trained and prepared to advocate for a policy that implements a Patient Bill of Rights that explicitly guarantees health care and prohibits discrimination of gender-minority veterans. This change would foster trust and confidence from transgender individuals. A study found that 83% of providers and 83% of lesbian, gay, bisexual, and transgender veterans believe that this policy change would make the VHA environment more welcoming.48 Providing transgender-affirming materials and language on standard forms also would eliminate barriers, promote patient-centered care, and empower transgender patients by creating an environment that is more inclusive of everyone.48
Conclusion
The nurse leader is well positioned to implement the QSEN framework to integrate research, practice, and policy to create a more inclusive, patient-centered health care system for transgender veterans. By using the essential principles of doctoral education for advanced nursing practice, the nurse leader is prepared to advocate for changing the organization at the systems level. The nurse leader also is equipped to direct the implementation of patient-centered transgender care initiatives by ensuring the integration of the nursing organization as a partner in strategic planning as well as the development of solutions.
The VHA Blueprint of Excellence envisions organization and collaboration to promote new relationships that serve and benefit veterans. The DNP preparation allows the nurse leader to demonstrate the ability to collaborate with VHA stakeholders and develop alliances within and outside the organization by advocating for policy changes that will be transformational in improving health care delivery and patient outcomes to vulnerable transgender veteran populations. The IOM has tasked nurse executives with creating a health care infrastructure of doctorally prepared nurses to provide patient care that is increasingly growing more complex. With an increasing number of veterans using services, VHA has prioritized an expansion in the number of doctorally prepared nurses.55
As the largest integrated health care system in the U.S., the VHA provides an ideal setting for initiating these organizational changes as a result of having developed an integrated infrastructure to collect evidence-based data at the regional (network) and state facilities and make comparisons with national benchmarks. Therefore, changes are less difficult to disseminate throughout the hierarchy of the VHA. Consequently, the VHA has been a leader in the U.S. for equity in the health care arena and provides a model for international health care systems. Finally, these changes address an urgent need to reduce health disparities, morbidity, and mortality by improving quality care and health care delivery to a vulnerable transgender population.
1. Greiner AC, Knebel E, eds. Health Professions Education: A Bridge to Quality. Washington, DC: National Academies Press; 2003.
2. Institute of Medicine. Bisexual, and Transgender People: Building a Foundation for Better Understanding. Washington, DC: National Academy of Sciences; 2011.
3. Mintzberg H. The structuring of organizations: a synthesis of the research. https://papers.ssrn.com/sol3/papers.cfm?abstract_id=1496182 1979. Posted November 4, 2009. Accessed November 30, 2016.
4. U.S. Department of Veterans Affairs. VHA blue print for excellence. https://www.va.gov/health/docs/VHA_Blueprint_for_Excellence.pdf. Published September 21, 2014. Accessed November 30, 2016.
5. Morgan RO, Teal CR, Reddy SG, Ford ME, Ashton CM. Measurement in Veterans Affairs Health Services Research: veterans as a special population. Health Serv Res. 2005;40(5, part 2):1573-1583.
6. Grant JM, Mottet L, Tanis JE, Harrison J, Herman J, Keisling M. Injustice at every turn: a report of the National Transgender Discrimination Survey. http://www.thetaskforce.org/static_html/downloads /reports/reports/ntds_full.pdf. Published 2011. Accessed November 30, 2016.
7. Office of Disease Prevention and Health Promotion. Lesbian, gay, bisexual, and transgender health. http://www.healthypeople.gov/2020/topics-objec tives/topic/lesbian-gay-bisexual-and-transgender -health. Updated November 16, 2016. Accessed November 16, 2016.
8. Institute of Medicine Committee on Lesbian Gay, Bisexual, and Transgender Health Issues and Research Gaps and Opportunities. The Health of Lesbian, Gay, Bisexual, and Transgender People: Building a Foundation for Better Understanding. Washington, DC: National Academy of Sciences; 2011.
9. U.S. Department of Veterans Affairs. VHA Directive 2013-003: Providing Health Care for Transgender and Intersex Veterans. Washington, DC: U.S. Department of Veterans Affairs; 2013.
10. Zucker KJ, Lawrence AA. Epidemiology of gender identity disorder: recommendations for the Standards of Care of the World Professional Association for Transgender Health. Int J Transgenderism. 2009;11(1):8-18.
11. Arcelus J, Bouman WP, Van Den Noortgate W, Claes L, Witcomb G, Fernandez-Aranda F. Systematic review and meta-analysis of prevalence studies in transsexualism. Eur Psychiatry. 2015;30(6):807-815.
12. Gates GJ, Herman JL. Transgender military service in the United States. http://williamsinstitute.law.ucla.edu/wp-content/uploads/Transgender-Military -Service-May-2014.pdf. Published May 2014. Accessed November 30, 2016.
13. Flores AR, Brown TNT, and Herman JL. Race and ethnicity of adults who identify as transgender in the United States. http://williamsinstitute.law.ucla .edu/wp-content/uploads/Race-and-Ethnicity-of -Transgender-Identified-Adults-in-the-US.pdf. Published October 2016. Accessed December 13, 2016.
14. Harris BC. Likely Transgender individuals in US federal administrative records and the 2010 census. https://www.census.gov/srd/carra/15_03_Likely_Transgender_Individuals_in_ARs_and_2010Census.pdf. Published May 4, 2015. Accessed November 30, 2016.
15. Kenagy GP, Bostwick WB. Health and social service needs of transgender people in Chicago. Int J Transgenderism. 2005;8(2-3):57-66.
16. Centers for Disease Control and Prevention. National intimate partner and sexual violence survey, 2010 summary report. https://www.cdc.gov/viole nceprevention/pdf/nisvs_report2010-a.pdf. Published November 2011. Accessed December 12, 2016.
17. Bauer GR, Travers R, Scanlon K, Coleman TA. High heterogeneity of HIV-related sexual risk among transgender people in Ontario, Canada: a province-wide respondent-driven sampling survey. BMC Public Health. 2012;12(1):292-291.
18. Devis-Devis J, Pereira-Garcia S, Valencia-Peris A, Fuentes-Miguel J, López-Cañada E, Pérez-Samaniego V. Harassment patterns and risk profile in Spanish trans persons. J Homosex. 2016. [Epub ahead of print.]
19. Gates GJ. How many people are lesbian, gay, bisexual, and transgender? http://williamsinstitute.law.ucla.edu/wp-content/uploads/Gates-How-Many -People-LGBT-Apr-2011.pdf. Published April 2011. Accessed December 1, 2016.
20. Center for Disease Control and Prevention. HIV Among Women. http://www.cdc.gov/hiv/group/gender/women/index.html. Accessed December 10, 2016.
21. Bauer GR, Scheim AI, Pyne J, Travers R, Hammond R. Intervenable factors associated with suicide risk in transgender persons: a respondent driven sampling study in Ontario, Canada. BMC Public Health. 2015;15(1):525.
22. McCann E. People who are transgender: mental health concerns. J Psychiatr Ment Health Nurs. 2015;22(1):76-81.
23. Green R. Transsexual legal rights in the United States and United Kingdom: employment, medical treatment, and civil status. Arch Sex Behav. 2010;39(1):153-160.
24. Sharpe VA, Uchendu US. Ensuring appropriate care for LGBT veterans in the Veterans Health Administration. Hastings Cent Rep. 2014;44(suppl 4):S53-S55.
25. Kauth MR, Shipherd JC, Lindsay J, Blosnich JR, Brown GR, Jones KT. Access to care for transgender veterans in the Veterans Health Administration: 2006-2013. Am J Public Health. 2014;104(suppl 4):S532-S534.
26. Snelgrove JW, Jasudavisius AM, Rowe BW, Head EM, Bauer GR. "Completely out-at-sea" with "two-gender medicine": a qualitative analysis of physician-side barriers to providing healthcare for transgender patients. BMC Health Serv Res. 2012;12(1):110.
27. U.S. Department of Health and Human Services. Key features of the affordable care act. http://www .hhs.gov/healthcare/facts-and-features/key-features -of-aca/index.html. Last reviewed November 18, 2014. Accessed December 1, 2016.
28. U.S. Department of Veterans Affairs. Federal benefits for veterans, dependents, and survivors. https://www.va.gov/opa/publications/benefits_book/Chapter_1_Health_Care_Benefits.asp. Accessed December 1, 2016.
29. HealthyPeople.gov. Lesbian, gay, bisexual, and transgender health. https://www.healthypeople.gov/2020/topics-objectives/topic/lesbian-gay-bi sexual-and-transgender-health. Updated December 1, 2016. Accessed December 1, 2016.
30. Lutwak N, Byne W, Erickson-Schroth L, et al. Transgender veterans are inadequately understood by health care providers. Mil Med. 2014;179(5):483-485.
31. Dorsen C. An integrative review of nurse attitudes towards lesbian, gay, bisexual, and transgender patients. Can J Nurs Res. 2012;44(3):18-43.
32. Eliason MJ, Dibble SL, Robertson PA. Lesbian, gay, bisexual, and transgender (LGBT) physicians' experiences in the workplace. J Homosex. 2011;58(10):1355-1371.
33. Carabez R, Pellegrini M, Mankovitz A, Eliason M, Ciano M, Scott M. "Never in All My Years...": Nurses' education about LGBT health. J Prof Nurs. 2015;31(4):323-329
34. Buchholz L. Transgender care moves into the mainstream. JAMA. 2015;314(17):1785-1787.
35. VA Boston Healthcare System. Patient Care Memorandum-11-046-LM. Management of transgender veteran patients. http://www.boston.va.gov/services/images/lgbt_patient_care_memo_transgender_care.pdf. Published May 2011. Accessed December 1, 2016.
36. Cronenwett L, Sherwood G, Pohl J, et al. Quality and safety education for advanced nursing practice. Nurs Outlook. 2009;57(6):338-348.
37. Institute of Medicine. Committee on the Robert Wood Johnson Foundation Initiative on the Future of Nursing. The Future of Nursing: Leading Change, Advancing Health. Washington, DC: National Academies Press; 2011.
38. Smith EL, Cronenwett L, Sherwood G. Current assessments of quality and safety education in nursing. Nurs Outlook. 2007;55(3):132-137.
39. World Professional Association for Transgender Health (WPATH).The standards of care. http://www.wpath.org/site_page.cfm?pk_association _webpage_menu=1351&pk_association_web page=4655. Accessed December 1, 2016.
40. University of California San Francisco Department of Family and Community Medicine. Center of Excellence for Transgender Health. http://www.tran shealth.ucsf.edu/trans?page=home-00-00 Accessed December 1, 2016.
41. Center for Disease Control and Prevention. Lesbian, gay, bisexual and transgender health. http://www.cdc.gov/lgbthealth/transgender.htm. Accessed December 1, 2016.
42. American Association of Colleges of Nursing. QSEN education consortium: graduate-level QSEN competencies, knowledge, skills and attitudes. http://www.aacn.nche.edu/faculty/qsen/competen cies.pdf. Accessed December 1, 2016.
43. Andrews MM, Boyle JS. Transcultural Concepts in Nursing Care. Philadelphia, PA: Lippincott Williams & Wilkins; 2008.
44. Moran KJ, Burson R, Conrad D. The Doctor of Nursing Practice Scholarly Project: A Framework for Success. Burlington, MA: Jones & Bartlett; 2013.
45. Hanssmann C, Morrison D, Russian E, Shiu-Thornton S, Bowen D. A community-based program evaluation of community competency trainings. J Assoc Nurses AIDS Care.
46. Knapp H, Fletcher M, Taylor A, Chan K, Goetz MB. No clinic left behind: providing cost-effective in-services via distance learning. J Healthc Qual. 2011;33(5):17-24.
47. Kauth MR, Shipherd JC, Lindsay JA, Kirsh S, Knapp H, Matza L. Teleconsultation and training of VHA providers on transgender care: implementation of a multisite hub system. Telemed J E Health. 2015;21(12):1012-1018.
48. Sherman MD, Kauth MR, Ridener L, Shipherd JC, Bratkovich K, Beaulieu G. An empirical investigation of challenges and recommendations for welcoming sexual and gender minority veterans into VA care. Prof Psychol: Res Pract. 2014;45(6):433-442.
49. American Association of Colleges of Nursing. The essentials of doctoral education for advanced nursing practice. http://www.aacn.nche.edu/pub lications/position/DNPEssentials.pdf. Published October 2006. Accessed December 1, 2016.
50. Boutain DM. Social justice as a framework for professional nursing. J Nurs Educ. 2005;44(9):404-408.
51. Poteat T, German D, Kerrigan D. Managing uncertainty: a grounded theory of stigma in transgender health care encounters. Soc Sci Med. 2013;84:22-29.
52. Thornhill L, Klein P. Creating environments of care with transgender communities. J Assoc Nurs AIDS Care. 2010;21(3):230-239.
53. Collins J. Nursing cultural competencies: Improving patient care quality and satisfaction. Ohio Nurses Rev. 2015;90(1):10-11.
54. Sherman MD, Kauth MR, Shipherd JC, Street RL Jr. Communication between VA providers and sexual and gender minority veterans: a pilot study. Psychol Serv. 2014;11(2):235-242.
55. Cowan L, Fasoli DR, Hagle ME, et al. Creating an infrastructure to advance nursing practice and care for veterans. Nurse Leader. 2013;11(5):33-36.
1. Greiner AC, Knebel E, eds. Health Professions Education: A Bridge to Quality. Washington, DC: National Academies Press; 2003.
2. Institute of Medicine. Bisexual, and Transgender People: Building a Foundation for Better Understanding. Washington, DC: National Academy of Sciences; 2011.
3. Mintzberg H. The structuring of organizations: a synthesis of the research. https://papers.ssrn.com/sol3/papers.cfm?abstract_id=1496182 1979. Posted November 4, 2009. Accessed November 30, 2016.
4. U.S. Department of Veterans Affairs. VHA blue print for excellence. https://www.va.gov/health/docs/VHA_Blueprint_for_Excellence.pdf. Published September 21, 2014. Accessed November 30, 2016.
5. Morgan RO, Teal CR, Reddy SG, Ford ME, Ashton CM. Measurement in Veterans Affairs Health Services Research: veterans as a special population. Health Serv Res. 2005;40(5, part 2):1573-1583.
6. Grant JM, Mottet L, Tanis JE, Harrison J, Herman J, Keisling M. Injustice at every turn: a report of the National Transgender Discrimination Survey. http://www.thetaskforce.org/static_html/downloads /reports/reports/ntds_full.pdf. Published 2011. Accessed November 30, 2016.
7. Office of Disease Prevention and Health Promotion. Lesbian, gay, bisexual, and transgender health. http://www.healthypeople.gov/2020/topics-objec tives/topic/lesbian-gay-bisexual-and-transgender -health. Updated November 16, 2016. Accessed November 16, 2016.
8. Institute of Medicine Committee on Lesbian Gay, Bisexual, and Transgender Health Issues and Research Gaps and Opportunities. The Health of Lesbian, Gay, Bisexual, and Transgender People: Building a Foundation for Better Understanding. Washington, DC: National Academy of Sciences; 2011.
9. U.S. Department of Veterans Affairs. VHA Directive 2013-003: Providing Health Care for Transgender and Intersex Veterans. Washington, DC: U.S. Department of Veterans Affairs; 2013.
10. Zucker KJ, Lawrence AA. Epidemiology of gender identity disorder: recommendations for the Standards of Care of the World Professional Association for Transgender Health. Int J Transgenderism. 2009;11(1):8-18.
11. Arcelus J, Bouman WP, Van Den Noortgate W, Claes L, Witcomb G, Fernandez-Aranda F. Systematic review and meta-analysis of prevalence studies in transsexualism. Eur Psychiatry. 2015;30(6):807-815.
12. Gates GJ, Herman JL. Transgender military service in the United States. http://williamsinstitute.law.ucla.edu/wp-content/uploads/Transgender-Military -Service-May-2014.pdf. Published May 2014. Accessed November 30, 2016.
13. Flores AR, Brown TNT, and Herman JL. Race and ethnicity of adults who identify as transgender in the United States. http://williamsinstitute.law.ucla .edu/wp-content/uploads/Race-and-Ethnicity-of -Transgender-Identified-Adults-in-the-US.pdf. Published October 2016. Accessed December 13, 2016.
14. Harris BC. Likely Transgender individuals in US federal administrative records and the 2010 census. https://www.census.gov/srd/carra/15_03_Likely_Transgender_Individuals_in_ARs_and_2010Census.pdf. Published May 4, 2015. Accessed November 30, 2016.
15. Kenagy GP, Bostwick WB. Health and social service needs of transgender people in Chicago. Int J Transgenderism. 2005;8(2-3):57-66.
16. Centers for Disease Control and Prevention. National intimate partner and sexual violence survey, 2010 summary report. https://www.cdc.gov/viole nceprevention/pdf/nisvs_report2010-a.pdf. Published November 2011. Accessed December 12, 2016.
17. Bauer GR, Travers R, Scanlon K, Coleman TA. High heterogeneity of HIV-related sexual risk among transgender people in Ontario, Canada: a province-wide respondent-driven sampling survey. BMC Public Health. 2012;12(1):292-291.
18. Devis-Devis J, Pereira-Garcia S, Valencia-Peris A, Fuentes-Miguel J, López-Cañada E, Pérez-Samaniego V. Harassment patterns and risk profile in Spanish trans persons. J Homosex. 2016. [Epub ahead of print.]
19. Gates GJ. How many people are lesbian, gay, bisexual, and transgender? http://williamsinstitute.law.ucla.edu/wp-content/uploads/Gates-How-Many -People-LGBT-Apr-2011.pdf. Published April 2011. Accessed December 1, 2016.
20. Center for Disease Control and Prevention. HIV Among Women. http://www.cdc.gov/hiv/group/gender/women/index.html. Accessed December 10, 2016.
21. Bauer GR, Scheim AI, Pyne J, Travers R, Hammond R. Intervenable factors associated with suicide risk in transgender persons: a respondent driven sampling study in Ontario, Canada. BMC Public Health. 2015;15(1):525.
22. McCann E. People who are transgender: mental health concerns. J Psychiatr Ment Health Nurs. 2015;22(1):76-81.
23. Green R. Transsexual legal rights in the United States and United Kingdom: employment, medical treatment, and civil status. Arch Sex Behav. 2010;39(1):153-160.
24. Sharpe VA, Uchendu US. Ensuring appropriate care for LGBT veterans in the Veterans Health Administration. Hastings Cent Rep. 2014;44(suppl 4):S53-S55.
25. Kauth MR, Shipherd JC, Lindsay J, Blosnich JR, Brown GR, Jones KT. Access to care for transgender veterans in the Veterans Health Administration: 2006-2013. Am J Public Health. 2014;104(suppl 4):S532-S534.
26. Snelgrove JW, Jasudavisius AM, Rowe BW, Head EM, Bauer GR. "Completely out-at-sea" with "two-gender medicine": a qualitative analysis of physician-side barriers to providing healthcare for transgender patients. BMC Health Serv Res. 2012;12(1):110.
27. U.S. Department of Health and Human Services. Key features of the affordable care act. http://www .hhs.gov/healthcare/facts-and-features/key-features -of-aca/index.html. Last reviewed November 18, 2014. Accessed December 1, 2016.
28. U.S. Department of Veterans Affairs. Federal benefits for veterans, dependents, and survivors. https://www.va.gov/opa/publications/benefits_book/Chapter_1_Health_Care_Benefits.asp. Accessed December 1, 2016.
29. HealthyPeople.gov. Lesbian, gay, bisexual, and transgender health. https://www.healthypeople.gov/2020/topics-objectives/topic/lesbian-gay-bi sexual-and-transgender-health. Updated December 1, 2016. Accessed December 1, 2016.
30. Lutwak N, Byne W, Erickson-Schroth L, et al. Transgender veterans are inadequately understood by health care providers. Mil Med. 2014;179(5):483-485.
31. Dorsen C. An integrative review of nurse attitudes towards lesbian, gay, bisexual, and transgender patients. Can J Nurs Res. 2012;44(3):18-43.
32. Eliason MJ, Dibble SL, Robertson PA. Lesbian, gay, bisexual, and transgender (LGBT) physicians' experiences in the workplace. J Homosex. 2011;58(10):1355-1371.
33. Carabez R, Pellegrini M, Mankovitz A, Eliason M, Ciano M, Scott M. "Never in All My Years...": Nurses' education about LGBT health. J Prof Nurs. 2015;31(4):323-329
34. Buchholz L. Transgender care moves into the mainstream. JAMA. 2015;314(17):1785-1787.
35. VA Boston Healthcare System. Patient Care Memorandum-11-046-LM. Management of transgender veteran patients. http://www.boston.va.gov/services/images/lgbt_patient_care_memo_transgender_care.pdf. Published May 2011. Accessed December 1, 2016.
36. Cronenwett L, Sherwood G, Pohl J, et al. Quality and safety education for advanced nursing practice. Nurs Outlook. 2009;57(6):338-348.
37. Institute of Medicine. Committee on the Robert Wood Johnson Foundation Initiative on the Future of Nursing. The Future of Nursing: Leading Change, Advancing Health. Washington, DC: National Academies Press; 2011.
38. Smith EL, Cronenwett L, Sherwood G. Current assessments of quality and safety education in nursing. Nurs Outlook. 2007;55(3):132-137.
39. World Professional Association for Transgender Health (WPATH).The standards of care. http://www.wpath.org/site_page.cfm?pk_association _webpage_menu=1351&pk_association_web page=4655. Accessed December 1, 2016.
40. University of California San Francisco Department of Family and Community Medicine. Center of Excellence for Transgender Health. http://www.tran shealth.ucsf.edu/trans?page=home-00-00 Accessed December 1, 2016.
41. Center for Disease Control and Prevention. Lesbian, gay, bisexual and transgender health. http://www.cdc.gov/lgbthealth/transgender.htm. Accessed December 1, 2016.
42. American Association of Colleges of Nursing. QSEN education consortium: graduate-level QSEN competencies, knowledge, skills and attitudes. http://www.aacn.nche.edu/faculty/qsen/competen cies.pdf. Accessed December 1, 2016.
43. Andrews MM, Boyle JS. Transcultural Concepts in Nursing Care. Philadelphia, PA: Lippincott Williams & Wilkins; 2008.
44. Moran KJ, Burson R, Conrad D. The Doctor of Nursing Practice Scholarly Project: A Framework for Success. Burlington, MA: Jones & Bartlett; 2013.
45. Hanssmann C, Morrison D, Russian E, Shiu-Thornton S, Bowen D. A community-based program evaluation of community competency trainings. J Assoc Nurses AIDS Care.
46. Knapp H, Fletcher M, Taylor A, Chan K, Goetz MB. No clinic left behind: providing cost-effective in-services via distance learning. J Healthc Qual. 2011;33(5):17-24.
47. Kauth MR, Shipherd JC, Lindsay JA, Kirsh S, Knapp H, Matza L. Teleconsultation and training of VHA providers on transgender care: implementation of a multisite hub system. Telemed J E Health. 2015;21(12):1012-1018.
48. Sherman MD, Kauth MR, Ridener L, Shipherd JC, Bratkovich K, Beaulieu G. An empirical investigation of challenges and recommendations for welcoming sexual and gender minority veterans into VA care. Prof Psychol: Res Pract. 2014;45(6):433-442.
49. American Association of Colleges of Nursing. The essentials of doctoral education for advanced nursing practice. http://www.aacn.nche.edu/pub lications/position/DNPEssentials.pdf. Published October 2006. Accessed December 1, 2016.
50. Boutain DM. Social justice as a framework for professional nursing. J Nurs Educ. 2005;44(9):404-408.
51. Poteat T, German D, Kerrigan D. Managing uncertainty: a grounded theory of stigma in transgender health care encounters. Soc Sci Med. 2013;84:22-29.
52. Thornhill L, Klein P. Creating environments of care with transgender communities. J Assoc Nurs AIDS Care. 2010;21(3):230-239.
53. Collins J. Nursing cultural competencies: Improving patient care quality and satisfaction. Ohio Nurses Rev. 2015;90(1):10-11.
54. Sherman MD, Kauth MR, Shipherd JC, Street RL Jr. Communication between VA providers and sexual and gender minority veterans: a pilot study. Psychol Serv. 2014;11(2):235-242.
55. Cowan L, Fasoli DR, Hagle ME, et al. Creating an infrastructure to advance nursing practice and care for veterans. Nurse Leader. 2013;11(5):33-36.
IHS Gets Emergency Help
An “innovative collaboration” will bring best practices of the American College of Emergency Physicians (ACEP) to 26 emergency departments (EDs) in rural and remote Native communities. The IHS and ACEP are building on “the aggressive strategy at IHS to improve quality health care,” said IHS Principal Deputy Director Mary Smith.
Related: Dangerous Staff Shortages in the IHS
Top-level physicians and emergency medical professionals will share training resources and knowledge of telehealth and emergency care. At a work session in Winnebago, Nevada, participants covered topics, including ED leadership; responsibility, accountability, workflow, and workforce issues in rural facilities; how emergency telemedicine can help meet rural health care needs; and identifying areas for leveraging resources.
The new partnership’s plans dovetail with the Quality Framework, announced in November, which “provides a road map for quality at every level of IHS,” Smith said. The Quality Framework is the brainchild of experts from IHS, tribal partners, and HHS. Specific objectives include promoting a culture of patient safety in which all staff feel comfortable reporting medical errors, instituting processes to support learning from experiences, and reducing patient wait times for appointments.
Related: Pharmacists in the Emergency Department: Feasibility and Cost
The Quality Framework is but one product of a year in which IHS has been collaborating with tribal leaders and local health partners on a series of actions “to aggressively confront some long-standing health care service challenges.” Other actions include awarding a contract to the Joint Commission for accreditation services, technical assistance and training, and a contract with Avera Health to expand telehealth and emergency services in the Great Plains.
An “innovative collaboration” will bring best practices of the American College of Emergency Physicians (ACEP) to 26 emergency departments (EDs) in rural and remote Native communities. The IHS and ACEP are building on “the aggressive strategy at IHS to improve quality health care,” said IHS Principal Deputy Director Mary Smith.
Related: Dangerous Staff Shortages in the IHS
Top-level physicians and emergency medical professionals will share training resources and knowledge of telehealth and emergency care. At a work session in Winnebago, Nevada, participants covered topics, including ED leadership; responsibility, accountability, workflow, and workforce issues in rural facilities; how emergency telemedicine can help meet rural health care needs; and identifying areas for leveraging resources.
The new partnership’s plans dovetail with the Quality Framework, announced in November, which “provides a road map for quality at every level of IHS,” Smith said. The Quality Framework is the brainchild of experts from IHS, tribal partners, and HHS. Specific objectives include promoting a culture of patient safety in which all staff feel comfortable reporting medical errors, instituting processes to support learning from experiences, and reducing patient wait times for appointments.
Related: Pharmacists in the Emergency Department: Feasibility and Cost
The Quality Framework is but one product of a year in which IHS has been collaborating with tribal leaders and local health partners on a series of actions “to aggressively confront some long-standing health care service challenges.” Other actions include awarding a contract to the Joint Commission for accreditation services, technical assistance and training, and a contract with Avera Health to expand telehealth and emergency services in the Great Plains.
An “innovative collaboration” will bring best practices of the American College of Emergency Physicians (ACEP) to 26 emergency departments (EDs) in rural and remote Native communities. The IHS and ACEP are building on “the aggressive strategy at IHS to improve quality health care,” said IHS Principal Deputy Director Mary Smith.
Related: Dangerous Staff Shortages in the IHS
Top-level physicians and emergency medical professionals will share training resources and knowledge of telehealth and emergency care. At a work session in Winnebago, Nevada, participants covered topics, including ED leadership; responsibility, accountability, workflow, and workforce issues in rural facilities; how emergency telemedicine can help meet rural health care needs; and identifying areas for leveraging resources.
The new partnership’s plans dovetail with the Quality Framework, announced in November, which “provides a road map for quality at every level of IHS,” Smith said. The Quality Framework is the brainchild of experts from IHS, tribal partners, and HHS. Specific objectives include promoting a culture of patient safety in which all staff feel comfortable reporting medical errors, instituting processes to support learning from experiences, and reducing patient wait times for appointments.
Related: Pharmacists in the Emergency Department: Feasibility and Cost
The Quality Framework is but one product of a year in which IHS has been collaborating with tribal leaders and local health partners on a series of actions “to aggressively confront some long-standing health care service challenges.” Other actions include awarding a contract to the Joint Commission for accreditation services, technical assistance and training, and a contract with Avera Health to expand telehealth and emergency services in the Great Plains.
Oxygen May Not Help Some COPD Patients
Studies conducted in the 1970s found that patients with severely low blood oxygen levels (SpO2 ≤ 88% at rest) benefit from long-term oxygen treatment. But in nearly 50 years it hasn’t been established whether the same benefits accrue to patients with moderately low levels (SpO2 89 – 93% at rest or < 90% during a 6-minute walk test).
Related: Integrating Palliative Care in COPD Treatment
In the 7-year multicenter Long-Term Oxygen Treatment Trial (LOTT), National Heart, Lung, and Blood Institute researchers evaluated the use of oxygen in 738 patients with COPD and moderately low levels of blood oxygen. Half received long-term oxygen, the other half did not.
The researchers found no significant differences between the 2 groups in survival or time to first hospitalization. The groups also had similar rates of hospitalization and worsening COPD symptoms. Quality of life issues, such as levels of depression or anxiety, lung function, or ability to walk short distances, were also similar.
Related: Implications of the GOLD COPD Classification and Guidelines
“These results provide insight into a long-standing question about oxygen use in [these patients],” says James Kiley, PhD, director of NHLBI’s Division of Lung Diseases. “The findings also underscore the need for new treatments for COPD.”
Studies conducted in the 1970s found that patients with severely low blood oxygen levels (SpO2 ≤ 88% at rest) benefit from long-term oxygen treatment. But in nearly 50 years it hasn’t been established whether the same benefits accrue to patients with moderately low levels (SpO2 89 – 93% at rest or < 90% during a 6-minute walk test).
Related: Integrating Palliative Care in COPD Treatment
In the 7-year multicenter Long-Term Oxygen Treatment Trial (LOTT), National Heart, Lung, and Blood Institute researchers evaluated the use of oxygen in 738 patients with COPD and moderately low levels of blood oxygen. Half received long-term oxygen, the other half did not.
The researchers found no significant differences between the 2 groups in survival or time to first hospitalization. The groups also had similar rates of hospitalization and worsening COPD symptoms. Quality of life issues, such as levels of depression or anxiety, lung function, or ability to walk short distances, were also similar.
Related: Implications of the GOLD COPD Classification and Guidelines
“These results provide insight into a long-standing question about oxygen use in [these patients],” says James Kiley, PhD, director of NHLBI’s Division of Lung Diseases. “The findings also underscore the need for new treatments for COPD.”
Studies conducted in the 1970s found that patients with severely low blood oxygen levels (SpO2 ≤ 88% at rest) benefit from long-term oxygen treatment. But in nearly 50 years it hasn’t been established whether the same benefits accrue to patients with moderately low levels (SpO2 89 – 93% at rest or < 90% during a 6-minute walk test).
Related: Integrating Palliative Care in COPD Treatment
In the 7-year multicenter Long-Term Oxygen Treatment Trial (LOTT), National Heart, Lung, and Blood Institute researchers evaluated the use of oxygen in 738 patients with COPD and moderately low levels of blood oxygen. Half received long-term oxygen, the other half did not.
The researchers found no significant differences between the 2 groups in survival or time to first hospitalization. The groups also had similar rates of hospitalization and worsening COPD symptoms. Quality of life issues, such as levels of depression or anxiety, lung function, or ability to walk short distances, were also similar.
Related: Implications of the GOLD COPD Classification and Guidelines
“These results provide insight into a long-standing question about oxygen use in [these patients],” says James Kiley, PhD, director of NHLBI’s Division of Lung Diseases. “The findings also underscore the need for new treatments for COPD.”
Toxic Stress Takes a Toll on Native Children
Chronic poverty, long-term unemployment, substance abuse, and other adult problems can have drastic effects on children. Unrelenting stress—“toxic stress”—can disrupt early brain development, impair immune functioning, and set the stage for later alcoholism, depression, heart disease, diabetes, and other conditions.
Native American children are “particularly hard-hit by this health issue,” says a report in Native Health News. “Minimal parenting skills” and a lack of understanding about child development are risk factors. Moreover, parents may expect their children to be able to understand or cope with conflict or abuse—situations that are well beyond a child’s ability to process.
Related: IHS Funds Programs to Protect Native Youth from Substance Abuse
The health care delivery system in Indian Country “often falls short,” the article says. It cites a case described by Dr. Anitra Warrior, a mental health counselor with Many Nations Healing Counseling Center in Lincoln, Nebraska. She says 1 youth who was being sexually abused and who appeared suicidal was told the next appointment with a behavioral health provider was in 3 weeks.
But, like health care providers everywhere, Native health care providers are learning how to provide better care for children’s issues related to ongoing stress. In the article, Kerry Hawk Lessard, an applied medical anthropologist, executive director of Native American Lifelines, a Title V Indian Health Service Urban Indian Health program facility in Baltimore, says, “I see kids who don’t know any other way than aging out of welfare and applying for disability, because there has never been anyone in these families who have been employed. It limits their potential, their world is 1-dimensional.”
Related: IHS Campaign Focuses on Very Long, Healthy Life
Lessard’s program pairs at-risk youth with “functional, productive adults” from American Indian communities who provide positive cultural experiences and stimulate “retribalization,” Lessard says.
Warrior’s program in Nebraska targets reducing stress in children with help not typically offered by behavioral health clinics: paying for transportation, food, legal fees. “As we treat the individual, we cannot lose sight of the family or the community and the health of each.”
“When appropriate,” she adds, “cultural practices are vital components to treatment.” For instance, 1 child with a history of severe trauma would call his spirit when he experienced anxiety, she says. Using the child’s culture to deal with the anxiety proved the most effective approach. “Culture and the strength in those beliefs are essential to healing for our young relatives.”
Chronic poverty, long-term unemployment, substance abuse, and other adult problems can have drastic effects on children. Unrelenting stress—“toxic stress”—can disrupt early brain development, impair immune functioning, and set the stage for later alcoholism, depression, heart disease, diabetes, and other conditions.
Native American children are “particularly hard-hit by this health issue,” says a report in Native Health News. “Minimal parenting skills” and a lack of understanding about child development are risk factors. Moreover, parents may expect their children to be able to understand or cope with conflict or abuse—situations that are well beyond a child’s ability to process.
Related: IHS Funds Programs to Protect Native Youth from Substance Abuse
The health care delivery system in Indian Country “often falls short,” the article says. It cites a case described by Dr. Anitra Warrior, a mental health counselor with Many Nations Healing Counseling Center in Lincoln, Nebraska. She says 1 youth who was being sexually abused and who appeared suicidal was told the next appointment with a behavioral health provider was in 3 weeks.
But, like health care providers everywhere, Native health care providers are learning how to provide better care for children’s issues related to ongoing stress. In the article, Kerry Hawk Lessard, an applied medical anthropologist, executive director of Native American Lifelines, a Title V Indian Health Service Urban Indian Health program facility in Baltimore, says, “I see kids who don’t know any other way than aging out of welfare and applying for disability, because there has never been anyone in these families who have been employed. It limits their potential, their world is 1-dimensional.”
Related: IHS Campaign Focuses on Very Long, Healthy Life
Lessard’s program pairs at-risk youth with “functional, productive adults” from American Indian communities who provide positive cultural experiences and stimulate “retribalization,” Lessard says.
Warrior’s program in Nebraska targets reducing stress in children with help not typically offered by behavioral health clinics: paying for transportation, food, legal fees. “As we treat the individual, we cannot lose sight of the family or the community and the health of each.”
“When appropriate,” she adds, “cultural practices are vital components to treatment.” For instance, 1 child with a history of severe trauma would call his spirit when he experienced anxiety, she says. Using the child’s culture to deal with the anxiety proved the most effective approach. “Culture and the strength in those beliefs are essential to healing for our young relatives.”
Chronic poverty, long-term unemployment, substance abuse, and other adult problems can have drastic effects on children. Unrelenting stress—“toxic stress”—can disrupt early brain development, impair immune functioning, and set the stage for later alcoholism, depression, heart disease, diabetes, and other conditions.
Native American children are “particularly hard-hit by this health issue,” says a report in Native Health News. “Minimal parenting skills” and a lack of understanding about child development are risk factors. Moreover, parents may expect their children to be able to understand or cope with conflict or abuse—situations that are well beyond a child’s ability to process.
Related: IHS Funds Programs to Protect Native Youth from Substance Abuse
The health care delivery system in Indian Country “often falls short,” the article says. It cites a case described by Dr. Anitra Warrior, a mental health counselor with Many Nations Healing Counseling Center in Lincoln, Nebraska. She says 1 youth who was being sexually abused and who appeared suicidal was told the next appointment with a behavioral health provider was in 3 weeks.
But, like health care providers everywhere, Native health care providers are learning how to provide better care for children’s issues related to ongoing stress. In the article, Kerry Hawk Lessard, an applied medical anthropologist, executive director of Native American Lifelines, a Title V Indian Health Service Urban Indian Health program facility in Baltimore, says, “I see kids who don’t know any other way than aging out of welfare and applying for disability, because there has never been anyone in these families who have been employed. It limits their potential, their world is 1-dimensional.”
Related: IHS Campaign Focuses on Very Long, Healthy Life
Lessard’s program pairs at-risk youth with “functional, productive adults” from American Indian communities who provide positive cultural experiences and stimulate “retribalization,” Lessard says.
Warrior’s program in Nebraska targets reducing stress in children with help not typically offered by behavioral health clinics: paying for transportation, food, legal fees. “As we treat the individual, we cannot lose sight of the family or the community and the health of each.”
“When appropriate,” she adds, “cultural practices are vital components to treatment.” For instance, 1 child with a history of severe trauma would call his spirit when he experienced anxiety, she says. Using the child’s culture to deal with the anxiety proved the most effective approach. “Culture and the strength in those beliefs are essential to healing for our young relatives.”
Memory Skills Classes to Address Cognitive Concerns in Older Veterans With a History of Posttraumatic Stress Disorder
The Geriatric Research Education and Clinical Center (GRECC) Memory Disorders Clinic at the VA Puget Sound Health Care System (VAPSHCS) in Seattle, Washington, receives referrals from primary and specialty care. About a decade ago, this clinic began to see an influx of Vietnam-era veterans who presented with a variety of symptoms: not remembering where they were going when driving, forgetting why they went into another room, not remembering what their spouse told them, and feeling “out of it.” These symptoms were not associated with the loss of independence, but they were cause for concern. Family members and care providers typically corroborated the symptom description and perception of decline. Yet during workups, these veterans showed no primary medical causes for cognitive impairments and on neuropsychological evaluation demonstrated essentially normal cognition.
Memory Disorders Clinic staff largely were at a loss to know how to care for these patients. The simple reassurance, “You do not have dementia now,” seemed unsatisfactory given the patients’ ongoing concerns and the established risk factors for neurodegenerative disease.1,2 One theme emerged when talking with these veterans and their families: They all had a diagnosis of or history of treatment for posttraumatic stress disorder (PTSD).
To help these veterans, the VAPSHCS GRECC sought to address their key areas of concern related to memory. With input from veterans and their families, a quality improvement project was developed with the following goals: (1) to educate veterans and their families about PTSD and cognitive changes; (2) to build and field test a psychoeducational class to teach memory skills in this population; and (3) to inform VA staff about PTSD and cognitive change. In this article, the authors focus on how the first 2 goals were addressed and present preliminary results related to quality improvement.
Memory Skills Classes
Several strategies might promote memory skills, including printed materials for self-directed learning, individual sessions, interactive technologies, or groups. Given the patients’ reports about concentration problems, asking them to work through structured materials independently seemed unproductive. Individual clinical evaluations and cognitive interventions likely would not meet the demand or be cost-effective. Groups have long been used to treat PTSD, and Norrie and colleagues reported that at-risk adults benefited from a group psychoeducation program targeting healthy brain aging.3 At the same time, the Memory Disorders Clinic sought to distinguish itself from PTSD groups, because these groups tend to focus on treating active PTSD.
A better fit for this offering was the description of the sessions as classes. Although the focus was on promoting memory skills among those capable of learning them, the authors were mindful that some veterans might truly have prodromal dementia or acute PTSD symptoms that would require clinical management. The classes were not intended to address all these issues, and there was a plan to refer participants either before or during the class if warranted.
There was no formal evaluation of memory prior to starting the class. These classes were not developed as a research intervention and were exempt from institutional review board (IRB) approval requirements, according to prescreening by the VAPSHCS IRB and a memo from the GRECC director.
Core Components of Memory Skills
It may not be evident at first glance that PTSD or a history of PTSD influences memory. The symptom criteria for PTSD (involving reexperiencing, hyperarousal, and avoidance) might be described as “too much remembering” rather than forgetting. Yet problems with attention and concentration often occur in the setting of intrusive memories and alterations in reactivity. Research has found that older adults with PTSD have deficits of memory, especially new learning.
To appreciate these effects, it was important for participants in the memory skills classes to have some understanding of how memory works. The authors developed the Memory Model (Figure) as a visual aid and reference point to discuss the stages of new learning and how different aspects of brain activity are required for new learning and for memory to occur. This straightforward model is based on cognitive science and presented in layman’s terms. An important part of this model is the “filter” stage, which controls the information and stimuli that are available to the brain. Posttraumatic stress disorder involves involuntary emotional responses and efforts to avoid them and selects and colors the information that is processed in some situations (eg, avoidance of situations associated with trauma or dissociation of extreme memories). At other times, such as when a powerful stimulus is presented (eg, a helicopter flying close overhead), the filter may try to block out all inputs in order to preserve safety. The Memory Model also served as a visual aid during class discussions of normal cognitive aging.
Class sessions incorporated specific, measurable, attainable, realistic, and timely (SMART) goals, regular exercises based on mindfulness-based stress reduction approaches, and principles of behavioral activation.5 The SMART goals structure the sessions and permit customization of learning for participants. Class leaders record a goal for each participant and use these throughout the sessions to build rapport, develop communication, and teach memory skills.
Mindfulness-based stress reduction is an evidence-based treatment used in PTSD.6 It provides a counterpoint to the more didactic memory skills and is a method that even those with objective memory impairments can practice and apply successfully. Being in the current moment and emotional regulation are important skills to teach veterans as they learn to exert
Organization
Class sessions occurred weekly for 1 hour for a total of 8 sessions. The weekly class topics included introduction to memory; mood disorders, cognition, and cognitive disorders; barriers to effective memory: assessing readiness for change; developing a routine and becoming organized; attention and concentration; memory improvement (strategies internal and external aids); and reassessing goals.
Over the 3 years of classes reported in this article, the class sizes varied from 4 to 12 participants based on veteran interest, retention, and room size. The classes were structured so that important content areas were covered but with enough elasticity so leaders and veterans would develop a rapport and explore in greater depth the topics that resonated most for the attendees. Group participation was strongly encouraged. Veterans were expressly informed that the class was not for treatment of PTSD and that evidence-based therapies were encouraged to address PTSD especially if their symptoms flared up when compared with previous levels. The attendees also understood that they did not receive formal cognitive or memory testing but were encouraged to pursue testing if they showed significant deficits.
Preliminary Findings
From spring 2012 until spring 2015, 69 veterans agreed to participate and attended at least 1 memory skills class. Eighty-seven percent of participants (n = 60) attended 4 or more classes. The mean age (SD) was 67.3 years (4.2). All the participants were men, and the race/ethnic distribution was similar to that of the aging veteran population and very close to racial demographics for Washington state: 80% white, 14% African American, 2% Asian/Pacific Islander, 2% Native American, and 2% unknown.
Attendees were asked, but not required, to complete questionnaires before the classes began and again at completion. These questionnaires included self-assessments of cognitive strategies and compensatory methods used; an assessment of concern regarding cognition, life satisfaction, and community integration; the PTSD CheckList-Civilian Version (PCL-C); and the Geriatric Depression Scale (GDS).7,8 The questionnaire also included open response questions to providefeedback on what attendees liked about the classes and recommendations for improvements. The majority of comments for improvement focused on attendees’ desire for longer sessions and repeat offerings. Five veterans did not complete the full set of questionnaires at the beginning of the classes, and 7 did not complete the questionnaires at completion (the 2 subsets did not perfectly overlap).
At the start of the class, on average, veteran participants were experiencing mild depression and moderate symptoms of PTSD as measured by the GDS (n = 54) and the PCL-C (n = 56), respectively. Preliminary comparisons of ratings pre- and post-classes, using simple paired t tests, indicated a reduction in symptoms of depression on the GDS, improved sense of mastery over their memory symptoms, as well as improved quality of life ratings (all P < .01, no corrections). There was no evidence for a significant reduction in PTSD symptoms or report of elimination of cognitive difficulties. With the small sample and modest effects, the clinical significance of these scores cannot be determined. The authors are planning more detailed analyses on a larger set of participants, including measures of health care utilization before and after the class.
Future Directions
1. Chopra MP, Zhang H, Pless Kaiser A, et al. PTSD is a chronic, fluctuating disorder affecting the mental quality of life in older adults. Am J Geriatr Psychiatry. 2014;22(1):86-97.
2. Donovan NJ, Amariglio RE, Zoller AS, et al. Subjective cognitive concerns and neuropsychiatric predictors of progression to the early clinical stages of Alzheimer disease. Am J Geriatr Psychiatry. 2014;22(12):1642-1651.
3. Norrie LM, Diamond K, Hickie IB, Rogers NL, Fearns S, Naismith SL. Can older “at risk” adults benefit from psychoeducation targeting healthy brain aging? Int Psychogeriatr. 2011;23(3):413-424.
4. Hopko DR, Robertson SMC, Lejuez CW. Behavioral activation for anxiety disorders. Behav Anal Today. 2006;7(2):212-232.
5. Schuitevoerder S, Rosen JW, Twamley EW, et al. A meta-analysis of cognitive functioning in older adults with PTSD. J Anxiety Disord. 2013;27(6):550-558.
6. Polusny MA, Erbes CR, Thuras P, et al. Mindfulness-based stress reduction for posttraumatic stress disorder among veterans: a randomized clinical trial. JAMA. 2015;314(5):456-465.
7. Yesavage JA, Brink TL, Rose TL, et al. Development and validation of a geriatric depression screening scale: a preliminary report. J Psychiatr Res. 1982-1983;17(1):37-49.
8. Mental Illness Research, Education and Clinical Center. PTSD CheckList-Civilian Version (PCL-C). http://www.mirecc.va.gov/docs/visn6/3_PTSD _CheckList_and_Scoring.pdf Published December 2013. Accessed November 3, 2016.
9. Scott JC, Matt GE, Wrocklage KM, et al. A quantitative meta-analysis of neurocognitive functioning in posttraumatic stress disorder. Psychol Bull. 2015;141(1):105-140.
10. Wrocklage KM, Schweinsburg BC, Krystal JH, et al. Neuropsychological functioning in veterans with posttraumatic stress disorder: associations with performance validity, comorbidities, and functional outcomes. J Int Neuropsychol Soc. 2016;22(4):399-411.
11. Cook JM, O’Donnell C. Assessment and psychological treatment of posttraumatic stress disorder in older adults. J Geriatr Psychiatry Neurol. 2005;18(2):61-71.
12. Mota N, Tsai J, Kirwin PD, et al. Late-life exacerbation of PTSD symptoms in US veterans: results from the National Health and Resilience in Veterans Study. J Clin Psychiatry. 2016;77(3):348-354.
13. Yaffe K, Vittinghoff E, Lindquist K, et al. Posttraumatic stress disorder and risk of dementia among US veterans. Arch Gen Psychiatry. 2010;67(6):608-613.
The Geriatric Research Education and Clinical Center (GRECC) Memory Disorders Clinic at the VA Puget Sound Health Care System (VAPSHCS) in Seattle, Washington, receives referrals from primary and specialty care. About a decade ago, this clinic began to see an influx of Vietnam-era veterans who presented with a variety of symptoms: not remembering where they were going when driving, forgetting why they went into another room, not remembering what their spouse told them, and feeling “out of it.” These symptoms were not associated with the loss of independence, but they were cause for concern. Family members and care providers typically corroborated the symptom description and perception of decline. Yet during workups, these veterans showed no primary medical causes for cognitive impairments and on neuropsychological evaluation demonstrated essentially normal cognition.
Memory Disorders Clinic staff largely were at a loss to know how to care for these patients. The simple reassurance, “You do not have dementia now,” seemed unsatisfactory given the patients’ ongoing concerns and the established risk factors for neurodegenerative disease.1,2 One theme emerged when talking with these veterans and their families: They all had a diagnosis of or history of treatment for posttraumatic stress disorder (PTSD).
To help these veterans, the VAPSHCS GRECC sought to address their key areas of concern related to memory. With input from veterans and their families, a quality improvement project was developed with the following goals: (1) to educate veterans and their families about PTSD and cognitive changes; (2) to build and field test a psychoeducational class to teach memory skills in this population; and (3) to inform VA staff about PTSD and cognitive change. In this article, the authors focus on how the first 2 goals were addressed and present preliminary results related to quality improvement.
Memory Skills Classes
Several strategies might promote memory skills, including printed materials for self-directed learning, individual sessions, interactive technologies, or groups. Given the patients’ reports about concentration problems, asking them to work through structured materials independently seemed unproductive. Individual clinical evaluations and cognitive interventions likely would not meet the demand or be cost-effective. Groups have long been used to treat PTSD, and Norrie and colleagues reported that at-risk adults benefited from a group psychoeducation program targeting healthy brain aging.3 At the same time, the Memory Disorders Clinic sought to distinguish itself from PTSD groups, because these groups tend to focus on treating active PTSD.
A better fit for this offering was the description of the sessions as classes. Although the focus was on promoting memory skills among those capable of learning them, the authors were mindful that some veterans might truly have prodromal dementia or acute PTSD symptoms that would require clinical management. The classes were not intended to address all these issues, and there was a plan to refer participants either before or during the class if warranted.
There was no formal evaluation of memory prior to starting the class. These classes were not developed as a research intervention and were exempt from institutional review board (IRB) approval requirements, according to prescreening by the VAPSHCS IRB and a memo from the GRECC director.
Core Components of Memory Skills
It may not be evident at first glance that PTSD or a history of PTSD influences memory. The symptom criteria for PTSD (involving reexperiencing, hyperarousal, and avoidance) might be described as “too much remembering” rather than forgetting. Yet problems with attention and concentration often occur in the setting of intrusive memories and alterations in reactivity. Research has found that older adults with PTSD have deficits of memory, especially new learning.
To appreciate these effects, it was important for participants in the memory skills classes to have some understanding of how memory works. The authors developed the Memory Model (Figure) as a visual aid and reference point to discuss the stages of new learning and how different aspects of brain activity are required for new learning and for memory to occur. This straightforward model is based on cognitive science and presented in layman’s terms. An important part of this model is the “filter” stage, which controls the information and stimuli that are available to the brain. Posttraumatic stress disorder involves involuntary emotional responses and efforts to avoid them and selects and colors the information that is processed in some situations (eg, avoidance of situations associated with trauma or dissociation of extreme memories). At other times, such as when a powerful stimulus is presented (eg, a helicopter flying close overhead), the filter may try to block out all inputs in order to preserve safety. The Memory Model also served as a visual aid during class discussions of normal cognitive aging.
Class sessions incorporated specific, measurable, attainable, realistic, and timely (SMART) goals, regular exercises based on mindfulness-based stress reduction approaches, and principles of behavioral activation.5 The SMART goals structure the sessions and permit customization of learning for participants. Class leaders record a goal for each participant and use these throughout the sessions to build rapport, develop communication, and teach memory skills.
Mindfulness-based stress reduction is an evidence-based treatment used in PTSD.6 It provides a counterpoint to the more didactic memory skills and is a method that even those with objective memory impairments can practice and apply successfully. Being in the current moment and emotional regulation are important skills to teach veterans as they learn to exert
Organization
Class sessions occurred weekly for 1 hour for a total of 8 sessions. The weekly class topics included introduction to memory; mood disorders, cognition, and cognitive disorders; barriers to effective memory: assessing readiness for change; developing a routine and becoming organized; attention and concentration; memory improvement (strategies internal and external aids); and reassessing goals.
Over the 3 years of classes reported in this article, the class sizes varied from 4 to 12 participants based on veteran interest, retention, and room size. The classes were structured so that important content areas were covered but with enough elasticity so leaders and veterans would develop a rapport and explore in greater depth the topics that resonated most for the attendees. Group participation was strongly encouraged. Veterans were expressly informed that the class was not for treatment of PTSD and that evidence-based therapies were encouraged to address PTSD especially if their symptoms flared up when compared with previous levels. The attendees also understood that they did not receive formal cognitive or memory testing but were encouraged to pursue testing if they showed significant deficits.
Preliminary Findings
From spring 2012 until spring 2015, 69 veterans agreed to participate and attended at least 1 memory skills class. Eighty-seven percent of participants (n = 60) attended 4 or more classes. The mean age (SD) was 67.3 years (4.2). All the participants were men, and the race/ethnic distribution was similar to that of the aging veteran population and very close to racial demographics for Washington state: 80% white, 14% African American, 2% Asian/Pacific Islander, 2% Native American, and 2% unknown.
Attendees were asked, but not required, to complete questionnaires before the classes began and again at completion. These questionnaires included self-assessments of cognitive strategies and compensatory methods used; an assessment of concern regarding cognition, life satisfaction, and community integration; the PTSD CheckList-Civilian Version (PCL-C); and the Geriatric Depression Scale (GDS).7,8 The questionnaire also included open response questions to providefeedback on what attendees liked about the classes and recommendations for improvements. The majority of comments for improvement focused on attendees’ desire for longer sessions and repeat offerings. Five veterans did not complete the full set of questionnaires at the beginning of the classes, and 7 did not complete the questionnaires at completion (the 2 subsets did not perfectly overlap).
At the start of the class, on average, veteran participants were experiencing mild depression and moderate symptoms of PTSD as measured by the GDS (n = 54) and the PCL-C (n = 56), respectively. Preliminary comparisons of ratings pre- and post-classes, using simple paired t tests, indicated a reduction in symptoms of depression on the GDS, improved sense of mastery over their memory symptoms, as well as improved quality of life ratings (all P < .01, no corrections). There was no evidence for a significant reduction in PTSD symptoms or report of elimination of cognitive difficulties. With the small sample and modest effects, the clinical significance of these scores cannot be determined. The authors are planning more detailed analyses on a larger set of participants, including measures of health care utilization before and after the class.
Future Directions
The Geriatric Research Education and Clinical Center (GRECC) Memory Disorders Clinic at the VA Puget Sound Health Care System (VAPSHCS) in Seattle, Washington, receives referrals from primary and specialty care. About a decade ago, this clinic began to see an influx of Vietnam-era veterans who presented with a variety of symptoms: not remembering where they were going when driving, forgetting why they went into another room, not remembering what their spouse told them, and feeling “out of it.” These symptoms were not associated with the loss of independence, but they were cause for concern. Family members and care providers typically corroborated the symptom description and perception of decline. Yet during workups, these veterans showed no primary medical causes for cognitive impairments and on neuropsychological evaluation demonstrated essentially normal cognition.
Memory Disorders Clinic staff largely were at a loss to know how to care for these patients. The simple reassurance, “You do not have dementia now,” seemed unsatisfactory given the patients’ ongoing concerns and the established risk factors for neurodegenerative disease.1,2 One theme emerged when talking with these veterans and their families: They all had a diagnosis of or history of treatment for posttraumatic stress disorder (PTSD).
To help these veterans, the VAPSHCS GRECC sought to address their key areas of concern related to memory. With input from veterans and their families, a quality improvement project was developed with the following goals: (1) to educate veterans and their families about PTSD and cognitive changes; (2) to build and field test a psychoeducational class to teach memory skills in this population; and (3) to inform VA staff about PTSD and cognitive change. In this article, the authors focus on how the first 2 goals were addressed and present preliminary results related to quality improvement.
Memory Skills Classes
Several strategies might promote memory skills, including printed materials for self-directed learning, individual sessions, interactive technologies, or groups. Given the patients’ reports about concentration problems, asking them to work through structured materials independently seemed unproductive. Individual clinical evaluations and cognitive interventions likely would not meet the demand or be cost-effective. Groups have long been used to treat PTSD, and Norrie and colleagues reported that at-risk adults benefited from a group psychoeducation program targeting healthy brain aging.3 At the same time, the Memory Disorders Clinic sought to distinguish itself from PTSD groups, because these groups tend to focus on treating active PTSD.
A better fit for this offering was the description of the sessions as classes. Although the focus was on promoting memory skills among those capable of learning them, the authors were mindful that some veterans might truly have prodromal dementia or acute PTSD symptoms that would require clinical management. The classes were not intended to address all these issues, and there was a plan to refer participants either before or during the class if warranted.
There was no formal evaluation of memory prior to starting the class. These classes were not developed as a research intervention and were exempt from institutional review board (IRB) approval requirements, according to prescreening by the VAPSHCS IRB and a memo from the GRECC director.
Core Components of Memory Skills
It may not be evident at first glance that PTSD or a history of PTSD influences memory. The symptom criteria for PTSD (involving reexperiencing, hyperarousal, and avoidance) might be described as “too much remembering” rather than forgetting. Yet problems with attention and concentration often occur in the setting of intrusive memories and alterations in reactivity. Research has found that older adults with PTSD have deficits of memory, especially new learning.
To appreciate these effects, it was important for participants in the memory skills classes to have some understanding of how memory works. The authors developed the Memory Model (Figure) as a visual aid and reference point to discuss the stages of new learning and how different aspects of brain activity are required for new learning and for memory to occur. This straightforward model is based on cognitive science and presented in layman’s terms. An important part of this model is the “filter” stage, which controls the information and stimuli that are available to the brain. Posttraumatic stress disorder involves involuntary emotional responses and efforts to avoid them and selects and colors the information that is processed in some situations (eg, avoidance of situations associated with trauma or dissociation of extreme memories). At other times, such as when a powerful stimulus is presented (eg, a helicopter flying close overhead), the filter may try to block out all inputs in order to preserve safety. The Memory Model also served as a visual aid during class discussions of normal cognitive aging.
Class sessions incorporated specific, measurable, attainable, realistic, and timely (SMART) goals, regular exercises based on mindfulness-based stress reduction approaches, and principles of behavioral activation.5 The SMART goals structure the sessions and permit customization of learning for participants. Class leaders record a goal for each participant and use these throughout the sessions to build rapport, develop communication, and teach memory skills.
Mindfulness-based stress reduction is an evidence-based treatment used in PTSD.6 It provides a counterpoint to the more didactic memory skills and is a method that even those with objective memory impairments can practice and apply successfully. Being in the current moment and emotional regulation are important skills to teach veterans as they learn to exert
Organization
Class sessions occurred weekly for 1 hour for a total of 8 sessions. The weekly class topics included introduction to memory; mood disorders, cognition, and cognitive disorders; barriers to effective memory: assessing readiness for change; developing a routine and becoming organized; attention and concentration; memory improvement (strategies internal and external aids); and reassessing goals.
Over the 3 years of classes reported in this article, the class sizes varied from 4 to 12 participants based on veteran interest, retention, and room size. The classes were structured so that important content areas were covered but with enough elasticity so leaders and veterans would develop a rapport and explore in greater depth the topics that resonated most for the attendees. Group participation was strongly encouraged. Veterans were expressly informed that the class was not for treatment of PTSD and that evidence-based therapies were encouraged to address PTSD especially if their symptoms flared up when compared with previous levels. The attendees also understood that they did not receive formal cognitive or memory testing but were encouraged to pursue testing if they showed significant deficits.
Preliminary Findings
From spring 2012 until spring 2015, 69 veterans agreed to participate and attended at least 1 memory skills class. Eighty-seven percent of participants (n = 60) attended 4 or more classes. The mean age (SD) was 67.3 years (4.2). All the participants were men, and the race/ethnic distribution was similar to that of the aging veteran population and very close to racial demographics for Washington state: 80% white, 14% African American, 2% Asian/Pacific Islander, 2% Native American, and 2% unknown.
Attendees were asked, but not required, to complete questionnaires before the classes began and again at completion. These questionnaires included self-assessments of cognitive strategies and compensatory methods used; an assessment of concern regarding cognition, life satisfaction, and community integration; the PTSD CheckList-Civilian Version (PCL-C); and the Geriatric Depression Scale (GDS).7,8 The questionnaire also included open response questions to providefeedback on what attendees liked about the classes and recommendations for improvements. The majority of comments for improvement focused on attendees’ desire for longer sessions and repeat offerings. Five veterans did not complete the full set of questionnaires at the beginning of the classes, and 7 did not complete the questionnaires at completion (the 2 subsets did not perfectly overlap).
At the start of the class, on average, veteran participants were experiencing mild depression and moderate symptoms of PTSD as measured by the GDS (n = 54) and the PCL-C (n = 56), respectively. Preliminary comparisons of ratings pre- and post-classes, using simple paired t tests, indicated a reduction in symptoms of depression on the GDS, improved sense of mastery over their memory symptoms, as well as improved quality of life ratings (all P < .01, no corrections). There was no evidence for a significant reduction in PTSD symptoms or report of elimination of cognitive difficulties. With the small sample and modest effects, the clinical significance of these scores cannot be determined. The authors are planning more detailed analyses on a larger set of participants, including measures of health care utilization before and after the class.
Future Directions
1. Chopra MP, Zhang H, Pless Kaiser A, et al. PTSD is a chronic, fluctuating disorder affecting the mental quality of life in older adults. Am J Geriatr Psychiatry. 2014;22(1):86-97.
2. Donovan NJ, Amariglio RE, Zoller AS, et al. Subjective cognitive concerns and neuropsychiatric predictors of progression to the early clinical stages of Alzheimer disease. Am J Geriatr Psychiatry. 2014;22(12):1642-1651.
3. Norrie LM, Diamond K, Hickie IB, Rogers NL, Fearns S, Naismith SL. Can older “at risk” adults benefit from psychoeducation targeting healthy brain aging? Int Psychogeriatr. 2011;23(3):413-424.
4. Hopko DR, Robertson SMC, Lejuez CW. Behavioral activation for anxiety disorders. Behav Anal Today. 2006;7(2):212-232.
5. Schuitevoerder S, Rosen JW, Twamley EW, et al. A meta-analysis of cognitive functioning in older adults with PTSD. J Anxiety Disord. 2013;27(6):550-558.
6. Polusny MA, Erbes CR, Thuras P, et al. Mindfulness-based stress reduction for posttraumatic stress disorder among veterans: a randomized clinical trial. JAMA. 2015;314(5):456-465.
7. Yesavage JA, Brink TL, Rose TL, et al. Development and validation of a geriatric depression screening scale: a preliminary report. J Psychiatr Res. 1982-1983;17(1):37-49.
8. Mental Illness Research, Education and Clinical Center. PTSD CheckList-Civilian Version (PCL-C). http://www.mirecc.va.gov/docs/visn6/3_PTSD _CheckList_and_Scoring.pdf Published December 2013. Accessed November 3, 2016.
9. Scott JC, Matt GE, Wrocklage KM, et al. A quantitative meta-analysis of neurocognitive functioning in posttraumatic stress disorder. Psychol Bull. 2015;141(1):105-140.
10. Wrocklage KM, Schweinsburg BC, Krystal JH, et al. Neuropsychological functioning in veterans with posttraumatic stress disorder: associations with performance validity, comorbidities, and functional outcomes. J Int Neuropsychol Soc. 2016;22(4):399-411.
11. Cook JM, O’Donnell C. Assessment and psychological treatment of posttraumatic stress disorder in older adults. J Geriatr Psychiatry Neurol. 2005;18(2):61-71.
12. Mota N, Tsai J, Kirwin PD, et al. Late-life exacerbation of PTSD symptoms in US veterans: results from the National Health and Resilience in Veterans Study. J Clin Psychiatry. 2016;77(3):348-354.
13. Yaffe K, Vittinghoff E, Lindquist K, et al. Posttraumatic stress disorder and risk of dementia among US veterans. Arch Gen Psychiatry. 2010;67(6):608-613.
1. Chopra MP, Zhang H, Pless Kaiser A, et al. PTSD is a chronic, fluctuating disorder affecting the mental quality of life in older adults. Am J Geriatr Psychiatry. 2014;22(1):86-97.
2. Donovan NJ, Amariglio RE, Zoller AS, et al. Subjective cognitive concerns and neuropsychiatric predictors of progression to the early clinical stages of Alzheimer disease. Am J Geriatr Psychiatry. 2014;22(12):1642-1651.
3. Norrie LM, Diamond K, Hickie IB, Rogers NL, Fearns S, Naismith SL. Can older “at risk” adults benefit from psychoeducation targeting healthy brain aging? Int Psychogeriatr. 2011;23(3):413-424.
4. Hopko DR, Robertson SMC, Lejuez CW. Behavioral activation for anxiety disorders. Behav Anal Today. 2006;7(2):212-232.
5. Schuitevoerder S, Rosen JW, Twamley EW, et al. A meta-analysis of cognitive functioning in older adults with PTSD. J Anxiety Disord. 2013;27(6):550-558.
6. Polusny MA, Erbes CR, Thuras P, et al. Mindfulness-based stress reduction for posttraumatic stress disorder among veterans: a randomized clinical trial. JAMA. 2015;314(5):456-465.
7. Yesavage JA, Brink TL, Rose TL, et al. Development and validation of a geriatric depression screening scale: a preliminary report. J Psychiatr Res. 1982-1983;17(1):37-49.
8. Mental Illness Research, Education and Clinical Center. PTSD CheckList-Civilian Version (PCL-C). http://www.mirecc.va.gov/docs/visn6/3_PTSD _CheckList_and_Scoring.pdf Published December 2013. Accessed November 3, 2016.
9. Scott JC, Matt GE, Wrocklage KM, et al. A quantitative meta-analysis of neurocognitive functioning in posttraumatic stress disorder. Psychol Bull. 2015;141(1):105-140.
10. Wrocklage KM, Schweinsburg BC, Krystal JH, et al. Neuropsychological functioning in veterans with posttraumatic stress disorder: associations with performance validity, comorbidities, and functional outcomes. J Int Neuropsychol Soc. 2016;22(4):399-411.
11. Cook JM, O’Donnell C. Assessment and psychological treatment of posttraumatic stress disorder in older adults. J Geriatr Psychiatry Neurol. 2005;18(2):61-71.
12. Mota N, Tsai J, Kirwin PD, et al. Late-life exacerbation of PTSD symptoms in US veterans: results from the National Health and Resilience in Veterans Study. J Clin Psychiatry. 2016;77(3):348-354.
13. Yaffe K, Vittinghoff E, Lindquist K, et al. Posttraumatic stress disorder and risk of dementia among US veterans. Arch Gen Psychiatry. 2010;67(6):608-613.
“Where’s the Music?” Using Music Therapy for Pain Management
Staff at the Malcolm Randall VAMC (MRVAMC) outpatient pain clinic in Gainesville, Florida, found that procedures to reduce a patient’s pain could initially cause pain and anxiety. Typical nursing care plans involved measures to reduce anxiety in patients undergoing interventional procedures expected to produce pain, including identifying and reinforcing coping strategies, providing reassurance and comfort, and giving patients clear explanations slowly and calmly. The MRVAMC nursing staff therefore also advocated to add music therapy to the existing plan.
Background
As part of a quality improvement (QI) project, the authors conducted a literature search to find scientific evidence for the use of music therapy. Multiple medical databases were analyzed to find studies that included total time, dose of sedative medications, pain scores, patient experience, and willingness to repeat the same procedure in the future with use of music vs no music.1 The literature review revealed that music therapy demonstrated effectiveness in decreasing anxiety and pain, supporting relaxation, reducing sedation medication during procedures, and improving patient satisfaction.
As a result of the literature search the authors conducted a prospective, randomized controlled study to investigate music therapy as an adjunct intervention during painful procedures.
Radiofrequency Lesioning
One of the more common (and most painful) procedures performed at MRVAMC is radiofrequency lesioning (RFL).The procedure uses electrical pulses to block nerves for pain relief. Using fluoroscopy, the physician inserts a needle adjacent to the nerve that innervates the facet joint. The sensory and motor nerves are stimulated, causing a tingling or buzzing sensation and tapping. Once the tip of the needle is placed in the correct location, electrical pulses (small radiofrequency currents) are passed through the needle. A lesion is formed that temporarily interrupts the pain messages that the nerve sends to the brain. The procedure can take between30 and 60 minutes, which is longer than most pain clinic procedures.
Radiofrequency lesioning controls pain caused by degenerative disc disease, facet arthropathy, sacroiliac joints, stellate ganglions, and other nerve conditions. Due to the length of the RFL procedure, patients may experience pain and anxiety (as well as other complications, such as vasovagal responses).
The clinic staff anticipated that there would be 20 RFL procedures scheduled per week and selected it as the study procedure for 3 reasons: procedure length, high level of pain, and frequency performed.
After receiving approval from the University of Florida Institutional Review Board and VA Research and Development, the MRVAMC pain clinic initiated the study from September 2013 to April 2014. The purpose of the study was to measure the effects of music on patient’s self-reported anxiety and pain levels before and after nonsedating lumbar RFL.
Methods
Study Design
Veterans aged between 21 and 88 years who were scheduled to return for lumbar RFL and who did not require sedation were invited to participate. Sixty participants consented. The music group had 21 men and 2 women. The no-music group had 19 men and 2 women. Table 1 summarizes descriptive data. Table 2 describes the results of the comparison analysis. Patients were randomly assigned to either the music intervention group or no-music g
The study tools included the global anxiety VAS (GA-VAS) for pain and anxiety and a yes/no self-reported question, “Did music help?” for participants in the music group. Evaluation of the GA-VAS demonstrated reliability and validity and were patient friendly.2,3 Pain was recorded using a Likert scale of 0 for no pain and 10 for severe pain. Anxiety was recorded using a Likert scale of 0 for no anxiety and 4 for extreme anxiety.
Study subjects were recruited from patients who were on a maintenance lumbar RFL schedule, did not require sedation, and were willing to participate. If sedation was required, the patient was excluded from the study. Returning patients scheduled for RFL were informed about the music study and asked whether they were interested in participating. If they agreed, the study was explained in full, and informed consent was obtained prior to the day of their scheduled procedure. After obtaining informed consent, participants were asked to choose a music genre from 3 options: easy listening, jazz, or classical. Participants received a sealed envelope identifying their group (30 envelopes were created for each group) to be opened by the procedure nurse on the day of the procedure.4,5
Sixty participants consented to participate in the study. Of these 60 patients, 44 were studied. The 16 patients who did not participate had either a change in procedure or did not show for the appointment.
Data Collection
On procedure day, all participants completed the anxiety scale as well as a VAS pain scale (which is the MRVAMC standard of care), preoperatively and postprocedure. Envelopes were opened prior to going into the procedure room to prevent prior knowledge of who was assigned to the music group. Participants in the music intervention group listened to their preselected music on a portable CD player in the procedure room. The music was played softly so the patient could still hear and respond to the physicians instructions during the procedure. The no-music group received everything that the music intervention group received except for music (standard care throughout procedure, which consisted of nurse monitoring, measures to reduce fear and anxiety, and comfort measures). Procedures were performed with local anesthesia; neither group received moderate sedation.
Gender, age, and self-reported pain scores (before and after the lumber RFL procedure) were recorded in the patient’s chart and entered into the study database. Patients in both groups were queried before and after the procedure using the VAS to measure their pain and anxiety levels. Participants in the music intervention group were asked whether they felt that the music helped. They also were asked to provide feedback about their experience. Data were stored in locked filing cabinets, and all forms were de-identified.
Statistical Analysis
SAS version 9.2 (Cary, NC) was used for all analyses. Data were inspected for out-of-range values. The Fisher exact test was used to compare groups on categorical measures. An independent sample t test was used to compare groups on the age variable. Difference scores (formed by subtracting the after score from the before score) were analyzed using paired t tests. Analysis of covariance was used to test for significant group differences on the outcome variables of pain and anxiety with group as the independent variable and the preprocedure measure as the covariate. The level of significance was set at .05, and all testing was 2 sided.
Results
Of the 60 consenting patients, 44 participated in the study.Twenty-three were randomized to the music intervention and 21 to the no-music control group. Both pain and anxiety were significantly reduced (P < .0001) in the total sample (n = 44). The mean (SD) decrease in pain for all participants was 2.80 points (2.31) on a VAS of 0 to 10 and 0.86 points (0.93) decrease in anxiety. In the music intervention group, the mean decrease in pain and anxiety was 3.22 (2.66) and 1.00 (0.85), respectively. In the no-music group, the mean decrease in pain and anxiety was 2.33 (1.80) and 0.69 (1.00), respectively. The magnitude of pain decrease was larger in the music intervention group; however, the difference did not reach statistical significance.
Discussion
Although there was not a statistically significant difference in pain or anxiety reduction due to group assignment, a 2-point reduction in self-reported pain or anxiety may be considered clinically important and has been supported in older studies.6 Importantly, 87% of participants in the music intervention group reported that listening to music was helpful during the procedure (Figure 1).
Anxiety levels were not as high as expected when measured before and after the procedure, perhaps due to improvements in patient education and continuity of care (Figure 2). Since all participants were returning patients, they already were familiar with the procedure and the staff. Staff turnover rate is very low at this clinic, which may have contributed to the low anxiety rates among participants at baseline. Other contributing factors included good communication, expert technique, and teamwork.
During the study, few negative comments were noted. One participant did not hear the music due to faulty equipment setup. Another participant commented that the physician doing the procedure made negative remarks about the music the patient selected. A third participant commented that the music was too loud, and he was unable to hear the doctor’s instructions, indicating a need for guidelines.
There were many positive comments by participants in the music intervention group. Nurses reported comments such as “The music really helps”; “The music was great, but rock ‘n’ roll would be better”; and “Can I bring my own [music] next time?” Many patients returning for procedures frequently asked, “Where is the music?”
Limitations
Of the 60 consenting patients, only 44 participated, possibly lowering the power of the study to detect significant findings. During the study, the physician staff was reduced, resulting in fewer RFLs performed and causing the study to take longer to conduct and with fewer opportunities to recruit participants.
The CD players used for the study were old, and because earbuds could not be used, volume was difficult to modulate consistently. Earbuds were not used because patient participation was required during the procedure. Also, having only 3 music genres to choose from limited the participant’s choice.
Conclusion
Research supporting the use of music therapy to increase patient comfort is widely accepted and practiced.7 Music therapy is readily available, low risk, inexpensive, and does not require intense training by staff. It may reduce the need for moderate sedation and improve the overall patient experience. During the study, the MRVAMC nursing staff gained a greater appreciation of evidence-based practice; staff are more engaged in QI, based on their personal involvement in research.
Because 87% of the music therapy participants reported that music was helpful, the MRVAMC pain clinic plans to implement music therapy as a standard of care during RFL procedures and all procedure appointments. Music therapy may help reduce pain and anxiety during painful procedures. The goal is to continually increase patient satisfaction and overall procedure experience through integration of evidence-based practice.
Acknowledgments
The authors thank the study team who helped consent participants, perform the experiment, and gather and analyze data. They also acknowledge the pain clinic physicians, Dr. Egle Bavry and Dr. Heidi Goldstein, for their support throughout the study. Special thanks goes to Daniel Prince for his technical support.
1. Bechtold ML, Perez RA, Puli SR, Marshall JB. Effect of music on patients undergoing outpatient colonoscopy. World J Gastroenterol. 2006;12(45):7309-7312.
2. Miller SD, Duncan BL, Brown J, Sparks JA, Claud DA. The outcome rating scale: a preliminary study of the reliability, validity, and feasibility of a brief visual analog measure. J Brief Ther. 2003;2(2):91-100.
3. Williams VS, Morlock RJ, Feltner D. Psychometric evaluation of a visual analog scale for the assessment of anxiety. Health Qual Life Outcomes. 2010;8:57.
4. Dettori J. The random allocation process: two things you need to know. Evid Based Spine Care J. 2010;1(3):7-9.
5. Farrokhyar F, Bajammal S, Kahnamoui K, Bhandari M. Ensuring balanced groups in surgical trials. Can J Surg. 2010;53(6):418-423.
6. Hägg O, Fritzell P, Nordwall A; Swedish Lumbar Spine Study Group. The clinical importance of changes in outcome scores after treatment for chronic low back pain. Eur Spine J. 2003;12(1):12-20.
7. Sonke J. Music and the arts in health: a perspective from the United States. Music Arts Action. 2011;3(2):5-14
Staff at the Malcolm Randall VAMC (MRVAMC) outpatient pain clinic in Gainesville, Florida, found that procedures to reduce a patient’s pain could initially cause pain and anxiety. Typical nursing care plans involved measures to reduce anxiety in patients undergoing interventional procedures expected to produce pain, including identifying and reinforcing coping strategies, providing reassurance and comfort, and giving patients clear explanations slowly and calmly. The MRVAMC nursing staff therefore also advocated to add music therapy to the existing plan.
Background
As part of a quality improvement (QI) project, the authors conducted a literature search to find scientific evidence for the use of music therapy. Multiple medical databases were analyzed to find studies that included total time, dose of sedative medications, pain scores, patient experience, and willingness to repeat the same procedure in the future with use of music vs no music.1 The literature review revealed that music therapy demonstrated effectiveness in decreasing anxiety and pain, supporting relaxation, reducing sedation medication during procedures, and improving patient satisfaction.
As a result of the literature search the authors conducted a prospective, randomized controlled study to investigate music therapy as an adjunct intervention during painful procedures.
Radiofrequency Lesioning
One of the more common (and most painful) procedures performed at MRVAMC is radiofrequency lesioning (RFL).The procedure uses electrical pulses to block nerves for pain relief. Using fluoroscopy, the physician inserts a needle adjacent to the nerve that innervates the facet joint. The sensory and motor nerves are stimulated, causing a tingling or buzzing sensation and tapping. Once the tip of the needle is placed in the correct location, electrical pulses (small radiofrequency currents) are passed through the needle. A lesion is formed that temporarily interrupts the pain messages that the nerve sends to the brain. The procedure can take between30 and 60 minutes, which is longer than most pain clinic procedures.
Radiofrequency lesioning controls pain caused by degenerative disc disease, facet arthropathy, sacroiliac joints, stellate ganglions, and other nerve conditions. Due to the length of the RFL procedure, patients may experience pain and anxiety (as well as other complications, such as vasovagal responses).
The clinic staff anticipated that there would be 20 RFL procedures scheduled per week and selected it as the study procedure for 3 reasons: procedure length, high level of pain, and frequency performed.
After receiving approval from the University of Florida Institutional Review Board and VA Research and Development, the MRVAMC pain clinic initiated the study from September 2013 to April 2014. The purpose of the study was to measure the effects of music on patient’s self-reported anxiety and pain levels before and after nonsedating lumbar RFL.
Methods
Study Design
Veterans aged between 21 and 88 years who were scheduled to return for lumbar RFL and who did not require sedation were invited to participate. Sixty participants consented. The music group had 21 men and 2 women. The no-music group had 19 men and 2 women. Table 1 summarizes descriptive data. Table 2 describes the results of the comparison analysis. Patients were randomly assigned to either the music intervention group or no-music g
The study tools included the global anxiety VAS (GA-VAS) for pain and anxiety and a yes/no self-reported question, “Did music help?” for participants in the music group. Evaluation of the GA-VAS demonstrated reliability and validity and were patient friendly.2,3 Pain was recorded using a Likert scale of 0 for no pain and 10 for severe pain. Anxiety was recorded using a Likert scale of 0 for no anxiety and 4 for extreme anxiety.
Study subjects were recruited from patients who were on a maintenance lumbar RFL schedule, did not require sedation, and were willing to participate. If sedation was required, the patient was excluded from the study. Returning patients scheduled for RFL were informed about the music study and asked whether they were interested in participating. If they agreed, the study was explained in full, and informed consent was obtained prior to the day of their scheduled procedure. After obtaining informed consent, participants were asked to choose a music genre from 3 options: easy listening, jazz, or classical. Participants received a sealed envelope identifying their group (30 envelopes were created for each group) to be opened by the procedure nurse on the day of the procedure.4,5
Sixty participants consented to participate in the study. Of these 60 patients, 44 were studied. The 16 patients who did not participate had either a change in procedure or did not show for the appointment.
Data Collection
On procedure day, all participants completed the anxiety scale as well as a VAS pain scale (which is the MRVAMC standard of care), preoperatively and postprocedure. Envelopes were opened prior to going into the procedure room to prevent prior knowledge of who was assigned to the music group. Participants in the music intervention group listened to their preselected music on a portable CD player in the procedure room. The music was played softly so the patient could still hear and respond to the physicians instructions during the procedure. The no-music group received everything that the music intervention group received except for music (standard care throughout procedure, which consisted of nurse monitoring, measures to reduce fear and anxiety, and comfort measures). Procedures were performed with local anesthesia; neither group received moderate sedation.
Gender, age, and self-reported pain scores (before and after the lumber RFL procedure) were recorded in the patient’s chart and entered into the study database. Patients in both groups were queried before and after the procedure using the VAS to measure their pain and anxiety levels. Participants in the music intervention group were asked whether they felt that the music helped. They also were asked to provide feedback about their experience. Data were stored in locked filing cabinets, and all forms were de-identified.
Statistical Analysis
SAS version 9.2 (Cary, NC) was used for all analyses. Data were inspected for out-of-range values. The Fisher exact test was used to compare groups on categorical measures. An independent sample t test was used to compare groups on the age variable. Difference scores (formed by subtracting the after score from the before score) were analyzed using paired t tests. Analysis of covariance was used to test for significant group differences on the outcome variables of pain and anxiety with group as the independent variable and the preprocedure measure as the covariate. The level of significance was set at .05, and all testing was 2 sided.
Results
Of the 60 consenting patients, 44 participated in the study.Twenty-three were randomized to the music intervention and 21 to the no-music control group. Both pain and anxiety were significantly reduced (P < .0001) in the total sample (n = 44). The mean (SD) decrease in pain for all participants was 2.80 points (2.31) on a VAS of 0 to 10 and 0.86 points (0.93) decrease in anxiety. In the music intervention group, the mean decrease in pain and anxiety was 3.22 (2.66) and 1.00 (0.85), respectively. In the no-music group, the mean decrease in pain and anxiety was 2.33 (1.80) and 0.69 (1.00), respectively. The magnitude of pain decrease was larger in the music intervention group; however, the difference did not reach statistical significance.
Discussion
Although there was not a statistically significant difference in pain or anxiety reduction due to group assignment, a 2-point reduction in self-reported pain or anxiety may be considered clinically important and has been supported in older studies.6 Importantly, 87% of participants in the music intervention group reported that listening to music was helpful during the procedure (Figure 1).
Anxiety levels were not as high as expected when measured before and after the procedure, perhaps due to improvements in patient education and continuity of care (Figure 2). Since all participants were returning patients, they already were familiar with the procedure and the staff. Staff turnover rate is very low at this clinic, which may have contributed to the low anxiety rates among participants at baseline. Other contributing factors included good communication, expert technique, and teamwork.
During the study, few negative comments were noted. One participant did not hear the music due to faulty equipment setup. Another participant commented that the physician doing the procedure made negative remarks about the music the patient selected. A third participant commented that the music was too loud, and he was unable to hear the doctor’s instructions, indicating a need for guidelines.
There were many positive comments by participants in the music intervention group. Nurses reported comments such as “The music really helps”; “The music was great, but rock ‘n’ roll would be better”; and “Can I bring my own [music] next time?” Many patients returning for procedures frequently asked, “Where is the music?”
Limitations
Of the 60 consenting patients, only 44 participated, possibly lowering the power of the study to detect significant findings. During the study, the physician staff was reduced, resulting in fewer RFLs performed and causing the study to take longer to conduct and with fewer opportunities to recruit participants.
The CD players used for the study were old, and because earbuds could not be used, volume was difficult to modulate consistently. Earbuds were not used because patient participation was required during the procedure. Also, having only 3 music genres to choose from limited the participant’s choice.
Conclusion
Research supporting the use of music therapy to increase patient comfort is widely accepted and practiced.7 Music therapy is readily available, low risk, inexpensive, and does not require intense training by staff. It may reduce the need for moderate sedation and improve the overall patient experience. During the study, the MRVAMC nursing staff gained a greater appreciation of evidence-based practice; staff are more engaged in QI, based on their personal involvement in research.
Because 87% of the music therapy participants reported that music was helpful, the MRVAMC pain clinic plans to implement music therapy as a standard of care during RFL procedures and all procedure appointments. Music therapy may help reduce pain and anxiety during painful procedures. The goal is to continually increase patient satisfaction and overall procedure experience through integration of evidence-based practice.
Acknowledgments
The authors thank the study team who helped consent participants, perform the experiment, and gather and analyze data. They also acknowledge the pain clinic physicians, Dr. Egle Bavry and Dr. Heidi Goldstein, for their support throughout the study. Special thanks goes to Daniel Prince for his technical support.
Staff at the Malcolm Randall VAMC (MRVAMC) outpatient pain clinic in Gainesville, Florida, found that procedures to reduce a patient’s pain could initially cause pain and anxiety. Typical nursing care plans involved measures to reduce anxiety in patients undergoing interventional procedures expected to produce pain, including identifying and reinforcing coping strategies, providing reassurance and comfort, and giving patients clear explanations slowly and calmly. The MRVAMC nursing staff therefore also advocated to add music therapy to the existing plan.
Background
As part of a quality improvement (QI) project, the authors conducted a literature search to find scientific evidence for the use of music therapy. Multiple medical databases were analyzed to find studies that included total time, dose of sedative medications, pain scores, patient experience, and willingness to repeat the same procedure in the future with use of music vs no music.1 The literature review revealed that music therapy demonstrated effectiveness in decreasing anxiety and pain, supporting relaxation, reducing sedation medication during procedures, and improving patient satisfaction.
As a result of the literature search the authors conducted a prospective, randomized controlled study to investigate music therapy as an adjunct intervention during painful procedures.
Radiofrequency Lesioning
One of the more common (and most painful) procedures performed at MRVAMC is radiofrequency lesioning (RFL).The procedure uses electrical pulses to block nerves for pain relief. Using fluoroscopy, the physician inserts a needle adjacent to the nerve that innervates the facet joint. The sensory and motor nerves are stimulated, causing a tingling or buzzing sensation and tapping. Once the tip of the needle is placed in the correct location, electrical pulses (small radiofrequency currents) are passed through the needle. A lesion is formed that temporarily interrupts the pain messages that the nerve sends to the brain. The procedure can take between30 and 60 minutes, which is longer than most pain clinic procedures.
Radiofrequency lesioning controls pain caused by degenerative disc disease, facet arthropathy, sacroiliac joints, stellate ganglions, and other nerve conditions. Due to the length of the RFL procedure, patients may experience pain and anxiety (as well as other complications, such as vasovagal responses).
The clinic staff anticipated that there would be 20 RFL procedures scheduled per week and selected it as the study procedure for 3 reasons: procedure length, high level of pain, and frequency performed.
After receiving approval from the University of Florida Institutional Review Board and VA Research and Development, the MRVAMC pain clinic initiated the study from September 2013 to April 2014. The purpose of the study was to measure the effects of music on patient’s self-reported anxiety and pain levels before and after nonsedating lumbar RFL.
Methods
Study Design
Veterans aged between 21 and 88 years who were scheduled to return for lumbar RFL and who did not require sedation were invited to participate. Sixty participants consented. The music group had 21 men and 2 women. The no-music group had 19 men and 2 women. Table 1 summarizes descriptive data. Table 2 describes the results of the comparison analysis. Patients were randomly assigned to either the music intervention group or no-music g
The study tools included the global anxiety VAS (GA-VAS) for pain and anxiety and a yes/no self-reported question, “Did music help?” for participants in the music group. Evaluation of the GA-VAS demonstrated reliability and validity and were patient friendly.2,3 Pain was recorded using a Likert scale of 0 for no pain and 10 for severe pain. Anxiety was recorded using a Likert scale of 0 for no anxiety and 4 for extreme anxiety.
Study subjects were recruited from patients who were on a maintenance lumbar RFL schedule, did not require sedation, and were willing to participate. If sedation was required, the patient was excluded from the study. Returning patients scheduled for RFL were informed about the music study and asked whether they were interested in participating. If they agreed, the study was explained in full, and informed consent was obtained prior to the day of their scheduled procedure. After obtaining informed consent, participants were asked to choose a music genre from 3 options: easy listening, jazz, or classical. Participants received a sealed envelope identifying their group (30 envelopes were created for each group) to be opened by the procedure nurse on the day of the procedure.4,5
Sixty participants consented to participate in the study. Of these 60 patients, 44 were studied. The 16 patients who did not participate had either a change in procedure or did not show for the appointment.
Data Collection
On procedure day, all participants completed the anxiety scale as well as a VAS pain scale (which is the MRVAMC standard of care), preoperatively and postprocedure. Envelopes were opened prior to going into the procedure room to prevent prior knowledge of who was assigned to the music group. Participants in the music intervention group listened to their preselected music on a portable CD player in the procedure room. The music was played softly so the patient could still hear and respond to the physicians instructions during the procedure. The no-music group received everything that the music intervention group received except for music (standard care throughout procedure, which consisted of nurse monitoring, measures to reduce fear and anxiety, and comfort measures). Procedures were performed with local anesthesia; neither group received moderate sedation.
Gender, age, and self-reported pain scores (before and after the lumber RFL procedure) were recorded in the patient’s chart and entered into the study database. Patients in both groups were queried before and after the procedure using the VAS to measure their pain and anxiety levels. Participants in the music intervention group were asked whether they felt that the music helped. They also were asked to provide feedback about their experience. Data were stored in locked filing cabinets, and all forms were de-identified.
Statistical Analysis
SAS version 9.2 (Cary, NC) was used for all analyses. Data were inspected for out-of-range values. The Fisher exact test was used to compare groups on categorical measures. An independent sample t test was used to compare groups on the age variable. Difference scores (formed by subtracting the after score from the before score) were analyzed using paired t tests. Analysis of covariance was used to test for significant group differences on the outcome variables of pain and anxiety with group as the independent variable and the preprocedure measure as the covariate. The level of significance was set at .05, and all testing was 2 sided.
Results
Of the 60 consenting patients, 44 participated in the study.Twenty-three were randomized to the music intervention and 21 to the no-music control group. Both pain and anxiety were significantly reduced (P < .0001) in the total sample (n = 44). The mean (SD) decrease in pain for all participants was 2.80 points (2.31) on a VAS of 0 to 10 and 0.86 points (0.93) decrease in anxiety. In the music intervention group, the mean decrease in pain and anxiety was 3.22 (2.66) and 1.00 (0.85), respectively. In the no-music group, the mean decrease in pain and anxiety was 2.33 (1.80) and 0.69 (1.00), respectively. The magnitude of pain decrease was larger in the music intervention group; however, the difference did not reach statistical significance.
Discussion
Although there was not a statistically significant difference in pain or anxiety reduction due to group assignment, a 2-point reduction in self-reported pain or anxiety may be considered clinically important and has been supported in older studies.6 Importantly, 87% of participants in the music intervention group reported that listening to music was helpful during the procedure (Figure 1).
Anxiety levels were not as high as expected when measured before and after the procedure, perhaps due to improvements in patient education and continuity of care (Figure 2). Since all participants were returning patients, they already were familiar with the procedure and the staff. Staff turnover rate is very low at this clinic, which may have contributed to the low anxiety rates among participants at baseline. Other contributing factors included good communication, expert technique, and teamwork.
During the study, few negative comments were noted. One participant did not hear the music due to faulty equipment setup. Another participant commented that the physician doing the procedure made negative remarks about the music the patient selected. A third participant commented that the music was too loud, and he was unable to hear the doctor’s instructions, indicating a need for guidelines.
There were many positive comments by participants in the music intervention group. Nurses reported comments such as “The music really helps”; “The music was great, but rock ‘n’ roll would be better”; and “Can I bring my own [music] next time?” Many patients returning for procedures frequently asked, “Where is the music?”
Limitations
Of the 60 consenting patients, only 44 participated, possibly lowering the power of the study to detect significant findings. During the study, the physician staff was reduced, resulting in fewer RFLs performed and causing the study to take longer to conduct and with fewer opportunities to recruit participants.
The CD players used for the study were old, and because earbuds could not be used, volume was difficult to modulate consistently. Earbuds were not used because patient participation was required during the procedure. Also, having only 3 music genres to choose from limited the participant’s choice.
Conclusion
Research supporting the use of music therapy to increase patient comfort is widely accepted and practiced.7 Music therapy is readily available, low risk, inexpensive, and does not require intense training by staff. It may reduce the need for moderate sedation and improve the overall patient experience. During the study, the MRVAMC nursing staff gained a greater appreciation of evidence-based practice; staff are more engaged in QI, based on their personal involvement in research.
Because 87% of the music therapy participants reported that music was helpful, the MRVAMC pain clinic plans to implement music therapy as a standard of care during RFL procedures and all procedure appointments. Music therapy may help reduce pain and anxiety during painful procedures. The goal is to continually increase patient satisfaction and overall procedure experience through integration of evidence-based practice.
Acknowledgments
The authors thank the study team who helped consent participants, perform the experiment, and gather and analyze data. They also acknowledge the pain clinic physicians, Dr. Egle Bavry and Dr. Heidi Goldstein, for their support throughout the study. Special thanks goes to Daniel Prince for his technical support.
1. Bechtold ML, Perez RA, Puli SR, Marshall JB. Effect of music on patients undergoing outpatient colonoscopy. World J Gastroenterol. 2006;12(45):7309-7312.
2. Miller SD, Duncan BL, Brown J, Sparks JA, Claud DA. The outcome rating scale: a preliminary study of the reliability, validity, and feasibility of a brief visual analog measure. J Brief Ther. 2003;2(2):91-100.
3. Williams VS, Morlock RJ, Feltner D. Psychometric evaluation of a visual analog scale for the assessment of anxiety. Health Qual Life Outcomes. 2010;8:57.
4. Dettori J. The random allocation process: two things you need to know. Evid Based Spine Care J. 2010;1(3):7-9.
5. Farrokhyar F, Bajammal S, Kahnamoui K, Bhandari M. Ensuring balanced groups in surgical trials. Can J Surg. 2010;53(6):418-423.
6. Hägg O, Fritzell P, Nordwall A; Swedish Lumbar Spine Study Group. The clinical importance of changes in outcome scores after treatment for chronic low back pain. Eur Spine J. 2003;12(1):12-20.
7. Sonke J. Music and the arts in health: a perspective from the United States. Music Arts Action. 2011;3(2):5-14
1. Bechtold ML, Perez RA, Puli SR, Marshall JB. Effect of music on patients undergoing outpatient colonoscopy. World J Gastroenterol. 2006;12(45):7309-7312.
2. Miller SD, Duncan BL, Brown J, Sparks JA, Claud DA. The outcome rating scale: a preliminary study of the reliability, validity, and feasibility of a brief visual analog measure. J Brief Ther. 2003;2(2):91-100.
3. Williams VS, Morlock RJ, Feltner D. Psychometric evaluation of a visual analog scale for the assessment of anxiety. Health Qual Life Outcomes. 2010;8:57.
4. Dettori J. The random allocation process: two things you need to know. Evid Based Spine Care J. 2010;1(3):7-9.
5. Farrokhyar F, Bajammal S, Kahnamoui K, Bhandari M. Ensuring balanced groups in surgical trials. Can J Surg. 2010;53(6):418-423.
6. Hägg O, Fritzell P, Nordwall A; Swedish Lumbar Spine Study Group. The clinical importance of changes in outcome scores after treatment for chronic low back pain. Eur Spine J. 2003;12(1):12-20.
7. Sonke J. Music and the arts in health: a perspective from the United States. Music Arts Action. 2011;3(2):5-14
Neurosurgical Subspecialty Bedside Guide Improves Nursing Confidence
The VA Portland Healthcare System (VAPHCS) is a 277-bed facility that serves more than 85,000 inpatient and 880,000 outpatient visits each year from veterans in Oregon and southwestern Washington. The VAPHCS consists of a main tertiary care VAMC with an acute medical and surgical facility that includes 30 beds serving qualifying veterans. Supported surgical specialties include urology, general surgery, vascular surgery, otolaryngology, orthopedic surgery, ophthalmology, cardiothoracic surgery, transplant surgery, and neurological surgery. Neurosurgical patients account for about 12% to 13% of annual surgical patients. The VAPHCS also is partnered with Oregon Health & Science University in the training of health care professionals, such as physicians and nurses.
The expectation at the VAPHCS is that medical-surgical nurses care for 4 to 5 concurrent patients, often from different surgical services. Caring for patients with different medical and surgical needs, variable ambulatory, swallowing, and elimination functions, and different physician teams can become confusing; even within a single surgical service, postoperative care due to procedure complexity, specificity of care orders, and the real possibility of medical catastrophe can seem overwhelming. Therefore, subspecialty nursing training poses a challenge that requires technical in-service and didactic education and allocation of resources.
Despite systems level subspecialty nursing training, medical emergencies identified at the bedside can be mismanaged.1 Errors in care can be due to an incomplete knowledge of the patient’s procedure and misunderstanding of positioning and activity limitations.
To encourage medical-surgical nurses to become more engaged and confident in subspecialty patient care, the authors developed a bedside neurosurgical nursing guide to allow for independent procedure related education. The comprehensive guide summarized the clinical course for postoperative neurosurgical patients undergoing cranial and spinal surgeries. This guide included appropriate surgery-related images, procedure overviews, management decisions, potential postoperative complications, and wound care directions. The guide was distributed to medical-surgical nurses caring for neurosurgical patients. The authors hypothesized that the guide would enable nurses to better predict adverse outcomes and respond appropriately and would improve confidence in patient care.
Methods
For educational purposes, a bedside neurosurgical nursing guide (text and graphics) was created for the 16 surgical subspecialty nurses at the VAPHCS. The guide detailed the most common cranial and spinal neurosurgical procedures performed at VAPHCS and was written based on a typical postoperative course for each procedure by the chief neurosurgery resident at VAPHCS with collaboration from the attending neurosurgeons (Figure).
A quality improvement (QI) project was undertaken to assess nursing confidence with neurosurgical patients’ care pre- and postfamiliarity with the bedside neurosurgical nursing guide. A literature search revealed no validated survey assessing nursing confidence, so one was created using the Likert scale. Specifically, an anonymous 6-question survey was completed by all 16 surgical nurses prior to familiarization with the guide. Responses were recorded as scores of 1 to 5 for questions 1, 3, and 4, with a response of 1 indicative of no comfort or confidence and a response of 5 indicative of the highest level of comfort or confidence. Responses were recorded as either true or false for questions 2 and 6, and never, occasionally, frequently, or always for question 5.
The guide was made available to nurses for 6 months without encouragement to use it. After 6 months, a 3-week period of familiarization with and education about the availability of the guide was instituted at morning nursing reports; the total availability of the guide to nursing staff was 6 months 3 weeks. After this period the same 6-question survey was distributed, and data were collected.
Survey responses were categorized into 2 groups. Responses to questions 1, 3, and 4 were categorized as group 1, and responses to questions 4 and 5 were categorized as group 2. Responses (never and occasionally) to question 5, were categorized as group 1 and responses (frequently and always) as group 2 (Table). Responses to questions 2 and 6 were grouped 1 for true and 2 for false. Nurses participating in this study ranged in age from 22 to 57 years, education level ranged from registered nurse to a bachelor of science in nursing, and years of experience ranged from < 1 year to 27 years.
Statistics were calculated using chi-square analysis with Yates correction online calculator. For the chi-square analysis, the prefamiliarization data for groups 1 and 2 were used as the expected values, and the postfamiliarization data were used for the observed values. In this manner, differences were discerned between the before and after questionnaire responses. The VAPHCS institutional review board determined that the study was not human research and exempt from review.
Findings
Anonymous survey responses were collected from all 16 surgical subspecialty nurses both prior and after familiarization with the nursing guide.The response rate was 100% with only a few incomplete responses excluded from the analysis. Three questions in the prefamiliarization questionnaire had no appropriate response, and 1 question in the postfamiliarization survey had no appropriate response.
Improvement was statistically significant in responses for questions 1, 3, 5, and 6 (P = .026, .008, .004, and .033, respectively). No significant differences were found for questions 2 and 4 (P = .974 and .116, respectively). It is possible that there was no significant difference in question 2 because prefamiliarization responses were already favorable. Even if nurses did not feel comfortable taking care of neurosurgical patients (as assessed in question 1), they noted confidence improvement by working on the ward and through informal assimilation of knowledge and skill, which would have accumulated naturally over 1 year.
Prior to familiarization with the guide, 7 nurses did not feel confident in assessing the need to contact a physician (question 4). After familiarization with the nursing guide, favorable responses increased from 9 to 14 nurses. Results trended toward but did not reach statistical significance, likely due to the small sample size.
Ultimately, in the 16 surgical subspecialty nurses surveyed, familiarization with the nursing guide was shown to improve comfort in taking care of neurosurgical patients and increase confidence in patient care skills. At the end of the QI project (6 months, 3 weeks), all nurses knew where to locate the bedside neurosurgical nursing guide and were familiar with it and its use. The guide remains accessible to the medical-surgical nurses and continues to be used.
Discussion
Nursing confidence has an undervalued effect on patient care.2 Confidence, or a belief in one’s own ability, varies directly with competence. Systematic quantification of nursing competence has been extensively studied using self-report questionnaires and clinical simulations.2,3 Competency can be quantified and normalized using formal assessment; however, confidence is somewhat intangible. Nursing confidence is a situation-dependent subjective feeling of security and is derived from an internalized assessment of skills that are commensurate with patient needs. Nursing confidence is further influenced by an intuited value within the care team, adequate knowledge of the patient’s condition, and procedures and protocols.4
A similar but less specific definition deconstructs nursing confidence as “significance of a professional network of coworkers” and the “importance of confirmation of professional role and competence.”5 The professional network of coworkers is invaluable as it underlies the essence of patient-centered care. The adaptive leadership framework is integral to the modern delivery of patient care, and via this framework frontline clinical staff, including nurses, are empowered.6,7
The second portion of Haavardsholm and Nåden’s definition, “importance of confirmation of professional role and competence” describes the association of the most easily augmented correlate of confidence: competency.5 Nursing competency is supplemented continuously with in-service training and recertification processes; however, despite this, demands placed on nurses can be technologically advanced and extremely varied. Nursing competency is known to directly correlate with increasing education, as nurses holding a master’s degree have been shown to outperform those with a bachelor of nursing degree.3
Increased formal education as well as increased work experience (> 5 years) are correlated with increased critical thinking ability.4,5 The critical thinking ability of health care providers can be fortified by clinical simulation, which leads to statistically significant improvement in clinical competency.2,3
A literature review of Medline and the National Library of Medicine PubMed online databases for search terms (nurs*, confidence, bedside, guide) was performed but did not result in original research assessing nurse confidence related to bedside guides. In this population, nurses were anonymously compared against their own historical data obviating any effect of education or experience on survey measures.
Nursing Self-Confidence
Evidence suggests that nursing confidence is a complex manifestation of the security felt within the care team and the comfort of one’s own professional abilities.4 Patients’ trust in the team caring for them is based on the confidence exuded by the team.8 In this way, nursing confidence can affect the patient-care team profoundly. Value is maximized when a nurse’s self-confidence engenders patient confidence and trust. Due to the varied patient load and complexity of subspecialty nursing care, it is hypothesized that bedside manuals/guidelines can be used to educate the subspecialty nurses on specific patient-related issues.
Nursing practice competence and confidence is vital to providing care for patients with complex postsurgical health care needs. Patient safety and outcome are paramount. This can be intimidating for newly qualified surgical subspecialty nurses who have not yet had experience with or adequate exposure to patients with complex postsurgical needs. Surgical nursing continuing education places an emphasis on adaptation to ever-changing specialized surgical procedures and postoperative patient care. Nevertheless, it is difficult for surgical subspecialty nurses to learn and retain all the possible complexities of individual cases and to confidently, appropriately, and safely care for patients especially when adverse events arise.
Recognizing that leadership is personal and not dependent on hierarchy, surgical subspecialty nurses may be better suited to specific bedside training and counseling.6,9 A key factor influencing nursing confidence is communication and collaboration with physicians.9 The role of the physician at VA medical facilities is no longer to be a commanding figure with complete medical autonomy; rather, a unified team of specialized practitioners collaboratively facilitate and deliver patient care.
There is no specific research detailing the use of bedside nursing guides in caring for postoperative patients. However, at VAPHCS, nurses created supplemental material regarding postoperative acute care of vascular surgery patients, which was found to be subjectively helpful in elevating nursing confidence. To the authors’ knowledge, no such supplemental information/guide exists for other specialty surgical services.
The surgical nursing guide created here detailed visuals of many common neurosurgical procedures performed at VAPHCS and included a prioritized checklist, which the 16 surgical subspecialty nurses could reference postoperatively. The authors hypothesized that this would enhance the nurses’ ability to efficiently manage specific situations while bridging communication gaps between surgical teams and nurses. The survey results agree with previous reports that suggested that the application of an adaptive leadership framework would empower nurses to deliver excellent patient-centered care, care that can be augmented with subspecialty nursing guides.7,10
Based on these results the authors propose that subspecialty surgical services consider use of a practical nursing guide for all surgical subspecialty nurses to reference, improve familiarity with procedures, and provide guidance to manage adverse events. Since implementing this reader-friendly paradigm within neurosurgical care, a nurse driven expansion has now included other subspecialty services at the VAPHCS with success.
Limitations
Survey responses have inherent bias and sampling error rates. The sample size for this survey was small. Data were grouped for data analysis. Competency and patient outcomes were not measured.
Future Directions
Despite specific surgical specialty postoperative patient care training, an overall lack of confidence can persist. A physician-created neurosurgical nursing guide that detailed the most common neurosurgical procedures, expected postoperative care, and potential emergencies was shown to improve nursing confidence. Collaborative (physician and nursing leaders) QI projects, such as described here; development of specific surgical specialty initiatives designed to improve confidence and quality; and nurse-physician communication and teamwork could lead to improved patient satisfaction and outcome.
The costs associated with developing and using bedside nursing guides are relatively low, and efficiency can be considered high. Competency improvement could be measured by creating a specialty-specific case scenario question bank. Effects on patient satisfaction and outcome could be measured by a patient satisfaction survey. Improvements in beside catastrophe management could be prospectively tracked; for example, rates of mismanagement of mobility status, emergent transfers to the intensive care unit, or poor wound care could be compared pre- and postfamiliarization with a subspecialty guide.
Conclusion
Familiarization with the VAPHCS neurosurgical nursing guide had a positive impact on the confidence of medical-surgical nurses caring for neurosurgical patients. Medical-surgical nurses were more comfortable taking care of neurosurgical patients; they felt the guide helped improve skills and noted improved knowledge regarding involvement of physician oversight. Although objective parameters were not assessed, improvement in nursing confidence in general leads to improved overall nurse-physician communication and patient management. A further study might target objective parameters associated with guide usage, such as changes in the number of emergencies or calls to physicians regarding management.
Acknowledgments
The authors thank Andy Rekito, MS, for illustrative assistance.
1. Pusateri ME, Prior MM, Kiely SC. The role of the non-ICU staff nurse on a medical emergency team: perceptions and understanding. Am J Nurs. 2011;111(5):22-29, quiz 30-31.
2. Bambini D, Washburn J, Perkins R. Outcomes of clinical simulation for novice nursing students: communication, confidence, clinical judgment. Nurs Educ Perspect. 2009;30(2):79-82.
3. Chang MJ, Chang YJ, Kuo SH, Yang YH, Chou FH. Relationships between critical thinking ability and nursing competence in clinical nurses. J Clin Nurs. 2011;20(21-22):3224-3232.
4. Perry P. Concept analysis: confidence/self-confidence. Nurs Forum. 2011;46(4):218-230.
5. Haavardsholm I, Nåden D. The concept of confidence—the nurse’s perception. Eur J Cancer Care (Engl). 2009;18(5):483-491.
6. Bailey DE Jr, Docherty SL, Adams JA, et al. Studying the clinical encounter with the Adaptive Leadership framework. J Healthc Leadersh. 2012;2012(4):83-91.
7. Hall C, McCutcheon H, Deuter K, Matricciani L. Evaluating and improving a model of nursing care delivery: a process of partnership. Collegian. 2012;19(4):203-210.
8. Williams AM, Irurita VF. Therapeutic and non-therapeutic interpersonal interactions: the patient’s perspective. J Clin Nurs. 2004;13(7):806-815.
9. Carryer J. Collaboration between doctors and nurses. J Prim Health Care. 2011;3(1):77-79.
10. Chadwick MM. Creating order out of chaos: a leadership approach. AORN J. 2010;91(1):154-170.
The VA Portland Healthcare System (VAPHCS) is a 277-bed facility that serves more than 85,000 inpatient and 880,000 outpatient visits each year from veterans in Oregon and southwestern Washington. The VAPHCS consists of a main tertiary care VAMC with an acute medical and surgical facility that includes 30 beds serving qualifying veterans. Supported surgical specialties include urology, general surgery, vascular surgery, otolaryngology, orthopedic surgery, ophthalmology, cardiothoracic surgery, transplant surgery, and neurological surgery. Neurosurgical patients account for about 12% to 13% of annual surgical patients. The VAPHCS also is partnered with Oregon Health & Science University in the training of health care professionals, such as physicians and nurses.
The expectation at the VAPHCS is that medical-surgical nurses care for 4 to 5 concurrent patients, often from different surgical services. Caring for patients with different medical and surgical needs, variable ambulatory, swallowing, and elimination functions, and different physician teams can become confusing; even within a single surgical service, postoperative care due to procedure complexity, specificity of care orders, and the real possibility of medical catastrophe can seem overwhelming. Therefore, subspecialty nursing training poses a challenge that requires technical in-service and didactic education and allocation of resources.
Despite systems level subspecialty nursing training, medical emergencies identified at the bedside can be mismanaged.1 Errors in care can be due to an incomplete knowledge of the patient’s procedure and misunderstanding of positioning and activity limitations.
To encourage medical-surgical nurses to become more engaged and confident in subspecialty patient care, the authors developed a bedside neurosurgical nursing guide to allow for independent procedure related education. The comprehensive guide summarized the clinical course for postoperative neurosurgical patients undergoing cranial and spinal surgeries. This guide included appropriate surgery-related images, procedure overviews, management decisions, potential postoperative complications, and wound care directions. The guide was distributed to medical-surgical nurses caring for neurosurgical patients. The authors hypothesized that the guide would enable nurses to better predict adverse outcomes and respond appropriately and would improve confidence in patient care.
Methods
For educational purposes, a bedside neurosurgical nursing guide (text and graphics) was created for the 16 surgical subspecialty nurses at the VAPHCS. The guide detailed the most common cranial and spinal neurosurgical procedures performed at VAPHCS and was written based on a typical postoperative course for each procedure by the chief neurosurgery resident at VAPHCS with collaboration from the attending neurosurgeons (Figure).
A quality improvement (QI) project was undertaken to assess nursing confidence with neurosurgical patients’ care pre- and postfamiliarity with the bedside neurosurgical nursing guide. A literature search revealed no validated survey assessing nursing confidence, so one was created using the Likert scale. Specifically, an anonymous 6-question survey was completed by all 16 surgical nurses prior to familiarization with the guide. Responses were recorded as scores of 1 to 5 for questions 1, 3, and 4, with a response of 1 indicative of no comfort or confidence and a response of 5 indicative of the highest level of comfort or confidence. Responses were recorded as either true or false for questions 2 and 6, and never, occasionally, frequently, or always for question 5.
The guide was made available to nurses for 6 months without encouragement to use it. After 6 months, a 3-week period of familiarization with and education about the availability of the guide was instituted at morning nursing reports; the total availability of the guide to nursing staff was 6 months 3 weeks. After this period the same 6-question survey was distributed, and data were collected.
Survey responses were categorized into 2 groups. Responses to questions 1, 3, and 4 were categorized as group 1, and responses to questions 4 and 5 were categorized as group 2. Responses (never and occasionally) to question 5, were categorized as group 1 and responses (frequently and always) as group 2 (Table). Responses to questions 2 and 6 were grouped 1 for true and 2 for false. Nurses participating in this study ranged in age from 22 to 57 years, education level ranged from registered nurse to a bachelor of science in nursing, and years of experience ranged from < 1 year to 27 years.
Statistics were calculated using chi-square analysis with Yates correction online calculator. For the chi-square analysis, the prefamiliarization data for groups 1 and 2 were used as the expected values, and the postfamiliarization data were used for the observed values. In this manner, differences were discerned between the before and after questionnaire responses. The VAPHCS institutional review board determined that the study was not human research and exempt from review.
Findings
Anonymous survey responses were collected from all 16 surgical subspecialty nurses both prior and after familiarization with the nursing guide.The response rate was 100% with only a few incomplete responses excluded from the analysis. Three questions in the prefamiliarization questionnaire had no appropriate response, and 1 question in the postfamiliarization survey had no appropriate response.
Improvement was statistically significant in responses for questions 1, 3, 5, and 6 (P = .026, .008, .004, and .033, respectively). No significant differences were found for questions 2 and 4 (P = .974 and .116, respectively). It is possible that there was no significant difference in question 2 because prefamiliarization responses were already favorable. Even if nurses did not feel comfortable taking care of neurosurgical patients (as assessed in question 1), they noted confidence improvement by working on the ward and through informal assimilation of knowledge and skill, which would have accumulated naturally over 1 year.
Prior to familiarization with the guide, 7 nurses did not feel confident in assessing the need to contact a physician (question 4). After familiarization with the nursing guide, favorable responses increased from 9 to 14 nurses. Results trended toward but did not reach statistical significance, likely due to the small sample size.
Ultimately, in the 16 surgical subspecialty nurses surveyed, familiarization with the nursing guide was shown to improve comfort in taking care of neurosurgical patients and increase confidence in patient care skills. At the end of the QI project (6 months, 3 weeks), all nurses knew where to locate the bedside neurosurgical nursing guide and were familiar with it and its use. The guide remains accessible to the medical-surgical nurses and continues to be used.
Discussion
Nursing confidence has an undervalued effect on patient care.2 Confidence, or a belief in one’s own ability, varies directly with competence. Systematic quantification of nursing competence has been extensively studied using self-report questionnaires and clinical simulations.2,3 Competency can be quantified and normalized using formal assessment; however, confidence is somewhat intangible. Nursing confidence is a situation-dependent subjective feeling of security and is derived from an internalized assessment of skills that are commensurate with patient needs. Nursing confidence is further influenced by an intuited value within the care team, adequate knowledge of the patient’s condition, and procedures and protocols.4
A similar but less specific definition deconstructs nursing confidence as “significance of a professional network of coworkers” and the “importance of confirmation of professional role and competence.”5 The professional network of coworkers is invaluable as it underlies the essence of patient-centered care. The adaptive leadership framework is integral to the modern delivery of patient care, and via this framework frontline clinical staff, including nurses, are empowered.6,7
The second portion of Haavardsholm and Nåden’s definition, “importance of confirmation of professional role and competence” describes the association of the most easily augmented correlate of confidence: competency.5 Nursing competency is supplemented continuously with in-service training and recertification processes; however, despite this, demands placed on nurses can be technologically advanced and extremely varied. Nursing competency is known to directly correlate with increasing education, as nurses holding a master’s degree have been shown to outperform those with a bachelor of nursing degree.3
Increased formal education as well as increased work experience (> 5 years) are correlated with increased critical thinking ability.4,5 The critical thinking ability of health care providers can be fortified by clinical simulation, which leads to statistically significant improvement in clinical competency.2,3
A literature review of Medline and the National Library of Medicine PubMed online databases for search terms (nurs*, confidence, bedside, guide) was performed but did not result in original research assessing nurse confidence related to bedside guides. In this population, nurses were anonymously compared against their own historical data obviating any effect of education or experience on survey measures.
Nursing Self-Confidence
Evidence suggests that nursing confidence is a complex manifestation of the security felt within the care team and the comfort of one’s own professional abilities.4 Patients’ trust in the team caring for them is based on the confidence exuded by the team.8 In this way, nursing confidence can affect the patient-care team profoundly. Value is maximized when a nurse’s self-confidence engenders patient confidence and trust. Due to the varied patient load and complexity of subspecialty nursing care, it is hypothesized that bedside manuals/guidelines can be used to educate the subspecialty nurses on specific patient-related issues.
Nursing practice competence and confidence is vital to providing care for patients with complex postsurgical health care needs. Patient safety and outcome are paramount. This can be intimidating for newly qualified surgical subspecialty nurses who have not yet had experience with or adequate exposure to patients with complex postsurgical needs. Surgical nursing continuing education places an emphasis on adaptation to ever-changing specialized surgical procedures and postoperative patient care. Nevertheless, it is difficult for surgical subspecialty nurses to learn and retain all the possible complexities of individual cases and to confidently, appropriately, and safely care for patients especially when adverse events arise.
Recognizing that leadership is personal and not dependent on hierarchy, surgical subspecialty nurses may be better suited to specific bedside training and counseling.6,9 A key factor influencing nursing confidence is communication and collaboration with physicians.9 The role of the physician at VA medical facilities is no longer to be a commanding figure with complete medical autonomy; rather, a unified team of specialized practitioners collaboratively facilitate and deliver patient care.
There is no specific research detailing the use of bedside nursing guides in caring for postoperative patients. However, at VAPHCS, nurses created supplemental material regarding postoperative acute care of vascular surgery patients, which was found to be subjectively helpful in elevating nursing confidence. To the authors’ knowledge, no such supplemental information/guide exists for other specialty surgical services.
The surgical nursing guide created here detailed visuals of many common neurosurgical procedures performed at VAPHCS and included a prioritized checklist, which the 16 surgical subspecialty nurses could reference postoperatively. The authors hypothesized that this would enhance the nurses’ ability to efficiently manage specific situations while bridging communication gaps between surgical teams and nurses. The survey results agree with previous reports that suggested that the application of an adaptive leadership framework would empower nurses to deliver excellent patient-centered care, care that can be augmented with subspecialty nursing guides.7,10
Based on these results the authors propose that subspecialty surgical services consider use of a practical nursing guide for all surgical subspecialty nurses to reference, improve familiarity with procedures, and provide guidance to manage adverse events. Since implementing this reader-friendly paradigm within neurosurgical care, a nurse driven expansion has now included other subspecialty services at the VAPHCS with success.
Limitations
Survey responses have inherent bias and sampling error rates. The sample size for this survey was small. Data were grouped for data analysis. Competency and patient outcomes were not measured.
Future Directions
Despite specific surgical specialty postoperative patient care training, an overall lack of confidence can persist. A physician-created neurosurgical nursing guide that detailed the most common neurosurgical procedures, expected postoperative care, and potential emergencies was shown to improve nursing confidence. Collaborative (physician and nursing leaders) QI projects, such as described here; development of specific surgical specialty initiatives designed to improve confidence and quality; and nurse-physician communication and teamwork could lead to improved patient satisfaction and outcome.
The costs associated with developing and using bedside nursing guides are relatively low, and efficiency can be considered high. Competency improvement could be measured by creating a specialty-specific case scenario question bank. Effects on patient satisfaction and outcome could be measured by a patient satisfaction survey. Improvements in beside catastrophe management could be prospectively tracked; for example, rates of mismanagement of mobility status, emergent transfers to the intensive care unit, or poor wound care could be compared pre- and postfamiliarization with a subspecialty guide.
Conclusion
Familiarization with the VAPHCS neurosurgical nursing guide had a positive impact on the confidence of medical-surgical nurses caring for neurosurgical patients. Medical-surgical nurses were more comfortable taking care of neurosurgical patients; they felt the guide helped improve skills and noted improved knowledge regarding involvement of physician oversight. Although objective parameters were not assessed, improvement in nursing confidence in general leads to improved overall nurse-physician communication and patient management. A further study might target objective parameters associated with guide usage, such as changes in the number of emergencies or calls to physicians regarding management.
Acknowledgments
The authors thank Andy Rekito, MS, for illustrative assistance.
The VA Portland Healthcare System (VAPHCS) is a 277-bed facility that serves more than 85,000 inpatient and 880,000 outpatient visits each year from veterans in Oregon and southwestern Washington. The VAPHCS consists of a main tertiary care VAMC with an acute medical and surgical facility that includes 30 beds serving qualifying veterans. Supported surgical specialties include urology, general surgery, vascular surgery, otolaryngology, orthopedic surgery, ophthalmology, cardiothoracic surgery, transplant surgery, and neurological surgery. Neurosurgical patients account for about 12% to 13% of annual surgical patients. The VAPHCS also is partnered with Oregon Health & Science University in the training of health care professionals, such as physicians and nurses.
The expectation at the VAPHCS is that medical-surgical nurses care for 4 to 5 concurrent patients, often from different surgical services. Caring for patients with different medical and surgical needs, variable ambulatory, swallowing, and elimination functions, and different physician teams can become confusing; even within a single surgical service, postoperative care due to procedure complexity, specificity of care orders, and the real possibility of medical catastrophe can seem overwhelming. Therefore, subspecialty nursing training poses a challenge that requires technical in-service and didactic education and allocation of resources.
Despite systems level subspecialty nursing training, medical emergencies identified at the bedside can be mismanaged.1 Errors in care can be due to an incomplete knowledge of the patient’s procedure and misunderstanding of positioning and activity limitations.
To encourage medical-surgical nurses to become more engaged and confident in subspecialty patient care, the authors developed a bedside neurosurgical nursing guide to allow for independent procedure related education. The comprehensive guide summarized the clinical course for postoperative neurosurgical patients undergoing cranial and spinal surgeries. This guide included appropriate surgery-related images, procedure overviews, management decisions, potential postoperative complications, and wound care directions. The guide was distributed to medical-surgical nurses caring for neurosurgical patients. The authors hypothesized that the guide would enable nurses to better predict adverse outcomes and respond appropriately and would improve confidence in patient care.
Methods
For educational purposes, a bedside neurosurgical nursing guide (text and graphics) was created for the 16 surgical subspecialty nurses at the VAPHCS. The guide detailed the most common cranial and spinal neurosurgical procedures performed at VAPHCS and was written based on a typical postoperative course for each procedure by the chief neurosurgery resident at VAPHCS with collaboration from the attending neurosurgeons (Figure).
A quality improvement (QI) project was undertaken to assess nursing confidence with neurosurgical patients’ care pre- and postfamiliarity with the bedside neurosurgical nursing guide. A literature search revealed no validated survey assessing nursing confidence, so one was created using the Likert scale. Specifically, an anonymous 6-question survey was completed by all 16 surgical nurses prior to familiarization with the guide. Responses were recorded as scores of 1 to 5 for questions 1, 3, and 4, with a response of 1 indicative of no comfort or confidence and a response of 5 indicative of the highest level of comfort or confidence. Responses were recorded as either true or false for questions 2 and 6, and never, occasionally, frequently, or always for question 5.
The guide was made available to nurses for 6 months without encouragement to use it. After 6 months, a 3-week period of familiarization with and education about the availability of the guide was instituted at morning nursing reports; the total availability of the guide to nursing staff was 6 months 3 weeks. After this period the same 6-question survey was distributed, and data were collected.
Survey responses were categorized into 2 groups. Responses to questions 1, 3, and 4 were categorized as group 1, and responses to questions 4 and 5 were categorized as group 2. Responses (never and occasionally) to question 5, were categorized as group 1 and responses (frequently and always) as group 2 (Table). Responses to questions 2 and 6 were grouped 1 for true and 2 for false. Nurses participating in this study ranged in age from 22 to 57 years, education level ranged from registered nurse to a bachelor of science in nursing, and years of experience ranged from < 1 year to 27 years.
Statistics were calculated using chi-square analysis with Yates correction online calculator. For the chi-square analysis, the prefamiliarization data for groups 1 and 2 were used as the expected values, and the postfamiliarization data were used for the observed values. In this manner, differences were discerned between the before and after questionnaire responses. The VAPHCS institutional review board determined that the study was not human research and exempt from review.
Findings
Anonymous survey responses were collected from all 16 surgical subspecialty nurses both prior and after familiarization with the nursing guide.The response rate was 100% with only a few incomplete responses excluded from the analysis. Three questions in the prefamiliarization questionnaire had no appropriate response, and 1 question in the postfamiliarization survey had no appropriate response.
Improvement was statistically significant in responses for questions 1, 3, 5, and 6 (P = .026, .008, .004, and .033, respectively). No significant differences were found for questions 2 and 4 (P = .974 and .116, respectively). It is possible that there was no significant difference in question 2 because prefamiliarization responses were already favorable. Even if nurses did not feel comfortable taking care of neurosurgical patients (as assessed in question 1), they noted confidence improvement by working on the ward and through informal assimilation of knowledge and skill, which would have accumulated naturally over 1 year.
Prior to familiarization with the guide, 7 nurses did not feel confident in assessing the need to contact a physician (question 4). After familiarization with the nursing guide, favorable responses increased from 9 to 14 nurses. Results trended toward but did not reach statistical significance, likely due to the small sample size.
Ultimately, in the 16 surgical subspecialty nurses surveyed, familiarization with the nursing guide was shown to improve comfort in taking care of neurosurgical patients and increase confidence in patient care skills. At the end of the QI project (6 months, 3 weeks), all nurses knew where to locate the bedside neurosurgical nursing guide and were familiar with it and its use. The guide remains accessible to the medical-surgical nurses and continues to be used.
Discussion
Nursing confidence has an undervalued effect on patient care.2 Confidence, or a belief in one’s own ability, varies directly with competence. Systematic quantification of nursing competence has been extensively studied using self-report questionnaires and clinical simulations.2,3 Competency can be quantified and normalized using formal assessment; however, confidence is somewhat intangible. Nursing confidence is a situation-dependent subjective feeling of security and is derived from an internalized assessment of skills that are commensurate with patient needs. Nursing confidence is further influenced by an intuited value within the care team, adequate knowledge of the patient’s condition, and procedures and protocols.4
A similar but less specific definition deconstructs nursing confidence as “significance of a professional network of coworkers” and the “importance of confirmation of professional role and competence.”5 The professional network of coworkers is invaluable as it underlies the essence of patient-centered care. The adaptive leadership framework is integral to the modern delivery of patient care, and via this framework frontline clinical staff, including nurses, are empowered.6,7
The second portion of Haavardsholm and Nåden’s definition, “importance of confirmation of professional role and competence” describes the association of the most easily augmented correlate of confidence: competency.5 Nursing competency is supplemented continuously with in-service training and recertification processes; however, despite this, demands placed on nurses can be technologically advanced and extremely varied. Nursing competency is known to directly correlate with increasing education, as nurses holding a master’s degree have been shown to outperform those with a bachelor of nursing degree.3
Increased formal education as well as increased work experience (> 5 years) are correlated with increased critical thinking ability.4,5 The critical thinking ability of health care providers can be fortified by clinical simulation, which leads to statistically significant improvement in clinical competency.2,3
A literature review of Medline and the National Library of Medicine PubMed online databases for search terms (nurs*, confidence, bedside, guide) was performed but did not result in original research assessing nurse confidence related to bedside guides. In this population, nurses were anonymously compared against their own historical data obviating any effect of education or experience on survey measures.
Nursing Self-Confidence
Evidence suggests that nursing confidence is a complex manifestation of the security felt within the care team and the comfort of one’s own professional abilities.4 Patients’ trust in the team caring for them is based on the confidence exuded by the team.8 In this way, nursing confidence can affect the patient-care team profoundly. Value is maximized when a nurse’s self-confidence engenders patient confidence and trust. Due to the varied patient load and complexity of subspecialty nursing care, it is hypothesized that bedside manuals/guidelines can be used to educate the subspecialty nurses on specific patient-related issues.
Nursing practice competence and confidence is vital to providing care for patients with complex postsurgical health care needs. Patient safety and outcome are paramount. This can be intimidating for newly qualified surgical subspecialty nurses who have not yet had experience with or adequate exposure to patients with complex postsurgical needs. Surgical nursing continuing education places an emphasis on adaptation to ever-changing specialized surgical procedures and postoperative patient care. Nevertheless, it is difficult for surgical subspecialty nurses to learn and retain all the possible complexities of individual cases and to confidently, appropriately, and safely care for patients especially when adverse events arise.
Recognizing that leadership is personal and not dependent on hierarchy, surgical subspecialty nurses may be better suited to specific bedside training and counseling.6,9 A key factor influencing nursing confidence is communication and collaboration with physicians.9 The role of the physician at VA medical facilities is no longer to be a commanding figure with complete medical autonomy; rather, a unified team of specialized practitioners collaboratively facilitate and deliver patient care.
There is no specific research detailing the use of bedside nursing guides in caring for postoperative patients. However, at VAPHCS, nurses created supplemental material regarding postoperative acute care of vascular surgery patients, which was found to be subjectively helpful in elevating nursing confidence. To the authors’ knowledge, no such supplemental information/guide exists for other specialty surgical services.
The surgical nursing guide created here detailed visuals of many common neurosurgical procedures performed at VAPHCS and included a prioritized checklist, which the 16 surgical subspecialty nurses could reference postoperatively. The authors hypothesized that this would enhance the nurses’ ability to efficiently manage specific situations while bridging communication gaps between surgical teams and nurses. The survey results agree with previous reports that suggested that the application of an adaptive leadership framework would empower nurses to deliver excellent patient-centered care, care that can be augmented with subspecialty nursing guides.7,10
Based on these results the authors propose that subspecialty surgical services consider use of a practical nursing guide for all surgical subspecialty nurses to reference, improve familiarity with procedures, and provide guidance to manage adverse events. Since implementing this reader-friendly paradigm within neurosurgical care, a nurse driven expansion has now included other subspecialty services at the VAPHCS with success.
Limitations
Survey responses have inherent bias and sampling error rates. The sample size for this survey was small. Data were grouped for data analysis. Competency and patient outcomes were not measured.
Future Directions
Despite specific surgical specialty postoperative patient care training, an overall lack of confidence can persist. A physician-created neurosurgical nursing guide that detailed the most common neurosurgical procedures, expected postoperative care, and potential emergencies was shown to improve nursing confidence. Collaborative (physician and nursing leaders) QI projects, such as described here; development of specific surgical specialty initiatives designed to improve confidence and quality; and nurse-physician communication and teamwork could lead to improved patient satisfaction and outcome.
The costs associated with developing and using bedside nursing guides are relatively low, and efficiency can be considered high. Competency improvement could be measured by creating a specialty-specific case scenario question bank. Effects on patient satisfaction and outcome could be measured by a patient satisfaction survey. Improvements in beside catastrophe management could be prospectively tracked; for example, rates of mismanagement of mobility status, emergent transfers to the intensive care unit, or poor wound care could be compared pre- and postfamiliarization with a subspecialty guide.
Conclusion
Familiarization with the VAPHCS neurosurgical nursing guide had a positive impact on the confidence of medical-surgical nurses caring for neurosurgical patients. Medical-surgical nurses were more comfortable taking care of neurosurgical patients; they felt the guide helped improve skills and noted improved knowledge regarding involvement of physician oversight. Although objective parameters were not assessed, improvement in nursing confidence in general leads to improved overall nurse-physician communication and patient management. A further study might target objective parameters associated with guide usage, such as changes in the number of emergencies or calls to physicians regarding management.
Acknowledgments
The authors thank Andy Rekito, MS, for illustrative assistance.
1. Pusateri ME, Prior MM, Kiely SC. The role of the non-ICU staff nurse on a medical emergency team: perceptions and understanding. Am J Nurs. 2011;111(5):22-29, quiz 30-31.
2. Bambini D, Washburn J, Perkins R. Outcomes of clinical simulation for novice nursing students: communication, confidence, clinical judgment. Nurs Educ Perspect. 2009;30(2):79-82.
3. Chang MJ, Chang YJ, Kuo SH, Yang YH, Chou FH. Relationships between critical thinking ability and nursing competence in clinical nurses. J Clin Nurs. 2011;20(21-22):3224-3232.
4. Perry P. Concept analysis: confidence/self-confidence. Nurs Forum. 2011;46(4):218-230.
5. Haavardsholm I, Nåden D. The concept of confidence—the nurse’s perception. Eur J Cancer Care (Engl). 2009;18(5):483-491.
6. Bailey DE Jr, Docherty SL, Adams JA, et al. Studying the clinical encounter with the Adaptive Leadership framework. J Healthc Leadersh. 2012;2012(4):83-91.
7. Hall C, McCutcheon H, Deuter K, Matricciani L. Evaluating and improving a model of nursing care delivery: a process of partnership. Collegian. 2012;19(4):203-210.
8. Williams AM, Irurita VF. Therapeutic and non-therapeutic interpersonal interactions: the patient’s perspective. J Clin Nurs. 2004;13(7):806-815.
9. Carryer J. Collaboration between doctors and nurses. J Prim Health Care. 2011;3(1):77-79.
10. Chadwick MM. Creating order out of chaos: a leadership approach. AORN J. 2010;91(1):154-170.
1. Pusateri ME, Prior MM, Kiely SC. The role of the non-ICU staff nurse on a medical emergency team: perceptions and understanding. Am J Nurs. 2011;111(5):22-29, quiz 30-31.
2. Bambini D, Washburn J, Perkins R. Outcomes of clinical simulation for novice nursing students: communication, confidence, clinical judgment. Nurs Educ Perspect. 2009;30(2):79-82.
3. Chang MJ, Chang YJ, Kuo SH, Yang YH, Chou FH. Relationships between critical thinking ability and nursing competence in clinical nurses. J Clin Nurs. 2011;20(21-22):3224-3232.
4. Perry P. Concept analysis: confidence/self-confidence. Nurs Forum. 2011;46(4):218-230.
5. Haavardsholm I, Nåden D. The concept of confidence—the nurse’s perception. Eur J Cancer Care (Engl). 2009;18(5):483-491.
6. Bailey DE Jr, Docherty SL, Adams JA, et al. Studying the clinical encounter with the Adaptive Leadership framework. J Healthc Leadersh. 2012;2012(4):83-91.
7. Hall C, McCutcheon H, Deuter K, Matricciani L. Evaluating and improving a model of nursing care delivery: a process of partnership. Collegian. 2012;19(4):203-210.
8. Williams AM, Irurita VF. Therapeutic and non-therapeutic interpersonal interactions: the patient’s perspective. J Clin Nurs. 2004;13(7):806-815.
9. Carryer J. Collaboration between doctors and nurses. J Prim Health Care. 2011;3(1):77-79.
10. Chadwick MM. Creating order out of chaos: a leadership approach. AORN J. 2010;91(1):154-170.