User login
Combined Clinics, Personalized Medicine for Psoriatic Disease Face Barriers
NEW YORK CITY — The idea of having dermatologists and rheumatologists under one roof to see patients with psoriasis prone to psoriatic arthritis (PsA) — a concept known as combined clinics — has been around for more than a decade, and the idea of personalized medicine for these patients even longer than that, yet both approaches to care have encountered a host of obstacles, a longtime research rheumatologist said.
“It’s important that we work together, but there is a problem in terms of staffing — managing the meetings with patients together — and in the states in particular it’s a matter of who’s charging for what,” Dafna Gladman, MD, a rheumatologist at the University of Toronto, in Ontario, Canada, told attendees at the annual New York University (NYU) Langone Advanced Seminar in Psoriasis and Psoriatic Arthritis. Her institution has one of the 44 worldwide combined clinics registered in the Psoriasis & Psoriatic Arthritis Clinics Multicenter Advancement Network (PPACMAN), of which Gladman is an advisory board member.
Barriers to Combined Clinics
“Some of the barriers are physical in the sense that, for the dermatologists and rheumatologists to work at the same time, you need the right space, and in many places, you just don’t have the space to have the two specialists sitting at the same time,” Gladman told Medscape Medical News.
Some centers get around this by having the dermatology and rheumatology clinics next to or near each other. “So these two specialists are close enough to be able to go from room to room,” she added.
Another challenge facing combined clinics lies in the nature of how dermatologists and rheumatologists see patients. “The dermatologist sees patients a lot faster than the rheumatologist, so if the dermatologist and rheumatologist are sitting together, the dermatologist may not see as many patients as they would otherwise and therefore may not get reimbursed properly,” Gladman said.
To overcome these challenges, different models have emerged, Gladman said. If space allows, the ideal model is to have both specialties in one clinic, she said, while compensating for the different pace at which dermatologists and rheumatologists see patients.
The other model is to locate the two clinics close enough so that a person with suspected PsA can get to the rheumatology clinic soon after their dermatologic consult, or the rheumatologist can go to the dermatology clinic, Gladman said. Or the situation may be reversed when the rheumatologist needs a dermatology consult, she added.
When that’s not possible, a virtual visit may be the solution, Gladman said. She noted that PPACMAN offers ways to overcome the challenges of running a combined clinic.
Whatever combined clinic model a center chooses, clinicians must be mindful of preventing patients from falling through the cracks, Gladman said.
“When you treat patients separately, the patient sees the rheumatologist, and the rheumatologist wants to do one thing; then they go to the dermatologist and the dermatologist wants to do another thing, and the patient doesn’t do anything because they don’t know what to choose,” she said.
The combined clinic allows the patient to get the opinions of both specialists and avoid the uncertainty about the course of treatment, Gladman added.
Some combined clinics may also house other specialists, such as gastroenterologists, cardiologists, and nurse practitioners, noted Jose U. Scher, MD, director of the Arthritis Clinic and Psoriatic Arthritis Center at NYU Langone Health in New York City. Such centers are typically in academic centers “given challenges with space, scheduling, and reimbursement,” he told Medscape Medical News. NYU has a PPACMAN-registered combined clinic.
Regardless of how combined clinics are organized, Scher said, “We have found that the most important aspect of combined clinics is the open communication and integration of care between and amongst specialists and patients.”
The Potential of Personalized Medicine
“Personalized medicine is where we need to get to,” Gladman told seminar attendees. She said she had hoped it would be further along by now and be more integrated into the care of patients with psoriasis and PsA. “The idea is to identify psoriasis patients that are destined to develop psoriatic arthritis,” she said.
Besides that, identifying biomarkers is key to advancing personalized medicine for psoriasis, Gladman noted.
“In the skin, it’s easy; even the patient can assess their psoriasis,” she said. “But in the joints, it’s very difficult, so it would be nice to have some kind of biomarker, whether it’s the blood or an imaging modality. We want to identify the biomarkers for drug response or lack thereof so we know what drugs would be appropriate for the individual patient, and therefore, we can provide the right drug for the right person and fortunately at the right time.”
In explaining why personalized medicine isn’t further along in dermatology and rheumatology, Gladman told Medscape Medical News, “It’s a matter of finding the right things; we haven’t solved the mystery.” She cited a previous discussion at the seminar about the pathogenesis of PsA. “One person thinks it’s the bone marrow and another thinks it’s the T cells, so we haven’t quite put it all together to have a definitive answer.”
Personalized medicine in psoriasis and PsA is a “key unmet need,” Scher said. “Multiomics” — a biological analysis approach that uses multiple “omes,” such as the genome and microbiome — digital features, and wearables “can unlock novel diagnostic and therapeutic pathways that are desperately needed to enhance clinical response in PsA,” he said.
Also emerging are humanized animal models for laboratory research, which Scher called “potentially very useful tools to personalize approaches to PsA pathogenesis and treatment.”
Gladman disclosed financial relationships with AbbVie, Amgen, Bristol Myers Squibb, Eli Lilly, Galapagos, Gilead, Janssen, Novartis, Pfizer, and UCB. Scher had no relevant financial relationships.
A version of this article first appeared on Medscape.com.
NEW YORK CITY — The idea of having dermatologists and rheumatologists under one roof to see patients with psoriasis prone to psoriatic arthritis (PsA) — a concept known as combined clinics — has been around for more than a decade, and the idea of personalized medicine for these patients even longer than that, yet both approaches to care have encountered a host of obstacles, a longtime research rheumatologist said.
“It’s important that we work together, but there is a problem in terms of staffing — managing the meetings with patients together — and in the states in particular it’s a matter of who’s charging for what,” Dafna Gladman, MD, a rheumatologist at the University of Toronto, in Ontario, Canada, told attendees at the annual New York University (NYU) Langone Advanced Seminar in Psoriasis and Psoriatic Arthritis. Her institution has one of the 44 worldwide combined clinics registered in the Psoriasis & Psoriatic Arthritis Clinics Multicenter Advancement Network (PPACMAN), of which Gladman is an advisory board member.
Barriers to Combined Clinics
“Some of the barriers are physical in the sense that, for the dermatologists and rheumatologists to work at the same time, you need the right space, and in many places, you just don’t have the space to have the two specialists sitting at the same time,” Gladman told Medscape Medical News.
Some centers get around this by having the dermatology and rheumatology clinics next to or near each other. “So these two specialists are close enough to be able to go from room to room,” she added.
Another challenge facing combined clinics lies in the nature of how dermatologists and rheumatologists see patients. “The dermatologist sees patients a lot faster than the rheumatologist, so if the dermatologist and rheumatologist are sitting together, the dermatologist may not see as many patients as they would otherwise and therefore may not get reimbursed properly,” Gladman said.
To overcome these challenges, different models have emerged, Gladman said. If space allows, the ideal model is to have both specialties in one clinic, she said, while compensating for the different pace at which dermatologists and rheumatologists see patients.
The other model is to locate the two clinics close enough so that a person with suspected PsA can get to the rheumatology clinic soon after their dermatologic consult, or the rheumatologist can go to the dermatology clinic, Gladman said. Or the situation may be reversed when the rheumatologist needs a dermatology consult, she added.
When that’s not possible, a virtual visit may be the solution, Gladman said. She noted that PPACMAN offers ways to overcome the challenges of running a combined clinic.
Whatever combined clinic model a center chooses, clinicians must be mindful of preventing patients from falling through the cracks, Gladman said.
“When you treat patients separately, the patient sees the rheumatologist, and the rheumatologist wants to do one thing; then they go to the dermatologist and the dermatologist wants to do another thing, and the patient doesn’t do anything because they don’t know what to choose,” she said.
The combined clinic allows the patient to get the opinions of both specialists and avoid the uncertainty about the course of treatment, Gladman added.
Some combined clinics may also house other specialists, such as gastroenterologists, cardiologists, and nurse practitioners, noted Jose U. Scher, MD, director of the Arthritis Clinic and Psoriatic Arthritis Center at NYU Langone Health in New York City. Such centers are typically in academic centers “given challenges with space, scheduling, and reimbursement,” he told Medscape Medical News. NYU has a PPACMAN-registered combined clinic.
Regardless of how combined clinics are organized, Scher said, “We have found that the most important aspect of combined clinics is the open communication and integration of care between and amongst specialists and patients.”
The Potential of Personalized Medicine
“Personalized medicine is where we need to get to,” Gladman told seminar attendees. She said she had hoped it would be further along by now and be more integrated into the care of patients with psoriasis and PsA. “The idea is to identify psoriasis patients that are destined to develop psoriatic arthritis,” she said.
Besides that, identifying biomarkers is key to advancing personalized medicine for psoriasis, Gladman noted.
“In the skin, it’s easy; even the patient can assess their psoriasis,” she said. “But in the joints, it’s very difficult, so it would be nice to have some kind of biomarker, whether it’s the blood or an imaging modality. We want to identify the biomarkers for drug response or lack thereof so we know what drugs would be appropriate for the individual patient, and therefore, we can provide the right drug for the right person and fortunately at the right time.”
In explaining why personalized medicine isn’t further along in dermatology and rheumatology, Gladman told Medscape Medical News, “It’s a matter of finding the right things; we haven’t solved the mystery.” She cited a previous discussion at the seminar about the pathogenesis of PsA. “One person thinks it’s the bone marrow and another thinks it’s the T cells, so we haven’t quite put it all together to have a definitive answer.”
Personalized medicine in psoriasis and PsA is a “key unmet need,” Scher said. “Multiomics” — a biological analysis approach that uses multiple “omes,” such as the genome and microbiome — digital features, and wearables “can unlock novel diagnostic and therapeutic pathways that are desperately needed to enhance clinical response in PsA,” he said.
Also emerging are humanized animal models for laboratory research, which Scher called “potentially very useful tools to personalize approaches to PsA pathogenesis and treatment.”
Gladman disclosed financial relationships with AbbVie, Amgen, Bristol Myers Squibb, Eli Lilly, Galapagos, Gilead, Janssen, Novartis, Pfizer, and UCB. Scher had no relevant financial relationships.
A version of this article first appeared on Medscape.com.
NEW YORK CITY — The idea of having dermatologists and rheumatologists under one roof to see patients with psoriasis prone to psoriatic arthritis (PsA) — a concept known as combined clinics — has been around for more than a decade, and the idea of personalized medicine for these patients even longer than that, yet both approaches to care have encountered a host of obstacles, a longtime research rheumatologist said.
“It’s important that we work together, but there is a problem in terms of staffing — managing the meetings with patients together — and in the states in particular it’s a matter of who’s charging for what,” Dafna Gladman, MD, a rheumatologist at the University of Toronto, in Ontario, Canada, told attendees at the annual New York University (NYU) Langone Advanced Seminar in Psoriasis and Psoriatic Arthritis. Her institution has one of the 44 worldwide combined clinics registered in the Psoriasis & Psoriatic Arthritis Clinics Multicenter Advancement Network (PPACMAN), of which Gladman is an advisory board member.
Barriers to Combined Clinics
“Some of the barriers are physical in the sense that, for the dermatologists and rheumatologists to work at the same time, you need the right space, and in many places, you just don’t have the space to have the two specialists sitting at the same time,” Gladman told Medscape Medical News.
Some centers get around this by having the dermatology and rheumatology clinics next to or near each other. “So these two specialists are close enough to be able to go from room to room,” she added.
Another challenge facing combined clinics lies in the nature of how dermatologists and rheumatologists see patients. “The dermatologist sees patients a lot faster than the rheumatologist, so if the dermatologist and rheumatologist are sitting together, the dermatologist may not see as many patients as they would otherwise and therefore may not get reimbursed properly,” Gladman said.
To overcome these challenges, different models have emerged, Gladman said. If space allows, the ideal model is to have both specialties in one clinic, she said, while compensating for the different pace at which dermatologists and rheumatologists see patients.
The other model is to locate the two clinics close enough so that a person with suspected PsA can get to the rheumatology clinic soon after their dermatologic consult, or the rheumatologist can go to the dermatology clinic, Gladman said. Or the situation may be reversed when the rheumatologist needs a dermatology consult, she added.
When that’s not possible, a virtual visit may be the solution, Gladman said. She noted that PPACMAN offers ways to overcome the challenges of running a combined clinic.
Whatever combined clinic model a center chooses, clinicians must be mindful of preventing patients from falling through the cracks, Gladman said.
“When you treat patients separately, the patient sees the rheumatologist, and the rheumatologist wants to do one thing; then they go to the dermatologist and the dermatologist wants to do another thing, and the patient doesn’t do anything because they don’t know what to choose,” she said.
The combined clinic allows the patient to get the opinions of both specialists and avoid the uncertainty about the course of treatment, Gladman added.
Some combined clinics may also house other specialists, such as gastroenterologists, cardiologists, and nurse practitioners, noted Jose U. Scher, MD, director of the Arthritis Clinic and Psoriatic Arthritis Center at NYU Langone Health in New York City. Such centers are typically in academic centers “given challenges with space, scheduling, and reimbursement,” he told Medscape Medical News. NYU has a PPACMAN-registered combined clinic.
Regardless of how combined clinics are organized, Scher said, “We have found that the most important aspect of combined clinics is the open communication and integration of care between and amongst specialists and patients.”
The Potential of Personalized Medicine
“Personalized medicine is where we need to get to,” Gladman told seminar attendees. She said she had hoped it would be further along by now and be more integrated into the care of patients with psoriasis and PsA. “The idea is to identify psoriasis patients that are destined to develop psoriatic arthritis,” she said.
Besides that, identifying biomarkers is key to advancing personalized medicine for psoriasis, Gladman noted.
“In the skin, it’s easy; even the patient can assess their psoriasis,” she said. “But in the joints, it’s very difficult, so it would be nice to have some kind of biomarker, whether it’s the blood or an imaging modality. We want to identify the biomarkers for drug response or lack thereof so we know what drugs would be appropriate for the individual patient, and therefore, we can provide the right drug for the right person and fortunately at the right time.”
In explaining why personalized medicine isn’t further along in dermatology and rheumatology, Gladman told Medscape Medical News, “It’s a matter of finding the right things; we haven’t solved the mystery.” She cited a previous discussion at the seminar about the pathogenesis of PsA. “One person thinks it’s the bone marrow and another thinks it’s the T cells, so we haven’t quite put it all together to have a definitive answer.”
Personalized medicine in psoriasis and PsA is a “key unmet need,” Scher said. “Multiomics” — a biological analysis approach that uses multiple “omes,” such as the genome and microbiome — digital features, and wearables “can unlock novel diagnostic and therapeutic pathways that are desperately needed to enhance clinical response in PsA,” he said.
Also emerging are humanized animal models for laboratory research, which Scher called “potentially very useful tools to personalize approaches to PsA pathogenesis and treatment.”
Gladman disclosed financial relationships with AbbVie, Amgen, Bristol Myers Squibb, Eli Lilly, Galapagos, Gilead, Janssen, Novartis, Pfizer, and UCB. Scher had no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FDA Approves Ustekinumab Biosimilar Steqeyma, the Seventh of Its Kind
The Food and Drug Administration (FDA) has approved ustekinumab-stba (Steqeyma) as a biosimilar to the interleukin-12 and -23 inhibitor ustekinumab (Stelara) for the treatment of adults with active Crohn’s disease or ulcerative colitis and for both children aged ≥ 6 years and adults with moderate to severe plaque psoriasis or active psoriatic arthritis.
This is the seventh ustekinumab biosimilar approved by the FDA. The biosimilar, developed by Celltrion, has a license entry date in February 2025 as part of the settlement and license agreement with the manufacturer of the reference biologic, Johnson & Johnson.
Ustekinumab-stba will be available in two formulations: A subcutaneous injection in two strengths — a 45 mg/0.5 mL or 90 mg/1 mL solution in a single-dose, prefilled syringe — and an intravenous infusion of a 130 mg/26 mL (5 mg/mL) solution in a single-dose vial.
“The approval of Steqeyma reflects Celltrion’s continued investment in providing treatment options to patients diagnosed with ulcerative colitis, Crohn’s disease, psoriasis, and psoriatic arthritis,” said Thomas Nusbickel, Chief Commercial Officer at Celltrion USA, Jersey City, New Jersey, in a press release.
The FDA has previously approved the company’s adalimumab biosimilar Yuflyma and its infliximab biosimilar Zymfentra.
The full prescribing information for ustekinumab-stba is available here.
A version of this article first appeared on Medscape.com.
The Food and Drug Administration (FDA) has approved ustekinumab-stba (Steqeyma) as a biosimilar to the interleukin-12 and -23 inhibitor ustekinumab (Stelara) for the treatment of adults with active Crohn’s disease or ulcerative colitis and for both children aged ≥ 6 years and adults with moderate to severe plaque psoriasis or active psoriatic arthritis.
This is the seventh ustekinumab biosimilar approved by the FDA. The biosimilar, developed by Celltrion, has a license entry date in February 2025 as part of the settlement and license agreement with the manufacturer of the reference biologic, Johnson & Johnson.
Ustekinumab-stba will be available in two formulations: A subcutaneous injection in two strengths — a 45 mg/0.5 mL or 90 mg/1 mL solution in a single-dose, prefilled syringe — and an intravenous infusion of a 130 mg/26 mL (5 mg/mL) solution in a single-dose vial.
“The approval of Steqeyma reflects Celltrion’s continued investment in providing treatment options to patients diagnosed with ulcerative colitis, Crohn’s disease, psoriasis, and psoriatic arthritis,” said Thomas Nusbickel, Chief Commercial Officer at Celltrion USA, Jersey City, New Jersey, in a press release.
The FDA has previously approved the company’s adalimumab biosimilar Yuflyma and its infliximab biosimilar Zymfentra.
The full prescribing information for ustekinumab-stba is available here.
A version of this article first appeared on Medscape.com.
The Food and Drug Administration (FDA) has approved ustekinumab-stba (Steqeyma) as a biosimilar to the interleukin-12 and -23 inhibitor ustekinumab (Stelara) for the treatment of adults with active Crohn’s disease or ulcerative colitis and for both children aged ≥ 6 years and adults with moderate to severe plaque psoriasis or active psoriatic arthritis.
This is the seventh ustekinumab biosimilar approved by the FDA. The biosimilar, developed by Celltrion, has a license entry date in February 2025 as part of the settlement and license agreement with the manufacturer of the reference biologic, Johnson & Johnson.
Ustekinumab-stba will be available in two formulations: A subcutaneous injection in two strengths — a 45 mg/0.5 mL or 90 mg/1 mL solution in a single-dose, prefilled syringe — and an intravenous infusion of a 130 mg/26 mL (5 mg/mL) solution in a single-dose vial.
“The approval of Steqeyma reflects Celltrion’s continued investment in providing treatment options to patients diagnosed with ulcerative colitis, Crohn’s disease, psoriasis, and psoriatic arthritis,” said Thomas Nusbickel, Chief Commercial Officer at Celltrion USA, Jersey City, New Jersey, in a press release.
The FDA has previously approved the company’s adalimumab biosimilar Yuflyma and its infliximab biosimilar Zymfentra.
The full prescribing information for ustekinumab-stba is available here.
A version of this article first appeared on Medscape.com.
Optimal Exercise Levels for Dermatology Patients With Psoriasis
Optimal Exercise Levels for Dermatology Patients With Psoriasis
There is a direct link between psoriasis and metabolic conditions such as diabetes mellitus and obesity.1 Exercise of varied intensity in patients with chronic inflammatory and metabolic conditions can help improve quality of life and severity of disease; however, there has not been a clear consensus on the recommended duration and types of exercise that are most advantageous.1-5 We reviewed the literature to identify physical and mental health impacts of exercise on patients with psoriasis, and we present the recommended duration and types of exercise that are most impactful for these patients.
One indicator of the link between psoriasis and exercise is the level of peroxisome proliferator activated receptor gamma coactivator-1 α (PGC-1α) in muscle cells.2 This marker reduces inflammation. When levels are low in muscle cells, an induction occurs that leads to systemic or local inflammation; however, skeletal muscle PGC-1α levels increase following exercise, indicating reduced inflammation.2 The level of PGC-1α is measured through muscle biopsy and polymerase chain reaction.6 Another indicator of the correlation between exercise and inflammation is lipoprotein-associated phospholipase A2, which is produced by inflammatory cells and has a correlation with cardiovascular disease. Exercise reduces lipoprotein-associated phospholipase A2 levels, and a sedentary lifestyle correlates with increased levels of this marker.3 Lipoprotein-associated phospholipase A2 is measured through an enzyme-linked immunosorbent assay of the blood, with levels around 200 ng/mL considered high.7 Patients with psoriasis are 30% less likely to participate in physical activity compared to patients without psoriasis, which can be attributed to psychosocial impairment and other factors. Sedentary lifestyle is associated with new or worsening metabolic disease and prevalence of psoriatic lesions.1
A metabolic equivalent task score is a classification system that measures the rate of the body’s oxygen uptake for any given activity.4 A score of 20.9 or more metabolic equivalent task hours of vigorous exercise per week—equal to 105 minutes of running or 180 minutes of swimming or playing tennis—is linked with a 25% to 30% risk reduction of psoriasis in women.4 Therefore, we recommend 30 minutes of exercise 4 to 5 times per week for women. These periods of exercise should consist mainly of activities that will not cause psoriasis flares due to excessive sweating, skin trauma, or prolonged sun exposure.5 Walking, yoga, and bike riding all could be good exercise options for those with psoriasis. The National Psoriasis Foundation offers guidance on physical activity in patients with psoriasis or psoriatic arthritis.8 Psoriasis has apparent physical and psychosocial impacts on patients that can be prevented and improved through the exercise recommendations presented in this article. Dermatologists should use these recommendations to address psoriasis in their everyday practice.
- Do YK, Lakhani N, Malhotra R, et al. Association between psoriasis and leisure-time physical activity: findings from the National Health and Nutrition Examination Survey. J Dermatol. 2015;42:148-153. doi:10.1111/1346-8138.12721
- Handschin C, Spiegelman BM. The role of exercise and PGC1alpha in inflammation and chronic disease. Nature. 2008;454: 463-469. doi:10.1038/nature07206
- Clark K, Sharp S, Womack CJ, et al. Increased sedentary time and decreased physical activity increases lipoprotein associated phospholipase A2 in obese individuals. Nutr Metab Cardiovasc Dis. 2022;32:1703-1710. doi:10.1016/j.numecd.2022.04.023
- Yeh C, Flatley E, Elkattawy O, et al. Exercise in dermatology: exercise’s influence on skin aging, skin cancer, psoriasis, venous ulcers, and androgenetic alopecia. J Am Acad Dermatol. 2022;87:183-184. doi:10.1016/j.jaad.2021.07.023
- Sheppard R, Gan WK, Onambele-Pearson GL, et al. Developing an aerobic exercise intervention for patients with psoriasis to support lifestyle behaviour change and improve health outcomes. Clin Exp Dermatol. 2023;48:5-11. doi:10.1093/ced/llac008
- Lin J, Wu H, Tarr P, et al. Transcriptional co-activator PGC-1a drives the formation of slow-twitch muscle fibres. Nature. 2002;418:797-801. doi:10.1038/nature00904
- Lin J, Wu H, Tarr P, et al. Transcriptional co-activator PGC-1a drives the formation of slow-twitch muscle fibres. Nature. 2002;418:797-801. doi:10.1038/nature00904.023
- National Psoriasis Foundation. Active and mindful lifestyles. https://www.psoriasis.org/active-and-mindful-lifestyles/
There is a direct link between psoriasis and metabolic conditions such as diabetes mellitus and obesity.1 Exercise of varied intensity in patients with chronic inflammatory and metabolic conditions can help improve quality of life and severity of disease; however, there has not been a clear consensus on the recommended duration and types of exercise that are most advantageous.1-5 We reviewed the literature to identify physical and mental health impacts of exercise on patients with psoriasis, and we present the recommended duration and types of exercise that are most impactful for these patients.
One indicator of the link between psoriasis and exercise is the level of peroxisome proliferator activated receptor gamma coactivator-1 α (PGC-1α) in muscle cells.2 This marker reduces inflammation. When levels are low in muscle cells, an induction occurs that leads to systemic or local inflammation; however, skeletal muscle PGC-1α levels increase following exercise, indicating reduced inflammation.2 The level of PGC-1α is measured through muscle biopsy and polymerase chain reaction.6 Another indicator of the correlation between exercise and inflammation is lipoprotein-associated phospholipase A2, which is produced by inflammatory cells and has a correlation with cardiovascular disease. Exercise reduces lipoprotein-associated phospholipase A2 levels, and a sedentary lifestyle correlates with increased levels of this marker.3 Lipoprotein-associated phospholipase A2 is measured through an enzyme-linked immunosorbent assay of the blood, with levels around 200 ng/mL considered high.7 Patients with psoriasis are 30% less likely to participate in physical activity compared to patients without psoriasis, which can be attributed to psychosocial impairment and other factors. Sedentary lifestyle is associated with new or worsening metabolic disease and prevalence of psoriatic lesions.1
A metabolic equivalent task score is a classification system that measures the rate of the body’s oxygen uptake for any given activity.4 A score of 20.9 or more metabolic equivalent task hours of vigorous exercise per week—equal to 105 minutes of running or 180 minutes of swimming or playing tennis—is linked with a 25% to 30% risk reduction of psoriasis in women.4 Therefore, we recommend 30 minutes of exercise 4 to 5 times per week for women. These periods of exercise should consist mainly of activities that will not cause psoriasis flares due to excessive sweating, skin trauma, or prolonged sun exposure.5 Walking, yoga, and bike riding all could be good exercise options for those with psoriasis. The National Psoriasis Foundation offers guidance on physical activity in patients with psoriasis or psoriatic arthritis.8 Psoriasis has apparent physical and psychosocial impacts on patients that can be prevented and improved through the exercise recommendations presented in this article. Dermatologists should use these recommendations to address psoriasis in their everyday practice.
There is a direct link between psoriasis and metabolic conditions such as diabetes mellitus and obesity.1 Exercise of varied intensity in patients with chronic inflammatory and metabolic conditions can help improve quality of life and severity of disease; however, there has not been a clear consensus on the recommended duration and types of exercise that are most advantageous.1-5 We reviewed the literature to identify physical and mental health impacts of exercise on patients with psoriasis, and we present the recommended duration and types of exercise that are most impactful for these patients.
One indicator of the link between psoriasis and exercise is the level of peroxisome proliferator activated receptor gamma coactivator-1 α (PGC-1α) in muscle cells.2 This marker reduces inflammation. When levels are low in muscle cells, an induction occurs that leads to systemic or local inflammation; however, skeletal muscle PGC-1α levels increase following exercise, indicating reduced inflammation.2 The level of PGC-1α is measured through muscle biopsy and polymerase chain reaction.6 Another indicator of the correlation between exercise and inflammation is lipoprotein-associated phospholipase A2, which is produced by inflammatory cells and has a correlation with cardiovascular disease. Exercise reduces lipoprotein-associated phospholipase A2 levels, and a sedentary lifestyle correlates with increased levels of this marker.3 Lipoprotein-associated phospholipase A2 is measured through an enzyme-linked immunosorbent assay of the blood, with levels around 200 ng/mL considered high.7 Patients with psoriasis are 30% less likely to participate in physical activity compared to patients without psoriasis, which can be attributed to psychosocial impairment and other factors. Sedentary lifestyle is associated with new or worsening metabolic disease and prevalence of psoriatic lesions.1
A metabolic equivalent task score is a classification system that measures the rate of the body’s oxygen uptake for any given activity.4 A score of 20.9 or more metabolic equivalent task hours of vigorous exercise per week—equal to 105 minutes of running or 180 minutes of swimming or playing tennis—is linked with a 25% to 30% risk reduction of psoriasis in women.4 Therefore, we recommend 30 minutes of exercise 4 to 5 times per week for women. These periods of exercise should consist mainly of activities that will not cause psoriasis flares due to excessive sweating, skin trauma, or prolonged sun exposure.5 Walking, yoga, and bike riding all could be good exercise options for those with psoriasis. The National Psoriasis Foundation offers guidance on physical activity in patients with psoriasis or psoriatic arthritis.8 Psoriasis has apparent physical and psychosocial impacts on patients that can be prevented and improved through the exercise recommendations presented in this article. Dermatologists should use these recommendations to address psoriasis in their everyday practice.
- Do YK, Lakhani N, Malhotra R, et al. Association between psoriasis and leisure-time physical activity: findings from the National Health and Nutrition Examination Survey. J Dermatol. 2015;42:148-153. doi:10.1111/1346-8138.12721
- Handschin C, Spiegelman BM. The role of exercise and PGC1alpha in inflammation and chronic disease. Nature. 2008;454: 463-469. doi:10.1038/nature07206
- Clark K, Sharp S, Womack CJ, et al. Increased sedentary time and decreased physical activity increases lipoprotein associated phospholipase A2 in obese individuals. Nutr Metab Cardiovasc Dis. 2022;32:1703-1710. doi:10.1016/j.numecd.2022.04.023
- Yeh C, Flatley E, Elkattawy O, et al. Exercise in dermatology: exercise’s influence on skin aging, skin cancer, psoriasis, venous ulcers, and androgenetic alopecia. J Am Acad Dermatol. 2022;87:183-184. doi:10.1016/j.jaad.2021.07.023
- Sheppard R, Gan WK, Onambele-Pearson GL, et al. Developing an aerobic exercise intervention for patients with psoriasis to support lifestyle behaviour change and improve health outcomes. Clin Exp Dermatol. 2023;48:5-11. doi:10.1093/ced/llac008
- Lin J, Wu H, Tarr P, et al. Transcriptional co-activator PGC-1a drives the formation of slow-twitch muscle fibres. Nature. 2002;418:797-801. doi:10.1038/nature00904
- Lin J, Wu H, Tarr P, et al. Transcriptional co-activator PGC-1a drives the formation of slow-twitch muscle fibres. Nature. 2002;418:797-801. doi:10.1038/nature00904.023
- National Psoriasis Foundation. Active and mindful lifestyles. https://www.psoriasis.org/active-and-mindful-lifestyles/
- Do YK, Lakhani N, Malhotra R, et al. Association between psoriasis and leisure-time physical activity: findings from the National Health and Nutrition Examination Survey. J Dermatol. 2015;42:148-153. doi:10.1111/1346-8138.12721
- Handschin C, Spiegelman BM. The role of exercise and PGC1alpha in inflammation and chronic disease. Nature. 2008;454: 463-469. doi:10.1038/nature07206
- Clark K, Sharp S, Womack CJ, et al. Increased sedentary time and decreased physical activity increases lipoprotein associated phospholipase A2 in obese individuals. Nutr Metab Cardiovasc Dis. 2022;32:1703-1710. doi:10.1016/j.numecd.2022.04.023
- Yeh C, Flatley E, Elkattawy O, et al. Exercise in dermatology: exercise’s influence on skin aging, skin cancer, psoriasis, venous ulcers, and androgenetic alopecia. J Am Acad Dermatol. 2022;87:183-184. doi:10.1016/j.jaad.2021.07.023
- Sheppard R, Gan WK, Onambele-Pearson GL, et al. Developing an aerobic exercise intervention for patients with psoriasis to support lifestyle behaviour change and improve health outcomes. Clin Exp Dermatol. 2023;48:5-11. doi:10.1093/ced/llac008
- Lin J, Wu H, Tarr P, et al. Transcriptional co-activator PGC-1a drives the formation of slow-twitch muscle fibres. Nature. 2002;418:797-801. doi:10.1038/nature00904
- Lin J, Wu H, Tarr P, et al. Transcriptional co-activator PGC-1a drives the formation of slow-twitch muscle fibres. Nature. 2002;418:797-801. doi:10.1038/nature00904.023
- National Psoriasis Foundation. Active and mindful lifestyles. https://www.psoriasis.org/active-and-mindful-lifestyles/
Optimal Exercise Levels for Dermatology Patients With Psoriasis
Optimal Exercise Levels for Dermatology Patients With Psoriasis
PRACTICE POINTS
- Patients with psoriasis should exercise for less time (~30 min) more frequently (4–5 times per week).
- Exercise that involves excessive sweating should be avoided; recommended types of exercise for patients with psoriasis include walking, yoga, and bike riding.
- Physicians should educate patients on the processes behind psoriasis and direct them to the National Psoriasis Foundation’s website when needed.
Geriatric Dermatology: Q&A With Daniel C. Butler, MD
Daniel C. Butler, MD, is associate professor of dermatology and director of the new Inflammatory and Aging Skin Research Program in the Division of Dermatology at the University of Arizona College of Medicine, Tucson, Arizona. Before returning to Arizona, where he had attended medical school, Butler practiced and was a researcher at the University of California, San Francisco, and its geriatric dermatology clinic. He is a co-founder and continues to co-lead the American Academy of Dermatology (AAD) Geriatric Dermatology Expert Resource Group (ERG).
Butler’s interest in geriatric dermatology is rooted in his experience growing up with four grandparents and witnessing their wisdom, relationships, moments with loved ones, and other unique and desirable parts of growing old. “When I looked later at how aging was perceived in dermatology, I found it was a lot about ‘antiaging,’” he told this news organization. “I thought there was a needed voice in dermatology for healthy aging, for all the desirable things that only growing old can provide, along with all the incredible ‘antiaging’ things we can do.”
In interviews, Butler spoke about research priorities in geriatric dermatology, how the “4M” model of geriatrics should be applied within dermatology, how dermatologists can best work with older complex patients, and more. The conversation was edited for clarity and length.
What is geriatric dermatology? It is described by the AAD’s Geriatric Dermatology ERG as “an emerging subspecialty.” Yet it’s also viewed more broadly. Please speak about its various identities and meanings and its importance for dermatology.
If you’re a Mohs surgeon, you’re seeing a strong majority of over 65 patients. And in various specialty clinics, such as inflammatory skin disease, geriatric dermatology pertains to you. In many ways, it can be viewed as a mindset.
From a framework standpoint, and as a field, geriatric dermatology is a basic science initiative, a clinical initiative, an educational initiative, and an advocacy initiative. The goal is to be able to influence, grow, and learn in each of these categories for our older patients. This is happening: Research in this field has progressed, and education has progressed, which has driven some progress in clinical care.
How has research progressed in the basic science of aging skin? What are key questions for dermatology?
There has been a lot of basic science research on aging skin and on how an aging immune system, for instance, is reflected in conditions such as bullous pemphigoid, atopic dermatitis (AD), and chronic itch. But aging involves more than immunosenescence. I think of aging skin as a three-headed monster that involves changes in the skin barrier and the microbiome as well. But is there a primary piece of aging in the skin? What comes first or influences the other? More research on these questions can potentially influence our treatments.
With respect to the immune system, what we’re finding in the skin is that age-related change is not a decline in the immune system per se, but rather aberrance in response. Parts of the system tend to become overactive, with a skew toward overexpression of type 2 inflammation. This can be problematic, driving conditions such as chronic itch.
With respect to the skin barrier, we lose essential fatty acids, and we lose a lot of our recovery ability and our ability to respond quickly to environmental stressors. But are barrier changes triggering the immune system? Or is it the other way around?
The microbiome, which is a big focus of research, involves similar chicken-and-egg discussions. Is it the microbiome that changes and alters the barrier, which then entices the immune system? Which one happens first? We have a lot to learn, and there’s probably not one answer for every patient.
Please speak about research more broadly. What questions and issues need to be answered and addressed to improve the dermatologic care of older adults?
In general, research in dermatology is very disease-specific and not particularly conducive to looking at the larger demographic populations. We have a huge opportunity, therefore, to break the mold and grow geriatric dermatology as an area of population-based research — so that geriatric dermatology research encompasses not only the melanoma researcher who’s trying to understand how aging influences the melanocytes but also the epidemiologic researcher looking at how our diagnoses and coding and prescription practices are different in the 65-plus age group.
Clinically speaking, researchers want to better understand how aging influences the clinical presentations of our diseases. And there’s research to be done on best practices. For example, what are the best practices for treating basal cell carcinomas in patients with mild cognitive impairment? How should we consider the use of topicals in a patient who has severe arthritis or who lives alone? And then how should we teach practical approaches to help providers meet people where they are?
Looking at it from a healthcare system standpoint, there are many care delivery and access issues — practical pieces — to research, and we’re getting a lot better with this. We’re also advocating not only for more inclusion of older adults in clinical trials of treatments but also for the use of evaluations and outcomes that are relevant and important for older adults.
One piece of good news is that we’re seeing safer treatment options with tremendous efficacy that target known pathways for diseases like AD and chronic itch that affect older adults. Again, now we must find ways to improve access to these novel, safe options.
Our research program at the University of Arizona College of Medicine, which we’re just getting off the ground, aims to be dual-sided, looking both at the basic science of aging skin and at access and care delivery issues, such as how to ensure that patients on Medicare have access to medications that are at least on par with others with private insurance.
What are the most common dermatologic problems experienced by older adults?
Based on my experience and on research that we expect to be published soon, it’s absolutely nonmelanoma skin cancers, precancers like actinic keratoses — and on the inflammatory disease side, itch, AD, and psoriasis. Of course, also common are the age-related changes to the skin that we put in the benign category, such as solar lentigines.
How does age influence dermatologic diseases from a pathophysiological and clinical standpoint?
Diseases overall are very similar and respond to the same treatments, but age in and of itself does influence little pieces. For example, there is more crossover in the presentation of psoriasis and AD in older adults, leading to delays in the diagnosis of psoriasis.
With AD, we’ve found that itch is the predominant symptom for older adults rather than the red rash. We see higher or more severe itch scores in older adults with AD with less visual changes on the skin than in younger cohorts. And rash occurs in different locations than in young patients. Older adults typically present with it on their chest, back, and across the trunk, rather than in folded areas. They’re also more likely to get it on their legs in a nummular pattern as opposed to the more traditional flexural area presentation.
What unique considerations need to be made in treating older adults? How should the 4M model of geriatrics be applied to dermatologic care?
Our care model pushes us to be very algorithmic, but at the end of the day, what’s really important are the 4Ms: Mobility, medication, mentation, and “what matters most.” As you’re having your shared decision-making conversations with your patients and their families, these should be your priorities.
A patient with physical limitations, for instance, may not be able to apply a topical cream twice a day all over the body. They may have comorbidities and treatments for these comorbidities that may conflict with medications you’re considering.
And then mentation is so important. For a long time, we used antihistamines for older adults, but this has been proven to be bad for their mentation and risky in other ways. We need to be sure we’re prioritizing their ability to be clear mentally when we’re prescribing medications and even when we’re considering surgical approaches. Do they show capacity for that procedure or treatment, and how will they respond to that treatment later on?
Using the 4M model to drive conversations is a way to get all of us to connect to the patient and learn about what’s most important for them. In many ways, geriatrics is about taking a step back from your specialist skills and thinking about how you would want a family member treated.
We want to avoid treating just the lesion or the pathologic diagnosis. We want to avoid the “conveyor belt” from a biopsy to Mohs. I have 95-year-olds who say, “Heck yeah, if Mohs is the best treatment, that’s what I want.” And I have 70-year-olds who say, “I think I’ll go with another option,” and that’s the right decision for them. It’s having the conversation that matters.
In practice, given time constraints and other confines, how can dermatologists best work with more complex older patients? What are your practical tips?
People talk about having 45-minute “golden year” conversations with their older patients, but it doesn’t have to be this way. In pursuing geriatric dermatology, I decided early on that I wanted to make sure it was practical, so I’ve focused on maximizing shorter visits and on embracing the concept that relationships can be developed over time. Each time we meet with someone, we’re building equity to have bigger conversations later on.
I can have a 15-minute conversation about whether my patient may want to have Mohs surgery, for instance, or escalate treatment to a systemic agent for their chronic inflammatory disease. If that time isn’t enough, I can encourage further thought about treatment options, acknowledge that decisions aren’t necessarily easy, and schedule a follow-up or offer to call the patient after clinic to continue the conversation.
Sometimes, when I’m at an impasse and my patient is unsure how to proceed, I’ll use clear metrics relevant to older adults — sleep, activity level, and caregiver burden — to help my patient. If someone is not sleeping because of their lesion — if they’re so itchy or their inflammatory disease is uncontrolled, for instance — I’ll point out that the side effects of not sleeping are worse than the medications or surgery we’d pursue. If someone removes themselves from an activity due to their skin condition, that’s a red flag. And if the caregiver in the room is overwhelmed or frustrated by having to put cream on twice a day, I’ll use this to advance treatment.
What resources are available for dermatologists interested in improving their geriatric dermatology skills or advancing the area?
For those interested in investigating these issues or improving their practices, the AAD’s Geriatric Dermatology ERG is always welcoming of new members. The ERG will have an all-inclusive meeting at the 2025 annual AAD meeting in March.
The AAD also has educational modules on geriatric dermatology that were recently published as an initiative of our ERG. More information is available on the website. Also valuable is the ElderDerm conference hosted by the George Washington University School of Medicine and Health Sciences, Washington, DC; the second such conference takes place in May 2025.
Butler reported that he had no relevant financial disclosures.
A version of this article appeared on Medscape.com.
Daniel C. Butler, MD, is associate professor of dermatology and director of the new Inflammatory and Aging Skin Research Program in the Division of Dermatology at the University of Arizona College of Medicine, Tucson, Arizona. Before returning to Arizona, where he had attended medical school, Butler practiced and was a researcher at the University of California, San Francisco, and its geriatric dermatology clinic. He is a co-founder and continues to co-lead the American Academy of Dermatology (AAD) Geriatric Dermatology Expert Resource Group (ERG).
Butler’s interest in geriatric dermatology is rooted in his experience growing up with four grandparents and witnessing their wisdom, relationships, moments with loved ones, and other unique and desirable parts of growing old. “When I looked later at how aging was perceived in dermatology, I found it was a lot about ‘antiaging,’” he told this news organization. “I thought there was a needed voice in dermatology for healthy aging, for all the desirable things that only growing old can provide, along with all the incredible ‘antiaging’ things we can do.”
In interviews, Butler spoke about research priorities in geriatric dermatology, how the “4M” model of geriatrics should be applied within dermatology, how dermatologists can best work with older complex patients, and more. The conversation was edited for clarity and length.
What is geriatric dermatology? It is described by the AAD’s Geriatric Dermatology ERG as “an emerging subspecialty.” Yet it’s also viewed more broadly. Please speak about its various identities and meanings and its importance for dermatology.
If you’re a Mohs surgeon, you’re seeing a strong majority of over 65 patients. And in various specialty clinics, such as inflammatory skin disease, geriatric dermatology pertains to you. In many ways, it can be viewed as a mindset.
From a framework standpoint, and as a field, geriatric dermatology is a basic science initiative, a clinical initiative, an educational initiative, and an advocacy initiative. The goal is to be able to influence, grow, and learn in each of these categories for our older patients. This is happening: Research in this field has progressed, and education has progressed, which has driven some progress in clinical care.
How has research progressed in the basic science of aging skin? What are key questions for dermatology?
There has been a lot of basic science research on aging skin and on how an aging immune system, for instance, is reflected in conditions such as bullous pemphigoid, atopic dermatitis (AD), and chronic itch. But aging involves more than immunosenescence. I think of aging skin as a three-headed monster that involves changes in the skin barrier and the microbiome as well. But is there a primary piece of aging in the skin? What comes first or influences the other? More research on these questions can potentially influence our treatments.
With respect to the immune system, what we’re finding in the skin is that age-related change is not a decline in the immune system per se, but rather aberrance in response. Parts of the system tend to become overactive, with a skew toward overexpression of type 2 inflammation. This can be problematic, driving conditions such as chronic itch.
With respect to the skin barrier, we lose essential fatty acids, and we lose a lot of our recovery ability and our ability to respond quickly to environmental stressors. But are barrier changes triggering the immune system? Or is it the other way around?
The microbiome, which is a big focus of research, involves similar chicken-and-egg discussions. Is it the microbiome that changes and alters the barrier, which then entices the immune system? Which one happens first? We have a lot to learn, and there’s probably not one answer for every patient.
Please speak about research more broadly. What questions and issues need to be answered and addressed to improve the dermatologic care of older adults?
In general, research in dermatology is very disease-specific and not particularly conducive to looking at the larger demographic populations. We have a huge opportunity, therefore, to break the mold and grow geriatric dermatology as an area of population-based research — so that geriatric dermatology research encompasses not only the melanoma researcher who’s trying to understand how aging influences the melanocytes but also the epidemiologic researcher looking at how our diagnoses and coding and prescription practices are different in the 65-plus age group.
Clinically speaking, researchers want to better understand how aging influences the clinical presentations of our diseases. And there’s research to be done on best practices. For example, what are the best practices for treating basal cell carcinomas in patients with mild cognitive impairment? How should we consider the use of topicals in a patient who has severe arthritis or who lives alone? And then how should we teach practical approaches to help providers meet people where they are?
Looking at it from a healthcare system standpoint, there are many care delivery and access issues — practical pieces — to research, and we’re getting a lot better with this. We’re also advocating not only for more inclusion of older adults in clinical trials of treatments but also for the use of evaluations and outcomes that are relevant and important for older adults.
One piece of good news is that we’re seeing safer treatment options with tremendous efficacy that target known pathways for diseases like AD and chronic itch that affect older adults. Again, now we must find ways to improve access to these novel, safe options.
Our research program at the University of Arizona College of Medicine, which we’re just getting off the ground, aims to be dual-sided, looking both at the basic science of aging skin and at access and care delivery issues, such as how to ensure that patients on Medicare have access to medications that are at least on par with others with private insurance.
What are the most common dermatologic problems experienced by older adults?
Based on my experience and on research that we expect to be published soon, it’s absolutely nonmelanoma skin cancers, precancers like actinic keratoses — and on the inflammatory disease side, itch, AD, and psoriasis. Of course, also common are the age-related changes to the skin that we put in the benign category, such as solar lentigines.
How does age influence dermatologic diseases from a pathophysiological and clinical standpoint?
Diseases overall are very similar and respond to the same treatments, but age in and of itself does influence little pieces. For example, there is more crossover in the presentation of psoriasis and AD in older adults, leading to delays in the diagnosis of psoriasis.
With AD, we’ve found that itch is the predominant symptom for older adults rather than the red rash. We see higher or more severe itch scores in older adults with AD with less visual changes on the skin than in younger cohorts. And rash occurs in different locations than in young patients. Older adults typically present with it on their chest, back, and across the trunk, rather than in folded areas. They’re also more likely to get it on their legs in a nummular pattern as opposed to the more traditional flexural area presentation.
What unique considerations need to be made in treating older adults? How should the 4M model of geriatrics be applied to dermatologic care?
Our care model pushes us to be very algorithmic, but at the end of the day, what’s really important are the 4Ms: Mobility, medication, mentation, and “what matters most.” As you’re having your shared decision-making conversations with your patients and their families, these should be your priorities.
A patient with physical limitations, for instance, may not be able to apply a topical cream twice a day all over the body. They may have comorbidities and treatments for these comorbidities that may conflict with medications you’re considering.
And then mentation is so important. For a long time, we used antihistamines for older adults, but this has been proven to be bad for their mentation and risky in other ways. We need to be sure we’re prioritizing their ability to be clear mentally when we’re prescribing medications and even when we’re considering surgical approaches. Do they show capacity for that procedure or treatment, and how will they respond to that treatment later on?
Using the 4M model to drive conversations is a way to get all of us to connect to the patient and learn about what’s most important for them. In many ways, geriatrics is about taking a step back from your specialist skills and thinking about how you would want a family member treated.
We want to avoid treating just the lesion or the pathologic diagnosis. We want to avoid the “conveyor belt” from a biopsy to Mohs. I have 95-year-olds who say, “Heck yeah, if Mohs is the best treatment, that’s what I want.” And I have 70-year-olds who say, “I think I’ll go with another option,” and that’s the right decision for them. It’s having the conversation that matters.
In practice, given time constraints and other confines, how can dermatologists best work with more complex older patients? What are your practical tips?
People talk about having 45-minute “golden year” conversations with their older patients, but it doesn’t have to be this way. In pursuing geriatric dermatology, I decided early on that I wanted to make sure it was practical, so I’ve focused on maximizing shorter visits and on embracing the concept that relationships can be developed over time. Each time we meet with someone, we’re building equity to have bigger conversations later on.
I can have a 15-minute conversation about whether my patient may want to have Mohs surgery, for instance, or escalate treatment to a systemic agent for their chronic inflammatory disease. If that time isn’t enough, I can encourage further thought about treatment options, acknowledge that decisions aren’t necessarily easy, and schedule a follow-up or offer to call the patient after clinic to continue the conversation.
Sometimes, when I’m at an impasse and my patient is unsure how to proceed, I’ll use clear metrics relevant to older adults — sleep, activity level, and caregiver burden — to help my patient. If someone is not sleeping because of their lesion — if they’re so itchy or their inflammatory disease is uncontrolled, for instance — I’ll point out that the side effects of not sleeping are worse than the medications or surgery we’d pursue. If someone removes themselves from an activity due to their skin condition, that’s a red flag. And if the caregiver in the room is overwhelmed or frustrated by having to put cream on twice a day, I’ll use this to advance treatment.
What resources are available for dermatologists interested in improving their geriatric dermatology skills or advancing the area?
For those interested in investigating these issues or improving their practices, the AAD’s Geriatric Dermatology ERG is always welcoming of new members. The ERG will have an all-inclusive meeting at the 2025 annual AAD meeting in March.
The AAD also has educational modules on geriatric dermatology that were recently published as an initiative of our ERG. More information is available on the website. Also valuable is the ElderDerm conference hosted by the George Washington University School of Medicine and Health Sciences, Washington, DC; the second such conference takes place in May 2025.
Butler reported that he had no relevant financial disclosures.
A version of this article appeared on Medscape.com.
Daniel C. Butler, MD, is associate professor of dermatology and director of the new Inflammatory and Aging Skin Research Program in the Division of Dermatology at the University of Arizona College of Medicine, Tucson, Arizona. Before returning to Arizona, where he had attended medical school, Butler practiced and was a researcher at the University of California, San Francisco, and its geriatric dermatology clinic. He is a co-founder and continues to co-lead the American Academy of Dermatology (AAD) Geriatric Dermatology Expert Resource Group (ERG).
Butler’s interest in geriatric dermatology is rooted in his experience growing up with four grandparents and witnessing their wisdom, relationships, moments with loved ones, and other unique and desirable parts of growing old. “When I looked later at how aging was perceived in dermatology, I found it was a lot about ‘antiaging,’” he told this news organization. “I thought there was a needed voice in dermatology for healthy aging, for all the desirable things that only growing old can provide, along with all the incredible ‘antiaging’ things we can do.”
In interviews, Butler spoke about research priorities in geriatric dermatology, how the “4M” model of geriatrics should be applied within dermatology, how dermatologists can best work with older complex patients, and more. The conversation was edited for clarity and length.
What is geriatric dermatology? It is described by the AAD’s Geriatric Dermatology ERG as “an emerging subspecialty.” Yet it’s also viewed more broadly. Please speak about its various identities and meanings and its importance for dermatology.
If you’re a Mohs surgeon, you’re seeing a strong majority of over 65 patients. And in various specialty clinics, such as inflammatory skin disease, geriatric dermatology pertains to you. In many ways, it can be viewed as a mindset.
From a framework standpoint, and as a field, geriatric dermatology is a basic science initiative, a clinical initiative, an educational initiative, and an advocacy initiative. The goal is to be able to influence, grow, and learn in each of these categories for our older patients. This is happening: Research in this field has progressed, and education has progressed, which has driven some progress in clinical care.
How has research progressed in the basic science of aging skin? What are key questions for dermatology?
There has been a lot of basic science research on aging skin and on how an aging immune system, for instance, is reflected in conditions such as bullous pemphigoid, atopic dermatitis (AD), and chronic itch. But aging involves more than immunosenescence. I think of aging skin as a three-headed monster that involves changes in the skin barrier and the microbiome as well. But is there a primary piece of aging in the skin? What comes first or influences the other? More research on these questions can potentially influence our treatments.
With respect to the immune system, what we’re finding in the skin is that age-related change is not a decline in the immune system per se, but rather aberrance in response. Parts of the system tend to become overactive, with a skew toward overexpression of type 2 inflammation. This can be problematic, driving conditions such as chronic itch.
With respect to the skin barrier, we lose essential fatty acids, and we lose a lot of our recovery ability and our ability to respond quickly to environmental stressors. But are barrier changes triggering the immune system? Or is it the other way around?
The microbiome, which is a big focus of research, involves similar chicken-and-egg discussions. Is it the microbiome that changes and alters the barrier, which then entices the immune system? Which one happens first? We have a lot to learn, and there’s probably not one answer for every patient.
Please speak about research more broadly. What questions and issues need to be answered and addressed to improve the dermatologic care of older adults?
In general, research in dermatology is very disease-specific and not particularly conducive to looking at the larger demographic populations. We have a huge opportunity, therefore, to break the mold and grow geriatric dermatology as an area of population-based research — so that geriatric dermatology research encompasses not only the melanoma researcher who’s trying to understand how aging influences the melanocytes but also the epidemiologic researcher looking at how our diagnoses and coding and prescription practices are different in the 65-plus age group.
Clinically speaking, researchers want to better understand how aging influences the clinical presentations of our diseases. And there’s research to be done on best practices. For example, what are the best practices for treating basal cell carcinomas in patients with mild cognitive impairment? How should we consider the use of topicals in a patient who has severe arthritis or who lives alone? And then how should we teach practical approaches to help providers meet people where they are?
Looking at it from a healthcare system standpoint, there are many care delivery and access issues — practical pieces — to research, and we’re getting a lot better with this. We’re also advocating not only for more inclusion of older adults in clinical trials of treatments but also for the use of evaluations and outcomes that are relevant and important for older adults.
One piece of good news is that we’re seeing safer treatment options with tremendous efficacy that target known pathways for diseases like AD and chronic itch that affect older adults. Again, now we must find ways to improve access to these novel, safe options.
Our research program at the University of Arizona College of Medicine, which we’re just getting off the ground, aims to be dual-sided, looking both at the basic science of aging skin and at access and care delivery issues, such as how to ensure that patients on Medicare have access to medications that are at least on par with others with private insurance.
What are the most common dermatologic problems experienced by older adults?
Based on my experience and on research that we expect to be published soon, it’s absolutely nonmelanoma skin cancers, precancers like actinic keratoses — and on the inflammatory disease side, itch, AD, and psoriasis. Of course, also common are the age-related changes to the skin that we put in the benign category, such as solar lentigines.
How does age influence dermatologic diseases from a pathophysiological and clinical standpoint?
Diseases overall are very similar and respond to the same treatments, but age in and of itself does influence little pieces. For example, there is more crossover in the presentation of psoriasis and AD in older adults, leading to delays in the diagnosis of psoriasis.
With AD, we’ve found that itch is the predominant symptom for older adults rather than the red rash. We see higher or more severe itch scores in older adults with AD with less visual changes on the skin than in younger cohorts. And rash occurs in different locations than in young patients. Older adults typically present with it on their chest, back, and across the trunk, rather than in folded areas. They’re also more likely to get it on their legs in a nummular pattern as opposed to the more traditional flexural area presentation.
What unique considerations need to be made in treating older adults? How should the 4M model of geriatrics be applied to dermatologic care?
Our care model pushes us to be very algorithmic, but at the end of the day, what’s really important are the 4Ms: Mobility, medication, mentation, and “what matters most.” As you’re having your shared decision-making conversations with your patients and their families, these should be your priorities.
A patient with physical limitations, for instance, may not be able to apply a topical cream twice a day all over the body. They may have comorbidities and treatments for these comorbidities that may conflict with medications you’re considering.
And then mentation is so important. For a long time, we used antihistamines for older adults, but this has been proven to be bad for their mentation and risky in other ways. We need to be sure we’re prioritizing their ability to be clear mentally when we’re prescribing medications and even when we’re considering surgical approaches. Do they show capacity for that procedure or treatment, and how will they respond to that treatment later on?
Using the 4M model to drive conversations is a way to get all of us to connect to the patient and learn about what’s most important for them. In many ways, geriatrics is about taking a step back from your specialist skills and thinking about how you would want a family member treated.
We want to avoid treating just the lesion or the pathologic diagnosis. We want to avoid the “conveyor belt” from a biopsy to Mohs. I have 95-year-olds who say, “Heck yeah, if Mohs is the best treatment, that’s what I want.” And I have 70-year-olds who say, “I think I’ll go with another option,” and that’s the right decision for them. It’s having the conversation that matters.
In practice, given time constraints and other confines, how can dermatologists best work with more complex older patients? What are your practical tips?
People talk about having 45-minute “golden year” conversations with their older patients, but it doesn’t have to be this way. In pursuing geriatric dermatology, I decided early on that I wanted to make sure it was practical, so I’ve focused on maximizing shorter visits and on embracing the concept that relationships can be developed over time. Each time we meet with someone, we’re building equity to have bigger conversations later on.
I can have a 15-minute conversation about whether my patient may want to have Mohs surgery, for instance, or escalate treatment to a systemic agent for their chronic inflammatory disease. If that time isn’t enough, I can encourage further thought about treatment options, acknowledge that decisions aren’t necessarily easy, and schedule a follow-up or offer to call the patient after clinic to continue the conversation.
Sometimes, when I’m at an impasse and my patient is unsure how to proceed, I’ll use clear metrics relevant to older adults — sleep, activity level, and caregiver burden — to help my patient. If someone is not sleeping because of their lesion — if they’re so itchy or their inflammatory disease is uncontrolled, for instance — I’ll point out that the side effects of not sleeping are worse than the medications or surgery we’d pursue. If someone removes themselves from an activity due to their skin condition, that’s a red flag. And if the caregiver in the room is overwhelmed or frustrated by having to put cream on twice a day, I’ll use this to advance treatment.
What resources are available for dermatologists interested in improving their geriatric dermatology skills or advancing the area?
For those interested in investigating these issues or improving their practices, the AAD’s Geriatric Dermatology ERG is always welcoming of new members. The ERG will have an all-inclusive meeting at the 2025 annual AAD meeting in March.
The AAD also has educational modules on geriatric dermatology that were recently published as an initiative of our ERG. More information is available on the website. Also valuable is the ElderDerm conference hosted by the George Washington University School of Medicine and Health Sciences, Washington, DC; the second such conference takes place in May 2025.
Butler reported that he had no relevant financial disclosures.
A version of this article appeared on Medscape.com.
Successful Treatment of Severe Dystrophic Nail Psoriasis With Deucravacitinib
Successful Treatment of Severe Dystrophic Nail Psoriasis With Deucravacitinib
To the Editor:
Psoriasis is a chronic inflammatory skin condition that commonly affects the nail matrix and/or nail bed.1 Nail involvement is present in up to 50% of patients with cutaneous psoriasis and 80% of patients with psoriatic arthritis.1 Approximately 5% to 10% of patients with psoriasis demonstrate isolated nail involvement with no skin or joint manifestations.1 Nail psoriasis can cause severe pain and psychological distress, and extreme cases may cause considerable morbidity and functional impairment.2,3 Treatment often requires a long duration and may not result in complete recovery due to the slow rate of nail growth. Patients can progress to permanent nail loss if not treated properly, making early recognition and treatment crucial.1,2 Despite the availability of various treatment options, many cases remain refractory to standard interventions, which underscores the need for novel therapeutic approaches. Herein, we present a severe case of refractory isolated nail psoriasis that was successfully treated with deucravacitinib, an oral tyrosine kinase 2 (TYK2) inhibitor.
A 59-year-old woman presented with a progressive, yellow, hyperkeratotic lesion on the left thumbnail of 2 years’ duration. The patient noted initial discoloration and peeling at the distal end of the nail. Over time, the discoloration progressed to encompass the entire nail. Previous treatments performed by outside physicians including topical corticosteroids, calcineurin inhibitors, and 2 surgeries to remove the nail plate and nail bed all were unsuccessful. The patient also reported severe left thumbnail pain and pruritus that considerably impaired her ability to work. The rest of the nails were unaffected, and she had no personal or family history of psoriasis. Her medical history was notable for hypertension, gastroesophageal reflux disease, and osteomyelitis of the right thumb without nail involvement. Drug allergies included penicillin G benzathine, sulfonamides, amoxicillin, and ciprofloxacin.
Physical examination of the left thumbnail revealed severe yellow, hyperkeratotic, dystrophic changes with a large, yellow, crumbling hyperkeratotic plaque that extended from approximately 1 cm beyond the nail plate to the proximal end of the distal interphalangeal joint, to and along the lateral nail folds, with extensive distal onycholysis. The proximal and lateral nail folds demonstrated erythema as well as maceration that was extremely tender to minimal palpation (Figure 1). No cutaneous lesions were noted elsewhere on the body. The patient had no tenderness, swelling, or stiffness in any of the joints. The differential diagnosis at the time included squamous cell carcinoma of the nail bed and acrodermatitis continua of Hallopeau.
Radiography of the left thumb revealed irregular swelling and nonspecific soft tissue enlargement at the tip of the digit. A nail clipping from the left thumbnail and 3-mm punch biopsies of the lateral and proximal nail folds as well as the horn of the proximal nail fold (Figure 2) were negative for fungus and confirmed psoriasiform dermatitis of the nail.
The patient was started on vinegar soaks (1:1 ratio of vinegar to water) every other day as well as urea cream 10%, ammonium lactate 15%, and petrolatum twice daily for 2 months without considerable improvement. Due to lack of improvement during this 2-month period, the patient subsequently was started on oral deucravacitinib 6 mg/d along with continued use of petrolatum twice daily and vinegar soaks every other day. We selected a trial of deucravacitinib for our patient because of its convenient daily oral dosing and promising clinical evidence.4,5 After 2 months of treatment with deucravacitinib, the patient reported substantial improvement and satisfaction with the treatment results. Physical examination of the left thumbnail after 2 months of deucravacitinib treatment revealed mildly hyperkeratotic, yellow, dystrophic changes of the nail with notable improvement of the yellow hyperkeratotic plaque on the distal thumbnail. Normal-appearing nail growth was noted at the proximal nail fold, demonstrating considerable improvement from the initial presentation (Figure 3). However, the patient had developed multiple oral ulcers, generalized pruritus, and an annular urticarial plaque on the left arm. As such, deucravacitinib was discontinued after 2 months of treatment. These symptoms resolved within a week of discontinuing deucravacitinib.
While the etiology of nail psoriasis remains unclear, it is believed to be due to a combination of immunologic, genetic, and environmental factors.3 Classical clinical features include nail pitting, leukonychia, onycholysis, nail bed hyperkeratosis, and splinter hemorrhages.1,3 Our patient exhibited a severe form of nail psoriasis, encompassing the entire nail matrix and bed and extending to the distal interphalangeal joint and lateral nail folds. Previous surgical interventions may have triggered the Koebner phenomenon—which commonly is associated with psoriasis—and resulted in new skin lesions as a secondary response to the surgical trauma.6 The severity of the condition profoundly impacted her quality of life and considerably hindered her ability to work.
Treatment for nail psoriasis includes topical or systemic therapies such as corticosteroids, vitamin D analogs, tacrolimus, and tumor necrosis factor α inhibitors.1,3 Topical treatment is challenging because it is difficult to deliver medication effectively to the nail bed and nail matrix, and patient adherence may be poor.2 Although it has been shown to be effective, intralesional triamcinolone can be associated with pain as the most common adverse effect.7 Systemic medications such as oral methotrexate also may be effective but are contraindicated in pregnant patients and are associated with potential adverse events (AEs), including hepatotoxicity and acute kidney injury.8 The use of biologics may be challenging due to potential AEs and patient reluctance toward injection-based treatments.9
Deucravacitinib is a TYK2 inhibitor approved for treatment of plaque psoriasis.10 Tyrosine kinase 2 is an intracellular kinase that mediates the signaling of IL-23 and other cytokines involved in psoriasis pathogenesis.10 Deucravacitinib selectively binds to the regulatory domain of TYK2, leading to targeted allosteric inhibition of TYK2-mediated IL-23 and type I interferon signaling.4,5,10 Compared with biologics, deucravacitinib is advantageous because it can be administered as a daily oral pill, encouraging high patient compliance.
In the POETYK PSO-1 and PSO-2 phase 3 randomized controlled trials, 20.9% (n=332) and 20.3% (n=510) of deucravacitinib-treated patients with moderate to severe nail involvement achieved a Physician’s Global Assessment of Fingernail score of 0/1 compared with 8.8% (n=165) and 7.9% (n=254) of patients in the placebo group, respectively. All patients in these trials had a diagnosis of plaque psoriasis with at least 10% body surface area involvement; none of the patients had isolated nail psoriasis.4,5
The phase 3 POETYK PSO-1 and PSO-2 trials demonstrated deucravacitinib to be safe and well tolerated with minimal AEs.4,5 However, the development of AEs in our patient, including oral ulcers and generalized pruritus, underscores the need for close monitoring and consideration of potential risks of treatment. Common AEs associated with deucravacitinib include upper respiratory infections (19.2% [n=840]), increased blood creatine phosphokinase levels (2.7% [n=840]), herpes simplex virus (2.0% [n=840]), and mouth ulcers (1.9% [n=840]).11
Patient education also is a crucial component in the treatment of nail psoriasis. Physicians should emphasize the slow growth of nails and need for prolonged treatment. Clear communication and realistic expectations are essential for ensuring patient adherence to treatment.
Our case highlights the potential efficacy and safety of deucravacitinib for treatment of nail psoriasis, potentially laying the groundwork for future clinical studies. Our patient had a severe case of nail psoriasis that involved the entire nail bed and nail plate, resulting in extreme pain, pruritus, and functional impairment. Her case was unique because involvement was isolated to the nail without any accompanying skin or joint manifestations. She showed a favorable response to deucravacitinib within only 2 months of treatment and exhibited considerable improvement of nail psoriasis, with a reported high level of satisfaction with the treatment. We plan to continue to monitor the patient for long-term results. Future randomized clinical trials with longer follow-up periods are crucial to further establish the efficacy and safety of deucravacitinib for treatment of nail psoriasis.
- Hwang JK, Grover C, Iorizzo M, et al. Nail psoriasis and nail lichen planus: updates on diagnosis and management. J Am Acad Dermatol. 2024;90:585-596. doi:10.1016/j.jaad.2023.11.024
- Ji C, Wang H, Bao C, et al. Challenge of nail psoriasis: an update review. Clin Rev Allergy Immunol. 2021;61:377-402. doi:10.1007/s12016-021-08896-9
- Muneer H, Sathe NC, Masood S. Nail psoriasis. StatPearls [Internet]. StatPearls Publishing; 2024 Jan-. Updated March 1, 2024. Accessed October 24, 2024. https://www.ncbi.nlm.nih.gov/books/NBK559260/
- Armstrong AW, Gooderham M, Warren RB, et al. Deucravacitinib versus placebo and apremilast in moderate to severe plaque psoriasis: efficacy and safety results from the 52-week, randomized, double-blinded, placebo-controlled phase 3 POETYK PSO-1 trial. J Am Acad Dermatol. 2023;88:29-39. doi:10.1016/j.jaad.2022.07.002
- Strober B, Thaçi D, Sofen H, et al. Deucravacitinib versus placebo and apremilast in moderate to severe plaque psoriasis: efficacy and safety results from the 52-week, randomized, double-blinded, phase 3 Program fOr Evaluation of TYK2 inhibitor psoriasis second trial. J Am Acad Dermatol. 2023;88:40-51. doi:10.1016/j.jaad.2022.08.061
- Sanchez DP, Sonthalia S. Koebner phenomenon. StatPearls [Internet]. StatPearls Publishing; 2024 Jan-. Updated November 14, 2022. Accessed April 11, 2024. https://www.ncbi.nlm.nih.gov/books/NBK553108/
- Grover C, Kharghoria G, Bansal S. Triamcinolone acetonide injections in nail psoriasis: a pragmatic analysis. Skin Appendage Disord. 2024;10:50-59. doi:10.1159/000534699
- Hanoodi M, Mittal M. Methotrexate. StatPearls [Internet]. StatPearls Publishing; 2024 Jan-. Updated August 16, 2023. Accessed April 11, 2024. https://www.ncbi.nlm.nih.gov/books/NBK556114/
- Singh JA, Wells GA, Christensen R, et al. Adverse effects of biologics: a network meta-analysis and Cochrane overview. Cochrane Database Syst Rev. 2011;2011:Cd008794. doi:10.1002/14651858.CD008794.pub2
- Thaçi D, Strober B, Gordon KB, et al. Deucravacitinib in moderate to severe psoriasis: clinical and quality-of-life outcomes in a phase 2 trial. Dermatol Ther (Heidelb). 2022;12:495-510. doi:10.1007/s13555-021-00649-y
- Week 0-16: demonstrated safety profile. Bristol-Myers Squibb. 2024. Accessed October 24, 2024. https://www.sotyktuhcp.com/safety-profile?cid=sem_2465603&gclid=CjwKCAiA9ourBhAVEiwA3L5RFnyYqmxbqkz1_zBNPz3dcyHKCSFf1XQ-7acznV0XbR5DDJHYkZcKJxoCWN0QAvD_BwE&gclsrc=aw.ds
To the Editor:
Psoriasis is a chronic inflammatory skin condition that commonly affects the nail matrix and/or nail bed.1 Nail involvement is present in up to 50% of patients with cutaneous psoriasis and 80% of patients with psoriatic arthritis.1 Approximately 5% to 10% of patients with psoriasis demonstrate isolated nail involvement with no skin or joint manifestations.1 Nail psoriasis can cause severe pain and psychological distress, and extreme cases may cause considerable morbidity and functional impairment.2,3 Treatment often requires a long duration and may not result in complete recovery due to the slow rate of nail growth. Patients can progress to permanent nail loss if not treated properly, making early recognition and treatment crucial.1,2 Despite the availability of various treatment options, many cases remain refractory to standard interventions, which underscores the need for novel therapeutic approaches. Herein, we present a severe case of refractory isolated nail psoriasis that was successfully treated with deucravacitinib, an oral tyrosine kinase 2 (TYK2) inhibitor.
A 59-year-old woman presented with a progressive, yellow, hyperkeratotic lesion on the left thumbnail of 2 years’ duration. The patient noted initial discoloration and peeling at the distal end of the nail. Over time, the discoloration progressed to encompass the entire nail. Previous treatments performed by outside physicians including topical corticosteroids, calcineurin inhibitors, and 2 surgeries to remove the nail plate and nail bed all were unsuccessful. The patient also reported severe left thumbnail pain and pruritus that considerably impaired her ability to work. The rest of the nails were unaffected, and she had no personal or family history of psoriasis. Her medical history was notable for hypertension, gastroesophageal reflux disease, and osteomyelitis of the right thumb without nail involvement. Drug allergies included penicillin G benzathine, sulfonamides, amoxicillin, and ciprofloxacin.
Physical examination of the left thumbnail revealed severe yellow, hyperkeratotic, dystrophic changes with a large, yellow, crumbling hyperkeratotic plaque that extended from approximately 1 cm beyond the nail plate to the proximal end of the distal interphalangeal joint, to and along the lateral nail folds, with extensive distal onycholysis. The proximal and lateral nail folds demonstrated erythema as well as maceration that was extremely tender to minimal palpation (Figure 1). No cutaneous lesions were noted elsewhere on the body. The patient had no tenderness, swelling, or stiffness in any of the joints. The differential diagnosis at the time included squamous cell carcinoma of the nail bed and acrodermatitis continua of Hallopeau.
Radiography of the left thumb revealed irregular swelling and nonspecific soft tissue enlargement at the tip of the digit. A nail clipping from the left thumbnail and 3-mm punch biopsies of the lateral and proximal nail folds as well as the horn of the proximal nail fold (Figure 2) were negative for fungus and confirmed psoriasiform dermatitis of the nail.
The patient was started on vinegar soaks (1:1 ratio of vinegar to water) every other day as well as urea cream 10%, ammonium lactate 15%, and petrolatum twice daily for 2 months without considerable improvement. Due to lack of improvement during this 2-month period, the patient subsequently was started on oral deucravacitinib 6 mg/d along with continued use of petrolatum twice daily and vinegar soaks every other day. We selected a trial of deucravacitinib for our patient because of its convenient daily oral dosing and promising clinical evidence.4,5 After 2 months of treatment with deucravacitinib, the patient reported substantial improvement and satisfaction with the treatment results. Physical examination of the left thumbnail after 2 months of deucravacitinib treatment revealed mildly hyperkeratotic, yellow, dystrophic changes of the nail with notable improvement of the yellow hyperkeratotic plaque on the distal thumbnail. Normal-appearing nail growth was noted at the proximal nail fold, demonstrating considerable improvement from the initial presentation (Figure 3). However, the patient had developed multiple oral ulcers, generalized pruritus, and an annular urticarial plaque on the left arm. As such, deucravacitinib was discontinued after 2 months of treatment. These symptoms resolved within a week of discontinuing deucravacitinib.
While the etiology of nail psoriasis remains unclear, it is believed to be due to a combination of immunologic, genetic, and environmental factors.3 Classical clinical features include nail pitting, leukonychia, onycholysis, nail bed hyperkeratosis, and splinter hemorrhages.1,3 Our patient exhibited a severe form of nail psoriasis, encompassing the entire nail matrix and bed and extending to the distal interphalangeal joint and lateral nail folds. Previous surgical interventions may have triggered the Koebner phenomenon—which commonly is associated with psoriasis—and resulted in new skin lesions as a secondary response to the surgical trauma.6 The severity of the condition profoundly impacted her quality of life and considerably hindered her ability to work.
Treatment for nail psoriasis includes topical or systemic therapies such as corticosteroids, vitamin D analogs, tacrolimus, and tumor necrosis factor α inhibitors.1,3 Topical treatment is challenging because it is difficult to deliver medication effectively to the nail bed and nail matrix, and patient adherence may be poor.2 Although it has been shown to be effective, intralesional triamcinolone can be associated with pain as the most common adverse effect.7 Systemic medications such as oral methotrexate also may be effective but are contraindicated in pregnant patients and are associated with potential adverse events (AEs), including hepatotoxicity and acute kidney injury.8 The use of biologics may be challenging due to potential AEs and patient reluctance toward injection-based treatments.9
Deucravacitinib is a TYK2 inhibitor approved for treatment of plaque psoriasis.10 Tyrosine kinase 2 is an intracellular kinase that mediates the signaling of IL-23 and other cytokines involved in psoriasis pathogenesis.10 Deucravacitinib selectively binds to the regulatory domain of TYK2, leading to targeted allosteric inhibition of TYK2-mediated IL-23 and type I interferon signaling.4,5,10 Compared with biologics, deucravacitinib is advantageous because it can be administered as a daily oral pill, encouraging high patient compliance.
In the POETYK PSO-1 and PSO-2 phase 3 randomized controlled trials, 20.9% (n=332) and 20.3% (n=510) of deucravacitinib-treated patients with moderate to severe nail involvement achieved a Physician’s Global Assessment of Fingernail score of 0/1 compared with 8.8% (n=165) and 7.9% (n=254) of patients in the placebo group, respectively. All patients in these trials had a diagnosis of plaque psoriasis with at least 10% body surface area involvement; none of the patients had isolated nail psoriasis.4,5
The phase 3 POETYK PSO-1 and PSO-2 trials demonstrated deucravacitinib to be safe and well tolerated with minimal AEs.4,5 However, the development of AEs in our patient, including oral ulcers and generalized pruritus, underscores the need for close monitoring and consideration of potential risks of treatment. Common AEs associated with deucravacitinib include upper respiratory infections (19.2% [n=840]), increased blood creatine phosphokinase levels (2.7% [n=840]), herpes simplex virus (2.0% [n=840]), and mouth ulcers (1.9% [n=840]).11
Patient education also is a crucial component in the treatment of nail psoriasis. Physicians should emphasize the slow growth of nails and need for prolonged treatment. Clear communication and realistic expectations are essential for ensuring patient adherence to treatment.
Our case highlights the potential efficacy and safety of deucravacitinib for treatment of nail psoriasis, potentially laying the groundwork for future clinical studies. Our patient had a severe case of nail psoriasis that involved the entire nail bed and nail plate, resulting in extreme pain, pruritus, and functional impairment. Her case was unique because involvement was isolated to the nail without any accompanying skin or joint manifestations. She showed a favorable response to deucravacitinib within only 2 months of treatment and exhibited considerable improvement of nail psoriasis, with a reported high level of satisfaction with the treatment. We plan to continue to monitor the patient for long-term results. Future randomized clinical trials with longer follow-up periods are crucial to further establish the efficacy and safety of deucravacitinib for treatment of nail psoriasis.
To the Editor:
Psoriasis is a chronic inflammatory skin condition that commonly affects the nail matrix and/or nail bed.1 Nail involvement is present in up to 50% of patients with cutaneous psoriasis and 80% of patients with psoriatic arthritis.1 Approximately 5% to 10% of patients with psoriasis demonstrate isolated nail involvement with no skin or joint manifestations.1 Nail psoriasis can cause severe pain and psychological distress, and extreme cases may cause considerable morbidity and functional impairment.2,3 Treatment often requires a long duration and may not result in complete recovery due to the slow rate of nail growth. Patients can progress to permanent nail loss if not treated properly, making early recognition and treatment crucial.1,2 Despite the availability of various treatment options, many cases remain refractory to standard interventions, which underscores the need for novel therapeutic approaches. Herein, we present a severe case of refractory isolated nail psoriasis that was successfully treated with deucravacitinib, an oral tyrosine kinase 2 (TYK2) inhibitor.
A 59-year-old woman presented with a progressive, yellow, hyperkeratotic lesion on the left thumbnail of 2 years’ duration. The patient noted initial discoloration and peeling at the distal end of the nail. Over time, the discoloration progressed to encompass the entire nail. Previous treatments performed by outside physicians including topical corticosteroids, calcineurin inhibitors, and 2 surgeries to remove the nail plate and nail bed all were unsuccessful. The patient also reported severe left thumbnail pain and pruritus that considerably impaired her ability to work. The rest of the nails were unaffected, and she had no personal or family history of psoriasis. Her medical history was notable for hypertension, gastroesophageal reflux disease, and osteomyelitis of the right thumb without nail involvement. Drug allergies included penicillin G benzathine, sulfonamides, amoxicillin, and ciprofloxacin.
Physical examination of the left thumbnail revealed severe yellow, hyperkeratotic, dystrophic changes with a large, yellow, crumbling hyperkeratotic plaque that extended from approximately 1 cm beyond the nail plate to the proximal end of the distal interphalangeal joint, to and along the lateral nail folds, with extensive distal onycholysis. The proximal and lateral nail folds demonstrated erythema as well as maceration that was extremely tender to minimal palpation (Figure 1). No cutaneous lesions were noted elsewhere on the body. The patient had no tenderness, swelling, or stiffness in any of the joints. The differential diagnosis at the time included squamous cell carcinoma of the nail bed and acrodermatitis continua of Hallopeau.
Radiography of the left thumb revealed irregular swelling and nonspecific soft tissue enlargement at the tip of the digit. A nail clipping from the left thumbnail and 3-mm punch biopsies of the lateral and proximal nail folds as well as the horn of the proximal nail fold (Figure 2) were negative for fungus and confirmed psoriasiform dermatitis of the nail.
The patient was started on vinegar soaks (1:1 ratio of vinegar to water) every other day as well as urea cream 10%, ammonium lactate 15%, and petrolatum twice daily for 2 months without considerable improvement. Due to lack of improvement during this 2-month period, the patient subsequently was started on oral deucravacitinib 6 mg/d along with continued use of petrolatum twice daily and vinegar soaks every other day. We selected a trial of deucravacitinib for our patient because of its convenient daily oral dosing and promising clinical evidence.4,5 After 2 months of treatment with deucravacitinib, the patient reported substantial improvement and satisfaction with the treatment results. Physical examination of the left thumbnail after 2 months of deucravacitinib treatment revealed mildly hyperkeratotic, yellow, dystrophic changes of the nail with notable improvement of the yellow hyperkeratotic plaque on the distal thumbnail. Normal-appearing nail growth was noted at the proximal nail fold, demonstrating considerable improvement from the initial presentation (Figure 3). However, the patient had developed multiple oral ulcers, generalized pruritus, and an annular urticarial plaque on the left arm. As such, deucravacitinib was discontinued after 2 months of treatment. These symptoms resolved within a week of discontinuing deucravacitinib.
While the etiology of nail psoriasis remains unclear, it is believed to be due to a combination of immunologic, genetic, and environmental factors.3 Classical clinical features include nail pitting, leukonychia, onycholysis, nail bed hyperkeratosis, and splinter hemorrhages.1,3 Our patient exhibited a severe form of nail psoriasis, encompassing the entire nail matrix and bed and extending to the distal interphalangeal joint and lateral nail folds. Previous surgical interventions may have triggered the Koebner phenomenon—which commonly is associated with psoriasis—and resulted in new skin lesions as a secondary response to the surgical trauma.6 The severity of the condition profoundly impacted her quality of life and considerably hindered her ability to work.
Treatment for nail psoriasis includes topical or systemic therapies such as corticosteroids, vitamin D analogs, tacrolimus, and tumor necrosis factor α inhibitors.1,3 Topical treatment is challenging because it is difficult to deliver medication effectively to the nail bed and nail matrix, and patient adherence may be poor.2 Although it has been shown to be effective, intralesional triamcinolone can be associated with pain as the most common adverse effect.7 Systemic medications such as oral methotrexate also may be effective but are contraindicated in pregnant patients and are associated with potential adverse events (AEs), including hepatotoxicity and acute kidney injury.8 The use of biologics may be challenging due to potential AEs and patient reluctance toward injection-based treatments.9
Deucravacitinib is a TYK2 inhibitor approved for treatment of plaque psoriasis.10 Tyrosine kinase 2 is an intracellular kinase that mediates the signaling of IL-23 and other cytokines involved in psoriasis pathogenesis.10 Deucravacitinib selectively binds to the regulatory domain of TYK2, leading to targeted allosteric inhibition of TYK2-mediated IL-23 and type I interferon signaling.4,5,10 Compared with biologics, deucravacitinib is advantageous because it can be administered as a daily oral pill, encouraging high patient compliance.
In the POETYK PSO-1 and PSO-2 phase 3 randomized controlled trials, 20.9% (n=332) and 20.3% (n=510) of deucravacitinib-treated patients with moderate to severe nail involvement achieved a Physician’s Global Assessment of Fingernail score of 0/1 compared with 8.8% (n=165) and 7.9% (n=254) of patients in the placebo group, respectively. All patients in these trials had a diagnosis of plaque psoriasis with at least 10% body surface area involvement; none of the patients had isolated nail psoriasis.4,5
The phase 3 POETYK PSO-1 and PSO-2 trials demonstrated deucravacitinib to be safe and well tolerated with minimal AEs.4,5 However, the development of AEs in our patient, including oral ulcers and generalized pruritus, underscores the need for close monitoring and consideration of potential risks of treatment. Common AEs associated with deucravacitinib include upper respiratory infections (19.2% [n=840]), increased blood creatine phosphokinase levels (2.7% [n=840]), herpes simplex virus (2.0% [n=840]), and mouth ulcers (1.9% [n=840]).11
Patient education also is a crucial component in the treatment of nail psoriasis. Physicians should emphasize the slow growth of nails and need for prolonged treatment. Clear communication and realistic expectations are essential for ensuring patient adherence to treatment.
Our case highlights the potential efficacy and safety of deucravacitinib for treatment of nail psoriasis, potentially laying the groundwork for future clinical studies. Our patient had a severe case of nail psoriasis that involved the entire nail bed and nail plate, resulting in extreme pain, pruritus, and functional impairment. Her case was unique because involvement was isolated to the nail without any accompanying skin or joint manifestations. She showed a favorable response to deucravacitinib within only 2 months of treatment and exhibited considerable improvement of nail psoriasis, with a reported high level of satisfaction with the treatment. We plan to continue to monitor the patient for long-term results. Future randomized clinical trials with longer follow-up periods are crucial to further establish the efficacy and safety of deucravacitinib for treatment of nail psoriasis.
- Hwang JK, Grover C, Iorizzo M, et al. Nail psoriasis and nail lichen planus: updates on diagnosis and management. J Am Acad Dermatol. 2024;90:585-596. doi:10.1016/j.jaad.2023.11.024
- Ji C, Wang H, Bao C, et al. Challenge of nail psoriasis: an update review. Clin Rev Allergy Immunol. 2021;61:377-402. doi:10.1007/s12016-021-08896-9
- Muneer H, Sathe NC, Masood S. Nail psoriasis. StatPearls [Internet]. StatPearls Publishing; 2024 Jan-. Updated March 1, 2024. Accessed October 24, 2024. https://www.ncbi.nlm.nih.gov/books/NBK559260/
- Armstrong AW, Gooderham M, Warren RB, et al. Deucravacitinib versus placebo and apremilast in moderate to severe plaque psoriasis: efficacy and safety results from the 52-week, randomized, double-blinded, placebo-controlled phase 3 POETYK PSO-1 trial. J Am Acad Dermatol. 2023;88:29-39. doi:10.1016/j.jaad.2022.07.002
- Strober B, Thaçi D, Sofen H, et al. Deucravacitinib versus placebo and apremilast in moderate to severe plaque psoriasis: efficacy and safety results from the 52-week, randomized, double-blinded, phase 3 Program fOr Evaluation of TYK2 inhibitor psoriasis second trial. J Am Acad Dermatol. 2023;88:40-51. doi:10.1016/j.jaad.2022.08.061
- Sanchez DP, Sonthalia S. Koebner phenomenon. StatPearls [Internet]. StatPearls Publishing; 2024 Jan-. Updated November 14, 2022. Accessed April 11, 2024. https://www.ncbi.nlm.nih.gov/books/NBK553108/
- Grover C, Kharghoria G, Bansal S. Triamcinolone acetonide injections in nail psoriasis: a pragmatic analysis. Skin Appendage Disord. 2024;10:50-59. doi:10.1159/000534699
- Hanoodi M, Mittal M. Methotrexate. StatPearls [Internet]. StatPearls Publishing; 2024 Jan-. Updated August 16, 2023. Accessed April 11, 2024. https://www.ncbi.nlm.nih.gov/books/NBK556114/
- Singh JA, Wells GA, Christensen R, et al. Adverse effects of biologics: a network meta-analysis and Cochrane overview. Cochrane Database Syst Rev. 2011;2011:Cd008794. doi:10.1002/14651858.CD008794.pub2
- Thaçi D, Strober B, Gordon KB, et al. Deucravacitinib in moderate to severe psoriasis: clinical and quality-of-life outcomes in a phase 2 trial. Dermatol Ther (Heidelb). 2022;12:495-510. doi:10.1007/s13555-021-00649-y
- Week 0-16: demonstrated safety profile. Bristol-Myers Squibb. 2024. Accessed October 24, 2024. https://www.sotyktuhcp.com/safety-profile?cid=sem_2465603&gclid=CjwKCAiA9ourBhAVEiwA3L5RFnyYqmxbqkz1_zBNPz3dcyHKCSFf1XQ-7acznV0XbR5DDJHYkZcKJxoCWN0QAvD_BwE&gclsrc=aw.ds
- Hwang JK, Grover C, Iorizzo M, et al. Nail psoriasis and nail lichen planus: updates on diagnosis and management. J Am Acad Dermatol. 2024;90:585-596. doi:10.1016/j.jaad.2023.11.024
- Ji C, Wang H, Bao C, et al. Challenge of nail psoriasis: an update review. Clin Rev Allergy Immunol. 2021;61:377-402. doi:10.1007/s12016-021-08896-9
- Muneer H, Sathe NC, Masood S. Nail psoriasis. StatPearls [Internet]. StatPearls Publishing; 2024 Jan-. Updated March 1, 2024. Accessed October 24, 2024. https://www.ncbi.nlm.nih.gov/books/NBK559260/
- Armstrong AW, Gooderham M, Warren RB, et al. Deucravacitinib versus placebo and apremilast in moderate to severe plaque psoriasis: efficacy and safety results from the 52-week, randomized, double-blinded, placebo-controlled phase 3 POETYK PSO-1 trial. J Am Acad Dermatol. 2023;88:29-39. doi:10.1016/j.jaad.2022.07.002
- Strober B, Thaçi D, Sofen H, et al. Deucravacitinib versus placebo and apremilast in moderate to severe plaque psoriasis: efficacy and safety results from the 52-week, randomized, double-blinded, phase 3 Program fOr Evaluation of TYK2 inhibitor psoriasis second trial. J Am Acad Dermatol. 2023;88:40-51. doi:10.1016/j.jaad.2022.08.061
- Sanchez DP, Sonthalia S. Koebner phenomenon. StatPearls [Internet]. StatPearls Publishing; 2024 Jan-. Updated November 14, 2022. Accessed April 11, 2024. https://www.ncbi.nlm.nih.gov/books/NBK553108/
- Grover C, Kharghoria G, Bansal S. Triamcinolone acetonide injections in nail psoriasis: a pragmatic analysis. Skin Appendage Disord. 2024;10:50-59. doi:10.1159/000534699
- Hanoodi M, Mittal M. Methotrexate. StatPearls [Internet]. StatPearls Publishing; 2024 Jan-. Updated August 16, 2023. Accessed April 11, 2024. https://www.ncbi.nlm.nih.gov/books/NBK556114/
- Singh JA, Wells GA, Christensen R, et al. Adverse effects of biologics: a network meta-analysis and Cochrane overview. Cochrane Database Syst Rev. 2011;2011:Cd008794. doi:10.1002/14651858.CD008794.pub2
- Thaçi D, Strober B, Gordon KB, et al. Deucravacitinib in moderate to severe psoriasis: clinical and quality-of-life outcomes in a phase 2 trial. Dermatol Ther (Heidelb). 2022;12:495-510. doi:10.1007/s13555-021-00649-y
- Week 0-16: demonstrated safety profile. Bristol-Myers Squibb. 2024. Accessed October 24, 2024. https://www.sotyktuhcp.com/safety-profile?cid=sem_2465603&gclid=CjwKCAiA9ourBhAVEiwA3L5RFnyYqmxbqkz1_zBNPz3dcyHKCSFf1XQ-7acznV0XbR5DDJHYkZcKJxoCWN0QAvD_BwE&gclsrc=aw.ds
Successful Treatment of Severe Dystrophic Nail Psoriasis With Deucravacitinib
Successful Treatment of Severe Dystrophic Nail Psoriasis With Deucravacitinib
PRACTICE POINTS
- Nail psoriasis can masquerade as other dermatologic conditions, including squamous cell carcinoma of the nail bed and acrodermatitis continua of Hallopeau.
- Nail psoriasis can progress to permanent nail loss if not treated properly, making early recognition and treatment crucial.
- Deucravacitinib, an oral tyrosine kinase 2 inhibitor approved for the treatment of plaque psoriasis, has shown promise as an effective treatment for nail psoriasis in cases that are refractory to standard therapies.

Adalimumab for Psoriasis: Study Compares Biosimilars Vs. Originator
TOPLINE:
rate than those who remained on Humira.
METHODOLOGY:
- Researchers conducted a cohort study using data on patients with psoriasis who were treated with adalimumab, a tumor necrosis factor alpha inhibitor used to treat moderate to severe psoriasis, from the French National Health Data System, British Association of Dermatologists Biologics and Immunomodulators Register, and Spanish Registry of Systemic Therapy in Psoriasis.
- The analysis included 7387 adalimumab-naive patients who were new users of an adalimumab biosimilar and 3654 patients (switchers) who switched from Humira to a biosimilar. Patients were matched and compared with patients receiving Humira.
- Co-primary outcomes of the study were drug discontinuation and serious adverse events.
- Researchers assessed the following adalimumab biosimilar brands: Amgevita, Imraldi, Hyrimoz, Idacio, and Hulio.
TAKEAWAY:
- All-cause drug discontinuation rates were similar between new users of biosimilars and Humira new users (hazard ratio [HR], 0.99; 95% CI, 0.94-1.04).
- Discontinuation rates were higher among those who switched from Humira to a biosimilar (HR, 1.35; 95% CI, 1.19-1.52) than among those who stayed on Humira. Switching to Amgevita (HR, 1.25; 95% CI, 1.13-1.27), Imraldi (HR, 1.53; 95% CI, 1.33-1.76), and Hyrimoz (HR, 1.80; 95% CI, 1.29-2.52) was associated with higher discontinuation rates.
- Serious adverse events were not significantly different between new users of Humira and biosimilar new users (incidence rate ratio [IRR], 0.91; 95% CI, 0.80-1.05), and between patients who switched from a biosimilar to Humira and those who stayed on Humira (IRR, 0.92; 95% CI, 0.83-1.01).
- No significant differences in discontinuation because of ineffectiveness were found between biosimilar and Humira new users (HR, 0.97; 95% CI, 0.88-1.08). Discontinuation because of adverse events was also comparable for all biosimilars among new users, except for Hyrimoz (HR, 0.54; 95% CI, 0.35-0.85), which showed fewer discontinuations than Humira.
IN PRACTICE:
“This study found comparable drug survival and safety between adalimumab biosimilars and Humira in adalimumab-naive patients, supporting the use of biosimilars as viable alternatives for new patients,” the authors wrote. However, noting that discontinuation was more likely among those who switched from Humira to a biosimilar, they added: “Changes in treatment response, skin or injection site reactions, and nocebo effects may contribute to treatment discontinuation post-switch. Thus, patients who switch from Humira to biosimilars may require closer monitoring and support to alleviate these challenges.”
SOURCE:
The study was led by Duc Binh Phan, Dermatology Centre, Northern Care Alliance NHS Foundation Trust in Manchester, England. It was published online in The British Journal of Dermatology.
LIMITATIONS:
Unmeasured factors including psychological perceptions, regional policies, and drug availability could influence drug survival, making the results not fully reflective of treatment effectiveness or safety. Most Humira users in registries were enrolled before biosimilars became available, making it impractical to match new users on the basis of treatment initiation years. Additionally, reasons for discontinuation were not available in the French National Health Data System.
DISCLOSURES:
In the United Kingdom, the research was funded by the Psoriasis Association PhD studentship and supported by the NIHR Manchester Biomedical Research Centre. In France, the authors are employees of the French National Health Insurance, the French National Agency for the Safety of Medicines and Health Products, and the Assistance Publique — Hôpitaux de Paris and received no funding. The authors reported receiving consulting and speaker fees and clinical trial sponsorship from various pharmaceutical companies. Additional disclosures are noted in the original article.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
TOPLINE:
rate than those who remained on Humira.
METHODOLOGY:
- Researchers conducted a cohort study using data on patients with psoriasis who were treated with adalimumab, a tumor necrosis factor alpha inhibitor used to treat moderate to severe psoriasis, from the French National Health Data System, British Association of Dermatologists Biologics and Immunomodulators Register, and Spanish Registry of Systemic Therapy in Psoriasis.
- The analysis included 7387 adalimumab-naive patients who were new users of an adalimumab biosimilar and 3654 patients (switchers) who switched from Humira to a biosimilar. Patients were matched and compared with patients receiving Humira.
- Co-primary outcomes of the study were drug discontinuation and serious adverse events.
- Researchers assessed the following adalimumab biosimilar brands: Amgevita, Imraldi, Hyrimoz, Idacio, and Hulio.
TAKEAWAY:
- All-cause drug discontinuation rates were similar between new users of biosimilars and Humira new users (hazard ratio [HR], 0.99; 95% CI, 0.94-1.04).
- Discontinuation rates were higher among those who switched from Humira to a biosimilar (HR, 1.35; 95% CI, 1.19-1.52) than among those who stayed on Humira. Switching to Amgevita (HR, 1.25; 95% CI, 1.13-1.27), Imraldi (HR, 1.53; 95% CI, 1.33-1.76), and Hyrimoz (HR, 1.80; 95% CI, 1.29-2.52) was associated with higher discontinuation rates.
- Serious adverse events were not significantly different between new users of Humira and biosimilar new users (incidence rate ratio [IRR], 0.91; 95% CI, 0.80-1.05), and between patients who switched from a biosimilar to Humira and those who stayed on Humira (IRR, 0.92; 95% CI, 0.83-1.01).
- No significant differences in discontinuation because of ineffectiveness were found between biosimilar and Humira new users (HR, 0.97; 95% CI, 0.88-1.08). Discontinuation because of adverse events was also comparable for all biosimilars among new users, except for Hyrimoz (HR, 0.54; 95% CI, 0.35-0.85), which showed fewer discontinuations than Humira.
IN PRACTICE:
“This study found comparable drug survival and safety between adalimumab biosimilars and Humira in adalimumab-naive patients, supporting the use of biosimilars as viable alternatives for new patients,” the authors wrote. However, noting that discontinuation was more likely among those who switched from Humira to a biosimilar, they added: “Changes in treatment response, skin or injection site reactions, and nocebo effects may contribute to treatment discontinuation post-switch. Thus, patients who switch from Humira to biosimilars may require closer monitoring and support to alleviate these challenges.”
SOURCE:
The study was led by Duc Binh Phan, Dermatology Centre, Northern Care Alliance NHS Foundation Trust in Manchester, England. It was published online in The British Journal of Dermatology.
LIMITATIONS:
Unmeasured factors including psychological perceptions, regional policies, and drug availability could influence drug survival, making the results not fully reflective of treatment effectiveness or safety. Most Humira users in registries were enrolled before biosimilars became available, making it impractical to match new users on the basis of treatment initiation years. Additionally, reasons for discontinuation were not available in the French National Health Data System.
DISCLOSURES:
In the United Kingdom, the research was funded by the Psoriasis Association PhD studentship and supported by the NIHR Manchester Biomedical Research Centre. In France, the authors are employees of the French National Health Insurance, the French National Agency for the Safety of Medicines and Health Products, and the Assistance Publique — Hôpitaux de Paris and received no funding. The authors reported receiving consulting and speaker fees and clinical trial sponsorship from various pharmaceutical companies. Additional disclosures are noted in the original article.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
TOPLINE:
rate than those who remained on Humira.
METHODOLOGY:
- Researchers conducted a cohort study using data on patients with psoriasis who were treated with adalimumab, a tumor necrosis factor alpha inhibitor used to treat moderate to severe psoriasis, from the French National Health Data System, British Association of Dermatologists Biologics and Immunomodulators Register, and Spanish Registry of Systemic Therapy in Psoriasis.
- The analysis included 7387 adalimumab-naive patients who were new users of an adalimumab biosimilar and 3654 patients (switchers) who switched from Humira to a biosimilar. Patients were matched and compared with patients receiving Humira.
- Co-primary outcomes of the study were drug discontinuation and serious adverse events.
- Researchers assessed the following adalimumab biosimilar brands: Amgevita, Imraldi, Hyrimoz, Idacio, and Hulio.
TAKEAWAY:
- All-cause drug discontinuation rates were similar between new users of biosimilars and Humira new users (hazard ratio [HR], 0.99; 95% CI, 0.94-1.04).
- Discontinuation rates were higher among those who switched from Humira to a biosimilar (HR, 1.35; 95% CI, 1.19-1.52) than among those who stayed on Humira. Switching to Amgevita (HR, 1.25; 95% CI, 1.13-1.27), Imraldi (HR, 1.53; 95% CI, 1.33-1.76), and Hyrimoz (HR, 1.80; 95% CI, 1.29-2.52) was associated with higher discontinuation rates.
- Serious adverse events were not significantly different between new users of Humira and biosimilar new users (incidence rate ratio [IRR], 0.91; 95% CI, 0.80-1.05), and between patients who switched from a biosimilar to Humira and those who stayed on Humira (IRR, 0.92; 95% CI, 0.83-1.01).
- No significant differences in discontinuation because of ineffectiveness were found between biosimilar and Humira new users (HR, 0.97; 95% CI, 0.88-1.08). Discontinuation because of adverse events was also comparable for all biosimilars among new users, except for Hyrimoz (HR, 0.54; 95% CI, 0.35-0.85), which showed fewer discontinuations than Humira.
IN PRACTICE:
“This study found comparable drug survival and safety between adalimumab biosimilars and Humira in adalimumab-naive patients, supporting the use of biosimilars as viable alternatives for new patients,” the authors wrote. However, noting that discontinuation was more likely among those who switched from Humira to a biosimilar, they added: “Changes in treatment response, skin or injection site reactions, and nocebo effects may contribute to treatment discontinuation post-switch. Thus, patients who switch from Humira to biosimilars may require closer monitoring and support to alleviate these challenges.”
SOURCE:
The study was led by Duc Binh Phan, Dermatology Centre, Northern Care Alliance NHS Foundation Trust in Manchester, England. It was published online in The British Journal of Dermatology.
LIMITATIONS:
Unmeasured factors including psychological perceptions, regional policies, and drug availability could influence drug survival, making the results not fully reflective of treatment effectiveness or safety. Most Humira users in registries were enrolled before biosimilars became available, making it impractical to match new users on the basis of treatment initiation years. Additionally, reasons for discontinuation were not available in the French National Health Data System.
DISCLOSURES:
In the United Kingdom, the research was funded by the Psoriasis Association PhD studentship and supported by the NIHR Manchester Biomedical Research Centre. In France, the authors are employees of the French National Health Insurance, the French National Agency for the Safety of Medicines and Health Products, and the Assistance Publique — Hôpitaux de Paris and received no funding. The authors reported receiving consulting and speaker fees and clinical trial sponsorship from various pharmaceutical companies. Additional disclosures are noted in the original article.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
Post COVID-19, Long-term Risk for Autoimmune, Autoinflammatory Skin Disorders Increased, Study Finds
In addition, the authors reported that COVID-19 vaccination appears to reduce these risks.
The study was published in JAMA Dermatology.
‘Compelling Evidence’
“This well-executed study by Heo et al provides compelling evidence to support an association between COVID-19 infection and the development of subsequent autoimmune and autoinflammatory skin diseases,” wrote authors led by Lisa M. Arkin, MD, of the Department of Dermatology, University of Wisconsin School of Medicine and Public Health in Madison, in an accompanying editorial.
Using databases from Korea’s National Health Insurance Service and the Korea Disease Control and Prevention Agency, investigators led by Yeon-Woo Heo, MD, a dermatology resident at Yonsei University Wonju College of Medicine, Wonju, Republic of Korea, compared 3.1 million people who had COVID-19 with 3.8 million controls, all with at least 180 days’ follow-up through December 31, 2022.
At a mean follow-up of 287 days in both cohorts, authors found significantly elevated risks for AA and vitiligo (adjusted hazard ratio [aHR], 1.11 for both), AT (aHR, 1.24), Behçet disease (aHR, 1.45), and BP (aHR, 1.62) in the post–COVID-19 cohort. The infection also raised the risk for other conditions such as systemic lupus erythematosus (aHR, 1.14) and Crohn’s disease (aHR, 1.35).
In subgroup analyses, demographic factors were associated with diverse effects: COVID-19 infection was associated with significantly higher odds of developing AA (for both men and women), vitiligo (men), Behçet disease (men and women), Crohn’s disease (men), ulcerative colitis (men), rheumatoid arthritis (men and women), systemic lupus erythematosus (men), ankylosing spondylitis (men), AT (women), and BP (women) than controls.
Those aged under 40 years were more likely to develop AA, primary cicatricial alopecia, Behçet disease, and ulcerative colitis, while those aged 40 years or older were more likely to develop AA, AT, vitiligo, Behçet disease, Crohn’s disease, rheumatoid arthritis, systemic lupus erythematosus, Sjögren’s syndrome, ankylosing spondylitis, and BP.
Additionally, severe COVID-19 requiring intensive care unit admission was associated with a significantly increased risk for autoimmune diseases, including AA, psoriasis, BP, and sarcoidosis. By timeframe, risks for AA, AT, and psoriasis were significantly higher during the initial Delta-dominant period.
Vaccination Effect
Moreover, vaccinated individuals were less likely to develop AA, AT, psoriasis, Behçet disease, and various nondermatologic conditions than were those who were unvaccinated. This finding, wrote Heo and colleagues, “may provide evidence to support the hypothesis that COVID-19 vaccines can help prevent autoimmune diseases.”
“That’s the part we all need to take into our offices tomorrow,” said Brett King, MD, PhD, a Fairfield, Connecticut–based dermatologist in private practice. He was not involved with the study but was asked to comment.
Overall, King said, the study carries two main messages. “The first is that COVID-19 infection increases the likelihood of developing an autoimmune or autoinflammatory disease in a large population.” The second and very important message is that being vaccinated against COVID-19 provides protection against developing an autoimmune or autoinflammatory disease.
“My concern is that the popular media highlights the first part,” said King, “and everybody who develops alopecia areata, vitiligo, or sarcoidosis blames COVID-19. That’s not what this work says.”
The foregoing distinction is especially important during the fall and winter, he added, when people getting influenza vaccines are routinely offered COVID-19 vaccines. “Many patients have said, ‘I got the COVID vaccine and developed alopecia areata 6 months later.’ Nearly everybody who has developed a new or worsening health condition in the last almost 5 years has had the perfect fall guy — the COVID vaccine or infection.”
With virtually all patients asking if they should get an updated COVID-19 vaccine or booster, he added, many report having heard that such vaccines cause AA, vitiligo, or other diseases. “To anchor these conversations in real data and not just anecdotes from a blog or Facebook is very useful,” said King, “and now we have very good data saying that the COVID vaccine is protective against these disorders.”
George Han, MD, PhD, associate professor of dermatology at the Donald and Barbara Zucker School of Medicine at Hofstra/Northwell in Hempstead, New York, applauds investigators’ use of a large, robust database but suggests interpreting results cautiously. He was not involved with the study but was asked to comment.
“You could do a large, well-done study,” Han said, “but it could still not necessarily be generalizable. These autoimmune conditions they’re looking at have clear ethnic and racial biases.” Heo and colleagues acknowledged shortcomings including their study population’s monomorphic nature.
Additional issues that limit the study’s impact, said Han, include the difficulty of conceptualizing a 10%-20% increase in conditions that at baseline are rare. And many of the findings reflected natural patterns, he said. For instance, BP more commonly affects older people, COVID-19 notwithstanding.
Han said that for him, the study’s main value going forward is helping to explain a rash of worsening inflammatory skin disease that many dermatologists saw early in the pandemic. “We would regularly see patients who were well controlled with, for example, psoriasis or eczema. But after COVID-19 infection or a vaccine (usually mRNA-type), in some cases they would come in flaring badly.” This happened at least a dozen times during the first year of post-shutdown appointments, he said.
“We’ve seen patients who have flared multiple times — they get the booster, then flare again,” Han added. Similar patterns occurred with pyoderma gangrenosum and other inflammatory skin diseases, he said.
Given the modest effect sizes of the associations reported in the Korean study, Arkin and colleagues wrote in their JAMA Dermatology editorial that surveillance for autoimmune disease is probably not warranted without new examination findings or symptoms. “For certain,” King said, “we should not go hunting for things that aren’t obviously there.”
Rather, Arkin and colleagues wrote, the higher autoimmunity rates seen among the unvaccinated, as well as during the Delta phase (when patients were sicker and hospitalizations were more likely) and in patients requiring intensive care, suggest that “interventions that reduce disease severity could also potentially reduce long-term risk of subsequent autoimmune sequelae.”
Future research addressing whether people with preexisting autoimmune conditions are at greater risk for flares or developing new autoimmune diseases following COVID-19 infection “would help to frame an evidence-based approach for patients with autoimmune disorders who develop COVID-19 infection, including the role for antiviral treatments,” they added.
The study was supported by grants from the Research Program of the Korea Medical Institute, the Korea Health Industry Development Institute, and the National Research Foundation of Korea. Han and King reported no relevant financial relationships. Arkin disclosed receiving research grants to her institution from Amgen and Eli Lilly, personal fees from Sanofi/Regeneron for consulting, and personal consulting fees from Merck outside the submitted work. Another author reported personal consulting fees from Dexcel Pharma and Honeydew outside the submitted work. No other disclosures were reported.
A version of this article appeared on Medscape.com.
In addition, the authors reported that COVID-19 vaccination appears to reduce these risks.
The study was published in JAMA Dermatology.
‘Compelling Evidence’
“This well-executed study by Heo et al provides compelling evidence to support an association between COVID-19 infection and the development of subsequent autoimmune and autoinflammatory skin diseases,” wrote authors led by Lisa M. Arkin, MD, of the Department of Dermatology, University of Wisconsin School of Medicine and Public Health in Madison, in an accompanying editorial.
Using databases from Korea’s National Health Insurance Service and the Korea Disease Control and Prevention Agency, investigators led by Yeon-Woo Heo, MD, a dermatology resident at Yonsei University Wonju College of Medicine, Wonju, Republic of Korea, compared 3.1 million people who had COVID-19 with 3.8 million controls, all with at least 180 days’ follow-up through December 31, 2022.
At a mean follow-up of 287 days in both cohorts, authors found significantly elevated risks for AA and vitiligo (adjusted hazard ratio [aHR], 1.11 for both), AT (aHR, 1.24), Behçet disease (aHR, 1.45), and BP (aHR, 1.62) in the post–COVID-19 cohort. The infection also raised the risk for other conditions such as systemic lupus erythematosus (aHR, 1.14) and Crohn’s disease (aHR, 1.35).
In subgroup analyses, demographic factors were associated with diverse effects: COVID-19 infection was associated with significantly higher odds of developing AA (for both men and women), vitiligo (men), Behçet disease (men and women), Crohn’s disease (men), ulcerative colitis (men), rheumatoid arthritis (men and women), systemic lupus erythematosus (men), ankylosing spondylitis (men), AT (women), and BP (women) than controls.
Those aged under 40 years were more likely to develop AA, primary cicatricial alopecia, Behçet disease, and ulcerative colitis, while those aged 40 years or older were more likely to develop AA, AT, vitiligo, Behçet disease, Crohn’s disease, rheumatoid arthritis, systemic lupus erythematosus, Sjögren’s syndrome, ankylosing spondylitis, and BP.
Additionally, severe COVID-19 requiring intensive care unit admission was associated with a significantly increased risk for autoimmune diseases, including AA, psoriasis, BP, and sarcoidosis. By timeframe, risks for AA, AT, and psoriasis were significantly higher during the initial Delta-dominant period.
Vaccination Effect
Moreover, vaccinated individuals were less likely to develop AA, AT, psoriasis, Behçet disease, and various nondermatologic conditions than were those who were unvaccinated. This finding, wrote Heo and colleagues, “may provide evidence to support the hypothesis that COVID-19 vaccines can help prevent autoimmune diseases.”
“That’s the part we all need to take into our offices tomorrow,” said Brett King, MD, PhD, a Fairfield, Connecticut–based dermatologist in private practice. He was not involved with the study but was asked to comment.
Overall, King said, the study carries two main messages. “The first is that COVID-19 infection increases the likelihood of developing an autoimmune or autoinflammatory disease in a large population.” The second and very important message is that being vaccinated against COVID-19 provides protection against developing an autoimmune or autoinflammatory disease.
“My concern is that the popular media highlights the first part,” said King, “and everybody who develops alopecia areata, vitiligo, or sarcoidosis blames COVID-19. That’s not what this work says.”
The foregoing distinction is especially important during the fall and winter, he added, when people getting influenza vaccines are routinely offered COVID-19 vaccines. “Many patients have said, ‘I got the COVID vaccine and developed alopecia areata 6 months later.’ Nearly everybody who has developed a new or worsening health condition in the last almost 5 years has had the perfect fall guy — the COVID vaccine or infection.”
With virtually all patients asking if they should get an updated COVID-19 vaccine or booster, he added, many report having heard that such vaccines cause AA, vitiligo, or other diseases. “To anchor these conversations in real data and not just anecdotes from a blog or Facebook is very useful,” said King, “and now we have very good data saying that the COVID vaccine is protective against these disorders.”
George Han, MD, PhD, associate professor of dermatology at the Donald and Barbara Zucker School of Medicine at Hofstra/Northwell in Hempstead, New York, applauds investigators’ use of a large, robust database but suggests interpreting results cautiously. He was not involved with the study but was asked to comment.
“You could do a large, well-done study,” Han said, “but it could still not necessarily be generalizable. These autoimmune conditions they’re looking at have clear ethnic and racial biases.” Heo and colleagues acknowledged shortcomings including their study population’s monomorphic nature.
Additional issues that limit the study’s impact, said Han, include the difficulty of conceptualizing a 10%-20% increase in conditions that at baseline are rare. And many of the findings reflected natural patterns, he said. For instance, BP more commonly affects older people, COVID-19 notwithstanding.
Han said that for him, the study’s main value going forward is helping to explain a rash of worsening inflammatory skin disease that many dermatologists saw early in the pandemic. “We would regularly see patients who were well controlled with, for example, psoriasis or eczema. But after COVID-19 infection or a vaccine (usually mRNA-type), in some cases they would come in flaring badly.” This happened at least a dozen times during the first year of post-shutdown appointments, he said.
“We’ve seen patients who have flared multiple times — they get the booster, then flare again,” Han added. Similar patterns occurred with pyoderma gangrenosum and other inflammatory skin diseases, he said.
Given the modest effect sizes of the associations reported in the Korean study, Arkin and colleagues wrote in their JAMA Dermatology editorial that surveillance for autoimmune disease is probably not warranted without new examination findings or symptoms. “For certain,” King said, “we should not go hunting for things that aren’t obviously there.”
Rather, Arkin and colleagues wrote, the higher autoimmunity rates seen among the unvaccinated, as well as during the Delta phase (when patients were sicker and hospitalizations were more likely) and in patients requiring intensive care, suggest that “interventions that reduce disease severity could also potentially reduce long-term risk of subsequent autoimmune sequelae.”
Future research addressing whether people with preexisting autoimmune conditions are at greater risk for flares or developing new autoimmune diseases following COVID-19 infection “would help to frame an evidence-based approach for patients with autoimmune disorders who develop COVID-19 infection, including the role for antiviral treatments,” they added.
The study was supported by grants from the Research Program of the Korea Medical Institute, the Korea Health Industry Development Institute, and the National Research Foundation of Korea. Han and King reported no relevant financial relationships. Arkin disclosed receiving research grants to her institution from Amgen and Eli Lilly, personal fees from Sanofi/Regeneron for consulting, and personal consulting fees from Merck outside the submitted work. Another author reported personal consulting fees from Dexcel Pharma and Honeydew outside the submitted work. No other disclosures were reported.
A version of this article appeared on Medscape.com.
In addition, the authors reported that COVID-19 vaccination appears to reduce these risks.
The study was published in JAMA Dermatology.
‘Compelling Evidence’
“This well-executed study by Heo et al provides compelling evidence to support an association between COVID-19 infection and the development of subsequent autoimmune and autoinflammatory skin diseases,” wrote authors led by Lisa M. Arkin, MD, of the Department of Dermatology, University of Wisconsin School of Medicine and Public Health in Madison, in an accompanying editorial.
Using databases from Korea’s National Health Insurance Service and the Korea Disease Control and Prevention Agency, investigators led by Yeon-Woo Heo, MD, a dermatology resident at Yonsei University Wonju College of Medicine, Wonju, Republic of Korea, compared 3.1 million people who had COVID-19 with 3.8 million controls, all with at least 180 days’ follow-up through December 31, 2022.
At a mean follow-up of 287 days in both cohorts, authors found significantly elevated risks for AA and vitiligo (adjusted hazard ratio [aHR], 1.11 for both), AT (aHR, 1.24), Behçet disease (aHR, 1.45), and BP (aHR, 1.62) in the post–COVID-19 cohort. The infection also raised the risk for other conditions such as systemic lupus erythematosus (aHR, 1.14) and Crohn’s disease (aHR, 1.35).
In subgroup analyses, demographic factors were associated with diverse effects: COVID-19 infection was associated with significantly higher odds of developing AA (for both men and women), vitiligo (men), Behçet disease (men and women), Crohn’s disease (men), ulcerative colitis (men), rheumatoid arthritis (men and women), systemic lupus erythematosus (men), ankylosing spondylitis (men), AT (women), and BP (women) than controls.
Those aged under 40 years were more likely to develop AA, primary cicatricial alopecia, Behçet disease, and ulcerative colitis, while those aged 40 years or older were more likely to develop AA, AT, vitiligo, Behçet disease, Crohn’s disease, rheumatoid arthritis, systemic lupus erythematosus, Sjögren’s syndrome, ankylosing spondylitis, and BP.
Additionally, severe COVID-19 requiring intensive care unit admission was associated with a significantly increased risk for autoimmune diseases, including AA, psoriasis, BP, and sarcoidosis. By timeframe, risks for AA, AT, and psoriasis were significantly higher during the initial Delta-dominant period.
Vaccination Effect
Moreover, vaccinated individuals were less likely to develop AA, AT, psoriasis, Behçet disease, and various nondermatologic conditions than were those who were unvaccinated. This finding, wrote Heo and colleagues, “may provide evidence to support the hypothesis that COVID-19 vaccines can help prevent autoimmune diseases.”
“That’s the part we all need to take into our offices tomorrow,” said Brett King, MD, PhD, a Fairfield, Connecticut–based dermatologist in private practice. He was not involved with the study but was asked to comment.
Overall, King said, the study carries two main messages. “The first is that COVID-19 infection increases the likelihood of developing an autoimmune or autoinflammatory disease in a large population.” The second and very important message is that being vaccinated against COVID-19 provides protection against developing an autoimmune or autoinflammatory disease.
“My concern is that the popular media highlights the first part,” said King, “and everybody who develops alopecia areata, vitiligo, or sarcoidosis blames COVID-19. That’s not what this work says.”
The foregoing distinction is especially important during the fall and winter, he added, when people getting influenza vaccines are routinely offered COVID-19 vaccines. “Many patients have said, ‘I got the COVID vaccine and developed alopecia areata 6 months later.’ Nearly everybody who has developed a new or worsening health condition in the last almost 5 years has had the perfect fall guy — the COVID vaccine or infection.”
With virtually all patients asking if they should get an updated COVID-19 vaccine or booster, he added, many report having heard that such vaccines cause AA, vitiligo, or other diseases. “To anchor these conversations in real data and not just anecdotes from a blog or Facebook is very useful,” said King, “and now we have very good data saying that the COVID vaccine is protective against these disorders.”
George Han, MD, PhD, associate professor of dermatology at the Donald and Barbara Zucker School of Medicine at Hofstra/Northwell in Hempstead, New York, applauds investigators’ use of a large, robust database but suggests interpreting results cautiously. He was not involved with the study but was asked to comment.
“You could do a large, well-done study,” Han said, “but it could still not necessarily be generalizable. These autoimmune conditions they’re looking at have clear ethnic and racial biases.” Heo and colleagues acknowledged shortcomings including their study population’s monomorphic nature.
Additional issues that limit the study’s impact, said Han, include the difficulty of conceptualizing a 10%-20% increase in conditions that at baseline are rare. And many of the findings reflected natural patterns, he said. For instance, BP more commonly affects older people, COVID-19 notwithstanding.
Han said that for him, the study’s main value going forward is helping to explain a rash of worsening inflammatory skin disease that many dermatologists saw early in the pandemic. “We would regularly see patients who were well controlled with, for example, psoriasis or eczema. But after COVID-19 infection or a vaccine (usually mRNA-type), in some cases they would come in flaring badly.” This happened at least a dozen times during the first year of post-shutdown appointments, he said.
“We’ve seen patients who have flared multiple times — they get the booster, then flare again,” Han added. Similar patterns occurred with pyoderma gangrenosum and other inflammatory skin diseases, he said.
Given the modest effect sizes of the associations reported in the Korean study, Arkin and colleagues wrote in their JAMA Dermatology editorial that surveillance for autoimmune disease is probably not warranted without new examination findings or symptoms. “For certain,” King said, “we should not go hunting for things that aren’t obviously there.”
Rather, Arkin and colleagues wrote, the higher autoimmunity rates seen among the unvaccinated, as well as during the Delta phase (when patients were sicker and hospitalizations were more likely) and in patients requiring intensive care, suggest that “interventions that reduce disease severity could also potentially reduce long-term risk of subsequent autoimmune sequelae.”
Future research addressing whether people with preexisting autoimmune conditions are at greater risk for flares or developing new autoimmune diseases following COVID-19 infection “would help to frame an evidence-based approach for patients with autoimmune disorders who develop COVID-19 infection, including the role for antiviral treatments,” they added.
The study was supported by grants from the Research Program of the Korea Medical Institute, the Korea Health Industry Development Institute, and the National Research Foundation of Korea. Han and King reported no relevant financial relationships. Arkin disclosed receiving research grants to her institution from Amgen and Eli Lilly, personal fees from Sanofi/Regeneron for consulting, and personal consulting fees from Merck outside the submitted work. Another author reported personal consulting fees from Dexcel Pharma and Honeydew outside the submitted work. No other disclosures were reported.
A version of this article appeared on Medscape.com.
FROM JAMA DERMATOLOGY
Updated Guidance for Psoriatic Arthritis Ultrasound Comes at Time of Growing Use, New Technology
WASHINGTON — New draft guidance on the use of musculoskeletal ultrasound (MSUS) for diagnosis, monitoring, and prognosis of psoriatic arthritis was presented at the American College of Rheumatology (ACR) 2024 Annual Meeting. The new recommendations, intended to update 2012 guidance on rheumatologic use of MSUS, will go through another round of expert committee voting before being finalized and published.
“Even in the last 12 years, we’ve seen substantive advances, and there’s been significant improvements in musculoskeletal ultrasound technology,” Veena K. Ranganath, MD, professor of clinical medicine at the University of California, Los Angeles, and director of their Rheumatology Fellowship Musculoskeletal Ultrasound Training Program, told attendees. She noted that more than 30,000 articles on MSUS and arthritis have been published since the 2012 guidance. “We’ve seen mastery in teaching and really a wide distribution of this education to the next generation of rheumatologists, and this has led to significant increases in the use of musculoskeletal ultrasound in clinical practices.”
She also noted there have been significant improvements in therapeutic agents and strategies in psoriatic arthritis medications and that differences in today’s patients compared with those of a decade ago have influenced clinical questions related to the use of MSUS in rheumatology.
To develop the guidelines, a committee identified key domains and relevant clinical questions for ultrasonography using the PICO model (patient/population, intervention, comparison, and outcomes). A review of the literature published since 1993 in PubMed, Embase, and the Cochrane Database provided the evidence base, and a committee of 11 experts voted on the strength of the evidence for 22 statements. They rejected two that lacked consensus, and another round of voting will occur before the guidance is published.
Michael Stein, MD, assistant professor of medicine in rheumatology at McGill University in Montreal, Quebec, Canada, who was not involved in the guidance development, said he hopes and expects this new guidance will help persuade more clinicians to recognize the value of using MSUS in their practice.
“Number one, it’ll highlight the huge amount of data that exist that support using this technology for managing these groups of patients, among others, and I think it’ll also highlight the enormous number of questions that still exist that will hopefully be answered in the future, promoting new research,” Stein told this news organization.
“I do think it does allow people who are not comfortable with technology to adopt technology in a very gradual way and make it less threatening,” Stein added.
“Ultrasound is becoming part of the landscape, and so increasingly, we’re trying to promote it as being part of the standard of care, or at least an adjunct to care. I commend the committee for doing all this amazing work.”
Predicting and Diagnosing Early Psoriatic Arthritis
Catherine J. Bakewell, MD, a rheumatologist at Intermountain Health in Salt Lake City, Utah, reviewed the committee’s statements, starting with strong consensus that MSUS can help with diagnosing early psoriatic arthritis. Evidence has shown that patients with psoriasis who have subclinical synovitis, enthesitis, and other features have gone on to develop psoriatic arthritis, and researchers have documented the transition with ultrasonography.
“We can use it to enhance our CASPAR classification criteria” by using ultrasound to change how clinicians apply the classification criteria, Bakewell said. “For example, in order to go through those classification criteria, a patient has to have confirmed inflammatory articular disease, either the joint synthesis or spine, and ultrasound can help clarify that state for us.”
She also noted the potential for ultrasonography to help as a screening tool because studies have suggested that dermatologists’ use of handheld ultrasound transducers can help in screening appropriate patients to refer to rheumatologists.
Patients with psoriasis being evaluated for a potential early psoriatic arthritis diagnosis should undergo MSUS of the bilateral quadriceps tendon, patellar ligament, Achilles tendon, and plantar fascia entheses at a minimum, per moderate consensus.
“This truly is just designed to be the highest bang for your buck. This is designed for clinicians in practice,” Bakewell said. She noted criticism about the exclusion of upper extremities — something that will be discussed in the future published paper — but one reason that was excluded is because common findings have occurred in healthy individuals in some areas.
Moderate consensus also supported reliance on entheseal features — including hypoechogenicity, thickening, Doppler signal, bone erosions, enthesophytes/calcifications, and bursal enlargement — to support a diagnosis. Interpretation of entheseal changes in patients with psoriasis should take into account characteristics such as age, body mass index (BMI), and biomechanical stress.
“There are numerous articles already existing pointing out that people who are over the age of 50 with a BMI over 30 kg/m2 or who have higher levels of biomechanical stress will score more highly on endocytoscoring systems, even in the absence of an underlying disorder,” Bakewell said. Among the mitigating strategies proposed in the literature are to have at least three positive sites to qualify for an indication or to look at the specificity of each elementary lesion. “Whatever mitigating strategy the clinician chooses to use, they need to bear in mind some of these features are not exclusive to spondyloarthritis,” she said. “It has to be taken in the clinical context.”
Scanning the hand, wrist, foot, and relevant symptomatic joints with MSUS to diagnose early psoriatic arthritis in patients with psoriasis received strong consensus. Intracapsular findings of synovitis and erosions may help support an early diagnosis in patients with psoriasis. “These are not obviously specific to psoriatic arthritis but support the diagnosis” with moderate consensus, Bakewell said. “The more specific findings are these extracapsular findings — which did attain a strong level of consensus — which are enthesitis, tenosynovitis, and dactylitis, all supporting that diagnosis of early psoriatic arthritis.”
For patients with psoriatic arthritis, the cutoff for defining a positive joint received moderate consensus for grayscale (GS) of at least 2 or at least 1 with power Doppler (PD) of at least 1.
Strong consensus supported confirming the presence of dactylitis in patients with psoriasis or psoriatic arthritis through a combination of features including tenosynovitis, subcutaneous edema, soft tissue thickening, synovitis, paratenonitis, and pulley thickening.
“I will also note that enthesitis is missing from this definition of dactylitis,” Bakewell said. “It is, however, a feature that is detectable with those higher-frequency transducers, but this is a relatively early area of research and did not make it into this guidance statement.”
Moderate consensus supported determination of an increased risk of radiographic erosions in patients with a dactylitis PD score of at least 1.
“We know as far back as 2005, Brockbank et al taught us that the dactylitic digit is associated with radiographic erosion in that particular digit,” Bakewell said. “Flash forward all the way to 2021: Dubash et al published the paper, ‘Dactylitis is an indicator of a more severe phenotype independently associated with greater swollen joint counts, C-reactive protein, ultrasound synovitis, and erosive damage,’ showing us that this is more than just that particular digit. It is a more severe phenotype, and very minimal Doppler signal, just 1+, is associated with erosive damage.”
Progression of Psoriatic Arthritis and Shared Decision-Making
Strong consensus existed for all statements related to progression of psoriatic arthritis and the role of MSUS in shared decision-making. The first is that synovitis and enthesitis in MSUS can predict radiographic progression and worsening of patient-related outcomes. Second, sonographic features — including increased Doppler signal in synovitis, enthesitis, and tenosynovitis — and presence of bone erosions and dactylitis can help inform decisions regarding therapy escalation.
“This is the first treatment management–specific statement we have made, but we feel this to be justified because each of these ultrasonographic features is associated with overall inflammatory burden and worse outcomes, be it health assessment questionnaires, disability index, or patient-reported outcomes to harder endpoints, such as radiographic erosions or relapse of clinical remission,” Bakewell said.
Finally, MSUS can help inform patients of their disease activity to assist in shared decision-making regarding escalation or de-escalation of therapy.
“We’ve all had this in our practices. You’ve had the patient in front of you who is very inflamed, and they say, ‘Doctor, can’t I please use doTERRA oils? Do I really need to go on one of these toxic drugs? I’ve read the package insert,’” Bakewell said. “Aside from having that conversation about the relative risk–benefit of any individual medication that you recommend, it’s helpful to put the ultrasound transducer on the patient, show them the fire of the Doppler, show them the erosion, show them the damage that is being done. It comes to life for them, especially if they’re not suffering that much with pain or stiffness.”
Bakewell also addressed patients at the other end of the pain spectrum who are suffering more. “You’ve also probably had the patient with psoriatic arthritis and fibromyalgia who comes in and tells you, ‘Doctor, my psoriatic arthritis has been terrible. I’m flaring. I need more immune-suppressing medication,’” she said. “Their exam looks pretty good, and it’s helpful to put that transducer on them and show them the absence of Doppler signal, show them that you’re taking them very seriously. You didn’t just squeeze them and say they’re fine, but you looked more deeply. You looked underneath the skin, and that helps with that patient–provider understanding and communication. I use this every day.”
Clarifying Disease State and Defining Remission
As with patients with psoriasis undergoing evaluation, there was strong consensus for interpreting entheseal changes in psoriatic arthritis in the context of patient characteristics such as age, BMI, and biomechanical stress.
There was moderate consensus for confirming psoriatic arthritis flare with MSUS. Bakewell noted that many have seen in their practices how physical exams can be misleading, such as when a patient appears clinically normal but has ongoing synovitis, or on the flip side, the patient has a swollen joint but nothing is lighting up with Doppler on the ultrasound.
All of the statements on MSUS for remission received moderate consensus. These included defining MSUS remission as a PD score of 0 in entheses and synovial tissues and defining ultrasonographic remission as a total PD ultrasound score of 0, summing all analyzed joints and entheses, at a single given time point.
When using MSUS to evaluate for remission, it’s reasonable to screen the lower-extremity entheses, wrists, metacarpophalangeal joints, interphalangeal hand joints, metatarsophalangeal joints, and relevant symptomatic joints. The inflammatory features to evaluate to confirm ultrasound-defined remission include PD enthesitis, GS and PD synovitis, tenosynovitis, and dactylitis. Finally, for those in remission, subclinical inflammation detected by MSUS likely predicts a higher rate of flare.
During the discussion, Bakewell reiterated that MSUS should be regarded as a tool for patient subsets who can benefit from its use, rather than being used routinely across large patient groups without a clear purpose. “It’s used to answer a question,” she said. “If you’re going to demonstrate the efficacy of a tool, you have to use it appropriately, aka when there’s a question. We don’t need to ultrasound every patient every visit.”
No external funding for the development of the guidance was noted. Ranganath has reported receiving research support from Bristol Myers Squibb and Mallinckrodt. Bakewell has reported receiving speaking/consulting fees from AbbVie, UCB, Lilly, Janssen, Novartis, Sanofi/Regeneron/Genzyme, and Pfizer. Stein had no disclosures.
A version of this article first appeared on Medscape.com.
WASHINGTON — New draft guidance on the use of musculoskeletal ultrasound (MSUS) for diagnosis, monitoring, and prognosis of psoriatic arthritis was presented at the American College of Rheumatology (ACR) 2024 Annual Meeting. The new recommendations, intended to update 2012 guidance on rheumatologic use of MSUS, will go through another round of expert committee voting before being finalized and published.
“Even in the last 12 years, we’ve seen substantive advances, and there’s been significant improvements in musculoskeletal ultrasound technology,” Veena K. Ranganath, MD, professor of clinical medicine at the University of California, Los Angeles, and director of their Rheumatology Fellowship Musculoskeletal Ultrasound Training Program, told attendees. She noted that more than 30,000 articles on MSUS and arthritis have been published since the 2012 guidance. “We’ve seen mastery in teaching and really a wide distribution of this education to the next generation of rheumatologists, and this has led to significant increases in the use of musculoskeletal ultrasound in clinical practices.”
She also noted there have been significant improvements in therapeutic agents and strategies in psoriatic arthritis medications and that differences in today’s patients compared with those of a decade ago have influenced clinical questions related to the use of MSUS in rheumatology.
To develop the guidelines, a committee identified key domains and relevant clinical questions for ultrasonography using the PICO model (patient/population, intervention, comparison, and outcomes). A review of the literature published since 1993 in PubMed, Embase, and the Cochrane Database provided the evidence base, and a committee of 11 experts voted on the strength of the evidence for 22 statements. They rejected two that lacked consensus, and another round of voting will occur before the guidance is published.
Michael Stein, MD, assistant professor of medicine in rheumatology at McGill University in Montreal, Quebec, Canada, who was not involved in the guidance development, said he hopes and expects this new guidance will help persuade more clinicians to recognize the value of using MSUS in their practice.
“Number one, it’ll highlight the huge amount of data that exist that support using this technology for managing these groups of patients, among others, and I think it’ll also highlight the enormous number of questions that still exist that will hopefully be answered in the future, promoting new research,” Stein told this news organization.
“I do think it does allow people who are not comfortable with technology to adopt technology in a very gradual way and make it less threatening,” Stein added.
“Ultrasound is becoming part of the landscape, and so increasingly, we’re trying to promote it as being part of the standard of care, or at least an adjunct to care. I commend the committee for doing all this amazing work.”
Predicting and Diagnosing Early Psoriatic Arthritis
Catherine J. Bakewell, MD, a rheumatologist at Intermountain Health in Salt Lake City, Utah, reviewed the committee’s statements, starting with strong consensus that MSUS can help with diagnosing early psoriatic arthritis. Evidence has shown that patients with psoriasis who have subclinical synovitis, enthesitis, and other features have gone on to develop psoriatic arthritis, and researchers have documented the transition with ultrasonography.
“We can use it to enhance our CASPAR classification criteria” by using ultrasound to change how clinicians apply the classification criteria, Bakewell said. “For example, in order to go through those classification criteria, a patient has to have confirmed inflammatory articular disease, either the joint synthesis or spine, and ultrasound can help clarify that state for us.”
She also noted the potential for ultrasonography to help as a screening tool because studies have suggested that dermatologists’ use of handheld ultrasound transducers can help in screening appropriate patients to refer to rheumatologists.
Patients with psoriasis being evaluated for a potential early psoriatic arthritis diagnosis should undergo MSUS of the bilateral quadriceps tendon, patellar ligament, Achilles tendon, and plantar fascia entheses at a minimum, per moderate consensus.
“This truly is just designed to be the highest bang for your buck. This is designed for clinicians in practice,” Bakewell said. She noted criticism about the exclusion of upper extremities — something that will be discussed in the future published paper — but one reason that was excluded is because common findings have occurred in healthy individuals in some areas.
Moderate consensus also supported reliance on entheseal features — including hypoechogenicity, thickening, Doppler signal, bone erosions, enthesophytes/calcifications, and bursal enlargement — to support a diagnosis. Interpretation of entheseal changes in patients with psoriasis should take into account characteristics such as age, body mass index (BMI), and biomechanical stress.
“There are numerous articles already existing pointing out that people who are over the age of 50 with a BMI over 30 kg/m2 or who have higher levels of biomechanical stress will score more highly on endocytoscoring systems, even in the absence of an underlying disorder,” Bakewell said. Among the mitigating strategies proposed in the literature are to have at least three positive sites to qualify for an indication or to look at the specificity of each elementary lesion. “Whatever mitigating strategy the clinician chooses to use, they need to bear in mind some of these features are not exclusive to spondyloarthritis,” she said. “It has to be taken in the clinical context.”
Scanning the hand, wrist, foot, and relevant symptomatic joints with MSUS to diagnose early psoriatic arthritis in patients with psoriasis received strong consensus. Intracapsular findings of synovitis and erosions may help support an early diagnosis in patients with psoriasis. “These are not obviously specific to psoriatic arthritis but support the diagnosis” with moderate consensus, Bakewell said. “The more specific findings are these extracapsular findings — which did attain a strong level of consensus — which are enthesitis, tenosynovitis, and dactylitis, all supporting that diagnosis of early psoriatic arthritis.”
For patients with psoriatic arthritis, the cutoff for defining a positive joint received moderate consensus for grayscale (GS) of at least 2 or at least 1 with power Doppler (PD) of at least 1.
Strong consensus supported confirming the presence of dactylitis in patients with psoriasis or psoriatic arthritis through a combination of features including tenosynovitis, subcutaneous edema, soft tissue thickening, synovitis, paratenonitis, and pulley thickening.
“I will also note that enthesitis is missing from this definition of dactylitis,” Bakewell said. “It is, however, a feature that is detectable with those higher-frequency transducers, but this is a relatively early area of research and did not make it into this guidance statement.”
Moderate consensus supported determination of an increased risk of radiographic erosions in patients with a dactylitis PD score of at least 1.
“We know as far back as 2005, Brockbank et al taught us that the dactylitic digit is associated with radiographic erosion in that particular digit,” Bakewell said. “Flash forward all the way to 2021: Dubash et al published the paper, ‘Dactylitis is an indicator of a more severe phenotype independently associated with greater swollen joint counts, C-reactive protein, ultrasound synovitis, and erosive damage,’ showing us that this is more than just that particular digit. It is a more severe phenotype, and very minimal Doppler signal, just 1+, is associated with erosive damage.”
Progression of Psoriatic Arthritis and Shared Decision-Making
Strong consensus existed for all statements related to progression of psoriatic arthritis and the role of MSUS in shared decision-making. The first is that synovitis and enthesitis in MSUS can predict radiographic progression and worsening of patient-related outcomes. Second, sonographic features — including increased Doppler signal in synovitis, enthesitis, and tenosynovitis — and presence of bone erosions and dactylitis can help inform decisions regarding therapy escalation.
“This is the first treatment management–specific statement we have made, but we feel this to be justified because each of these ultrasonographic features is associated with overall inflammatory burden and worse outcomes, be it health assessment questionnaires, disability index, or patient-reported outcomes to harder endpoints, such as radiographic erosions or relapse of clinical remission,” Bakewell said.
Finally, MSUS can help inform patients of their disease activity to assist in shared decision-making regarding escalation or de-escalation of therapy.
“We’ve all had this in our practices. You’ve had the patient in front of you who is very inflamed, and they say, ‘Doctor, can’t I please use doTERRA oils? Do I really need to go on one of these toxic drugs? I’ve read the package insert,’” Bakewell said. “Aside from having that conversation about the relative risk–benefit of any individual medication that you recommend, it’s helpful to put the ultrasound transducer on the patient, show them the fire of the Doppler, show them the erosion, show them the damage that is being done. It comes to life for them, especially if they’re not suffering that much with pain or stiffness.”
Bakewell also addressed patients at the other end of the pain spectrum who are suffering more. “You’ve also probably had the patient with psoriatic arthritis and fibromyalgia who comes in and tells you, ‘Doctor, my psoriatic arthritis has been terrible. I’m flaring. I need more immune-suppressing medication,’” she said. “Their exam looks pretty good, and it’s helpful to put that transducer on them and show them the absence of Doppler signal, show them that you’re taking them very seriously. You didn’t just squeeze them and say they’re fine, but you looked more deeply. You looked underneath the skin, and that helps with that patient–provider understanding and communication. I use this every day.”
Clarifying Disease State and Defining Remission
As with patients with psoriasis undergoing evaluation, there was strong consensus for interpreting entheseal changes in psoriatic arthritis in the context of patient characteristics such as age, BMI, and biomechanical stress.
There was moderate consensus for confirming psoriatic arthritis flare with MSUS. Bakewell noted that many have seen in their practices how physical exams can be misleading, such as when a patient appears clinically normal but has ongoing synovitis, or on the flip side, the patient has a swollen joint but nothing is lighting up with Doppler on the ultrasound.
All of the statements on MSUS for remission received moderate consensus. These included defining MSUS remission as a PD score of 0 in entheses and synovial tissues and defining ultrasonographic remission as a total PD ultrasound score of 0, summing all analyzed joints and entheses, at a single given time point.
When using MSUS to evaluate for remission, it’s reasonable to screen the lower-extremity entheses, wrists, metacarpophalangeal joints, interphalangeal hand joints, metatarsophalangeal joints, and relevant symptomatic joints. The inflammatory features to evaluate to confirm ultrasound-defined remission include PD enthesitis, GS and PD synovitis, tenosynovitis, and dactylitis. Finally, for those in remission, subclinical inflammation detected by MSUS likely predicts a higher rate of flare.
During the discussion, Bakewell reiterated that MSUS should be regarded as a tool for patient subsets who can benefit from its use, rather than being used routinely across large patient groups without a clear purpose. “It’s used to answer a question,” she said. “If you’re going to demonstrate the efficacy of a tool, you have to use it appropriately, aka when there’s a question. We don’t need to ultrasound every patient every visit.”
No external funding for the development of the guidance was noted. Ranganath has reported receiving research support from Bristol Myers Squibb and Mallinckrodt. Bakewell has reported receiving speaking/consulting fees from AbbVie, UCB, Lilly, Janssen, Novartis, Sanofi/Regeneron/Genzyme, and Pfizer. Stein had no disclosures.
A version of this article first appeared on Medscape.com.
WASHINGTON — New draft guidance on the use of musculoskeletal ultrasound (MSUS) for diagnosis, monitoring, and prognosis of psoriatic arthritis was presented at the American College of Rheumatology (ACR) 2024 Annual Meeting. The new recommendations, intended to update 2012 guidance on rheumatologic use of MSUS, will go through another round of expert committee voting before being finalized and published.
“Even in the last 12 years, we’ve seen substantive advances, and there’s been significant improvements in musculoskeletal ultrasound technology,” Veena K. Ranganath, MD, professor of clinical medicine at the University of California, Los Angeles, and director of their Rheumatology Fellowship Musculoskeletal Ultrasound Training Program, told attendees. She noted that more than 30,000 articles on MSUS and arthritis have been published since the 2012 guidance. “We’ve seen mastery in teaching and really a wide distribution of this education to the next generation of rheumatologists, and this has led to significant increases in the use of musculoskeletal ultrasound in clinical practices.”
She also noted there have been significant improvements in therapeutic agents and strategies in psoriatic arthritis medications and that differences in today’s patients compared with those of a decade ago have influenced clinical questions related to the use of MSUS in rheumatology.
To develop the guidelines, a committee identified key domains and relevant clinical questions for ultrasonography using the PICO model (patient/population, intervention, comparison, and outcomes). A review of the literature published since 1993 in PubMed, Embase, and the Cochrane Database provided the evidence base, and a committee of 11 experts voted on the strength of the evidence for 22 statements. They rejected two that lacked consensus, and another round of voting will occur before the guidance is published.
Michael Stein, MD, assistant professor of medicine in rheumatology at McGill University in Montreal, Quebec, Canada, who was not involved in the guidance development, said he hopes and expects this new guidance will help persuade more clinicians to recognize the value of using MSUS in their practice.
“Number one, it’ll highlight the huge amount of data that exist that support using this technology for managing these groups of patients, among others, and I think it’ll also highlight the enormous number of questions that still exist that will hopefully be answered in the future, promoting new research,” Stein told this news organization.
“I do think it does allow people who are not comfortable with technology to adopt technology in a very gradual way and make it less threatening,” Stein added.
“Ultrasound is becoming part of the landscape, and so increasingly, we’re trying to promote it as being part of the standard of care, or at least an adjunct to care. I commend the committee for doing all this amazing work.”
Predicting and Diagnosing Early Psoriatic Arthritis
Catherine J. Bakewell, MD, a rheumatologist at Intermountain Health in Salt Lake City, Utah, reviewed the committee’s statements, starting with strong consensus that MSUS can help with diagnosing early psoriatic arthritis. Evidence has shown that patients with psoriasis who have subclinical synovitis, enthesitis, and other features have gone on to develop psoriatic arthritis, and researchers have documented the transition with ultrasonography.
“We can use it to enhance our CASPAR classification criteria” by using ultrasound to change how clinicians apply the classification criteria, Bakewell said. “For example, in order to go through those classification criteria, a patient has to have confirmed inflammatory articular disease, either the joint synthesis or spine, and ultrasound can help clarify that state for us.”
She also noted the potential for ultrasonography to help as a screening tool because studies have suggested that dermatologists’ use of handheld ultrasound transducers can help in screening appropriate patients to refer to rheumatologists.
Patients with psoriasis being evaluated for a potential early psoriatic arthritis diagnosis should undergo MSUS of the bilateral quadriceps tendon, patellar ligament, Achilles tendon, and plantar fascia entheses at a minimum, per moderate consensus.
“This truly is just designed to be the highest bang for your buck. This is designed for clinicians in practice,” Bakewell said. She noted criticism about the exclusion of upper extremities — something that will be discussed in the future published paper — but one reason that was excluded is because common findings have occurred in healthy individuals in some areas.
Moderate consensus also supported reliance on entheseal features — including hypoechogenicity, thickening, Doppler signal, bone erosions, enthesophytes/calcifications, and bursal enlargement — to support a diagnosis. Interpretation of entheseal changes in patients with psoriasis should take into account characteristics such as age, body mass index (BMI), and biomechanical stress.
“There are numerous articles already existing pointing out that people who are over the age of 50 with a BMI over 30 kg/m2 or who have higher levels of biomechanical stress will score more highly on endocytoscoring systems, even in the absence of an underlying disorder,” Bakewell said. Among the mitigating strategies proposed in the literature are to have at least three positive sites to qualify for an indication or to look at the specificity of each elementary lesion. “Whatever mitigating strategy the clinician chooses to use, they need to bear in mind some of these features are not exclusive to spondyloarthritis,” she said. “It has to be taken in the clinical context.”
Scanning the hand, wrist, foot, and relevant symptomatic joints with MSUS to diagnose early psoriatic arthritis in patients with psoriasis received strong consensus. Intracapsular findings of synovitis and erosions may help support an early diagnosis in patients with psoriasis. “These are not obviously specific to psoriatic arthritis but support the diagnosis” with moderate consensus, Bakewell said. “The more specific findings are these extracapsular findings — which did attain a strong level of consensus — which are enthesitis, tenosynovitis, and dactylitis, all supporting that diagnosis of early psoriatic arthritis.”
For patients with psoriatic arthritis, the cutoff for defining a positive joint received moderate consensus for grayscale (GS) of at least 2 or at least 1 with power Doppler (PD) of at least 1.
Strong consensus supported confirming the presence of dactylitis in patients with psoriasis or psoriatic arthritis through a combination of features including tenosynovitis, subcutaneous edema, soft tissue thickening, synovitis, paratenonitis, and pulley thickening.
“I will also note that enthesitis is missing from this definition of dactylitis,” Bakewell said. “It is, however, a feature that is detectable with those higher-frequency transducers, but this is a relatively early area of research and did not make it into this guidance statement.”
Moderate consensus supported determination of an increased risk of radiographic erosions in patients with a dactylitis PD score of at least 1.
“We know as far back as 2005, Brockbank et al taught us that the dactylitic digit is associated with radiographic erosion in that particular digit,” Bakewell said. “Flash forward all the way to 2021: Dubash et al published the paper, ‘Dactylitis is an indicator of a more severe phenotype independently associated with greater swollen joint counts, C-reactive protein, ultrasound synovitis, and erosive damage,’ showing us that this is more than just that particular digit. It is a more severe phenotype, and very minimal Doppler signal, just 1+, is associated with erosive damage.”
Progression of Psoriatic Arthritis and Shared Decision-Making
Strong consensus existed for all statements related to progression of psoriatic arthritis and the role of MSUS in shared decision-making. The first is that synovitis and enthesitis in MSUS can predict radiographic progression and worsening of patient-related outcomes. Second, sonographic features — including increased Doppler signal in synovitis, enthesitis, and tenosynovitis — and presence of bone erosions and dactylitis can help inform decisions regarding therapy escalation.
“This is the first treatment management–specific statement we have made, but we feel this to be justified because each of these ultrasonographic features is associated with overall inflammatory burden and worse outcomes, be it health assessment questionnaires, disability index, or patient-reported outcomes to harder endpoints, such as radiographic erosions or relapse of clinical remission,” Bakewell said.
Finally, MSUS can help inform patients of their disease activity to assist in shared decision-making regarding escalation or de-escalation of therapy.
“We’ve all had this in our practices. You’ve had the patient in front of you who is very inflamed, and they say, ‘Doctor, can’t I please use doTERRA oils? Do I really need to go on one of these toxic drugs? I’ve read the package insert,’” Bakewell said. “Aside from having that conversation about the relative risk–benefit of any individual medication that you recommend, it’s helpful to put the ultrasound transducer on the patient, show them the fire of the Doppler, show them the erosion, show them the damage that is being done. It comes to life for them, especially if they’re not suffering that much with pain or stiffness.”
Bakewell also addressed patients at the other end of the pain spectrum who are suffering more. “You’ve also probably had the patient with psoriatic arthritis and fibromyalgia who comes in and tells you, ‘Doctor, my psoriatic arthritis has been terrible. I’m flaring. I need more immune-suppressing medication,’” she said. “Their exam looks pretty good, and it’s helpful to put that transducer on them and show them the absence of Doppler signal, show them that you’re taking them very seriously. You didn’t just squeeze them and say they’re fine, but you looked more deeply. You looked underneath the skin, and that helps with that patient–provider understanding and communication. I use this every day.”
Clarifying Disease State and Defining Remission
As with patients with psoriasis undergoing evaluation, there was strong consensus for interpreting entheseal changes in psoriatic arthritis in the context of patient characteristics such as age, BMI, and biomechanical stress.
There was moderate consensus for confirming psoriatic arthritis flare with MSUS. Bakewell noted that many have seen in their practices how physical exams can be misleading, such as when a patient appears clinically normal but has ongoing synovitis, or on the flip side, the patient has a swollen joint but nothing is lighting up with Doppler on the ultrasound.
All of the statements on MSUS for remission received moderate consensus. These included defining MSUS remission as a PD score of 0 in entheses and synovial tissues and defining ultrasonographic remission as a total PD ultrasound score of 0, summing all analyzed joints and entheses, at a single given time point.
When using MSUS to evaluate for remission, it’s reasonable to screen the lower-extremity entheses, wrists, metacarpophalangeal joints, interphalangeal hand joints, metatarsophalangeal joints, and relevant symptomatic joints. The inflammatory features to evaluate to confirm ultrasound-defined remission include PD enthesitis, GS and PD synovitis, tenosynovitis, and dactylitis. Finally, for those in remission, subclinical inflammation detected by MSUS likely predicts a higher rate of flare.
During the discussion, Bakewell reiterated that MSUS should be regarded as a tool for patient subsets who can benefit from its use, rather than being used routinely across large patient groups without a clear purpose. “It’s used to answer a question,” she said. “If you’re going to demonstrate the efficacy of a tool, you have to use it appropriately, aka when there’s a question. We don’t need to ultrasound every patient every visit.”
No external funding for the development of the guidance was noted. Ranganath has reported receiving research support from Bristol Myers Squibb and Mallinckrodt. Bakewell has reported receiving speaking/consulting fees from AbbVie, UCB, Lilly, Janssen, Novartis, Sanofi/Regeneron/Genzyme, and Pfizer. Stein had no disclosures.
A version of this article first appeared on Medscape.com.
FROM ACR 2024
Eating Disorder Risk Factors and the Impact of Obesity in Patients With Psoriasis
Psoriasis is a chronic multisystemic inflammatory skin disease with a worldwide prevalence of 2% to 3%.1 Psoriasis can be accompanied by other conditions such as psoriatic arthritis, obesity, metabolic syndrome, diabetes mellitus, hypertension, dyslipidemia, atherosclerotic disease, inflammatory bowel disease, and anxiety/depression. It is important to manage comorbidities of psoriasis in addition to treating the cutaneous manifestations of the disease.1
Obesity is a major public health concern worldwide. Numerous observational and epidemiologic studies have reported a high prevalence of obesity among patients with psoriasis.2 Current evidence indicates that obesity may initiate or worsen psoriasis; furthermore, it is important to note that obesity may negatively impact the effectiveness of psoriasis-specific treatments or increase the incidence of adverse effects. Therefore, managing obesity is crucial in the treatment of psoriasis.3 Numerous studies have investigated the association between psoriasis and obesity, and they commonly conclude that both conditions share the same genetic metabolic pathways.2-4 However, it is important to consider environmental factors such as dietary habits, smoking, alcohol consumption, and a sedentary lifestyle—all of which are associated with psoriasis and also can contribute to the development of obesity.5 Because of the effects of obesity in psoriasis patients, factors that impact the development of obesity have become a popular research topic.
Eating disorders (EDs) are a crucial risk factor for both developing and maintaining obesity. In particular, two EDs that are associated with obesity include binge eating disorder and bulimia nervosa.6 According to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition,7 binge eating disorder can be diagnosed when a patient has at least 1 episode of binge eating per week over a 3-month period. Bulimia nervosa can be diagnosed when a patient is excessively concerned with their body weight and shape and engages in behaviors to prevent weight gain (eg, forced vomiting, excessive use of laxatives).7 Psychiatrists who specialize in EDs make diagnoses based on these criteria. In daily practice, there are several quick and simple questionnaires available to screen for EDs that can be used by nonpsychiatrist physicians, including the commonly used 26-item Eating Attitudes Test (EAT-26).8 The EAT-26 has been used to screen for EDs in patients with inflammatory disorders.9
The aim of this study was to screen for EDs in patients with psoriasis to identify potential risk factors for development of obesity.
Materials and Methods
This study included patients with psoriasis who were screened for EDs at a tertiary dermatology clinic in Turkey between January 2021 and December 2023. This study was approved by the local ethics committee and was in accordance with the Declaration of Helsinki (decision number E-93471371-514.99-225000079).
Study Design and Patient Inclusion Criteria—This quantitative cross-sectional study utilized EAT-26, Dermatology Life Quality Index (DLQI), Attitude Scale for Healthy Nutrition (ASHN), and Depression Anxiety Stress Scale-21 (DASS-21) scores. All the questionnaire scales used in the study were adapted and validated in Turkey.8,10-12 The inclusion criteria consisted of being older than 18 years of age, being literate, having psoriasis for at least 1 year that was not treated topically or systemically, and having no psychiatric diseases outside an ED. The questionnaires were presented in written format following the clinical examination. Literacy was an inclusion criterion in this study due to the absence of auxiliary health personnel.
Study Variables—The study variables included age, sex, marital status (single/divorced or married), education status (primary/secondary school or high school/university), employment status (employed or unemployed/retired), body mass index (BMI), smoking status, alcohol-consumption status, Psoriasis Area Severity Index score, presence of nail psoriasis and psoriatic arthritis, duration of psoriasis, family history of psoriasis, EAT-26 score, ASHN score, DLQI score, and DASS-21 score. Body mass index was calculated by taking a participant’s weight in kilograms and dividing it by their height in meters squared. The BMI values were classified into 3 categories: normal (18.5–24.9 kg/m2), overweight (25.0–29.9 kg/m2), and obese (≥30 kg/m2).13
Questionnaires—The EAT-26 questionnaire includes 26 questions that are used to detect EDs. Responses to each question include Likert-type answer options (ie, “always,” “usually,” “often,” “sometimes,” “rarely,” and “never.”) Patients with scores of 20 points or higher (range, 0–78) are classified as high risk for EDs.8 In our study, EAT-26 scores were grouped into 2 categories: patients scoring less than 20 points and those scoring 20 points or higher.
The DLQI questionnaire includes 10 questions to measure dermatologic symptoms and qualiy of life. Responses to each question include Likert-type answer options (ie, “not at all,” “a little,” “a lot,” or “very much.”) On the DLQI scale, the higher the score, the lower the quality of life (score range, 0–30).10
The ASHN questionnaire includes 21 questions that measure attitudes toward healthy nutrition with 5 possible answer options (“strongly disagree,” “disagree,” “undecided,” “agree,” and “strongly agree”). On this scale, higher scores indicate the participant is more knowledgeable about healthy nutrition (score range, 0–78).11
The DASS-21 questionnaire includes 21 questions that measure the severity of a range of symptoms common to depression, anxiety, and stress. Responses include Likert-type answer options (eg, “never,” “sometimes,” “often,” and “almost always.”) On this scale, a higher score (range of 0–21 for each) indicates higher levels of depression, anxiety, and stress.12
Statistical Analysis—Descriptive statistics were analyzed using SPSS software version 22.0 (IBM). The Shapiro-Wilk test was applied to determine whether the data were normally distributed. For categorical variables, frequency differences among groups were compared using the Pearson χ2 test. A t test was used to compare the means of 2 independent groups with a normal distribution. One-way analysis of variance and Tukey Honest Significant Difference post hoc analysis were used to test whether there was a statistically significant difference among the normally distributed means of independent groups. Pearson correlation analysis was used to determine whether there was a linear relationship between 2 numeric measurements and, if so, to determine the direction and severity of this relationship. P<.05 indicated statistical significance in this study.
Results
Study Participant Demographics—This study included 82 participants with a mean age of 44.3 years; 52.4% (43/82) were female, and 85.4% (70/82) were married. The questionnaire took an average of 4.2 minutes for participants to complete. A total of 57.3% (47/82) of patients had completed primary/secondary education and 59.8% (49/82) were employed. The mean BMI was 28.1 kg/m2. According to the BMI classification, 26.8% (22/82) participants had a normal weight, 36.6% (30/82) were overweight, and 43.9% (36/82) were obese. A total of 48.8% (40/82) of participants smoked, and 4.9% (4/82) consumed alcohol. The mean Psoriasis Area and Severity Index score was 5.4. A total of 54.9% (45/82) of participants had nail psoriasis, and 24.4% (20/82) had psoriatic arthritis. The mean duration of psoriasis was 153 months. A total of 29.3% (24/82) of participants had a positive family history of psoriasis. The mean EAT-26 score was 11.1. A total of 12.2% (10/82) of participants had an EAT-26 score of 20 points or higher and were considered at high risk for an ED. The mean ASHN score was 72.9; the mean DLQI score was 5.5; and on the DASS-21 scale, mean scores for depression, anxiety, and stress were 6.3, 8.7, and 10.0, respectively (Table).
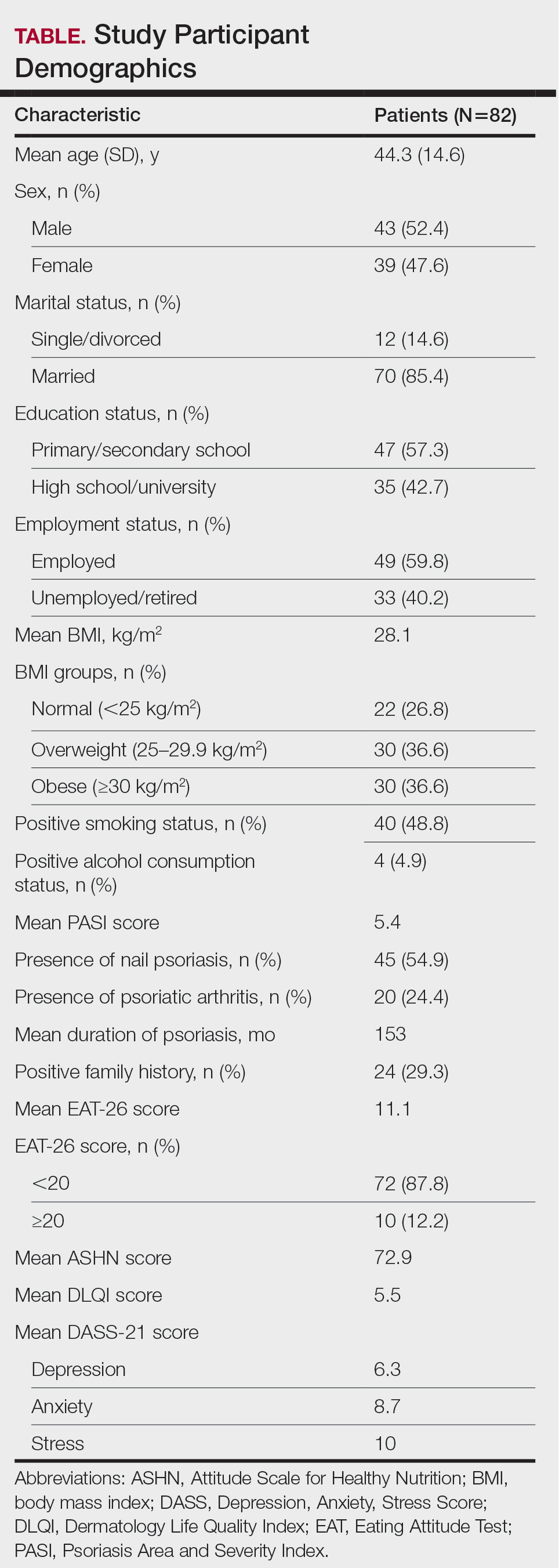
Comparative Evaluation of the BMI Groups—The only statistically significant differences among the 3 BMI groups were related to marital status, EAT-26 score, and anxiety and stress scores (P=.02, <.01, <.01, and <.01, respectively)(eTable 1). The number of single/divorced participants in the overweight group was significantly (P=.02) greater than in the normal weight group. The mean EAT-26 score for the normal weight group was significantly (P<.01) lower than for the overweight and obese groups; there was no significant difference in mean EAT-26 scores between the overweight and obese groups. The mean anxiety score was significantly (P<.01) lower in the normal weight group compared with the overweight and obese groups. There was no significant difference between the overweight and obese groups according to the mean depression score. The mean stress and anxiety scores were significantly (P<.01) lower in the normal weight group than in the overweight and obese groups. There was no significant difference between the overweight and obese groups according to the mean anxiety score.
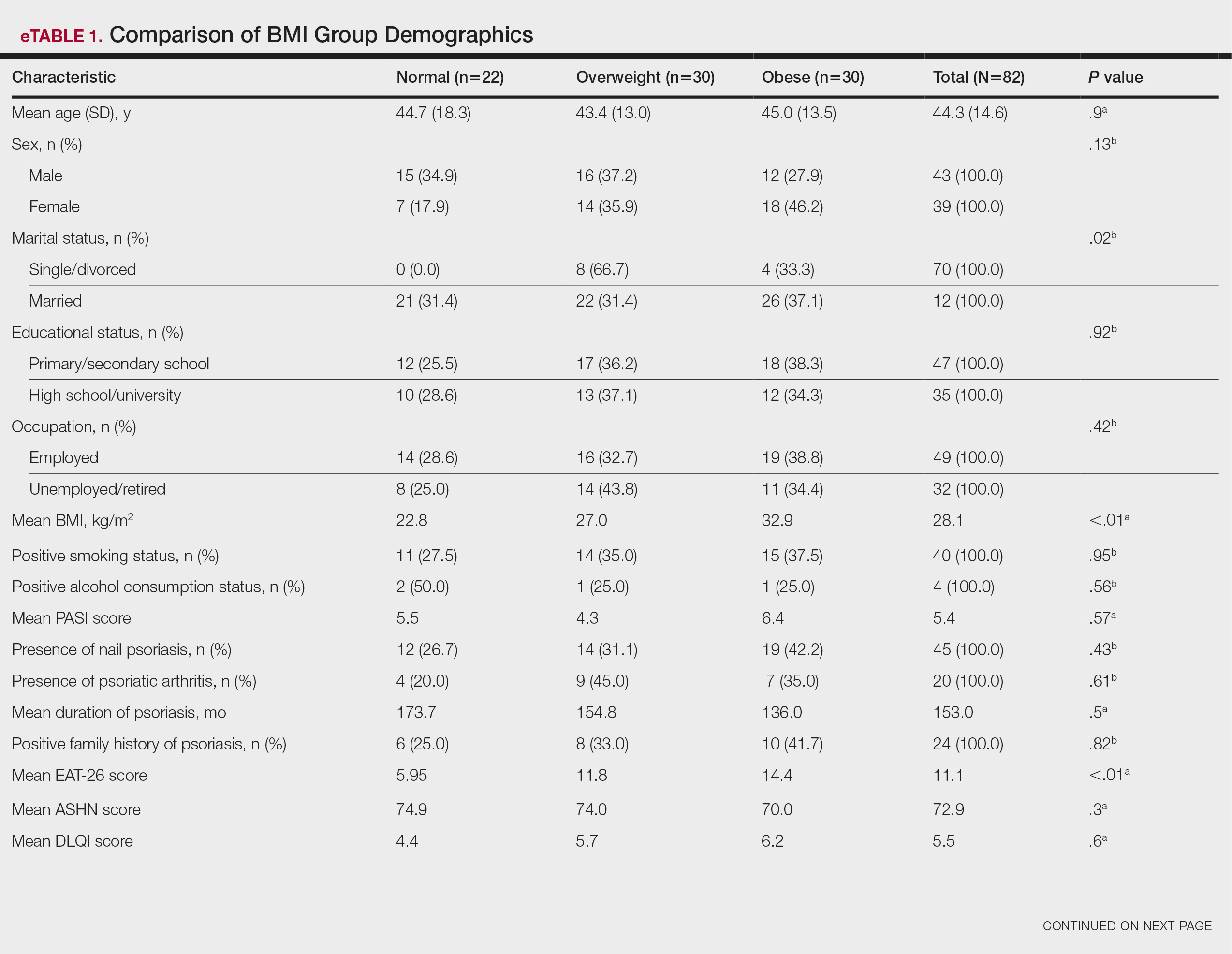
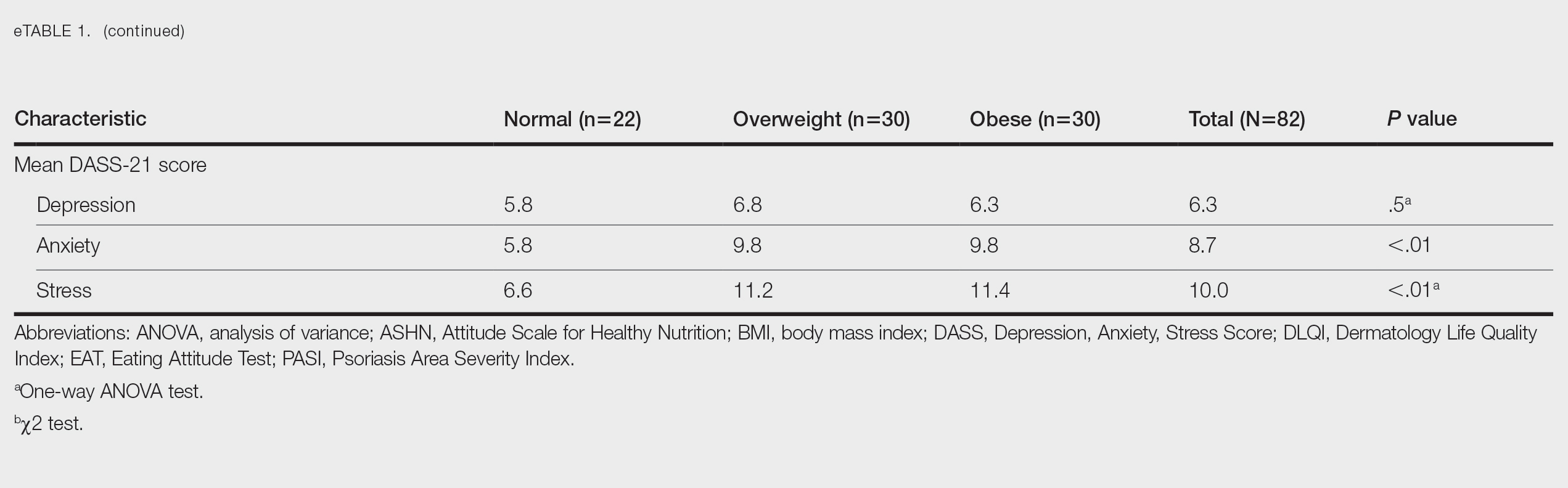
Comparative Evaluation of the EAT-26 Scores—There were statistically significant differences among the EAT-26 scores related to sex; BMI; and depression, anxiety, and stress scores (P=.04, .02, <.01, <.01, and <.01, respectively). The number of females in the group with a score of 20 points or higher was significantly (P=.04) less than that in the group scoring less than 20 points. The mean BMI in the group with a score of 20 points or higher was significantly (P=.02) greater than in group scoring less than 20 points. The mean depression, anxiety, and stress scores of the group scoring 20 points or higher were significantly (P<.01 for all) greater than in the group scoring less than 20 points (eTable 2).
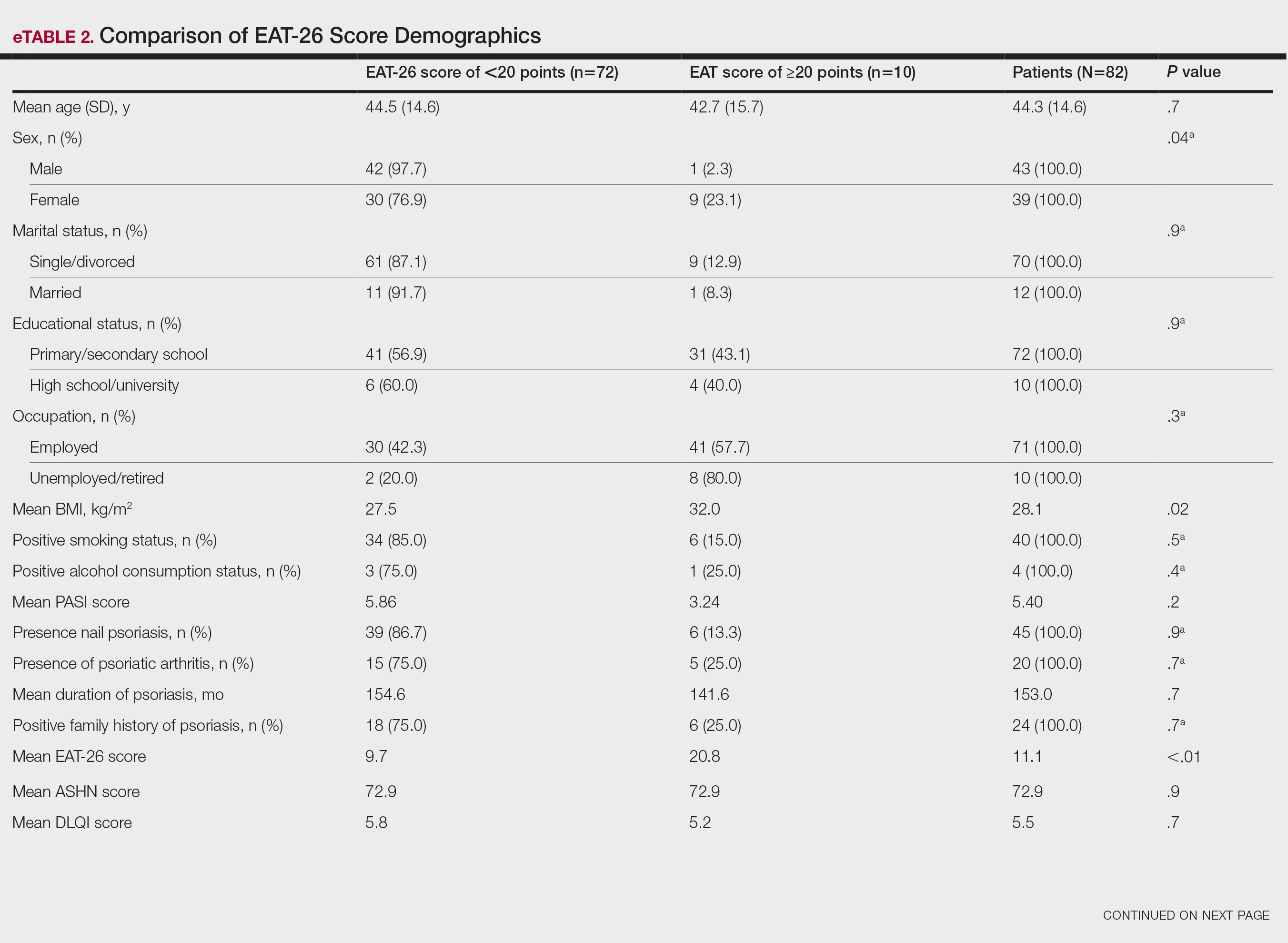
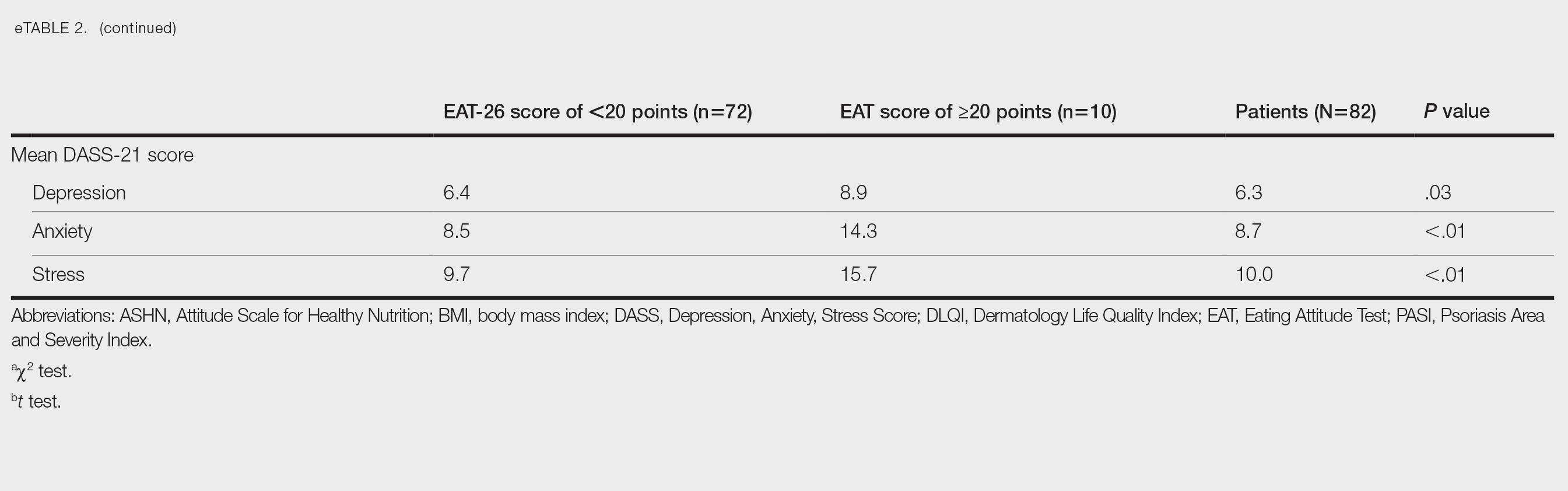
Correlation Analysis of the Study Variables—The EAT-26 scores were positively correlated with BMI, anxiety, depression, and stress (P<.01 for all)(eTable 3).
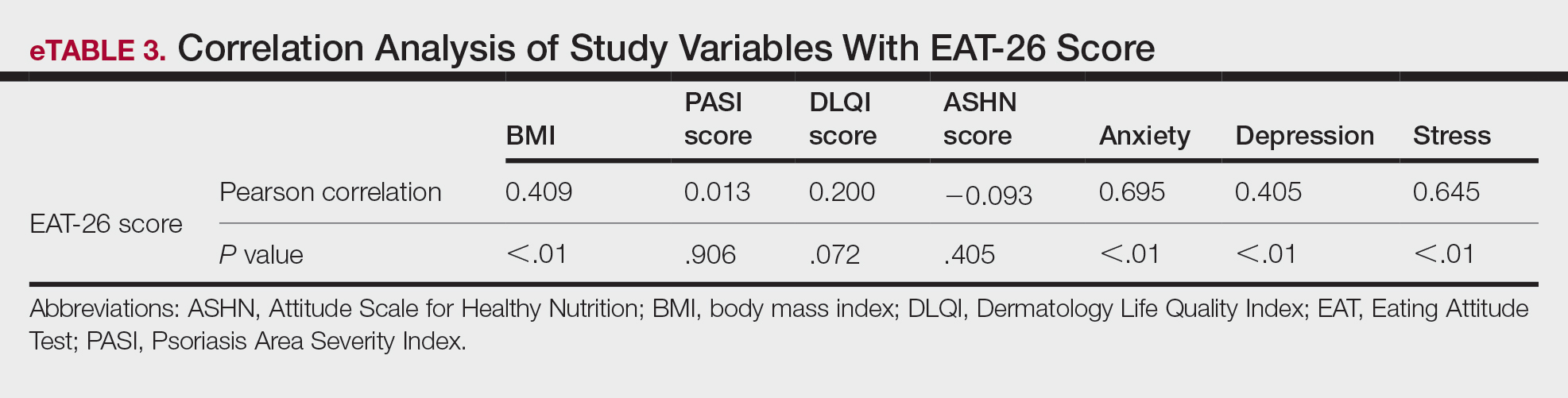
Comment
Eating disorders are psychiatric conditions that require a multidisciplinary approach. Nonpsychiatric medical departments may be involved due to the severe consequences (eg, various skin changes14) of these disorders. Psoriasis is not known to be directly affected by the presence of an ED; however, it is possible that EDs could indirectly affect patients with psoriasis by influencing obesity. Therefore, this study aimed to examine the relationship between ED risk factors and obesity in this population.
The relationship between psoriasis and obesity has been a popular research topic in dermatology since the 1990s.15 Epidemiologic and observational studies have reported that patients with psoriasis are more likely to be overweight or have obesity, which is an independent risk factor for psoriasis.3,16 However, the causal relationship between psoriasis and obesity remains unclear. In a comprehensive review, Barros et al17 emphasized the causal relationship between obesity and psoriasis under several headings. Firstly, a higher BMI increases the risk for psoriasis by promoting cytokine release and immune system dysregulation. Secondly, a Western diet (eg, processed foods and fast food) triggers obesity and psoriasis by increasing adipose tissue. Thirdly, the alteration of the skin and gut microbiota triggers chronic inflammation as a result of bacterial translocation in patients with obesity. Fourthly, a high-fat diet and palmitic acid disrupt the intestinal integrity of the gut and increase the risk for psoriasis and obesity by triggering chronic inflammation of bacterial fragments that pass into the blood. Finally, the decrease in the amount of adiponectin and the increase in the amount of leptin in patients with obesity may cause psoriasis by increasing proinflammatory cytokines, which are similar to those involved in the pathogenesis of psoriasis.17 Additionally, psoriatic inflammation can cause insulin resistance and metabolic dysfunction, leading to obesity.18 The relationship between psoriasis and obesity cannot be solely explained by metabolic pathways. Smoking, alcohol consumption, and a sedentary lifestyle all are associated with psoriasis and also can contribute to obesity.5 Our study revealed no significant difference in smoking or alcohol consumption between the normal weight and overweight/obesity groups. Based on our data, we determined that smoking and alcohol consumption did not affect obesity in our patients with psoriasis.
Observational and epidemiologic studies have shown that patients with psoriasis experience increased rates of depression, anxiety, and stress.19 In studies of pathogenesis, a connection between depression and psoriatic inflammation has been established.20 It is known that inflammatory cytokines similar to those in psoriasis are involved in the development of obesity.18 In addition, depression and anxiety can lead to binge eating, unhealthy food choices, and a more sedentary lifestyle.5 All of these variables may contribute to the associations between depression and anxiety with psoriasis and obesity. Zafiriou et al21 conducted a study to investigate the relationship between psoriasis, obesity, and depression through inflammatory pathways with a focus on the importance of IL-17. Data showing that IL-17–producing Th17-cell subgroups play a considerable role in the development of obesity and depression prompted the authors to suggest that psoriasis, obesity, and anxiety/depression may be interconnected manifestations of immune dysregulation, potentially linked to IL-17 and its associated cells.21 Mrowietz et al22 also suggested that metabolic inflammation may contribute to obesity and depression in patients with psoriasis and highlighted the importance of several cytokines, including tumor necrosis factor α, IL-6, IL-8, IL-17, and IL-23. Our study revealed no significant differences in depression scores between BMI groups. Another meta-analysis reported conflicting findings on the incidence of depression in obese patients with psoriasis.23 Some of the studies had a small number of participants. Compared to depression, anxiety has received less attention in studies of patients with obesity with psoriasis. However, these studies have shown a positive correlation between anxiety scores and BMI in patients with psoriasis.24,25 In our study, similar to the findings of previous studies, overweight patients and those with obesitywho have psoriasis had significantly (P<.01) greater anxiety and stress scores than did normal weight patients with psoriasis.
Obesity should be assessed in patients with psoriasis via a biopsychosocial approach that takes into account genetic, behavioral, and environmental factors.26 Eating disorders are considered to be one of the factors contributing to obesity. Numerous studies in the literature have demonstrated a greater incidence of EDs in patients with obesity vs those without obesity.5,6,27 Obesity and EDs have a bidirectional relationship: individuals with obesity are at risk for EDs due to body dissatisfaction, dieting habits, and depressive states. Conversely, poor eating behaviors in individuals with a normal weight can lead to obesity.28
There are few studies in the literature exploring the relationship between psoriasis and EDs. Crosta et al29 demonstrated that patients with psoriasis had impaired results on ED screening tests and that these scores deteriorated further as BMI increased. Moreover, Altunay et al30 demonstrated that patients with psoriasis and metabolic syndrome had higher scores on the ED screening test. In this study, patients with higher scores also exhibited high levels of anxiety.30 In our study, similar to the findings of previous studies, patients with psoriasis who were overweight or had obesity had significantly (P<.01) greater EAT-26 scores than those in the normal weight group. Patients with high EAT-26 scores also exhibited elevated levels of depression, anxiety, and stress. Additionally, EAT-26 scores were positively correlated with BMI, anxiety, depression, and stress scores. Our study as well as other studies in the literature indicate that additional research is needed to determine the associations between EDs and obesity in psoriasis.
Conclusion
Managing obesity is crucial for patients with psoriasis. This study showed that EAT-26 scores were higher in patients with psoriasis who were overweight or had obesity than in those who were normal weight. Participants with high EAT-26 scores (≥20 points) were more likely to be female and have higher anxiety and stress scores. In addition, EAT-26 scores were positively correlated with BMI as well as depression, anxiety, and stress scores. Eating disorders may contribute to the development of obesity in patients with psoriasis. Although our study was limited by a small sample size, the results suggest that there is a need for large-scale multicenter studies to investigate the relationship between psoriasis and EDs.
- Kalkan G. Comorbidities in psoriasis: the recognition of psoriasis as a systemic disease and current management. Turkderm-Turk Arch Dermatol Venereol. 2017;51:71-77.
- Armstrong AW, Harskamp CT, Armstrong EJ. The association between psoriasis and obesity: a systematic review and meta-analysis of observational studies. Nutr Diabetes. 2012;2:E54.
- Jensen P, Skov L. Psoriasis and obesity. Dermatology. 2016;232:633-639.
- Mirghani H, Altemani AT, Altemani ST, et al. The cross talk between psoriasis, obesity, and dyslipidemia: a meta-analysis. Cureus. 2023;15:e49253.
- Roehring M, Mashep MR, White MA, et al. The metabolic syndrome and behavioral correlates in obese patients with binge disorders. Obesity. 2009;17:481-486.
- da Luz FQ, Hay P, Touyz S, et al. Obesity with comorbid eating disorders: associated health risks and treatment approaches. Nutrients. 2018;10:829.
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition. American Psychiatric Association; 2013.
- Ergüney Okumus¸ FE, Sertel Berk HÖ. The psychometric properties of the Eating Attitudes Test short form (EAT-26) in a college sample. Stud Psychol. 2020;40:57-78.
- Stoleru G, Leopold A, Auerbach A, et al. Female gender, dissatisfaction with weight, and number of IBD related surgeries as independent risk factors for eating disorders among patients with inflammatory bowel diseases. BMC Gastroenterol. 2022;22:438.
- Öztürkcan S, Ermertcan AT, Eser E, et al. Cross validation of the Turkish version of dermatology life quality index. Int J Dermatol. 2006;45:1300-1307.
- Demir GT, Ciciog˘lu HI˙. Attitude scale for healthy nutrition (ASHN): validity and reliability study. Gaziantep Univ J Sport Sci. 2019;4:256-274.
- Yılmaz O, Boz H, Arslan A. The validity and reliability of depression stress and anxiety scale (DASS 21) Turkish short form. Res Financial Econ Soc Stud. 2017;2:78-91.
- Nuttall FQ. Body mass index: obesity, BMI, and health: a critical review. Nutr Today. 2015;50:117-128.
- Strumia R, Manzata E, Gualandi M. Is there a role for dermatologists in eating disorders? Expert Rev Dermatol. 2017; 2:109-112.
- Henseler T, Christophers E. Disease concomitance in psoriasis. J Am Acad Dermatol. 1995;32:982-986.
- Naldi L, Addis A, Chimenti S, et al. Impact of body mass index and obesity on clinical response to systemic treatment for psoriasis. evidence from the Psocare project. Dermatology. 2008;217:365-373.
- Barros G, Duran P, Vera I, et al. Exploring the links between obesity and psoriasis: a comprehensive review. Int J Mol Sci. 2022;23:7499.
- Hao Y, Zhu YJ, Zou S, et al. Metabolic syndrome and psoriasis: mechanisms and future directions. Front Immunol. 2021;12:711060.
- Jing D, Xiao H, Shen M, et al. Association of psoriasis with anxiety and depression: a case–control study in Chinese patients. Front Med (Lausanne). 2021;8:771645.
- Sahi FM, Masood A, Danawar NA, et al. Association between psoriasis and depression: a traditional review. Cureus. 2020;12:E9708.
- Zafiriou E, Daponte AI, Siokas V, et al. Depression and obesity in patients with psoriasis and psoriatic arthritis: is IL-17–mediated immune dysregulation the connecting link? Front Immunol. 2021;12:699848.
- Mrowietz U, Sümbül M, Gerdes S. Depression, a major comorbidity of psoriatic disease, is caused by metabolic inflammation. J Eur Acad Dermatol Venereol. 2023;37:1731-1738.
- Pavlova NT, Kioskli K, Smith C, et al. Psychosocial aspects of obesity in adults with psoriasis: a systematic review. Skin Health Dis. 2021;1:E33.
- Innamorati M, Quinto RM, Imperatori C, et al. Health-related quality of life and its association with alexithymia and difficulties in emotion regulation in patients with psoriasis. Compr Psychiatry. 2016;70:200-208.
- Tabolli S, Naldi L, Pagliarello C, et al. Evaluation of the impact of writing exercises interventions on quality of life in patients with psoriasis undergoing systemic treatments. Br J Dermatol. 2012;167:1254‐1264.
- Albuquerque D, Nóbrega C, Manco L, et al. The contribution of genetics and environment to obesity. Br Med Bull. 2017;123:159‐173.
- Balantekin KN, Grammer AC, Fitzsimmons-Craft EE, et al. Overweight and obesity are associated with increased eating disorder correlates and general psychopathology in university women with eating disorders. Eat Behav. 2021;41:101482.
- Jebeile H, Lister NB, Baur LA, et al. Eating disorder risk in adolescents with obesity. Obes Rev. 2021;22:E13173.
- Crosta ML, Caldarola G, Fraietta S, et al. Psychopathology and eating disorders in patients with psoriasis. G Ital Dermatol Venereol. 2014;149:355-361.
- Altunay I, Demirci GT, Ates B, et al. Do eating disorders accompany metabolic syndrome in psoriasis patients? results of a preliminary study. Clin Cosmet Investig Dermatol. 2011;4:139-143.
Psoriasis is a chronic multisystemic inflammatory skin disease with a worldwide prevalence of 2% to 3%.1 Psoriasis can be accompanied by other conditions such as psoriatic arthritis, obesity, metabolic syndrome, diabetes mellitus, hypertension, dyslipidemia, atherosclerotic disease, inflammatory bowel disease, and anxiety/depression. It is important to manage comorbidities of psoriasis in addition to treating the cutaneous manifestations of the disease.1
Obesity is a major public health concern worldwide. Numerous observational and epidemiologic studies have reported a high prevalence of obesity among patients with psoriasis.2 Current evidence indicates that obesity may initiate or worsen psoriasis; furthermore, it is important to note that obesity may negatively impact the effectiveness of psoriasis-specific treatments or increase the incidence of adverse effects. Therefore, managing obesity is crucial in the treatment of psoriasis.3 Numerous studies have investigated the association between psoriasis and obesity, and they commonly conclude that both conditions share the same genetic metabolic pathways.2-4 However, it is important to consider environmental factors such as dietary habits, smoking, alcohol consumption, and a sedentary lifestyle—all of which are associated with psoriasis and also can contribute to the development of obesity.5 Because of the effects of obesity in psoriasis patients, factors that impact the development of obesity have become a popular research topic.
Eating disorders (EDs) are a crucial risk factor for both developing and maintaining obesity. In particular, two EDs that are associated with obesity include binge eating disorder and bulimia nervosa.6 According to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition,7 binge eating disorder can be diagnosed when a patient has at least 1 episode of binge eating per week over a 3-month period. Bulimia nervosa can be diagnosed when a patient is excessively concerned with their body weight and shape and engages in behaviors to prevent weight gain (eg, forced vomiting, excessive use of laxatives).7 Psychiatrists who specialize in EDs make diagnoses based on these criteria. In daily practice, there are several quick and simple questionnaires available to screen for EDs that can be used by nonpsychiatrist physicians, including the commonly used 26-item Eating Attitudes Test (EAT-26).8 The EAT-26 has been used to screen for EDs in patients with inflammatory disorders.9
The aim of this study was to screen for EDs in patients with psoriasis to identify potential risk factors for development of obesity.
Materials and Methods
This study included patients with psoriasis who were screened for EDs at a tertiary dermatology clinic in Turkey between January 2021 and December 2023. This study was approved by the local ethics committee and was in accordance with the Declaration of Helsinki (decision number E-93471371-514.99-225000079).
Study Design and Patient Inclusion Criteria—This quantitative cross-sectional study utilized EAT-26, Dermatology Life Quality Index (DLQI), Attitude Scale for Healthy Nutrition (ASHN), and Depression Anxiety Stress Scale-21 (DASS-21) scores. All the questionnaire scales used in the study were adapted and validated in Turkey.8,10-12 The inclusion criteria consisted of being older than 18 years of age, being literate, having psoriasis for at least 1 year that was not treated topically or systemically, and having no psychiatric diseases outside an ED. The questionnaires were presented in written format following the clinical examination. Literacy was an inclusion criterion in this study due to the absence of auxiliary health personnel.
Study Variables—The study variables included age, sex, marital status (single/divorced or married), education status (primary/secondary school or high school/university), employment status (employed or unemployed/retired), body mass index (BMI), smoking status, alcohol-consumption status, Psoriasis Area Severity Index score, presence of nail psoriasis and psoriatic arthritis, duration of psoriasis, family history of psoriasis, EAT-26 score, ASHN score, DLQI score, and DASS-21 score. Body mass index was calculated by taking a participant’s weight in kilograms and dividing it by their height in meters squared. The BMI values were classified into 3 categories: normal (18.5–24.9 kg/m2), overweight (25.0–29.9 kg/m2), and obese (≥30 kg/m2).13
Questionnaires—The EAT-26 questionnaire includes 26 questions that are used to detect EDs. Responses to each question include Likert-type answer options (ie, “always,” “usually,” “often,” “sometimes,” “rarely,” and “never.”) Patients with scores of 20 points or higher (range, 0–78) are classified as high risk for EDs.8 In our study, EAT-26 scores were grouped into 2 categories: patients scoring less than 20 points and those scoring 20 points or higher.
The DLQI questionnaire includes 10 questions to measure dermatologic symptoms and qualiy of life. Responses to each question include Likert-type answer options (ie, “not at all,” “a little,” “a lot,” or “very much.”) On the DLQI scale, the higher the score, the lower the quality of life (score range, 0–30).10
The ASHN questionnaire includes 21 questions that measure attitudes toward healthy nutrition with 5 possible answer options (“strongly disagree,” “disagree,” “undecided,” “agree,” and “strongly agree”). On this scale, higher scores indicate the participant is more knowledgeable about healthy nutrition (score range, 0–78).11
The DASS-21 questionnaire includes 21 questions that measure the severity of a range of symptoms common to depression, anxiety, and stress. Responses include Likert-type answer options (eg, “never,” “sometimes,” “often,” and “almost always.”) On this scale, a higher score (range of 0–21 for each) indicates higher levels of depression, anxiety, and stress.12
Statistical Analysis—Descriptive statistics were analyzed using SPSS software version 22.0 (IBM). The Shapiro-Wilk test was applied to determine whether the data were normally distributed. For categorical variables, frequency differences among groups were compared using the Pearson χ2 test. A t test was used to compare the means of 2 independent groups with a normal distribution. One-way analysis of variance and Tukey Honest Significant Difference post hoc analysis were used to test whether there was a statistically significant difference among the normally distributed means of independent groups. Pearson correlation analysis was used to determine whether there was a linear relationship between 2 numeric measurements and, if so, to determine the direction and severity of this relationship. P<.05 indicated statistical significance in this study.
Results
Study Participant Demographics—This study included 82 participants with a mean age of 44.3 years; 52.4% (43/82) were female, and 85.4% (70/82) were married. The questionnaire took an average of 4.2 minutes for participants to complete. A total of 57.3% (47/82) of patients had completed primary/secondary education and 59.8% (49/82) were employed. The mean BMI was 28.1 kg/m2. According to the BMI classification, 26.8% (22/82) participants had a normal weight, 36.6% (30/82) were overweight, and 43.9% (36/82) were obese. A total of 48.8% (40/82) of participants smoked, and 4.9% (4/82) consumed alcohol. The mean Psoriasis Area and Severity Index score was 5.4. A total of 54.9% (45/82) of participants had nail psoriasis, and 24.4% (20/82) had psoriatic arthritis. The mean duration of psoriasis was 153 months. A total of 29.3% (24/82) of participants had a positive family history of psoriasis. The mean EAT-26 score was 11.1. A total of 12.2% (10/82) of participants had an EAT-26 score of 20 points or higher and were considered at high risk for an ED. The mean ASHN score was 72.9; the mean DLQI score was 5.5; and on the DASS-21 scale, mean scores for depression, anxiety, and stress were 6.3, 8.7, and 10.0, respectively (Table).
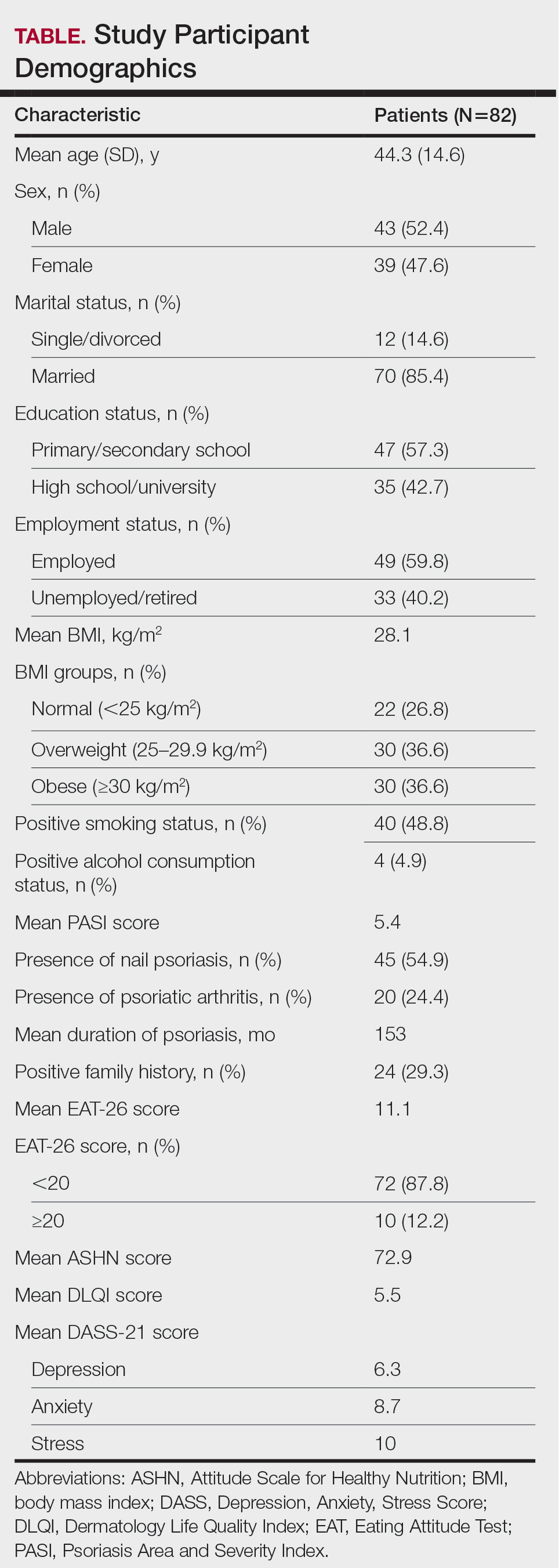
Comparative Evaluation of the BMI Groups—The only statistically significant differences among the 3 BMI groups were related to marital status, EAT-26 score, and anxiety and stress scores (P=.02, <.01, <.01, and <.01, respectively)(eTable 1). The number of single/divorced participants in the overweight group was significantly (P=.02) greater than in the normal weight group. The mean EAT-26 score for the normal weight group was significantly (P<.01) lower than for the overweight and obese groups; there was no significant difference in mean EAT-26 scores between the overweight and obese groups. The mean anxiety score was significantly (P<.01) lower in the normal weight group compared with the overweight and obese groups. There was no significant difference between the overweight and obese groups according to the mean depression score. The mean stress and anxiety scores were significantly (P<.01) lower in the normal weight group than in the overweight and obese groups. There was no significant difference between the overweight and obese groups according to the mean anxiety score.
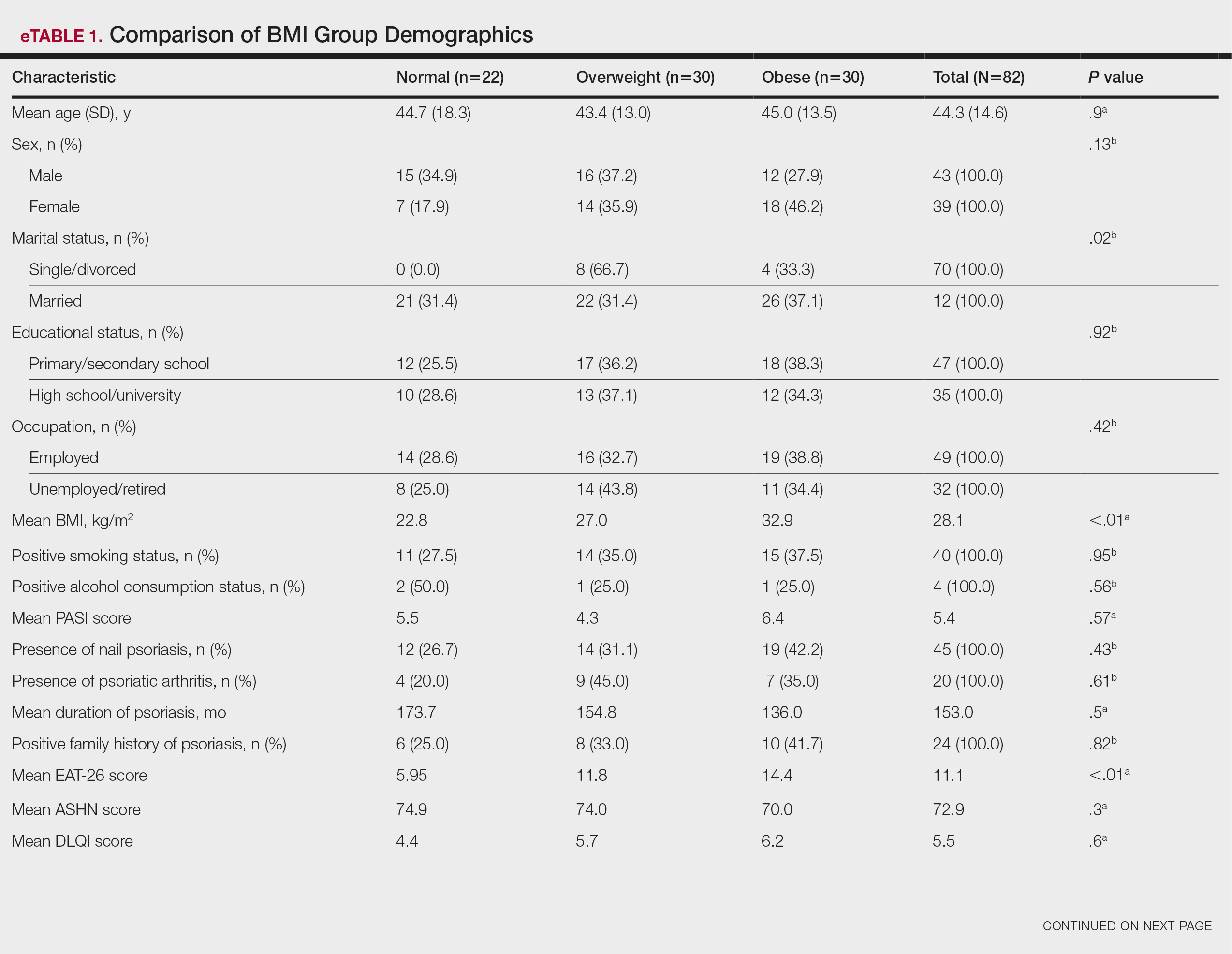
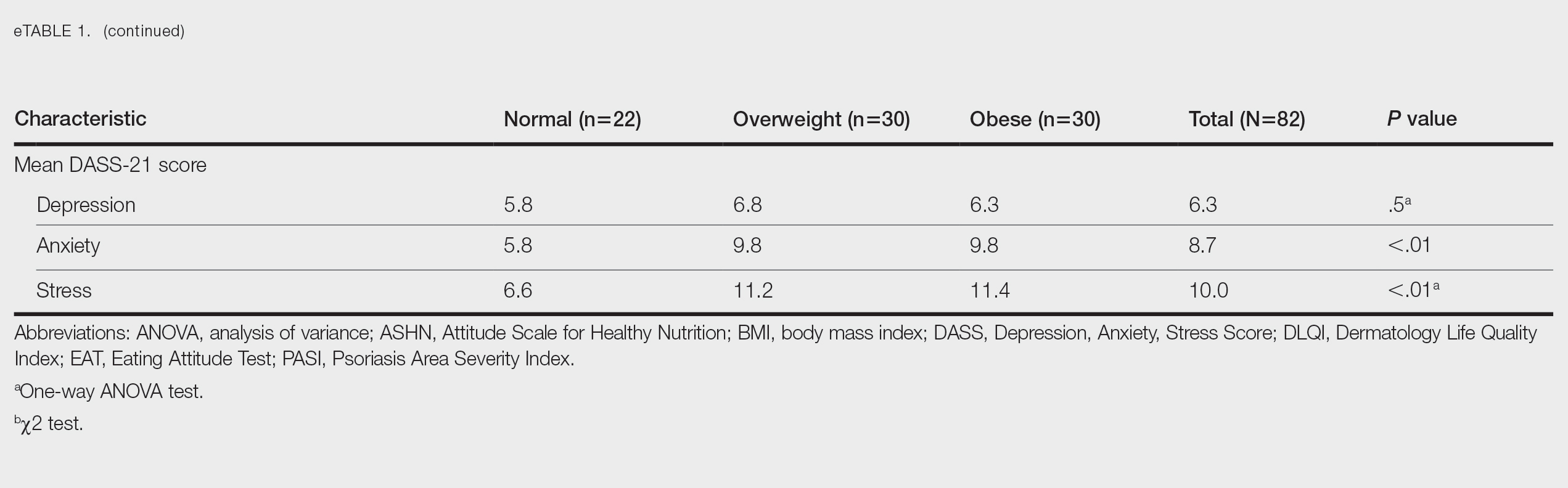
Comparative Evaluation of the EAT-26 Scores—There were statistically significant differences among the EAT-26 scores related to sex; BMI; and depression, anxiety, and stress scores (P=.04, .02, <.01, <.01, and <.01, respectively). The number of females in the group with a score of 20 points or higher was significantly (P=.04) less than that in the group scoring less than 20 points. The mean BMI in the group with a score of 20 points or higher was significantly (P=.02) greater than in group scoring less than 20 points. The mean depression, anxiety, and stress scores of the group scoring 20 points or higher were significantly (P<.01 for all) greater than in the group scoring less than 20 points (eTable 2).
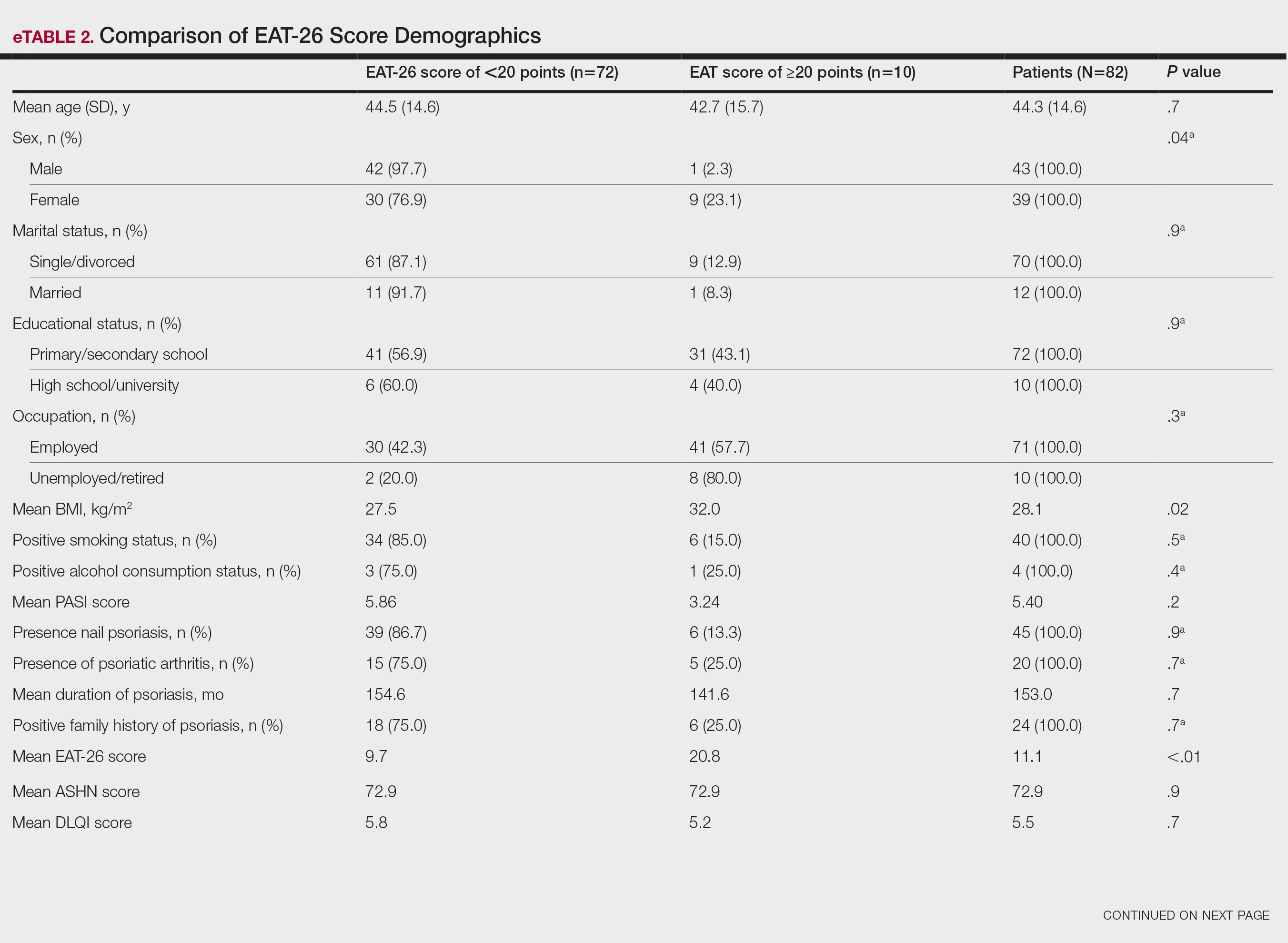
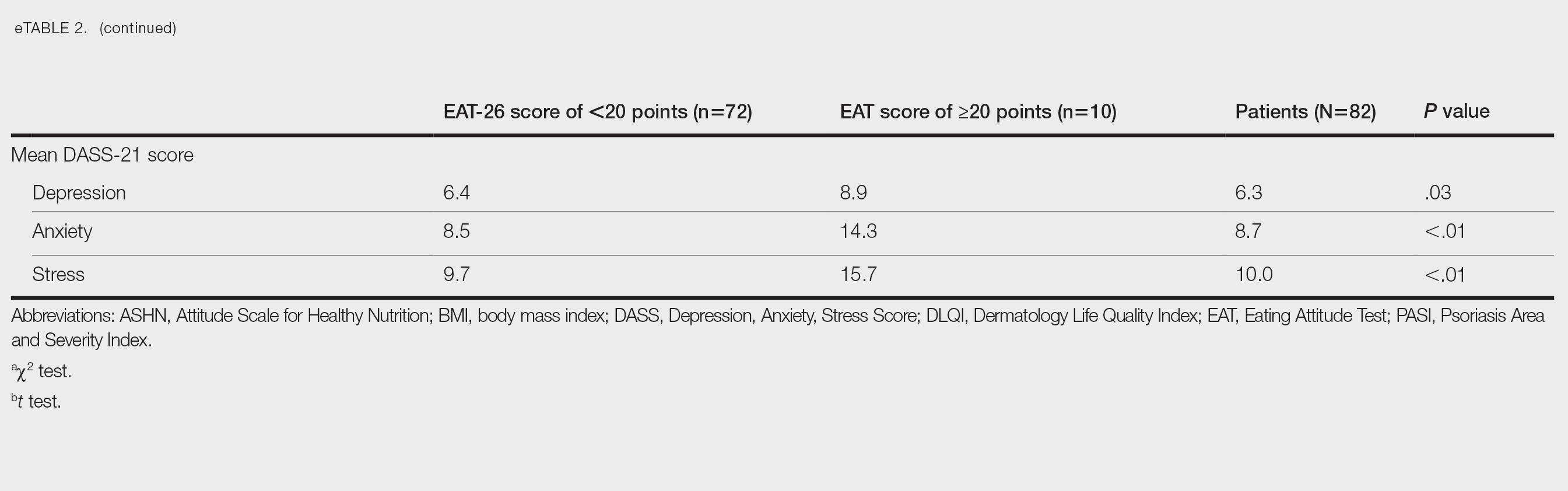
Correlation Analysis of the Study Variables—The EAT-26 scores were positively correlated with BMI, anxiety, depression, and stress (P<.01 for all)(eTable 3).
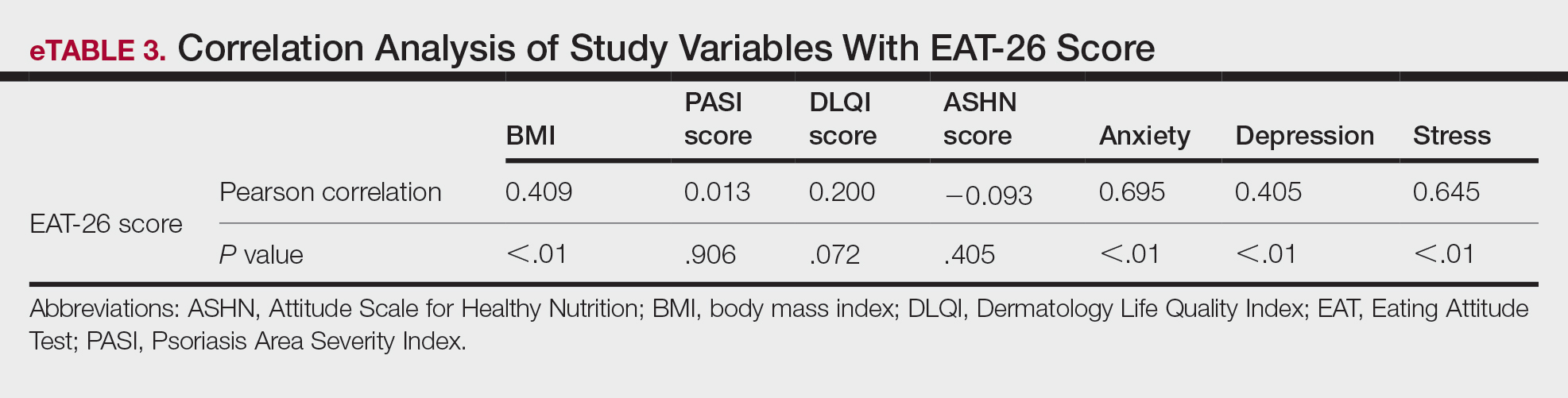
Comment
Eating disorders are psychiatric conditions that require a multidisciplinary approach. Nonpsychiatric medical departments may be involved due to the severe consequences (eg, various skin changes14) of these disorders. Psoriasis is not known to be directly affected by the presence of an ED; however, it is possible that EDs could indirectly affect patients with psoriasis by influencing obesity. Therefore, this study aimed to examine the relationship between ED risk factors and obesity in this population.
The relationship between psoriasis and obesity has been a popular research topic in dermatology since the 1990s.15 Epidemiologic and observational studies have reported that patients with psoriasis are more likely to be overweight or have obesity, which is an independent risk factor for psoriasis.3,16 However, the causal relationship between psoriasis and obesity remains unclear. In a comprehensive review, Barros et al17 emphasized the causal relationship between obesity and psoriasis under several headings. Firstly, a higher BMI increases the risk for psoriasis by promoting cytokine release and immune system dysregulation. Secondly, a Western diet (eg, processed foods and fast food) triggers obesity and psoriasis by increasing adipose tissue. Thirdly, the alteration of the skin and gut microbiota triggers chronic inflammation as a result of bacterial translocation in patients with obesity. Fourthly, a high-fat diet and palmitic acid disrupt the intestinal integrity of the gut and increase the risk for psoriasis and obesity by triggering chronic inflammation of bacterial fragments that pass into the blood. Finally, the decrease in the amount of adiponectin and the increase in the amount of leptin in patients with obesity may cause psoriasis by increasing proinflammatory cytokines, which are similar to those involved in the pathogenesis of psoriasis.17 Additionally, psoriatic inflammation can cause insulin resistance and metabolic dysfunction, leading to obesity.18 The relationship between psoriasis and obesity cannot be solely explained by metabolic pathways. Smoking, alcohol consumption, and a sedentary lifestyle all are associated with psoriasis and also can contribute to obesity.5 Our study revealed no significant difference in smoking or alcohol consumption between the normal weight and overweight/obesity groups. Based on our data, we determined that smoking and alcohol consumption did not affect obesity in our patients with psoriasis.
Observational and epidemiologic studies have shown that patients with psoriasis experience increased rates of depression, anxiety, and stress.19 In studies of pathogenesis, a connection between depression and psoriatic inflammation has been established.20 It is known that inflammatory cytokines similar to those in psoriasis are involved in the development of obesity.18 In addition, depression and anxiety can lead to binge eating, unhealthy food choices, and a more sedentary lifestyle.5 All of these variables may contribute to the associations between depression and anxiety with psoriasis and obesity. Zafiriou et al21 conducted a study to investigate the relationship between psoriasis, obesity, and depression through inflammatory pathways with a focus on the importance of IL-17. Data showing that IL-17–producing Th17-cell subgroups play a considerable role in the development of obesity and depression prompted the authors to suggest that psoriasis, obesity, and anxiety/depression may be interconnected manifestations of immune dysregulation, potentially linked to IL-17 and its associated cells.21 Mrowietz et al22 also suggested that metabolic inflammation may contribute to obesity and depression in patients with psoriasis and highlighted the importance of several cytokines, including tumor necrosis factor α, IL-6, IL-8, IL-17, and IL-23. Our study revealed no significant differences in depression scores between BMI groups. Another meta-analysis reported conflicting findings on the incidence of depression in obese patients with psoriasis.23 Some of the studies had a small number of participants. Compared to depression, anxiety has received less attention in studies of patients with obesity with psoriasis. However, these studies have shown a positive correlation between anxiety scores and BMI in patients with psoriasis.24,25 In our study, similar to the findings of previous studies, overweight patients and those with obesitywho have psoriasis had significantly (P<.01) greater anxiety and stress scores than did normal weight patients with psoriasis.
Obesity should be assessed in patients with psoriasis via a biopsychosocial approach that takes into account genetic, behavioral, and environmental factors.26 Eating disorders are considered to be one of the factors contributing to obesity. Numerous studies in the literature have demonstrated a greater incidence of EDs in patients with obesity vs those without obesity.5,6,27 Obesity and EDs have a bidirectional relationship: individuals with obesity are at risk for EDs due to body dissatisfaction, dieting habits, and depressive states. Conversely, poor eating behaviors in individuals with a normal weight can lead to obesity.28
There are few studies in the literature exploring the relationship between psoriasis and EDs. Crosta et al29 demonstrated that patients with psoriasis had impaired results on ED screening tests and that these scores deteriorated further as BMI increased. Moreover, Altunay et al30 demonstrated that patients with psoriasis and metabolic syndrome had higher scores on the ED screening test. In this study, patients with higher scores also exhibited high levels of anxiety.30 In our study, similar to the findings of previous studies, patients with psoriasis who were overweight or had obesity had significantly (P<.01) greater EAT-26 scores than those in the normal weight group. Patients with high EAT-26 scores also exhibited elevated levels of depression, anxiety, and stress. Additionally, EAT-26 scores were positively correlated with BMI, anxiety, depression, and stress scores. Our study as well as other studies in the literature indicate that additional research is needed to determine the associations between EDs and obesity in psoriasis.
Conclusion
Managing obesity is crucial for patients with psoriasis. This study showed that EAT-26 scores were higher in patients with psoriasis who were overweight or had obesity than in those who were normal weight. Participants with high EAT-26 scores (≥20 points) were more likely to be female and have higher anxiety and stress scores. In addition, EAT-26 scores were positively correlated with BMI as well as depression, anxiety, and stress scores. Eating disorders may contribute to the development of obesity in patients with psoriasis. Although our study was limited by a small sample size, the results suggest that there is a need for large-scale multicenter studies to investigate the relationship between psoriasis and EDs.
Psoriasis is a chronic multisystemic inflammatory skin disease with a worldwide prevalence of 2% to 3%.1 Psoriasis can be accompanied by other conditions such as psoriatic arthritis, obesity, metabolic syndrome, diabetes mellitus, hypertension, dyslipidemia, atherosclerotic disease, inflammatory bowel disease, and anxiety/depression. It is important to manage comorbidities of psoriasis in addition to treating the cutaneous manifestations of the disease.1
Obesity is a major public health concern worldwide. Numerous observational and epidemiologic studies have reported a high prevalence of obesity among patients with psoriasis.2 Current evidence indicates that obesity may initiate or worsen psoriasis; furthermore, it is important to note that obesity may negatively impact the effectiveness of psoriasis-specific treatments or increase the incidence of adverse effects. Therefore, managing obesity is crucial in the treatment of psoriasis.3 Numerous studies have investigated the association between psoriasis and obesity, and they commonly conclude that both conditions share the same genetic metabolic pathways.2-4 However, it is important to consider environmental factors such as dietary habits, smoking, alcohol consumption, and a sedentary lifestyle—all of which are associated with psoriasis and also can contribute to the development of obesity.5 Because of the effects of obesity in psoriasis patients, factors that impact the development of obesity have become a popular research topic.
Eating disorders (EDs) are a crucial risk factor for both developing and maintaining obesity. In particular, two EDs that are associated with obesity include binge eating disorder and bulimia nervosa.6 According to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition,7 binge eating disorder can be diagnosed when a patient has at least 1 episode of binge eating per week over a 3-month period. Bulimia nervosa can be diagnosed when a patient is excessively concerned with their body weight and shape and engages in behaviors to prevent weight gain (eg, forced vomiting, excessive use of laxatives).7 Psychiatrists who specialize in EDs make diagnoses based on these criteria. In daily practice, there are several quick and simple questionnaires available to screen for EDs that can be used by nonpsychiatrist physicians, including the commonly used 26-item Eating Attitudes Test (EAT-26).8 The EAT-26 has been used to screen for EDs in patients with inflammatory disorders.9
The aim of this study was to screen for EDs in patients with psoriasis to identify potential risk factors for development of obesity.
Materials and Methods
This study included patients with psoriasis who were screened for EDs at a tertiary dermatology clinic in Turkey between January 2021 and December 2023. This study was approved by the local ethics committee and was in accordance with the Declaration of Helsinki (decision number E-93471371-514.99-225000079).
Study Design and Patient Inclusion Criteria—This quantitative cross-sectional study utilized EAT-26, Dermatology Life Quality Index (DLQI), Attitude Scale for Healthy Nutrition (ASHN), and Depression Anxiety Stress Scale-21 (DASS-21) scores. All the questionnaire scales used in the study were adapted and validated in Turkey.8,10-12 The inclusion criteria consisted of being older than 18 years of age, being literate, having psoriasis for at least 1 year that was not treated topically or systemically, and having no psychiatric diseases outside an ED. The questionnaires were presented in written format following the clinical examination. Literacy was an inclusion criterion in this study due to the absence of auxiliary health personnel.
Study Variables—The study variables included age, sex, marital status (single/divorced or married), education status (primary/secondary school or high school/university), employment status (employed or unemployed/retired), body mass index (BMI), smoking status, alcohol-consumption status, Psoriasis Area Severity Index score, presence of nail psoriasis and psoriatic arthritis, duration of psoriasis, family history of psoriasis, EAT-26 score, ASHN score, DLQI score, and DASS-21 score. Body mass index was calculated by taking a participant’s weight in kilograms and dividing it by their height in meters squared. The BMI values were classified into 3 categories: normal (18.5–24.9 kg/m2), overweight (25.0–29.9 kg/m2), and obese (≥30 kg/m2).13
Questionnaires—The EAT-26 questionnaire includes 26 questions that are used to detect EDs. Responses to each question include Likert-type answer options (ie, “always,” “usually,” “often,” “sometimes,” “rarely,” and “never.”) Patients with scores of 20 points or higher (range, 0–78) are classified as high risk for EDs.8 In our study, EAT-26 scores were grouped into 2 categories: patients scoring less than 20 points and those scoring 20 points or higher.
The DLQI questionnaire includes 10 questions to measure dermatologic symptoms and qualiy of life. Responses to each question include Likert-type answer options (ie, “not at all,” “a little,” “a lot,” or “very much.”) On the DLQI scale, the higher the score, the lower the quality of life (score range, 0–30).10
The ASHN questionnaire includes 21 questions that measure attitudes toward healthy nutrition with 5 possible answer options (“strongly disagree,” “disagree,” “undecided,” “agree,” and “strongly agree”). On this scale, higher scores indicate the participant is more knowledgeable about healthy nutrition (score range, 0–78).11
The DASS-21 questionnaire includes 21 questions that measure the severity of a range of symptoms common to depression, anxiety, and stress. Responses include Likert-type answer options (eg, “never,” “sometimes,” “often,” and “almost always.”) On this scale, a higher score (range of 0–21 for each) indicates higher levels of depression, anxiety, and stress.12
Statistical Analysis—Descriptive statistics were analyzed using SPSS software version 22.0 (IBM). The Shapiro-Wilk test was applied to determine whether the data were normally distributed. For categorical variables, frequency differences among groups were compared using the Pearson χ2 test. A t test was used to compare the means of 2 independent groups with a normal distribution. One-way analysis of variance and Tukey Honest Significant Difference post hoc analysis were used to test whether there was a statistically significant difference among the normally distributed means of independent groups. Pearson correlation analysis was used to determine whether there was a linear relationship between 2 numeric measurements and, if so, to determine the direction and severity of this relationship. P<.05 indicated statistical significance in this study.
Results
Study Participant Demographics—This study included 82 participants with a mean age of 44.3 years; 52.4% (43/82) were female, and 85.4% (70/82) were married. The questionnaire took an average of 4.2 minutes for participants to complete. A total of 57.3% (47/82) of patients had completed primary/secondary education and 59.8% (49/82) were employed. The mean BMI was 28.1 kg/m2. According to the BMI classification, 26.8% (22/82) participants had a normal weight, 36.6% (30/82) were overweight, and 43.9% (36/82) were obese. A total of 48.8% (40/82) of participants smoked, and 4.9% (4/82) consumed alcohol. The mean Psoriasis Area and Severity Index score was 5.4. A total of 54.9% (45/82) of participants had nail psoriasis, and 24.4% (20/82) had psoriatic arthritis. The mean duration of psoriasis was 153 months. A total of 29.3% (24/82) of participants had a positive family history of psoriasis. The mean EAT-26 score was 11.1. A total of 12.2% (10/82) of participants had an EAT-26 score of 20 points or higher and were considered at high risk for an ED. The mean ASHN score was 72.9; the mean DLQI score was 5.5; and on the DASS-21 scale, mean scores for depression, anxiety, and stress were 6.3, 8.7, and 10.0, respectively (Table).
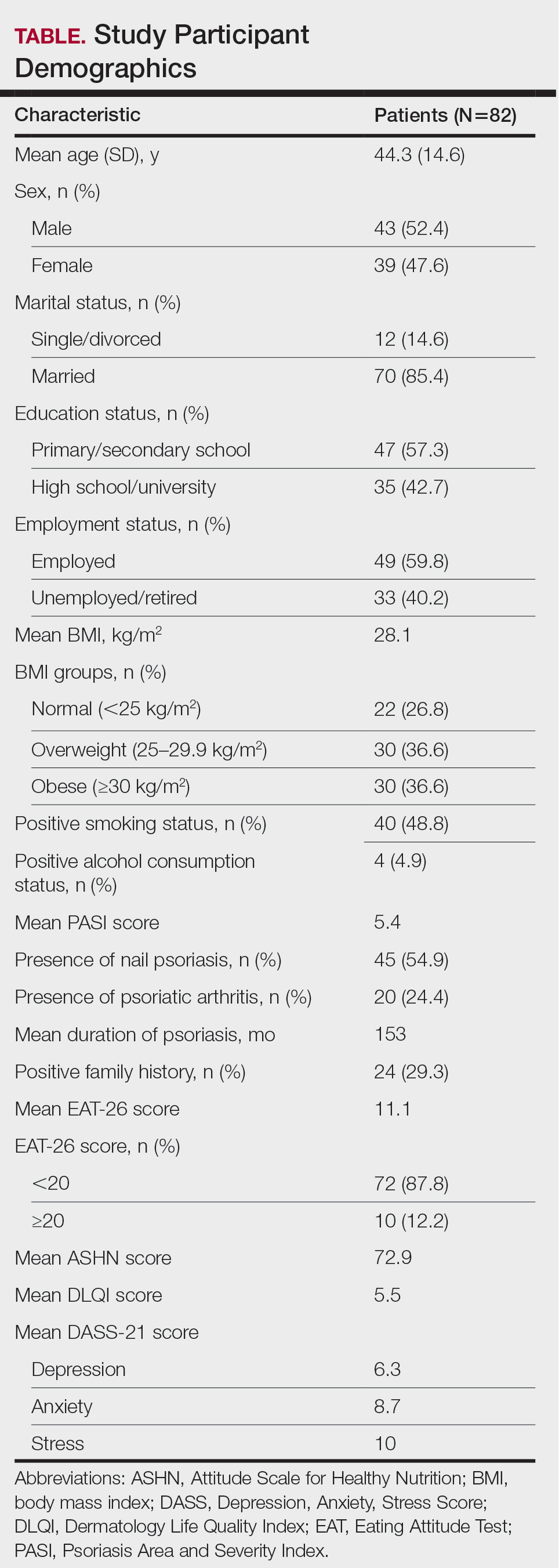
Comparative Evaluation of the BMI Groups—The only statistically significant differences among the 3 BMI groups were related to marital status, EAT-26 score, and anxiety and stress scores (P=.02, <.01, <.01, and <.01, respectively)(eTable 1). The number of single/divorced participants in the overweight group was significantly (P=.02) greater than in the normal weight group. The mean EAT-26 score for the normal weight group was significantly (P<.01) lower than for the overweight and obese groups; there was no significant difference in mean EAT-26 scores between the overweight and obese groups. The mean anxiety score was significantly (P<.01) lower in the normal weight group compared with the overweight and obese groups. There was no significant difference between the overweight and obese groups according to the mean depression score. The mean stress and anxiety scores were significantly (P<.01) lower in the normal weight group than in the overweight and obese groups. There was no significant difference between the overweight and obese groups according to the mean anxiety score.
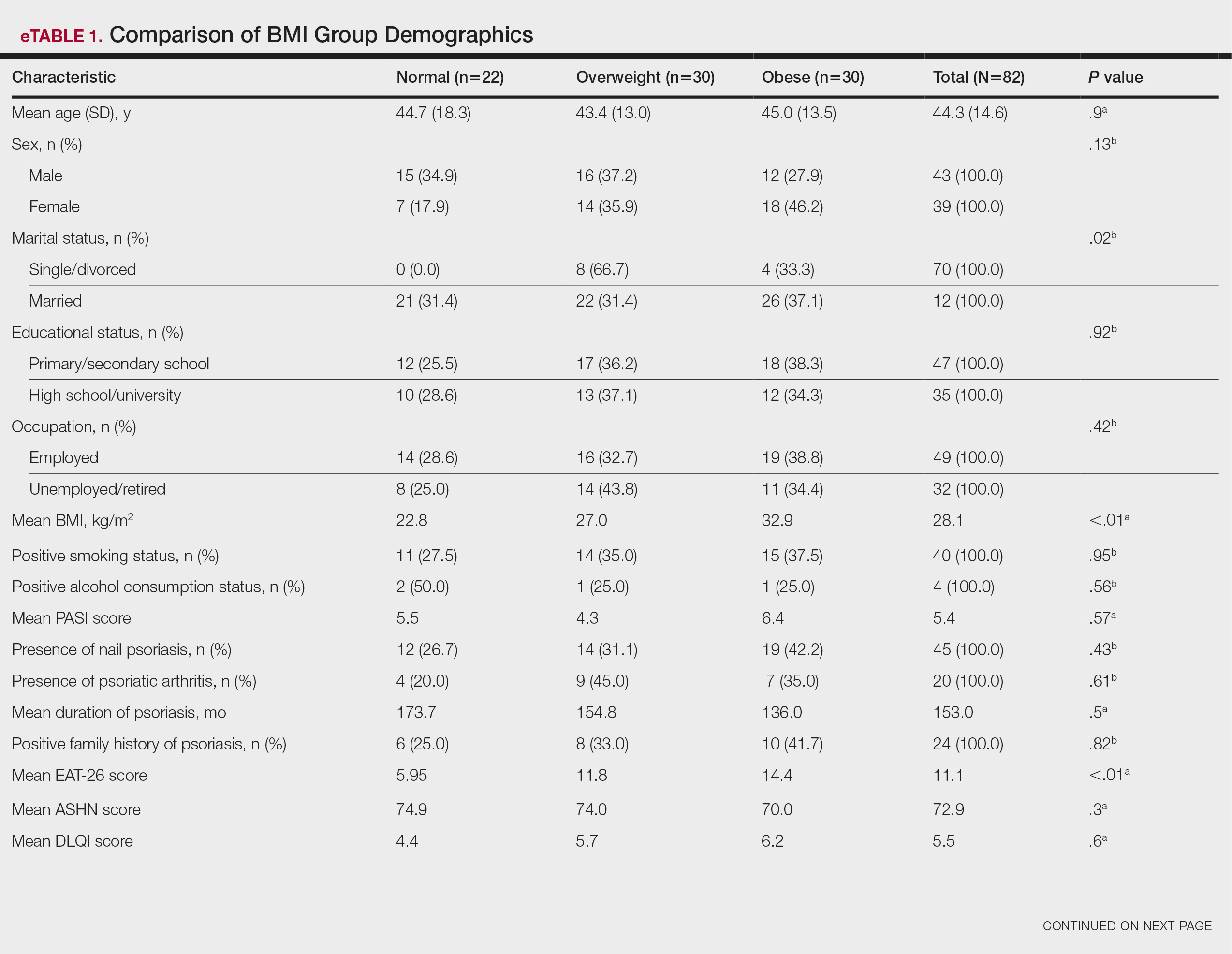
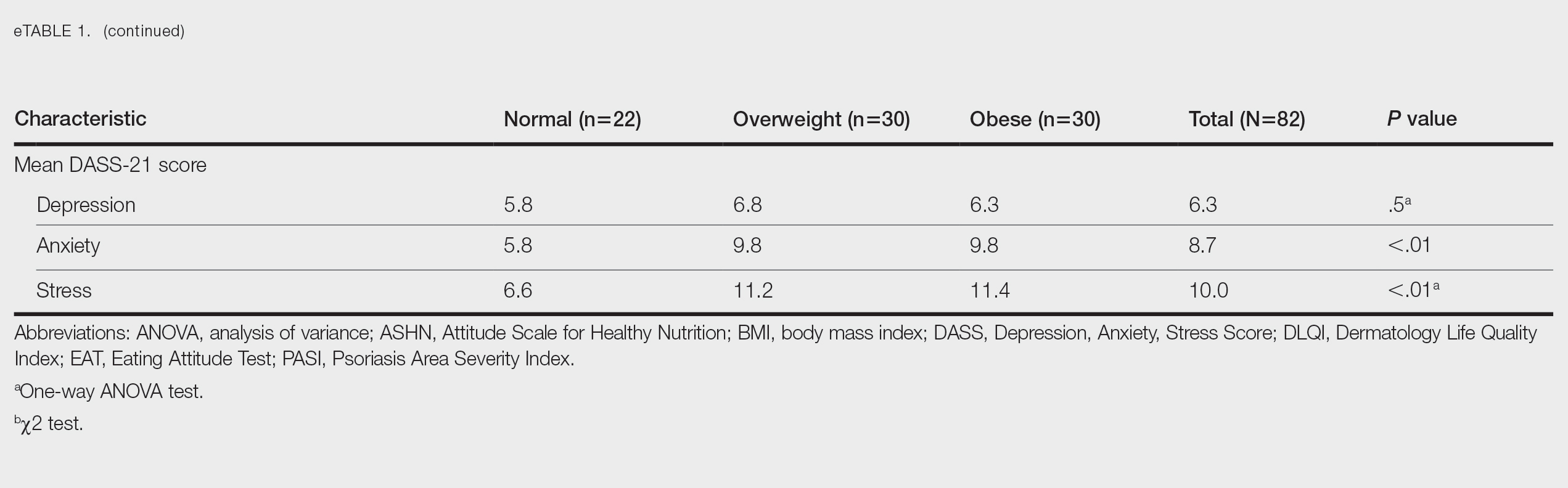
Comparative Evaluation of the EAT-26 Scores—There were statistically significant differences among the EAT-26 scores related to sex; BMI; and depression, anxiety, and stress scores (P=.04, .02, <.01, <.01, and <.01, respectively). The number of females in the group with a score of 20 points or higher was significantly (P=.04) less than that in the group scoring less than 20 points. The mean BMI in the group with a score of 20 points or higher was significantly (P=.02) greater than in group scoring less than 20 points. The mean depression, anxiety, and stress scores of the group scoring 20 points or higher were significantly (P<.01 for all) greater than in the group scoring less than 20 points (eTable 2).
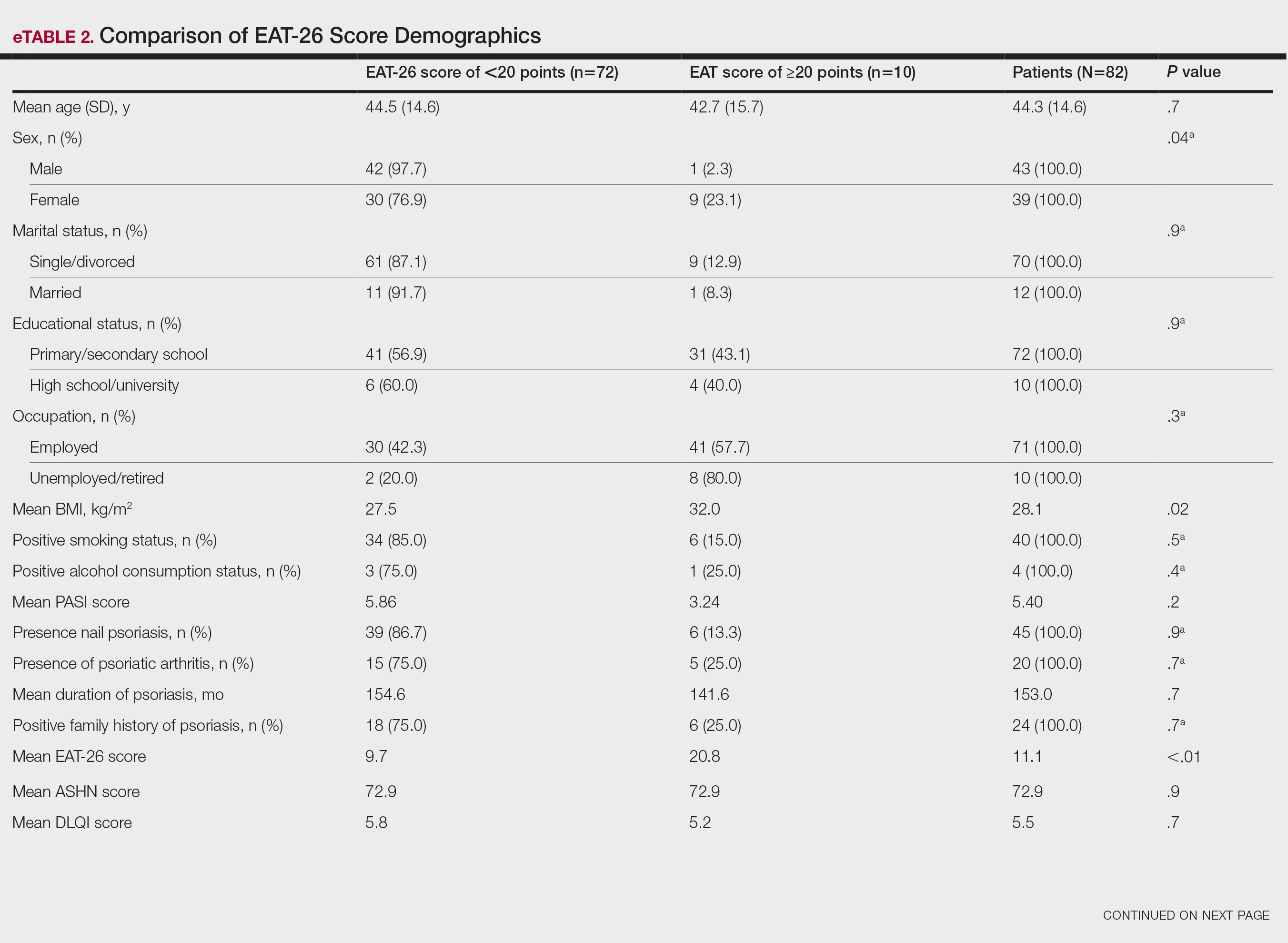
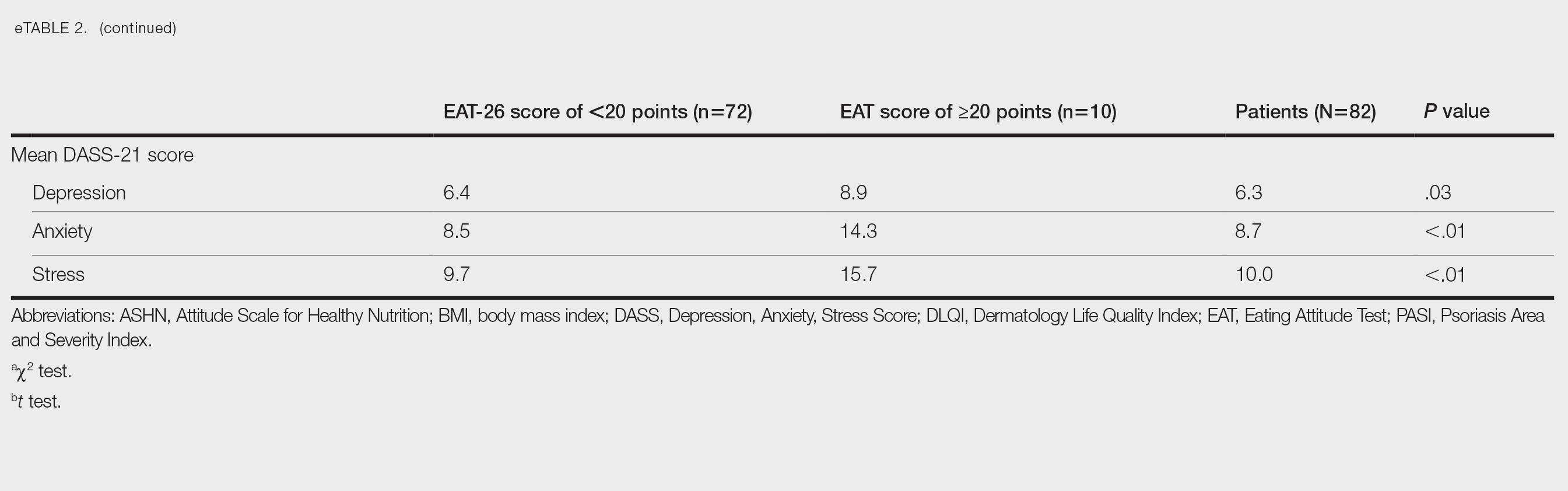
Correlation Analysis of the Study Variables—The EAT-26 scores were positively correlated with BMI, anxiety, depression, and stress (P<.01 for all)(eTable 3).
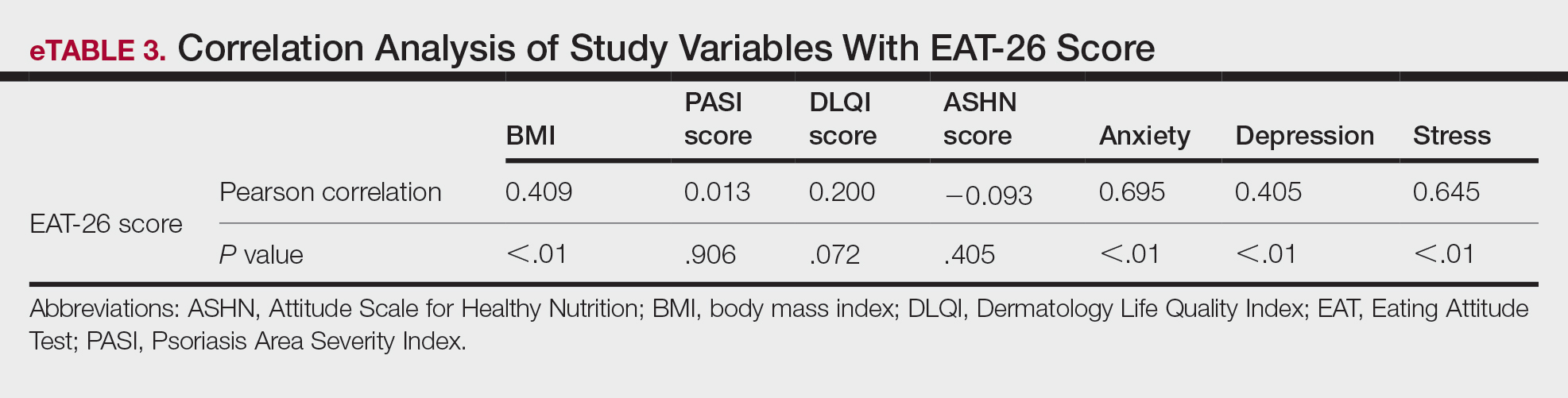
Comment
Eating disorders are psychiatric conditions that require a multidisciplinary approach. Nonpsychiatric medical departments may be involved due to the severe consequences (eg, various skin changes14) of these disorders. Psoriasis is not known to be directly affected by the presence of an ED; however, it is possible that EDs could indirectly affect patients with psoriasis by influencing obesity. Therefore, this study aimed to examine the relationship between ED risk factors and obesity in this population.
The relationship between psoriasis and obesity has been a popular research topic in dermatology since the 1990s.15 Epidemiologic and observational studies have reported that patients with psoriasis are more likely to be overweight or have obesity, which is an independent risk factor for psoriasis.3,16 However, the causal relationship between psoriasis and obesity remains unclear. In a comprehensive review, Barros et al17 emphasized the causal relationship between obesity and psoriasis under several headings. Firstly, a higher BMI increases the risk for psoriasis by promoting cytokine release and immune system dysregulation. Secondly, a Western diet (eg, processed foods and fast food) triggers obesity and psoriasis by increasing adipose tissue. Thirdly, the alteration of the skin and gut microbiota triggers chronic inflammation as a result of bacterial translocation in patients with obesity. Fourthly, a high-fat diet and palmitic acid disrupt the intestinal integrity of the gut and increase the risk for psoriasis and obesity by triggering chronic inflammation of bacterial fragments that pass into the blood. Finally, the decrease in the amount of adiponectin and the increase in the amount of leptin in patients with obesity may cause psoriasis by increasing proinflammatory cytokines, which are similar to those involved in the pathogenesis of psoriasis.17 Additionally, psoriatic inflammation can cause insulin resistance and metabolic dysfunction, leading to obesity.18 The relationship between psoriasis and obesity cannot be solely explained by metabolic pathways. Smoking, alcohol consumption, and a sedentary lifestyle all are associated with psoriasis and also can contribute to obesity.5 Our study revealed no significant difference in smoking or alcohol consumption between the normal weight and overweight/obesity groups. Based on our data, we determined that smoking and alcohol consumption did not affect obesity in our patients with psoriasis.
Observational and epidemiologic studies have shown that patients with psoriasis experience increased rates of depression, anxiety, and stress.19 In studies of pathogenesis, a connection between depression and psoriatic inflammation has been established.20 It is known that inflammatory cytokines similar to those in psoriasis are involved in the development of obesity.18 In addition, depression and anxiety can lead to binge eating, unhealthy food choices, and a more sedentary lifestyle.5 All of these variables may contribute to the associations between depression and anxiety with psoriasis and obesity. Zafiriou et al21 conducted a study to investigate the relationship between psoriasis, obesity, and depression through inflammatory pathways with a focus on the importance of IL-17. Data showing that IL-17–producing Th17-cell subgroups play a considerable role in the development of obesity and depression prompted the authors to suggest that psoriasis, obesity, and anxiety/depression may be interconnected manifestations of immune dysregulation, potentially linked to IL-17 and its associated cells.21 Mrowietz et al22 also suggested that metabolic inflammation may contribute to obesity and depression in patients with psoriasis and highlighted the importance of several cytokines, including tumor necrosis factor α, IL-6, IL-8, IL-17, and IL-23. Our study revealed no significant differences in depression scores between BMI groups. Another meta-analysis reported conflicting findings on the incidence of depression in obese patients with psoriasis.23 Some of the studies had a small number of participants. Compared to depression, anxiety has received less attention in studies of patients with obesity with psoriasis. However, these studies have shown a positive correlation between anxiety scores and BMI in patients with psoriasis.24,25 In our study, similar to the findings of previous studies, overweight patients and those with obesitywho have psoriasis had significantly (P<.01) greater anxiety and stress scores than did normal weight patients with psoriasis.
Obesity should be assessed in patients with psoriasis via a biopsychosocial approach that takes into account genetic, behavioral, and environmental factors.26 Eating disorders are considered to be one of the factors contributing to obesity. Numerous studies in the literature have demonstrated a greater incidence of EDs in patients with obesity vs those without obesity.5,6,27 Obesity and EDs have a bidirectional relationship: individuals with obesity are at risk for EDs due to body dissatisfaction, dieting habits, and depressive states. Conversely, poor eating behaviors in individuals with a normal weight can lead to obesity.28
There are few studies in the literature exploring the relationship between psoriasis and EDs. Crosta et al29 demonstrated that patients with psoriasis had impaired results on ED screening tests and that these scores deteriorated further as BMI increased. Moreover, Altunay et al30 demonstrated that patients with psoriasis and metabolic syndrome had higher scores on the ED screening test. In this study, patients with higher scores also exhibited high levels of anxiety.30 In our study, similar to the findings of previous studies, patients with psoriasis who were overweight or had obesity had significantly (P<.01) greater EAT-26 scores than those in the normal weight group. Patients with high EAT-26 scores also exhibited elevated levels of depression, anxiety, and stress. Additionally, EAT-26 scores were positively correlated with BMI, anxiety, depression, and stress scores. Our study as well as other studies in the literature indicate that additional research is needed to determine the associations between EDs and obesity in psoriasis.
Conclusion
Managing obesity is crucial for patients with psoriasis. This study showed that EAT-26 scores were higher in patients with psoriasis who were overweight or had obesity than in those who were normal weight. Participants with high EAT-26 scores (≥20 points) were more likely to be female and have higher anxiety and stress scores. In addition, EAT-26 scores were positively correlated with BMI as well as depression, anxiety, and stress scores. Eating disorders may contribute to the development of obesity in patients with psoriasis. Although our study was limited by a small sample size, the results suggest that there is a need for large-scale multicenter studies to investigate the relationship between psoriasis and EDs.
- Kalkan G. Comorbidities in psoriasis: the recognition of psoriasis as a systemic disease and current management. Turkderm-Turk Arch Dermatol Venereol. 2017;51:71-77.
- Armstrong AW, Harskamp CT, Armstrong EJ. The association between psoriasis and obesity: a systematic review and meta-analysis of observational studies. Nutr Diabetes. 2012;2:E54.
- Jensen P, Skov L. Psoriasis and obesity. Dermatology. 2016;232:633-639.
- Mirghani H, Altemani AT, Altemani ST, et al. The cross talk between psoriasis, obesity, and dyslipidemia: a meta-analysis. Cureus. 2023;15:e49253.
- Roehring M, Mashep MR, White MA, et al. The metabolic syndrome and behavioral correlates in obese patients with binge disorders. Obesity. 2009;17:481-486.
- da Luz FQ, Hay P, Touyz S, et al. Obesity with comorbid eating disorders: associated health risks and treatment approaches. Nutrients. 2018;10:829.
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition. American Psychiatric Association; 2013.
- Ergüney Okumus¸ FE, Sertel Berk HÖ. The psychometric properties of the Eating Attitudes Test short form (EAT-26) in a college sample. Stud Psychol. 2020;40:57-78.
- Stoleru G, Leopold A, Auerbach A, et al. Female gender, dissatisfaction with weight, and number of IBD related surgeries as independent risk factors for eating disorders among patients with inflammatory bowel diseases. BMC Gastroenterol. 2022;22:438.
- Öztürkcan S, Ermertcan AT, Eser E, et al. Cross validation of the Turkish version of dermatology life quality index. Int J Dermatol. 2006;45:1300-1307.
- Demir GT, Ciciog˘lu HI˙. Attitude scale for healthy nutrition (ASHN): validity and reliability study. Gaziantep Univ J Sport Sci. 2019;4:256-274.
- Yılmaz O, Boz H, Arslan A. The validity and reliability of depression stress and anxiety scale (DASS 21) Turkish short form. Res Financial Econ Soc Stud. 2017;2:78-91.
- Nuttall FQ. Body mass index: obesity, BMI, and health: a critical review. Nutr Today. 2015;50:117-128.
- Strumia R, Manzata E, Gualandi M. Is there a role for dermatologists in eating disorders? Expert Rev Dermatol. 2017; 2:109-112.
- Henseler T, Christophers E. Disease concomitance in psoriasis. J Am Acad Dermatol. 1995;32:982-986.
- Naldi L, Addis A, Chimenti S, et al. Impact of body mass index and obesity on clinical response to systemic treatment for psoriasis. evidence from the Psocare project. Dermatology. 2008;217:365-373.
- Barros G, Duran P, Vera I, et al. Exploring the links between obesity and psoriasis: a comprehensive review. Int J Mol Sci. 2022;23:7499.
- Hao Y, Zhu YJ, Zou S, et al. Metabolic syndrome and psoriasis: mechanisms and future directions. Front Immunol. 2021;12:711060.
- Jing D, Xiao H, Shen M, et al. Association of psoriasis with anxiety and depression: a case–control study in Chinese patients. Front Med (Lausanne). 2021;8:771645.
- Sahi FM, Masood A, Danawar NA, et al. Association between psoriasis and depression: a traditional review. Cureus. 2020;12:E9708.
- Zafiriou E, Daponte AI, Siokas V, et al. Depression and obesity in patients with psoriasis and psoriatic arthritis: is IL-17–mediated immune dysregulation the connecting link? Front Immunol. 2021;12:699848.
- Mrowietz U, Sümbül M, Gerdes S. Depression, a major comorbidity of psoriatic disease, is caused by metabolic inflammation. J Eur Acad Dermatol Venereol. 2023;37:1731-1738.
- Pavlova NT, Kioskli K, Smith C, et al. Psychosocial aspects of obesity in adults with psoriasis: a systematic review. Skin Health Dis. 2021;1:E33.
- Innamorati M, Quinto RM, Imperatori C, et al. Health-related quality of life and its association with alexithymia and difficulties in emotion regulation in patients with psoriasis. Compr Psychiatry. 2016;70:200-208.
- Tabolli S, Naldi L, Pagliarello C, et al. Evaluation of the impact of writing exercises interventions on quality of life in patients with psoriasis undergoing systemic treatments. Br J Dermatol. 2012;167:1254‐1264.
- Albuquerque D, Nóbrega C, Manco L, et al. The contribution of genetics and environment to obesity. Br Med Bull. 2017;123:159‐173.
- Balantekin KN, Grammer AC, Fitzsimmons-Craft EE, et al. Overweight and obesity are associated with increased eating disorder correlates and general psychopathology in university women with eating disorders. Eat Behav. 2021;41:101482.
- Jebeile H, Lister NB, Baur LA, et al. Eating disorder risk in adolescents with obesity. Obes Rev. 2021;22:E13173.
- Crosta ML, Caldarola G, Fraietta S, et al. Psychopathology and eating disorders in patients with psoriasis. G Ital Dermatol Venereol. 2014;149:355-361.
- Altunay I, Demirci GT, Ates B, et al. Do eating disorders accompany metabolic syndrome in psoriasis patients? results of a preliminary study. Clin Cosmet Investig Dermatol. 2011;4:139-143.
- Kalkan G. Comorbidities in psoriasis: the recognition of psoriasis as a systemic disease and current management. Turkderm-Turk Arch Dermatol Venereol. 2017;51:71-77.
- Armstrong AW, Harskamp CT, Armstrong EJ. The association between psoriasis and obesity: a systematic review and meta-analysis of observational studies. Nutr Diabetes. 2012;2:E54.
- Jensen P, Skov L. Psoriasis and obesity. Dermatology. 2016;232:633-639.
- Mirghani H, Altemani AT, Altemani ST, et al. The cross talk between psoriasis, obesity, and dyslipidemia: a meta-analysis. Cureus. 2023;15:e49253.
- Roehring M, Mashep MR, White MA, et al. The metabolic syndrome and behavioral correlates in obese patients with binge disorders. Obesity. 2009;17:481-486.
- da Luz FQ, Hay P, Touyz S, et al. Obesity with comorbid eating disorders: associated health risks and treatment approaches. Nutrients. 2018;10:829.
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition. American Psychiatric Association; 2013.
- Ergüney Okumus¸ FE, Sertel Berk HÖ. The psychometric properties of the Eating Attitudes Test short form (EAT-26) in a college sample. Stud Psychol. 2020;40:57-78.
- Stoleru G, Leopold A, Auerbach A, et al. Female gender, dissatisfaction with weight, and number of IBD related surgeries as independent risk factors for eating disorders among patients with inflammatory bowel diseases. BMC Gastroenterol. 2022;22:438.
- Öztürkcan S, Ermertcan AT, Eser E, et al. Cross validation of the Turkish version of dermatology life quality index. Int J Dermatol. 2006;45:1300-1307.
- Demir GT, Ciciog˘lu HI˙. Attitude scale for healthy nutrition (ASHN): validity and reliability study. Gaziantep Univ J Sport Sci. 2019;4:256-274.
- Yılmaz O, Boz H, Arslan A. The validity and reliability of depression stress and anxiety scale (DASS 21) Turkish short form. Res Financial Econ Soc Stud. 2017;2:78-91.
- Nuttall FQ. Body mass index: obesity, BMI, and health: a critical review. Nutr Today. 2015;50:117-128.
- Strumia R, Manzata E, Gualandi M. Is there a role for dermatologists in eating disorders? Expert Rev Dermatol. 2017; 2:109-112.
- Henseler T, Christophers E. Disease concomitance in psoriasis. J Am Acad Dermatol. 1995;32:982-986.
- Naldi L, Addis A, Chimenti S, et al. Impact of body mass index and obesity on clinical response to systemic treatment for psoriasis. evidence from the Psocare project. Dermatology. 2008;217:365-373.
- Barros G, Duran P, Vera I, et al. Exploring the links between obesity and psoriasis: a comprehensive review. Int J Mol Sci. 2022;23:7499.
- Hao Y, Zhu YJ, Zou S, et al. Metabolic syndrome and psoriasis: mechanisms and future directions. Front Immunol. 2021;12:711060.
- Jing D, Xiao H, Shen M, et al. Association of psoriasis with anxiety and depression: a case–control study in Chinese patients. Front Med (Lausanne). 2021;8:771645.
- Sahi FM, Masood A, Danawar NA, et al. Association between psoriasis and depression: a traditional review. Cureus. 2020;12:E9708.
- Zafiriou E, Daponte AI, Siokas V, et al. Depression and obesity in patients with psoriasis and psoriatic arthritis: is IL-17–mediated immune dysregulation the connecting link? Front Immunol. 2021;12:699848.
- Mrowietz U, Sümbül M, Gerdes S. Depression, a major comorbidity of psoriatic disease, is caused by metabolic inflammation. J Eur Acad Dermatol Venereol. 2023;37:1731-1738.
- Pavlova NT, Kioskli K, Smith C, et al. Psychosocial aspects of obesity in adults with psoriasis: a systematic review. Skin Health Dis. 2021;1:E33.
- Innamorati M, Quinto RM, Imperatori C, et al. Health-related quality of life and its association with alexithymia and difficulties in emotion regulation in patients with psoriasis. Compr Psychiatry. 2016;70:200-208.
- Tabolli S, Naldi L, Pagliarello C, et al. Evaluation of the impact of writing exercises interventions on quality of life in patients with psoriasis undergoing systemic treatments. Br J Dermatol. 2012;167:1254‐1264.
- Albuquerque D, Nóbrega C, Manco L, et al. The contribution of genetics and environment to obesity. Br Med Bull. 2017;123:159‐173.
- Balantekin KN, Grammer AC, Fitzsimmons-Craft EE, et al. Overweight and obesity are associated with increased eating disorder correlates and general psychopathology in university women with eating disorders. Eat Behav. 2021;41:101482.
- Jebeile H, Lister NB, Baur LA, et al. Eating disorder risk in adolescents with obesity. Obes Rev. 2021;22:E13173.
- Crosta ML, Caldarola G, Fraietta S, et al. Psychopathology and eating disorders in patients with psoriasis. G Ital Dermatol Venereol. 2014;149:355-361.
- Altunay I, Demirci GT, Ates B, et al. Do eating disorders accompany metabolic syndrome in psoriasis patients? results of a preliminary study. Clin Cosmet Investig Dermatol. 2011;4:139-143.
Practice Points
- Eating disorders are considered a contributing factor in obesity.
- Obesity is prevalent in patients with psoriasis, and current evidence indicates that obesity may initiate psoriasis or worsen existing disease.
- Obesity should be considered as contributory to the development of psoriasis via a biopsychosocial approach that accounts for genetic, behavioral, and environmental factors.
Projected 2023 Cost Reduction From Tumor Necrosis Factor α Inhibitor Biosimilars in Dermatology: A National Medicare Analysis
To the Editor:
Although biologics provide major therapeutic benefits for dermatologic conditions, they also come with a substantial cost, making them among the most expensive medications available. Medicare and Medicaid spending on biologics for dermatologic conditions increased by 320% from 2012 to 2018, reaching a staggering $10.6 billion in 2018 alone.1 Biosimilars show promise in reducing health care spending for dermatologic conditions; however, their utilization has been limited due to multiple factors, including delayed market entry from patent thickets, exclusionary formulary contracts, and prescriber skepticism regarding their safety and efficacy.2 For instance, a national survey of 1201 US physicians in specialties that are high prescribers of biologics reported that 55% doubted the safety and appropriateness of biosimilars.3
US Food and Drug Administration approval of biosimilars for adalimumab and etanercept offers the potential to reduce health care spending for dermatologic conditions. However, this cost reduction is dependent on utilization rates among dermatologists. In this national cross-sectional review of Medicare data, we predicted the impact of these biosimilars on dermatologic Medicare costs and demonstrated how differing utilization rates among dermatologists can influence potential savings.
To model 2023 utilization and cost reduction from biosimilars, we analyzed Medicare Part D data from 2020 on existing biosimilars, including granulocyte colony–stimulating factors, erythropoiesis-stimulating agents, and tumor necrosis factor α inhibitors.4 Methods in line with a 2021 report from the US Department of Health and Human Services5 as well as those of Yazdany et al6 were used. For each class, we calculated the 2020 distribution of biosimilar and originator drug claims as well as biosimilar cost reduction per 30-day claim. We utilized 2018-2021 annual growth rates for branded adalimumab and etanercept to estimate 30-day claims for 2023 and the cost of these branded agents in the absence of biosimilars. The hypothetical 2023 cost reduction from adalimumab and etanercept biosimilars was estimated by assuming 2020 biosimilar utilization rates and mean cost reduction per claim. This study utilized publicly available or aggregate summary data (not attributable to specific patients) and did not qualify as human subject research; therefore, institutional review board approval was not required.
In 2020, biosimilar utilization proportions ranged from 6.4% (tumor necrosis factor α inhibitors) to 82.7% (granulocyte colony–stimulating factors), with a mean across all classes of 35.7%. On average, the cost per 30-day claim of biosimilars was 66.8% of originator agents (Table 1). In 2021, we identified 57,868 30-day claims for branded adalimumab and etanercept submitted by dermatologists. From 2018 to 2021, 30-day branded adalimumab claims increased by 1.27% annually (cost + 10.62% annually), while claims for branded etanercept decreased by 13.0% annually (cost + 5.68% annually). Assuming these trends, the cost of branded adalimumab and etanercept was estimated to be $539 million in 2023. Applying the aforementioned 35.7% utilization, the introduction of biosimilars in dermatology would yield a cost reduction of approximately $118 million (21.9%). A high utilization rate (82.7%) of biosimilars among dermatologists would increase cost savings to $199 million (36.9%)(Table 2).

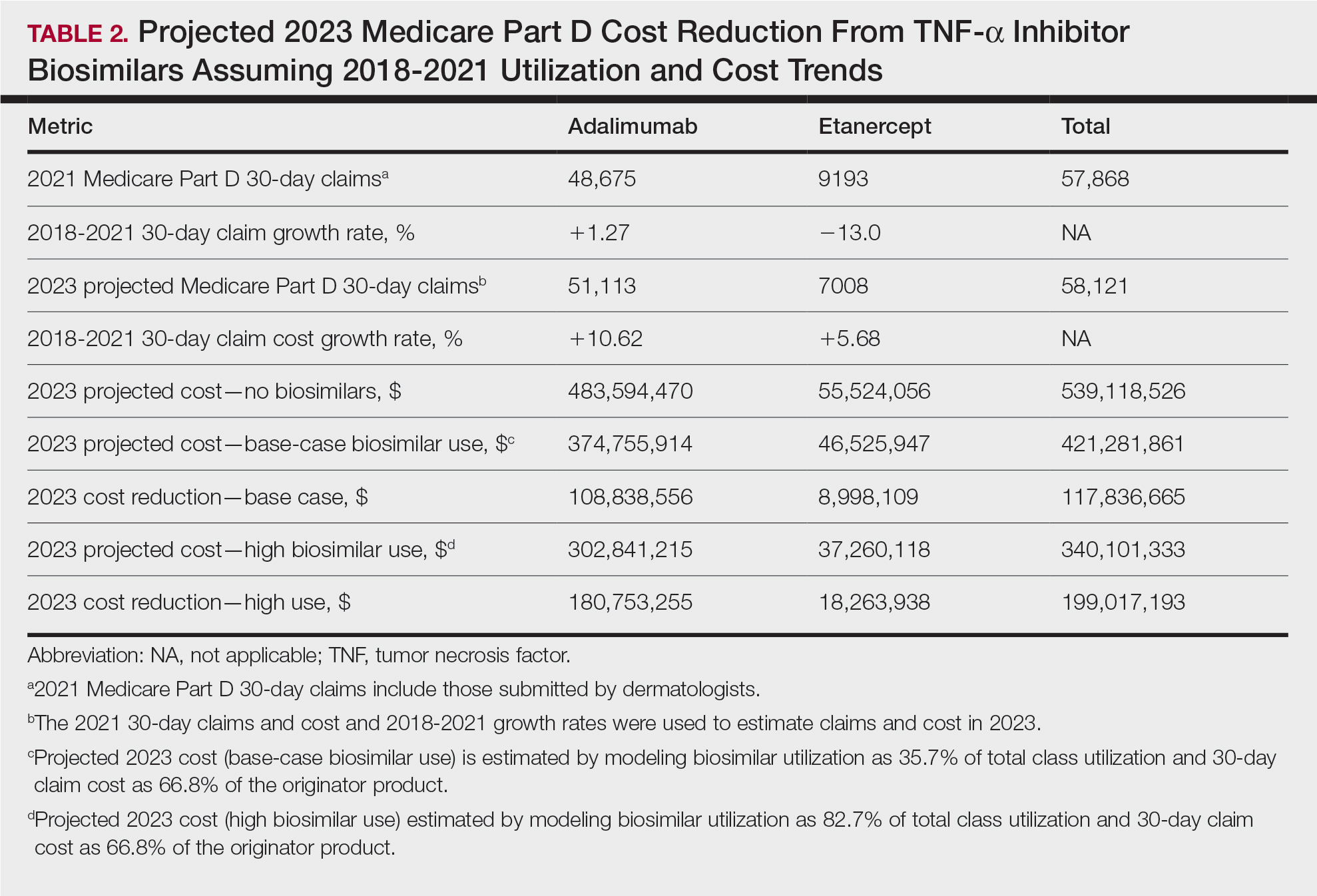
Our study demonstrates that the introduction of 2 biosimilars into dermatology may result in a notable reduction in Medicare expenditures. The savings observed are likely to translate to substantial cost savings for patients. A cross-sectional analysis of 2020 Medicare data indicated that coverage for psoriasis medications was 10.0% to 99.8% across different products and Medicare Part D plans. Consequently, patients faced considerable out-of-pocket expenses, amounting to $5653 and $5714 per year for adalimumab and etanercept, respectively.7
We found that the extent of savings from biosimilars was dependent on the utilization rates among dermatologists, with the highest utilization rate almost doubling the total savings of average utilization rates. Given the impact of high utilization and the wide variation observed, understanding the factors that have influenced uptake of biosimilars is important to increasing utilization as these medications become integrated into dermatology. For instance, limited uptake of infliximab initially may have been influenced by concerns about efficacy and increased adverse events.8,9 In contrast, the high utilization of filgrastim biosimilars (82.7%) may be attributed to its longevity in the market and familiarity to prescribers, as filgrastim was the first biosimilar to be approved in the United States.10
Promoting reasonable utilization of biosimilars may require prescriber education on their safety and approval processes, which could foster increased utilization and reduce skepticism.4 Under the Biologics Price Competition and Innovation Act, the US Food and Drug Administration approves biosimilars only when they exhibit “high similarity” and show no “clinically meaningful differences” compared to the reference biologic, with no added safety risks or reduced efficacy.11 Moreover, a 2023 systematic review of 17 studies found no major difference in efficacy and safety between biosimilars and originators of etanercept, infliximab, and other biologics.12 Understanding these findings may reassure dermatologists and patients about the reliability and safety of biosimilars.
A limitation of our study is that it solely assesses Medicare data and estimates derived from existing (separate) biologic classes. It also does not account for potential expenditure shifts to newer biologic agents (eg, IL-12/17/23 inhibitors) or changes in manufacturer behavior or promotions. Nevertheless, it indicates notable financial savings from new biosimilar agents in dermatology; along with their compelling efficacy and safety profiles, this could represent a substantial benefit to patients and the health care system.
- Price KN, Atluri S, Hsiao JL, et al. Medicare and medicaid spending trends for immunomodulators prescribed for dermatologic conditions. J Dermatolog Treat. 2020;33:575-579.
- Zhai MZ, Sarpatwari A, Kesselheim AS. Why are biosimilars not living up to their promise in the US? AMA J Ethics. 2019;21:E668-E678. doi:10.1001/amajethics.2019.668
- Cohen H, Beydoun D, Chien D, et al. Awareness, knowledge, and perceptions of biosimilars among specialty physicians. Adv Ther. 2017;33:2160-2172.
- Centers for Medicare & Medicaid Services. Medicare Part D prescribers— by provider and drug. Accessed September 11, 2024. https://data.cms.gov/provider-summary-by-type-of-service/medicare-part-d-prescribers/medicare-part-d-prescribers-by-provider-and-drug/data
- US Department of Health and Human Services. Office of Inspector General. Medicare Part D and beneficiaries could realize significant spending reductions with increased biosimilar use. Accessed September 11, 2024. https://oig.hhs.gov/oei/reports/OEI-05-20-00480.pdf
- Yazdany J, Dudley RA, Lin GA, et al. Out-of-pocket costs for infliximab and its biosimilar for rheumatoid arthritis under Medicare Part D. JAMA. 2018;320:931-933. doi:10.1001/jama.2018.7316
- Pourali SP, Nshuti L, Dusetzina SB. Out-of-pocket costs of specialty medications for psoriasis and psoriatic arthritis treatment in the medicare population. JAMA Dermatol. 2021;157:1239-1241. doi:10.1001/ jamadermatol.2021.3616
- Lebwohl M. Biosimilars in dermatology. JAMA Dermatol. 2021; 157:641-642. doi:10.1001/jamadermatol.2021.0219
- Westerkam LL, Tackett KJ, Sayed CJ. Comparing the effectiveness and safety associated with infliximab vs infliximab-abda therapy for patients with hidradenitis suppurativa. JAMA Dermatol. 2021;157:708-711. doi:10.1001/jamadermatol.2021.0220
- Awad M, Singh P, Hilas O. Zarxio (Filgrastim-sndz): the first biosimilar approved by the FDA. P T. 2017;42:19-23.
- Development of therapeutic protein biosimilars: comparative analytical assessment and other quality-related considerations guidance for industry. US Department of Health and Human Services website. Updated June 15, 2022. Accessed October 21, 2024. https://www.fda.gov/regulatory-information/search-fda-guidance-documents/development-therapeutic-protein-biosimilars-comparative-analyticalassessment-and-other-quality
- Phan DB, Elyoussfi S, Stevenson M, et al. Biosimilars for the treatment of psoriasis: a systematic review of clinical trials and observational studies. JAMA Dermatol. 2023;159:763-771. doi:10.1001/jamadermatol.2023.1338
To the Editor:
Although biologics provide major therapeutic benefits for dermatologic conditions, they also come with a substantial cost, making them among the most expensive medications available. Medicare and Medicaid spending on biologics for dermatologic conditions increased by 320% from 2012 to 2018, reaching a staggering $10.6 billion in 2018 alone.1 Biosimilars show promise in reducing health care spending for dermatologic conditions; however, their utilization has been limited due to multiple factors, including delayed market entry from patent thickets, exclusionary formulary contracts, and prescriber skepticism regarding their safety and efficacy.2 For instance, a national survey of 1201 US physicians in specialties that are high prescribers of biologics reported that 55% doubted the safety and appropriateness of biosimilars.3
US Food and Drug Administration approval of biosimilars for adalimumab and etanercept offers the potential to reduce health care spending for dermatologic conditions. However, this cost reduction is dependent on utilization rates among dermatologists. In this national cross-sectional review of Medicare data, we predicted the impact of these biosimilars on dermatologic Medicare costs and demonstrated how differing utilization rates among dermatologists can influence potential savings.
To model 2023 utilization and cost reduction from biosimilars, we analyzed Medicare Part D data from 2020 on existing biosimilars, including granulocyte colony–stimulating factors, erythropoiesis-stimulating agents, and tumor necrosis factor α inhibitors.4 Methods in line with a 2021 report from the US Department of Health and Human Services5 as well as those of Yazdany et al6 were used. For each class, we calculated the 2020 distribution of biosimilar and originator drug claims as well as biosimilar cost reduction per 30-day claim. We utilized 2018-2021 annual growth rates for branded adalimumab and etanercept to estimate 30-day claims for 2023 and the cost of these branded agents in the absence of biosimilars. The hypothetical 2023 cost reduction from adalimumab and etanercept biosimilars was estimated by assuming 2020 biosimilar utilization rates and mean cost reduction per claim. This study utilized publicly available or aggregate summary data (not attributable to specific patients) and did not qualify as human subject research; therefore, institutional review board approval was not required.
In 2020, biosimilar utilization proportions ranged from 6.4% (tumor necrosis factor α inhibitors) to 82.7% (granulocyte colony–stimulating factors), with a mean across all classes of 35.7%. On average, the cost per 30-day claim of biosimilars was 66.8% of originator agents (Table 1). In 2021, we identified 57,868 30-day claims for branded adalimumab and etanercept submitted by dermatologists. From 2018 to 2021, 30-day branded adalimumab claims increased by 1.27% annually (cost + 10.62% annually), while claims for branded etanercept decreased by 13.0% annually (cost + 5.68% annually). Assuming these trends, the cost of branded adalimumab and etanercept was estimated to be $539 million in 2023. Applying the aforementioned 35.7% utilization, the introduction of biosimilars in dermatology would yield a cost reduction of approximately $118 million (21.9%). A high utilization rate (82.7%) of biosimilars among dermatologists would increase cost savings to $199 million (36.9%)(Table 2).

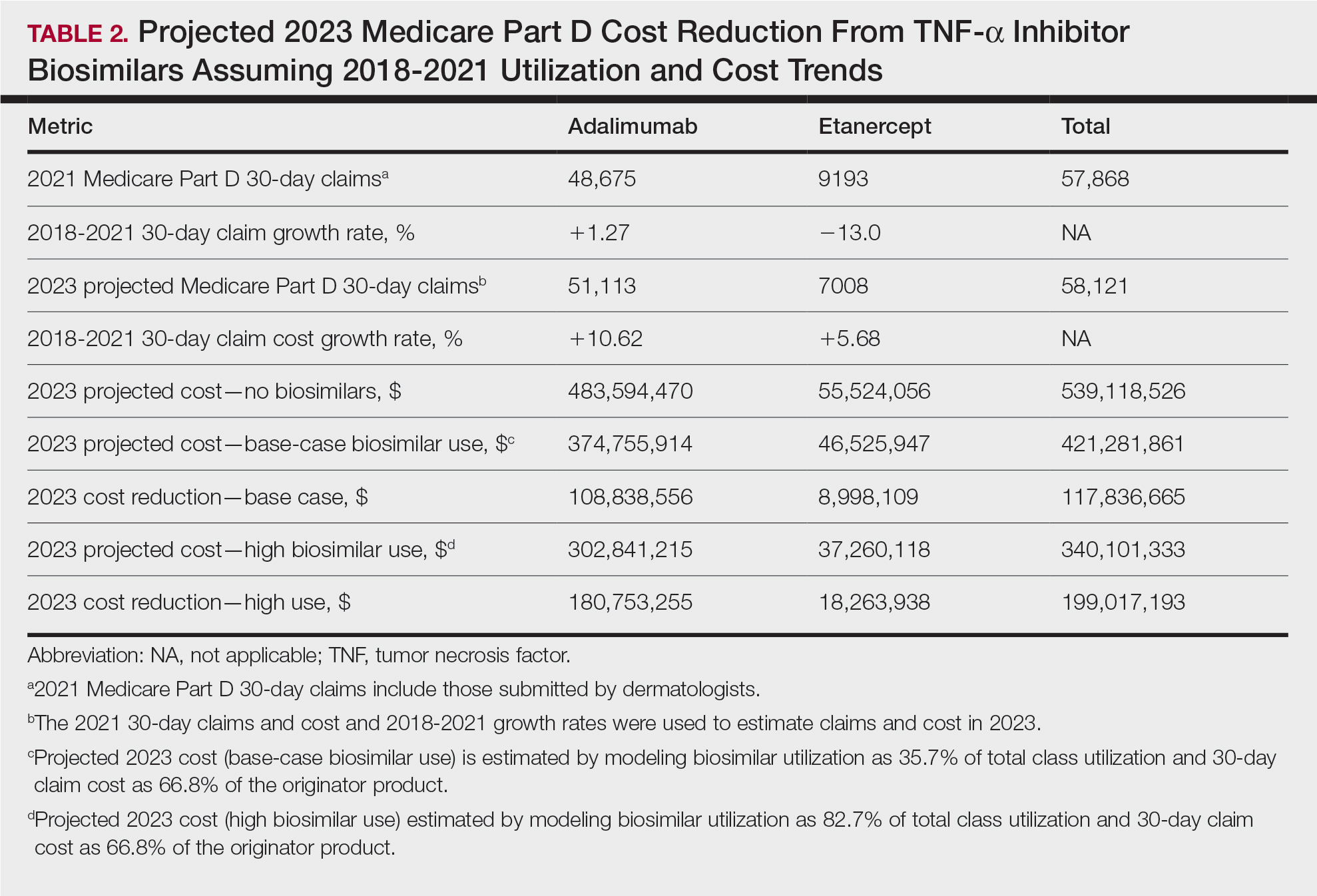
Our study demonstrates that the introduction of 2 biosimilars into dermatology may result in a notable reduction in Medicare expenditures. The savings observed are likely to translate to substantial cost savings for patients. A cross-sectional analysis of 2020 Medicare data indicated that coverage for psoriasis medications was 10.0% to 99.8% across different products and Medicare Part D plans. Consequently, patients faced considerable out-of-pocket expenses, amounting to $5653 and $5714 per year for adalimumab and etanercept, respectively.7
We found that the extent of savings from biosimilars was dependent on the utilization rates among dermatologists, with the highest utilization rate almost doubling the total savings of average utilization rates. Given the impact of high utilization and the wide variation observed, understanding the factors that have influenced uptake of biosimilars is important to increasing utilization as these medications become integrated into dermatology. For instance, limited uptake of infliximab initially may have been influenced by concerns about efficacy and increased adverse events.8,9 In contrast, the high utilization of filgrastim biosimilars (82.7%) may be attributed to its longevity in the market and familiarity to prescribers, as filgrastim was the first biosimilar to be approved in the United States.10
Promoting reasonable utilization of biosimilars may require prescriber education on their safety and approval processes, which could foster increased utilization and reduce skepticism.4 Under the Biologics Price Competition and Innovation Act, the US Food and Drug Administration approves biosimilars only when they exhibit “high similarity” and show no “clinically meaningful differences” compared to the reference biologic, with no added safety risks or reduced efficacy.11 Moreover, a 2023 systematic review of 17 studies found no major difference in efficacy and safety between biosimilars and originators of etanercept, infliximab, and other biologics.12 Understanding these findings may reassure dermatologists and patients about the reliability and safety of biosimilars.
A limitation of our study is that it solely assesses Medicare data and estimates derived from existing (separate) biologic classes. It also does not account for potential expenditure shifts to newer biologic agents (eg, IL-12/17/23 inhibitors) or changes in manufacturer behavior or promotions. Nevertheless, it indicates notable financial savings from new biosimilar agents in dermatology; along with their compelling efficacy and safety profiles, this could represent a substantial benefit to patients and the health care system.
To the Editor:
Although biologics provide major therapeutic benefits for dermatologic conditions, they also come with a substantial cost, making them among the most expensive medications available. Medicare and Medicaid spending on biologics for dermatologic conditions increased by 320% from 2012 to 2018, reaching a staggering $10.6 billion in 2018 alone.1 Biosimilars show promise in reducing health care spending for dermatologic conditions; however, their utilization has been limited due to multiple factors, including delayed market entry from patent thickets, exclusionary formulary contracts, and prescriber skepticism regarding their safety and efficacy.2 For instance, a national survey of 1201 US physicians in specialties that are high prescribers of biologics reported that 55% doubted the safety and appropriateness of biosimilars.3
US Food and Drug Administration approval of biosimilars for adalimumab and etanercept offers the potential to reduce health care spending for dermatologic conditions. However, this cost reduction is dependent on utilization rates among dermatologists. In this national cross-sectional review of Medicare data, we predicted the impact of these biosimilars on dermatologic Medicare costs and demonstrated how differing utilization rates among dermatologists can influence potential savings.
To model 2023 utilization and cost reduction from biosimilars, we analyzed Medicare Part D data from 2020 on existing biosimilars, including granulocyte colony–stimulating factors, erythropoiesis-stimulating agents, and tumor necrosis factor α inhibitors.4 Methods in line with a 2021 report from the US Department of Health and Human Services5 as well as those of Yazdany et al6 were used. For each class, we calculated the 2020 distribution of biosimilar and originator drug claims as well as biosimilar cost reduction per 30-day claim. We utilized 2018-2021 annual growth rates for branded adalimumab and etanercept to estimate 30-day claims for 2023 and the cost of these branded agents in the absence of biosimilars. The hypothetical 2023 cost reduction from adalimumab and etanercept biosimilars was estimated by assuming 2020 biosimilar utilization rates and mean cost reduction per claim. This study utilized publicly available or aggregate summary data (not attributable to specific patients) and did not qualify as human subject research; therefore, institutional review board approval was not required.
In 2020, biosimilar utilization proportions ranged from 6.4% (tumor necrosis factor α inhibitors) to 82.7% (granulocyte colony–stimulating factors), with a mean across all classes of 35.7%. On average, the cost per 30-day claim of biosimilars was 66.8% of originator agents (Table 1). In 2021, we identified 57,868 30-day claims for branded adalimumab and etanercept submitted by dermatologists. From 2018 to 2021, 30-day branded adalimumab claims increased by 1.27% annually (cost + 10.62% annually), while claims for branded etanercept decreased by 13.0% annually (cost + 5.68% annually). Assuming these trends, the cost of branded adalimumab and etanercept was estimated to be $539 million in 2023. Applying the aforementioned 35.7% utilization, the introduction of biosimilars in dermatology would yield a cost reduction of approximately $118 million (21.9%). A high utilization rate (82.7%) of biosimilars among dermatologists would increase cost savings to $199 million (36.9%)(Table 2).

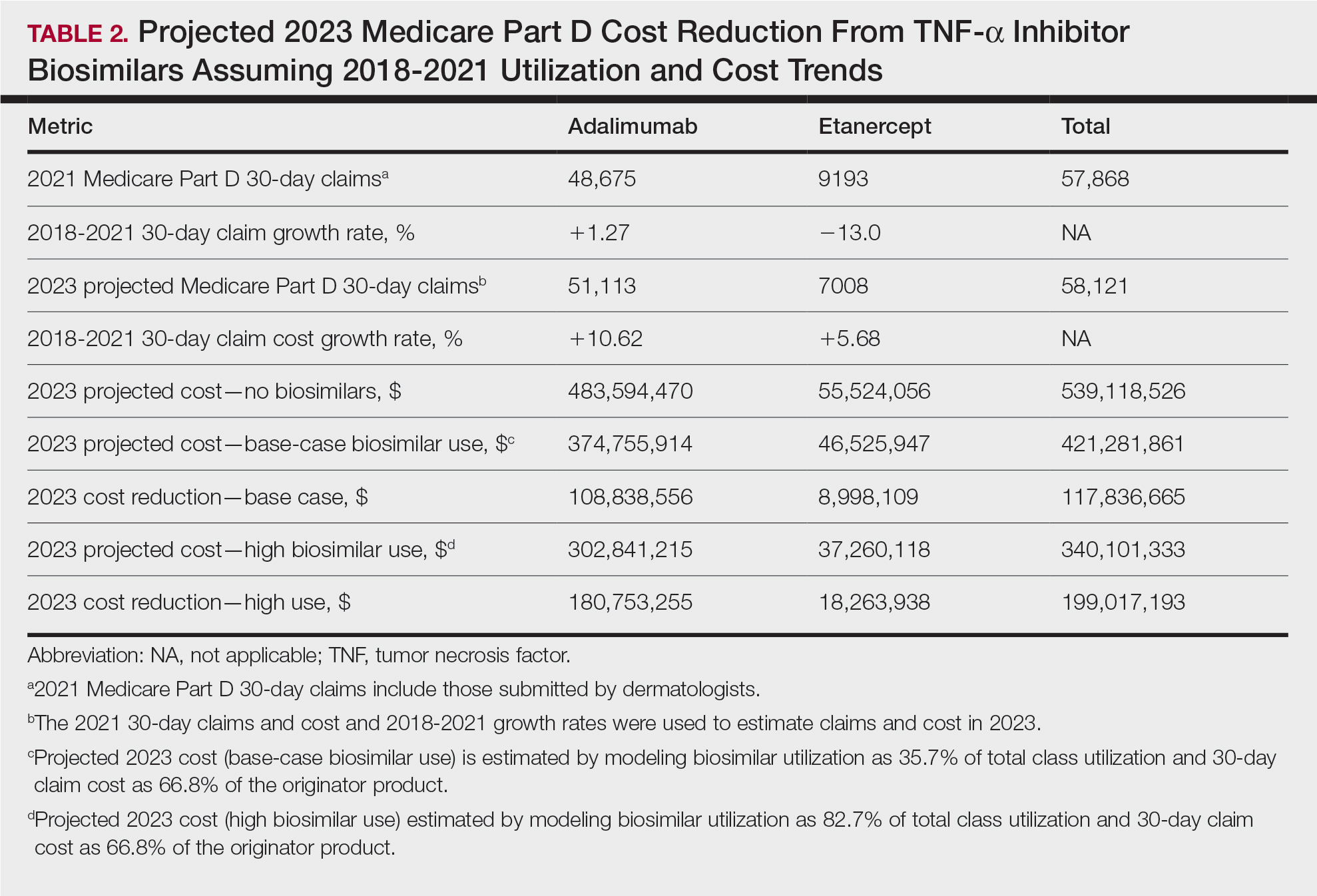
Our study demonstrates that the introduction of 2 biosimilars into dermatology may result in a notable reduction in Medicare expenditures. The savings observed are likely to translate to substantial cost savings for patients. A cross-sectional analysis of 2020 Medicare data indicated that coverage for psoriasis medications was 10.0% to 99.8% across different products and Medicare Part D plans. Consequently, patients faced considerable out-of-pocket expenses, amounting to $5653 and $5714 per year for adalimumab and etanercept, respectively.7
We found that the extent of savings from biosimilars was dependent on the utilization rates among dermatologists, with the highest utilization rate almost doubling the total savings of average utilization rates. Given the impact of high utilization and the wide variation observed, understanding the factors that have influenced uptake of biosimilars is important to increasing utilization as these medications become integrated into dermatology. For instance, limited uptake of infliximab initially may have been influenced by concerns about efficacy and increased adverse events.8,9 In contrast, the high utilization of filgrastim biosimilars (82.7%) may be attributed to its longevity in the market and familiarity to prescribers, as filgrastim was the first biosimilar to be approved in the United States.10
Promoting reasonable utilization of biosimilars may require prescriber education on their safety and approval processes, which could foster increased utilization and reduce skepticism.4 Under the Biologics Price Competition and Innovation Act, the US Food and Drug Administration approves biosimilars only when they exhibit “high similarity” and show no “clinically meaningful differences” compared to the reference biologic, with no added safety risks or reduced efficacy.11 Moreover, a 2023 systematic review of 17 studies found no major difference in efficacy and safety between biosimilars and originators of etanercept, infliximab, and other biologics.12 Understanding these findings may reassure dermatologists and patients about the reliability and safety of biosimilars.
A limitation of our study is that it solely assesses Medicare data and estimates derived from existing (separate) biologic classes. It also does not account for potential expenditure shifts to newer biologic agents (eg, IL-12/17/23 inhibitors) or changes in manufacturer behavior or promotions. Nevertheless, it indicates notable financial savings from new biosimilar agents in dermatology; along with their compelling efficacy and safety profiles, this could represent a substantial benefit to patients and the health care system.
- Price KN, Atluri S, Hsiao JL, et al. Medicare and medicaid spending trends for immunomodulators prescribed for dermatologic conditions. J Dermatolog Treat. 2020;33:575-579.
- Zhai MZ, Sarpatwari A, Kesselheim AS. Why are biosimilars not living up to their promise in the US? AMA J Ethics. 2019;21:E668-E678. doi:10.1001/amajethics.2019.668
- Cohen H, Beydoun D, Chien D, et al. Awareness, knowledge, and perceptions of biosimilars among specialty physicians. Adv Ther. 2017;33:2160-2172.
- Centers for Medicare & Medicaid Services. Medicare Part D prescribers— by provider and drug. Accessed September 11, 2024. https://data.cms.gov/provider-summary-by-type-of-service/medicare-part-d-prescribers/medicare-part-d-prescribers-by-provider-and-drug/data
- US Department of Health and Human Services. Office of Inspector General. Medicare Part D and beneficiaries could realize significant spending reductions with increased biosimilar use. Accessed September 11, 2024. https://oig.hhs.gov/oei/reports/OEI-05-20-00480.pdf
- Yazdany J, Dudley RA, Lin GA, et al. Out-of-pocket costs for infliximab and its biosimilar for rheumatoid arthritis under Medicare Part D. JAMA. 2018;320:931-933. doi:10.1001/jama.2018.7316
- Pourali SP, Nshuti L, Dusetzina SB. Out-of-pocket costs of specialty medications for psoriasis and psoriatic arthritis treatment in the medicare population. JAMA Dermatol. 2021;157:1239-1241. doi:10.1001/ jamadermatol.2021.3616
- Lebwohl M. Biosimilars in dermatology. JAMA Dermatol. 2021; 157:641-642. doi:10.1001/jamadermatol.2021.0219
- Westerkam LL, Tackett KJ, Sayed CJ. Comparing the effectiveness and safety associated with infliximab vs infliximab-abda therapy for patients with hidradenitis suppurativa. JAMA Dermatol. 2021;157:708-711. doi:10.1001/jamadermatol.2021.0220
- Awad M, Singh P, Hilas O. Zarxio (Filgrastim-sndz): the first biosimilar approved by the FDA. P T. 2017;42:19-23.
- Development of therapeutic protein biosimilars: comparative analytical assessment and other quality-related considerations guidance for industry. US Department of Health and Human Services website. Updated June 15, 2022. Accessed October 21, 2024. https://www.fda.gov/regulatory-information/search-fda-guidance-documents/development-therapeutic-protein-biosimilars-comparative-analyticalassessment-and-other-quality
- Phan DB, Elyoussfi S, Stevenson M, et al. Biosimilars for the treatment of psoriasis: a systematic review of clinical trials and observational studies. JAMA Dermatol. 2023;159:763-771. doi:10.1001/jamadermatol.2023.1338
- Price KN, Atluri S, Hsiao JL, et al. Medicare and medicaid spending trends for immunomodulators prescribed for dermatologic conditions. J Dermatolog Treat. 2020;33:575-579.
- Zhai MZ, Sarpatwari A, Kesselheim AS. Why are biosimilars not living up to their promise in the US? AMA J Ethics. 2019;21:E668-E678. doi:10.1001/amajethics.2019.668
- Cohen H, Beydoun D, Chien D, et al. Awareness, knowledge, and perceptions of biosimilars among specialty physicians. Adv Ther. 2017;33:2160-2172.
- Centers for Medicare & Medicaid Services. Medicare Part D prescribers— by provider and drug. Accessed September 11, 2024. https://data.cms.gov/provider-summary-by-type-of-service/medicare-part-d-prescribers/medicare-part-d-prescribers-by-provider-and-drug/data
- US Department of Health and Human Services. Office of Inspector General. Medicare Part D and beneficiaries could realize significant spending reductions with increased biosimilar use. Accessed September 11, 2024. https://oig.hhs.gov/oei/reports/OEI-05-20-00480.pdf
- Yazdany J, Dudley RA, Lin GA, et al. Out-of-pocket costs for infliximab and its biosimilar for rheumatoid arthritis under Medicare Part D. JAMA. 2018;320:931-933. doi:10.1001/jama.2018.7316
- Pourali SP, Nshuti L, Dusetzina SB. Out-of-pocket costs of specialty medications for psoriasis and psoriatic arthritis treatment in the medicare population. JAMA Dermatol. 2021;157:1239-1241. doi:10.1001/ jamadermatol.2021.3616
- Lebwohl M. Biosimilars in dermatology. JAMA Dermatol. 2021; 157:641-642. doi:10.1001/jamadermatol.2021.0219
- Westerkam LL, Tackett KJ, Sayed CJ. Comparing the effectiveness and safety associated with infliximab vs infliximab-abda therapy for patients with hidradenitis suppurativa. JAMA Dermatol. 2021;157:708-711. doi:10.1001/jamadermatol.2021.0220
- Awad M, Singh P, Hilas O. Zarxio (Filgrastim-sndz): the first biosimilar approved by the FDA. P T. 2017;42:19-23.
- Development of therapeutic protein biosimilars: comparative analytical assessment and other quality-related considerations guidance for industry. US Department of Health and Human Services website. Updated June 15, 2022. Accessed October 21, 2024. https://www.fda.gov/regulatory-information/search-fda-guidance-documents/development-therapeutic-protein-biosimilars-comparative-analyticalassessment-and-other-quality
- Phan DB, Elyoussfi S, Stevenson M, et al. Biosimilars for the treatment of psoriasis: a systematic review of clinical trials and observational studies. JAMA Dermatol. 2023;159:763-771. doi:10.1001/jamadermatol.2023.1338
Practice Points
- Biosimilars for adalimumab and etanercept are safe and effective alternatives with the potential to reduce health care costs in dermatology by approximately $118 million.
- A high utilization rate of biosimilars by dermatologists would increase cost savings even further.



