User login
Erenumab demonstrates more favorable efficacy than rimegepant for migraine prevention
Key clinical point: Erenumab demonstrated a more favorable efficacy profile than rimegepant for the prevention of episodic and chronic migraine.
Major finding: Compared with 75 mg rimegepant, 70 mg erenumab significantly reduced monthly migraine days (MMD) by 0.90 days at 3 months (P = .042) and 140 mg erenumab significantly reduced MMD by 0.94 (P = .014) and 1.28 (P = .005) days at 1 month and 3 months, respectively. Erenumab showed advantages over rimegepant in improving Migraine-Specific Quality-of-life role function-restrictive domain and Migraine Disability Assessment scores (MIDAS) at 3 months.
Study details: This study performed anchored matching-adjusted indirect comparison of the relative efficacy of two erenumab regimens (70 mg and 140 mg) with rimegepant (75 mg) for migraine prevention using data from two phase 2/3 trials for erenumab (295 and STRIVE) and a phase 2/3 trial for rimegepant.
Disclosures: This study was funded by Novartis Healthcare Pvt. Ltd. Several authors declared being employees of and holding stocks or stock options in Novartis.
Source: Mahon R et al. Comparative effectiveness of erenumab versus rimegepant for migraine prevention using matching-adjusted indirect comparison. J Comp Eff Res. 2024 (Jan 4). doi: 10.57264/cer-2023-0122
Key clinical point: Erenumab demonstrated a more favorable efficacy profile than rimegepant for the prevention of episodic and chronic migraine.
Major finding: Compared with 75 mg rimegepant, 70 mg erenumab significantly reduced monthly migraine days (MMD) by 0.90 days at 3 months (P = .042) and 140 mg erenumab significantly reduced MMD by 0.94 (P = .014) and 1.28 (P = .005) days at 1 month and 3 months, respectively. Erenumab showed advantages over rimegepant in improving Migraine-Specific Quality-of-life role function-restrictive domain and Migraine Disability Assessment scores (MIDAS) at 3 months.
Study details: This study performed anchored matching-adjusted indirect comparison of the relative efficacy of two erenumab regimens (70 mg and 140 mg) with rimegepant (75 mg) for migraine prevention using data from two phase 2/3 trials for erenumab (295 and STRIVE) and a phase 2/3 trial for rimegepant.
Disclosures: This study was funded by Novartis Healthcare Pvt. Ltd. Several authors declared being employees of and holding stocks or stock options in Novartis.
Source: Mahon R et al. Comparative effectiveness of erenumab versus rimegepant for migraine prevention using matching-adjusted indirect comparison. J Comp Eff Res. 2024 (Jan 4). doi: 10.57264/cer-2023-0122
Key clinical point: Erenumab demonstrated a more favorable efficacy profile than rimegepant for the prevention of episodic and chronic migraine.
Major finding: Compared with 75 mg rimegepant, 70 mg erenumab significantly reduced monthly migraine days (MMD) by 0.90 days at 3 months (P = .042) and 140 mg erenumab significantly reduced MMD by 0.94 (P = .014) and 1.28 (P = .005) days at 1 month and 3 months, respectively. Erenumab showed advantages over rimegepant in improving Migraine-Specific Quality-of-life role function-restrictive domain and Migraine Disability Assessment scores (MIDAS) at 3 months.
Study details: This study performed anchored matching-adjusted indirect comparison of the relative efficacy of two erenumab regimens (70 mg and 140 mg) with rimegepant (75 mg) for migraine prevention using data from two phase 2/3 trials for erenumab (295 and STRIVE) and a phase 2/3 trial for rimegepant.
Disclosures: This study was funded by Novartis Healthcare Pvt. Ltd. Several authors declared being employees of and holding stocks or stock options in Novartis.
Source: Mahon R et al. Comparative effectiveness of erenumab versus rimegepant for migraine prevention using matching-adjusted indirect comparison. J Comp Eff Res. 2024 (Jan 4). doi: 10.57264/cer-2023-0122
Genetic factors influence response to anti-CGRP antibodies in migraine
Key clinical point: Monoclonal antibodies targeting the anti-calcitonin gene-related peptide (CGRP) showed persistent and comparable outcomes within a real-world cohort of patients with migraine leading to a reduction in migraine days per month (MDM) among responders with large effect sizes; however, the response was influenced by genetic factors.
Major finding: Patients responding to anti-CGRP monoclonal antibodies demonstrated persistent reduction in MDM (usually ≥50% reduction from baseline) at first (η2 = 0.26) and second (η2 = 0.22) follow-up, with all treatments showing similar effects and large effect sizes. Non-responders vs responders had a lower mean genetic risk score (P = .041) without any difference in polygenic risk score.
Study details: This retrospective clinical and genetic study included 481 patients with migraine who were prescribed preventive erenumab (n = 166), galcanezumab (n = 164), or fremanezumab (n = 151).
Disclosures: This study was funded by the US Agency for Healthcare Research and Quality. S Meyers declared serving on the speakers’ bureau for Biohaven Pharmaceuticals and Allergan.
Source: Chase BA et al. Characteristics associated with response to subcutaneously administered anti-CGRP monoclonal antibody medications in a real-world community cohort of persons living with migraine: A retrospective clinical and genetic study. Headache. 2023 (Dec 10). doi:
Key clinical point: Monoclonal antibodies targeting the anti-calcitonin gene-related peptide (CGRP) showed persistent and comparable outcomes within a real-world cohort of patients with migraine leading to a reduction in migraine days per month (MDM) among responders with large effect sizes; however, the response was influenced by genetic factors.
Major finding: Patients responding to anti-CGRP monoclonal antibodies demonstrated persistent reduction in MDM (usually ≥50% reduction from baseline) at first (η2 = 0.26) and second (η2 = 0.22) follow-up, with all treatments showing similar effects and large effect sizes. Non-responders vs responders had a lower mean genetic risk score (P = .041) without any difference in polygenic risk score.
Study details: This retrospective clinical and genetic study included 481 patients with migraine who were prescribed preventive erenumab (n = 166), galcanezumab (n = 164), or fremanezumab (n = 151).
Disclosures: This study was funded by the US Agency for Healthcare Research and Quality. S Meyers declared serving on the speakers’ bureau for Biohaven Pharmaceuticals and Allergan.
Source: Chase BA et al. Characteristics associated with response to subcutaneously administered anti-CGRP monoclonal antibody medications in a real-world community cohort of persons living with migraine: A retrospective clinical and genetic study. Headache. 2023 (Dec 10). doi:
Key clinical point: Monoclonal antibodies targeting the anti-calcitonin gene-related peptide (CGRP) showed persistent and comparable outcomes within a real-world cohort of patients with migraine leading to a reduction in migraine days per month (MDM) among responders with large effect sizes; however, the response was influenced by genetic factors.
Major finding: Patients responding to anti-CGRP monoclonal antibodies demonstrated persistent reduction in MDM (usually ≥50% reduction from baseline) at first (η2 = 0.26) and second (η2 = 0.22) follow-up, with all treatments showing similar effects and large effect sizes. Non-responders vs responders had a lower mean genetic risk score (P = .041) without any difference in polygenic risk score.
Study details: This retrospective clinical and genetic study included 481 patients with migraine who were prescribed preventive erenumab (n = 166), galcanezumab (n = 164), or fremanezumab (n = 151).
Disclosures: This study was funded by the US Agency for Healthcare Research and Quality. S Meyers declared serving on the speakers’ bureau for Biohaven Pharmaceuticals and Allergan.
Source: Chase BA et al. Characteristics associated with response to subcutaneously administered anti-CGRP monoclonal antibody medications in a real-world community cohort of persons living with migraine: A retrospective clinical and genetic study. Headache. 2023 (Dec 10). doi:
Agomelatine offers an effective preventive treatment for episodic migraine without aura
Key clinical point: Agomelatine appeared to be an effective preventive treatment for episodic migraine without aura.
Major finding: After 3 months of treatment, patients receiving agomelatine vs placebo had significant reduction in headache frequency (4.8 vs 5.82; P = .009) and severity (─4.1 vs ─0.71; P < .001), mean monthly migraine days (8.86 vs 10.63; P = .025), and Migraine Disability Assessment Score (MIDAS; ─1.06 vs ─0.36; P < .001).
Study details: Findings are from a parallel randomized controlled trial that included 99 patients with episodic migraine without aura who were randomly assigned to receive either agomelatine (n = 49) or placebo (vitamin B1 tablets; n = 50).
Disclosures: This study did not receive any funding. The authors declared no conflicts of interest.
Source: Farzin K et al. The effectiveness of agomelatine on headache severity and frequency in episodic migraine without aura; a parallel randomized controlled trial study. BMC Neurol. 2024;24:2 (Jan 2). doi: 10.1186/s12883-023-03516-9
Key clinical point: Agomelatine appeared to be an effective preventive treatment for episodic migraine without aura.
Major finding: After 3 months of treatment, patients receiving agomelatine vs placebo had significant reduction in headache frequency (4.8 vs 5.82; P = .009) and severity (─4.1 vs ─0.71; P < .001), mean monthly migraine days (8.86 vs 10.63; P = .025), and Migraine Disability Assessment Score (MIDAS; ─1.06 vs ─0.36; P < .001).
Study details: Findings are from a parallel randomized controlled trial that included 99 patients with episodic migraine without aura who were randomly assigned to receive either agomelatine (n = 49) or placebo (vitamin B1 tablets; n = 50).
Disclosures: This study did not receive any funding. The authors declared no conflicts of interest.
Source: Farzin K et al. The effectiveness of agomelatine on headache severity and frequency in episodic migraine without aura; a parallel randomized controlled trial study. BMC Neurol. 2024;24:2 (Jan 2). doi: 10.1186/s12883-023-03516-9
Key clinical point: Agomelatine appeared to be an effective preventive treatment for episodic migraine without aura.
Major finding: After 3 months of treatment, patients receiving agomelatine vs placebo had significant reduction in headache frequency (4.8 vs 5.82; P = .009) and severity (─4.1 vs ─0.71; P < .001), mean monthly migraine days (8.86 vs 10.63; P = .025), and Migraine Disability Assessment Score (MIDAS; ─1.06 vs ─0.36; P < .001).
Study details: Findings are from a parallel randomized controlled trial that included 99 patients with episodic migraine without aura who were randomly assigned to receive either agomelatine (n = 49) or placebo (vitamin B1 tablets; n = 50).
Disclosures: This study did not receive any funding. The authors declared no conflicts of interest.
Source: Farzin K et al. The effectiveness of agomelatine on headache severity and frequency in episodic migraine without aura; a parallel randomized controlled trial study. BMC Neurol. 2024;24:2 (Jan 2). doi: 10.1186/s12883-023-03516-9
Gut microbiota and migraine: Is there a link?
Key clinical point: Gut microbiota may have a potential casual association with migraine symptoms, with evidence indicating a connection between gut microbiota and increased or decreased risk for migraine.
Major finding: A higher abundance of genus Lactobacillus (inverse variance weighted [IVW] odds ratio [OR] 1.10; P = .004) and family Prevotellaceae (IVW OR 0.89; P = .02) were causally associated with a higher and lower risk for migraine, respectively.
Study details: This study used a two-sample Mendelian randomization framework to assess the causal effects of gut microbiota on migraine risk using 2651 single nucleotide polymorphisms as instrumental variables. Large-scale genome-wide association studies consisting of 18,340 participants from 24 cohorts provided the summary-level statistics for gut microbiota.
Disclosures: This study was funded by the National Key Research and Development Program. The authors declared no conflicts of interest.
Source: Meng X et al. Exploring the role of gut microbiota in migraine risk: A two-sample Mendelian randomization study. Scand J Gastroenterol. 2023 (Dec 27). doi: 10.1080/00365521.2023.2298370
Key clinical point: Gut microbiota may have a potential casual association with migraine symptoms, with evidence indicating a connection between gut microbiota and increased or decreased risk for migraine.
Major finding: A higher abundance of genus Lactobacillus (inverse variance weighted [IVW] odds ratio [OR] 1.10; P = .004) and family Prevotellaceae (IVW OR 0.89; P = .02) were causally associated with a higher and lower risk for migraine, respectively.
Study details: This study used a two-sample Mendelian randomization framework to assess the causal effects of gut microbiota on migraine risk using 2651 single nucleotide polymorphisms as instrumental variables. Large-scale genome-wide association studies consisting of 18,340 participants from 24 cohorts provided the summary-level statistics for gut microbiota.
Disclosures: This study was funded by the National Key Research and Development Program. The authors declared no conflicts of interest.
Source: Meng X et al. Exploring the role of gut microbiota in migraine risk: A two-sample Mendelian randomization study. Scand J Gastroenterol. 2023 (Dec 27). doi: 10.1080/00365521.2023.2298370
Key clinical point: Gut microbiota may have a potential casual association with migraine symptoms, with evidence indicating a connection between gut microbiota and increased or decreased risk for migraine.
Major finding: A higher abundance of genus Lactobacillus (inverse variance weighted [IVW] odds ratio [OR] 1.10; P = .004) and family Prevotellaceae (IVW OR 0.89; P = .02) were causally associated with a higher and lower risk for migraine, respectively.
Study details: This study used a two-sample Mendelian randomization framework to assess the causal effects of gut microbiota on migraine risk using 2651 single nucleotide polymorphisms as instrumental variables. Large-scale genome-wide association studies consisting of 18,340 participants from 24 cohorts provided the summary-level statistics for gut microbiota.
Disclosures: This study was funded by the National Key Research and Development Program. The authors declared no conflicts of interest.
Source: Meng X et al. Exploring the role of gut microbiota in migraine risk: A two-sample Mendelian randomization study. Scand J Gastroenterol. 2023 (Dec 27). doi: 10.1080/00365521.2023.2298370
Considering high-dose EPA/DHA as a primary option for migraine prevention
Key clinical point: High-dose eicosapentaenoic acid (EPA)/docosahexaenoic acid (DHA) supplementation demonstrated highest efficacy and acceptability among all studied treatments, emphasizing its potential as a first-choice treatment for migraine prophylaxis.
Major finding: Among all prophylactic treatments, high-dose EPA/DHA supplementation showed the highest decrease in migraine frequency (standardized mean difference [SMD] ─1.36; 95% CI ─2.32 to ─0.39) and severity (SMD ─2.23; 95% CI ─3.17 to ─1.30) and the most favorable acceptability rate (odds ratio 1.00; 95% CI 0.06 to 17.41) compared with placebo.
Study details: The data come from a network meta-analysis of 40 randomized controlled trials that included 6616 patients with either episodic or chronic migraine.
Disclosures: This study did not receive any funding. The authors declared no conflicts of interest.
Source: Tseng PT et al. Efficacy of high dosage anti-inflammatory eicosapentaenoic acid/docosahexaenoic acid for migraine prophylaxis: A network meta-analysis. Adv Nutr. 2023;15(2):100163 (Dec 16). doi: 10.1016/j.advnut.2023.100163
Key clinical point: High-dose eicosapentaenoic acid (EPA)/docosahexaenoic acid (DHA) supplementation demonstrated highest efficacy and acceptability among all studied treatments, emphasizing its potential as a first-choice treatment for migraine prophylaxis.
Major finding: Among all prophylactic treatments, high-dose EPA/DHA supplementation showed the highest decrease in migraine frequency (standardized mean difference [SMD] ─1.36; 95% CI ─2.32 to ─0.39) and severity (SMD ─2.23; 95% CI ─3.17 to ─1.30) and the most favorable acceptability rate (odds ratio 1.00; 95% CI 0.06 to 17.41) compared with placebo.
Study details: The data come from a network meta-analysis of 40 randomized controlled trials that included 6616 patients with either episodic or chronic migraine.
Disclosures: This study did not receive any funding. The authors declared no conflicts of interest.
Source: Tseng PT et al. Efficacy of high dosage anti-inflammatory eicosapentaenoic acid/docosahexaenoic acid for migraine prophylaxis: A network meta-analysis. Adv Nutr. 2023;15(2):100163 (Dec 16). doi: 10.1016/j.advnut.2023.100163
Key clinical point: High-dose eicosapentaenoic acid (EPA)/docosahexaenoic acid (DHA) supplementation demonstrated highest efficacy and acceptability among all studied treatments, emphasizing its potential as a first-choice treatment for migraine prophylaxis.
Major finding: Among all prophylactic treatments, high-dose EPA/DHA supplementation showed the highest decrease in migraine frequency (standardized mean difference [SMD] ─1.36; 95% CI ─2.32 to ─0.39) and severity (SMD ─2.23; 95% CI ─3.17 to ─1.30) and the most favorable acceptability rate (odds ratio 1.00; 95% CI 0.06 to 17.41) compared with placebo.
Study details: The data come from a network meta-analysis of 40 randomized controlled trials that included 6616 patients with either episodic or chronic migraine.
Disclosures: This study did not receive any funding. The authors declared no conflicts of interest.
Source: Tseng PT et al. Efficacy of high dosage anti-inflammatory eicosapentaenoic acid/docosahexaenoic acid for migraine prophylaxis: A network meta-analysis. Adv Nutr. 2023;15(2):100163 (Dec 16). doi: 10.1016/j.advnut.2023.100163
Elevated odds of motor vehicle crashes in older adults after newly diagnosed migraine
Key clinical point: The likelihood of motor vehicle crashes (MVC) in the year following diagnosis is significantly higher among older drivers who have recently been diagnosed with migraine, emphasizing the necessity for driving safety interventions for these individuals.
Major finding: The risk for an MVC in the year after migraine onset was > 3 times higher among older adult drivers with new-onset migraine compared with those who never had a migraine (adjusted odds ratio [aOR] 3.27; P = .019). Prevalent migraine was not associated with MVC in the subsequent 2 years (aOR 0.97; P = .88).
Study details: Findings are from the AAA Longitudinal Research on Aging Drivers study, which included 2589 older drivers (age 65-79 years) with a valid driver’s license, of whom 12.5% and 1.3% reported prevalent and incident migraines, respectively.
Disclosures: This study was funded by the AAA Foundation for Traffic Safety and National Center for Advancing Translational Sciences. The authors declared no conflicts of interest.
Source: DiGuiseppi CG et al. Migraine headaches are associated with motor vehicle crashes and driving habits among older drivers: Prospective cohort study. J Am Geriatr Soc. 2023 (Dec 22). doi: 10.1111/jgs.18719
Key clinical point: The likelihood of motor vehicle crashes (MVC) in the year following diagnosis is significantly higher among older drivers who have recently been diagnosed with migraine, emphasizing the necessity for driving safety interventions for these individuals.
Major finding: The risk for an MVC in the year after migraine onset was > 3 times higher among older adult drivers with new-onset migraine compared with those who never had a migraine (adjusted odds ratio [aOR] 3.27; P = .019). Prevalent migraine was not associated with MVC in the subsequent 2 years (aOR 0.97; P = .88).
Study details: Findings are from the AAA Longitudinal Research on Aging Drivers study, which included 2589 older drivers (age 65-79 years) with a valid driver’s license, of whom 12.5% and 1.3% reported prevalent and incident migraines, respectively.
Disclosures: This study was funded by the AAA Foundation for Traffic Safety and National Center for Advancing Translational Sciences. The authors declared no conflicts of interest.
Source: DiGuiseppi CG et al. Migraine headaches are associated with motor vehicle crashes and driving habits among older drivers: Prospective cohort study. J Am Geriatr Soc. 2023 (Dec 22). doi: 10.1111/jgs.18719
Key clinical point: The likelihood of motor vehicle crashes (MVC) in the year following diagnosis is significantly higher among older drivers who have recently been diagnosed with migraine, emphasizing the necessity for driving safety interventions for these individuals.
Major finding: The risk for an MVC in the year after migraine onset was > 3 times higher among older adult drivers with new-onset migraine compared with those who never had a migraine (adjusted odds ratio [aOR] 3.27; P = .019). Prevalent migraine was not associated with MVC in the subsequent 2 years (aOR 0.97; P = .88).
Study details: Findings are from the AAA Longitudinal Research on Aging Drivers study, which included 2589 older drivers (age 65-79 years) with a valid driver’s license, of whom 12.5% and 1.3% reported prevalent and incident migraines, respectively.
Disclosures: This study was funded by the AAA Foundation for Traffic Safety and National Center for Advancing Translational Sciences. The authors declared no conflicts of interest.
Source: DiGuiseppi CG et al. Migraine headaches are associated with motor vehicle crashes and driving habits among older drivers: Prospective cohort study. J Am Geriatr Soc. 2023 (Dec 22). doi: 10.1111/jgs.18719
Why Are Women More Likely to Get Long COVID?
Annette Gillaspie, a nurse in a small Oregon hospital, hoped she would be back working with patients by now. She contracted COVID-19 on the job early in the pandemic and ended up with long COVID.
After recovering a bit, her fatigue and dizziness returned, and today she is still working a desk job. She has also experienced more severe menstrual periods than before she had COVID.
“Being a female with long COVID definitely does add to the roller-coaster effect of symptoms,” Ms. Gillaspie said.
reported by the Centers for Disease Control and Prevention (CDC). Researchers are trying to determine why, what causes the gender disparity, and how best to treat it.
Scientists are also starting to look at the impact of long COVID on female reproductive health, including menstruation, pregnancy, and menopause.
Sex differences are common in infection-associated illnesses, said Beth Pollack, MS, a research scientist specializing in long COVID in the Massachusetts Institute of Technology’s Department of Biological Engineering, Cambridge, Massachusetts. “It informs research priorities and the lens with which we understand long COVID.”
For example, reproductive health issues for women, such as puberty, pregnancy, and menopause, can alter the course of illness in a subset of women in myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) and postural orthostatic tachycardia syndrome (POTS), a condition that can cause dizziness and worse.
“This suggests that sex hormones may play key roles in immune responses to infections,” Ms. Pollack said.
ME/CFS and a Possible Link to Long COVID in Women
Some of the research into long COVID is being led by teams studying infection-associated chronic illnesses like ME/CFS.
The problem: Advocates say ME/CFS has been under-researched. Poorly understood for years, the condition is one of a handful of chronic illnesses linked to infections, including Lyme disease and now long COVID. Perhaps not coincidently, they are more likely to affect women.
Many of the research findings about long COVID mirror data that emerged in past ME/CFS research, said Jaime Seltzer, the scientific director at #MEAction, Santa Monica, California, an advocacy group. One point in particular: ME/CFS strikes women about twice as much as men, according to the CDC.
Ms. Seltzer said the response to long COVID could be much further ahead if the research community acknowledged the work done over the years on ME/CFS. Many of the potential biomarkers and risk factors emerging for long COVID were also suspected in ME/CFS, but not thoroughly studied, she said.
She also said not enough work has been done to unravel the links between gender and these chronic conditions.
“We’re stuck in this Groundhog Day situation,” she said. “There isn’t any research, so we can’t say anything definitively.”
Some New Research, Some New Clues
Scientists like Ms. Pollack are slowly making inroads. She was lead author on a 2023 review investigating the impact of long COVID on female reproductive health. The paper highlights long COVID links to ME/CFS, POTS, and Ehlers-Danlos syndrome (EDS), as well as a resulting laundry list of female reproductive health issues. The hope is physicians will examine how the menstrual cycle, pregnancy, and menopause affect symptoms and illness progression of long COVID.
The Tal Research group at MIT (where Ms. Pollack works) has also added long COVID to the list of infection-associated illnesses it studies. The lab is conducting a large study looking into both Lyme disease and long COVID. The goals are to identify biomarkers that can predict who will not recover and to advance available treatments.
Another MIT program, “SEXX + Immunity” holds seminars and networking sessions for scientists looking into the role of female and male biology in immune responses to infection.
Barriers to Progress Remain
On the clinical side, female patients with long COVID also have to deal with a historical bias that still lurks in medicine when it comes to women’s health, said Alba Azola, MD, an assistant professor of physical medicine at Johns Hopkins Medicine, Baltimore, Maryland.
Dr. Azola said she has discovered clinical descriptions of ME/CFE in the literature archives that describe it as “neurasthenia” and dismiss it as psychological.
Patients say that it is still happening, and while it may not be so blunt, “you can read between the lines,” Dr. Azola said.
Dr. Azola, who has worked with long COVID patients and is now seeing people with ME/CFS, said the symptoms of infection-associated chronic illness can mimic menopause, and many of her patients received that misdiagnosis. She recommends that doctors rule out long COVID for women with multiple symptoms before attributing symptoms to menopause.
Seeing that some long COVID patients were developing ME/CFS, staff at the Bateman Horne Center in Salt Lake City, Utah, set up a program for the condition in 2021. They were already treating patients with ME/CFS and what they call “multi-symptom chronic complex diseases.”
Jennifer Bell, a certified nurse practitioner at the center, said she has not seen any patients with ovarian failure but plenty with reproductive health issues.
“There definitely is a hormonal connection, but I don’t think there’s a good understanding about what is happening,” she said.
Most of her patients are female, and the more serious patients tend to go through a worsening of their symptoms in the week prior to getting a period, she said.
One thing Ms. Bell said she’s noticed in the past year is an increase in patients with EDS, which is also more common in women.
Like long COVID, many of the conditions traditionally treated at the center have no cure. But Ms. Bell said the center has developed an expertise in treating post-exertional malaise, a common symptom of long COVID, and keeps up with the literature for treatments to try, like the combination of guanfacine and the antioxidant N-acetyl cysteine to treat brain fog, an approach developed at Yale.
“It’s a very challenging illness to treat,” Ms. Bell said.
Since the emergence of long COVID, researchers have warned that symptoms vary so much from person to person that treatment will need to be targeted.
Ms. Pollack of MIT agrees and sees a big role for personalized medicine.
We need to “identify phenotypes within and across these overlapping and co-occurring illnesses so that we can identify the right therapeutics for each person,” she said.
As for Annette Gillaspie, she still hopes her long COVID will subside so she can get out from behind the desk and return to her normal nursing duties.
“I just got to a point where I realized I’m likely never going to be able to do my job,” she said. “It was incredibly heart breaking, but it’s the reality of long COVID, and I know I’m not the only one to have to step away from a job I loved.”
A version of this article appeared on Medscape.com.
Annette Gillaspie, a nurse in a small Oregon hospital, hoped she would be back working with patients by now. She contracted COVID-19 on the job early in the pandemic and ended up with long COVID.
After recovering a bit, her fatigue and dizziness returned, and today she is still working a desk job. She has also experienced more severe menstrual periods than before she had COVID.
“Being a female with long COVID definitely does add to the roller-coaster effect of symptoms,” Ms. Gillaspie said.
reported by the Centers for Disease Control and Prevention (CDC). Researchers are trying to determine why, what causes the gender disparity, and how best to treat it.
Scientists are also starting to look at the impact of long COVID on female reproductive health, including menstruation, pregnancy, and menopause.
Sex differences are common in infection-associated illnesses, said Beth Pollack, MS, a research scientist specializing in long COVID in the Massachusetts Institute of Technology’s Department of Biological Engineering, Cambridge, Massachusetts. “It informs research priorities and the lens with which we understand long COVID.”
For example, reproductive health issues for women, such as puberty, pregnancy, and menopause, can alter the course of illness in a subset of women in myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) and postural orthostatic tachycardia syndrome (POTS), a condition that can cause dizziness and worse.
“This suggests that sex hormones may play key roles in immune responses to infections,” Ms. Pollack said.
ME/CFS and a Possible Link to Long COVID in Women
Some of the research into long COVID is being led by teams studying infection-associated chronic illnesses like ME/CFS.
The problem: Advocates say ME/CFS has been under-researched. Poorly understood for years, the condition is one of a handful of chronic illnesses linked to infections, including Lyme disease and now long COVID. Perhaps not coincidently, they are more likely to affect women.
Many of the research findings about long COVID mirror data that emerged in past ME/CFS research, said Jaime Seltzer, the scientific director at #MEAction, Santa Monica, California, an advocacy group. One point in particular: ME/CFS strikes women about twice as much as men, according to the CDC.
Ms. Seltzer said the response to long COVID could be much further ahead if the research community acknowledged the work done over the years on ME/CFS. Many of the potential biomarkers and risk factors emerging for long COVID were also suspected in ME/CFS, but not thoroughly studied, she said.
She also said not enough work has been done to unravel the links between gender and these chronic conditions.
“We’re stuck in this Groundhog Day situation,” she said. “There isn’t any research, so we can’t say anything definitively.”
Some New Research, Some New Clues
Scientists like Ms. Pollack are slowly making inroads. She was lead author on a 2023 review investigating the impact of long COVID on female reproductive health. The paper highlights long COVID links to ME/CFS, POTS, and Ehlers-Danlos syndrome (EDS), as well as a resulting laundry list of female reproductive health issues. The hope is physicians will examine how the menstrual cycle, pregnancy, and menopause affect symptoms and illness progression of long COVID.
The Tal Research group at MIT (where Ms. Pollack works) has also added long COVID to the list of infection-associated illnesses it studies. The lab is conducting a large study looking into both Lyme disease and long COVID. The goals are to identify biomarkers that can predict who will not recover and to advance available treatments.
Another MIT program, “SEXX + Immunity” holds seminars and networking sessions for scientists looking into the role of female and male biology in immune responses to infection.
Barriers to Progress Remain
On the clinical side, female patients with long COVID also have to deal with a historical bias that still lurks in medicine when it comes to women’s health, said Alba Azola, MD, an assistant professor of physical medicine at Johns Hopkins Medicine, Baltimore, Maryland.
Dr. Azola said she has discovered clinical descriptions of ME/CFE in the literature archives that describe it as “neurasthenia” and dismiss it as psychological.
Patients say that it is still happening, and while it may not be so blunt, “you can read between the lines,” Dr. Azola said.
Dr. Azola, who has worked with long COVID patients and is now seeing people with ME/CFS, said the symptoms of infection-associated chronic illness can mimic menopause, and many of her patients received that misdiagnosis. She recommends that doctors rule out long COVID for women with multiple symptoms before attributing symptoms to menopause.
Seeing that some long COVID patients were developing ME/CFS, staff at the Bateman Horne Center in Salt Lake City, Utah, set up a program for the condition in 2021. They were already treating patients with ME/CFS and what they call “multi-symptom chronic complex diseases.”
Jennifer Bell, a certified nurse practitioner at the center, said she has not seen any patients with ovarian failure but plenty with reproductive health issues.
“There definitely is a hormonal connection, but I don’t think there’s a good understanding about what is happening,” she said.
Most of her patients are female, and the more serious patients tend to go through a worsening of their symptoms in the week prior to getting a period, she said.
One thing Ms. Bell said she’s noticed in the past year is an increase in patients with EDS, which is also more common in women.
Like long COVID, many of the conditions traditionally treated at the center have no cure. But Ms. Bell said the center has developed an expertise in treating post-exertional malaise, a common symptom of long COVID, and keeps up with the literature for treatments to try, like the combination of guanfacine and the antioxidant N-acetyl cysteine to treat brain fog, an approach developed at Yale.
“It’s a very challenging illness to treat,” Ms. Bell said.
Since the emergence of long COVID, researchers have warned that symptoms vary so much from person to person that treatment will need to be targeted.
Ms. Pollack of MIT agrees and sees a big role for personalized medicine.
We need to “identify phenotypes within and across these overlapping and co-occurring illnesses so that we can identify the right therapeutics for each person,” she said.
As for Annette Gillaspie, she still hopes her long COVID will subside so she can get out from behind the desk and return to her normal nursing duties.
“I just got to a point where I realized I’m likely never going to be able to do my job,” she said. “It was incredibly heart breaking, but it’s the reality of long COVID, and I know I’m not the only one to have to step away from a job I loved.”
A version of this article appeared on Medscape.com.
Annette Gillaspie, a nurse in a small Oregon hospital, hoped she would be back working with patients by now. She contracted COVID-19 on the job early in the pandemic and ended up with long COVID.
After recovering a bit, her fatigue and dizziness returned, and today she is still working a desk job. She has also experienced more severe menstrual periods than before she had COVID.
“Being a female with long COVID definitely does add to the roller-coaster effect of symptoms,” Ms. Gillaspie said.
reported by the Centers for Disease Control and Prevention (CDC). Researchers are trying to determine why, what causes the gender disparity, and how best to treat it.
Scientists are also starting to look at the impact of long COVID on female reproductive health, including menstruation, pregnancy, and menopause.
Sex differences are common in infection-associated illnesses, said Beth Pollack, MS, a research scientist specializing in long COVID in the Massachusetts Institute of Technology’s Department of Biological Engineering, Cambridge, Massachusetts. “It informs research priorities and the lens with which we understand long COVID.”
For example, reproductive health issues for women, such as puberty, pregnancy, and menopause, can alter the course of illness in a subset of women in myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) and postural orthostatic tachycardia syndrome (POTS), a condition that can cause dizziness and worse.
“This suggests that sex hormones may play key roles in immune responses to infections,” Ms. Pollack said.
ME/CFS and a Possible Link to Long COVID in Women
Some of the research into long COVID is being led by teams studying infection-associated chronic illnesses like ME/CFS.
The problem: Advocates say ME/CFS has been under-researched. Poorly understood for years, the condition is one of a handful of chronic illnesses linked to infections, including Lyme disease and now long COVID. Perhaps not coincidently, they are more likely to affect women.
Many of the research findings about long COVID mirror data that emerged in past ME/CFS research, said Jaime Seltzer, the scientific director at #MEAction, Santa Monica, California, an advocacy group. One point in particular: ME/CFS strikes women about twice as much as men, according to the CDC.
Ms. Seltzer said the response to long COVID could be much further ahead if the research community acknowledged the work done over the years on ME/CFS. Many of the potential biomarkers and risk factors emerging for long COVID were also suspected in ME/CFS, but not thoroughly studied, she said.
She also said not enough work has been done to unravel the links between gender and these chronic conditions.
“We’re stuck in this Groundhog Day situation,” she said. “There isn’t any research, so we can’t say anything definitively.”
Some New Research, Some New Clues
Scientists like Ms. Pollack are slowly making inroads. She was lead author on a 2023 review investigating the impact of long COVID on female reproductive health. The paper highlights long COVID links to ME/CFS, POTS, and Ehlers-Danlos syndrome (EDS), as well as a resulting laundry list of female reproductive health issues. The hope is physicians will examine how the menstrual cycle, pregnancy, and menopause affect symptoms and illness progression of long COVID.
The Tal Research group at MIT (where Ms. Pollack works) has also added long COVID to the list of infection-associated illnesses it studies. The lab is conducting a large study looking into both Lyme disease and long COVID. The goals are to identify biomarkers that can predict who will not recover and to advance available treatments.
Another MIT program, “SEXX + Immunity” holds seminars and networking sessions for scientists looking into the role of female and male biology in immune responses to infection.
Barriers to Progress Remain
On the clinical side, female patients with long COVID also have to deal with a historical bias that still lurks in medicine when it comes to women’s health, said Alba Azola, MD, an assistant professor of physical medicine at Johns Hopkins Medicine, Baltimore, Maryland.
Dr. Azola said she has discovered clinical descriptions of ME/CFE in the literature archives that describe it as “neurasthenia” and dismiss it as psychological.
Patients say that it is still happening, and while it may not be so blunt, “you can read between the lines,” Dr. Azola said.
Dr. Azola, who has worked with long COVID patients and is now seeing people with ME/CFS, said the symptoms of infection-associated chronic illness can mimic menopause, and many of her patients received that misdiagnosis. She recommends that doctors rule out long COVID for women with multiple symptoms before attributing symptoms to menopause.
Seeing that some long COVID patients were developing ME/CFS, staff at the Bateman Horne Center in Salt Lake City, Utah, set up a program for the condition in 2021. They were already treating patients with ME/CFS and what they call “multi-symptom chronic complex diseases.”
Jennifer Bell, a certified nurse practitioner at the center, said she has not seen any patients with ovarian failure but plenty with reproductive health issues.
“There definitely is a hormonal connection, but I don’t think there’s a good understanding about what is happening,” she said.
Most of her patients are female, and the more serious patients tend to go through a worsening of their symptoms in the week prior to getting a period, she said.
One thing Ms. Bell said she’s noticed in the past year is an increase in patients with EDS, which is also more common in women.
Like long COVID, many of the conditions traditionally treated at the center have no cure. But Ms. Bell said the center has developed an expertise in treating post-exertional malaise, a common symptom of long COVID, and keeps up with the literature for treatments to try, like the combination of guanfacine and the antioxidant N-acetyl cysteine to treat brain fog, an approach developed at Yale.
“It’s a very challenging illness to treat,” Ms. Bell said.
Since the emergence of long COVID, researchers have warned that symptoms vary so much from person to person that treatment will need to be targeted.
Ms. Pollack of MIT agrees and sees a big role for personalized medicine.
We need to “identify phenotypes within and across these overlapping and co-occurring illnesses so that we can identify the right therapeutics for each person,” she said.
As for Annette Gillaspie, she still hopes her long COVID will subside so she can get out from behind the desk and return to her normal nursing duties.
“I just got to a point where I realized I’m likely never going to be able to do my job,” she said. “It was incredibly heart breaking, but it’s the reality of long COVID, and I know I’m not the only one to have to step away from a job I loved.”
A version of this article appeared on Medscape.com.
Best Practices for Hiring, Training, Retaining Rheumatology Advanced Practice Providers
Once considered a luxury, hiring a nurse, nurse practitioner, or physician assistant is becoming a necessity in many rheumatology practices.
Seeing the wait lists pile up in her Florida practice, Stacy Yonker, MBA, chief executive officer of Sarasota Arthritis Center, knew she had to make some changes. “Everyone’s aging in the boomer generations. Particularly in Florida, we have a lot of people who retire here. In the more southern demographics, it is a very difficult challenge for practices to get new patients in,” she said.
Ms. Yonker is in the process of hiring several nurse practitioners (NPs) to assist in the clinics and infusion suites, lightening the load for the practice’s 11 rheumatologists.
Hiring an advanced practice provider (APP) to support the practice is just a first step. Getting these additional personnel up to speed means an investment in education and fostering good working relationships with NPs, PAs, and the staff’s physicians. Even more importantly, practices need to set realistic expectations on workload for these new hires.
“I tried to hire them, but I couldn’t keep them,” is a statement Christine A. Stamatos, DNP, ANP-C, hears all the time from rheumatologists. Oftentimes it’s because the practice saddles the new hire with 20 patients a day, said Dr. Stamatos, director of the Fibromyalgia Wellness Center within the division of rheumatology at Northwell Health in Huntington, New York. She is also an assistant professor at Hofstra Northwell School of Graduate Nursing and Physician Assistant Studies in Hempstead, New York.
“Twenty patients a day is too much,” Dr. Stamatos said. Overload someone, and they won’t stay. Offer them the support, mentoring, and tools they need to practice in their setting — and they will.
Why the Profession Needs APPs
Rheumatology is a much smaller specialty than most, with only a set number of rheumatologists in the field that can provide care to patients. A growing shortage is also looming. Reports from the American College of Rheumatology have projected troubling shortfalls in rheumatologists over the next decade in all regions of the United States.
Many of them aging into retirement “poses a significant issue on being able to continue providing care for the population that experiences the rheumatic disease,” said Ms. Yonker, a director of the National Organization of Rheumatology Management (NORM), a forum that promotes education and advocacy for rheumatology practice managers. People are also living longer, which means more patients are developing arthritis and autoimmune diseases.
Julia M. Swafford, PA-C, a rheumatology physician assistant in Battle Creek, Michigan, sees many advantages of hiring NPs and PAs, and not just from a financial perspective.
Salaries for PAs and NPs aren’t as high and they’re also more accessible than a rheumatologist. “You could train an NP or PA a lot quicker during that same time frame it would take to find a new rheumatology provider,” she offered. And while they may not be as experienced as rheumatologists, “you can kind of mold me on how you like to practice, what medications you may like to use, how you like to treat your patients,” Ms. Swafford said.
Hiring Someone With Experience
Recruiting and retaining APPs is not without its challenges.
Finding individuals compatible with this specialty isn’t easy, noted Mark Box, MD, medical director of Carondelet Rheumatology in Kansas City, Missouri. Ideally, APPs should be inquisitive, compassionate, and ready to learn. “Rheumatology is a cognitive specialty where you have to fit many pieces together. You need an APP who wants to embrace that,” he said.
The profession isn’t that “sexy” either, noted Katie Taylor, Carondelet’s practice manager. Patients are often in head-to-toe pain, and miserable. Many have been to other specialists without answers to their questions. For these reasons, rheumatology can be a hard sell for some PAs and NPs.
Nurse practitioners aren’t always comfortable with administering things such as controlled medications, for example. “It’s a hard patient population, and it’s a specialty of exclusion. You’ve got to be really smart to understand our diseases and our processes and our drugs,” Ms. Taylor said. In other words, it’s a difficult environment for an NP to walk into if their previous experience has been limited to upper respiratory issues and urinary tract infections in the primary care setting.
When hiring an APP, rheumatologists should look for someone who demonstrates an interest in lifelong learning, because the field is changing every day. They should exhibit good scores in educational training and have experience working in an emergency department or another field that translates well into rheumatology such as critical care, immunology, hematology, and orthopedics, she said.
Carondelet Rheumatology was specifically looking for an NP with rheumatology experience to support Dr. Box’s solo practice.
He was facing enormous pressure to be in the office every single day of the week. The practice had to cancel patients for its infusion suite on a regular basis when he was out of the office, Ms. Taylor said. “We couldn’t see new patients, and he wasn’t able to touch as many patients as he wanted to. The doctor takes the oath of touching as many in your community as possible, and you’re limited when you’re a one-man show.”
The practice eventually found an NP who already knew how to do joint injections. “We started her with easier diagnoses for things like osteoporosis and gout. She had an orthopedic background, so she was familiar with some of those diseases,” she said.
Even so, she often leaves with questions every day. “It’s a commitment for her to understand and learn so much,” Ms. Taylor said.
New hires will need support from the practice to get comfortable with rheumatology, Dr. Stamatos said. Responsibility should come in gradual steps.
Instead of loading an NP with 20 patients a day, 2 or 3 patients in the first quarter, eventually graduating to 6-8 patients is a more realistic expectation, Dr. Stamatos advised.
Shadowing the Physician
Partnerships with physicians is a critical component to this onboarding process.
A nurse practitioner recently hired at Dr. Stamatos’ practice works alongside a physician to manage a panel of 25 patients. “We make sure she gets her training, the resources she needs. I personally meet with her to make sure her education is moving forward, connecting her with radiology, pulmonary, hematology,” and other areas of the practice relevant to her training, she added.
The NP also attends weekly grand rounds and case conferences with the fellows. This is the type of well-rounded support any APP needs, she stressed. “Without proper training, you lose people.”
At Sarasota Arthritis Center, NPs help cover the suites but also get assigned to specific physicians so that they can familiarize themselves with that physician’s panel of patients.
“When we start an APP, they shadow for about twice as long as a new physician would. Usually, they’re shadowing for about 6 weeks, just kind of learning the space. There’s a lot of nurse practitioners or PAs who may not have prior rheumatology experience, so we’re essentially training them from the ground up on rheumatology,” Ms. Yonker said.
Pairing them with one provider often directs what type of disease state they focus on, she continued. This dynamic relationship helps guide decisions on whether to include these NPs in the care of patients with more complex diseases.
At least in her practice, the NPs do not see any new patients. They are simply part of the larger care team. “That’s kind of how we present it to our patients, and it makes them feel more comfortable just because they know that they’re not necessarily being handed off to somebody — that the doctor is still overseeing their care,” Ms. Yonker said.
At the same time, the NPs know that they’re supported, that they too have access to tools and mentorship if they need it, she added.
The new NP at Carondelet Rheumatology piggybacked on the doctor’s schedule for 3 months, slowly taking on infusion patients so she could get familiar with their diseases and respective drugs. Eventually, she got her own schedule and was able to take on new patients.
It’s a team effort, Ms. Taylor noted. The NP does the preliminary workup and then the physician comes in and greets the new patient. Together, they develop a follow-up plan for the patient.
Education Resources for Practices
In the case of Dr. Box’s one-physician practice, he was looking for an NP who was willing to be independent and cover things in his absence. “The training has to be there to accomplish that,” said Dr. Box, who likened the training of APPs to a medical residency.
Encouraging them to ask questions, do continuing medical education online and outside reading, are important steps, he added.
In a recent editorial, rheumatologists Eli M. Miloslavsky, MD, and Bethany Marston, MD, offered some strategies for better prepping the APP workforce to meet the demands of rheumatology practices. “Consideration should be given to formal curricula or training programs to help APPs achieve both competence and confidence in treating rheumatologic conditions,” they offered, suggesting an online curriculum developed by the ACR for such a purpose. Fellowship training should also focus on working effectively with APPs, they added.
“Finally, incorporating APPs more effectively into rheumatology professional societies and supporting practices in hiring and training APPs will all be important steps in addressing the rheumatology workforce shortage,” Dr. Miloslavsky and Dr. Marston wrote.
Ms. Yonker said all her APPs take various courses that the ACR and other organizations provide for rheumatology-specific, midlevel positions. “We provide as much training as possible for them to feel comfortable in this space. They are set directly with a physician for a long time and then eventually go into their own space.”
In addition to ACR, the Rheumatology Nurses Society and the Association of Women in Rheumatology offer excellent online training resources for APPs, Ms. Yonker said. “Also, the Bone Health and Osteoporosis Foundation offers an osteoporosis fracture liaison certification which we put APPs through as well,” she added.
Rheumatology practices should also look into an important clinical training grant program from the Rheumatology Research Foundation, Dr. Stamatos advised.
To date, they have “funded almost everyone that applies,” she said. Each grantee receives $25,000 to support training and education involved in onboarding an APP to a rheumatology practice. The money covers attendance at a live rheumatology conference, online educational programs, textbooks, and any society memberships while defraying the cost of training this employee. To increase awareness of the program, the foundation has since expanded the number of available submission dates and the number of grant awardees per year. Currently, the application deadlines for the grants are December 1 and March 1.
For her own health system, Dr. Stamatos has been working on a rheumatology fellowship program for APPs. Through simulation labs, leadership exercises, and other activities, these APPs will learn how to transition from being a new provider to someone who can become part of a practice, she said.
APPs themselves can also get proactive in this learning cycle, Ms. Swafford said. In her view, both APPs and rheumatologists should be conducting didactic lectures and organizing elective rotations with medical students to get them excited about the field. This would establish a good education base that would encourage PAs and NPs to choose rheumatology.
“That’s a huge thing that’s probably missing,” Ms. Swafford said.
Buy-in From the Doctor
No recruitment effort is going to work if the rheumatologists in the practice aren’t committed to the model of having an APP, Ms. Yonker said. “Everybody wants to know their purpose in their company and that they’re valued and they’re needed. And so, I think a pitfall would be if your rheumatologist is not sold on the model of expanding the care team. Because this takes work on behalf of the doctor.”
Rheumatologists are very busy, so it’s a hard sell for them to take time out of their busy clinics to train somebody to do a good job taking care of their patients, Ms. Taylor agreed. “I think that we need the physicians that have had success with this and allow them to coach the physicians that are still resistant.”
In his small practice, Dr. Box has encouraged his NP to assist with practice improvements, working with the office manager. These workers are providers and need to be treated as such, he said. “They need to feel like they contribute to the practice more than just grinding through patients.”
Peer support is another successful ingredient for these workers. Ms. Taylor’s NP finds the time to commiserate with her fellow nurse practitioners — other rheumatology nurses who are also learning the ropes. Rheumatologists are smart, and they can be very intimidating, Ms. Taylor said. In their small office, the rheumatologist is her only peer.
“She likes to get out and sort of integrate with other nurse practitioners that are learning too.”
When APPs Make a Difference
Practices that take on APPs are reporting positive metrics — mainly, shorter wait times for patients. Ms. Yonker’s physicians have been able to add on one to two new patients a day. Wait times have since dwindled from a 5-month to a 3-month wait with the addition of the NPs. “Three months is still long, but we’re working on getting it to that ideal 6-week wait period, which we’re hoping we can accomplish. So we’re able to get more new patients in for sure,” she said.
Prior to hiring an NP, Ms. Taylor’s practice had to defer acceptances for new patients by at least a year. Now, they’re able to accept about half of all new patient referrals. With the NP on board, “We can get them in within 30 days,” she said.
Sometimes, an APP will go beyond their scope of work to make a difference and better support patients.
Patients with rheumatic and osteopathic conditions are often underdiagnosed in the primary care space. As a result, they are not treated as often as they should be. Seeing a need for specialty care, Ms. Swafford took action.
She currently runs the only bone health clinic in southwest Michigan, coordinating with rheumatologists, NPs, urgent care, hospitalists, and interventional radiologists to attend to these patients more quickly and reduce wait times for care. Specialists will flag things such as nontraumatic hip fractures and vertebral fractures and refer them to Ms. Swafford’s clinic, which is part of Bronson Rheumatology Specialists.
The clinic gets quite a few referrals, and the practice is growing. “Usually, they don’t take as long as a rheumatology referral for a workup, so we can see them a little bit quicker,” usually within 3 weeks, she added.
APPs have an opportunity to make their mark in rheumatology at a time when the profession is experiencing significant gaps in care, Ms. Swafford continued. “Unless we find a way to fill that niche, we’re going to be in a world of trouble in the next 10, 20 years.”
None of the sources reported any disclosures or conflicts of interest.
Once considered a luxury, hiring a nurse, nurse practitioner, or physician assistant is becoming a necessity in many rheumatology practices.
Seeing the wait lists pile up in her Florida practice, Stacy Yonker, MBA, chief executive officer of Sarasota Arthritis Center, knew she had to make some changes. “Everyone’s aging in the boomer generations. Particularly in Florida, we have a lot of people who retire here. In the more southern demographics, it is a very difficult challenge for practices to get new patients in,” she said.
Ms. Yonker is in the process of hiring several nurse practitioners (NPs) to assist in the clinics and infusion suites, lightening the load for the practice’s 11 rheumatologists.
Hiring an advanced practice provider (APP) to support the practice is just a first step. Getting these additional personnel up to speed means an investment in education and fostering good working relationships with NPs, PAs, and the staff’s physicians. Even more importantly, practices need to set realistic expectations on workload for these new hires.
“I tried to hire them, but I couldn’t keep them,” is a statement Christine A. Stamatos, DNP, ANP-C, hears all the time from rheumatologists. Oftentimes it’s because the practice saddles the new hire with 20 patients a day, said Dr. Stamatos, director of the Fibromyalgia Wellness Center within the division of rheumatology at Northwell Health in Huntington, New York. She is also an assistant professor at Hofstra Northwell School of Graduate Nursing and Physician Assistant Studies in Hempstead, New York.
“Twenty patients a day is too much,” Dr. Stamatos said. Overload someone, and they won’t stay. Offer them the support, mentoring, and tools they need to practice in their setting — and they will.
Why the Profession Needs APPs
Rheumatology is a much smaller specialty than most, with only a set number of rheumatologists in the field that can provide care to patients. A growing shortage is also looming. Reports from the American College of Rheumatology have projected troubling shortfalls in rheumatologists over the next decade in all regions of the United States.
Many of them aging into retirement “poses a significant issue on being able to continue providing care for the population that experiences the rheumatic disease,” said Ms. Yonker, a director of the National Organization of Rheumatology Management (NORM), a forum that promotes education and advocacy for rheumatology practice managers. People are also living longer, which means more patients are developing arthritis and autoimmune diseases.
Julia M. Swafford, PA-C, a rheumatology physician assistant in Battle Creek, Michigan, sees many advantages of hiring NPs and PAs, and not just from a financial perspective.
Salaries for PAs and NPs aren’t as high and they’re also more accessible than a rheumatologist. “You could train an NP or PA a lot quicker during that same time frame it would take to find a new rheumatology provider,” she offered. And while they may not be as experienced as rheumatologists, “you can kind of mold me on how you like to practice, what medications you may like to use, how you like to treat your patients,” Ms. Swafford said.
Hiring Someone With Experience
Recruiting and retaining APPs is not without its challenges.
Finding individuals compatible with this specialty isn’t easy, noted Mark Box, MD, medical director of Carondelet Rheumatology in Kansas City, Missouri. Ideally, APPs should be inquisitive, compassionate, and ready to learn. “Rheumatology is a cognitive specialty where you have to fit many pieces together. You need an APP who wants to embrace that,” he said.
The profession isn’t that “sexy” either, noted Katie Taylor, Carondelet’s practice manager. Patients are often in head-to-toe pain, and miserable. Many have been to other specialists without answers to their questions. For these reasons, rheumatology can be a hard sell for some PAs and NPs.
Nurse practitioners aren’t always comfortable with administering things such as controlled medications, for example. “It’s a hard patient population, and it’s a specialty of exclusion. You’ve got to be really smart to understand our diseases and our processes and our drugs,” Ms. Taylor said. In other words, it’s a difficult environment for an NP to walk into if their previous experience has been limited to upper respiratory issues and urinary tract infections in the primary care setting.
When hiring an APP, rheumatologists should look for someone who demonstrates an interest in lifelong learning, because the field is changing every day. They should exhibit good scores in educational training and have experience working in an emergency department or another field that translates well into rheumatology such as critical care, immunology, hematology, and orthopedics, she said.
Carondelet Rheumatology was specifically looking for an NP with rheumatology experience to support Dr. Box’s solo practice.
He was facing enormous pressure to be in the office every single day of the week. The practice had to cancel patients for its infusion suite on a regular basis when he was out of the office, Ms. Taylor said. “We couldn’t see new patients, and he wasn’t able to touch as many patients as he wanted to. The doctor takes the oath of touching as many in your community as possible, and you’re limited when you’re a one-man show.”
The practice eventually found an NP who already knew how to do joint injections. “We started her with easier diagnoses for things like osteoporosis and gout. She had an orthopedic background, so she was familiar with some of those diseases,” she said.
Even so, she often leaves with questions every day. “It’s a commitment for her to understand and learn so much,” Ms. Taylor said.
New hires will need support from the practice to get comfortable with rheumatology, Dr. Stamatos said. Responsibility should come in gradual steps.
Instead of loading an NP with 20 patients a day, 2 or 3 patients in the first quarter, eventually graduating to 6-8 patients is a more realistic expectation, Dr. Stamatos advised.
Shadowing the Physician
Partnerships with physicians is a critical component to this onboarding process.
A nurse practitioner recently hired at Dr. Stamatos’ practice works alongside a physician to manage a panel of 25 patients. “We make sure she gets her training, the resources she needs. I personally meet with her to make sure her education is moving forward, connecting her with radiology, pulmonary, hematology,” and other areas of the practice relevant to her training, she added.
The NP also attends weekly grand rounds and case conferences with the fellows. This is the type of well-rounded support any APP needs, she stressed. “Without proper training, you lose people.”
At Sarasota Arthritis Center, NPs help cover the suites but also get assigned to specific physicians so that they can familiarize themselves with that physician’s panel of patients.
“When we start an APP, they shadow for about twice as long as a new physician would. Usually, they’re shadowing for about 6 weeks, just kind of learning the space. There’s a lot of nurse practitioners or PAs who may not have prior rheumatology experience, so we’re essentially training them from the ground up on rheumatology,” Ms. Yonker said.
Pairing them with one provider often directs what type of disease state they focus on, she continued. This dynamic relationship helps guide decisions on whether to include these NPs in the care of patients with more complex diseases.
At least in her practice, the NPs do not see any new patients. They are simply part of the larger care team. “That’s kind of how we present it to our patients, and it makes them feel more comfortable just because they know that they’re not necessarily being handed off to somebody — that the doctor is still overseeing their care,” Ms. Yonker said.
At the same time, the NPs know that they’re supported, that they too have access to tools and mentorship if they need it, she added.
The new NP at Carondelet Rheumatology piggybacked on the doctor’s schedule for 3 months, slowly taking on infusion patients so she could get familiar with their diseases and respective drugs. Eventually, she got her own schedule and was able to take on new patients.
It’s a team effort, Ms. Taylor noted. The NP does the preliminary workup and then the physician comes in and greets the new patient. Together, they develop a follow-up plan for the patient.
Education Resources for Practices
In the case of Dr. Box’s one-physician practice, he was looking for an NP who was willing to be independent and cover things in his absence. “The training has to be there to accomplish that,” said Dr. Box, who likened the training of APPs to a medical residency.
Encouraging them to ask questions, do continuing medical education online and outside reading, are important steps, he added.
In a recent editorial, rheumatologists Eli M. Miloslavsky, MD, and Bethany Marston, MD, offered some strategies for better prepping the APP workforce to meet the demands of rheumatology practices. “Consideration should be given to formal curricula or training programs to help APPs achieve both competence and confidence in treating rheumatologic conditions,” they offered, suggesting an online curriculum developed by the ACR for such a purpose. Fellowship training should also focus on working effectively with APPs, they added.
“Finally, incorporating APPs more effectively into rheumatology professional societies and supporting practices in hiring and training APPs will all be important steps in addressing the rheumatology workforce shortage,” Dr. Miloslavsky and Dr. Marston wrote.
Ms. Yonker said all her APPs take various courses that the ACR and other organizations provide for rheumatology-specific, midlevel positions. “We provide as much training as possible for them to feel comfortable in this space. They are set directly with a physician for a long time and then eventually go into their own space.”
In addition to ACR, the Rheumatology Nurses Society and the Association of Women in Rheumatology offer excellent online training resources for APPs, Ms. Yonker said. “Also, the Bone Health and Osteoporosis Foundation offers an osteoporosis fracture liaison certification which we put APPs through as well,” she added.
Rheumatology practices should also look into an important clinical training grant program from the Rheumatology Research Foundation, Dr. Stamatos advised.
To date, they have “funded almost everyone that applies,” she said. Each grantee receives $25,000 to support training and education involved in onboarding an APP to a rheumatology practice. The money covers attendance at a live rheumatology conference, online educational programs, textbooks, and any society memberships while defraying the cost of training this employee. To increase awareness of the program, the foundation has since expanded the number of available submission dates and the number of grant awardees per year. Currently, the application deadlines for the grants are December 1 and March 1.
For her own health system, Dr. Stamatos has been working on a rheumatology fellowship program for APPs. Through simulation labs, leadership exercises, and other activities, these APPs will learn how to transition from being a new provider to someone who can become part of a practice, she said.
APPs themselves can also get proactive in this learning cycle, Ms. Swafford said. In her view, both APPs and rheumatologists should be conducting didactic lectures and organizing elective rotations with medical students to get them excited about the field. This would establish a good education base that would encourage PAs and NPs to choose rheumatology.
“That’s a huge thing that’s probably missing,” Ms. Swafford said.
Buy-in From the Doctor
No recruitment effort is going to work if the rheumatologists in the practice aren’t committed to the model of having an APP, Ms. Yonker said. “Everybody wants to know their purpose in their company and that they’re valued and they’re needed. And so, I think a pitfall would be if your rheumatologist is not sold on the model of expanding the care team. Because this takes work on behalf of the doctor.”
Rheumatologists are very busy, so it’s a hard sell for them to take time out of their busy clinics to train somebody to do a good job taking care of their patients, Ms. Taylor agreed. “I think that we need the physicians that have had success with this and allow them to coach the physicians that are still resistant.”
In his small practice, Dr. Box has encouraged his NP to assist with practice improvements, working with the office manager. These workers are providers and need to be treated as such, he said. “They need to feel like they contribute to the practice more than just grinding through patients.”
Peer support is another successful ingredient for these workers. Ms. Taylor’s NP finds the time to commiserate with her fellow nurse practitioners — other rheumatology nurses who are also learning the ropes. Rheumatologists are smart, and they can be very intimidating, Ms. Taylor said. In their small office, the rheumatologist is her only peer.
“She likes to get out and sort of integrate with other nurse practitioners that are learning too.”
When APPs Make a Difference
Practices that take on APPs are reporting positive metrics — mainly, shorter wait times for patients. Ms. Yonker’s physicians have been able to add on one to two new patients a day. Wait times have since dwindled from a 5-month to a 3-month wait with the addition of the NPs. “Three months is still long, but we’re working on getting it to that ideal 6-week wait period, which we’re hoping we can accomplish. So we’re able to get more new patients in for sure,” she said.
Prior to hiring an NP, Ms. Taylor’s practice had to defer acceptances for new patients by at least a year. Now, they’re able to accept about half of all new patient referrals. With the NP on board, “We can get them in within 30 days,” she said.
Sometimes, an APP will go beyond their scope of work to make a difference and better support patients.
Patients with rheumatic and osteopathic conditions are often underdiagnosed in the primary care space. As a result, they are not treated as often as they should be. Seeing a need for specialty care, Ms. Swafford took action.
She currently runs the only bone health clinic in southwest Michigan, coordinating with rheumatologists, NPs, urgent care, hospitalists, and interventional radiologists to attend to these patients more quickly and reduce wait times for care. Specialists will flag things such as nontraumatic hip fractures and vertebral fractures and refer them to Ms. Swafford’s clinic, which is part of Bronson Rheumatology Specialists.
The clinic gets quite a few referrals, and the practice is growing. “Usually, they don’t take as long as a rheumatology referral for a workup, so we can see them a little bit quicker,” usually within 3 weeks, she added.
APPs have an opportunity to make their mark in rheumatology at a time when the profession is experiencing significant gaps in care, Ms. Swafford continued. “Unless we find a way to fill that niche, we’re going to be in a world of trouble in the next 10, 20 years.”
None of the sources reported any disclosures or conflicts of interest.
Once considered a luxury, hiring a nurse, nurse practitioner, or physician assistant is becoming a necessity in many rheumatology practices.
Seeing the wait lists pile up in her Florida practice, Stacy Yonker, MBA, chief executive officer of Sarasota Arthritis Center, knew she had to make some changes. “Everyone’s aging in the boomer generations. Particularly in Florida, we have a lot of people who retire here. In the more southern demographics, it is a very difficult challenge for practices to get new patients in,” she said.
Ms. Yonker is in the process of hiring several nurse practitioners (NPs) to assist in the clinics and infusion suites, lightening the load for the practice’s 11 rheumatologists.
Hiring an advanced practice provider (APP) to support the practice is just a first step. Getting these additional personnel up to speed means an investment in education and fostering good working relationships with NPs, PAs, and the staff’s physicians. Even more importantly, practices need to set realistic expectations on workload for these new hires.
“I tried to hire them, but I couldn’t keep them,” is a statement Christine A. Stamatos, DNP, ANP-C, hears all the time from rheumatologists. Oftentimes it’s because the practice saddles the new hire with 20 patients a day, said Dr. Stamatos, director of the Fibromyalgia Wellness Center within the division of rheumatology at Northwell Health in Huntington, New York. She is also an assistant professor at Hofstra Northwell School of Graduate Nursing and Physician Assistant Studies in Hempstead, New York.
“Twenty patients a day is too much,” Dr. Stamatos said. Overload someone, and they won’t stay. Offer them the support, mentoring, and tools they need to practice in their setting — and they will.
Why the Profession Needs APPs
Rheumatology is a much smaller specialty than most, with only a set number of rheumatologists in the field that can provide care to patients. A growing shortage is also looming. Reports from the American College of Rheumatology have projected troubling shortfalls in rheumatologists over the next decade in all regions of the United States.
Many of them aging into retirement “poses a significant issue on being able to continue providing care for the population that experiences the rheumatic disease,” said Ms. Yonker, a director of the National Organization of Rheumatology Management (NORM), a forum that promotes education and advocacy for rheumatology practice managers. People are also living longer, which means more patients are developing arthritis and autoimmune diseases.
Julia M. Swafford, PA-C, a rheumatology physician assistant in Battle Creek, Michigan, sees many advantages of hiring NPs and PAs, and not just from a financial perspective.
Salaries for PAs and NPs aren’t as high and they’re also more accessible than a rheumatologist. “You could train an NP or PA a lot quicker during that same time frame it would take to find a new rheumatology provider,” she offered. And while they may not be as experienced as rheumatologists, “you can kind of mold me on how you like to practice, what medications you may like to use, how you like to treat your patients,” Ms. Swafford said.
Hiring Someone With Experience
Recruiting and retaining APPs is not without its challenges.
Finding individuals compatible with this specialty isn’t easy, noted Mark Box, MD, medical director of Carondelet Rheumatology in Kansas City, Missouri. Ideally, APPs should be inquisitive, compassionate, and ready to learn. “Rheumatology is a cognitive specialty where you have to fit many pieces together. You need an APP who wants to embrace that,” he said.
The profession isn’t that “sexy” either, noted Katie Taylor, Carondelet’s practice manager. Patients are often in head-to-toe pain, and miserable. Many have been to other specialists without answers to their questions. For these reasons, rheumatology can be a hard sell for some PAs and NPs.
Nurse practitioners aren’t always comfortable with administering things such as controlled medications, for example. “It’s a hard patient population, and it’s a specialty of exclusion. You’ve got to be really smart to understand our diseases and our processes and our drugs,” Ms. Taylor said. In other words, it’s a difficult environment for an NP to walk into if their previous experience has been limited to upper respiratory issues and urinary tract infections in the primary care setting.
When hiring an APP, rheumatologists should look for someone who demonstrates an interest in lifelong learning, because the field is changing every day. They should exhibit good scores in educational training and have experience working in an emergency department or another field that translates well into rheumatology such as critical care, immunology, hematology, and orthopedics, she said.
Carondelet Rheumatology was specifically looking for an NP with rheumatology experience to support Dr. Box’s solo practice.
He was facing enormous pressure to be in the office every single day of the week. The practice had to cancel patients for its infusion suite on a regular basis when he was out of the office, Ms. Taylor said. “We couldn’t see new patients, and he wasn’t able to touch as many patients as he wanted to. The doctor takes the oath of touching as many in your community as possible, and you’re limited when you’re a one-man show.”
The practice eventually found an NP who already knew how to do joint injections. “We started her with easier diagnoses for things like osteoporosis and gout. She had an orthopedic background, so she was familiar with some of those diseases,” she said.
Even so, she often leaves with questions every day. “It’s a commitment for her to understand and learn so much,” Ms. Taylor said.
New hires will need support from the practice to get comfortable with rheumatology, Dr. Stamatos said. Responsibility should come in gradual steps.
Instead of loading an NP with 20 patients a day, 2 or 3 patients in the first quarter, eventually graduating to 6-8 patients is a more realistic expectation, Dr. Stamatos advised.
Shadowing the Physician
Partnerships with physicians is a critical component to this onboarding process.
A nurse practitioner recently hired at Dr. Stamatos’ practice works alongside a physician to manage a panel of 25 patients. “We make sure she gets her training, the resources she needs. I personally meet with her to make sure her education is moving forward, connecting her with radiology, pulmonary, hematology,” and other areas of the practice relevant to her training, she added.
The NP also attends weekly grand rounds and case conferences with the fellows. This is the type of well-rounded support any APP needs, she stressed. “Without proper training, you lose people.”
At Sarasota Arthritis Center, NPs help cover the suites but also get assigned to specific physicians so that they can familiarize themselves with that physician’s panel of patients.
“When we start an APP, they shadow for about twice as long as a new physician would. Usually, they’re shadowing for about 6 weeks, just kind of learning the space. There’s a lot of nurse practitioners or PAs who may not have prior rheumatology experience, so we’re essentially training them from the ground up on rheumatology,” Ms. Yonker said.
Pairing them with one provider often directs what type of disease state they focus on, she continued. This dynamic relationship helps guide decisions on whether to include these NPs in the care of patients with more complex diseases.
At least in her practice, the NPs do not see any new patients. They are simply part of the larger care team. “That’s kind of how we present it to our patients, and it makes them feel more comfortable just because they know that they’re not necessarily being handed off to somebody — that the doctor is still overseeing their care,” Ms. Yonker said.
At the same time, the NPs know that they’re supported, that they too have access to tools and mentorship if they need it, she added.
The new NP at Carondelet Rheumatology piggybacked on the doctor’s schedule for 3 months, slowly taking on infusion patients so she could get familiar with their diseases and respective drugs. Eventually, she got her own schedule and was able to take on new patients.
It’s a team effort, Ms. Taylor noted. The NP does the preliminary workup and then the physician comes in and greets the new patient. Together, they develop a follow-up plan for the patient.
Education Resources for Practices
In the case of Dr. Box’s one-physician practice, he was looking for an NP who was willing to be independent and cover things in his absence. “The training has to be there to accomplish that,” said Dr. Box, who likened the training of APPs to a medical residency.
Encouraging them to ask questions, do continuing medical education online and outside reading, are important steps, he added.
In a recent editorial, rheumatologists Eli M. Miloslavsky, MD, and Bethany Marston, MD, offered some strategies for better prepping the APP workforce to meet the demands of rheumatology practices. “Consideration should be given to formal curricula or training programs to help APPs achieve both competence and confidence in treating rheumatologic conditions,” they offered, suggesting an online curriculum developed by the ACR for such a purpose. Fellowship training should also focus on working effectively with APPs, they added.
“Finally, incorporating APPs more effectively into rheumatology professional societies and supporting practices in hiring and training APPs will all be important steps in addressing the rheumatology workforce shortage,” Dr. Miloslavsky and Dr. Marston wrote.
Ms. Yonker said all her APPs take various courses that the ACR and other organizations provide for rheumatology-specific, midlevel positions. “We provide as much training as possible for them to feel comfortable in this space. They are set directly with a physician for a long time and then eventually go into their own space.”
In addition to ACR, the Rheumatology Nurses Society and the Association of Women in Rheumatology offer excellent online training resources for APPs, Ms. Yonker said. “Also, the Bone Health and Osteoporosis Foundation offers an osteoporosis fracture liaison certification which we put APPs through as well,” she added.
Rheumatology practices should also look into an important clinical training grant program from the Rheumatology Research Foundation, Dr. Stamatos advised.
To date, they have “funded almost everyone that applies,” she said. Each grantee receives $25,000 to support training and education involved in onboarding an APP to a rheumatology practice. The money covers attendance at a live rheumatology conference, online educational programs, textbooks, and any society memberships while defraying the cost of training this employee. To increase awareness of the program, the foundation has since expanded the number of available submission dates and the number of grant awardees per year. Currently, the application deadlines for the grants are December 1 and March 1.
For her own health system, Dr. Stamatos has been working on a rheumatology fellowship program for APPs. Through simulation labs, leadership exercises, and other activities, these APPs will learn how to transition from being a new provider to someone who can become part of a practice, she said.
APPs themselves can also get proactive in this learning cycle, Ms. Swafford said. In her view, both APPs and rheumatologists should be conducting didactic lectures and organizing elective rotations with medical students to get them excited about the field. This would establish a good education base that would encourage PAs and NPs to choose rheumatology.
“That’s a huge thing that’s probably missing,” Ms. Swafford said.
Buy-in From the Doctor
No recruitment effort is going to work if the rheumatologists in the practice aren’t committed to the model of having an APP, Ms. Yonker said. “Everybody wants to know their purpose in their company and that they’re valued and they’re needed. And so, I think a pitfall would be if your rheumatologist is not sold on the model of expanding the care team. Because this takes work on behalf of the doctor.”
Rheumatologists are very busy, so it’s a hard sell for them to take time out of their busy clinics to train somebody to do a good job taking care of their patients, Ms. Taylor agreed. “I think that we need the physicians that have had success with this and allow them to coach the physicians that are still resistant.”
In his small practice, Dr. Box has encouraged his NP to assist with practice improvements, working with the office manager. These workers are providers and need to be treated as such, he said. “They need to feel like they contribute to the practice more than just grinding through patients.”
Peer support is another successful ingredient for these workers. Ms. Taylor’s NP finds the time to commiserate with her fellow nurse practitioners — other rheumatology nurses who are also learning the ropes. Rheumatologists are smart, and they can be very intimidating, Ms. Taylor said. In their small office, the rheumatologist is her only peer.
“She likes to get out and sort of integrate with other nurse practitioners that are learning too.”
When APPs Make a Difference
Practices that take on APPs are reporting positive metrics — mainly, shorter wait times for patients. Ms. Yonker’s physicians have been able to add on one to two new patients a day. Wait times have since dwindled from a 5-month to a 3-month wait with the addition of the NPs. “Three months is still long, but we’re working on getting it to that ideal 6-week wait period, which we’re hoping we can accomplish. So we’re able to get more new patients in for sure,” she said.
Prior to hiring an NP, Ms. Taylor’s practice had to defer acceptances for new patients by at least a year. Now, they’re able to accept about half of all new patient referrals. With the NP on board, “We can get them in within 30 days,” she said.
Sometimes, an APP will go beyond their scope of work to make a difference and better support patients.
Patients with rheumatic and osteopathic conditions are often underdiagnosed in the primary care space. As a result, they are not treated as often as they should be. Seeing a need for specialty care, Ms. Swafford took action.
She currently runs the only bone health clinic in southwest Michigan, coordinating with rheumatologists, NPs, urgent care, hospitalists, and interventional radiologists to attend to these patients more quickly and reduce wait times for care. Specialists will flag things such as nontraumatic hip fractures and vertebral fractures and refer them to Ms. Swafford’s clinic, which is part of Bronson Rheumatology Specialists.
The clinic gets quite a few referrals, and the practice is growing. “Usually, they don’t take as long as a rheumatology referral for a workup, so we can see them a little bit quicker,” usually within 3 weeks, she added.
APPs have an opportunity to make their mark in rheumatology at a time when the profession is experiencing significant gaps in care, Ms. Swafford continued. “Unless we find a way to fill that niche, we’re going to be in a world of trouble in the next 10, 20 years.”
None of the sources reported any disclosures or conflicts of interest.
Testosterone Replacement May Cause ... Fracture?
This transcript has been edited for clarity.
I am showing you a graph without any labels.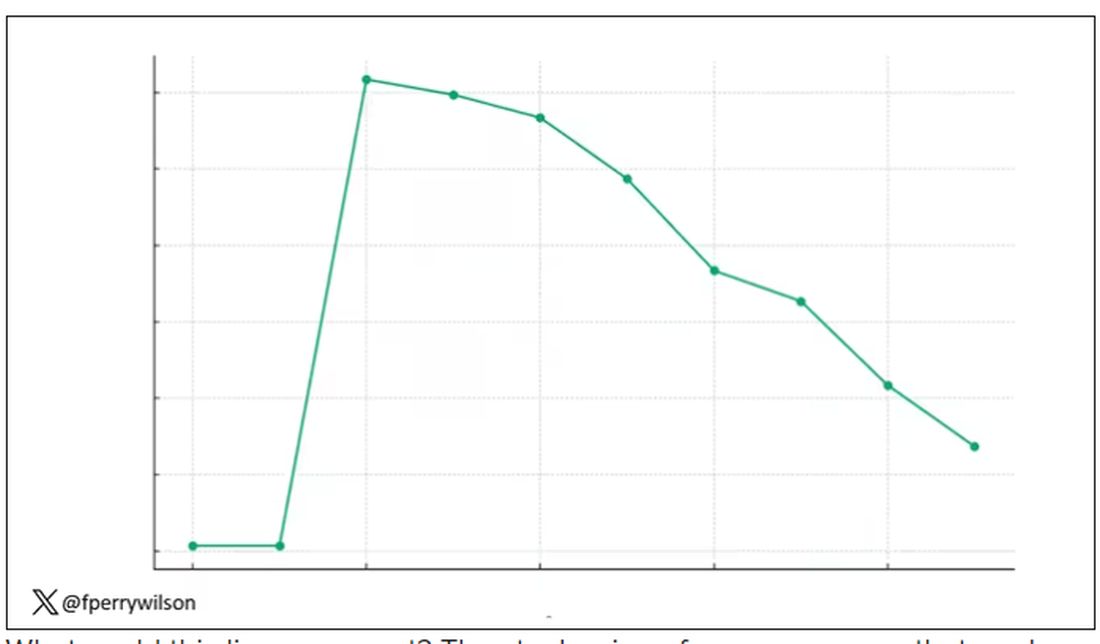
What could this line represent? The stock price of some company that made a big splash but failed to live up to expectations? An outbreak curve charting the introduction of a new infectious agent to a population? The performance of a viral tweet?
I’ll tell you what it is in a moment, but I wanted you to recognize that there is something inherently wistful in this shape, something that speaks of past glory and inevitable declines. It’s a graph that induces a feeling of resistance — no, do not go gently into that good night.
The graph actually represents (roughly) the normal level of serum testosterone in otherwise-healthy men as they age.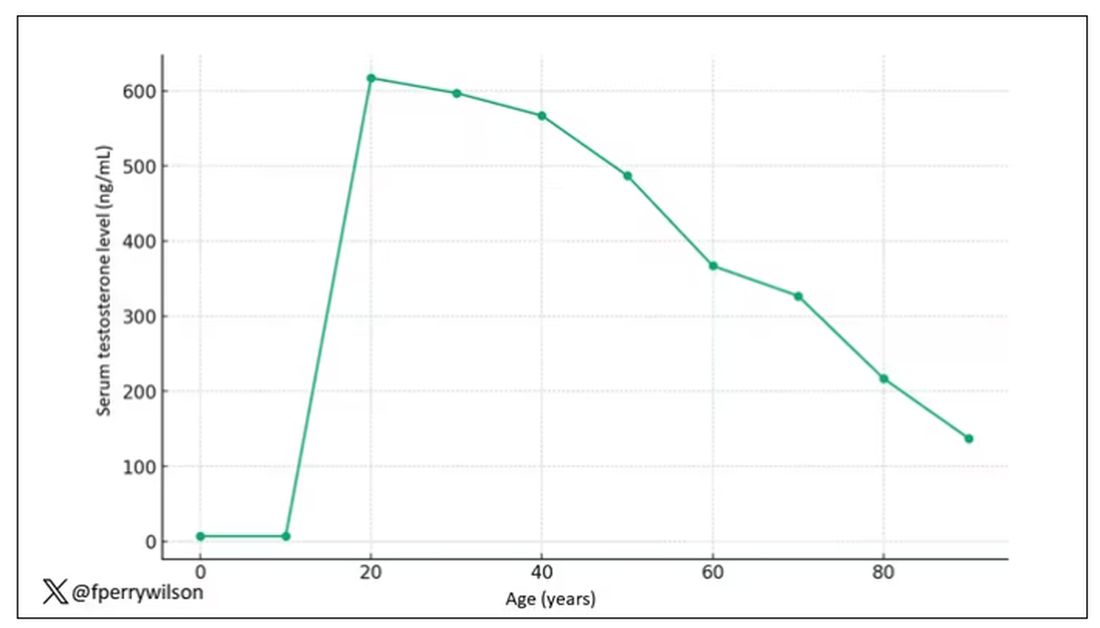
A caveat here: These numbers are not as well defined as I made them seem on this graph, particularly for those older than 65 years. But it is clear that testosterone levels decline with time, and the idea to supplement testosterone is hardly new. Like all treatments, testosterone supplementation has risks and benefits. Some risks are predictable, like exacerbating the symptoms of benign prostatic hyperplasia. Some risks seem to come completely out of left field. That’s what we have today, in a study suggesting that testosterone supplementation increases the risk for bone fractures.
Let me set the stage here by saying that nearly all prior research into the effects of testosterone supplementation has suggested that it is pretty good for bone health. It increases bone mineral density, bone strength, and improves bone architecture.
So if you were to do a randomized trial of testosterone supplementation and look at fracture risk in the testosterone group compared with the placebo group, you would expect the fracture risk would be much lower in those getting supplemented. Of course, this is why we actually do studies instead of assuming we know the answer already — because in this case, you’d be wrong.
I’m talking about this study, appearing in The New England Journal of Medicine.
It’s a prespecified secondary analysis of a randomized trial known as the TRAVERSE trial, which randomly assigned 5246 men with low testosterone levels to transdermal testosterone gel vs placebo. The primary goal of that trial was to assess the cardiovascular risk associated with testosterone supplementation, and the major take-home was that there was no difference in cardiovascular event rates between the testosterone and placebo groups.
This secondary analysis looked at fracture incidence. Researchers contacted participants multiple times in the first year of the study and yearly thereafter. Each time, they asked whether the participant had sustained a fracture. If they answered in the affirmative, a request for medical records was made and the researchers, still blinded to randomization status, adjudicated whether there was indeed a fracture or not, along with some details as to location, situation, and so on.
This was a big study, though, and that translates to just a 3.5% fracture rate in testosterone vs 2.5% in control, but the difference was statistically significant.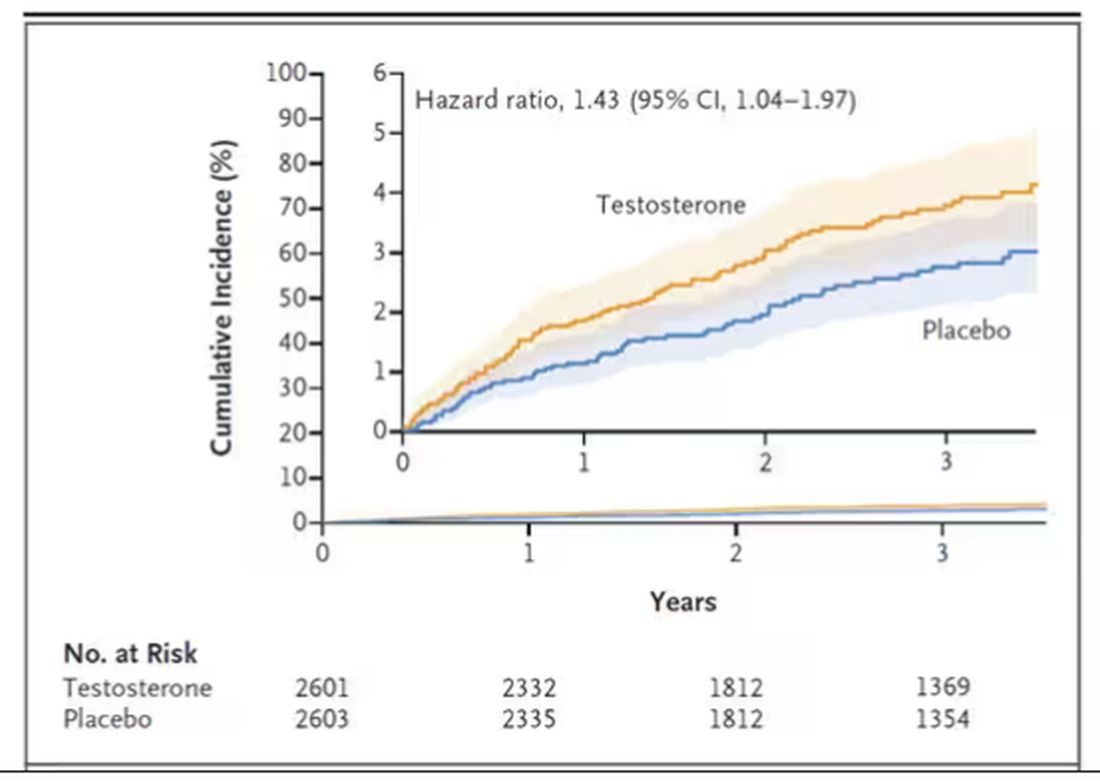
This difference persisted across various fracture types (non–high-impact fractures, for example) after excluding the small percentage of men taking osteoporosis medication.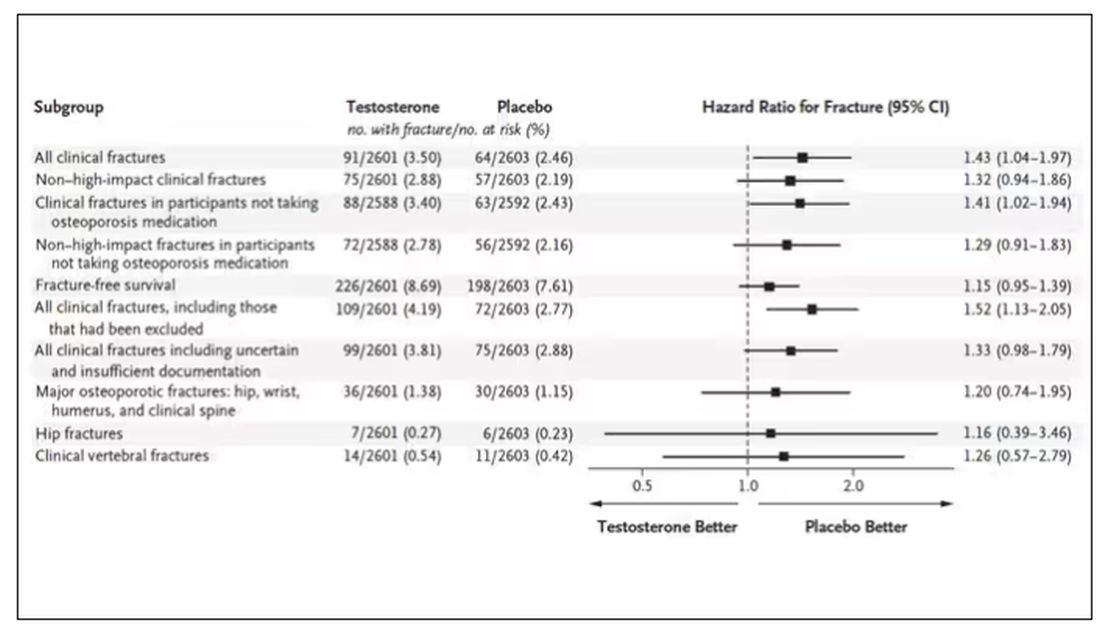
How does a drug that increases bone mineral density and bone strength increase the risk for fracture?
Well, one clue — and this was pointed out in a nice editorial by Matthis Grossman and Bradley Anawalt — is that the increased risk for fracture occurs quite soon after starting treatment, which is not consistent with direct bone effects. Rather, this might represent behavioral differences. Testosterone supplementation seems to increase energy levels; might it lead men to engage in activities that put them at higher risk for fracture?
Regardless of the cause, this adds to our knowledge about the rather complex mix of risks and benefits of testosterone supplementation and probably puts a bit more weight on the risks side. The truth is that testosterone levels do decline with age, as do many things, and it may not be appropriate to try to fight against that in all people. It’s worth noting that all of these studies use low levels of total serum testosterone as an entry criterion. But total testosterone is not what your body “sees.” It sees free testosterone, the portion not bound to sex hormone–binding globulin. And that binding protein is affected by lots of stuff — diabetes and obesity lower it, for example — making total testosterone levels seem low when free testosterone might be just fine.
In other words, testosterone supplementation is probably not terrible, but it is definitely not the cure for aging. In situations like this, we need better data to guide exactly who will benefit from the therapy and who will only be exposed to the risks.
Dr. Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Conn. He has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
I am showing you a graph without any labels.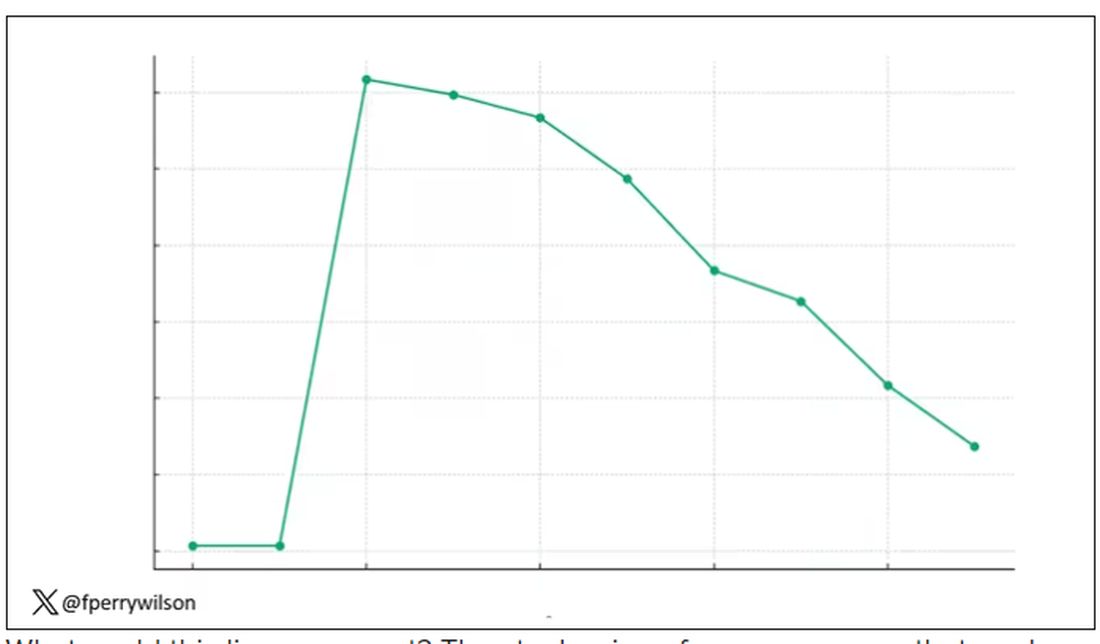
What could this line represent? The stock price of some company that made a big splash but failed to live up to expectations? An outbreak curve charting the introduction of a new infectious agent to a population? The performance of a viral tweet?
I’ll tell you what it is in a moment, but I wanted you to recognize that there is something inherently wistful in this shape, something that speaks of past glory and inevitable declines. It’s a graph that induces a feeling of resistance — no, do not go gently into that good night.
The graph actually represents (roughly) the normal level of serum testosterone in otherwise-healthy men as they age.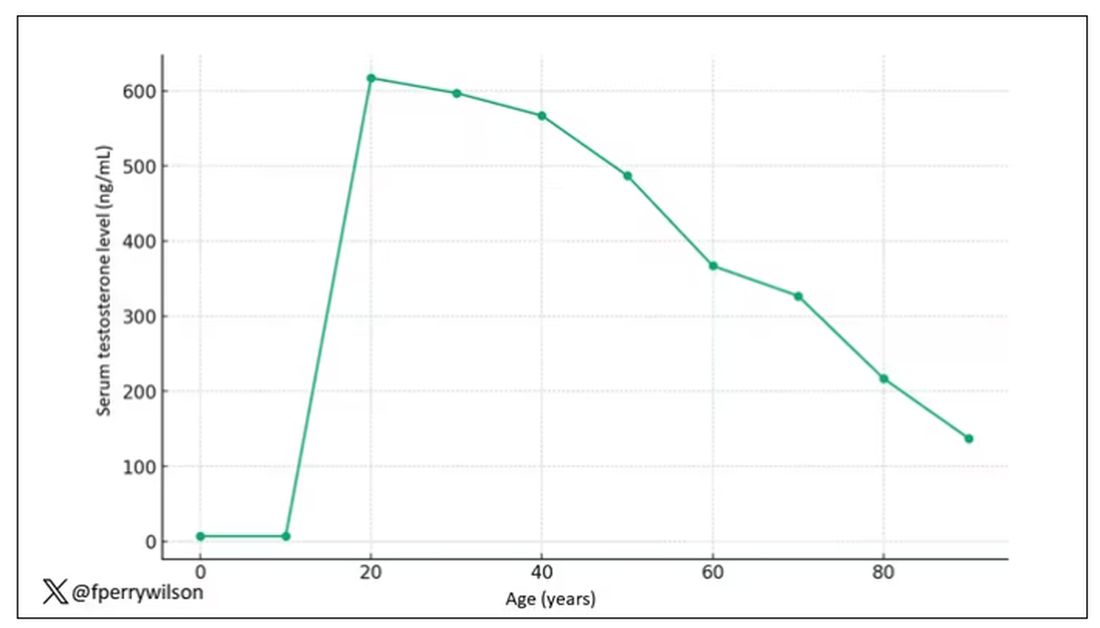
A caveat here: These numbers are not as well defined as I made them seem on this graph, particularly for those older than 65 years. But it is clear that testosterone levels decline with time, and the idea to supplement testosterone is hardly new. Like all treatments, testosterone supplementation has risks and benefits. Some risks are predictable, like exacerbating the symptoms of benign prostatic hyperplasia. Some risks seem to come completely out of left field. That’s what we have today, in a study suggesting that testosterone supplementation increases the risk for bone fractures.
Let me set the stage here by saying that nearly all prior research into the effects of testosterone supplementation has suggested that it is pretty good for bone health. It increases bone mineral density, bone strength, and improves bone architecture.
So if you were to do a randomized trial of testosterone supplementation and look at fracture risk in the testosterone group compared with the placebo group, you would expect the fracture risk would be much lower in those getting supplemented. Of course, this is why we actually do studies instead of assuming we know the answer already — because in this case, you’d be wrong.
I’m talking about this study, appearing in The New England Journal of Medicine.
It’s a prespecified secondary analysis of a randomized trial known as the TRAVERSE trial, which randomly assigned 5246 men with low testosterone levels to transdermal testosterone gel vs placebo. The primary goal of that trial was to assess the cardiovascular risk associated with testosterone supplementation, and the major take-home was that there was no difference in cardiovascular event rates between the testosterone and placebo groups.
This secondary analysis looked at fracture incidence. Researchers contacted participants multiple times in the first year of the study and yearly thereafter. Each time, they asked whether the participant had sustained a fracture. If they answered in the affirmative, a request for medical records was made and the researchers, still blinded to randomization status, adjudicated whether there was indeed a fracture or not, along with some details as to location, situation, and so on.
This was a big study, though, and that translates to just a 3.5% fracture rate in testosterone vs 2.5% in control, but the difference was statistically significant.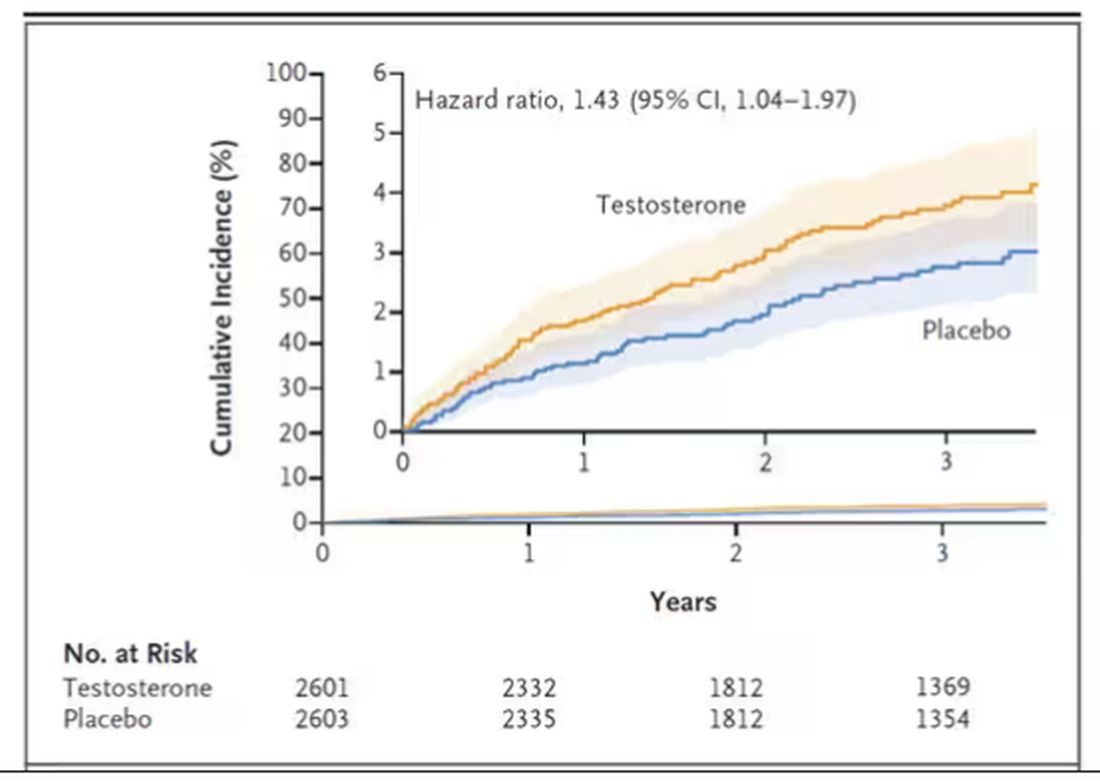
This difference persisted across various fracture types (non–high-impact fractures, for example) after excluding the small percentage of men taking osteoporosis medication.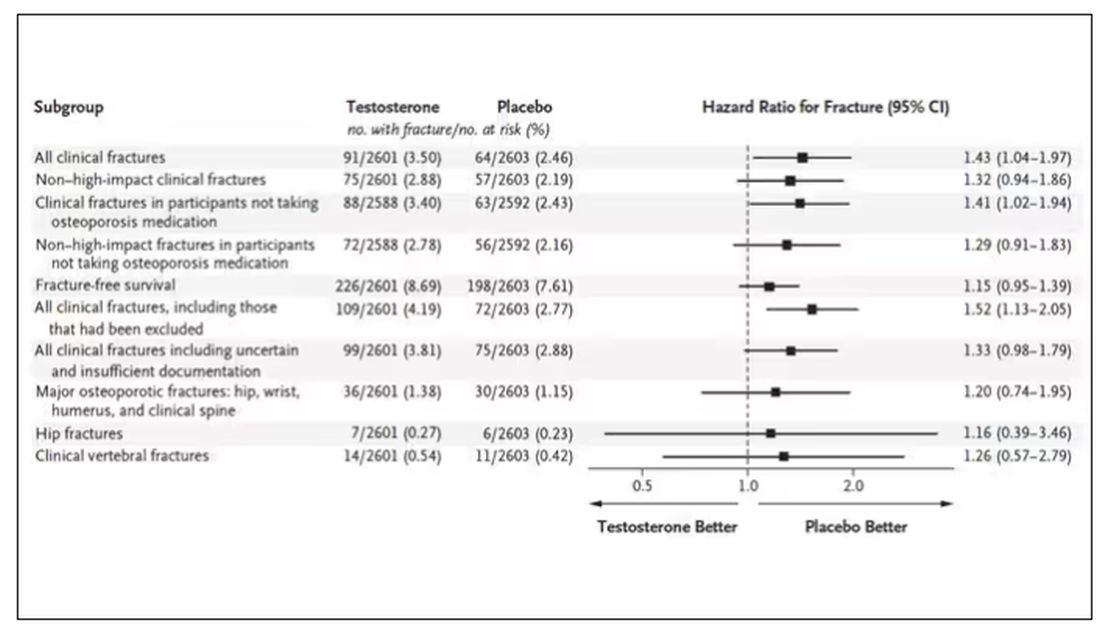
How does a drug that increases bone mineral density and bone strength increase the risk for fracture?
Well, one clue — and this was pointed out in a nice editorial by Matthis Grossman and Bradley Anawalt — is that the increased risk for fracture occurs quite soon after starting treatment, which is not consistent with direct bone effects. Rather, this might represent behavioral differences. Testosterone supplementation seems to increase energy levels; might it lead men to engage in activities that put them at higher risk for fracture?
Regardless of the cause, this adds to our knowledge about the rather complex mix of risks and benefits of testosterone supplementation and probably puts a bit more weight on the risks side. The truth is that testosterone levels do decline with age, as do many things, and it may not be appropriate to try to fight against that in all people. It’s worth noting that all of these studies use low levels of total serum testosterone as an entry criterion. But total testosterone is not what your body “sees.” It sees free testosterone, the portion not bound to sex hormone–binding globulin. And that binding protein is affected by lots of stuff — diabetes and obesity lower it, for example — making total testosterone levels seem low when free testosterone might be just fine.
In other words, testosterone supplementation is probably not terrible, but it is definitely not the cure for aging. In situations like this, we need better data to guide exactly who will benefit from the therapy and who will only be exposed to the risks.
Dr. Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Conn. He has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
I am showing you a graph without any labels.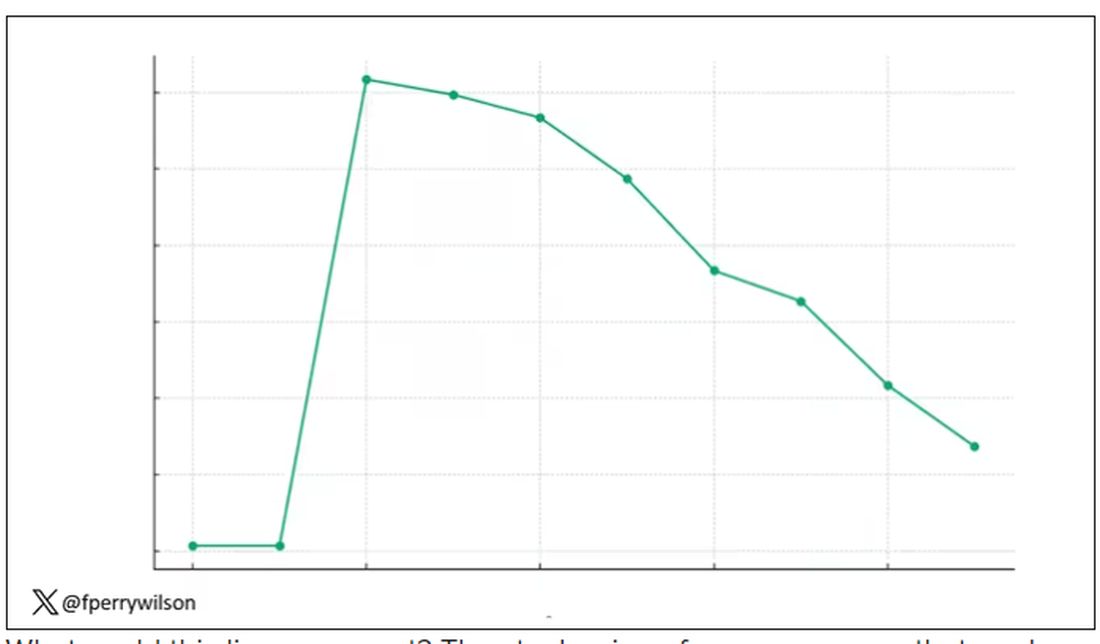
What could this line represent? The stock price of some company that made a big splash but failed to live up to expectations? An outbreak curve charting the introduction of a new infectious agent to a population? The performance of a viral tweet?
I’ll tell you what it is in a moment, but I wanted you to recognize that there is something inherently wistful in this shape, something that speaks of past glory and inevitable declines. It’s a graph that induces a feeling of resistance — no, do not go gently into that good night.
The graph actually represents (roughly) the normal level of serum testosterone in otherwise-healthy men as they age.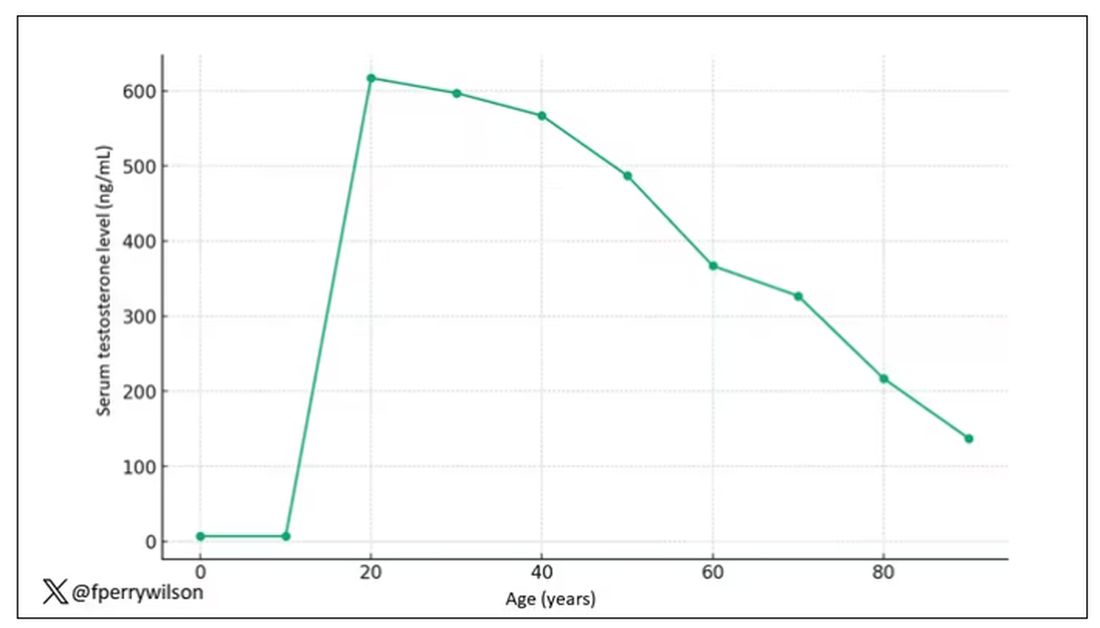
A caveat here: These numbers are not as well defined as I made them seem on this graph, particularly for those older than 65 years. But it is clear that testosterone levels decline with time, and the idea to supplement testosterone is hardly new. Like all treatments, testosterone supplementation has risks and benefits. Some risks are predictable, like exacerbating the symptoms of benign prostatic hyperplasia. Some risks seem to come completely out of left field. That’s what we have today, in a study suggesting that testosterone supplementation increases the risk for bone fractures.
Let me set the stage here by saying that nearly all prior research into the effects of testosterone supplementation has suggested that it is pretty good for bone health. It increases bone mineral density, bone strength, and improves bone architecture.
So if you were to do a randomized trial of testosterone supplementation and look at fracture risk in the testosterone group compared with the placebo group, you would expect the fracture risk would be much lower in those getting supplemented. Of course, this is why we actually do studies instead of assuming we know the answer already — because in this case, you’d be wrong.
I’m talking about this study, appearing in The New England Journal of Medicine.
It’s a prespecified secondary analysis of a randomized trial known as the TRAVERSE trial, which randomly assigned 5246 men with low testosterone levels to transdermal testosterone gel vs placebo. The primary goal of that trial was to assess the cardiovascular risk associated with testosterone supplementation, and the major take-home was that there was no difference in cardiovascular event rates between the testosterone and placebo groups.
This secondary analysis looked at fracture incidence. Researchers contacted participants multiple times in the first year of the study and yearly thereafter. Each time, they asked whether the participant had sustained a fracture. If they answered in the affirmative, a request for medical records was made and the researchers, still blinded to randomization status, adjudicated whether there was indeed a fracture or not, along with some details as to location, situation, and so on.
This was a big study, though, and that translates to just a 3.5% fracture rate in testosterone vs 2.5% in control, but the difference was statistically significant.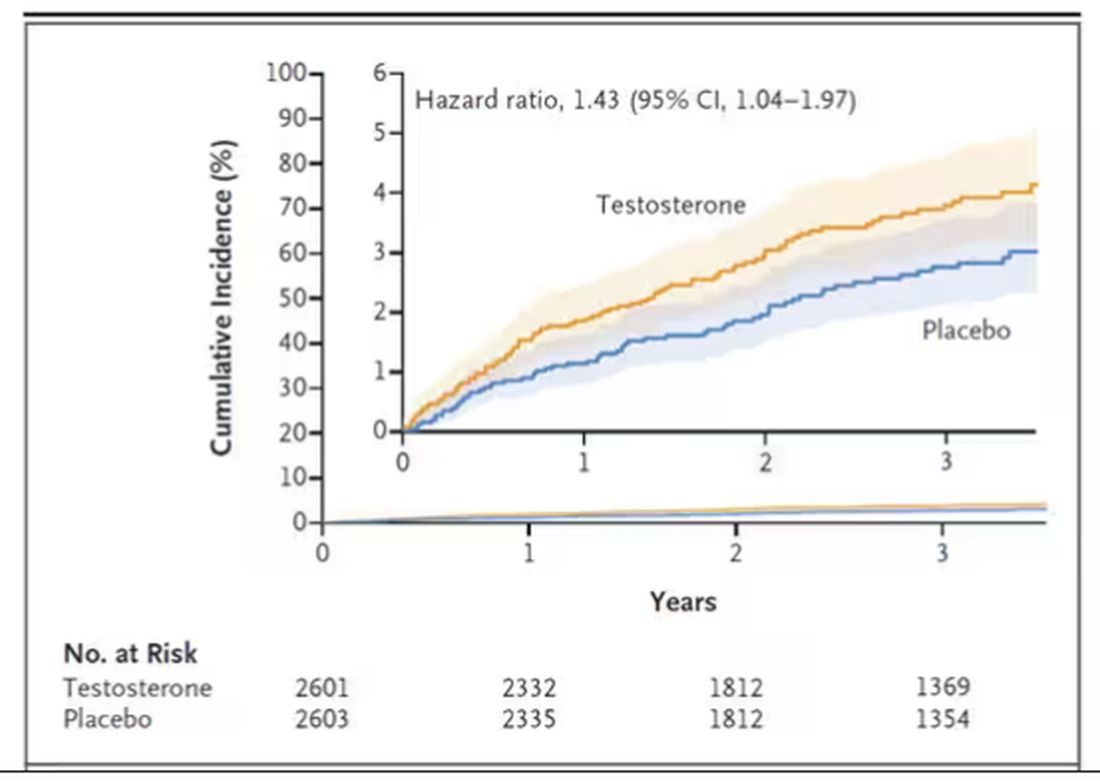
This difference persisted across various fracture types (non–high-impact fractures, for example) after excluding the small percentage of men taking osteoporosis medication.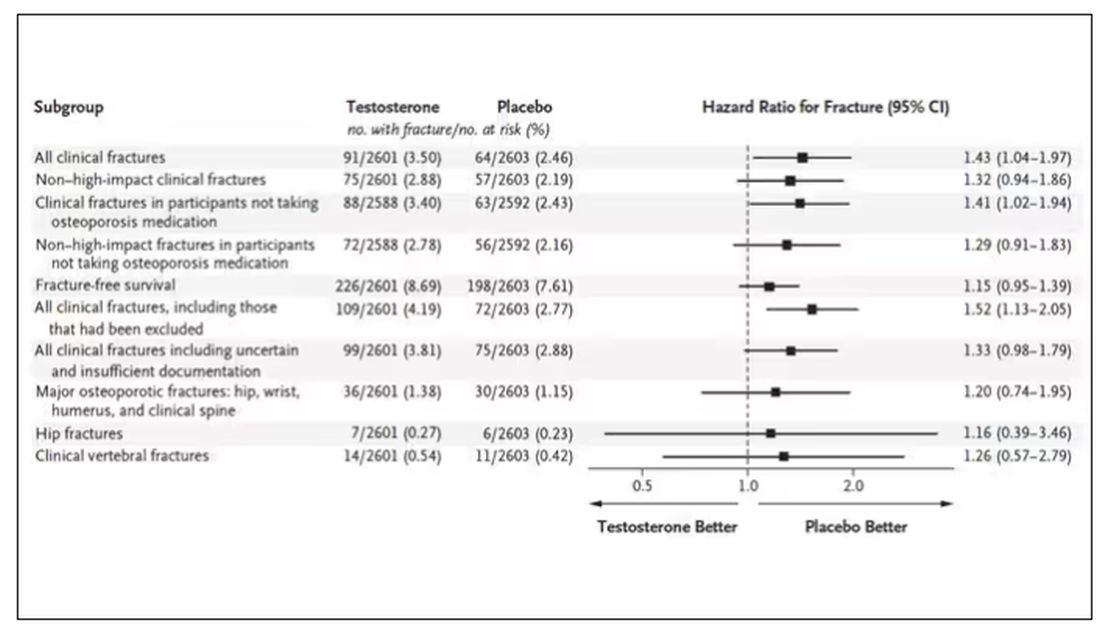
How does a drug that increases bone mineral density and bone strength increase the risk for fracture?
Well, one clue — and this was pointed out in a nice editorial by Matthis Grossman and Bradley Anawalt — is that the increased risk for fracture occurs quite soon after starting treatment, which is not consistent with direct bone effects. Rather, this might represent behavioral differences. Testosterone supplementation seems to increase energy levels; might it lead men to engage in activities that put them at higher risk for fracture?
Regardless of the cause, this adds to our knowledge about the rather complex mix of risks and benefits of testosterone supplementation and probably puts a bit more weight on the risks side. The truth is that testosterone levels do decline with age, as do many things, and it may not be appropriate to try to fight against that in all people. It’s worth noting that all of these studies use low levels of total serum testosterone as an entry criterion. But total testosterone is not what your body “sees.” It sees free testosterone, the portion not bound to sex hormone–binding globulin. And that binding protein is affected by lots of stuff — diabetes and obesity lower it, for example — making total testosterone levels seem low when free testosterone might be just fine.
In other words, testosterone supplementation is probably not terrible, but it is definitely not the cure for aging. In situations like this, we need better data to guide exactly who will benefit from the therapy and who will only be exposed to the risks.
Dr. Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Conn. He has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
Smoking Associated With Increased Risk for Hair Loss Among Men
, according to a new study.
In addition, the odds of developing AGA are higher among those who smoke at least 10 cigarettes per day than among those who smoke less, the study authors found.
“Men who smoke are more likely to develop and experience progression of male pattern hair loss,” lead author Aditya Gupta, MD, PhD, professor of medicine at the University of Toronto, Toronto, and director of clinical research at Mediprobe Research Inc., London, Ontario, Canada, told this news organization.
“Our patients with male pattern baldness need to be educated about the negative effects of smoking, given that this condition can have a profound negative psychological impact on those who suffer from it,” he said.
The study was published online in the Journal of Cosmetic Dermatology.
Analyzing Smoking’s Effects
Smoking generally has been accepted as a risk factor for the development and progression of AGA or the most common form of hair loss. The research evidence on this association has been inconsistent, however, the authors wrote.
The investigators conducted a review and meta-analysis of eight observational studies to understand the links between smoking and AGA. Ever-smokers were defined as current and former smokers.
Overall, based on six studies, men who have ever smoked are 1.8 times more likely (P < .05) to develop AGA.
Based on two studies, men who smoke 10 or more cigarettes daily are about twice as likely (P < .05) to develop AGA than those who smoke up to 10 cigarettes per day.
Based on four studies, ever smoking is associated with 1.3 times higher odds of AGA progressing from mild (ie, Norwood-Hamilton stages I-III) to more severe (stages IV-VII) than among those who have never smoked.
Based on two studies, there’s no association between AGA progression and smoking intensity (as defined as smoking up to 20 cigarettes daily vs smoking 20 or more cigarettes per day).
“Though our pooled analysis found no significant association between smoking intensity and severity of male AGA, a positive correlation may exist and be detected through an analysis that is statistically better powered,” said Dr. Gupta.
The investigators noted the limitations of their analysis, such as its reliance on observational studies and its lack of data about nicotine levels, smoking intensity, and smoking cessation among study participants.
Additional studies are needed to better understand the links between smoking and hair loss, said Dr. Gupta, as well as the effects of smoking cessation.
Improving Practice and Research
Commenting on the findings for this news organization, Arash Babadjouni, MD, a dermatologist at Midwestern University, Glendale, Arizona, said, “Smoking is not only a preventable cause of significant systemic disease but also affects the follicular growth cycle and fiber pigmentation. The prevalence of hair loss and premature hair graying is higher in smokers than nonsmokers.”
Dr. Babadjouni, who wasn’t involved with this study, has researched the associations between smoking and hair loss and premature hair graying.
“Evidence of this association can be used to clinically promote smoking cessation and emphasize the consequences of smoking on hair,” he said. “Smoking status should be assessed in patients who are presenting to their dermatologist and physicians alike for evaluation of alopecia and premature hair graying.”
The study was conducted without outside funding, and the authors declared no conflicts of interest. Dr. Babadjouni reported no relevant disclosures.
A version of this article appeared on Medscape.com.
, according to a new study.
In addition, the odds of developing AGA are higher among those who smoke at least 10 cigarettes per day than among those who smoke less, the study authors found.
“Men who smoke are more likely to develop and experience progression of male pattern hair loss,” lead author Aditya Gupta, MD, PhD, professor of medicine at the University of Toronto, Toronto, and director of clinical research at Mediprobe Research Inc., London, Ontario, Canada, told this news organization.
“Our patients with male pattern baldness need to be educated about the negative effects of smoking, given that this condition can have a profound negative psychological impact on those who suffer from it,” he said.
The study was published online in the Journal of Cosmetic Dermatology.
Analyzing Smoking’s Effects
Smoking generally has been accepted as a risk factor for the development and progression of AGA or the most common form of hair loss. The research evidence on this association has been inconsistent, however, the authors wrote.
The investigators conducted a review and meta-analysis of eight observational studies to understand the links between smoking and AGA. Ever-smokers were defined as current and former smokers.
Overall, based on six studies, men who have ever smoked are 1.8 times more likely (P < .05) to develop AGA.
Based on two studies, men who smoke 10 or more cigarettes daily are about twice as likely (P < .05) to develop AGA than those who smoke up to 10 cigarettes per day.
Based on four studies, ever smoking is associated with 1.3 times higher odds of AGA progressing from mild (ie, Norwood-Hamilton stages I-III) to more severe (stages IV-VII) than among those who have never smoked.
Based on two studies, there’s no association between AGA progression and smoking intensity (as defined as smoking up to 20 cigarettes daily vs smoking 20 or more cigarettes per day).
“Though our pooled analysis found no significant association between smoking intensity and severity of male AGA, a positive correlation may exist and be detected through an analysis that is statistically better powered,” said Dr. Gupta.
The investigators noted the limitations of their analysis, such as its reliance on observational studies and its lack of data about nicotine levels, smoking intensity, and smoking cessation among study participants.
Additional studies are needed to better understand the links between smoking and hair loss, said Dr. Gupta, as well as the effects of smoking cessation.
Improving Practice and Research
Commenting on the findings for this news organization, Arash Babadjouni, MD, a dermatologist at Midwestern University, Glendale, Arizona, said, “Smoking is not only a preventable cause of significant systemic disease but also affects the follicular growth cycle and fiber pigmentation. The prevalence of hair loss and premature hair graying is higher in smokers than nonsmokers.”
Dr. Babadjouni, who wasn’t involved with this study, has researched the associations between smoking and hair loss and premature hair graying.
“Evidence of this association can be used to clinically promote smoking cessation and emphasize the consequences of smoking on hair,” he said. “Smoking status should be assessed in patients who are presenting to their dermatologist and physicians alike for evaluation of alopecia and premature hair graying.”
The study was conducted without outside funding, and the authors declared no conflicts of interest. Dr. Babadjouni reported no relevant disclosures.
A version of this article appeared on Medscape.com.
, according to a new study.
In addition, the odds of developing AGA are higher among those who smoke at least 10 cigarettes per day than among those who smoke less, the study authors found.
“Men who smoke are more likely to develop and experience progression of male pattern hair loss,” lead author Aditya Gupta, MD, PhD, professor of medicine at the University of Toronto, Toronto, and director of clinical research at Mediprobe Research Inc., London, Ontario, Canada, told this news organization.
“Our patients with male pattern baldness need to be educated about the negative effects of smoking, given that this condition can have a profound negative psychological impact on those who suffer from it,” he said.
The study was published online in the Journal of Cosmetic Dermatology.
Analyzing Smoking’s Effects
Smoking generally has been accepted as a risk factor for the development and progression of AGA or the most common form of hair loss. The research evidence on this association has been inconsistent, however, the authors wrote.
The investigators conducted a review and meta-analysis of eight observational studies to understand the links between smoking and AGA. Ever-smokers were defined as current and former smokers.
Overall, based on six studies, men who have ever smoked are 1.8 times more likely (P < .05) to develop AGA.
Based on two studies, men who smoke 10 or more cigarettes daily are about twice as likely (P < .05) to develop AGA than those who smoke up to 10 cigarettes per day.
Based on four studies, ever smoking is associated with 1.3 times higher odds of AGA progressing from mild (ie, Norwood-Hamilton stages I-III) to more severe (stages IV-VII) than among those who have never smoked.
Based on two studies, there’s no association between AGA progression and smoking intensity (as defined as smoking up to 20 cigarettes daily vs smoking 20 or more cigarettes per day).
“Though our pooled analysis found no significant association between smoking intensity and severity of male AGA, a positive correlation may exist and be detected through an analysis that is statistically better powered,” said Dr. Gupta.
The investigators noted the limitations of their analysis, such as its reliance on observational studies and its lack of data about nicotine levels, smoking intensity, and smoking cessation among study participants.
Additional studies are needed to better understand the links between smoking and hair loss, said Dr. Gupta, as well as the effects of smoking cessation.
Improving Practice and Research
Commenting on the findings for this news organization, Arash Babadjouni, MD, a dermatologist at Midwestern University, Glendale, Arizona, said, “Smoking is not only a preventable cause of significant systemic disease but also affects the follicular growth cycle and fiber pigmentation. The prevalence of hair loss and premature hair graying is higher in smokers than nonsmokers.”
Dr. Babadjouni, who wasn’t involved with this study, has researched the associations between smoking and hair loss and premature hair graying.
“Evidence of this association can be used to clinically promote smoking cessation and emphasize the consequences of smoking on hair,” he said. “Smoking status should be assessed in patients who are presenting to their dermatologist and physicians alike for evaluation of alopecia and premature hair graying.”
The study was conducted without outside funding, and the authors declared no conflicts of interest. Dr. Babadjouni reported no relevant disclosures.
A version of this article appeared on Medscape.com.
FROM THE JOURNAL OF COSMETIC DERMATOLOGY





