User login
Does ‘Brain Training’ Really Improve Cognition and Forestall Cognitive Decline?
The concept that cognitive health can be preserved or improved is often expressed as “use it or lose it.” Numerous modifiable risk factors are associated with “losing” cognitive abilities with age, and a cognitively active lifestyle may have a protective effect.
But what is a “cognitively active lifestyle” — do crosswords and Sudoku count?
One popular approach is “brain training.” While not a scientific term with an established definition, it “typically refers to tasks or drills that are designed to strengthen specific aspects of one’s cognitive function,” explained Yuko Hara, PhD, director of Aging and Alzheimer’s Prevention at the Alzheimer’s Drug Discovery Foundation.
Manuel Montero-Odasso, MD, PhD, director of the Gait and Brain Lab, Parkwood Institute, London, Ontario, Canada, elaborated: “Cognitive training involves performing a definitive task or set of tasks where you increase attentional demands to improve focus and concentration and memory. You try to execute the new things that you’ve learned and to remember them.”
In a commentary published by this news organization in 2022, neuroscientist Michael Merzenich, PhD, professor emeritus at University of California San Francisco, said that growing a person’s cognitive reserve and actively managing brain health can play an important role in preventing or delaying Alzheimer’s disease. Important components of this include brain training and physical exercise.
Brain Training: Mechanism of Action
Dr. Montero-Odasso, team leader at the Canadian Consortium on Neurodegeneration in Aging and team co-leader at the Ontario Neurodegenerative Research Initiative, explained that cognitive training creates new synapses in the brain, thus stimulating neuroplasticity.
“When we try to activate networks mainly in the frontal lobe, the prefrontal cortex, a key mechanism underlying this process is enhancement of the synaptic plasticity at excitatory synapses, which connect neurons into networks; in other words, we generate new synapses, and that’s how we enhance brain health and cognitive abilities.”
The more neural connections, the greater the processing speed of the brain, he continued. “Cognitive training creates an anatomical change in the brain.”
Executive functions, which include attention, inhibition, planning, and multitasking, are regulated predominantly by the prefrontal cortex. Damage in this region of the brain is also implicated in dementia. Alterations in the connectivity of this area are associated with cognitive impairment, independent of other structural pathological aberrations (eg, gray matter atrophy). These patterns may precede structural pathological changes associated with cognitive impairment and dementia.
Neuroplasticity changes have been corroborated through neuroimaging, which has demonstrated that after cognitive training, there is more activation in the prefrontal cortex that correlates with new synapses, Dr. Montero-Odasso said.
Henry Mahncke, PhD, CEO of the brain training company Posit Science/BrainHQ, explained that early research was conducted on rodents and monkeys, with Dr. Merzenich as one of the leading pioneers in developing the concept of brain plasticity. Dr. Merzenich cofounded Posit Science and is currently its chief scientific officer.
Dr. Mahncke recounted that as a graduate student, he had worked with Dr. Merzenich researching brain plasticity. When Dr. Merzenich founded Posit Science, he asked Dr. Mahncke to join the company to help develop approaches to enhance brain plasticity — building the brain-training exercises and running the clinical trials.
“It’s now well understood that the brain can rewire itself at any age and in almost any condition,” Dr. Mahncke said. “In kids and in younger and older adults, whether with healthy or unhealthy brains, the fundamental way the brain works is by continually rewiring and rebuilding itself, based on what we ask it to do.”
Dr. Mahncke said.
Unsubstantiated Claims and Controversy
Brain training is not without controversy, Dr. Hara pointed out. “Some manufacturers of brain games have been criticized and even fined for making unsubstantiated claims,” she said.
A 2016 review found that brain-training interventions do improve performance on specific trained tasks, but there is less evidence that they improve performance on closely related tasks and little evidence that training improves everyday cognitive performance. A 2017 review reached similar conclusions, calling evidence regarding prevention or delay of cognitive decline or dementia through brain games “insufficient,” although cognitive training could “improve cognition in the domain trained.”
“The general consensus is that for most brain-training programs, people may get better at specific tasks through practice, but these improvements don’t necessarily translate into improvement in other tasks that require other cognitive domains or prevention of dementia or age-related cognitive decline,” Dr. Hara said.
She noted that most brain-training programs “have not been rigorously tested in clinical trials” — although some, such as those featured in the ACTIVE trial, did show evidence of effectiveness.
Dr. Mahncke agreed. “Asking whether brain training works is like asking whether small molecules improve health,” he said noting that some brain-training programs are nonsense and not evidence based. He believes that his company’s product, BrainHQ, and some others are “backed by robust evidence in their ability to stave off, slow, or even reverse cognitive changes.”
BrainHQ is a web-based brain game suite that can be used independently as an app or in group settings (classes and webinars) and is covered by some Medicare Advantage insurance plans. It encompasses “dozens of individual brain-training exercises, linked by a common thread. Each one is intensively designed to make the brain faster and more accurate,” said Dr. Mahncke.
He explained that human brains “get noisy as people get older, like a radio which is wearing out, so there’s static in the background. This makes the music hard to hear, and in the case of the human brain, it makes it difficult to pay attention.” The exercises are “designed to tamp down the ‘noise,’ speed up the brain, and make information processing more accurate.”
Dr. Mahncke called this a “bottom-up” approach, in contrast to many previous cognitive-training approaches that come from the brain injury rehabilitation field. They teach “top-down” skills and strategies designed to compensate for deficits in specific domains, such as reading, concentration, or fine motor skills.
By contrast, the approach of BrainHQ is “to improve the overall processing system of the brain with speed, attention, working memory, and executive function, which will in turn impact all skills and activities.”
Supporting Evidence
Dr. Mahncke cited several supporting studies. For example, the IMPACT study randomized 487 adults (aged ≥ 65 years) to receive either a brain plasticity–based computerized cognitive training program (BrainHQ) or a novelty- and intensity-matched general cognitive stimulation treatment program (intervention and control group, respectively) for an 8-week period.
Those who underwent brain training showed significantly greater improvement in the repeatable Battery for the Assessment of Neuropsychological Status (RBANS Auditory Memory/Attention) compared with those in the control group (3.9 vs 1.8, respectively; P =.02). The intervention group also showed significant improvements on multiple secondary measures of attention and memory. The magnitude of the effect sizes suggests that the results are clinically significant, according to the authors.
The ACTIVE study tested the effects of different cognitive training programs on cognitive function and time to dementia. The researchers randomized 2802 healthy older adults (mean age, 74 years) to a control group with no cognitive training or one of three brain-training groups comprising:
1. In-person training on verbal memory skills
2. In-person training on reasoning and problem-solving
3. Computer-based speed-of-processing training on visual attention
Participants in the training groups completed 10 sessions, each lasting 60-75 minutes, over a 5- to 6-week period. A random subsample of each training group was selected to receive “booster” sessions, with four-session booster training delivered at 11 and 35 months. All study participants completed follow-up tests of cognition and function after 1, 2, 3, 5, and 10 years.
At the end of 10 years, those assigned to the speed-of-processing training, now part of BrainHQ, had a 29% lower risk for dementia than those in the control group who received no training. No reduction was found in the memory or reasoning training groups. Participants who completed the “booster” sessions had an even greater reduction: Each additional booster session was associated with a 10% lower risk for dementia.
Dr. Montero-Odasso was involved in the SYNERGIC study that randomized 175 participants with mild cognitive impairment (MCI; average age, 73 years) to one of five study arms:
1. Multidomain intervention with exercise, cognitive training, and vitamin D
2. Exercise, cognitive training, and placebo
3. Exercise, sham cognitive training, and vitamin D
4. Exercise, sham cognitive training, and placebo
5. Control group with balance-toning exercise, sham cognitive training, and placebo
“Sham” cognitive training consisted of alternating between two tasks (touristic search and video watching) performed on a tablet, with the same time exposure as the intervention training.
The researchers found that after 6 months of interventions, all active arms with aerobic-resistance exercise showed improvement in the ADAS-Cog-13, an established outcome to evaluate dementia treatments, when compared with the control group — regardless of the addition of cognitive training or vitamin D.
Compared with exercise alone (arms 3 and 4), those who did exercise plus cognitive training (arms 1 and 2) showed greater improvements in their ADAS-Cog-13l score, with a mean difference of −1.45 points (P = .02). The greatest improvement was seen in those who underwent the multidomain intervention in arm 1.
The authors noted that the mean 2.64-point improvement seen in the ADAS-Cog-13 for the multidomain intervention is actually larger than changes seen in previous pharmaceutical trials among individuals with MCI or mild dementia and “approaches” the three points considered clinically meaningful.
“We found that older adults with MCI who received aerobic-resistance exercise with sequential computerized cognitive training significantly improved cognition,” Dr. Montero-Odasso said. “The cognitive training we used was called Neuropeak, a multidomain lifestyle training delivered through a web-based platform developed by our co-leader Louis Bherer at Université de Montréal.”
He explained that the purpose “is to challenge your brain to the point where you need to make an effort to remember things, pay attention, and later to execute tasks. The evidence from clinical trials, including ours, shows this type of brain challenge is effective in slowing and even reversing cognitive decline.”
A follow-up study, SYNERGIC 2.0, is ongoing.
Puzzles, Board Games, and New Challenges
Formal brain-training programs aren’t the only way to improve brain plasticity, Dr. Hara said. Observational studies suggested an association between improved cognitive performance and/or lower dementia risk and engaging in number and word puzzles, such as crosswords, cards, or board games.
Some studies suggested that older adults who use technology might also protect their cognitive reserve. Dr. Hara cited a US longitudinal study of more than 18,000 older adults suggesting that regular Internet users had roughly half the risk for dementia compared to nonregular Internet users. Estimates of daily Internet use suggested a U-shaped relationship with dementia with 0.1-2.0 hours daily (excluding time spent watching television or movies online) associated with the lowest risk. Similar associations between Internet use and a lower risk for cognitive decline have been reported in the United Kingdom and Europe.
“Engaging in mentally stimulating activities can increase ‘cognitive reserve’ — meaning, capacity of the brain to resist the effects of age-related changes or disease-related pathology, such that one can maintain cognitive function for longer,” Dr. Hara said. “Cognitively stimulating activities, regardless of the type, may help delay the onset of cognitive decline.”
She listed several examples of activities that are stimulating to the brain, including learning a new game or puzzle, a new language, or a new dance, and learning how to play a musical instrument.
Dr. Montero-Odasso emphasized that the “newness” is key to increasing and preserving cognitive reserve. “Just surfing the Internet, playing word or board games, or doing crossword puzzles won’t be enough if you’ve been doing these things all your life,” he said. “It won’t hurt, of course, but it won’t necessarily increase your cognitive abilities.
“For example, a person who regularly engages in public speaking may not improve cognition by taking a public-speaking course, but someone who has never spoken before an audience might show cognitive improvements as a result of learning a new skill,” he said. “Or someone who knows several languages already might gain from learning a brand-new language.”
He cited research supporting the benefits of dancing, which he called “an ideal activity because it’s physical, so it provides the exercise that’s been associated with improved cognition. But it also requires learning new steps and moves, which builds the synapses in the brain. And the socialization of dance classes adds another component that can improve cognition.”
Dr. Mahncke hopes that beyond engaging in day-to-day new activities, seniors will participate in computerized brain training. “There’s no reason that evidence-based training can’t be offered in senior and community centers, as yoga and swimming are,” he said. “It doesn’t have to be simply something people do on their own virtually.”
Zoom classes and Medicare reimbursements are “good steps in the right direction, but it’s time to expand this potentially life-transformative intervention so that it reaches the ever-expanding population of seniors in the United States and beyond.”
Dr. Hara reported having no disclosures. Dr. Montero-Odasso reported having no commercial or financial interest related to this topic. He serves as the president of the Canadian Geriatrics Société and is team leader in the Canadian Consortium of Neurodegeneration in Aging. Dr. Mahncke is CEO of the brain training company Posit Science/BrainHQ.
A version of this article appeared on Medscape.com.
The concept that cognitive health can be preserved or improved is often expressed as “use it or lose it.” Numerous modifiable risk factors are associated with “losing” cognitive abilities with age, and a cognitively active lifestyle may have a protective effect.
But what is a “cognitively active lifestyle” — do crosswords and Sudoku count?
One popular approach is “brain training.” While not a scientific term with an established definition, it “typically refers to tasks or drills that are designed to strengthen specific aspects of one’s cognitive function,” explained Yuko Hara, PhD, director of Aging and Alzheimer’s Prevention at the Alzheimer’s Drug Discovery Foundation.
Manuel Montero-Odasso, MD, PhD, director of the Gait and Brain Lab, Parkwood Institute, London, Ontario, Canada, elaborated: “Cognitive training involves performing a definitive task or set of tasks where you increase attentional demands to improve focus and concentration and memory. You try to execute the new things that you’ve learned and to remember them.”
In a commentary published by this news organization in 2022, neuroscientist Michael Merzenich, PhD, professor emeritus at University of California San Francisco, said that growing a person’s cognitive reserve and actively managing brain health can play an important role in preventing or delaying Alzheimer’s disease. Important components of this include brain training and physical exercise.
Brain Training: Mechanism of Action
Dr. Montero-Odasso, team leader at the Canadian Consortium on Neurodegeneration in Aging and team co-leader at the Ontario Neurodegenerative Research Initiative, explained that cognitive training creates new synapses in the brain, thus stimulating neuroplasticity.
“When we try to activate networks mainly in the frontal lobe, the prefrontal cortex, a key mechanism underlying this process is enhancement of the synaptic plasticity at excitatory synapses, which connect neurons into networks; in other words, we generate new synapses, and that’s how we enhance brain health and cognitive abilities.”
The more neural connections, the greater the processing speed of the brain, he continued. “Cognitive training creates an anatomical change in the brain.”
Executive functions, which include attention, inhibition, planning, and multitasking, are regulated predominantly by the prefrontal cortex. Damage in this region of the brain is also implicated in dementia. Alterations in the connectivity of this area are associated with cognitive impairment, independent of other structural pathological aberrations (eg, gray matter atrophy). These patterns may precede structural pathological changes associated with cognitive impairment and dementia.
Neuroplasticity changes have been corroborated through neuroimaging, which has demonstrated that after cognitive training, there is more activation in the prefrontal cortex that correlates with new synapses, Dr. Montero-Odasso said.
Henry Mahncke, PhD, CEO of the brain training company Posit Science/BrainHQ, explained that early research was conducted on rodents and monkeys, with Dr. Merzenich as one of the leading pioneers in developing the concept of brain plasticity. Dr. Merzenich cofounded Posit Science and is currently its chief scientific officer.
Dr. Mahncke recounted that as a graduate student, he had worked with Dr. Merzenich researching brain plasticity. When Dr. Merzenich founded Posit Science, he asked Dr. Mahncke to join the company to help develop approaches to enhance brain plasticity — building the brain-training exercises and running the clinical trials.
“It’s now well understood that the brain can rewire itself at any age and in almost any condition,” Dr. Mahncke said. “In kids and in younger and older adults, whether with healthy or unhealthy brains, the fundamental way the brain works is by continually rewiring and rebuilding itself, based on what we ask it to do.”
Dr. Mahncke said.
Unsubstantiated Claims and Controversy
Brain training is not without controversy, Dr. Hara pointed out. “Some manufacturers of brain games have been criticized and even fined for making unsubstantiated claims,” she said.
A 2016 review found that brain-training interventions do improve performance on specific trained tasks, but there is less evidence that they improve performance on closely related tasks and little evidence that training improves everyday cognitive performance. A 2017 review reached similar conclusions, calling evidence regarding prevention or delay of cognitive decline or dementia through brain games “insufficient,” although cognitive training could “improve cognition in the domain trained.”
“The general consensus is that for most brain-training programs, people may get better at specific tasks through practice, but these improvements don’t necessarily translate into improvement in other tasks that require other cognitive domains or prevention of dementia or age-related cognitive decline,” Dr. Hara said.
She noted that most brain-training programs “have not been rigorously tested in clinical trials” — although some, such as those featured in the ACTIVE trial, did show evidence of effectiveness.
Dr. Mahncke agreed. “Asking whether brain training works is like asking whether small molecules improve health,” he said noting that some brain-training programs are nonsense and not evidence based. He believes that his company’s product, BrainHQ, and some others are “backed by robust evidence in their ability to stave off, slow, or even reverse cognitive changes.”
BrainHQ is a web-based brain game suite that can be used independently as an app or in group settings (classes and webinars) and is covered by some Medicare Advantage insurance plans. It encompasses “dozens of individual brain-training exercises, linked by a common thread. Each one is intensively designed to make the brain faster and more accurate,” said Dr. Mahncke.
He explained that human brains “get noisy as people get older, like a radio which is wearing out, so there’s static in the background. This makes the music hard to hear, and in the case of the human brain, it makes it difficult to pay attention.” The exercises are “designed to tamp down the ‘noise,’ speed up the brain, and make information processing more accurate.”
Dr. Mahncke called this a “bottom-up” approach, in contrast to many previous cognitive-training approaches that come from the brain injury rehabilitation field. They teach “top-down” skills and strategies designed to compensate for deficits in specific domains, such as reading, concentration, or fine motor skills.
By contrast, the approach of BrainHQ is “to improve the overall processing system of the brain with speed, attention, working memory, and executive function, which will in turn impact all skills and activities.”
Supporting Evidence
Dr. Mahncke cited several supporting studies. For example, the IMPACT study randomized 487 adults (aged ≥ 65 years) to receive either a brain plasticity–based computerized cognitive training program (BrainHQ) or a novelty- and intensity-matched general cognitive stimulation treatment program (intervention and control group, respectively) for an 8-week period.
Those who underwent brain training showed significantly greater improvement in the repeatable Battery for the Assessment of Neuropsychological Status (RBANS Auditory Memory/Attention) compared with those in the control group (3.9 vs 1.8, respectively; P =.02). The intervention group also showed significant improvements on multiple secondary measures of attention and memory. The magnitude of the effect sizes suggests that the results are clinically significant, according to the authors.
The ACTIVE study tested the effects of different cognitive training programs on cognitive function and time to dementia. The researchers randomized 2802 healthy older adults (mean age, 74 years) to a control group with no cognitive training or one of three brain-training groups comprising:
1. In-person training on verbal memory skills
2. In-person training on reasoning and problem-solving
3. Computer-based speed-of-processing training on visual attention
Participants in the training groups completed 10 sessions, each lasting 60-75 minutes, over a 5- to 6-week period. A random subsample of each training group was selected to receive “booster” sessions, with four-session booster training delivered at 11 and 35 months. All study participants completed follow-up tests of cognition and function after 1, 2, 3, 5, and 10 years.
At the end of 10 years, those assigned to the speed-of-processing training, now part of BrainHQ, had a 29% lower risk for dementia than those in the control group who received no training. No reduction was found in the memory or reasoning training groups. Participants who completed the “booster” sessions had an even greater reduction: Each additional booster session was associated with a 10% lower risk for dementia.
Dr. Montero-Odasso was involved in the SYNERGIC study that randomized 175 participants with mild cognitive impairment (MCI; average age, 73 years) to one of five study arms:
1. Multidomain intervention with exercise, cognitive training, and vitamin D
2. Exercise, cognitive training, and placebo
3. Exercise, sham cognitive training, and vitamin D
4. Exercise, sham cognitive training, and placebo
5. Control group with balance-toning exercise, sham cognitive training, and placebo
“Sham” cognitive training consisted of alternating between two tasks (touristic search and video watching) performed on a tablet, with the same time exposure as the intervention training.
The researchers found that after 6 months of interventions, all active arms with aerobic-resistance exercise showed improvement in the ADAS-Cog-13, an established outcome to evaluate dementia treatments, when compared with the control group — regardless of the addition of cognitive training or vitamin D.
Compared with exercise alone (arms 3 and 4), those who did exercise plus cognitive training (arms 1 and 2) showed greater improvements in their ADAS-Cog-13l score, with a mean difference of −1.45 points (P = .02). The greatest improvement was seen in those who underwent the multidomain intervention in arm 1.
The authors noted that the mean 2.64-point improvement seen in the ADAS-Cog-13 for the multidomain intervention is actually larger than changes seen in previous pharmaceutical trials among individuals with MCI or mild dementia and “approaches” the three points considered clinically meaningful.
“We found that older adults with MCI who received aerobic-resistance exercise with sequential computerized cognitive training significantly improved cognition,” Dr. Montero-Odasso said. “The cognitive training we used was called Neuropeak, a multidomain lifestyle training delivered through a web-based platform developed by our co-leader Louis Bherer at Université de Montréal.”
He explained that the purpose “is to challenge your brain to the point where you need to make an effort to remember things, pay attention, and later to execute tasks. The evidence from clinical trials, including ours, shows this type of brain challenge is effective in slowing and even reversing cognitive decline.”
A follow-up study, SYNERGIC 2.0, is ongoing.
Puzzles, Board Games, and New Challenges
Formal brain-training programs aren’t the only way to improve brain plasticity, Dr. Hara said. Observational studies suggested an association between improved cognitive performance and/or lower dementia risk and engaging in number and word puzzles, such as crosswords, cards, or board games.
Some studies suggested that older adults who use technology might also protect their cognitive reserve. Dr. Hara cited a US longitudinal study of more than 18,000 older adults suggesting that regular Internet users had roughly half the risk for dementia compared to nonregular Internet users. Estimates of daily Internet use suggested a U-shaped relationship with dementia with 0.1-2.0 hours daily (excluding time spent watching television or movies online) associated with the lowest risk. Similar associations between Internet use and a lower risk for cognitive decline have been reported in the United Kingdom and Europe.
“Engaging in mentally stimulating activities can increase ‘cognitive reserve’ — meaning, capacity of the brain to resist the effects of age-related changes or disease-related pathology, such that one can maintain cognitive function for longer,” Dr. Hara said. “Cognitively stimulating activities, regardless of the type, may help delay the onset of cognitive decline.”
She listed several examples of activities that are stimulating to the brain, including learning a new game or puzzle, a new language, or a new dance, and learning how to play a musical instrument.
Dr. Montero-Odasso emphasized that the “newness” is key to increasing and preserving cognitive reserve. “Just surfing the Internet, playing word or board games, or doing crossword puzzles won’t be enough if you’ve been doing these things all your life,” he said. “It won’t hurt, of course, but it won’t necessarily increase your cognitive abilities.
“For example, a person who regularly engages in public speaking may not improve cognition by taking a public-speaking course, but someone who has never spoken before an audience might show cognitive improvements as a result of learning a new skill,” he said. “Or someone who knows several languages already might gain from learning a brand-new language.”
He cited research supporting the benefits of dancing, which he called “an ideal activity because it’s physical, so it provides the exercise that’s been associated with improved cognition. But it also requires learning new steps and moves, which builds the synapses in the brain. And the socialization of dance classes adds another component that can improve cognition.”
Dr. Mahncke hopes that beyond engaging in day-to-day new activities, seniors will participate in computerized brain training. “There’s no reason that evidence-based training can’t be offered in senior and community centers, as yoga and swimming are,” he said. “It doesn’t have to be simply something people do on their own virtually.”
Zoom classes and Medicare reimbursements are “good steps in the right direction, but it’s time to expand this potentially life-transformative intervention so that it reaches the ever-expanding population of seniors in the United States and beyond.”
Dr. Hara reported having no disclosures. Dr. Montero-Odasso reported having no commercial or financial interest related to this topic. He serves as the president of the Canadian Geriatrics Société and is team leader in the Canadian Consortium of Neurodegeneration in Aging. Dr. Mahncke is CEO of the brain training company Posit Science/BrainHQ.
A version of this article appeared on Medscape.com.
The concept that cognitive health can be preserved or improved is often expressed as “use it or lose it.” Numerous modifiable risk factors are associated with “losing” cognitive abilities with age, and a cognitively active lifestyle may have a protective effect.
But what is a “cognitively active lifestyle” — do crosswords and Sudoku count?
One popular approach is “brain training.” While not a scientific term with an established definition, it “typically refers to tasks or drills that are designed to strengthen specific aspects of one’s cognitive function,” explained Yuko Hara, PhD, director of Aging and Alzheimer’s Prevention at the Alzheimer’s Drug Discovery Foundation.
Manuel Montero-Odasso, MD, PhD, director of the Gait and Brain Lab, Parkwood Institute, London, Ontario, Canada, elaborated: “Cognitive training involves performing a definitive task or set of tasks where you increase attentional demands to improve focus and concentration and memory. You try to execute the new things that you’ve learned and to remember them.”
In a commentary published by this news organization in 2022, neuroscientist Michael Merzenich, PhD, professor emeritus at University of California San Francisco, said that growing a person’s cognitive reserve and actively managing brain health can play an important role in preventing or delaying Alzheimer’s disease. Important components of this include brain training and physical exercise.
Brain Training: Mechanism of Action
Dr. Montero-Odasso, team leader at the Canadian Consortium on Neurodegeneration in Aging and team co-leader at the Ontario Neurodegenerative Research Initiative, explained that cognitive training creates new synapses in the brain, thus stimulating neuroplasticity.
“When we try to activate networks mainly in the frontal lobe, the prefrontal cortex, a key mechanism underlying this process is enhancement of the synaptic plasticity at excitatory synapses, which connect neurons into networks; in other words, we generate new synapses, and that’s how we enhance brain health and cognitive abilities.”
The more neural connections, the greater the processing speed of the brain, he continued. “Cognitive training creates an anatomical change in the brain.”
Executive functions, which include attention, inhibition, planning, and multitasking, are regulated predominantly by the prefrontal cortex. Damage in this region of the brain is also implicated in dementia. Alterations in the connectivity of this area are associated with cognitive impairment, independent of other structural pathological aberrations (eg, gray matter atrophy). These patterns may precede structural pathological changes associated with cognitive impairment and dementia.
Neuroplasticity changes have been corroborated through neuroimaging, which has demonstrated that after cognitive training, there is more activation in the prefrontal cortex that correlates with new synapses, Dr. Montero-Odasso said.
Henry Mahncke, PhD, CEO of the brain training company Posit Science/BrainHQ, explained that early research was conducted on rodents and monkeys, with Dr. Merzenich as one of the leading pioneers in developing the concept of brain plasticity. Dr. Merzenich cofounded Posit Science and is currently its chief scientific officer.
Dr. Mahncke recounted that as a graduate student, he had worked with Dr. Merzenich researching brain plasticity. When Dr. Merzenich founded Posit Science, he asked Dr. Mahncke to join the company to help develop approaches to enhance brain plasticity — building the brain-training exercises and running the clinical trials.
“It’s now well understood that the brain can rewire itself at any age and in almost any condition,” Dr. Mahncke said. “In kids and in younger and older adults, whether with healthy or unhealthy brains, the fundamental way the brain works is by continually rewiring and rebuilding itself, based on what we ask it to do.”
Dr. Mahncke said.
Unsubstantiated Claims and Controversy
Brain training is not without controversy, Dr. Hara pointed out. “Some manufacturers of brain games have been criticized and even fined for making unsubstantiated claims,” she said.
A 2016 review found that brain-training interventions do improve performance on specific trained tasks, but there is less evidence that they improve performance on closely related tasks and little evidence that training improves everyday cognitive performance. A 2017 review reached similar conclusions, calling evidence regarding prevention or delay of cognitive decline or dementia through brain games “insufficient,” although cognitive training could “improve cognition in the domain trained.”
“The general consensus is that for most brain-training programs, people may get better at specific tasks through practice, but these improvements don’t necessarily translate into improvement in other tasks that require other cognitive domains or prevention of dementia or age-related cognitive decline,” Dr. Hara said.
She noted that most brain-training programs “have not been rigorously tested in clinical trials” — although some, such as those featured in the ACTIVE trial, did show evidence of effectiveness.
Dr. Mahncke agreed. “Asking whether brain training works is like asking whether small molecules improve health,” he said noting that some brain-training programs are nonsense and not evidence based. He believes that his company’s product, BrainHQ, and some others are “backed by robust evidence in their ability to stave off, slow, or even reverse cognitive changes.”
BrainHQ is a web-based brain game suite that can be used independently as an app or in group settings (classes and webinars) and is covered by some Medicare Advantage insurance plans. It encompasses “dozens of individual brain-training exercises, linked by a common thread. Each one is intensively designed to make the brain faster and more accurate,” said Dr. Mahncke.
He explained that human brains “get noisy as people get older, like a radio which is wearing out, so there’s static in the background. This makes the music hard to hear, and in the case of the human brain, it makes it difficult to pay attention.” The exercises are “designed to tamp down the ‘noise,’ speed up the brain, and make information processing more accurate.”
Dr. Mahncke called this a “bottom-up” approach, in contrast to many previous cognitive-training approaches that come from the brain injury rehabilitation field. They teach “top-down” skills and strategies designed to compensate for deficits in specific domains, such as reading, concentration, or fine motor skills.
By contrast, the approach of BrainHQ is “to improve the overall processing system of the brain with speed, attention, working memory, and executive function, which will in turn impact all skills and activities.”
Supporting Evidence
Dr. Mahncke cited several supporting studies. For example, the IMPACT study randomized 487 adults (aged ≥ 65 years) to receive either a brain plasticity–based computerized cognitive training program (BrainHQ) or a novelty- and intensity-matched general cognitive stimulation treatment program (intervention and control group, respectively) for an 8-week period.
Those who underwent brain training showed significantly greater improvement in the repeatable Battery for the Assessment of Neuropsychological Status (RBANS Auditory Memory/Attention) compared with those in the control group (3.9 vs 1.8, respectively; P =.02). The intervention group also showed significant improvements on multiple secondary measures of attention and memory. The magnitude of the effect sizes suggests that the results are clinically significant, according to the authors.
The ACTIVE study tested the effects of different cognitive training programs on cognitive function and time to dementia. The researchers randomized 2802 healthy older adults (mean age, 74 years) to a control group with no cognitive training or one of three brain-training groups comprising:
1. In-person training on verbal memory skills
2. In-person training on reasoning and problem-solving
3. Computer-based speed-of-processing training on visual attention
Participants in the training groups completed 10 sessions, each lasting 60-75 minutes, over a 5- to 6-week period. A random subsample of each training group was selected to receive “booster” sessions, with four-session booster training delivered at 11 and 35 months. All study participants completed follow-up tests of cognition and function after 1, 2, 3, 5, and 10 years.
At the end of 10 years, those assigned to the speed-of-processing training, now part of BrainHQ, had a 29% lower risk for dementia than those in the control group who received no training. No reduction was found in the memory or reasoning training groups. Participants who completed the “booster” sessions had an even greater reduction: Each additional booster session was associated with a 10% lower risk for dementia.
Dr. Montero-Odasso was involved in the SYNERGIC study that randomized 175 participants with mild cognitive impairment (MCI; average age, 73 years) to one of five study arms:
1. Multidomain intervention with exercise, cognitive training, and vitamin D
2. Exercise, cognitive training, and placebo
3. Exercise, sham cognitive training, and vitamin D
4. Exercise, sham cognitive training, and placebo
5. Control group with balance-toning exercise, sham cognitive training, and placebo
“Sham” cognitive training consisted of alternating between two tasks (touristic search and video watching) performed on a tablet, with the same time exposure as the intervention training.
The researchers found that after 6 months of interventions, all active arms with aerobic-resistance exercise showed improvement in the ADAS-Cog-13, an established outcome to evaluate dementia treatments, when compared with the control group — regardless of the addition of cognitive training or vitamin D.
Compared with exercise alone (arms 3 and 4), those who did exercise plus cognitive training (arms 1 and 2) showed greater improvements in their ADAS-Cog-13l score, with a mean difference of −1.45 points (P = .02). The greatest improvement was seen in those who underwent the multidomain intervention in arm 1.
The authors noted that the mean 2.64-point improvement seen in the ADAS-Cog-13 for the multidomain intervention is actually larger than changes seen in previous pharmaceutical trials among individuals with MCI or mild dementia and “approaches” the three points considered clinically meaningful.
“We found that older adults with MCI who received aerobic-resistance exercise with sequential computerized cognitive training significantly improved cognition,” Dr. Montero-Odasso said. “The cognitive training we used was called Neuropeak, a multidomain lifestyle training delivered through a web-based platform developed by our co-leader Louis Bherer at Université de Montréal.”
He explained that the purpose “is to challenge your brain to the point where you need to make an effort to remember things, pay attention, and later to execute tasks. The evidence from clinical trials, including ours, shows this type of brain challenge is effective in slowing and even reversing cognitive decline.”
A follow-up study, SYNERGIC 2.0, is ongoing.
Puzzles, Board Games, and New Challenges
Formal brain-training programs aren’t the only way to improve brain plasticity, Dr. Hara said. Observational studies suggested an association between improved cognitive performance and/or lower dementia risk and engaging in number and word puzzles, such as crosswords, cards, or board games.
Some studies suggested that older adults who use technology might also protect their cognitive reserve. Dr. Hara cited a US longitudinal study of more than 18,000 older adults suggesting that regular Internet users had roughly half the risk for dementia compared to nonregular Internet users. Estimates of daily Internet use suggested a U-shaped relationship with dementia with 0.1-2.0 hours daily (excluding time spent watching television or movies online) associated with the lowest risk. Similar associations between Internet use and a lower risk for cognitive decline have been reported in the United Kingdom and Europe.
“Engaging in mentally stimulating activities can increase ‘cognitive reserve’ — meaning, capacity of the brain to resist the effects of age-related changes or disease-related pathology, such that one can maintain cognitive function for longer,” Dr. Hara said. “Cognitively stimulating activities, regardless of the type, may help delay the onset of cognitive decline.”
She listed several examples of activities that are stimulating to the brain, including learning a new game or puzzle, a new language, or a new dance, and learning how to play a musical instrument.
Dr. Montero-Odasso emphasized that the “newness” is key to increasing and preserving cognitive reserve. “Just surfing the Internet, playing word or board games, or doing crossword puzzles won’t be enough if you’ve been doing these things all your life,” he said. “It won’t hurt, of course, but it won’t necessarily increase your cognitive abilities.
“For example, a person who regularly engages in public speaking may not improve cognition by taking a public-speaking course, but someone who has never spoken before an audience might show cognitive improvements as a result of learning a new skill,” he said. “Or someone who knows several languages already might gain from learning a brand-new language.”
He cited research supporting the benefits of dancing, which he called “an ideal activity because it’s physical, so it provides the exercise that’s been associated with improved cognition. But it also requires learning new steps and moves, which builds the synapses in the brain. And the socialization of dance classes adds another component that can improve cognition.”
Dr. Mahncke hopes that beyond engaging in day-to-day new activities, seniors will participate in computerized brain training. “There’s no reason that evidence-based training can’t be offered in senior and community centers, as yoga and swimming are,” he said. “It doesn’t have to be simply something people do on their own virtually.”
Zoom classes and Medicare reimbursements are “good steps in the right direction, but it’s time to expand this potentially life-transformative intervention so that it reaches the ever-expanding population of seniors in the United States and beyond.”
Dr. Hara reported having no disclosures. Dr. Montero-Odasso reported having no commercial or financial interest related to this topic. He serves as the president of the Canadian Geriatrics Société and is team leader in the Canadian Consortium of Neurodegeneration in Aging. Dr. Mahncke is CEO of the brain training company Posit Science/BrainHQ.
A version of this article appeared on Medscape.com.
Highlights in Atherosclerosis and Lipid Management From ACC 2024
Lipid highlights from the 2024 American College of Cardiology Scientific Sessions included positive outcomes for bempedoic acid in statin-intolerant patients and a inclisiran-first strategy for patients with atherosclerosis. The presentations are reported by Dr Erin Michos, associate director of preventive cardiology, Johns Hopkins University. Dr Michos begins with an update of the CLEAR Outcomes trial, which examined bempedoic acid, a nonstatin inhibitor of cholesterol synthesis, in patients who had cardiovascular disease or were at high risk of developing it. The trial found that bempedoic acid safely reduced cardiovascular events by 13% compared with placebo — findings of particular value for patients unable or unwilling to take guideline-recommended doses of statins. Commendably, the trial enrolled 48% women and 17% Hispanic/Latinx persons. Dr Michos also reports on a trial investigating an inclisiran-first strategy vs usual care in patients with atherosclerosis. The reduction in LDL cholesterol was 60% for patients in the inclisiran upfront arm vs only 7% for patients provided with usual care. In closing, Dr Michos discusses the TACTIC trial, which was an evaluation of a technology-assisted web application used to qualify patients for nonprescription statin administration.
--
Erin D. Michos, MD, MHS, Associate Professor, Department of Medicine (Cardiology), Johns Hopkins University School of Medicine; Director of Women's Cardiovascular Health Research, Associate Director of Preventive Cardiology, Johns Hopkins Hospital, Baltimore, Maryland
Erin D. Michos, MD, MHS, has disclosed the following relevant financial relationships: Serve(d) as a director, officer, partner, employee, advisor, consultant, or trustee for: Amgen; AstraZeneca; Boehringer Ingelheim; Edwards Lifesciences; Esperion; Merck; Medtronic; New Amsterdam; Novo Nordisk; Novartis; Pfizer
Lipid highlights from the 2024 American College of Cardiology Scientific Sessions included positive outcomes for bempedoic acid in statin-intolerant patients and a inclisiran-first strategy for patients with atherosclerosis. The presentations are reported by Dr Erin Michos, associate director of preventive cardiology, Johns Hopkins University. Dr Michos begins with an update of the CLEAR Outcomes trial, which examined bempedoic acid, a nonstatin inhibitor of cholesterol synthesis, in patients who had cardiovascular disease or were at high risk of developing it. The trial found that bempedoic acid safely reduced cardiovascular events by 13% compared with placebo — findings of particular value for patients unable or unwilling to take guideline-recommended doses of statins. Commendably, the trial enrolled 48% women and 17% Hispanic/Latinx persons. Dr Michos also reports on a trial investigating an inclisiran-first strategy vs usual care in patients with atherosclerosis. The reduction in LDL cholesterol was 60% for patients in the inclisiran upfront arm vs only 7% for patients provided with usual care. In closing, Dr Michos discusses the TACTIC trial, which was an evaluation of a technology-assisted web application used to qualify patients for nonprescription statin administration.
--
Erin D. Michos, MD, MHS, Associate Professor, Department of Medicine (Cardiology), Johns Hopkins University School of Medicine; Director of Women's Cardiovascular Health Research, Associate Director of Preventive Cardiology, Johns Hopkins Hospital, Baltimore, Maryland
Erin D. Michos, MD, MHS, has disclosed the following relevant financial relationships: Serve(d) as a director, officer, partner, employee, advisor, consultant, or trustee for: Amgen; AstraZeneca; Boehringer Ingelheim; Edwards Lifesciences; Esperion; Merck; Medtronic; New Amsterdam; Novo Nordisk; Novartis; Pfizer
Lipid highlights from the 2024 American College of Cardiology Scientific Sessions included positive outcomes for bempedoic acid in statin-intolerant patients and a inclisiran-first strategy for patients with atherosclerosis. The presentations are reported by Dr Erin Michos, associate director of preventive cardiology, Johns Hopkins University. Dr Michos begins with an update of the CLEAR Outcomes trial, which examined bempedoic acid, a nonstatin inhibitor of cholesterol synthesis, in patients who had cardiovascular disease or were at high risk of developing it. The trial found that bempedoic acid safely reduced cardiovascular events by 13% compared with placebo — findings of particular value for patients unable or unwilling to take guideline-recommended doses of statins. Commendably, the trial enrolled 48% women and 17% Hispanic/Latinx persons. Dr Michos also reports on a trial investigating an inclisiran-first strategy vs usual care in patients with atherosclerosis. The reduction in LDL cholesterol was 60% for patients in the inclisiran upfront arm vs only 7% for patients provided with usual care. In closing, Dr Michos discusses the TACTIC trial, which was an evaluation of a technology-assisted web application used to qualify patients for nonprescription statin administration.
--
Erin D. Michos, MD, MHS, Associate Professor, Department of Medicine (Cardiology), Johns Hopkins University School of Medicine; Director of Women's Cardiovascular Health Research, Associate Director of Preventive Cardiology, Johns Hopkins Hospital, Baltimore, Maryland
Erin D. Michos, MD, MHS, has disclosed the following relevant financial relationships: Serve(d) as a director, officer, partner, employee, advisor, consultant, or trustee for: Amgen; AstraZeneca; Boehringer Ingelheim; Edwards Lifesciences; Esperion; Merck; Medtronic; New Amsterdam; Novo Nordisk; Novartis; Pfizer

Primary Care Shortage Reshaping How Patients Seek Care
By February of 2022, Ella, a 25-year-old behavioral interventionist in Colorado Springs, Colorado, was sick with strep-like symptoms for the third time in 3 months. She didn’t bother to call her doctor.
The first two times she had strep throat, she’d tried to schedule an appointment with her newest primary care doctor but couldn’t get in. They only had available appointments 5 and even 10 days out, but she’d already had symptoms for 3 days.
Until she graduated college, Ella had only known easy-access primary care. Her childhood family doctor and the nurse practitioners at her college clinic knew her. They anticipated her yearly allergies and knew about her predisposition for strep throat. Appointments were easy to schedule, and providers responded to her messages. But since entering the workforce and leaving her parent’s insurance, the kind of primary care she’d come to rely on was nearly impossible to find.
“I went to urgent care, and that became my primary care,” she told this news organization.
Patients Can’t Get Appointments
Primary care is in crisis. A growing number of Americans, like Ella, can’t access care when they need it. According to a 2024 report, 29% of adults and 14% of children don’t have a regular source of care. Those looking for a new primary care provider face extensive research and 6- to 9-month waits for a new patient appointment — if they can get in at all.
But even those with a primary care provider face long wait times: Days to weeks for a sick visit and months for a wellness checkup. Over one third of Medicare beneficiaries wait more than a month to see a doctor. Accessing primary care is more difficult than access to surgery, physical therapy, or rehabilitative care, according to a survey of Medicare beneficiaries by the Commonwealth Fund.
“Shortages tend to be in rural and urban underserved areas, but now, you’re hearing about primary care shortages in Boston, which is a mecca of healthcare,” said Ann Greiner, president and CEO of the Primary Care Coalition.
While retail clinics, urgent care, and telehealth help close the gap in acute needs, they miss one of primary care’s most critical benefits: A doctor who knows you. There’s strong evidence that ongoing treatment from a primary care physician (PCP) who knows your history, family, and context results in better long-term outcomes and fewer hospitalizations and emergency room visits.
If patients continue to find it too hard to break into primary care or set up an appointment, experts are concerned that they’ll stop pursuing primary care altogether.
Doctors’ Hands Are Tied
“I want to highlight that this is not an issue of primary care doctors not wanting to be accessible,” said Lisa Rotenstein, MD, MBA, a PCP and medical director of Ambulatory Quality and Safety at the University of California San Francisco Health. “These access issues are symptoms of the design of primary care in the United States.”
Across the United States, there’s a dearth of family medicine doctors, pediatricians, and internists. And without significantly more primary care providers, there’s simply no way for all Americans to get optimal primary care. The Health Resources and Services administration estimates a current shortage of 13,000 primary care providers. And that shortage will skyrocket to 68,000 by 2036 as the number of Americans needing care balloons and existing PCPs retire with too few trainees to fill their shoes.
The American Association of Medical Colleges predicts a slightly lower shortage in 2036 — between 20,000 and 40,000 primary care physicians — only if more residency positions are funded nationwide.
However, even with more positions, medical trainees see little incentive to pursue primary care. Young doctors are avoiding primary care because of the pressures, Dr. Rotenstein said. There’s incredible pressure to get reimbursement for primary care doctors. And the added administrative burden makes “the work life of these specialties not really manageable,” she said.
Continued Shortages of PCPs
“We know there’s a documented pajama time,” Ms. Greiner said. For every 1 hour spent with a patient, primary care must spend nearly 2 additional hours on electronic health records and desk work, according to a study by the American Medical Association. Even with all those additional hours devoted to getting paid, primary care doctors make an average of $103,000 less annually compared with their counterparts in surgery and oncology.
It’s not an attractive combination for a new doctor with medical debt. This year, Ms. Greiner said that residency positions in internal medicine and pediatrics went unfilled. Of those trainees who do go into a primary care specialty, many won’t last. Only half of primary care residents practice in primary care 3-5 years later. The rest choose to subspecialize or become hospitalists.
These untenable demands on a primary care provider don’t go unnoticed by patients. In Ella’s attempts to invest in a new primary care relationship, she often doesn’t feel heard and can tell the doctor is rushed. “[Urgent care is] probably not the best care because they don’t know me, but it does seem like they are able to listen to me better,” Ella said.
Patients Want to Invest in Primary Care
Primary care should work like putting money in a bank account, Dr. Rotenstein said. Young patients invest in the relationship and reap the benefits of a doctor who knows them later in life when they need more complex care. But if seeing a doctor is so difficult, many young people may stop investing in their PCP relationship.
“One thing ... that I worry about in this kind of situation where patients really have to put in a lot of work to get the care they need is in inequities of care,” Dr. Rotenstein said. “We know some of our patients are more able to undertake that work.”
Alternatively, the primary care shortage could be reshaping how patients seek care. A 2023 study showed the proportion of primary care preventative visits increased over 20 years. Policies under the Affordable Care Act were the driving force. But it’s also true that sick visits are being diverted to urgent care.
Ella told this news organization she doesn’t even consider primary care for sick visits at this point. “I can’t wait 5 days or a week and a half. Unless I have bigger issues, like I need tests, I’m not even going to go to primary care.” It’s possible that other patients also see primary care as a place for testing and wellness checks and leave sick visits to retail and urgent care.
The Road Ahead
There’s no single fix for primary care, but experts agree that the fee-for-service model is a core issue for the specialty. In a 2021 report, the National Association of Engineering and Medicine said that primary care reform needs to include higher reimbursement rates for primary care and that US primary care should be restructured so that payers “pay primary care teams to care for people, not doctors to deliver services.”
In the current model, the doctor-patient clinic time is the only income-generating part of a primary care practice. A better model would consider the communication, administration, teams, and support doctors have to fund to provide the best primary care.
“We need to change how we pay and how much we pay, so [primary care doctors] are properly incentivized to build out a team to provide the comprehensive care you need,” Ms. Greiner said.
In the meantime, primary care doctors are adapting. Some drop down to part-time to account for the additional administrative workload. Others are transitioning to concierge services to offer the quality of care they want while getting the income they need. Still, others specialize their practice, offering primary care to a subset of the population, like older adults.
Employers are also looking to improve care access for their employees, hiring in-house doctors to provide primary care on site. Ms. Greiner recently met with a group of chief medical officers from major companies to discuss expanding primary care access via the workplace.
The efforts to adapt amid a broken system are admirable, Dr. Rotenstein said. And whatever a PCP has to do to keep practicing in primary care is laudable. The only problem with these adaptations is they largely limit a doctor’s patient pool and, therefore, limit access, she said. More significant reforms that adequately reimburse primary care and incentivize new doctors are still needed.
As for Ella, she got married. Her wife is in the military, so now she has Tricare, which comes with a more streamlined process to access primary care. However, doctor shortages are just as evident in that system. The couple called to schedule new patient appointments after their recent move to Virginia. The first available ones were 6 weeks out.
A version of this article appeared on Medscape.com.
By February of 2022, Ella, a 25-year-old behavioral interventionist in Colorado Springs, Colorado, was sick with strep-like symptoms for the third time in 3 months. She didn’t bother to call her doctor.
The first two times she had strep throat, she’d tried to schedule an appointment with her newest primary care doctor but couldn’t get in. They only had available appointments 5 and even 10 days out, but she’d already had symptoms for 3 days.
Until she graduated college, Ella had only known easy-access primary care. Her childhood family doctor and the nurse practitioners at her college clinic knew her. They anticipated her yearly allergies and knew about her predisposition for strep throat. Appointments were easy to schedule, and providers responded to her messages. But since entering the workforce and leaving her parent’s insurance, the kind of primary care she’d come to rely on was nearly impossible to find.
“I went to urgent care, and that became my primary care,” she told this news organization.
Patients Can’t Get Appointments
Primary care is in crisis. A growing number of Americans, like Ella, can’t access care when they need it. According to a 2024 report, 29% of adults and 14% of children don’t have a regular source of care. Those looking for a new primary care provider face extensive research and 6- to 9-month waits for a new patient appointment — if they can get in at all.
But even those with a primary care provider face long wait times: Days to weeks for a sick visit and months for a wellness checkup. Over one third of Medicare beneficiaries wait more than a month to see a doctor. Accessing primary care is more difficult than access to surgery, physical therapy, or rehabilitative care, according to a survey of Medicare beneficiaries by the Commonwealth Fund.
“Shortages tend to be in rural and urban underserved areas, but now, you’re hearing about primary care shortages in Boston, which is a mecca of healthcare,” said Ann Greiner, president and CEO of the Primary Care Coalition.
While retail clinics, urgent care, and telehealth help close the gap in acute needs, they miss one of primary care’s most critical benefits: A doctor who knows you. There’s strong evidence that ongoing treatment from a primary care physician (PCP) who knows your history, family, and context results in better long-term outcomes and fewer hospitalizations and emergency room visits.
If patients continue to find it too hard to break into primary care or set up an appointment, experts are concerned that they’ll stop pursuing primary care altogether.
Doctors’ Hands Are Tied
“I want to highlight that this is not an issue of primary care doctors not wanting to be accessible,” said Lisa Rotenstein, MD, MBA, a PCP and medical director of Ambulatory Quality and Safety at the University of California San Francisco Health. “These access issues are symptoms of the design of primary care in the United States.”
Across the United States, there’s a dearth of family medicine doctors, pediatricians, and internists. And without significantly more primary care providers, there’s simply no way for all Americans to get optimal primary care. The Health Resources and Services administration estimates a current shortage of 13,000 primary care providers. And that shortage will skyrocket to 68,000 by 2036 as the number of Americans needing care balloons and existing PCPs retire with too few trainees to fill their shoes.
The American Association of Medical Colleges predicts a slightly lower shortage in 2036 — between 20,000 and 40,000 primary care physicians — only if more residency positions are funded nationwide.
However, even with more positions, medical trainees see little incentive to pursue primary care. Young doctors are avoiding primary care because of the pressures, Dr. Rotenstein said. There’s incredible pressure to get reimbursement for primary care doctors. And the added administrative burden makes “the work life of these specialties not really manageable,” she said.
Continued Shortages of PCPs
“We know there’s a documented pajama time,” Ms. Greiner said. For every 1 hour spent with a patient, primary care must spend nearly 2 additional hours on electronic health records and desk work, according to a study by the American Medical Association. Even with all those additional hours devoted to getting paid, primary care doctors make an average of $103,000 less annually compared with their counterparts in surgery and oncology.
It’s not an attractive combination for a new doctor with medical debt. This year, Ms. Greiner said that residency positions in internal medicine and pediatrics went unfilled. Of those trainees who do go into a primary care specialty, many won’t last. Only half of primary care residents practice in primary care 3-5 years later. The rest choose to subspecialize or become hospitalists.
These untenable demands on a primary care provider don’t go unnoticed by patients. In Ella’s attempts to invest in a new primary care relationship, she often doesn’t feel heard and can tell the doctor is rushed. “[Urgent care is] probably not the best care because they don’t know me, but it does seem like they are able to listen to me better,” Ella said.
Patients Want to Invest in Primary Care
Primary care should work like putting money in a bank account, Dr. Rotenstein said. Young patients invest in the relationship and reap the benefits of a doctor who knows them later in life when they need more complex care. But if seeing a doctor is so difficult, many young people may stop investing in their PCP relationship.
“One thing ... that I worry about in this kind of situation where patients really have to put in a lot of work to get the care they need is in inequities of care,” Dr. Rotenstein said. “We know some of our patients are more able to undertake that work.”
Alternatively, the primary care shortage could be reshaping how patients seek care. A 2023 study showed the proportion of primary care preventative visits increased over 20 years. Policies under the Affordable Care Act were the driving force. But it’s also true that sick visits are being diverted to urgent care.
Ella told this news organization she doesn’t even consider primary care for sick visits at this point. “I can’t wait 5 days or a week and a half. Unless I have bigger issues, like I need tests, I’m not even going to go to primary care.” It’s possible that other patients also see primary care as a place for testing and wellness checks and leave sick visits to retail and urgent care.
The Road Ahead
There’s no single fix for primary care, but experts agree that the fee-for-service model is a core issue for the specialty. In a 2021 report, the National Association of Engineering and Medicine said that primary care reform needs to include higher reimbursement rates for primary care and that US primary care should be restructured so that payers “pay primary care teams to care for people, not doctors to deliver services.”
In the current model, the doctor-patient clinic time is the only income-generating part of a primary care practice. A better model would consider the communication, administration, teams, and support doctors have to fund to provide the best primary care.
“We need to change how we pay and how much we pay, so [primary care doctors] are properly incentivized to build out a team to provide the comprehensive care you need,” Ms. Greiner said.
In the meantime, primary care doctors are adapting. Some drop down to part-time to account for the additional administrative workload. Others are transitioning to concierge services to offer the quality of care they want while getting the income they need. Still, others specialize their practice, offering primary care to a subset of the population, like older adults.
Employers are also looking to improve care access for their employees, hiring in-house doctors to provide primary care on site. Ms. Greiner recently met with a group of chief medical officers from major companies to discuss expanding primary care access via the workplace.
The efforts to adapt amid a broken system are admirable, Dr. Rotenstein said. And whatever a PCP has to do to keep practicing in primary care is laudable. The only problem with these adaptations is they largely limit a doctor’s patient pool and, therefore, limit access, she said. More significant reforms that adequately reimburse primary care and incentivize new doctors are still needed.
As for Ella, she got married. Her wife is in the military, so now she has Tricare, which comes with a more streamlined process to access primary care. However, doctor shortages are just as evident in that system. The couple called to schedule new patient appointments after their recent move to Virginia. The first available ones were 6 weeks out.
A version of this article appeared on Medscape.com.
By February of 2022, Ella, a 25-year-old behavioral interventionist in Colorado Springs, Colorado, was sick with strep-like symptoms for the third time in 3 months. She didn’t bother to call her doctor.
The first two times she had strep throat, she’d tried to schedule an appointment with her newest primary care doctor but couldn’t get in. They only had available appointments 5 and even 10 days out, but she’d already had symptoms for 3 days.
Until she graduated college, Ella had only known easy-access primary care. Her childhood family doctor and the nurse practitioners at her college clinic knew her. They anticipated her yearly allergies and knew about her predisposition for strep throat. Appointments were easy to schedule, and providers responded to her messages. But since entering the workforce and leaving her parent’s insurance, the kind of primary care she’d come to rely on was nearly impossible to find.
“I went to urgent care, and that became my primary care,” she told this news organization.
Patients Can’t Get Appointments
Primary care is in crisis. A growing number of Americans, like Ella, can’t access care when they need it. According to a 2024 report, 29% of adults and 14% of children don’t have a regular source of care. Those looking for a new primary care provider face extensive research and 6- to 9-month waits for a new patient appointment — if they can get in at all.
But even those with a primary care provider face long wait times: Days to weeks for a sick visit and months for a wellness checkup. Over one third of Medicare beneficiaries wait more than a month to see a doctor. Accessing primary care is more difficult than access to surgery, physical therapy, or rehabilitative care, according to a survey of Medicare beneficiaries by the Commonwealth Fund.
“Shortages tend to be in rural and urban underserved areas, but now, you’re hearing about primary care shortages in Boston, which is a mecca of healthcare,” said Ann Greiner, president and CEO of the Primary Care Coalition.
While retail clinics, urgent care, and telehealth help close the gap in acute needs, they miss one of primary care’s most critical benefits: A doctor who knows you. There’s strong evidence that ongoing treatment from a primary care physician (PCP) who knows your history, family, and context results in better long-term outcomes and fewer hospitalizations and emergency room visits.
If patients continue to find it too hard to break into primary care or set up an appointment, experts are concerned that they’ll stop pursuing primary care altogether.
Doctors’ Hands Are Tied
“I want to highlight that this is not an issue of primary care doctors not wanting to be accessible,” said Lisa Rotenstein, MD, MBA, a PCP and medical director of Ambulatory Quality and Safety at the University of California San Francisco Health. “These access issues are symptoms of the design of primary care in the United States.”
Across the United States, there’s a dearth of family medicine doctors, pediatricians, and internists. And without significantly more primary care providers, there’s simply no way for all Americans to get optimal primary care. The Health Resources and Services administration estimates a current shortage of 13,000 primary care providers. And that shortage will skyrocket to 68,000 by 2036 as the number of Americans needing care balloons and existing PCPs retire with too few trainees to fill their shoes.
The American Association of Medical Colleges predicts a slightly lower shortage in 2036 — between 20,000 and 40,000 primary care physicians — only if more residency positions are funded nationwide.
However, even with more positions, medical trainees see little incentive to pursue primary care. Young doctors are avoiding primary care because of the pressures, Dr. Rotenstein said. There’s incredible pressure to get reimbursement for primary care doctors. And the added administrative burden makes “the work life of these specialties not really manageable,” she said.
Continued Shortages of PCPs
“We know there’s a documented pajama time,” Ms. Greiner said. For every 1 hour spent with a patient, primary care must spend nearly 2 additional hours on electronic health records and desk work, according to a study by the American Medical Association. Even with all those additional hours devoted to getting paid, primary care doctors make an average of $103,000 less annually compared with their counterparts in surgery and oncology.
It’s not an attractive combination for a new doctor with medical debt. This year, Ms. Greiner said that residency positions in internal medicine and pediatrics went unfilled. Of those trainees who do go into a primary care specialty, many won’t last. Only half of primary care residents practice in primary care 3-5 years later. The rest choose to subspecialize or become hospitalists.
These untenable demands on a primary care provider don’t go unnoticed by patients. In Ella’s attempts to invest in a new primary care relationship, she often doesn’t feel heard and can tell the doctor is rushed. “[Urgent care is] probably not the best care because they don’t know me, but it does seem like they are able to listen to me better,” Ella said.
Patients Want to Invest in Primary Care
Primary care should work like putting money in a bank account, Dr. Rotenstein said. Young patients invest in the relationship and reap the benefits of a doctor who knows them later in life when they need more complex care. But if seeing a doctor is so difficult, many young people may stop investing in their PCP relationship.
“One thing ... that I worry about in this kind of situation where patients really have to put in a lot of work to get the care they need is in inequities of care,” Dr. Rotenstein said. “We know some of our patients are more able to undertake that work.”
Alternatively, the primary care shortage could be reshaping how patients seek care. A 2023 study showed the proportion of primary care preventative visits increased over 20 years. Policies under the Affordable Care Act were the driving force. But it’s also true that sick visits are being diverted to urgent care.
Ella told this news organization she doesn’t even consider primary care for sick visits at this point. “I can’t wait 5 days or a week and a half. Unless I have bigger issues, like I need tests, I’m not even going to go to primary care.” It’s possible that other patients also see primary care as a place for testing and wellness checks and leave sick visits to retail and urgent care.
The Road Ahead
There’s no single fix for primary care, but experts agree that the fee-for-service model is a core issue for the specialty. In a 2021 report, the National Association of Engineering and Medicine said that primary care reform needs to include higher reimbursement rates for primary care and that US primary care should be restructured so that payers “pay primary care teams to care for people, not doctors to deliver services.”
In the current model, the doctor-patient clinic time is the only income-generating part of a primary care practice. A better model would consider the communication, administration, teams, and support doctors have to fund to provide the best primary care.
“We need to change how we pay and how much we pay, so [primary care doctors] are properly incentivized to build out a team to provide the comprehensive care you need,” Ms. Greiner said.
In the meantime, primary care doctors are adapting. Some drop down to part-time to account for the additional administrative workload. Others are transitioning to concierge services to offer the quality of care they want while getting the income they need. Still, others specialize their practice, offering primary care to a subset of the population, like older adults.
Employers are also looking to improve care access for their employees, hiring in-house doctors to provide primary care on site. Ms. Greiner recently met with a group of chief medical officers from major companies to discuss expanding primary care access via the workplace.
The efforts to adapt amid a broken system are admirable, Dr. Rotenstein said. And whatever a PCP has to do to keep practicing in primary care is laudable. The only problem with these adaptations is they largely limit a doctor’s patient pool and, therefore, limit access, she said. More significant reforms that adequately reimburse primary care and incentivize new doctors are still needed.
As for Ella, she got married. Her wife is in the military, so now she has Tricare, which comes with a more streamlined process to access primary care. However, doctor shortages are just as evident in that system. The couple called to schedule new patient appointments after their recent move to Virginia. The first available ones were 6 weeks out.
A version of this article appeared on Medscape.com.
Do No Harm: What Smoldering Myeloma Teaches Us
My approach to treating SMM takes into account what its history can teach us about 1) how advancements in imaging and diagnostic reclassifications can revise the entire natural history of a disease, and 2) how evidence generated by even the best of studies may have an expiration date.
Much of what we know about SMM today dates to a pivotal study by Robert A. Kyle, MD, and colleagues, published in 2007. That inspirational team of investigators followed people diagnosed with SMM from 1970 to 1995 and established the first natural history of the condition. Their monumental effort and the data and conclusions it generated (eg,10% risk annually of SMM becoming MM for the first 5 years) are still cited today in references, papers, and slide sets.
Despite the seminal importance of this work, from today’s perspective the 2007 study might just as well have been describing a different disease. Back then people were diagnosed with SMM if their blood work detected a monoclonal protein and a follow-up bone marrow biopsy found at least 10% plasma cells (or a monoclonal protein exceeding 3g/dL). If there were no signs of end-organ damage (ie, no anemia or kidney problems) and an x-ray showed no fractures or lesions in the bones, the diagnosis was determined to be SMM.
What’s different in 2024? First and foremost: advanced, highly sensitive imaging techniques. MRIs can pick up small lytic lesions (and even the precursor to lytic lesions) that would not appear on an x-ray. In fact, relying solely on x-rays risks missing half of the lytic lesions.
Therefore, using the same criteria, many people who in the past were diagnosed with SMM would today be diagnosed with MM. Furthermore, in 2014 a diagnostic change reclassified people’s diagnosis from the highest risk category of SMM to the category of active MM.
Due to these scientific advances and classification changes, I believe that the natural history of SMM is unknown. Risk stratification models for SMM derived from data sets of people who had not undergone rigorous advanced imaging likely are skewed by data from people who had MM. In addition, current risk stratification models have very poor concordance with each other. I routinely see people whose 2-year risk according to different models varies by more than 30%-40%.
All this information tells us that SMM today is more indolent than the SMM of the past. Paradoxically, however, our therapies keep getting more and more aggressive, exposing this vulnerable group of people to intense treatment regimens that they may not require. Therapies tested on people diagnosed with SMM include an aggressive three-drug regimen, autologous stem cell transplant, and 2 years of additional therapy, as well as, more recently CAR T-cell therapy which so far has at least a 4%-5% treatment-related mortality risk in people with myeloma and a strong signal for secondary cancer risk. Other trials are testing bispecific therapies such as talquetamab, a drug which in my experience causes horrendous skin toxicity, profound weight loss, and one’s nails to fall off.
Doctors routinely keep showing slides from Kyle’s pivotal work to describe the natural history of SMM and to justify the need for treatment, and trials continue to use outdated progression prediction models. In my opinion, as people with MM keep living longer and treatments for MM keep getting better, the threshold for intervening with asymptomatic, healthy people with SMM should be getting higher, not lower.
I strongly believe that the current landscape of SMM treatment exemplifies good intentions leading to bad outcomes. A routine blood test in a completely healthy person that finds elevated total protein in the blood could culminate in well-intentioned but aggressive therapies that can lead to many serious side effects. (I repeat: Secondary cancers and deaths from infections have all occurred in SMM trials.)
With no control arm, we simply don’t know how well these people might have fared without any therapy. For all we know, treatment may have shortened their lives due to complications up to and including death — all because of a blood test often conducted for reasons that have no evidentiary basis.
For example, plasma cell diseases are not linked to low bone density or auto-immune diseases, yet these labs are sent routinely as part of a workup for those conditions, leading to increasing anxiety and costs.
So, what is my approach? When treating people with SMM, I hold nuanced discussions of this data to help prioritize and reach informed decisions. After our honest conversation about the limitations of SMM models, older data, and the limitations of prospective data studying pharmacological treatment, almost no one signs up for treatment.
I want these people to stay safe, and I’m proud to be a part of a trial (SPOTLIGHT, NCT06212323) that aims to show prospectively that these people can be watched off treatment with monitoring via advanced imaging modalities.
In conclusion: SMM teaches us how, even in the absence of pharmacological interventions, the natural history of a disease can change over time, simply via better imaging techniques and changes in diagnostic classifications. Unfortunately, SMM also illustrates how good intentions can lead to harm.
Dr. Mohyuddin is assistant professor in the multiple myeloma program at the Huntsman Cancer Institute at the University of Utah in Salt Lake City.
My approach to treating SMM takes into account what its history can teach us about 1) how advancements in imaging and diagnostic reclassifications can revise the entire natural history of a disease, and 2) how evidence generated by even the best of studies may have an expiration date.
Much of what we know about SMM today dates to a pivotal study by Robert A. Kyle, MD, and colleagues, published in 2007. That inspirational team of investigators followed people diagnosed with SMM from 1970 to 1995 and established the first natural history of the condition. Their monumental effort and the data and conclusions it generated (eg,10% risk annually of SMM becoming MM for the first 5 years) are still cited today in references, papers, and slide sets.
Despite the seminal importance of this work, from today’s perspective the 2007 study might just as well have been describing a different disease. Back then people were diagnosed with SMM if their blood work detected a monoclonal protein and a follow-up bone marrow biopsy found at least 10% plasma cells (or a monoclonal protein exceeding 3g/dL). If there were no signs of end-organ damage (ie, no anemia or kidney problems) and an x-ray showed no fractures or lesions in the bones, the diagnosis was determined to be SMM.
What’s different in 2024? First and foremost: advanced, highly sensitive imaging techniques. MRIs can pick up small lytic lesions (and even the precursor to lytic lesions) that would not appear on an x-ray. In fact, relying solely on x-rays risks missing half of the lytic lesions.
Therefore, using the same criteria, many people who in the past were diagnosed with SMM would today be diagnosed with MM. Furthermore, in 2014 a diagnostic change reclassified people’s diagnosis from the highest risk category of SMM to the category of active MM.
Due to these scientific advances and classification changes, I believe that the natural history of SMM is unknown. Risk stratification models for SMM derived from data sets of people who had not undergone rigorous advanced imaging likely are skewed by data from people who had MM. In addition, current risk stratification models have very poor concordance with each other. I routinely see people whose 2-year risk according to different models varies by more than 30%-40%.
All this information tells us that SMM today is more indolent than the SMM of the past. Paradoxically, however, our therapies keep getting more and more aggressive, exposing this vulnerable group of people to intense treatment regimens that they may not require. Therapies tested on people diagnosed with SMM include an aggressive three-drug regimen, autologous stem cell transplant, and 2 years of additional therapy, as well as, more recently CAR T-cell therapy which so far has at least a 4%-5% treatment-related mortality risk in people with myeloma and a strong signal for secondary cancer risk. Other trials are testing bispecific therapies such as talquetamab, a drug which in my experience causes horrendous skin toxicity, profound weight loss, and one’s nails to fall off.
Doctors routinely keep showing slides from Kyle’s pivotal work to describe the natural history of SMM and to justify the need for treatment, and trials continue to use outdated progression prediction models. In my opinion, as people with MM keep living longer and treatments for MM keep getting better, the threshold for intervening with asymptomatic, healthy people with SMM should be getting higher, not lower.
I strongly believe that the current landscape of SMM treatment exemplifies good intentions leading to bad outcomes. A routine blood test in a completely healthy person that finds elevated total protein in the blood could culminate in well-intentioned but aggressive therapies that can lead to many serious side effects. (I repeat: Secondary cancers and deaths from infections have all occurred in SMM trials.)
With no control arm, we simply don’t know how well these people might have fared without any therapy. For all we know, treatment may have shortened their lives due to complications up to and including death — all because of a blood test often conducted for reasons that have no evidentiary basis.
For example, plasma cell diseases are not linked to low bone density or auto-immune diseases, yet these labs are sent routinely as part of a workup for those conditions, leading to increasing anxiety and costs.
So, what is my approach? When treating people with SMM, I hold nuanced discussions of this data to help prioritize and reach informed decisions. After our honest conversation about the limitations of SMM models, older data, and the limitations of prospective data studying pharmacological treatment, almost no one signs up for treatment.
I want these people to stay safe, and I’m proud to be a part of a trial (SPOTLIGHT, NCT06212323) that aims to show prospectively that these people can be watched off treatment with monitoring via advanced imaging modalities.
In conclusion: SMM teaches us how, even in the absence of pharmacological interventions, the natural history of a disease can change over time, simply via better imaging techniques and changes in diagnostic classifications. Unfortunately, SMM also illustrates how good intentions can lead to harm.
Dr. Mohyuddin is assistant professor in the multiple myeloma program at the Huntsman Cancer Institute at the University of Utah in Salt Lake City.
My approach to treating SMM takes into account what its history can teach us about 1) how advancements in imaging and diagnostic reclassifications can revise the entire natural history of a disease, and 2) how evidence generated by even the best of studies may have an expiration date.
Much of what we know about SMM today dates to a pivotal study by Robert A. Kyle, MD, and colleagues, published in 2007. That inspirational team of investigators followed people diagnosed with SMM from 1970 to 1995 and established the first natural history of the condition. Their monumental effort and the data and conclusions it generated (eg,10% risk annually of SMM becoming MM for the first 5 years) are still cited today in references, papers, and slide sets.
Despite the seminal importance of this work, from today’s perspective the 2007 study might just as well have been describing a different disease. Back then people were diagnosed with SMM if their blood work detected a monoclonal protein and a follow-up bone marrow biopsy found at least 10% plasma cells (or a monoclonal protein exceeding 3g/dL). If there were no signs of end-organ damage (ie, no anemia or kidney problems) and an x-ray showed no fractures or lesions in the bones, the diagnosis was determined to be SMM.
What’s different in 2024? First and foremost: advanced, highly sensitive imaging techniques. MRIs can pick up small lytic lesions (and even the precursor to lytic lesions) that would not appear on an x-ray. In fact, relying solely on x-rays risks missing half of the lytic lesions.
Therefore, using the same criteria, many people who in the past were diagnosed with SMM would today be diagnosed with MM. Furthermore, in 2014 a diagnostic change reclassified people’s diagnosis from the highest risk category of SMM to the category of active MM.
Due to these scientific advances and classification changes, I believe that the natural history of SMM is unknown. Risk stratification models for SMM derived from data sets of people who had not undergone rigorous advanced imaging likely are skewed by data from people who had MM. In addition, current risk stratification models have very poor concordance with each other. I routinely see people whose 2-year risk according to different models varies by more than 30%-40%.
All this information tells us that SMM today is more indolent than the SMM of the past. Paradoxically, however, our therapies keep getting more and more aggressive, exposing this vulnerable group of people to intense treatment regimens that they may not require. Therapies tested on people diagnosed with SMM include an aggressive three-drug regimen, autologous stem cell transplant, and 2 years of additional therapy, as well as, more recently CAR T-cell therapy which so far has at least a 4%-5% treatment-related mortality risk in people with myeloma and a strong signal for secondary cancer risk. Other trials are testing bispecific therapies such as talquetamab, a drug which in my experience causes horrendous skin toxicity, profound weight loss, and one’s nails to fall off.
Doctors routinely keep showing slides from Kyle’s pivotal work to describe the natural history of SMM and to justify the need for treatment, and trials continue to use outdated progression prediction models. In my opinion, as people with MM keep living longer and treatments for MM keep getting better, the threshold for intervening with asymptomatic, healthy people with SMM should be getting higher, not lower.
I strongly believe that the current landscape of SMM treatment exemplifies good intentions leading to bad outcomes. A routine blood test in a completely healthy person that finds elevated total protein in the blood could culminate in well-intentioned but aggressive therapies that can lead to many serious side effects. (I repeat: Secondary cancers and deaths from infections have all occurred in SMM trials.)
With no control arm, we simply don’t know how well these people might have fared without any therapy. For all we know, treatment may have shortened their lives due to complications up to and including death — all because of a blood test often conducted for reasons that have no evidentiary basis.
For example, plasma cell diseases are not linked to low bone density or auto-immune diseases, yet these labs are sent routinely as part of a workup for those conditions, leading to increasing anxiety and costs.
So, what is my approach? When treating people with SMM, I hold nuanced discussions of this data to help prioritize and reach informed decisions. After our honest conversation about the limitations of SMM models, older data, and the limitations of prospective data studying pharmacological treatment, almost no one signs up for treatment.
I want these people to stay safe, and I’m proud to be a part of a trial (SPOTLIGHT, NCT06212323) that aims to show prospectively that these people can be watched off treatment with monitoring via advanced imaging modalities.
In conclusion: SMM teaches us how, even in the absence of pharmacological interventions, the natural history of a disease can change over time, simply via better imaging techniques and changes in diagnostic classifications. Unfortunately, SMM also illustrates how good intentions can lead to harm.
Dr. Mohyuddin is assistant professor in the multiple myeloma program at the Huntsman Cancer Institute at the University of Utah in Salt Lake City.
Managing Obesity Can Lead to Sarcopenia: A ‘Hidden’ Problem
ASUNCIÓN, PARAGUAY — Sarcopenic obesity, which is characterized by excess adiposity and muscle loss, is an “underestimated and underdiagnosed” condition, said the panelists at a session of the XV Latin American Obesity Congress (FLASO 2024) and II Paraguayan Congress of Obesity. The condition often affects older adults but can also occur at any age as a result of unhealthy habits or intensive or repeated weight loss efforts.
“The drugs currently used for managing obesity promote significant weight loss, but by losing fat, muscle is also lost,” said Fabiola Romero Gómez, MD, a professor of medicine at the National University of Asunción and president of the Paraguayan Society of Endocrinology and Metabolism. “We must handle [these drugs] with extreme care. When we employ a strategy that achieves this significant weight loss, we must ensure that the patient receives a good protein intake and engages in resistance exercises, because otherwise, the cure may be worse than the disease.”
Some patients develop sarcopenic obesity after using glucagon-like peptide-1 (GLP-1) analogs, undergoing bariatric surgery, or pursuing restrictive diets, Dr. Romero said in an interview. The condition is more common when there are long-standing cycles of weight loss and subsequent gain, “which accounts for the majority of our patients,” she said.
“An important, largely ignored aspect of weight loss, whether through pharmacological or lifestyle intervention, is that a portion of the weight loss comprises lean muscle,” according to a recent editorial in Nature Medicine. “Weight regain, however, is almost entirely fat. People with chronic obesity often lose and regain weight in repeated cycles, each of which results in body-composition changes (even if they experience some net weight loss). This cycling puts people unable to sustain weight loss at risk of being metabolically less healthy than they were before the initial weight loss was achieved — in effect, at risk of developing sarcopenic obesity.”
A ‘Hidden’ Problem
,” said Dr. Romero.
According to the 2022 consensus of the European Society for Clinical Nutrition and Metabolism and the European Association for the Study of Obesity, clinical signs or factors suggesting sarcopenic obesity include age over 70 years, diagnosis of a chronic disease, repeated falls or weakness, and nutritional events such as recent weight loss or rapid gain, long-standing restrictive diets, and bariatric surgery.
The European guidelines also propose screening in individuals at risk to check for an increased body mass index (BMI) or waist circumference and suspicion parameters of sarcopenia. In this group of patients, the diagnosis should be made based on the analysis of alterations in muscle-skeletal functional parameters, such as grip or pinch strength or the 30-second chair stand test, followed by a determination of body mass alteration using dual-energy x-ray absorptiometry or electrical bioimpedance.
Electrical bioimpedance is Dr. Romero’s preferred method. It is an economical, simple, and easily transportable test that calculates lean muscle mass, fat mass, and body water based on electrical conductivity, she said. Experts have pointed out that bioimpedance scales “will revolutionize the way we measure obesity,” she added.
In an as-yet-unpublished study that received an honorable mention at the 3rd Paraguayan Congress of Endocrinology, Diabetes, and Metabolism last year, Dr. Romero and colleagues studied 126 patients (median age, 45 years) with obesity defined by percentage of fat mass determined by bioimpedance. When their BMI was analyzed, 11.1% were “normal” weight, and 35.7% were “overweight.” Even waist circumference measurement suggested that about 15% of participants were without obesity. Moreover, almost one in four participants presented with sarcopenia, “implying a decrease in quality of life and physical disability in the future if not investigated, diagnosed, and treated correctly,” said Dr. Romero.
Prevention and Recommendations
Exercise and nutrition are two key components in the prevention and management of sarcopenic obesity. Physicians prescribing GLP-1 receptor agonists “must also counsel patients about incorporating aerobic exercise and resistance training as part of the treatment plan, as well as ensuring they eat a high-protein diet,” Yoon Ji Ahn, MD, and Vibha Singhal, MD, MPH, of the Weight Management Center of Massachusetts General Hospital in Boston, wrote in a commentary published by this news organization.
Paraguayan nutritionist Patricia López Soto, a diabetes educator with postgraduate degrees in obesity, diabetes, and bariatric surgery from Favaloro University in Buenos Aires, shared with this news organization the following general recommendations to prevent sarcopenic obesity in patients undergoing weight loss treatment:
- Follow a healthy and balanced Mediterranean or DASH-style diet.
- Increase protein intake at the three to four main meals to a minimum of 1.4-1.5 g/kg/day.
- Try to make the protein intake mostly of high biological value: Beef, chicken, fish, eggs, seafood, cheese, skim milk, and yogurt.
- Ensure protein intake at each meal of between 25 g and 30 g to increase protein synthesis. For example, a 150 g portion of meat or chicken provides 30 g of protein.
- If the protein intake is not achieved through food, a supplement measure like isolated and hydrolyzed whey protein is a good option.
- Engage in strength or resistance training (weightlifting) three to four times per week and 30 minutes of cardiovascular exercise every day.
- To improve adherence, treatment should be carried out with a multidisciplinary team that includes a physician, nutritionist, and physical trainer, with frequent check-ups and body composition studies by bioimpedance.
Dr. Romero and Ms. López declared no relevant financial relationships.
This story was translated from the Medscape Spanish edition using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
ASUNCIÓN, PARAGUAY — Sarcopenic obesity, which is characterized by excess adiposity and muscle loss, is an “underestimated and underdiagnosed” condition, said the panelists at a session of the XV Latin American Obesity Congress (FLASO 2024) and II Paraguayan Congress of Obesity. The condition often affects older adults but can also occur at any age as a result of unhealthy habits or intensive or repeated weight loss efforts.
“The drugs currently used for managing obesity promote significant weight loss, but by losing fat, muscle is also lost,” said Fabiola Romero Gómez, MD, a professor of medicine at the National University of Asunción and president of the Paraguayan Society of Endocrinology and Metabolism. “We must handle [these drugs] with extreme care. When we employ a strategy that achieves this significant weight loss, we must ensure that the patient receives a good protein intake and engages in resistance exercises, because otherwise, the cure may be worse than the disease.”
Some patients develop sarcopenic obesity after using glucagon-like peptide-1 (GLP-1) analogs, undergoing bariatric surgery, or pursuing restrictive diets, Dr. Romero said in an interview. The condition is more common when there are long-standing cycles of weight loss and subsequent gain, “which accounts for the majority of our patients,” she said.
“An important, largely ignored aspect of weight loss, whether through pharmacological or lifestyle intervention, is that a portion of the weight loss comprises lean muscle,” according to a recent editorial in Nature Medicine. “Weight regain, however, is almost entirely fat. People with chronic obesity often lose and regain weight in repeated cycles, each of which results in body-composition changes (even if they experience some net weight loss). This cycling puts people unable to sustain weight loss at risk of being metabolically less healthy than they were before the initial weight loss was achieved — in effect, at risk of developing sarcopenic obesity.”
A ‘Hidden’ Problem
,” said Dr. Romero.
According to the 2022 consensus of the European Society for Clinical Nutrition and Metabolism and the European Association for the Study of Obesity, clinical signs or factors suggesting sarcopenic obesity include age over 70 years, diagnosis of a chronic disease, repeated falls or weakness, and nutritional events such as recent weight loss or rapid gain, long-standing restrictive diets, and bariatric surgery.
The European guidelines also propose screening in individuals at risk to check for an increased body mass index (BMI) or waist circumference and suspicion parameters of sarcopenia. In this group of patients, the diagnosis should be made based on the analysis of alterations in muscle-skeletal functional parameters, such as grip or pinch strength or the 30-second chair stand test, followed by a determination of body mass alteration using dual-energy x-ray absorptiometry or electrical bioimpedance.
Electrical bioimpedance is Dr. Romero’s preferred method. It is an economical, simple, and easily transportable test that calculates lean muscle mass, fat mass, and body water based on electrical conductivity, she said. Experts have pointed out that bioimpedance scales “will revolutionize the way we measure obesity,” she added.
In an as-yet-unpublished study that received an honorable mention at the 3rd Paraguayan Congress of Endocrinology, Diabetes, and Metabolism last year, Dr. Romero and colleagues studied 126 patients (median age, 45 years) with obesity defined by percentage of fat mass determined by bioimpedance. When their BMI was analyzed, 11.1% were “normal” weight, and 35.7% were “overweight.” Even waist circumference measurement suggested that about 15% of participants were without obesity. Moreover, almost one in four participants presented with sarcopenia, “implying a decrease in quality of life and physical disability in the future if not investigated, diagnosed, and treated correctly,” said Dr. Romero.
Prevention and Recommendations
Exercise and nutrition are two key components in the prevention and management of sarcopenic obesity. Physicians prescribing GLP-1 receptor agonists “must also counsel patients about incorporating aerobic exercise and resistance training as part of the treatment plan, as well as ensuring they eat a high-protein diet,” Yoon Ji Ahn, MD, and Vibha Singhal, MD, MPH, of the Weight Management Center of Massachusetts General Hospital in Boston, wrote in a commentary published by this news organization.
Paraguayan nutritionist Patricia López Soto, a diabetes educator with postgraduate degrees in obesity, diabetes, and bariatric surgery from Favaloro University in Buenos Aires, shared with this news organization the following general recommendations to prevent sarcopenic obesity in patients undergoing weight loss treatment:
- Follow a healthy and balanced Mediterranean or DASH-style diet.
- Increase protein intake at the three to four main meals to a minimum of 1.4-1.5 g/kg/day.
- Try to make the protein intake mostly of high biological value: Beef, chicken, fish, eggs, seafood, cheese, skim milk, and yogurt.
- Ensure protein intake at each meal of between 25 g and 30 g to increase protein synthesis. For example, a 150 g portion of meat or chicken provides 30 g of protein.
- If the protein intake is not achieved through food, a supplement measure like isolated and hydrolyzed whey protein is a good option.
- Engage in strength or resistance training (weightlifting) three to four times per week and 30 minutes of cardiovascular exercise every day.
- To improve adherence, treatment should be carried out with a multidisciplinary team that includes a physician, nutritionist, and physical trainer, with frequent check-ups and body composition studies by bioimpedance.
Dr. Romero and Ms. López declared no relevant financial relationships.
This story was translated from the Medscape Spanish edition using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
ASUNCIÓN, PARAGUAY — Sarcopenic obesity, which is characterized by excess adiposity and muscle loss, is an “underestimated and underdiagnosed” condition, said the panelists at a session of the XV Latin American Obesity Congress (FLASO 2024) and II Paraguayan Congress of Obesity. The condition often affects older adults but can also occur at any age as a result of unhealthy habits or intensive or repeated weight loss efforts.
“The drugs currently used for managing obesity promote significant weight loss, but by losing fat, muscle is also lost,” said Fabiola Romero Gómez, MD, a professor of medicine at the National University of Asunción and president of the Paraguayan Society of Endocrinology and Metabolism. “We must handle [these drugs] with extreme care. When we employ a strategy that achieves this significant weight loss, we must ensure that the patient receives a good protein intake and engages in resistance exercises, because otherwise, the cure may be worse than the disease.”
Some patients develop sarcopenic obesity after using glucagon-like peptide-1 (GLP-1) analogs, undergoing bariatric surgery, or pursuing restrictive diets, Dr. Romero said in an interview. The condition is more common when there are long-standing cycles of weight loss and subsequent gain, “which accounts for the majority of our patients,” she said.
“An important, largely ignored aspect of weight loss, whether through pharmacological or lifestyle intervention, is that a portion of the weight loss comprises lean muscle,” according to a recent editorial in Nature Medicine. “Weight regain, however, is almost entirely fat. People with chronic obesity often lose and regain weight in repeated cycles, each of which results in body-composition changes (even if they experience some net weight loss). This cycling puts people unable to sustain weight loss at risk of being metabolically less healthy than they were before the initial weight loss was achieved — in effect, at risk of developing sarcopenic obesity.”
A ‘Hidden’ Problem
,” said Dr. Romero.
According to the 2022 consensus of the European Society for Clinical Nutrition and Metabolism and the European Association for the Study of Obesity, clinical signs or factors suggesting sarcopenic obesity include age over 70 years, diagnosis of a chronic disease, repeated falls or weakness, and nutritional events such as recent weight loss or rapid gain, long-standing restrictive diets, and bariatric surgery.
The European guidelines also propose screening in individuals at risk to check for an increased body mass index (BMI) or waist circumference and suspicion parameters of sarcopenia. In this group of patients, the diagnosis should be made based on the analysis of alterations in muscle-skeletal functional parameters, such as grip or pinch strength or the 30-second chair stand test, followed by a determination of body mass alteration using dual-energy x-ray absorptiometry or electrical bioimpedance.
Electrical bioimpedance is Dr. Romero’s preferred method. It is an economical, simple, and easily transportable test that calculates lean muscle mass, fat mass, and body water based on electrical conductivity, she said. Experts have pointed out that bioimpedance scales “will revolutionize the way we measure obesity,” she added.
In an as-yet-unpublished study that received an honorable mention at the 3rd Paraguayan Congress of Endocrinology, Diabetes, and Metabolism last year, Dr. Romero and colleagues studied 126 patients (median age, 45 years) with obesity defined by percentage of fat mass determined by bioimpedance. When their BMI was analyzed, 11.1% were “normal” weight, and 35.7% were “overweight.” Even waist circumference measurement suggested that about 15% of participants were without obesity. Moreover, almost one in four participants presented with sarcopenia, “implying a decrease in quality of life and physical disability in the future if not investigated, diagnosed, and treated correctly,” said Dr. Romero.
Prevention and Recommendations
Exercise and nutrition are two key components in the prevention and management of sarcopenic obesity. Physicians prescribing GLP-1 receptor agonists “must also counsel patients about incorporating aerobic exercise and resistance training as part of the treatment plan, as well as ensuring they eat a high-protein diet,” Yoon Ji Ahn, MD, and Vibha Singhal, MD, MPH, of the Weight Management Center of Massachusetts General Hospital in Boston, wrote in a commentary published by this news organization.
Paraguayan nutritionist Patricia López Soto, a diabetes educator with postgraduate degrees in obesity, diabetes, and bariatric surgery from Favaloro University in Buenos Aires, shared with this news organization the following general recommendations to prevent sarcopenic obesity in patients undergoing weight loss treatment:
- Follow a healthy and balanced Mediterranean or DASH-style diet.
- Increase protein intake at the three to four main meals to a minimum of 1.4-1.5 g/kg/day.
- Try to make the protein intake mostly of high biological value: Beef, chicken, fish, eggs, seafood, cheese, skim milk, and yogurt.
- Ensure protein intake at each meal of between 25 g and 30 g to increase protein synthesis. For example, a 150 g portion of meat or chicken provides 30 g of protein.
- If the protein intake is not achieved through food, a supplement measure like isolated and hydrolyzed whey protein is a good option.
- Engage in strength or resistance training (weightlifting) three to four times per week and 30 minutes of cardiovascular exercise every day.
- To improve adherence, treatment should be carried out with a multidisciplinary team that includes a physician, nutritionist, and physical trainer, with frequent check-ups and body composition studies by bioimpedance.
Dr. Romero and Ms. López declared no relevant financial relationships.
This story was translated from the Medscape Spanish edition using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
Pancreatic Fat Is the Main Driver for Exocrine and Endocrine Pancreatic Diseases
TOPLINE:
Excessive intrapancreatic fat deposition (IPFD) leading to fatty change of the pancreas (FP) was prevalent in almost 18% of participants in a large population-based cohort, and both IPFD and FP were associated with an increased risk for diabetes, acute pancreatitis, and pancreatic cancer.
METHODOLOGY:
- This prospective cohort study conducted from July 2014 to January 2023 investigated the prevalence of FP and the link between IPFD and pancreatic diseases in 42,599 participants (median age, 65 years; 46.6% men) from the UK Biobank who underwent abdominal Dixon MRI.
- IPFD levels were measured using MRI and a deep learning-based framework called nnUNet.
- The outcomes assessed in this study were diseases of the exocrine pancreas and endocrine pancreas, including acute pancreatitis, pancreatic cancer, diabetes, and other pancreatic conditions.
TAKEAWAY:
- The prevalence of FP was 17.86%.
- Elevation in IPFD levels by one quintile increased the risk for the development of acute pancreatitis by 51.3% (P = .001), pancreatic cancer by 36.5% (P = .017), diabetes by 22.1% (P < .001), and all pancreatic diseases by 22.7% (P < .001).
- FP increased the risk for acute pancreatitis by 298.2% (P < .001), pancreatic cancer by 97.6% (P = .034), diabetes by 33.7% (P = .001), and all pancreatic diseases by 44.1% (P < .001).
- An increasing trend in the prevalence of FP with advancing age was observed in both men and women.
IN PRACTICE:
“FP is a common pancreatic disorder. Fat in the pancreas is an independent risk factor for diseases of both the exocrine pancreas and endocrine pancreas,” the authors wrote.
SOURCE:
This study, led by Xiaowu Dong, MD, of the Pancreatic Center, Department of Gastroenterology, Yangzhou Key Laboratory of Pancreatic Disease, Affiliated Hospital of Yangzhou University, Yangzhou University, Yangzhou, China, was published online in The American Journal of Gastroenterology.
LIMITATIONS:
The authors acknowledged that most of the enrolled participants were White and older than 45 years. A low response rate to recruitment invitations in the UK Biobank database may have introduced self-selection bias. The median follow-up duration of 4.61 years was short and may be insufficient to fully capture the impact of IPFD. Additionally, the use of the average fat fraction for the entire pancreas may have led to spatial variations being ignored.
DISCLOSURES:
This work was supported by the National Natural Science Foundation of China, Cultivation Foundation of Yangzhou Municipal Key Laboratory, The Medical Research Project of Jiangsu Provincial Health Commission, Yangzhou key research and development plan, and Suzhou Innovation Platform Construction Projects-Municipal Key Laboratory Construction. The authors declared no conflicts of interest.
A version of this article appeared on Medscape.com.
TOPLINE:
Excessive intrapancreatic fat deposition (IPFD) leading to fatty change of the pancreas (FP) was prevalent in almost 18% of participants in a large population-based cohort, and both IPFD and FP were associated with an increased risk for diabetes, acute pancreatitis, and pancreatic cancer.
METHODOLOGY:
- This prospective cohort study conducted from July 2014 to January 2023 investigated the prevalence of FP and the link between IPFD and pancreatic diseases in 42,599 participants (median age, 65 years; 46.6% men) from the UK Biobank who underwent abdominal Dixon MRI.
- IPFD levels were measured using MRI and a deep learning-based framework called nnUNet.
- The outcomes assessed in this study were diseases of the exocrine pancreas and endocrine pancreas, including acute pancreatitis, pancreatic cancer, diabetes, and other pancreatic conditions.
TAKEAWAY:
- The prevalence of FP was 17.86%.
- Elevation in IPFD levels by one quintile increased the risk for the development of acute pancreatitis by 51.3% (P = .001), pancreatic cancer by 36.5% (P = .017), diabetes by 22.1% (P < .001), and all pancreatic diseases by 22.7% (P < .001).
- FP increased the risk for acute pancreatitis by 298.2% (P < .001), pancreatic cancer by 97.6% (P = .034), diabetes by 33.7% (P = .001), and all pancreatic diseases by 44.1% (P < .001).
- An increasing trend in the prevalence of FP with advancing age was observed in both men and women.
IN PRACTICE:
“FP is a common pancreatic disorder. Fat in the pancreas is an independent risk factor for diseases of both the exocrine pancreas and endocrine pancreas,” the authors wrote.
SOURCE:
This study, led by Xiaowu Dong, MD, of the Pancreatic Center, Department of Gastroenterology, Yangzhou Key Laboratory of Pancreatic Disease, Affiliated Hospital of Yangzhou University, Yangzhou University, Yangzhou, China, was published online in The American Journal of Gastroenterology.
LIMITATIONS:
The authors acknowledged that most of the enrolled participants were White and older than 45 years. A low response rate to recruitment invitations in the UK Biobank database may have introduced self-selection bias. The median follow-up duration of 4.61 years was short and may be insufficient to fully capture the impact of IPFD. Additionally, the use of the average fat fraction for the entire pancreas may have led to spatial variations being ignored.
DISCLOSURES:
This work was supported by the National Natural Science Foundation of China, Cultivation Foundation of Yangzhou Municipal Key Laboratory, The Medical Research Project of Jiangsu Provincial Health Commission, Yangzhou key research and development plan, and Suzhou Innovation Platform Construction Projects-Municipal Key Laboratory Construction. The authors declared no conflicts of interest.
A version of this article appeared on Medscape.com.
TOPLINE:
Excessive intrapancreatic fat deposition (IPFD) leading to fatty change of the pancreas (FP) was prevalent in almost 18% of participants in a large population-based cohort, and both IPFD and FP were associated with an increased risk for diabetes, acute pancreatitis, and pancreatic cancer.
METHODOLOGY:
- This prospective cohort study conducted from July 2014 to January 2023 investigated the prevalence of FP and the link between IPFD and pancreatic diseases in 42,599 participants (median age, 65 years; 46.6% men) from the UK Biobank who underwent abdominal Dixon MRI.
- IPFD levels were measured using MRI and a deep learning-based framework called nnUNet.
- The outcomes assessed in this study were diseases of the exocrine pancreas and endocrine pancreas, including acute pancreatitis, pancreatic cancer, diabetes, and other pancreatic conditions.
TAKEAWAY:
- The prevalence of FP was 17.86%.
- Elevation in IPFD levels by one quintile increased the risk for the development of acute pancreatitis by 51.3% (P = .001), pancreatic cancer by 36.5% (P = .017), diabetes by 22.1% (P < .001), and all pancreatic diseases by 22.7% (P < .001).
- FP increased the risk for acute pancreatitis by 298.2% (P < .001), pancreatic cancer by 97.6% (P = .034), diabetes by 33.7% (P = .001), and all pancreatic diseases by 44.1% (P < .001).
- An increasing trend in the prevalence of FP with advancing age was observed in both men and women.
IN PRACTICE:
“FP is a common pancreatic disorder. Fat in the pancreas is an independent risk factor for diseases of both the exocrine pancreas and endocrine pancreas,” the authors wrote.
SOURCE:
This study, led by Xiaowu Dong, MD, of the Pancreatic Center, Department of Gastroenterology, Yangzhou Key Laboratory of Pancreatic Disease, Affiliated Hospital of Yangzhou University, Yangzhou University, Yangzhou, China, was published online in The American Journal of Gastroenterology.
LIMITATIONS:
The authors acknowledged that most of the enrolled participants were White and older than 45 years. A low response rate to recruitment invitations in the UK Biobank database may have introduced self-selection bias. The median follow-up duration of 4.61 years was short and may be insufficient to fully capture the impact of IPFD. Additionally, the use of the average fat fraction for the entire pancreas may have led to spatial variations being ignored.
DISCLOSURES:
This work was supported by the National Natural Science Foundation of China, Cultivation Foundation of Yangzhou Municipal Key Laboratory, The Medical Research Project of Jiangsu Provincial Health Commission, Yangzhou key research and development plan, and Suzhou Innovation Platform Construction Projects-Municipal Key Laboratory Construction. The authors declared no conflicts of interest.
A version of this article appeared on Medscape.com.
Metabolic Dysfunction–Associated Steatotic Liver Disease Plus HIV Ups Risk for CVD but Not Liver Disease
TOPLINE:
Metabolic dysfunction-associated steatotic liver disease (MASLD) co-occurring with HIV infection does not appear to increase the risk for cirrhosis or hepatocellular carcinoma (HCC) compared with MASLD alone. However, the incidence of major adverse cardiovascular events (MACE) is significantly increased among patients with MASLD and HIV, a large study suggested.
METHODOLOGY:
- MASLD is highly prevalent in people living with HIV, but the impact of HIV on liver and cardiovascular disease (CVD) outcomes in people with MASLD remains unclear.
- To investigate, researchers created a propensity score-matched cohort of veterans with noncirrhotic MASLD, with and without HIV (920 patients in each group).
- They evaluated the incidence of cirrhosis, HCC, and MACE, as well as overall survival, among the two groups. They also assessed these outcomes in MASLD patients with HIV on the basis of whether they were on antiretroviral therapy (ART).
TAKEAWAY:
- During a median follow-up of 10.4 years in the MASLD with HIV group and 11.8 years in the MASLD-only group, the overall incidence of cirrhosis and HCC was similar in MASLD with vs without HIV (cirrhosis: 0.97 vs 1.06 per 100 person-years, P = .54; HCC: 0.26 vs 0.17 per 100,000 person-years, P = .23), regardless of ART use.
- In contrast, the incidence of MACE was significantly higher in MASLD with vs without HIV (5.18 vs 4.48 per 100 person-years, P = .03). The incidence also was higher in patients with MASLD and HIV who were not on ART compared with those on ART (5.83 vs 4.7 per 100 person-years, P = .07).
- Compared with MASLD without HIV, the overall 5-year survival was significantly lower in MASLD with HIV (91.3% vs 85.7%). In MASLD with HIV, receipt of ART was associated with a significantly higher 5-year survival than no ART (87.4% vs 81.6%).
IN PRACTICE:
“Ensuring timely and appropriate initiation of HIV treatment is critical in patients with MASLD who have concurrent HIV infection, as well as optimizing metabolic comorbidities that may also contribute to increased risks of CVD and increased mortality,” the authors wrote.
SOURCE:
The study, led by Robert J. Wong, MD, Division of Gastroenterology and Hepatology, Stanford University School of Medicine, Palo Alto, California, was published online in the American Journal of Gastroenterology.
LIMITATIONS:
The study cohort consisted predominantly of older men, which may limit generalizability to women and younger populations. Metabolic comorbidities are more common in veterans compared with the general population, potentially affecting the generalizability of the CVD risk findings.
DISCLOSURES:
The study was supported by an investigator-initiated research grant from Theratechnologies. Wong has received funding for his institution from Gilead Sciences, Exact Sciences, and Durect Corporation and has served as a consultant for Gilead Sciences.
A version of this article appeared on Medscape.com.
TOPLINE:
Metabolic dysfunction-associated steatotic liver disease (MASLD) co-occurring with HIV infection does not appear to increase the risk for cirrhosis or hepatocellular carcinoma (HCC) compared with MASLD alone. However, the incidence of major adverse cardiovascular events (MACE) is significantly increased among patients with MASLD and HIV, a large study suggested.
METHODOLOGY:
- MASLD is highly prevalent in people living with HIV, but the impact of HIV on liver and cardiovascular disease (CVD) outcomes in people with MASLD remains unclear.
- To investigate, researchers created a propensity score-matched cohort of veterans with noncirrhotic MASLD, with and without HIV (920 patients in each group).
- They evaluated the incidence of cirrhosis, HCC, and MACE, as well as overall survival, among the two groups. They also assessed these outcomes in MASLD patients with HIV on the basis of whether they were on antiretroviral therapy (ART).
TAKEAWAY:
- During a median follow-up of 10.4 years in the MASLD with HIV group and 11.8 years in the MASLD-only group, the overall incidence of cirrhosis and HCC was similar in MASLD with vs without HIV (cirrhosis: 0.97 vs 1.06 per 100 person-years, P = .54; HCC: 0.26 vs 0.17 per 100,000 person-years, P = .23), regardless of ART use.
- In contrast, the incidence of MACE was significantly higher in MASLD with vs without HIV (5.18 vs 4.48 per 100 person-years, P = .03). The incidence also was higher in patients with MASLD and HIV who were not on ART compared with those on ART (5.83 vs 4.7 per 100 person-years, P = .07).
- Compared with MASLD without HIV, the overall 5-year survival was significantly lower in MASLD with HIV (91.3% vs 85.7%). In MASLD with HIV, receipt of ART was associated with a significantly higher 5-year survival than no ART (87.4% vs 81.6%).
IN PRACTICE:
“Ensuring timely and appropriate initiation of HIV treatment is critical in patients with MASLD who have concurrent HIV infection, as well as optimizing metabolic comorbidities that may also contribute to increased risks of CVD and increased mortality,” the authors wrote.
SOURCE:
The study, led by Robert J. Wong, MD, Division of Gastroenterology and Hepatology, Stanford University School of Medicine, Palo Alto, California, was published online in the American Journal of Gastroenterology.
LIMITATIONS:
The study cohort consisted predominantly of older men, which may limit generalizability to women and younger populations. Metabolic comorbidities are more common in veterans compared with the general population, potentially affecting the generalizability of the CVD risk findings.
DISCLOSURES:
The study was supported by an investigator-initiated research grant from Theratechnologies. Wong has received funding for his institution from Gilead Sciences, Exact Sciences, and Durect Corporation and has served as a consultant for Gilead Sciences.
A version of this article appeared on Medscape.com.
TOPLINE:
Metabolic dysfunction-associated steatotic liver disease (MASLD) co-occurring with HIV infection does not appear to increase the risk for cirrhosis or hepatocellular carcinoma (HCC) compared with MASLD alone. However, the incidence of major adverse cardiovascular events (MACE) is significantly increased among patients with MASLD and HIV, a large study suggested.
METHODOLOGY:
- MASLD is highly prevalent in people living with HIV, but the impact of HIV on liver and cardiovascular disease (CVD) outcomes in people with MASLD remains unclear.
- To investigate, researchers created a propensity score-matched cohort of veterans with noncirrhotic MASLD, with and without HIV (920 patients in each group).
- They evaluated the incidence of cirrhosis, HCC, and MACE, as well as overall survival, among the two groups. They also assessed these outcomes in MASLD patients with HIV on the basis of whether they were on antiretroviral therapy (ART).
TAKEAWAY:
- During a median follow-up of 10.4 years in the MASLD with HIV group and 11.8 years in the MASLD-only group, the overall incidence of cirrhosis and HCC was similar in MASLD with vs without HIV (cirrhosis: 0.97 vs 1.06 per 100 person-years, P = .54; HCC: 0.26 vs 0.17 per 100,000 person-years, P = .23), regardless of ART use.
- In contrast, the incidence of MACE was significantly higher in MASLD with vs without HIV (5.18 vs 4.48 per 100 person-years, P = .03). The incidence also was higher in patients with MASLD and HIV who were not on ART compared with those on ART (5.83 vs 4.7 per 100 person-years, P = .07).
- Compared with MASLD without HIV, the overall 5-year survival was significantly lower in MASLD with HIV (91.3% vs 85.7%). In MASLD with HIV, receipt of ART was associated with a significantly higher 5-year survival than no ART (87.4% vs 81.6%).
IN PRACTICE:
“Ensuring timely and appropriate initiation of HIV treatment is critical in patients with MASLD who have concurrent HIV infection, as well as optimizing metabolic comorbidities that may also contribute to increased risks of CVD and increased mortality,” the authors wrote.
SOURCE:
The study, led by Robert J. Wong, MD, Division of Gastroenterology and Hepatology, Stanford University School of Medicine, Palo Alto, California, was published online in the American Journal of Gastroenterology.
LIMITATIONS:
The study cohort consisted predominantly of older men, which may limit generalizability to women and younger populations. Metabolic comorbidities are more common in veterans compared with the general population, potentially affecting the generalizability of the CVD risk findings.
DISCLOSURES:
The study was supported by an investigator-initiated research grant from Theratechnologies. Wong has received funding for his institution from Gilead Sciences, Exact Sciences, and Durect Corporation and has served as a consultant for Gilead Sciences.
A version of this article appeared on Medscape.com.
Chronic Cribriform Ulcerated Plaque on the Left Calf
The Diagnosis: Nodular Basal Cell Carcinoma
Histopathology of the lesion showed a large basaloid lobule with focal epidermal attachment, peripheral nuclear palisading with cleft formation between the tumor and surrounding stroma, fibromyxoid stroma and mild pleomorphism, and variable mitotic activity and apoptosis (Figure). Based on the clinical presentation and histopathology, the patient was diagnosed with nodular basal cell carcinoma (BCC). He underwent a wide local excision of the affected area that was repaired with a splitthickness skin graft.
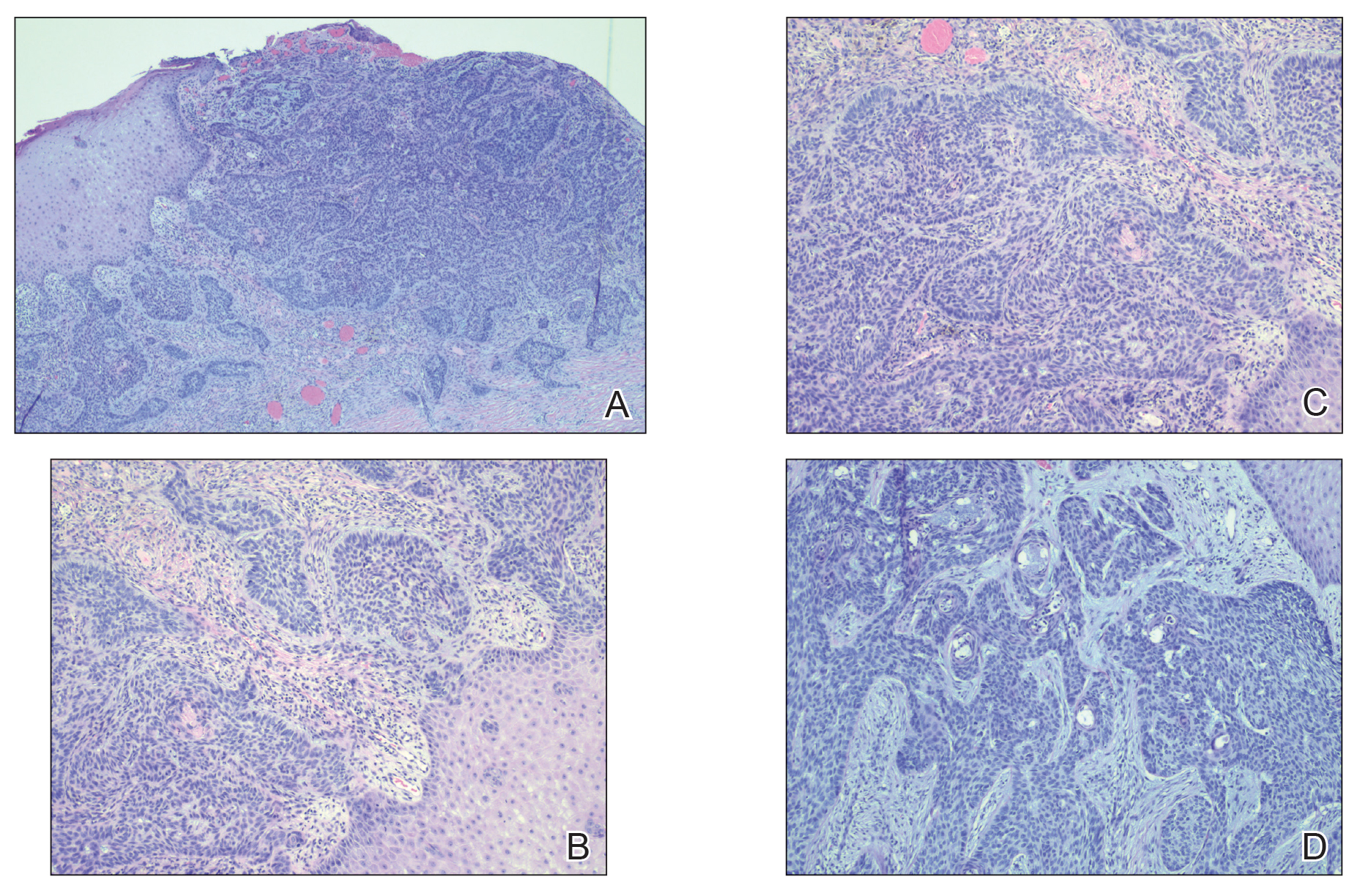
Basal cell carcinoma is the most common skin cancer worldwide and typically occurs due to years of UV radiation damage on sun-exposed skin, which accounts for a higher frequency of BCC occurring in patients residing in geographic locations with greater UV exposure (eg, higher and lower latitudes). In addition to cumulative UV dose, the duration of the exposure as well as its intensity also play a role in the development of BCC, particularly in early childhood and adolescence. Nevertheless, UV exposure is not the only risk factor, as 20% of BCCs arise in skin that is not exposed to the sun. Other risk factors include exposure to ionizing radiation and arsenic, immunosuppression, and genetic predisposition.1 Although these malignancies typically do not metastasize, growth can lead to local tissue destruction and major disfigurement if not treated in a timely fashion.2
In our patient, the differential diagnosis included pyoderma gangrenosum (PG) given the clinical appearance of the cribriform base and violaceous undermined rim of the ulcer. Pyoderma gangrenosum is a rare neutrophilic disorder that often results in ulcers that have been associated with various systemic autoimmune and inflammatory conditions, such as inflammatory bowel disease. There are 4 main subtypes of PG: the classic ulcerative type (our patient); the pustular type, which most often is seen in patients with inflammatory bowel disease; the bullous type, which can be seen in patients with an associated lymphoproliferative disorder; and the vegetative type. It frequently is thought of as both a clinical and histologic diagnosis of exclusion due to the nonspecific histopathologic features; most lesions demonstrate an infiltrate of neutrophils in the dermis. A biopsy was crucial in our patient, considering that diagnosis and treatment would have been further delayed had the patient been empirically treated with oral and topical steroids for presumed PG, which is precisely why PG is a diagnosis of exclusion. It is imperative for clinicians to rule out other pathologies, such as infection or malignancy, as demonstrated in our patient. The progressive onset and slow evolution of the lesion over years along with a lack of pain were more suggestive of BCC rather than PG. However, there is a report in the literature of PG mimicking BCC with both clinical and dermoscopic findings.3
Venous or stasis ulcers are painless, and although they rarely occur on the calf, they typically are seen lower on the leg such as on the medial ankles. Our patient endorsed occasional swelling of the affected leg and presented with edema, but overlying stasis change and other signs of venous insufficiency were absent.
Buruli ulcer is a painless chronic debilitating cutaneous disease resulting in indolent necrotizing skin as well as subcutaneous and bone lesions. It is caused by the environmental organism Mycobacterium ulcerans and typically is reported in Africa, Central/South America, the Western Pacific Region, and Australia.4 Histopathology usually demonstrates necrosis of subcutaneous tissue and dermal collagen accompanied by inflammation and acidfast bacilli highlighted by Ziehl-Neelsen stain.5 Smears of the lesions as well as culture and polymerase chain reaction for acid-fast bacilli also can be performed. Our patient reported no recent travel to any endemic areas and had no other risk factors or exposures to the pathogen responsible for this condition.
Traumatic ulcer also was included in the differential diagnosis, but the patient denied preceding trauma to the area, and the contralateral foot prosthesis did not rub on or impact the affected leg.
Basal cell carcinoma typically is treated surgically, but choice of treatment can depend on the subtype, size, tumor site, and/or patient preference.1 Other treatment modalities include electrodesiccation and curettage, cryosurgical destruction, photodynamic therapy, radiation, topical therapies, and systemic medications. Radiotherapy can be considered as a primary treatment option for BCC if surgery is contraindicated or declined by the patient, but it also is useful as an adjuvant therapy when there is perineural invasion of the tumor or positive margins. Hedgehog pathway inhibitors such as vismodegib currently are indicated for patients who are not candidates for surgery or radiation as well as for those with metastatic or locally advanced, recurrent BCC. There is no single treatment method ideal for every lesion or patient. Specific populations such as the elderly, the immunosuppressed, or those with poor baseline functional status may warrant a nonsurgical approach. The clinician must take into consideration all factors while at the same time thinking about how to best accomplish the goals of recurrencefree tumor removal, correction of any underlying functional impairment from the tumor, and maintenance of cosmesis.1
- McDaniel B, Badri T, Steele RB. Basal cell carcinoma. In: StatPearls. StatPearls; 2022.
- Marzuka AG, Book SE. Basal cell carcinoma: pathogenesis, epidemiology, clinical features, diagnosis, histopathology, and management. Yale J Biol Med. 2015;88:167-179.
- Rosina P, Papagrigoraki A, Colato C. A case of superficial granulomatous pyoderma mimicking a basal cell carcinoma. Acta Dermatovenerol Croat. 2014;22:48-51.
- Yotsu RR, Suzuki K, Simmonds RE, et al. Buruli ulcer: a review of the current knowledge. Curr Trop Med Rep. 2018;5:247-256.
- Guarner J, Bartlett J, Whitney EA, et al. Histopathologic features of Mycobacterium ulcerans infection. Emerg Infect Dis. 2003;9:651-656.
The Diagnosis: Nodular Basal Cell Carcinoma
Histopathology of the lesion showed a large basaloid lobule with focal epidermal attachment, peripheral nuclear palisading with cleft formation between the tumor and surrounding stroma, fibromyxoid stroma and mild pleomorphism, and variable mitotic activity and apoptosis (Figure). Based on the clinical presentation and histopathology, the patient was diagnosed with nodular basal cell carcinoma (BCC). He underwent a wide local excision of the affected area that was repaired with a splitthickness skin graft.
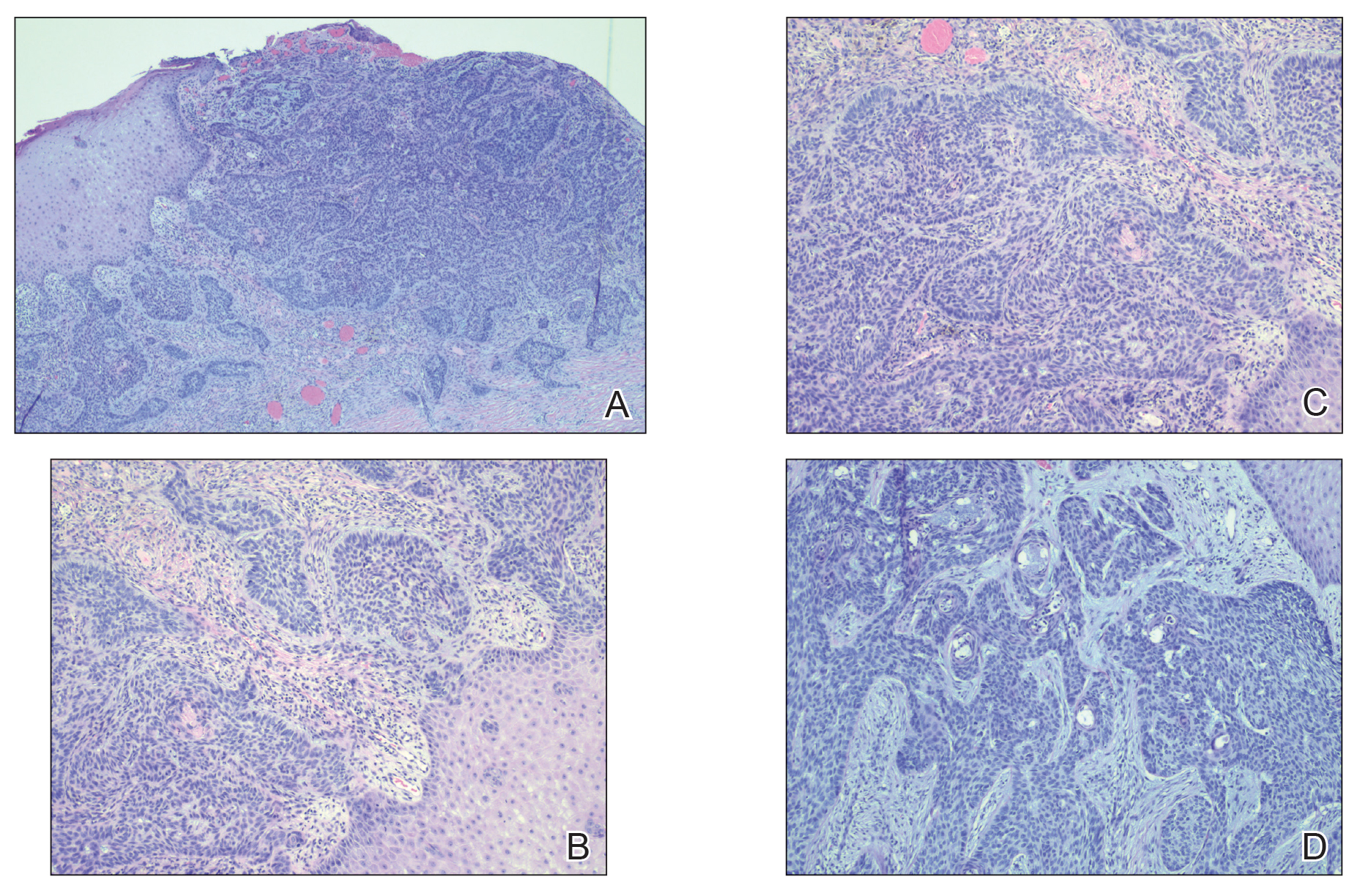
Basal cell carcinoma is the most common skin cancer worldwide and typically occurs due to years of UV radiation damage on sun-exposed skin, which accounts for a higher frequency of BCC occurring in patients residing in geographic locations with greater UV exposure (eg, higher and lower latitudes). In addition to cumulative UV dose, the duration of the exposure as well as its intensity also play a role in the development of BCC, particularly in early childhood and adolescence. Nevertheless, UV exposure is not the only risk factor, as 20% of BCCs arise in skin that is not exposed to the sun. Other risk factors include exposure to ionizing radiation and arsenic, immunosuppression, and genetic predisposition.1 Although these malignancies typically do not metastasize, growth can lead to local tissue destruction and major disfigurement if not treated in a timely fashion.2
In our patient, the differential diagnosis included pyoderma gangrenosum (PG) given the clinical appearance of the cribriform base and violaceous undermined rim of the ulcer. Pyoderma gangrenosum is a rare neutrophilic disorder that often results in ulcers that have been associated with various systemic autoimmune and inflammatory conditions, such as inflammatory bowel disease. There are 4 main subtypes of PG: the classic ulcerative type (our patient); the pustular type, which most often is seen in patients with inflammatory bowel disease; the bullous type, which can be seen in patients with an associated lymphoproliferative disorder; and the vegetative type. It frequently is thought of as both a clinical and histologic diagnosis of exclusion due to the nonspecific histopathologic features; most lesions demonstrate an infiltrate of neutrophils in the dermis. A biopsy was crucial in our patient, considering that diagnosis and treatment would have been further delayed had the patient been empirically treated with oral and topical steroids for presumed PG, which is precisely why PG is a diagnosis of exclusion. It is imperative for clinicians to rule out other pathologies, such as infection or malignancy, as demonstrated in our patient. The progressive onset and slow evolution of the lesion over years along with a lack of pain were more suggestive of BCC rather than PG. However, there is a report in the literature of PG mimicking BCC with both clinical and dermoscopic findings.3
Venous or stasis ulcers are painless, and although they rarely occur on the calf, they typically are seen lower on the leg such as on the medial ankles. Our patient endorsed occasional swelling of the affected leg and presented with edema, but overlying stasis change and other signs of venous insufficiency were absent.
Buruli ulcer is a painless chronic debilitating cutaneous disease resulting in indolent necrotizing skin as well as subcutaneous and bone lesions. It is caused by the environmental organism Mycobacterium ulcerans and typically is reported in Africa, Central/South America, the Western Pacific Region, and Australia.4 Histopathology usually demonstrates necrosis of subcutaneous tissue and dermal collagen accompanied by inflammation and acidfast bacilli highlighted by Ziehl-Neelsen stain.5 Smears of the lesions as well as culture and polymerase chain reaction for acid-fast bacilli also can be performed. Our patient reported no recent travel to any endemic areas and had no other risk factors or exposures to the pathogen responsible for this condition.
Traumatic ulcer also was included in the differential diagnosis, but the patient denied preceding trauma to the area, and the contralateral foot prosthesis did not rub on or impact the affected leg.
Basal cell carcinoma typically is treated surgically, but choice of treatment can depend on the subtype, size, tumor site, and/or patient preference.1 Other treatment modalities include electrodesiccation and curettage, cryosurgical destruction, photodynamic therapy, radiation, topical therapies, and systemic medications. Radiotherapy can be considered as a primary treatment option for BCC if surgery is contraindicated or declined by the patient, but it also is useful as an adjuvant therapy when there is perineural invasion of the tumor or positive margins. Hedgehog pathway inhibitors such as vismodegib currently are indicated for patients who are not candidates for surgery or radiation as well as for those with metastatic or locally advanced, recurrent BCC. There is no single treatment method ideal for every lesion or patient. Specific populations such as the elderly, the immunosuppressed, or those with poor baseline functional status may warrant a nonsurgical approach. The clinician must take into consideration all factors while at the same time thinking about how to best accomplish the goals of recurrencefree tumor removal, correction of any underlying functional impairment from the tumor, and maintenance of cosmesis.1
The Diagnosis: Nodular Basal Cell Carcinoma
Histopathology of the lesion showed a large basaloid lobule with focal epidermal attachment, peripheral nuclear palisading with cleft formation between the tumor and surrounding stroma, fibromyxoid stroma and mild pleomorphism, and variable mitotic activity and apoptosis (Figure). Based on the clinical presentation and histopathology, the patient was diagnosed with nodular basal cell carcinoma (BCC). He underwent a wide local excision of the affected area that was repaired with a splitthickness skin graft.
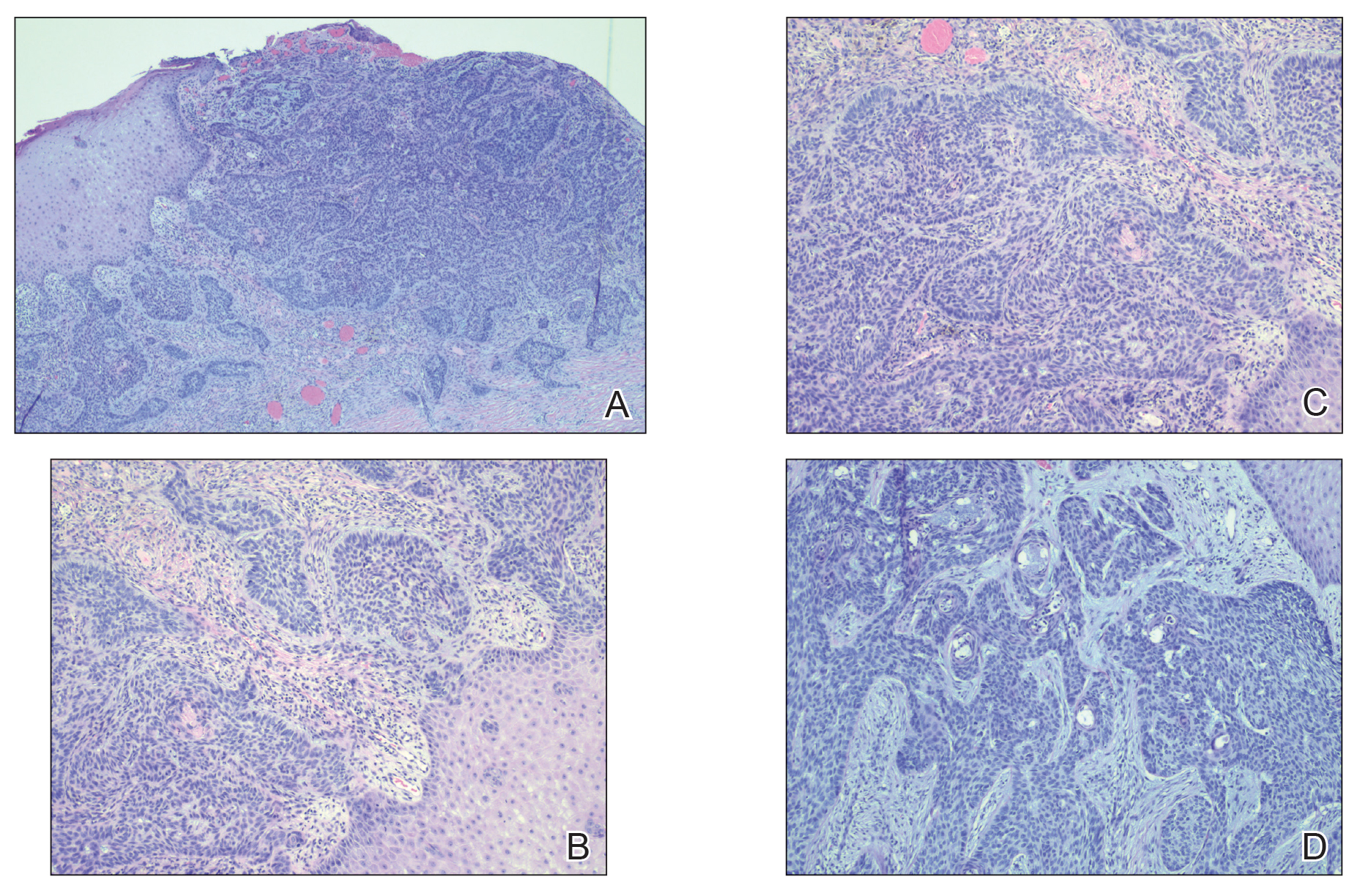
Basal cell carcinoma is the most common skin cancer worldwide and typically occurs due to years of UV radiation damage on sun-exposed skin, which accounts for a higher frequency of BCC occurring in patients residing in geographic locations with greater UV exposure (eg, higher and lower latitudes). In addition to cumulative UV dose, the duration of the exposure as well as its intensity also play a role in the development of BCC, particularly in early childhood and adolescence. Nevertheless, UV exposure is not the only risk factor, as 20% of BCCs arise in skin that is not exposed to the sun. Other risk factors include exposure to ionizing radiation and arsenic, immunosuppression, and genetic predisposition.1 Although these malignancies typically do not metastasize, growth can lead to local tissue destruction and major disfigurement if not treated in a timely fashion.2
In our patient, the differential diagnosis included pyoderma gangrenosum (PG) given the clinical appearance of the cribriform base and violaceous undermined rim of the ulcer. Pyoderma gangrenosum is a rare neutrophilic disorder that often results in ulcers that have been associated with various systemic autoimmune and inflammatory conditions, such as inflammatory bowel disease. There are 4 main subtypes of PG: the classic ulcerative type (our patient); the pustular type, which most often is seen in patients with inflammatory bowel disease; the bullous type, which can be seen in patients with an associated lymphoproliferative disorder; and the vegetative type. It frequently is thought of as both a clinical and histologic diagnosis of exclusion due to the nonspecific histopathologic features; most lesions demonstrate an infiltrate of neutrophils in the dermis. A biopsy was crucial in our patient, considering that diagnosis and treatment would have been further delayed had the patient been empirically treated with oral and topical steroids for presumed PG, which is precisely why PG is a diagnosis of exclusion. It is imperative for clinicians to rule out other pathologies, such as infection or malignancy, as demonstrated in our patient. The progressive onset and slow evolution of the lesion over years along with a lack of pain were more suggestive of BCC rather than PG. However, there is a report in the literature of PG mimicking BCC with both clinical and dermoscopic findings.3
Venous or stasis ulcers are painless, and although they rarely occur on the calf, they typically are seen lower on the leg such as on the medial ankles. Our patient endorsed occasional swelling of the affected leg and presented with edema, but overlying stasis change and other signs of venous insufficiency were absent.
Buruli ulcer is a painless chronic debilitating cutaneous disease resulting in indolent necrotizing skin as well as subcutaneous and bone lesions. It is caused by the environmental organism Mycobacterium ulcerans and typically is reported in Africa, Central/South America, the Western Pacific Region, and Australia.4 Histopathology usually demonstrates necrosis of subcutaneous tissue and dermal collagen accompanied by inflammation and acidfast bacilli highlighted by Ziehl-Neelsen stain.5 Smears of the lesions as well as culture and polymerase chain reaction for acid-fast bacilli also can be performed. Our patient reported no recent travel to any endemic areas and had no other risk factors or exposures to the pathogen responsible for this condition.
Traumatic ulcer also was included in the differential diagnosis, but the patient denied preceding trauma to the area, and the contralateral foot prosthesis did not rub on or impact the affected leg.
Basal cell carcinoma typically is treated surgically, but choice of treatment can depend on the subtype, size, tumor site, and/or patient preference.1 Other treatment modalities include electrodesiccation and curettage, cryosurgical destruction, photodynamic therapy, radiation, topical therapies, and systemic medications. Radiotherapy can be considered as a primary treatment option for BCC if surgery is contraindicated or declined by the patient, but it also is useful as an adjuvant therapy when there is perineural invasion of the tumor or positive margins. Hedgehog pathway inhibitors such as vismodegib currently are indicated for patients who are not candidates for surgery or radiation as well as for those with metastatic or locally advanced, recurrent BCC. There is no single treatment method ideal for every lesion or patient. Specific populations such as the elderly, the immunosuppressed, or those with poor baseline functional status may warrant a nonsurgical approach. The clinician must take into consideration all factors while at the same time thinking about how to best accomplish the goals of recurrencefree tumor removal, correction of any underlying functional impairment from the tumor, and maintenance of cosmesis.1
- McDaniel B, Badri T, Steele RB. Basal cell carcinoma. In: StatPearls. StatPearls; 2022.
- Marzuka AG, Book SE. Basal cell carcinoma: pathogenesis, epidemiology, clinical features, diagnosis, histopathology, and management. Yale J Biol Med. 2015;88:167-179.
- Rosina P, Papagrigoraki A, Colato C. A case of superficial granulomatous pyoderma mimicking a basal cell carcinoma. Acta Dermatovenerol Croat. 2014;22:48-51.
- Yotsu RR, Suzuki K, Simmonds RE, et al. Buruli ulcer: a review of the current knowledge. Curr Trop Med Rep. 2018;5:247-256.
- Guarner J, Bartlett J, Whitney EA, et al. Histopathologic features of Mycobacterium ulcerans infection. Emerg Infect Dis. 2003;9:651-656.
- McDaniel B, Badri T, Steele RB. Basal cell carcinoma. In: StatPearls. StatPearls; 2022.
- Marzuka AG, Book SE. Basal cell carcinoma: pathogenesis, epidemiology, clinical features, diagnosis, histopathology, and management. Yale J Biol Med. 2015;88:167-179.
- Rosina P, Papagrigoraki A, Colato C. A case of superficial granulomatous pyoderma mimicking a basal cell carcinoma. Acta Dermatovenerol Croat. 2014;22:48-51.
- Yotsu RR, Suzuki K, Simmonds RE, et al. Buruli ulcer: a review of the current knowledge. Curr Trop Med Rep. 2018;5:247-256.
- Guarner J, Bartlett J, Whitney EA, et al. Histopathologic features of Mycobacterium ulcerans infection. Emerg Infect Dis. 2003;9:651-656.
A 61-year-old man presented to the dermatology clinic for evaluation of a painless nonhealing wound on the left calf of 4 years’ duration. The patient had a history of amputation of the right foot as an infant, for which he wore an orthopedic prosthesis. He also had chronic lymphedema of the left leg, hyperlipidemia, and osteoarthritis of the right hip. There was no history of gastrointestinal tract issues. The lesion initially was small, then grew and began to ulcerate and bleed. His presentation to dermatology was delayed due to office closures during the COVID-19 pandemic. Physical examination revealed a 5-cm, erythematous, cribriform ulcer with a violaceous undermined rim. A punch biopsy was performed on the edge of the ulcer.

Could Aspirin Help Treat Breast Cancer?
These data are more robust than the efficacy signals from previous studies, meaning healthcare providers should not recommend aspirin as adjuvant therapy for breast cancer, reported lead author Wendy Y. Chen, MD, of Dana Farber Cancer Institute, Boston, and colleagues.
What Data Support Aspirin for Treating Breast Cancer?
“Multiple observational studies have reported a decreased risk of death among survivors of breast cancer who were regular aspirin users,” the investigators wrote in JAMA. “Even more compelling were data from randomized trials of aspirin for cardiovascular disease.”
This possible benefit was reported with mechanistic support, as aspirin’s anti-inflammatory and anti-platelet properties could theoretically control tumor growth, they added. Furthermore, aspirin impacts several cancer pathways currently targeted by agents approved by the US Food and Drug Administration (FDA).
“Collectively, evidence from laboratory and epidemiologic studies and randomized trials strongly suggested a role for aspirin to improve breast cancer outcomes, leading to [this new study, Alliance for Clinical Trials in Oncology (Alliance) A011502,] which, to our knowledge, is the first randomized, placebo-controlled trial of aspirin to report results among survivors of breast cancer,” Dr. Chen and colleagues wrote.
What Were The Key Findings From The A011502 Trial?
The A011502 trial enrolled 3,020 patients aged 18-70 years with ERBB2-negative breast cancer who had received standard therapy via routine clinical care. Eligibility required that chemotherapy and local therapy were complete, but ongoing endocrine therapy was allowed.
Participants were randomized in a 1:1 ratio to receive aspirin 300 mg per day or matching placebo for 5 years. The primary outcome was invasive disease-free survival, and the key secondary outcome was overall survival.
After a median follow-up of almost 3 years, at the first interim analysis, the study was suspended early due to statistical futility. By that timepoint, 253 invasive disease-free survival events occurred, of which 141 occurred in the aspirin group, compared with 112 in the placebo group, providing a hazard ratio of 1.27 (95% CI, 0.99-1.63) that was not statistically significant (P = .06). No statistically significant difference in overall survival was observed (hazard ratio, 1.19; 95% CI, 0.82-1.72). Safety profiles were similar across groups.
How Will This Study Change Practice?
In an accompanying editorial, Jeanne S. Mandelblatt, MD, of Georgetown Lombardi Institute for Cancer and Aging Research, Washington, and colleagues, praised the trial for its comprehensive approach, but they predicted that the negative result could spell friction for health care providers.
“[C]linicians may find it challenging to communicate with their patients about the negative result in the Alliance trial, because prior lay press articles, observational studies, and meta-analyses of cardiovascular trials suggested that aspirin may decrease breast cancer recurrence,” they wrote.
Dr. Mandelblatt and colleagues went on to explore broader implications beyond breast cancer, including considerations for communication of negative results in other medical specialties, discussions between clinicians and patients regarding aspirin use for non–breast cancer purposes, and questions about the timing of aspirin use and the role of age and biological aging.
How Might the Findings From the A011502 Trial Impact Future Research?
Finally, and “most critically,” the editorialists raised concerns about health equity, noting the limited diversity in trial participants and the potential exclusion of subgroups that might benefit from aspirin use, particularly those more likely to experience accelerated biological aging and disparities in cancer risk and outcomes due to systemic racism or adverse social determinants of health.
They concluded by emphasizing the need to consider the intersectionality of aging, cancer, and disparities in designing future trials to advance health equity.
This study was funded by the Department of Defense Breast Cancer Research Program and the National Cancer Institute of the National Institutes of Health. The research was also supported in part by Bayer, which provided the study drug. The investigators disclosed relationships with Novartis, Seagen, Orum Clinical, and others. The editorialists disclosed relationships with Cantex Pharmaceuticals, and Pfizer.
These data are more robust than the efficacy signals from previous studies, meaning healthcare providers should not recommend aspirin as adjuvant therapy for breast cancer, reported lead author Wendy Y. Chen, MD, of Dana Farber Cancer Institute, Boston, and colleagues.
What Data Support Aspirin for Treating Breast Cancer?
“Multiple observational studies have reported a decreased risk of death among survivors of breast cancer who were regular aspirin users,” the investigators wrote in JAMA. “Even more compelling were data from randomized trials of aspirin for cardiovascular disease.”
This possible benefit was reported with mechanistic support, as aspirin’s anti-inflammatory and anti-platelet properties could theoretically control tumor growth, they added. Furthermore, aspirin impacts several cancer pathways currently targeted by agents approved by the US Food and Drug Administration (FDA).
“Collectively, evidence from laboratory and epidemiologic studies and randomized trials strongly suggested a role for aspirin to improve breast cancer outcomes, leading to [this new study, Alliance for Clinical Trials in Oncology (Alliance) A011502,] which, to our knowledge, is the first randomized, placebo-controlled trial of aspirin to report results among survivors of breast cancer,” Dr. Chen and colleagues wrote.
What Were The Key Findings From The A011502 Trial?
The A011502 trial enrolled 3,020 patients aged 18-70 years with ERBB2-negative breast cancer who had received standard therapy via routine clinical care. Eligibility required that chemotherapy and local therapy were complete, but ongoing endocrine therapy was allowed.
Participants were randomized in a 1:1 ratio to receive aspirin 300 mg per day or matching placebo for 5 years. The primary outcome was invasive disease-free survival, and the key secondary outcome was overall survival.
After a median follow-up of almost 3 years, at the first interim analysis, the study was suspended early due to statistical futility. By that timepoint, 253 invasive disease-free survival events occurred, of which 141 occurred in the aspirin group, compared with 112 in the placebo group, providing a hazard ratio of 1.27 (95% CI, 0.99-1.63) that was not statistically significant (P = .06). No statistically significant difference in overall survival was observed (hazard ratio, 1.19; 95% CI, 0.82-1.72). Safety profiles were similar across groups.
How Will This Study Change Practice?
In an accompanying editorial, Jeanne S. Mandelblatt, MD, of Georgetown Lombardi Institute for Cancer and Aging Research, Washington, and colleagues, praised the trial for its comprehensive approach, but they predicted that the negative result could spell friction for health care providers.
“[C]linicians may find it challenging to communicate with their patients about the negative result in the Alliance trial, because prior lay press articles, observational studies, and meta-analyses of cardiovascular trials suggested that aspirin may decrease breast cancer recurrence,” they wrote.
Dr. Mandelblatt and colleagues went on to explore broader implications beyond breast cancer, including considerations for communication of negative results in other medical specialties, discussions between clinicians and patients regarding aspirin use for non–breast cancer purposes, and questions about the timing of aspirin use and the role of age and biological aging.
How Might the Findings From the A011502 Trial Impact Future Research?
Finally, and “most critically,” the editorialists raised concerns about health equity, noting the limited diversity in trial participants and the potential exclusion of subgroups that might benefit from aspirin use, particularly those more likely to experience accelerated biological aging and disparities in cancer risk and outcomes due to systemic racism or adverse social determinants of health.
They concluded by emphasizing the need to consider the intersectionality of aging, cancer, and disparities in designing future trials to advance health equity.
This study was funded by the Department of Defense Breast Cancer Research Program and the National Cancer Institute of the National Institutes of Health. The research was also supported in part by Bayer, which provided the study drug. The investigators disclosed relationships with Novartis, Seagen, Orum Clinical, and others. The editorialists disclosed relationships with Cantex Pharmaceuticals, and Pfizer.
These data are more robust than the efficacy signals from previous studies, meaning healthcare providers should not recommend aspirin as adjuvant therapy for breast cancer, reported lead author Wendy Y. Chen, MD, of Dana Farber Cancer Institute, Boston, and colleagues.
What Data Support Aspirin for Treating Breast Cancer?
“Multiple observational studies have reported a decreased risk of death among survivors of breast cancer who were regular aspirin users,” the investigators wrote in JAMA. “Even more compelling were data from randomized trials of aspirin for cardiovascular disease.”
This possible benefit was reported with mechanistic support, as aspirin’s anti-inflammatory and anti-platelet properties could theoretically control tumor growth, they added. Furthermore, aspirin impacts several cancer pathways currently targeted by agents approved by the US Food and Drug Administration (FDA).
“Collectively, evidence from laboratory and epidemiologic studies and randomized trials strongly suggested a role for aspirin to improve breast cancer outcomes, leading to [this new study, Alliance for Clinical Trials in Oncology (Alliance) A011502,] which, to our knowledge, is the first randomized, placebo-controlled trial of aspirin to report results among survivors of breast cancer,” Dr. Chen and colleagues wrote.
What Were The Key Findings From The A011502 Trial?
The A011502 trial enrolled 3,020 patients aged 18-70 years with ERBB2-negative breast cancer who had received standard therapy via routine clinical care. Eligibility required that chemotherapy and local therapy were complete, but ongoing endocrine therapy was allowed.
Participants were randomized in a 1:1 ratio to receive aspirin 300 mg per day or matching placebo for 5 years. The primary outcome was invasive disease-free survival, and the key secondary outcome was overall survival.
After a median follow-up of almost 3 years, at the first interim analysis, the study was suspended early due to statistical futility. By that timepoint, 253 invasive disease-free survival events occurred, of which 141 occurred in the aspirin group, compared with 112 in the placebo group, providing a hazard ratio of 1.27 (95% CI, 0.99-1.63) that was not statistically significant (P = .06). No statistically significant difference in overall survival was observed (hazard ratio, 1.19; 95% CI, 0.82-1.72). Safety profiles were similar across groups.
How Will This Study Change Practice?
In an accompanying editorial, Jeanne S. Mandelblatt, MD, of Georgetown Lombardi Institute for Cancer and Aging Research, Washington, and colleagues, praised the trial for its comprehensive approach, but they predicted that the negative result could spell friction for health care providers.
“[C]linicians may find it challenging to communicate with their patients about the negative result in the Alliance trial, because prior lay press articles, observational studies, and meta-analyses of cardiovascular trials suggested that aspirin may decrease breast cancer recurrence,” they wrote.
Dr. Mandelblatt and colleagues went on to explore broader implications beyond breast cancer, including considerations for communication of negative results in other medical specialties, discussions between clinicians and patients regarding aspirin use for non–breast cancer purposes, and questions about the timing of aspirin use and the role of age and biological aging.
How Might the Findings From the A011502 Trial Impact Future Research?
Finally, and “most critically,” the editorialists raised concerns about health equity, noting the limited diversity in trial participants and the potential exclusion of subgroups that might benefit from aspirin use, particularly those more likely to experience accelerated biological aging and disparities in cancer risk and outcomes due to systemic racism or adverse social determinants of health.
They concluded by emphasizing the need to consider the intersectionality of aging, cancer, and disparities in designing future trials to advance health equity.
This study was funded by the Department of Defense Breast Cancer Research Program and the National Cancer Institute of the National Institutes of Health. The research was also supported in part by Bayer, which provided the study drug. The investigators disclosed relationships with Novartis, Seagen, Orum Clinical, and others. The editorialists disclosed relationships with Cantex Pharmaceuticals, and Pfizer.
FROM JAMA
Optimized Hospital Care for Gout Improves Uptake of Urate-Lowering Therapy
LIVERPOOL, ENGLAND — Optimizing how people experiencing a gout flare are managed in hospital and then followed-up afterwards can substantially increase the uptake of guideline-recommended urate-lowering therapy (ULT), researchers reported at the annual meeting of the British Society for Rheumatology (BSR).
In a prospective study, 92% of 97 people admitted to hospital for gout flares were using ULT within 6 months of discharge after a multifaceted intervention was introduced. By comparison, 49% of 94 people admitted for gout flares before the introduction of the intervention were taking ULT within the same postdischarge time frame.
Moreover, a higher proportion of individuals had urate blood tests done at least once within the 6-month postdischarge period after the intervention’s introduction (58% vs 32%) and fewer (9% vs 15%) needed repeated hospital treatment.
“Gout is the most common inflammatory arthritis affecting one in 30 adults in the United Kingdom, yet it’s one of the most poorly managed,” study investigator Mark D. Russell, MB, BChir, pointed out during a poster presentation.
“There are very effective treatments,” added Dr. Russell, a rheumatology registrar and postdoctoral research fellow at King’s College London in London, England. “Urate-lowering therapies such as allopurinol, which when taken at the correct dose, in the long term, effectively cures patients of their symptoms and prevents complications.”
Dr. Russell said in an interview that there was still work to be done as the rate of people achieving urate levels below the recommended threshold of 360 micromol/L (6 mg/dL) within 6 months was still low, at 27%, even it if was still better than the 11% seen before the intervention was introduced.
Improving the In- and Post-Hospital Pathway
“We developed and implemented an in-hospital management pathway which encouraged urate-lowering therapy initiation prior to discharge, followed by a post-discharge nurse-led review,” Dr. Russell explained.
The in-hospital pathway was based upon BSR, European Alliance of Associations for Rheumatology, and American College of Rheumatology guidelines and involved diagnosing and managing the gout flare appropriately. This may have been via early joint aspiration, medication, or both, as directed by the rheumatology team. Affected individuals also received education and were directed where to obtain further information on the use of ULT. Outpatient follow-up was considered if an individual had severe or tophaceous gout, recurrent episodes, or contraindications or intolerances to ULT. Otherwise, a rheumatology nurse telephoned the individual 2 weeks later to review symptoms and discuss next steps.
The researchers recorded improvements in in-hospital outcomes. The frequency of in-hospital serum urate level measurements rose from 66% in the 12-month preimplementation period to 93% in the 12-month period after the intervention’s introduction. Almost two thirds (62%) of patients were discharged on ULT compared with 18% preimplementation. And gout-specific recommendations were given 86% of the time compared with 59% before the intervention.
Related Work on Gout Incidence
Separately, Dr. Russell also presented data from a nationwide, population-level cohort study that used data from OpenSAFELY, the secure data analytics platform used by the National Health Service in England.
“We did an analysis previously using the CPRD [Clinical Research Practice Datalink], which is another good primary care database, showing that only a third of people with gout in the UK get urate-lowering drugs, when really it should be the vast majority,” he said in the interview.
“And then we wanted to look at, on top of that, what was the impact of the [COVID-19] pandemic,” Russell added. Specifically, the aim was to look at how the pandemic had affected the incidence, management, and prevalence of gout.
Between March 2015 and February 2023, 246,695 new cases of gout were identified among 17.9 million adults, seen in primary and secondary care.
COVID-19 Pandemic Affected Cases
“The number of new cases of gout dropped by about one third in the first year of the pandemic,” Dr. Russell said. Incidence declined from 1.78 to 1.23 per 1000 adults. “Whether that was through people not feeling comfortable going to their GP [general practitioner] or not being able to get an appointment, we don’t know.”
While there was a subsequent increase in new cases of gout since this time, the rates still haven’t reached what they were before the pandemic. This implies that there could be a substantial number of people who may be undiagnosed because of the pandemic, Dr. Russell suggested.
Moreover, he reported that in 2022-2023, the prevalence of gout was 3.21%, up slightly from the 3.07% recorded 7 years earlier in 2015-2016.
ULT Treatment Rates Low
“If you did see a GP, however, so as long as you saw someone, the treatment wasn’t any worse,” Dr. Russell said. Just under 30% of people with incident gout for whom follow-up data were available had initiated ULT within 6 months of their diagnosis. And, of these new starters, around a quarter had a serum urate level below a target of 360 micromol/L.
“This doesn’t detract from the fact that this is pretty low. Despite guidelines, we’re still not getting the majority of people on these very effective urate-lowering drugs,” Dr. Russell said.
There is perhaps too much reliance on modifying diet and lifestyle, he added, which are important for many reasons but will not do much to lower blood urate levels.
As a final word, Dr. Russell said, “It’s not just a case of preventing a bit of joint pain. People get lots of complications when they’re undertreated — erosive joint damage, work disability, impaired quality of life — and yet we’ve got very cheap, well-tolerated drugs.”
The work was independently funded. Dr. Russell acknowledged grant or research support from Eli Lilly, Janssen, Pfizer, and UCB and receipt of honoraria from AbbVie, Biogen, Eli Lilly, Galapagos, and Menarini.
A version of this article appeared on Medscape.com.
LIVERPOOL, ENGLAND — Optimizing how people experiencing a gout flare are managed in hospital and then followed-up afterwards can substantially increase the uptake of guideline-recommended urate-lowering therapy (ULT), researchers reported at the annual meeting of the British Society for Rheumatology (BSR).
In a prospective study, 92% of 97 people admitted to hospital for gout flares were using ULT within 6 months of discharge after a multifaceted intervention was introduced. By comparison, 49% of 94 people admitted for gout flares before the introduction of the intervention were taking ULT within the same postdischarge time frame.
Moreover, a higher proportion of individuals had urate blood tests done at least once within the 6-month postdischarge period after the intervention’s introduction (58% vs 32%) and fewer (9% vs 15%) needed repeated hospital treatment.
“Gout is the most common inflammatory arthritis affecting one in 30 adults in the United Kingdom, yet it’s one of the most poorly managed,” study investigator Mark D. Russell, MB, BChir, pointed out during a poster presentation.
“There are very effective treatments,” added Dr. Russell, a rheumatology registrar and postdoctoral research fellow at King’s College London in London, England. “Urate-lowering therapies such as allopurinol, which when taken at the correct dose, in the long term, effectively cures patients of their symptoms and prevents complications.”
Dr. Russell said in an interview that there was still work to be done as the rate of people achieving urate levels below the recommended threshold of 360 micromol/L (6 mg/dL) within 6 months was still low, at 27%, even it if was still better than the 11% seen before the intervention was introduced.
Improving the In- and Post-Hospital Pathway
“We developed and implemented an in-hospital management pathway which encouraged urate-lowering therapy initiation prior to discharge, followed by a post-discharge nurse-led review,” Dr. Russell explained.
The in-hospital pathway was based upon BSR, European Alliance of Associations for Rheumatology, and American College of Rheumatology guidelines and involved diagnosing and managing the gout flare appropriately. This may have been via early joint aspiration, medication, or both, as directed by the rheumatology team. Affected individuals also received education and were directed where to obtain further information on the use of ULT. Outpatient follow-up was considered if an individual had severe or tophaceous gout, recurrent episodes, or contraindications or intolerances to ULT. Otherwise, a rheumatology nurse telephoned the individual 2 weeks later to review symptoms and discuss next steps.
The researchers recorded improvements in in-hospital outcomes. The frequency of in-hospital serum urate level measurements rose from 66% in the 12-month preimplementation period to 93% in the 12-month period after the intervention’s introduction. Almost two thirds (62%) of patients were discharged on ULT compared with 18% preimplementation. And gout-specific recommendations were given 86% of the time compared with 59% before the intervention.
Related Work on Gout Incidence
Separately, Dr. Russell also presented data from a nationwide, population-level cohort study that used data from OpenSAFELY, the secure data analytics platform used by the National Health Service in England.
“We did an analysis previously using the CPRD [Clinical Research Practice Datalink], which is another good primary care database, showing that only a third of people with gout in the UK get urate-lowering drugs, when really it should be the vast majority,” he said in the interview.
“And then we wanted to look at, on top of that, what was the impact of the [COVID-19] pandemic,” Russell added. Specifically, the aim was to look at how the pandemic had affected the incidence, management, and prevalence of gout.
Between March 2015 and February 2023, 246,695 new cases of gout were identified among 17.9 million adults, seen in primary and secondary care.
COVID-19 Pandemic Affected Cases
“The number of new cases of gout dropped by about one third in the first year of the pandemic,” Dr. Russell said. Incidence declined from 1.78 to 1.23 per 1000 adults. “Whether that was through people not feeling comfortable going to their GP [general practitioner] or not being able to get an appointment, we don’t know.”
While there was a subsequent increase in new cases of gout since this time, the rates still haven’t reached what they were before the pandemic. This implies that there could be a substantial number of people who may be undiagnosed because of the pandemic, Dr. Russell suggested.
Moreover, he reported that in 2022-2023, the prevalence of gout was 3.21%, up slightly from the 3.07% recorded 7 years earlier in 2015-2016.
ULT Treatment Rates Low
“If you did see a GP, however, so as long as you saw someone, the treatment wasn’t any worse,” Dr. Russell said. Just under 30% of people with incident gout for whom follow-up data were available had initiated ULT within 6 months of their diagnosis. And, of these new starters, around a quarter had a serum urate level below a target of 360 micromol/L.
“This doesn’t detract from the fact that this is pretty low. Despite guidelines, we’re still not getting the majority of people on these very effective urate-lowering drugs,” Dr. Russell said.
There is perhaps too much reliance on modifying diet and lifestyle, he added, which are important for many reasons but will not do much to lower blood urate levels.
As a final word, Dr. Russell said, “It’s not just a case of preventing a bit of joint pain. People get lots of complications when they’re undertreated — erosive joint damage, work disability, impaired quality of life — and yet we’ve got very cheap, well-tolerated drugs.”
The work was independently funded. Dr. Russell acknowledged grant or research support from Eli Lilly, Janssen, Pfizer, and UCB and receipt of honoraria from AbbVie, Biogen, Eli Lilly, Galapagos, and Menarini.
A version of this article appeared on Medscape.com.
LIVERPOOL, ENGLAND — Optimizing how people experiencing a gout flare are managed in hospital and then followed-up afterwards can substantially increase the uptake of guideline-recommended urate-lowering therapy (ULT), researchers reported at the annual meeting of the British Society for Rheumatology (BSR).
In a prospective study, 92% of 97 people admitted to hospital for gout flares were using ULT within 6 months of discharge after a multifaceted intervention was introduced. By comparison, 49% of 94 people admitted for gout flares before the introduction of the intervention were taking ULT within the same postdischarge time frame.
Moreover, a higher proportion of individuals had urate blood tests done at least once within the 6-month postdischarge period after the intervention’s introduction (58% vs 32%) and fewer (9% vs 15%) needed repeated hospital treatment.
“Gout is the most common inflammatory arthritis affecting one in 30 adults in the United Kingdom, yet it’s one of the most poorly managed,” study investigator Mark D. Russell, MB, BChir, pointed out during a poster presentation.
“There are very effective treatments,” added Dr. Russell, a rheumatology registrar and postdoctoral research fellow at King’s College London in London, England. “Urate-lowering therapies such as allopurinol, which when taken at the correct dose, in the long term, effectively cures patients of their symptoms and prevents complications.”
Dr. Russell said in an interview that there was still work to be done as the rate of people achieving urate levels below the recommended threshold of 360 micromol/L (6 mg/dL) within 6 months was still low, at 27%, even it if was still better than the 11% seen before the intervention was introduced.
Improving the In- and Post-Hospital Pathway
“We developed and implemented an in-hospital management pathway which encouraged urate-lowering therapy initiation prior to discharge, followed by a post-discharge nurse-led review,” Dr. Russell explained.
The in-hospital pathway was based upon BSR, European Alliance of Associations for Rheumatology, and American College of Rheumatology guidelines and involved diagnosing and managing the gout flare appropriately. This may have been via early joint aspiration, medication, or both, as directed by the rheumatology team. Affected individuals also received education and were directed where to obtain further information on the use of ULT. Outpatient follow-up was considered if an individual had severe or tophaceous gout, recurrent episodes, or contraindications or intolerances to ULT. Otherwise, a rheumatology nurse telephoned the individual 2 weeks later to review symptoms and discuss next steps.
The researchers recorded improvements in in-hospital outcomes. The frequency of in-hospital serum urate level measurements rose from 66% in the 12-month preimplementation period to 93% in the 12-month period after the intervention’s introduction. Almost two thirds (62%) of patients were discharged on ULT compared with 18% preimplementation. And gout-specific recommendations were given 86% of the time compared with 59% before the intervention.
Related Work on Gout Incidence
Separately, Dr. Russell also presented data from a nationwide, population-level cohort study that used data from OpenSAFELY, the secure data analytics platform used by the National Health Service in England.
“We did an analysis previously using the CPRD [Clinical Research Practice Datalink], which is another good primary care database, showing that only a third of people with gout in the UK get urate-lowering drugs, when really it should be the vast majority,” he said in the interview.
“And then we wanted to look at, on top of that, what was the impact of the [COVID-19] pandemic,” Russell added. Specifically, the aim was to look at how the pandemic had affected the incidence, management, and prevalence of gout.
Between March 2015 and February 2023, 246,695 new cases of gout were identified among 17.9 million adults, seen in primary and secondary care.
COVID-19 Pandemic Affected Cases
“The number of new cases of gout dropped by about one third in the first year of the pandemic,” Dr. Russell said. Incidence declined from 1.78 to 1.23 per 1000 adults. “Whether that was through people not feeling comfortable going to their GP [general practitioner] or not being able to get an appointment, we don’t know.”
While there was a subsequent increase in new cases of gout since this time, the rates still haven’t reached what they were before the pandemic. This implies that there could be a substantial number of people who may be undiagnosed because of the pandemic, Dr. Russell suggested.
Moreover, he reported that in 2022-2023, the prevalence of gout was 3.21%, up slightly from the 3.07% recorded 7 years earlier in 2015-2016.
ULT Treatment Rates Low
“If you did see a GP, however, so as long as you saw someone, the treatment wasn’t any worse,” Dr. Russell said. Just under 30% of people with incident gout for whom follow-up data were available had initiated ULT within 6 months of their diagnosis. And, of these new starters, around a quarter had a serum urate level below a target of 360 micromol/L.
“This doesn’t detract from the fact that this is pretty low. Despite guidelines, we’re still not getting the majority of people on these very effective urate-lowering drugs,” Dr. Russell said.
There is perhaps too much reliance on modifying diet and lifestyle, he added, which are important for many reasons but will not do much to lower blood urate levels.
As a final word, Dr. Russell said, “It’s not just a case of preventing a bit of joint pain. People get lots of complications when they’re undertreated — erosive joint damage, work disability, impaired quality of life — and yet we’ve got very cheap, well-tolerated drugs.”
The work was independently funded. Dr. Russell acknowledged grant or research support from Eli Lilly, Janssen, Pfizer, and UCB and receipt of honoraria from AbbVie, Biogen, Eli Lilly, Galapagos, and Menarini.
A version of this article appeared on Medscape.com.
FROM BSR 2024